- 1Clinical Research Institute for Developmental Medicine, Johannes Kepler University, Linz, Austria
- 2Institute of Neurology of Senses and Language, Hospital of St. John of God, Linz, Austria
- 3Department of Communication Sciences and Disorders, The University of Vermont, Burlington, VT, United States
Background: There is a lack of valid measures for the differential diagnosis of childhood apraxia of speech (CAS) worldwide, especially ones that are suitable for young children. With newly developed assessments, one key question is their feasibility in a community clinical setting.
Aim: The aim of this study is to examine the feasibility of a play-based tool to assess CAS, using the “Language-Neutral Assessment of Motor Speech” (LAMS) as an example, trialing it for the first time in a German-speaking region.
Methods: This exploratory study is conducted as a series of single case descriptions (N = 7) with monolingual German-speaking children. The feasibility aspects of practicality, acceptance, and adaptation are examined. The collected data are processed solely descriptively with additional qualitative observations.
Results: The practicality of a complete administration of the LAMS in a clinical setting is limited because it is time-consuming; however, acceptance by children and caregivers is high for most parts of the test. Adaptations to economize the time investment (primarily by omitting video analysis) seem possible without a significant reduction of quality.
Conclusions and clinical implications: Implementation of a flexible, playful assessment, such as the LAMS, in local clinical settings looks promising. In German-speaking countries, a German adaptation of the LAMS could fill a gap in the assessment of motor speech disorders in young, hard-to-test children. More data regarding reliability and validity are needed.
1 Introduction
In depth assessment of childhood apraxia of speech is required for a number of children but differential diagnosis is still debated. Despite some consensus on core criteria (American Speech-Language-Hearing Association, 2007), recent studies and reviews indicate that the current clinical standard of relying on perceptual assessment of core features or feature lists (e.g., Shriberg et al., 2012) may not be optimal or sufficient. Issues like lack of operability, psychometrical robustness, and overlapping features of speech disorders have to be considered (Iuzzini-Seigel et al., 2022, 2017; Murray et al., 2021, 2015). A recent study also showed issues in reliability when it comes to expert diagnosis (Murray et al., 2023). In an attempt to lessen those issues, tools like the DEMSS1 (Strand et al., 2013) and the pause marker (Shriberg et al., 2017) have been proposed recently.
Despite progress in CAS diagnostics in the English speaking world, there is still much potential in other languages (Allison et al., 2020; Murray et al., 2021), including in German where there are no standardized tests or diagnostic guidelines for CAS. Diagnostic procedures largely follow the ASHA 2007 criteria (Föllner, 2015; Obry and Siegmüller, 2013; Siegmüller and Bartels, 2017).
In addition to these issues, early diagnosis is preferable, which means assessing young children, often with complex presentations, who will likely not accept long, rigorous evaluation of oral motor and speech motor abilities. An assessment is required to be flexible and play-based (to the extent possible) for this population, but also not too time-consuming. With no currently available instruments, there is a need to explore possible effective ways of testing for motor speech disorders in this population.
One assessment tool that seems to address many of these issues (including the need for a standardized tool in the German speaking world) is the Language-neutral Assessment of Motor Speech (LAMS, Velleman et al., 2017).
When exploring a new type of assessment, one key question is its feasibility: is a tool likely to be successful in everyday clinical conditions, on a larger scale (Thabane et al., 2010)? Therefore, in this exploratory study the LAMS—as an example of a play-based assessment—was trialed for the first time with Austrian German-speaking children diagnosed with CAS, exploring and using its largely language-neutral design and its playful approach, customized to young, hard-to-test children. The results have been described in detail and put in context with current clinical standards and local clinical procedures, alongside some initial data on reliability (Erlacher, 2021). This paper focuses on the feasibility aspects. Given the small sample size (N = 7), this study's outcome is only descriptive, but it may offer some initial information on practicality and implementation, acceptance, and possible adaptations.
2 Aims and hypotheses
The primary objective of this study was to examine the feasibility of a flexible, play-based assessment, like the LAMS, in a community clinical setting and particularly to test time management adaptations. To achieve this, the following hypotheses (based on areas of focus for feasibility studies proposed by Bowen et al. (2009) are evaluated:
(1) Practicality:
From a clinical perspective:
• The time requirements of a full test administration, including video analysis, exceed the time constraints of a typical clinical setting.
• Partial implementation (by using time-saving measures) is feasible.
From a caregiver perspective:
• Caregivers perceive the test procedure as feasible within a routine assessment visit.
(2) Acceptance:
From a clinical perspective:
• The assessment and its materials and play activities are well accepted by children and caregivers.
• It can be fully administered to most children.
• From a caregiver perspective:
• Caregivers and children experience the assessment as meaningful.
(3) Adaptation:
• Adaptations regarding the scoring procedure that ensure clinical feasibility in sufficient economy of time are possible while maintaining test quality.
To test these hypotheses, some initial adaptations were deemed necessary for the implementation in the German language area.
While the main focus of this exploratory study is on feasibility, we also describe the assessment (as a German adaptation) and put it in the context of current clinical procedures. For more details and for initial reliability results, see Erlacher (2021).
3 Materials and methods
The project was carried out as a descriptive case series study at the Institute of Neurology of Senses and Language (Hospital of St. John of God, Linz). For each child, written consent was obtained before testing. The study was approved by the ethics committee of the Johannes Kepler University, Linz, approval number EK 1292/2020.
3.1 Materials
3.1.1 LAMS
The LAMS has been used in pilot studies since 2009 (Rupela et al., 2016). For the current study, we used the 2017 version (Velleman et al., 2017), which was also trialed on 82 children throughout mostly English speaking countries. Since then further adaptations have been made in preparation for norming (for a detailed history see Appendix I).
Intended for young, hard-to-test children, the LAMS was also designed to be language-neutral in the sense that English words do not have to be used. The items are flexible so that:
• Culturally-appropriate and language-appropriate materials can be used.
• Analysis of the child's speech can be done while keeping the phonological system of their language in mind.
It aims for differential diagnosis of speech sound disorders and ultimately of motor speech disorders in children. The test was developed for children from the ages of 2;6 to 8;0 years (Velleman et al., 2022). It is designed as an overall playful, mostly imitative interaction, using toys to encourage specific speech acts while keeping children engaged. The procedure is recorded on video; the scoring is done via video analysis. It consists of four parts:
(1) “Interactive Speech Sample”: a 15-min unstructured play situation (child and caregiver), in which ideally 100 vocalizations are transcribed and evaluated for volubility and intelligibility as well as number of different vowels, initial consonants, and word shapes.
(2) “Observations of Structures at Rest and Automatic/ Vegetative Functions” (e.g., observing reflexes, evaluating the oral mechanism at rest).
