- 1Department of Obstetrics, Sichuan Provincial Women’s and Children’s Hospital, The Affiliated Women’s and Children’s Hospital of Chengdu Medical College, Chengdu, Sichuan, China
- 2Department of Reproductive Medicine, Sichuan Jinxin Xinan Women and Children’s Hospital, Chengdu, Sichuan, China
- 3Reproductive Medicine Center, Sichuan Provincial Women’s and Children’s Hospital, The Affiliated Women’s and Children’s Hospital of Chengdu Medical College, Chengdu, Sichuan, China
- 4School of Clinical Medicine, Chengdu Medical College, Chengdu, Sichuan, China
- 5Reproductive Endocrinology, Department of Obstetrics and Gynecology, West China Second University Hospital, Sichuan University, Chengdu, Sichuan, China
- 6Center of Medical Genetics, West China Second University Hospital, Sichuan University, Chengdu, Sichuan, China
- 7West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, Sichuan, China
Background: Studies have reported that the age at natural menopause may vary between different ethnic groups. Chinese Han and Tibetan women exhibit substantial differences in their living environment, dietary habits, and lifestyle; however, few studies have specifically investigated the potential differences in their age at natural menopause. This study was designed to identify the discrepancy in the age at natural menopause between postmenopausal women of Chinese Han and Tibetan ethnicities.
Methods: A cross-section study has been conducted on 5,562 Han and 1,049 Tibetan postmenopausal women who were recruited by the China Multi-ethnic Cohort study from May 2018 to September 2019. The participants have resided in Chengdu City and Aba Prefecture, respectively, with ethnicity set as the primary exposure variable. Linear and multinomial logistic regression model was used to assess the association of the age at natural menopause with influencing factors and odds ratios for the association between premature ovarian failure, early and late menopause with the ethnicity, and influencing factors.
Results: The mean age at natural menopause of Han women was 0.74 year earlier than Tibetan women (P = 0.003). The Han women also showed a lower likelihood for experiencing late menopause with an adjusted odds ratio (95% confidence intervals) of 0.54 (0.34, 0.88) compared with the Tibetan women. Factors associated with later menopause have included older age at survey, ever married, high school and above educational level, annual household income of ≥200,000 RMB, no smoking, habit of eating spicy food, no history of severe food shortage, more gravidity, less parity, use of intrauterine device, and no history of using oral contraceptives.
Conclusions: The age at natural menopause of Chinese Han women was earlier than that of Chinese Tibetan women. Demographic, lifestyle, dietary habits, and reproductive factors may influence the age at natural menopause.
Introduction
Natural menopause is defined as the permanent cessation of menstruation due to the exhaustion of ovarian reserve, which is diagnosed as amenorrhea lasting for 12 consecutive months (1). Age at natural menopause (ANM) may reflect the reproductive lifespan of the ovary (2) and is 46 to 52 years old as reported worldwide (3). The ANM has been associated with health conditions. Earlier ANM (younger than 45 years old) has been associated with cardiovascular disease, type 2 diabetes, osteoporosis, and early death (4–6), while later ANM may increase the risk of endometrial cancer (7). Factors influencing the ANM have included genetics, ovarian diseases or surgery, environment, and unhealthy lifestyle (3, 8). Research on the ANM and its associated factors may facilitate the prevention of the disease, improving the quality of life and making reproductive plans.
The ANM has appeared to vary across different regions and ethnic groups (3). Studies have found that the ANM is earlier in Africans, Latin Americans, and Asians and is later in Europeans, Australians, and Americans (3, 9), which suggested that race/ethnicity is an independent predictor for the ANM (2, 9, 10), while others have reported that the difference in ANM among different ethnic groups may be explained to a large extent by controlling covariates such as socio-demography, lifestyle, and health conditions (11, 12). Therefore, whether ethnicity is an independent factor for the ANM has remained controversial.
China is a country with 56 ethnic groups. The different living environments, lifestyles, health conditions, and genetic backgrounds may have all contributed to the discrepancy in the ANM between different ethnic groups. Some studies have reported the ANM of Chinese women (13–15). Some have reported the average menopausal age for ethnic Han women to be later than that for Uyghur women from Xinjiang (48.11 vs. 47.01) (16) but was earlier than Tibetan women from Yunnan (48.30 vs. 48.90) (17). It is interesting to note that both natural and pathologically menopausal women have been included in these studies (16, 17). Only one study has reported that the ANM of Han women was earlier than that of Miao women from Guiyang (47.83 vs. 48.05) (18).
