- 1School of Nursing, Columbia University Irving Medical School, Columbia University, New York, NY, United States
- 2School of Systems and Enterprises, Stevens Institute of Technology, Hoboken, NJ, United States
- 3Department of Medicine, Medical College of Wisconsin, Milwaukee, WI, United States
- 4John Theurer Cancer Center, Hackensack University Medical Center, Hackensack, NJ, United States
Introduction: The diagnosis of cancer creates immediate psychosocial distress for patients. New cancer patients are required to make important decisions about their treatment. Thus, it is essential to investigate their communication needs. This study examines the association between patient-centered communication and newly diagnosed cancer patients’ trust in their healthcare providers, satisfaction with the care visits, and perception of technology use during the visits.
Methods: We collected data from the Hackensack Meridian Health between February 2021 and May 2022. One hundred thirty-five participants were included in the study.
Results: The findings captured the significant effect of patient-centered communication on the trust in doctors and satisfaction with care services. However, no association was noticed with the perception of EHR use among this population.
Discussion: In the first visits after cancer diagnosis, patients need to build strong communication with their doctors to build trust in them. Future studies should focus on testing the hypotheses longitudinally to validate the findings in other phases of the cancer care continuum.
1 Introduction
Patient-centered care approaches and strategies consider patients’ needs and engagement levels for better care and patient outcomes (Street et al., 2009; Elkefi, 2023). When the diagnosis is cancer, the patient’s needs vary, and they experience challenges resulting from the diagnosis and treatment (Cliff and MacDonagh, 2000). Health outcomes, unmet expectations, socio-demographic traits, and other factors affect the perception of quality, comfort, and care in the cancer journey (Keller et al., 2013). It is, therefore, essential to determine their communication needs as a medium for their psychological support (Skilbeck and Payne, 2003). Because of these unique needs, it is necessary for doctors to adopt a patient-centered communication strategy during the visits to ensure a safe, efficient clinical cancer experience (Johansen and Saunders, 2017). While physicians generally support their patients’ engagement in healthcare by involving them in shared decision-making (McGuire et al., 2005), oncologists’ role is more complex. They may not understand their patients’ beliefs and needs in delivering diagnostic and prognostic information (Prouty et al., 2014). This behavior can result in a disconnection between patients and doctors (Prouty et al., 2014; Elkefi and Asan, 2023a). Delivering a communication that does not answer the needs of cancer patients can negatively impact their health outcomes and quality of life (Prouty et al., 2014). Thus, promoting cancer communication is a clinical and public health priority (Davis et al., 2002). Many organizations, such as government, volunteer health agencies (VHAs), health care systems, and providers, focus on improving cancer communication to enhance cancer prevention, detection, and treatment (Davis et al., 2002).
Many studies show that patients’ satisfaction and the evaluation of the quality of care are directly related to communication between doctors and patients (Keller et al., 2013; Elkefi and Asan, 2021). Patient-centered communication encompasses a broad range of verbal and non-verbal behaviors, including active listening and effective verbal and non-verbal communication, which is essential in optimizing patient interactions (Travaline et al., 2005). In another word, patient-centered communication entails actively interacting with patients to establish a shared understanding of how the physician’s thoughts and proposed care align with the patient’s expectations, interests, and individual needs (Travaline et al., 2005). Doctors’ communication styles influence patients’ involvement in health care and their satisfaction and intention to be loyal (Travaline et al., 2005). Interpersonal communication primarily involves exchanging information, reaching treatment-related decisions, and establishing positive relationships between providers and patients (Ong et al., 1995). The ability to communicate well is one of the core competencies of healthcare providers and is essential for creating mutually trusting relationships with patients (van Dalen, 2013). In primary care settings, a patient-centered approach to communication is associated with several positive outcomes, including increased levels of satisfaction and alleviated health-related symptoms (Little et al., 2001). It appears that patients are more likely to report higher satisfaction levels when they believe they are treated with dignity and when they participate in treatment decisions (Rahmqvist and Bara, 2010). Patients value communication and information more than the efficiency of care or access to nurses and doctors (Sofaer and Firminger, 2005).
The use of health information technology (HIT) such as patient portals, mobile health, wearable devices, and telehealth, among other types of technology, has been shown to empower cancer patients’ involvement in care, facilitating information seeking and exchange within the visits and at home (Clauser et al., 2011; Elkefi and Asan, 2021; Elkefi et al., 2023; Elkefi and Asan, 2023b). For example, due to COVID-19, telehealth has been extensively used to provide safe, cost-effective, and acceptable follow-up visits to cancer patients (Dickinson et al., 2014). A study by Garg et al. showed that implementing AI-based digital devices during visits can help reduce costs and workflow inefficiency and improve overall patient outcomes and quality of life (Garg et al., 2018). Additionally, oncologists use several computer-based decision tools such as TakeTheWind, COMBAT, and Prostaat to promote shared therapeutic decision-making during consultations (Raj et al., 2017; Cuypers et al., 2019; Wyatt et al., 2019). Lastly, online medical records have been shown to improve visits workflows by informing decisions and processes (Coylewright et al., 2020; Elkefi and Asan, 2023a; Mayo et al., 2023).
The diagnosis of a life-threatening illness creates immediate psychosocial distress for patients (Safaie et al., 2022). Due to fear and shock, patients with new cancer diagnoses find it challenging to adjust to their situation (Safaie et al., 2022). In addition, they must make difficult decisions about their treatment, including the type of treatment they will receive and whether to participate in clinical trials independently from the anxiety they are experiencing. Cancer patients who have been living with the disease for some time face different challenges than newly diagnosed cancer patients (Safaie et al., 2022). Experienced cancer patients have had time to adjust to their diagnosis and may have already established a treatment plan and developed coping strategies. They may also have a better understanding of their prognosis and the potential side effects of their treatment. On the other hand, newly diagnosed cancer patients often face a range of difficult emotions and must quickly adjust to a new diagnosis and treatment plan (Safaie et al., 2022). They may also be overwhelmed by the information they need to process and the decisions they need to make. Additionally, they may have to confront the reality of a potentially life-threatening illness and the uncertainty of the future. This study investigates the association between effective doctor-patient communication and newly diagnosed cancer patients’ perceptions of technology use in healthcare, trust of doctors, and satisfaction with visits.