(3) “Single Functions”: non-speech and speech, such as sticking out the tongue and imitating single vowels and
(4) “Sequential Tasks (non-speech and speech)”: imitating stimuli of increasing complexity (e.g., part 2B2—sequences of vowels/consonants, part 2C—imitating changes in volume or pitch, part 4B—alternating syllables, part 4D—repeating non-words several times as a diadochokinetic task).
An oral sensory questionnaire completed by caregivers will not be discussed in this paper, as it is irrelevant to the feasibility issues addressed here.
During sections 2–4 the following characteristics are scored separately on various items: motor control/accuracy, smoothness, range of motion, rate, sequence maintenance, and consistency. There are rules for not completing a set of items as well as for giving auditory, visual, and tactile cues (which are recorded and factor into the scoring). Throughout the test, qualitative observations are recorded of tone differences, coordination, symmetry, rate, strength, range of motion, consistency, resonance, and involuntary movement.
The different characteristics of parts 2–4 are scored from 0–2 (0 meaning “within normal limits”)3 and summary scores are calculated. If a child is unable to imitate, a score of 2 is given; no distinction is made between compliance issues and motor abilities at that level.
For this study, it was important to consider that the LAMS is not yet standardized; it is in the norming process by Academic Therapy Publications. The number of parameters and items scored in each section vary, and therefore so do the maximum error points in each category. To create an individual scoring profile, the percentage of the maximum possible errors for each category was calculated. This was relevant for describing clinical presentations and evaluating adaptation. For deeper understanding, the absolute score values were additionally calculated in some cases.
Before commencing the study, the examiner (an Austrian certified and experienced speech and language therapist and clinical linguist) completed training and received feedback on scoring and videos from the assessment authors. Then the LAMS was tested on a typically developing child (P1, female, 6;0 years) and a pilot child (P2, female, 4;0 years) who met criteria for the project. This was done to identify the necessary adaptations for carrying out the current study, such as creating a locally appropriate phonetic inventory sheet for the speech sample with German and local dialect phonemes and adapting the play materials to the local cultural setting. Otherwise, recording and scoring were completed using the original English forms.
3.1.2 Caregiver questionnaire
In addition, a feasibility questionnaire was completed by caregivers (see Appendix III). This measure recorded their level of acceptance (approval) of the assessment procedures, evaluations of their children's acceptance (tolerance of the assessment procedures), and assessment of the practicality and implementation of the test.
3.2 Feasibility measures and data analysis
From a clinical perspective the following aspects of feasibility were considered as most relevant and quantitatively evaluated:
• Practicality: the total duration of the assessment, video analysis, scoring, and data entry of the results was measured, as well as the time required for the different stages separately. Any extra time spent per child to gather data on adaptation was recorded and subtracted from the total time spent, in order not to skew the time results (see “Adaptation” below). The average assessment time and also its range were calculated.
• Acceptance: through video analysis of the test administration, each assessable item was evaluated for administrability and completeness using a four-point scale (“promptly done”, “some delay” [two or fewer prompts required], “significant delay” [more than two prompts required], “not done”). Excluded from this assessment were the free play situation (test part 1A) and the observation of structures at rest (part 1B). A total of 56 test items were scored on this four-point scale, resulting in a percentage distribution of administrability for each individual test part, ranging from “promptly done” to “not done”. Overall completeness percentages were also calculated and test sections were analyzed for their degree of completion separately. These results were combined with qualitative observations of behavior including an evaluation of rapport during testing, facilitating some conclusions about acceptance.
• Adaptation: with regard to possible adaptations, a comparison was made between live scoring (during and immediately after the test) and (as intended by the test authors) scoring via additional video analysis with regard to average time saved by direct scoring and the resulting differences in the participants' scores. For this purpose, the results had to be entered and calculated twice for all sections of the test: once directly after the live assessment, then again after the video analysis. The extra time spent for this was not included in the analysis of the time spent (with respect to practicality considerations). For spontaneous speech (part 1), differences in all scoring parameters, such as differences in the total number of sentence-like utterances or of different vowels, were calculated. For parts 2–4 of the test, differences in points scored were calculated. Then the percentage of the maximum possible difference in error score that occurred for each evaluation category was calculated, as well as the percentage of the maximum possible difference in the total error score that occurred for each participant.
Possible sources of error that could be observed during live scoring in comparison to video analysis were documented as a qualitative supplement.
To measure feasibility from the caregivers' perspective, they were asked to rate 12 statements in the questionnaire, such as “The duration of the assessment was acceptable to me.” and “My child was motivated to participate.” on a Likert Scale from 1–4 (1 = “I agree completely”, 2 = ‘I agree mostly”, 3 = “I agree partly”, 4 = “I disagree”). Percentages of agreement were calculated for the overall questionnaire and also for the individual aspects of feasibility.
Data analysis was carried out in pseudonymized form.
Owing to the limited number of participants (N = 7) and because there are no normative data for the LAMS available yet, the analysis was purely descriptive. It comprised mean and median values and minimum and maximum values. In addition, qualitative data are reported.
3.3 Participants
Seven children (P3–P9, 5 male, 2 female) were recruited from a pool of children recently diagnosed with CAS (or suspected CAS), during a comprehensive set of developmental assessments (medical, cognitive, hearing, speech, language). They were re-invited for an appointment of approximately 1 h. Two children were also invited to undergo a separate retest of the LAMS, to gather data on retest reliability (Erlacher, 2021). The inclusion criteria were diagnosis or suspected diagnosis of CAS at the Institute of Neurology of Senses and Language (Linz) in accordance with the characteristics from the American Speech Language Hearing Association (2007) technical report on CAS as well as an age of 3;0–4;11 years. Children were excluded on the basis of bi- or multilingualism (in order to minimize practical issues related to communication with caregivers in a feasibility study, e.g., explaining the study process or filling in the caregiver questionnaire), a non-verbal cognitive developmental age < 3 years, permanent hearing impairment, severe visual impairment, autism spectrum disorder or other pervasive developmental disorder, severe language comprehension disorder (reference age for comprehension < 2;6 years), or organic causes of speech disorders. Participants could drop out at any time via withdrawal of guardian consent.