Sichuan is a Chinese province where all 56 ethnic groups reside and is also the second largest Tibetan residential area in China. In Chengdu (basin), the capital of Sichuan province, the major inhabitants are ethnic Hans. In Aba Prefecture (plateau), with a high altitude, low oxygen level, and intense ultraviolet radiation, the major inhabitants are Tibetans. Most Tibetans are engaged in animal husbandry, and their diets are mainly characterized by high-caloric and high-protein (19). Based on existing literature and documented ethnic differences (17), this study proposes the research hypothesis that the ANM of Han women was earlier than that of Tibetan women. Using data from the China Multi-ethnic Cohort (CMEC), we investigated the differences in the ANM between the Han and Tibetan postmenopausal women in Sichuan as well as the influencing factors.
Materials and methods
Study population
Our study utilized baseline data from the CMEC, a prospective cohort study aimed to investigate the genetic and environmental determinants of non-communicable diseases across diverse ethnic groups in Southwest China. The participants (n = 99,556; aged 30–79 years) were recruited voluntarily between May 2018 and September 2019 using multistage stratified cluster sampling through local communities. The main contents of the baseline survey have included demographic and socio-economic status, smoking habit, alcohol intake, diet, disease history, physical activity, and reproductive history. All participants completed a full questionnaire based on laptops through face-to-face interviews with audio recording in the local community health service centers or township health centers. On the same day of the survey, data quality inspectors randomly selected questionnaires and evaluated their data quality by listening to the audio recordings. All participants provided written informed consent and retained the right to withdraw at any time without penalty. The CMEC study design and survey methods has been described previously (20). The CMEC study has been approved by the Sichuan University Medical Ethical Review Board (IRB number: K2016038).
For this study, ethical approval was obtained from the Medical Ethics Committee of Sichuan Provincial Women’s and Children’s Hospital (no. 20240903) and then registered in the Chinese Clinical Trial Registry (ChiCTR2400090175). In this study, postmenopausal Han women who lived in Chengdu and postmenopausal Tibetan women who lived in Aba were enrolled from CMEC. Menopause was diagnosed as without menstruation for ≥12 months (1). All participants were permanent residents. The ethnic group was determined by their identity cards. Individuals were excluded for any of the following conditions: missing the information of ANM, history of cancer, hysterectomy, and ovariectomy before menopause.
Study factors
On the baseline questionnaire, postmenopausal women were asked about the age of last menstruation. Self-reported ANM was the primary outcome. Based on the ANM, menopause was divided into four types: premature ovarian failure (POF) (<40 years), early menopause (EM) (40 to 44 years), normal menopause (NM) (45 to 54 years), and late menopause (LM) (≥55 years) (4, 21).
Ethnicity was the primary exposure variable. Basal characteristics with potential effect on the ANM were included, such as sociodemographic factors (age at survey, marriage status, education level, and annual household income), lifestyle (smoking habit, passive smoking, labor history, pesticide exposure history, coal smoke exposure history, and severe food shortage history), dietary habit (alcohol intake, tea drinking, soft drink consumption, spicy foods, and numb foods), and reproductive history [(age at menarche, number of gravidity and parity, age at first birth, duration of breastfeeding per child, utilization of the intrauterine device (IUD), and utilization of an oral contraceptive (OC)].
Statistical analysis
Analyses were completed using R-4.2.0 (R Foundation for Statistical Computing). Descriptive statistics were presented as median and interquartile range (IQR) for continuous variables and numbers (percentages) for categorical variables. Kruskal–Wallis H test for continuous variables and chi-square test for categorical variables were used to compare the differences in baseline characteristics between Chinese Han and Tibetan postmenopausal women. Linear regression models were used to assess the association of ANM with ethnicity and influencing factors. To further estimate the adjusted regression coefficients (β) and 95% confidence intervals (CI), we have used the multivariable linear regression models. Multinomial logistic regression was used to estimate the adjusted odds ratios (ORs) and 95% CI for the association among POF, EM, and LM with ethnicity and the influencing factors. Two-sided P-values <0.05 were considered statistically significant. Considering that the recall bias among elderly respondents may have influenced the study outcomes, we conducted a sensitivity analysis by excluding females whose age at survey was over 75 years.
