- 1Department of Health Promotion and Behavioral Sciences, Faculty of Public Health, Diponegoro University, Semarang, Indonesia
- 2Department of Epidemiology, Faculty of Public Health, Dian Nuswantoro University, Semarang, Indonesia
- 3Department of Health Administration and Policy, Faculty of Public Health, Diponegoro University, Semarang, Indonesia
- 4Department of Biostatistics and Demography, Faculty of Public Health, Diponegoro University, Semarang, Indonesia
- 5Department of Health Administration and Policy, Faculty of Public Health, Dian Nuswantoro University, Semarang, Indonesia
Introduction: In Indonesia, tuberculosis (TB) remains a significant public health challenge. In coastal urban areas, where poverty, overcrowding, stigma, and inadequate health infrastructure intersect, TB emerges through a network of social, cultural, environmental, and institutional vulnerabilities. This study explored TB as a wicked problem in urban coastal settlements, where issues related to structures, culture, and communication all interact, making it harder to control the disease effectively.
Methods: A qualitative exploratory study was conducted in Semarang’s coastal urban settlements, which were identified as high-risk areas for TB. In-depth interviews were done with 27 participants, including TB patients, household contacts, health cadres, health staff, local stakeholders, and community members. Data were analyzed thematically, focusing on how social, cultural, and institutional factors shaped TB vulnerability and control.
Results: Six interrelated identifiers TB as a wicked problem in coastal area emerged: (1) euphemistic and stigmatized communication, with widespread avoidance of the term “TB”; (2) symptom mis-recognition, where coughing and fatigue were normalized or overlooked; (3) structuring stigma, reinforcing social silence and delayed disclosure; (4) culturally embedded illness narratives, including moral, spiritual, and lifestyle explanations; (5) Perceptions of health based on functionality, where health was defined by the ability to perform daily activities, often minimizing the urgency of treatment; and (6) fragmented health system responses, including under-resourced outreach, unaligned service hours, and superficial health education. These factors interact within a fragile coastal environment characterized by tidal flooding, high humidity, and overcrowding, which collectively increase TB exposure. Unlike in mountainous areas, coastal communities face compounded ecological and institutional vulnerabilities.
Conclusion: Efforts to eliminate TB in Indonesia must go beyond biomedical solutions to address the complex interplay of cultural beliefs, environmental vulnerability, and systemic health system weaknesses. Adaptive, multisectoral, and culturally informed interventions are urgently needed to tackle TB as a wicked problem in coastal urban contexts.
1 Introduction
According to the Global Tuberculosis (TB) report, Indonesia ranks as the second-highest country with a significant TB burden, accounting for 10% of the global TB cases (World Health Organization, 2024). In response to this issue, the Indonesian government has adopted the END-TB program strategy through Presidential Decree No. 67 in 2021 for TB elimination, aiming for an incidence rate (IR) of 65 per 100.000 population by 2030. However, in 2023, the World Health Organization (WHO) still estimated Indonesia’s IR at 395 per 100,000 population, and approximately 14% of cases remained undiagnosed (World Health Organization, 2024). These showed the significant gap between current progress and elimination goals, which needed to develop more comprehensive and inclusive TB control efforts.
TB elimination in Indonesia requires more than biomedical intervention. It showed that study found a significant gap in TB detection and standard treatment, although private providers are licensed and capable of diagnosing TB, limited supervision has contributed to their low rate of case detection and limits access to TB quality care (Jiang et al., 2024). On the other hand, 74.6% of patients first sought care at an informal or private provider and experienced complex and prolonged diagnosis pathways. The longest delays occur at the patient level (Wiem Lestari et al., 2020). These delays are frequently caused by a lack of awareness of TB symptoms, stigma, and economic hardship (Ritonga et al., 2023; Wako et al., 2021; Wiem Lestari et al., 2020). Consequently, it led to more severe conditions, increased infectiousness, and disrupted TB management and control efforts (Tedla et al., 2020). These condition points to the complexity of TB control in Indonesia and indicate that the delays are rooted not only in medical issues but also in social determinants.
Cultural beliefs and perceptions have further complicated TB management in Indonesia. As a multicultural country, the community has different understandings of health and illness (Dwi Laksono et al., 2020). For example, in the Javanese community, illness is often interpreted through a cultural-spiritual lens, with conditions like chronic cough or fatigue sometimes attributed to mystical causes such as sawan, ancestral displeasure, or spiritual imbalance (Suyami et al., 2025). These interpretations often lead individuals to seek traditional healing methods such as ritual cleansing, herbal salves, or incantations before they turn to formal health services. Additionally, illness may be viewed as a moral trial or spiritual imbalance that influences how individuals respond to symptoms or adhere to treatment (Nawiyanto, 2017). Cultural norms related to politeness, shame, and avoidance of conflict also prevent open discussion about illness, reinforcing stigma and social silence around illness symptoms (Subandi and Good, 2018). Additionally, communal living arrangements where multiple families share limited spaces both intensify TB transmission risks and complicate efforts for isolation or adherence to treatment (Kurtuluş et al., 2020). This culturally rooted health behavior creates further barriers to timely TB diagnosis and control, particularly when public health programs fail to account for these beliefs.
While these culturally rooted health behaviors significantly shape help-seeking practices, in Urban areas, they intersect with the pressing environmental and socioeconomic challenges, where overcrowding and inadequate infrastructure further worsen TB transmission and treatment delays (Oloyede et al., 2022; Puspita et al., 2021). Data show that TB prevalence in Indonesia is higher in the urban areas than rural areas, with the cases in urban areas at 8,458 per 100.000 population (Noviyani et al., 2021). Along with the cultural factors, study identified that the risk of TB in an urban setting was associated with in-house density, lack of ventilation, and a low socioeconomic status, especially among slum area communities (Lee et al., 2022; Puspita et al., 2021; Singal et al., 2025). As an archipelagic country, many urban populations live in coastal settlements such as Semarang, North Jakarta, and Surabaya. These coastal communities often experience overlapping vulnerabilities, including poor housing conditions, high TB incidence, and informal employment (Oloyede et al., 2022). Moreover, many residents work as fishermen, which makes it difficult to seek timely diagnosis and complete treatment (Neethiselvan et al., 2021). These condition makes the coastal settlement at the margin of the health system and a hotspot of TB transmission and missed cases.
The coastal area presents a unique physical environment that influences the airborne diseases transmission. Factors such as inadequate ventilation, elevated indoor humidity, and crowded living conditions contribute to the heightened risk of TB transmission (Ifon et al., 2021). Analyses that focus on climate sensitivity suggest that variations in local climate and extreme weather conditions can be linked to changes in TB incidence. This indicates that tidal flooding and the seasonal patterns typical of coastal areas might create periods of heightened vulnerability or disruptions in services (Tosepu et al., 2024). Frequent tidal flooding, along with coastal inundation, further deteriorates housing conditions by causing dampness and mold. These conditions occasionally make health facilities and roads inaccessible, hindering diagnosis, contact tracing, and follow-up treatments. Such disruptions in services due to flooding have been found to obstruct frontline healthcare delivery and diminish the continuity of care in coastal areas prone to flooding (Indriyani et al., 2022; Rosadi et al., 2025).
The occupational and livelihood patterns in coastal communities, particularly those involving fishing, seasonal trading, and informal day labor, result in irregular work schedules, high mobility, and economic instability, which limit the ability to seek care and adhere to treatment. Research on fishing communities highlights how the demands of their livelihoods, such as time spent at sea and unpredictable income, lead individuals to deprioritize preventive and long-term treatments, thereby increasing the chances of delayed diagnosis and interrupted therapy (Mulholland et al., 2023; Wekunda et al., 2021).
This condition further created a wicked problem for TB control in Indonesia. A wicked problem is defined as a complex, ill-structured issue and causes that are deeply embedded in a social system (Lönngren and van Poeck, 2021). Wicked problems such as TB require adaptive and beyond medical responses, it also needs a multisector effort that addresses social and structural determinants. In the case of TB, especially in coastal urban settlements, the challenge goes beyond treating the disease, it needs to involve addressing the structural inequities and cultural framings that sustain vulnerability. Despite national initiatives, a lack of service integration, weak social protection, and culturally uninformed health communication continue to undermine TB control efforts in these communities.
