- 1Department of Orthopedics, Zhejiang Hospital, Hangzhou, China
- 2Department of Orthopedics, The Second Clinical Medical College of Zhejiang Chinese Medical University, Hangzhou, China
- 3Department of Orthopedics, Traumatology and Orthopedics Hospital of Traditional Chinese Medicine of Xiaoshan District, Hangzhou, China
Summary: By analyzing data from NHANES, we aimed to evaluate the prevalence, characteristics, and associated factors of wrist fractures in Americans aged 50 and above.
Introduction: Wrist fractures, whose prevalence increases with age, are one of the most common fractures in the United States. However, epidemiological studies on the prevalence of wrist fractures of certain ages were limited.
Methods: The data of Americans aged 50 or above from 2013–2014 and 2017–2018 in NHANES were extracted and analyzed.
Results: The prevalence of wrist fractures among Americans whose age was 50 or above was 12%, which was similar between men and women (men 12.8% vs. women 11.4%, p = 0.267). Among those who had experienced their first wrist fracture, 17.8% of the population experienced a second wrist fracture. The top two causes of the first wrist fracture were a fall from a standing height (56%) or a hard fall (34.8%). The prevalence of wrist fractures was higher in men than in women (13.7% versus 8.7%, p = 0.023) aged < 60, but higher in women than in men aged ≥ 60 (11.8% versus 14.3%, p = 0.007). Multivariate analysis showed that obesity, frequent drinking, current smoking, high serum phosphate level, non-Hispanic white women, and osteoporosis were independently associated with wrist fractures. Stratified by race, osteoporosis, frequent drinking, and high serum phosphate level were risk factors for wrist fractures in all races. As for Mexican Americans, non-Hispanic whites, and other races including multi-racial, current smoking was a risk factor of wrist factures. Furthermore, obesity was positively associated with wrist fractures in Mexican Americans, other Hispanics, and non-Hispanic whites.
Conclusion: The prevalence of wrist fractures in Americans aged 50 and above was 12%. Falling from a standing height was the main cause of the first wrist fracture. Frequent drinking, current smoker, high serum phosphate level, osteoporosis, obesity, and non-Hispanic women were more likely to experience wrist fractures.
Introduction
Wrist fractures are one of the most common fractures in the United States, accounting for about one-sixth of all fractures treated in emergency departments. The prevalence of wrist fractures increases with age (1–4). Studies have implied a significantly increased risk of recurrent wrist fractures within 7 years after the incidence of the initial wrist fracture, and risks of hip and vertebral fractures increased as well (5–7). Wrist fractures are usually followed by acute pain and swelling in the wrist and lead to dysfunction of wrist and even the quality of life if not being treated timely or appropriately (8, 9). There is also an increased risk of death following wrist fractures: within 5 years of the occurrence of distal fracture of the forearm, patients aged 65 to 74 have a death risk of 13.1%, while that of patients above 85 years old was 44.8% (10). It is predicted that by the year 2040, treatment cost for fractures would add up to $50 billion, which adds to the burden of the national healthcare system (11). In the U.S., the incidence rate of wrist fractures was three times higher than that of hip fractures. Therefore, even though the cost for hip fracture treatment per patient is higher, the overall treatment fee for wrist fractures surpasses that for hip and other fractures, which is why wrist fractures have drawn more attention from healthcare (7, 12). Therefore, it is high time that we design more studies to assess the prevalence, characteristics, and associated risk factors of wrist fracture, contributing to their prevention and treatment measures. However, epidemiological studies on incidence of wrist fractures were limited (5, 13). There has not been reports on the prevalence of wrist fractures yet. Therefore, this study aimed to comprehensively investigate the prevalence, characteristics, and related risk factors of wrist fracture among Americans aged 50 and above according to NHANES data in two year groups of 2013–2014 and 2017–2018. To the best of our knowledge, our study conducts the first research on patients with wrist fractures above 50 years of age based on data extracted from the NHANES database, which can enlighten the understanding for the disease as well as lending insight into prevention and improving prognosis.
Methods
Study Population
The National Health and Nutrition Examination Survey (NHANES) is a cross-sectional study of the American population collected every 2 years by the Center for Disease Control and Prevention (CDC), whose data are publicly available for use worldwide. NHANES was approved by the CDC for written informed consent from each participant. The data of 5,846 Americans aged 50 or above from 2013–2014 and 2017–2018 NHANES were extracted to estimate the prevalence of wrist fractures among the U.S. civilian population aged ≥ 50. All study subjects were examined physically and evaluated at medical centers. In this study, 4 subjects who had poor memory of their own past wrist fractures were excluded, while a total of 5,842 remaining subjects were included into the cohort, which contained 554 wrist fracture cases (male subjects, n = 239; female subjects, n = 315).
Study Variables and Covariates
Self-reported conditions of individuals in the NHANES data were collected through methods of standardized questionnaires and medical evaluation at medical centers with professional assistance. To define diagnosis of current wrist fracture or wrist fracture history, participants were asked to recall whether they had previously been diagnosed with wrist fracture by a professional orthopedist. Answers included yes, no, refused, don’t know, and missing. Participants who refused to answer the questions, or whose answer is “I don’t know” or “missing” were excluded from the analysis. Details of questionnaires could be accessed online: https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/OSQ_H.htm and https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/OSQ_J.htm. In combination with the epidemiological characteristics of previous wrist fractures and NHANES data variables, we collected the following variables of Americans aged 50 and above: age, gender, number of fracture onsets, the specific age and reason of the first wrist fracture [reasons include (1) a fall from a standing height or less, for example, tripped, slipped, fell out of bed; (2) a hard fall, such as falling off a ladder or step stool, or down the stairs; and (3) a car accident or other severe trauma], race (Mexican Americans, other Hispanics, non-Hispanic whites, non-Hispanic blacks, and other race, including multi-racial), education (less than high school, high school or greater), marital status, smoking history, drinking history, obesity, hypertension, diabetes, osteoporosis, medication history of prednisone or cortisone, wrist fracture history of parents, and serum calcium and phosphorus level. Participants were defined as high blood pressure patients if they complied with at least one of the following conditions: (1) currently taking antihypertensive medications; (2) previously diagnosed by a physician; (3) four blood pressure measurements indicated a mean systolic blood pressure ≥ 130 mmHg; (4) diastolic blood pressure ≥ 80 mmHg (14). Obesity was defined by body mass index (BMI) ≥ 30 kg/m2 (15). Diabetes was defined if the participant complied with at least one of the following conditions: (1) diagnosed by a physician; (2) currently taking hypoglycemic drugs; (3) fasting blood glucose ≥ 130 mg/dl; (4) glycated hemoglobin ≥ 6.5% (16). Kidney conditions were estimated based on the glomerular filtration rate in serum creatinine: eGFR (ml/min/1.73 m2) = 175 × standardized Scr−1.154 × age−0.203 × 1.212 [if black] × 0.742 [if female] (17). EGFR < 60 ml/min/1.73 m2 was defined as chronic kidney disease (CKD), indicated by the Modification of Diet in Renal Disease (MDRD) Study (18). Marital status included living alone (unmarried, separated, divorced, and widowed) and not living alone (living with a partner and married). All details of study variables and covariates in the present study could be accessed through the webpage www.cdc.gov/nchs/nhanes.