Research has shown that providing cancer patients with patient-centered communication is associated with their trust in physicians (Zwingmann et al., 2017; Elkefi and Asan, 2023a). We, thus, hypothesize that for patients with newly diagnosed cancer in their first visit with an oncology doctor:
Hypothesis 1: Patient-centered communication is positively associated with trust of doctors.
Several studies have supported the role of technology use during the visits in promoting health outcomes such as patient engagement, communication and quality of care (Snyder et al., 2011; Tai-Seale et al., 2021). Studies have also shown that patients who receive better communication are more likely to accept the use of technology within the visits (Elkefi and Asan, 2023a,b). We thus hypothesize that:
Hypothesis 2: Patient-centered communication is positively associated with patients’ perception of health information technology use during visits.
Prior research has also associated the patient-centered communication to better quality of care perceptions (Wanzer et al., 2004; Bredart et al., 2005; Elkefi and Asan, 2024). Thus, we hypothesize that:
Hypothesis 3: Patient-centered communication is positively associated with satisfaction with the care visits.
2 Methods
2.1 Data collection and participants
We used a convenience sampling method to recruit newly diagnosed patients when they came for their initial diagnosis visit with a cancer provider at the Cancer Center from February 2021 through May 2022 (Elkefi and Asan, 2023b,c). Convenience sampling is a non-probability sampling technique that involves selecting your research sample based on convenience and accessibility.
Patients who came to the clinic for their first visit after diagnosis were approached and introduced to the study (within 24 h of the visits). If they were interested in participating, they completed a consent form. We, then, administered the survey over the phone by asking each question individually. The surveys were conducted over the phone due to COVID-19 restrictions. Each participant completing the survey was given a $30 gift card. Based on Green’s rule of thumb, the sample size for regression analysis should be equal to 6 for medium effect (VanVoorhis and Morgan, 2007; Elkefi and Asan, 2023c). In this study, we recruited 135 patients whom 13 doctors had seen.
The patients had different types of cancer. Most of them (25.19%) had breast cancer, and (20%) lymphoma. The distribution of cancer types is shown in Appendix 1.
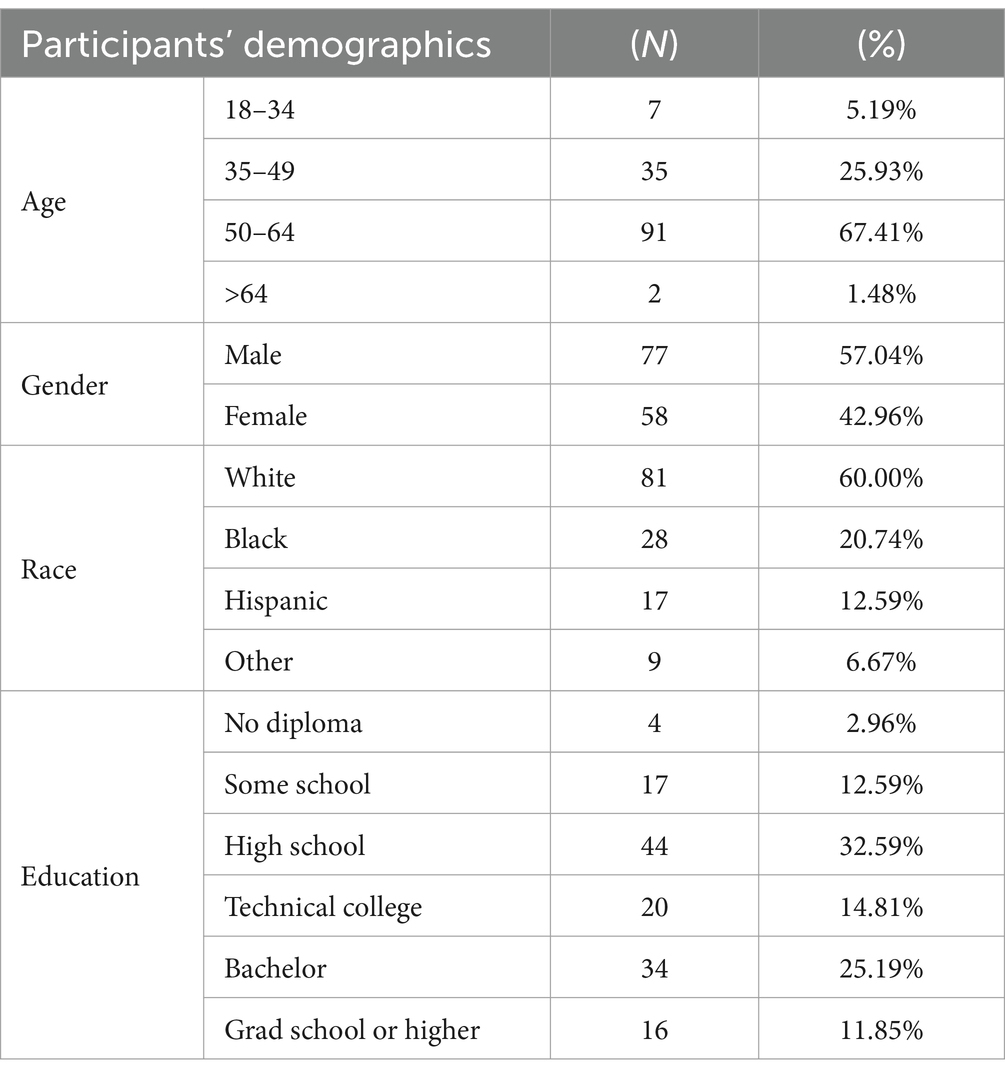
Out of the 135 participants, 58 were females. In addition, we had 45 participants from minority groups (Hispanic and African American). Most participants were between 50 and 64 years old (Table 1).