This study aimed to explore how TB manifests as a wicked problem in Indonesia’s coastal urban settlements by examining the social, cultural, and structural determinants of vulnerability, identifying communication and institutional breakdowns, and analyzing gaps in policy implementation that contribute to persistent TB risk in coastal settlement settings.
2 Methods
2.1 Study design
A qualitative exploratory design was employed to investigate TB as a wicked problem in coastal urban settlements in Indonesia. The evaluation framework for clinical and health networks was used to guide the study in exploring how communication breakdowns, structural barriers, and policy gaps contributed to TB vulnerability (Cunningham et al., 2019). We conducted an in-depth interview with TB patients, health cadres, local stakeholders, community members, and health staff to comprehensively understand the lived experiences, service delivery challenges, and institutional responses related to TB control in a coastal area.
2.2 Study setting
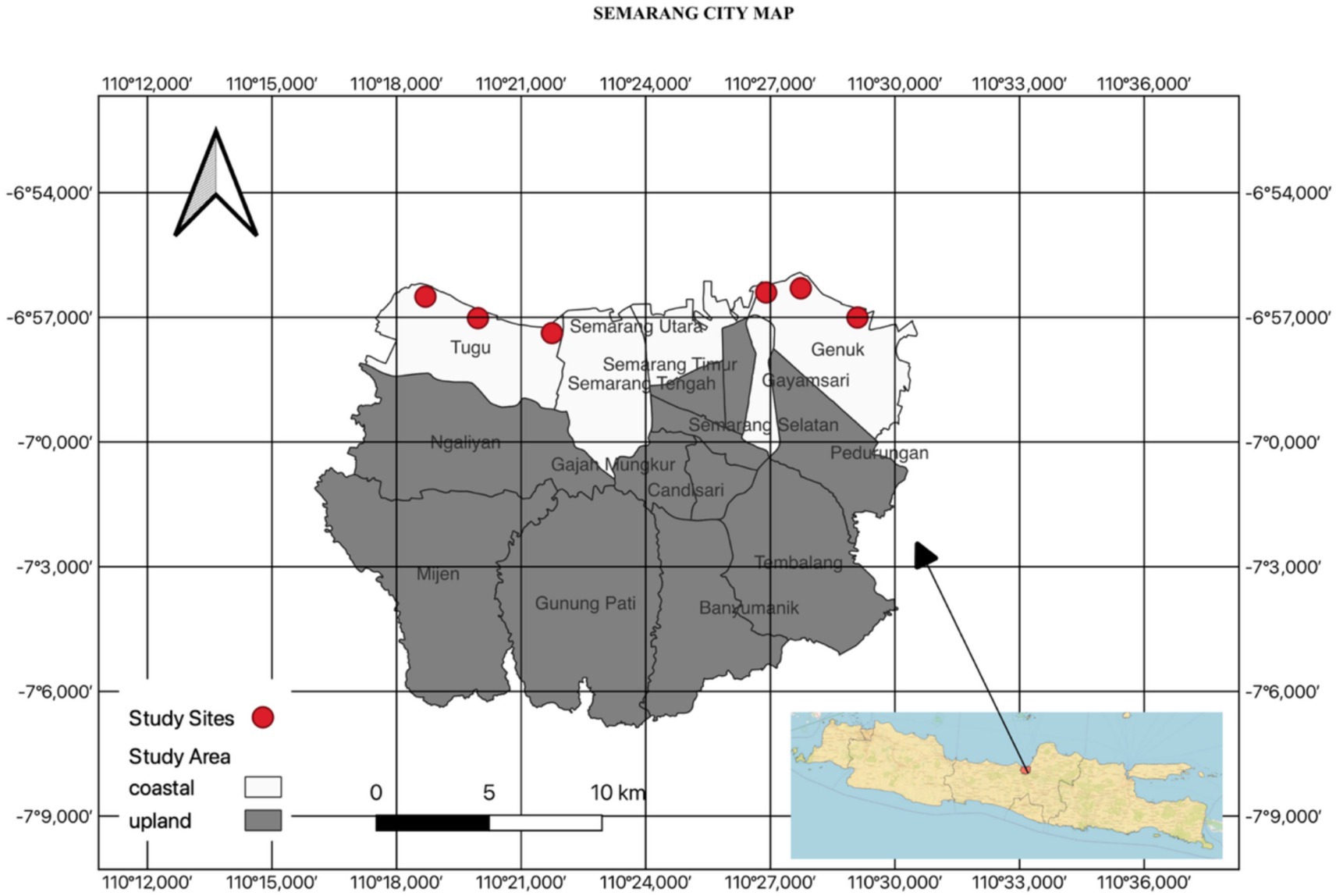
This study was conducted in three coastal urban settlements in Semarang (Mangkang, Karanganyar and Genuk). This area was chosen based on local health authorities classifying it as a high vulnerability for TB transmission. The study sites were located along the northern coastline of Java and are administratively part of the western and eastern coastal zones of Semarang (Figure 1). This community is living in a high-density area and is frequently affected by tidal flooding. These regions are characterized by low-lying urban areas that are highly susceptible to tidal flooding (rob), saltwater intrusion, and coastal erosion. The land slopes vary from 0–15%, and a significant portion of the residential zones is located within 100 meters of the highest tide line and within river buffer zones, highlighting their considerable spatial vulnerability. The population density surpasses 1,000 individuals per km2, with over 100 housing units per hectare, primarily consisting of semi-permanent structures with inadequate ventilation and limited drainage systems. The water supply largely relies on shallow wells and sporadic piped distribution, while wastewater frequently flows into open channels. The frequent flooding and poor sanitation contribute to the rapid deterioration of housing and increase health risks, including respiratory and infectious diseases. Most inhabitants depend on informal jobs such as fishing, seafood processing, small-scale trading, and day labor, which are marked by economic instability, irregular movement, and limited access to healthcare services (Dewi et al., 2021).
2.3 Participants
Participants of this study were purposefully selected to capture the diverse perspectives on TB control. Participants were drawn from four main groups:
a. TB patients (6 persons)
b. Household members close contact (6 persons)
c. Healthcare workers (5 persons)
d. Local Stakeholders including health cadres (7 persons)
e. Community members (3 persons)
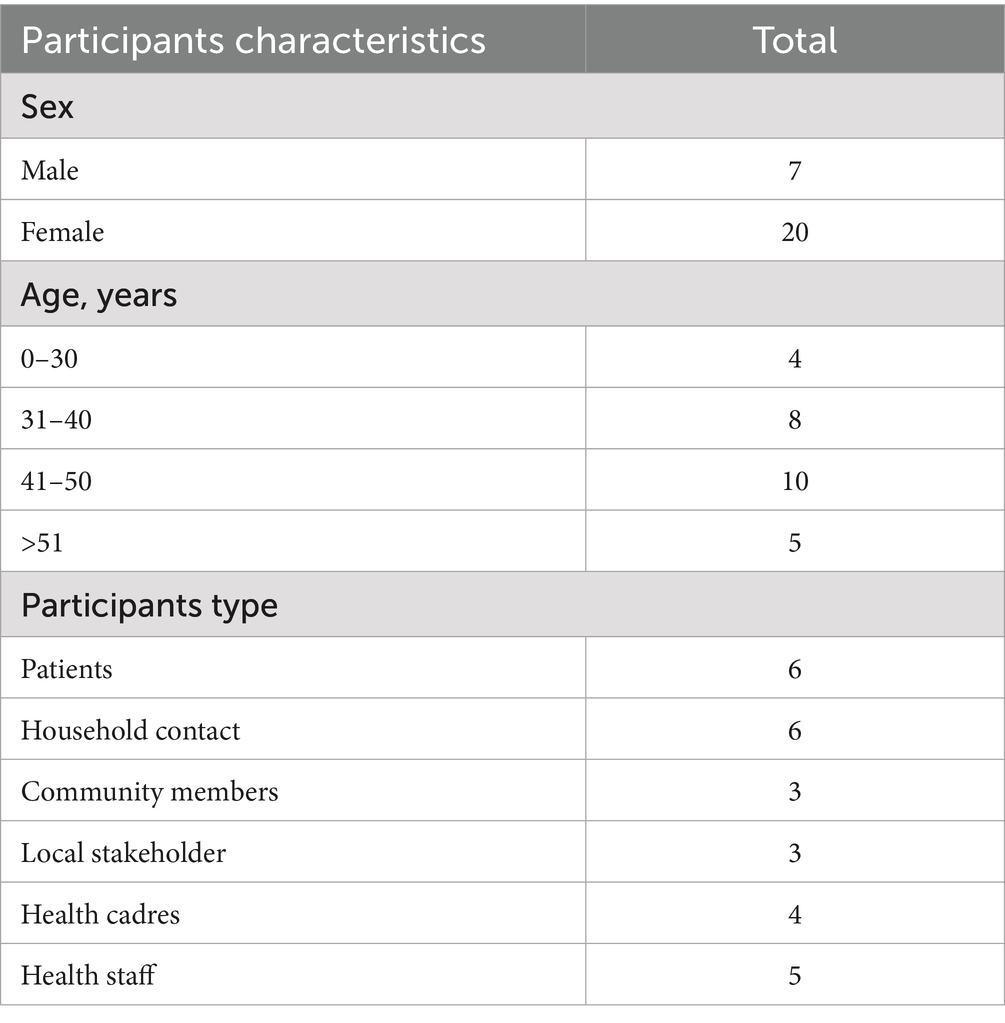
Participants’ recruitment was facilitated by the health cadres and the local health center. A total of 27 participants were included in this study (six TB patients, six household contacts, three community members, three local stakeholders, four health cadres, and five health staff). Observations were also conducted during TB patient services within healthcare facilities to capture interactions, service delivery, and communication processes. Additionally, observations took place at patients’ homes and involved interactions with health cadres to gain a comprehensive understanding of the community-based aspects of TB care.
