- 1Department of Applied Dental Sciences, College of Applied Medical Sciences, Jordan University of Science and Technology, Irbid, Jordan
- 2Department of Prosthodontics, Faculty of Dentistry, Jordan University of Science and Technology, Irbid, Jordan
- 3Department of Cardiology, Odontology School, Sahlgrenska Academy, Gothenburg University, Gothenburg, Sweden
- 4Dental Research Unit, Center for Global Health Research, Saveetha Medical College and Hospital, Saveetha Institute of Medical and Technical Sciences, Chennai, India
- 5Department of Pediatric Dentistry, University of Illinois Chicago, Chicago, IL, United States
- 6Faculty of Dentistry, University of Puthisastra, Phnom Penh, Cambodia
- 7Department of Dental Research Cell, Dr. D. Y. Patil Dental College & Hospital, Dr. D. Y. Patil Vidyapeeth (Deemed to be University), Pune, India
Background: Individuals with hearing impairments face significant barriers in accessing oral health information, which may negatively influence their oral hygiene practices and outcomes. This study aimed to compare oral health knowledge and dental behavior between individuals with and without hearing impairments in Jordan.
Methods: A cross-sectional comparative study was conducted among 289 participants, comprising 149 individuals with hearing impairments and 140 individuals without hearing impairments. A validated, self-designed closed-ended questionnaire assessed participants’ oral health knowledge and behaviors. Convenience sampling was employed to recruit participants from centers associated with hearing impairment. Data were analyzed using SPSS® version 22, with a significance level set at P < 0.05. Chi-square tests and contingency table analyses assessed group differences.
Results: Individuals with hearing impairments demonstrated significantly less knowledge regarding toothbrush hardness, frequency of brushing, the importance of routine dental visits, and recognition of gum disease signs (P < 0.05). A smaller proportion of the hearing-impaired group brushed their teeth once or twice daily (82.8% vs. 93.3%, P < 0.001), used dental floss and mouthwash, consumed soda more frequently (P < 0.001), and reported using fluoridated toothpaste compared to individuals without hearing impairments (P < 0.05).
Conclusions: The substantial gaps in oral health knowledge and practices among individuals with hearing impairments highlight the need for targeted educational interventions. Culturally sensitive tools, such as visual aids, videos, and tailored oral health programs, could improve hygiene practices, reduce disease risk, and enhance the quality of life in this underserved population.
Introduction
Hearing impairment is the third most common disability worldwide (1). Its etiology may be hereditary, congenital, or acquired, and it can present as conductive, sensorineural, mixed, or central hearing loss. The severity of hearing impairment ranges from mild (less than 40 decibels) to profound (greater than 40 decibels), and it may occur prelingually, perilingually, or postlingually, depending on the timing relative to language acquisition (2). According to the World Health Organization (WHO), over 5% of the global population—432 million adults and 34 million children—live with hearing loss that requires intervention. By 2050, this number is projected to rise to over 700 million, affecting approximately 1 in 10 people (3).
Studies have consistently demonstrated that individuals with hearing impairments exhibit poorer oral hygiene compared to the general population, primarily due to limited access to oral health information and communication barriers (4, 5). Bhadauria et al.'s study (6), conducted in India, surveyed 500 individuals with hearing difficulties and found that they had a 30% higher prevalence of caries compared to the general population. Cannobbio et al.'s study, conducted in Italy, found that individuals with hearing difficulties were 20% less likely to utilize preventive dental services compared to those without hearing impairments.
Because health information is frequently delivered verbally, people with hearing loss may not receive or fully comprehend oral health guidance, contributing to lower health awareness and higher rates of oral disease (7, 8). In particular, difficulties in understanding dental terminology, oral hygiene practices, and the importance of routine care hinder their ability to maintain their oral health. Every individual has unique sensing skills, which influence their degree of understanding. Studies from high-income countries demonstrate that children with hearing impairments have significantly poorer oral hygiene than their hearing peers. A systematic review reported mean plaque and gingival index scores of 0.99 and 1.27, respectively, among individuals with hearing loss (3). Visually based interventions have shown efficacy in improving outcomes—for example, a UK-based randomized controlled trial (RCT) demonstrated that video instruction reduced plaque and gingival indices by 0.37 and 0.39, respectively, in this population (9).
