- 1Canadian Food Inspection Agency, National Centre for Foreign Animal Disease, Winnipeg, MB, Canada
- 2Department of Immunology, University of Manitoba, Winnipeg, MB, Canada
- 3Department of Medical Microbiology, University of Manitoba, Winnipeg, MB, Canada
- 4Center of Excellence for Emerging and Zoonotic Animal Diseases (CEEZAD), Manhattan, KS, United States
- 5USDA, Arthropod-Borne Animal Diseases Research Unit (ABADRU), Manhattan, KS, United States
Since the discovery of Rift Valley Fever virus (RVFV) in Kenya in 1930, the virus has become widespread throughout most of Africa and is characterized by sporadic outbreaks. A mosquito-borne pathogen, RVFV is poised to move beyond the African continent and the Middle East and emerge in Europe and Asia. There is a risk that RVFV could also appear in the Americas, similar to the West Nile virus. In light of this potential threat, multiple studies have been undertaken to establish international surveillance programs and diagnostic tools, develop models of transmission dynamics and risk factors for infection, and to develop a variety of vaccines as countermeasures. Furthermore, considerable efforts to establish reliable challenge models of Rift Valley fever virus have been made and platforms for testing potential vaccines and therapeutics in target species have been established. This review emphasizes the progress and insights from a North American perspective to establish challenge models in target livestock such as cattle, sheep, and goats in comparisons to other researchers' reports. A brief summary of the potential role of wildlife, such as buffalo and white-tailed deer as reservoir species will also be discussed.
Background and Introduction
In the last 20 years there has been a re-emergence of various well-known arboviral diseases, many of which are zoonotic in nature, such as West Nile, Japanese encephalitis, Rift Valley fever, Venezuelan equine encephalitis, and Eastern equine encephalitis (1). Among these, Rift Valley fever (RVF) is considered a significant threat to animal and public health, economy, and food (2–4). Rift Valley fever was first reported in Kenya in 1930 (5), and has since created sporadic outbreaks in cattle and small ruminants with associated zoonotic spread to humans in sub-Saharan Africa. The disease first came to global attention during an outbreak in Egypt in 1977–78, involving at least 200,000 human infections (6). It was during the Egyptian outbreak when ocular degeneration was first associated with RVFV infections in humans (7). Global concerns were raised when RVF virus (RVFV) spread to Saudi Arabia and Yemen in 2000 (8) as well as during an outbreak in East Africa (Kenya, Tanzania, Somalia, and the Sudan) in 2006/7 (9–13). Since then there have been outbreaks in Madagascar (3), Mauritania 2010 (14), Namibia 2010 (15), South Africa 2008–2011 (16), Mozambique 2014 (17), Republic of Niger 2016 (18), and Kenya 2018 (WHO). The presence of the disease, especially during outbreaks, has significant socio-economic impact in endemic regions (19, 20). This along with the potential risk of RVFV importation into Europe and the U.S. (4) as well as its potential use as a biological weapon (21, 22), has led to intensified research on developing mitigation strategies. Developing such strategies requires a detailed understanding of the mosquito-transmitted virus that causes RVF disease.
RVFV is endemic in Sub-Saharan Africa and continues to cause sporadic outbreaks that are of veterinary and public health concern. Although RVFV is primarily a disease of domestic and wild animals, there can be spillover to humans during outbreaks than can lead in rare cases to lethal hemorrhagic disease in humans. RVFV outbreaks occur in 7–10 year cycles presumably as the number of seropositive animals in the population decrease, and/or ideal weather conditions for the mosquito vectors are present. It has also been suggested that recently emerged strains of RVFV might be more virulent to humans (23). Thus, RVF is clearly a disease that requires a “One Health” approach to mitigation strategies (24, 25) as it is a potential threat to animal and public health, economy, and food security (4, 25–27).
Outbreaks of RVF occur when conditions are ideal for mosquito expansion and virus transmission. Aedes mcintoshi mosquito species are thought to initiate epizootic outbreaks because of their transovarial transmission capability (28). Once the outbreak has been established, it can then be maintained by Aedes and other species (e.g., Culex and Mansonia) which can both replicate and transmit the virus (29). Although this is a well-accepted hypothesis for RVFV maintenance, transovarial transmission has only been demonstrated in one study. Alternatively, the mosquito to animal transmission cycle could be continuous at low levels and only become observed when ideal environmental conditions occur. The importance of understanding the potential role of transovarial transmission in mosquito-borne viruses has been reviewed (30). An increasing number of studies have also identified other species of mosquitoes that are either susceptible to RVFV and/or are capable of transmitting RVFV in the Anopheles, Mansonia, and other mosquito genera (13, 31). North American species such as Aedes canadensis, Aedes taeniorhynchus, and Culex tarsalis (32–34) and the stable fly species Stomoxys calcitrans (33) have also been shown to be capable of transmitting RVFV. The control of mosquitoes involved in RVFV transmission is complex because there are numerous mosquito species present in endemic and non-endemic areas that are capable of virus infection and transmission [reviewed in Linthicum et al. (29)], and continuous low-level transmission of RVFV to domestic and wild animals in endemic areas may also help maintain the virus. Other species that may play a role in RVFV ecology and have been reported to be susceptible to RVFV are mice, rats, shrews, dormice, and bats (35–40). Additional wild animal species that have been investigated include the African buffalo, primates, elephants, rhinoceros, deer, and coyotes (41–45). However, it is difficult to determine the role of susceptible wild animals in maintenance and transmission of RVFV. Based on a risk model, transmission and seroprevalence rates in both domestic and wild animals correlate positively with the risk of zoonotic infection of people (46).
RVFV is in the order Bunyavirales (Phenuiviridae; genus Phlebovirus), with a genome consisting of three negative-sense, single stranded RNA segments; L (large), M (medium), and S (small). The L segment encodes the RNA-dependent RNA polymerase (47). The M segment encodes the precursor protein of two structural glycoproteins, Gn and Gc, which are present on the virus surface. Cleavage of the precursor protein leads to two additional non-structural proteins of 78 kDa (P78 or LGp) and 14 kDa (NSm) in molecular mass (48–51). The Gn and Gc form heterodimers on the virus surface (52) and are involved in attachment of the virus to the host cell (53, 54). The NSm has been shown to inhibit apoptosis but is not essential for virus replication (55). Although also not critical for RVFV virulence, lack of NSm did reduce mortality and increase the number of animals demonstrating neurological disease in subcutaneously infected rats (56) and NSm mutated viruses were attenuated in intraperitoneally infected mice (57). The LGp/P78 protein, which is not associated with RVFV virulence in mice, is packaged into viruses grown in C6/36 (Aedes albopictus) insect cells, but not in mammalian cells, and is a major determinant of virus dissemination in mosquitoes (57, 58). Interestingly, additional studies showed that NSm is involved in virus replication and dissemination in Aedes aegypti mosquitoes (59, 60). The S segment utilizes an ambisense strategy encoding the nucleocapsid (N) protein in the anti-sense direction and the NSs protein in the sense direction (61). The N protein is the most abundant protein in the virion and plays a key role in transcription and replication and reconstitutes the ribonucleoprotein (RNP) complex together with the vRNA and the L protein (62). The N protein is immuno-dominant and is used as an antigen for diagnostic assays (63). The NSs protein has immunomodulatory functions and acts as interferon-antagonist via the inhibition of host gene transcription (64–66). The NSs protein is produced early during RVFV infection and has also a positive effect on viral replication and RNA transcription (67). The above described studies indicate that both, LGp/P78 and NSm seem important for virus maintenance in mammalian and insect hosts, and that NSs is an important virulence factor. This information led to the development of a NSm and NSs double deleted virus that was shown to be attenuated in rats (68). When used as a vaccine, RVF virus containing NSm and NSs deletions were shown to be safe and non-teratogenic in pregnant sheep as well as protective against the development of viremia and RVF disease (69). These findings are supportive of the mechanistic studies in but since just rodent model systems; however, there have been only a few studies directed at understanding of the molecular basis of RVFV virulence and molecular pathogenesis in target livestock species.
RVFV research conducted in target livestock species has been primarily focused on the development of diagnostics and vaccines. As a result of the 2006/2007 RVF outbreak in Kenya (12, 70), this disease garnered increased attention from global scientific communities. This has led to an increased focus on identifying North American mosquito species that are capable of being infected and able to transmit RVFV, as well as improving RVFV diagnostic tools (71–75), developing better risk models for RVF (76–79) and evaluating these models using seroprevalence data (46). Several studies have also published data demonstrating that RVFV circulates in endemic countries during inter-epidemic periods (43, 80, 81).
Currently, there are modified live virus (MLV) or attenuated (82, 83) and inactivated/killed vaccines licensed for veterinary use in RVFV endemic countries and one attenuated MLV vaccine with a conditional license in the United States (USDA-APHIS, CVB Notice 13-12). Since various RVFV vaccine approaches were recently reviewed in several publications (25, 84–86), they will be only discussed briefly here. Other recent reviews have focused on the molecular biology, reassortment capacity, diagnostics, and vaccines (86, 87). Thus, this review will focus on the development of target livestock infection models.
Developing RVFV Infections in Target Species
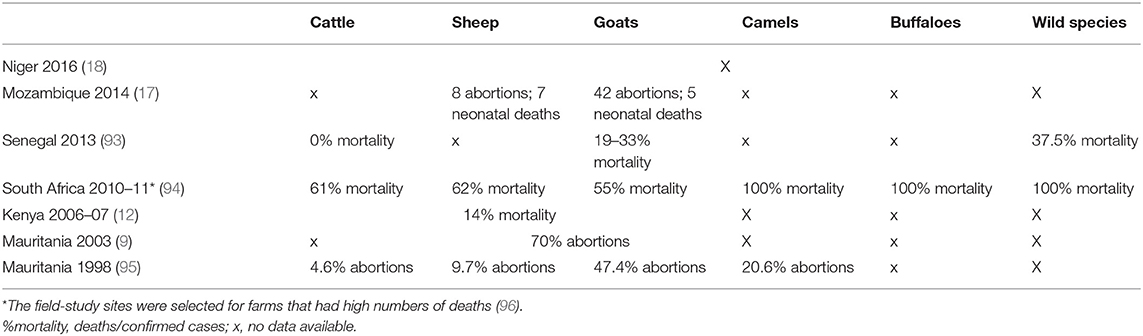
The animals most susceptible to RVFV consist of ruminants such as sheep, goats and cattle, as well as camels, buffaloes, and humans (88). These animals all produce viremia upon infection with clinical signs that typically range from asymptomatic to moderate and high severity to death; in addition, pregnant animals suffer from high rates of abortion (17, 89–91). Although the documentation of confirmed RVFV cases, deaths and abortions in animals has been sparse, recent studies with confirmed RVFV antibody status have provided estimates of animal mortality rates during different outbreaks [(92); see Table 1].