2.4 Data collection
In-depth interviews were conducted from March to June 2025. Interviews were conducted in Bahasa Indonesia, each lasting between 45 and 90 min, with an average of 2–3 visits per participant. Observations at health care facilities were carried out during regular operational hours, covering the entire service day from opening to closing, across three primary health care centers. Additionally, observations for interactions between patients and health cadres took place during home visits. We also continuously evaluated the adequacy of our sampling throughout the data collection process. After conducting 21 interviews, an initial analysis revealed that the main ideas were being repeated. To ensure thoroughness, we carried out three more interviews to identify any contradictory cases. We determined that data saturation was reached when no new categories of codes appeared in two successive interview rounds, and when further interviews only provided more detail on existing themes.
2.5 Analysis
Audio recordings were transcribed verbatim and analyzed with a thematic approach. Thematic analysis was utilized to uncover key patterns and insights within the data, following a structured six-phase approach (Braun and Clarke, 2006). The process began with familiarization, which involved transcribing and repeatedly reading the interview data to gain an in-depth understanding. Initial coding was then conducted using ATLAS TI software to systematically organize relevant excerpts from interviews and field observations. Similar codes were grouped into broader thematic categories: knowledge and belief, stigma, and social response. These emerging themes were carefully reviewed to ensure they were internally coherent and distinct from one another. Each theme was then clearly defined and labeled in alignment with the study’s research questions. Finally, the findings were synthesized into a comprehensive report, supported by selected quotations that illustrated the key themes. Initial coding was performed by the first author and independently reviewed by the other author. Discrepancies were solved by discussion.
2.6 Trustworthiness
To ensure the credibility and trustworthiness of the findings, the study applied multiple qualitative validation techniques. Triangulation was conducted at four levels. First, source triangulation involved gathering information from diverse participants, including community members, health officials, local stakeholders, and health cadres to compare and validate perspectives across different roles. Second, method triangulation was employed by using in-depth interviews and participant observations, allowing for cross-validation of data from different methods. Third, the study ensured peer debriefing, where emerging themes and interpretations were regularly discussed with fellow researchers to challenge assumptions, reduce researcher bias, and strengthen analytical rigor. Furthermore, prolonged engagement in the field enabled the researchers to build trust with participants, gain deeper contextual understanding, and verify data accuracy over time. These strategies collectively enhanced the credibility and depth of the study’s findings.
2.7 Ethical considerations
This study received ethical approval from the Health Research Ethics Committee, Faculty of Public Health, Diponegoro University (IRB no: 172/EA/KEPK-FKM/2025). Verbal consent and signed was obtained for all participants before data collection, including consent for audio recording. Anonymity and confidentiality were ensured by assigning pseudonyms and securely storing all data.
3 Results
A total of 27 participants, including TB patients, household contacts, local stakeholders, healthcare workers, health cadres, and community members (Table 1). The analysis of interviews showed multiple intersecting dimensions that explain how TB persists as a wicked problem in coastal urban settlements. Themes presented below reflect the entangled social, cultural, environmental, and institutional determinants of TB vulnerability.
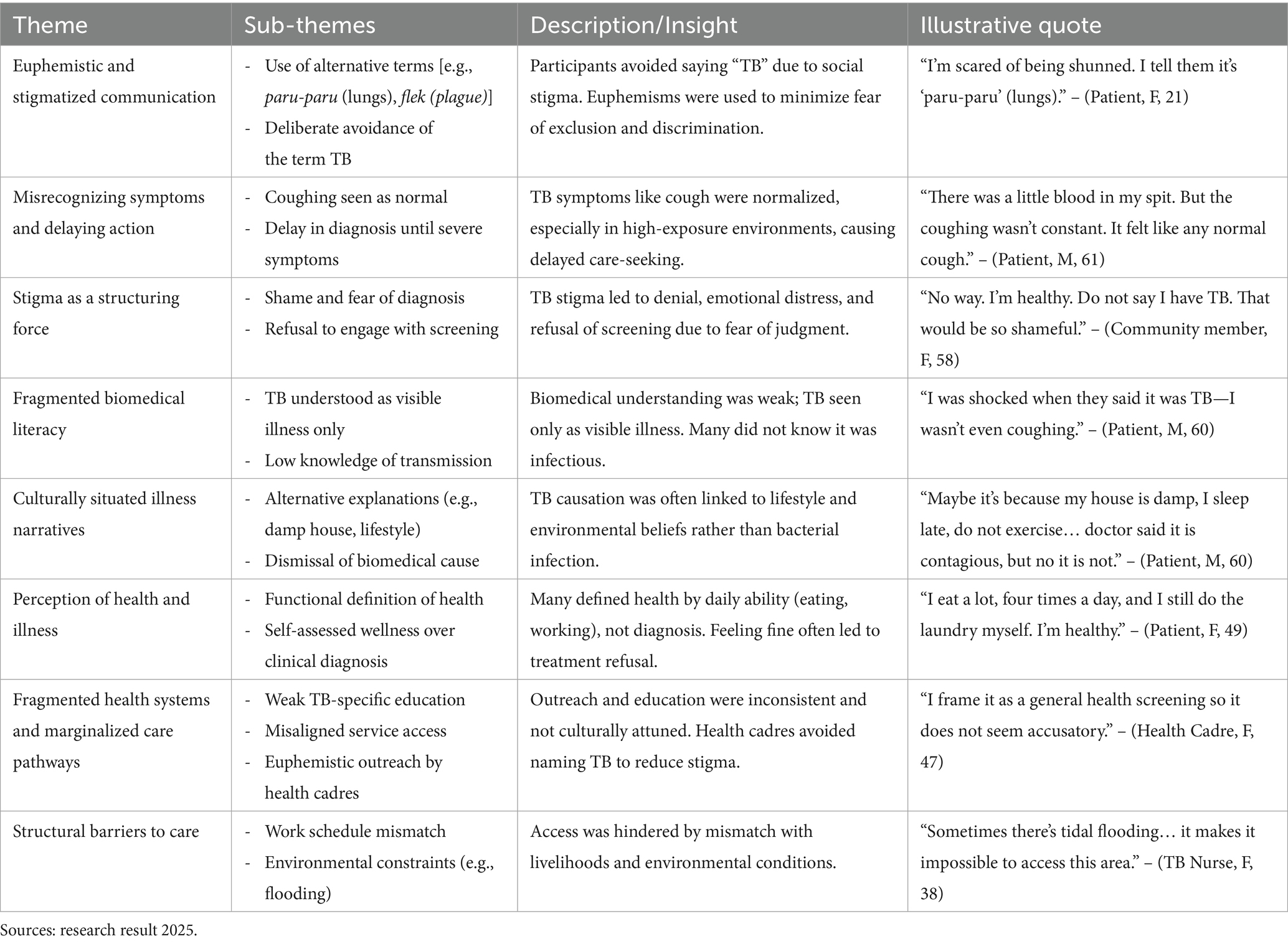
The analysis highlights how euphemistic communication, stigma, cultural beliefs, and weak biomedical literacy intersect with fragmented health systems and structural barriers, collectively shaping delayed diagnosis and marginalized TB care pathways. Table 2 shows the summary of themes and sub-themes from thematic analysis.
