- 1Department of Sport, Physical Education and Health, Faculty of Social Sciences, Hong Kong Baptist University, Kowloon, Hong Kong SAR, China
- 2School of Business, Social and Decision Sciences,Constructor University, Bremen, Germany
- 3College of Physical Education, Shenzhen University, Shenzhen, China
Background: Aging individuals are vulnerable to various Noncommunicable Diseases (NCDs). Different behaviors are closely related to a decreased risk of suffering from NCDs: sufficient Physical Activity (PA) (e.g., at least 150 mins Moderate-to-vigorous Physical Activity (MVPA) per week) and a healthy daily diet (e.g., at least five portions of Fruit and Vegetable Intake (FVI), 5–6 taels (189.0–226.8 g) Meat, Fish, Egg and Alternatives (MFEA)). Traditional face-to-face interventions were effective in behavior change. However, it was revealed to be resource-intensive and limited transfer due to poor self-regulation skills outside of face-to-face sessions. Thus, eHealth could be a supplement for older adults outside traditional face-to-face settings. The blended approach combining these two interventions might optimize the intervention effects on lifestyle behavior initiation and maintenance, but little research can be found among Hong Kong older adults. Therefore, the study aims to test a blended intervention to promote PA, diet, and health outcomes among Hong Kong community-dwelling older adults.
Methods: This study will adopt a 10-week three-arm randomized controlled trial. The blended group will receive weekly (1) two 60-min face-to-face sessions with one for PA and one for diet, and (2) two web-based sessions with one for PA and one for diet. The face-to-face group will receive the same intervention content as the face-to-face sessions in the blended group. The control condition will receive a biweekly telephone call. The outcomes will include MVPA (minutes/week), FVI (portions/day), MFEA consumption (taels/day), social-cognitive factors (self-efficacy, planning, social support, action control), physical health outcomes (clinical indicators, senior physical fitness), mental health outcomes (depression, loneliness) and health-related quality of life. Data collection will be implemented at the pre-test, post-test, and 3-month follow-up test.
Discussion: This is the first study evaluating a blended intervention promoting multiple health behaviors among Hong Kong community-dwelling older adults. If the effect of the blended intervention is superior to the traditional face-to-face group and the control group, it will enrich lifestyle intervention approaches and can be applied to older adults, helping them obtain health benefits. Furthermore, a better understanding of mechanisms will also have implications for theory-building.
Clinical trial registration: https://www.isrctn.com/ISRCTN32329348, ISRCTN32329348.
1 Introduction
Noncommunicable diseases (NCDs), such as cardiovascular diseases, cancer, diabetes, and obesity, are responsible for the mortality of approximately 41 million individuals annually, accounting for a staggering 74% of all global deaths (1). NCDs are of high prevalence due to a confluence of factors, including the globalization of unhealthy lifestyles and the demographic shift toward an aging population (2). Physical inactivity and unhealthy dietary patterns contribute to the manifestation of metabolic risk factors, such as elevated blood pressure, hyperglycemia, dyslipidemia, and obesity (3, 4). However, over one-quarter of adults were physically inactive, while over 3 million NCD-related deaths per year could be averted by increasing physical activity (PA) (5). The evidence indicates that 28% of adults were physically inactive and did not meet the World Health Organization (WHO) recommendation level of PA (5). The survey conducted in America suggested that the prevalence of physical inactivity significantly increases with age, with 26.9% among those aged 65–74 years and 35.3% among those aged ≥75 years (6). In Hong Kong, 24.8% of adults do not meet the WHO PA recommendation (at least 150 minutes Moderate-to-vigorous Physical Activity (MVPA) per week), while the percentage among older people is higher than that of other age groups (7).
Less than 50% of older adults adhere to the recommended five portions per day of fruit and vegetables (8, 9). An estimated 3.9 million deaths worldwide were attributable to inadequate fruit and vegetable consumption in 2017 (10). For Fruit and Vegetable Intake (FVI), most Hong Kong older adults consume less than five servings per day, in particular, 94.8% in the 65–74 age group, 96.6% in the 75–84 age group, and 99.3% in the 85 or above age group (7). As individual household incomes rise, global meat consumption and average per capita meat consumption are also increasing, driven by globalization and evolving food preferences, which heightened meat consumption is closely linked to the development of various diseases (11), particularly NCDs (12). It is essential to avoid excessive consumption of certain foods, such as meat consumption. In Hong Kong, the per capita meat consumption was 375 g, which ranked first in the world (13), while older people are recommended to have 5–6 taels Meat, Fish, Egg and Alternatives (MFEA) (189.0–226.8 g) per day (7). Engaging in multiple risk behaviors can lead to adverse health effects. Healthy lifestyle interventions among older adults are essential and meaningful to prevent harmful effects on individual health, medical systems, and medical costs (14).
Face-to-face workshops enable providers to deliver individualized interventions, facilitate interactive communication, and protect privacy (15). Empirical evidence supports the efficacy of face-to-face interventions in promoting health behaviors, such as PA and dietary choices (16, 17). Notwithstanding the practical support of face-to-face health interventions, this approach exhibits several limitations. Previous research also indicated significant barriers to older adults’ attendance and adherence to health behavior change intervention, including lack of perceived social support, low motivation, and poor self-regulation skills (18). The adherence rate of stand-alone face-to-face intervention on health promotion among older adults decreased over time (19).
eHealth is an emerging channel for delivering healthcare services and information through the Internet and associated technologies and media (e.g., computers and smartphones). It can complement face-to-face interventions for older adults in their homes or beyond traditional care settings (20). eHealth efficiently provides personalized feedback and long-term monitoring related to healthy lifestyles, which can enhance the maintenance of a healthy lifestyle over an extended period (21).
This study used the Health Action Process Approach (HAPA) model as a theoretical backdrop for the eHealth intervention (22). The HAPA model posited two phases (motivational and volitional) in the process of behavior change (23). During this dynamic process, individuals move from forming a behavioral intention to executing and sustaining a specific health behavior. In the process of behavioral change, several psychosocial factors play a crucial role. The motivational stage focuses on developing a behavioral intention, with action self-efficacy, outcome expectancies, and risk perceptions identified as contributing factors (24, 25). After individuals have established a behavioral intention, volitional factors such as action planning, coping planning, maintenance and recovery self-efficacies, and external resources like social support become essential in overcoming the intention-behavior gap (26). These factors collectively facilitate the execution and maintenance of the desired behavior (27). The widespread approval of the HAPA model in promoting various health behaviors among adults underscores its applicability (28). The effect of the techniques can be explained by theory, mainly relating to Behavior Change Techniques (27, 29).
However, eHealth intervention may also have disadvantages compared to face-to-face interventions. It demands specific skills, including electronic device functionality and reading comprehension proficiency. Providing individualized attention from professional medical care may pose challenges for caregivers (30). Furthermore, adherence is a crucial challenge in any eHealth intervention program, as many participants drop out before completion (31, 32).
In recent years, the blended intervention combining face-to-face workshops and eHealth intervention anticipates that the strengths of one delivery mode would offset the weaknesses of the other (33–36). A recent meta-analysis reported that the blended intervention can significantly promote total PA levels and diet behavior among adults (37). However, whether a blended intervention is more effective than traditional face-to-face interventions is unclear. Also, only limited findings reported the effectiveness of blended interventions in promoting PA and diet among older adults.
