- 1School of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran
- 2Social Determinants of Health Research Center, Zanjan University of Medical Sciences, Zanjan, Iran
- 3Department of Clinical Psychology, School of Medicine, Dr Beheshti Hospital, Zanjan University of Medical Sciences, Zanjan, Iran
Background: Women with a history of preeclampsia frequently have a lower level of physical well-being and emotional problems.
Objective: This study aimed to determine the effect of integrating religiosity and spirituality into postpartum care can improve the quality of life in women with preeclampsia.
Methods: This study was a randomized controlled clinical trial conducted on 40 women with preeclampsia. All eligible participants were allocated to two control and intervention groups using a random blocking method. Data were collected using Mother-Generated Index (MGI) in pre-intervention and 6 weeks later and analyzed using descriptive statistics, Chi-square test, and independent t-tests. The significance level was p < 0.05.
Results: The mean, Standard deviation (SD) of the total score of MGI before intervention in the intervention group was 5.35 (1.09) which increased to 8.00 (0.50) 6 weeks after intervention. In the control group, the pre-test score of MGI was 5.81 (0.97) which increased to 6.69 (1.37) after 6 weeks of follow-up. The difference between the two groups was statistically significant after the intervention based on an independent t-test (p = 0.001).
The mean (SD) of five subscales included Feelings toward herself, Feelings toward the child, Feelings toward her husband and others, Feelings toward sex, and Physical health status after intervention in the intervention group statistically significantly increased compared to the control group (p < 0.011).
Conclusion: The integration of spiritual counseling with the educational content of postpartum care had a positive impact on improving the postpartum QoL of women with preeclampsia. For better conclusions, a study with a large sample size needed to be conducted in the future.
Clinical Trial Registration: https://en.irct.ir/user/trial/50832/view, identifier IRCT20150731023423N16.
Introduction
Preeclampsia is one of the hypertensive disorders in pregnancy that affects 4.6% of pregnancies worldwide (1). Also, it is responsible for 10% of preterm births and 3% of perinatal mortality (2). Women with a history of preeclampsia frequently have a lower level of physical well-being (3) and emotional problems such as Post-traumatic stress disorder (PTSD) symptoms compared to women who have had uncomplicated pregnancies, especially if the disease occurs in the early stage of pregnancy (4). Taking care of the mother’s health during pregnancy and preventing her worries, anxieties, and psychological pressures will reduce the severe impairment during this period (5).
According to the World Health Organization definition, quality of life (QoL) is an individual’s understanding of their position in life, goals, expectations, relationships, needs, and beliefs which are affected by one’s cultural context and value systems (6). Spirituality is a significant dimension of quality of life that empowers people to deal emotionally with aspects of illness, life concerns, beliefs, and spiritual values (7). By targeting individual beliefs, people may be able to better handle negative situations and gain greater control than they have at present (8).
Spirituality is distinct from religiosity and is defined as the way people seek and express meaning and purpose in life, and experience their relationship with others, nature, and sacred things. This definition serves as the foundation for the spiritual care approach (9).
Positive effects of spiritual care through the improvement of meaningful communication and positive thinking in controlling postpartum stress disorder among preeclamptic women have been reported (10). Also, spiritual counseling combined with other counseling approaches was found to be significantly effective in reducing anxiety and improving the quality of life of hypertensive patients (11). However, there is a knowledge gap regarding the effectiveness of this approach in improving the quality of life after childbirth in women with preeclampsia. It appears that “spiritual care, “with its broad range of dimensions, as one of the fundamental aspects of holistic treatment in mothers with preeclampsia, could be somewhat effective in controlling their problems and improving their patients’ quality of life. Consequently, the present study examined the effect of integrating religiosity and spirituality into postpartum care on the quality of life in women with preeclampsia.
Hypothesis
Integrating religiosity and spirituality into postpartum care is effective in improving the quality of life among women with preeclampsia compared to the control group.
Materials and methods
Study design
This study was a randomized controlled trial that was conducted on 40 women with preeclampsia who were admitted to the postpartum ward at Ayatollah Mousavi Teaching Hospital in Zanajn a city in northwest Iran from October 2020 to May 2021.