Early work on RVFV livestock infections was done in South Africa (89, 90, 97), and a few RVFV experimental infections of livestock were conducted in the 1970/80s at the Plum Island Animal Disease Center (USDA) (98). These early studies included safety and efficacy trials for both inactivated (98) and a mutagen-attenuated MLV vaccine (99, 100). No RVFV infection studies using livestock had been conducted on the mainland of North America since these earlier studies. In 2006, the Canadian Food Inspection Agency (CFIA) and the United States Department of Agriculture (USDA) were tasked with developing target animal infection models to develop and evaluate diagnostic and control strategies. The procedures and models developed through this cooperative research were then transferred to the Biosecurity Research Institute (BRI) at Kansas State University (KSU) through collaboration with the Center of Excellence for Emerging and Zoonotic Animal Diseases (CEEZAD) at KSU. The results of this ongoing three-way collaboration are reviewed here and discussed within context of the literature.
There are several traits desirable in a veterinary RVFV vaccine, but at a minimum the vaccine should protect against abortions in pregnant animals and should prevent viremia to avoid transmission. In addition, the vaccine should be safe and efficacious in the most vulnerable target species and groups, that is, in fetal and newborn animals. For example, RVFV can be transmitted vertically from pregnant ewes to their fetus (101). Newborn lambs also remain highly susceptible to RVFV after they have been weaned as they lose any protection from maternally-derived antibodies. As weaning can occur any time between 3 weeks and 4 months, the earlier a vaccine can be given, the better. Therefore, in developing challenge models, these are important aspects of the disease that should be considered. For example, previous studies have utilized pregnant ewe models to evaluate whether experimental attenuated or MLV vaccines cross the placenta (102) and are safe to administer during pregnancy. Although this model is highly susceptible to RVFV and is useful for evaluating vaccine safety, using pregnant animals in high containment animal rooms (i.e., BSL-3Ag) is logistically challenging. Therefore, alternative models have also been developed and will be discussed.
Sheep Model Development
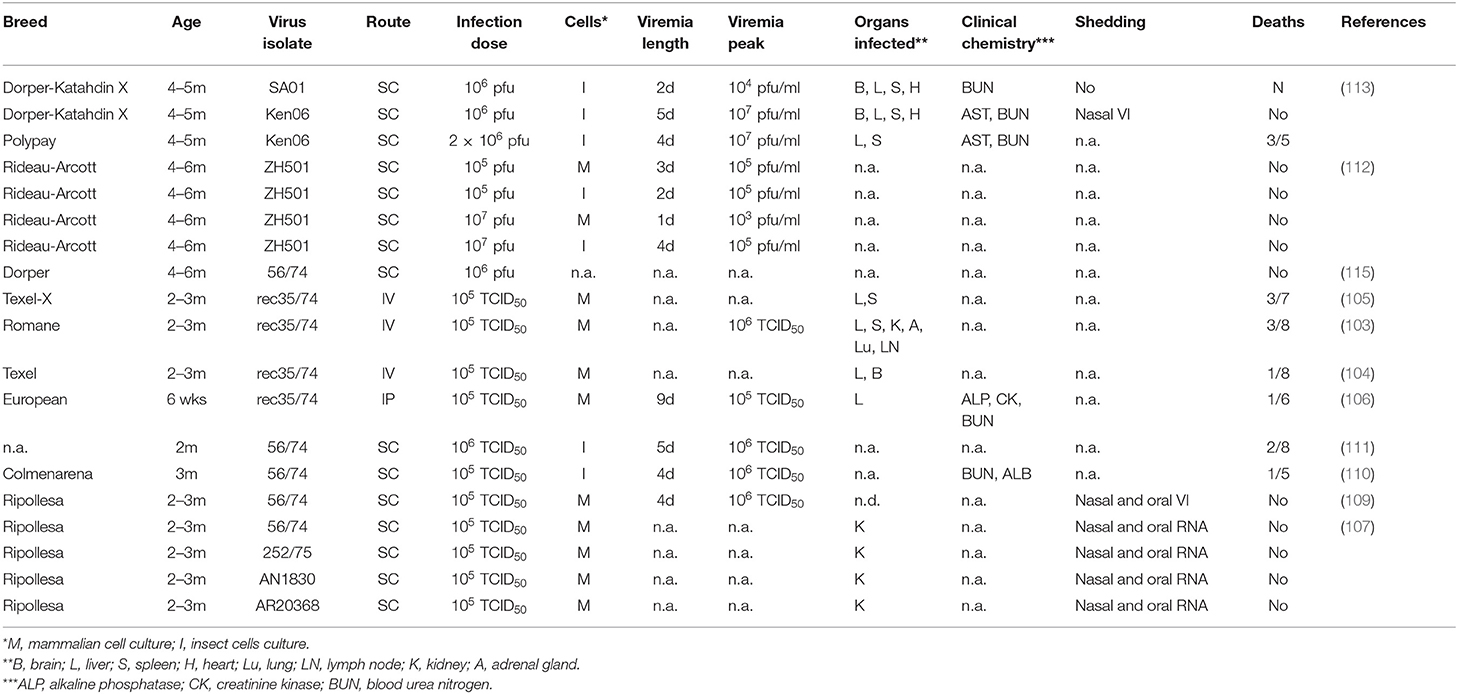
Several challenge models have been developed in 2–3 month old lambs that display significant pathology that is typical of RVFV. For example, Kortekaas et al. has utilized intravenous (103–105) and intraperitoneal inoculation (106) of the recombinant 35/74 RVFV isolate grown in mammalian cells in Texel, Romane, and other European breeds at 105 TCID50. The challenge controls in these studies developed peracute clinical signs and fever, viremia for 4–6 days with peak titers of 105-106 TCID50, and virus was detected in the liver. Clinical markers also indicated elevated levels of plasma alkaline phosphatase and alanine transferase (hepatic dysfunction) as well as blood urea nitrogen and creatinine (renal dysfunction) (106). Pathology varied between different individual animals as is typically seen in studies with ruminants, but heavily affected the liver, and could also include abdominal hemorrhage, pulmonary edema and petechiae in the spleen, heart and lungs (104). Notably, these studies indicated an overall rate of 20% mortality with up to 70% mortality in some studies. Other pathological findings have been found in a study where 2–3 month-old lambs were infected with various field isolates (56/74, 252/75, AN1830, AR20368) and included the development of corneal opacity (107). A study with the Zinga isolate also induced severe clinical signs characterized by hyperactivity, watery and mucoid nasal discharges, projectiles and bloody diarrhea, external hemorrhage and neurological signs (108).
Other groups have developed 2–3 month old challenge models with the 56/74 RVFV isolate in Ripolessa (107, 109), Colmenarena (110) and other (111) sheep breeds using subcutaneous inoculation at 105-106 TCID50. Similarly, these animals also developed clinical signs and fever and viremia for 4–5 days with peak titers of 105-106 TCID50. Interestingly, two of these studies detected oral and nasal shedding of viral RNA between one and 7 days post infection (107, 109) with a few samples also leading to viral isolation (109); one of the uninfected sentinel animals even became seropositive suggesting that horizontal transmission may have occurred. The only other study to report horizontal transmission in sheep is after challenge with the Zagazig strain (98). While the studies by Busquets utilized passage 12 virus stocks grown in mammalian cells and had no deaths, the two studies by Chrun and Lorenzo had ~20% mortality and both used passage 5 mosquito-cell derived viral stocks. Since these three studies were performed independently in different breeds of sheep, it is not possible to directly compare these results; however, it is interesting to note that the age, viral strain, route, and dose were all similar in these studies, leaving breed, source of virus, and virus passage history as the main differences.
Challenge models have also been developed in older lambs at 4–6 months of age. For example, Suffolk and Arcott-Rideau breeds were challenged subcutaneously with 105 or 107 pfu of the ZH-501 RVFV isolate and compared virus stocks that had been grown in either mammalian Vero or mosquito C6/36 cells (112). While the mosquito-cell grown virus produced a robust and consistent infection, the mammalian-cell produced virus had reduced efficacy with viremia only present on day 1 and lower titers (102 pfu/ml serum) (112). In contrast to the acute illness seen in the 2–3 month old lambs, 4–6 month old sheep only produced a mild, self-resolving disease with transient pyrexia during the first week after infection and had no obvious gross pathology at 7 days post infection.
At KSU, 4–6 month-old Dorper-Katahdin and Polypay sheep were inoculated subcutaneously with 106 pfu passage-2 mosquito-derived virus stock using either RVFV isolate Kenya-128B-15 (Ken06) or SA01-1322 (SA01) (113). SA01 originated from the Saudi Arabian outbreak in 2001 (8) and Ken06 from the Kenyan outbreak in 2006 (114) which had affected an unusually large number of people and was speculated to possibly be more pathogenic. Both RVFV strains produced detectable viremia between days 1 and 5, and both strains produced gross pathology and histopathology consistent with RVFV virus infection at between days 3–5 (113). However, the Ken06 group tended to have higher viremia and serum aspartate aminotransferase (AST) levels indicating that liver damage was significantly higher in Ken06 infected lambs as compared to SA1 infected animals. Virus isolation from nasal swabs detected infectious virus in a three out of six animals infected with the Ken06 strain while no shedding was seen in SA01-infected lambs. Histopathology and viral antigen was detectable in a wide variety of organs including the spleen, liver, adrenal gland, and kidney during the first week after infection, although no specific differences were attributed to one isolate compared to the other. In addition, histopathology without antigen staining was detected in the brain, intestine, and the eye at later time points, and infectious virus could also be isolated from several tissues including the spleen and the liver between 3–5 days post challenge (25, 113). Three of five animals inoculated with Ken06 had large necrotic foci in the liver, hemorrhage in the liver and spleen, and pulmonary edema.
A summary of the discussed sheep models can be found in Table 2.