This study builds upon earlier work that views TB as an issue deeply rooted in social and structural factors, highlighting how these elements manifest uniquely in coastal areas. The six identifiers below demonstrate how the coastal environment exacerbates the complexity of TB through the interaction of social stigma, cultural perceptions, and environmental vulnerability.
3.1 Euphemistic and stigmatized communication
Throughout the interviews, participants rarely mentioned tuberculosis directly. Instead, they referred to it by using generalized respiratory terms such as paru-paru (lungs), flek (plague), or nafas (breath). These terms are culturally embedded and lack diagnostic specificity that often used to describe a wide range of respiratory diseases from asthma to bronchitis without a clear distinction. This choice of term was a way to respond to the social implications of being TB ill. Participants often stated that TB was a label that brought stigma, linking it to contagion, blame, and social exclusion. This blurred nomenclature contributed to widespread misunderstanding of TB and downplayed its infectious nature. Avoidance of the term TB was often found as a deliberate act of self-protection. Participants preferred euphemisms to avoid the social stigma attached to TB, particularly fears of isolation and discrimination.
“…it seems like I’m embarrassed, I’m scared too, ma’am… I’m scared of being shunned. I am afraid they don’t want to be friends anymore, so I tell them it’s “paru-paru” (lungs).” (Patient, Female, 21 years old)
This avoidance of terminology also appeared in doctor visits. A participant remembered that during his visit to a doctor to seek a diagnosis, the doctor gave the diagnosis as flek (plague) and being treated with common medication.
“The doctor just said it was flek (plague)… so I kept taking the flek (plague) medicine. But I was still coughing, no improvement, then I took a private check for my lungs, the I was diagnosed TB.” (Patient, Male, 40 years)
The widespread use of euphemisms and avoidance of the term TB identified the deep-seated fears of social rejection and discrimination. This linguistic behavior not only reflects the social implications of TB but also affects how individuals perceive and respond to their health conditions, as a result increasing the potential for delays in seeking care and misunderstandings about the disease.
3.2 Misrecognizing symptoms and delaying action
Most participants did not see early symptoms like coughing or night sweats as signs of a serious illness. Coughing was viewed as a routine, normal occurrence that led to failing to recognize it as a possible symptom of TB unless it significantly interfered with daily activities or was accompanied by alarming signs such as blood in sputum or physical weakness.
“It started as just coughing. I didn’t think much of it until I began feeling dizzy and chilled. That’s when I went to a doctor.” (Patient, Male, 40 years)
“There was a little blood in my spit…that’s why I went to the health center. But the coughing wasn’t constant. It felt like any normal cough.” (Patient, Male, 61 years)
The acceptance of coughing, especially in households with tobacco smoke or cramped conditions, led to delays in seeking a formal diagnosis. This also affected how communities responded to contact tracing. Participants often resisted screening if they had no symptoms, especially no cough. The common pushback was described by a TB health worker, indicating that if someone is not coughing, they will not come, and it is often questioned why testing is needed if they feel fine. This showed that biomedical indicators of risk are often overlooked in favor of personal experiences, leading to missed chances for early diagnosis and treatment.
3.3 Stigma as a structuring force: fear, rejection, and denial
Stigma emerged as a strong force that shaped not just behavior but also perception. The diagnosis of TB was feared not only for its health risks but also for its ability to change how people were seen socially, from healthy and respectable to sick and morally judged. This moral view of TB led to fears of being rejected.
“No way. I’m healthy. Don’t say I have TB. That would be so shameful.” (Community member, Female, 58 years)
Stigma also created strong emotional responses. Reactions to community TB screening were often intense. These responses show that TB is stigmatized both due to fear of spreading it and because of its moral implications, linking it to dirtiness or neglect. This may explain why some patients felt blamed or chose to hide their illness, even from family.
“Eeeeh astaghfirullah (praying), so it is TB screening… it’s okay if we go home too, right? God forbid, no way, I’d be so embarrassed, they’d think I have TB, they’d think I have TB.” (Community member, Female, 57 years)
3.4 Fragmented biomedical literacy and culturally situated illness narratives
Participants in this study exhibited incomplete and culturally embedded understandings of tuberculosis, grounded more in lived experience, community narratives, and observable symptoms than in formal health information. Instead of being seen as a specific infectious disease caused by Mycobacterium tuberculosis, TB was viewed as a general respiratory illness, mainly identified by symptoms such as coughing, chest pain, and shortness of breath. The absence of these symptoms invalidated the TB diagnosis, leading to confusion, denial, or delayed treatment.
“As far as I know, TB looks like constant coughing, the disease is in the lungs, it causes shortness of breath and chest pain—that’s what I thought TB was. I was shocked when they said it was TB—I wasn’t even coughing. From what I understand, TB means constant coughing and breathlessness." (Patient, Male, 60 years)
TB was not perceived as a “silent” or asymptomatic infection but as something that must manifest visibly to be legitimate. This mismatch between experiential knowledge and biomedical models led some to question their diagnosis altogether. Knowledge about TB transmission was similarly limited or absent. Even among patients diagnosed with TB, there was little awareness that the disease could spread from one person to another.
"When my father was sick, we didn’t take any precautions, because I didn’t know it was contagious." (Patient, Female, 21 years)
Other participants recognized TB as contagious but lacked specific knowledge about how it spreads, when someone is infectious, or what measures are needed to protect others. These gaps in knowledge were not the result of indifference but rather reflected a lack of accessible and sustained health education in their communities.
"The understanding is just that TB is a contagious disease, that’s it." (Local stakeholder, Female, 48 years)
"I don’t really know, his weight wouldn’t go up, then they checked and said there were signs of TB." (Household Contact, Male, 34 years)
Beyond symptom recognition and transmission, many participants held distinct cultural logics about what causes TB. These beliefs often included lifestyle factors (e.g., irregular sleep, stress, lack of exercise), environmental conditions (e.g., humidity), and moral framings. Rather than accepting TB as a bacterial infection, some reinterpreted it through local explanations of bodily vulnerability. One participant, for instance, dismissed the role of smoking and infection entirely, instead attributing his illness to his daily routine. This demonstrates a behavioral-environmental logic of illness causation that often supersedes microbial understanding. It reflects not just misinformation but an internally coherent system of belief, shaped by observation, community experience, and everyday reasoning.
“In my view, it’s probably because of an unhealthy lifestyle, not necessarily smoking. I know many elderly people who smoke and have never got TB. Maybe it’s because my house is damp, I often sleep late, don’t exercise, and stay up all night… Maybe that’s why I got sick….doctor said it is contagious, but no it is not" (Patient, Male, 60 years)
Several participants also expressed fatalistic beliefs, suggesting that illness is a matter of fate or divine will, rather than personal behavior or biology. These beliefs diminished the perceived importance of prevention or early care-seeking, as disease was seen as something that strikes arbitrarily. These views coexisted with skepticism toward biomedical treatment. Some patients defaulted from their medication regimen due to side effects, perceiving the treatment as more harmful than helpful. In these cases, traditional medicine (jamu) was preferred, not simply due to accessibility, but because it aligned better with their perceptions of safety and body harmony.
