- 1Department of Critical Care Nursing, Razi Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran
- 2Nursing Research Center, Kerman University of Medical Sciences, Kerman, Iran
Background: Postmenopausal women are interested in using complementary and alternative medicine because of their menopausal symptoms and the side effects of chemical medications and hormone therapy. Therefore, this study aimed to investigate the relationship between the use of complementary medicine (CAM) and menopausal symptoms among postmenopausal women.
Methods: This cross-sectional study was conducted among 288 postmenopausal women who were referred to health centers in Kerman, southeastern Iran, from 2020 to 2021. Data were collected using a demographic questionnaire, the CAM questionnaire, and the Menopause Rating Scale (MRS).
Results: The mean score for the menopausal symptoms of the participants was 8.73 ± 6.11. Only 28.8% of the participants had no/little symptoms. About 65.3% of the participants used at least one type of CAM in the previous year. The most commonly used types of CAM were nutritional supplements, prayer, and medicinal herbs. A significant association was found between the use of medicinal herbs, dry cupping, relaxation and meditation, prayer, and menopausal symptoms. Women experiencing menopausal symptoms used more CAM methods than those without menopausal symptoms (Odds ratio = 2.25, 95% confidence interval = 1.33–3.80).
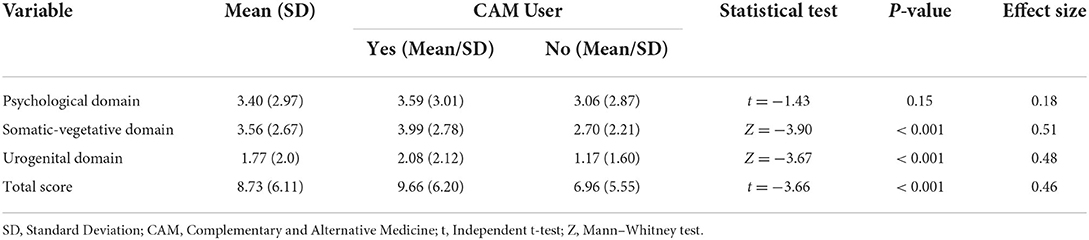
Conclusion: The study results indicated that the severity of menopausal symptoms and scores in somatic-vegetative and urogenital domains were higher in CAM users compared to non-CAM users. But there was no significant difference in the psychological domain between CAM and non-CAM users. Based on the results, it is suggested that more research be done in different communities with different healthcare systems to find out how complementary and alternative medicine affects menopausal symptoms in women.
Introduction
Menopause is defined as decreased ovarian follicular function and estrogen level, which may begin as early as your mid-30s or as late as your mid-50s. When a woman is in menopause, her menstrual period has been gone for 12 consecutive months (1). Today, 95% of the women in some communities are in menopause, and this population is predicted to reach 1.2 billion by 2030, with an annual increase of 47 million new cases (2). About five million Iranian women were in menopause in 2021 (3). However, menopause is affected by genetic factors, obesity, alcoholism, ethnicity, diet, vitamin D and calcium intake, prolonged menstrual periods, and the use of oral contraceptives (4). Therefore, 50–75% of women experience pre-menopausal or menopausal symptoms, including hot flashes and night sweats (vasomotor symptoms), insomnia, musculoskeletal pain, and urogenital disorders, such as incontinence, vaginal dryness, painful intercourse, anxiety, fatigue, and depression (5–7).
Hormone therapy and non-hormonal treatments, as well as CAM, are the ways to prevent and reduce menopausal symptoms (3, 8–10). Hormone therapy is the primary treatment for menopausal symptoms. However, many women cannot use this therapy due to an increased risk of endometrial and ovarian neoplasia, uterine cancer, breast cancer, ovarian cancer, and an increased risk of stroke (11, 12). Non-hormonal treatments, such as clonidine, gabapentin, and antidepressants, can also reduce menopausal symptoms, but they have many side effects, such as sleep disorders, dizziness, nausea, fatigue, and constipation (13). Therefore, women have focused on complementary and alternative medicine (CAM), which is more cost-effective and has fewer side effects than other therapies. People use complementary medicine to support and strengthen their general health, as well as to improve the symptoms of diseases or drug side effects (14).
CAM refers to a broad set of healthcare practices that are not part of the current healthcare system. According to recent studies, about 73.6% of women experiencing menopause in Turkey (15) and 70% of women with polycystic ovary syndrome (16) in Australia used CAM. Studies showed that dry and wet cuppings (17), acupuncture (18), acupressure (19), massage (20), relaxation (21) and yoga (22), aromatherapy (23), diets (24), homeopathy (25), music therapy (26), hydrotherapy (27), and prayer (28) affected the improvement of vasomotor symptoms, urogenital disorders, fatigue, and depression caused by menopause. In addition, herbal products, such as chamomile (29), Vitex agnus-castus (30), Hypericum Perforatum (31), Crocus sativus (32), Curcumin (33), Melissa Officinalis (34), Thymes (35), Wheat Germ (36), Fennel (Foeniculum vulgare) (37), Valerian Root (38), Ginger (39) and Flaxseed (40), and Soy Isoflavones (41) affected physical and psychological symptoms caused by menopause. Postmenopausal women increasingly use a variety of complementary medicine methods to improve their menopausal symptoms due to the widespread complications of drug and hormone therapies. No research in Iran examines the relationship between complementary medicine methods and menopausal symptoms. Therefore, this study aimed to investigate the relationship between menopausal symptoms and the use of complementary medicine methods among women who were referred to health centers in Kerman from 2020 to 2021.
Methods
Study design and setting
This cross-sectional study was conducted on postmenopausal women referred to health centers in Kerman from 2020 to 2021. Health centers provide healthcare for the community (42). Kerman is located in southeastern Iran and consists of 47 health centers, of which 31 centers collaborated with researchers. Only 10 health centers made the contact numbers of postmenopausal women available, and 21 health centers collaborated with researchers in face-to-face sampling.
Sampling and sample size
The sample size was estimated to be 267 using Cochran's formula for an infinite population following the study's primary objective (Z = 1.96, d = 0.06). Power analysis calculations with G*Power software (version 3.1.9.2) indicated that (power = 90%, α = 0.05, number of groups, i.e., CAM users: yes/no = two) 86 participants in each group would be needed to detect an effect size of 0.5.