Participants’ inclusion and exclusion criteria
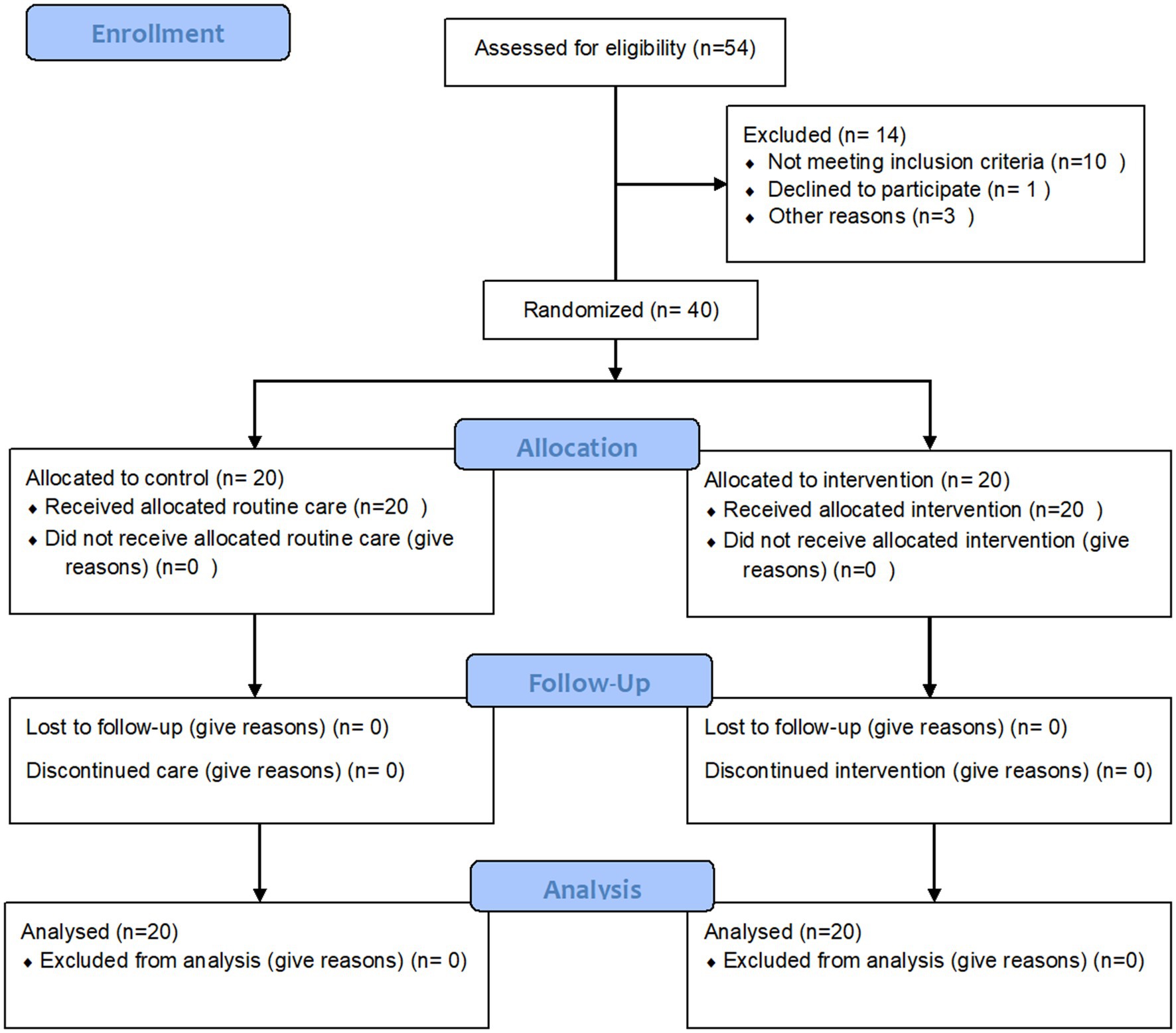
Among 54 preeclamptic women who were evaluated by the researcher, 40 women met the inclusion criteria and 14 women were excluded before being randomly allocated to groups. Preeclampsia was diagnosed based on the International Society for the Study of Hypertension in Pregnancy (ISSHP) guidelines (12). After the interventions, there was no attrition in our study. The process of sampling showed in Figure 1.
Inclusion criteria included hospitalization with a diagnosis of preeclampsia less than 5 days, willingness to participate in the study, having a delivery with a singleton pregnancy, having a minimum of elementary education, getting a score less than 22 based on the General Health Questionnaire (GHQ-28), and mild to moderate level of Daily Spiritual Experiences Scale (DSES). Exclusion criteria included having a history of chronic diseases, having a known mental illness, use of any psychiatric medicine, a known neonatal abnormality, intrauterine fetal death, having postpartum complications (such as bleeding and infection), no phone number for calling, and changing the treatment process (for example, transfer to the intensive care unit). The sample size was calculated based on the quality-of-life variable reported by Kalhornia’s study (11). Accordingly, the mean (SD) of quality of life was , in intervention group, and , in control group, respectively. With considering α = 0.05, Power = 95%, and a 15% drop, the sample size was calculated as 20 people in each group.