Statistical Analysis
Statistical analysis was performed using R version 4.1.0. Considering the complex design of study of NHANES, we applied the survey package in R to calculate sample-weighted prevalence and other statistics to study the population characteristics of American wrist fracture patients. In addition, generalized linear model was used to analyze variables including age, gender, race, education, marital status, smoking, drinking, hypertension, diabetes mellitus, heart failure, obesity, chronic kidney diseases, osteoporosis, medication history of prednisone or cortisone, history of parental wrist fracture, and univariate and multivariate relationships with wrist fractures. The covariate with p-value < 0.20 in univariate analysis was included in the multivariate logistic regression analysis to study risk factors related to wrist fracture. p < 0.05 (two-sided) was considered statistically significant.
Results
Clinical Characteristics
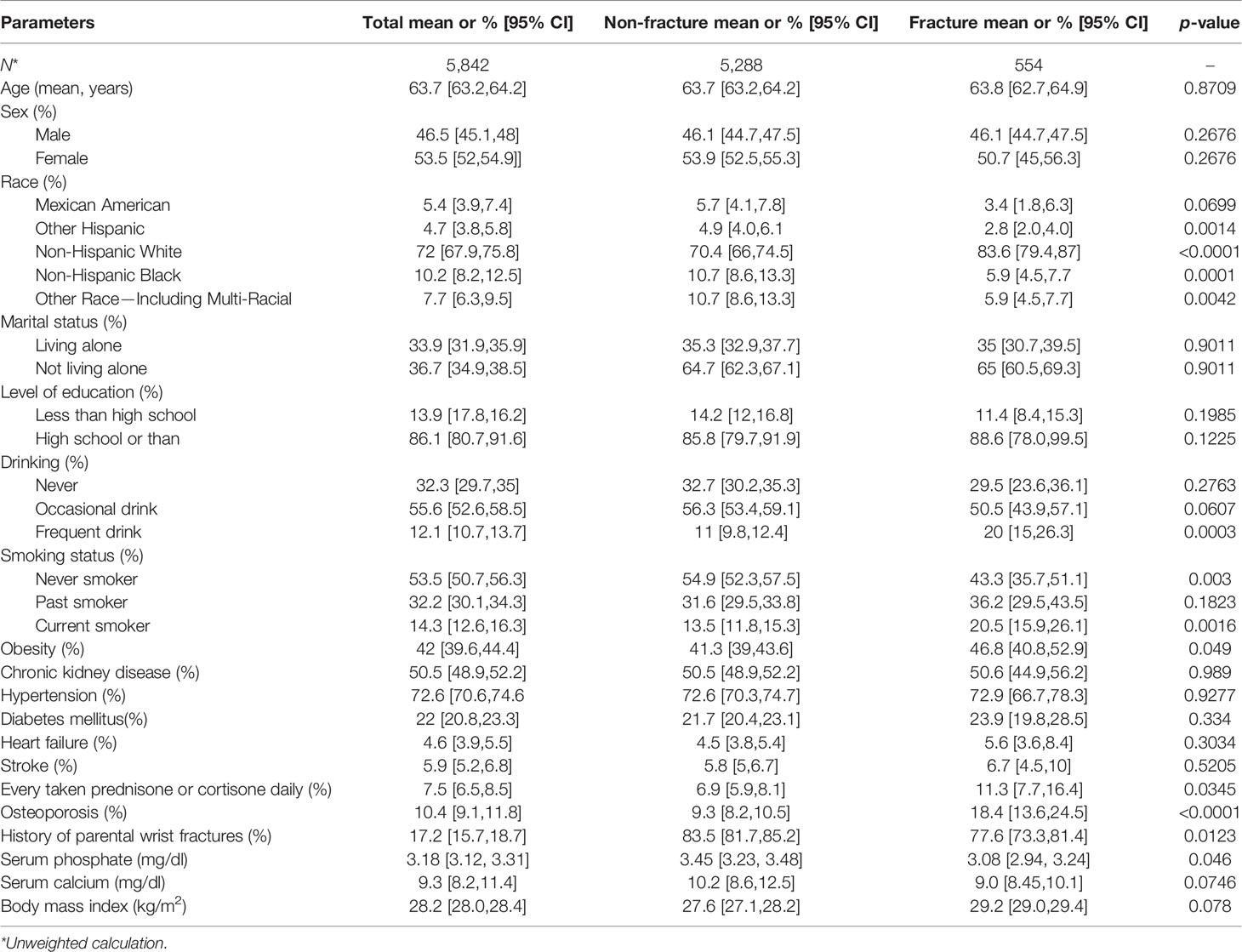
Clinical characteristics of the study population are displayed in Table 1. Men took up 46.5% of the total cases while women took up 53.5%. The weighted mean age was 63.7. Other Hispanics, non-Hispanic blacks, and other races including multi-racial, as well as never smokers and participants with a history of parental wrist fracture were higher in the wrist fracture group; serum calcium and serum phosphorus levels were lower in the wrist fracture group compared to the non-wrist fracture group. Non-Hispanic whites and participants with osteoporosis, obesity, daily oral administration of cortisone or prednisone, frequent drinking, and current smoking were more likely to be present in the non-wrist fracture group.