The convenience sampling method was used in the present study. Inclusion criteria were participants aged 50–60 years, in normal menopause (rather than by hysterectomy and surgery), and whose menstrual period had been gone for at least 12 consecutive months (19, 36). Incomplete questionnaires (say 10% or more) were excluded from the study. Totally 220 questionnaires were given to postmenopausal women referred to Kerman health centers. Of these, 189 were returned (a response rate of 85.9%) and 36 were excluded due to not being eligible. In the online sampling form, 191 questionnaires were completed (a response rate of 12.44%) and 47 questionnaires were excluded due to the inclusion criteria. After checking completed questionnaires by statistical analysis, 9 samples were excluded from the study. Therefore, 288 samples were included in the study. The overall response rate was 56.71%.
Ethical issue
The Kerman University of Medical Sciences approved this project (IR.KMU.REC.1399.444 and NO: 99000487). Then, permission was issued to the management of the healthcare centers. The researcher provided some oral information, including the study goals and objectives, data confidentiality, and anonymity, and she assured the participants that they could withdraw from the study at any time. Then, written informed consent was obtained individually.
Questionnaire
Demographic information questionnaire
This questionnaire includes the variables of age, education level, marital status, occupation, duration of menopause, number of children, a history of addiction (smoking), a history of diabetes, a history of ovarian and uterine cancer, a history of breast cancer, a history of hysterectomy, a history of hypertension, and a history of chronic diseases (43).
The menopause rating scale
Heinemann et al. designed the questionnaire, which is an international scale for assessing menopausal symptoms (44, 45). This scale consists of 11 items with three subscales of somatic-vegetative symptoms (hot flashes, night sweats, heart palpitations, sleep disorders, and muscle and joint disorders), psychological symptoms (depression, anxiety, fatigue, and irritability), and urogenital symptoms (sexual dysfunction, vaginal dryness, and urinary symptoms). This questionnaire was rated on a 5-point Likert scale (from zero: no symptoms to four: very severe) (44, 46). Scores for each subscale are based on the sum of the item scores of the respective subscale. The total score of the questionnaire is the sum of the subscale scores (45). The minimum score is zero, while the maximum is 44, with total scores ≤ 11, 12–35, and ≥ 36 being no symptoms, mild to moderate symptoms, and severe to very severe symptoms, respectively (47, 48). Heinemann confirmed the face validity and reliability of this questionnaire with a Cronbach's alpha coefficient of 0.98 and an intra-class correlation coefficient of 0.97 (48). In addition, Darsareh et al. (49) and Shakeri et al. (50) in Iran confirmed the validity of this scale. Masjoudi et al. (48) in Iran reported a Cronbach's alpha coefficient of 0.83 for this questionnaire. In the present study, Cronbach's alpha coefficient was 0.86.
CAM questionnaire and Satisfaction with the use of complementary medicine questionnaire
The questionnaire of Dehghan et al. was used to assess the use of complementary medicine among women in the menopausal stage. This questionnaire contains 10 items on the use of some types of CAM (herbal medicine, wet cupping, dry cupping, massage, acupuncture, homeopathy, and relaxation techniques, such as yoga and prayer). Yes-no questions are used; if the answer is yes, the rate of consumption will be asked (from rarely to once a day) (50). Nine questions were asked to measure satisfaction with the use of complementary drugs, including their accessibility, ease of use, harmlessness, non-interference with daily activities, concerns about drug interaction, feeling good after using the treatment, suggesting this method to others, and their inexpensiveness. This questionnaire is scored on a five-point Likert scale (from four = very satisfied to zero = no idea). The score for satisfaction with the use of complementary medicines ranged from 0 to 36, with high scores indicating high satisfaction. Dehghan et al. (51) confirmed the questionnaire reliability (0.96), while Sheikhrabori (52) confirmed its validity (0.77). In the present study, Cronbach's alpha coefficient was 0.79.
Data collection
The researcher began sampling women in menopause after obtaining the necessary permits from the management of health centers in Kerman. She did sampling both in person and virtually due to the prevalence of COVID-19. Researchers referred to the health centers of Kerman in the morning for 8 months from January to August 2021 to collect in-person data. First, they explained the study objectives and inclusion criteria. Then, they started sampling after obtaining informed consent and after participants received healthcare services, so they had enough time to answer the questionnaires. Participants completed self-report questionnaires on the demographic information, the use of complementary medicine, and the MRS. The researcher read the questionnaires to uneducated participants. She prepared an electronic questionnaire for online sampling. First, she prepared a list of contact numbers of the women in menopause from 10 health centers, examined their inclusion criteria, and identified the eligible ones. She contacted them and explained the study condition. Furthermore, the researcher explained the study objectives, method, and completion process of the electronic questionnaire to each of the participants, and then asked them to sign the written informed consent form. The link to the questionnaire was sent to eligible postmenopausal women via SMS, WhatsApp, and Telegram. The women had enough time to fill out the questionnaires, which were then automatically sent to the researcher.
Data analysis
SPSS25 was used for data analysis. Descriptive statistics (frequency, percentage, mean, and standard deviation) were used to describe the underlying characteristics of women in menopause, their use of CAM, their satisfaction with CAM, and menopausal symptoms. An independent t-test or Mann–Whitney U test was used to compare menopausal symptoms and their dimensions between CAM and non-CAM users. Mann–Whitney U, ANOVA, Kruskal–Wallis, and t-tests were used to compare the scores of menopausal symptoms in terms of demographic variables. Multivariate logistic regression was used to determine the predictors of menopausal symptoms. A significance level of 0.05 was considered.
Results
The mean age of the participants was 54.94 ± 3.08 years (Min = 50 and Max = 60). The mean time passed from the last menstruation was 5.31 ± 3.66 years (Min = 1 and Max = 20). The majority of the participants were educated and unemployed. Only 4.2% of the participants had a history of addiction (opium, cigarettes, or alcohol). About 10.1–49.7% of the participants had a history of diabetes, hypertension, or other chronic diseases (Table 1). In addition, all the participants were married and had no history of uterine cancer or hysterectomy. Only two participants (0.7%) had a history of breast cancer.
