- 1Department of Ultrasound Imaging, Zhongshan City People’s Hospital, Zhongshan, China
- 2Department of Breast Surgery, Zhongshan City People’s Hospital, Zhongshan, China
Background: Several obstacles can hinder breast cancer screening. This study aimed to investigate the knowledge, attitude, and practice (KAP) toward ultrasound screening for breast cancer in women.
Methods: This cross-sectional study recruited women who visited the breast specialist clinic of Zhongshan City People’s Hospital (a tertiary hospital) between August 2022 and April 2023 through convenience sampling. KAP scores ≥70% were considered adequate.
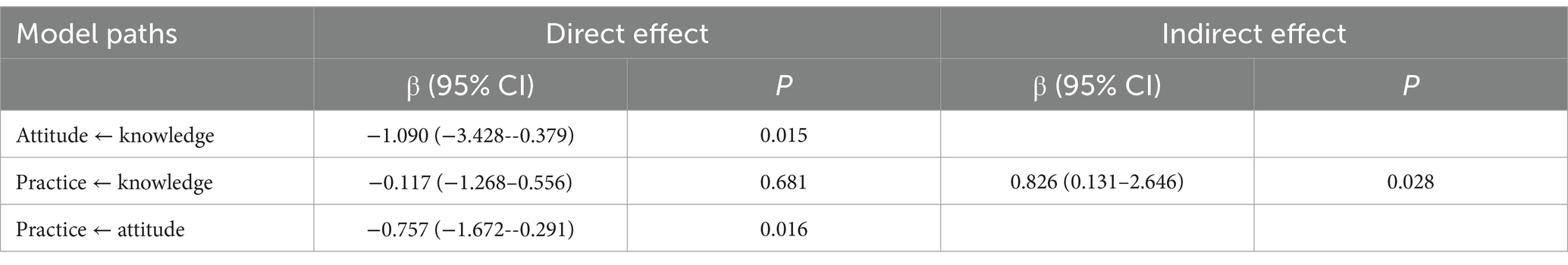
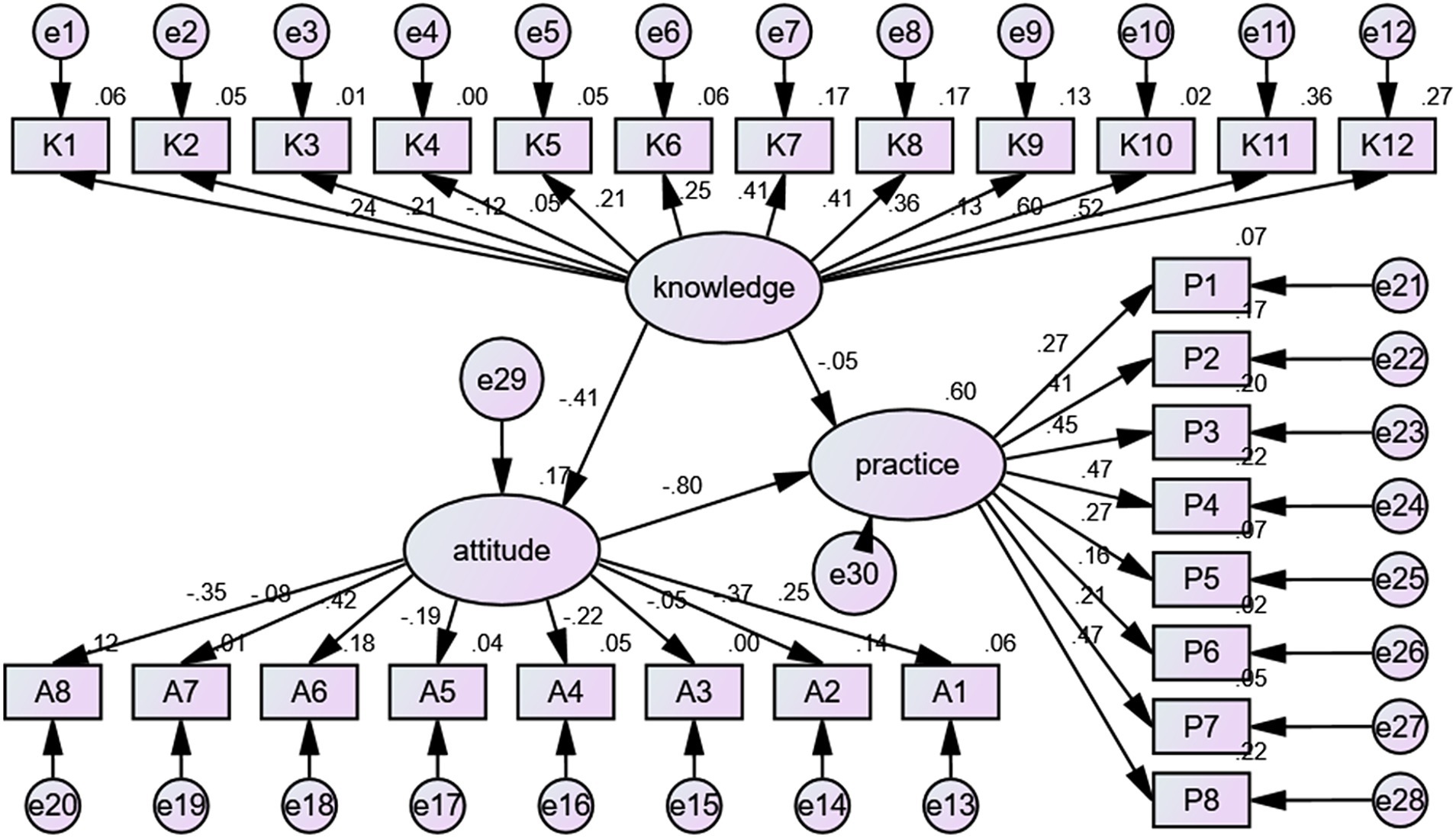
Results: This study enrolled 501 participants. The mean knowledge, attitude, and practice levels were 8.56 ± 1.81/12 (possible range 0–12, 71.33%), 29.80 ± 2.71 (possible range 8–40, 74.50%), and 32.04 ± 3.09 (possible range 8–40, 80.10%). Senior high school education (vs. junior high school and below, coefficient = 1.531, 95%CI: 1.013–2.312, p = 0.044), bachelor’s education and above (vs. junior high school and below, coefficient = 5.315, 95%CI: 3.546–7.966, p < 0.001), housewife or unemployed (vs. employed, coefficient = 0.671, 95%CI: 0.466–0.966, p = 0.032), and a history of breast ultrasound (vs. no, coefficient = 1.466, 95%CI: 1.121–1.917, p = 0.005) were independently and positively associated with knowledge. Knowledge (coefficient = 1.303, 95%CI: 1.100–1.544, p = 0.002) and monthly income >10,000 (vs. <5,000, coefficient = 4.364, 95%CI: 1.738–10.956, p = 0.002) were independently and positively associated with attitude. Only attitude (coefficient = 1.212, 95%CI: 1.096–1.340, p < 0.001) was independently and positively associated with the practice. A structural equation modeling (SEM) analysis was used to estimate causality among KAP dimensions, showing that knowledge directly influenced attitude (β = −1.090, p = 0.015), knowledge did not directly influence practice (β = −0.117, p = 0.681) but had an indirect influence (β = 0.826, p = 0.028), and attitude directly influenced practice (β = −0.757, p = 0.016).
Conclusion: Women in Zhongshan City had good knowledge, favorable attitudes, and active practice toward breast ultrasound screening for breast cancer. Women’s characteristics associated with a poorer KAP were identified, allowing for more targeted interventions.