Results
A total of 5,562 Han and 1,049 Tibetan postmenopausal women were enrolled, and 180 postmenopausal women were excluded (Figure 1). The exposure variables and operational definitions are summarized in Supplementary Table S1.
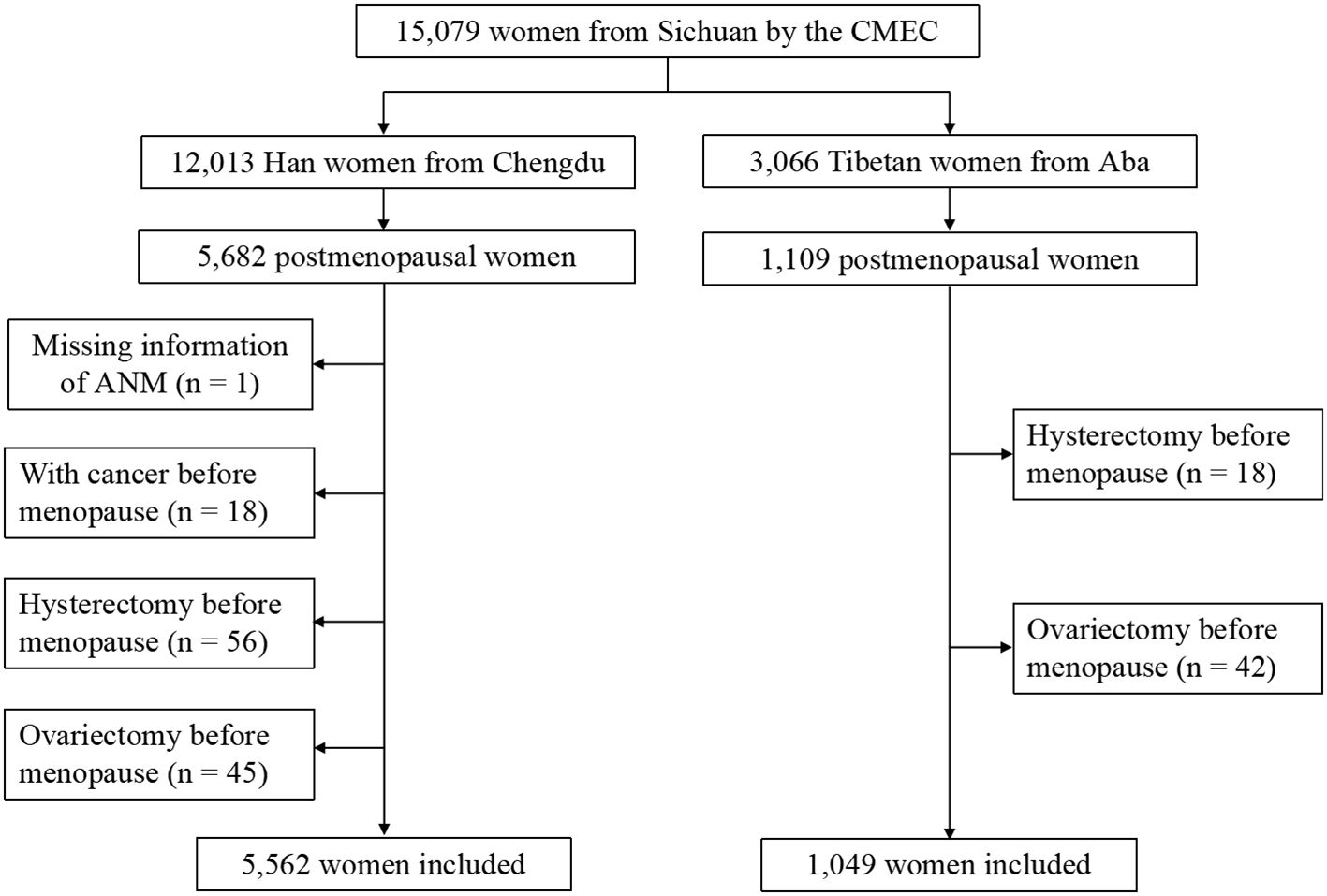
Figure 1. Flowchart of enrollment. Progress of retrospective cohort study including enrollment and exclusion.