Oral health knowledge, which encompasses understanding the significance of regular brushing, appropriate toothbrush selection, brushing techniques, dietary habits, and the importance of routine dental visits, is crucial for maintaining good oral health. Communication barriers often hinder individuals with hearing impairments from obtaining this information effectively (10). Health promotion strategies, including the use of visual aids and tailored educational programs, have been shown to improve knowledge and facilitate positive behavior change (11, 12). A randomized controlled trial in the UK demonstrated that visual instruction significantly reduced plaque and gingival indices in children with hearing impairments (13).
Despite the recognized link between oral health literacy, behavior, and clinical outcomes, there is limited data on the oral health knowledge and practices of individuals with hearing impairments in Jordan. Dentists may also encounter challenges in providing care to this group due to communication difficulties and limited training in accommodating their needs.
This study aims to assess oral health knowledge and dental behavior among individuals with hearing impairments compared to those without hearing impairments in Jordan. The findings are expected to provide a baseline for developing targeted interventions that enhance oral health awareness and outcomes in this underserved population.
Materials and methods
A researcher-developed questionnaire in Arabic, the official language in Jordan, was used to assess oral health knowledge and dental behavior among individuals with hearing impairments. The content validity of the questionnaire was established by two professional experts. The average congruency percentage (ACP) was calculated, which reflects the level of agreement among the expert panel members. The ACP was 92%, which indicates that the questionnaire was deemed to be valid by the professional experts and the items of the questionnaire were relevant and appropriate for this study. The consistency of the questionnaire was assessed by test–retest reliability, which was done by administering the same questionnaire twice to the same participants (n = 10). The internal reliability of the questionnaire was assessed using Cronbach's alpha coefficient, with an acceptable internal consistency of 0.75, indicating that the items in the questionnaire are related to each other. A pilot test for this study was conducted by administering the questionnaire to 10 caregivers of individuals with hearing impairments to provide feedback on the questionnaire’s content, clarity, and format. The questionnaire includes three parts. The first part focused on demographic information and included five items related to basic demographic information. In the second part, there were 12 items that evaluated the participant's oral health knowledge. Finally, in the third part, there were seven items that assessed the participant's dental behavior. The severity of a participant’s hearing impairment was objectively classified based on diagnostic records obtained from files provided by the school’s or center’s administrators. Thus, the severity was not self-reported but determined by professional clinical examination and documented in official records. Participants with hearing impairments were recruited from special-care centers and schools across Jordan through convenience sampling, which may have introduced selection bias. The participants were required to have basic reading ability in Arabic as part of the inclusion criteria to ensure consistent understanding and independent completion of the questionnaire.
The institutions were identified through the Ministries of Social Development and Education. Participation was contingent on the willingness of the administrators to distribute the questionnaire. A printed copy of the questionnaire and a cover letter explaining the study were distributed to the participants. Individuals who were literate completed the form themselves, while caregivers assisted those who were not. A group of individuals without hearing impairments was recruited from the same geographical areas using convenience sampling, which may have introduced selection bias. They were not matched by age or socioeconomic status, which may have affected comparability between the groups.
G*Power Sample Size Calculator software was used for the sample size calculation, with an 80% power and a margin of error of 5% based on Alshatrat et al. (14). The minimum sample size required for this study was 139 for each group.
A total of 200 questionnaires were sent to individuals with hearing impairment, of which 149 were completed and returned. In addition, 140 completed questionnaires from the individuals without hearing impairment were returned out of the 200 sent.
Data were collected and analyzed using the IBM SPSS Statistics for Windows Version 25.0 (IBM Corp., NY, USA; https://www.ibm.com). We conducted a descriptive statistical analysis of the sociodemographic characteristics and responses to the questions. The results are presented in terms of numbers and proportions. Intergroup comparisons were performed using two-tailed chi-square tests. Results were considered statistically significant at p < 0.05.