1 Introduction
Breast cancer is the most common cancer diagnosed in women worldwide (1, 2), with 2,261,419 new cases in 2020 (estimated) and 684,996 deaths (3). The risk factors include gene mutations and polymorphisms, older age, no pregnancies, hormone exposure, lifestyle, and radiation exposure (4, 5). Despite the high incidence and mortality, breast cancer survivors in the United States of America display a 5-year survival of 99% for women with localized disease, 85% for regional disease, and 27% for women with distant metastases (6).
Many patients are asymptomatic until reaching the advanced or metastatic stage. Hence, breast cancer is mainly detected through screening for abnormalities, including palpable breast mass, palpable axillary mass, nipple discharge, skin changes, asymmetric changes, or pain (5). Screening for breast cancer refers to testing performed in asymptomatic women to detect the disease early to decrease morbidity and/or mortality (5). The 15-year absolute reduction in BC-related mortality with mammography is 40.6 deaths per 100,000 women aged 40–49, 61.7 deaths per 100,000 women ≥50 years of age, and 211.8 deaths per 100,000 women aged 60–69 (7, 8). Still, the impact on overall survival remains controversial (8, 9).
Screening modalities include breast self-examination, physical examination, and imaging, with mammography being the screening modality of choice for the early detection of breast cancer (5). Ultrasound is also a modality of choice for examining breast symptoms like a mass or nipple discharge (5). Ultrasound can be used as an adjunct to mammography for detecting breast cancer, especially in women with dense breasts (10–14). In women with dense breasts, the sensitivity of mammography is 50%, while the sensitivity of mammography plus ultrasound is 77.5% (10, 15). Still, breast ultrasound screening can be performed stand-alone and is popular in some countries, with many women living in remote areas (16). Indeed, suitcase-sized portable ultrasound systems are available and have no special power or occupational exposure requirements, while portable mammography systems are not available. In addition, mammography requires radiation safety procedures.
Because Chinese women have denser breasts than Westerners (17) and because breast ultrasound is non-invasive and inexpensive, it is a popular BC screening modality in China (18). A central feature of breast cancer screening programs is their voluntary aspect (16, 19). The women’s health literacy and beliefs will influence how they participate in breast cancer screening. Hence, Chinese women from the general population may lack the proper knowledge and awareness of ultrasound screening for breast cancer. In addition, several programs offer different screening modalities, and the women’s choices can influence the screening outcomes. The knowledge, attitude, and practice (KAP) methodology provides qualitative and quantitative data about the gaps, misunderstandings, misconceptions, and barriers toward the optimal implementation of a given healthcare concept in a given population (20, 21).
No data on the KAP toward breast cancer ultrasound screening in continental China are available. Still, previous studies reported highly variable KAP toward breast cancer screening in different countries (22–25). Breast screening services and programs vary widely among countries with different characteristics, socioeconomic characteristics, customs, patient education, and healthcare systems, and the results of KAP studies cannot be extrapolated to other countries or sometimes regions. Therefore, it is crucial to identify the obstacles hindering breast cancer screening in China to adopt more effective methods to promote screening. Therefore, this study aimed to assess the KAP of women toward ultrasound screening for breast cancer. The results could be used to design and implement educational and motivational interventions to improve the KAP toward breast cancer screening in Chinese women.
2 Methods
2.1 Study design and participants
This cross-sectional study was conducted at Zhongshan City People’s Hospital between August 2022 and April 2023. The participants were women recruited by convenience sampling. The study was approved by the Medical Ethics Committee of Zhongshan People’s Hospital. All participants signed the informed consent form.
The inclusion criteria were (1) Han nationality and (2) ≥18 years of age. The exclusion criteria were (1) cognitive impairment, (2) communication disorder, or (3) not completing the questionnaire.
2.2 Questionnaire
The questionnaire was designed according to previous studies (26, 27). The questionnaire was reviewed by two senior experts. The questionnaire was pre-tested by 53 women, and Cronbach’s α coefficient value was 0.782 (i.e., acceptable internal consistency).
The final questionnaire included four dimensions: demographic characteristics, knowledge dimension (including knowledge of breast cancer and breast ultrasound), attitude dimension, and practice dimension (Supplementary material). The basic characteristics were covered by nine items. The knowledge part included 12 items; correct answers were scored 1 point, and wrong/unclear answers were scored 0 points, with a theoretical score range of 0–12 points. The attitude part consisted of eight items, using a 5-point Likert scale, from very positive (5 points) to very negative (1 point). The total score ranged from 8 to 40 points. The practice part included eight items, using a 5-point Likert scale, from very positive (5 points) to very negative (1 point). The total score ranged from 8 to 40 points.
The questionnaires were distributed to the participants in breast specialist clinics. Five doctors and nurses were responsible for promoting and distributing the questionnaires were trained for this study and acted as research assistants.
2.3 Sample size
The formula
can be used to calculate the sample size of cross-sectional surveys. In the formula, “n” represents the sample size for each group, “α” represents the type I error, which is typically set at 0.05, Z1-α/2 = 1.96, δ represents the allowable error, typically set at 0.05, and “p” is set at 0.5 (as setting it at 0.5 maximizes the value and ensures a sufficiently large sample size). Hence, the calculated sample size was 384. Considering an estimated questionnaire response rate of 80%, 480 valid questionnaires were needed.
2.4 Statistical analysis
SPSS 26.0 (IBM Corporation, Armonk, NY, United States) was used for analysis. The continuous variables were presented as mean ± standard deviation (SD) and analyzed using Student’s t-test (two groups) or one-way ANOVA (more than two groups). Categorical variables were expressed as n (%). The Spearman analysis was used to analyze the correlation of knowledge, attitude, and practice scores. The variables with p < 0.10 in the univariable analyses were entered in the multivariable linear regression analyses to determine the factors independently associated with KAP. A structural equation modeling (SEM) is a statistical statement of the relationship between variables, sometimes called a path diagram, and is a specific representation of the model in a graphical manner. The relationship between each latent variable should be supported theoretically or proved in practice, and finally, a research framework diagram. SEM was employed to test the following hypotheses: (1) knowledge had impacts on attitude; (2) knowledge had impacts on practice; (3) attitude had impacts on practice. Confirmatory factor analysis and model fitting were evaluated using the following indices: CFI (comparative fit index), IFI (incremental fit index), TLI (Tucker–Lewis index), RMSEA (root mean square error of approximation), and CMIN/DF (chi-square value/degrees of freedom). Two-sided p-values <0.05 were regarded as statistically significant.