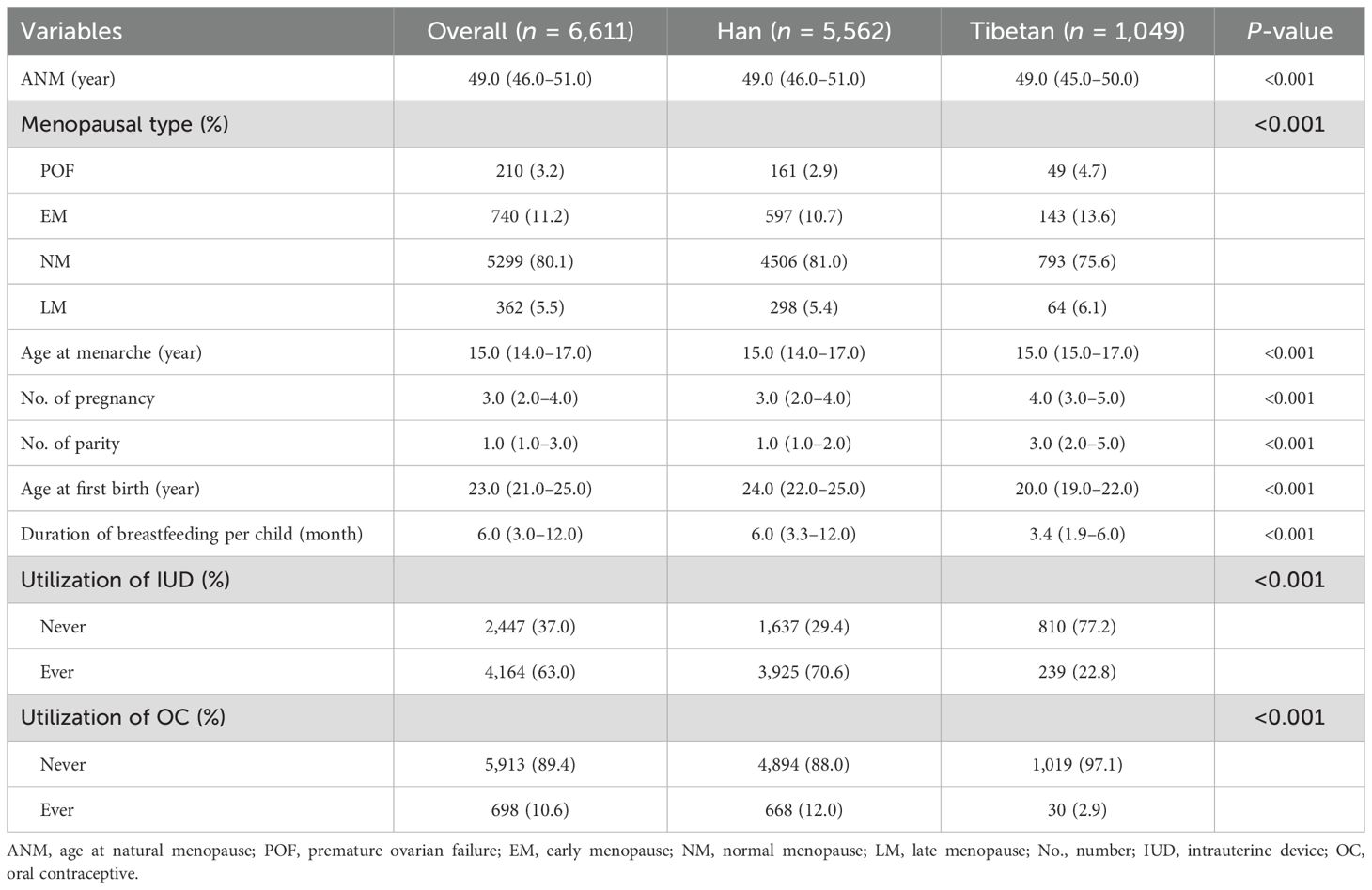
Menstruation and gestation of the postmenopausal women
In Han postmenopausal women, ANM, the age at first birth, duration of breastfeeding per child, utilization of IUD, and utilization of OC were significantly higher, whereas the age at menarche, number of gravidity, and parity were significantly lower than those of Tibetan postmenopausal women (P < 0.001). The proportion of menopausal types was also significantly different between the two groups, with the Han women tending to have more NM and fewer POF, EM, and LM (P < 0.001) (Table 1, Figure 2).
