- 1College of Nursing, University of Utah, Salt Lake City, UT, United States
- 2Primary Children’s Hospital, University of Utah Health, Salt Lake City, UT, United States
- 3Department of Psychology, University of Utah, Salt Lake City, UT, United States
Introduction: Screening for unmet social needs (such as food or housing insecurity) in healthcare settings has the potential to promote patient health by connecting them with needed resources, but many patients decline to complete screening instruments. The purpose of this paper was to identify the barriers and facilitators of patient participation in social needs screening.
Methods: Between December 2022 and March 2023, we conducted four virtual focus groups with community-dwelling adults regarding social needs screening questions. Our sample included 32 adults (10 English-speaking and 22 Spanish-speaking). Based on current theoretical models of human threat vigilance, we coded participant speech into two broad categories: social threat (such as vulnerability, exclusion, and aggression) and social safety (such as helpfulness, inclusivity, and predictability). NVivo software was used to conduct qualitative analysis between May and December 2023.
Results: Participants discussed social threats seven times more often than they discussed social safety, and all of these social threats were expectations (rather than experiences). In contrast, communication surrounding social safety centered on previous positive experiences, rather than expectations.
Discussion: These results align with the notion that human brains maintain a default state of threat vigilance until cues of safety and inclusion are detected. Accordingly, the only way to increase screening rates is to “head off” patients’ automatic threat vigilance with clear and concrete communication of social safety, before they are even given a screening instrument. These findings can assist healthcare organizations in developing “safety first” communication practices and screening protocols that can enhance screening and rates of successful follow-up.
Introduction
The role that social factors play in influencing health is commonly recognized. The WHO reports that social determinants of health (SDOH)—the conditions in which people are born, grow, work, live, and age—account for up to 55% of health outcomes (World Health Organization, n.d.). Other research suggests that SDOH may account for up to 85% of health outcomes (Hood et al., 2016). To facilitate the positive influence of SDOH on health and ultimately improve population health, healthcare organizations have begun integrating social needs screening and resource referrals into routine care (National Academies of Sciences, Engineering, and Medicine, 2019). Screening for unmet social needs and addressing those needs can potentially prevent adverse health outcomes. Despite this integration, many individuals decline to complete social needs screening and or decline outreach by resource navigators (Kulie et al., 2021; Schickedanz et al., 2019; Wallace et al., 2020). To improve the screening process to capture a broader swath of the population, we need to understand why some patients decline screening.
Our previous research shows the sizeable gaps in our screening processes: We developed and validated SINCERE, a 10-item social needs screening instrument (Wallace et al., 2020; Wallace et al., 2021; Guo et al., 2022). This instrument asks participants if they have experienced the following unmet social needs in the past month: transportation, medical expenses, medication expenses, food, material goods, utilities, rent/mortgage, housing, employment, and childcare/eldercare. Between January 2019 and February 2020, we approached 4,608 individuals in a Level I Trauma Center Emergency Department (ED) in the Intermountain West to conduct social needs screening using SINCERE (Wallace et al., 2021). Of the 4,608 approached, 1787 (38%) declined the screening. Of those screened, 47% reported at least one unmet social need. Among these 1,324 patients, only 453 (34%) agreed to be contacted with community resource referrals after discharge, and only 21% were contacted. Hence, a screening process applied to 4,608 patients yielded only 95 “hits,” in which unmet needs were identified and responded to—representing only 2% of the patients approached (additional details published elsewhere) (Wallace et al., 2021). We need to retain more patients in all phases of the screening process to adequately address social determinants of health (Wallace et al., 2021; Husk et al., 2020). The purpose of this follow-up study was to identify specific factors impeding or facilitating social needs screening and referral processes. Gaining an improved understanding of individuals’ hesitancy to respond to social needs screening questions or to decline outreach by an information specialist can improve the screening process to successfully address patients’ needs.
Theoretical framework
This study takes a phenomenological approach, rooted in the constructivist research paradigm, as we were interested in understanding participants’ lived experiences of social needs screening and referral processes (Pilarska, 2021). Our study is grounded in two related theoretical models within health psychology, specifically the Generalized Unsafety Theory of Stress (GUTS) (Brosschot et al., 2018) and Social Safety Theory (Slavich, 2020), both of which align with constructivist views that “social and cultural realities to be investigated are subjective.” (Pilarska, 2021) GUTS theory posits that chronic threat vigilance is the baseline state for the human nervous system because humans evolved in dangerous and uncertain environments, in which it was adaptive to maintain a default state of wariness. According to GUTS, automatic threat vigilance is only disengaged by unmistakable safety cues. Slavich’s Social Safety Theory expands these insights by showing that the most important safety cues are social. Humans are a social species deeply dependent on the group for survival and therefore need social inclusion and protection to feel safe and secure. Accordingly, the most powerful “off switch” for chronic threat vigilance communication and interaction with a warm, affirmative, and protective human being.