2.2 Instrumentation
The survey included validated questions measuring patient-centered cancer communication as dependent variables. The independent variables consist of the patient’s trust towards doctors, EHR use perception, and their satisfaction with the care. We capture patient satisfaction through the following question (“How satisfied were you with the overall visit?”) and demographics (age, gender, race, and education level). We used the PCC-Ca-6 (Patient-centered communication in cancer, six questions) measure, the short version of PCC-Ca-6 (Reeve et al., 2017) for communication evaluation. The measure is a psychometrically sound scale developed and tested to assess patient-centered communication effectiveness perception among cancer patients and their providers (Treiman et al., 2017). Trust in healthcare providers is measured using the subscale “trust in healthcare providers” of the “Multidimensional Trust in Health Care Systems Scale,” developed and validated by Egede and Ellis (2008). It is a score composed of 10 questions with 4 Likert scale answers (Egede and Ellis, 2008). The score is turned into a score over 100 and interpreted as follows. If the overall score is above 50, then we consider it high trust; otherwise, we consider it low trust (Elkefi and Asan, 2023c). Patient perception of technology use (use of computer/electronic medical record) during the clinic visit is measured through the “Patient-Reported Satisfaction with Physician Computer Use scale,” which is assessed and validated for electronic health records and other computer uses in healthcare settings (Lee et al., 2016). For satisfaction with care, we use a 5-Likert scale question where patients are asked about their satisfaction with the visit. We test the overall score and the components’ associations for each variable (Elkefi and Asan, 2023c).
2.3 Data analysis
First, we ran descriptive statistics for all the study variables. Second, logistic regression analysis was run for the scores and the components to explore the correlation between the variables and test the hypothesis. All the regression models were adjusted for the demographics (age, race, gender, and education level). Odds ratios and p-value of the regression models were reported to assess the type of association between the dependent and independent variables and its significance. A p-value of <0.05 was considered significant.
Model variables (trust, satisfaction, communication, and perception of technology use) were dichotomized for analysis purposes based on the information existing in the literature with a cut-off of 50% as done in previous studies (Blanch-Hartigan et al., 2015; Masci et al., 2020; Elkefi, 2023; Elkefi and Asan, 2023a). All the analyses were run using Python 3.6 (New Jersey, Python Software Foundation).
3 Results
Over 2/3 (69.73%) of the participants perceived the communication received during their initial consultation after cancer diagnosis as patient-centered. This trend was persistent across all the demographic groups, as shown in Table 2. All patient groups perceived the communication received as positive (for each group of age, gender, education, and race, the rate of patients that rated the communication received as good is always greater than 50%).
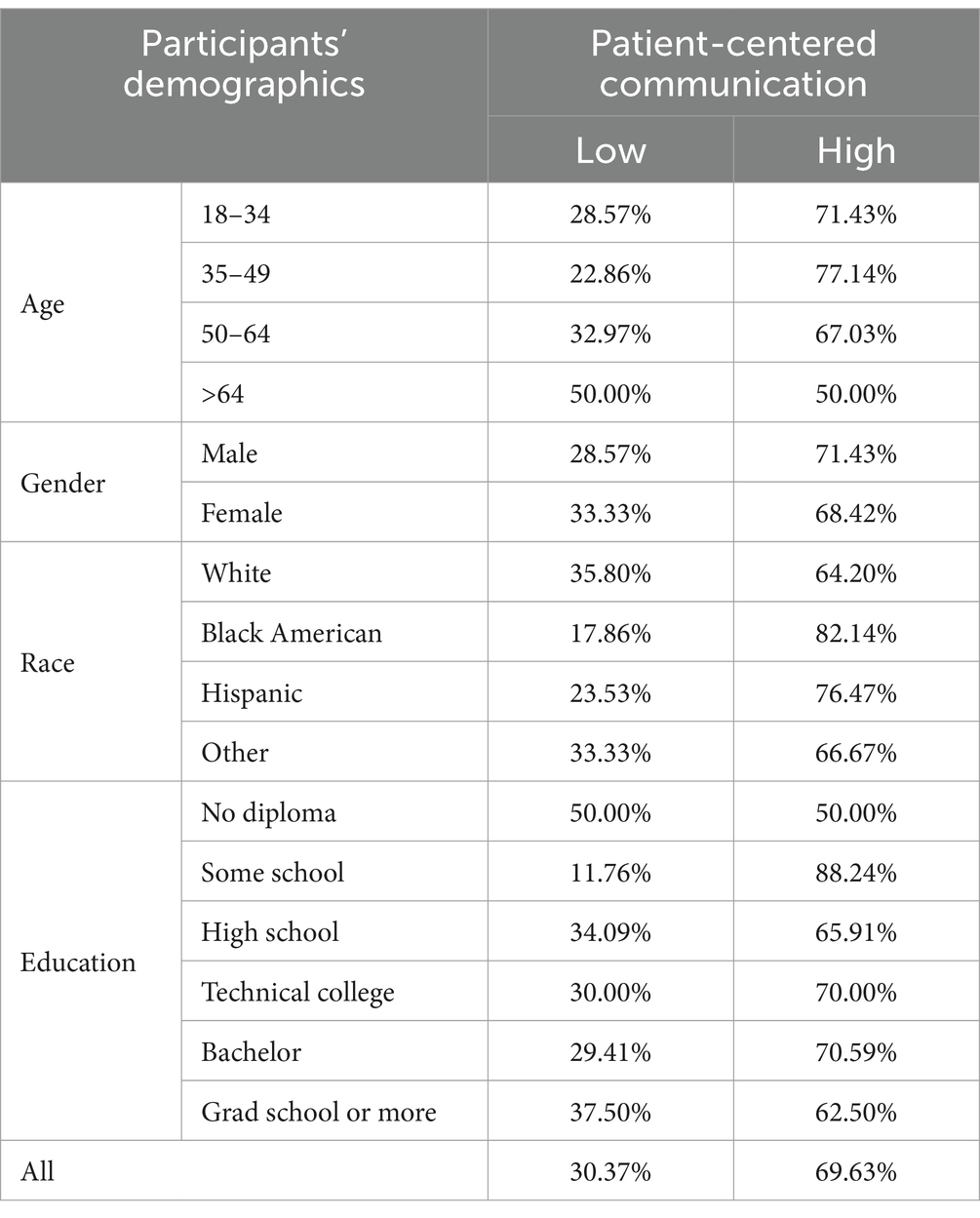
Table 2. Distribution of the patients’ patient-centered communication perception across demographics.