Goat Model Development
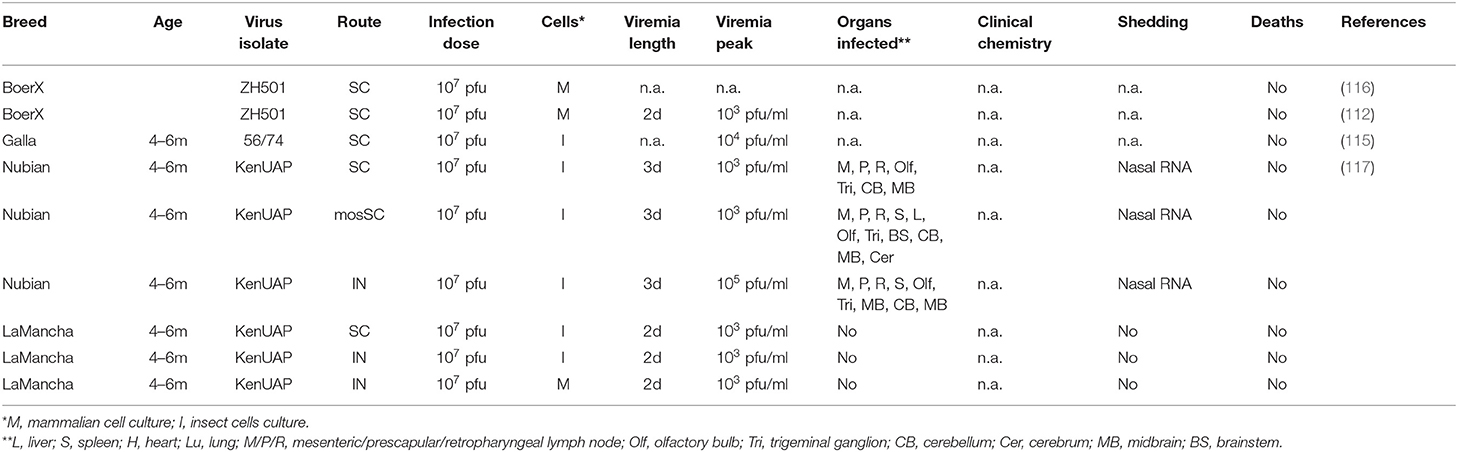
Initial experimental goat infection studies were performed with RVFV strain ZH501 (112) and were intended to establish the dose required for the induction of viremia, the timing of viremia and a comparison of inoculation virus grown in mammalian and insect cells. In this study, viremia occurred very quickly in goats, appearing on the first day post infection after SQ inoculation and lasted 2–5 days. By comparing an inoculation dose of 105 pfu and 107 pfu of the ZH-501 strain (112) we determined that the higher dose achieved more robust and reliable titers. A second study in Boer goats focused on the characterization of innate and adaptive immune responses in the blood after RVFV infection (116). Flow cytometry indicated that after RVFV infection there was a decline in CD5+ (T cells), CD172+ cells (monocytes and dendritic cells), and CD8+ T cells (cytotoxic T lymphocytes) and an increase in CD21+ cells (B cells). Interestingly, these effects were more pronounced in goats infected with mosquito cell-grown virus compared to goats infected with mammalian cell-grown virus (116). In addition, cytokine profiling in the blood demonstrated an increase of interleukin-12 at 1 dpi, an increase of IFN-γ at 2 dpi, and a steady increase of TNF-α, IL-6 and IL-1β up until the end of the observation period at 21 dpi (116). A Kenyan RVFV isolate (“Ken-UAP,” Genbank #MH175203.1, MH175204.1, MH175205.1) that had been proposed to be more pathogenic than ZH501 has also been tested in goats (117). Although the Ken-UAP and ZH501 RVFV isolates were not compared directly in the same goat breed, viremia titers after subcutaneous inoculations of each were comparable (112, 117).
Several novel alternative routes of infection have also been explored. For example, numerous manuscripts describing arbovirus infections have demonstrated that mosquito saliva can modulate the pathogenicity of the virus upon infection (118–123). To test the effect of saliva on RVFV infection in goats, we mimicked a methodology developed by Le Coupanec et al. (119) in mice; first, we allowed naïve mosquitoes to feed at a shaved site on the goats' skin and second, we then injected a known amount of virus subcutaneously (SQ) into the same area. Although the “mosquito-SQ” infection did not result in significant differences in viremia or antibody titers when compared to the “only SQ” infection, we noted that the “mosquito SQ” group retained higher levels of viral RNA in tissues at 28 days post challenge (117). Interestingly, viremia is delayed by 1 day when the virus is inoculated intranasally, suggesting that it has a longer transition (i.e., 48 h) route to travel to the bloodstream (117). Seroconversion kinetics are similar to that in sheep and cattle, occurring at 4–5 days post infection, and producing robust antibody titers at 21–28 days post infection. The tissues that are infected by RVFV may differ with breed, route of inoculation, and RVFV strain. However, spleen, liver, and lymph nodes are consistently positive and reliable targets for RVF diagnosis (112, 117). Other tissues that may be infected by RVFV include a variety of CNS regions such as the olfactory bulb, the trigeminal nerve, the cerebellum, the midbrain and the brainstem. The development of clinical signs varied from asymptomatic to mild and most commonly consisted of fever and diarrhea. To assist in identifying and quantifying other more subtle signs of disease, a RVFV clinical scoring sheet was developed for ruminants (see Supplementary Table 1). Using the clinical scoring sheet, subcutaneous infection of Nubian goats demonstrated slightly higher clinical scores than intranasal infection (Supplementary Figures 2A,C). In contrast, LaMancha goats had a higher clinical score after intranasal infection when compared to a subcutaneous infection, and a higher clinical score when infected with mosquito cell grown virus compared to mammalian cell grown virus (Supplementary Figures 2E,F). Different clinical outcomes after RVFV infection are also seen amongst different experimental groups with Boer goats remaining almost asymptomatic with mild clinical signs with ZH501, whereas Nubian and LaMancha goats exhibited clear clinical signs with Ken06 (Supplementary Figures 2A–I).
A few other goat breeds have been successfully used for RVFV model development or RVFV vaccine testing including the Galla (115) and Saanen (124) goat breed. Both experiments produced viremia but no clinical signs.
A summary of the discussed goat models can be found in Table 3.
Cattle Model Development
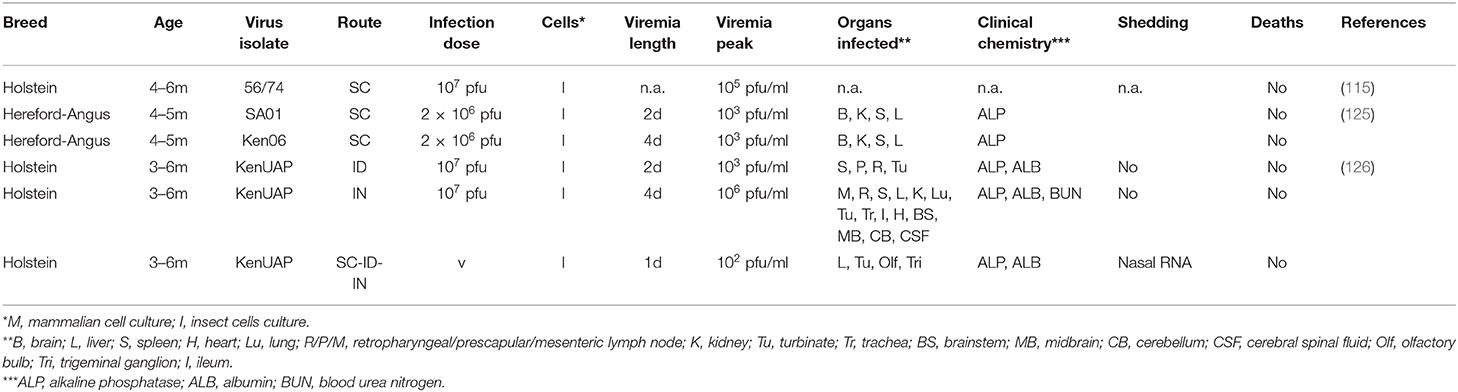
At KSU, an initial cattle model was established using an Angus or Hereford cross (125), which are commonly bred in North America or Europe for beef production and could be sourced from local farms. Similar in design to our study with sheep, a subcutaneous injection of mosquito-cell grown Kenya-128B-15 (Ken06) or SA01-1322 (SA01) at a titer of 106 pfu was inoculated (125). There was variation in the responses to RVFV infection. Most of the infected animals had detectable viremia at least 1 day post infection (4 of 5), but some were asymptomatic, some were febrile and one animal died of infection. There was detectable virus in nasal swabs during the peak of viremia but no evidence of contact transmission to the contact control animals (125).
In an effort to increase the reliability of the infection in cattle, a second study was undertaken in Holstein calves in which we used three different routes of infections, including intradermal, intranasal and a combination of subcutaneous, intradermal, and intranasal. Despite an adherence to subcutaneous RVFV infections in a majority of manuscripts, we tested whether an intradermal challenge model could result in an enhanced clinical course of RVFV infection. Our results indicated that the degree of viremia was similar to that of a subcutaneous infection, although far fewer tissues tested positive for virus presence in the intradermal model. After intradermal inoculation, infectious virus was only found in turbinates, prescapular lymph nodes, and retropharyngeal lymph nodes (126). Although ruminants are not known to become infected intranasally in the wild, they are quite susceptible to intranasal infection. Intranasal inoculation of cattle led to high titers of viremia with peak titers of 6 × 105 pfu/ml blood and produced infectious virus in a variety of tissues including spleen, liver, kidney, lymph nodes, heart, thyroid, turbinates, and cerebellum (126). We speculated that during intranasal and subcutaneous/intradermal RVFV inoculations, the virus may follow different pathways to reach the bloodstream (117). This led us to hypothesize that combining these three routes could produce an additive effect and increase viremia. However, when cattle were infected using the intranasal, intradermal, and subcutaneous inoculation routes at the same time, this method produced less viremia than using each route individually. All three routes of infection all produced viremia in all animals as well as mild but observable clinical signs such as fever, a depressed disposition, and a lessened appetite in some animals (Supplementary Figure 1). Viral RNA was detected in nasal swabs but no infectious virus was present (126).
In a third study, Warimwe et al. challenged 4–6 month-old Holstein-Friesian cattle with 107 pfu RVFV 56/74IN subcutaneously. Similar to the experiments performed at NCFAD and KSU, control cattle developed fever and viremia, with peak viremia levels of 105 relative pfu (115).
A summary of the discussed cattle models can be found in Table 4.