Population Characteristics of Wrist Fractures From NHANES, 2013–2014, and 2017–2018
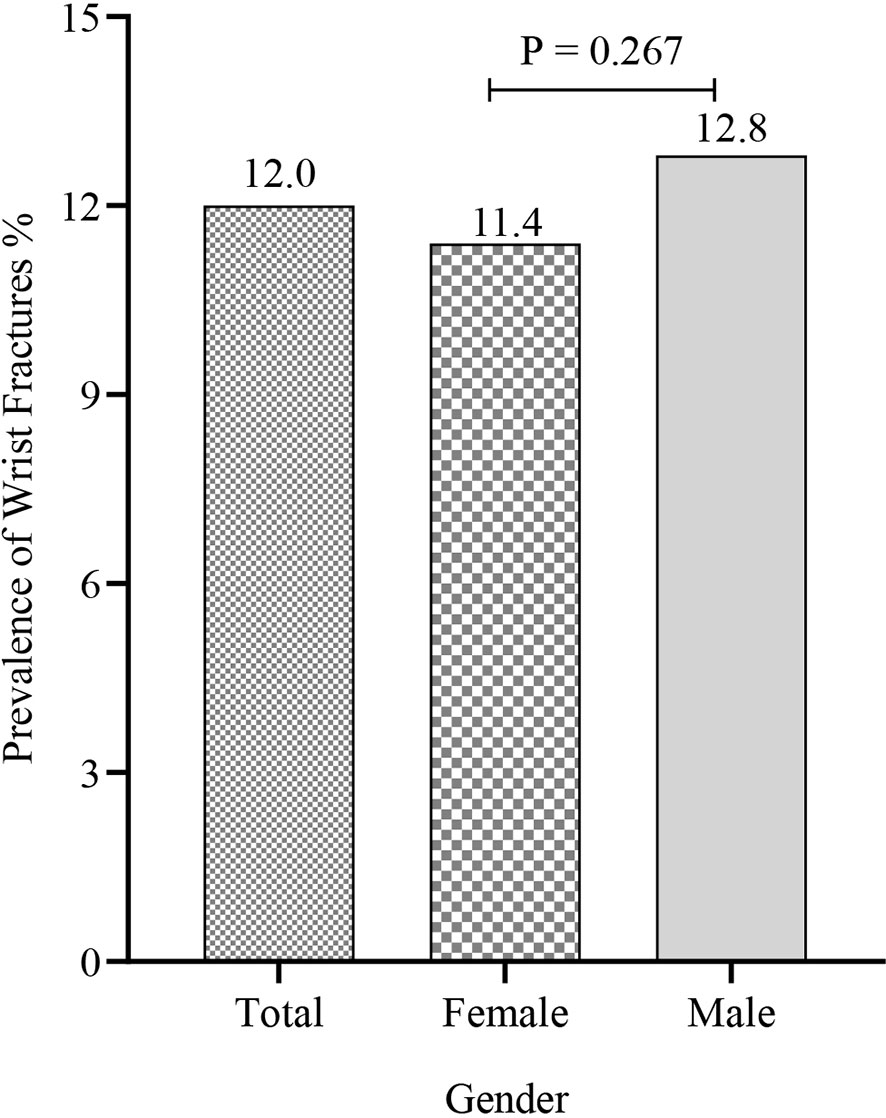
Among the total 5,842 US participants ≥ 50 years of age, 554 patients with wrist fractures were identified via standard questionnaire described above. The prevalence of wrist fractures was 12%, with similarities in men and women (men 12.8% vs. women 11.4%, p = 0.267) (Figure 1 and Additional file: Table S1). Non-Hispanic whites had the highest wrist fracture prevalence of 14% and there was a significant difference in prevalence between non-Hispanic whites and other ethnic groups (Mexican Americans: 7.6%, Other Hispanics: 7.3%, Non-Hispanic blacks: 6.9%, Other Race—Including Multi-Racial: 6.7%) (Figure 2 and Additional file: Tables S2, S3). Among the wrist fracture cases, a fall from a standing height or less (56%) or a hard fall (34.8%) was the leading cause of the first wrist fracture; 17.8% of the population experienced a second wrist fracture and 1.7% experienced four or more fractures. However, there was no gender difference in the cause and frequency (Table 2). Figure 3 demonstrates the difference in the prevalence of wrist fractures between the sexes when the first wrist fracture occurred before age 60 and after age 60. The prevalence of wrist fracture was higher in men than in women before the age of 60 years when the first wrist fracture occurred (13.7% vs. 8.7%, p = 0.023). However, after the age ≥ 60 years, the prevalence in women was higher than in men (11.8% vs. 14.3%, p = 0.007).
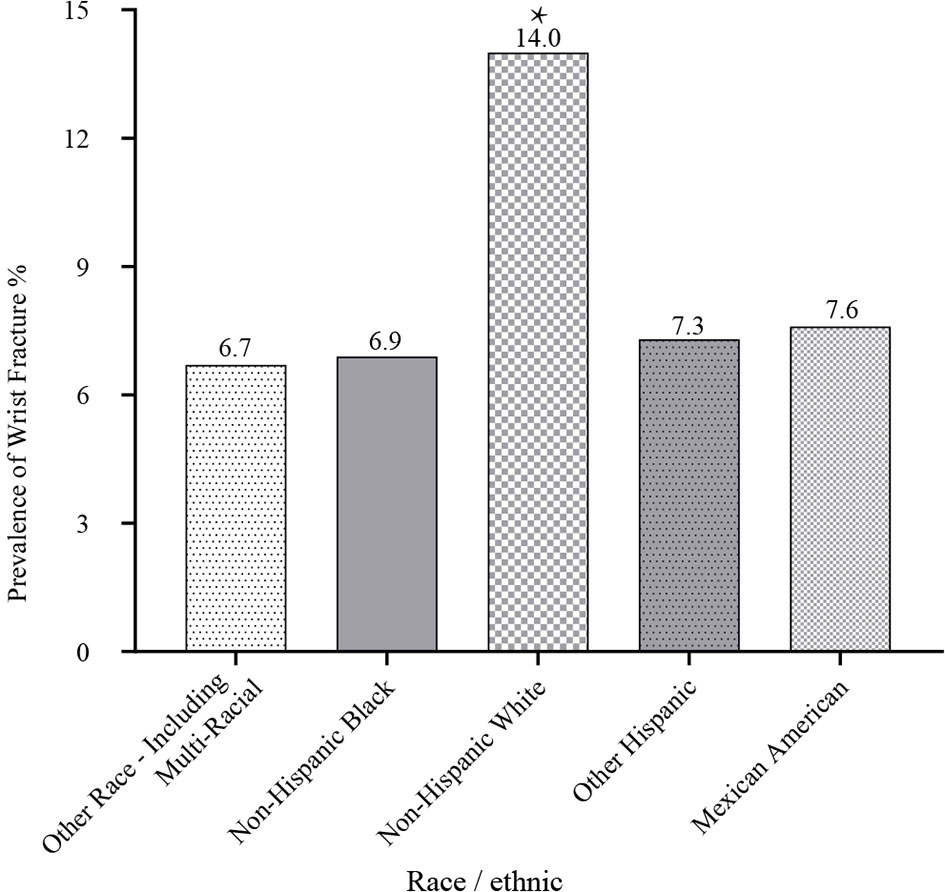
Figure 2 Relationship between race/ethnic and prevalence of wrist fractures. *p < 0.05 non-Hispanic white vs. other race/ethnic (Mexican Americans, other Hispanics, non-Hispanic blacks, and other races including multi-racial).