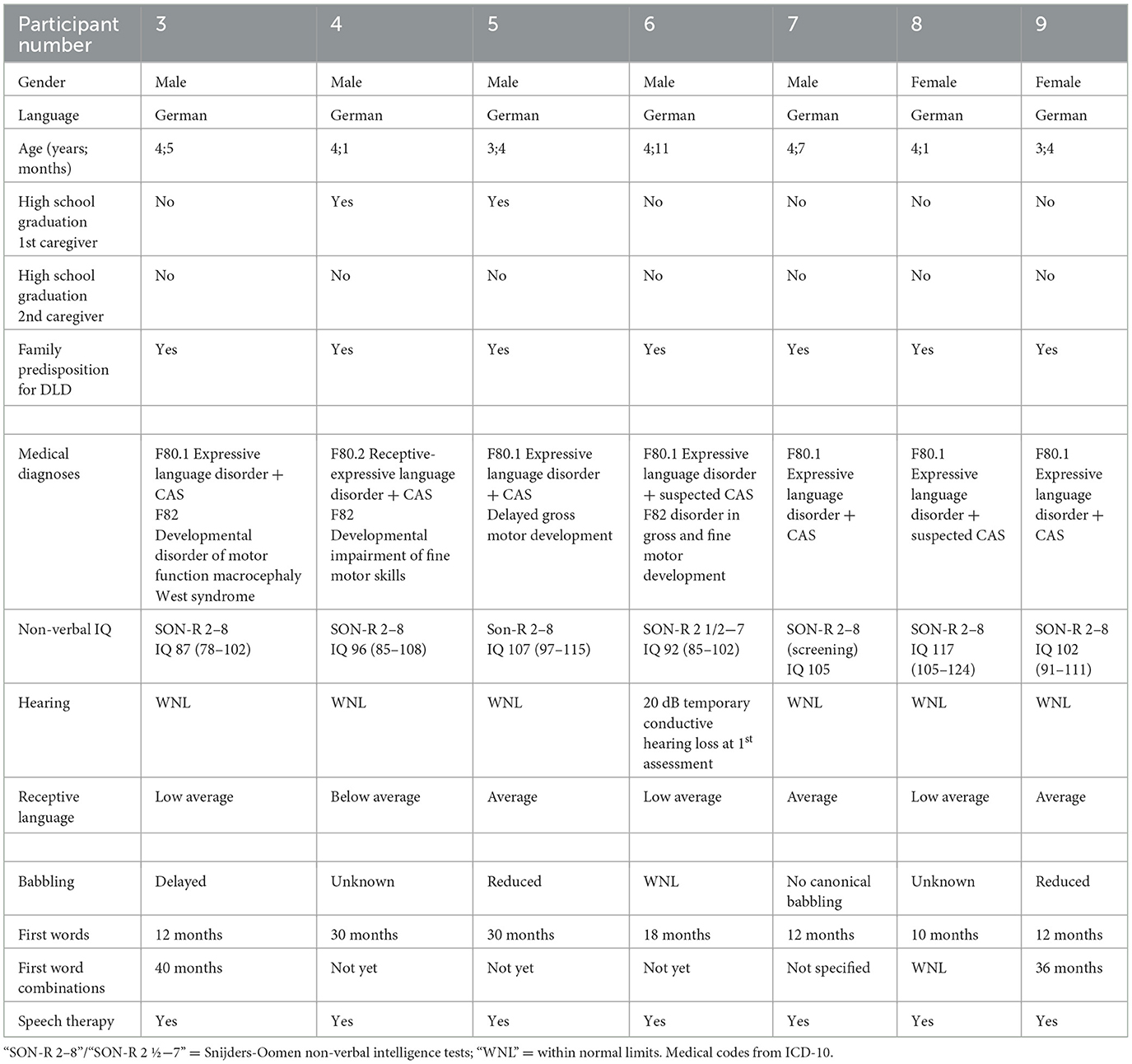
Sample characteristics are provided in Table 1. Developmental assessments were administered at the ages of 3;0 to 4;1 years, using German-language standardized tests. All children were diagnosed with expressive language impairment and one child also had a receptive language impairment. All were cognitively within normal limits. Four had non-speech motor deficits.
Differential diagnosis of CAS was done during the initial developmental assessment in varying depth, depending on time constraints and compliance. Spontaneous speech as well as a picture naming test were analyzed for the three core features named in the ASHA Technical Report (2007) as well as other possible manifestations (Iuzzini-Seigel et al., 2022), such as token-to-token inconsistencies, vowel distortions, groping or slow rate as reflections of coarticulatory difficulties, and/or prosodic issues. If possible, an imitation task devised for clinical use in this hospital (similar to the DEMSS) was carried out, as well as orofacial examination and assessment of speech diadochokinesis. Vowel, consonant, and syllable structure inventories were developed as well. Based on these measures, 5 children were diagnosed with CAS. In two cases the information that could be gathered from the children was slightly insufficient due to compliance reasons and time constraints. As a result, a diagnosis of suspected CAS was made, rather than a formal diagnosis of CAS.
4 Results
In the following section the most important feasibility outcomes will be highlighted.
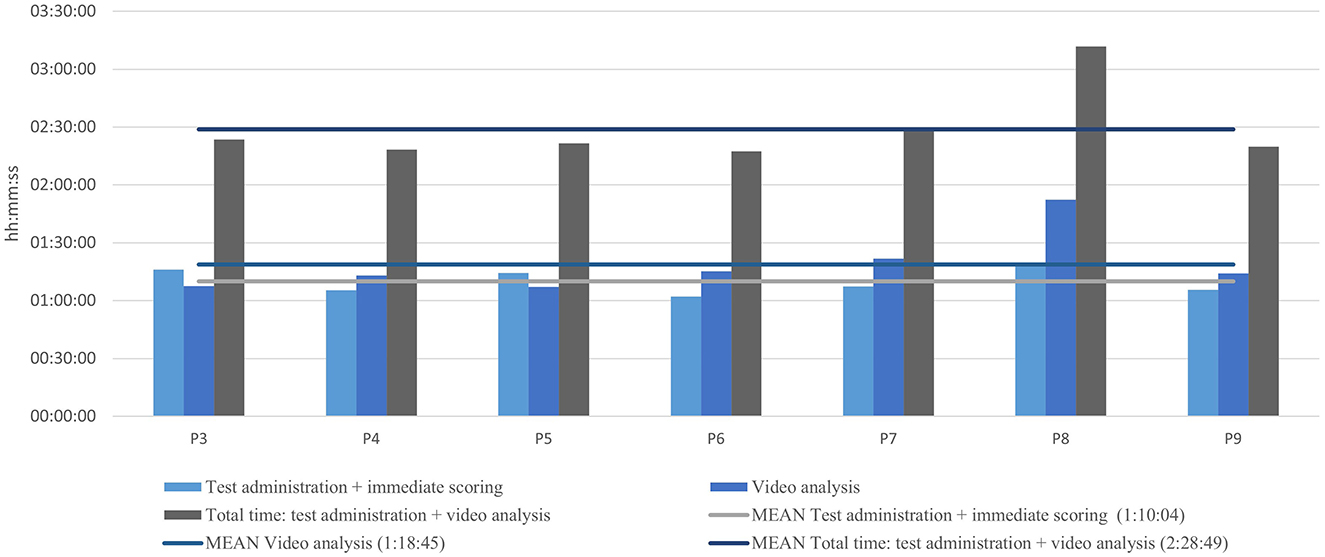
4.1 Practicality: time requirements
The average assessment time (hours:minutes:seconds) was 2:28:49 (range: 2:17:26–3:11:54) including video analysis (see Figure 1). The amount of time spent was evenly distributed among the children examined, with one exception (see individual results for P8).