The findings of this study aim to fill the research gap, and its research design will be outlined in the following sections. There are two research objectives in this study. The primary aim is to compare the intervention effects between blended, face-to-face, and control groups in primary outcomes, including PA, diet (FVI and MFEA), and adherence to the health recommendations of PA and diet (FVI and MFEA). The second objective is to compare the intervention effects between blended, face-to-face, and control groups in secondary outcomes, including social-cognitive variables of behavior change (i.e., self-efficacy, planning, social support, and action control), physical health outcomes (i.e., clinical indicators, senior physical fitness), mental health outcomes (i.e., depression, loneliness), and health-related quality of life (HRQoL).
2 Methods and design
2.1 Study design and procedure
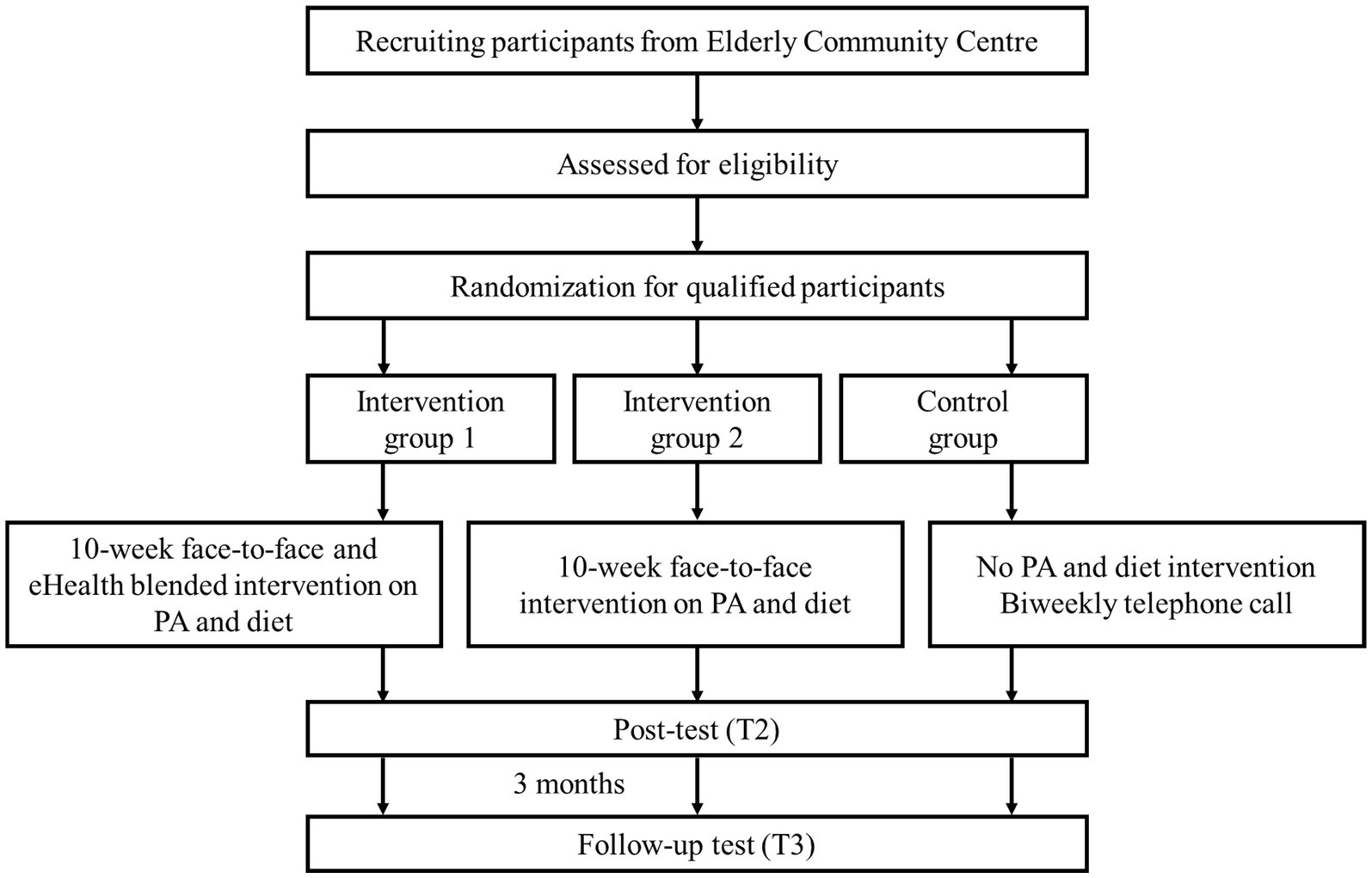
This study is a single-blind randomized controlled trial (RCT) comprising three groups: a blended face-to-face and eHealth intervention group (IG-1), a stand-alone face-to-face intervention group (IG-2), and a control group (CG). Evaluation will be conducted at pre-intervention (T1), post-intervention (T2), and 3 months follow-up after intervention completion (T3). The target population will be Hong Kong community-dwelling older adults. Participants will be recruited and randomly assigned into one of three groups. The intervention givers (i.e., PA coach and nutritionist) will be blinded from the assignment results to the intervention. The study process is presented in Figure 1.
2.2 Target population
Participants will be recruited from two Senior Centers in Hong Kong. The e-poster and video will be advertised by the staff in the Senior Centers. There are over 3,000 members in these two centers. Therefore, recruiting participants by advocating for the Senior Centers is feasible and advantageous. Potential study participants will be informed that there will be a health promotion program in which they can obtain health-related programs and receive a $300HKD (about $39USD) supermarket gift card as an incentive if the participants complete the 10-week health project and finish three times data collection.
Once the older adults express their interests, they will be encouraged to register in the program. After finishing all the registration and eligible screening, they will receive the study consent forms. The eligible criteria include: (1) aged 65 years and above; (2) owning a smartphone and having access to the Internet; (3) passing the Physical Activity Readiness Questionnaire (PAR-Q); (4) having sufficient reading and listening skills in Cantonese; (5) at least one health behavior (PA, FVI, MFEA) fails to meet the recommended health guideline. Exclusion criteria will include: (1) under special situations that seriously affected their diet (e.g., oral allergy syndrome) and mobility (e.g., physical disability); (2) meet all the health guidelines of PA, FVI, and MFEA; (3) participate in other ongoing project related to PA and diet intervention. Then, all participants will be allocated to one of three groups with an equal ratio (in a 1:1:1 ratio). The group allocation will be blinded. The researchers will provide the individual web link for the blended intervention group participants.
The sample size was calculated using G*Power 3.1 software. For achieving a medium effect size (Cohen’s f 0.26) on PA and diet based on a previous similar blended study among adults (35), with a statistical power (1-β) of 0.8 and an alpha of 0.05 (38), a total of 91 participants is required for the three groups (IG-1, IG-2, and CG). Considering the dropout rate of approximately 20% (35), a total of N = 114 participants is required to enable a robust evaluation.
2.3 Intervention content
2.3.1 Face-to-face intervention group
Previous findings indicated that the majority of the face-to-face sessions conducted exercise training and education among older adults without theory backdrop (39). The participants in the face-to-face intervention group will engage in two 60-min sessions per week, including one session for PA at the gym and one for diet at the neighborhood senior center (40) for 10 weeks. Each PA session will consist of two parts: health education on PA and health (10 minutes) and physical exercise (50 minutes). Each session will include a warm-up exercise (5 minutes), a main exercise (40 minutes), and a cool-down exercise (5 minutes). The main activity will consist of diverse components such as aerobic training, resistance training, balance training, and mindfulness meditation training. The feedback will be given during PA courses if the participants have questions. Each PA session will be delivered by a PA coach with the assistance of two to four research helpers to ensure safety and feasibility.
