- 13rd Department of Psychiatry, School of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 2Society for Neurosciences and Rehabilitation (E.N.A.), Thessaloniki, Greece
- 3Consultant, NHS, Thessaloniki, Greece
Bipolar disorder (BD) is such a complex mental disorder, that even the development of true, reliable, and valid treatment guidelines seems to be a goal almost impossible to achieve. The challenges include the complexity and uniqueness of the clinical picture and the therapeutical options available, special issues including gender, pregnancy, and the different views of therapists and patients. An additional issue is the method for the development of the guidelines, with systematic reviews of the hard evidence to constitute the most recent trend. The grading of the literature findings could be crucial for the whole process, as it is often ‘contaminated’ by expert opinion. Unfortunately, in the literature, BD is treated as a fragmented condition and each fragment is studied separately as if it were independent. This, in combination with incomplete reporting of the findings, makes the synthesis of the landscape almost impossible and the development of a comprehensive single algorithm for the continuous treatment of BD, extremely difficult. Overall, developing treatment guidelines for BD constitutes a great challenge. This task demands an exhaustive review of the existing literature, searching for unpublished data and digging deep into them to comprehend their nature. It also needs to manage to synthesize the fragmented research picture that refers to isolated faces of the disorder, into a comprehensive network of decision-making that will incorporate the knowledge of the past with decisions for the present by having the mind in the future (the three-fingers rule).
1 Introduction
Bipolar disorder (BD) is an incredibly complex condition—so much so that even among mental health disorders, its intricacies stand out. A wide range of factors contribute to its development and course, including biological, psychological, social, and even environmental influences (1–3). Given this complexity, precise treatment guidelines are crucial for clinicians. Over the past few decades, these guidelines have become an increasingly vital part of modern medicine. This is important, especially as the sheer volume of research—often intricate and sometimes contradictory—makes it harder to translate findings into everyday clinical practice.
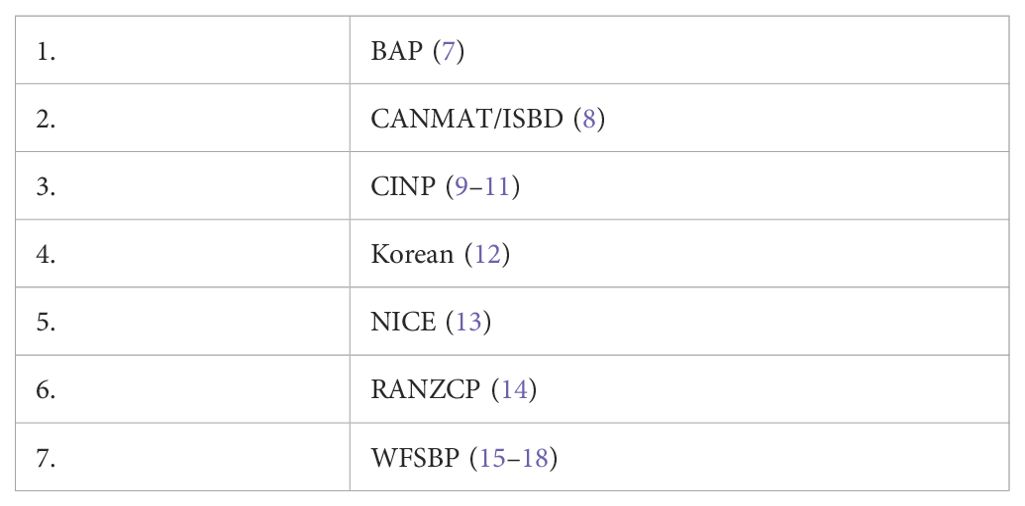
These guidelines serve multiple purposes: they help clinicians and policymakers make informed decisions about patient care, establish standards for healthcare professionals, and highlight key areas where more research is needed. While they are primarily based on existing scientific evidence, in cases where research is lacking, expert consensus helps fill the gaps (4–6). A list of the most important contemporary guidelines is shown in Table 1.
That said, as we will explore further, the current body of knowledge on BD treatment and management is so vast and complex that developing truly comprehensive and universally reliable treatment guidelines remains an incredibly difficult, if not nearly impossible, challenge (19).
2 Challenges stemming from the clinical picture
The goal of treatment for BD is to relieve clinical symptoms, reduce suffering, and help individuals regain their ability to function in daily life. What makes BD particularly challenging compared to other mental health conditions is its complex and unpredictable nature. It presents with distinct episodes—some completely different from one another—that can appear independently or share overlapping features. Unlike schizophrenia, which tends to follow a more stable long-term course, BD is marked by unpredictable fluctuations in symptoms and levels of disability.
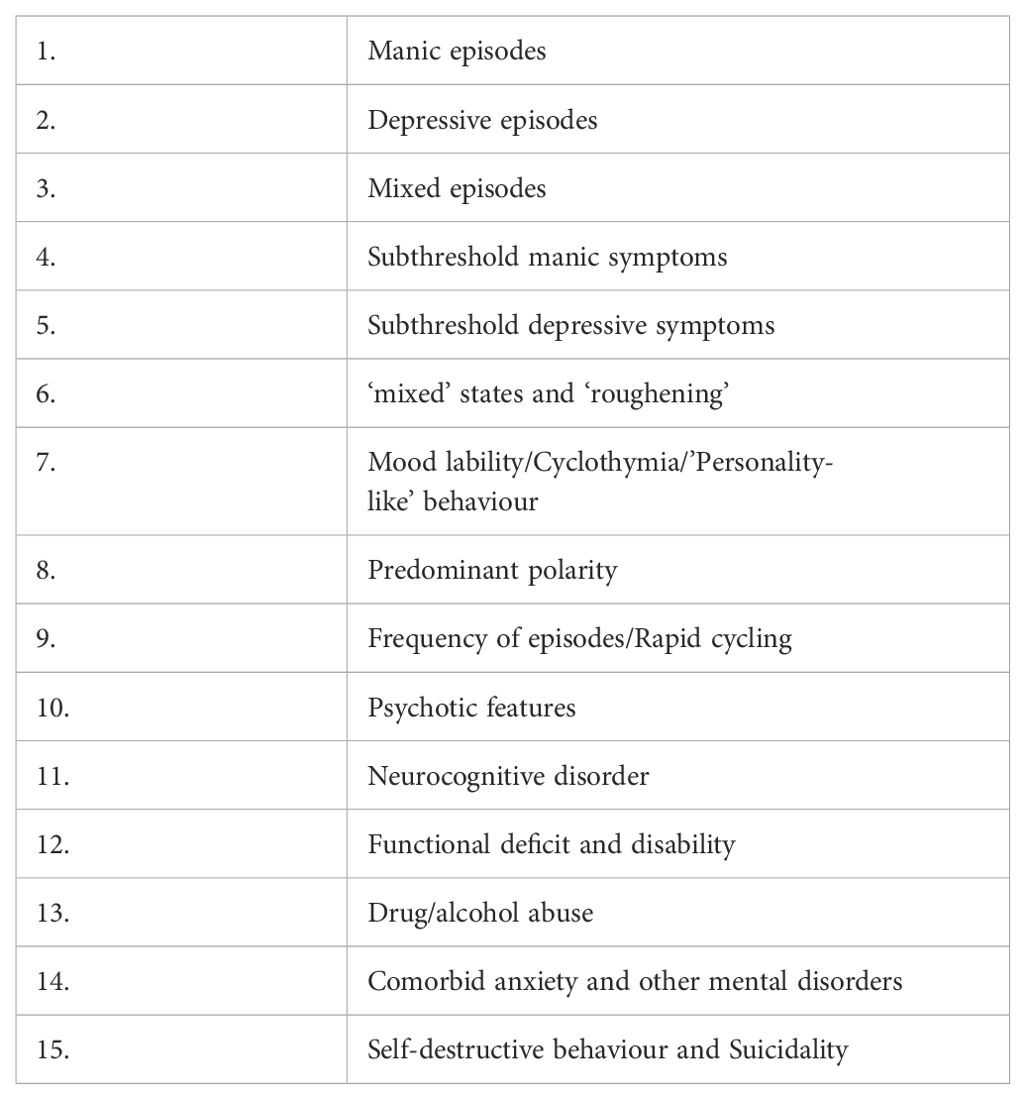
A detailed breakdown of the different facets and syndromes that make up BD can be found in Table 2. The most pressing clinical challenges—which in turn complicate treatment efforts and the development of clear treatment guidelines—are outlined below.
● Difficulty in making early correct diagnosis One of the biggest challenges in managing BD is accurately diagnosing it early on (20–23). In fact, up to 70% of patients experience a depressive episode first, leading to a misdiagnosis of unipolar depression and, as a result, inappropriate treatment with antidepressant monotherapy (20, 22, 24–26). In some cases, manic symptoms may not appear until 20 years after the initial depressive episode, further prolonging the delay in receiving the correct diagnosis (27, 28). Treatment guidelines should focus on strategies to navigate this “grey zone” of diagnostic uncertainty and help clinicians identify BD as early as possible.
● Suicidal thoughts are another major concern, affecting 78.6% of BD patients at some point in their lives (29). BD is also one of the psychiatric conditions with the highest risk of suicide attempts and completed suicides (30–34). Suicidality is often an acute crisis requiring immediate intervention, yet the most effective long-term treatments, such as lithium and lamotrigine, take time to work, while others, like certain antidepressants, may even be harmful. Because of this, treatment guidelines should establish a structured approach—an algorithmic strategy that carefully balances the need for rapid symptom relief with long-term stability, ensuring that urgent interventions do not come at the cost of worsening the overall prognosis.
● Some individuals with BD consistently experience one type of episode more frequently than the other—a pattern known as predominant polarity. Nearly half of BD patients fall into this category, with the majority tending toward the depressive pole (35–52). This distinction is critical for treatment, as it suggests that therapy should be tailored to the dominant symptom pattern. Treatment guidelines must take this into account, encouraging clinicians to approach current symptoms by considering past patterns while also anticipating future episodes (treating the present by taking into consideration the past to predict the future; the three-fingers rule, Figure 1).
● BD can also present with rapid cycling, a pattern in which mood episodes switch more frequently than usual. Variants include rapid, ultra-rapid, ultra-ultra-rapid, and ultradian cycling, with mood shifts occurring anywhere from months to within a single day. At some point in their illness, anywhere from one-quarter to one-half of BD patients will experience some form of rapid cycling (53–67). Treating these patients is especially challenging because very few medications work well for both poles of BD, and most require time to take effect. As a result, treatment guidelines must find a careful balance—providing swift relief for immediate symptoms without disrupting the long-term stability of the patient.
● Another key factor in treatment planning is the long-term course of BD, which varies widely among patients. In most cases (69.6%), BD follows a recurrent episodic pattern with distinct periods of illness and remission. However, in 25% of cases, the disorder takes a more chronic course, with continuous symptoms and little to no remission. A small percentage of patients (5.4%) experience only a single manic episode, while around 5% have chronic mania without depressive episodes (29). Since different long-term patterns require fundamentally different treatment approaches, treatment guidelines must acknowledge this variability and provide flexible strategies that can be adapted to each patient’s unique trajectory.
● The neurocognitive impairment in BD affects nearly all areas of thinking and occurs across different phases of the illness. Research has shown that psychosocial functioning is closely linked to processing speed (68, 69), abstract thinking (68), verbal memory, and executive function—even in patients who are in remission (euthymic phase) (70, 71). The severity of cognitive deficits is most pronounced during acute episodes but remains significant, though to a lesser extent, even during euthymia. While BD patients tend to have milder cognitive deficits compared to those with schizophrenia, the pattern of impairment is strikingly similar in both disorders (72, 73).
● A particularly urgent clinical issue in BD is agitation and its management. Recently, experts have even published a consensus paper outlining best practices for managing agitation in BD patients, underscoring the need for clear treatment strategies (74).
● Another major challenge in BD treatment is psychiatric comorbidity, which complicates diagnosis and management. In BD, having coexisting mental health conditions is the norm rather than the exception (75). Over half to two-thirds of BD patients experience at least one comorbid disorder in their lifetime (76–86), while 42% have two, and 25% have three or more comorbid psychiatric conditions (80). The prevalence of current (cross-sectional) comorbidity is lower, with around one-third of BD patients having at least one additional mental health disorder at any given time (76, 79, 86–88). Comorbidity in BD is associated with a more complex clinical picture, an earlier age of onset (89), and worse long-term outcomes, including higher suicidality and self-harm risk (78, 80, 86, 89, 90), poor treatment adherence (86), and less favorable response to lithium (82, 90). Anxiety disorders, in particular, are highly prevalent in BD, affecting 42–93% of patients at some point in their lifetime and 11–70% at any given time (57, 79, 80, 87, 91–113). Anxiety in BD is also strongly linked to predominant depressive polarity, further influencing treatment decisions and prognosis (96, 114).
● Alcohol and substance use disorders (SUD) significantly complicate the course of BD, increasing the risk of legal issues and suicidality (115). Data from the Epidemiological Catchment Area (ECA) study indicate that, at any given time, drug abuse is present in 13% of BD-I and 9% of BD-II patients, while drug dependence is observed in 28% and 12%, respectively (116). SUDs may also serve as either a risk factor or a prognostic marker for the development of BD with psychotic features, with a hazard ratio (HR) of 3 (117). Among BD-I patients, the lifetime prevalence of SUDs is at least 40%, with alcohol and cannabis being the most commonly abused substances, followed by cocaine and opioids (118, 119). Clinical studies suggest that alcohol use disorder affects anywhere from one-third to 75% of BD patients (120–125). According to ECA data, alcohol abuse is found in 15% of BD-I and 18% of BD-II patients, while alcohol dependence is present in 31% and 21%, respectively (116). Other substance use rates in BD patients include cannabis use disorder (5–65%) (F. 126, 127), gambling disorder (6–20%) (128, 129), cocaine abuse or dependence (3–7%) (K. N. 121, 130–132), and heroin abuse (5–25%) (121, 133). Substance use often correlates with mood states in BD, potentially altering the clinical presentation and leading to a higher prevalence of “mixed” states (134, 135). It may also increase the risk of mood switching when patients are treated with antidepressants (136). Beyond psychiatric complications, SUD is linked to higher medical comorbidity, including HIV infection (137–139), as well as an increased risk of suicide (98, 140).
● Many BD patients experience severe disability, and only a minority achieve full functional recovery (71, 141–146). As early as 1990, the World Health Organization (WHO) ranked BD among the top 10 most disabling conditions in terms of disability-adjusted life years (DALYs), highlighting its devastating impact on general health, employment, relationships, education, and overall quality of life (147–151). Studies show that at least one major area of life (e.g., work, social life, or family life) is significantly impaired in 52–54% of BD patients, while in 37%, disability affects two or more areas (152). Specifically, BD-I patients are reported to be completely unable to perform work-related tasks 30% of the time, while BD-II patients experience this level of impairment 20% of the time (153). A key observation is that disability in BD is more strongly correlated with depressive symptoms—even when these symptoms are subsyndromal (5, 69, 152, 154–163). Additionally, cognitive and functional impairments persist even during euthymic periods (157, 160, 161).
● The quality of life (QoL) of BD patients is closely linked to current depressive symptoms, whether they meet full diagnostic criteria or are subthreshold (164–166). Other key factors that negatively impact QoL include neurocognitive impairment (164, 167), the presence of psychotic symptoms (164), and daily stressors (168). However, research suggests that some BD patients in the euthymic phase may have a quality of life comparable to that of the general population (164, 168).
● Bipolar disorder does not only affect the individual—it also places a significant burden on caregivers and family members (149, 169–171). This burden can be categorized into: Objective burden – tangible consequences such as financial strain, job loss, hospitalizations, and divorce (172) and subjective burden – the emotional distress and psychological toll on caregivers, including feelings of exhaustion, frustration, and anxiety (171–176). Nearly all caregivers of BD patients report at least a moderate level of burden (177–181), and it is related to patient-related factors like the chronicity of the disease and high levels of impairment (182). The severity of this burden is influenced by factors such as the chronicity of the illness, levels of patient impairment, caregiver beliefs about BD (180), personality traits, and coping styles (177). The most distressing behaviors reported by caregivers include hyperactivity, irritability, withdrawal, impulsivity, aggression, and excessive spending. BD is associated with higher rates of violence compared to other psychiatric disorders, especially during acute manic or mixed episodes (183–185). Research indicates that family members are the victims in 70% of BD-related violent episodes, and in 81% of cases, these episodes were preceded by some form of provocation (185). Additionally, depression and suicidality in BD patients significantly contribute to caregiver distress (147, 172, 180, 186). Over time, the mental health of caregivers may deteriorate due to chronic stress, potentially leading them to develop depression and an increased need for mental health services themselves (181, 187–192).
● Increased suicidality: Suicidal thoughts and behaviors are unfortunately common in BD, with both persistent suicidal ideation and a high rate of completed suicides being key concerns (31, 193–195). Research shows that alcohol and substance use significantly increase the risk of suicide attempts in BD patients (196). This effect appears to be more pronounced in BD-I than in BD-II, likely due to higher levels of impulsivity, hostility, aggression, and an earlier onset of the disorder in BD-I patients (197, 198).
● For BD patients and their families, the financial strain can be overwhelming. Studies consistently show that BD is one of the most expensive mental disorders—both in terms of insurance costs and out-of-pocket expenses for patients and their loved ones (199). When compared to other psychiatric conditions, BD ranks among the most costly, not only in mental health care but across all areas of medicine (200–206). Interestingly, BD remains the most expensive disorder in nearly every category of health benefits, yet a small group of patients (2.4%) accounts for 20% of the total costs. This cost disparity isn’t due to BD treatment alone but rather the high costs of treating medical comorbidities that frequently accompany the disorder (207, 208). This big difference in the costs is caused not because of the treatment of the primary mental diagnosis but because of comorbid somatic conditions (209).
● Medical conditions in BD patients are often overlooked and undertreated—especially in those who fall within the broader bipolar spectrum (210). Multiple somatic comorbidity seems to be the rule rather than the exception with BD patients suffering from an average of 2.7 or more medical conditions (211–213) and facing up to four times higher healthcare costs compared to those without mental illness, largely due to medical comorbidities (200, 209, 214, 215). Tragically, their life expectancy is reduced by approximately 30%, making it lower not only than the general population but also compared to those with other psychiatric disorders (216–218). The leading cause of early death in BD is premature cardiovascular disease, but other common medical issues include endocrine disorders, gastrointestinal problems, and chronic pain (219). Depending on the study, anywhere from 11.5% to 75.7% of BD patients suffer from at least one physical health condition, with most experiencing multiple comorbidities—on average, 2.7 or more medical conditions per patient (77, 83, 84, 88, 111, 137, 212, 220–229).
● The concept of staging in BD aims to define the severity, progression, physiological changes, and long-term impact of the disorder (230). So far, five major staging models have been proposed (231–237), but while some evidence supports these models, the research is still limited. Studies tend to have small sample sizes, and data inconsistencies make it difficult to establish a universal framework.

Figure 1. The three-fingers rule: treating the present by taking into consideration the past to predict the future.
Currently, research suggests that BD follows a progression that includes:
● An asymptomatic “at-risk” phase – when an individual may be vulnerable to developing BD but has not yet shown clear symptoms.
● A non-specific prodromal phase – an early warning period where symptoms emerge but are not yet distinct enough to diagnose BD. This phase appears to overlap with other psychiatric disorders, making prediction difficult.
● An early stage of full-blown BD – characterized by well-defined episodes, minimal inter-episode symptoms, good response to treatment, and low disability.
● A late stage of BD – a more chronic and treatment-resistant phase, often featuring depressive predominant polarity, psychotic symptoms, and significant disability.
One major gap in research is the lack of studies on treatment effectiveness in the later stages of BD, which leaves clinicians with limited guidance on how to best manage patients with chronic, severe forms of the disorder (238). There are only a few exceptions where treatments specifically for late-stage BD have been explored (239).