Results
The study included 289 participants, with 149 individuals with hearing impairments (HI group) and 140 individuals without hearing impairments. The mean age of the participants was 15 years, with most participants under 18 years. In the HI group, 57.1% had a severe hearing impairment, and 32.9% had a moderate impairment. Additional sociodemographic characteristics, including gender distribution, education level, and family income, are detailed in Table 1.

Table 1. Sociodemographic characteristics of the participants with hearing impairments and those without hearing impairments.
Regarding oral health knowledge, the analysis revealed no statistically significant differences between the HI group and those without hearing impairments in their understanding of plaque formation, caries etiology, the effects of sugar and soft drinks, and the relationship between oral health and general health (P > 0.05). However, notable differences were observed in other areas.
The individuals with hearing impairments were significantly less likely to know that gums should not bleed or swell during brushing (P < 0.001). They also demonstrated poorer knowledge regarding toothbrush hardness, with 77.1% of the HI group incorrectly believing that a hard toothbrush is needed to clean teeth, compared to only 4.7% of the individuals without hearing impairments (P < 0.001). In addition, 54.3% of the HI group thought dental visits were only necessary in the presence of a toothache, compared to 21.5% of the individuals without hearing impairments (P < 0.001). Notably, the HI group showed higher awareness regarding the necessity of dental floss use (87.9% vs. 75.8%, P = 0.019), possibly reflecting targeted health messages at the centers from which the participants were recruited. Full details of the oral health knowledge responses are presented in Table 2.

Table 2. Oral health knowledge among individuals with hearing impairments compared to those without hearing impairments.
Regarding dental behavior, differences in habits were observed between groups. A smaller percentage of hearing-impaired individuals reported brushing their teeth once or twice daily compared to the individuals without hearing impairments (82.8% vs. 93.3%, P < 0.001). Although 91.3% of the HI group were able to brush their teeth independently, this figure was significantly lower than that of the individuals without hearing impairments, where 100% were able to do so (P = 0.001).
The use of dental floss, mouthwash, and fluoridated toothpaste was significantly lower among the individuals with hearing impairments (P < 0.05). For instance, only 5.8% of the HI group flossed daily compared to 16.8% of the individuals without hearing impairments (P = 0.009). Soda consumption was notably higher in the HI group (94.3% vs. 98.7% reporting no soda consumption; P < 0.001).
No significant differences were observed in the duration of brushing or the frequency of sweet consumption between the groups (P > 0.05). Detailed behavioral responses are provided in Table 3.
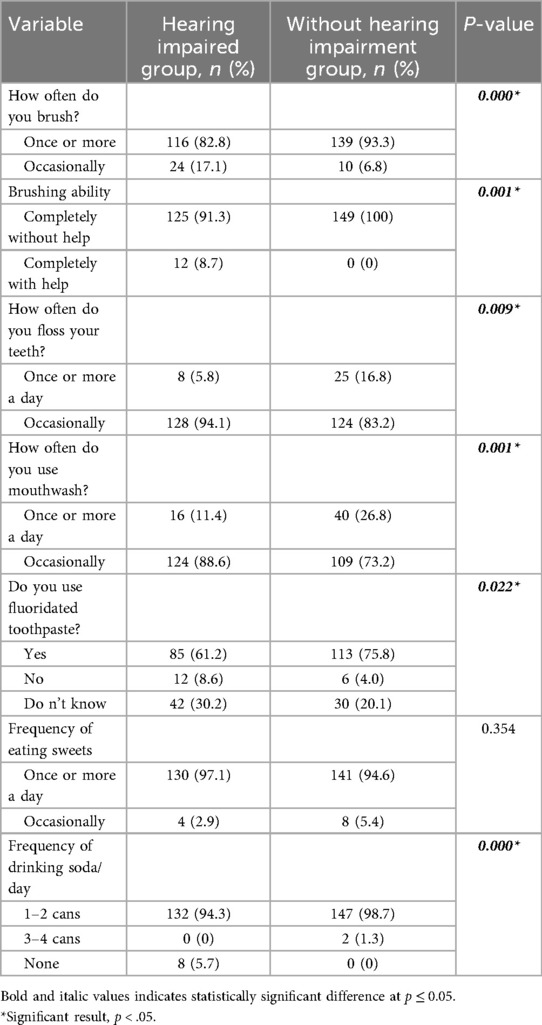
Table 3. Dental behavior among individuals with hearing impairments compared to those without hearing impairments.