Two major insights about healthcare screening derive from these models: First, patients in healthcare settings are likely to occupy a threat-vigilant state, given that these settings provoke feelings of vulnerability and uncertainty. Thus, patients may have negative and threatening expectations of screening before even knowing the screening questions or how the process might help them. Essentially, patients already experience heightened defensiveness when the healthcare screener approaches them. This leads us to expect that the most common reasons for declining the screening process and or outreach are expectations of social threats, such as rejection, abandonment, and judgment (as opposed to disinterest or a lack of time). The second major insight is that interpersonal cues of safety from the screener, such as warmth, empathy, and responsive communication, can play a primary role in disengaging patients’ chronic threat vigilance and motivating their engagement in screening and referral processes. GUTS and Social Safety Theory indicate that humans do not need clear evidence to feel threatened. Rather, social fear is part of the brain’s default response to uncertainty. When patients have a warm, affirming, authentic, and respectful interaction with a screener, it should cue the nervous system to “call off the guard dogs,” making patients more likely to engage. By examining participant responses through the framework of Social Safety and GUTS theories, our findings can directly inform efforts to create communication and social-needs screening processes that successfully capture patients with the greatest needs.
Materials and methods
Study sample
Participants included 10 English- and 22 Spanish-speaking community-dwelling individuals, recruited via word-of-mouth, flyers, and snowball sampling by the University of Utah Clinical and Translational Science Institute’s (CTSI) Community Collaboration and Engagement Team (CCET). Focus group size followed best practices for conducting focus groups in qualitative research which suggest a sample of between seven and 12 participants per group (Marshall and Rossman, 2014). Participants were consecutively grouped into four focus groups, which were conducted between December 2022 and March 2023. The focus group in English contained eight participants, and the remaining three in Spanish had eight, nine, and nine participants, respectively.
CCET sent potential participants a screening questionnaire to verify their eligibility. As the study team wanted to obtain information from individuals representing the “typical users” of the SINCERE screening tool—which was designed for implementation in medical settings—participants were eligible if they were over 18 years of age, English or Spanish speaking, and had a healthcare visit for themselves or their child in the past year. Focus groups were facilitated by CCET staff, who are bilingual and bicultural. The research team had no prior relationship with the study participants. However, the researchers acknowledged that their personal attributes may influence the research throughout the scientific process. Researchers were US-based investigators from the disciplines of nursing, social work, psychology, pediatric medicine, and informatics. To enhance reflexivity, researchers engaged in frequent open dialogue regarding how their experiences and attributes may influence their assumptions or interactions.
Measures
To characterize the participants involved in our focus groups, CCET collected the following demographic information from participants before the focus group via a questionnaire which was emailed to participants: age, sex assigned at birth, gender, sexual orientation, ethnicity, race, annual household income, religious affiliation, highest level of education, neighborhood characteristics (rural, suburban, urban), zip code, and the number of people in the household for additional data collected (Wallace et al., 2021).
Procedure
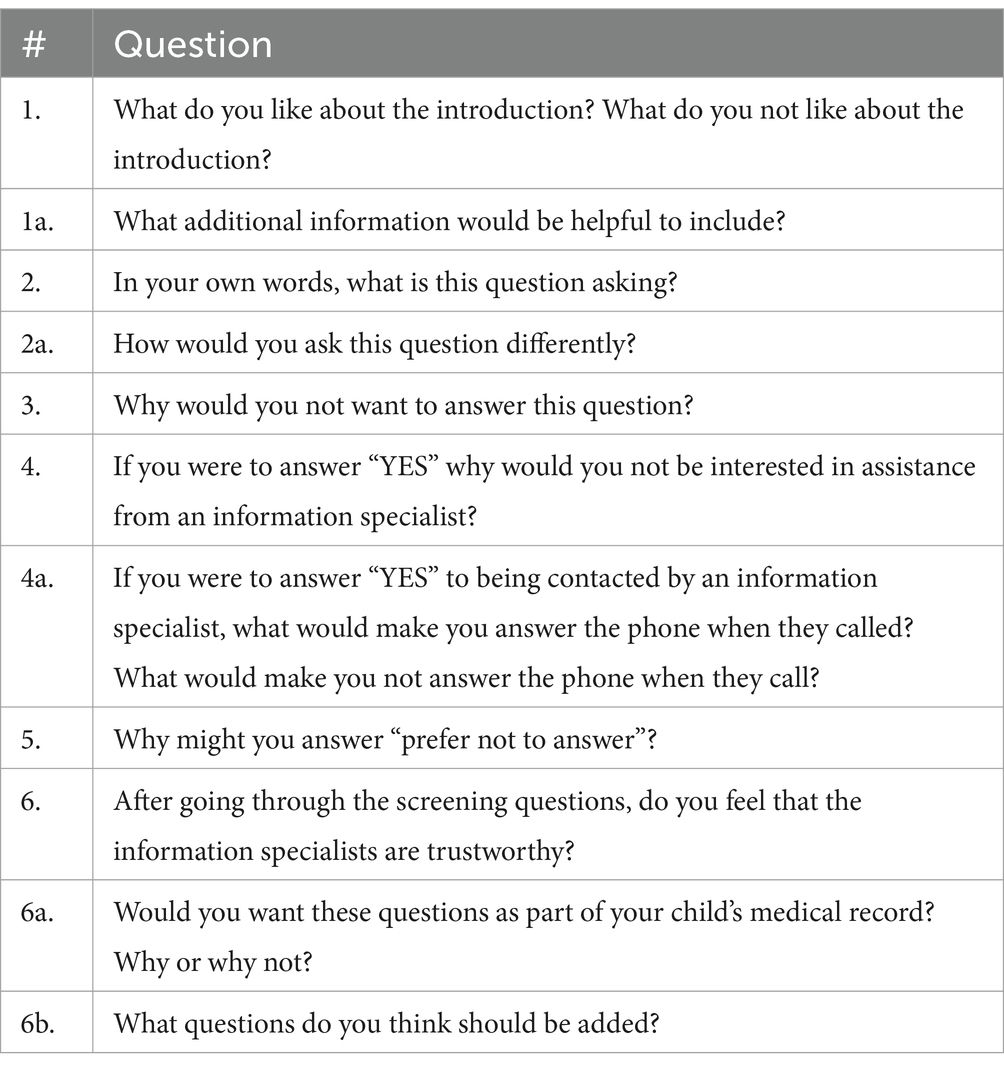
This study was approved by the IRB number. Before the focus group, participants received electronic copies of the consent form, a copy of the 10-item screening instrument, and focus group questions. Questions centered on participants’ responses to the screening instrument, including the introductory explanation offered when patients are approached about the instrument (see Table 1). Focus group questions did not change from group to group or throughout the study, as they focused on each question within the screening instrument and whether the question was understandable to participants.