More than 50% of each population subgroup perceived the communication as positive. The lowest patient-centered communication perceptions were recorded among patients above 64 years old and among people without diplomas (50% each).
Table 3 illustrates the association between their perception of patient-centered communication and outcomes (satisfaction, trust, and EHR perception). Most patients thought the doctors helped them deal with their uncertainty about cancer visits (58.52%). Providers helped patients understand the following steps (78.52%), shared information that helped patients make decisions (65.93%), had open, honest communication with patients (73.33%), and made patients comfortable asking questions during the visits (71.11%). However, most of the patients thought that doctors were not able to help them cope with their feelings of stress and fear (49.63%). Furthermore, Patients who ranked satisfaction, trust, and perception of EHR use high usually had a more positive perception of patient-centeredness (94.68, 69.15, 56.82% consecutively).
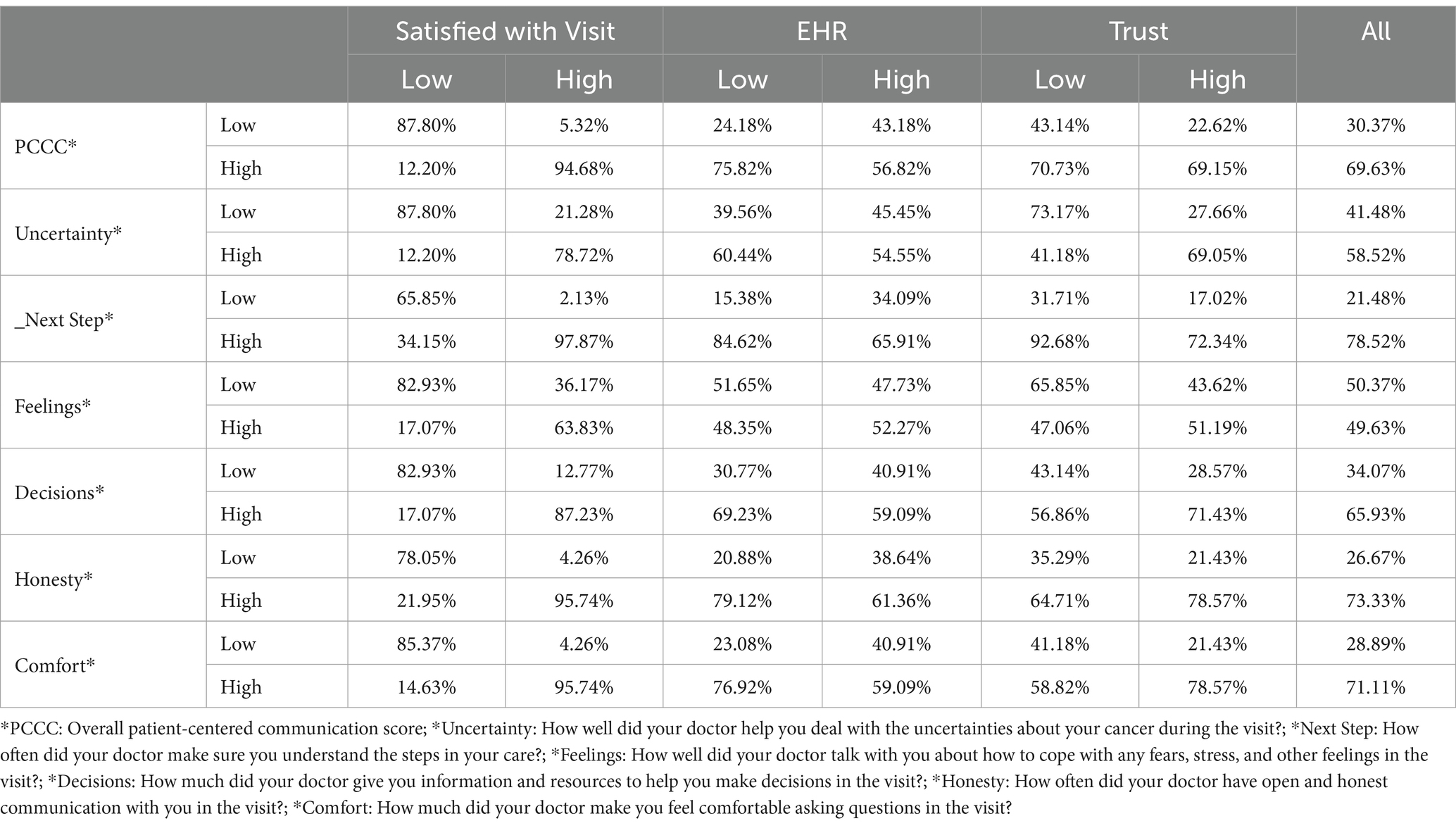
Table 3. Cross table of the impact of patient-centered cancer communication on satisfaction, trust and technology use.