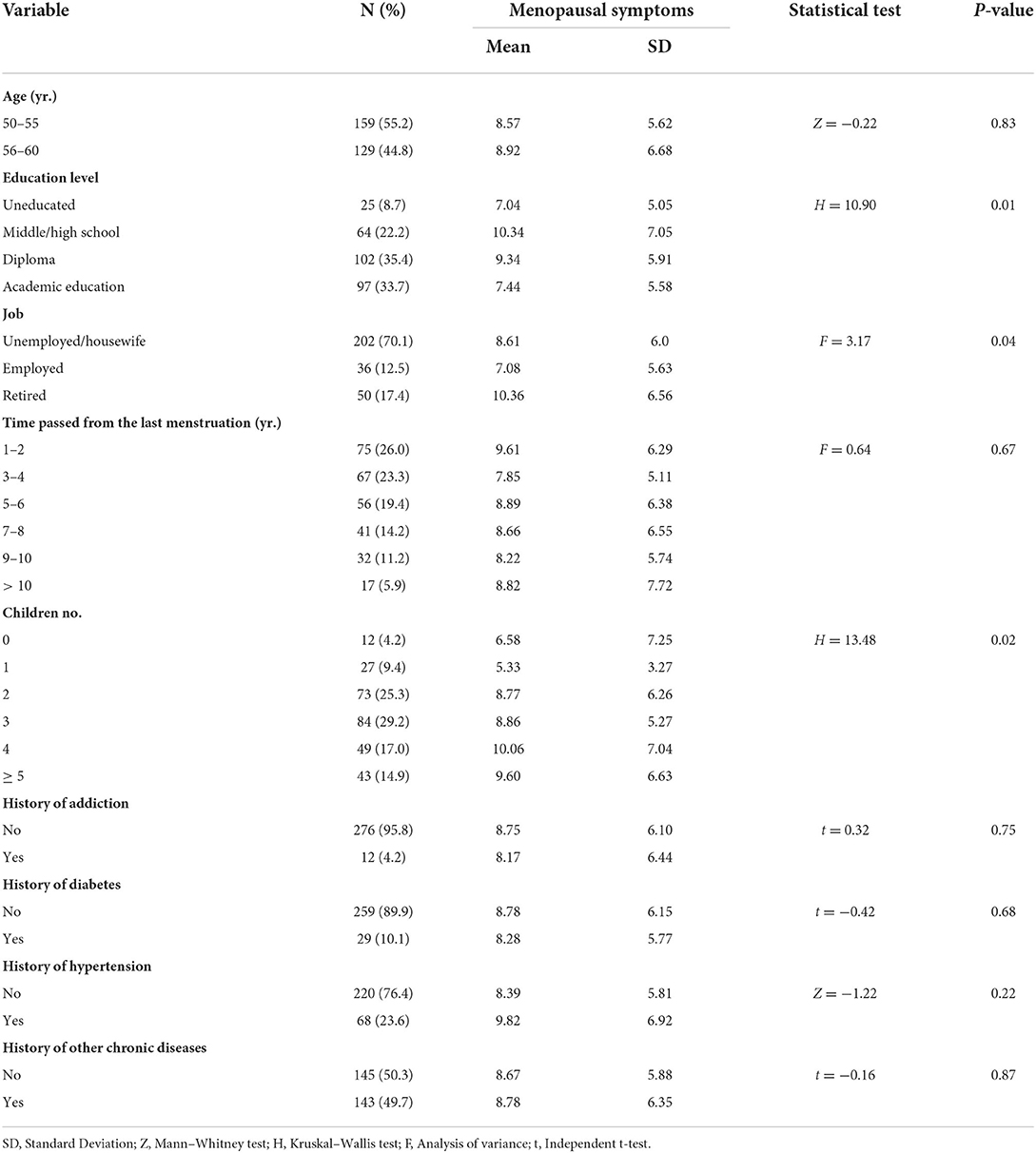
Table 1. Demographic and clinical information of the participants and their association with menopausal symptoms.
The mean score for the menopausal symptoms of the participants was 8.73 ± 6.11 (Min = 0 and Max = 44). And 28.8% (n = 83) of the participants had no/little symptoms, 26.4% (n = 76) had mild, 30.6% (n = 88) had moderate, and 14.2% (n = 41) had severe symptoms. The mean scores for the psychological, somatic-vegetative, and urogenital symptoms are presented in Table 2. In this, 31.6% (n = 91) of the participants had no/little psychological symptoms, 27.4% (n = 79) had mild, 25.4% (n = 73) had moderate, and 15.6% (n = 45) had severe symptoms. A 41.7% (n = 120) of the participants had no/little somatic-vegetative symptoms, 27.8% (n = 80) had mild, 24.7% (n = 71) had moderate, and 5.8% (n = 17) had severe symptoms; 33.7% (n = 97) of the participants had no/little urogenital symptoms, 25.3% (n = 73) had mild, 21.2% (n = 61) had moderate, and 19.8% (n = 57) had severe symptoms.