Sampling
The researcher referred to the postpartum ward of Ayatollah Mousavi Teaching Hospital in Zanjan and after obtaining written consent to participate in the study from all participants, the inclusion and exclusion criteria were checked and eligible women completed the demographic questions and postnatal quality of life Questionnaire (Mother-Generated Index).
Randomization
All eligible participants were allocated to two control and intervention groups using a random blocking method with block sizes of four. Randomization was done by a person who was not directly involved in our study using a research Randomizer. It is a free resource and a quick way for researchers to generate random numbers or assign participants to control and intervention groups. The generated numbers were placed in an opaque envelope and then sequentially numbered. When the participants entered the study, the assigned group was identified by opening each envelope.
Routine care
All women with preeclampsia were admitted to the postpartum ward at Ayatollah Mousavi Teaching Hospital in Zanajn, in addition, to controlling bleeding, prescribing medicine, and recording vital signs, received an educational package that included personal hygiene, breastfeeding, and warning signs of maternal and neonatal complications. Women are not routinely educated on the content of spirituality postpartum.
Intervention
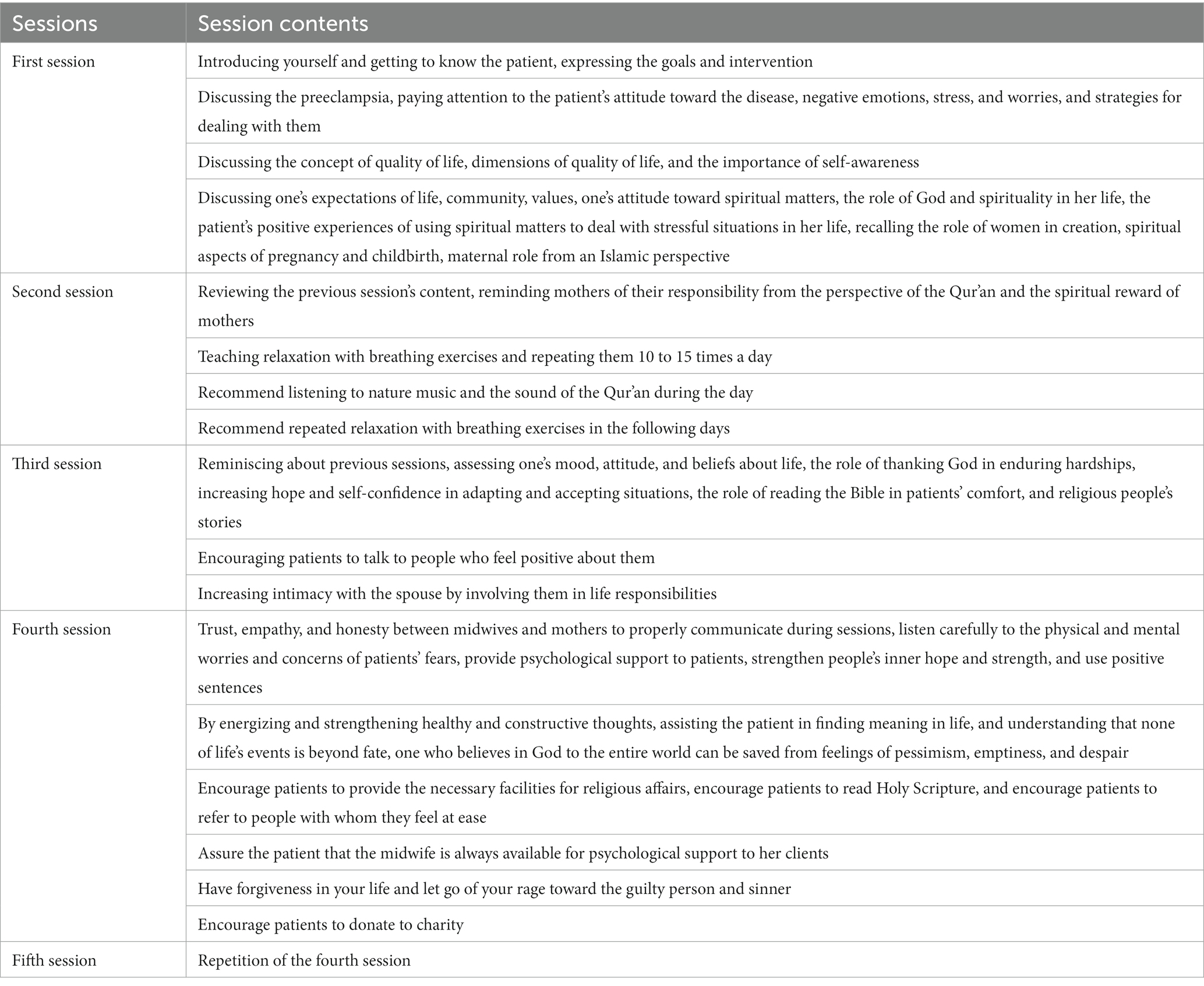
In this study, the intervention group received counseling individually in five sessions with spiritual content based on Richards and Bergin’s protocol by the first author. A spiritual content program was developed by the researchers and a religious counselor. In the counseling group, the intervention was started 12 h after delivery and stabilization of the mother’s general condition. Three sessions were held in the postpartum ward during the hospitalization period in a place with adequate space to observe social distancing and other health protocols to prevent Covid-19 diseases such as proper air conditioning and using a face mask. The next two sessions were held weekly after discharge by telephone counseling. Each counseling session lasted 45–60 min.