Deer
The role of wildlife as maintenance hosts has been and continues to be a concern in endemic regions in Africa and the Arabian Peninsula (43, 46), and is also of critical significance if the RVFV emerges in other, previously non-endemic regions. To predict the potential of North American wildlife to act as RVFV maintenance hosts, a panel of available wildlife-based cell lines were assessed for RVFV susceptibility (42). Cells derived from white-tailed deer (WTD, Odocoileus virginianus), an important wildlife species in North America, were found to be susceptible to RVFV infection. The abundance and wide distribution of WTD in North America and their known susceptibility to other vector-borne diseases is a serious concern (127–129). Risk models for RVFV have also addressed the issue of the potential role that WTD could play if RVFV were introduced to North America (130–133). To address this concern, a group of young, farm-reared WTD were experimentally infected with 106 pfu of the Ken06 RVFV strain at the KSU BSL-3Ag facility using specially designed and constructed pens. Surprisingly, WTD were found to be highly susceptible to RVFV infection with lethality in two of the four animals after subcutaneous inoculation. A sentinel contact control animal, which was co-housed with the principally infected deer also became RVFV infected and had to be humanely euthanized due to severe clinical signs. All dead/euthanized animals had severe clinical signs including bloody diarrhea, which most likely caused the transmission of the virus via the oronasal route to the uninfected contact control animal (134).
Overview on Factors Influencing RVFV Infection in Ruminants
(a) Age: The age of the animal is arguably one of the most important parameters to consider in a RVFV challenge model. All young ruminants (<3 months) are highly susceptible to RVFV infection and typically succumb to acute liver failure (89, 135–137). Recent studies at KSU and NCFAD have opted to develop challenge models in animals old enough to be weaned (4–6 months) due to the logistics of working in high containment (112, 113, 117, 125, 126). However, numerous vaccine studies have also successfully used younger animals at 2–3 months of age (104) as well as pregnant ewes to induce protective immunity (138).
(b) Isolate and passage history: Experiments at CFIA used a low passage ZH-501 strain kindly provided by Stuart Nichol, Centers for Disease Control, Atlanta, GA as well as a human isolate from the Kenya 2006/7 outbreak provided by Health Canada. At KSU, a mosquito isolate (SA01-1322) from the Saudi Arabia outbreak in 2001 was provided by Barry Miller CDC Fort Collins, CO through Richard Bowen Colorado state university and the Kenya 2006 strain was also a mosquito isolate (13); both isolates were propagated twice in Vero cells and twice in on mosquito C6/36 cells (8).
South African researchers have used two other strains of RVFV in a vaccine efficacy trial (82). The first RVFV strain was Buffalo/99/MB/CER, isolated from an aborted fetus from an outbreak in 1998, and the second strain was the reference strain RVF 35-74, isolated from a sick sheep from an outbreak in 1974. Both virus strains were isolated using intra-cranial inoculation of mice plus one passage in BHK cells. Subcutaneous infection of sheep with 106 pfu of the Zimbabwean strain of RVF produced viremia by 4 days post-infection (dpi) and caused transient fever, viraemia, leucopaenia, relative thrombocytopaenia, haemoconcentration and raised serum enzyme levels that indicated the development of necrotic hepatitis and virulence (139).
In another study evaluating an adenovirus-based vaccine in Kenya, researchers used the RVF 56/74IN strain propagated in C6/36 cells and purified before challenge. This virus strain caused clinical disease and viremia following subcutaneous inoculation of a rather high dose of 107 pfu per animal (115). In addition, a variety of field isolates have been compared in sheep including RVFV strains 56/74, 252/75, AN-1830 and AR-20368 (107), 1678/78 and Lunyo (139) and Zinga (108).
Overall, there are very few studies that directly compare different RVFV isolates to each other and the question has been raised of whether RVFV virulence is increasing (23). Although the genetic variation among strains of RVFV is very small (≤ %5), there are still clear genetic lineages and distinct clades from outbreaks (140– 143). Because RVFV appears to circulate between vectors and naïve animals during the inter-epidemic periods (81), which could affect virus genetic population variation, it would also be beneficial to understand what effect this has on the virus' virulence. Faburay's study demonstrated distinct virulence between two outbreak isolates in livestock that suggest that Ken06 has increased virulence over SA01. Egyptian RVFV strains were shown to be almost ten-fold more virulent than sub-Saharan African strains in rats (144). Differences ranging between 50 and 90% mortality were also demonstrated in a mouse model (143). Studies are needed to confirm that these phenotypic differences are also observed in target livestock species and if genetic characteristics could be correlated.
(c) Cell line: Perhaps one of the most intriguing aspects of arbovirus infections is that the virus's pathogenicity can be changed depending on whether the inoculum is produced in a mammalian or insect host cell. This phenomenon was first characterized in vitro for alphaviruses (145) and then also for RVFV (146); importantly, we were able to demonstrate that these source effects also apply to RVFV infections in vivo (112). In addition, we could show that RVFV which is grown in mosquito cells incorporates the viral P78 protein into its virions, i.e., P78 is a structural protein of RFV viruses produced in insect cells. In contrast, P78 is not found in the virion when the virus is grown in mammalian cells (58). We proposed that the p78 present in virions of mosquito-grown viruses may function as a type I interferon antagonist, which may allow for a productive infection of initial target cells (58), as was shown earlier for alphaviruses (145).
(d) Route of inoculation: In addition to the experimental infections performed at NCFAD and KSU, other studies have shown that viremia can be induced by a wide variety of different routes including intramuscular (IM), intravenous (IV), intraperitoneal (IP), intracerebral (IC), subcutaneous (SQ), conjunctival, and oral inoculations (112, 137, 147–149). Subcutaneous injection consistently produced clinical responses and is easy to administer under BSL-3Ag conditions thus is a common method of administration (113, 125).
Future Directions and Unanswered questions
In the field, the infecting dose of RVFV is widely variable ranging from a single mosquito bite which may contain a low level of infectious virions to animals being fed on repeatedly by numerous RVFV-infected mosquitoes, potentially resulting in inoculation with high levels of infectious virions. Understanding the minimal infectious dose required for infection in ruminants and humans is currently an area requiring further investigation. In addition, it is not well-understood what the effect of mosquito saliva has on in vivo RVFV infection or pathogenesis, especially in ruminants. In containment and field studies, inoculations such as subcutaneous injections are used to mimic a mosquito bite; however, the differences between a natural infection and a subcutaneous (or intradermal) injection are not well-characterized.
Moreover, it has recently been shown that goats (117) and cattle (126) produce robust viremia when experimentally inoculated through the intranasal route. This is not necessarily unexpected since humans can be infected by inhaling aerosols produced during animal slaughtering of infected livestock (91), but the differences between an intranasal and subcutaneous infection are not well-understood. While intranasal RVFV infection can produce severe encephalitis in rodents (102), NHPs (150) and people, it did not create any neurological disease in goats (117). However, the neurological effects of intranasal infection in cattle are still unknown, as the study was terminated at peak infection at 4 dpi. Therefore, it would be interesting to also characterize the intranasal infection in cattle over a longer period of time.
The transmission of RVFV in livestock in the absence of mosquitoes is also not fully understood and there have been conflicting reports. Although it was demonstrated in sheep that transmission could occur through contact exposure (98, 109), more recent studies have not demonstrated transmission from subcutaneously infected lambs to naïve or immunosuppressed lambs (105). One possible explanation for these conflicting results is that transmission between animals requires a minimum virus dose which likely varies between different virus strains. Alternatively, upper respiratory infections with parainfluenza 3 virus, adenoviruses, reoviruses, infectious bovine rhinotreacheitis virus, maedi-visna virus, sheeppox virus, goatpox virus, peste des petits ruminants virus or Mycoplasma spp. could cause perturbations in the nasal mucosa which could possibly enhance transmission efficiency in the field but are usually absent in laboratory experiments. The potential role of urine in transmission or RVFV has recently been highlighted by a study that isolated RVFV from the urine of an infected person (151), and it is possible that milk may serve as a source of RVFV transmission (152) to animal offspring and human consumers; both of these areas require further investigation. Mosquito transmission has been considered the primary route of exposure for livestock and wildlife, but not for humans. Additional investigations of alternative routes of exposure will provide further insights into the infectability of different RVFV strains and might allow correlation of phenotype with genotype.
The selection of mosquito cell line propagated virus for livestock inoculation studies at KSU was based on the observation of more consistent viremia in our early studies. The importance of the p78 protein in the insect vs mammalian hosts has been reported (57, 58, 60) but mechanistic understanding of how this might affect virulence in the vertebrate host has not been determined yet. Studies are also needed to examine whether the individual host animal or cell selects for specific genotypes, and how that might affect viral maintenance and virulence in both the vertebrate and invertebrate host. For example, the basis of the increased virulence of RVFV in recent outbreaks is yet unknown. So far, Sanger sequencing of many RVFV isolates has demonstrated a surprisingly high stability of RVFV (140, 142) however, there are no studies on the quasi-species variation of RVFV within a specific virus population either over a period of several days in a target animal or during and after several passages in the same or different animals. Such information would be important to understand the relative fitness and overall replication ability of RVF viruses.
It was recently determined that there is low level transmission during the inter-epidemic period (81); whether this is the only mechanism of viral maintenance is not clear yet. Also, how low level transmission restricts viral evolution is not known. Similarly, there is empirical evidence that various animal breeds have different susceptibilities to RVFV infection. However, well-designed controlled studies are needed to substantiate this observation. If confirmed, this could change husbandry techniques in RVFV endemic areas, and not only improve animal health but also have a significant effect on public health.
Conclusion
The renewed interest in RVFV since the 2006/7 outbreak in Kenya has resulted in many advances in our basic knowledge about RVFV replication strategies and molecular pathogenesis in small animal and livestock models. It also has resulted in novel vaccine candidates and novel experimental challenge models as discussed in this review. In addition, novel tools for the detection of viral nucleic acids and antibodies, both for laboratory and point-of need use have been developed. These recent advances in RVFV mitigation strategies will allow a more rapid and effective control of the disease; unfortunately, the availability of these tools in endemic areas is rather limited (84). There are still many questions about the mechanisms and factors affecting viral maintenance and virulence. The models described here provide a good basis for developing studies to investigate these factors. There are still many questions to be addressed in RVF biology and epidemiology as discussed above in this review. We hope that the RVFV livestock models described here in detail will provide a sound basis for the design of studies to investigate these yet unknown questions.
Author Contributions
WW, JR, and AK conceived the review topic. AK and WW prepared and wrote the manuscript. JR, SB, and BP critically reviewed the manuscript.
Funding
NBAF Transition Funds from the State of Kansas. DHS Grant Award Number: DHS-2010-ST-061-AG0001. USDA-ARS CRIS Project 3020-3200-009-00D.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2020.00238/full#supplementary-material
References
1. Gubler DJ. The global emergence/resurgence of arboviral diseases as public health problems. Arch Med Res. (2002) 33:330–42. doi: 10.1016/S0188-4409(02)00378-8
2. Bonnet P, Tibbo M, Workalemahu A, Gau M. Rift Valley Fever - an Emerging Threat to Livestock Trade and Food Secruity in the Horn of Africa: a Review. Ethiopian Society of Animal Production. (2001).