4.2 Acceptance: items completed
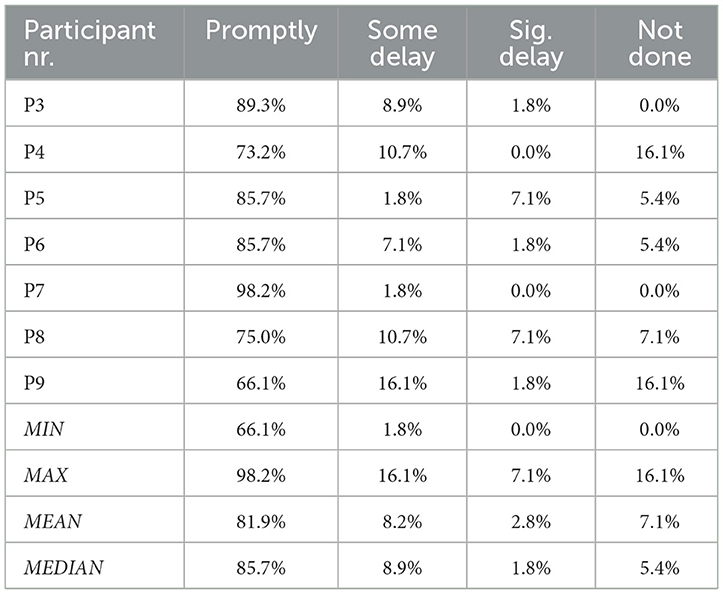
For individual results per participant see Table 2.
In total, 56 items were analyzed. The percentage of items completed ranged from 60.7 to 100% in the various test sections, with 9 of 12 subtests reaching >90% completion.
Severe delays, requiring multiple repetitions, were recorded in particular in test parts 2B (single sound production), 2C (sequential volume and pitch control), and 4B (alternate motion rate) at 14.3% of the time each. Verbal refusals, leaving the play situation, and zero responses were observed during these sections. Slight delays were observed in 11 out of 12 test items, up to 22.7% (2B – single consonant and vowel production).
In summary, tasks involving automated, vegetative functions were the easiest to perform with 100% completion, followed by single functions (with a somewhat wider range). The most difficult items were sequential tasks (subtests 2C and 4D), with an overall completion rate below 90%.
The overall degree of completion of the procedure was high, at 92.7% (see Figure 2).
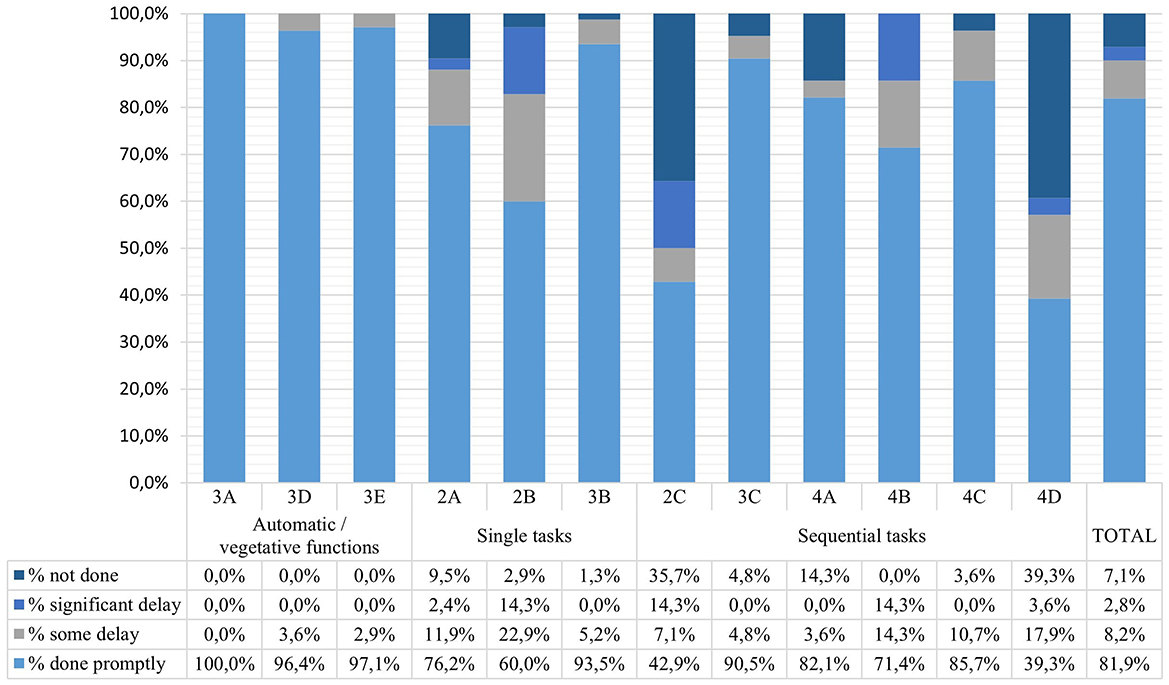
Figure 2. Acceptance per item (For details regarding the coding see Appendix II).
4.3 Adaptation: omitting video analysis
If video analysis had been omitted, the average time saved would have been 52.6% (47.0–58.5%, Appendix IV).
Although on average only 73.2% (59.2–92.5%) of sentence-length utterances and 68.5% (56.1–83.6%) of word-length vocalizations of the spontaneous speech sample (see Appendix V) could be transcribed live, there was only an 8.1% difference in intelligibility between live and video transcription. The recorded repertoires of vowels and consonants were almost identical under the two analysis conditions, with differences ranging from 0–2 segments. However, the inventory of word shapes differed more widely, ranging from 0–8 different numbers of shapes identified, especially in the two children with the largest number of different word shapes.
When comparing live scoring and additional video analysis, agreement was very high (see Table 3) in sections 2–4. Of the 98 categories evaluated, 78 (79.6%) were congruent (i.e., the number of points determined in the live scoring was the same as for the video analysis). In total there were percentage differences of 20% and 25% in 2 categories; otherwise the differences were below 10%. Overall, the differences in total scores ranged from 0 to 9 (out of a possible 214 total points), and the differences in the total percentage of errors ranged from 0 to 4.2%. For two children (P7, P9) the live scoring and the scoring with video were completely congruent (representing 28.6% of the total number of categories assessed).