Table 1 shows the content of the intervention separately by session. The control group received routine care.
Data collection tools
The outcome of the study was to determine the postnatal quality of life.
Data collection tools included demographic questions, postnatal quality of life Questionnaire (Mother-Generated Index) that were completed in two-stage (pre-intervention and 6 weeks after the last session of counseling).
The questionnaire included education, spouse education, family income, insurance status, job, spouse job, residence, homeownership, and parity.
Postnatal quality of life questionnaire: mother-generated index
The MGI was designed by Symon et al. It is a subjective tool to measure the postnatal quality of life and contains 30 questions in eight areas. The dimensions of the questionnaire include the mother’s feelings toward herself (6 questions), feelings toward the child (3 questions), feelings toward her husband and other family members (8 questions), feelings toward sex with a spouse (3 questions), physical health status (7 questions), Satisfaction with childbirth (one question), the status of the economics associated with childbirth (one question), and the re-selection of the method of childbirth in subsequent pregnancies (one question). The MGI score was calculated by weighting the means of the values on visual analog scales between one and 10. A high score in any area indicates a better situation in terms of quality of life. The face, criterion, and construct validity of the questionnaire were at an acceptable level (13). Psychometric properties of the Persian version of the questionnaire were tested by Khabiri, et al. In their study, the face, criterion, and construct validity of the questionnaire were at an acceptable level (14). The reliability of the questionnaire in the present study was confirmed by calculating Cronbach’s alpha coefficient of 0.78.
Data analysis
Data were analyzed using SPSS 16. Descriptive statistics were used to describe the demographic information. The Chi-square test was used to compare demographic characteristics between the two groups. Kolmogorov–Smirnov test showed that MGI scores have a normal distribution. Therefore, to compare the scores of MGI between groups independent t-tests were used. The significance level was p < 0.05.
Results
Among 54 women evaluated by the researcher, the data of 40 women met the eligibility criteria for analysis.
Demographic characteristic
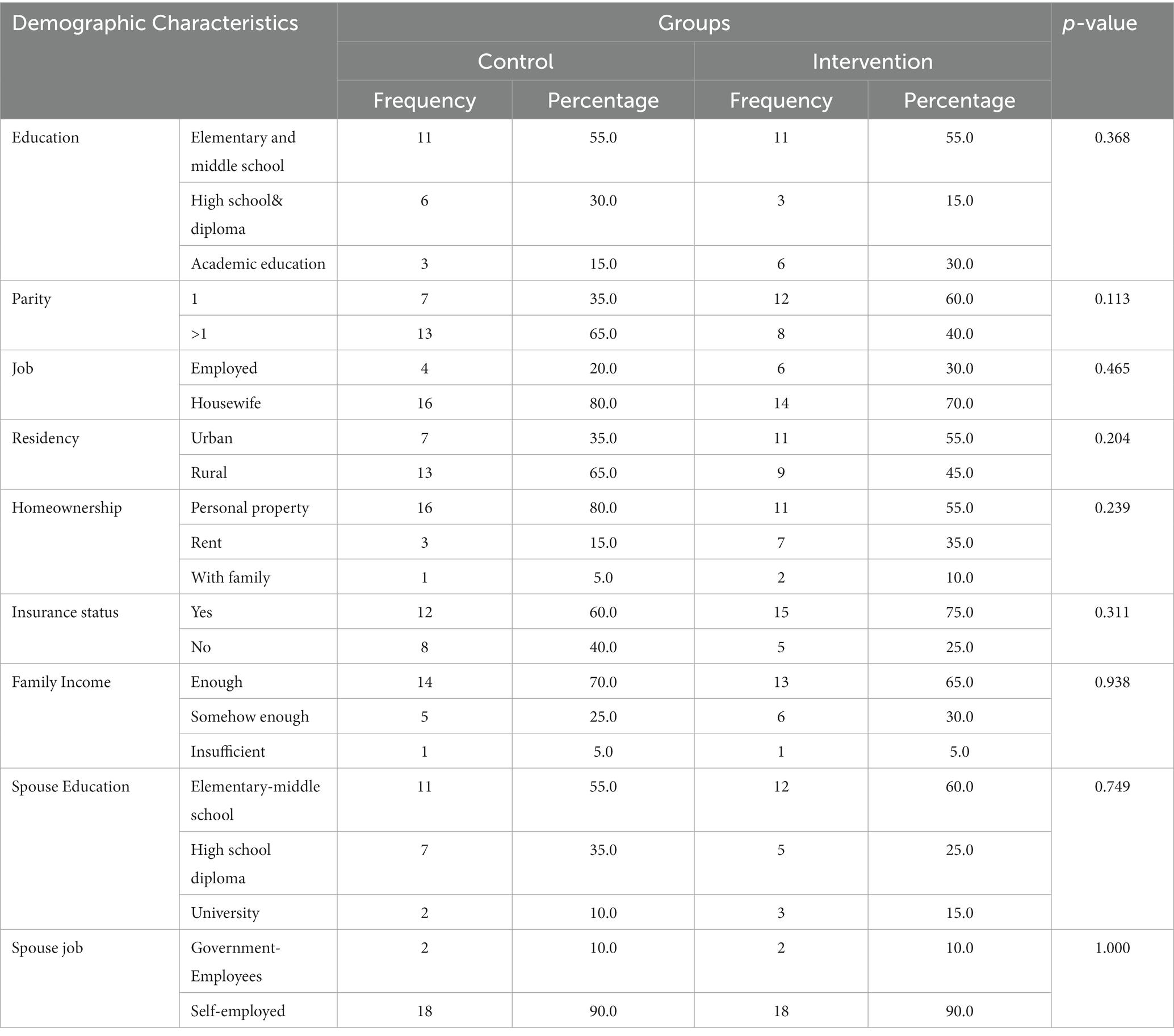