Discussion
Hearing impairment is widely recognized as a barrier to effective communication, affecting social interaction, educational attainment, and overall quality of life (15). According to WHO estimates, 1 in 10 people globally will experience hearing loss by 2050 (3). In Jordan, the prevalence of significant hearing loss among infants was reported at 1.5% in 2014 (16), with a study conducted in 2024 estimating hearing impairment in only 0.06% of individuals aged 12 and above (17). This lower prevalence, compared to other nations, may reflect differences in screening programs or reporting methods. Notably, most participants in the present study had a severe hearing impairment, likely reflecting the recruitment from specialized centers catering to individuals with greater needs.
The prevalence of dental caries and caries experience, rate of gingival bleeding, and dental trauma in children with hearing impairment is high compared to figures observed in studies conducted among Jordanian schoolchildren with normal hearing (18).
Dental diseases and oral health can significantly impact the quality of life of individuals, as oral health is considered a crucial component of overall health and wellbeing (19). Although hearing impairment can reduce or eliminate the ability to receive and comprehend oral instructions and health promotion information, appropriate education on oral health hygiene using verbal and visual aids has been found to improve their oral health status and positively influence their perception of their quality of life (20).
Nevertheless, investigations into awareness, knowledge, and dental practices among individuals with hearing impairments have not been carried out in Jordan. Hence, this study aimed to investigate the oral health knowledge and dental practices amongst a cohort of Jordanian individuals with hearing impairments. Such an investigation was deemed necessary to scrutinize and analyze the gaps that exist in oral health knowledge that may need to be bridged through the implementation of applicable recommendations among people with hearing impairments.
The study found that hearing-impaired individuals exhibited comparable knowledge to individuals without hearing impairments in several key areas, including the role of plaque and bacteria in dental caries, the effects of sugary foods and carbonated beverages, and the relationship between oral and general health (21). This contrasts with a previous study conducted in Saudi Arabia, in which many hearing-impaired individuals were unaware of oral health basics or preventive care (22). Such findings suggest that in Jordan, efforts to raise awareness, perhaps through school-based programs or center-led initiatives, may have achieved some success. However, significant differences were observed in other domains. Individuals without hearing impairments demonstrated superior knowledge regarding toothbrushing.
The prevalence of regular tooth brushing for good oral health was higher among the Jordanian participants in the current study compared to a similar cohort of hearing-impaired individuals in other countries in the region, such as Saudi Arabia and Iran (22, 23).
In addition, most of the participants with hearing impairments reported that the primary reason for visiting a dentist was due to symptomatic oral disease. In contrast, a significant majority of the individuals without hearing impairments stated they visit the dentist even in the absence of a toothache. This lack of awareness regarding the importance of regular dental visits for asymptomatic individuals may contribute to a decline in their oral health. Without timely intervention, early-stage dental diseases are less likely to be detected, leading to more advanced dental issues with distressing symptoms and poor prognoses. This finding aligns with previous research by Mustafa et al. (2018) and Suma et al. (2011) (22, 24). Furthermore, irregular dentist visits have been associated with increased morbidity linked to dental caries (25). This pattern may also lead to a greater economic burden related to oral healthcare for this population.
Moreover, the hearing-impaired participants were less likely to recognize bleeding or swollen gums as signs of disease. These gaps highlight potential shortcomings in how oral health education reaches this population.
Interestingly, the hearing-impaired individuals showed greater awareness of the necessity of dental floss and correctly identified that healthy gums should not be red. This discrepancy, superior knowledge in some areas but poorer behaviors, warrants further exploration. One possible explanation is the role of visual learning tools, such as posters or video demonstrations, which may emphasize certain concepts more effectively than others (26). Studies from high-income countries also support the efficacy of visual and interactive education for hearing-impaired individuals (27, 28). Another possibility is prior exposure to tailored educational interventions at the centers where participants were recruited, although this could not be confirmed in the current study.