3.5 Perception of health and illness
Perceptions of health and illness among participants were rooted primarily in subjective experiences and the ability to function in daily life, rather than biomedical assessments or formal diagnosis. In many cases, individuals who had been diagnosed with TB still considered themselves “healthy” because they could work, eat, and carry out household responsibilities. Health, in this context, was defined by bodily capacity and visible performance, not by disease status or laboratory findings.
"Back then, I was still working. My husband coughed up blood, the room was full of smoke, he was always smoking, eventually he got sick and was treated at the health center. But I am healthy, miss. Even though I’m thin, that’s just how I am. My appetite hasn’t dropped; I eat a lot, four times a day, and I still do the laundry myself. I’m healthy." (Patient, Female, 49 years)
Several health cadres described difficulties in convincing patients or family members to begin or continue therapy once the patient claimed to “feel fine.”
"The hardest thing is when we meet patients who feel they’re healthy. If they don’t think they’re sick, it’s really hard to persuade them to seek treatment—both the patients and their families." (Health cadre, Female, 49 years)
"They take it lightly. Only when the cough gets bad do they start to worry. If you suggest a sputum test or X-ray when symptoms are mild, they refuse. They just don’t take it seriously." (Health cadre, Female, 47 years)
3.6 Fragmented health systems and marginalized care pathways
The study found systemic gaps in TB-related service delivery marked by fragmented communication, under-resourced outreach, and structural misalignment between community needs and institutional health responses. These conditions collectively entrenched the risk environment for TB and contributed to delays in diagnosis, discontinuities in treatment, and the reproduction of stigma. An absence of structured or targeted TB education. Instead, health information was often transmitted sporadically through ad hoc channels such as WhatsApp groups, occasional door-to-door visits, or general health promotion events that rarely addressed TB specifically.
It seems like it's been done often — during PJN activities, they might include a little bit about TB, just a small part. Usually, it’s just slipped into other activities. (TB nurse. Female, 38 years)
"It’s not widespread, because there are so many health education topics we need to deliver to the community, not just TB. We do have a WhatsApp group. All the flyers are shared there and are supposed to be forwarded down to the neighborhood (RT) level — whether they’re actually read or not, we don’t know." (Epidemiologist, Male, 33 Years)
Moreover, available education was frequently superficial and lacked the visual or written reinforcement necessary for retention and action, particularly among residents with lower literacy levels. Health cadres often struggled to engage residents due to anticipated rejection or fear of stigma, leading them to adopt euphemistic strategies that obscured the purpose of their visits.
“Yes, when I plan to do the screening, I frame it as a general health screening so it doesn’t seem accusatory. I just casually ask neighbors if anyone in the family has a cough or diabetes.” (Health cadre, Female, 47 Years)
Temporal mismatches between clinic operating hours and local work rhythms, particularly among fishing communities, posed additional access barriers. Individuals working night shifts found it difficult to adhere to conventional health service schedules. And also, environmental vulnerabilities, which tidal flooding (rob) further restricted mobility and delayed healthcare-seeking behavior.
"Sometimes there’s tidal flooding (rob), and when the water is still high, it makes it impossible to access this area." (TB Nurse, Female, 38 Years)
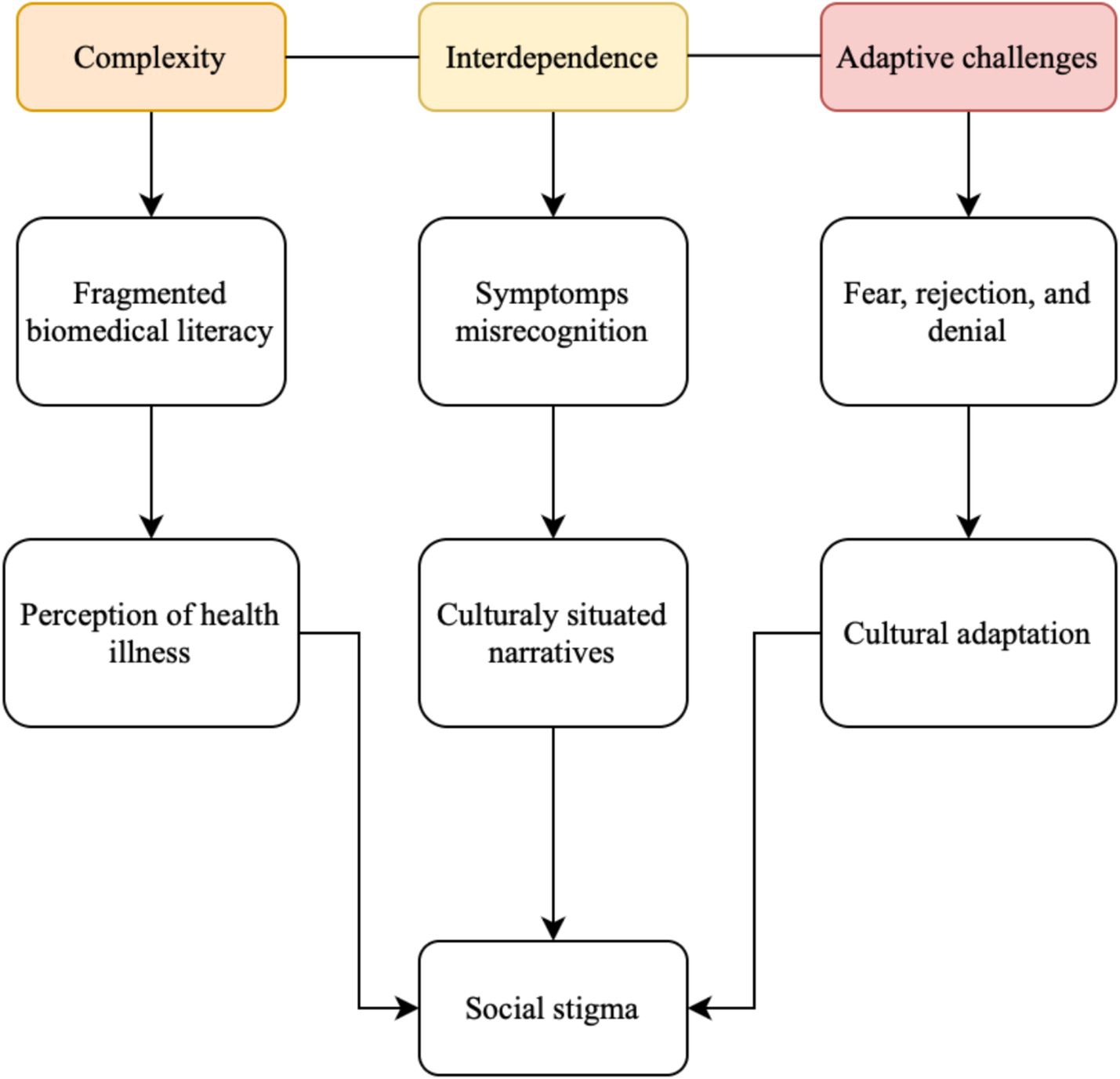
We operationalized the ‘wicked problem’ framework by mapping each empirical theme to the three core dimensions of wickedness: complexity, interdependence, and adaptive challenges (Crilly, 2025; Lönngren and van Poeck, 2021). As illustrated in Figure 2, euphemistic and stigmatized communication, fear and denial, and fragmented biomedical literacy represent the complexity of TB-related behaviors and discourses. The interdependence dimension captures how perceptions of health, cultural illness narratives, and systemic fragmentation interact across social and institutional levels. Lastly, adaptive challenges emerge from stigma, fear of rejection, and the need for culturally responsive interventions that extend beyond biomedical solutions.
