- 1Global Antibiotic Stewardship, The Ohio State University Wexner Medical Center, Columbus, OH, United States
- 2Department of Pharmacy, The Ohio State University College of Pharmacy, Columbus, OH, United States
- 3Public Health Reserve Corp, Seattle, WA, United States
- 4Infectious Diseases Division, Loyola University Medical Center, Chicago, IL, United States
- 5Departments of Medicine and Research, Edward Hines Jr. VA Hospital, Hines, IL, United States
- 6Gilbert and Goff Prosthodontists, Upper Arlington, Columbus, OH, United States
Introduction
Antibiotics are commonly prescribed as prophylaxis for dental procedures and for treatment of dental infections. Although antibiotics have an important role in preventing and treating infections, antibiotics may have unintended consequences when they disrupt the oral and intestinal microbiome of the patient (1). The consequences of antibiotic use may include a lengthy disruption (lasting 2–6 months) of the protective microbiome, leading to increased risk of infection by opportunistic pathogens (such as Streptococcus mutans or Clostridioides difficile), development of antibiotic-associated diarrhea (AAD), development of antibiotic-resistant bacteria, and the development of adverse reactions ranging from mild rash to serious reactions requiring hospitalization (2–5). AAD occurs in 10%–40% of patients receiving antibiotics (15% in outpatients) and may last 1–22 days (2). AAD caused by C. difficile ranges from mild diarrhea to severe pseudomembranous colitis and may result in hospitalization and death (2). Probiotics may have three potential roles in dental practices: (1) the prevention of antibiotic-associated complications, (2) prevention of dental caries, or (3) treatment of periodontal disease. The interest in probiotics in dental practices has been growing, but there is no current consensus on how probiotics can best be utilized (6, 7). Our aims are to discuss the role of probiotics when used to limit complications of antibiotics and to prevent or treat dental infections.
Probiotics to prevent antibiotic-associated consequences
Probiotics are living microbes which have proven health benefits and typically are well-tolerated. Probiotics may have multiple mechanisms prevent antibiotic-associated diarrhea: restoration of the normally protective microbiome, interference with pathogen attachment to oral or intestinal cells, and regulating immune responses (8–11). Recent guidelines from the American Gastroenterology Association (AGA) recommend four types of probiotics for the prevention of C. difficile infections: Saccharomyces boulardii CNCM I-745 (Floratsor™), a three-strain mixture of Lactobacillus acidophilus CL1285, L. casei LBC80R, L. rhamnosus CLR2 (Bio-K+™), another three-strain mixture of L. acidophilus, L. bulgaricus and Bifidobacterium bifidum and a four-strain mixture of L. acidophilus, L. bulgaricus, Bifidobacterium bifidum and Streptococcus thermophilus (12). However, recommendations for the last two of the probiotic mixtures were based on only one trial and only meeting abstracts were published, thus the evidence is weak. Another review found strong evidence for two probiotics [L. rhamnosus GG (Culturelle™) and S. boulardii CNCM I-745 (Florastor™)] to prevent AAD (13). Typically the probiotic was started within 24 h of the antibiotic and continued while the patient was on antibiotics, then given for five-seven days afterwards to allow the normally protective microbiome to recover (14). It should be noted that not all “probiotic” strains or mixtures are equally effective to prevent these complications. The efficacy of probiotics has been determined to be both strain-specific and disease-specific, thus conclusions on which probiotic should be recommended to prevent different complications such as AAD or C. difficile infections, etc. need to be based on evidence done with specific strains (15). Often the type of probiotic that is available in stores or online are not the appropriate type of probiotic that is needed to prevent these complications. Based on the published evidence, several probiotics can be recommended for the prevention of AAD and CDI, as shown in the Table 1.
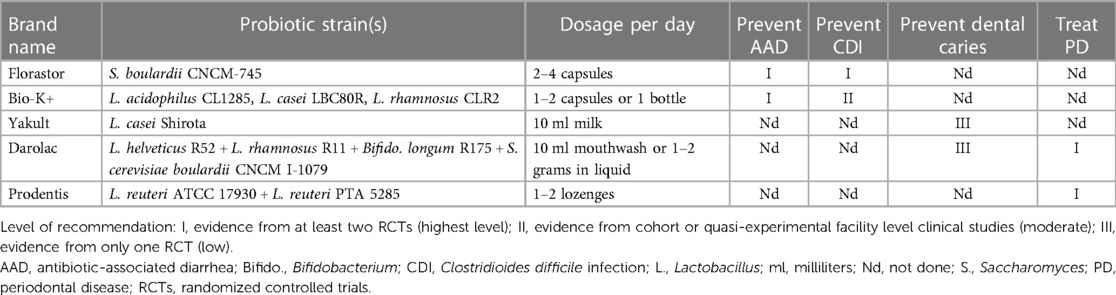
Table 1. Levels of recommendations for probiotic products for antibiotic-associated diarrhea, C. difficile infections and periodontal disease.