3 Therapeutic challenges
As already said and elaborated, BD is a complex, long-term condition with an unpredictable course (240). Different aspects of the disorder respond to different medications, yet many of these treatments come with the risk of triggering the opposite mood state—for example, a medication that helps with depression may induce mania, and vice versa (241, 242). For decades, BD treatment has centered around the broad idea of “mood stabilizers”, though, in reality, this category includes only a small number of medications (243–246). More recently, research has suggested that targeting specific receptors could be a more effective approach (247). However, integrating acute-phase treatment with long-term management remains an ongoing challenge (248). One of the biggest difficulties in BD treatment is the difficulty in designing an evidence-based long-term strategy. While treatment guidelines exist, they struggle to balance current symptoms, past psychiatric history, and the potential for future relapse. This problem is comfounded by the fact that there is limited research on how to manage specific facets of BD, making it difficult for clinicians to create comprehensive, individualized treatment plans (5, 249–251). Although acute episodes (such as full-blown mania or major depression) make up only a small percentage of a patient’s lifetime, subthreshold or subclinical symptoms—mild but persistent mood disturbances—tend to dominate daily life, contributing to ongoing impairment, disability, and emotional distress (42, 252, 253). Since no single medication can fully manage all phases and symptoms of BD, most patients require a combination of treatments to achieve a reasonable quality of life (254).
Clinicians and treatment guidelines face a difficult dilemma. What should be the long-term maintenance plan for patients who initially respond well to a medication that lacks long-term safety and efficacy data—or worse, one that has negative evidence regarding its potential long-term impact on mental health? There is no clear answer, and expert opinions differ significantly. This is further complicated by the fact that most maintenance studies are conducted on “enriched samples”, meaning they focus on patients who already responded well to a specific medication during the acute phase. This creates uncertainty, especially when a first-line treatment fails or provides only partial relief. Should the clinician switch medications, potentially prolonging the patient’s suffering? Or should they add a second medication, increasing the complexity of treatment and the risk of side effects? Making these decisions requires careful consideration of various factors, including specific indications, contraindications, potential pitfalls, and patient history (244, 255–260).
The introduction of second-generation antipsychotics (SGAs) has significantly changed the landscape of BD treatment, making antipsychotics a core component of treatment guidelines. However, the role of antidepressants in BD remains controversial. While antidepressants have historically been seen as a viable treatment option for bipolar depression, particularly in Europe, recent studies question their effectiveness and even suggest that they may increase the risk of mood destabilization (261). At the same time, the value of psychosocial interventions—such as psychotherapy, lifestyle changes, and support groups—remains uncertain, as research on their effectiveness in treating specific BD symptoms is still limited (30, 262).
Residual symptoms—those that persist between major episodes—can have a major impact on a patient’s ability to function in daily life. These symptoms may interfere with access to healthcare, employment, financial stability, and even basic social support systems (263). The situation is even worse for patients with severe disability, functional decline, or poor quality of life, as they also face higher mortality rates due to medical comorbidities (227) and an increased risk of suicide (253). This not only increases the burden on caregivers and families but also drives up healthcare costs due to frequent hospitalizations and medical interventions. In many parts of the world, these challenges are worsened by discriminatory insurance policies, which limit coverage for mental health treatment and create additional financial strain on patients and their families (253, 264).
One of the biggest debates in BD treatment revolves around the very concept of “mood stabilizers.” While lithium, valproate, and carbamazepine were traditionally considered the gold standard, newer research suggests that some atypical antipsychotics—such as quetiapine and olanzapine—may meet many of the same criteria. However, no single medication is effective against all phases of BD, including manic, mixed, and depressive episodes, as well as rapid cycling. In practice, antipsychotics tend to work more quickly during acute mania and are particularly effective for psychotic symptoms. However, each medication comes with its own set of risks—for example, antipsychotics can increase the risk of metabolic syndrome, while lithium can cause kidney and thyroid issues. As already said, treating BD is inherently complex (240) and for decades, treatment was built around the concept of mood stabilizers, but in recent years, a wave of new research, particularly on atypical antipsychotics, has reshaped the field. As a result, clinicians must navigate numerous treatment considerations, including drug interactions, contraindications, and unexpected complications (244, 255–260). The definition of “mood stabilizers” remains unclear. Research does not support the idea that all traditionally labeled mood stabilizers—such as lithium, valproate, and carbamazepine—are equally effective across all phases of BD. Instead, newer studies highlight significant limitations in their effectiveness. Even more concerning, some aspects of BD may be resistant to treatment, a problem that has only recently gained attention.
Another important problem is that not only the evidence is limited concerning the treatment of specific facets and issues of BD (5, 249, 250, 265, 266), but also continued scientific training and reading are inadequate. Thus, research findings are not making it to the everyday clinical practice. Focused educational intervention might be necessary to change this attitude. Part of this problem is reflected in the common practice among clinicians to use medication based on a ‘class effect’. This means that they consider that a whole class of medications possesses a specific action. This class effect is often considered in combination with a ‘syndromal approach’ which means that irrespective of the nosological entity, a specific kind of symptoms respond to a specific class of medication.
Many clinicians also follow a “syndromal approach”, assuming that certain symptoms will respond to specific medication classes, regardless of the underlying disorder. For example, some clinicians assume that all antipsychotics work equally well for psychosis, regardless of diagnosis, and that all antidepressants are equally effective for depression. While this simplifies treatment decisions, research has repeatedly disproven this approach, particularly in BD, where the concept of mood stabilizers has been overly broad and imprecise (243). The extent to which this outdated approach still influences clinical practice worldwide is unclear, but it likely has a significant impact on treatment outcomes. If clinicians were to shift toward a more evidence-based approach, BD patients might see better long-term outcomes.
With the introduction of second-generation antipsychotics (SGAs), these medications have become a cornerstone of BD treatment, aligning with current treatment guidelines. In contrast, recent studies have cast doubt on the effectiveness of antidepressants for BD, challenging their traditional role in bipolar depression (261). Additionally, long-term treatment strategies have become more complex, as research shows that medications previously thought to be mood stabilizers may be more effective for one mood state than the other (248) Given the rapid pace of new research, it can be difficult for clinicians to stay updated and integrate these findings into their daily practice. At the same time, there is still limited data on the effectiveness of psychosocial interventions in BD. While therapy and social support play a role, their specific impact on BD symptoms remains uncertain (30, 262).
4 Special issues
● While it is well established that gender-specific factors influence the treatment and overall management of BD (267–270), research in this area remains limited. This gap is significant because the unmet needs of male and female patients may differ, potentially affecting treatment outcomes and quality of life (253, 267). Although BD-I is equally common in both males and females (253), BD-II appears to be more prevalent in females (269) as does depressive predominant polarity (45). Females with BD also tend to experience more rapid cycling, mixed episodes, and dysphoric mania (252, 253, 271–273), Additionally, they face higher rates of hypothyroidism and a greater likelihood of comorbid personality disorders (252, 253, 271–273). On the other hand, males with BD are more likely to present with suicidality, psychotic features, and a higher frequency of hospitalizations (253). One of the most significant concerns in female BD patients revolves around the reproductive cycle and its physiological impact on the disorder. Hormonal fluctuations throughout life—during menstruation, pregnancy, postpartum, and menopause—can all affect the course of BD and response to treatment. Beyond reproductive concerns, females with BD also appear to be at greater risk for specific medication-related side effects, including weight gain (274, 275) and, in severe cases, extreme obesity (276). Long-term use of certain medications, particularly those that elevate prolactin levels, may lead to a decrease in bone mineral density due to prolonged hyperprolactinemia (277). In some cases, this can even result in a hypogonadal state, further complicating overall health and treatment considerations (278). Despite these clear gender-based differences in symptoms, treatment response, and side effects, research on how to tailor BD management by gender remains insufficient. Addressing these knowledge gaps could lead to more effective, personalized treatment strategies that better meet the unique needs of both males and females.
● One of the most pressing concerns for females with BD is the risk of unplanned pregnancy (279). Given the potential impact of pregnancy on both the course of BD and treatment safety, females of childbearing age should receive comprehensive counseling on contraceptive options, medication interactions, and the effects of pregnancy and childbirth on their mental health. Discussions should also cover safe treatment options during pregnancy and breastfeeding, as well as the emotional and physical stress of pregnancy and parenting. Additionally, the potential risks and benefits of specific medications during different stages of pregnancy should be thoroughly explored to help patients make informed decisions (280, 281). Certain BD medications—including carbamazepine, oxcarbazepine, lamotrigine, and topiramate—are known to increase the clearance rate of oral contraceptives, potentially reducing their effectiveness. Females taking these medications may require dose adjustments or alternative contraceptive strategies as part of their standard care plan. Failing to account for these interactions can lead to contraceptive failure, increasing the risk of unintended pregnancy and associated complications. The postpartum period is one of the most vulnerable times for women with BD, with the highest risk of illness exacerbation occurring within the first 90 days after delivery (269, 282–288). This period requires careful monitoring and, in many cases, preventive treatment strategies to reduce the likelihood of severe mood episodes, which could impact both maternal well-being and infant care. Given these complexities, reproductive health should be an integral part of BD management for women, ensuring they receive personalized guidance on contraception, pregnancy planning, and postpartum care to minimize risks and promote stability.
● There is not much data concerning the point of view of psychiatrists and therapists in general on the unmet needs in the treatment of BD patients. However, mental health professionals generally agree that both acute episode management and long-term treatment could be improved by focusing on better treatment effectiveness, increased patient adherence, and enhanced long-term safety in maintenance therapy. Among BD patients, those with comorbid alcohol and/or substance use disorders are seen as having the greatest unmet needs, followed closely by those who experience rapid cycling (289). These populations present unique challenges, often requiring more intensive and specialized care, yet existing treatment strategies may not adequately address their specific needs. Surprisingly, only half of surveyed psychiatrists considered treatment guidelines to be an essential part of their day-to-day clinical decision-making. Even more unexpectedly, they reported that clinical trial findings had the least influence on their treatment choices. Additionally, only about one-third of clinicians were familiar with large-scale practical clinical trials or with scientific organizations and associations related to BD (290, 291). These findings highlight a critical gap between research and clinical practice, suggesting a need for greater dissemination of evidence-based knowledge and better integration of research findings into real-world treatment approaches. Bridging this gap could help ensure that patients receive the most effective, scientifically supported care while also addressing the complex challenges that come with managing BD.
● The point of view of patients and caregivers might vary considerably from the point of view of mental health professionals (292). One of the key factors contributing to poor treatment adherence is that clinical research often fails to focus on the unmet needs that patients themselves experience. As a result, real-world challenges are not always addressed, leaving gaps between what research prioritizes and what truly impacts daily life for those living with BD (293). There is also a significant disconnect between how mental health professionals interpret the evidence supporting different BD treatments and how patients perceive the impact of these treatments in their own lives (294). This mismatch can lead to frustration, dissatisfaction, and disengagement from care, making it even harder to achieve long-term stability. If the true measure of treatment success is based on patients’ self-reported quality of life, research presents a concerning reality. Studies show that individuals with severe mental illness, including BD, frequently report dissatisfaction with their social lives, overall health, and the level of support they receive. Many express that their unmet needs go beyond medication, extending to case management services, social and recreational opportunities, and vocational rehabilitation—all of which are crucial for achieving meaningful recovery and reintegration into society (295). Bridging the gap between clinical priorities and real-world patient needs requires a more patient-centered approach, ensuring that treatment strategies focus not only on symptom control but also on improving overall well-being, daily functioning, and quality of life.
● Poor treatment adherence is a major challenge in mental health care, particularly in BD, where it is strongly linked to worse outcomes (296, 297) Depending on how adherence is defined and the setting in which it is studied, research suggests that between one-third and two-thirds of BD patients do not consistently follow their prescribed treatment plans (297–299). One of the primary reasons for non-adherence is the side effects of medications, which can be difficult for patients to tolerate over long periods. Additionally, some individuals are reluctant to give up the experience of manic or hypomanic episodes, especially hypomania, which can bring increased energy, creativity, and euphoria—making it difficult for patients to fully commit to treatment that dampens these states (300). Another significant barrier to adherence is a lack of understanding about BD management. Many patients and their families do not fully grasp the long-term nature of the disorder, the importance of maintenance treatment, or the need for regular follow-up care. Without this awareness, treatment adherence can become inconsistent, increasing the risk of relapse and worsening symptoms (22). Addressing these challenges requires a combination of patient education, open communication about side effects, and individualized treatment plans that consider both clinical effectiveness and patient preferences. A more collaborative approach between patients, families, and healthcare providers may help improve adherence and lead to better long-term stability and quality of life for those living with BD.
5 Defining the clinical parameters to take into consideration
The key clinical and therapeutic challenges in BD have been outlined above. However, in real-world practice, these challenges often appear in unique and unpredictable combinations, which do not always fit neatly into the categories defined by modern classification systems. This makes it difficult to apply a one-size-fits-all approach to diagnosis and treatment. While it would be ideal to treat the full spectrum of symptoms as a whole rather than focusing on specific symptom clusters, current research does not always provide enough evidence to support this broader approach. Despite these limitations, it remains crucial to carefully examine the available literature when developing treatment guidelines, ensuring that they directly address these real-world complexities and provide practical solutions for clinicians.
6 Search of the literature and type of studies
There are three primary approaches to developing a knowledge base for BD treatment guidelines (301):
6.1 Expert opinion
This method is straightforward and convenient, relying on the insights of experienced professionals. However, it comes with significant risks, including the reinforcement of outdated assumptions, personal biases, and treatment approaches that may not align with the latest research findings.
6.2 Clinician surveys
Gathering input from a broad range of practicing clinicians can result in practical, real-world guidelines that reflect the challenges of everyday patient care. However, this approach is also prone to bias, as it may be influenced by individual experiences, unscientific beliefs, and variations in clinical training.
6.3 Systematic literature reviews
Examining existing research is the most scientifically rigorous way to develop guidelines, though it can take various forms. In the past, selective literature reviews were common, but today, systematic reviews are the gold standard. These reviews aim to incorporate all relevant research, minimizing personal bias and ensuring greater scientific credibility and broader acceptance. The PRISMA method is widely recognized as the most reliable approach for conducting systematic reviews and reporting of their process and results, as it ensures transparency, comprehensiveness, and methodological rigor (302–305).
While each approach has its strengths and limitations, the most reliable and widely accepted guidelines are those that rely on systematic reviews, ensuring that treatment recommendations are based on the best available evidence rather than personal or anecdotal experience. When conducting literature reviews to develop evidence-based treatment guidelines for BD, different types of research papers can be targeted. However, the most critical sources of information are Randomized Controlled Trials (RCTs). These studies may be either placebo-controlled or involve head-to-head comparisons with established treatment options. They can also focus on monotherapy (a single treatment) or combination strategies, such as add-on therapy or polypharmacy.
The distinction between add-on therapy and combination therapy is important. Combination therapy is tested in a general patient population, meaning the study includes both treatment-responsive and treatment-resistant patients. In contrast, add-on therapy specifically involves patients who have already shown resistance to treatment. A second agent is then added to determine whether it enhances effectiveness.
Another crucial aspect of interpreting research findings is understanding the difference between “failed” and “negative” trials”. A failed trial occurs when a study does not detect a positive treatment effect, even if one actually exists. This often happens due to issues such as an inappropriate study sample, such as testing a treatment on chronic patients who may not respond to the intervention. In contrast, a negative trial occurs when a treatment is genuinely ineffective, as determined by a well-designed study with an appropriate patient sample and methodology.
A classic example of a failed study is a three-arm study, where one group receives the new treatment, another receives an established treatment, and the third receives a placebo. If neither the new treatment nor the established treatment shows a meaningful difference from placebo, the trial is considered failed rather than negative—since it is likely that factors such as poor study design or patient selection interfered with the results. Unfortunately, outside of three-arm studies, it is extremely difficult—if not impossible—to distinguish between failed and negative studies in two-arm trials (where only the new treatment and placebo are compared). This often leads to the interchangeable use of the terms “failed” and “negative”, even though they describe different scenarios.
Beyond primary RCTs, post-hoc analyses can provide valuable insights that may not be explicitly addressed in the original study publication. However, a major limitation is that most post-hoc analyses are not pre-registered, making them vulnerable to selective reporting bias—where only the most favorable or significant findings are published.
Meta-analyses are another important source of information, but they are often overvalued. The sheer number of meta-analytical studies being published today is overwhelming, and many are of poor quality, sometimes leading to misleading conclusions. One common issue is that meta-analyses using raw scores instead of standardized mean differences (ratio of raw score change to standard deviation) are highly likely to produce misleading results because very often, large differences in terms of raw scores are accompanied by large standard deviations; the use of standardized mean difference might even reverse the results. Additionally, when studies vary significantly in their methodology, the combined conclusions from meta-analyses can differ both from each other and from the original findings of RCTs (306, 307).
Unpublished studies can sometimes be found in research repositories, but interpreting their results requires expertise. Many studies remain unpublished or are canceled due to negative interim findings, insufficient funding, or recruitment challenges. While these studies can still offer valuable insights, they should be approached with caution and critical analysis to determine why they were never formally published.
In summary, while systematic reviews of the literature provide essential insights for treatment guidelines, not all studies carry the same weight. RCTs remain the gold standard, but understanding nuances such as failed vs. negative trials, post-hoc biases, and limitations of meta-analyses is crucial for ensuring that treatment recommendations are truly evidence-based and clinically relevant.
To ensure a comprehensive and reliable review of the literature when developing BD treatment guidelines, search strategies should follow a structured approach that includes multiple sources and verification methods.
● Using Appropriate Keywords – A well-defined keyword strategy is essential to capture all relevant studies on BD treatments.
● Searching Key Research Databases – At a minimum, literature reviews should include searches in major medical and psychological research repositories, such as PubMed/Medline, Scopus, and PsycINFO. These databases contain peer-reviewed studies, systematic reviews, and meta-analyses that form the backbone of evidence-based guidelines.
● Reviewing Clinical Trial Registries – Websites that list clinical trials should also be searched, including ClinicalTrials.gov (http://clinicaltrials.gov) and Clinical Study Results (http://www.clinicalstudyresults.org). Additionally, the official websites of pharmaceutical companies producing medications for BD should be reviewed. These sources provide original pre-registered study protocols, detailing the primary and secondary outcomes of clinical trials. Such information can help identify cases of misleading reporting in published studies—for instance, the discrepancies seen in publications on lamotrigine for acute bipolar depression (308).
● Examining Reference Lists of Relevant Reviews and Guidelines – Reviewing the citations in existing systematic reviews and previously published treatment guidelines can help identify key studies that may not appear in a standard database search.
● Determining Language Inclusion Criteria – A decision must be made about whether to restrict searches to English-language publications or include studies in other languages, depending on the availability of resources for accurate translation. Important findings from non-English sources could contribute valuable insights if they can be reliably translated.
● Seeking Additional Unpublished Data – In some cases, unpublished research, particularly from pharmaceutical manufacturers or study authors, can provide critical information that is missing from published literature. These sources may contain data from studies that were never published due to negative results, funding issues, or recruitment difficulties, offering a more complete picture of treatment effectiveness and safety.
7 Methods to grade the findings in the literature
The process of grading medical evidence and formulating clinical recommendations has been in use since the early 1980s (309). All grading systems aim to assess the quality of available data and determine how confidently the benefits of a treatment outweigh its risks. Factors such as patient values and preferences are also considered, though in this particular framework, cost was not taken into account by the workgroup.
In 1992, a five-step approach was introduced to streamline individual-level clinical decision-making, and by 2005, it was formally published as a structured guideline (310). These five steps include:
● Formulating a Clear, Answerable Question – The first step is to define a precise and well-structured question that avoids ambiguity and uncertainty. A well-formulated question ensures that research efforts are focused and effective in addressing specific clinical concerns (311, 312).
● Conducting a Systematic Search for Evidence – A comprehensive and methodically structured search should be conducted to identify all relevant research on the topic, ensuring that no key evidence is overlooked (313).