3 Results
3.1 Characteristics of the study population
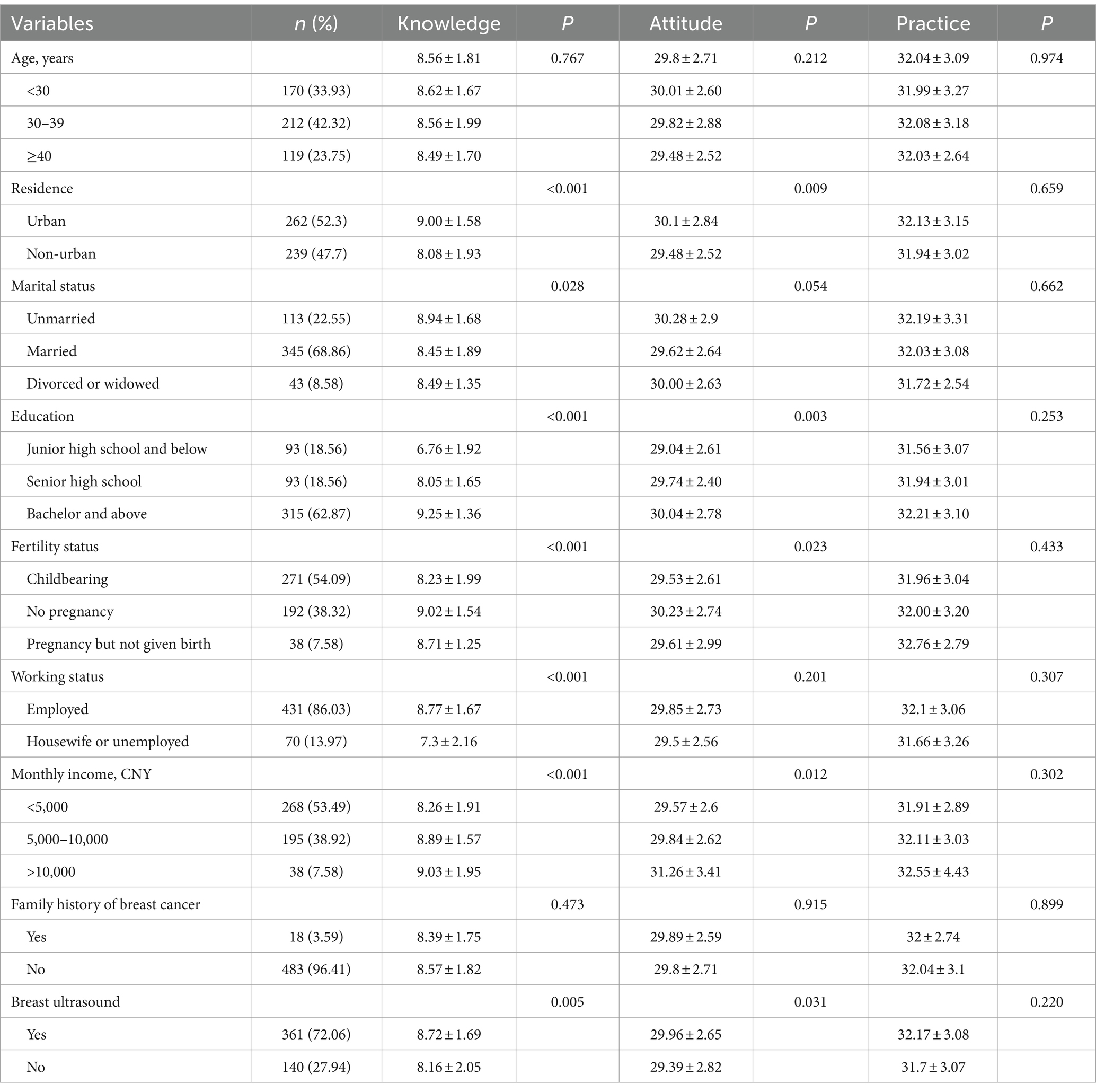
The study enrolled 514 participants, with two persons under 18 years of age and 11 persons belonging to ethnic minorities. Finally, 501 valid questionnaires were valid. Most participants were 30–39 (42.32%), living in urban areas (52.3%), had a bachelor’s degree or above (62.87%), with children (54.09%), employed (86.03%), with monthly income <5,000 (53.49%), without a family history of breast cancer (96.41%), and underwent a breast ultrasound (72.06%) (Table 1).
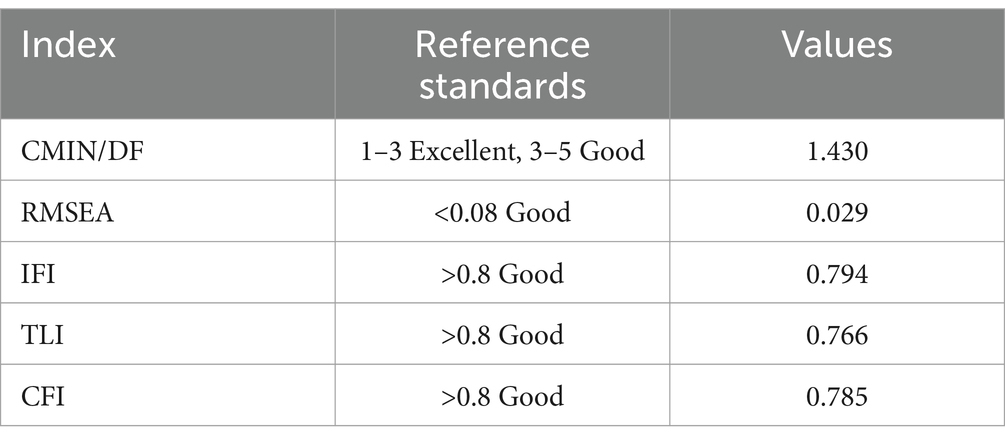
The confirmatory factor analysis showed CFI = 0.816 (>0.8 is good), IFI = 0.826 (>0.8 is good), RMSEA = 0.025 (<0.08 is good), and CMIN/DF = 1.306.
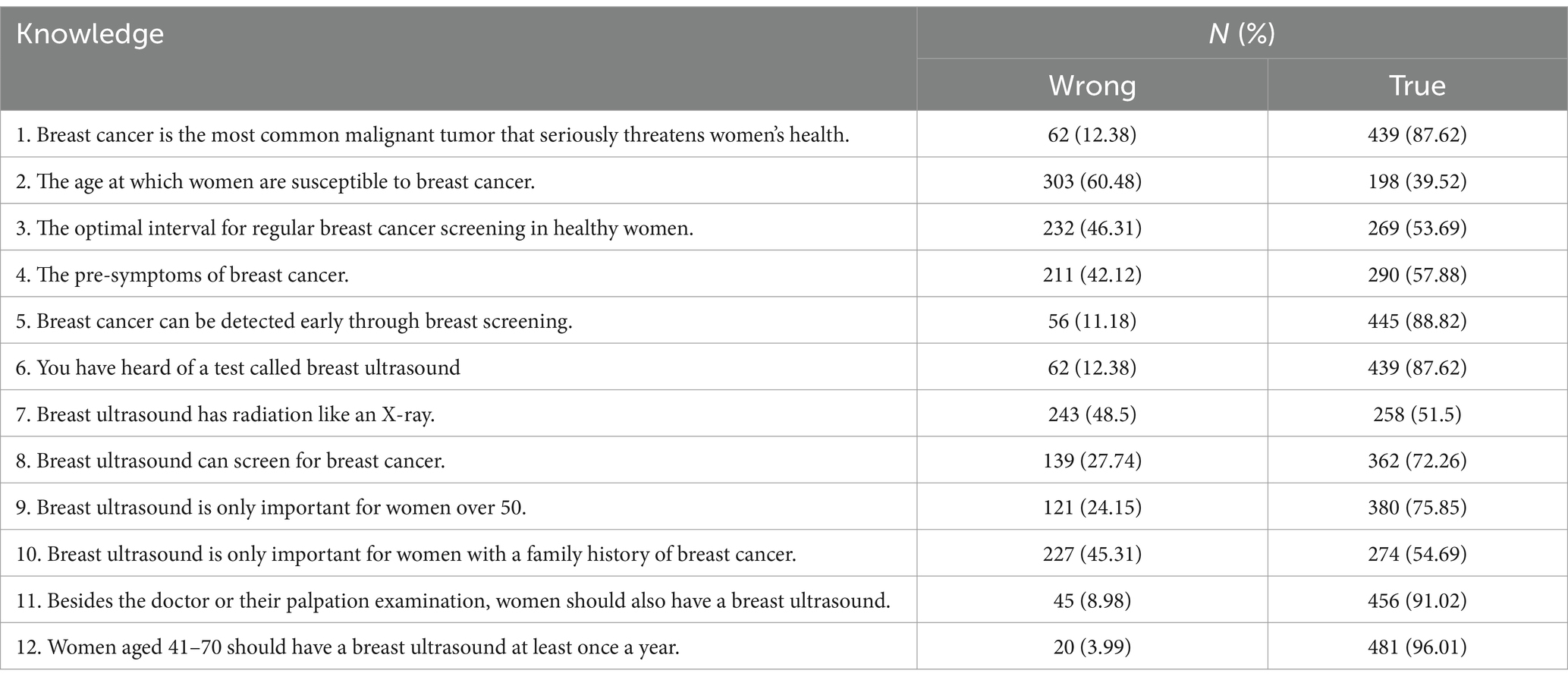
3.2 Knowledge
The knowledge score was 8.56 ± 1.81 (0–12, 71.33%). Better knowledge was observed in urban residents (p < 0.001), unmarried women (p = 0.028), with higher education (p < 0.001), women without children (p < 0.001), employed (p < 0.001), with higher income (p < 0.001), and already underwent breast ultrasound (p = 0.005) (Table 1). The items with scores <70% were K2 (39.52%; “The age at which women are susceptible to breast cancer”), K7 (51.50%; “Breast ultrasound has radiation like an X-ray”), K3 (53.69%; “The optimal interval for regular breast cancer screening in healthy women”), K10 (54.69%; “Breast ultrasound is only important for women with a family history of breast cancer”), and K4 (57.88%; “The pre-symptoms of breast cancer”) (Table 2).