We obtained free and informed consent of all participants. Focus groups were conducted virtually using secure videoconferencing software and began with an introduction of the research team and the reasons for the study. Focus groups lasted on average 98.7 min (SD = 11.09, range = 87–113). They were video-recorded via Zoom, transcribed verbatim by professional transcription services, translated into English (if they were conducted in Spanish), and uploaded into NVivo qualitative analysis software (QSR International Pty Ltd, 2018). One CCET staff member facilitated the focus groups, and one took field notes and monitored the chat function on the videoconferencing platform.
Analytic plan
Analysis occurred between May and September 2023. Demographic characteristics were summarized with descriptive statistics including percentages, means, and SDs. Thematic coding and directed content analysis were applied to code the focus group transcripts and to differentiate between discussions of social threat and social safety (Assarroudi et al., 2018). The primary coder read the transcripts and used NVivo (QSR International Pty Ltd, 2018) qualitative software to define units of analysis—meaningful units of participant speech that introduced factors constituting social safety or social threat.
Using a combination of deductive concepts derived from Social Safety theory (inclusion, validation, predictability, authenticity, aggression, devaluation, discrimination, rejection, exclusion) and inductive concepts from the focus group transcripts (reassurance, sincerity, breach of confidentiality, insincerity, shame/guilt/embarrassment, lack of information/misinformation, vulnerability), the primary coder developed a list of codes related to social safety and social threats. Initial definitions and exemplar quotes were added to code labels in the development of a codebook. The research team reviewed the codebook until a consensus was reached on all code labels and definitions and collectively coded one focus group transcript using this codebook. Revisions were made to the codebook based on team members’ feedback.
The primary and second coders utilized this revised codebook to double-code one focus group transcript. The following process of unitization (Campbell et al., 2013) was used to improve intercoder reliability: (1) the primary coder coded the transcript using the codebook, (2) the primary coder removed the code labels from the coded excerpts but left the excerpts highlighted, (3) the second coder applied a code to each highlighted excerpt using the codebook. This process improves intercoder reliability