● Critically Reviewing and Classifying the Evidence – Once relevant studies are gathered, they must be carefully evaluated for quality, considering factors such as systematic errors, different types of bias, confounding factors, reliability, and validity. Additionally, the clinical significance and generalizability of the findings must be taken into account, as results from a highly controlled study may not always translate directly to real-world clinical practice (314, 315).
● Applying the Findings in Clinical Practice – After assessing the evidence, the results must be translated into practical treatment recommendations, ensuring they align with patient needs, safety considerations, and therapeutic goals.
● Evaluating Performance and Outcomes – Finally, it is essential to monitor and assess how well the implemented guidelines perform in actual clinical practice. This includes tracking patient outcomes, treatment adherence, and any emerging concerns, allowing for continuous improvement and refinement of recommendations (316–319).
By following this structured approach, treatment guidelines can be developed in a way that ensures scientific rigor, clinical relevance, and practical applicability, ultimately improving the quality of care for individuals living with bipolar disorder.
Evaluating the quality of evidence is a crucial step in developing treatment guidelines for BD. The strength of evidence is determined by how well studies minimize biases that can distort research findings. As already discussed, the gold standard in medical research includes triple-blind, placebo-controlled trials with allocation concealment and complete follow-up in a homogeneous patient population. These studies are considered to provide the highest level of evidence, whereas case reports rank the lowest. While expert opinion can be valuable in shaping guidelines, it should not be considered a source of scientific evidence (320).
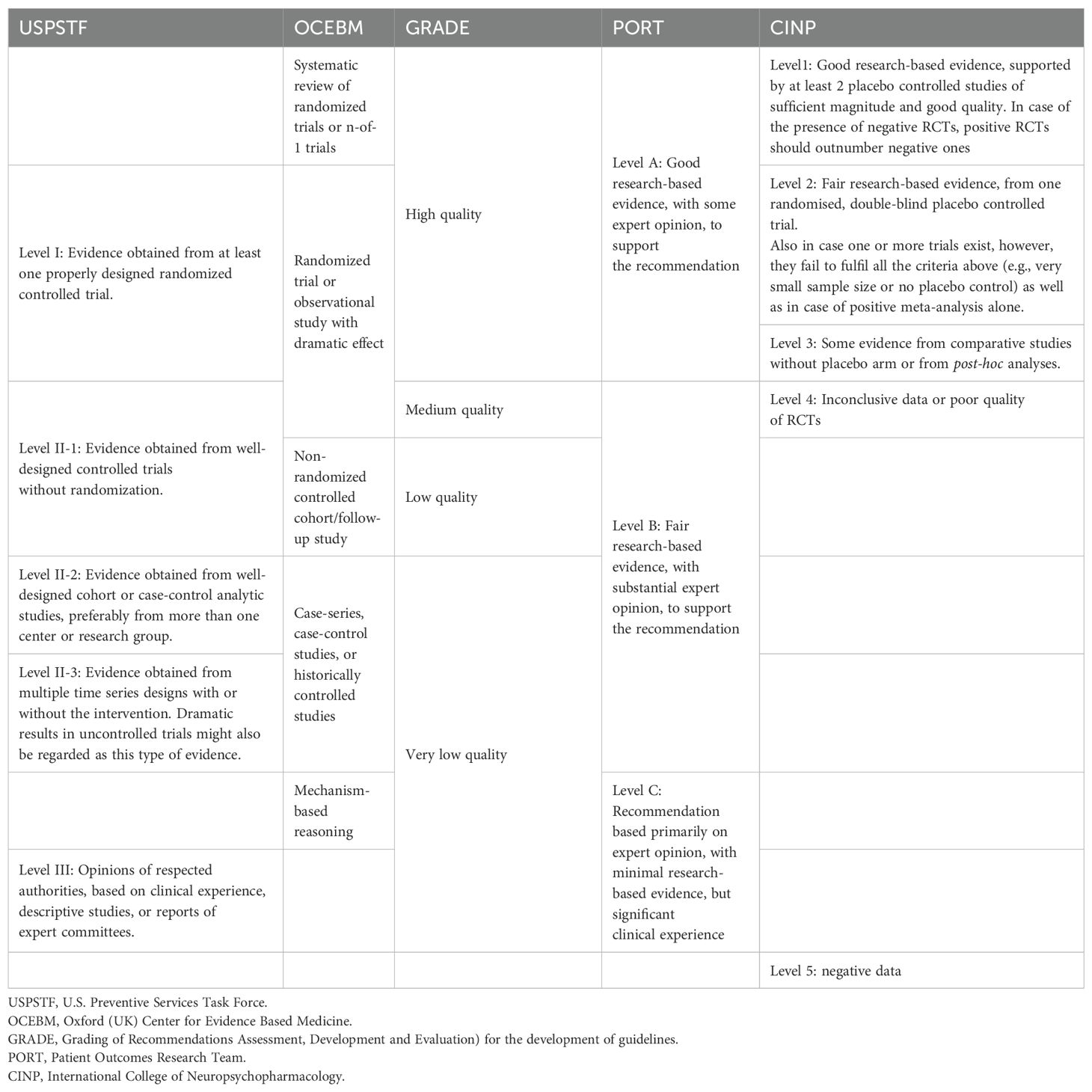
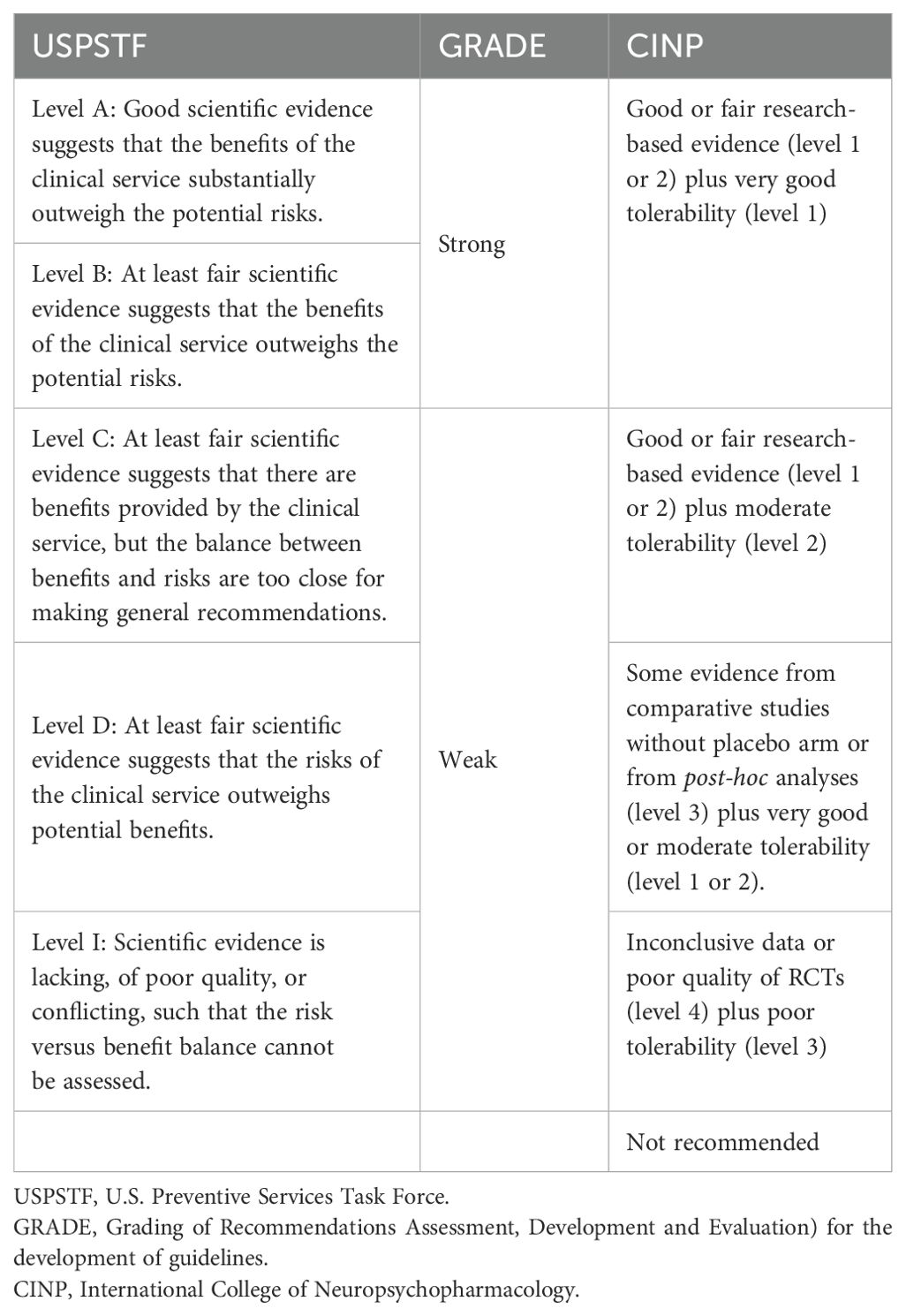
Several grading systems have been developed by various organizations to assess the quality of evidence. Among the most widely used are:
● The U.S. Preventive Services Task Force (USPSTF) – A system designed to evaluate the strength of clinical evidence and inform preventive healthcare recommendations (321, 322).
● The Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence – A framework useful for grading diagnostic tests, prognostic markers, and treatment risks (323). This system played a role in the development of the BCLC staging system for hepatocellular carcinoma in Canada (324).
● The PORT Method (Patient Outcomes Research Team) – Used by the World Federation of Societies of Biological Psychiatry (WFSBP) in formulating their bipolar disorder guidelines (325) (326–328). In 1992, the Agency for Health Care Policy and Research (AHCPR) and the National Institute of Mental Health (NIMH) collaborated to establish the PORT for Schizophrenia, adopting similar criteria to those used in the AHCPR Depression Guidelines.
Among modern grading systems, the GRADE Method (Grading of Recommendations Assessment, Development, and Evaluation) is one of the most widely adopted approaches for guideline development (329, 330) A key feature of GRADE is that it separates the quality of evidence from the strength of recommendations. It emphasizes the importance of defining a clear clinical question, including four essential components: patient population, intervention, comparison, and outcomes of interest (331) It also categorizes outcomes based on their relevance to clinical decision-making, prioritizing those that are critical for treatment recommendations over those that are less significant (332).
The GRADE system evaluates evidence quality based on:
● Study limitations (e.g., lack of allocation concealment or blinding).
● Inconsistency of results.
● Indirectness of evidence.
● Imprecision in findings.
Under certain conditions, evidence quality can be upgraded—for example, if a study demonstrates an exceptionally strong treatment effect (339). While GRADE provides a robust method for grading a wide range of evidence sources, it is less effective for evaluating datasets that focus solely on RCTs—such as those used in the current bipolar disorder guidelines. According to GRADE criteria, the evidence supporting the current guideline effort is considered high quality, with only two potential limitations: large losses to follow-up and early trial termination due to treatment benefits or failure to report outcomes. The GRADE method provides guidance to grade the data from a variety of sources (340), but it is not sensitive for datasets that focus solely on RCTs like the dataset of the current workgroup. According to the GRADE grading system, all the data included in the current effort to develop guidelines are of high quality. From the limitations recognized by the GRADE (lack of allocation concealment, lack of blinding, large losses to follow-up, failure to adhere to an intention to treat analysis and stopping early for benefit or failure to report outcomes) only large losses to follow-up and stopping early for benefit or failure to report outcomes could apply to the current study.
The most recent grading system was developed by the CINP Bipolar Guidelines Workgroup (341). This method was specifically designed to evaluate evidence from RCTs, post-hoc analyses, and meta-analyses, as no existing grading system had been developed for this purpose. While traditional grading systems rank RCTs and meta-analyses as the highest levels of evidence, they do not distinguish between conflicting results, inconsistencies between RCTs and meta-analyses, or findings derived only from secondary outcomes. The CINP system addresses these gaps by integrating a detailed evaluation of treatment efficacy across studies.
A comparative overview of these grading methods is presented in Table 3, while Table 4 summarizes the different approaches for developing treatment recommendations.
For example, all systems exept for the CINP are either to crude or are calibrated for use with lower quality data. Especially the USPSTF can not distinguish between scenarios with different admixture of positive and negative RCTs and meta-analyses. The greatest problem today is to rank the evidence that come from such combinations, and only the CINP method provides three levels concerning that specific area of available evidence (301, 342).
8 Study design and outcome
The complexity of BD presents significant challenges in treatment research, starting with the very definitions used in clinical trials. While it is relatively straightforward to define acute episodes, whether manic, hypomanic, or depressive, other terms—such as continuation and maintenance treatment—are often used interchangeably in randomized controlled trials (RCTs), leading to confusion (51, 343). By strict definition, continuation treatment lasts up to 12 months and is intended to sustain recovery from an acute episode until the point at which the episode would have naturally resolved. In contrast, maintenance treatment is designed to prevent future episodes and typically extends for several years beyond the continuation phase. However, a major challenge is that very few patients in RCTs achieve complete remission, making it difficult to clearly distinguish relapse from recurrence and continuation from maintenance treatment (344). In RCT terminology, the terms relapse and maintenance are preferred. However, the U.S. Food and Drug Administration (FDA) accepts data from patients who have been in remission for less than two months, further blurring the line between continuation and maintenance treatment (345). Even the term relapse is problematic in BD. Traditionally, a relapse is defined as the return of symptoms of the same polarity as the original episode, usually within the first few months of improvement. However, given the polymorphic nature of BD, this definition may be too restrictive, as it excludes cases where an episode of the opposite polarity emerges early in recovery. Licensing authorities tend to accept the broader definition, which includes opposite-pole relapses as part of the overall relapse rate. This variability in definitions also complicates the ability to define treatment resistance and refractoriness in BD (5, 11, 346). Another important concept in BD research is the index episode, referring to the acute episode that leads to a patient’s enrollment in a maintenance trial. Most maintenance trials follow an enriched study design, meaning that only patients who initially responded to a specific treatment during the acute phase are included in the double-blind maintenance phase. This design has important consequences. First, it biases the study sample toward patients with a specific predominant polarity (e.g., those more prone to mania or depression). Second, it favors patients who have already shown a good response to the medication being tested. As a result, findings from these trials may not apply to the general BD population, particularly patients who do not continue with the same medication in the maintenance phase or those who require a switch to another treatment (347, 348). These limitations make it difficult to translate research findings into real-world clinical practice, underscoring the need for more inclusive study designs that reflect the diverse and unpredictable course of BD.
The majority of BD treatment research focuses on measuring changes in symptom severity using standardized rating scales. While this approach provides valuable insights into short-term symptom relief, it often overlooks other critical aspects of patient well-being, such as disability, quality of life, caregiver burden, and economic impact. These factors are just as important in determining the long-term success of treatment, yet they remain understudied in clinical trials. Most experts agree that current BD treatments are more effective at reducing symptoms than at addressing functional impairment and overall long-term outcomes (296, 349–351). This gap in treatment effectiveness is particularly concerning in bipolar depression, which is notoriously difficult to treat and associated with a high risk of suicide (10, 11, 24, 251, 350, 352, 353) and profound and lasting functional impairment (354).
Beyond its impact on mental health, bipolar depression often leads to profound and long-lasting functional impairment, making it one of the most challenging phases of BD to manage (354). To improve real-world outcomes, future research should focus not only on symptom reduction but also on strategies to enhance overall functioning, reduce disability, and improve quality of life. This shift would provide a more comprehensive understanding of treatment effectiveness and help develop more patient-centered approaches to managing BD.
The vast majority of randomized controlled trials (RCTs) in BD treatment are industry-sponsored, meaning their primary goal is to obtain regulatory approval for a medication. As a result, these studies are designed to focus on specific, standardized outcome measures that align with the approval process, rather than broader aspects of patient well-being and real-world effectiveness. In acute-phase trials, the primary outcome is almost always the change in total score on a symptom severity scale, such as the Young Mania Rating Scale (YMRS), Mania Rating Scale (MRS), Montgomery-Åsberg Depression Rating Scale (MADRS), or Hamilton Depression Rating Scale (HAM-D). Other clinical measures, such as the Clinical Global Impressions (CGI) scale or the Positive and Negative Syndrome Scale (PANSS), are typically included as secondary outcomes. Additionally, response rates (percentage of patients who show significant symptom improvement) and remission rates (patients achieving minimal symptoms) are almost always secondary outcomes. For maintenance studies, the most common primary outcome is relapse into a mood episode, which helps assess how well a treatment prevents recurrence over time. However, rarely do these studies measure broader, real-world aspects of BD, such as general impairment, neurocognitive function, social and occupational quality of life, or long-term daily functioning. While the current outcome measures are useful for determining whether a drug is effective, they often fail to capture the full spectrum of what truly matters in clinical practice. Long-term success in BD treatment is not just about symptom reduction but also about improving daily life, enhancing functional recovery, and supporting overall well-being. Expanding the scope of clinical trials to include these aspects would lead to more meaningful treatment insights and better align research with the actual needs of patients and clinicians.
While including too many assessment scales in RCTs can create challenges in trial completion, it is crucial to prioritize scales that are most relevant to everyday clinical practice. Instead of relying solely on global symptom scores, trial reports should provide detailed insights into which specific BD features and specifiers respond to a given treatment. At the same time, trial feasibility and costs must be carefully balanced against the potential research benefits. A well-designed study should incorporate clinically meaningful measures without overwhelming participants or compromising trial efficiency.
Future RCTs should focus on outcomes that reflect real-world challenges, including mixed features, anxiety, psychotic symptoms, neurocognitive impairment, and disability. Currently, data on mixed features in acute bipolar depression are scarce, with most findings on mixed episodes coming from acute mania trials. At the same time, trial design should minimize the burden on both patients and researchers by avoiding unnecessary assessments, ensuring that RCTs remain both comprehensive and feasible.
One key concern in BD research is the duration of the continuation phase before transitioning into maintenance treatment, which is often too short to ensure long-term stability. This issue is particularly evident in acute-phase studies, especially for bipolar depression trials. A clear example is seen in studies on aripiprazole, where results were positive at week 6 but negative by the study endpoint at week 8 (355). This suggests that at least 8 weeks is needed in acute bipolar depression trials to capture true and lasting improvement. However, some medications have still gained approval based on studies as short as 6 weeks, raising concerns about the adequacy of current trial durations in assessing long-term effectiveness (356).
While enriched study designs help determine whether a medication remains effective long-term for patients who initially responded during the acute phase, they do not clarify whether it offers broader prophylactic benefits—particularly for patients who responded to a different treatment during the acute phase. Although many acute-phase treatments seem to provide ongoing benefits in maintenance therapy, it remains uncertain whether this applies to all medications. As a result, the generalizability of maintenance treatment efficacy beyond those who initially responded to a given agent is still largely unknown.
A three-week study duration for acute mania is likely insufficient, yet it remains the standard in most randomized controlled trials (RCTs). A more effective approach would be a 12-week study design for both acute mania and bipolar depression trials, allowing researchers to assess both manic and depressive symptoms, which frequently co-occur. While the use of placebo controls is scientifically valid, including a third arm with an active comparator would enhance assay sensitivity, providing more meaningful comparisons and improving the reliability of study findings (357).
Despite the availability of data, both authors and manufacturers often choose not to disclose certain findings. This includes key outcomes such as a treatment’s impact on core manic or depressive symptoms, mixed features, psychotic symptoms, and rapid cycling. In many cases, only p-values are reported without means and standard deviations, while in other instances, means are provided without statistical significance markers, leading to confusion in interpretation. Additionally, some studies report total scale scores, such as the PANSS total score, without offering a detailed breakdown of symptom domains, making it difficult to assess specific treatment effects. Another concern is the lack of transparency in sample sizes. Often, data are missing for portions of the study population, leading to varying sample sizes for different outcomes—yet this is not always clearly stated. A particularly unacceptable practice is seen in studies on mixed episodes, where only the effect of treatment on manic symptoms is reported, while the impact on depressive symptoms is omitted. This selective reporting limits clinicians’ ability to make informed decisions, emphasizing the need for greater transparency and comprehensive data presentation in BD research.