4 Discussion
Recent research has increasingly identified TB as a social and structural issue rather than solely a biomedical one, highlighting the role of stigma, miscommunication, and inadequate service integration in perpetuating the epidemic in low- and middle-income countries (Craig et al., 2017; Kılıç et al., 2025). However, there has been limited exploration of how these factors interact with environmental and livelihood vulnerabilities in coastal urban areas. This study addresses this gap by illustrating how TB emerges as a complex problem in Indonesia’s coastal communities, where social, cultural, and structural factors intersect with environmental instability, perpetuating cycles of invisibility and delay.
The results showed that various social, cultural, and structural factors interact in complex ways, making TB difficult to manage in these communities. One of the key findings was how people talk about the disease. Many participants avoided saying “TB” directly, instead using words like paru-paru (lungs) or flek (plague). This choice of words reflects how stigma and fear of being judged still influence how people think and act around TB. By avoiding the word “TB,” people may feel more comfortable, but this also creates problems. It makes TB less visible and harder to talk about openly. As a result, it becomes more difficult for health workers and communities to agree on what the problem is and how to deal with it. This gap in shared understanding is one reason TB remains a wicked problem.
Similar findings have been reported in other countries. A study in East Africa found that people often hid their illness because of stigma, and some chose spiritual or herbal remedies rather than going to a clinic, which delayed diagnosis and treatment (Msoka et al., 2021). In India, a study found that many patients did not tell others about their TB and often kept their distance from others to avoid being stigmatized (Mukerji and Turan, 2018). Our study showed similar patterns. Cultural beliefs and fears about how others would react made TB less visible and harder to address through collective efforts.
Our study highlights that the use of non-medical terminology (plague) by general practitioners with antibiotic prescribing contributes significantly to delayed TB diagnosis. This practice reflects wider trends identified in primary care settings in low- and middle-income countries (LMICs) (Salomon et al., 2022; Sulis et al., 2020). Additionally, several studies have noted that limited knowledge about TB among general practitioners often leads to misdiagnosis and mistreatment, further delaying appropriate care (Mahendradhata et al., 2015; Winardi et al., 2022).
These diagnostic challenges are compounded by how patients themselves interpret early symptoms. Participants commonly viewed persistent coughing, fatigue, or even mild hemoptysis as non-serious, especially when these symptoms did not interfere with daily functioning. As such, many delay seeking care. This misrecognition of symptoms also affected contact tracing and TB screening. Several participants declined testing simply because they did not feel sick or did not have a cough. Moreover, delays in diagnosis were not solely due to patient perceptions. Frequent tidal flooding not only damages housing but also makes chronic illnesses and fatigue seem normal, causing persistent coughing to appear commonplace. This normalization blurs the line between illness and daily struggles, postponing diagnosis and reducing the perceived urgency of seeking treatment. Health facilities also appeared to deprioritize TB screening and testing, which contributed to missed opportunities for early intervention (de Vos et al., 2022). This combination of clinical, institutional, and sociocultural barriers illustrates the fragmented and poorly coordinated nature of TB care, reinforcing the wicked nature of the problem.
The communication patterns we observed are consistent with health-communication and stigma theories and help to explain why conventional biomedical messaging is insufficient in this setting. From a Health Belief Model perspective, low perceived susceptibility (cough normalized) and low perceived severity (functionality metric) reduce cues to action; simultaneously, perceived social costs (stigma) raise barriers to seeking care. The Social Ecological Model clarifies how individual beliefs are embedded within interpersonal (family shame), community (euphemistic norms), and institutional (misaligned services) layers that must be targeted together. Communication Accommodation Theory and evidence on stigma management further explain why health cadres and clinicians intentionally modify language (euphemisms) to avoid face-threats as a short-term strategy that reduces immediate resistance but undermines problem definition and surveillance (Alyafei and Easton-Carr, 2025; Giles, 2008).
Another major theme that emerged from this study was the fragmented nature of health systems and the marginalized pathways through which communities engage with TB-related services. Participants described systemic gaps in TB service delivery, characterized by weak coordination, under-resourced outreach, and a lack of alignment between health system functions and the lived realities of vulnerable populations. These conditions collectively reinforced the risk environment for TB, contributing to delays in diagnosis, inconsistent treatment adherence, and the persistence of social stigma.
The coastal economy exacerbates these dynamics. The sectors of fishing, seafood processing, and daily wage labor contribute to irregular working hours and economic precarity, thereby constraining individuals’ ability to access clinics or adhere to extended treatment regimens. This aligns with previous research linking mobility and livelihood instability to treatment interruptions in other maritime communities (Gray et al., 2008; Mulholland et al., 2023). However, the coastal context in Indonesia introduces an additional layer of vulnerability, wherein environmental disruptions directly compromise the reach of health systems. Clinics are frequently impacted by flooding, transportation barriers, and temporary displacement, which disrupt the continuity of care and weaken surveillance systems.
Health education within these settings was often delivered informally, such as through WhatsApp groups, community gatherings, or door-to-door visits that rarely emphasized TB specifically. Prior research indicates that such informal and nonspecific health education is associated with poor information retention and low levels of public awareness (Maneze et al., 2019). Given that communication is a fundamental element of human interaction and a key pillar in public health efforts, strengthening health communication strategies is critical. Effective communication underpins the success of government-led health promotion programs by shaping health-related knowledge, attitudes, and behaviors across communities (Zhang et al., 2024).
Health workers and health cadres also described adopting euphemistic communication strategies to mitigate anticipated resistance or stigma from community members. While these strategies were aimed at avoiding confrontation, they often diluted the clarity and urgency of TB-related messaging. Framing TB screening as part of a general health check may prevent alienating individuals, but it also obscures the seriousness of TB and reduces the likelihood of early detection (Sommerland et al., 2017). These findings echo studies in other low and middle-income contexts where fear of stigma leads to communication avoidance, contributing to underdiagnosis and treatment delays (Ahad et al., 2023; Dolezal, 2022; Garpenhag and Dahlman, 2021).
This study showed the complexity of TB as a wicked problem in Indonesia’s coastal urban settlements, shaped by the convergence of social stigma, cultural beliefs, environmental vulnerability, and fragmented health systems. The findings demonstrated that TB control in these communities is not merely a matter of delivering biomedical services but requires confronting deeply entrenched cultural narratives, addressing structural misalignment, and reshaping health communication strategies.
Avoidance of the term “TB,” normalization of symptoms, and culturally rooted interpretations of illness all contribute to delayed diagnosis and treatment. Stigma not only isolates individuals socially but also distorts community engagement and public health messaging. Meanwhile, the health system’s limited outreach, poorly targeted education, and inflexible service delivery mechanisms fail to address the lived realities of marginalized populations, particularly those in flood-prone, high-density, and informal coastal settlements.
The fragmented pathways of care, euphemistic communication, and culturally embedded illness narratives observed in coastal Semarang reflect broader gaps in implementing truly patient-centered approaches. The WHO framework emphasizes early diagnosis, equitable access, and integrated care that addresses both medical and social determinants. However, this study demonstrates that these ideals remain out of reach in marginalized and geographically isolated communities. Stigma, fragmented health systems, and the lack of customized community engagement strategies hinder the integration of primary health care, social protection, and behavioral interventions, challenges that are also noted in global assessments of TB care continuity in low-resource environments. Consequently, the complexity of TB in coastal regions is not just a local issue but a reflection of the systemic and structural obstacles that hinder progress toward the End TB goals globally (World Health Organization, 2015).
By integrating these insights, our study contributes to the academic discourse on the complexity of TB in three significant ways. Firstly, it positions stigma and communication avoidance within an ecological framework, demonstrating how coastal vulnerability and economic instability exacerbate social silence. Secondly, it elucidates how the fragmentation of health systems interacts with spatial and occupational marginalization to perpetuate structural exclusion. Thirdly, it reconceptualizes TB control as an adaptive, multisectoral challenge that must address not only biomedical deficiencies but also the environmental and socio-cultural determinants inherent in coastal communities. In doing so, this study enriches the global discourse on complex health issues by anchoring it in a distinctly environmental and localized context.