In both groups, the most of participants have Elementary & middle school level education (55%). Regarding the parity, the most of participants in the control group had >1 parity (65%), and in the intervention group was equal to one parity (60%). Regarding the family-income and insurance, and job status, the most of participants in both groups were at enough level, had insurance, and had jobs were housewives. Also, personal property was the most common form of homeownership in both groups. The residence of most people was rural in the intervention group (55%) and urban (65%) in the control group. Regarding their spouses’ jobs and education, most of them in both groups have Elementary and middle school level and self-employed jobs. The comparison of demographic characteristics using the Chi-square showed that there is no significant difference between the two groups (Table 2).
The mother-generated index
The mean, Standard deviation (SD) of the total score of MGI before intervention in the intervention group was 5.35 (1.09) which increased to 8.00 (0.50) 6 weeks after intervention. In the control group, the pre-test score was 5.81 (0.97) which increased to 6.69 (1.37) after 6 weeks of follow-up. The difference between the two groups was statistically significant after 6 weeks of follow-up based on an independent t-test (p = 0.001).
The mean (SD) of five subscales included Feelings toward herself, Feelings toward the child, Feelings toward her husband and others, Feelings toward sex, and Physical health status after intervention in the intervention group statistically significantly increased compared to the control group (p < 0.011). But three subscales included satisfaction with childbirth, the economic difficulty, and the re-selection of the method of childbirth after intervention based on an independent t-test was not significant (p > 0.05; Table 3).
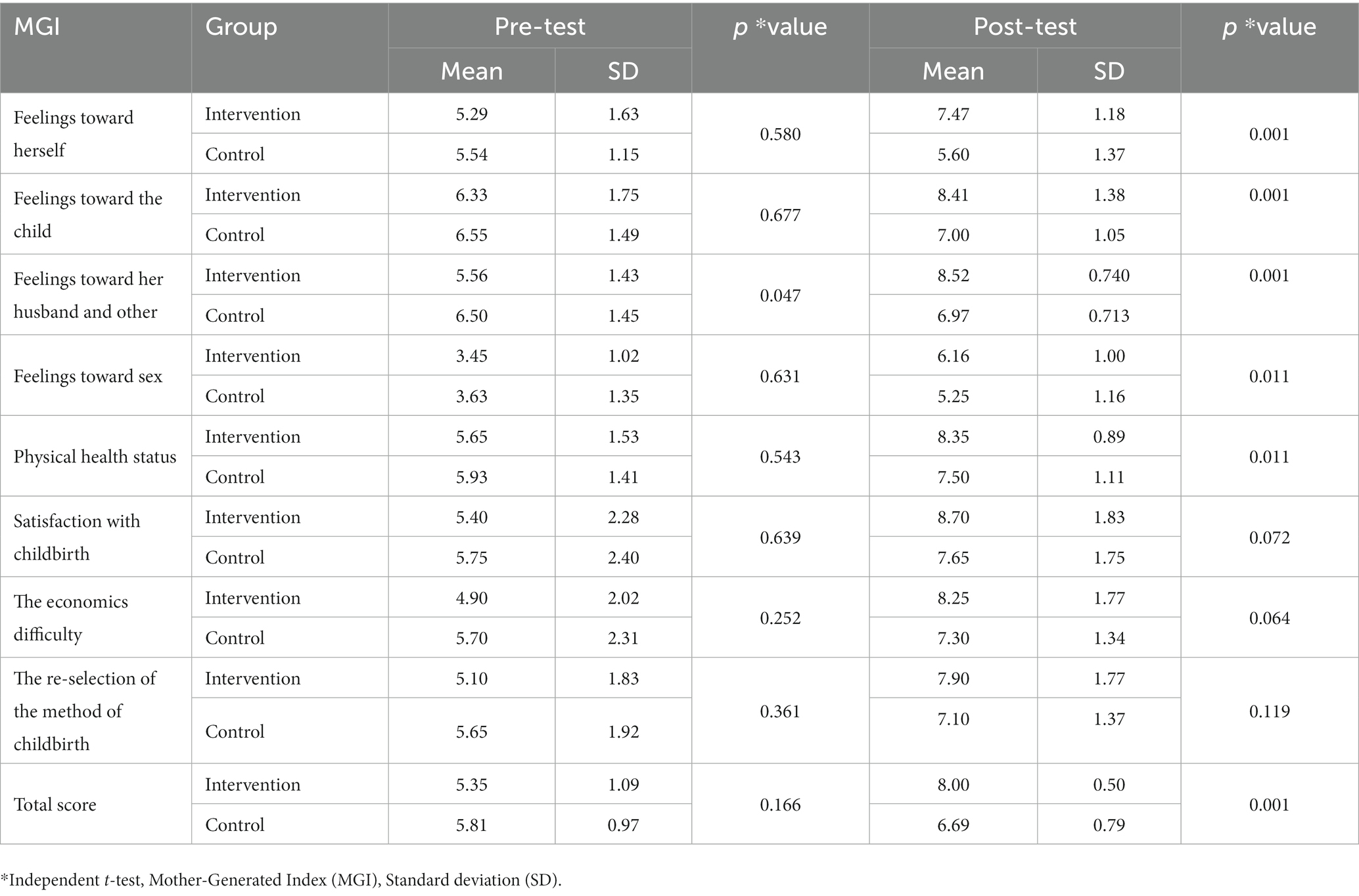
Table 3. The comparison of MGI scores between two groups in pre-intervention and 6 weeks after intervention.
Discussion
The current study was conducted to examine the effect of integrating spirituality into postpartum care on improving the quality of life in women with preeclampsia. Our result revealed that the intervention can improve the total score of quality of life and its subscales compared to the control group. According to our knowledge, this is the first study to assess the effect of integrating spirituality into postpartum care on the quality of life among women with preeclampsia. However, our results are consistent