Despite having greater knowledge of flossing, the participants with hearing impairments used floss, mouthwash, and fluoridated toothpaste less frequently than their peers.
This gap between knowledge and practice underscores the critical insight that knowledge alone does not consistently motivate compatible dental health behaviors. Barriers such as affordability, limited product availability, and misconceptions about preventive care could contribute to this discrepancy (29, 30). Similar findings have been reported in other populations where awareness of preventive measures did not translate into action (31).
Confounding factors, including socioeconomic status, education level, and school type (mainstream vs. special education), may also influence these results. For example, lower family income and limited access to health services—more common among individuals with hearing impairments—could restrict opportunities to apply oral health knowledge in practice (32).
The contradiction between participants’ acknowledgment of sweets and soft drinks as detrimental and their continued high consumption highlights a broader challenge in public health: bridging the gap between awareness and sustained behavioral change (24, 33). Such patterns reinforce the importance of multifaceted interventions that address not only knowledge but also accessibility, affordability, and cultural attitudes toward oral health (26, 27).
Studies consistently demonstrate that hearing-impaired populations tend to have poorer oral hygiene, higher rates of caries, and worse oral health-related quality of life than their hearing peers (34, 35). However, the findings from this study suggest that targeted educational programs incorporating visual aids and culturally sensitive materials may help address these disparities.
Similar approaches in high-income countries have shown promising results, improving oral hygiene behaviors and reducing plaque and gingival scores (26, 28).
Although the current study employed a validated questionnaire, its reliance on literacy may have limited its applicability to all individuals with hearing impairments. Future studies should consider alternative data collection tools tailored to this population, such as sign language interviews or pictorial questionnaires, to enhance inclusivity. In addition, participants with hearing impairments were recruited through convenience sampling, which may have introduced selection bias. Moreover, while data were collected from multiple centers in Jordan, the sample size could be expanded in future research to improve generalizability and allow for adjustments based on age, gender, and socioeconomic status.
To our knowledge, this is the first study in Jordan to investigate oral health knowledge and practices among individuals with hearing impairments. The findings provide a valuable baseline for designing interventions to reduce oral health disparities and promote equitable access to dental care.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
This study involving humans was approved by Jordan University of Science and Technology. This study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
SA: Project administration, Supervision, Methodology, Writing – review & editing, Validation, Investigation, Writing – original draft, Formal analysis, Software, Data curation, Funding acquisition, Resources, Conceptualization. WA-O: Writing – original draft, Writing – review & editing, Data curation, Conceptualization. AT: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. MA: Writing – original draft, Writing – review & editing. SS: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by Jordan University of Science and Technology Research (Grant no: 20170032).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cannobbio VC, Cartes-Velásquez R, McKee M. Oral health and dental care in deaf and hard of hearing population: a scoping review. Oral Health Prev Dent. (2020) 18(3):417–25. doi: 10.3290/j.ohpd.a44687
2. Sharby N, Martire K, Iversen MD. Decreasing health disparities for people with disabilities through improved communication strategies and awareness. Int J Environ Res Public Health. (2015) 12:3301–16. doi: 10.3390/ijerph120303301
3. World Health Organization. Deafness and Hearing Loss. Geneva: World Health Organization (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
4. Babu NV, Moureen A. Comparative assessment of salivary osmolality as a caries risk indicator in cerebral palsy children. Int J Res Publ Sci IT Manag. (2017) 6(10):1–6.
5. McKee M, Moreland C, Atcherson S, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. (2015) 434:24–8.26161525
6. Bhadauria US, Purohit B, Agarwal D, Priya H. Dental caries status in individuals with hearing difficulties: a systematic review and meta-analysis. Spec Care Dentist. (2023) 43(1):9–16. doi: 10.1111/scd.12745
7. McKee M. Deaf or hard of hearing message recipient sociodemographic characteristics. In: Powers M, editor. Oxford Research Encyclopedia of Communication. Oxford: Oxford University Press (2017). Available online at: https://doi.org/10.1093/acrefore/9780190228613.013.353 (Accessed March 18, 2025).