by removing the need for the second coder to establish the length of a code in addition to the application of the code name (Campbell et al., 2013). Intercoder reliability was calculated using NVivo software, resulting in a Cohen’s Kappa of 0.66, indicating good agreement (Landis and Koch, 1977). The two coders discussed data saturation and coding discrepancies and revised the coding rules and code definitions until a consensus was reached on all codebook material. Each coder then independently coded one additional focus group transcript (see Supplementary material for the codebook).
Results
Demographic data
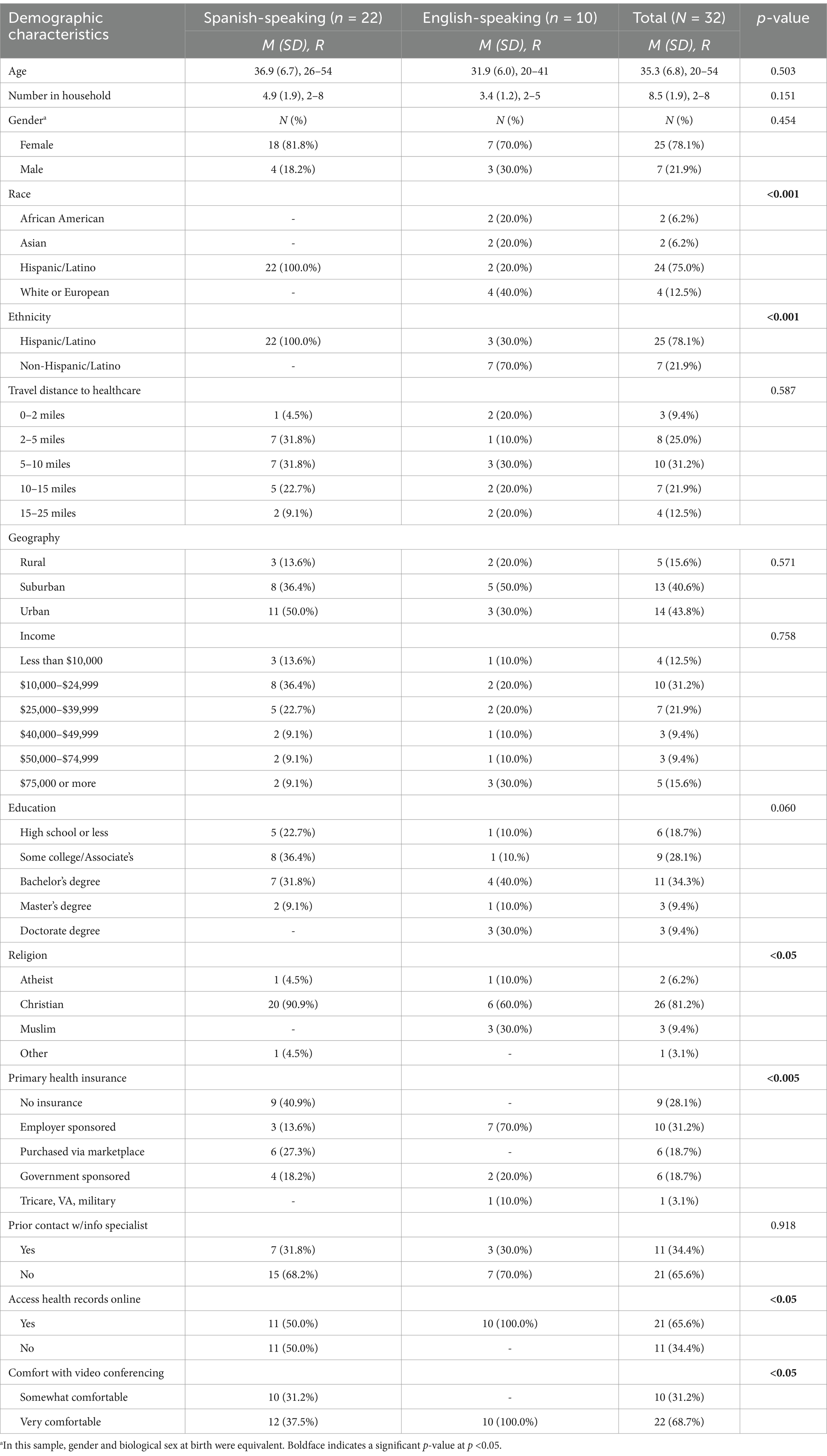
Participants were 35.3 years on average (SD = 6.8 L; Range = 20–54). Most participants were female 25 (78.1%) and identified their ethnicity as Hispanic/Latino (n = 25, 78.1%). Participants lived in urban (n = 14, 43.8%), suburban (n = 13, 40.6%), or rural areas (n = 5, 15.6%). Of the sample, 21 (65.6%) reported no prior contact with an information specialist. See Table 2 for all demographic characteristics.
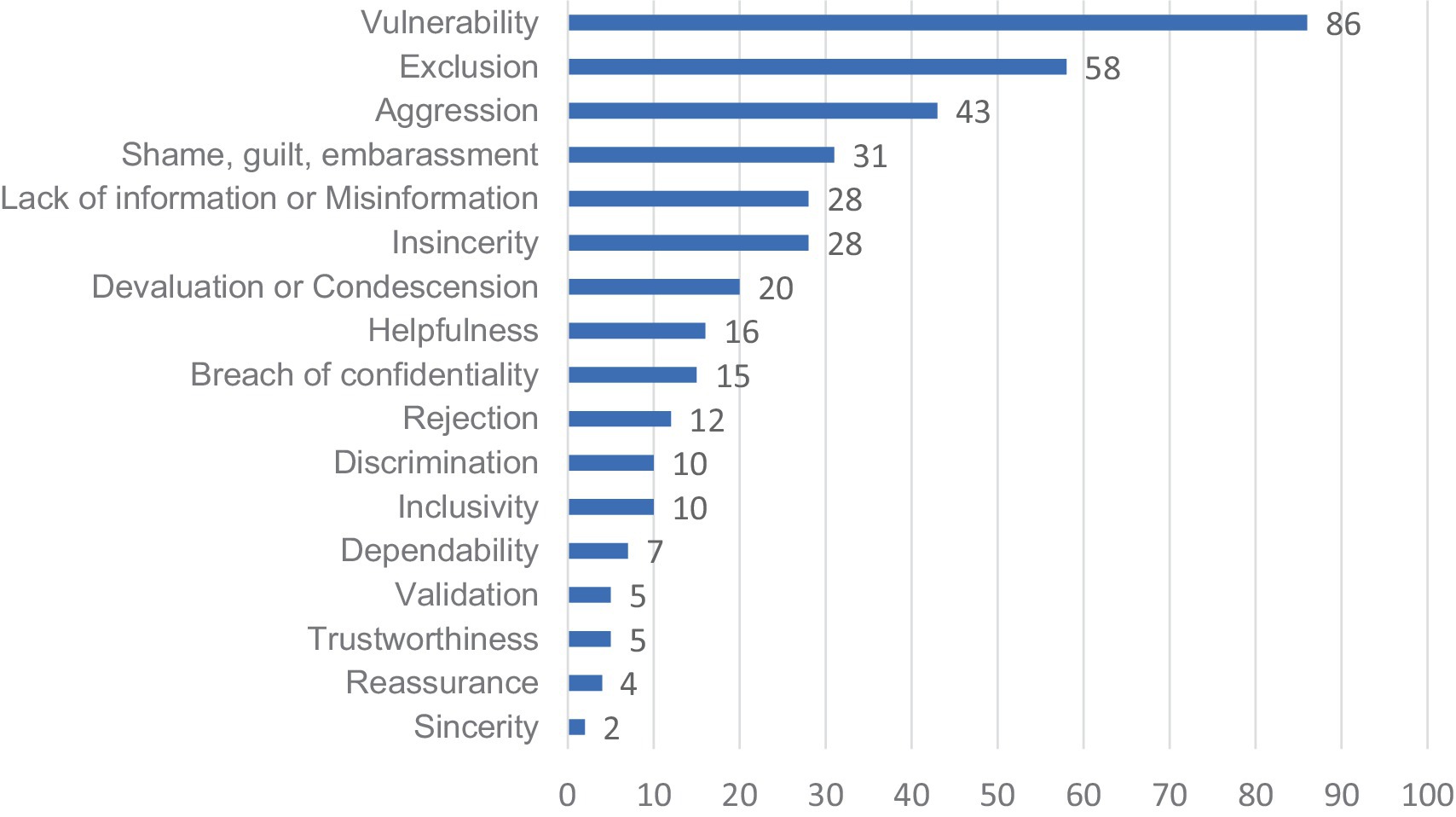
Social safety
Forty-nine codes related to social safety were applied among the four focus group transcripts, constituting 12.9% of all codes (see Figure 1 for a graph of coding frequencies). Social safety codes included predictability, helpfulness, inclusivity, reassurance, sincerity, authenticity, and validation (see appendix for the final codebook with all code labels, definitions, and example quotations). The subcodes within social safety that were most frequently reported were helpfulness (n = 16, 4.2% of all codes), inclusivity (n = 10, 2.6%), and predictability (n = 7, 1.8%).
The subcode helpfulness involved participants feeling as if the individual doing the screening, offering resources, or within a community service organization operates in a way that will relieve burden and meet their reported needs. For example, one participant stated that the information specialist, “connected me to what I was looking for, so I thought it was awesome.” Another participant described needing help finding a tutor for their child and stated that the information specialist, “found me a free program so I could get a tutor.”
Inclusivity was reported when participants felt the community resource, organization, or person conducting the screening was culturally welcoming and that the resource, organization, or help offered was meant for people like them or in their situation. A participant shared their experience of inclusivity by relaying that the information specialists speak other languages besides Spanish and English. Another participant recounted that a rideshare program they had wanted to utilize was initially unavailable in Provo but that 4 months later, “It was finally available in Provo. So that seemed really great to me.”