Probiotics to prevent dental caries
One mechanism to prevent the development of dental caries involves reducing the number of carigenic bacteria, such as Streptococccus mutans. A review of 17 different types of probiotics found 14/19 of the trials reduced the counts of Strept. mutans after probiotic use, but many types were supported by only one trial (16). Several types of probiotics may show promise in reducing caries by this mechanism: L. casei Shirota (17) or a 3-strain probiotic blend of L. rhamnosus R011 Bifidobacterium longum R175 and Saccharomyces cerevisiae boulardii CNCM I-1077 (Sporolac™) (18) or a four-strain blend (Durolac ™), which added L. helveticus R052 to the three strains in Sporolac (19).
Probiotics to treat dental infections
Another role for probiotics may be for the treatment of dental infections. Several reviews and meta-analyses assessed randomized, controlled trials of different probiotics for periodontal diseases and found promising results with Lactobacilli probiotics, but were unable to identify which specific Lactobacilli strains are the most effective (20–22). A meta-analysis of 36 randomized, controlled trials found 15 of 17 (88%) of trials with a two-strained probiotic (L. reuteri ATCC 17930 and L. reuteri PTA5289) significantly improved chronic periodontitis symptoms, but other types of probiotics (L. rhamnosus SP-1, L. rhamnosus DSM14869, L. brevis CD2, etc.) were not effective (23). The mechanisms of probiotics for the treatment of periodontal infections involve the interference with pathogen attachment of mucosal surfaces, production of antibacterial bacterocins and reducing pro-inflammatory cytokine production (20, 23–25). The ability of probiotic strains to reduce periodontal pathogens, such as Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans, Prevotella intermedia or Fusobacterium nucleatum has not be well studied (26). A two-strain mixture of L. reuteri 17930 and L. reuteri PTA5285 (24) and a four-strain mixture of L. helveticus R52 + L. rhamnosus R11 + Bifido. longum R175 + S. cerevisiae boulardii CNCM I-1079 (27, 28) have shown potential for treating periodontal disease, as shown in Table 1. The effect of probiotics for the treatment of dental infections may fade after probiotics are discontinued, thus further research into not only which probiotic strains are most effective, but the optimum duration and dose is needed.
Dentists may consider recommending probiotics to their patients who require antibiotics and may be at higher risk of developing antibiotic-associated complications, such as AAD or CDI. Risk factors for CDI include age >65, use of proton pump inhibitors, antibiotics, immune-compromised or hospitalization (2). A probiotic protocol similar to what was used in a prospective intervention study at one large skilled-nursing home may be considered (14). A 3-strained Lactobacilli blend was started (2 capsules of Bio-K+ once daily) within 24 h of the antibiotic start and continued while the patient was on the antibiotic. After the antibiotics were stopped, the probiotic was continued for an additional 7 days. A significant reduction of CDI rates were noted at this facility after the probiotic blend was implemented. Contraindications for probiotic use include severely immunocompromised states or patients at high risk for translocation, which can lead to sepsis. Dentists should be aware of which probiotic products have evidence-based clinical studies so they can educate their patients and help inform them of signs and symptoms of AAD and CDI.
In conclusion, not all probiotic products are equal. Evidence-based studies show usefulness of some probiotics, but not all for the prevention of AAD and CDI. Until further guidance is available, practitioners might consider adding one of the following probiotics during antibiotic administration and for 5–7 days after antibiotics are discontinued to allow the oral microbiome to recover: S. boulardii CNCM I-745 (Florastor™), L. rhamnosus GG (Culturelle™) or the 3-strain blend of L. acidophilus CL1285, L. casei LBC80R and L. rhamnosus CLR2 (Bio-K+ ™). The role of probiotic strains to reduce dental caries and treat periodontal disease requires more research. The role of probiotics in dentistry requires further studies.
Author contributions
DAG: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. LM: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing, Project administration, Software. SJ: Writing – review & editing. DWG: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Publication fees paid for by Bio-K+, a Kerry company.