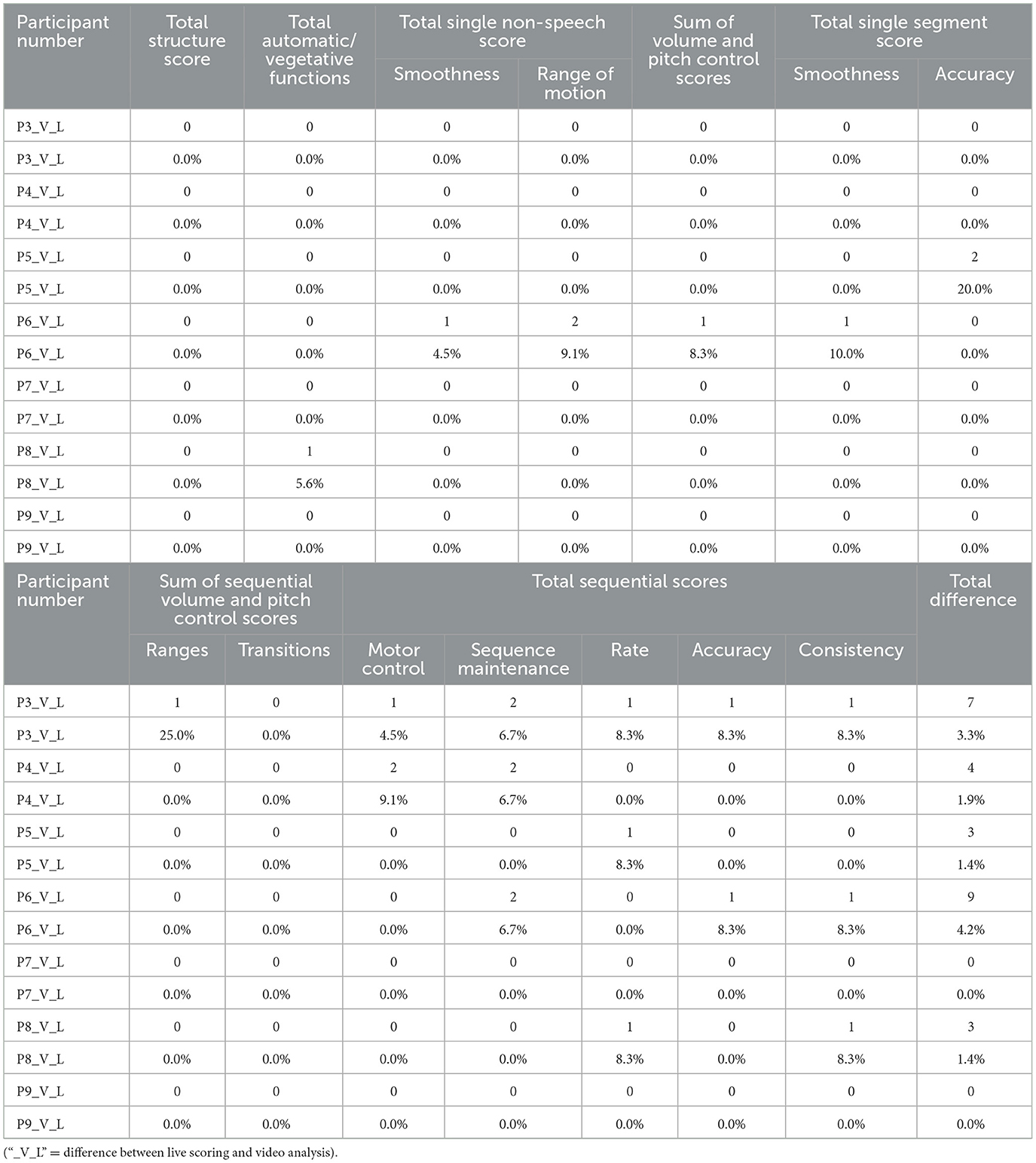
Table 3. Adaptation: live scoring vs. scoring with video analysis—differences in scoring points and percents.
4.4 Acceptance, practicality and implementation: caregiver questionnaire
Overall, caregivers' agreement with the statements in the caregiver questionnaire was high, with 71.4% of the statements receiving full agreement (see Figure 3). There was high agreement particularly with regard to practicality and acceptance. Responses regarding whether the child was comfortable with the test (acceptance) were somewhat more mixed with 57.1% in full agreement. This was especially true of statement no. 9, which dealt with the child's cooperation in comparison to other assessments (“My child participated better than during the initial assessment of speech.”). Here, the level of agreement was widely distributed. One statement questioned implementation; 57.1% of the caregivers could fully picture this test being administered as part of an initial speech-language examination; 42.9% could mostly imagine this.
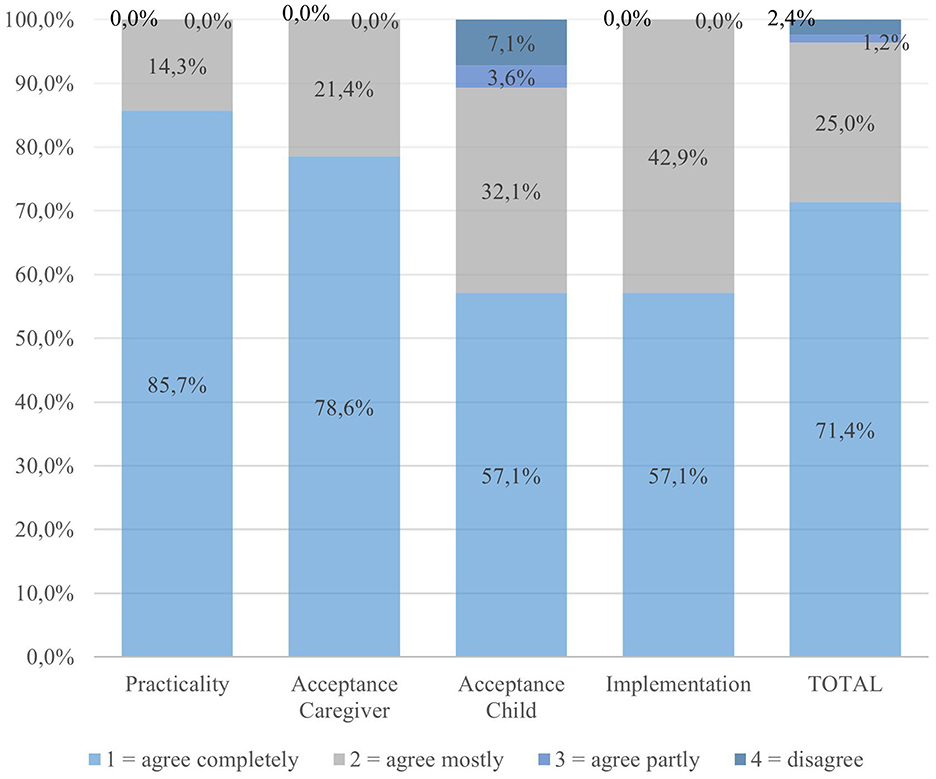
Figure 3. Caregiver questionnaire—percentage agreement grouped by feasibility aspects4 and overall.
4.5 Qualitative observations with regard to each participant
Qualitative observations were made of each LAMS testing session, including possible reasons for scoring differences, observations on administrability and acceptance, as well as overall rapport and clinical impression directly after the session.