Predictability involved instances wherein participants felt they could count on the person conducting the social needs screening, the information specialist, or another community resource; participants felt the resource was reliable and would follow through with what they promised. For example, one focus group participant had indicated on a postpartum screening that they felt sad, unmotivated, and were experiencing anhedonia: “They called me. And that was really comforting for me and it was easier to connect and have them follow through by calling you, instead of giving you a piece of paper with the information.” For this participant, it was reassuring that the pediatrician’s office followed up as promised and called the participant with resources related to depression.
Social threats
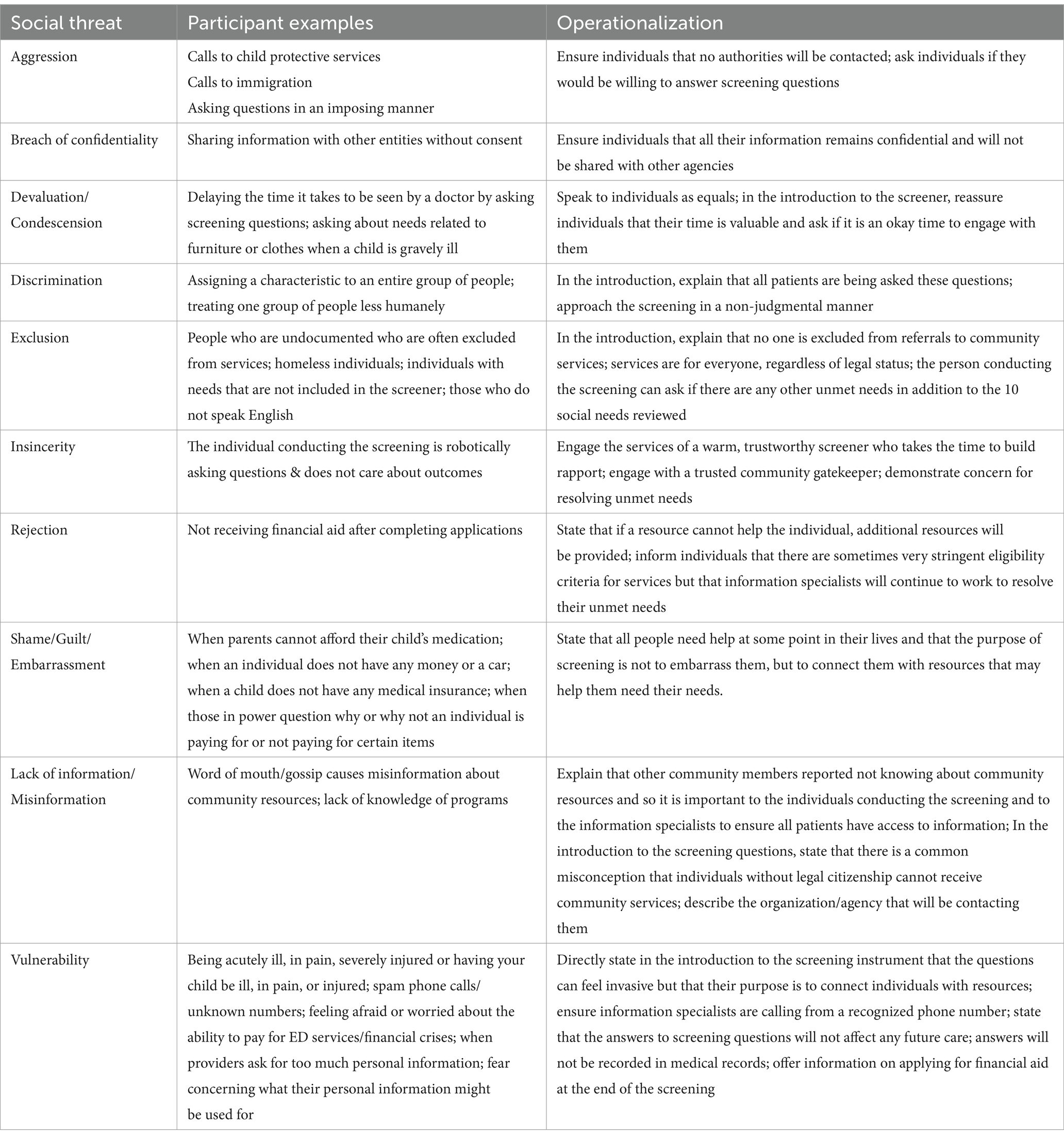
Social threats included the following subcodes: aggression, breach of confidentiality, devaluation or condescension, discrimination, exclusion, insincerity, rejection, shame/guilt/embarrassment, lack of information or misinformation, and vulnerability (see appendix for all code definitions). Across all transcripts, social threats were coded 331 times, representing 87.1% of all codes. Vulnerability (n = 86, 22.6%) was the subcode most frequently reported, followed by exclusion (n = 58, 15.3%) and aggression (n = 43, 11.3%).
Vulnerability involved feeling afraid, defensive, or susceptible to physical, emotional, or financial attack, harm, or damage and was specific to an external threat; participants frequently referred to being sick, seeking medical care in an ED, or simply asking for help in a vulnerable situation. One participant stated, “It’s just a very hard and vulnerable situation to put yourself in and to ask for help.” In responding to the screening question about having enough food to eat, another participant reported, “This question is more invasive, I’m not saying that it’s bad, but it’s more invasive, it’s more private. I do not have to answer if I’ve got food in my house or not, I came here to get treated.”
Exclusion involved participants feeling left out of the offered help and as though their beliefs were not considered or as if help was not designed with participants’ beliefs in mind. For example, in thinking about why someone might choose not to answer the screening questions, a participant said, “A lot of undocumented people can say, ‘Well, these services are provided, but are they provided for me?’”