3.3 Attitude
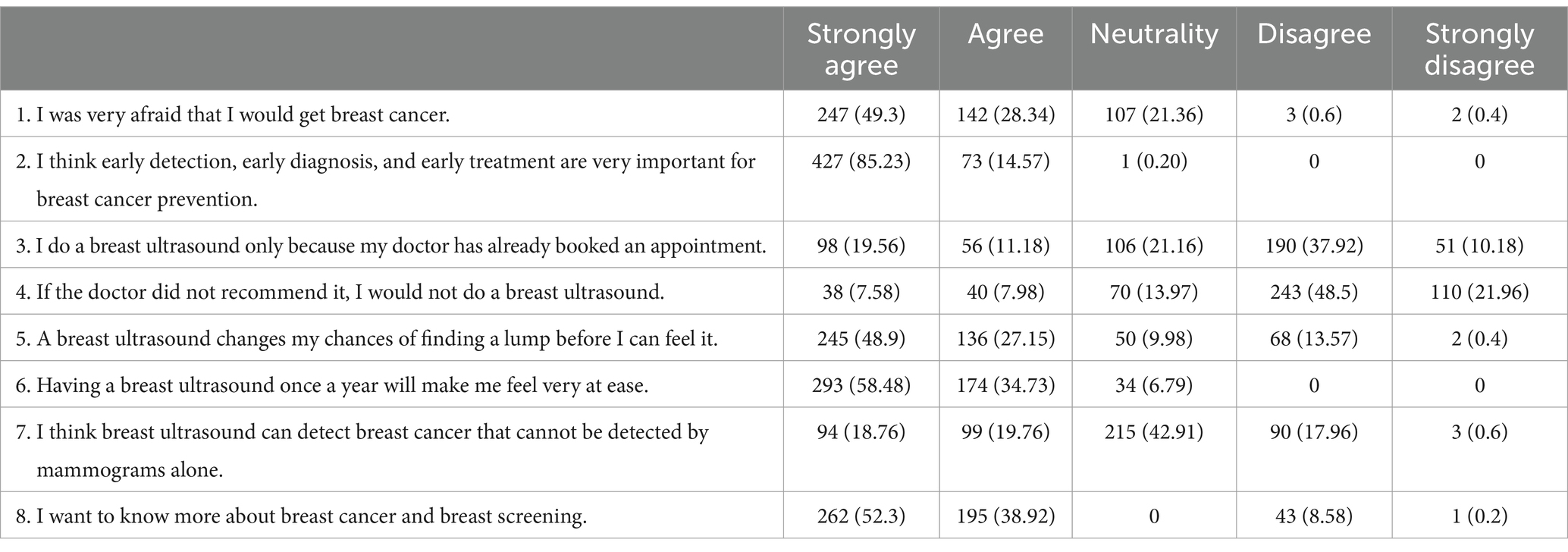
The attitude score was 29.80 ± 2.71 (5–40, 74.50%). A better attitude was observed in urban residents (p = 0.009), higher education (p = 0.003), without children (p = 0.023), higher income (p = 0.012), and already underwent breast ultrasound (p = 0.031) (Table 1). Table 3 shows the distribution of the responses to each attitude item.
3.4 Practice
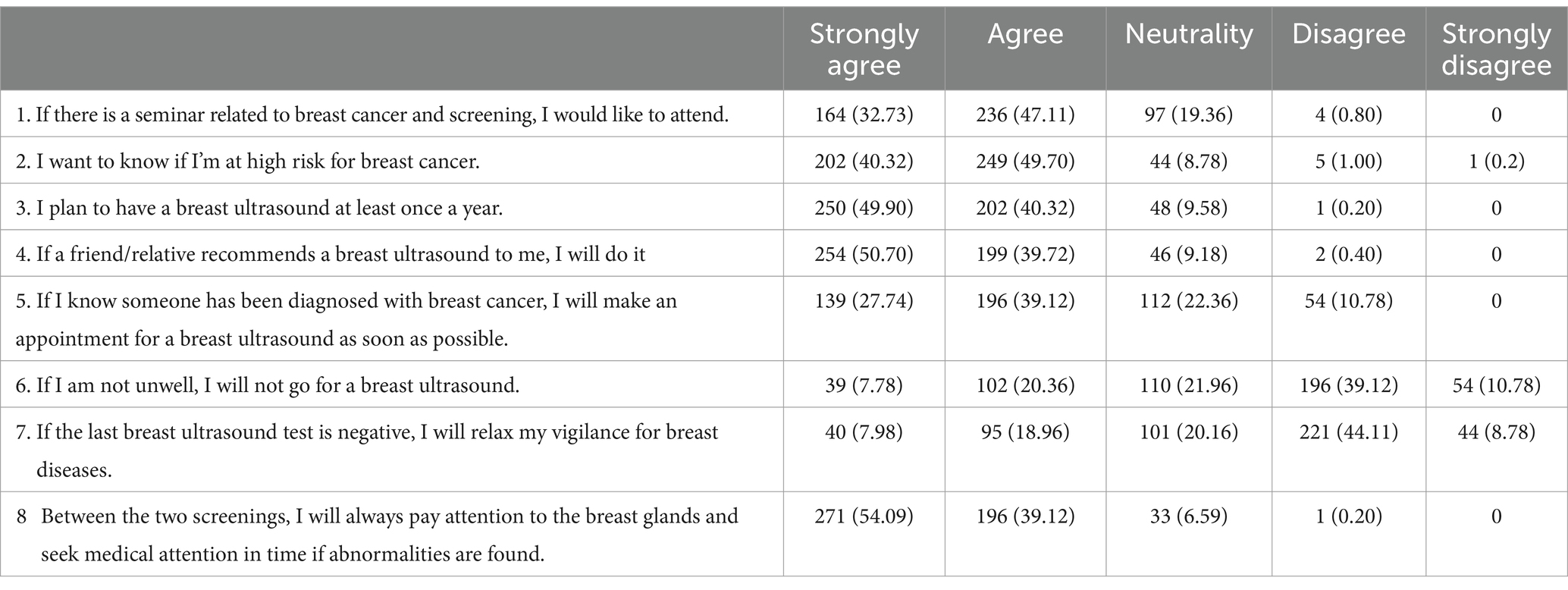
The practice score was 32.04 ± 3.09 (5–40, 80.10%) (Table 1). Table 4 shows the distribution of the responses to the practice items.