3. Chevalier V, Rakotondrafara T, Jourdan M, Heraud JM, Andriamanivo HR, Durand B, et al. An unexpected recurrent transmission of Rift Valley fever virus in cattle in a temperate and mountainous area of Madagascar. PLoS Negl Trop Dis. (2011) 5:e1423. doi: 10.1371/journal.pntd.0001423
4. Rolin AI, Berrang-Ford L, Kulkarni MA. The risk of Rift Valley fever virus introduction and establishment in the United States and European Union. Emerg Microbes Infect. (2013) 2:e81. doi: 10.1038/emi.2013.81
5. Daubney R, Hudson JR, Garnham PC. Enzoonotic hepatitis or rift valley fever. An undescribed virus disease of sheep, cattle and man from east africa. J Pathol Bacteriol. (1931) 34:545–79. doi: 10.1002/path.1700340418
6. Meegan JM. The Rift Valley fever epizootic in Egypt 1977-78. 1. Description of the epizzotic and virological studies. Trans R Soc Trop Med Hyg. (1979) 73:618–23. doi: 10.1016/0035-9203(79)90004-X
7. Siam AL, Meegan JM, Gharbawi KF. Rift Valley fever ocular manifestations: observations during the 1977 epidemic in Egypt. Br J Ophthalmol. (1980) 64:366–74. doi: 10.1136/bjo.64.5.366
8. Miller BR, Godsey MS, Crabtree MB, Savage HM, Al-Mazrao Y, Al-Jeffri MH, et al. Isolation and genetic characterization of Rift Valley fever virus from Aedes vexans arabiensis, Kingdom of Saudi Arabia. Emerg Infect Dis. (2002) 8:1492–4. doi: 10.3201/eid0812.020194
9. Faye O, Diallo M, Diop D, Bezeid OE, Ba H, Niang M, et al. Rift Valley fever outbreak with East-Central African virus lineage in Mauritania, 2003. Emerg Infect Dis. (2007) 13:1016–23. doi: 10.3201/eid1307.061487
10. Hassan OA, Ahlm C, Sang R, Evander M. The Rift Valley fever outbreak in Sudan. PLoS Negl Trop Dis. (2007) 5:e1229. doi: 10.1371/journal.pntd.0001229
11. Jost CC, Nzietchueng S, Kihu S, Bett B, Njogu G, Swai ES, et al. Epidemiological assessment of the Rift Valley fever outbreak in Kenya and Tanzania in 2006 and 2007. Am J Trop Med Hyg. (2010) 83:65–72. doi: 10.4269/ajtmh.2010.09-0290
12. Munyua P, Murithi RM, Wainwright S, Githinji J, Hightower A, Mutonga D, et al. Rift Valley fever outbreak in livestock in Kenya, 2006-2007. Am J Trop Med Hyg. (2010) 83:58–64. doi: 10.4269/ajtmh.2010.09-0292
13. Sang R, Kioko E, Lutomiah J, Warigia M, Ochieng C, O'Guinn M, et al. Rift Valley fever virus epidemic in Kenya, 2006/2007: the entomologic investigations. Am J Trop Med Hyg. (2010) 83:28–37. doi: 10.4269/ajtmh.2010.09-0319
14. El Mamy AB, Baba MO, Barry Y, Isselmou K, Dia ML, El Kory MO, et al. Unexpected Rift Valley fever outbreak, northern Mauritania. Emerg Infect Dis. (2011) 17:1894–6. doi: 10.3201/eid1710.110397
15. Monaco F, Pinoni C, Cosseddu GM, Khaiseb S, Calistri P, Molini U, et al. Rift Valley fever in Namibia, 2010. Emerg Infect Dis. (2013) 19:2025–7. doi: 10.3201/eid1912.130593
16. Archer BN, Weyer J, Paweska J, Nkosi D, Leman P, Tint KS, et al. Outbreak of Rift Valley fever affecting veterinarians and farmers in South Africa, 2008. S Afr Med J. (2011) 101:263–6. doi: 10.7196/SAMJ.4544
17. Fafetine JM, Coetzee P, Mubemba B, Nhambirre O, Neves L, Coetzer JA, et al. Rift valley fever outbreak in livestock, Mozambique, 2014. Emerg Infect Dis. (2016) 22:2165–67. doi: 10.3201/eid2212.160310
18. Lagare A, Fall G, Ibrahim A, Ousmane S, Sadio B, Abdoulaye M, et al. First occurrence of Rift Valley fever outbreak in Niger, 2016. Vet Med Sci. (2019) 5:70–78. doi: 10.1002/vms3.135
19. Andayi F, Charrel RN, Kieffer A, Richet H, Pastorino B, Leparc-Goffart I, et al. A sero-epidemiological study of arboviral fevers in Djibouti, Horn of Africa. PLoS Negl Trop Dis. (2014) 8:e3299. doi: 10.1371/journal.pntd.0003299
20. Nanyingi MO, Munyua P, Kiama SG, Muchemi GM, Thumbi SM, Bitek AO, et al. A systematic review of Rift Valley Fever epidemiology 1931-2014. Infect Ecol Epidemiol. (2015) 5:28024. doi: 10.3402/iee.v5.28024
21. Dar O, Hogarth S, McIntyre S. Tempering the risk: Rift Valley fever and bioterrorism. Trop Med Int Health. (2013) 18:1036–41. doi: 10.1111/tmi.12108
22. Mandell RB, Flick R. Rift Valley fever virus: an unrecognized emerging threat?. Hum Vaccin. (2010) 6:597–601. doi: 10.4161/hv.6.7.11761
23. Baba M, Masiga DK, Sang R, Villinger J. Has Rift Valley fever virus evolved with increasing severity in human populations in East Africa? Emerg Microbes Infect. (2016) 5:e58. doi: 10.1038/emi.2016.57
24. Bird BH, Nichol ST. Breaking the chain: Rift Valley fever virus control via livestock vaccination. Curr Opin Virol. (2012) 2:315–23. doi: 10.1016/j.coviro.2012.02.017
25. Faburay B. The case for a 'one health' approach to combating vector-borne diseases. Infect Ecol Epidemiol. (2015) 5:28132. doi: 10.3402/iee.v5.28132
26. Chevalier V, Pepin M, Plee L, Lancelot R. Rift Valley fever–a threat for Europe? Euro Surveill. (2010) 15:19506. doi: 10.2807/ese.15.10.19506-en
27. Kortekaas J. One Health approach to Rift Valley fever vaccine development. Antiviral Res. (2014) 106:24–32. doi: 10.1016/j.antiviral.2014.03.008
28. Linthicum KJ, Davies FG, Kairo A, Bailey CL. Rift Valley fever virus (family Bunyaviridae, genus Phlebovirus). Isolations from Diptera collected during an inter-epizootic period in Kenya. J Hyg (Lond). (1985) 95:197–209. doi: 10.1017/S0022172400062434
29. Linthicum KJ, Britch SC, Anyamba A. Rift Valley Fever: an emerging mosquito-borne disease. Annu Rev Entomol. (2016) 61:395–415. doi: 10.1146/annurev-ento-010715-023819
30. Bergren NA, Kading RC. The Ecological Significance and Implications of Transovarial Transmission among the Vector-Borne Bunyaviruses: a review. Insects. (2018) 9:173. doi: 10.3390/insects9040173
31. Mwaengo D, Lorenzo G, Iglesias J, Warigia M, Sang R, Bishop RP, et al. Detection and identification of Rift Valley fever virus in mosquito vectors by quantitative real-time PCR. Virus Res. (2012) 169:137–43. doi: 10.1016/j.virusres.2012.07.019
32. Gargan T. P. 2nd, Clark GG, Dohm DJ, Turell MJ, Bailey CL. Vector potential of selected North American mosquito species for Rift Valley fever virus. Am J Trop Med Hyg. (1988) 38:440–6. doi: 10.4269/ajtmh.1988.38.440
33. Turell MJ, Dohm DJ, Geden CJ, Hogsette JA, Linthicum KJ. Potential for stable flies and house flies (Diptera: Muscidae) to transmit Rift Valley fever virus. J Am Mosq Control Assoc. (2010) 26:445–8. doi: 10.2987/10-6070.1
34. Turell MJ, Wilson WC, Bennett K. E. Potential for North American mosquitoes (Diptera: Culicidae) to transmit rift valley fever virus. J Med Entomol. (2010) 47:884–9. doi: 10.1093/jmedent/47.5.884
35. Balkema-Buschmann A, Rissmann M, Kley N, Ulrich R, Eiden M, Groschup MH. Productive Propagation of Rift Valley Fever Phlebovirus Vaccine Strain MP-12 in Rousettus aegyptiacus Fruit Bats. Viruses. (2018) 10:681. doi: 10.3390/v10120681
36. Imam IZ, El-Karamany R, Darwish MA. An epidemic of Rift Valley fever in Egypt. 2. Isolation of the virus from animals. Bull World Health Organ. (1979) 57:441–3.
37. Kading RC, Kityo RM, Mossel EC, Borland EM, Nakayiki T, Nalikka B, et al. Neutralizing antibodies against flaviviruses, Babanki virus, and Rift Valley fever virus in Ugandan bats. Infect Ecol Epidemiol. (2018) 8:1439215. doi: 10.1080/20008686.2018.1439215
38. Oelofsen MJ, Van der Ryst E. Could bats act as reservoir hosts for Rift Valley fever virus? Onderstepoort J Vet Res. (1999) 66:51–4.
39. Swanepoel R, Blackburn NK, Efstratiou S, Condy JB. Studies on Rift Valley fever in some African murids (Rodentia: Muridae). J Hyg (Lond). (1978) 80:183–96. doi: 10.1017/S0022172400053535
40. Youssef BZ, Donia HA. The potential role of Rattus rattus in enzootic cycle of Rift Valley Fever in Egypt. 1-Detection of RVF antibodies in R. rattus blood samples by both enzyme linked immuno sorbent assay (ELISA) and immuno-diffusion technique (ID). J Egypt Public Health Assoc. (2001) 76:431–41.