Aggression was defined as fear or threat of action(s) such as involvement with child protective services, eviction, deportation, violence, or the use of hostile language or a hostile attitude. When asked why someone would choose not to answer one of the screening questions, a participant said, “Families do not answer questions because they are worried it will lead to repercussions of child protective services being contacted for neglect. So they refuse to answer.” Another participant posited, “Some people may worry that answering this could affect their living situation; if it were reported to their apartments, they would get kicked out.”
Discussion
The present research demonstrates that screening procedures aimed at identifying and addressing patients’ unmet social needs must account for patients’ preexisting fears and negative expectations, which may impede the screening process or prevent patients from following through on referrals. Seeking medical care places individuals in a state of vulnerability, heightening their attention to potential dangers (such as breaches of confidentiality). While other research has previously highlighted participant concerns regarding confidentiality and feelings of uncertainty regarding the resources offered (Hare et al., 2023), GUTS theory helps to make sense of these findings by clarifying that chronic threat vigilance is the default state for the human nervous system. The fact that social threat codes typically involved expectations, fears, and perceptions, rather than concrete experiences, shows that we must assess and address these negative expectations before attempting to administer any screening. Some of the anticipated social threats may also be more than expectations. For example, while participants may have phrased their responses as future concerns, these could have been based in prior real-life experiences of social threats.
The high frequency of social threat codes in the present study may also reflect patients’ prior negative experiences in medical and service settings: Many participants shared stories (their own and others’) of harmful breaches of personal information or punitive legal consequences of speaking frankly to medical providers. Negative experiences and expectations may be particularly likely among historically marginalized and underserved populations (such as the Spanish-speaking participants in the present study), as research demonstrates 20% of Latinos reported discrimination in medical encounters (Findling et al., 2019).