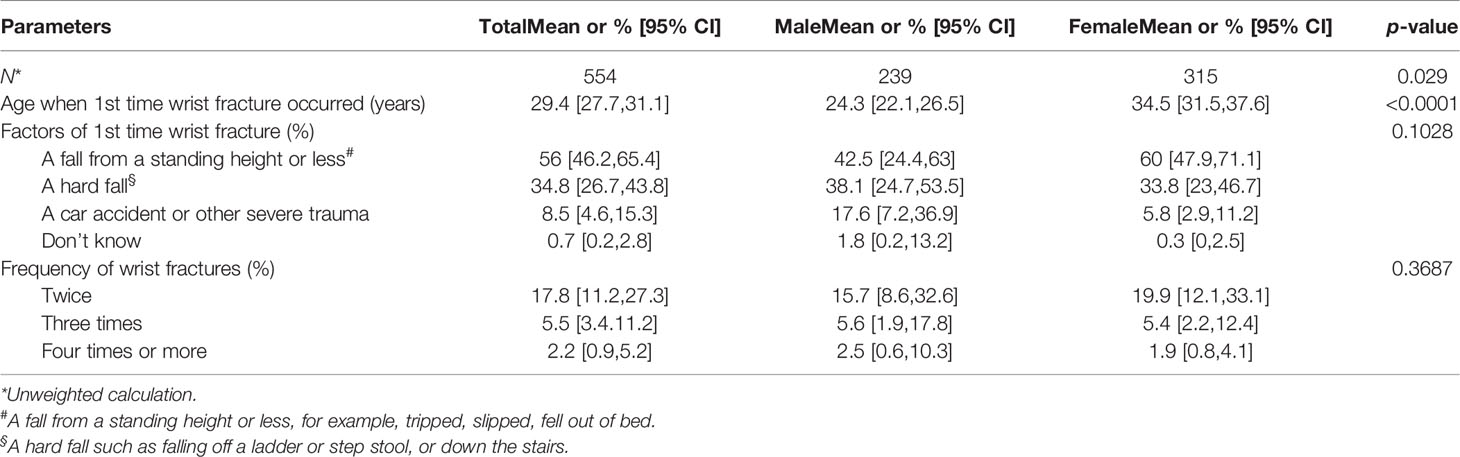
Table 2 Epidemiological characteristics of wrist fractures in the population aged 50 years or older.
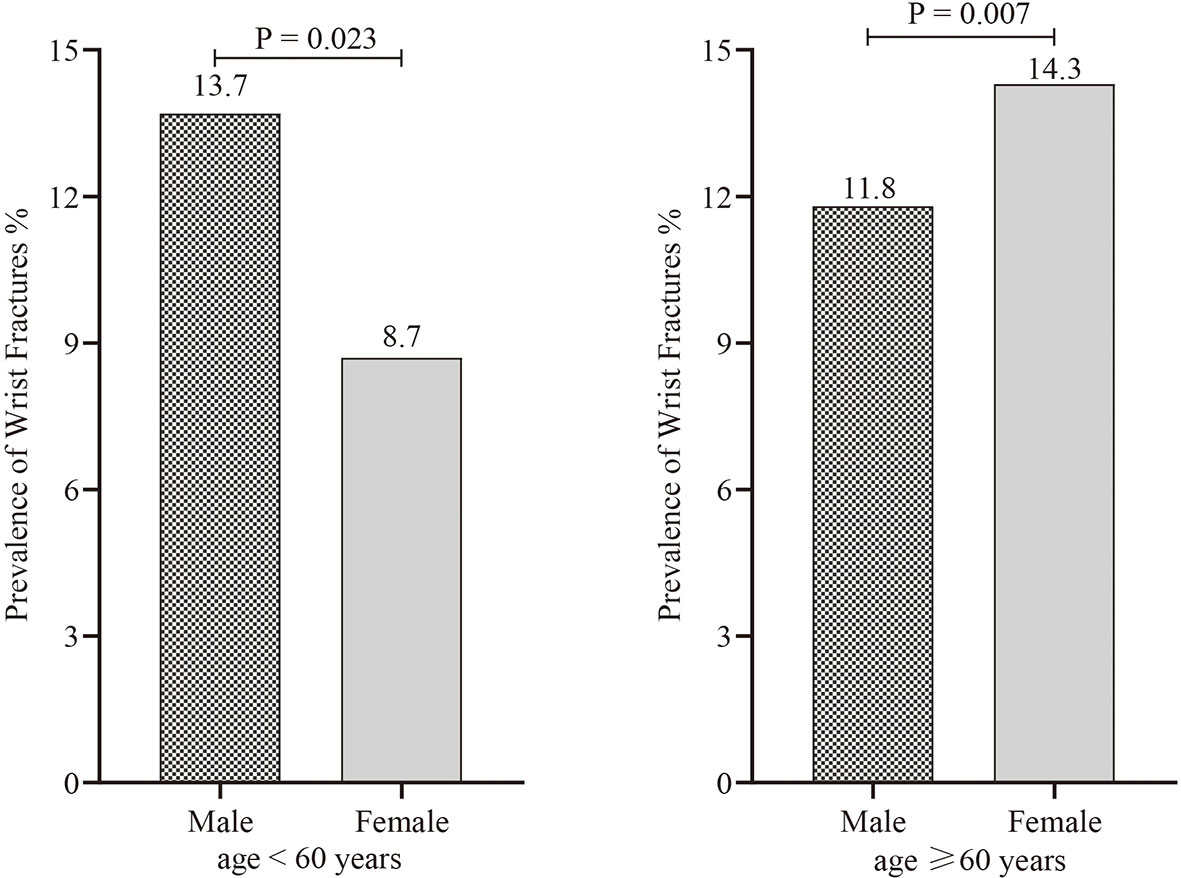
Figure 3 The difference in the prevalence of wrist fractures between the sexes when the first wrist fracture occurred at age < 60 years and age ≥ 60 years.