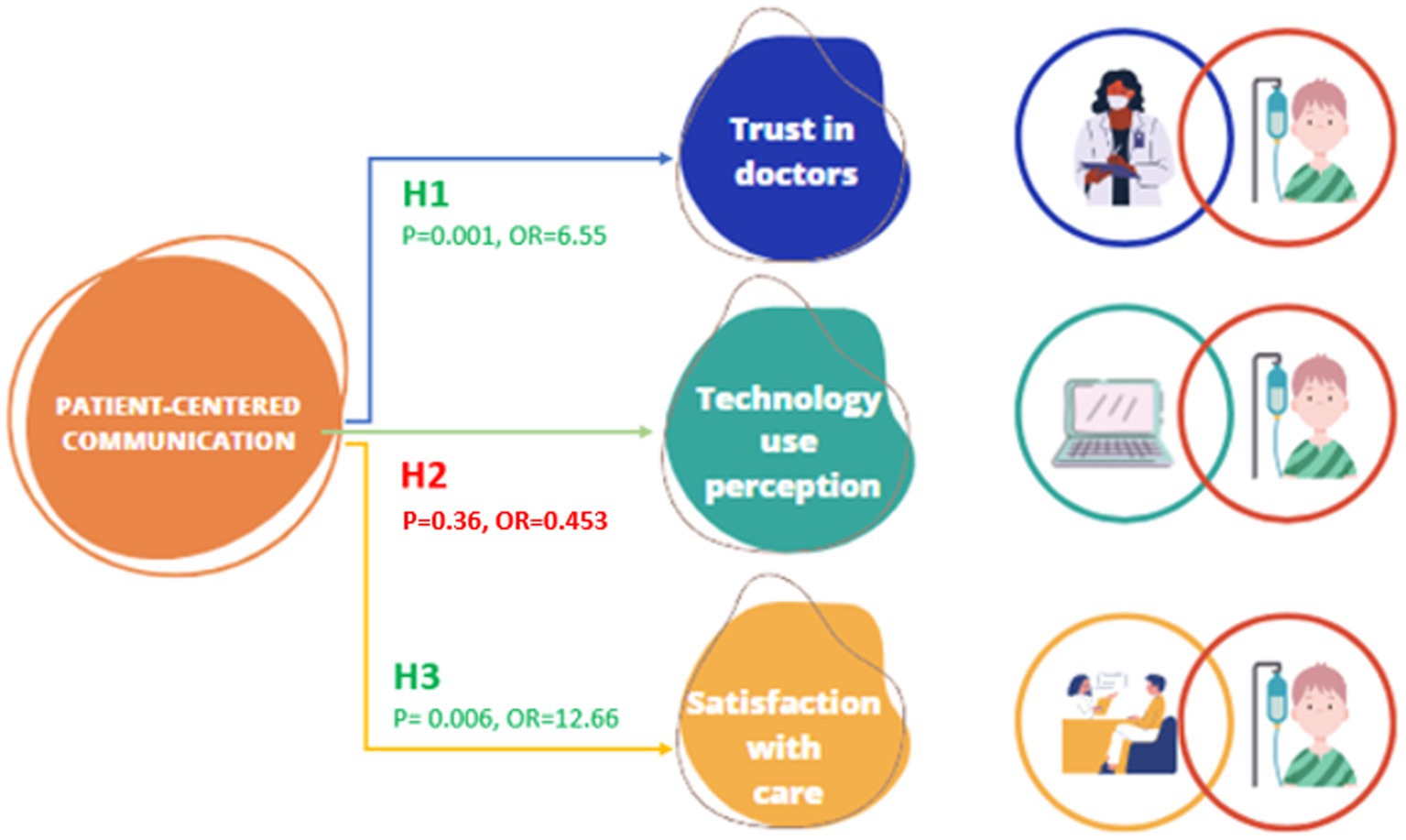
Finally, we also tested the hypothesis using regression analysis. Figure 1 shows the results of the different models tested. Newly diagnosed cancer patients with a positive perception of the patient-centered communication received expressed a positive trust towards their doctors (p = 0.001, OR = 6.55 [2.40–17.35]). Thus, we fail to reject Hypothesis 1.
In addition, the better the communication was, the more the new cancer patients felt satisfied with their visits (p = 0.006, OR = 12.66 [3.38–47.35]), which is why we failed to reject Hypothesis 3. However, contrary to what we hypothesized, the perception of technology use during the visit was negatively correlated with the new cancer patients’ perception of communication (p = 0.36, OR = 0.45 [0.20–0.95]). Thus, we reject Hypothesis 2.
4 Discussion
This study explores the association between patient-centered communication and patients’ trust in their doctor, perception of technology use, and patient satisfaction during their initial visit for newly diagnosed cancer. The analysis shows that when patients perceive a high level of patient-centered communication during the visit, they will have higher trust in doctors and satisfaction with the visit. However, the patient-centered communication was not associated with their perception of EHR use during the visit.
Trust can be viewed as a characteristic of physician–patient relationship depth (Ridd et al., 2009). It is generally considered an important therapeutic or working alliance component (Boulware et al., 2003; Ridd et al., 2009; Hillen et al., 2011). Communicating an initial cancer diagnosis, a specific context of sharing unfavorable news is an important doctor–patient communication process during which doctors disclose diagnoses, help their patients understand the diseases and the stages, discuss treatment plans, and answer questions (Cao et al., 2017). The adverse effects due to the ineffective communication of bad news will linger and cannot be easily reversed after the initial delivery of information (Ptacek and Eberhardt, 1996; Cao et al., 2017). This study found that patient-centered communication is positively associated with the patient’s trust in their doctor. This finding is similar to Hillen et al., who showed that oncologists can influence their patients’ trust by enhanced conveyance of their level of competence, honesty, and caring (Hillen et al., 2014). Due to the uncertainties encountered by cancer patients resulting from the considerable challenges for information transfer and communication, many questions arise about how impactful this can be on patients’ decision-making regarding treatment plans (Pichler et al., 2021). A study by Pichler et al. shows that communication based on trust relationship with the physician, built on competence and care, can offer a secure and reassuring counterpart against the uncertainties experienced (Pichler et al., 2021).
Patient satisfaction is by far the most recognized and widely used outcome. This probably has to do with the fact that it has a “logical and intuitive appeal” (Kaplan et al., 1989). However, there are obvious shortcomings in using outcomes such as satisfaction. For instance, patients may be satisfied with inadequate health care (Woolley et al., 1978). If medical care aims to produce optimal health outcomes, then ideally, effective doctor–patient communication should lead to better patient health (Kaplan et al., 1989). This study found that satisfaction is positively associated with the patient-centered communication provided to patients with new cancer diagnoses. A previous study by Ong et al. showed that doctor–patient communication during the oncological consultation is related to patients’ quality of life and satisfaction (Ong et al., 2000). Our finding extends the finding of that study by focusing on the early stage after diagnosis, confirming the correlation between satisfaction with the quality of care and patient-centered communication.
Patient-centered cancer communication is an integral part of healthcare, but it is not necessarily associated with the acceptance of health information technology (Elkefi and Asan, 2021). Good communication between cancer patients and doctors focuses on creating a relationship between the healthcare provider and patient based on respect, trust, and understanding (Street et al., 2016). This type of communication involves actively listening to the patient, responding to their questions and concerns, and providing information tailored to their needs (Street et al., 2016). Effective communication centered around the needs of patients who are newly diagnosed with cancer and respecting their needs has the potential to build trust in doctors and to change these patients’ perception of the quality of care they are receiving. Strategies that improve confidence and satisfaction with cancer care should consider effective communication as a pillar, beginning at the time of cancer diagnosis. In addition, studies show that conversational outcomes might also be linked to some health outcomes (Street et al., 2009). Future studies should also longitudinally explore how the quality of communication during patient visits will impact cancer treatment outcomes.