41. Beechler BR, Bengis R, Swanepoel R, Paweska JT, Kemp A, van Vuren PJ, et al. Rift valley Fever in Kruger national park: do buffalo play a role in the inter-epidemic circulation of virus? Transbound Emerg Dis. (2015) 62:24–32. doi: 10.1111/tbed.12197
42. Gaudreault NN, Indran SV, Bryant PK, Richt JA, Wilson WC. Comparison of Rift Valley fever virus replication in North American livestock and wildlife cell lines. Front Microbiol. (2015) 6:664. doi: 10.3389/fmicb.2015.00664
43. Olive MM, Goodman SM, Reynes JM. The role of wild mammals in the maintenance of Rift Valley fever virus. J Wildl Dis. (2012) 48:241–66. doi: 10.7589/0090-3558-48.2.241
44. Rostal MK, Liang JE, Zimmermann D, Bengis R, Paweska J, Karesh WB. Rift Valley Fever: does wildlife play a role? ILAR J. (2017) 58:359–70. doi: 10.1093/ilar/ilx023
45. Walsh MG, Mor SM. Interspecific network centrality, host range and early-life development are associated with wildlife hosts of Rift Valley fever virus. Transbound Emerg Dis. (2018) 65:1568–75. doi: 10.1111/tbed.12903
46. Britch SC, Binepal YS, Ruder MG, Kariithi HM, Linthicum KJ, Anyamba A, et al. Rift Valley fever risk map model and seroprevalence in selected wild ungulates and camels from Kenya. PLoS ONE. (2013) 8:e66626. doi: 10.1371/journal.pone.0066626
47. Muller R, Saluzzo JF, Lopez N, Dreier T, Turell M, Smith J, et al. Characterization of clone 13, a naturally attenuated avirulent isolate of Rift Valley fever virus, which is altered in the small segment. Am J Trop Med Hyg. (1995) 53:405–11. doi: 10.4269/ajtmh.1995.53.405
48. Collett M. S. Messenger RNA of the M segment RNA of Rift Valley fever virus. Virology. (1986) 151:151–6. doi: 10.1016/0042-6822(86)90114-5
49. Kakach LT, Suzich JA, Collett MS. Rift Valley fever virus M segment: phlebovirus expression strategy and protein glycosylation. Virology. (1989) 170:505–10. doi: 10.1016/0042-6822(89)90442-X
50. Suzich JA, Collett MS. Rift Valley fever virus M segment: cell-free transcription and translation of virus-complementary RNA. Virology. (1988) 164:478–86. doi: 10.1016/0042-6822(88)90562-4
51. Suzich JA, Kakach LT, Collett MS. Expression strategy of a phlebovirus: biogenesis of proteins from the Rift Valley fever virus M segment. J Virol. (1990) 64:1549–55. doi: 10.1128/JVI.64.4.1549-1555.1990
52. Huiskonen JT, Overby AK, Weber F, Grunewald K. Electron cryo-microscopy and single-particle averaging of Rift Valley fever virus: evidence for GN-GC glycoprotein heterodimers. J Virol. (2009) 83:3762–9. doi: 10.1128/JVI.02483-08
53. Lozach PY, Kuhbacher A, Meier R, Mancini R, Bitto D, Bouloy M, et al. DC-SIGN as a receptor for phleboviruses. Cell Host Microbe. (2011) 10:75–88. doi: 10.1016/j.chom.2011.06.007
54. Riblett AM, Blomen VA, Jae LT, Altamura LA, Doms RW, Brummelkamp TR, et al. A haploid genetic screen identifies heparan sulfate proteoglycans supporting Rift Valley Fever Virus infection. J Virol. (2016) 90:1414–23. doi: 10.1128/JVI.02055-15
55. Won S, Ikegami T, Peters CJ, Makino S. NSm protein of Rift Valley fever virus suppresses virus-induced apoptosis. J Virol. (2007) 81:13335–45. doi: 10.1128/JVI.01238-07
56. Bird BH, Albarino CG, Nichol ST. Rift Valley fever virus lacking NSm proteins retains high virulence in vivo and may provide a model of human delayed onset neurologic disease. Virology. (2007) 362:10–5. doi: 10.1016/j.virol.2007.01.046
57. Kreher F, Tamietti C, Gommet C, Guillemot L, Ermonval M, Failloux AB, et al. The Rift Valley fever accessory proteins NSm and P78/NSm-GN are distinct determinants of virus propagation in vertebrate and invertebrate hosts. Emerg Microbes Infect. (2014) 3:e71. doi: 10.1038/emi.2014.71
58. Weingartl HM, Zhang S, Marszal P, McGreevy A, Burton L, Wilson WC. Rift Valley fever virus incorporates the 78 kDa glycoprotein into virions matured in mosquito C6/36 cells. PLoS ONE. (2014) 9:e87385. doi: 10.1371/journal.pone.0087385
59. Crabtree MB, Kent Crockett RJ, Bird BH, Nichol ST, Erickson BR, Biggerstaff BJ, et al. Infection and transmission of Rift Valley fever viruses lacking the NSs and/or NSm genes in mosquitoes: potential role for NSm in mosquito infection. PLoS Negl Trop Dis. (2012) 6:e1639. doi: 10.1371/journal.pntd.0001639
60. Kading RC, Crabtree MB, Bird BH, Nichol ST, Erickson BR, Horiuchi K, et al. Deletion of the NSm virulence gene of Rift Valley fever virus inhibits virus replication in and dissemination from the midgut of Aedes aegypti mosquitoes. PLoS Negl Trop Dis. (2014) 8:e2670. doi: 10.1371/journal.pntd.0002670
61. Vialat P, Billecocq A, Kohl A, Bouloy M. The S segment of rift valley fever phlebovirus (Bunyaviridae) carries determinants for attenuation and virulence in mice. J Virol. (2000) 74:1538–43. doi: 10.1128/JVI.74.3.1538-1543.2000
62. Le May N, Gauliard N, Billecocq A, Bouloy M. The N terminus of Rift Valley fever virus nucleoprotein is essential for dimerization. J Virol. (2005) 79:11974–80. doi: 10.1128/JVI.79.18.11974-11980.2005
63. Jansen van Vuren P, Paweska JT. Laboratory safe detection of nucleocapsid protein of Rift Valley fever virus in human and animal specimens by a sandwich ELISA. J Virol Methods. (2009) 157:15–24. doi: 10.1016/j.jviromet.2008.12.003
64. Billecocq A, Spiegel M, Vialat P, Kohl A, Weber F, Bouloy M, et al. NSs protein of Rift Valley fever virus blocks interferon production by inhibiting host gene transcription. J Virol. (2004) 78:9798–9806. doi: 10.1128/JVI.78.18.9798-9806.2004
65. Habjan M, Pichlmair A, Elliott RM, Overby A. K., Glatter T, Gstaiger M, et al. NSs protein of rift valley fever virus induces the specific degradation of the double-stranded RNA-dependent protein kinase. J Virol. (2009) 83:4365–75. doi: 10.1128/JVI.02148-08
66. Ikegami T, Narayanan K, Won S, Kamitani W, Peters CJ, Makino S. Dual functions of Rift Valley fever virus NSs protein: inhibition of host mRNA transcription and post-transcriptional downregulation of protein kinase PKR. Ann N Y Acad Sci. (2009) 1171(Suppl. 1):E75–85. doi: 10.1111/j.1749-6632.2009.05054.x
67. Ikegami T, Peters CJ, Makino S. Rift valley fever virus nonstructural protein NSs promotes viral RNA replication and transcription in a minigenome system. J Virol. (2005) 79:5606–15. doi: 10.1128/JVI.79.9.5606-5615.2005
68. Bird BH, Albarino CG, Hartman AL, Erickson BR, Ksiazek TG, Nichol ST. Rift valley fever virus lacking the NSs and NSm genes is highly attenuated, confers protective immunity from virulent virus challenge, and allows for differential identification of infected and vaccinated animals. J Virol. (2008) 82:2681–91. doi: 10.1128/JVI.02501-07
69. Bird BH, Maartens LH, Campbell S, Erasmus BJ, Erickson BR, Dodd KA, et al. Rift Valley fever virus vaccine lacking the NSs and NSm genes is safe, nonteratogenic, and confers protection from viremia, pyrexia, and abortion following challenge in adult and pregnant sheep. J Virol. (2011) 85:12901–9. doi: 10.1128/JVI.06046-11
70. Hightower A, Kinkade C, Nguku PM, Anyangu A, Mutonga D, Omolo J, et al. Relationship of climate, geography, and geology to the incidence of Rift Valley fever in Kenya during the 2006-2007 outbreak. Am J Trop Med Hyg. (2012) 86:373–80. doi: 10.4269/ajtmh.2012.11-0450
71. Drolet BS, Weingartl HM, Jiang J, Neufeld J, Marszal P, Lindsay R, et al. Development and evaluation of one-step rRT-PCR and immunohistochemical methods for detection of Rift Valley fever virus in biosafety level 2 diagnostic laboratories. J Virol Methods. (2012) 179:373–82. doi: 10.1016/j.jviromet.2011.11.025
72. Turell M, Dave K, Mayda M, Parker Z, Coleman R, Dave S, et al. Wicking assay for the rapid detection of Rift Valley fever viral antigens in mosquitoes (Diptera: Culicidae). J Med Entomol. (2011) 48:628–33. doi: 10.1603/ME10219
73. van Vuren PJ, Paweska JT. Comparison of enzyme-linked immunosorbent assay-based techniques for the detection of antibody to Rift Valley fever virus in thermochemically inactivated sheep sera. Vector Borne Zoonotic Dis. (2010) 10:697–9. doi: 10.1089/vbz.2009.0213
74. Wilson WC, Romito M, Jasperson DC, Weingartl H, Binepal YS, Maluleke MR, et al. Development of a Rift Valley fever real-time RT-PCR assay that can detect all three genome segments. J Virol Methods. (2013) 193:426–31. doi: 10.1016/j.jviromet.2013.07.006
75. Wilson WC, Weingartl HM, Drolet BS, Dave K, Harpster MH, Johnson P. A, et al. Diagnostic approaches for Rift Valley fever. Dev Biol (Basel). (2013) 135:73–8. doi: 10.1159/000276828
76. Anyamba A, Linthicum KJ, Small J, Britch SC, Pak ES, et al. Prediction, assessment of the Rift Valley fever activity in East and Southern Africa 2006-2008 and possible vector control strategies. Am J Trop Med Hyg. (2010) 83:43–51. doi: 10.4269/ajtmh.2010.09-0289
77. Gaff HD, Gross LJ. Modeling tick-borne disease: a metapopulation model. Bull Math Biol. (2007) 69:265–88. doi: 10.1007/s11538-006-9125-5
78. Xue L, Cohnstaedt LW, Scott HM, Scoglio C. A hierarchical network approach for modeling Rift Valley fever epidemics with applications in North America. PLoS ONE. (2013) 8:e62049. doi: 10.1371/journal.pone.0062049
79. Xue L, Scott HM, Cohnstaedt LW, Scoglio C. A network-based meta-population approach to model Rift Valley fever epidemics. J Theor Biol. (2012) 306:129–44. doi: 10.1016/j.jtbi.2012.04.029
80. LaBeaud AD, Ochiai Y, Peters CJ, Muchiri EM, King CH. Spectrum of Rift Valley fever virus transmission in Kenya: insights from three distinct regions. Am J Trop Med Hyg. (2007) 76:795–800. doi: 10.4269/ajtmh.2007.76.795
81. Lichoti JK, Kihara A, Oriko AA, Okutoyi LA, Wauna JO, Tchouassi DP, et al. Detection of rift valley Fever virus interepidemic activity in some hotspot areas of kenya by sentinel animal surveillance, 2009-2012. Vet Med Int. (2014) 2014:379010. doi: 10.1155/2014/379010
82. Dungu B, Louw I, Lubisi AP, Hunter von Teichman BF, Bouloy M. Evaluation of the efficacy and safety of the Rift Valley Fever Clone 13 vaccine in sheep. Vaccine. (2010) 28:4581–7. doi: 10.1016/j.vaccine.2010.04.085
83. von Teichman B, Engelbrecht A, Zulu G, Dungu B, Pardini A, Bouloy M. Safety and efficacy of Rift Valley fever Smithburn and Clone 13 vaccines in calves. Vaccine. (2011) 29:5771–7. doi: 10.1016/j.vaccine.2011.05.055
84. Dungu B, Lubisi BA, Ikegami T. Rift Valley fever vaccines: current and future needs. Curr Opin Virol. (2018) 29:8–15. doi: 10.1016/j.coviro.2018.02.001
85. Ikegami T. Rift Valley fever vaccines: an overview of the safety and efficacy of the live-attenuated MP-12 vaccine candidate. Expert Rev Vaccines. (2017) 16:601–11. doi: 10.1080/14760584.2017.1321482
86. Mansfield KL, Banyard AC, McElhinney L, Johnson N, Horton DL, Hernandez-Triana LM, et al. Rift Valley fever virus: A review of diagnosis and vaccination, and implications for emergence in Europe. Vaccine. (2015) 33:5520–31. doi: 10.1016/j.vaccine.2015.08.020
87. Gaudreault NN, Indran SV, Balaraman V, Wilson WC, Richt JA. Molecular aspects of Rift Valley fever virus and the emergence of reassortants. Virus Genes. (2019) 55:1–11. doi: 10.1007/s11262-018-1611-y
88. Davies FG. The historical and recent impact of Rift Valley fever in Africa. Am J Trop Med Hyg. (2010) 83:73–4. doi: 10.4269/ajtmh.2010.83s2a02
89. Coetzer JA. The pathology of Rift Valley fever. I Lesions occurring in natural cases in new-born lambs. Onderstepoort J Vet Res. (1977) 44:205–11.