P3 (4;5 years; CAS; non-speech motor deficits). In the live transcription of the child's spontaneous speech, longer, especially hard-to-understand utterances were not fully recorded, resulting in discrepancies in the results (lower intelligibility outcome from the video analysis). In parts 2–4, the scoring was largely congruent across transcription and scoring types. Minor differences were due to an item that was undocumented due to time pressure in live scoring. The test procedure was mostly administered following the standard protocol.
Overall rapport with the child was experienced as positive; the child's acceptance of the procedures was very good. Also, immediately after the assessment and scoring (without video analysis), a complete clinical impression had been formed.
P4 (4;1 years; CAS; receptive language disorder; non-speech motor deficits). In the qualitative analysis of spontaneous speech, difficulty in quickly differentiating between meaningful and non-meaningful utterances was noted, due to numerous vocalic interjections. Regarding the child's acceptance of the test procedures, there were several instances of clear rejection with head shakes, lack of response, or persistence in a different activity, especially when the child was asked to imitate. As a result, the procedure required repeated adjustments.
Overall, testing rapport was perceived as positive, with slightly increased demands on the examiner's flexibility. The immediate clinical assessment of the child was considered to be sufficiently complete, despite the incomplete transcription of the spontaneous speech sample. Video analysis did not change the clinician's impression.
P5 (3;4 years; CAS; non-speech motor deficits). In the live transcription of the speech sample, intelligibility was calculated to be lower in the video analysis than in the live assessment, due to difficulty in quickly documenting unintelligible vowel insertions during simultaneous transcription.
A complete assessment was not possible; refusal to cooperate indicated by head shaking and failing to reply was observed for the missing items. Changes in play types were necessary, especially for difficult imitation tasks. The overall experience was perceived as positive, nevertheless, due to the flexibility of the assessment.
A comprehensive subjective assessment of this child's speech could be made based on the immediate evaluation, without the video.
P6 (4;11 years; suspected CAS; non-speech motor deficits). Comprehension was impeded by sound transmission into the adjacent room, thus making live transcription of the spontaneous speech challenging. Incomprehensible utterances were often missed in the live transcription. The scoring for sections 2–4 was incomplete due to time constraints caused by the child's high level of motor restlessness. Behaviors such as leaving the play situation, requesting food, and verbally refusing participation occurred, resulting in some incomplete items.
Overall, rapport was perceived to be limited, and the examination situation to be laborious due to the child's motor restlessness and high distractibility. These factors rendered clinical assessment of the child correspondingly difficult. Video analysis was deemed helpful.
P7 (4;7 years; CAS). In this case there was a large difference between the live vs. video transcription of the identified syllable structures in spontaneous speech. Individual longer words were not completely documented under time pressure. The assessment of the second part of the session revealed full alignment in all scoring categories between the live assessment and the video analysis. The examiner recorded rapport as being very positive, with only a few quick adaptations to the procedure.
Overall, most parameters could be adequately assessed through live evaluation, except for the documentation of complex syllable structures, which was not feasible during the session.
P8 (4;1 years; suspected CAS). The administration and analysis of the test were the most time-consuming for this participant. Items in half of the subtests initially produced zero responses, due to persisting in a different activity, walking away, motor restlessness, head shaking, etc. The overall test experience was demanding, with challenges in establishing rapport due to high levels of motor restlessness and distractibility. Therefore, the procedure was highly individualized. An unusual communication produced within the spontaneous speech sample (the child quickly counting from 1 to 30) affected the calculation of intelligibility; therefore, a thorough analysis was required. Overall, to get an accurate picture of the clinical features of this child's speech disorder, video analysis, especially of spontaneous speech, was necessary.
P9 (3;4 years; CAS). It was not possible to complete the assessment with P9. For all missing items there was initially a clear verbal refusal, and in a third of the cases the test was subsequently abandoned in accordance with the instructions in the manual because of strong doubts about the child's ability to perform the items.
The qualitative reflection described the situation as somewhat demanding, with limited rapport, exemplified by refusal of more difficult speech tasks. Frequent adjustments to play procedures were necessary.
The clinical analysis during and immediately after the test situation was relatively complete, and the video analysis did not yield significant further insight.
5 Discussion
Given the limited number of participants, a discussion can only be descriptive. Nevertheless, important points of discussion can be identified and some statements can be made regarding the hypotheses.
• Practicality: the results of this small study show that the LAMS (or rather the detailed analysis of spontaneous speech and scoring via video) is too time consuming for daily clinical use, but it seems possible and more practical if the video analysis is omitted. From a caregiver's point of few the practical requirements of the test administration seem feasible.
• Acceptance: overall, analysis shows that the assessment procedure is mostly well accepted by children and caregivers with some exceptions regarding specific subtests.
• Adaptation: the hypothesis that changing the scoring procedure and thus ensuring time economy by leaving out the video analysis can be done while maintaining testing quality seems partly confirmed. In some instances, it seems justifiable but in other cases it does have some impact on the accuracy of some aspects of the speech analysis.
More specifically, from a clinical point of view, the issue of time requirements is central to the practicality of the LAMS, although this would depend to some degree on the examiner's routine, the child's compliance, and other practical considerations. With respect to spontaneous speech analyses, in particular, previous studies have highlighted the extended time needed for such procedures, and some have questioned the value of the information gained (Fox-Boyer, 2016; Snyder, 2010). However, despite criticisms about the imprecision and inefficiency of quantitative evaluation, an unstructured sample provides a wealth of speech and language information and can be analyzed at many levels. As a low-threshold entry point, it can also make a positive contribution to young children's cooperation. Its diagnostic value can be considered high if time efficient implementation is taken into account.
The average total time required for the administration and scoring of the LAMS was almost 149 min in this study, undoubtedly too long for clinical use. Under typical clinical conditions, an hour-long assessment procedure would appear suitable; it would fall within the time constraints of one assessment or therapy session in customary Austrian speech services. This could be achieved by leaving out video analysis and potentially saving an average of almost 53% of the LAMS assessment time.
A few practical aspects worth mentioning relate to the materials and physical setting. The LAMS manual recommends video recording and that observations of the caregiver-child play session be made from another location. Not every examination venue possesses full recording equipment, let alone the option to observe from an adjacent room, which could pose an extra implementation challenge.
Meanwhile, caregivers described the time spent on carrying out the assessment as fully acceptable for themselves and their children. However, it is important to note that in a routine assessment, families would have to allocate extra time if separate video evaluation necessitated postponing discussion of the child's diagnosis.
Based on the degree of completion of the assessment and on the qualitative observations, one can cautiously deduce the tested children's acceptance of this test. Thus, the second hypothesis was partially confirmed. Beginning with a relaxed free play situation, which may serve as an important “warm-up”, the LAMS could be implemented to a high degree of completeness. One exception is that some sections of the assessment, such as 4D (a complex diadochokinetic task), were often incomplete due to being aborted per the instructions (due to difficulty level).