Each diet session will consist of two parts: health education on diet (30 minutes) and nutrition counseling (30 minutes). The education topics, such as dietary fiber, cholesterol, fruits and vegetables, and red and white meat, were developed based on suggestions from a nutritionist. The nutrition counseling will include a 15 minutes group discussion with 3–4 participants in one group to design daily dishes and 15 minutes of dish sharing. Personalized nutritional advice will be offered by the nutritionist accordingly. Each diet session will be delivered by a nutritionist with the assistance of one research helper.
2.3.2 Face-to-face and eHealth blended intervention group
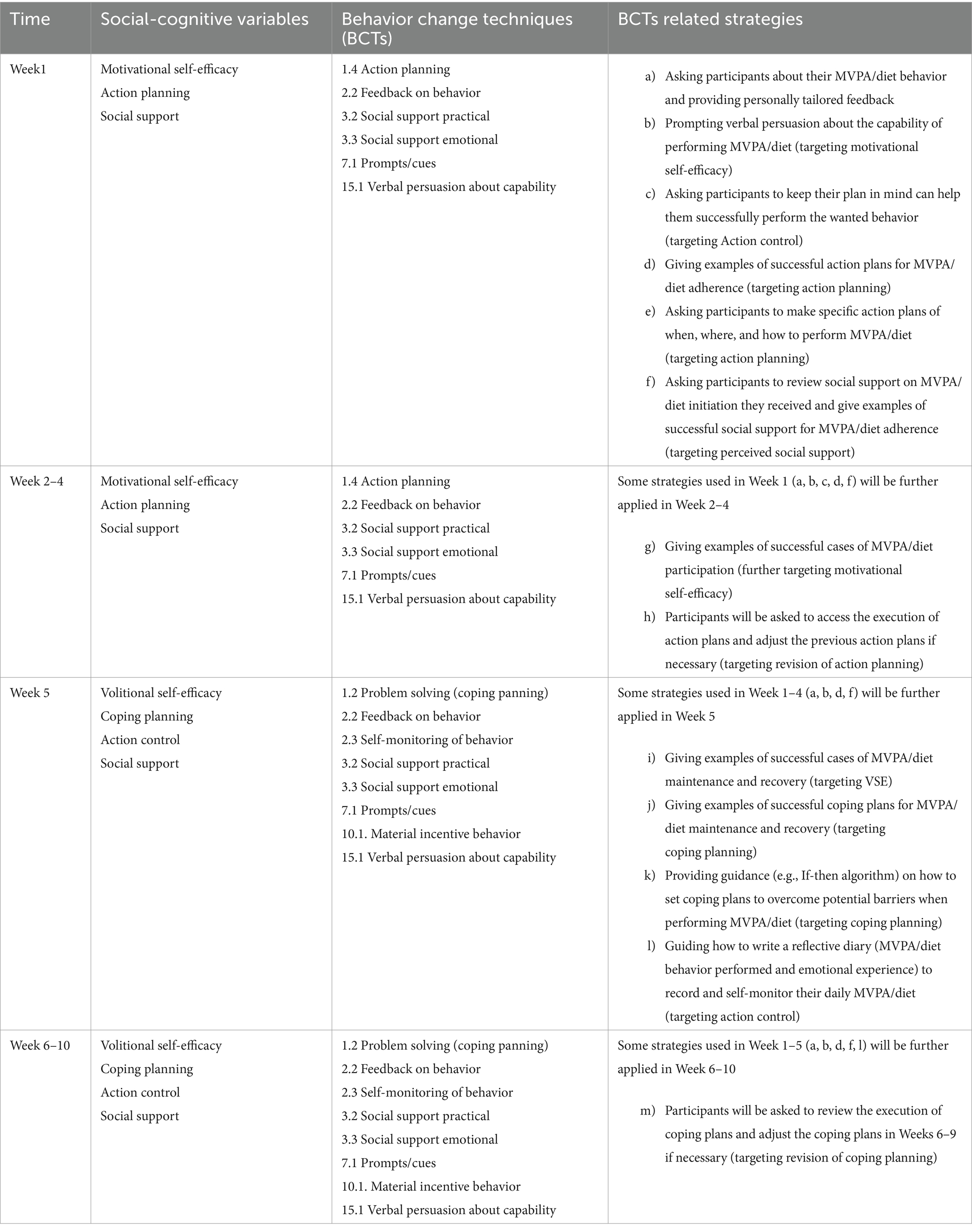
In addition to attending all face-to-face sessions, participants in the blended intervention group will participate in a theory-based and web-based behavioral change promotion eHealth intervention, including one program for PA and one program for diet each week. A mobile-based website, namely Perfect Diet and Exercise (in Cantonese: “食” 全十美, 行大 “運”), will be established to facilitate the intervention. The website’s homepage will have the PA module and the diet (FVI and MFEA) module. Participants can access each module to take part in respective online learning activities. Each module will consist of two sections. Section 1 comprises a theory-based 10-week intervention program targeting social-cognitive predictors of PA/diet (FVI and MFEA). Participants will access this section once a week. Section 2 is a data repository platform collecting former exercises and incentive activities. Participants can access their files at any time throughout the 10-week intervention period, including behavior records of PA/diet, action planning of PA/diet, coping planning of PA/diet, and “my diary” about PA/diet behaviors. The weekly eHealth intervention component will be developed based on the Health Action Process Approach (HAPA) (41). Following the HAPA-based social-cognitive variables, the weekly intervention content will be designed accordingly (see Table 1).
In addition, the intervention will apply different behavior change techniques (BCTs) to facilitate behavior (42). The detailed strategies of BCTs are presented in Table 1. For example, the participants will receive two types of feedback in the weekly web-based health session. This will include individualized feedback on their behavior performance in the 1st week, 2nd week, 3rd week, 4th week, and 5th week, respectively. Furthermore, the normative feedback on the criterion-based behavior recommendations (e.g., accumulated at least 150 minutes with moderate intensity of PA per week, five portions of FVI per day, 5–6 taels of MFEA per day) (see Figure 2) will be contained.