Making raw data accessible to the scientific community could lead to major advancements in our understanding of BD without requiring new and costly research. A more exhaustive analysis of existing data could provide valuable insights, improve treatment strategies, and enhance the real-world applicability of findings. Additionally, open access to data would help eliminate publication bias and improve the reliability of research conclusions.
A review of the literature suggests that study results are reported inconsistently, often lacking a uniform structure despite the existence of general reporting templates (9, 301, 341, 342). This inconsistency creates significant challenges when attempting to extract data for meta-analyses. Frequently, important details are missing, such as scores on the positive symptom subscale of the PANSS, while less critical information, like the total PANSS score, is provided instead. Most studies rely on the Last Observation Carried Forward (LOCF) approach, while a smaller number use the Mixed-Effect Model Repeated Measure (MMRM) method. In some cases, results are selectively reported from either model, despite each having its own strengths and limitations (358). Another notable issue is the inconsistency in reported sample sizes across different publications of the same original study. This lack of clarity further complicates data interpretation and comparison. To improve the quality and transparency of research, it is essential for study reports to adhere to CONSORT guidelines, ensuring that data is accurately and consistently presented for both researchers and clinicians.
9 Development of the actual guideline
One of the biggest challenges in developing treatment guidelines for BD is that research tends to treat BD as a collection of separate, independent phases, rather than as a single, interconnected disorder. This creates a critical dilemma for both clinicians and guideline developers: how should maintenance treatment be determined if a patient responded well to an acute-phase treatment, but there is little to no data on its long-term preventive effects—or worse if existing data suggest negative outcomes in the long run? For example, consider a patient who successfully responded to haloperidol for an acute manic episode. However, if this patient’s history shows that most of their past mood episodes were depressive, depression will likely remain the predominant issue in the future. This puts the clinician in a difficult position: should they add another medication with proven efficacy in preventing depressive episodes, such as quetiapine, resulting in combination therapy? Or should they switch to monotherapy with a drug that offers prophylactic protection against both manic and depressive episodes? There is no clear answer, and expert opinions vary, especially since most maintenance trials use enriched study samples—meaning that they only include patients who initially responded to the tested medication during the acute phase. This makes it even harder to determine what to do for patients who did not respond well to first-line treatment. Should the clinician switch medications, which might prolong suffering due to delayed stabilization? Or should they add another agent, increasing the risk of polypharmacy and side effects? Future research should prioritize finding solutions to these challenges. Ideally, all treatment options should be tested across all phases and clinical features of BD, so that those with the broadest efficacy are given priority in clinical use. Of course, even when broader efficacy is established, safety and tolerability concerns can further complicate treatment decisions, making it crucial to weigh both effectiveness and long-term patient well-being (5, 11, 346).
Designing the format of treatment guidelines presents its own set of challenges. One possible approach is to develop a precise, step-by-step algorithm based entirely on scientific evidence. This algorithm would be the final stage of guideline development, following the grading of available data and treatment recommendations. Such an algorithm would be strictly data-driven, providing clear and precise treatment pathways. However, it would likely be limited in its real-world clinical applicability. There would be no flexibility to accommodate individual patient nuances, as evidence-based decision-making would take absolute priority over clinical intuition or practical considerations. While it would reflect the most current state of scientific knowledge, it would lack the adaptability needed for everyday clinical practice, making its implementation challenging. Clinicians interested in using such a model would need to understand both its strengths and its limitations. Given the complexity of bipolar disorder treatment, such an algorithm may end up being so intricate that it could only be effectively applied through a digital tool, such as a mobile application, to guide decision-making in real-time.
An alternative approach to developing BD treatment guidelines is to incorporate clinical wisdom alongside research evidence. While this method introduces the risk of biases and, in some cases, may even lead to overlooking certain research findings, it would likely be more practical, easier to adopt, and more intuitive for clinicians in real-world practice. For guidelines to be effective and widely accepted, they should be rooted in solid research evidence while also being adaptable to everyday clinical challenges. A rigid, purely data-driven model may be scientifically sound but impractical, whereas an approach that blends research with real-world insights could enhance clinical decision-making and increase usability. Although the core framework of such guidelines should remain evidence-based, their interpretation and application should avoid excessively rigid interpretations of research findings. Instead, they should be structured in a way that acknowledges the complexity of BD and allows clinicians to make well-informed, patient-centered decisions without being constrained by an overly narrow or impractical set of recommendations.
10 Economic considerations
Estimating the true economic cost of BD is incredibly challenging due to its highly variable and unpredictable nature. The financial burden extends far beyond the direct costs of hospitalizations and medication—it also includes the expense of healthcare infrastructure, the impact of comorbid medical conditions, and indirect costs such as out-of-pocket expenses, lost productivity due to work absences, and even premature death (359). Because BD affects multiple aspects of a person’s life, its financial toll is not easily captured by traditional healthcare cost analyses. A comprehensive assessment must account for both short-term medical expenses and long-term socioeconomic consequences, ensuring that the full burden of the disorder is properly recognized and addressed.
In the UK, the total cost of BD was estimated at £2.055 billion in 1999/2000 prices (202). Notably, the majority of this cost (86%) was due to productivity loss and unemployment, while only 10% was directly related to National Health Service (NHS) expenses. Medication costs in primary care were relatively low at £8.5 million, making up just 0.4% of the total cost and 4.3% of NHS-related costs. However, a more recent analysis found that NHS costs had doubled, with medication expenses rising disproportionately to £25.2 million, accounting for 7.4% of NHS costs (360). In the United States, medication costs were minimal throughout the 1990s but increased significantly after 2000, eventually reaching 2% of the total cost, although exact figures remain unclear (204, 361–363). In Germany, the total annual cost of BD was estimated at 5.8 billion euros, with a staggering 98% attributed to productivity loss (364). Similar estimates have been reported worldwide, though figures vary depending on prevalence rates, healthcare systems, and societal structures (365–367). These findings highlight that the economic impact of BD extends far beyond direct medical costs, with lost productivity and unemployment being the largest financial burden, reinforcing the need for effective long-term management strategies to reduce both individual and societal costs.
While medication costs make up only a small fraction of the total cost of BD (368), they play a critical role in managing the illness. Effective pharmacological treatment is the foundation of BD management, enabling the resolution of acute episodes, reducing long-term impairment, and enhancing patient insight and treatment adherence. By stabilizing symptoms, medication also allows for other therapeutic interventions, such as psychotherapy, rehabilitation, and social support, to be more effective. However, in some parts of the world and during certain periods, medication costs have risen disproportionately, raising economic concerns. While cost-containment strategies—such as prioritizing cheaper medications over newer treatments—may seem appealing, they must be approached with caution. A short-term reduction in medication expenses that disregards clinical evidence could ultimately lead to a disproportionate increase in the total cost of BD, as poorly managed treatment could result in higher rates of hospitalization, disability, and lost productivity. Balancing cost efficiency with clinical effectiveness is essential to ensuring both financial sustainability and optimal patient outcomes.
11 Discussion
Just as BD is a complex and demanding condition to treat, developing treatment guidelines for BD presents an equally challenging task. Compared to more linear disorders such as schizophrenia or unipolar depression, BD is inherently more variable, requiring a more nuanced approach across all aspects of research, clinical practice, and treatment planning. Its episodic nature, diverse symptomatology, and fluctuating treatment needs make it difficult to establish one-size-fits-all recommendations. As a result, BD remains one of the most challenging psychiatric conditions to address, both in clinical care and in the development of structured treatment guidelines.
Guidelines should carefully address the unmet clinical needs that exist across all phases of BD, as these represent a key priority. Treatment guidelines are only truly valuable when they lead to improved outcomes, and this improvement must come from directly tackling the gaps in current care. A review of the literature suggests that early and accurate diagnosis, along with better education for patients and their families, may be among the most pressing unmet needs in bipolar disorder. However, research has also highlighted other significant issues, not only in terms of available treatment knowledge but also in the methods used to conduct clinical research. Addressing these gaps should be a fundamental goal in the development of more effective and applicable treatment guidelines.
One key takeaway message is that existing research may already hold answers to many clinical questions, including how to tailor treatment for specific patient subgroups. This could encourage guideline developers to rely heavily—if not entirely—on hard scientific data. However, the literature often lacks exhaustive analyses, and raw data are rarely made available. Maximizing the use of already collected data could have a more immediate impact on clinical practice than conducting new studies. Given the urgency of improving treatment outcomes, making these data accessible and conducting thorough analyses should be a priority for public health.
It is becoming increasingly clear that future RCTs should follow a standardized design that captures the full complexity of bipolar disorder. This means assessing manic, depressive, and psychotic symptoms simultaneously across all phases of the illness. Standardization would help reduce biases and inconsistencies that often arise due to the way studies are currently conducted. Equally important is the need for a uniform approach to reporting results. At present, only a limited and often fragmented portion of trial findings is made available, and it is not uncommon for different reports of the same study to present slightly varying figures. This raises concerns about the overall reliability of scientific reporting and highlights the need for greater transparency. Beyond summarizing and evaluating the evidence, treatment guidelines should also serve as an educational tool, promoting best practices and ensuring that clinicians have access to clear, consistent, and reliable information to guide patient care.
How clinicians would best use guidelines is an open question and difficult to answer. Simple logic and common sense dictate that studying them and including them in their library of knowledge will, by definition, improve clinical practice since it will improve the base of knowledge one relies on, even if no specific step is followed explicitly. Additionally, trying to chart individual cases on the landscape of treatment strategies and trajectories that guidelines provide, is expected to improve, at least partially, the outcome.
In conclusion, creating treatment guidelines for bipolar disorder is a complex and demanding task. It requires a thorough review of existing literature, including uncovering and analyzing unpublished data to fully understand its implications. Beyond gathering information, the real challenge lies in weaving together the fragmented research, which often focuses on isolated aspects of the disorder, into a cohesive framework for decision-making. A well-developed guideline must bridge past knowledge with present clinical decisions while anticipating future challenges. It should not only reflect the best available evidence but also provide a practical, forward-thinking approach to managing the disorder in real-world settings.
Apart from how guidelines should handle this fragmentation, it is necessary for future research to adopt a different approach and model of trial design; this should be more longitudinal with multiple clinically informed primary outcomes and interventions (341).
Author contributions
KNF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NKF: Conceptualization, Data curation, Investigation, Methodology, Resources, Validation, Visualization, Writing – review & editing. DA: Conceptualization, Data curation, Investigation, Methodology, Resources, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
KF has received grants and served as a consultant, advisor, or CME speaker for the following entities: AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Ferrer, Gedeon Richter, Janssen, Lundbeck, Otsuka, Pfizer, the Pfizer Foundation, Sanofi-Aventis, Servier, Shire and others. DA has received support for various farma industries to participate in congresses.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bauer M, Glenn T, Alda M, Andreassen OA, Angelopoulos E, Ardau R, et al. Influence of light exposure during early life on the age of onset of bipolar disorder. J Psychiatr Res. (2015) 64:1–8. doi: 10.1016/j.jpsychires.2015.03.013
2. Bauer M, Glenn T, Alda M, Andreassen OA, Angelopoulos E, Ardau R, et al. Relationship between sunlight and the age of onset of bipolar disorder: an international multisite study. J Affect Disord. (2014) 167:104–11. doi: 10.1016/j.jad.2014.05.032
3. Carvalho AF, Hyphantis TN, Taunay TC, Macêdo DS, Floros GD, Ottoni GL, et al. The relationship between affective temperaments, defensive styles and depressive symptoms in a large sample. J Affect Disord. (2013) 146:58–65. doi: 10.1016/j.jad.2012.08.038
4. Fountoulakis K. Treatment guidelines. In: Fountoulakis K, editor. Bipolar Disorder: An Evidence-Based Guide to Manic Depression. Springer-Verlag Berlin Heidelberg (2015). p. 643–58.
5. Fountoulakis KN. An update of evidence-based treatment of bipolar depression: where do we stand? Curr Opin Psychiatry. (2010) 23:19–24. doi: 10.1097/YCO.0b013e328333e132
6. Fountoulakis KN, Moeller HJ, and Kasper S. Personalised and precision psychiatry: what do the CINP bipolar guidelines suggest? Int J Psychiatry Clin Pract. (2019) 23:80–1. doi: 10.1080/13651501.2018.1470246
7. Goodwin GM, Haddad PM, Ferrier IN, Aronson JK, Barnes T, Cipriani A, et al. Evidence-based guidelines for treating bipolar disorder: Revised third edition recommendations from the British Association for Psychopharmacology. J Psychopharmacol. (2016) 30:495–553. doi: 10.1177/0269881116636545
8. Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Bond DJ, Frey BN, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. (2018) 20:97–170. doi: 10.1111/bdi.12609
9. Fountoulakis KN, Grunze H, Vieta E, Young A, Yatham L, Blier P, et al. The international college of neuro-psychopharmacology (CINP) treatment guidelines for bipolar disorder in adults (CINP-BD-2017), part 3: the clinical guidelines. Int J Neuropsychopharmacol. (2017) 20:180–95. doi: 10.1093/ijnp/pyw109
10. Fountoulakis KN, Magiria S, Siamouli M, Panagiotidis P, Nimatoudis I, Iacovides A, et al. A seven- year follow-up of an extremely refractory bipolar I patient. CNS Spectr. (2007) 12:733–4. doi: 10.1017/s109285290001539x
11. Fountoulakis KN, Yatham LN, Grunze H, Vieta E, Young AH, Blier P, et al. The CINP guidelines on the definition and evidence-based interventions for treatment-resistant bipolar disorder. Int J Neuropsychopharmacol. (2020) 23:230–56. doi: 10.1093/ijnp/pyz064
12. Woo YS, Bahk WM, Lee JG, Jeong JH, Kim MD, Sohn I, et al. Korean medication algorithm project for bipolar disorder 2018 (KMAP-BP 2018): fourth revision. Clin Psychopharmacol Neurosci. (2018) 16:434–48. doi: 10.9758/cpn.2018.16.4.434
13. NICE. Bipolar disorder guidelines 2020 amendment (CG185) (2020). Available online at: https://www.nice.org.uk/Guidance/Conditions-and-diseases/Mental-health-and-behavioural-conditions/Bipolar-disorder (Accessed March 30, 2025).
14. Malhi GS, Outhred T, Morris G, Boyce PM, Bryant R, Fitzgerald PB, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders: bipolar disorder summary. Med J Aust. (2018) 208:219–25. doi: 10.5694/mja17.00658
15. Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Azorin JM, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders: Acute and long-term treatment of mixed states in bipolar disorder. World J Biol Psychiatry. (2018) 19:2–58. doi: 10.1080/15622975.2017.1384850
16. Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Moller HJ, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2009 on the treatment of acute mania. World J Biol Psychiatry. (2009) 10:85–116. doi: 10.1080/15622970902823202
17. Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Moller HJ, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders: Update 2010 on the treatment of acute bipolar depression. World J Biol Psychiatry. (2010) 11:81–109. doi: 10.3109/15622970903555881
18. Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Moller HJ, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2012 on the long-term treatment of bipolar disorder. World J Biol Psychiatry. (2013) 14:154–219. doi: 10.3109/15622975.2013.770551
19. Fountoulakis KN. Treatment guidelines for mental disorders: reality or illusion? Psychiatriki. (2015) 26:89–92.
20. Hirschfeld RM, Lewis L, and Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. (2003) 64:161–74. doi: 10.4088/JCP.v64n0209
21. Lewis L. The national depressive and manic-depressive association: an introduction. Biol Psychiatry. (2000) 47:692. doi: 10.1016/s0006-3223(00)00827-1
22. Lish JD, Dime-Meenan S, Whybrow PC, Price RA, and Hirschfeld RM. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord. (1994) 31:281–94. doi: 10.1016/0165-0327(94)90104-x
23. Morselli PL, Elgie R, and Europe G. GAMIAN-Europe/BEAM survey I–global analysis of a patient questionnaire circulated to 3450 members of 12 European advocacy groups operating in the field of mood disorders. Bipolar Disord. (2003) 5:265–78. doi: 10.1034/j.1399-5618.2003.00037.x
24. Frye MA, Gitlin MJ, and Altshuler LL. Unmet needs in bipolar depression. Depress Anxiety. (2004) 19:199–208. doi: 10.1002/da.20013
25. Ketter TA. Nosology, diagnostic challenges, and unmet needs in managing bipolar disorder. J Clin Psychiatry. (2010) 71:e27. doi: 10.4088/JCP.8125tx12c
26. Vieta E. Antidepressants in bipolar I disorder: never as monotherapy. Am J Psychiatry. (2014) 171:1023–6. doi: 10.1176/appi.ajp.2014.14070826
27. Angst J. The bipolar spectrum. Br J Psychiatry. (2007) 190:189–91. doi: 10.1192/bjp.bp.106.030957
28. Angst J, Sellaro R, Stassen HH, and Gamma A. Diagnostic conversion from depression to bipolar disorders: results of a long-term prospective study of hospital admissions. J Affect Disord. (2005) 84:149–57. doi: 10.1016/S0165-0327(03)00195-2
29. Akiskal H. Mood Disorders. In: Sadock B and Sadock V, editors. Comprehensive Textbook of Psychiatry, vol. I . Lippincott Williams & Wilkins, Philadelphia (2000). p. 1338–77.
30. Fountoulakis KN, Gonda X, Siamouli M, and Rihmer Z. Psychotherapeutic intervention and suicide risk reduction in bipolar disorder: a review of the evidence. J Affect Disord. (2009) 113:21–9. doi: 10.1016/j.jad.2008.06.014
31. Fountoulakis KN, Iacovides A, Fotiou F, Nimatoudis J, Bascialla F, Ioannidou C, et al. Neurobiological and psychological correlates of suicidal attempts and thoughts of death in patients with major depression. Neuropsychobiology. (2004) 49:42–52. doi: 10.1159/000075338
32. Fountoulakis KN, Karakatsoulis GN, Abraham S, Adorjan K, Ahmed HU, Alarcon RD, et al. Somatic multicomorbidity and disability in patients with psychiatric disorders in comparison to the general population: a quasi-epidemiological investigation in 54,826 subjects from 40 countries (COMET-G study). CNS Spectr. (2024) 29:126–49. doi: 10.1017/S1092852924000026
33. Gonda X, Fountoulakis KN, Harro J, Pompili M, Akiskal HS, Bagdy G, et al. The possible contributory role of the S allele of 5-HTTLPR in the emergence of suicidality. J Psychopharmacol. (2011) 25:857–66. doi: 10.1177/0269881110376693
34. Rihmer Z, Gonda X, Rihmer A, and Fountoulakis KN. Suicidal and violent behaviour in mood disorders: A major public health problem. A review for the clinician. Int J Psychiatry Clin Pract. (2010) 14:88–94. doi: 10.3109/13651501003624712
35. Angst J. The course of affective disorders. II. Typology of bipolar manic-depressive illness. Arch Psychiatr Nervenkr (1970). (1978) 226:65–73. doi: 10.1007/BF00344125
36. Baldessarini RJ, Undurraga J, Vazquez GH, Tondo L, Salvatore P, Ha K, et al. Predominant recurrence polarity among 928 adult international bipolar I disorder patients. Acta Psychiatr Scand. (2012) 125:293–302. doi: 10.1111/j.1600-0447.2011.01818.x
37. Carvalho AF, McIntyre RS, Dimelis D, Gonda X, Berk M, Nunes-Neto PR, et al. Predominant polarity as a course specifier for bipolar disorder: a systematic review. J Affect Disord. (2014) 163:56–64. doi: 10.1016/j.jad.2014.03.035
38. Carvalho AF, Quevedo J, McIntyre RS, Soeiro-de-Souza MG, Fountoulakis KN, Berk M, et al. Treatment implications of predominant polarity and the polarity index: a comprehensive review. Int J Neuropsychopharmacol. (2014) 18. doi: 10.1093/ijnp/pyu079
39. Carvalho AF, Quevedo J, McIntyre RS, Soeiro-de-Souza MG, Fountoulakis KN, Berk M, et al. Treatment implications of predominant polarity and the polarity index: a comprehensive review. Int J Neuropsychopharmacol. (2015) 18:pyu079. doi: 10.1093/ijnp/pyu079
40. Colom F, Vieta E, Daban C, Pacchiarotti I, and Sanchez-Moreno J. Clinical and therapeutic implications of predominant polarity in bipolar disorder. J Affect Disord. (2006) 93:13–7. doi: 10.1016/j.jad.2006.01.032
41. García-López A, De Dios-Perrino C, and Ezquiaga E. P.3.e.007 Polarity of the first episode and predominant polarity in a cohort of bipolar outpatients. Eur Neuropsychopharmacol. (2009) 19:S571–1. doi: 10.1016/s0924-977x(09)70912-5
42. Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, et al. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry. (2003) 60:261–9. doi: 10.1001/archpsyc.60.3.261
43. Leonhard K. Die prapsychotische Temperamente bei den monopolaren und bipolaren phasischen Psychosen. Psychiat Neurol (Basel). (1963) 146:105–15.