with studies that were conducted on other high-risk pregnancy samples. In this regard, the result of two similar studies showed that the implementation of Islamic- spiritual psychotherapy could be improved the quality of life of infertile women (15, 16). Also, integrating cognitive-behavioral therapy with Islamic spirituality instructions had an effective impact on the quality of life of pregnant women (17). Beigi et al. showed that the implementation of group spiritual therapy was effective in reducing anxiety and increasing the quality-of-life score in women with gestational diabetes (18). Also, similar efficacy has been reported in another study conducted by Niaz Azari et al. in women with gestational diabetes (19). Constituency in results emphasized that the spiritual-based approach can be used to improve the quality of life of women in the antenatal and postpartum periods.
The positive effects of spiritual counseling on improving blood pressure, life satisfaction, and quality of life of non-pregnant hypertensive patients have also been emphasized in some studies (11, 20). Religion and spirituality can increase QoL by changing people’s attitudes, increasing their sense of responsibility toward themselves and others, promoting the search for meaning in life, and having a greater sense of happiness and self-esteem. Spiritual experience is a unique experience that entails understanding the meaning of life, having positive experiences in life, and feeling happy, and satisfied with life (21).
In the current study, intervention can improve the sense of women toward themselves, child, their husbands, and others. Participants had positive feelings toward sex and Physical health status after the intervention. While, satisfaction with childbirth, the economic difficulty, and the re-selection of the delivery method have not major changes. Similar to our result, the positive effect of integration of spirituality in antenatal care can improve the general health perceptions and physical and emotional role function of healthy pregnant women (22). On the contrary Dehestani et al. revealed that spiritual health had a positive effect on preventing labor pains and childbirth satisfaction in women (23). Furthermore, a negative correlation between spiritual intelligence and fear of giving birth was reported (24). The reason for inconsistent results regarding satisfaction with childbirth could be that in our study the intervention was performed after delivery and in mothers with high-risk pregnancies.