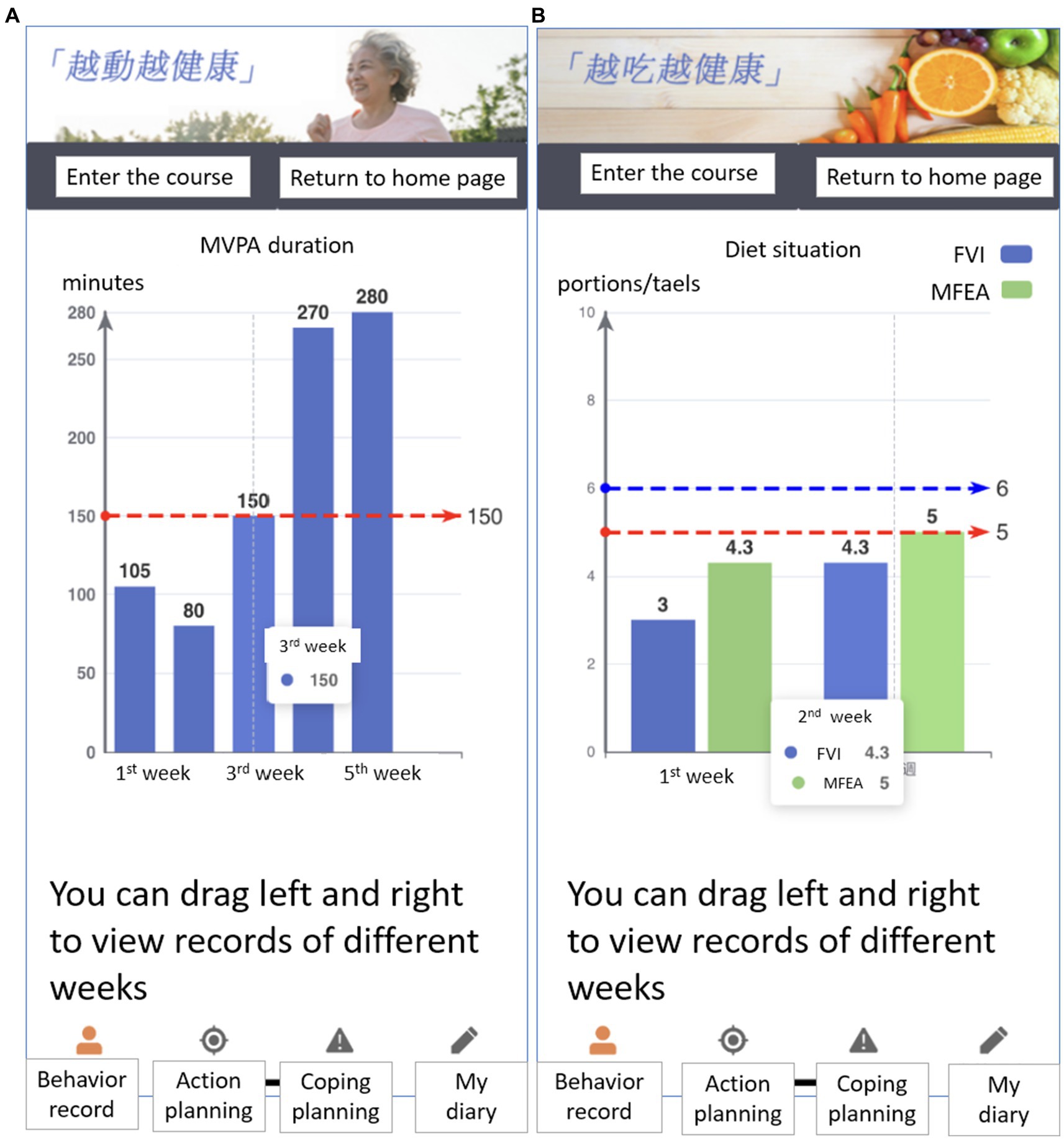
Figure 2. Individualized and normative feedback regarding PA per week during the past 5 weeks (A) as well as portions of fruit and vegetable, and taels of meat, fish, egg, and alternatives consumption in average per day during the past 2 weeks (B) for the blended intervention group.
Each weekly web-based section for PA and diet will last about 15 minutes. In the first week, once the participants complete the face-to-face intervention, the researcher will immediately organize a web-based intervention course for older adults at the PA gymnasium and the senior center for diet, respectively. The researcher will first introduce the website’s content and then demonstrate the steps to use this web-based program. Afterward, research helpers will guide participants in accessing the website and finishing the online study. In the 2nd week, the web-based intervention course will be continuously offered at the gym and the senior center to ensure older adults are familiar with the website’s usage. From the 3rd week, participants will be encouraged to finish the online courses at home to support transfer.
2.3.3 Control group
The participants in the control group will receive a biweekly telephone call. Each call will last about 5 minutes. The participants will be asked several health-related questions, such as “Has your physical activity changed in the last 2 weeks?” “If it changed, what are the reasons for the increase or decrease?” “Have you changed your diet in the last 2 weeks?” and “What has changed? What are the reasons for the increase or decrease if it changed?”
2.4 Outcome evaluation of the intervention
All the outcomes will be measured at T1 (baseline pre-test), T2 (post-test), and T3 (follow-up). Only demographics will be collected at T1. All measurement scales will be in Cantonese, which has been widely used in previous studies conducted in Hong Kong.
2.4.1 Primary outcomes: behavior indicators
2.4.1.1 Physical activity (PA)
The waist-worn accelerometer (wGT3XBT, ActiGraph Inc., Pensacola, FL, USA) will objectively assess moderate-to-vigorous intensity physical activity (MVPA) during the last 7 days. The participants will be guided to wear accelerometers attached to elastic belts around their waists during all waking hours for seven consecutive days. They must remove the waist-worn accelerometers only during sleeping or water-based activities (43). The Troiano wear time validation algorithm will be applied to activity counts (44). With this algorithm, periods of 60+ consecutive minutes of continuous zero counts with a tolerance of up to 2 minutes of activity counts between 0 to 100 counts/min will be classified as non-wear time (44). Data of at least 10 hours per day for at least 3 days will be considered valid and included in data analysis according to a previous systematic review (45). For the estimated PA intensity, the Sasaki et al. cut-point will be applied, 200–2,690 counts/min is for LPA, and ≥ 2,691 counts/min is for MVPA (46).
2.4.1.2 Fruit and vegetable intake (FVI) and meat, fish, egg & alternatives (MFEA)
To assess the FVI and MFEA during the past 7 days, participants will be asked to finish a diet record booklet and fill in how many portions of fruit, vegetable, and fruit and vegetable juice as well as how many taels of meat, fish, egg, and alternatives they have consumed within 1 day. The items will include “On the first day, I ate xxx portions of vegetables, I ate xxx portions of fruits, I drank xxx portions of vegetable and fruit juice. In total, xxx portions fruit and vegetables” and “On the first day, I ate xxx taels of meat (including fish), I ate xxx taels of eggs, I ate xxx taels of alternatives and a total of xxx taels meat, fish, egg, and alternatives.” The average number of FVI and MFEA they ate daily will be calculated based on the records they filled out during the past 7 days. These items are developed based on the diet recommendations provided by the Center for Health Protection Department of Health in Hong Kong (47). One tael is equal to 37.799 grams. Each participant will receive an assessment guide booklet on the portion of fruit and vegetables and the tael of MFEA.
2.4.2 Secondary outcomes: health outcomes
2.4.2.1 Physical health outcomes
The Senior Fitness Test (SFT) Manual will be applied to assess the physical fitness of participants (48). The testing materials have been widely used in many countries and translated into many languages, including Chinese (49). The physical fitness testing includes the measurements of the 30-Second Chair Stand Test (lower body strength), 30-Second Arm Curl Test (upper body strength), 2-Minute Step Test (aerobic endurance), Chair Sit-and-Reach Test (lower body flexibility), Back Scratch Test (upper body flexibility), 8-foot Up-and-Go Test (agility and dynamic balance), and body mass index (BMI). Detailed testing guidance will be provided during testing. For example, 30-Second Chair Stand Test will be used to test lower body strength. Required measuring tools include a straight back or folding chair without armrests (seat 17 inches/43 cm high) and a stopwatch. The participant will be asked to sit in the middle of the seat, with their feet shoulder-width apart, flat on the floor. The arms should be crossed at the wrists and held close to the chest. The participant will be required to keep their back straight and keep their arms against the chest. After listening to the “Go” instruction, the participant should rise to a full standing position, and then sit back down again. The participant should repeat this action for 30 s. If the participant has completed a full stand from the sitting position when the time has elapsed, the final stand is counted in the total. The reliability of SFT items ranged from 0.80 to 0.98 (49).
The blood pressure will be measured by an automated portable device (Omron HEM-7121 Standard, Japan) following the procedure guidelines (50). Participants will be asked to sit quietly for 5–10 minutes before their blood pressure is measured. The blood pressure will then be recorded on an electronic screen and written on paper for recording. The unit would be mmHg. Capillary blood samples will be collected by finger-prick (51). The glycosylated hemoglobin (HbA1c, mmol/mol) and lipid (Total Cholesterol, CHOL; triglycerides, TG; high-density lipoprotein, HDL; mg/dL) will be tested by Point of Care (POC) Cobas b 101 system (Roche Diagnostics, Mannheim, Germany). A 30 uL fingertip blood sample will be collected from participants and immediately tested using two test trips. The system can generate HbA1c and lipid assay results by using 2 uL for the HbA1c test and 19 uL for the lipid test by finger-prick blood samples within 15 minutes (52). Participants will be asked to stay in a fasted state for 12 hours before the blood test.