The Relationship Between Each Variable and Wrist Fracture
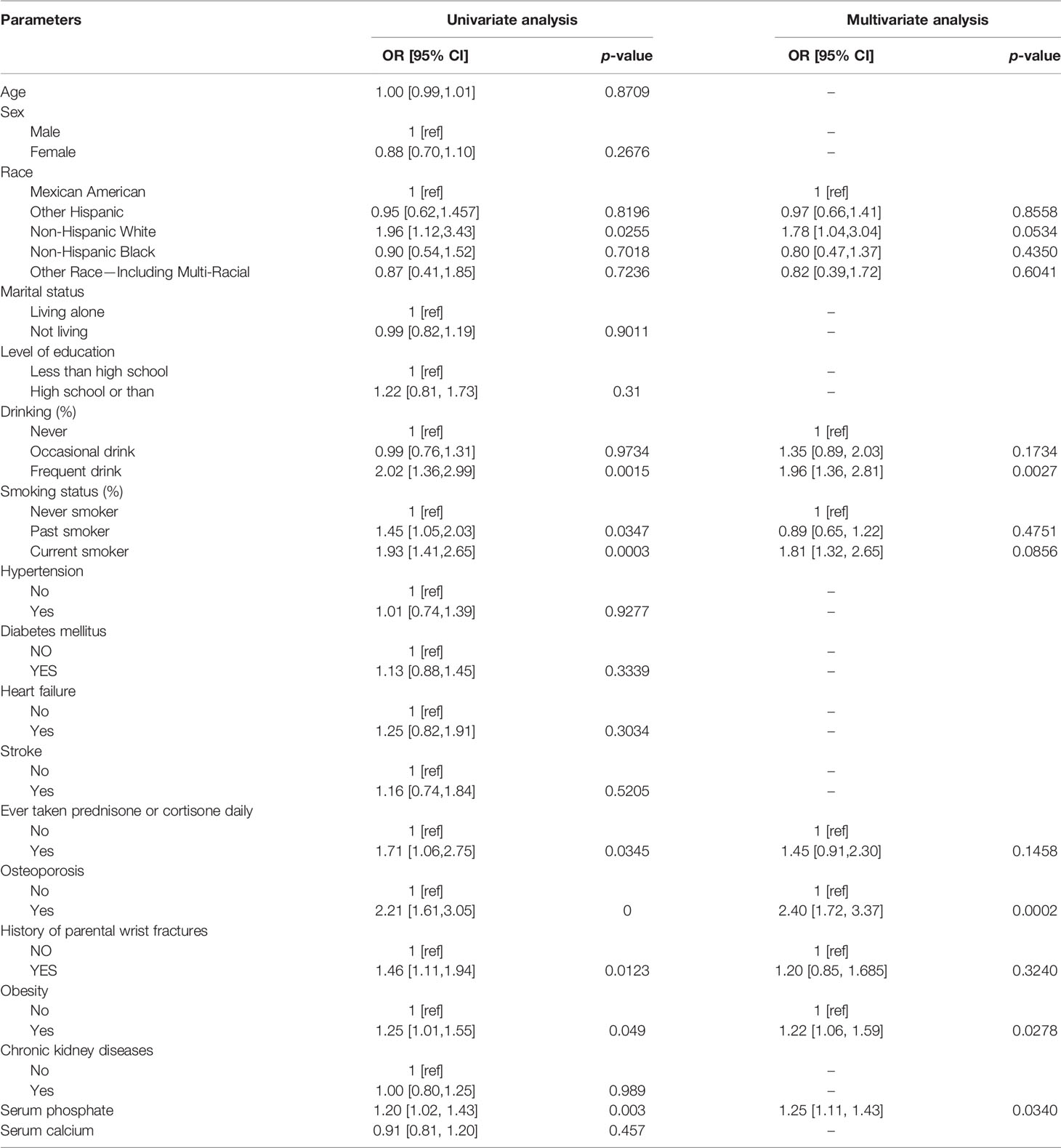
Univariate analysis of the wrist fractures and demographic characteristics of American men and women aged ≥ 50 are shown (Table 3): correlated risk factors included frequent drinking, smoking, daily oral administration of cortisone, concomitant osteoporosis, and fractures in family history and obesity.
Multivariate analysis of the wrist fractures and demographic characteristics of American men and women aged ≥ 50 are shown (Table 3): frequent drinking (OR: 1.96, 95% CI: 1.36–2.81), current smoker (OR: 1.81, 95% CI: 1.32–2.65), serum phosphate level (OR: 1.25, 95% CI: 1.11–1.43), osteoporosis (OR: 2.40, 95% CI: 1.72–3.37), and obesity (OR: 1.22, 95% CI: 1.06–1.59) were independent risk factors associated with wrist fractures (Table 3).
Subgroups
The analysis of sex and race subgroups was conducted. Non-Hispanic white women were positively associated with the occurrence of wrist fractures (Additional File: Table S4). Osteoporosis, frequent drinking, and high serum phosphate level were risk factors of wrist fractures in all races. Current smokers among Mexican Americans, non-Hispanic whites, and other race including multi-racial were significantly more likely to experience wrist fractures. Mexican Americans, other Hispanics, and non-Hispanic whites with obesity were more susceptible to wrist fractures (Additional file: Table S5).
Discussion
In the present cross-sectional study of 5,842 Americans ≥ 50 years of age, the prevalence of wrist fractures was 12%, without gender difference. Non-Hispanic whites had a higher risk of wrist fractures than other races. In addition, this study also showed that the first wrist fracture was mostly caused by a fall from a standing height (56%) or a hard fall (34.8%). Among those who had experienced their first wrist fracture, 17.8% had experienced a second wrist fracture, while 1.7% had experienced four or more fractures. The difference in the prevalence of wrist fractures between male and female was related to the age at which the first fracture occurred. Before the age of 60, men had a higher prevalence of their first wrist fracture than women. However, the situation became the opposite after the age of 60. Obesity, frequent drinking, current smoking, high serum phosphate level, non-Hispanic white women, and osteoporosis in women in the wrist fracture population were positively associated with wrist fractures. To the best of our knowledge, our study conducted the first research on patients with wrist fractures above the age of 50 based on data extracted from the NHANES, which enlightens the understanding of the disease as well as lends insight into prevention and improving the prognosis.
In 2000, WHO reported that the prevalence of wrist fracture in the total population whose ages ≥ 50 was 18.5% (19). Hye-Young Kwon et al. suggested that the prevalence in Korea was 4.52% with no gender difference (20). In a retrospective study of pediatric anterior wall fractures, the prevalence of forearm fractures in children aged 0 to 17 years was 24.1% in Washington, D.C (21). In the Oslo Health Study conducted on 5,976 participants, the prevalence of anterior wall fractures was 7.2% in men and 10.1% in women between the age of 59 and 60, and was 9.1% in men and 34.5% in women between the age of 75 and 76 (22). The Study of Women’s Health Across the Nation suggested that the prevalence of forearm fractures in postmenopausal women was 15% (23). The reason why these results differed from our result (prevalence of 12%) might be due to the different parameters included in the studied cases, such as age, region, and the initial occurrence time. Furthermore, we discovered that non-Hispanic whites had a higher risk of fracture, which was consistent with the results of a study of fracture risk in the diabetic population (24). The higher risk that non-Hispanic whites experienced might be related to race-specific genes and dietary characteristics (25). We also found that the first fracture presented earlier in women than in men, which was supported by the Oslo Health study (22). This phenomenon may be attributed to the menopausal period in women age above 50 (6, 13, 26–28).