Our findings showed that while patient-centered communication is essential to ensure that the cancer patient feels comfortable and informed, it is not necessarily associated with the acceptance of health information technology. Health information technology is accepted based on how useful and practical it improves patient care and outcomes (Marangunić and Granić, 2015). It is also associated with many socioeconomic factors such as education, income, and age (Peek et al., 2014). So, despite the importance of patient-centered communication, it is not associated with the perception of technology use. Furthermore, the findings also show another important implication regarding the relationship between the perception of communication and technology use, unlike some previously published papers. Past studies have shown that EHR use is associated with communication perception in primary care visits and ambulatory visits, either positively or negatively, depending on how it is used. The literature also indicates that doctors avoid using computers heavily when there is an emotional discussion and only focus on the patient. Given the nature of first cancer visits, our findings also show that the use of technology is not associated with the perception of communication; in other words, patients care more about how physicians talk to them about the future of their cancer treatment regardless of how technology is used. This relationship might differ in the follow-up visits with the cancer patients. Future studies should investigate this relationship, computer use patterns in cancer visits longitudinally, and their potential association with various health outcomes.
Despite the originality of our work, the study has a few limitations worth noting. First, the survey is cross-sectional, which does not give us a clear idea of how the measures change with time. A longitudinal study should be considered to ensure that the correlation between the variables remains unchanged over time. In addition, the study includes patients at the time of their initial visits after cancer diagnosis. At this stage, patients are overwhelmed by the diagnosis and the initial decisions they have to make, which may bias their perceptions towards trust and quality of care. Future studies should consider ways to overcome these challenges by accounting for the situational bias and the trust levels among newly diagnosed patients. Finally, we do not have data to link patient centered communication to the patient health outcomes. Future longitudinal studies can explore how quality of patient centered communication can influence treatment as well as adherence outcomes among cancer patients.
5 Conclusion
Communication is a fundamental pillar of cancer care. In this study, we explored the association between patient-centered communication and trust, satisfaction with care, and perception of technology use among patients newly diagnosed with cancer. We found that patient-centered communication is positively associated with the patients’ confidence in their doctors and their satisfaction with the quality of care. However, no association was noticed on their perception of EHR use. Future studies should focus on testing the hypotheses longitudinally to confirm the findings for the other phases of the cancer care continuum.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the study obtained ethical approval from both the Stevens Institute of Technology and the Hackensack Meridian John Theurer Cancer Center IRB offices (IRB ID 00011536). Informed consent was sought verbally and documented electronically prior to each phone survey. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SE: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. OA: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. ZY: Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. TY: Writing – original draft, Writing – review & editing. SR: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Research reported in this publication is supported by the National Institute of Nursing Research of the National Institute of Health under Award Number 1R15NR018965-01. The content is solely the authors’ responsibility and does not necessarily represent the official views of the National Institute of Health.
Acknowledgments
This study occurred at the Hackensack Meridian Health, John Theurer Cancer Center. The study obtained ethical approval from the Stevens Institute of Technology and the Hackensack Meridian John Theurer Cancer Center IRB offices (IRB ID 00011536).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2024.1391981/full#supplementary-material
References
Blanch-Hartigan, D., Chawla, N., Beckjord, E. I., Forsythe, L. P., de Moor, J. S., Hesse, B. W., et al. (2015). Cancer survivors’ receipt of treatment summaries and implications for patient-centered communication and quality of care. Patient Educ. Couns. 98, 1274–1279. doi: 10.1016/j.pec.2015.06.005
Boulware, L. E., Cooper, L. A., Ratner, L. E., LaVeist, T. A., and Powe, N. R. (2003). Race and trust in the health care system. Public Health Rep. 118, 358–365. doi: 10.1016/S0033-3549(04)50262-5
Bredart, A., Bouleuc, C., and Dolbeault, S. (2005). Doctor-patient communication and satisfaction with care in oncology. Curr. Opin. Oncol. 17, 351–354. doi: 10.1097/01.cco.0000167734.26454.30
Cao, W., Qi, X., Yao, T., Han, X., and Feng, X. (2017). How doctors communicate the initial diagnosis of cancer matters: cancer disclosure and its relationship with Patients' hope and trust. Psycho-Oncology 26, 640–648. doi: 10.1002/pon.4063
Clauser, S. B., Wagner, E. H., Aiello Bowles, E. J., Tuzzio, L., and Greene, S. M. (2011). Improving modern cancer care through information technology. Am. J. Prev. Med. 40, S198–S207. doi: 10.1016/j.amepre.2011.01.014
Cliff, A., and MacDonagh, R. (2000). Psychosocial morbidity in prostate cancer: II. A comparison of patients and partners. BJU Int. 86, 834–839. doi: 10.1046/j.1464-410x.2000.00914.x
Coylewright, M., Keevil, J. G., Xu, K., Dodge, S. E., Frosch, D., and Field, M. E. (2020). Pragmatic study of clinician use of a personalized patient decision aid integrated into the electronic health record: an 8-year experience. Telemed J E Health 26, 597–602. doi: 10.1089/tmj.2019.0112
Cuypers, M., Lamers, R. E., Kil, P. J., van Tol-Geerdink, J. J., van Uden-Kraan, C. F., van de Poll-Franse, L. V., et al. (2019). Uptake and usage of an online prostate cancer treatment decision aid in Dutch clinical practice: a quantitative analysis from the prostate Cancer patient centered care trial. Health Informatics J. 25, 1498–1510. doi: 10.1177/1460458218779110
Davis, T. C., Williams, M. V., Marin, E., Parker, R. M., and Glass, J. (2002). Health literacy and cancer communication. CA Cancer J. Clin. 52, 134–149. doi: 10.3322/canjclin.52.3.134
Dickinson, R., Hall, S., Sinclair, J. E., Bond, C., and Murchie, P. (2014). Using technology to deliver cancer follow-up: a systematic review. BMC Cancer 14, 1–16. doi: 10.1186/1471-2407-14-311
Egede, L. E., and Ellis, C. (2008). Development and testing of the multidimensional Trust in Health Care Systems Scale. J. Gen. Intern. Med. 23, 808–815. doi: 10.1007/s11606-008-0613-1
Elkefi, S. (2023). Evaluation of patient-centeredness in Cancer care: A mixed methods study with a human factors approach. Hoboken, NJ: Stevens Institute of Technology.