Conflict of interest
DAG: Advisory Board Member for Bio-K+ International Inc., Ferring Pharmaceuticals, Danone North American; LM: Consultant and Advisory Board Member for Bio-K+ International Inc. and consultant and Microbiome Advisory Board Member for Biocodex consultant for Axon Pharma and Reddy’s Laboratories; SJ: Advisory Board Member for Bio-K+ International Inc., Acurx Pharmaceuticals, Ferring Pharmaceuticals, and Summit Therapeutics.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Anthony WE, Wang B, Sukhum KV, D'Souza AW, Hink T, Cass C, et al. Acute and persistent effects of commonly used antibiotics on the gut microbiome and resistome in healthy adults. Cell Rep. (2022) 39(2):110649. doi: 10.1016/j.celrep.2022.110649
2. McFarland LV, Ozen M, Dinleyici EC, Goh S. Comparison of pediatric and adult antibiotic-associated diarrhea and Clostridium difficile infections. World J Gastroenterol. (2016) 22(11):3078–104. doi: 10.3748/wjg.v22.i11.3078
3. Bye M, Whitten T, Holzbauer S. Antibiotic prescribing for dental procedures in community-associated Clostridium difficile cases, Minnesota, 2009–2015. Open Forum Infect Dis. (2017) 4(Suppl 1):S1. doi: 10.1093/ofid/ofx162
4. Gross AE, Suda KJ, Zhou J, Calip GS, Rowan SA, Hershow RC, et al. Serious antibiotic-related adverse effects following unnecessary dental prophylaxis in the United States. Infect Contr Hosp Epidemiol. (2021) 42(1):110–2. doi: 10.1017/ice.2020.1261
5. Goff DA, Mangino JE, Glassman AH, Goff D, Larsen P, Scheetz R. Review of guidelines for dental antibiotic prophylaxis for prevention of endocarditis and prosthetic joint infections and need for dental stewardship. Clin Infect Dis. (2020) 71(2):455–62. doi: 10.1093/cid/ciz1118
6. Alqahtani F, Alshaikh M, Mehmood A, Alqhtani N, Alkhtani F, Alenazi A. Efficacy of antibiotic versus probiotics as adjuncts to mechanical debridement for the treatment of peri-implant mucositis. J Oral Implantol. (2022) 48(2):99–104. doi: 10.1563/aaid-joi-D-20-00259
7. Babina K, Salikhova D, Doroshina V, Makeeva I, Zaytsev A, Uvarichev M, et al. Antigingivitis and antiplaque effects of oral probiotic containing the Streptococcus salivarius M18 strain: a randomized clinical trial. Nutrients. (2023) 15(18):3882. doi: 10.3390/nu15183882
8. Auclair J, Frappier M, Millette M. Lactobacillus acidophilus CL1285, Lactobacillus casei LBC80R, and Lactobacillus rhamnosus CLR2 (bio-K+): characterization, manufacture, mechanisms of action, and quality control of a specific probiotic combination for primary prevention of Clostridium difficile infection. Clin Infect Dis. (2015) 60(Suppl 2):S135–43. doi: 10.1093/cid/civ179
9. Kopacz K, Phadtare S. Probiotics for the prevention of antibiotic-associated diarrhea. Healthcare. (2022) 10(8):1450. doi: 10.3390/healthcare10081450
10. Mekonnen SA, Merenstein D, Fraser CM, Marco ML. Molecular mechanisms of probiotic prevention of antibiotic-associated diarrhea. Curr Opin Biotechnol. (2020) 61:226–34. doi: 10.1016/j.copbio.2020.01.005
11. Milner E, Stevens B, An M, Lam V, Ainsworth M, Dihle P, et al. Utilizing probiotics for the prevention and treatment of gastrointestinal diseases. Front Microbiol. (2021) 12:689958. doi: 10.3389/fmicb.2021.689958
12. Preidis GA, Weizman AV, Kashyap PC, Morgan RL. AGA Technical review on the role of probiotics in the management of gastrointestinal disorders. Gastroenterol. (2020) 159(2):708–38. doi: 10.1053/j.gastro.2020.05.060
13. Sniffen JC, McFarland LV, Evans CT, Goldstein EJ. Choosing an appropriate probiotic product for your patient: an evidence-based practical guide. PloS One. (2018) 13(12):e0209205. doi: 10.1371/journal.pone.0209205
14. Olson B, Ship N, Butera ML, Warm K, Oen R, Howard J. Clostridioides difficile infection in a skilled nursing facility (SNF): cost savings of an automated, standardized probiotic antimicrobial stewardship programme (ASP) policy. JAC Antimicrob Resist. (2023) 5(5):dlad102. doi: 10.1093/jacamr/dlad102