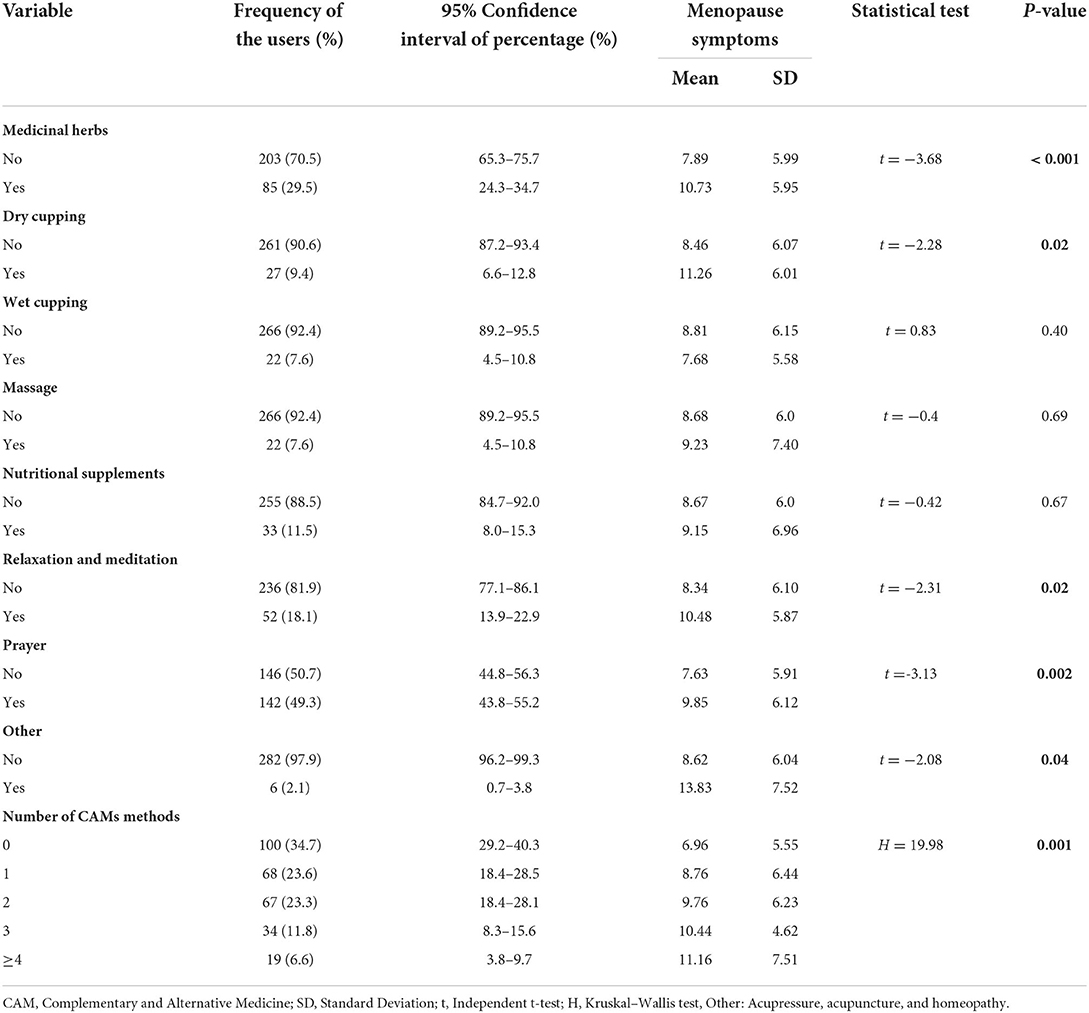
About 65.3% (n = 188, 95% confidence interval = 59.7–71.2) of the participants reported using at least one type of CAM in the previous year. The frequency of using each type of CAM is presented in Table 3. Here, 60.6% (n = 20), 59.15% (n = 84), and 31.76% (n = 27) used nutritional supplements, prayer, and medicinal herbs once a day, respectively; 22.73% (n = 5), 18.18% (n = 4), and 14.81% (n = 4) used massage, wet cupping, and dry cupping once a month, respectively. In addition, 61.54% (n = 32) used relaxation and meditation more than once a week. The mean score of satisfaction with using CAMs was 21.60 ± 5.87 (Min = 0 and Max = 36), which was higher than the midpoint of the scale, that is, 18.
There were significant differences in menopausal symptoms, somatic-vegetative, and urogenital domains between the CAM-users and non-CAM users (p < 0.001) (Table 2). In addition, there was a significant association between medicinal herbs (p < 0.001), dry cupping (p = 0.02), relaxation and meditation (p = 0.02), prayer (p = 0.002), and other methods (p = 0.04), and menopausal symptoms (Table 3).
Among the other study variables, there was a significant association between educational level (p = 0.01), job (p = 0.04), number of children (p = 0.02), and menopausal symptoms (Table 1). A multivariate logistic regression model with a backward method was used for further analysis. The independent variable was the menopausal symptoms (yes/no), while the dependent variables were educational level, job, number of children, and CAM user. The results showed an association only between CAM users and menopausal symptoms. On the other hand, women with menopausal symptoms used more CAM methods compared with women without menopausal symptoms (Odds ratio = 2.25, 95% confidence interval = 1.33–3.80).
Discussion
The study results showed that the menopausal symptoms were mild and desirable, with 28.8% of the women having no menopausal symptoms, while 14.2% of them had severe menopausal symptoms. The mean score of the somatic-vegetative domain was high, which included symptoms such as sexual dysfunction, vaginal dryness, and urinary symptoms. Bahri et al. (53) in Iran also showed a desirable level of menopausal symptoms. According to Rathnayake et al. (54) in Sri Lanka, 47.6% of the women in the menopausal stage reported severe to very severe musculoskeletal disorders, which was inconsistent with the present study. Masjoudi et al. (48) in Iran found that 43.8% of the women in the menopausal stage were asymptomatic, 55.2% experienced mild to severe menopausal symptoms, and 1% experienced moderate to severe menopausal symptoms, which was inconsistent with the present study. Jalili et al. (55) in Iran reported that moderate, severe, and very severe menopausal symptoms were related to sleep disorders, muscle pain, and hot flashes, respectively, which contradicted the present study. According to Makvandi et al. (56) in Iran, the total score of menopausal symptoms was moderate, and the most common menopausal symptoms were muscle pain, sleep problems, and memory loss, which contradicted the results of the present study. This study was different from that of Makvandi et al., Masjoudi et al., Jalili et al., and Rathnayake et al. due to participants' ages, ethnic differences between the studied cities, and geographical, individual, and cultural differences between the studied countries, respectively (56). Menopause exposes women to extensive changes caused by low estrogen levels, including hot flashes and night sweats, dizziness, irregular and rapid heartbeat, atrophy of the vaginal mucosa, sleep disturbance, musculoskeletal pain, difficulty concentrating and memory disorders, and despair (2, 57–59).
The study results also showed that 65.3% of the participants used at least one type of complementary and alternative medicine in the last year, and 60.60, 59.15, and 31.76% of people used dietary supplements, prayers, and medicinal herbs once a day, respectively. According to Ozcan et al. (15) the majority of Turkish women used herbal medicines, dietary supplements, mind-body exercises, and religious approaches to combat hot flashes. Arentz et al. (16) found that more than 70% of Australian women with polycystic ovary syndrome used dietary and herbal supplements. However, Witteman et al. (60) showed that 68.7% reported using CAM/self-care strategies to treat the symptoms of vaginal infection. The types and patterns of CAM are related to socio-cultural backgrounds and are generally influenced by culture, history, and sometimes religion (51). The studies inconsistent with the present one had differences in the sample size, research tools, and cultural and religious factors. The majority of Iranian people are Muslims, who pray every day, and religion and spirituality are tied to their lives (51).