3.5 Correlations
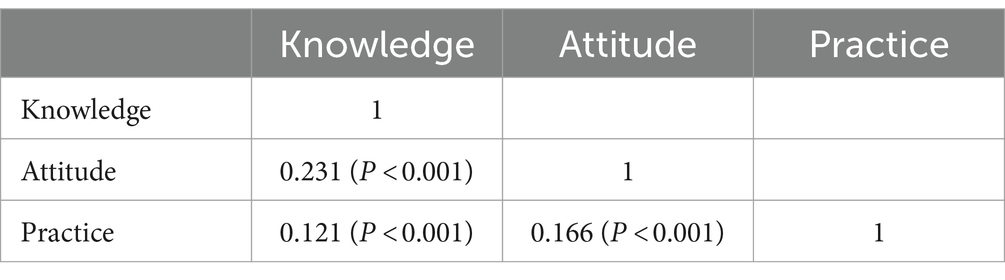
The knowledge scores were correlated to the attitude (r = 0.231, p < 0.001) and practice (r = 0.121, p < 0.001) scores. The attitude scores were correlated to the practice scores (r = 0.166, p < 0.001) (Table 5).
3.6 Multivariable analyses
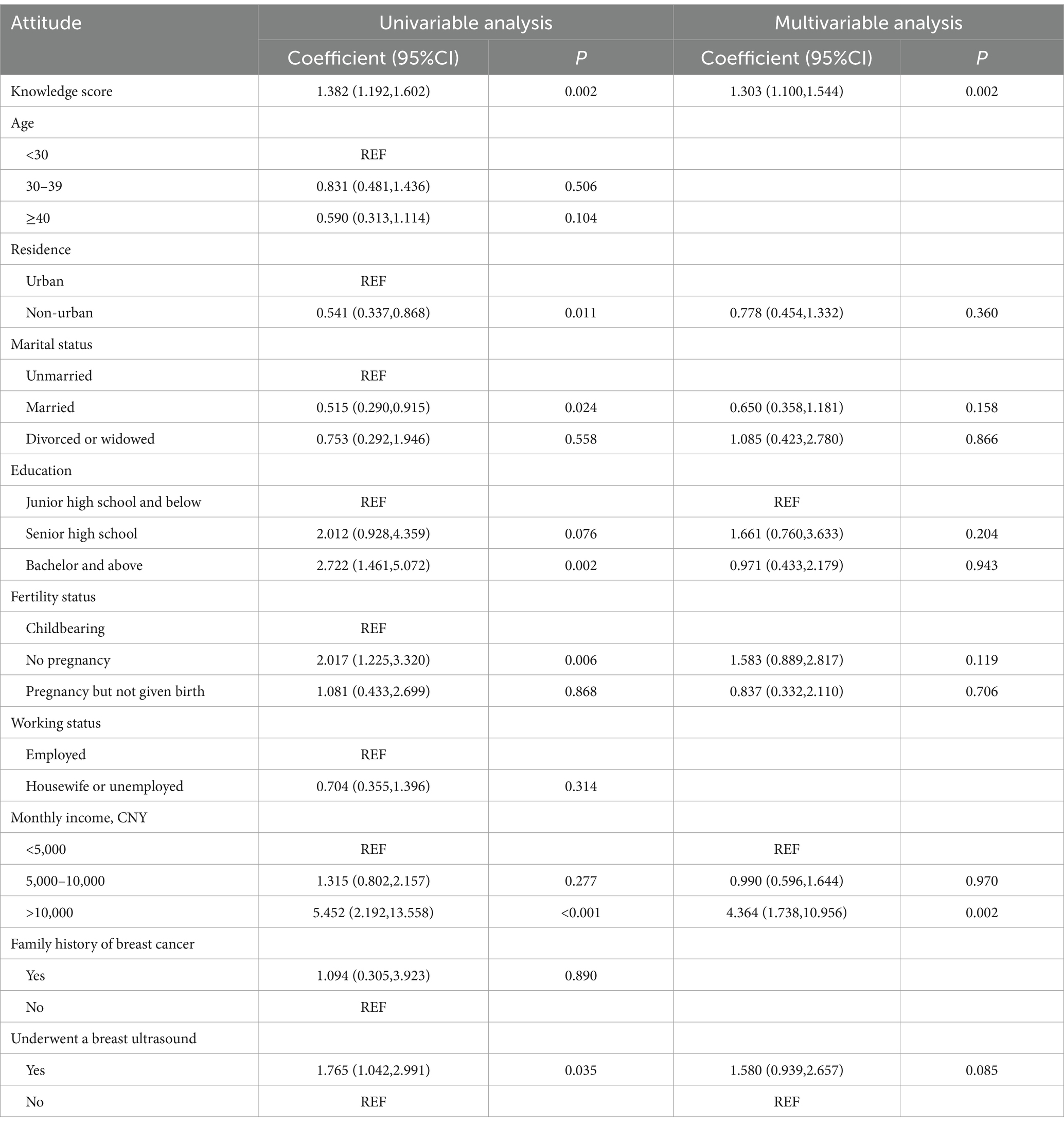
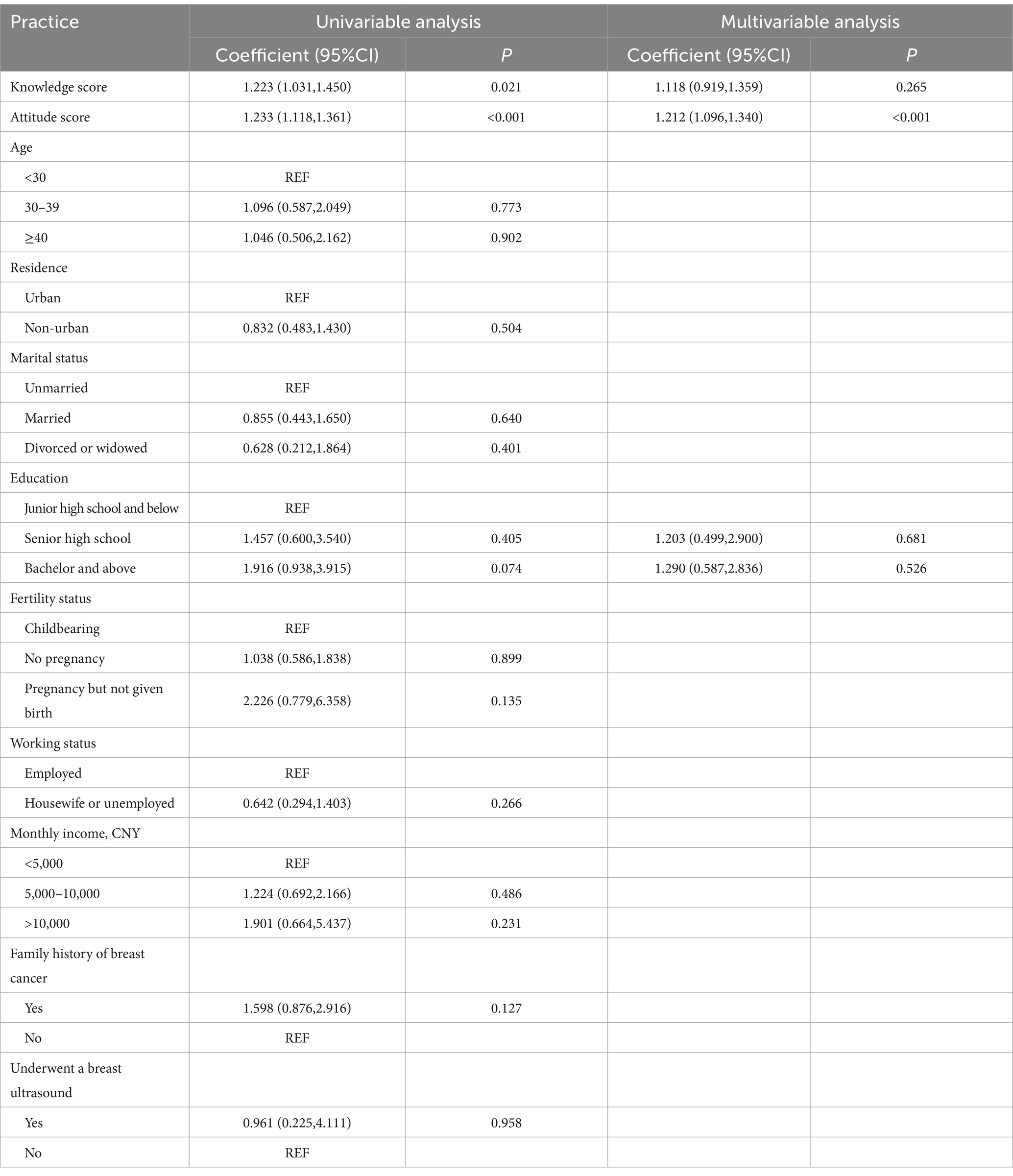
Multivariate linear regression analysis showed senior high school education (vs. junior high school and below, coefficient = 1.531, 95%CI: 1.013–2.312, p = 0.044), bachelor’s education and above (vs. junior high school and below, coefficient = 5.315, 95%CI: 3.546–7.966, p < 0.001), housewife or unemployed (vs. employed, coefficient = 0.671, 95%CI: 0.466–0.966, p = 0.032), and a history of breast ultrasound (vs. no, coefficient = 1.466, 95%CI: 1.121–1.917, p = 0.005) were independently and positively associated with knowledge (Table 6). Knowledge (coefficient = 1.303, 95%CI: 1.100–1.544, p = 0.002) and monthly income >10,000 (vs. <5,000, coefficient = 4.364, 95%CI: 1.738–10.956, p = 0.002) were independently and positively associated with attitude (Table 7). Only attitude (coefficient = 1.212, 95%CI: 1.096–1.340, p < 0.001) was independently and positively associated with practice (Table 8). Hence, those factors are independently associated with a better KAP toward breast ultrasound screening. Still, multivariable analyses of cross-sectional data cannot provide causality.
3.7 Structural equation modeling
The SEM analyses are surrogates for causality, providing an estimation of causality based on prespecified hypotheses and a graphical model of the possible relationships among variables (28–30). Table 9 shows that the goodness-of-fit of the SEM analysis was good/excellent. SEM analysis showed knowledge directly influenced attitude (β = −1.090, p = 0.015). Knowledge did not directly influence practice (β = −0.117, p = 0.681) but had an indirect influence (β = 0.826, p = 0.028). Attitude directly influenced practice (β = −0.757, p = 0.016) (Table 10 and Figure 1).
4 Discussion
The results suggest that women in Zhongshan had adequate knowledge, favorable attitudes, and active practice toward breast ultrasound, but gaps were still observed, and they should be the focus of future educational and motivational interventions. This study also identified broad categories of women in Zhongshan who might benefit more from such interventions. The SEM analysis showed knowledge influenced attitude but not practice, while attitude influenced practice. This study may provide a basis for whether to carry out educational intervention and improve women’s KAP for ultrasound breast cancer screening in Zhongshan. Of course, additional studies are necessary to determine whether the results are similar in other areas in China.
Breast cancer screening is voluntary and requires the willingness and participation of the women (5). Therefore, basic knowledge and good attitudes toward breast cancer and breast cancer screening are essential for participation in screening. Several countries have screening programs for breast cancer, with letters sent to women reaching a certain age inviting them to participate, followed by letters at regular intervals to remind them to participate (16, 19). The KAP toward breast cancer screening varies widely among countries with different characteristics, customs, and healthcare systems (22–25). A study in Saudi Arabia showed that most women had poor knowledge of breast cancer screening and screening methods, and social media was their main source of information (22). Saudi Arabia offers a free breast cancer screening program to all women above age 40 (31), and access to breast cancer screening should not be an impediment to knowledge acquisition. In Jordan, most women had adequate knowledge of breast cancer screening, but the participation rates in screening mammography were low (23). Jordan also has a breast cancer screening program. Heena et al. (24) showed that female healthcare professionals (including physicians, nurses, and other healthcare professionals) in Saudi Arabia, Pakistan, and the United Arab Emirates had lower-than-expected knowledge about breast cancer screening, considering their educational background and medical training. Qatari women also have poor knowledge and participation in breast cancer screening (25), despite the fact that Qatar has a program inviting women ages 45–69 to undergo breast cancer screening every 3 years (32). Healthcare professionals are first-line sources of reliable health-related knowledge for many individuals (33, 34), highlighting the need for proper training and knowledge.
The Chinese economy is developing at a rapid pace, and society is evolving at a similarly fast pace. Hence, improving breast cancer prevention and control is a crucial public health issue. The breasts of Chinese women are generally smaller and denser than those of Western women (18). In addition, the incidence of breast cancer onset peaks at 40–50 years in Chinese women, i.e., 5–10 years younger than in their Western counterparts (18). Therefore, developing screening guidelines based on the Chinese population is crucial. Some breast cancer screening programs are being developed in China (35). China is a vast country with a large population, and cancer screening programs were historically implemented in specific areas in the 1980s, mainly Shanghai and Beijing areas, with smaller cities and rural areas implementing their programs later (36). Nevertheless, the idea of breast cancer screening has been public knowledge for a long time despite the fact that access was not incorporated into the basic public health services until 2019 (36).
Since most Chinese women have dense breasts, ultrasound has a better detection value than mammography (37). Beyond basic breast cancer screening, the present study showed that the participants had a good KAP toward breast cancer and screening using ultrasound. Of note, the participants had a relatively high socioeconomic status (i.e., high education, employed, and urban residents), and it is well-known that health literacy is related to socioeconomic status (38). Previous studies performed in the United States of America (27, 39), Saudi Arabia (40), and Macao (41) showed relatively poor enthusiasm toward ultrasound screening. Except for the study by Gan et al. (41), the other studies were performed in populations with generally less dense breasts in which mammography is generally more suitable as the first-line screening modality (5).
Higher knowledge scores were associated with higher education, as supported by the association of a better socioeconomic status with higher health literacy (38). A higher socioeconomic status is also associated with easier access to healthcare information, either because of easier access to healthcare professionals or reliable sources of information or knowing where to search for reliable information (42). Furthermore, socioeconomic status influences health-seeking behaviors, with people with a lower socioeconomic status visiting the emergency departments and primary physicians and people with a higher status visiting more specialists, buying more prescription drugs, and undergoing more imaging examinations (43). The individuals also have the feeling that their socioeconomic status influences their healthcare (44). The same is seen for breast cancer screening, with a higher likelihood of participating in screening in women with a higher socioeconomic status than those with a lower status (45, 46). As shown by the SEM analysis and supported by the multivariable analyses, knowledge was also related to attitude, which influenced practice, as supported by the KAP theory, which states that knowledge is the basis for attitude and knowledge, while attitude is the force driving practice (20, 21). A history of breast ultrasound was also independently associated with better knowledge and attitude scores, probably because the women sought information or received more information regarding breast ultrasound.