A key finding of the present study is that the best way to counteract patients’ negative fears and expectations may be with affirmative, warm, respectful, and helpful behavior and communication (see Table 3 for perceived social threats and potential remedies). Consistent with this view, participants’ discussions of social safety centered on specific acts or interpersonal experiences such as calling a participant back, demonstrating reliable follow-up, and the role of interpersonal warmth and empathy in creating a climate of safety. These findings (from potential service users) are consistent with views described by social prescribing service providers on the importance of adopting a person-centered approach (Cooper et al., 2024). For Hispanic/Latino participants, these findings may reflect familismo, a cultural value referring to the importance of family closeness and “getting along with and contributing to the wellbeing of the nuclear family, extended family, and kinship networks” (Ayón et al., 2010). Individuals engaging with Hispanic/Latino participants may be seen as extended networks, emphasizing the importance of creating a safe and warm environment. In sum, the screening and referral process cannot be achieved without adopting a person-centered approach which first establishes a baseline of safety with the patient.
The fact that participants mentioned far more social threats in their focus group discussions (n = 331, 87.1%) than social safety experiences (n = 49, 12.9%), underscores that patients start with a baseline state of threat vigilance which must be actively down-regulated before screening begins. As the authors of GUTS state, “Our bodies do not necessarily react to stressful events, but rather cease reacting when safety is perceived or when safety would have been perceived by our ancestors” (Brosschot, 2017). In sum, our findings have transferability across health systems as anticipating and addressing perceived social threats can be achieved regardless of screening instrument or method of administering screening for social needs.
Limitations
This study is limited by the relatively small sample size and by the overrepresentation of Hispanic/Latino and male voices. Among Hispanic/Latino participants, cultural norms of collectivism, family values, and attitudes towards healthcare could influence the perceptions of social needs screening. In fact, many of our Spanish-speaking participants indicated that it can be difficult for Hispanics/Latinos to ask for help, due to cultural norms that discourage dependency and prize self-reliance in times of adversity (Fregoso, 2024). Our sample was consecutively enrolled and engaged in conversation via focus groups, which could either suggest participants may represent those who were more eager to share their experiences or that some participants may have not felt comfortable discussing sensitive topics. This study may therefore not capture the breadth of experiences of individuals being screened for unmet social needs. Future research should include a larger and more diverse sample of participants in order to capture a wider range of perspectives and to understand how different social positions influence the social needs screening process. Despite these potential limitations, our results suggest that establishing a climate of safety and trust with patients at each stage of the screening process is critical to increase rates of screening and follow-up. The more screeners can address and counteract patients’ negative expectations with warm, trustworthy, authentic behavior, the more successful the screening process will be.
Conclusion
While screening for and responding to unmet social needs is critical for improving population health, the individuals with the greatest social needs may be least likely to complete the screening process if it does not directly address their unspoken fears and disconfirm their negative expectations. Accordingly, the priority for the screener should be establishing safety and trust with the patient, with a combination of interpersonal warmth and clear communication (in the patient’s language). It is particularly critical to clarify that help and assistance is available to all, regardless of immigration status, and that there will be no legal ramifications for participating in the screening process or accepting help. The more the screener can establish a climate of warmth, responsiveness, and authentic helpfulness, the more successful the screening and referral process will be. Establishing a sense of safety may yield significant gains in the number of patients completing the screening process and receiving assistance with unmet needs. By assuming that all patients start out with negative fears and expectations and designing the screening process to respond to these fears, we will be better able to identify and address the unmet social needs that are known to affect health and well-being.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University of Utah Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because Written informed consent was obtained but this was not an option in the drop down questions. Question number 4 was answered ‘no’ because our participants were all over 18 years of age and were therefore able to sign consent for themselves and thus we did not need the signature of a guardian.
Author contributions
SB: Conceptualization, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. NT: Formal analysis, Validation, Writing – original draft, Writing – review & editing. EG: Investigation, Project administration, Writing – original draft, Writing – review & editing. BL: Conceptualization, Validation, Writing – original draft, Writing – review & editing. J-WG: Validation, Writing – original draft, Writing – review & editing. BW: Project administration, Writing – original draft, Writing – review & editing. LD: Conceptualization, Writing – original draft, Writing – review & editing. AW: Conceptualization, Funding acquisition, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Sara Bybee, Natalie Tedford, Brenda Luther, Jia-Wen Guo, Bob Wong, and Andrea Wallace would like to acknowledge the funding received through the National Institutes of Nursing Research (1R01NR019944-01).Natalie Tedford discloses that research reported in this publication was supported by the American Academy of Pediatrics Community Access to Child Health Implementation Grant (award number 2688).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2025.1558250/full#supplementary-material
References
Assarroudi, A., Heshmati Nabavi, F., Armat, M. R., Ebadi, A., and Vaismoradi, M. (2018). Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process. J. Res. Nurs. 23, 42–55. doi: 10.1177/1744987117741667
Ayón, C., Marsiglia, F. F., and Bermudez-Parsai, M. (2010). Latino family mental health: exploring the role of discrimination and familismo. J. Commun. Psychol. 38, 742–756. doi: 10.1002/jcop.20392
Brosschot, J. F. (2017). Ever at the ready for events that never happen. Eur. J. Psychotraumatol. 8:1309934. doi: 10.1080/20008198.2017.1309934
Brosschot, J. F., Verkuil, B., and Thayer, J. F. (2018). Generalized unsafety theory of stress: unsafe environments and conditions, and the default stress response. Int. J. Environ. Res. Public Health 15:464. doi: 10.3390/ijerph15030464
Campbell, J. L., Quincy, C., Osserman, J., and Pedersen, O. K. (2013). Coding in-depth Semistructured interviews: problems of unitization and Intercoder reliability and agreement. Sociol. Methods Res. 42, 294–320. doi: 10.1177/0049124113500475
Cooper, M., Flynn, D., Scott, J., Ashley, K., and Avery, L. (2024). Barriers and facilitators to the design and delivery of social prescribing services to support adult Mental health: perspectives of social prescribing service providers. Health Soc. Care Commun. 2024:5581012. doi: 10.1155/2024/5581012
Findling, M. G., Bleich, S. N., Casey, L. S., Blendon, R. J., Benson, J. M., Sayde, J. M., et al. (2019). Discrimination in the United States: experiences of Latinos. Health Serv. Res. 54, 1409–1418. doi: 10.1111/1475-6773.13216
Fregoso, J. (2024). “Beyond the bootstraps mentality: the fallacy of grit as a measure of success for black and Latine/x men in California community colleges” in A. M. Locks, R. Mendoza, D. F. Carter (eds.) Debunking the grit narrative in higher education (New York: Routledge), 135–157.