2.4.2.2 Mental health outcomes
The Geriatric Depression Scale 15-item (GDS-15) - Cantonese Version will be used to assess depression among participants. The validity and reliability of the GDS-15 were validated as satisfactory among Chinese older adults in previous studies and were regarded as a valuable method for measuring depression in older adults (Cronbach’s α = 0.81–0.83) (53, 54). Participants will be asked 15 items referring to the past week, such as “Are you satisfied with your life?” and “Have you dropped many of your activities and interests?.” Answers are indicated as yes “1” or no “0.” For items 1, 5, 7, 11, and 13, the answer is yes “0” or no “1.”
The Chinese translation of the 6-item De Jong Gierveld Loneliness Scale will be applied to assessing loneliness. This scale was reliable and valid for measuring loneliness among Hong Kong older adults (Cronbach α = 0.76) (55). The participants will be informed, “Please see if these statements describe your situations or feelings now. If you think that they are describing you, answer yes; if you disagree with the statements, answer more or less; if you do not think that they are describing you, answer no.” Participants will be asked six items including two domains (emotional loneliness and social loneliness), such as “I experience a general sense of emptiness” and “There are plenty of people I can rely on when I have problems.” For the first three items related to emotional loneliness, answers are indicated as yes “1,” more or less “1,” and no “0.” For the last three items related to social loneliness, answers are indicated as yes “0,” more or less “1,” and no “1.”
2.4.2.3 Social-cognitive factors
The validated questionnaires will be used to assess the four social-cognitive variables (56–58), including Questionnaires of Self-efficacy (five items for each behavior) (59), Questionnaires of Planning (six items for PA, four items for each diet behavior) (60, 61), Questionnaires of Social Support (3 items for each behavior) (62), and Questionnaires of Action Control (6 items for each behavior) (63).
2.4.2.4 Health-related quality of life (HRQoL)
A brief version of the World Health Organization’s Quality of Life questionnaire (WHOQOL-BREF HK) will be used to evaluate the HRQoL (62) in Hong Kong. Participants will be first asked about their general quality of life using the question “How would you rate your quality of life?” on a two-item five-point scale (1 = very poor; 5 = very good). The physical health subdomain with seven items will also be used (Cronbach’s α = 0.71), such as “Are you satisfied with your ability to do everyday things?” and “Do you have enough energy to cope with daily life?” (1 = very dissatisfied; 5 = very satisfied). However, for item 3 and item 4, the participants will be asked, “Do you need medical help to cope with everyday life?” and “Do you feel pain and discomfort holding you back?” (1 = an extreme amount; 5 = not at all).
2.4.2.5 Demographics
Items will include name, mobile number, gender, age, marital status, number of children, educational level, professional status, household income, and history of chronic diseases.
2.5 Pilot study
A pilot study of blended intervention was run before the main study. The aim was to ensure that the recruitment procedure, data collection instruments, and intervention content were feasible and acceptable. The preparation study was conducted for 4 weeks. Four older adults were recruited through Purposive Sampling with two females and two males (Mean age = 69.3 years, SD = 3.30) (64).
The participants were asked to finish all the measurements once and to attend a 4-week blended intervention program. The intervention content was the same as the first 4-week out of the proposed 10-week intervention content in the main study. After finishing the pilot study, the participants were invited to give suggestions and feedback. Depending on the input from the participants (e.g., making web pages more accessible to operate, shortening the health talk), the intervention content was further adapted. The participants in the pilot study will not be involved in the main study.
2.6 Retention strategies
Different strategies will be applied to improve the adherence rate of the three assessments and the participation rate of all intervention sessions throughout the program. Such methods will include (1) a WhatsApp message will be sent to older adults in all groups 1 day before the interventions start to remind participants to participate by then; (2) there will be a check-in before each face-to-face class to help participants and researchers keep track of the attendance rate of all study participants throughout the course; (3) the printed materials of the face-to-face health talk will be distributed to the older adults in each face-to-face session. Since older people tend to have declining memories, this will help them look it up at home after they finish the course; (4) starting from the fifth week, the participants who document a valid diary three times a week on the website for each behavior will receive a cash reward of $10HKD, which will be distributed once a week; (5) after the completion of each data collection (T1, T2, and T3), the individualized health report including physical and mental health outcomes will be provided to the older adults.
2.7 Data analysis
All data will be analyzed by using SPSS 29.0. The Expectation Maximization (EM) method will be applied for missing values. Intention-to-treat principles will be used for all analyses. Independent samples t-tests, F-tests, and Chi-square tests will be used to compare the baseline characteristics at T1. Statistical significance will be set at the 5% level (two-tailed).
A series of generalized linear mixed models (GLMM) will be applied to evaluate the intervention effects on behaviors (PA, FVI, and MFEA), social-cognitive variables of behaviors (i.e., self-efficacy, planning, social support, and action control), physical health outcomes (i.e., physical fitness test, clinical indicators), mental health outcomes (i.e., depression, loneliness), and health-related quality of life (HRQoL).
2.8 Time schedule of the study
The proposed study will be completed over 36 months, as shown in Figure 3.
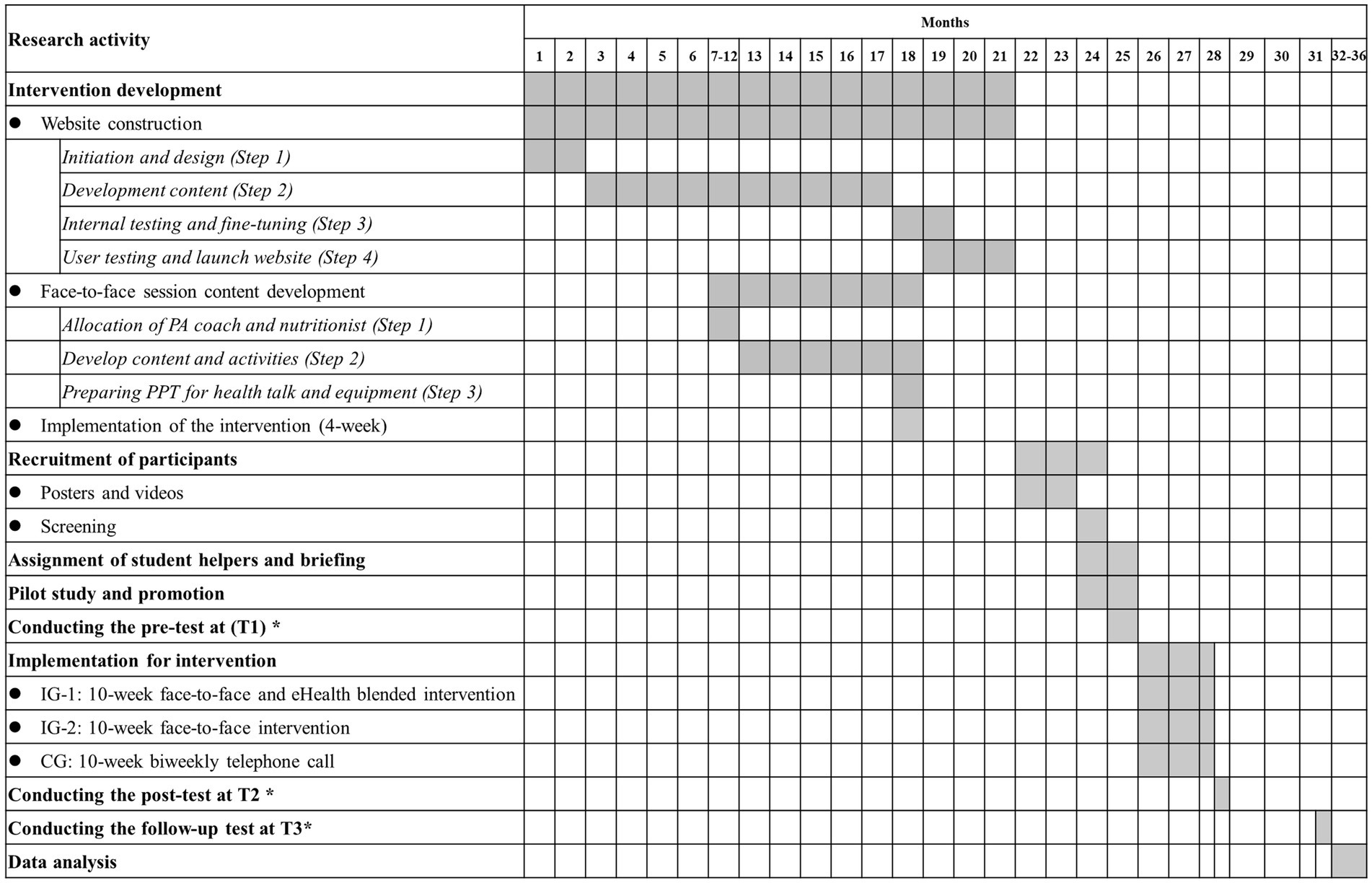
Figure 3. Gantt chart of research activities. *: The lengths of outcome tests at each time point, interventions, and follow-ups will be 1 month, 2.5 months (10 weeks), and 3 months, respectively.