90. Coetzer JA. The pathology of Rift Valley fever. II. Lesions occurring in field cases in adult cattle, calves and aborted foetuses. Onderstepoort J Vet Res. (1982) 49:11–7.
91. WHO. Rift Valley Fever (2019). Available online at: https://www.who.int/emergencies/diseases/rift-valley-fever/en/
92. Nyakarahuka L, de St Maurice A, Purpura L, Ervin E, Balinandi S, Tumusiime A, et al. Prevalence and risk factors of Rift Valley fever in humans and animals from Kabale district in Southwestern Uganda, 2016. PLoS Negl Trop Dis. (2018) 12:e0006412. doi: 10.1371/journal.pntd.0006412
93. Sow A, Faye O, Ba Y, Diallo D, Fall G, Faye O, et al. Widespread Rift Valley Fever Emergence in Senegal in 2013-2014. Open Forum Infect Dis. (2016) 3:ofw149. doi: 10.1093/ofid/ofw149
94. Brand RF, Rostal MK, Kemp A, Anyamba A, Zwiegers H, Van Huyssteen CW, et al. A phytosociological analysis and description of wetland vegetation and ecological factors associated with locations of high mortality for the 2010-11 Rift Valley fever outbreak in South Africa. PLoS ONE. (2018) 13:e0191585. doi: 10.1371/journal.pone.0191585
95. Nabeth P, Kane Y, Abdalahi MO, Diallo M, Ndiaye K, Ba K, et al. Rift Valley fever outbreak, Mauritania, 1998: seroepidemiologic, virologic, entomologic, zoologic investigations. Emerg Infect Dis. (2001) 7:1052–4. doi: 10.3201/eid0706.010627
96. OIE. Rift Valley Fever, South Africa (2010). Available online at: https://www.oie.int/wahis_2/public/wahid.php/Reviewreport/Review?page_refer=MapEventSummary&reportid=8967
97. Barnard BJ. Rift Valley fever vaccine–antibody and immune response in cattle to a live and an inactivated vaccine. J S Afr Vet Assoc. (1979) 50:155–7.
98. Harrington DG, Lupton HW, Crabbs CL, Peters CJ, Reynolds JA, Slone TW, et al. Evaluation of a formalin-inactivated Rift Valley fever vaccine in sheep. Am J Vet Res. (1980) 41:1559–64.
99. Morrill JC, Mebus CA, Peters CJ. Safety of a mutagen-attenuated Rift Valley fever virus vaccine in fetal and neonatal bovids. Am J Vet Res. (1997) 58:1110–4.
100. Morrill JC, Mebus CA, Peters CJ. Safety and efficacy of a mutagen-attenuated Rift Valley fever virus vaccine in cattle. Am J Vet Res. (1997) 58:1104–9.
101. Oymans J, Wichgers Schreur PJ, van Keulen L, Kant J, Kortekaas J. Rift Valley fever virus targets the maternal-foetal interface in ovine and human placentas. PLoS Negl Trop Dis. (2020) 14:e0007898. doi: 10.1371/journal.pntd.0007898
102. Ross TM, Bhardwaj N, Bissel SJ, Hartman AL, Smith DR. Animal models of Rift Valley fever virus infection. Virus Res. (2012) 163:417–23. doi: 10.1016/j.virusres.2011.10.023
103. Kortekaas J, Oreshkova N, van Keulen L, Kant J, Bosch BJ, Bouloy M, et al. Comparative efficacy of two next-generation Rift Valley fever vaccines. Vaccine. (2014) 32:4901–8. doi: 10.1016/j.vaccine.2014.07.037
104. Oreshkova N, van Keulen L, Kant J, Moormann RJ, Kortekaas J. A single vaccination with an improved nonspreading Rift Valley fever virus vaccine provides sterile immunity in lambs. PLoS One. (2013) 8:e77461.
105. Wichgers Schreur PJ, Kant J, van Keulen L, Moormann RJM, Kortekaas J. Four-segmented Rift Valley fever virus induces sterile immunity in sheep after a single vaccination. Vaccine. (2015) 33:1459–64. doi: 10.1016/j.vaccine.2015.01.077
106. Kortekaas J, Antonis AF, Kant J, Vloet RP, Vogel A, Oreshkova N, et al. Efficacy of three candidate Rift Valley fever vaccines in sheep. Vaccine. (2012) 30:3423–9. doi: 10.1016/j.vaccine.2012.03.027
107. Busquets N, Xavier F, Martin-Folgar R, Lorenzo G, Galindo-Cardiel I, del Val BP, et al. Experimental infection of young adult European breed sheep with Rift Valley fever virus field isolates. Vector Borne Zoonotic Dis. (2010) 10:689–96. doi: 10.1089/vbz.2009.0205
108. Olaleye OD, Tomori O, Fajimi JL, Schmitz H. Experimental infection of three Nigerian breeds of sheep with the Zinga strain of the Rift Valley Fever virus. Rev Elev Med Vet Pays Trop. (1996) 49:6–16.