Guo, J. W., Wallace, A. S., Luther, B. L., and Wong, B. (2022). Psychometric evaluation of the screener for intensifying community referrals for health. Eval. Health Prof. 45, 270–276. doi: 10.1177/01632787211029360
Hare, A. J., Honig, K., Cronholm, P. F., Shabazz-McKlaine, S., and Morgan, A. U. (2023). Patient perspectives on technology-based approaches to social needs screening. Am. J. Manag. Care 29, e18–e23. doi: 10.37765/ajmc.2023.89309
Hood, C. M., Gennuso, K. P., Swain, G. R., and Catlin, B. B. (2016). County health rankings: relationships between determinant factors and health outcomes. Am. J. Prev. Med. 50, 129–135. doi: 10.1016/j.amepre.2015.08.024
Husk, K., Blockley, K., Lovell, R., Bethel, A., Lang, I., Byng, R., et al. (2020). What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health Soc. Care Commun. 28, 309–324. doi: 10.1111/hsc.12839
Kulie, P., Steinmetz, E., Johnson, S., and McCarthy, M. L. (2021). A health-related social needs referral program for Medicaid beneficiaries treated in an emergency department. Am. J. Emerg. Med. 47, 119–124. doi: 10.1016/j.ajem.2021.03.069
Landis, J. R., and Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics 33, 159–174. doi: 10.2307/2529310
National Academies of Sciences, Engineering, and Medicine. (2019). Integrating social care into the delivery of health care: Moving upstream to improve the Nation's health. Washington, D.C: National Academies Press.
Pilarska, J. (2021). The constructivist paradigm and phenomenological qualitative research design. Res. Pparadigm Consid. Emerg. Schol., 64–83. doi: 10.2307/jj.22730542.10
Schickedanz, A., Sharp, A., Hu, Y. R., Shah, N. R., Adams, J. L., Francis, D., et al. (2019). Impact of social needs navigation on utilization among high utilizers in a large integrated health system: a quasi-experimental study. J. Gen. Intern. Med. 34, 2382–2389. doi: 10.1007/s11606-019-05123-2
Slavich, G. M. (2020). Social safety theory: a biologically based evolutionary perspective on life stress, health, and behavior. Annu. Rev. Clin. Psychol. 16, 265–295. doi: 10.1146/annurev-clinpsy-032816-045159
Wallace, A. S., Luther, B., Guo, J. W., Wang, C. Y., Sisler, S., and Wong, B. (2020). Implementing a social determinants screening and referral infrastructure during routine emergency department visits, Utah, 2017-2018. Prev. Chronic Dis. 17:E45. doi: 10.5888/pcd17.190339
Wallace, A. S., Luther, B. L., Sisler, S. M., Wong, B., and Guo, J.-W. (2021). Integrating social determinants of health screening and referral during routine emergency department care: evaluation of reach and implementation challenges. Implem. Sci. Commun. 2:114. doi: 10.1186/s43058-021-00212-y
World Health Organization (n.d.). Social determinants of health. Available online at: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (Accessed December 18, 2023).
Keywords: social determinants of health, social needs, safety, threat vigilance, screening, social services
Citation: Bybee SG, Tedford NJ, Grigorian EG, Luther B, Guo J-W, Wong B, Diamond L and Wallace AS (2025) Focus groups reveal how threat vigilance hinders social needs screening and referrals in the emergency department. Front. Commun. 10:1558250. doi: 10.3389/fcomm.2025.1558250
Edited by:
Andrew Carter, San Jose State University, United StatesReviewed by:
Joy D. Doll, Creighton University, United StatesLe Khanh Ngan Nguyen, University of Strathclyde, United Kingdom
Copyright © 2025 Bybee, Tedford, Grigorian, Luther, Guo, Wong, Diamond and Wallace. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara G. Bybee, c2FyYS5ieWJlZUBudXJzLnV0YWguZWR1
†Present address: Natalie J. Tedford, School of Medicine and Public Health, University of Wisconsin, Madison, WI, United States
 Sara G. Bybee
Sara G. Bybee Natalie J. Tedford
Natalie J. Tedford Ernest G. Grigorian
Ernest G. Grigorian Brenda Luther1
Brenda Luther1 Jia-Wen Guo
Jia-Wen Guo Bob Wong
Bob Wong Andrea S. Wallace
Andrea S. Wallace