44. Mazzarini L, Pacchiarotti I, Colom F, Sani G, Kotzalidis GD, Rosa AR, et al. Predominant polarity and temperament in bipolar and unipolar affective disorders. J Affect Disord. (2009) 119:28–33. doi: 10.1016/j.jad.2009.03.016
45. Nivoli AM, Pacchiarotti I, Rosa AR, Popovic D, Murru A, Valenti M, et al. Gender differences in a cohort study of 604 bipolar patients: the role of predominant polarity. J Affect Disord. (2011) 133:443–9. doi: 10.1016/j.jad.2011.04.055
46. Pacchiarotti I, Nivoli AM, Mazzarini L, Kotzalidis GD, Sani G, Koukopoulos A, et al. The symptom structure of bipolar acute episodes: in search for the mixing link. J Affect Disord. (2013) 149:56–66. doi: 10.1016/j.jad.2013.01.003
47. Perris C and d’Elia G. A study of bipolar (manic-depressive) and unipolar recurrent depressive psychoses. IX. therapy and prognosis. Acta Psychiatr Scand Suppl. (1966) 194:153–71. doi: 10.1111/j.1600-0447.1966.tb11018.x
48. Perris C and d’Elia G. A study of bipolar (manic-depressive) and unipolar recurrent depressive psychoses. X. Mortality, suicide and life-cycles. Acta Psychiatr Scand Suppl. (1966) 194:172–89. doi: 10.1111/j.1600-0447.1966.tb11019.x
49. Quitkin FM, Rabkin JG, and Prien RF. Bipolar disorder: are there manic-prone and depressive-prone forms? J Clin Psychopharmacol. (1986) 6:167–72.
50. Rosa AR, Andreazza AC, Kunz M, Gomes F, Santin A, Sanchez-Moreno J, et al. Predominant polarity in bipolar disorder: diagnostic implications. J Affect Disord. (2008) 107:45–51. doi: 10.1016/j.jad.2007.07.021
51. Tohen M, Frank E, Bowden CL, Colom F, Ghaemi SN, Yatham LN, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. (2009) 11:453–73. doi: 10.1111/j.1399-5618.2009.00726.x
52. Vieta E, Berk M, Wang W, Colom F, Tohen M, and Baldessarini RJ. Predominant previous polarity as an outcome predictor in a controlled treatment trial for depression in bipolar I disorder patients. J Affect Disord. (2009) 119:22–7. doi: 10.1016/j.jad.2009.02.028
53. Azorin JM, Kaladjian A, Adida M, Hantouche EG, Hameg A, Lancrenon S, et al. Factors associated with rapid cycling in bipolar I manic patients: findings from a French national study. CNS Spectr. (2008) 13:780–7. doi: 10.1017/s1092852900013900
54. Coryell W, Endicott J, and Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry. (1992) 49:126–31. doi: 10.1001/archpsyc.1992.01820020046006
55. Coryell W, Solomon D, Turvey C, Keller M, Leon AC, Endicott J, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. (2003) 60:914–20. doi: 10.1001/archpsyc.60.9.914
56. Cruz N, Vieta E, Comes M, Haro JM, Reed C, Bertsch J, et al. Rapid-cycling bipolar I disorder: course and treatment outcome of a large sample across Europe. J Psychiatr Res. (2008) 42:1068–75. doi: 10.1016/j.jpsychires.2007.12.004
57. Dittmann S, Biedermann NC, Grunze H, Hummel B, Scharer LO, Kleindienst N, et al. The Stanley Foundation Bipolar Network: results of the naturalistic follow-up study after 2.5 years of follow-up in the German centres. Neuropsychobiology. (2002) 46 Suppl 1:2–9. doi: 10.1159/000068018
58. Dunner DL and Fieve RR. Clinical factors in lithium carbonate prophylaxis failure. Arch Gen Psychiatry. (1974) 30:229–33. doi: 10.1001/archpsyc.1974.01760080077013
59. Garcia-Amador M, Colom F, Valenti M, Horga G, and Vieta E. Suicide risk in rapid cycling bipolar patients. J Affect Disord. (2009) 117:74–8. doi: 10.1016/j.jad.2008.12.005
60. Hajek T, Hahn M, Slaney C, Garnham J, Green J, Ruzickova M, et al. Rapid cycling bipolar disorders in primary and tertiary care treated patients. Bipolar Disord. (2008) 10:495–502. doi: 10.1111/j.1399-5618.2008.00587.x
61. Kramlinger KG and Post RM. Ultra-rapid and ultradian cycling in bipolar affective illness. Br J Psychiatry. (1996) 168:314–23. doi: 10.1192/bjp.168.3.314
62. Kukopulos A, Reginaldi D, Laddomada P, Floris G, Serra G, and Tondo L. Course of the manic-depressive cycle and changes caused by treatment. Pharmakopsychiatr Neuropsychopharmakol. (1980) 13:156–67. doi: 10.1055/s-2007-1019628
63. Lee S, Tsang A, Kessler RC, Jin R, Sampson N, Andrade L, et al. Rapid-cycling bipolar disorder: cross-national community study. Br J Psychiatry. (2010) 196:217–25. doi: 10.1192/bjp.bp.109.067843
64. Nurnberger J Jr., Guroff JJ, Hamovit J, Berrettini W, and Gershon E. A family study of rapid-cycling bipolar illness. J Affect Disord. (1988) 15:87–91. doi: 10.1016/0165-0327(88)90013-4
65. Schneck CD, Miklowitz DJ, Calabrese JR, Allen MH, Thomas MR, Wisniewski SR, et al. Phenomenology of rapid-cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry. (2004) 161:1902–8. doi: 10.1176/ajp.161.10.1902
66. Schneck CD, Miklowitz DJ, Miyahara S, Araga M, Wisniewski S, Gyulai L, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. (2008) 165:370–377; quiz 410. doi: 10.1176/appi.ajp.2007.05081484
67. Yildiz A and Sachs GS. Characteristics of rapid cycling bipolar-I patients in a bipolar speciality clinic. J Affect Disord. (2004) 79:247–51. doi: 10.1016/S0165-0327(02)00350-6
68. Burdick KE, Goldberg JF, and Harrow M. Neurocognitive dysfunction and psychosocial outcome in patients with bipolar I disorder at 15-year follow-up. Acta Psychiatr Scand. (2010) 122:499–506. doi: 10.1111/j.1600-0447.2010.01590.x
69. Mur M, Portella MJ, Martinez-Aran A, Pifarre J, and Vieta E. Influence of clinical and neuropsychological variables on the psychosocial and occupational outcome of remitted bipolar patients. Psychopathology. (2009) 42:148–56. doi: 10.1159/000207456
70. Martinez-Aran A, Vieta E, Colom F, Reinares M, Benabarre A, Torrent C, et al. Neuropsychological performance in depressed and euthymic bipolar patients. Neuropsychobiology. (2002) 46 Suppl 1:16–21. doi: 10.1159/000068016
71. Martinez-Aran A, Vieta E, Torrent C, Sanchez-Moreno J, Goikolea JM, Salamero M, et al. Functional outcome in bipolar disorder: the role of clinical and cognitive factors. Bipolar Disord. (2007) 9:103–13. doi: 10.1111/j.1399-5618.2007.00327.x
72. Cullen B, Ward J, Graham NA, Deary IJ, Pell JP, Smith DJ, et al. Prevalence and correlates of cognitive impairment in euthymic adults with bipolar disorder: A systematic review. J Affect Disord. (2016) 205:165–81. doi: 10.1016/j.jad.2016.06.063
73. Tsitsipa E and Fountoulakis KN. The neurocognitive functioning in bipolar disorder: a systematic review of data. Ann Gen Psychiatry. (2015) 14:42. doi: 10.1186/s12991-015-0081-z
74. Garriga M, Pacchiarotti I, Kasper S, Zeller SL, Allen MH, Vazquez G, et al. Assessment and management of agitation in psychiatry: Expert consensus. World J Biol Psychiatry. (2016) 17:86–128. doi: 10.3109/15622975.2015.1132007
75. Maj M. Psychiatric comorbidity”: an artefact of current diagnostic systems? Br J Psychiatry. (2005) 186:182–4. doi: 10.1192/bjp.186.3.182
76. Dell’Osso B, Buoli M, Bortolussi S, Camuri G, Vecchi V, and Altamura AC. Patterns of Axis I comorbidity in relation to age in patients with Bipolar Disorder: a cross-sectional analysis. J Affect Disord. (2011) 130:318–22. doi: 10.1016/j.jad.2010.10.008
77. Krishnan KR. Psychiatric and medical comorbidities of bipolar disorder. Psychosom Med. (2005) 67:1–8. doi: 10.1097/01.psy.0000151489.36347.18
78. Leverich GS, Altshuler LL, Frye MA, Suppes T, Keck PE Jr., McElroy SL, et al. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. J Clin Psychiatry. (2003) 64:506–15. doi: 10.4088/jcp.v64n0503
79. Mantere O, Melartin TK, Suominen K, Rytsala HJ, Valtonen HM, Arvilommi P, et al. Differences in Axis I and II comorbidity between bipolar I and II disorders and major depressive disorder. J Clin Psychiatry. (2006) 67:584–93. doi: 10.4088/jcp.v67n0409
80. McElroy SL, Altshuler LL, Suppes T, Keck PE Jr., Frye MA, Denicoff KD, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry. (2001) 158:420–6. doi: 10.1176/appi.ajp.158.3.420
81. Preti A, Vrublevska J, Veroniki AA, Huedo-Medina TB, and Fountoulakis KN. Prevalence, impact and treatment of generalised anxiety disorder in bipolar disorder: a systematic review and meta-analysis. Evid Based Ment Health. (2016) 19:73–81. doi: 10.1136/eb-2016-102412
82. Sasson Y, Chopra M, Harrari E, Amitai K, and Zohar J. Bipolar comorbidity: from diagnostic dilemmas to therapeutic challenge. Int J Neuropsychopharmacol. (2003) 6:139–44. doi: 10.1017/S1461145703003432
83. Strakowski SM, Tohen M, Stoll AL, Faedda GL, and Goodwin DC. Comorbidity in mania at first hospitalization. Am J Psychiatry. (1992) 149:554–6. doi: 10.1176/ajp.149.4.554
84. Subramaniam M, Abdin E, Vaingankar JA, and Chong SA. Prevalence, correlates, comorbidity and severity of bipolar disorder: results from the Singapore Mental Health Study. J Affect Disord. (2013) 146:189–96. doi: 10.1016/j.jad.2012.09.002
85. Tohen M, Zarate CA Jr., Hennen J, Khalsa HM, Strakowski SM, Gebre-Medhin P, et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. (2003) 160:2099–107. doi: 10.1176/appi.ajp.160.12.2099
86. Vieta E, Colom F, Corbella B, Martinez-Aran A, Reinares M, Benabarre A, et al. Clinical correlates of psychiatric comorbidity in bipolar I patients. Bipolar Disord. (2001) 3:253–8. doi: 10.1034/j.1399-5618.2001.30504.x
87. Bellani M, Hatch JP, Nicoletti MA, Ertola AE, Zunta-Soares G, Swann AC, et al. Does anxiety increase impulsivity in patients with bipolar disorder or major depressive disorder? J Psychiatr Res. (2012) 46:616–21. doi: 10.1016/j.jpsychires.2012.01.016
88. Oreski I, Jakovljevic M, Aukst-Margetic B, Orlic ZC, and Vuksan-Cusa B. Comorbidity and multimorbidity in patients with schizophrenia and bipolar disorder: similarities and differencies. Psychiatr Danub. (2012) 24:80–5.
89. Moor S, Crowe M, Luty S, Carter J, and Joyce PR. Effects of comorbidity and early age of onset in young people with Bipolar Disorder on self harming behaviour and suicide attempts. J Affect Disord. (2012) 136:1212–5. doi: 10.1016/j.jad.2011.10.018
90. Young LT, Cooke RG, Robb JC, Levitt AJ, and Joffe RT. Anxious and non-anxious bipolar disorder. J Affect Disord. (1993) 29:49–52. doi: 10.1016/0165-0327(93)90118-4
91. Altshuler LL, Kupka RW, Hellemann G, Frye MA, Sugar CA, McElroy SL, et al. Gender and depressive symptoms in 711 patients with bipolar disorder evaluated prospectively in the Stanley Foundation bipolar treatment outcome network. Am J Psychiatry. (2010) 167:708–15. doi: 10.1176/appi.ajp.2009.09010105
92. Azorin JM, Kaladjian A, Adida M, Hantouche EG, Hameg A, Lancrenon S, et al. Psychopathological correlates of lifetime anxiety comorbidity in bipolar I patients: findings from a French national cohort. Psychopathology. (2009) 42:380–6. doi: 10.1159/000241193
93. Boylan KR, Bieling PJ, Marriott M, Begin H, Young LT, and MacQueen GM. Impact of comorbid anxiety disorders on outcome in a cohort of patients with bipolar disorder. J Clin Psychiatry. (2004) 65:1106–13. doi: 10.4088/jcp.v65n0813
94. Ciapparelli A, Paggini R, Marazziti D, Carmassi C, Bianchi M, Taponecco C, et al. Comorbidity with axis I anxiety disorders in remitted psychotic patients 1 year after hospitalization. CNS Spectr. (2007) 12:913–9. doi: 10.1017/s1092852900015704
95. Cosoff SJ and Hafner RJ. The prevalence of comorbid anxiety in schizophrenia, schizoaffective disorder and bipolar disorder. Aust N Z J Psychiatry. (1998) 32:67–72. doi: 10.3109/00048679809062708
96. Das A. Anxiety disorders in bipolar I mania: prevalence, effect on illness severity, and treatment implications. Indian J Psychol Med. (2013) 35:53–9. doi: 10.4103/0253-7176.112202
97. Freeman MP, Freeman SA, and McElroy SL. The comorbidity of bipolar and anxiety disorders: prevalence, psychobiology, and treatment issues. J Affect Disord. (2002) 68:1–23. doi: 10.1016/s0165-0327(00)00299-8
98. Goldstein BI and Levitt AJ. The specific burden of comorbid anxiety disorders and of substance use disorders in bipolar I disorder. Bipolar Disord. (2008) 10:67–78. doi: 10.1111/j.1399-5618.2008.00461.x
99. Henry C, Van den Bulke D, Bellivier F, Etain B, Rouillon F, and Leboyer M. Anxiety disorders in 318 bipolar patients: prevalence and impact on illness severity and response to mood stabilizer. J Clin Psychiatry. (2003) 64:331–5. doi: 10.4088/JCP.v64n0316
100. Kawa I, Carter JD, Joyce PR, Doughty CJ, Frampton CM, Wells JE, et al. Gender differences in bipolar disorder: age of onset, course, comorbidity, and symptom presentation. Bipolar Disord. (2005) 7:119–25. doi: 10.1111/j.1399-5618.2004.00180.x
101. Kessler RC, Rubinow DR, Holmes C, Abelson JM, and Zhao S. The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychol Med. (1997) 27:1079–89. doi: 10.1017/s0033291797005333
102. Levander E, Frye MA, McElroy S, Suppes T, Grunze H, Nolen WA, et al. Alcoholism and anxiety in bipolar illness: differential lifetime anxiety comorbidity in bipolar I women with and without alcoholism. J Affect Disord. (2007) 101:211–7. doi: 10.1016/j.jad.2006.11.023
103. Mantere O, Isometsa E, Ketokivi M, Kiviruusu O, Suominen K, Valtonen HM, et al. A prospective latent analyses study of psychiatric comorbidity of DSM-IV bipolar I and II disorders. Bipolar Disord. (2010) 12:271–84. doi: 10.1111/j.1399-5618.2010.00810.x
104. Nakagawa A, Grunebaum MF, Sullivan GM, Currier D, Ellis SP, Burke AK, et al. Comorbid anxiety in bipolar disorder: does it have an independent effect on suicidality? Bipolar Disord. (2008) 10:530–8. doi: 10.1111/j.1399-5618.2008.00590.x
105. Nery-Fernandes F, Quarantini LC, Galvao-De-Almeida A, Rocha MV, Kapczinski F, and Miranda-Scippa A. Lower rates of comorbidities in euthymic bipolar patients. World J Biol Psychiatry. (2009) 10:474–9. doi: 10.1080/15622970802688929
106. Otto MW, Simon NM, Wisniewski SR, Miklowitz DJ, Kogan JN, Reilly-Harrington NA, et al. Prospective 12-month course of bipolar disorder in out-patients with and without comorbid anxiety disorders. Br J Psychiatry. (2006) 189:20–5. doi: 10.1192/bjp.bp.104.007773
107. Schaffer A, Cairney J, Cheung A, Veldhuizen S, and Levitt A. Community survey of bipolar disorder in Canada: lifetime prevalence and illness characteristics. Can J Psychiatry. (2006) 51:9–16. doi: 10.1177/070674370605100104
108. Simon NM, Otto MW, Wisniewski SR, Fossey M, Sagduyu K, Frank E, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry. (2004) 161:2222–9. doi: 10.1176/appi.ajp.161.12.2222
109. Szadoczky E, Papp Z, Vitrai J, Rihmer Z, and Furedi J. The prevalence of major depressive and bipolar disorders in Hungary. Results from a national epidemiologic survey. J Affect Disord. (1998) 50:153–62. doi: 10.1016/s0165-0327(98)00056-1
110. Tamam L and Ozpoyraz N. Comorbidity of anxiety disorder among patients with bipolar I disorder in remission. Psychopathology. (2002) 35:203–9. doi: 10.1159/000063824
111. Weber NS, Fisher JA, Cowan DN, and Niebuhr DW. Psychiatric and general medical conditions comorbid with bipolar disorder in the National Hospital Discharge Survey. Psychiatr Serv. (2011) 62:1152–8. doi: 10.1176/ps.62.10.pss6210_1152
112. Young S, Pfaff D, Lewandowski KE, Ravichandran C, Cohen BM, and Ongur D. Anxiety disorder comorbidity in bipolar disorder, schizophrenia and schizoaffective disorder. Psychopathology. (2013) 46:176–85. doi: 10.1159/000339556
113. Zutshi A, Reddy YC, Thennarasu K, and Chandrashekhar CR. Comorbidity of anxiety disorders in patients with remitted bipolar disorder. Eur Arch Psychiatry Clin Neurosci. (2006) 256:428–36. doi: 10.1007/s00406-006-0658-2
114. Coryell W, Solomon DA, Fiedorowicz JG, Endicott J, Schettler PJ, and Judd LL. Anxiety and outcome in bipolar disorder. Am J Psychiatry. (2009) 166:1238–43. doi: 10.1176/appi.ajp.2009.09020218
115. Swann AC. The strong relationship between bipolar and substance-use disorder. Ann N Y Acad Sci. (2010) 1187:276–93. doi: 10.1111/j.1749-6632.2009.05146.x
116. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. (1990) 264:2511–8. doi: 10.1001/jama.1990.03450190043026
117. Duffy A, Horrocks J, Milin R, Doucette S, Persson G, and Grof P. Adolescent substance use disorder during the early stages of bipolar disorder: a prospective high-risk study. J Affect Disord. (2012) 142:57–64. doi: 10.1016/j.jad.2012.04.010
118. Cerullo MA and Strakowski SM. The prevalence and significance of substance use disorders in bipolar type I and II disorder. Subst Abuse Treat Prev Policy. (2007) 2:29. doi: 10.1186/1747-597X-2-29
119. Lagerberg TV, Andreassen OA, Ringen PA, Berg AO, Larsson S, Agartz I, et al. Excessive substance use in bipolar disorder is associated with impaired functioning rather than clinical characteristics, a descriptive study. BMC Psychiatry. (2010) 10:9. doi: 10.1186/1471-244X-10-9
120. Di Florio A, Craddock N, and van den Bree M. Alcohol misuse in bipolar disorder. A systematic review and meta-analysis of comorbidity rates. Eur Psychiatry. (2014) 29:117–24. doi: 10.1016/j.eurpsy.2013.07.004
121. Estroff TW, Dackis CA, Gold MS, and Pottash AL. Drug abuse and bipolar disorders. Int J Psychiatry Med. (1985) 15:37–40. doi: 10.2190/6d4m-j23x-l21c-tp21
122. Farren CK, Hill KP, and Weiss RD. Bipolar disorder and alcohol use disorder: a review. Curr Psychiatry Rep. (2012) 14:659–66. doi: 10.1007/s11920-012-0320-9
123. Freed EX. Alcohol abuse by manic patients. Psychol Rep. (1969) 25:280. doi: 10.2466/pr0.1969.25.1.280
124. Lai HM, Sitharthan T, and Huang QR. Exploration of the comorbidity of alcohol use disorders and mental health disorders among inpatients presenting to all hospitals in New South Wales, Australia. Subst Abus. (2012) 33:138–45. doi: 10.1080/08897077.2011.634967
125. Morrison JR. Bipolar affective disorder and alcoholism. Am J Psychiatry. (1974) 131:1130–3. doi: 10.1176/ajp.131.10.1130