Elkefi, S., and Asan, O. (2021). How technology impacts communication between cancer patients and their health care providers: a systematic literature review. Int. J. Med. Inform. 149:104430. doi: 10.1016/j.ijmedinf.2021.104430
Elkefi, S., and Asan, O. (2023a). The impact of patient-centered care on cancer patients’ QOC, self-efficacy, and trust towards doctors: analysis of a national survey. J Patient Exp 10:237437352311515. doi: 10.1177/23743735231151533
Elkefi, S., and Asan, O. (2023b). The health information technology preferences and perceptions of newly diagnosed patients with cancer. Int. J. Med. Inform. 180:105275. doi: 10.1016/j.ijmedinf.2023.105275
Elkefi, S., and Asan, O. (2023c). Perceived patient workload and its impact on outcomes during new Cancer patient visits: analysis of a convenience sample. JMIR Hum. Factors 10:e49490. doi: 10.2196/49490
Elkefi, S., and Asan, O. (2024). Effectiveness of patient-centered Cancer care (E-PACCC) framework: impact of work system factors on patient-centered care and quality of care among newly diagnosed cancer patients. JMIR Hum. Factors. 11:e53053. doi: 10.2196/53053
Elkefi, S., Trapani, D., and Ryan, S. (2023). The role of digital health in supporting cancer patients' mental health and psychological well-being for a better quality of life: a systematic literature review. Int. J. Med. Inform. 176:105065. doi: 10.1016/j.ijmedinf.2023.105065
Garg, S., Williams, N. L., Ip, A., and Dicker, A. P. (2018). Clinical integration of digital solutions in health care: an overview of the current landscape of digital technologies in cancer care. JCO Clin Cancer Inform 2, 1–9. doi: 10.1200/CCI.17.00159
Hillen, M. A., De Haes, H. C., and Smets, E. M. (2011). Cancer patients' trust in their physician—a review. Psycho-Oncology 20, 227–241. doi: 10.1002/pon.1745
Hillen, M. A., de Haes, H. C. J. M., Stalpers, L. J. A., Klinkenbijl, J. H. G., Eddes, E. H., Butow, P. N., et al. (2014). How can communication by oncologists enhance patients' trust? An experimental study. Ann. Oncol. 25, 896–901. doi: 10.1093/annonc/mdu027
Johansen, N. J., and Saunders, C. M. (2017). Value-based care in the worldwide battle against cancer. Cureus 9:e1039. doi: 10.7759/cureus.1039
Kaplan, S. H., Greenfield, S., and Ware, J. E. Jr. (1989). Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med. Care 27, S110–S127. doi: 10.1097/00005650-198903001-00010
Keller, A. C., Bergman, M. M., Heinzmann, C., Todorov, A., Weber, H., and Heberer, M. (2013). The relationship between hospital patients' ratings of quality of care and communication. Int. J. Qual. Health Care 26, 26–33. doi: 10.1093/intqhc/mzt083
Lee, W. W., Alkureishi, M. A., Ukabiala, O., Venable, L. R., Ngooi, S. S., Staisiunas, D. D., et al. (2016). Patient perceptions of electronic medical record use by faculty and resident physicians: a mixed methods study. J. Gen. Intern. Med. 31, 1315–1322. doi: 10.1007/s11606-016-3774-3
Little, P., Everitt, H., Williamson, I., Warner, G., Moore, M., Gould, C., et al. (2001). Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ 323, 908–911. doi: 10.1136/bmj.323.7318.908
Marangunić, N., and Granić, A. (2015). Technology acceptance model: a literature review from 1986 to 2013. Univ. Access Inf. Soc. 14, 81–95. doi: 10.1007/s10209-014-0348-1
Masci, F., Rosecrance, J., Mixco, A., Cortinovis, I., Calcante, A., Mandic-Rajcevic, S., et al. (2020). Personal and occupational factors contributing to biomechanical risk of the distal upper limb among dairy workers in the Lombardy region of Italy. Appl. Ergon. 83:102796. doi: 10.1016/j.apergo.2018.12.013
Mayo, C. S., Mierzwa, M., Yalamanchi, P., Evans, J., Worden, F., Medlin, R., et al. (2023). Machine learning model of emergency department use for patients undergoing treatment for head and neck cancer using comprehensive multifactor electronic health records. JCO Clin Cancer Inform 7:e2200037. doi: 10.1200/CCI.22.00037
McGuire, A. L., McCullough, L. B., Weller, S. C., and Whitney, S. N. (2005). Missed expectations?: physicians’ views of patients’ participation in medical decision-making. Med. Care 43, 466–470. doi: 10.1097/01.mlr.0000160415.08497.11
Ong, L. M., De Haes, J. C., Hoos, A. M., and Lammes, F. B. (1995). Doctor-patient communication: a review of the literature. Soc. Sci. Med. 40, 903–918. doi: 10.1016/0277-9536(94)00155-M
Ong, L. M. L., Visser, M. R. M., Lammes, F. B., and de Haes, J. C. J. M. (2000). Doctor–patient communication and cancer patients’ quality of life and satisfaction. Patient Educ. Couns. 41, 145–156. doi: 10.1016/S0738-3991(99)00108-1
Peek, S. T., Wouters, E. J., van Hoof, J., Luijkx, K. G., Boeije, H. R., and Vrijhoef, H. J. (2014). Factors influencing acceptance of technology for aging in place: a systematic review. Int. J. Med. Inform. 83, 235–248. doi: 10.1016/j.ijmedinf.2014.01.004
Pichler, T., Rohrmoser, A., Letsch, A., Westphalen, C. B., Keilholz, U., Heinemann, V., et al. (2021). Information, communication, and cancer patients’ trust in the physician: what challenges do we have to face in an era of precision cancer medicine? Support. Care Cancer 29, 2171–2178. doi: 10.1007/s00520-020-05692-7