The study results showed that the severity of menopausal symptoms and scores in somatic-vegetative and urogenital domains were higher in CAM users compared to non-CAM users. Women experiencing menopausal symptoms used complementary and alternative medicine more than other postmenopausal non-CAM users. However, the study results indicate no significant difference in the psychological domain between CAM and non-CAM users. According to the study results, there was a statistically significant difference in the severity of menopausal symptoms, medicinal herbs, dry cupping, relaxation and meditation, prayer, and other methods between CAM and non-CAM users. The study results showed that women in the menopausal stage suffered from vasomotor symptoms, psychological symptoms, musculoskeletal pain, osteoporosis, sleep problems, and genital symptoms. Menopause is very stressful for some women, so stress management strategies, such as relaxation, biofeedback, aerobics, yoga, meditation, and breathing techniques can help them cope with menopause and aging in general, and improve their menopausal symptoms (61). According to Ozcan et al. (15) in Turkey, the majority of CAM users in menopause reported lower severity of hot flashes compared with other women in menopause. The results of an evidence-based systematic review study showed that licorice, valerian, soy, sage, ginseng, and so on, improved menopausal symptoms (62). Kheirkhah and Firooznia in Iran also found that herbal tea capsules, Passion flower, Vitex agnus-castus, Liquorice, and soy improved hot flashes among women in menopause (63, 64). Taavoni et al. (65) in Iran showed that Lemon Balm reduced physical, psychological, and reproductive symptoms in postmenopausal women. The studies mentioned above contradicted the present study, in which women who used medicinal herbs experienced more menopausal symptoms. This discrepancy can be attributed to differences in research type, age, and research tools. Johnson et al. (66) showed that mind-body exercise might help reduce stress and some menopausal symptoms among women, and hypnosis clinically had a significant effect on reducing hot flashes. Their result was inconsistent with that of the present study, in which users of yoga had a high level of menopausal symptoms. According to the present study, dietary supplements did not affect the severity of menopausal symptoms. Therefore, Jokar et al. (67) in Iran showed that vitamin C was not effective in reducing depression among postmenopausal women. They recommended further studies on the effect of vitamin C on anxiety and depression among postmenopausal women. Shafiee et al. (28) indicated that spiritual interventions were effective in reducing depression and improving the psychological dimension among postmenopausal women. Their study was inconsistent with the present one regarding the psychological dimension. The present study showed the effectiveness of acupressure in improving menopausal symptoms, but according to Armand et al. and Abedian et al. acupressure was effective in reducing anxiety, hot flashes, night sweats (68), and sleep disorders (69). Sultana in India found that dry cupping was effective in reducing the pain intensity of dysmenorrhea, which was inconsistent with the present study (70). The differences among recent studies may be due to the differences in research tools, the type of intervention, and sample size, as well as personal, cultural, and geographical differences.
Limitations
Self-assessment was used to collect the data, so the menopausal symptoms might be reported less realistically. Therefore, a female researcher gathered information to overcome this limitation so that the participants felt less ashamed and upset. Postmenopausal women were rarely referred to the health centers during the COVID-19 outbreak. To overcome this limitation, a combination of face-to-face and virtual sampling was used. Postmenopausal women did not know about some complementary and alternative medicines, so the researchers tried to give them information about the types of complementary medicine. Another limitation was that postmenopausal women were selected from only one city. Performing national and international studies makes it possible to generalize these results. In addition, the small number of female researchers was one of the limitations of the present study.
Conclusion
According to the study results, 30.6% of the women suffered from menopausal symptoms moderately, while 14.2% of them suffered from menopausal symptoms severely. The total score of menopausal symptoms and the scores of somatic-vegetative and urogenital domains were higher in CAM users compared with non-CAM users. However, the study results indicated no significant difference in the psychological domain between CAM and non-CAM users. There was also a statistically significant difference in the severity of menopausal symptoms between users and non-users of the medicinal herbs, dry cupping, relaxation and meditation, prayer, and other methods. According to the study results as well as the severity of menopausal symptoms in women who used complementary medicine, more studies are suggested to investigate the use of complementary and alternative medicine among postmenopausal women. In addition, further studies are recommended to investigate the effects of complementary and alternative medicine on the psychological domain to relieve anxiety, stress, depression, and sleep disorders among women. Given that the present study was performed on women aged 50–60 years who were in normal menopause, it is recommended that other studies be conducted to evaluate the effect of complementary medicine on the severity of menopause in women aged above 60 years who were not in normal menopause.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Kerman University of Medical Sciences. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MD designed the study. MD, ZI, and AGH wrote the manuscript. MD and AGH contributed to the study design, provided critical feedback on the study and statistical analysis, and inputted the draft of this manuscript. ZI and MHA collected data. All authors have read and approved the final manuscript.