126. Goodwin F and Jamison K. Manic-depressive illness. 2nd ed. New York: Oxford University Press (2007).
127. Lai HM and Sitharthan T. Exploration of the comorbidity of cannabis use disorders and mental health disorders among inpatients presenting to all hospitals in New South Wales, Australia. Am J Drug Alcohol Abuse. (2012) 38:567–74. doi: 10.3109/00952990.2012.694523
128. Kennedy SH, Welsh BR, Fulton K, Soczynska JK, McIntyre RS, O’Donovan C, et al. Frequency and correlates of gambling problems in outpatients with major depressive disorder and bipolar disorder. Can J Psychiatry. (2010) 55:568–76. doi: 10.1177/070674371005500905
129. McIntyre RS, McElroy SL, Konarski JZ, Soczynska JK, Wilkins K, and Kennedy SH. Problem gambling in bipolar disorder: results from the Canadian Community Health Survey. J Affect Disord. (2007) 102:27–34. doi: 10.1016/j.jad.2006.12.005
130. Chengappa KN, Levine J, Gershon S, and Kupfer DJ. Lifetime prevalence of substance or alcohol abuse and dependence among subjects with bipolar I and II disorders in a voluntary registry. Bipolar Disord. (2000) 2:191–5. doi: 10.1034/j.1399-5618.2000.020306.x
131. Weiss RD and Mirin SM. Subtypes of cocaine abusers. Psychiatr Clin North Am. (1986) 9:491–501. doi: 10.1016/S0193-953X(18)30608-7
132. Weiss RD, Mirin SM, Michael JL, and Sollogub AC. Psychopathology in chronic cocaine abusers. Am J Drug Alcohol Abuse. (1986) 12:17–29. doi: 10.3109/00952998609083740
133. Miller FT, Busch F, and Tanenbaum JH. Drug abuse in schizophrenia and bipolar disorder. Am J Drug Alcohol Abuse. (1989) 15:291–5. doi: 10.3109/00952998908993409
134. Himmelhoch JM, Mulla D, Neil JF, Detre TP, and Kupfer DJ. Incidence and signficiance of mixed affective states in a bipolar population. Arch Gen Psychiatry. (1976) 33:1062–6. doi: 10.1001/archpsyc.1976.01770090052004
136. Goldberg JF and Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry. (2002) 63:791–5. doi: 10.4088/jcp.v63n0907
137. Magalhaes PV, Kapczinski F, Nierenberg AA, Deckersbach T, Weisinger D, Dodd S, et al. Illness burden and medical comorbidity in the Systematic Treatment Enhancement Program for Bipolar Disorder. Acta Psychiatr Scand. (2012) 125:303–8. doi: 10.1111/j.1600-0447.2011.01794.x
138. McIntyre RS, McElroy SL, Konarski JZ, Soczynska JK, Bottas A, Castel S, et al. Substance use disorders and overweight/obesity in bipolar I disorder: preliminary evidence for competing addictions. J Clin Psychiatry. (2007) 68:1352–7. doi: 10.4088/jcp.v68n0905
139. Meade CS, Graff FS, Griffin ML, and Weiss RD. HIV risk behavior among patients with co-occurring bipolar and substance use disorders: associations with mania and drug abuse. Drug Alcohol Depend. (2008) 92:296–300. doi: 10.1016/j.drugalcdep.2007.07.013
140. Goldstein BI, Strober MA, Birmaher B, Axelson DA, Esposito-Smythers C, Goldstein TR, et al. Substance use disorders among adolescents with bipolar spectrum disorders. Bipolar Disord. (2008) 10:469–78. doi: 10.1111/j.1399-5618.2008.00584.x
141. Daban C, Martinez-Aran A, Torrent C, Tabares-Seisdedos R, Balanza-Martinez V, Salazar-Fraile J, et al. Specificity of cognitive deficits in bipolar disorder versus schizophrenia. A systematic review. Psychother Psychosom. (2006) 75:72–84. doi: 10.1159/000090891
142. Goldberg JF, Harrow M, and Grossman LS. Course and outcome in bipolar affective disorder: a longitudinal follow-up study. Am J Psychiatry. (1995) 152:379–84. doi: 10.1176/ajp.152.3.379
143. Goldberg JF, Harrow M, and Grossman LS. Recurrent affective syndromes in bipolar and unipolar mood disorders at follow-up. Br J Psychiatry. (1995) 166:382–5. doi: 10.1192/bjp.166.3.382
144. Keck PE Jr., McElroy SL, Strakowski SM, West SA, Sax KW, Hawkins JM, et al. 12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry. (1998) 155:646–52. doi: 10.1176/ajp.155.5.646
145. Mur M, Portella MJ, Martinez-Aran A, Pifarre J, and Vieta E. Persistent neuropsychological deficit in euthymic bipolar patients: executive function as a core deficit. J Clin Psychiatry. (2007) 68:1078–86. doi: 10.4088/jcp.v68n0715
146. Strakowski SM, Keck PE Jr., McElroy SL, West SA, Sax KW, Hawkins JM, et al. Twelve-month outcome after a first hospitalization for affective psychosis. Arch Gen Psychiatry. (1998) 55:49–55. doi: 10.1001/archpsyc.55.1.49
147. Dore G and Romans SE. Impact of bipolar affective disorder on family and partners. J Affect Disord. (2001) 67:147–58. doi: 10.1016/s0165-0327(01)00450-5
148. Huxley N and Baldessarini RJ. Disability and its treatment in bipolar disorder patients. Bipolar Disord. (2007) 9:183–96. doi: 10.1111/j.1399-5618.2007.00430.x
149. Murray CJL and Lopez AD eds. The global burden of disease. A comprehensive assessment of the mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Boston, MA: Harvard School of Public Health on behalf of the World Health Organisation, and the World Bank (1996).
150. Pope M, Dudley R, and Scott J. Determinants of social functioning in bipolar disorder. Bipolar Disord. (2007) 9:38–44. doi: 10.1111/j.1399-5618.2007.00323.x
151. Simon GE. Social and economic burden of mood disorders. Biol Psychiatry. (2003) 54:208–15. doi: 10.1016/s0006-3223(03)00420-7
152. Gutierrez-Rojas L, Jurado D, and Gurpegui M. Factors associated with work, social life and family life disability in bipolar disorder patients. Psychiatry Res. (2011) 186:254–60. doi: 10.1016/j.psychres.2010.06.020
153. Judd LL, Schettler PJ, Solomon DA, Maser JD, Coryell W, Endicott J, et al. Psychosocial disability and work role function compared across the long-term course of bipolar I, bipolar II and unipolar major depressive disorders. J Affect Disord. (2008) 108:49–58. doi: 10.1016/j.jad.2007.06.014
154. Bauer M, Glenn T, Grof P, Rasgon NL, Marsh W, Sagduyu K, et al. Frequency of subsyndromal symptoms and employment status in patients with bipolar disorder. Soc Psychiatry Psychiatr Epidemiol. (2009) 44:515–22. doi: 10.1007/s00127-008-0464-4
155. Bowden CL and Krishnan AA. Pharmacotherapy for bipolar depression: an economic assessment. Expert Opin Pharmacother. (2004) 5:1101–7. doi: 10.1517/14656566.5.5.1101
156. Bowie CR, Depp C, McGrath JA, Wolyniec P, Mausbach BT, Thornquist MH, et al. Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am J Psychiatry. (2010) 167:1116–24. doi: 10.1176/appi.ajp.2010.09101406
157. Judd LL, Akiskal HS, Schettler PJ, Endicott J, Leon AC, Solomon DA, et al. Psychosocial disability in the course of bipolar I and II disorders: a prospective, comparative, longitudinal study. Arch Gen Psychiatry. (2005) 62:1322–30. doi: 10.1001/archpsyc.62.12.1322
158. Kauer-Sant’Anna M, Bond DJ, Lam RW, and Yatham LN. Functional outcomes in first-episode patients with bipolar disorder: a prospective study from the Systematic Treatment Optimization Program for Early Mania project. Compr Psychiatry. (2009) 50:1–8. doi: 10.1016/j.comppsych.2008.05.013
159. Marangell LB. The importance of subsyndromal symptoms in bipolar disorder. J Clin Psychiatry. (2004) 65 Suppl 10:24–7.
160. Rosa AR, Reinares M, Michalak EE, Bonnin CM, Sole B, Franco C, et al. Functional impairment and disability across mood states in bipolar disorder. Value Health. (2010) 13:984–8. doi: 10.1111/j.1524-4733.2010.00768.x
161. Sanchez-Moreno J, Martinez-Aran A, Tabares-Seisdedos R, Torrent C, Vieta E, and Ayuso-Mateos JL. Functioning and disability in bipolar disorder: an extensive review. Psychother Psychosom. (2009) 78:285–97. doi: 10.1159/000228249
162. Simon GE, Bauer MS, Ludman EJ, Operskalski BH, and Unutzer J. Mood symptoms, functional impairment, and disability in people with bipolar disorder: specific effects of mania and depression. J Clin Psychiatry. (2007) 68:1237–45. doi: 10.4088/jcp.v68n0811
163. Wingo AP, Baldessarini RJ, Compton MT, and Harvey PD. Correlates of recovery of social functioning in types I and II bipolar disorder patients. Psychiatry Res. (2010) 177:131–4. doi: 10.1016/j.psychres.2010.02.020
164. Depp CA, Davis CE, Mittal D, Patterson TL, and Jeste DV. Health-related quality of life and functioning of middle-aged and elderly adults with bipolar disorder. J Clin Psychiatry. (2006) 67:215–21. doi: 10.4088/jcp.v67n0207
165. Michalak EE, Murray G, Young AH, and Lam RW. Burden of bipolar depression: impact of disorder and medications on quality of life. CNS Drugs. (2008) 22:389–406. doi: 10.2165/00023210-200822050-00003
166. Ozer S, Ulusahin A, Batur S, Kabakci E, and Saka MC. Outcome measures of interepisode bipolar patients in a Turkish sample. Soc Psychiatry Psychiatr Epidemiol. (2002) 37:31–7. doi: 10.1007/s127-002-8211-z
167. Depp CA, Mausbach BT, Eyler LT, Palmer BW, Cain AE, Lebowitz BD, et al. Performance-based and subjective measures of functioning in middle-aged and older adults with bipolar disorder. J Nerv Ment Dis. (2009) 197:471–5. doi: 10.1097/NMD.0b013e3181ab5c9b
168. Chand PK, Mattoo SK, and Sharan P. Quality of life and its correlates in patients with bipolar disorder stabilized on lithium prophylaxis. Psychiatry Clin Neurosci. (2004) 58:311–8. doi: 10.1111/j.1440-1819.2004.01237.x
169. Brodaty H and Green A. Who cares for the carer? The often forgotten patient. Aust Fam Physician. (2002) 31:833–6.
170. Lowery K, Mynt P, Aisbett J, Dixon T, O’Brien J, and Ballard C. Depression in the carers of dementia sufferers: a comparison of the carers of patients suffering from dementia with Lewy bodies and the carers of patients with Alzheimer’s disease. J Affect Disord. (2000) 59:61–5. doi: 10.1016/s0165-0327(99)00123-8
171. Platt S. Measuring the burden of psychiatric illness on the family: an evaluation of some rating scales. Psychol Med. (1985) 15:383–93. doi: 10.1017/s0033291700023680
172. Fadden G, Bebbington P, and Kuipers L. The burden of care: the impact of functional psychiatric illness on the patient’s family. Br J Psychiatry. (1987) 150:285–92. doi: 10.1192/bjp.150.3.285
173. Grad J and Sainbury M. Evaluating a community care service. In: Freeman H and Farndale J, editors. Trends in mental health services. Pergamon Press, Oxford (1963).
174. Grad J and Sainsbury P. Mental illness and the family. Lancet. (1963) 1:544–7. doi: 10.1016/s0140-6736(63)91339-4
175. Hoenig J and Hamilton M. The desegregation of the mentally ill. London: Routledge and Keegan-Paul (1969).
176. Hoenig J and Hamilton MW. The schizophrenic patient in the community and his effect on the household. Int J Soc Psychiatry. (1966) 12:165–76. doi: 10.1177/002076406601200301
177. Chakrabarti S and Gill S. Coping and its correlates among caregivers of patients with bipolar disorder: a preliminary study. Bipolar Disord. (2002) 4:50–60. doi: 10.1034/j.1399-5618.2002.01167.x
178. Cook JA, Lefley HP, Pickett SA, and Cohler BJ. Age and family burden among parents of offspring with severe mental illness. Am J Orthopsychiatry. (1994) 64:435–47. doi: 10.1037/h0079535
179. Maji KR, Sood M, Sagar R, and Khandelwal SK. A follow-up study of family burden in patients with bipolar affective disorder. Int J Soc Psychiatry. (2012) 58:217–23. doi: 10.1177/0020764010390442
180. Perlick D, Clarkin JF, Sirey J, Raue P, Greenfield S, Struening E, et al. Burden experienced by care-givers of persons with bipolar affective disorder. Br J Psychiatry. (1999) 175:56–62. doi: 10.1192/bjp.175.1.56
181. Perlick DA, Rosenheck RA, Miklowitz DJ, Chessick C, Wolff N, Kaczynski R, et al. Prevalence and correlates of burden among caregivers of patients with bipolar disorder enrolled in the Systematic Treatment Enhancement Program for Bipolar Disorder. Bipolar Disord. (2007) 9:262–73. doi: 10.1111/j.1399-5618.2007.00365.x
182. Chakrabarti S, Kulhara P, and Verma SK. Extent and determinants of burden among families of patients with affective disorders. Acta Psychiatr Scand. (1992) 86:247–52. doi: 10.1111/j.1600-0447.1992.tb03261.x
183. Amore M, Menchetti M, Tonti C, Scarlatti F, Lundgren E, Esposito W, et al. Predictors of violent behavior among acute psychiatric patients: clinical study. Psychiatry Clin Neurosci. (2008) 62:247–55. doi: 10.1111/j.1440-1819.2008.01790.x
184. Currier GW and Allen MH. Emergency psychiatry: physical and chemical restraint in the psychiatric emergency service. Psychiatr Serv. (2000) 51:717–9. doi: 10.1176/appi.ps.51.6.717
185. Raveendranathan D, Chandra PS, and Chaturvedi SK. Violence among psychiatric inpatients: a victim’s perspective. East Asian Arch Psychiatry. (2012) 22:141–5.
186. Targum SD, Dibble ED, Davenport YB, and Gershon ES. The Family Attitudes Questionnaire. Patients’ and spouses’ views of bipolar illness. Arch Gen Psychiatry. (1981) 38:562–8. doi: 10.1001/archpsyc.1980.01780300074009
187. Eisdorfer C. Caregiving: an emerging risk factor for emotional and physical pathology. Bull Menninger Clin. (1991) 55:238–47.
188. Gallagher SK and Mechanic D. Living with the mentally ill: effects on the health and functioning of other household members. Soc Sci Med. (1996) 42:1691–701. doi: 10.1016/0277-9536(95)00296-0
189. Iacovides A, Fountoulakis K, Moysidou C, and Ierodiakonou C. Burnout in nursing staff: a clinical syndrome rather than a psychological reaction? Gen Hosp Psychiatry. (1997) 19:419–28.
190. Perlick DA, Hohenstein JM, Clarkin JF, Kaczynski R, and Rosenheck RA. Use of mental health and primary care services by caregivers of patients with bipolar disorder: a preliminary study. Bipolar Disord. (2005) 7:126–35. doi: 10.1111/j.1399-5618.2004.00172.x
191. Perlick DA, Rosenheck RA, Miklowitz DJ, Kaczynski R, Link B, Ketter T, et al. Caregiver burden and health in bipolar disorder: a cluster analytic approach. J Nerv Ment Dis. (2008) 196:484–91. doi: 10.1097/NMD.0b013e3181773927
192. Steele A, Maruyama N, and Galynker I. Psychiatric symptoms in caregivers of patients with bipolar disorder: a review. J Affect Disord. (2010) 121:10–21. doi: 10.1016/j.jad.2009.04.020
193. Angst J, Angst F, Gerber-Werder R, and Gamma A. Suicide in 406 mood-disorder patients with and without long-term medication: a 40 to 44 years’ follow-up. Arch Suicide Res. (2005) 9:279–300. doi: 10.1080/13811110590929488
194. Goodwin FK, Jamison KR, and Goodwin F. Suicide. In: Goodwin FK and Jamison KR, editors. Manic-depressive illness. Oxford University Press, New York (1990). p. 227–44.