Strength of study
All the principles of control trial studies were observed in this study and we do not have a loss of following in participants. Data collection tools were standard and psychometric properties of the Persian form of the questionnaires have been evaluated based on Iranian culture.
Limitation
The sample size was small and the follow-up period was short. Also, samples were limited to the participants of the Shiite religion, which can affect the generalizability of findings. It is suggested that a similar study should be performed on other ethnicities and cultures in future studies. Furthermore, for better conclusions about the long-term effects of the spiritual-based intervention on postpartum QoL, studies with a long follow-up period and large sample size are needed to be conducted in the future.
Highlighted
Preeclampsia can affect the physical and emotional well-being of women.
Spiritual counseling can improve the postpartum QoL of women with preeclampsia compared to the control group.
Conclusion
Preliminary results show spiritual counseling had a positive impact on improving the postpartum QoL of women with preeclampsia. For better conclusions, a study with a large sample size needed to be conducted in the future.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary materials, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Zanjan University of Medical Sciences, Iran, with the approval number IR.ZUMS.REC.1398.376. The patients/participants provided their written informed consent to participate in this study.
Author contributions
RR undertaken the conception, design of the study, and data collection process. AM was the supervisor who also contributed to the design of the study and reporting of the results, supervised analysis, interpretation, and reporting. SZ as the second supervisor contributed to all the stages of the study. All authors contributed to the drafting and revising of the article and agreed with the final version of the manuscript to be submitted to the journal, they also meet the criteria of authorship.
Funding
This study was part of MSc thesis and funded by the Research Deputy of Zanjan University of Medical Sciences, Iran, with the approval number (Code “A-11-344-13”).
Acknowledgments
The authors would like to thank the Social Determinants of Health Research Center, Zanjan University of Medical Sciences, and the vice-chancellor of research and technology for their financial support to carry out the study (The code “A-11-344-13”). We would like to thank the Clinical Research Development Center of Ayatollah Mousavi Hospital, Zanjan University of Medical Sciences for their collaboration and the women for their participation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PTSD, Post-traumatic stress disorder; SD, Standard deviation; MGI, Mother-Generated Index; QoL, The Quality of Life; COVID-19, Coronavirus disease; GHQ-28, The General Health Questionnaire; DSES, Daily Spiritual Experiences Scale; ISSHP, Hypertension in Pregnancy.
References
1. Abalos, E, Cuesta, C, Grosso, AL, Chou, D, and Say, L. Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol. (2013) 170:1–7. doi: 10.1016/j.ejogrb.2013.05.005
2. Bilano, VL, Ota, E, Ganchimeg, T, Mori, R, and Souza, JP. Risk factors of pre-eclampsia/eclampsia and its adverse outcomes in low-and middle-income countries: a WHO secondary analysis. PLoS One. (2014) 9:e91198. doi: 10.1371/journal.pone.0091198
3. Roes, EM, Raijmakers, MT, Schoonenberg, M, Wanner, N, Peters, WH, and Steegers, EA. Physical well-being in women with a history of severe preeclampsia. J Matern Fetal Neonatal Med. (2005) 18:39–45. doi: 10.1080/14767050500127740
4. Roberts, L, Davis, GK, and Homer, CS. Depression, anxiety, and post-traumatic stress disorder following a hypertensive disorder of pregnancy: a narrative literature review. Front Cardiovasc Med. (2019) 6:147. doi: 10.3389/fcvm.2019.00147
5. Golshani, F, Gholmohammad Nejad, GR, and Aghdasi, AN. The effectiveness of teaching life skills during pregnancy on pregnant mothers’ mental health. J Instr Eval. (2014) 7:89–101.
6. Group W. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. (1995) 41:1403–9. doi: 10.1016/0277-9536(95)00112-K
7. Sotodeh-Asl, N, Neshat-Dust, H, Kalantari, M, Talebi, H, and Khosravi, A. Comparison of effectiveness of two methods of hope therapy and drug therapy on the quality of life in the patients with essential hypertension. J Clin Psychol. (2010) 2:1–5.
8. Yilmaz, CK, and Kara, FŞ. The effect of spiritual well-being on adaptation to chronic illness among people with chronic illnesses. Perspect Psychiatr Care. (2021) 57:318–25. doi: 10.1111/ppc.12566
9. Richards, PS, and Bergin, AE. Religious and spiritual assessment. Richards, PS, and Bergin, AE. A spiritual strategy for counseling and psychotherapy. Washington, DC: American Psychological Association. (2005).