109. Busquets N, Lorenzo G, Lopez-Gil E, Rivas R, Solanes D, Galindo-Cardiel I, et al. Efficacy assessment of an MVA vectored Rift Valley Fever vaccine in lambs. Antiviral Res. (2014) 108:165–172. doi: 10.1016/j.antiviral.2014.05.020
110. Lorenzo G, Lopez-Gil E, Ortego J, Brun A. Efficacy of different DNA and MVA prime-boost vaccination regimens against a Rift Valley fever virus (RVFV) challenge in sheep 12 weeks following vaccination. Vet Res. (2018) 49:21. doi: 10.1186/s13567-018-0516-z
111. Chrun T, Lacote S, Urien C, Jouneau L, Barc C, Bouguyon E, et al. A Rift Valley fever virus Gn ectodomain-based DNA vaccine induces a partial protection not improved by APC targeting. NPJ Vaccines. (2018) 3:14. doi: 10.1038/s41541-018-0052-x
112. Weingartl HM, Miller M, Nfon C, Wilson WC. Development of a Rift Valley fever virus viremia challenge model in sheep and goats. Vaccine. (2014) 32:2337–44. doi: 10.1016/j.vaccine.2014.02.066
113. Faburay B, Gaudreault NN, Liu Q, Davis AS, Shivanna V, Sunwoo SY, et al. Development of a sheep challenge model for Rift Valley fever. Virology. (2016) 489:128–40. doi: 10.1016/j.virol.2015.12.003
114. Nguku PM, Sharif SK, Mutonga D, Amwayi S, Omolo J, Mohammed O, et al. An investigation of a major outbreak of Rift Valley fever in Kenya: 2006-2007. Am J Trop Med Hyg. (2010) 83:5–13. doi: 10.4269/ajtmh.2010.09-0288
115. Warimwe GM, Gesharisha J, Carr BV, Otieno S, Otingah K, Wright D, et al. Chimpanzee adenovirus vaccine provides multispecies protection against Rift Valley Fever. Sci Rep. (2016) 6:20617. doi: 10.1038/srep20617
116. Nfon CK, Marszal P, Zhang S, Weingartl HM. Innate immune response to Rift Valley fever virus in goats. PLoS Negl Trop Dis. (2012) 6:e1623. doi: 10.1371/journal.pntd.0001623
117. Kroeker AL, Smid V, Embury-Hyatt C, Moffat E, Collignon B, Lung O, et al. RVFV Infection in Goats by Different Routes of Inoculation. Viruses. (2018) 10. doi: 10.20944/preprints201811.0022.v1
118. Conway MJ, Watson AM, Colpitts TM, Dragovic SM, Li Z, Wang P, et al. Mosquito saliva serine protease enhances dissemination of dengue virus into the mammalian host. J Virol. (2014) 88:164–75. doi: 10.1128/JVI.02235-13
119. Le Coupanec A, Babin D, Fiette L, Jouvion G, Ave P, Misse D, et al. Aedes mosquito saliva modulates Rift Valley fever virus pathogenicity. PLoS Negl Trop Dis. (2013) 7:e2237. doi: 10.1371/journal.pntd.0002237
120. Pingen M, Bryden SR, Pondeville E, Schnettler E, Kohl A, Merits A, et al. Host inflammatory response to mosquito bites enhances the severity of arbovirus infection. Immunity. (2016) 44:1455–69. doi: 10.1016/j.immuni.2016.06.002
121. Pingen M, Schmid MA, Harris E, McKimmie CS. Mosquito biting modulates skin response to virus infection. Trends Parasitol. (2017) 33:645–57. doi: 10.1016/j.pt.2017.04.003
122. Schmid MA, Glasner DR, Shah S, Michlmayr D, Kramer LD, Harris E. Mosquito saliva increases endothelial permeability in the skin, immune cell migration, and dengue pathogenesis during antibody-dependent enhancement. PLoS Pathog. (2016) 12:e1005676. doi: 10.1371/journal.ppat.1005676
123. Wichit S, Diop F, Hamel R, Talignani L, Ferraris P, Cornelie S, et al. Aedes Aegypti saliva enhances chikungunya virus replication in human skin fibroblasts via inhibition of the type I interferon signaling pathway. Infect Genet Evol. (2017) 55:68–70. doi: 10.1016/j.meegid.2017.08.032
124. Ayari-Fakhfakh E, Ghram A, Albina E, Cetre-Sossah C. Expression of cytokines following vaccination of goats with a recombinant capripoxvirus vaccine expressing Rift Valley fever virus proteins. Vet Immunol Immunopathol. (2018) 197:15–20. doi: 10.1016/j.vetimm.2018.01.001
125. Wilson WC, Davis AS, Gaudreault NN, Faburay B, Trujillo JD, Shivanna V, et al. Experimental infection of calves by two genetically-distinct strains of Rift Valley Fever Virus. Viruses. (2016) 8:145. doi: 10.3390/v8050145
126. Kroeker AL, Smid V, Embury-Hyatt C, Collignon B, Pinette M, Babiuk S, et al. Increased susceptibility of cattle to intranasal RVFV infection. Front Vet Sci. (2020). doi: 10.3389/fvets.2020.00137
127. Campagnolo ER, Tewari D, Farone TS, Livengood JL, Mason KL. Evidence of Powassan/deer tick virus in adult black-legged ticks (Ixodes scapularis) recovered from hunter-harvested white-tailed deer (Odocoileus virginianus) in Pennsylvania: a public health perspective. Zoonoses Public Health. (2018) 65:589–94. doi: 10.1111/zph.12476
128. Hollis-Etter KM, Anchor CL, Chelsvig JE, Dubey JP, Warner RE. Suburban white-tailed deer seropositive for Toxoplasma gondii from Chicago, Illinois. Parasitol Res. (2019) 118:2271–76. doi: 10.1007/s00436-019-06347-1
129. Ruder MG, Stallknecht DE, Allison AB, Mead DG, Carter DL, Howerth EW. Host and potential vector susceptibility to an emerging orbivirus in the United States: epizootic hemorrhagic disease virus serotype 6. Vet Pathol. (2016) 53:574–84. doi: 10.1177/0300985815610387
130. Kasari TR, Carr DA, Lynn TV, Weaver JT. Evaluation of pathways for release of Rift Valley fever virus into domestic ruminant livestock, ruminant wildlife, and human populations in the continental United States. J Am Vet Med Assoc. (2008) 232:514–29. doi: 10.2460/javma.232.4.514
131. Kakani S, LaBeaud AD, King CH. Planning for Rift Valley fever virus: use of geographical information systems to estimate the human health threat of white-tailed deer (Odocoileus virginianus)-related transmission. Geospat Health. (2010) 5:33–43. doi: 10.4081/gh.2010.185
132. Hartley DM, Rinderknecht JL, Nipp TL, Clarke NP, Snowder GD. Animal National Center for Foreign, and Fever Zoonotic Disease Defense Advisory Group on Rift Valley. Potential effects of Rift Valley fever in the United States. Emerg Infect Dis. (2011) 17:e1. doi: 10.3201/eid1708.101088
133. Golnar AJ, Kading RC, Hamer GL. Quantifying the potential pathways and locations of Rift Valley fever virus entry into the United States. Transbound Emerg Dis. (2018) 65:85–95. doi: 10.1111/tbed.12608
134. Wilson WC, Kim IJ, Trujillo JD, Sunwoo SY, Noronha LE, Urbaniak K, et al. Susceptibility of White-Tailed Deer to Rift Valley Fever Virus. Emerg Infect Dis. (2018) 24:1717–19. doi: 10.3201/eid2409.180265
135. Van der Lugt JJ, Coetzer JA, Smit MM. Distribution of viral antigen in tissues of new-born lambs infected with Rift Valley fever virus. Onderstepoort J Vet Res. (1996) 63:341–7.
136. Coetzer JA, Ishak KG, Calvert RC. Sequential development of the liver lesions in new-born lambs infected with Rift Valley fever virus. II Ultrastructural findings. Onderstepoort J Vet Res. (1982) 49:109–22.
137. Easterday B. C., Gavran Mh, M.c, Rooney JR, Murphy LC. The pathogenesis of Rift Valley fever in lambs. Am J Vet Res. (1962) 23:470–9.
138. Wichgers Schreur PJ, van Keulen L, Kant J, Kortekaas J. Four-segmented Rift Valley fever virus-based vaccines can be applied safely in ewes during pregnancy. Vaccine. (2017) 35:3123–8. doi: 10.1016/j.vaccine.2017.04.024
139. Swanepoel R, Struthers JK, Erasmus MJ, Shepherd SP, McGillivray GM, Shepherd AJ, et al. Comparative pathogenicity and antigenic cross-reactivity of Rift Valley fever and other African phleboviruses in sheep. J Hyg (Lond). (1986) 97:331–46. doi: 10.1017/S0022172400065426
140. Bird BH, Khristova ML, Rollin PE, Ksiazek TG, Nichol ST. Complete genome analysis of 33 ecologically and biologically diverse Rift Valley fever virus strains reveals widespread virus movement and low genetic diversity due to recent common ancestry. J Virol. (2007) 81:2805–16. doi: 10.1128/JVI.02095-06
141. Bird BH, Githinji JW, Macharia JM, Kasiiti JL, Muriithi RM, Gacheru SG, et al. Multiple virus lineages sharing recent common ancestry were associated with a Large Rift Valley fever outbreak among livestock in Kenya during 2006-2007. J Virol. (2008) 82:11152–66. doi: 10.1128/JVI.01519-08
142. Grobbelaar AA, Weyer J, Leman PA, Kemp A, Paweska JT, Swanepoel R. Molecular epidemiology of Rift Valley fever virus. Emerg Infect Dis. (2011) 17:2270–6. doi: 10.3201/eid1712.111035
143. Ikegami T, Balogh A, Nishiyama S, Lokugamage N, Saito TB, Morrill JC, et al. Distinct virulence of Rift Valley fever phlebovirus strains from different genetic lineages in a mouse model. PLoS ONE. (2017) 12:e0189250. doi: 10.1371/journal.pone.0189250
144. Anderson GW Jr, Peters CJ. Viral determinants of virulence for Rift Valley fever (RVF) in rats. Microb Pathog. (1988) 5:241–50. doi: 10.1016/0882-4010(88)90096-4
145. Shabman RS, Morrison TE, Moore C, White L, Suthar MS, Hueston L, et al. Differential induction of type I interferon responses in myeloid dendritic cells by mosquito and mammalian-cell-derived alphaviruses. J Virol. (2007) 81:237–47. doi: 10.1128/JVI.01590-06
146. Moutailler S, Roche B, Thiberge JM, Caro V, Rougeon F, Failloux AB. Host alternation is necessary to maintain the genome stability of rift valley fever virus. PLoS Negl Trop Dis. (2011) 5:e1156. doi: 10.1371/journal.pntd.0001156
148. Findlay GM. The relation between dengue and rift valley fever. Trans Royal Soc Tropic Med Hygiene. (1932) 26:157–60. doi: 10.1016/S0035-9203(32)90115-1
149. Wallace DB, Ellis CE, Espach A, Smith SJ, Greyling RR, Viljoen GJ. Protective immune responses induced by different recombinant vaccine regimes to Rift Valley fever. Vaccine. (2006) 24:7181–9. doi: 10.1016/j.vaccine.2006.06.041
150. Hartman AL, Powell DS, Bethel LM, Caroline AL, Schmid RJ, Oury T, et al. Aerosolized rift valley fever virus causes fatal encephalitis in african green monkeys and common marmosets. J Virol. (2014) 88:2235–45. doi: 10.1128/JVI.02341-13
151. Li M, Wang B, Li L, Wong G, Liu Y, Ma J, et al. Rift Valley Fever Virus and yellow fever virus in urine: a potential source of infection. Virol Sin. (2019) 34:342–45. doi: 10.1007/s12250-019-00096-2
Keywords: Rift Valley Fever virus, RVFV, vaccine, cattle, sheep, goat, deer, ruminants
Citation: Kroeker AL, Babiuk S, Pickering BS, Richt JA and Wilson WC (2020) Livestock Challenge Models of Rift Valley Fever for Agricultural Vaccine Testing. Front. Vet. Sci. 7:238. doi: 10.3389/fvets.2020.00238
Received: 25 September 2019; Accepted: 07 April 2020;
Published: 27 May 2020.
Edited by:
Armanda Bastos, University of Pretoria, South AfricaReviewed by:
Jeroen Kortekaas, Central Veterinary Institute, NetherlandsGema Lorenzo, Instituto Nacional de Investigación y Tecnología Agraria y Alimentaria (INIA), Spain
Copyright © 2020 Kroeker, Babiuk, Pickering, Richt and Wilson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrea Louise Kroeker, QW5kcmVhLktyb2VrZXJAdXNhc2suY2E=
†Present address: Andrea Louise Kroeker, VIDO-InterVac, University of Saskatchewan, Saskatoon, SK, Canada
 Andrea Louise Kroeker
Andrea Louise Kroeker Shawn Babiuk
Shawn Babiuk Bradley S. Pickering
Bradley S. Pickering Juergen A. Richt4
Juergen A. Richt4