Acknowledgments
We would like to thank all the menopausal women and staff of the health centers in Kerman for their cooperation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ilankoon IMPS, Samarasinghe K, Elgán C. Menopause is a natural stage of aging: a qualitative study. BMC Womens Health. (2021) 21:47. doi: 10.1186/s12905-020-01164-6
2. Abbasiniya H, Bandalizadeh Z, Vakilian KK, Jafari Z, Matouripour P, Ranjbaran M, et al. Effect of chamomile extract on sleep disorder in menopausal women. Iran J Obstet Gynecol Infertil. (2016) 19:1–7. doi: 10.22038/ijogi.2016.7631
3. Bahri N, Pourali L, Esmaeeli H. Application of various menopausal symptoms treatment options and its related factors, Gonabad-2016. Iran J Obstet Gynecol Infertil. (2016) 19:1–8. doi: 10.22038/ijogi.2016.7796
4. Zamaniyan M, Moosazadeh M, Peyvandi S, Jaefari K, Goudarzi R, Moradinazar M, et al. Age of natural menopause and related factors among the tabari cohort. J Menopausal Med. (2020) 26:18. doi: 10.6118/jmm.19004
5. Sharman Moser S, Chodick G, Bar-On Bar-On S, Shalev V. Healthcare utilization and prevalence of symptoms in women with menopause: a real-world analysis. Int J Womens Health. (2020) 12:445–54. doi: 10.2147/IJWH.S246113
6. Yisma E, Eshetu N, Ly S, Dessalegn B. Prevalence and severity of menopause symptoms among perimenopausal and postmenopausal women aged 30-49 years in gulele sub-city of addis Ababa, Ethiopia. BMC Womens Health. (2017) 17:124. doi: 10.1186/s12905-017-0484-x
7. Santoro N, Epperson CN, Mathews SB. Menopausal symptoms and their management. Endocrinol Metab Clin North Am. (2015) 44:497–515. doi: 10.1016/j.ecl.2015.05.001
8. Heydari L, Suhrabi Z, Sayehmiri F, Sayehmiri K. Effect of herbaceous medicines effective in hot flashes of menopause women: a systematic review and meta-analysis in Iran. Iran J Obstet Gynecol Infertil. (2014) 17:16–25. Available online at: http://www.sid.ir/fa/VEWSSID/J_pdf/638139310903.pdf
9. Sarayloo K, Latifnejad Roudsari R. Critical evaluation of the published clinical trials regarding the effect of complementary medicine on menopausal symptoms. Iran J Obstet Gynecol Infertil. (2018) 21:87–98. doi: 10.22038/ijogi.2018.11231
10. Amiri Pebdani M, Taavoni S, Haghani H. The effect of ginkgo biloba extract on sexual activity in 50–60 years menopausal women amiri pebdani. Complement Med J Fac Nurs Midwifery. (2012) 2:23–33. Available online at: http://cmja.arakmu.ac.ir/article-1-120-en.html
11. Posadzki P, Lee MS, Moon TW, Choi TY, Park TY, Ernst E. Prevalence of complementary and alternative medicine (CAM) use by menopausal women: a systematic review of surveys. Maturitas. (2013) 75:34–43. doi: 10.1016/j.maturitas.2013.02.005
12. Fait T. Menopause hormone therapy: latest developments and clinical practice. Drugs Context. (2019) 8:212551. doi: 10.7573/dic.212551
13. Lund KS, Siersma V, Brodersen J, Waldorff FB. Efficacy of a standardised acupuncture approach for women with bothersome menopausal symptoms: a pragmatic randomised study in primary care (the ACOM study). BMJ Open. (2019) 9:e023637. doi: 10.1136/bmjopen-2018-023637
14. Rosen JE, Gardiner P, Lee SL. Complementary and Integrative Treatments. Otolaryngol Clin North Am. (2013) 46:423–35. doi: 10.1016/j.otc.2013.02.004
15. Ozcan H, Çolak P, Oturgan B, Gülsever E. Complementary and alternative treatment methods for menopausal hot flashes used in Turkey. Afr Health Sci. (2019) 19:3001–8. doi: 10.4314/ahs.v19i4.21
16. Arentz S, Smith CA, Abbott JA, Bensoussan A. A survey of the use of complementary medicine by a self-selected community group of Australian women with polycystic ovary syndrome. BMC Complement Alternat Med. (2014) 14:472. doi: 10.1186/1472-6882-14-472
17. Parveen R, Shameem I. Effect of wet cupping (hijamat bil shurt) in the management of secondary amenorrhea (Ehtebas Tams Sanwi). Undefined. (2014) 1:12–9. Available online at: https://www.researchgate.net/publication/329521955
18. Avis NE, Coeytaux RR, Isom S, Prevette K, Morgan T. Acupuncture in Menopause (AIM) study: a pragmatic, randomized controlled trial. Menopause. (2016) 23:626–37. doi: 10.1097/GME.0000000000000597
19. Hadizadeh Talasaz Z, Khadivzadeh T, Firoozi M, Azizi H, Irani M. The usage of ear acupressure in gynecology and obstetrics: a systematic review of clinical Trials. Iran J Obstet Gynecol Infertil. (2018) 21:42–54. Available online at: http://ijogi.mums.ac.ir/article_11620.html
20. Espí-López G V., Monzani L, Gabaldón-García E, Zurriaga R. The beneficial effects of therapeutic craniofacial massage on quality of life, mental health and menopausal symptoms and body image: a randomized controlled clinical trial. Complement Ther Med. (2020) 51:102415. doi: 10.1016/j.ctim.2020.102415
21. Saensak S, Vutyavanich T, Somboonporn W, Srisurapanont M. Relaxation for perimenopausal and postmenopausal symptoms. Cochrane Database Syst Rev. (2014) 7:CD008582. doi: 10.1002/14651858.CD008582.pub2
22. Cramer H, Peng W, Lauche R. Yoga for menopausal symptoms—a systematic review and meta-analysis. Maturitas. (2018) 109:13–25. doi: 10.1016/j.maturitas.2017.12.005
23. Babakhanian M, Ghazanfarpour M, Kargarfard L, Roozbeh N, Darvish L, Khadivzadeh T, et al. Effect of aromatherapy on the treatment of psychological symptoms in postmenopausal and elderly women: a systematic review and meta-analysis. J menopausal Med. (2018) 24:127–32. doi: 10.6118/jmm.2018.24.2.127
24. Soleymani M, Siassi F, Qorbani M, Khosravi S, Aslany Z, Abshirini M, et al. Dietary patterns and their association with menopausal symptoms: a cross-sectional study. Menopause. (2019) 26:365–72. doi: 10.1097/GME.0000000000001245
25. Desiderio F, Rudnas B, Panzini I, Pini E, Gianni L, Tamburini E, et al. Homeopathy in the treatment of menopausal symptoms in patients with early breast cancer. Ann Oncol. (2015) 26:vi25. doi: 10.1093/annonc/mdv336.76
26. Mo Maddy &, Jang H.-J. Effects of music therapy on depression and quality of life in peri-menopausal women. Asia Life Sci. (2018) 913–9.