10. Kamali, Z, Tafazoli, M, Ebrahimi, M, Hosseini, M, Saki, A, Fayyazi-Bordbar, MR, et al. Effect of spiritual care education on postpartum stress disorder in women with preeclampsia. J Educ Health Promot. (2018):7. doi: 10.4103/jehp.jehp_170_17
11. Kalhornia-Golkar, M, Banijamali, S, Bahrami, H, Hatami, H, and Ahadi, H. Effectiveness of mixed therapy of stress management training and spiritual therapy on level of blood pressure, anxiety and quality of life of high blood pressure patients. J Clin Psychol. (2014) 6:1–11.
12. Tranquilli, A, Dekker, G, Magee, L, Roberts, J, Sibai, B, Steyn, W, et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens. (2014) 4:97–104. doi: 10.1016/j.preghy.2014.02.001
13. Symon, A, McGreavey, J, and Picken, C. Postnatal quality of life assessment: validation of the mother-generated index. BJOG Int J Obstet Gynaecol. (2003) 110:865–8. doi: 10.1111/j.1471-0528.2003.02030.x
14. Khabiri, R, Rashidian, A, Montazeri, A, Symon, A, Foroushani, AR, Arab, M, et al. Validation of the mother-generated index in Iran: a specific postnatal quality-of-life instrument. Int J Prev Med. (2013) 4:1371–9.
15. Moazedi, K, Porzoor, P, Pirani, Z, Adl, H, and Ahmadi, H. The effectiveness of Islamic teaching based religious-spiritual psychotherapy on quality of life, in infertile women. J Health. (2018) 9:589–98.
16. Pirani, Z. The effectiveness of Islamic teaching based religious-spiritual psychotherapy on quality of life, in infertile women. Iran: University of Mohaghegh Ardabili (2019).
17. Zamani, SN, Zarei, E, Alizadeh, KH, and Naami, AZ. Effectiveness of combination of cognitive-behavioral therapy and resilience training based on Islamic spirituality and cognitive flexibility on postpartum depression, fear of labor pain and quality of life. Hormozgan Med J. (2019) 22:e86489. doi: 10.5812/hmj.86489
18. Beigi, A, Habibi, S, Rezaei Hesar, H, Niasty, R, Shams Ali, Z, Ashoori, J, et al. Effect of spiritual training on decreased anxiety and increased quality of life of women with gestational diabetesin the assement of nursing and modern care. J Diabetes Nurs. (2016) 4:19–29.
19. Niaz Azari, M, Abdollahi, M, Zabihi Hesari, NK, and Ashoori, J. Effect of spiritual group therapy on anxiety and quality of life among gestational diabetic females. J Relig Health. (2017) 5:11–20.
20. Moeini, M. The effect of an Islamic spiritual program on life satisfaction of elderly patients with hypertension. J Clin Nurs Midwifery. (2016) 4:93–103.
21. Lent, RW. Toward a unifying theoretical and practical perspective on well-being and psychosocial adjustment. J Couns Psychol. (2004) 51:482–509. doi: 10.1037/0022-0167.51.4.482
22. MonfaredKashki, M, Maleki, A, and Amini, K. The effect of integrating midwifery counseling with a spiritual content on improving the antenatal quality of life: a randomized controlled trials. J Mother Child. (2021) 26:18–26. doi: 10.34763/jmotherandchild.20222601.d-22-00003
23. Dehestani, H, Tayebi, N, Moshfeghy, Z, and Akbarzadeh, M. The role of spiritual health experience with intensity and duration of labor pain while childbearing and postpartum. Curr Womens Health Rev. (2022) 18:77–84. doi: 10.2174/1573404817666210310165046
Keywords: women’s health, preeclampsia, spirituality, quality of life, counseling
Citation: Rasouli R, Maleki A and Zenoozian S (2023) Can integrating religiosity and spirituality into postpartum care improve the quality of life in women with preeclampsia. Front. Psychiatry. 14:985428. doi: 10.3389/fpsyt.2023.985428
Edited by:
Suraj Bahadur Thapa, University of Oslo, NorwayReviewed by:
Andrés Alexis Ramírez Coronel, Catholic University of Cuenca, EcuadorRishav Koirala, University of Oslo, Norway
Marius Lahti-Pulkkinen, University of Helsinki, Finland
Copyright © 2023 Rasouli, Maleki and Zenoozian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Azam Maleki, bWFsZWtpYUB6dW1zLmFjLmly; bWFsZWtpYTQxQHlhaG9vLmNvbQ==
†ORCID: Azam Maleki https://orcid.org/0000-0001-7888-1985
Saeedeh Zenoozian https://orcid.org/0000-0002-5469-9545
 Robab Rasouli1
Robab Rasouli1 Azam Maleki
Azam Maleki