In addition, this study also showed that a fall from a standing height was a major contributing factor to forearm fractures (56.0%), which was in line with the results reported by Norma J Mac Intyre and K C Chung (29, 30). People in their adolescence (under the age of 25) are more exposed to various activities and movements that have a potential danger of causing physical injuries, which included falling from a standing height (31–33). Therefore, active anti-osteoporosis treatment and various effective measures for preventing falls, such as wearing non-slip shoes, avoiding slippery road surface, and strengthening physical exercise, are vital for preventing forearm fractures. This study also discovered that sex differences in the prevalence of wrist fractures were associated with age at the time of fracture. The prevalence of wrist fractures was higher in men than in women when the first wrist fracture occurred before the age of 60, which was supported by previous epidemiological studies of wrist fractures in which young men were more likely to have wrist fractures than young women (34, 35). However, as women age, especially after menopause, they tend to lose more bone mass than men, which makes them more likely to suffer from wrist fractures (36, 37).
Obesity, smoking, drinking alcohol, high serum phosphate level, usage of corticosteroids, and osteoporosis are common factors associated with fractures (4, 38, 39). In our study, we have verified that obesity, occasional smoking, frequent smoking, excessive drinking, osteoporosis, and prednisolone intake accounted for a higher proportion in the population with wrist fractures. Smoking was an important risk factor for non-vertebral fracture in diabetic women, and the risk of non-vertebral fracture in diabetic women who have smoked is 3.47 times higher than that in non-smoking diabetic women (40). Smoking can promote fractures by reducing bone mineral density in a dose-dependent manner (41). Our study revealed that drinking alcohol also caused wrist fractures by affecting bone mineral density. Drinking alcohol was independently associated with an increased risk of forearm fractures in a dose–response manner. Compared with non-drinkers, the RR for forearm fractures was 1.38 for women who drank greater than or equal to 25 g daily (42). We further revealed the importance of smoking cessation and alcohol restriction for the prevention of hip fracture in the elderly. The positive association between osteoporosis and wrist fracture was only in women, presumably because as women age, estrogen decreases and BMD loss is more severe than in men, increasing the risk of fracture (43, 44). In line with the Osteoporotic Fractures in Men (MrOS) study, our study suggested that increased serum phosphate level can also increase the risk of wrist fractures (13). Increased serum phosphate level leads to decreased calcium absorption and may reflect hypoparathyroidism and liver disease, all of which are associated with osteoporosis, bone loss, and fracture risk (13, 45). Another interesting finding was that female non-Hispanic whites had an elevated risk of fractures (46). The mechanism for this may be gender and racial differences in serum 25(OH)D and BMD. Results of the 2003–2004 National Health and Nutrition Examination Survey (NHANES) showed that when serum 25(OH)D decreased in whites, BMD decreased significantly as well. However, such change was not observed in blacks (47).
The study conducted by Jason Lacombe et al. showed that high BMI was associated with a reduced risk of forearm and wrist neck fractures compared to women with an ideal BMI of 20.0 to 24.9 kg/m2 (48). The fact that a high BMI is protective and that weight loss appears to increase the risk of fractures may indicate an interaction between bone and fat (49).
Some limitations in this study should be addressed. First, this study could not avoid reporting bias and memory bias, such as the history of wrist fractures, medication history of prednisone or cortisone, and smoking and drinking history. Second, due to the design of a cross-sectional study, relative conclusions of causality could not be obtained. Finally, some variables that were closely related to fracture, such as activity level, use of vitamin D and/or calcium in dietary supplements, and BMD, were not considered as covariates because they involved too many missing values. Despite the discussed limitations, the overall data collected from the NHANES database were reliable and had undergone sufficient validation to filter accurate individual samples to determine the prevalence.
Conclusions
In conclusion, our study demonstrated that the prevalence of wrist fractures in Americans aged 50 and above was 12%. The prevalence was similar between male and female patients. Moreover, falling from a standing height was the main cause of the first wrist fracture. Frequent drinking, current smoker, high serum phosphate level, osteoporosis, and obesity were the risk factors for wrist fractures. In women, non-Hispanic whites are more likely to experience wrist fractures. Stratified by race, smoking was negatively associated with wrist fracture in other Hispanics and non-Hispanic blacks, while obesity was a risk factor of wrist fractures in Mexican Americans, other Hispanics, and non-Hispanic whites.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
This study was designed by JN. JY extracted the associated data from NHANES. QL performed statistical analysis. JY and QL completed the composition of the manuscript, helped supervised the analysis, and revised and approved the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the NHANES data for being publicly available on the Internet for use by researchers worldwide.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.800129/full#supplementary-material
Abbreviations
NHANES, National Health and Nutrition Examination Survey; CI, Confidence interval; OR, Odds ratio; BMI, Body mass index; EGFR, Estimate the glomerular filtration rate; CKD, Chronic kidney disease.
References
1. Hanel DP, Jones MD, Trumble TE. Wrist Fractures. Orthop Clin North Am (2002) 33(1):35–57, vii. doi: 10.1016/s0030-5898(03)00071-3
2. Black DM, Cooper C. Epidemiology of Fractures and Assessment of Fracture Risk. Clin Lab Med (2000) 20(3):439–53. doi: 10.1016/S0272-2712(18)30046-5
3. Cummings SR, Melton LJ. Epidemiology and Outcomes of Osteoporotic Fractures. Lancet (2002) 359(9319):1761–7. doi: 10.1016/s0140-6736(02)08657-9
4. Franic D, Verdenik I. Risk Factors for Osteoporosis in Postmenopausal Women - From The Point of View of Primary Care Gynecologist. Zdr Varst (2018) 57(1):33–8. doi: 10.2478/sjph-2018-0005
5. Crandall CJ, Hovey KM, Cauley JA, Andrews CA, Curtis JR, Wactawski-Wende J, et al. Wrist Fracture and Risk of Subsequent Fracture: Findings From the Women’s Health Initiative Study. J Bone Miner Res (2015) 30(11):2086–95. doi: 10.1002/jbmr.2559
6. Cerocchi I, Ghera S, Gasbarra E, Feola M, Tarantino U. The Clinical Significance of Wrist Fracture in Osteoporosis. Aging Clin Exp Res (2013) 25 Suppl 1:S81–2. doi: 10.1007/s40520-013-0083-0
7. Schousboe JT, Fink HA, Taylor BC, Stone KL, Hillier TA, Nevitt MC, et al. Association Between Self-Reported Prior Wrist Fractures and Risk of Subsequent Hip and Radiographic Vertebral Fractures in Older Women: A Prospective Study. J Bone Miner Res (2005) 20(1):100–6. doi: 10.1359/jbmr.041025
8. Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA. Functional Decline After Incident Wrist Fractures–Study of Osteoporotic Fractures: Prospective Cohort Study. Bmj (2010) 341:c3324. doi: 10.1136/bmj.c3324
9. Hsu H, Fahrenkopf MP, Nallamothu SV. Wrist Fracture. StatPearls. Treasure Island (FL: StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC (2021).