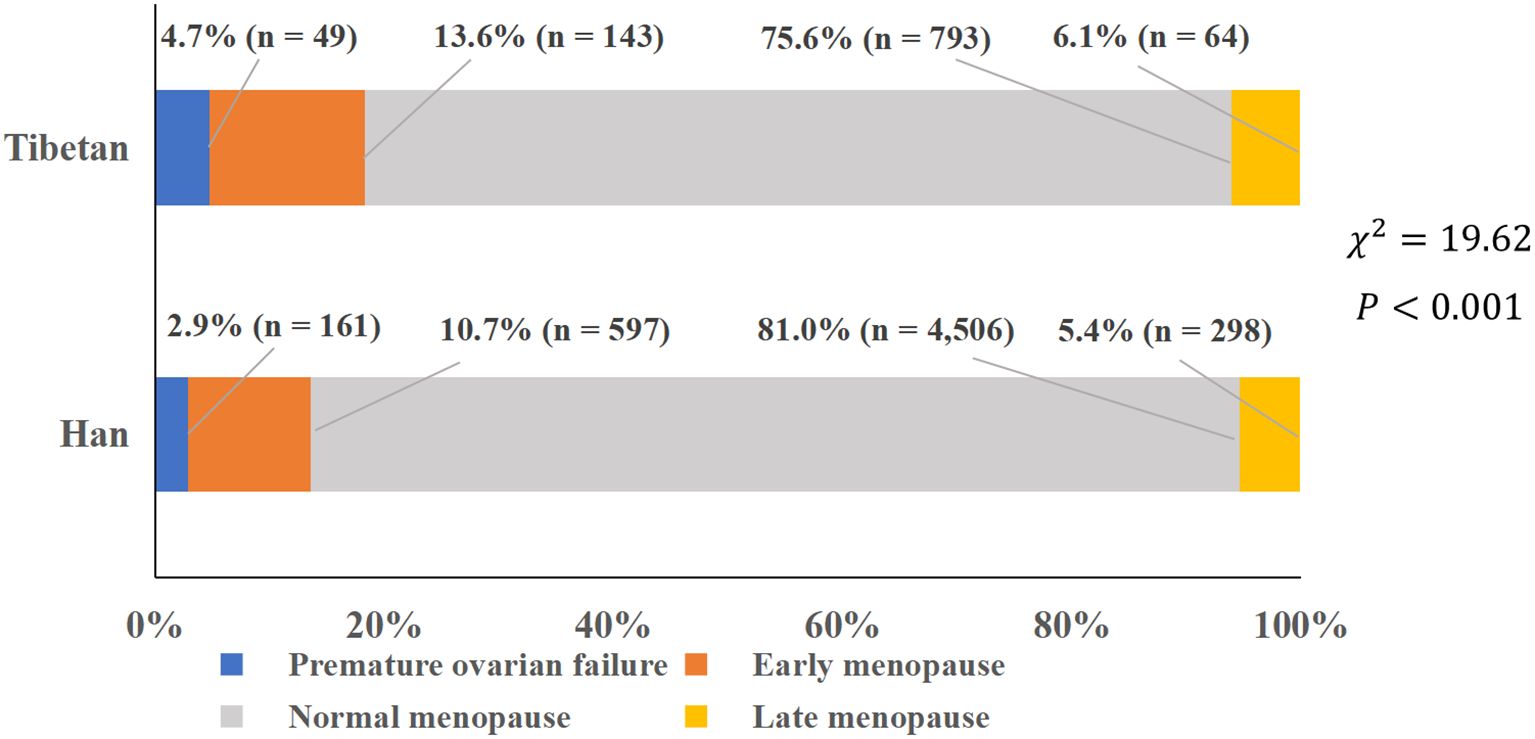
Figure 2. Proportion of various types of menopause. Proportions of premature ovarian failure, early menopause, normal menopause, and late menopause.