5 Conclusion
TB in coastal cities is a tough health problem. It is hard to solve with simple medical solutions because it is linked to space, environment, and social issues. Coastal areas like Mangkang, Karanganyar, and Genuk in Semarang have more risks, making TB harder to control than in other places. Problems like frequent flooding, crowded homes, poor sanitation, and unstable jobs lead to ongoing exposure, late diagnosis, and interrupted care. These issues, along with stigma and unclear communication, make TB less visible and harder to tackle together.
This study adds to the understanding of TB in developing countries by looking at how location affects the problem. While past studies focused on social and structural factors, few have looked at how geography, especially in coastal areas, worsens health system weaknesses. By examining TB in these coastal environments, this study offers a new way to see how environmental risks, social meanings, and weak institutions keep the disease going. This view adds to global health discussions on why TB is hard to fight in places with limited resources.
To effectively eliminate TB, strategies must go beyond medical solutions. They need to include multiple sectors, be culturally aware, and adaptable. These strategies should focus on early detection, better health system response, and addressing social and environmental factors. Policies should also include the voices and experiences of affected communities to create solutions that fit local needs. Without these integrated strategies, TB will remain a big problem in vulnerable coastal areas.
Future research should look into how community-based and culturally specific interventions can improve TB awareness and reduce stigma in coastal and informal urban areas by culturally tailored communication training for health cadres or integration of TB control into coastal resilience programs. Long-term studies are needed to see how changes in health communication, trust in healthcare, and environmental strength affect TB outcomes over time. Also, involving community members in creating and evaluating TB interventions is crucial for local relevance and sustainability.
6 Limitations
This study has several limitations. As a qualitative study conducted in selected coastal settlements of Semarang, its findings are context-specific and may not be generalizable to other settings. The reliance on self-reported narratives may have introduced recall or social desirability bias, particularly when discussing a stigmatized disease like TB. Additionally, the use of the “wicked problem” framework, while useful in revealing complexity and interdependence, may have constrained alternative interpretations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Health Research Ethics Committee, Faculty of Public Health, Diponegoro University (IRB no: 172/EA/KEPK-FKM/2025). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
ZS: Project administration, Formal analysis, Conceptualization, Writing – review & editing, Supervision, Funding acquisition, Methodology. SH: Data curation, Methodology, Writing – original draft, Visualization, Formal analysis. AS: Investigation, Methodology, Validation, Writing – review & editing. FA: Writing – review & editing, Software, Formal analysis, Validation. ER: Methodology, Data curation, Visualization, Writing – original draft, Formal analysis.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Ministry of Education, Culture, Research, and Technology of the Republic of Indonesia (Directorate General of Higher Education) under grant no. 359-025/UN7.D2.1/PP/V/2025.
Acknowledgments
The authors gratefully acknowledge the support of Diponegoro University and the local health authorities for facilitating this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer LA declared a shared affiliation with the authors ZS, AS, and FA to the handling editor at the time of review.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahad, A. A., Sanchez-Gonzalez, M., and Junquera, P. (2023). Understanding and addressing mental health stigma across cultures for improving psychiatric care: a narrative review. Cureus. 15:e39549. doi: 10.7759/cureus.39549
Alyafei, A., and Easton-Carr, R. (2025) The health belief model of behavior change. Treasure Island (FL): StatPearls Publishing.
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101. doi: 10.1191/1478088706qp063oa
Craig, G. M., Daftary, A., Engel, N., O’Driscoll, S., and Ioannaki, A. (2017). Tuberculosis stigma as a social determinant of health: a systematic mapping review of research in low incidence countries. Int. J. Infect. Dis. 56, 90–100. doi: 10.1016/j.ijid.2016.10.011
Crilly, N. (2025). Wicked problems: flexible characterizations and visual representations. She Ji 11, 31–60. doi: 10.1016/j.sheji.2025.01.002
Cunningham, F. C., Ranmuthugala, G., Westbrook, J. I., and Braithwaite, J. (2019). Tackling the wicked problem of health networks: the design of an evaluation framework. BMJ Open 9:e024231. doi: 10.1136/bmjopen-2018-024231
de Vos, L., Mazinyo, E., Bezuidenhout, D., Ngcelwane, N., Mandell, D. S., Schriger, S. H., et al. (2022). Reasons for missed opportunities to screen and test for TB in healthcare facilities. Public Health Action 12, 171–173. doi: 10.5588/pha.22.0042
Dewi, S. P., Ristianti, N. S., and Kurniati, R. (2021). Coastal settlement resilience to water-related disasters in Semarang City. IOP Conf. Series 623:012067. doi: 10.1088/1755-1315/623/1/012067
Dolezal, L. (2022). Shame anxiety, stigma and clinical encounters. J. Eval. Clin. Pract. 28, 854–860. doi: 10.1111/jep.13744
Dwi Laksono, A., Dwi Wulandari, R., Khaqiqi Nantabah, Z., Auliyati Agustina, Z., Ummu Aimanah, I., Rukmini, R., et al. (2020). The concept of illness among ethnic groups in Indonesia: a meta-ethnographic study. Syst. Rev. Pharm. 11, 584–591. doi: 10.31838/srp.2020.9.85
Garpenhag, L., and Dahlman, D. (2021). Perceived healthcare stigma among patients in opioid substitution treatment: a qualitative study. Subst. Abuse Treat. Prev. Policy 16:81. doi: 10.1186/s13011-021-00417-3
Giles, H. (2008). “Communication accommodation theory” in Engaging theories in interpersonal communication: Multiple perspectives In: LA Baxter and DO Braithwaite, editors. (Thousand oaks, California: SAGE Publications, Inc.), 161–174.
Gray, N. J., Hansen-Knarhoi, M., and Krause, V. L. (2008). Tuberculosis in illegal foreign fishermen: whose public health are we protecting? Med. J. Aust. 188, 144–147. doi: 10.5694/j.1326-5377.2008.tb01556.x
Ifon, I., Supodo, T., Sunarsih, S., Munir, S., and Harun, A. (2021). Risk factors pulmonary tuberculosis in Poasia health centres in the coastal region of Kendari City. Indoens. J. Health Sci. Res. Dev. 3, 149–158. doi: 10.36566/ijhsrd/Vol3.Iss1/68
Indriyani, W., Yudhistira, M. H., Sastiono, P., and Hartono, D. (2022). The relationship between the built environment and respiratory health: evidence from a longitudinal study in Indonesia. SSM Popul. Health 19:101193. doi: 10.1016/j.ssmph.2022.101193
Jiang, W., Dong, D., Febriani, E., Adeyi, O., Fuady, A., Surendran, S., et al. (2024). Policy gaps in addressing market failures and intervention misalignments in tuberculosis control: prospects for improvement in China, India, and Indonesia. Lancet Reg. Health 46:101045. doi: 10.1016/j.lanwpc.2024.101045
Kılıç, A., Zhou, X., Moon, Z., Hamada, Y., Duong, T., Layton, C., et al. (2025). A systematic review exploring the role of tuberculosis stigma on test and treatment uptake for tuberculosis infection. BMC Public Health 25:628. doi: 10.1186/s12889-024-20868-0
Kurtuluş, Ş., Can, R., and Sak, Z. H. A. (2020). New perspective on rise of tuberculosis cases: communal living. Cent. Eur. J. Public Health 28, 302–305. doi: 10.21101/cejph.a6016