3 Discussion
The high prevalence of inadequate PA and unhealthy dietary habits in the old population has garnered significant attention from health researchers and policymakers. Current research would investigate the effectiveness of a blended approach comprising face-to-face and eHealth interventions, specifically focusing on PA, dietary patterns, and health outcomes among older adults. It will be one of the first studies to apply blended intervention among older adults to promote healthy lifestyle behaviors theory- and evidence-based. Three unique aspects characterize the project.
The first unique aspect is the intervention channels, which include face-to-face workshops and eHealth sessions. The eHealth session will supplement traditional face-to-face treatment or seminars for older adults (65). Although the blended interventions are still under-explored, some potential benefits exist: The participants can review the intervention content anytime after the physical session. It is easier to get timely feedback from health care providers (e.g., doctors, health instructors, social workers), reducing the travel time, appointment process, and waiting time for feedback. It also helps increase the social interaction between healthcare providers (e.g., doctors, health instructors, social workers) and participants, reducing participants’ isolation after face-to-face contact. Besides, the healthcare providers can track the process and enhance adherence to the intervention (66).
The second unique aspect is that this is the first study applying eHealth technology to promote PA and diet behavior among Hong Kong community-dwelling older adults. Driven by the development of technology, more than 73.0% of Hong Kong’s older adults (≥ 65 years) have smartphones, and more than 70% use the Internet regularly in 2021 (67). Although many older adults have access to the Internet in Hong Kong, it is still difficult for them to use smartphones due to unfamiliarity with functions and unfriendly application design and operation (68). Hence, the stand-alone eHealth intervention might be complex for older people to adhere to. eHealth might be a complementary technology for the traditional face-to-face intervention project. It was found that 75% of people aged 65 years or above are suffering from one or more chronic diseases in Hong Kong. As these chronic diseases affect functionality and well-being, the old population accounts for more than 46% of patients’ hospital days (69). With the aging population and high prevalence of suffering from chronic diseases, this should be addressed immediately and appropriately to cope with the financial burden of treatment, rehabilitation, and residential care services. This study can develop and prove a blended intervention strategy for promoting lifestyle behaviors. It will be expected to be applied for disease management after the physical clinical.
The third unique aspect lies in exploring the psychosocial factors of behavior change and comprehensive health outcomes (BMI, physical fitness, clinical indicators, depression, loneliness, and health-related quality of life). The findings of this study can provide evidence about whether sufficient PA and a healthy diet are proven to be a protective factor for NCDs and associated with improvement in physical health, mental health, social well-being, cognitive function, and different aspects of body functions, which were proved by previous studies among other populations (70, 71). Besides, exploring the relationship between behavior change and psychosocial factors can enrich understanding mechanisms and have implications for theory-building.
Suggestions for further research encompass various aspects, including comparisons of a blended intervention with stand-alone eHealth interventions among older adults exploring aging effects and examining health lifestyle intervention effects in diverse geographical regions or countries. New research approaches are needed to enhance lifestyle behaviors, which can alleviate the growing demand for healthcare systems due to the aging population across the global landscape and within all medical and public health domains. Yet, identifying the critical predictive variables that underlie specific behavioral changes remains of utmost importance, a facet requiring comprehensive investigation in future research.
Ethics statement
The studies involving humans were approved by the Research Ethics Committee at Hong Kong Baptist University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MY: Conceptualization, Methodology, Project administration, Writing – original draft. YD: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. SL: Conceptualization, Supervision, Writing – review & editing, Methodology. WL: Investigation, Supervision, Writing – review & editing. NS: Investigation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization . Noncommunicable diseases. (2018). Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
2. Beaglehole, R, Bonita, R, Horton, R, Adams, C, Alleyne, G, Asaria, P, et al. Priority actions for the non-communicable disease crisis. Lancet. (2011) 377:1438–47. doi: 10.1016/S0140-6736(11)60393-0
3. Lee, IM, Shiroma, EJ, Lobelo, F, Puska, P, Blair, SN, Katzmarzyk, PT, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. (2012) 380:219–29. doi: 10.1016/S0140-6736(12)61031-9
4. Popkin, BM, and Ng, SW. The nutrition transition to a stage of high obesity and noncommunicable disease prevalence dominated by ultra-processed foods is not inevitable. Obes Rev. (2022) 23:e13366. doi: 10.1111/obr.13366
5. World Health Organization . Global status report on physical activity 2022. (2022). 1–112. Available at: https://www.who.int/teams/health-promotion/physical-activity/global-status-report-on-physical-activity-2022
6. Watson, KB, Carlson, SA, Gunn, JP, Galuska, DA, O’Connor, A, Greenlund, KJ, et al. Physical inactivity among adults aged 50 years and older — United States, 2014. Morb Mortal Wkly Rep. (2016) 65:954–8. doi: 10.15585/mmwr.mm6536a3
7. Centre for Health Protection . Diet and nutrition. (2022). Available at: https://www.chp.gov.hk/en/resources/465/8800.html
8. Pascual, RW, Phelan, S, La Frano, MR, Pilolla, KD, Griffiths, Z, and Foster, GD. Diet quality and micronutrient intake among long-term weight loss maintainers. Nutrients. (2019) 11:1–12. doi: 10.3390/nu11123046
9. Nicklett, EJ, and Kadell, AR. Fruit and vegetable intake among older adults: A scoping review. Maturitas. (2013) 75:305–12. doi: 10.1016/j.maturitas.2013.05.005
10. Afshin, A, Sur, PJ, Fay, KA, Cornaby, L, Ferrara, G, Salama, JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
11. Stanaway, JD, Afshin, A, Gakidou, E, Lim, SS, Abate, D, Abate, KH, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
12. Yip, CSC, Lam, W, and Fielding, R. A summary of meat intakes and health burdens. Eur J Clin Nutr. (2018) 72:18–29. doi: 10.1038/ejcn.2017.117
13. Food and Agriculture Organization of the United Nations . Daily meat consumption per person, 2021. (2020). Available at: https://ourworldindata.org/grapher/daily-meat-consumption-per-person
14. World Health Organization . Noncommunicable diseases. (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
15. Carey, KB, Scott-Sheldon, LAJ, Elliott, JC, Garey, L, and Carey, MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clin Psychol Rev. (2012) 32:690–703. doi: 10.1016/j.cpr.2012.08.001