195. Guze SB and Robins E. Suicide and primary affective disorders. Br J Psychiatry. (1970) 117:437–8. doi: 10.1192/bjp.117.539.437
196. Harris EC and Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. (1997) 170:205–28. doi: 10.1192/bjp.170.3.205
197. Elizabeth Sublette M, Carballo JJ, Moreno C, Galfalvy HC, Brent DA, Birmaher B, et al. Substance use disorders and suicide attempts in bipolar subtypes. J Psychiatr Res. (2009) 43:230–8. doi: 10.1016/j.jpsychires.2008.05.001
198. Oquendo MA, Currier D, Liu SM, Hasin DS, Grant BF, and Blanco C. Increased risk for suicidal behavior in comorbid bipolar disorder and alcohol use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry. (2010) 71:902–9. doi: 10.4088/JCP.09m05198gry
199. McCarthy JF, Valenstein M, Zivin K, Zeber JE, and Kilbourne AM. Access-related measures and out-of-system utilization among veterans with bipolar disorder. Psychiatr Serv. (2010) 61:1035–8. doi: 10.1176/ps.2010.61.10.1035
200. Centorrino F, Mark TL, Talamo A, Oh K, and Chang J. Health and economic burden of metabolic comorbidity among individuals with bipolar disorder. J Clin Psychopharmacol. (2009) 29:595–600. doi: 10.1097/JCP.0b013e3181bef8a6
201. Chisholm D, van Ommeren M, Ayuso-Mateos JL, and Saxena S. Cost-effectiveness of clinical interventions for reducing the global burden of bipolar disorder. Br J Psychiatry. (2005) 187:559–67. doi: 10.1192/bjp.187.6.559
202. Das Gupta R and Guest JF. Annual cost of bipolar disorder to UK society. Br J Psychiatry. (2002) 180:227–33. doi: 10.1192/bjp.180.3.227
203. de Zelicourt M, Dardennes R, Verdoux H, Gandhi G, Khoshnood B, Chomette E, et al. Frequency of hospitalisations and inpatient care costs of manic episodes: in patients with bipolar I disorder in France. Pharmacoeconomics. (2003) 21:1081–90. doi: 10.2165/00019053-200321150-00002
204. Dilsaver SC. An estimate of the minimum economic burden of bipolar I and II disorders in the United States: 2009. J Affect Disord. (2011) 129:79–83. doi: 10.1016/j.jad.2010.08.030
205. Fajutrao L, Locklear J, Priaulx J, and Heyes A. A systematic review of the evidence of the burden of bipolar disorder in Europe. Clin Pract Epidemiol Ment Health. (2009) 5:3. doi: 10.1186/1745-0179-5-3
206. Olie JP and Levy E. Manic episodes: the direct cost of a three-month period following hospitalisation. Eur Psychiatry. (2002) 17:278–86. doi: 10.1016/s0924-9338(02)00680-6
207. Brook RA, Rajagopalan K, Kleinman NL, Smeeding JE, Brizee TJ, and Gardner HH. Incurring greater health care costs: risk stratification of employees with bipolar disorder. Prim Care Companion J Clin Psychiatry. (2006) 8:17–24. doi: 10.4088/pcc.v08n0103
208. Peele PB, Xu Y, and Kupfer DJ. Insurance expenditures on bipolar disorder: clinical and parity implications. Am J Psychiatry. (2003) 160:1286–90. doi: 10.1176/appi.ajp.160.7.1286
209. Stender M, Bryant-Comstock L, and Phillips S. Medical resource use among patients treated for bipolar disorder: a retrospective, cross-sectional, descriptive analysis. Clin Ther. (2002) 24:1668–76. doi: 10.1016/s0149-2918(02)80070-4
210. Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. (2011) 68:241–51. doi: 10.1001/archgenpsychiatry.2011.12
211. Kilbourne AM, Perron BE, Mezuk B, Welsh D, Ilgen M, and Bauer MS. Co-occurring conditions and health-related quality of life in patients with bipolar disorder. Psychosom Med. (2009) 71:894–900. doi: 10.1097/PSY.0b013e3181b49948
212. McIntyre RS, Konarski JZ, Soczynska JK, Wilkins K, Panjwani G, Bouffard B, et al. Medical comorbidity in bipolar disorder: implications for functional outcomes and health service utilization. Psychiatr Serv. (2006) 57:1140–4. doi: 10.1176/ps.2006.57.8.1140
213. Soreca I, Frank E, and Kupfer DJ. The phenomenology of bipolar disorder: what drives the high rate of medical burden and determines long-term prognosis? Depress Anxiety. (2009) 26:73–82. doi: 10.1002/da.20521
214. Bryant-Comstock L, Stender M, and Devercelli G. Health care utilization and costs among privately insured patients with bipolar I disorder. Bipolar Disord. (2002) 4:398–405. doi: 10.1034/j.1399-5618.2002.01148.x
215. Gardner HH, Kleinman NL, Brook RA, Rajagopalan K, Brizee TJ, and Smeeding JE. The economic impact of bipolar disorder in an employed population from an employer perspective. J Clin Psychiatry. (2006) 67:1209–18. doi: 10.4088/jcp.v67n0806
217. Babigian HM and Odoroff CL. The mortality experience of a population with psychiatric illness. Am J Psychiatry. (1969) 126:470–80. doi: 10.1176/ajp.126.4.470
218. Fagiolini A and Goracci A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. J Clin Psychiatry. (2009) 70 Suppl 3:22–9. doi: 10.4088/JCP.7075su1c.04
219. Colton CW and Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. (2006) 3:A42.
220. Beyer J, Kuchibhatla M, Gersing K, and Krishnan KR. Medical comorbidity in a bipolar outpatient clinical population. Neuropsychopharmacology. (2005) 30:401–4. doi: 10.1038/sj.npp.1300608
221. Carney CP and Jones LE. Medical comorbidity in women and men with bipolar disorders: a population-based controlled study. Psychosom Med. (2006) 68:684–91. doi: 10.1097/01.psy.0000237316.09601.88
222. Castelo MS, Hyphantis TN, Macedo DS, Lemos GO, MaChado YO, Kapczinski F, et al. Screening for bipolar disorder in the primary care: a Brazilian survey. J Affect Disord. (2012) 143:118–24. doi: 10.1016/j.jad.2012.05.040
223. Douzenis A, Seretis D, Nika S, Nikolaidou P, Papadopoulou A, Rizos EN, et al. Factors affecting hospital stay in psychiatric patients: the role of active comorbidity. BMC Health Serv Res. (2012) 12:166. doi: 10.1186/1472-6963-12-166
224. Feldman NS, Gwizdowski IS, Fischer EG, Yang H, and Suppes T. Co-occurrence of serious or undiagnosed medical conditions with bipolar disorder preventing clinical trial randomization: a case series. J Clin Psychiatry. (2012) 73:874–7. doi: 10.4088/JCP.11m07331
225. Kemp DE, Sylvia LG, Calabrese JR, Nierenberg AA, Thase ME, Reilly-Harrington NA, et al. General medical burden in bipolar disorder: findings from the LiTMUS comparative effectiveness trial. Acta Psychiatr Scand. (2014) 129:24–34. doi: 10.1111/acps.12101
226. Kilbourne AM, Cornelius JR, Han X, Pincus HA, Shad M, Salloum I, et al. Burden of general medical conditions among individuals with bipolar disorder. Bipolar Disord. (2004) 6:368–73. doi: 10.1111/j.1399-5618.2004.00138.x
227. McIntyre RS, Soczynska JK, Beyer JL, Woldeyohannes HO, Law CW, Miranda A, et al. Medical comorbidity in bipolar disorder: re-prioritizing unmet needs. Curr Opin Psychiatry. (2007) 20:406–16. doi: 10.1097/YCO.0b013e3281938102
228. Perron BE, Howard MO, Nienhuis JK, Bauer MS, Woodward AT, and Kilbourne AM. Prevalence and burden of general medical conditions among adults with bipolar I disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. (2009) 70:1407–15. doi: 10.4088/JCP.08m04586yel
229. Strakowski SM, MeElroy SL, Keck PW Jr., and West SA. The co-occurrence of mania with medical and other psychiatric disorders. Int J Psychiatry Med. (1994) 24:305–28. doi: 10.2190/CM8E-46R5-9AJL-03FN
230. Fountoulakis K. Staging of bipolar disorder. In: Fountoulakis K, editor. Bipolar Disorder: An Evidence-Based Guide to Manic Depression. Springer-Verlag Berlin Heidelberg (2015). p. 437–59.
231. Berk M, Conus P, Lucas N, Hallam K, Malhi GS, Dodd S, et al. Setting the stage: from prodrome to treatment resistance in bipolar disorder. Bipolar Disord. (2007) 9:671–8. doi: 10.1111/j.1399-5618.2007.00484.x
232. Berk M, Hallam KT, and McGorry PD. The potential utility of a staging model as a course specifier: a bipolar disorder perspective. J Affect Disord. (2007) 100:279–81. doi: 10.1016/j.jad.2007.03.007
233. Cosci F and Fava GA. Staging of mental disorders: systematic review. Psychother Psychosom. (2013) 82:20–34. doi: 10.1159/000342243
234. Frank E, Nimgaonkar VL, Phillips ML, and Kupfer DJ. All the world’s a (clinical) stage: rethinking bipolar disorder from a longitudinal perspective. Mol Psychiatry. (2015) 20:23–31. doi: 10.1038/mp.2014.71
235. Kapczinski F, Dias VV, Kauer-Sant’Anna M, Frey BN, Grassi-Oliveira R, Colom F, et al. Clinical implications of a staging model for bipolar disorders. Expert Rev Neurother. (2009) 9:957–66. doi: 10.1586/ern.09.31
236. Post RM. Mechanisms of illness progression in the recurrent affective disorders. Neurotox Res. (2010) 18:256–71. doi: 10.1007/s12640-010-9182-2
237. Post RM, Fleming J, and Kapczinski F. Neurobiological correlates of illness progression in the recurrent affective disorders. J Psychiatr Res. (2012) 46:561–73. doi: 10.1016/j.jpsychires.2012.02.004
238. Berk M, Berk L, Udina M, Moylan S, Stafford L, Hallam K, et al. Palliative models of care for later stages of mental disorder: maximizing recovery, maintaining hope, and building morale. Aust N Z J Psychiatry. (2012) 46:92–9. doi: 10.1177/0004867411432072
239. Torrent C, Bonnin Cdel M, Martinez-Aran A, Valle J, Amann BL, Gonzalez-Pinto A, et al. Efficacy of functional remediation in bipolar disorder: a multicenter randomized controlled study. Am J Psychiatry. (2013) 170:852–9. doi: 10.1176/appi.ajp.2012.12070971
240. Fountoulakis KN. The contemporary face of bipolar illness: complex diagnostic and therapeutic challenges. CNS Spectr. (2008) 13:763–774, 777-769. doi: 10.1017/s1092852900013894
241. Fountoulakis K. Special issues. In: Fountoulakis K, editor. Bipolar Disorder: An Evidence-Based Guide to Manic Depression. Springer-Verlag Berlin Heidelberg (2015). p. 659–84.
242. Vrublevska J and Fountoulakis K. Medical comorbidity in bipolar disorder. In: Yildiz A, Ruiz P, and Nemeroff C, editors. The Bipolar Book. History, Neurobiology, and Treatment. Oxford University Press (2015). p. 497–506.
243. Fountoulakis KN, Gonda X, Vieta E, and Rihmer Z. Class effect of pharmacotherapy in bipolar disorder: fact or misbelief? Ann Gen Psychiatry. (2011) 10:8. doi: 10.1186/1744-859X-10-8
244. Fountoulakis KN, Vieta E, Sanchez-Moreno J, Kaprinis SG, Goikolea JM, and Kaprinis GS. Treatment guidelines for bipolar disorder: a critical review. J Affect Disord. (2005) 86:1–10. doi: 10.1016/j.jad.2005.01.004
245. Reinares M, Rosa AR, Franco C, Goikolea JM, Fountoulakis K, Siamouli M, et al. A systematic review on the role of anticonvulsants in the treatment of acute bipolar depression. Int J Neuropsychopharmacol. (2013) 16:485–96. doi: 10.1017/S1461145712000491
246. Rosa A, Fountoulakis K, Siamouli M, Gonda X, and Vieta E. Is anticonvulsant treatment of mania a class effect? Data from randomized clinical trials. CNS Neurosci Ther. (2011) 17:167–77. doi: 10.1111/j.1755-5949.2009.00089.x
247. Fountoulakis KN, Kelsoe JR, and Akiskal H. Receptor targets for antidepressant therapy in bipolar disorder: an overview. J Affect Disord. (2012) 138:222–38. doi: 10.1016/j.jad.2011.04.043
248. Popovic D, Reinares M, Goikolea JM, Bonnin CM, Gonzalez-Pinto A, and Vieta E. Polarity index of pharmacological agents used for maintenance treatment of bipolar disorder. Eur Neuropsychopharmacol. (2012) 22:339–46. doi: 10.1016/j.euroneuro.2011.09.008
249. Fountoulakis KN, Kontis D, Gonda X, Siamouli M, and Yatham LN. Treatment of mixed bipolar states. Int J Neuropsychopharmacol. (2012) 15:1015–26. doi: 10.1017/S1461145711001817
250. Fountoulakis KN, Kontis D, Gonda X, and Yatham LN. A systematic review of the evidence on the treatment of rapid cycling bipolar disorder. Bipolar Disord. (2013) 15:115–37. doi: 10.1111/bdi.12045
251. Nivoli AM, Colom F, Murru A, Pacchiarotti I, Castro-Loli P, Gonzalez-Pinto A, et al. New treatment guidelines for acute bipolar depression: a systematic review. J Affect Disord. (2011) 129:14–26. doi: 10.1016/j.jad.2010.05.018
252. Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. (2002) 59:530–7. doi: 10.1001/archpsyc.59.6.530
253. Morgan VA, Mitchell PB, and Jablensky AV. The epidemiology of bipolar disorder: sociodemographic, disability and service utilization data from the Australian National Study of Low Prevalence (Psychotic) Disorders. Bipolar Disord. (2005) 7:326–37. doi: 10.1111/j.1399-5618.2005.00229.x
254. Grande I, Berk M, Birmaher B, and Vieta E. Bipolar disorder. Lancet. (2016) 387:1561–72. doi: 10.1016/S0140-6736(15)00241-X
255. Fountoulakis K. Biological therapies. In: Fountoulakis K, editor. Bipolar Disorder: An Evidence-Based Guide to Manic Depression. Springer-Verlag Berlin Heidelberg (2015). p. 461–625.
256. Fountoulakis K. Psychosocial treatment and interventions. In: Fountoulakis K, editor. Bipolar Disorder: An Evidence-Based Guide to Manic Depression. Springer-Verlag Berlin Heidelberg (2015). p. 627–42.
257. Fountoulakis KN, Bech P, Panagiotidis P, Siamouli M, Kantartzis S, Papadopoulou A, et al. Comparison of depressive indices: reliability, validity, relationship to anxiety and personality and the role of age and life events. J Affect Disord. (2007) 97:187–95. doi: 10.1016/j.jad.2006.06.015
258. Fountoulakis KN, Grunze H, Panagiotidis P, and Kaprinis G. Treatment of bipolar depression: an update. J Affect Disord. (2008) 109:21–34. doi: 10.1016/j.jad.2007.10.016
259. Fountoulakis KN, Vieta E, Siamouli M, Valenti M, Magiria S, Oral T, et al. Treatment of bipolar disorder: a complex treatment for a multi-faceted disorder. Ann Gen Psychiatry. (2007) 6:27. doi: 10.1186/1744-859X-6-27
260. Gonda X, Fountoulakis KN, Rihmer Z, Lazary J, Laszik A, Akiskal KK, et al. Towards a genetically validated new affective temperament scale: a delineation of the temperament phenotype of 5-HTTLPR using the TEMPS-A. J Affect Disord. (2009) 112:19–29. doi: 10.1016/j.jad.2008.03.012
261. Pacchiarotti I, Bond DJ, Baldessarini RJ, Nolen WA, Grunze H, Licht RW, et al. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am J Psychiatry. (2013) 170:1249–62. doi: 10.1176/appi.ajp.2013.13020185
262. Reinares M, Sanchez-Moreno J, and Fountoulakis KN. Psychosocial interventions in bipolar disorder: what, for whom, and when. J Affect Disord. (2014) 156:46–55. doi: 10.1016/j.jad.2013.12.017
263. Gerson LD and Rose LE. Needs of persons with serious mental illness following discharge from inpatient treatment: patient and family views. Arch Psychiatr Nurs. (2012) 26:261–71. doi: 10.1016/j.apnu.2012.02.002
264. Charney DS, Reynolds CF 3rd, Lewis L, Lebowitz BD, Sunderland T, Alexopoulos GS, et al. Depression and Bipolar Support Alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Arch Gen Psychiatry. (2003) 60:664–72. doi: 10.1001/archpsyc.60.7.664
265. Muralidharan K, Ali M, Silveira LE, Bond DJ, Fountoulakis KN, Lam RW, et al. Efficacy of second generation antipsychotics in treating acute mixed episodes in bipolar disorder: a meta-analysis of placebo-controlled trials. J Affect Disord. (2013) 150:408–14. doi: 10.1016/j.jad.2013.04.032
266. Yatham LN, Fountoulakis KN, Rahman Z, Ammerman D, Fyans P, Marler SV, et al. Efficacy of aripiprazole versus placebo as adjuncts to lithium or valproate in relapse prevention of manic or mixed episodes in bipolar I patients stratified by index manic or mixed episode. J Affect Disord. (2013) 147:365–72. doi: 10.1016/j.jad.2012.11.042
267. Curtis V. Women are not the same as men: specific clinical issues for female patients with bipolar disorder. Bipolar Disord. (2005) 7 Suppl 1:16–24. doi: 10.1111/j.1399-5618.2005.00190.x
268. Hendrick V, Altshuler LL, Gitlin MJ, Delrahim S, and Hammen C. Gender and bipolar illness. J Clin Psychiatry. (2000) 61:393–396; quiz 397. doi: 10.4088/jcp.v61n0514
269. Leibenluft E. Women with bipolar illness: clinical and research issues. Am J Psychiatry. (1996) 153:163–73. doi: 10.1176/ajp.153.2.163
271. Arnold LM, McElroy SL, and Keck PE Jr. The role of gender in mixed mania. Compr Psychiatry. (2000) 41:83–7. doi: 10.1016/s0010-440x(00)90137-8
272. McElroy SL, Keck PE Jr., Pope HG Jr., Hudson JI, Faedda GL, and Swann AC. Clinical and research implications of the diagnosis of dysphoric or mixed mania or hypomania. Am J Psychiatry. (1992) 149:1633–44. doi: 10.1176/ajp.149.12.1633
273. Post RM, Denicoff KD, Leverich GS, Altshuler LL, Frye MA, Suppes TM, et al. Morbidity in 258 bipolar outpatients followed for 1 year with daily prospective ratings on the NIMH life chart method. J Clin Psychiatry. (2003) 64:680–690; quiz 738-689. doi: 10.4088/jcp.v64n0610
274. Fakhoury WK, Wright D, and Wallace M. Prevalence and extent of distress of adverse effects of antipsychotics among callers to a United Kingdom National Mental Health Helpline. Int Clin Psychopharmacol. (2001) 16:153–62. doi: 10.1097/00004850-200105000-00004
275. Russell JM and Mackell JA. Bodyweight gain associated with atypical antipsychotics: epidemiology and therapeutic implications. CNS Drugs. (2001) 15:537–51. doi: 10.2165/00023210-200115070-00004
276. McElroy SL, Frye MA, Suppes T, Dhavale D, Keck PE Jr., Leverich GS, et al. Correlates of overweight and obesity in 644 patients with bipolar disorder. J Clin Psychiatry. (2002) 63:207–13. doi: 10.4088/jcp.v63n0306
277. Wieck A and Haddad PM. Antipsychotic-induced hyperprolactinaemia in women: pathophysiology, severity and consequences. Selective literature review. Br J Psychiatry. (2003) 182:199–204. doi: 10.1192/bjp.182.3.199
278. Smith S, Wheeler MJ, Murray R, and O’Keane V. The effects of antipsychotic-induced hyperprolactinaemia on the hypothalamic-pituitary-gonadal axis. J Clin Psychopharmacol. (2002) 22:109–14. doi: 10.1097/00004714-200204000-00002
279. Coverdale JH, Turbott SH, and Roberts H. Family planning needs and STD risk behaviours of female psychiatric out-patients. Br J Psychiatry. (1997) 171:69–72. doi: 10.1192/bjp.171.1.69
280. Cohen LS, Friedman JM, Jefferson JW, Johnson EM, and Weiner ML. A reevaluation of risk of in utero exposure to lithium. JAMA. (1994) 271:146–50. doi: 10.1001/jama.1994.03510260078033
281. Packer S. Family planning for women with bipolar disorder. Hosp Community Psychiatry. (1992) 43:479–82. doi: 10.1176/ps.43.5.479
282. Blehar MC, DePaulo JR Jr., Gershon ES, Reich T, Simpson SG, and Nurnberger JI Jr. Women with bipolar disorder: findings from the NIMH Genetics Initiative sample. Psychopharmacol Bull. (1998) 34:239–43.