27. Rodrigues IF, Freitas GC do N, Oliveira MM de, Aranha REL de B, Martins WKN, Lemos MTM, et al. Impact of hydrotherapy on the quality of life of menopausal women. Res Soc Dev. (2020) 9:e62985292. doi: 10.33448/rsd-v9i8.5292
28. Shafiee Z, Zandiyeh Z, Moeini M, Gholami A. The effect of spiritual intervention on postmenopausal depression in women referred to urban healthcare centers in isfahan: a double-blind clinical trial. Nurs Midwifery Stud. (2016) 5:e32990. doi: 10.17795/nmsjournal32990
29. Khalesi ZB, Beiranvand SP, Bokaie M. Efficacy of chamomile in the treatment of premenstrual syndrome: a systematic review. J Pharmacopuncture. (2019) 22:204–9. doi: 10.3831/KPI.2019.22.028
30. Naseri R, Farnia V, Yazdchi K, Alikhani M, Basanj B, Salemi S. Comparison of vitex agnus-castus extracts with placebo in reducing menopausal symptoms: a randomized double-blind study. Korean J Fam Med. (2019) 40:362–7. doi: 10.4082/kjfm.18.0067
31. Eatemadnia A, Ansari S, Abedi P, Najar S. The effect of hypericum perforatum on postmenopausal symptoms and depression: a randomized controlled trial. Complement Ther Med. (2019) 45:109–13. doi: 10.1016/j.ctim.2019.05.028
32. Kashani L, Esalatmanesh S, Eftekhari F, Salimi S, Foroughifar T, Etesam F, et al. Efficacy of Crocus sativus (saffron) in treatment of major depressive disorder associated with post-menopausal hot flashes: a double-blind, randomized, placebo-controlled trial. Arch Gynecol Obstet. (2018) 297:717–24. doi: 10.1007/s00404-018-4655-2
33. Ataei-Almanghadim K, Farshbaf-Khalili A, Ostadrahimi AR, Shaseb E, Mirghafourvand M. The effect of oral capsule of curcumin and vitamin e on the hot flashes and anxiety in postmenopausal women: a triple blind randomised controlled trial. Complement Ther Med. (2020) 48:102267. doi: 10.1016/j.ctim.2019.102267
34. Shirazi M, Jalalian MN, Abed M, Ghaemi M. The effectiveness of melissa officinalis L. versus citalopram on quality of life of menopausal women with sleep disorder: a randomized double-blind clinical trial. Rev Bras Ginecol e Obs. (2021) 43:126–30. doi: 10.1055/s-0040-1721857
35. Saeidi A, Jabbour G, Ahmadian M, Abbassi-Daloii A, Malekian F, Hackney AC, et al. Independent and combined effects of antioxidant supplementation and circuit resistance training on selected adipokines in postmenopausal women. Front Physiol. (2019) 10:484. doi: 10.3389/fphys.2019.00484
36. Ataollahi M, Akbari SAA, Mojab F, Alavi Majd H. The effect of wheat germ extract on premenstrual syndrome symptoms. Iran J Pharm Res. (2015) 14:159–66. Available online at: https://pubmed.ncbi.nlm.nih.gov/25561922/
37. Lee HW, Lim H-J, Jun JH, Lim H-S, Lee MS. Fennel (Foeniculum vulgare) on management of menopausal symptoms. Medicine (Baltimore). (2018) 97:e0223. doi: 10.1097/MD.0000000000010223
38. Mirabi P, Mojab F. The effects of valerian root on hot flashes in menopausal women. Iran J Pharm Res. (2013) 12:217–22. Available online at: https://pubmed.ncbi.nlm.nih.gov/24250592/
39. Taavoni S, Ekbatani NN, Haghani H. Effect of tribulus terrestris , ginger, saffron, and cinnamomum on menopausal symptoms: a randomised, placebo-controlled clinical trial. Menopausal Rev. (2017) 1:19–22. doi: 10.5114/pm.2017.67366
40. Ghazanfarpour M, Sadeghi R, Latifnejad Roudsari R, Khadivzadeh T, Khorsand I, Afiat M, et al. Effects of flaxseed and hypericum perforatum on hot flash, vaginal atrophy and estrogen-dependent cancers in menopausal women: a systematic review and meta-analysis. Avicenna J phytomedicine. (2016)6:273–83. Available online at: https://pubmed.ncbi.nlm.nih.gov/27462550/
41. Ahsan M. The effect of soy isoflavones on the menopause rating scale scoring in perimenopausal and postmenopausal women: a pilot study. J Clin Diagnostic Res. (2017) 11:FC13–6. doi: 10.7860/JCDR/2017/26034.10654
42. Nouri Hekmat S. Implementation of Services Quality (SERVQUAL) Tool in Hazrate Rasoule Akram Hospital (dissertation). Tehran: TUMS (2006).
43. Masoumi SZ, Alavipour N, Parsa P, Kazemi F. Demographic factors affecting sexual dysfunction in postmenopausal women. J Educ Community Heal. (2020) 7:5–12. doi: 10.29252/jech.7.1.5
44. Azimipour A, Loripoor M, Sadeghi T. The effect of black cohosh (cimicifuga racemosa) on menopausal symptoms: a randomized clinical trial. J Rafsanjan Univ Med Sci. (2017) 16:715–26. Available online at: http://journal.rums.ac.ir/article-1-3523-en.html
45. Heinemann L, Potthoff P, Schneider H. International versions of the menopause rating scale (MRS). Heal Qual Life Outcomes. (2003) 30:28. doi: 10.1186/1477-7525-1-28
46. Taavoni S, Nazem Ekbatani N, Izadjoo M, Haghani H. Effect of lemon balm supplementation on menopausal symptoms. Complement Med J Fac Nurs Midwifery. (2016) 5:1324–36. Available online at: http://cmja.arakmu.ac.ir/article-1-382-en.html
47. Sadeghi T, Azimi A, Loripoor M. Comparing the effect of black Cohosh versus Vitagnus on the impovement of menopause symptoms. Iran J Obstet Gynecol Infertil. (2019) 21:1–10. Available online at: https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=749930
48. Masjoudi M, Amjadi MA, Leili EKN. Severity and frequency of menopausal symptoms in middle aged women, Rasht, Iran. J Clin Diagnostic Res. (2017) 11:QC17–21. doi: 10.7860/JCDR/2017/26994.10515
49. Darsareh F, Taavoni S, Joolaee S, Haghani H. Effect of aromatherapy massage on menopausal symptoms: a randomized placebo-controlled clinical trial. Menopause. (2012) 19:995–9. doi: 10.1097/gme.0b013e318248ea16
50. Shakeri F, Taavoni S, Goushegir A, Haghani H. Effectiveness of red clover in alleviating menopausal symptoms: a 12-week randomized, controlled trial. Climacteric. (2015) 18:568–73. doi: 10.3109/13697137.2014.999660
51. Dehghan M, Namjoo Z, Bahrami A, Tajedini H, Shamsaddini-lori Z, Zarei A, et al. The use of complementary and alternative medicines, and quality of life in patients under hemodialysis: a survey in southeast Iran. Complement Ther Med. (2020) 51:102431. doi: 10.1016/j.ctim.2020.102431