16. Kader, M, Sundblom, E, and Elinder, LS. Effectiveness of universal parental support interventions addressing children’s dietary habits, physical activity and bodyweight: a systematic review. Prev Med. (2015) 77:52–67. doi: 10.1016/j.ypmed.2015.05.005
17. Haghighi, MM, Mavros, Y, and Singh, MAF. The effects of structured exercise or lifestyle behavior interventions on long-term physical activity level and health outcomes in individuals with type 2 diabetes: a systematic review, meta-analysis, and Meta-regression. J Phys Act Health. (2018) 15:697–707. doi: 10.1123/jpah.2017-0589
18. Moschny, A, Platen, P, Klaaßen-Mielke, R, Trampisch, U, and Hinrichs, T. Barriers to physical activity in older adults in Germany: a cross-sectional study. Int J Behav Nutr Phys Act. (2011) 8:121–10. doi: 10.1186/1479-5868-8-121
19. Denny, KG, Chan, ML, Gravano, J, Harvey, D, Meyer, OL, Huss, O, et al. A randomized control trial of a behavioral intervention for older adults with subjective cognitive complaints that combines cognitive rehabilitation strategies and lifestyle modifications. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. (2023) 30:78–93. doi: 10.1080/13825585.2021.1965530
20. Boogerd, EA, Arts, T, Engelen, LJ, and van de Belt, TH. “What is eHealth”: time for an update? JMIR Res Protoc. (2015) 4:e29. doi: 10.2196/resprot.4065
21. Asbjørnsen, RA, Smedsrød, ML, Nes, LS, Wentzel, J, Varsi, C, Hjelmesæth, J, et al. Persuasive system design principles and behavior change techniques to stimulate motivation and adherence in electronic health interventions to support weight loss maintenance: scoping review. J Med Internet Res. (2019) 21:e14265. doi: 10.2196/14265
22. Schwarzer, R . Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. (2008) 57:1–29. doi: 10.1111/j.1464-0597.2007.00325.x
23. Schwarzer, R, Lippke, S, and Luszczynska, A. Mechanisms of health behavior change in persons with chronic illness or disability: the health action process approach (HAPA). Rehabil Psychol. (2011) 56:161–70. doi: 10.1037/a0024509
24. Duan, Y, Li, X, Guo, L, Liang, W, Shang, B, and Lippke, S. A WeChat Mini program-based intervention for physical activity, fruit and vegetable consumption among Chinese cardiovascular patients in home-based rehabilitation: a study protocol. Front Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.739100
25. Liang, W, Duan, YP, Shang, BR, Wang, YP, Hu, C, and Lippke, S. A web-based lifestyle intervention program for Chinese college students: study protocol and baseline characteristics of a randomized placebo-controlled trial. BMC Public Health. (2019) 19:1097. doi: 10.1186/s12889-019-7438-1
26. Sutton, S . How does the health action process approach (HAPA) bridge the intention-behavior gap? An examination of the model’s causal structure. Appl Psychol. (2008) 57:66–74. doi: 10.1111/j.1464-0597.2007.00326.x
27. Lippke, S, and Ziegelmann, JP. Theory-based health behavior change: developing, testing, and applying theories for evidence-based interventions. Appl Psychol. (2008) 57:698–716. doi: 10.1111/j.1464-0597.2008.00339.x
28. Zhang, CQ, Zhang, R, Schwarzer, R, and Hagger, MS. A Meta-analysis of the health action process approach. Health Psychol. (2019) 38:623–37. doi: 10.1037/hea0000728
29. Webb, TL, Joseph, J, Yardley, L, and Michie, S. Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. (2010) 12:1–18. doi: 10.2196/jmir.1376
30. Aref-Adib, G, O’Hanlon, P, Fullarton, K, Morant, N, Sommerlad, A, Johnson, S, et al. A qualitative study of online mental health information seeking behaviour by those with psychosis. BMC Psychiatry. (2016) 16:1–10. doi: 10.1186/s12888-016-0952-0
31. Pedersen, DH, Mansourvar, M, Sortsø, C, and Schmidt, T. Predicting dropouts from an electronic health platform for lifestyle interventions: analysis of methods and predictors. J Med Internet Res. (2019) 21:1–12. doi: 10.2196/13617
32. Lippke, S, Dahmen, A, Gao, L, Guza, E, and Nigg, CR. To what extent is internet activity predictive of psychological well-being? Psychol Res Behav Manag. (2021) 14:207–19. doi: 10.2147/PRBM.S274502
33. van der Vaart, R, Witting, M, Riper, H, Kooistra, L, Bohlmeijer, ET, and van Gemert-Pijnen, LJ. Blending online therapy into regular face-to-face therapy for depression: content, ratio and preconditions according to patients and therapists using a Delphi study. BMC Psychiatry. (2014) 14:1–10. doi: 10.1186/s12888-014-0355-z
34. Wentzel, J, van der Vaart, R, Bohlmeijer, ET, and van Gemert-Pijnen, JEWC. Mixing online and face-to-face therapy: how to benefit from blended Care in Mental Health Care. JMIR Ment Health. (2016) 3:e4534:e9. doi: 10.2196/mental.4534
35. Hurkmans, E, Matthys, C, Bogaerts, A, Scheys, L, Devloo, K, and Seghers, J. Face-to-face versus mobile versus blended weight loss program: randomized clinical trial. JMIR Mhealth Uhealth. (2018) 6:e14. doi: 10.2196/mhealth.7713
36. Erbe, D, Psych, D, Eichert, HC, Riper, H, and Ebert, DD. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: systematic review. J Med Internet Res. (2017) 19:e306. doi: 10.2196/jmir.6588
37. Yang, M, Duan, Y, Liang, W, Peiris, DLIHK, and Baker, JS. Effects of face-to-face and eHealth blended interventions on physical activity, diet, and weight-related outcomes among adults: a systematic review and Meta-analysis. Int J Environ Res Public Health. (2023) 20:1560. doi: 10.3390/ijerph20021560
38. Weisburd, D, Wilson, DB, Wooditch, A, and Britt, C. Statistical power. Adv Stat Criminol Crim Justice. (2022) 6:321–65. doi: 10.1007/978-3-030-67738-1_8
39. Moore, M, Warburton, J, O’Halloran, PD, Shields, N, and Kingsley, M. Effective community-based physical activity interventions for older adults living in rural and regional areas: A systematic review. J Aging Phys Act. (2016) 24:158–67. doi: 10.1123/japa.2014-0218
40. Zubala, A, MacGillivray, S, Frost, H, Kroll, T, Skelton, DA, Gavine, A, et al. Promotion of physical activity interventions for community dwelling older adults: a systematic review of reviews. PLoS One. (2017) 12:e0180902. doi: 10.1371/journal.pone.0180902
41. Schwarzer, R . Health action process approach (HAPA) as a theoretical framework to understand behavior change. Act Psic. (2016) 30:119. doi: 10.15517/ap.v30i121.23458
42. Abraham, C, and Michie, S. A taxonomy of behavior change techniques used in interventions. Health Psychol. (2008) 27:379–87. doi: 10.1037/0278-6133.27.3.379
43. Troiano, RP, McClain, JJ, Brychta, RJ, and Chen, KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med. (2014) 48:1019–23. doi: 10.1136/bjsports-2014-093546
44. Troiano, RP, Berrigan, D, Dodd, KW, Mâsse, LC, Tilert, T, and Mcdowell, M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. (2008) 40:181–8. doi: 10.1249/mss.0b013e31815a51b3
45. Migueles, JH, Cadenas-Sanchez, C, Ekelund, U, Delisle Nyström, C, Mora-Gonzalez, J, Löf, M, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sport Med. (2017) 47:1821–45. doi: 10.1007/s40279-017-0716-0
46. Sasaki, JE, Júnior, JH, Meneguci, J, Tribess, S, Marocolo Júnior, M, Stabelini Neto, A, et al. Number of days required for reliably estimating physical activity and sedentary behaviour from accelerometer data in older adults. J Sports Sci. (2018) 36:1572–7. doi: 10.1080/02640414.2017.1403527
47. Disease Branch Centre for Health Protection Department of Health . Report of health behaviour survey 2018/19. (2020). Available at: http://www.chp.gov.hk