15. McFarland LV, Evans CT, Goldstein EJC. Strain-specificity and disease-specificity of probiotic efficacy: a systematic review and meta-analysis. Front Med. (2018) 5(124):1–14. doi: 10.3389/fmed.2018.00124
16. Laleman I, Detailleur V, Slot DE, Slomka V, Quirynen M, Teughels W. Probiotics reduce Streptococci mutans counts in humans: a systematic review and meta-analysis. Clin Oral Invest. (2014) 18(6):1539–52. doi: 10.1007/s00784-014-1228-z
17. Janiani P, Ravindran V. Comparative evaluation of the antimicrobial effects of probiotic milk and probiotic powder on the salivary Streptococcus mutans counts and the plaque scores in children aged 3–6 years: a randomized controlled trial. Dental Med Prob. (2022) 59(1):99–104. doi: 10.17219/dmp/139731
18. Jindal G, Pandey RK, Agarwal J, Singh M. A comparative evaluation of probiotics on salivary mutans streptococci counts in Indian children. Euro Arch Paed Dent. (2011) 12:211–5. doi: 10.1007/BF03262809
19. Jothika M, Vanajassun PP, Someshwar B. Effectiveness of probiotic, chlorhexidine and fluoride mouthwash against Streptococcus mutans–randomized, single-blind, in vivo study. J Internatl Soc Prev Commun Dent. (2015) 5(Suppl 1):S44–8. doi: 10.4103/2231-0762.156153
20. Gheisary Z, Mahmood R, Shivanantham AH, Liu J, Lieffers JRL, Papagerakis P, et al. The clinical, microbiological, and immunological effects of probiotic supplementation on prevention and treatment of periodontal diseases: a systematic review and meta-analysis. Nutrients. (2022) 14(5):1036. doi: 10.3390/nu14051036
21. Hardan L, Bourgi R, Cuevas-Suárez CE, Flores-Rodriguez M, Omana-Covarrubias A, Nicastro M, et al. The use of probiotics as adjuvant therapy of periodontal treatment: a systematic review and meta-analysis of clinical trials. Pharmaceut. (2022) 14(5):1017. doi: 10.3390/pharmaceutics14051017
22. Hu D, Zhong T, Dai Q. Clinical efficacy of probiotics as an adjunctive therapy to scaling and root planning in the management of periodontitis: a systematic review and meta-analysis of randomized control trials. J Evid Based Dent Pract. (2021) 21(2):101547. doi: 10.1016/j.jebdp.2021.101547
23. Schlagenhauf U, Jockel-Schneider Y. Probiotics in the management of gingivitis and periodontitis. A review. Front Dent Med. (2021) 2:708666. doi: 10.3389/fdmed.2021.708666
24. Ikram S, Hassan N, Raffat MA, Mirza S, Akram Z. Systematic review and meta-analysis of double-blind, placebo-controlled, randomized clinical trials using probiotics in chronic periodontitis. J Invest Clin Dent. (2018) 9(3):e12338. doi: 10.1111/jicd.12338
25. Ng E, Tay JR, Saffari SE, Lim LP, Chung KM, Ong MM. Adjunctive probiotics after periodontal debridement versus placebo: a systematic review and meta-analysis. Acta Odontol Scand. (2022) 80(2):81–90. doi: 10.1080/00016357.2021.1942193
26. Mayanagi G, Kimura M, Nakaya S, Hirata H, Sakamoto M, Benno Y, et al. Probiotic effects of orally administered Lactobacillus salivarius WB21-containing tablets on periodontopathic bacteria: a double-blinded, placebo-controlled, randomized clinical trial. J Clin Periodontol. (2009) 36(6):506–13. doi: 10.1111/j.1600-051X.2009.01392.x27
27. Thakkar PK, Imranulla M, Kumar PN, Prashant GM, Sakeenabi B, Sushanth VH. Effect of probiotic mouthrinse on dental plaque accumulation: a randomized controlled trial. Dent Med Res. (2013) 1(1):7–12. doi: 10.4103/2348-1471.124988
Keywords: antibiotics, dental infections, antibiotic-associated diarrhea, Clostridioides difficile, probiotics
Citation: Goff DA, McFarland LV, Johnson S and Goff DW (2023) The dual role for probiotics use in dental practices. Front. Oral. Health 4:1336565. doi: 10.3389/froh.2023.1336565
Received: 10 November 2023; Accepted: 5 December 2023;
Published: 21 December 2023.
Edited by:
Fabian Cieplik, University Medical Center Regensburg, GermanyReviewed by:
Jessica Scoffield, University of Alabama at Birmingham, United States© 2023 Goff, McFarland, Johnson and Goff. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lynne V. McFarland bWNmYXJsYW5kLmx5bm5lLnZAZ21haWwuY29t
 Debra A. Goff1,2
Debra A. Goff1,2 Lynne V. McFarland
Lynne V. McFarland Stuart Johnson
Stuart Johnson