Prouty, C. D., Mazor, K. M., Greene, S. M., Roblin, D. W., Firneno, C. L., Lemay, C. A., et al. (2014). Providers’ perceptions of communication breakdowns in cancer care. J. Gen. Intern. Med. 29, 1122–1130. doi: 10.1007/s11606-014-2769-1
Ptacek, J. T., and Eberhardt, T. L. (1996). Breaking bad news: a review of the literature. JAMA 276, 496–502. doi: 10.1001/jama.1996.03540060072041
Rahmqvist, M., and Bara, A.-C. (2010). Patient characteristics and quality dimensions related to patient satisfaction. Int. J. Qual. Health Care 22, 86–92. doi: 10.1093/intqhc/mzq009
Raj, S. X., Brunelli, C., Klepstad, P., and Kaasa, S. (2017). COMBAT study–computer based assessment and treatment–a clinical trial evaluating impact of a computerized clinical decision support tool on pain in cancer patients. Scand J Pain 17, 99–106. doi: 10.1016/j.sjpain.2017.07.016
Reeve, B. B., Thissen, D. M., Bann, C. M., Mack, N., Treiman, K., Sanoff, H. K., et al. (2017). Psychometric evaluation and design of patient-centered communication measures for cancer care settings. Patient Educ. Couns. 100, 1322–1328. doi: 10.1016/j.pec.2017.02.011
Ridd, M., Shaw, A., Lewis, G., and Salisbury, C. (2009). The patient–doctor relationship: a synthesis of the qualitative literature on patients' perspectives. Br. J. Gen. Pract. 59, e116–e133. doi: 10.3399/bjgp09X420248
Safaie, N., Zeinali, H., Ghahramanfard, F., Mirmohammadkhani, M., and Moonesan, M. (2022). Anxiety and depression among new cancer patients. J. Family Med. Prim. Care 11, 4146–4150. doi: 10.4103/jfmpc.jfmpc_1984_21
Skilbeck, J., and Payne, S. (2003). Emotional support and the role of clinical nurse specialists in palliative care. J. Adv. Nurs. 43, 521–530. doi: 10.1046/j.1365-2648.2003.02749.x
Snyder, C. F., Wu, A. W., Miller, R. S., Jensen, R. E., Bantug, E. T., and Wolff, A. C. (2011). The role of informatics in promoting patient-centered care. Cancer J 17, 211–218. doi: 10.1097/PPO.0b013e318225ff89
Sofaer, S., and Firminger, K. (2005). Patient perceptions of the quality of health services. Annu. Rev. Public Health 26, 513–559. doi: 10.1146/annurev.publhealth.25.050503.153958
Street, R. L. Jr., Makoul, G., Arora, N. K., and Epstein, R. M. (2009). How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ. Couns. 74, 295–301. doi: 10.1016/j.pec.2008.11.015
Street, R. L. Jr., Mazor, K. M., and Arora, N. K. (2016). Assessing patient-centered communication in cancer care: measures for surveillance of communication outcomes. J. Oncol. Pract. 12, 1198–1202. doi: 10.1200/JOP.2016.013334
Tai-Seale, M., Rosen, R., Ruo, B., Hogarth, M., Longhurst, C. A., Lander, L., et al. (2021). Implementation of patient engagement tools in electronic health records to enhance patient-centered communication: protocol for feasibility evaluation and preliminary results. JMIR Res Protoc 10:e30431. doi: 10.2196/30431
Travaline, J. M., Ruchinskas, R., and D’Alonzo, G. E. (2005). Patient-physician communication: why and how. J AM Osteopath Med 105, 13–18. doi: 10.7556/jaoa.2005.105.1.13
Treiman, K., McCormack, L., Olmsted, M., Roach, N., Reeve, B. B., Martens, C. E., et al. (2017). Engaging patient advocates and other stakeholders to design measures of patient-centered communication in Cancer care. Patient 10, 93–103. doi: 10.1007/s40271-016-0188-6
van Dalen, J. (2013). Communication skills in context: trends and perspectives. Patient Educ. Couns. 92, 292–295. doi: 10.1016/j.pec.2013.05.020
VanVoorhis, C. W., and Morgan, B. L. (2007). Understanding power and rules of thumb for determining sample sizes. Tutor Quant Methods Psychol 3, 43–50. doi: 10.20982/tqmp.03.2.p043
Wanzer, M. B., Booth-Butterfield, M., and Gruber, K. (2004). Perceptions of health care providers' communication: relationships between patient-centered communication and satisfaction. Health Commun. 16, 363–384. doi: 10.1207/S15327027HC1603_6
Woolley, F. R., Kane, R. L., Hughes, C. C., and Wright, D. D. (1978). The effects of doctor-patient communication on satisfaction and outcome of care. Soc Sci Med A Med Psychol Med Sociol 12, 123–128. doi: 10.1016/0271-7123(78)90039-1
Wyatt, K. D., Jenkins, S. M., Plevak, M. F., Venegas Pont, M. R., and Pruthi, S. (2019). A personalized, web-based breast cancer decision making application: a pre-post survey. BMC Med. Inform. Decis. Mak. 19, 1–11. doi: 10.1186/s12911-019-0924-7
Keywords: communication, cancer, new cancer visits, trust, satisfaction, technology use communication, new cancer patients, clinic visit
Citation: Elkefi S, Asan O, Yu Z, Yen T and Rowley S (2024) Patient-centered communication’s association with trust, satisfaction, and perception of electronic health records use among newly diagnosed patients with cancer. Front. Commun. 9:1391981. doi: 10.3389/fcomm.2024.1391981
Edited by:
Tayana Soukup, Imperial College London, United KingdomReviewed by:
Charee Mooney Thompson, University of Illinois at Urbana-Champaign, United StatesBryan Abendschein, Western Michigan University, United States
Copyright © 2024 Elkefi, Asan, Yu, Yen and Rowley. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Onur Asan, b2FzYW5Ac3RldmVucy5lZHU=
 Safa Elkefi1
Safa Elkefi1 Onur Asan
Onur Asan Zhongyuan Yu
Zhongyuan Yu