In the present study, the knowledge items that should be improved included the women at risk of breast cancer, the no-radiation nature of ultrasound, the best breast cancer screening interval, the impact of a family history of cancer on a woman’s risk, and the warning symptoms of breast cancer. Some of these items are not specific to ultrasound screening, highlighting that general knowledge about breast cancer screening should be improved. Since knowledge was directly correlated to attitudes and practice, improving these relatively crucial points toward breast cancer in general and breast ultrasound should also translate into even better attitudes and practice. Educational material and interventions should be designed on breast cancer screening and breast ultrasound. Several interventions to improve the knowledge on breast cancer screening have been reported [22 interventions reviewed by Noman et al. (47)], but the interventions were highly heterogeneous, probably because of the heterogeneity in the study populations in terms of socioeconomic status, access to healthcare, healthcare systems, and public health education in general. A recent study highlighted the importance of community-based education programs to improve breast cancer screening and decrease anxiety related to screening (48). The bottom line should be that such education programs must be tailored to the specific population being targeted.
This study had limitations. The participants were from a single center, limiting the number of women recruited and limiting the representativeness of the general population. The results represent the KAP of women in Zhongshan, but whether similar results can be observed elsewhere in China remains to be determined. The participants were recruited by convenience sampling, which may have introduced bias into the study. The distribution of questionnaires within breast specialist facilities introduced a potential bias in the sample toward individuals who were already utilizing healthcare services. The potential for non-representativeness of the general population among participants who voluntarily present themselves at a hospital could restrict the external validity of the findings. Indeed, in the present study, most women enjoyed a higher socioeconomic status than the general population, limiting the generalizability of the conclusions. In addition, this study was cross-sectional, and no conclusion on causality could be made. The present study used a SEM analysis to obtain an estimate of causality, but it must be remembered that a SEM analysis statistically infers causality based on prespecified hypotheses, and the results (although useful for future studies) must be taken with caution (28–30). No previous KAP data were available from the same population, limiting the possible comparisons. Still, the present study could be a kind of baseline to evaluate the impact of future interventions. Nevertheless, studies should first identify the critical knowledge deficits or attitudes that would necessitate improvements. Finally, all KAP surveys are at risk of social desirability bias, in which the participants can answer what they should do instead of what they are doing (49, 50).
5 Conclusion
In conclusion, the results suggest that women in Zhongshan have good knowledge, favorable attitudes, and active practice toward breast ultrasound, but this study identified specific knowledge and attitude items that might require improvements. Education interventions should be carried out to improve the KAP of women toward ultrasound breast cancer screening.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of Zhongshan People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SL: Conceptualization, Investigation, Writing – original draft. SZ: Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing – review & editing. MQ: Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing – review & editing. YX: Data curation, Formal analysis, Writing – original draft. KY: Data curation, Formal analysis, Writing – original draft. XL: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1309797/full#supplementary-material
References
1. Harbeck, N, and Gnant, M. Breast cancer. Lancet. (2017) 389:1134–50. doi: 10.1016/S0140-6736(16)31891-8
2. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) . Breast Cancer. Version 4.2023. Fort Washington: National Comprehensive Cancer Network (2023).
3. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
4. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) . Breast Cancer risk reduction. Version 1.2023. Fort Washington: National Comprehensive Cancer Network (2022).
5. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) . Breast Cancer screening and diagnosis. Version 1.2022. Fort Washington: National Comprehensive Cancer Network (2022).
6. Siegel, RL, Miller, KD, Wagle, NS, and Jemal, A. Cancer statistics, 2023. CA Cancer J Clin. (2023) 73:17–48. doi: 10.3322/caac.21763
7. Myers, ER, Moorman, P, Gierisch, JM, Havrilesky, LJ, Grimm, LJ, Ghate, S, et al. Benefits and harms of breast Cancer screening: a systematic review. JAMA. (2015) 314:1615–34. doi: 10.1001/jama.2015.13183
8. Nelson, HD, Fu, R, Cantor, A, Pappas, M, Daeges, M, and Humphrey, L. Effectiveness of breast Cancer screening: systematic review and Meta-analysis to update the 2009 U.S. preventive services task force recommendation. Ann Intern Med. (2016) 164:244–55. doi: 10.7326/M15-0969
9. Gotzsche, PC, and Jorgensen, KJ. Screening for breast cancer with mammography. Cochrane Database Syst Rev. (2013) 2013:CD001877. doi: 10.1002/14651858.CD001877.pub5
10. Berg, WA, Blume, JD, Cormack, JB, Mendelson, EB, Lehrer, D, Bohm-Velez, M, et al. Combined screening with ultrasound and mammography vs. mammography alone in women at elevated risk of breast cancer. JAMA. (2008) 299:2151–63. doi: 10.1001/jama.299.18.2151
11. Berg, WA, Zhang, Z, Lehrer, D, Jong, RA, Pisano, ED, Barr, RG, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. (2012) 307:1394–404. doi: 10.1001/jama.2012.388
12. Bevers, TB . Ultrasound for the screening of breast cancer. Curr Oncol Rep. (2008) 10:527–8. doi: 10.1007/s11912-008-0079-7
13. Hooley, RJ, Greenberg, KL, Stackhouse, RM, Geisel, JL, Butler, RS, and Philpotts, LE. Screening US in patients with mammographically dense breasts: initial experience with Connecticut public act 09-41. Radiology. (2012) 265:59–69. doi: 10.1148/radiol.12120621
14. Scheel, JR, Lee, JM, Sprague, BL, Lee, CI, and Lehman, CD. Screening ultrasound as an adjunct to mammography in women with mammographically dense breasts. Am J Obstet Gynecol. (2015) 212:9–17. doi: 10.1016/j.ajog.2014.06.048
15. Weigert, J, and Steenbergen, S. The Connecticut experiments second year: ultrasound in the screening of women with dense breasts. Breast J. (2015) 21:175–80. doi: 10.1111/tbj.12386
16. Luo, C, Wang, L, Zhang, Y, Lu, M, Lu, B, Cai, J, et al. Advances in breast cancer screening modalities and status of global screening programs. Chronic Dis Transl Med. (2022) 8:112–23. doi: 10.1002/cdt3.21
17. Bae, JM, and Kim, EH. Breast density and risk of breast Cancer in Asian women: a meta-analysis of observational studies. J Prev Med Public Health. (2016) 49:367–75. doi: 10.3961/jpmph.16.054
18. Ding, R, Xiao, Y, Mo, M, Zheng, Y, Jiang, YZ, and Shao, ZM. Breast cancer screening and early diagnosis in Chinese women. Cancer Biol Med. (2022) 19:450–67. doi: 10.20892/j.issn.2095-3941.2021.0676
19. Ren, W, Chen, M, Qiao, Y, and Zhao, F. Global guidelines for breast cancer screening: a systematic review. Breast. (2022) 64:85–99. doi: 10.1016/j.breast.2022.04.003
20. Andrade, C, Menon, V, Ameen, S, and Kumar Praharaj, S. Designing and conducting knowledge, attitude, and practice surveys in psychiatry: practical guidance. Indian. J Psychol Med. (2020) 42:478–81. doi: 10.1177/0253717620946111
21. World Health Organization : Advocacy, communication and social mobilization for TB control: A guide to developing knowledge, attitude and practice surveys. Available at: http://whqlibdoc.who.int/publications/2008/9789241596176_eng.pdf (Accessed November 22, 2022). (2008)
22. Alshahrani, M, Alhammam, SYM, Al Munyif, HAS, Alwadei, AMA, Alwadei, AMA, Alzamanan, SSM, et al. Knowledge, attitudes, and practices of breast Cancer screening methods among female patients in primary healthcare centers in Najran, Saudi Arabia. J Cancer Educ. (2019) 34:1167–72. doi: 10.1007/s13187-018-1423-8
23. Al-Mousa, DS, Alakhras, M, Hossain, SZ, Al-Sa’di, AG, Al Hasan, M, Al-Hayek, Y, et al. Knowledge, attitude and practice around breast Cancer and mammography screening among Jordanian women. Breast Cancer. (2020) 12:231–42. doi: 10.2147/BCTT.S275445
24. Heena, H, Durrani, S, Riaz, M, AlFayyad, I, Tabasim, R, Parvez, G, et al. Knowledge, attitudes, and practices related to breast cancer screening among female health care professionals: a cross sectional study. BMC Womens Health. (2019) 19:122. doi: 10.1186/s12905-019-0819-x
25. Hamed, E, Alemrayat, B, Syed, MA, Daher-Nashif, S, Rasheed, HMA, and Kane, T. Breast Cancer knowledge, attitudes and practices amongst women in Qatar. Int J Environ Res Public Health. (2022) 19:3995. doi: 10.3390/ijerph19073995
26. Chukmaitov, A, Wan, TT, Menachemi, N, and Cashin, C. Breast cancer knowledge and attitudes toward mammography as predictors of breast cancer preventive behavior in Kazakh, Korean, and Russian women in Kazakhstan. Int J Public Health. (2008) 53:123–30. doi: 10.1007/s00038-008-7001-9
27. Moothathu, NS, Philpotts, LE, Busch, SH, Gross, CP, Staib, LH, and Hooley, RJ. Knowledge of density and screening ultrasound. Breast J. (2017) 23:323–32. doi: 10.1111/tbj.12734
28. Beran, TN, and Violato, C. Structural equation modeling in medical research: a primer. BMC Res Notes. (2010) 3:267. doi: 10.1186/1756-0500-3-267
29. Fan, Y, Chen, J, and Shirkey, G. Applications of structural equation modeling (SEM) in ecological studies: an updated review. Ecol Process. (2016) 5:19. doi: 10.1186/s13717-016-0063-3