283. Brockington IF, Cernik KF, Schofield EM, Downing AR, Francis AF, and Keelan C. Puerperal psychosis. Phenomena and diagnosis. Arch Gen Psychiatry. (1981) 38:829–33. doi: 10.1001/archpsyc.1981.01780320109013
284. Davidson J and Robertson E. A follow-up study of post partum illness 1946-1978. Acta Psychiatr Scand. (1985) 71:451–7. doi: 10.1111/j.1600-0447.1985.tb05057.x
285. Dunner DL, Patrick V, and Fieve RR. Life events at the onset of bipolar affective illness. Am J Psychiatry. (1979) 136:508–11. doi: 10.1176/ajp.1979.136.4b.508
286. Freeman MP, Smith KW, Freeman SA, McElroy SL, Kmetz GE, Wright R, et al. The impact of reproductive events on the course of bipolar disorder in women. J Clin Psychiatry. (2002) 63:284–7. doi: 10.4088/jcp.v63n0403
287. Kendell RE, Chalmers JC, and Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. (1987) 150:662–73. doi: 10.1192/bjp.150.5.662
288. Schopf J and Rust B. Follow-up and family study of postpartum psychoses. Part I: Overview. Eur Arch Psychiatry Clin Neurosci. (1994) 244:101–11. doi: 10.1007/BF02193527
289. Chengappa KR and Williams P. Barriers to the effective management of bipolar disorder: a survey of psychiatrists based in the UK and USA. Bipolar Disord. (2005) 7 Suppl 1:38–42. doi: 10.1111/j.1399-5618.2005.00193.x
290. Glauser TA, Cerenzia W, Wiley S, Howson A, and Thase M. Identifying psychiatrists’ practice patterns when managing depression in patients with bipolar I disorder: a descriptive study to inform education needs. Postgrad Med. (2013) 125:144–53. doi: 10.3810/pgm.2013.01.2606
291. Han C, Wang SM, Lee SJ, Patkar AA, Masand PS, and Pae CU. Dilemma for enhancing psychiatrists’ adherence to guideline (evidence)-based practice. Expert Rev Neurother. (2013) 13:751–4. doi: 10.1586/14737175.2013.811196
292. Chengappa KR and Goodwin GM. Characterizing barriers, challenges and unmet needs in the management of bipolar disorder. Bipolar Disord. (2005) 7 Suppl 1:5–7. doi: 10.1111/j.1399-5618.2005.00188.x
293. Bauer MS. A review of quantitative studies of adherence to mental health clinical practice guidelines. Harv Rev Psychiatry. (2002) 10:138–53. doi: 10.1080/10673220216217
294. Masand PS and Tracy N. Results from an online survey of patient and caregiver perspectives on unmet needs in the treatment of bipolar disorder. Prim Care Companion CNS Disord. (2014) 16. doi: 10.4088/PCC.14m01655
295. Badger TA, McNiece C, Bonham E, Jacobson J, and Gelenberg AJ. Health outcomes for people with serious mental illness: a case study. Perspect Psychiatr Care. (2003) 39:23–32. doi: 10.1111/j.1744-6163.2003.tb00670.x
296. Bauer MS, Kirk GF, Gavin C, and Williford WO. Determinants of functional outcome and healthcare costs in bipolar disorder: a high-intensity follow-up study. J Affect Disord. (2001) 65:231–41. doi: 10.1016/s0165-0327(00)00247-0
297. Keck PE Jr., McElroy SL, Strakowski SM, Stanton SP, Kizer DL, Balistreri TM, et al. Factors associated with pharmacologic noncompliance in patients with mania. J Clin Psychiatry. (1996) 57:292–7.
298. Johnson RE and McFarland BH. Lithium use and discontinuation in a health maintenance organization. Am J Psychiatry. (1996) 153:993–1000. doi: 10.1176/ajp.153.8.993
299. Murru A, Pacchiarotti I, Amann BL, Nivoli AM, Vieta E, and Colom F. Treatment adherence in bipolar I and schizoaffective disorder, bipolar type. J Affect Disord. (2013) 151:1003–8. doi: 10.1016/j.jad.2013.08.026
300. Sachs GS. Unmet needs in the assessment and management of bipolar I depression. J Clin Psychiatry. (2013) 74:e11. doi: 10.4088/JCP.12065tx1c
301. Fountoulakis KN, Young A, Yatham L, Grunze H, Vieta E, Blier P, et al. The international college of neuropsychopharmacology (CINP) treatment guidelines for bipolar disorder in adults (CINP-BD-2017), part 1: background and methods of the development of guidelines. Int J Neuropsychopharmacol. (2017) 20:98–120. doi: 10.1093/ijnp/pyw091
302. Hopewell S, Clarke M, Moher D, Wager E, Middleton P, Altman DG, et al. CONSORT for reporting randomized controlled trials in journal and conference abstracts: explanation and elaboration. PloS Med. (2008) 5:e20. doi: 10.1371/journal.pmed.0050020
303. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Bmj. (2009) 339:b2700. doi: 10.1136/bmj.b2700
304. Moher D, Liberati A, Tetzlaff J, Altman DG, and Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
305. Moher D, Liberati A, Tetzlaff J, Altman DG, and Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PloS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
306. Fountoulakis KN and Vieta E. Efficacy and safety of aripiprazole in the treatment of bipolar disorder: a systematic review. Ann Gen Psychiatry. (2009) 8:16. doi: 10.1186/1744-859X-8-16
307. Fountoulakis KN, Vieta E, and Schmidt F. Aripiprazole monotherapy in the treatment of bipolar disorder: a meta-analysis. J Affect Disord. (2011) 133:361–70. doi: 10.1016/j.jad.2010.10.018
308. Calabrese JR, Bowden CL, Sachs GS, Ascher JA, Monaghan E, and Rudd GD. A double-blind placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. Lamictal 602 Study Group. J Clin Psychiatry. (1999) 60:79–88. doi: 10.4088/jcp.v60n0203
309. Fletcher SW and Spitzer WO. Approach of the Canadian task force to the periodic health examination. Ann Intern Med. (1980) 92:253–4. doi: 10.7326/0003-4819-92-2-253
310. Dawes M, Summerskill W, Glasziou P, Cartabellotta A, Martin J, Hopayian K, et al. Sicily statement on evidence-based practice. BMC Med Educ. (2005) 5:1. doi: 10.1186/1472-6920-5-1
311. Richardson WS, Wilson MC, Nishikawa J, and Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J Club. (1995) 123:A12–13. doi: 10.7326/ACPJC-1995-123-3-A12
312. Schlosser RW, Koul R, and Costello J. Asking well-built questions for evidence-based practice in augmentative and alternative communication. J Commun Disord. (2007) 40:225–38. doi: 10.1016/j.jcomdis.2006.06.008
313. Rosenberg WM, Deeks J, Lusher A, Snowball R, Dooley G, and Sackett D. Improving searching skills and evidence retrieval. J R Coll Physicians Lond. (1998) 32:557–63. doi: 10.1016/S0035-8819(25)01804-5
314. Horsley T, Hyde C, Santesso N, Parkes J, Milne R, and Stewart R. Teaching critical appraisal skills in healthcare settings. Cochrane Database Syst Rev. (2011) 2011:CD001270. doi: 10.1002/14651858.CD001270.pub2
315. Parkes J, Hyde C, Deeks J, and Milne R. Teaching critical appraisal skills in health care settings. Cochrane Database Syst Rev. (2001) 3:CD001270. doi: 10.1002/14651858.CD001270
316. Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. (2012) 2012:CD000259. doi: 10.1002/14651858.CD000259.pub3
317. Jamtvedt G, Young JM, Kristoffersen DT, O’Brien MA, and Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. (2006) 2:CD000259. doi: 10.1002/14651858.CD000259.pub2
318. Jamtvedt G, Young JM, Kristoffersen DT, O’Brien MA, and Oxman AD. Does telling people what they have been doing change what they do? A systematic review of the effects of audit and feedback. Qual Saf Health Care. (2006) 15:433–6. doi: 10.1136/qshc.2006.018549
319. Jamtvedt G, Young JM, Kristoffersen DT, Thomson O’Brien MA, and Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. (2003) 3:CD000259. doi: 10.1002/14651858.CD000259
320. Tonelli MR. In defense of expert opinion. Acad Med. (1999) 74:1187–92. doi: 10.1097/00001888-199911000-00010
321. Sherman M, Burak K, Maroun J, Metrakos P, Knox JJ, Myers RP, et al. Multidisciplinary Canadian consensus recommendations for the management and treatment of hepatocellular carcinoma. Curr Oncol. (2011) 18:228–40. doi: 10.3747/co.v18i5.952
322. U.S. Preventive Services Task Force. Guide to clinical preventive services: report of the U.S. Preventive Services Task Force. DIANE Publishing (1989).
323. OCEBM Levels of Evidence Working Group. The Oxford 2011 levels of evidence (2015). Available online at: http://www.cebm.net/index.aspx?o=5653 (Accessed March 30, 2025).
324. Paul C, Gallini A, Archier E, Castela E, Devaux S, Aractingi S, et al. Evidence-based recommendations on topical treatment and phototherapy of psoriasis: systematic review and expert opinion of a panel of dermatologists. J Eur Acad Dermatol Venereol. (2012) 26 Suppl 3:1–10. doi: 10.1111/j.1468-3083.2012.04518.x
325. Lehman AF and Steinwachs DM. Translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophr Bull. (1998) 24:1–10. doi: 10.1093/oxfordjournals.schbul.a033302
326. Grunze H, Kasper S, Goodwin G, Bowden C, Baldwin D, Licht R, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of bipolar disorders. Part I: Treatment of bipolar depression. World J Biol Psychiatry. (2002) 3:115–24. doi: 10.3109/15622970209150612
327. Grunze H, Kasper S, Goodwin G, Bowden C, Baldwin D, Licht RW, et al. The world federation of societies of biological psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders, part II: treatment of mania. World J Biol Psychiatry. (2003) 4:5–13. doi: 10.3109/15622970309167904
328. Grunze H, Kasper S, Goodwin G, Bowden C, Moller HJ, and Disorders, W. T. F. o. T. G. f. B. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders, part III: maintenance treatment. World J Biol Psychiatry. (2004) 5:120–35. doi: 10.1080/15622970410029924
329. Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schunemann HJ, et al. What is “quality of evidence” and why is it important to clinicians? BMJ. (2008) 336:995–8. doi: 10.1136/bmj.39490.551019.BE
330. Jaeschke R, Guyatt GH, Dellinger P, Schunemann H, Levy MM, Kunz R, et al. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. Bmj. (2008) 337:a744. doi: 10.1136/bmj.a744
332. Schunemann HJ, Fretheim A, and Oxman AD. Improving the use of research evidence in guideline development: 10. Integrating values and consumer involvement. Health Res Policy Syst. (2006) 4:22. doi: 10.1186/1478-4505-4-22
333. Guyatt G, Oxman AD, Sultan S, Brozek J, Glasziou P, Alonso-Coello P, et al. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol. (2013) 66:151–7. doi: 10.1016/j.jclinepi.2012.01.006
334. Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence–imprecision. J Clin Epidemiol. (2011) 64:1283–93. doi: 10.1016/j.jclinepi.2011.01.012
335. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence–indirectness. J Clin Epidemiol. (2011) 64:1303–10. doi: 10.1016/j.jclinepi.2011.04.014
336. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence–inconsistency. J Clin Epidemiol. (2011) 64:1294–302. doi: 10.1016/j.jclinepi.2011.03.017
337. Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence–publication bias. J Clin Epidemiol. (2011) 64:1277–82. doi: 10.1016/j.jclinepi.2011.01.011
338. Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso-Coello P, et al. GRADE guidelines: 9. Rating up the quality of evidence. J Clin Epidemiol. (2011) 64:1311–6. doi: 10.1016/j.jclinepi.2011.06.004
339. Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence–study limitations (risk of bias). J Clin Epidemiol. (2011) 64:407–15. doi: 10.1016/j.jclinepi.2010.07.017
340. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. (2008) 336:924–6. doi: 10.1136/bmj.39489.470347.AD
341. Fountoulakis KN, Vieta E, Young A, Yatham L, Grunze H, Blier P, et al. The international college of neuropsychopharmacology (CINP) treatment guidelines for bipolar disorder in adults (CINP-BD-2017), part 4: unmet needs in the treatment of bipolar disorder and recommendations for future research. Int J Neuropsychopharmacol. (2017) 20:196–205. doi: 10.1093/ijnp/pyw072
342. Fountoulakis KN, Yatham L, Grunze H, Vieta E, Young A, Blier P, et al. The international college of neuro-psychopharmacology (CINP) treatment guidelines for bipolar disorder in adults (CINP-BD-2017), part 2: review, grading of the evidence, and a precise algorithm. Int J Neuropsychopharmacol. (2017) 20:121–79. doi: 10.1093/ijnp/pyw100
343. Ghaemi SN, Pardo TB, and Hsu DJ. Strategies for preventing the recurrence of bipolar disorder. J Clin Psychiatry 65 Suppl. (2004) 10:16–23.
344. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 4th Edition, Text Revision, DSM-IV-TR. Washington, DC: American Psychiatric Publishing (2000).
345. Calabrese JR, Goldberg JF, Ketter TA, Suppes T, Frye M, White R, et al. Recurrence in bipolar I disorder: a post hoc analysis excluding relapses in two double-blind maintenance studies. Biol Psychiatry. (2006) 59:1061–4. doi: 10.1016/j.biopsych.2006.02.034
346. Fountoulakis KN. Refractoriness in bipolar disorder: definitions and evidence-based treatment. CNS Neurosci Ther. (2012) 18:227–37. doi: 10.1111/j.1755-5949.2011.00259.x
347. Cipriani A, Barbui C, Rendell J, and Geddes JR. Clinical and regulatory implications of active run-in phases in long-term studies for bipolar disorder. Acta Psychiatr Scand. (2014) 129:328–42. doi: 10.1111/acps.12223
348. Grande I, Bernardo M, Bobes J, Saiz-Ruiz J, Alamo C, and Vieta E. Antipsychotic switching in bipolar disorders: a systematic review. Int J Neuropsychopharmacol. (2014) 17:497–507. doi: 10.1017/S1461145713001168
349. Calabrese JR, Fava M, Garibaldi G, Grunze H, Krystal AD, Laughren T, et al. Methodological approaches and magnitude of the clinical unmet need associated with amotivation in mood disorders. J Affect Disord. (2014) 168:439–51. doi: 10.1016/j.jad.2014.06.056
350. Frye MA, Prieto ML, Bobo WV, Kung S, Veldic M, Alarcon RD, et al. Current landscape, unmet needs, and future directions for treatment of bipolar depression. J Affect Disord. (2014) 169 Suppl 1:S17–23. doi: 10.1016/S0165-0327(14)70005-9
351. McElroy SL. Pros and cons of approved therapies for bipolar depression and ongoing unmet needs. J Clin Psychiatry. (2014) 75:e26. doi: 10.4088/JCP.13019tx4c
352. Akiskal HS, Walker P, Puzantian VR, King D, Rosenthal TL, and Dranon M. Bipolar outcome in the course of depressive illness. Phenomenologic, familial, and pharmacologic predictors. J Affect Disord. (1983) 5:115–28. doi: 10.1016/0165-0327(83)90004-6
353. Weissman MM, Prusoff BA, and Merikangas KR. Is delusional depression related to bipolar disorder? Am J Psychiatry. (1984) 141:892–3. doi: 10.1176/ajp.141.7.892
354. Bonnin CM, Reinares M, Hidalgo-Mazzei D, Undurraga J, Mur M, Saez C, et al. Predictors of functional outcome after a manic episode. J Affect Disord. (2015) 182:121–5. doi: 10.1016/j.jad.2015.04.043
355. Thase ME, Jonas A, Khan A, Bowden CL, Wu X, McQuade RD, et al. Aripiprazole monotherapy in nonpsychotic bipolar I depression: results of 2 randomized, placebo-controlled studies. J Clin Psychopharmacol. (2008) 28:13–20. doi: 10.1097/jcp.0b013e3181618eb4
356. Loebel A, Cucchiaro J, Silva R, Kroger H, Hsu J, Sarma K, et al. Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. (2014) 171:160–8. doi: 10.1176/appi.ajp.2013.13070984
357. Vieta E and Cruz N. Head to head comparisons as an alternative to placebo-controlled trials. Eur Neuropsychopharmacol. (2012) 22:800–3. doi: 10.1016/j.euroneuro.2011.11.011
358. Siddiqui O, Hung HM, and O’Neill R. MMRM vs. LOCF: a comprehensive comparison based on simulation study and 25 NDA datasets. J Biopharm Stat. (2009) 19:227–46. doi: 10.1080/10543400802609797
359. Fountoulakis K. Disability and overall burden related with bipolar disorder. In: Fountoulakis K, editor. Bipolar Disorder: An Evidence-Based Guide to Manic Depression. Springer-Verlag Berlin Heidelberg (2015). p. 361–88.
360. Young AH, Rigney U, Shaw S, Emmas C, and Thompson JM. Annual cost of managing bipolar disorder to the UK healthcare system. J Affect Disord. (2011) 133:450–6. doi: 10.1016/j.jad.2011.06.016
361. Begley CE, Annegers JF, Swann AC, Lewis C, Coan S, Schnapp WB, et al. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics. (2001) 19:483–95. doi: 10.2165/00019053-200119050-00004
362. McCrone P, Dhanasiri S, Patel A, Knapp M, and Lawton-Simth S. Paying the price. London: The King’s Fund (2008).
363. Wyatt RJ and Henter I. An economic evaluation of manic-depressive illness–1991. Soc Psychiatry Psychiatr Epidemiol. (1995) 30:213–9. doi: 10.1007/BF00789056
364. Runge C and Grunze H. Annual costs of bipolar disorders in Germany. Nervenarzt. (2004) 75:896–903. doi: 10.1007/s00115-004-1691-x
365. Ekman M, Granstrom O, Omerov S, Jacob J, and Landen M. The societal cost of bipolar disorder in Sweden. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:1601–10. doi: 10.1007/s00127-013-0724-9
366. Fisher LJ, Goldney RD, Dal Grande E, Taylor AW, and Hawthorne G. Bipolar disorders in Australia. A population-based study of excess costs. Soc Psychiatry Psychiatr Epidemiol. (2007) 42:105–9. doi: 10.1007/s00127-006-0133-4
367. Hakkaart-van Roijen L, Hoeijenbos MB, Regeer EJ, ten Have M, Nolen WA, Veraart CP, et al. The societal costs and quality of life of patients suffering from bipolar disorder in the Netherlands. Acta Psychiatr Scand. (2004) 110:383–92. doi: 10.1111/j.1600-0447.2004.00403.x
Keywords: bipolar disorder, treatment guidelines, treatment algorithms, anticonvulsants, antidepressants, antipsychotics, evidence-based, lithium
Citation: Fountoulakis KN, Fountoulakis NK and Antoniadis D (2025) Challenges in the development of treatment guidelines for bipolar disorder. Front. Psychiatry 16:1564004. doi: 10.3389/fpsyt.2025.1564004
Received: 20 January 2025; Accepted: 30 April 2025;
Published: 10 June 2025.
Edited by:
Heinz Grunze, Psychiatrie Schwäbisch Hall, GermanyReviewed by:
Diego Hidalgo-Mazzei, Hospital Clinic of Barcelona, SpainRalph Werner Kupka, VU Medical Center, Netherlands
Copyright © 2025 Fountoulakis, Fountoulakis and Antoniadis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Konstantinos N. Fountoulakis, Zm91bnRvdWxAYXV0aC5ncg==
†ORCID: Konstantinos N Fountoulakis, orcid.org/0000-0001-5503-0811
Nikolaos K. Fountoulakis, orcid.org/0000-0002-5965-707X
 Konstantinos N. Fountoulakis
Konstantinos N. Fountoulakis Nikolaos K. Fountoulakis2†
Nikolaos K. Fountoulakis2†