On the other hand, there were clear verbal or non-verbal refusals by some children during some subtests, along with lower degrees of completeness. In addition, there were long delays on several test sections. Behaviors such as not responding, persisting in different activities, or leaving the table are challenging to interpret in terms of overall acceptance. In particular, the fact that the elicited pitch and volume changes (e.g., pitch or volume rises and/or falls, as in the sound of an ambulance) in section 2C were often met with verbal rejection or lack of response highlight that this set of tasks is potentially the least acceptable one from the child's perspective.
Nevertheless, the overall picture seems clear: from a quantitative and qualitative point of view, the test procedure is deemed well accepted, as it can often be fully completed. The examiner also subjectively experienced the testing situation as mostly relaxed, playful, and tailored to young children.
With regard to the third sub-hypothesis about the caregivers' points of view, the questionnaire also revealed high levels of acceptance. A high proportion of caregivers described the procedure as suitable for their child; they also had no objections to video recording. The play situations and the child-examiner interactions were perceived as appropriate, meaningful, and reasonable for an in-depth examination. However, caregivers did not judge the children to be significantly more cooperative compared to the previous speech assessment despite the play-based nature of the LAMS.
Regarding adaptation, the first question is whether the LAMS can be implemented in German-speaking countries. In principle, a positive answer can be given; however, an appropriate translation of the test documents would be required. For the spontaneous speech analysis, there would need to be clearly defined target vowels and consonants for German (and its different dialect regions).
Concerning the question of whether a shortening of administration time (in particular abandoning the video analysis) is possible while maintaining test quality, the following can be stated:
Although this small exploratory study lacks reliable statistical evaluation, the differences in scores, especially for test segments 2–4, were relatively small based on live vs. video-based transcription and scoring, resulting in limited additional insight from video analysis. Furthermore, in a comparison of results (see Erlacher, 2021), differences between live scoring and video analysis seemed not to distinctly or systematically differ from test-retest differences. Subjectively, a clear clinical picture was apparent in 5 of the 7 children directly after assessment. For 2 children additional video analysis seemed necessary due to their restlessness (one way of being “hard to test”). As a side note, these were also the two children with “suspected CAS” in the original assessment. It is possible that their being hard to test made speech diagnosis more challenging under both standard and more playful assessment conditions.
From the qualitative notes, the following potential sources of error remain:
In two instances, scoring points were missing due to time pressure or distraction during the examination, resulting in missing values. Lack of time for observations and for noting useful cues may also have hampered thorough information gathering.
Spontaneous speech analysis presents a somewhat bigger challenge. Directly transcribing utterances in real time is a demanding task; data collected demonstrate that complete transcription during the testing session is unfeasible, with only about two-thirds of speech material being captured.
While one could argue that immediate transcription is closer to natural communication situations and that repeated viewing/listening to the video might affect subjective intelligibility, previous research has also reported a risk of overestimating intelligibility due to insufficient notation of hard-to understand-words (Wolk and Meisler, 1998).
Errors can also arise due to auditory distortion through an observation window when watching from an adjacent room. Furthermore, incomplete live transcription could result in a different set of utterances being analyzed compared to video analysis, resulting in discrepancies in calculated intelligibility and average utterance length between the two data sources. Vowel and initial consonant repertoires could be documented quite easily by live transcription. However, live documentation of complex syllable structures in talkative children (P7, P8) was difficult. It seems they can only be fully, accurately captured by video analysis. In live transcription, a significant portion of those data is lost.
Overall, for spontaneous speech samples there seems to be a choice between a time-consuming video-based analysis or some imprecision in recording and calculation. In a recent update, the authors of the assessment have proposed using a symptom checklist while observing spontaneous speech as a time-saving alternative (Velleman et al., 2022). This might be the more efficient option for assessing motor speech abilities. Nevertheless, from a clinical perspective, it seems advisable to try and record the sound inventory as well as word shapes (possibly also via checklists).
Overall, there may be advantages to foregoing video analysis when time is limited, as the discrepancy in quality appears justifiable. Nonetheless, it should be acknowledged that this approach may not be appropriate in every instance. In situations where uncertainty arises, conducting an analysis from video, especially for difficult sections, could prove valuable.
Overall, a flexible, playful approach to differential diagnosis of CAS can be seamlessly integrated into existing diagnostic processes, despite the fact that it does require some extra implementation time.
6 Limitations of the study
As a series of single case studies, this study is limited by group size; any results can only be preliminary. In addition, all assessments were administered by the same person, which might have affected outcomes to some extent. All qualitative evaluation was based on (years of) individual experience. This is especially important with regard to the idea of omitting video analysis.
Due to the small and exploratory nature of the study, minimal effort was made to reduce bias, aside from having two persons review the wording of the caregiver's questionnaire. The wording of some of the questions (e.g., “My child showed no signs of refusal”, which was phrased in the negative for scoring consistency) could have impacted responses.
Last but not least, all assessment for this study was done during the Covid 19 pandemic and therefore with strict hygiene measures. One cannot rule out the possibility that the examiner's FFP2-mask could have slightly altered the children's perception of the models, especially for non-word repetition, or that some restraint on the examiner's part impacted the use of tactile cues when children had difficulty achieving a task. Children were not required to wear masks.
7 Conclusions and clinical implications
In this exploratory study, the “Language Neutral Assessment of Motor Speech in Young Children” (LAMS), was implemented for the first time in the German speaking region, where there is no standardized procedure for diagnosing CAS. It was primarily assessed for feasibility of a flexible, play-based motor speech assessment in a clinical context through a series of single case studies.
Our results suggest that a play-based assessment (that ideally includes a spontaneous speech sample) can fill a gap in the German speaking world. Children and caregivers seem to accept it well; a mostly complete assessment is doable. Flexible test administration is practicable, except for the time required for the full procedure. However, omitting video analysis seems a plausible solution without risking loss of essential information. For the 2017 version of the LAMS, further recommended steps include taking language specific issues into account for the spontaneous speech sample, or—as has been done for the current (2024) version—changing to a checklist.
In conclusion, the answer to whether a play-based, flexible tool like the LAMS is a feasible assessment in the German-speaking region is undoubtedly positive, providing preliminary support for the hypotheses of this study.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics commission of the Faculty of Medicine, Johannes Kepler University Linz, Austria (approval number EK 1292/2020). The studies were conducted in accordance with local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
GE: Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Project administration, Data curation, Investigation, Formal analysis. SV: Supervision, Writing – review & editing. DH: Writing – review & editing, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Johannes Kepler Open Access Publishing Fund and the federal state Upper Austria.
Conflict of interest
SV is a co-author of the Language-neutral Assessment of Motor Speech (LAMS), which was featured in this paper and will be published by Academic Therapy Publications within the next few years.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2025.1470869/full#supplementary-material
Footnotes
1. ^“Dynamic Evaluation of Motor Speech Skills.”