8. Purohit BM, Abhina S. Oral health status of 1-year-old children with disabilities and control in southern India. WHO South East J Public Health. (2012) 1(3):330–8. doi: 10.4103/2224-3151.207029
9. Sandeep V, Vinay C, Madhuri V, Rao VV, Uloopi KS, Sekhar RC. Impact of visual instruction on oral hygiene status of children with hearing impairment. J Indian Soc Pedod Prev Dent. (2014) 32(1):39–43. doi: 10.4103/0970-4388.127053
10. Atmaja JR. Pendidikan dan Bimbingan Anak Berkebutuhan Khusus. Bandung: PT Remaja Rosdakarya (2018). p. 1.
11. Mitchell DA, Mitchell L. Oxford Handbook of Clinical Dentistry. Oxford: Oxford University Press (2014).
12. Susilowati D. Promosi Kesehatan: Modul Bahan Ajar Cetak Keperawatan. Jakarta: Kementerian Kesehatan Republik Indonesia (2016).
13. Selvaraj S, Naing NN, Wan-Arfah N, Abreu MHNGD. Assessment on oral health knowledge, attitude, and behaviour and its association with sociodemographic and habitual factors of South Indian population. Pesqui Bras Odontopediatria Clin Integr. (2021) 21:e0135. doi: 10.1590/pboci.2021.159
14. Alshatrat SM, Al-Omari WM, Tabnjh AK, Al-Bakri IA, Selvaraj S. A case-control study on oral health knowledge and dental behavior among individuals with developmental delays in Jordan: caregiver perspective. Front Dent Med. (2024) 5:1426568. doi: 10.3389/fdmed.2024.1426568
15. Robinshaw HM. Early intervention for hearing impairment: differences in the timing of communicative and linguistic development. Br J Audiol. (1995) 29(6):315–34. doi: 10.3109/03005369509076750
16. Abu-Shaheen A, Al-Masri M, El-Bakri N, Batieha A, Nofal A, Abdelmoety D. Prevalence and risk factors of hearing loss among infants in Jordan: initial results from universal neonatal screening. Int J Audiol. (2014) 53(12):915–20. doi: 10.3109/14992027.2014.944275
17. Alqudah S, Zuriekat M, Hassan S, Mahafdeh H, Alqudah Z, Shatarah A, et al. The prevalence and patterns of hearing loss in Jordan: a cross-sectional study. PLoS One. (2024) 19(8):e0304125. doi: 10.1371/journal.pone.0304125
18. Rajab LD, Da'as NM. Oral health status, behavior, and practices among hearing impaired children attending a specialized school in Jordan. Spec Care Dentist. (2024) 44(6):1651–60. doi: 10.1111/scd.13032
19. Paulson DR, Ingleshwar A, Theis-Mahon N, Lin L, John MT. The correlation between oral and general health-related quality of life in adults: a systematic review and meta-analysis. J Evid Based Dent Pract. (2025) 25(1S):102078. doi: 10.1016/j.jebdp.2024.102078
20. Manohar PS, Subramaniam P. Oral health-related quality of life and oral hygiene of children and adolescents with hearing impairment. Int J Clin Pediatr Dent. (2022) 15(3):311–5. doi: 10.5005/jp-journals-10005-2377
21. Bowyer V, Sutcliffe P, Ireland R, Lindenmeyer A, Gadsby R, Graveney M, et al. Oral health awareness in adult patients with diabetes: a questionnaire study. Br Dent J. (2011) 211:E12. doi: 10.1038/sj.bdj.2011.769
22. Mustafa M, Asiri FYI, AlGhannam S, AlQarni IAM, AlAteeg MA, Anil S. Extent of awareness regarding oral health and dental treatment needs among individuals with hearing and speech impairments in Saudi Arabia. J Int Soc Prev Community Dent. (2018) 8(1):70–6. doi: 10.4103/jispcd.JISPCD_194_17
23. Hashemi Z, Hajizamani A, Bozorgmehr E, Omrani F. Oral health status of a sample of disabled population in Iran. J Oral Health Oral Epidemiol. (2012) 1:23–8.