Lee, J. Y., Kwon, N., Goo, G. y., and Cho, S. i. (2022). Inadequate housing and pulmonary tuberculosis: a systematic review. BMC Public Health 22:622. doi: 10.1186/s12889-022-12879-6
Lönngren, J., and van Poeck, K. (2021). Wicked problems: a mapping review of the literature. Int. J. Sustain. Dev. World Ecol. 28, 481–502. doi: 10.1080/13504509.2020.1859415
Mahendradhata, Y., Lestari, T., Probandari, A., Indriarini, L. E., Burhan, E., Mustikawati, D., et al. (2015). How do private general practitioners manage tuberculosis cases? A survey in eight cities in Indonesia public health. BMC. Res. Notes 8. doi: 10.1186/s13104-015-1560-7
Maneze, D., Weaver, R., Kovai, V., Salamonson, Y., Astorga, C., Yogendran, D., et al. (2019). “Some say no, some say yes”: receiving inconsistent or insufficient information from healthcare professionals and consequences for diabetes self-management: a qualitative study in patients with type 2 diabetes. Diabetes Res. Clin. Pract. 156:107830. doi: 10.1016/j.diabres.2019.107830
Msoka, E. F., Orina, F., Sanga, E. S., Miheso, B., Mwanyonga, S., Meme, H., et al. (2021). Qualitative assessment of the impact of socioeconomic and cultural barriers on uptake and utilisation of tuberculosis diagnostic and treatment tools in East Africa: a cross-sectional study. BMJ Open 11:e050911. doi: 10.1136/bmjopen-2021-050911
Mukerji, R., and Turan, J. M. (2018). Exploring manifestations of tb-related stigma experienced by women in Kolkata, India. Ann. Glob. Health 84, 727–735. doi: 10.29024/aogh.2383
Mulholland, G. E., Herce, M. E., Bahemuka, U. M., Kwena, Z. A., Jeremiah, K., Okech, B. A., et al. (2023). Geographic mobility and treatment outcomes among people in care for tuberculosis in the Lake Victoria region of East Africa: a multi-site prospective cohort study. PLOS Glob. Public Health 3:e0001992. doi: 10.1371/journal.pgph.0001992
Nawiyanto, N. (2017). Indigenous medical tradition in a frontier society of Java, Indonesia Man India 97 283–298. Available online at: https://www.researchgate.net/publication/318777807
Neethiselvan, R., Gayathri, G., and Shanmughapriya, S. (2021). Assessment of health seeking behaviour among fishermen community in Puducherry. Int. J. Commun. Med. Public Health 8:732. doi: 10.18203/2394-6040.ijcmph20210230
Noviyani, A., Nopsopon, T., and Pongpirul, K. (2021). Variation of tuberculosis prevalence across diagnostic approaches and geographical areas of Indonesia. PLoS One 16:e0258809. doi: 10.1371/journal.pone.0258809
Oloyede, M. O., Williams, A. B., Ode, G. O., and Benson, N. U. (2022). Coastal vulnerability assessment: a case study of the Nigerian coastline. Sustainability 14:2097. doi: 10.3390/su14042097
Puspita, T., Suryatma, A., Simarmata, O. S., Veridona, G., Lestary, H., Athena, A., et al. (2021). Spatial variation of tuberculosis risk in Indonesia 2010-2019. Health Sci. J. Indonesia 12, 104–110. doi: 10.22435/hsji.v12i2.5467
Ritonga, I. L., Setyowati, S., Handiyani, H., and Nursasi, A. Y. (2023). Exploring the tuberculosis medication program in Indonesia as perceived by patients and their families: a qualitative study. Belitung Nurs. J. 9, 124–131. doi: 10.33546/bnj.2484
Rosadi, D., Lasari, H. H. D., Tazkiah, M., Fadillah, A., Sepira, Y., and Maulidah, S. (2025). Environmental factors associated with pulmonary tuberculosis in Martapura’s primary health center. Jurnal Presipitasi 22, 476–484. doi: 10.14710/presipitasi.v22i2.476-484
Salomon, A., Boffa, J., Moyo, S., Chikovore, J., Sulis, G., Daniels, B., et al. (2022). Prescribing practices for presumptive TB among private general practitioners in South Africa: a cross-sectional, standardised patient study. BMJ Glob. Health 7, 1–12. doi: 10.1136/bmjgh-2021-007456
Singal, S., Modi, N., Singal, A., and Agrawal, H. (2025). Investigating the prevalence of tuberculosis in urban slums: a pathological cross-sectional approach. Eur. J. Cardiovasc. Med. 15, 198–202. doi: 10.5083/ejcm/25-01-3
Sommerland, N., Wouters, E., Mitchell, E. M. H., Ngicho, M., Redwood, L., Masquillier, C., et al. (2017). Evidence-based interventions to reduce tuberculosis stigma: a systematic review. Int. J. Tuberc. Lung Dis. 21, S81–S86. doi: 10.5588/ijtld.16.0788
Subandi, M. A., and Good, B. J. (2018). Shame as a cultural index of illness and recovery from psychotic illness in Java. Asian J. Psychiatr. 34, 33–37. doi: 10.1016/j.ajp.2018.04.005
Sulis, G., Adam, P., Nafade, V., Gore, G., Daniels, B., Daftary, A., et al. (2020). Antibiotic prescription practices in primary care in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. 17:e1003139. doi: 10.1371/journal.pmed.1003139
Suyami, S., Fakhriati, F., Syahrul, N., Ma’rifat, D. F., Sumarno, S., Nurwanti, Y. H., et al. (2025). Sawan: exploring the knowledge and wisdom of Javanese traditional healing practices. Cogent Arts Humanit. 12, 1–13. doi: 10.1080/23311983.2025.2451517
Tedla, K., Medhin, G., Berhe, G., Mulugeta, A., and Berhe, N. (2020). Delay in treatment initiation and its association with clinical severity and infectiousness among new adult pulmonary tuberculosis patients in Tigray, northern Ethiopia. BMC Infect. Dis. 20:456. doi: 10.1186/s12879-020-05191-4
Tosepu, R., Sani, A., Effendy, D. S., and Ahmad, L. O. A. I. (2024). The association between climate variables and tuberculosis in Kolaka District, Southeast Sulawesi Province, Indonesia, 2013–2020: a Bayesian autoregressive model. F1000Res 12:1507. doi: 10.12688/f1000research.138859.2
Wako, W. G., Wasie, A., Wayessa, Z., and Fikrie, A. (2021). Determinants of health system diagnostic delay of pulmonary tuberculosis in Gurage and Siltie zones, South Ethiopia: a cross-sectional study. BMJ Open 11:e047986. doi: 10.1136/bmjopen-2020-047986
Wekunda, P. W., Aduda, D. S. O., and Guyah, B. (2021). Determinants of tuberculosis treatment interruption among patients in Vihiga County, Kenya. PLoS One 16:e0260669. doi: 10.1371/journal.pone.0260669
Wiem Lestari, B., McAllister, S., Fortuna Hadisoemarto, P., Afifah, N., Dewi Jani, I., Murray, M., et al. (2020). Patient pathways and delays to diagnosis and treatment of tuberculosis in an urban setting in Indonesia. Lancet Regi. Health Western Pacific 5, 5–9. doi: 10.1016/j.lanwpc.2020.10
Winardi, W., Nalapraya, W. Y., Sarifuddin, S., Anwar, S., Yufika, A., Wibowo, A., et al. (2022). Knowledge and attitudes of Indonesian general practitioners towards the isoniazid preventive therapy program in Indonesia. J. Prev. Med. Public Health 55, 428–435. doi: 10.3961/jpmph.22.248
World Health Organization. (2015). The end TB strategy. World Health Organization. Available online at: https://www.who.int/teams/global-tuberculosis-programme/the-end-tb-strategy
Keywords: tuberculosis, wicked problem, coastal urban settlements, stigma, health communication, health system fragmentation
Citation: Shaluhiyah Z, Handayani S, Sriatmi A, Agushybana F and Rimawati E (2025) Understanding tuberculosis as a wicked problem: a qualitative study in coastal urban settlements of Semarang, Indonesia. Front. Commun. 10:1719819. doi: 10.3389/fcomm.2025.1719819
Edited by:
Uttaran Dutta, Arizona State University, United StatesReviewed by:
Olih Solihin, Indonesia Computer University, IndonesiaMochamad Kevin Romadhona, Airlangga University, Indonesia
Laila Alfirdaus, Diponegoro University, Indonesia
Apriana Rahmawati, Universitas Jember, Indonesia
Copyright © 2025 Shaluhiyah, Handayani, Sriatmi, Agushybana and Rimawati. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zahroh Shaluhiyah, c2hhbHVoaXlhaC56YWhyb2hAZ21haWwuY29t
 Zahroh Shaluhiyah
Zahroh Shaluhiyah Sri Handayani
Sri Handayani Ayun Sriatmi
Ayun Sriatmi Farid Agushybana
Farid Agushybana Eti Rimawati
Eti Rimawati