30. Kline, RB . Principles and practice of structural equation modeling. New York: Guilford Press (2015).
31. AlAbdulKader, A, Gari, D, Al Yousif, G, Alghamdi, A, AlKaltham, S, AlDamigh, F, et al. Perceived barriers and facilitators to breast Cancer screening among women in Saudi. Arabia Breast Cancer. (2023) 15:505–13. doi: 10.2147/BCTT.S406029
32. Bujassoum, SM, Alassam, R, and Bugrein, H. Qatar experience of standard risk breast cancer screening program (BCSP). J Clin Oncol. (2014) 32:18–8. doi: 10.1200/jco.2014.32.26_suppl.18
33. Korshakova, E, Marsh, JK, and Kleinberg, S. Health information sourcing and health knowledge quality: repeated cross-sectional survey. JMIR Form Res. (2022) 6:e39274. doi: 10.2196/39274
34. Swoboda, CM, Van Hulle, JM, McAlearney, AS, and Huerta, TR. Odds of talking to healthcare providers as the initial source of healthcare information: updated cross-sectional results from the health information National Trends Survey (HINTS). BMC Fam Pract. (2018) 19:146. doi: 10.1186/s12875-018-0805-7
35. Hao, X, Tong, Z, Chen, K, Wang, Y, Liu, P, Gu, L, et al. Breast cancer screening guideline for Chinese women. Cancer Biol Med. (2019) 16:822–4. doi: 10.20892/j.issn.2095-3941.2019.0321
36. Xia, C, Basu, P, Kramer, BS, Li, H, Qu, C, Yu, XQ, et al. Cancer screening in China: a steep road from evidence to implementation. Lancet Public Health. (2023) 8:e996–e1005. doi: 10.1016/S2468-2667(23)00186-X
37. Thigpen, D, Kappler, A, and Brem, R. The role of ultrasound in screening dense breasts-a review of the literature and practical solutions for implementation. Diagnostics. (2018) 8:20. doi: 10.3390/diagnostics8010020
38. Svendsen, MT, Bak, CK, Sorensen, K, Pelikan, J, Riddersholm, SJ, Skals, RK, et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults. BMC Public Health. (2020) 20:565. doi: 10.1186/s12889-020-08498-8
39. Banegas, MP, Bird, Y, Moraros, J, King, S, Prapsiri, S, and Thompson, B. Breast cancer knowledge, attitudes, and early detection practices in United States-Mexico border Latinas. J Womens Health. (2012) 21:101–7. doi: 10.1089/jwh.2010.2638
40. Ahmed, RM . Knowledge and practices towards breast Cancer screening tools. Intl J Med Res Health. (2021) 10:157–65.
41. Gan, YX, Lao, CK, and Chan, A. Breast cancer screening behavior, attitude, barriers among middle-aged Chinese women in Macao. China J Public Health. (2018) 40:e560–70. doi: 10.1093/pubmed/fdy077
42. McMaughan, DJ, Oloruntoba, O, and Smith, ML. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front Public Health. (2020) 8:231. doi: 10.3389/fpubh.2020.00231
43. Filc, D, Davidovich, N, Novack, L, and Balicer, RD. Is socioeconomic status associated with utilization of health care services in a single-payer universal health care system? Int J Equity Health. (2014) 13:115. doi: 10.1186/s12939-014-0115-1
44. Arpey, NC, Gaglioti, AH, and Rosenbaum, ME. How socioeconomic status affects patient perceptions of health care: a qualitative study. J Prim Care Community Health. (2017) 8:169–75. doi: 10.1177/2150131917697439
45. Akinyemiju, T, Ogunsina, K, Sakhuja, S, Ogbhodo, V, and Braithwaite, D. Life-course socioeconomic status and breast and cervical cancer screening: analysis of the WHO’s study on global ageing and adult health (SAGE). BMJ Open. (2016) 6:e012753. doi: 10.1136/bmjopen-2016-012753
46. Zhang, S, Wang, H, Liu, B, Yu, J, and Gao, Y. Socioeconomic status index is an independent determinant of breast cancer screening practices: evidence from eastern China. PLoS One. (2022) 17:e0279107. doi: 10.1371/journal.pone.0279107
47. Noman, S, Shahar, HK, Abdul Rahman, H, Ismail, S, Abdulwahid Al-Jaberi, M, and Azzani, M. The effectiveness of educational interventions on breast Cancer screening uptake, knowledge, and beliefs among women: a systematic review. Int J Environ Res Public Health. (2020) 18:263. doi: 10.3390/ijerph18010263
48. Zafar, N, Wolf, AB, Kepniss, JL, Teal, AC, and Brem, RF. Effectiveness of community education for breast Cancer screening. J Breast Imaging. (2024) 6:166–74. doi: 10.1093/jbi/wbae002
49. Bergen, N, and Labonte, R. “Everything is perfect, and we have no problems”: detecting and limiting social desirability Bias in qualitative research. Qual Health Res. (2020) 30:783–92. doi: 10.1177/1049732319889354
Keywords: knowledge, attitude, practice, breast cancer, screening, ultrasound, cross-sectional study
Citation: Liu S, Zheng S, Qin M, Xie Y, Yang K and Liu X (2024) Knowledge, attitude, and practice toward ultrasound screening for breast cancer among women. Front. Public Health. 12:1309797. doi: 10.3389/fpubh.2024.1309797
Edited by:
Nyi Nyi Naing, Sultan Zainal Abidin University, MalaysiaReviewed by:
Aliete Cunha-Oliveira, Coimbra Nursing School, PortugalRano Sinuraya, Padjadjaran University, Indonesia
Bilgin Kadri Aribas, Bülent Ecevit University, Türkiye
Copyright © 2024 Liu, Zheng, Qin, Xie, Yang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaozhen Liu, sumsmichael@139.com
 Shaozhong Liu1
Shaozhong Liu1 Xiaozhen Liu
Xiaozhen Liu