2. ^The various parts of the test are coded for scoring purposes (e.g. 4A ‘Vowel Sequences'); some figures and tables will refer to these codes (see Appendix II).
3. ^The scoring has been changed to 2-1-0 since then (2 = “within normal limits”).
4. ^See Appendix III.
References
Allison, K. M., Cordella, C., Iuzzini-Seigel, J., and Green, J. R. (2020). Differential diagnosis of apraxia of speech in children and adults: a scoping review. J. Speech Lang. Hear. Res. 63, 2952–2994. doi: 10.1044/2020_JSLHR-20-00061
American Speech-Language-Hearing Association. (2007). Childhood Apraxia of Speech: [Technical Report]. Rockville, MD: American Speech-Language-Hearing Association.
Bowen, D. J., Kreuter, M., Spring, B., Cofta-Woerpel, L., Linnan, L., Weiner, D., et al. (2009). How we design feasibility studies. Am. J. Preventive Med. 36, 452–457. doi: 10.1016/j.amepre.2009.02.002
Erlacher, G. (2021). Machbarkeit der Diagnostik einer sprechmotorischen Störung im Kindesalter mithilfe des Language-Neutral Assessment of Motor Speech in Young Children (LAMS): [Feasibility of assessing a motor speech disorder with the Language-neutral Assessment in Young Children (LAMS)] (master's thesis). University of Salzburg, Salzburg, Austria.
Föllner, S. (2015). VED bei Kindern [Developmental verbal dyspraxia in children]. Schulz-Kirchner Verlag GmbH, Germany.
Fox-Boyer, A. (2016). Kindliche Aussprachestörungen [Speech sound disorders in children], 8th Edn. Idstein: Schulz-Kirchner Verlag.
Iuzzini-Seigel, J., Allison, K. M., and Stoeckel, R. (2022). A tool for differential diagnosis of childhood apraxia of speech and dysarthria in children: a tutorial. Lang. Speech Hear. Serv. Sch. 53, 926–946. doi: 10.1044/2022_LSHSS-21-00164
Iuzzini-Seigel, J., Hogan, T. P., and Green, J. R. (2017). Speech inconsistency in children with childhood apraxia of speech, language impairment, and speech delay: depends on the stimuli. J. Speech Lang. Hear. Res. 60, 1194–1210. doi: 10.1044/2016_JSLHR-S-15-0184
Murray, E., Iuzzini-Seigel, J., Maas, E., Terband, H., and Ballard, K. J. (2021). Differential diagnosis of childhood apraxia of speech compared to other speech sound disorders: a systematic review. Am. J. Speech Lang. Pathol. 30, 279–300. doi: 10.1044/2020_AJSLP-20-00063
Murray, E., McCabe, P., Heard, R., and Ballard, K. J. (2015). Differential diagnosis of children with suspected childhood apraxia of speech. J. Speech Lang. Hear. Res. 58, 43–60. doi: 10.1044/2014_JSLHR-S-12-0358
Murray, E., Velleman, S., Preston, J. L., Heard, R., Shibu, A., McCabe, P., et al. (2023). The reliability of expert diagnosis of childhood apraxia of speech. J. Speech Lang. Hear. Res. 67, 1–18. doi: 10.1044/2023_JSLHR-22-00677
Obry, S., and Siegmüller, J. (2013). Handbuch Spracherwerb und Sprachentwicklungsstörungen: Vol. 1. Schuleingangsphase: Sprechapraxie in der Schuleingangsphase (1. Auflage). Munich: Elsevier GmbH Urban Fischer Verlag.
Rupela, V., Velleman, S. L., and Andrianopoulos, M. V. (2016). Motor speech skills in children with down syndrome: a descriptive study. Int. J. Speech Lang. Pathol. 18, 483–492. doi: 10.3109/17549507.2015.1112836
Shriberg, L. D., Lohmeier, H. L., Strand, E. A., and Jakielski, K. J. (2012). Encoding, memory, and transcoding deficits in childhood apraxia of speech. Clin. Ling. Phonetics 26, 445–482. doi: 10.3109/02699206.2012.655841
Shriberg, L. D., Strand, E. A., Fourakis, M., Jakielski, K. J., Hall, S. D., Karlsson, H. B., et al. (2017). A diagnostic marker to discriminate childhood apraxia of speech from speech delay: I. Development and description of the pause marker. J. Speech Lang. Hear. Res. 60, S1096–S1117. doi: 10.1044/2016_JSLHR-S-15-0296
Siegmüller, J., and Bartels, H. (2017). German Medical Collection: Vol. 63. Leitfaden Sprache, Sprechen, Stimme, Schlucken, 5th Edn. Munich: Elsevier.
Snyder, E. (2010). A comparison of single word identification, connected speech samples, and imitated sentence tasks for assessment of children with a SSD (master's thesis). Portland State University, Portland, OR, USA.
Strand, E. A., McCauley, R. J., Weigand, S. D., Stoeckel, R. E., and Baas, B. S. (2013). A motor speech assessment for children with severe speech disorders: reliability and validity evidence. J. Speech Lang. Hear. Res. 56, 505–520. doi: 10.1044/1092-4388(2012/12-0094)
Thabane, L., Ma, J., Chu, R., Cheng, J., Ismaila, A., Rios, L. P., et al. (2010). A tutorial on pilot studies: the what, why and how. BMC Med. Res. Methodol. 10:1. doi: 10.1186/1471-2288-10-1
Velleman, S. L., Andrianopoulos, M., and Rupela, V. (2017). “Language-neutral assessment of motor speech (LAMS): administration manual (unpublished),” Communication Sciences and Disorders. University of Vermont.
Velleman, S. L., Andrianopoulos, M., and Rupela, V. (2022). “Language-neutral assessment of motor speech (LAMS): administration manual (unpublished),” Communication Sciences and Disorders. University of Vermont.
Keywords: childhood apraxia of speech, feasibility, motor speech, diagnosis, LAMS, assessment
Citation: Erlacher G, Velleman SL and Holzinger D (2025) Clinical feasibility of a play-based assessment of motor speech disorders in young children in Austria. Front. Commun. 10:1470869. doi: 10.3389/fcomm.2025.1470869
Received: 26 July 2024; Accepted: 20 June 2025;
Published: 10 July 2025.
Edited by:
Sarah Masso, The University of Sydney, AustraliaReviewed by:
Isabel Reyes Rodríguez-Ortiz, Sevilla University, SpainAnnette Fox-Boyer, University of Lübeck, Germany
Copyright © 2025 Erlacher, Velleman and Holzinger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gertraud Erlacher, Z2VydHJhdWQuZXJsYWNoZXJAamt1LmF0
 Gertraud Erlacher
Gertraud Erlacher Shelley L. Velleman3
Shelley L. Velleman3 Daniel Holzinger
Daniel Holzinger