52. Sheikhrabori A, Dehghan M, Ghaedi F, Khademi GR. Complementary and alternative medicine usage and its determinant factors among diabetic patients: an Iranian case. J Evidence-Based Complement Altern Med. (2017) 22:449–54. doi: 10.1177/2156587216675079
53. Bahri N, Afiat M, Aghamohamadian H, Delshad Noughabi A, Bahri N. Investigating the relationship between severity of menopausal symptoms and depression, anxiety and other menopausal symptoms. Iran J Obstet Gynecol Infer. (2013) 16:14–20. Available online at: http://ijogi.mums.ac.ir/article_639.html
54. Rathnayake N, Lenora J, Alwis G, Lekamwasam S. Prevalence and severity of menopausal symptoms and the quality of life in middle-aged women: a study from Sri Lanka. Nurs Res Pract. (2019) 2019:1–9. doi: 10.1155/2019/2081507
55. Jalili L, Yazdi Zadeh H, Sharifi N, Abedi P, Najar S, Asad Mobini E. The relationship between physical activity and the severity of menopause symptoms in menopausal women in ahvaz, Iran. Iran J Obstet Gynecol Infertil. (2014) 17:15–23. doi: 10.22038/IJOGI.2014.2830
56. Makvandi S, Zargar Shushtari S, Yazdizadeh H, Zaker Hoseini V, Bastami A. Frequency and severity of menopausal symptoms and its relationship with demographic factors in pre-and postmenopausal women of ahvaz, Iran. Iran J Obstet Gynecol Infertil. (2013) 16:7–15. doi: 10.22038/ijogi.2013.825
57. Graziottin A, Leiblum SR. Biological and psychosocial pathophysiology of female sexual dysfunction during the menopausal transition. J Sex Med. (2005) 2:133–45. doi: 10.1111/j.1743-6109.2005.00129.x
58. Shariat Moghani S, Simbar M, Rashidi Fakari F, Ghasemi V, Dolatian M, Golmakani N, et al. The relationship between stress, anxiety and depression with menopausal women experiences. Sci J Hamadan Nurs Midwifery Fac. (2018) 26:333–40. doi: 10.30699/sjhnmf.26.a5.333
59. Shafiei F, Asar Davalloei R, Ameri A, Fesharaki M, Ebadi Fard Azar F. Effect of training on level of knowledge and attitude of female health workers on menopause and its related proble. J Guilan Univ Med Sci. (2006) 14:67–73. Available online at: http://journal.gums.ac.ir/article-1-498-en.html
60. Witteman L, van Wietmarschen HA, van der WET. Complementary medicine andself-care strategies in women with(Recurrent) urinary tract and vaginal infections: a cross sectional study on use and perceived effectiveness in the Netherlands. Antibiotics. (2021) 10:250. doi: 10.3390/antibiotics10030250
61. Jayabharathi B, Arulappan J. Complementary health approach to quality of life in menopausal women : a community-based interventional study. Clin Interv Aging. (2014) 9:1913–21. doi: 10.2147/CIA.S70064
62. Ebrahimi A, Tayebi N, Fatemeh A, Akbarzadeh M. Investigation of the role of herbal medicine , acupressure , and acupuncture in the menopausal symptoms : an evidence - based systematic review study. J Fam Med Prim Care. (2020) 9:2638–49. . doi: 10.4103/jfmpc.jfmpc_1094_19
63. Kheirkhah M, Naieri SD, Tabari NS. The effect of herbal tea capsule on menopause hot flashes. J Family Med Prim Care. (2018) 7:1074–8. doi: 10.4103/jfmpc.jfmpc_332_17
64. Firooznia R, Hosseini M.A, Karbord A.A YS. A public educational guideline development to relieve post menopausal hot flashes symptoms in women between 45-60 years old based on proper diet and exercise. J Knowl Heal. (2014) 9:52–7. doi: 10.22100/jkh.v9i2.452
65. Taavoni S, Nazem Ekbatani N, Izadjoo M, Haghani H. Effect of lemon balm supplementation on menopausal symptoms. Complement Med J. (2015)5:1324–36. Available online at: http://cmja.arakmu.ac.ir/article-1-382-en.html
66. Johnson A, Roberts L, Elkins G. Complementary and alternative medicine for menopause. J Evidence-Based Integr Med. (2019) 24:1–14. doi: 10.1177/2515690X19829380
67. Jokar A, Farahi F. Effect of vitamin C on depression in menopausal women with balanced diet: a Randomized clinical trial. Iran J Obstetr Gynecol Infertility. (2014) 17:18–23. doi: 10.22038/ijogi.2014.3557
68. Armand M, Ozgoli G, Giti RH, Majd HA. Effect of acupressure on early complications of menopause in women referring to selected health care centers. Iran J Nursing Midwifery Res. (2017) 22:237–42. doi: 10.4103/1735-9066.208165
69. Abedian Z, Eskandari L, Abdi H, Ebrahimzadeh S. The effect of acupressure on sleep quality in menopausal women: a randomized control trial. Iran J Med Sci. (2015) 40:328–334. Available online at: https://pubmed.ncbi.nlm.nih.gov/26170519/
70. Sultana A, Ur Rahman K, Farzana M, Lone A. Efficacy of hijamat bila shurt (dry cupping) on intensity of pain in dysmenorrhoea-a preliminary study. Anc Sci Life. (2010) 30:47–50. Available online at: https://pubmed.ncbi.nlm.nih.gov/22557425/
Keywords: complementary and alternative medicine, menopause, women, symptom, psychological symptoms, somatic-vegetative symptoms, urogenital symptoms
Citation: Dehghan M, Isari Z, Abbaszadeh MH and Ghonchehpour A (2022) Menopause symptoms in women and its relation with using complementary and alternative medicines: A survey in southeast Iran. Front. Public Health 10:947061. doi: 10.3389/fpubh.2022.947061
Received: 18 May 2022; Accepted: 27 July 2022;
Published: 22 August 2022.
Edited by:
Naseem Akhtar Qureshi, Al-Falah University, IndiaReviewed by:
Mehdi Bamorovat, Kerman University of Medical Sciences, IranÖzge Öz Yildirim, Ondokuz Mayis University, Turkey
Copyright © 2022 Dehghan, Isari, Abbaszadeh and Ghonchehpour. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Asma Ghonchehpour, a.ghonchehpoor77@gmail.com
†Present address: Asma Ghonchehpour, Razi Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran
‡ORCID: Mahlagha Dehghan orcid.org/0000-0002-4205-829X
Asma Ghonchehpour orcid.org/0000-0002-0668-7072
 Mahlagha Dehghan
Mahlagha Dehghan Zahra Isari2
Zahra Isari2 Asma Ghonchehpour
Asma Ghonchehpour