10. Curtis JR, Arora T, Matthews RS, Taylor A, Becker DJ, Colon-Emeric C, et al. Is Withholding Osteoporosis Medication After Fracture Sometimes Rational? A Comparison of the Risk for Second Fracture Versus Death. J Am Med Dir Assoc (2010) 11(8):584–91. doi: 10.1016/j.jamda.2009.12.004
11. Lane NE. Epidemiology, Etiology, and Diagnosis of Osteoporosis. Am J Obstet Gynecol (2006) 194(2 Suppl):S3–11. doi: 10.1016/j.ajog.2005.08.047
12. Pike C, Birnbaum HG, Schiller M, Sharma H, Burge R, Edgell ET. Direct and Indirect Costs of non-Vertebral Fracture Patients With Osteoporosis in the US. Pharmacoeconomics (2010) 28(5):395–409. doi: 10.2165/11531040-000000000-00000
13. Wright NC, Hooker ER, Nielson CM, Ensrud KE, Harrison SL, Orwoll ES, et al. The Epidemiology of Wrist Fractures in Older Men: The Osteoporotic Fractures in Men (MrOS) Study. Osteoporos Int (2018) 29(4):859–70. doi: 10.1007/s00198-017-4349-9
14. Reboussin DM, Allen NB, Griswold ME, Guallar E, Hong Y, Lackland DT, et al. Systematic Review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol (2018) 71(19):2176–98. doi: 10.1016/j.jacc.2017.11.004
15. Flegal KM, Ogden CL, Fryar C, Afful J, Klein R, Huang DT. Comparisons of Self-Reported and Measured Height and Weight, BMI, and Obesity Prevalence From National Surveys: 1999-2016. Obes (Silver Spring) (2019) 27(10):1711–9. doi: 10.1002/oby.22591
16. Carpenter DL, Gregg SR, Xu K, Buchman TG, Coopersmith CM. Prevalence and Impact of Unknown Diabetes in the ICU. Crit Care Med (2015) 43(12):e541–50. doi: 10.1097/ccm.0000000000001353
17. Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using Standardized Serum Creatinine Values in the Modification of Diet in Renal Disease Study Equation for Estimating Glomerular Filtration Rate. Ann Intern Med (2006) 145(4):247–54. doi: 10.7326/0003-4819-145-4-200608150-00004
18. Murphy D, McCulloch CE, Lin F, Banerjee T, Bragg-Gresham JL, Eberhardt MS, et al. Trends in Prevalence of Chronic Kidney Disease in the United States. Ann Intern Med (2016) 165(7):473–81. doi: 10.7326/m16-0273
19. Johnell O, Kanis JA. An Estimate of the Worldwide Prevalence and Disability Associated With Osteoporotic Fractures. Osteoporos Int (2006) 17(12):1726–33. doi: 10.1007/s00198-006-0172-4
20. Kwon HY, Ha YC, Yoo JI. Health-Related Quality of Life in Accordance With Fracture History and Comorbidities in Korean Patients With Osteoporosis. J Bone Metab (2016) 23(4):199–206. doi: 10.11005/jbm.2016.23.4.199
21. Ryan LM, Teach SJ, Searcy K, Singer SA, Wood R, Wright JL, et al. Epidemiology of Pediatric Forearm Fractures in Washington, Dc. J Trauma (2010) 69(4 Suppl):S200–5. doi: 10.1097/TA.0b013e3181f1e837
22. Alver K, Meyer HE, Falch JA, Søgaard AJ. Outdoor Air Pollution, Bone Density and Self-Reported Forearm Fracture: The Oslo Health Study. Osteoporos Int (2010) 21(10):1751–60. doi: 10.1007/s00198-009-1130-8
23. Greendale GA, Huang M, Cauley JA, Harlow S, Finkelstein JS, Karlamangla AS. Premenopausal and Early Postmenopausal Trabecular Bone Score (TBS) and Fracture Risk: Study of Women’s Health Across the Nation (SWAN). Bone (2020) 140:115543. doi: 10.1016/j.bone.2020.115543
24. Jain RK, Weiner MG, Zhao H, Williams KJ, Vokes T. Diabetes-Related Fracture Risk Is Different in African Americans Compared With Hispanics and Caucasians. J Clin Endocrinol Metab (2019) 104(11):5729–36. doi: 10.1210/jc.2019-00931
25. Curtis EM, van der Velde R, Moon RJ, van den Bergh JP, Geusens P, de Vries F, et al. Epidemiology of Fractures in the United Kingdom 1988-2012: Variation With Age, Sex, Geography, Ethnicity and Socioeconomic Status. Bone (2016) 87:19–26. doi: 10.1016/j.bone.2016.03.006
26. Masud T, Jordan D, Hosking DJ. Distal Forearm Fracture History in an Older Community-Dwelling Population: The Nottingham Community Osteoporosis (NOCOS) Study. Age Ageing (2001) 30(3):255–8. doi: 10.1093/ageing/30.3.255
27. Haentjens P, Johnell O, Kanis JA, Bouillon R, Cooper C, Lamraski G, et al. Evidence From Data Searches and Life-Table Analyses for Gender-Related Differences in Absolute Risk of Hip Fracture After Colles’ or Spine Fracture: Colles’ Fracture as an Early and Sensitive Marker of Skeletal Fragility in White Men. J Bone Miner Res (2004) 19(12):1933–44. doi: 10.1359/jbmr.040917
28. Beringer TR, Finch M, Mc ATH, Whitehead E, Keegan DA, Kelly J, et al. A Study of Bone Mineral Density in Women With Forearm Fracture in Northern Ireland. Osteoporos Int (2005) 16(4):430–4. doi: 10.1007/s00198-004-1684-4
29. MacIntyre NJ, Dewan N. Epidemiology of Distal Radius Fractures and Factors Predicting Risk and Prognosis. J Handb Ther (2016) 29(2):136–45. doi: 10.1016/j.jht.2016.03.003
30. Chung KC, Spilson SV. The Frequency and Epidemiology of Hand and Forearm Fractures in the United States. J Handb Surg Am (2001) 26(5):908–15. doi: 10.1053/jhsu.2001.26322