48. Rikli, RE, and Jones, CJ. Senior fitness test manual-second version. Champaign, IL: Human Kinetics (2013).
49. Rikli, RE, and Jones, CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical Independence in later years. Gerontologist. (2013) 53:255–67. doi: 10.1093/geront/gns071
50. Goessler, KF, Buys, R, VanderTrappen, D, Vanhumbeeck, L, and Cornelissen, VA. A randomized controlled trial comparing home-based isometric handgrip exercise versus endurance training for blood pressure management. J Am Soc Hypertens. (2018) 12:285–93. doi: 10.1016/j.jash.2018.01.007
51. Kruijshoop, M, Feskens, EJM, Blaak, EE, and De Bruin, TWA. Validation of capillary glucose measurements to detect glucose intolerance or type 2 diabetes mellitus in the general population. Clin Chim Acta. (2004) 341:33–40. doi: 10.1016/j.cccn.2003.10.033
52. Kenealy, T, Herd, G, Musaad, S, and Wells, S. HbA 1c screening in the community: lessons for safety and quality management of a point of care programme. Prim Care Diabetes. (2019) 13:170–5. doi: 10.1016/j.pcd.2018.11.008
53. Zhao, H, He, J, Yi, J, and Yao, S. Factor structure and measurement invariance across gender groups of the 15-item geriatric depression scale among Chinese elders. Front Psychol. (2019) 10:1360. doi: 10.3389/fpsyg.2019.01360
54. Cheng, ST, and Chan, ACM. A brief version of the geriatric depression scale for the Chinese. Psychol Assess. (2004) 16:182–6. doi: 10.1037/1040-3590.16.2.182
55. Leung, GTY, De Jong, GJ, and Lam, LCW. Validation of the Chinese translation of the 6-item De Jong Gierveld loneliness scale in elderly Chinese. Int Psychogeriatr. (2008) 20:1262–72. doi: 10.1017/S1041610208007552
56. Duan, Y, Shang, B, Liang, W, Yang, M, and Brehm, W. Psychosocial profiles of physical activity fluctuation in office employees: A latent profile analysis. PLoS One. (2020) 15:1–15. doi: 10.1371/journal.pone.0227182
57. Duan, YP, Julian, W, Hu, C, Gang, M, Si, Y, and Lippke, S. Web-based intervention for physical activity and fruit and vegetable intake among Chinese university students: a randomized controlled trial. J Med Internet Res. (2017) 19:e106. doi: 10.2196/jmir.7152
58. Duan, YP, Liang, W, Guo, L, Wienert, J, Si, GY, and Lippke, S. Evaluation of a web-based intervention for multiple health behavior changes in patients with coronary heart disease in home-based rehabilitation: pilot randomized controlled trial. J Med Internet Res. (2018) 20:e12052. doi: 10.2196/12052
59. Luszczynska, A, and Sutton, S. Physical activity after cardiac rehabilitation: evidence that different types of self-efficacy are important in maintainers and relapsers. Rehabil Psychol. (2006) 51:314–21. doi: 10.1037/0090-5550.51.4.314
60. Scholz, U, Schüz, B, Ziegelmann, JR, Lippke, S, and Schwarzer, R. Beyond behavioural intentions: planning mediates between intentions and physical activity. Br J Health Psychol. (2008) 13:479–94. doi: 10.1348/135910707X216062
61. Lippke, S, Schwarzer, R, Ziegelmann, JP, Scholz, U, and Schüz, B. Testing stage-specific effects of a stage-matched intervention: A randomized controlled trial targeting physical exercise and its predictors. Health Educ Behav. (2010) 37:533–46. doi: 10.1177/1090198109359386
62. Jackson, J, Lippke, S, and Gray, CD. Stage-specific prediction of physical activity in orthopedic patients after rehabilitation treatment. Int J Sport Psychol. (2011) 42:586–609.
63. Sniehotta, FF, Scholz, U, and Schwarzer, R. Bridging the intention-behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol Health. (2005) 20:143–60. doi: 10.1080/08870440512331317670
64. Etikan, I, and RSAD, SAM. Comparison of convenience sampling and purposive sampling. Am J Theor Appl Stat. (2016) 5:1. doi: 10.11648/j.ajtas.20160501.11
65. Fitzpatrick, M, Nedeljkovic, M, Abbott, JA, Kyrios, M, and Moulding, R. “Blended” therapy: the development and pilot evaluation of an internet-facilitated cognitive behavioral intervention to supplement face-to-face therapy for hoarding disorder. Internet Interv. (2017) 12:16–25. doi: 10.1016/j.invent.2018.02.006
66. Richards, P, and Simpson, S. Beyond the therapeutic hour: an exploratory pilot study of using technology to enhance alliance and engagement within face-to-face psychotherapy. Brit J Guid Couns. (2015) 43:57–93. doi: 10.1080/03069885.2014.936824
67. Hong Kong Census and Statistics Department . “Thematic household survey report no. 69”. (2020). Available at: https://www.censtatd.gov.hk/en/press_release_detail.html?id=4766
68. The Hong Kong Council of Social Service . The distance between digital technology and the elderly. (2021). Available at: https://www.hkcss.org.hk/數碼科技與長者的距離/?lang=en
69. Hong Kong Elderly Commission . Report on healthy ageing executive summary. (2021). Available at: https://www.elderlycommission.gov.hk/en/library/Ex-sum.htm
70. Langhammer, B, Bergland, A, and Rydwik, E. The importance of physical activity exercise among older people. Biomed Res Int. (2018) 2018:1–3. doi: 10.1155/2018/7856823
Keywords: physical activity, diet, health outcomes, older adults, blended intervention
Citation: Yang M, Duan Y, Lippke S, Liang W and Su N (2024) A blended face-to-face and eHealth lifestyle intervention on physical activity, diet, and health outcomes in Hong Kong community-dwelling older adults: a study protocol for a randomized controlled trial. Front. Public Health. 12:1360037. doi: 10.3389/fpubh.2024.1360037
Edited by:
Elena Carrillo-Alvarez, Blanquerna Ramon Llull University, SpainReviewed by:
Ik-Whan Kwon, Saint Louis University, United StatesJuan Corral-Pérez, University of Cádiz, Spain
Copyright © 2024 Yang, Duan, Lippke, Liang and Su. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanping Duan, duanyp@hkbu.edu.hk
 Min Yang
Min Yang Yanping Duan
Yanping Duan Sonia Lippke2
Sonia Lippke2 Wei Liang
Wei Liang Ning Su
Ning Su