24. Suma G, Das UM, Akshatha BS. Dentition status and oral health practice among hearing and speech-impaired children: a cross-sectional study. Int J Clin Pediatr Dent. (2011) 4(2):105–8. doi: 10.5005/jp-journals-10005-1091
25. Krol DM, Whelan K, Section in Oral Health. Maintaining and improving the oral health of young children. Pediatrics. (2023) 151(1):e2022060417. doi: 10.1542/peds.2022-060417
26. Tugeman H, Rahman N, Yusoff A, Daud MK. Oral health knowledge, practice and dental plaque maturity status of hearing-impaired children. Sains Malaysiana. (2016) 45(5):761–8.
27. Hoang H, LaHousse SF, Nakazono TT, Davidson PL. Access to care for hearing-impaired patients: experiences and attitudes of dental providers. J Am Dent Assoc. (2011) 142(8):859–65. doi: 10.14219/jada.archive.2011.0275
28. Pollard RQ, Barnett S. Health-related vocabulary knowledge among deaf adults. Rehabil Psychol. (2009) 54(2):182–5. doi: 10.1037/a0015771
29. Freeman R. Barriers to accessing dental care: patient factors. Br Dent J. (1999) 187(3):141–4. doi: 10.1038/sj.bdj.4800236
30. Fellinger J, Holzinger D, Pollard R. Mental health of deaf people. Lancet. (2012) 379(9820):1037–44. doi: 10.1016/S0140-6736(11)61143-4
31. Glick M, Williams DM, Kleinman DV, et al. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. J Am Dent Assoc. (2016) 147(12):915–7. doi: 10.1016/j.adaj.2016.10.001
32. Blanchfield BB, Feldman JJ, Dunbar JL, Gardner EN. The severely to profoundly hearing-impaired population in the United States: prevalence estimates and demographics. J Am Acad Audiol. (2001) 12:183–9.11332518
33. Moin M, Saadat S, Rafique S, Maqsood A, Lal A, Vohra F, et al. Impact of oral health educational interventions on oral hygiene status of children with hearing loss: a randomized controlled trial. Biomed Res Int. (2021) 2021:5185613. doi: 10.1155/2021/5185613
34. Singh A, Agarwal A, Aeran H, Dhawan P. Oral health & quality of life in preadolescents with hearing impairment in Uttarakhand, India. J Oral Biol Craniofac Res. (2019) 9(2):161–5. doi: 10.1016/j.jobcr.2019.03.004
Keywords: oral care, hearing impairments, dental behavior, oral health knowledge, deaf
Citation: Alshatrat SM, Al-Omari WM, Tabnjh AK, Alsaleh MM and Selvaraj S (2025) Comparative assessment of oral health knowledge and dental behavior among individuals with and without hearing impairments in Jordan. Front. Oral Health 6:1643903. doi: 10.3389/froh.2025.1643903
Received: 9 June 2025; Accepted: 27 August 2025;
Published: 19 September 2025.
Edited by:
Rahul Siram Naidu, The University of the West Indies St. Augustine, Trinidad and TobagoReviewed by:
Amani Harrandah, Umm al-Qura University, Saudi ArabiaJocelyne Valerie Gare, University Ouaga I Prof Joseph Ki Zerbo, Burkina Faso
Copyright: © 2025 Alshatrat, Al-Omari, Tabnjh, Alsaleh and Selvaraj. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sabha Mahmoud Alshatrat, c21hbHNoYXRyYXRAanVzdC5lZHUuam8=; Abedelmalek Kalefh Tabnjh, YWJlZGVsbWFsZWsua2FsZWZoLnRhYm5qaEBndS5zZQ==
†ORCID:
Majd M. Alsaleh
orcid.org/0000-0002-5561-1613
 Sabha Mahmoud Alshatrat
Sabha Mahmoud Alshatrat Wael Mousa Al-Omari
Wael Mousa Al-Omari Abedelmalek Kalefh Tabnjh
Abedelmalek Kalefh Tabnjh Majd M. Alsaleh5,†
Majd M. Alsaleh5,† Siddharthan Selvaraj
Siddharthan Selvaraj