31. Earnshaw SA, Cawte SA, Worley A, Hosking DJ. Colles’ Fracture of the Wrist as an Indicator of Underlying Osteoporosis in Postmenopausal Women: A Prospective Study of Bone Mineral Density and Bone Turnover Rate. Osteoporos Int (1998) 8(1):53–60. doi: 10.1007/s001980050048
32. Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, Herndon JH. Distal Radius Fractures in Older Women: A 10-Year Follow-Up Study of Descriptive Characteristics and Risk Factors. The Study of Osteoporotic Fractures. J Am Geriatr Soc (2002) 50(1):97–103. doi: 10.1046/j.1532-5415.2002.50014.x
33. Diamantopoulos AP, Rohde G, Johnsrud I, Skoie IM, Hochberg M, Haugeberg G. The Epidemiology of Low- and High-Energy Distal Radius Fracture in Middle-Aged and Elderly Men and Women in Southern Norway. PloS One (2012) 7(8):e43367. doi: 10.1371/journal.pone.0043367
34. Donaldson LJ, Cook A, Thomson RG. Incidence of Fractures in a Geographically Defined Population. J Epidemiol Community Health (1990) 44(3):241–5. doi: 10.1136/jech.44.3.241
35. Maravic M, Taupin P, Landais P, Roux C. Hospitalized Wrist Fractures in France: Incidence and Burden Trend Changes. Orthop Traumatol Surg Res OTSR (2010) 96(6):662–6. doi: 10.1016/j.otsr.2010.04.012
36. Pinheiro MM, Reis Neto ET, Machado FS, Omura F, Yang JH, Szejnfeld J, et al. Risk Factors for Osteoporotic Fractures and Low Bone Density in Pre and Postmenopausal Women. Rev Saude Publica (2010) 44(3):479–85. doi: 10.1590/s0034-89102010000300011
37. Segheto KJ, Juvanhol LL, Carvalho CJ, Silva D, Kakehasi AM, Longo GZ. Factors Associated With Bone Mineral Density in Adults: A Cross-Sectional Population-Based Study. Rev da Escola Enfermagem da USP (2020) 54:e03572. doi: 10.1590/s1980-220x2018039903572
38. De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, et al. Body Mass Index as a Predictor of Fracture Risk: A Meta-Analysis. Osteoporos Int (2005) 16(11):1330–8. doi: 10.1007/s00198-005-1863-y
39. Hemenway D, Azrael DR, Rimm EB, Feskanich D, Willett WC. Risk Factors for Wrist Fracture: Effect of Age, Cigarettes, Alcohol, Body Height, Relative Weight, and Handedness on the Risk for Distal Forearm Fractures in Men. Am J Epidemiol (1994) 140(4):361–7. doi: 10.1093/oxfordjournals.aje.a117258
40. Jørgensen L, Joakimsen R, Ahmed L, Størmer J, Jacobsen BK. Smoking is a Strong Risk Factor for non-Vertebral Fractures in Women With Diabetes: The Tromsø Study. Osteoporos Int (2011) 22(4):1247–53. doi: 10.1007/s00198-010-1340-0
41. Ward KD, Klesges RC. A Meta-Analysis of the Effects of Cigarette Smoking on Bone Mineral Density. Calcif Tissue Int (2001) 68(5):259–70. doi: 10.1007/bf02390832
42. Hernandez-Avila M, Colditz GA, Stampfer MJ, Rosner B, Speizer FE, Willett WC. Caffeine, Moderate Alcohol Intake, and Risk of Fractures of the Hip and Forearm in Middle-Aged Women. Am J Clin Nutr (1991) 54(1):157–63. doi: 10.1093/ajcn/54.1.157
43. Aspray TJ, Hill TR. Osteoporosis and the Ageing Skeleton. Sub-cellular Biochem (2019) 91:453–76. doi: 10.1007/978-981-13-3681-2_16
44. Dontas IA, Yiannakopoulos CK. Risk Factors and Prevention of Osteoporosis-Related Fractures. J Musculoskelet Neuronal Interact (2007) 7(3):268–72.
45. Campos-Obando N, Koek WNH, Hooker ER, van der Eerden BC, Pols HA, Hofman A, et al. Serum Phosphate Is Associated With Fracture Risk: The Rotterdam Study and MrOS. J Bone Miner Res (2017) 32(6):1182–93. doi: 10.1002/jbmr.3094
46. Sakamoto R, Thorpe D, Knutsen R, Beeson L, Knutsen S. Ethnic Variations in Serum 25(Oh)D Levels and Bone Ultrasound Attenuation Measurements in Blacks and Whites. J Racial Ethn Health Disparities (2018) 5(2):439–48. doi: 10.1007/s40615-017-0387-4
47. Gutiérrez OM, Farwell WR, Kermah D, Taylor EN. Racial Differences in the Relationship Between Vitamin D, Bone Mineral Density, and Parathyroid Hormone in the National Health and Nutrition Examination Survey. Osteoporos Int (2011) 22(6):1745–53. doi: 10.1007/s00198-010-1383-2
48. Lacombe J, Cairns BJ, Green J, Reeves GK, Beral V, Armstrong MEG. The Effects of Age, Adiposity, and Physical Activity on the Risk of Seven Site-Specific Fractures in Postmenopausal Women. J Bone mineral Res (2016) 31(8):1559–68. doi: 10.1002/jbmr.2826
Keywords: wrist fracture, prevalence, cross-sectional study, NHANES, osteoporosis
Citation: Ye J, Li Q and Nie J (2022) Prevalence, Characteristics, and Associated Risk Factors of Wrist Fractures in Americans Above 50: The Cross-Sectional NHANES Study. Front. Endocrinol. 13:800129. doi: 10.3389/fendo.2022.800129
Received: 01 November 2021; Accepted: 11 March 2022;
Published: 25 April 2022.
Edited by:
Elaine Dennison, University of Southampton, United KingdomReviewed by:
Guido Zavatta, University of Bologna, ItalyMing Fu, Guangzhou Medical University, China
Deeptha Sukumar, Drexel University, United States
Chun-Ming Yin, First Affiliated Hospital of Gannan Medical University, China
Copyright © 2022 Ye, Li and Nie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juncai Ye, anVuY2FpangyMDIxQDE2My5jb20=; Jing Nie, ZHJqaW5nbmllQDEyNi5jb20=
 Juncai Ye1*
Juncai Ye1* Jing Nie
Jing Nie