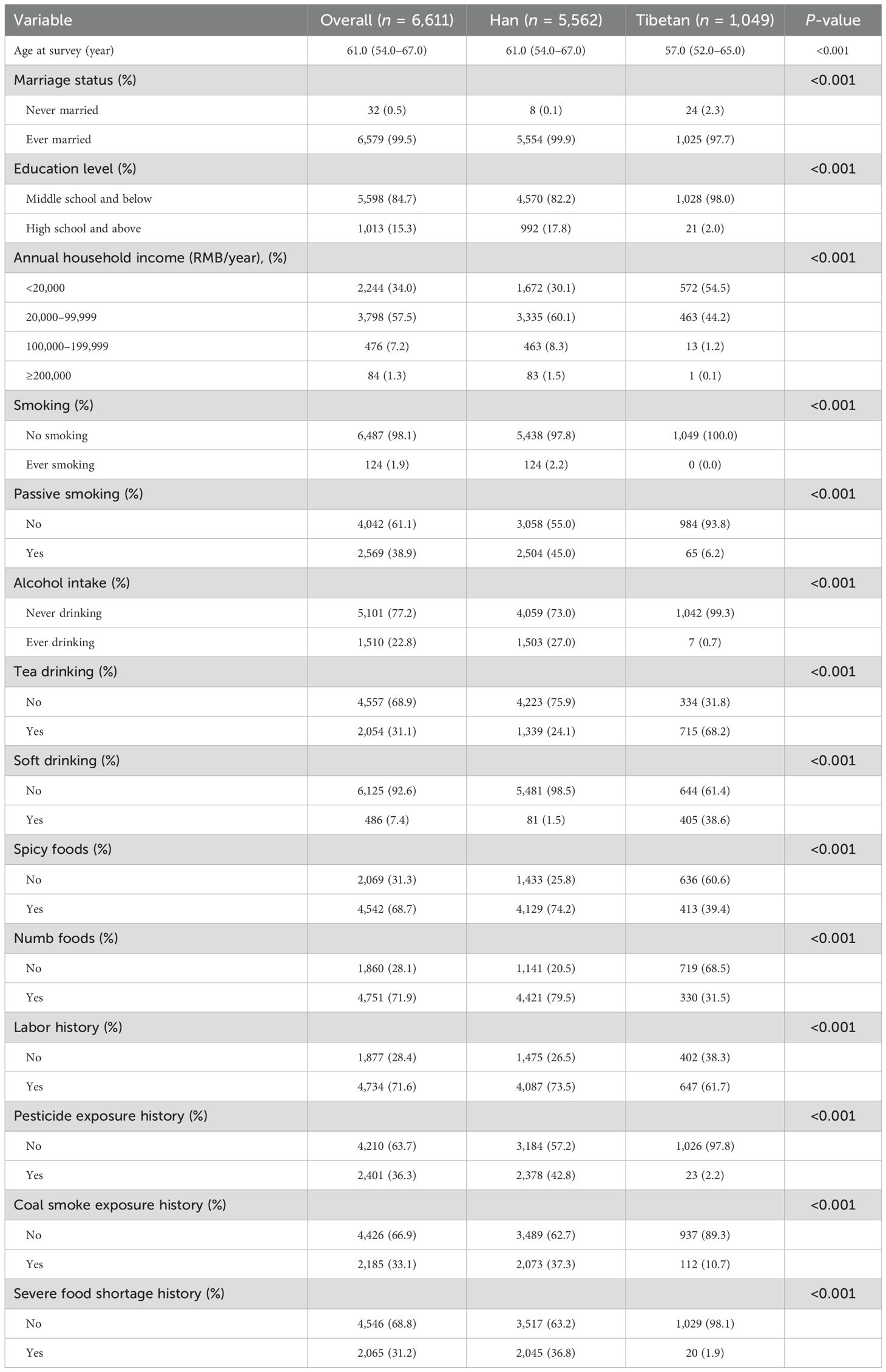
Basal characteristics of the Han and Tibetan postmenopausal women
The range of survey age was 37–79 years old for both Han and Tibetan postmenopausal women. In Han postmenopausal women, the age at survey, proportion of ever married, educational level, annual household income, smoking, passive smoking, alcohol intake, spicy foods, numb foods, history of labor, pesticide exposure, coal smoke exposure, and severe food shortage were significantly higher, whereas the proportion of tea drinking and soft drink consumption was significantly lower than those in Tibetan postmenopausal women (P < 0.001) (Table 2).
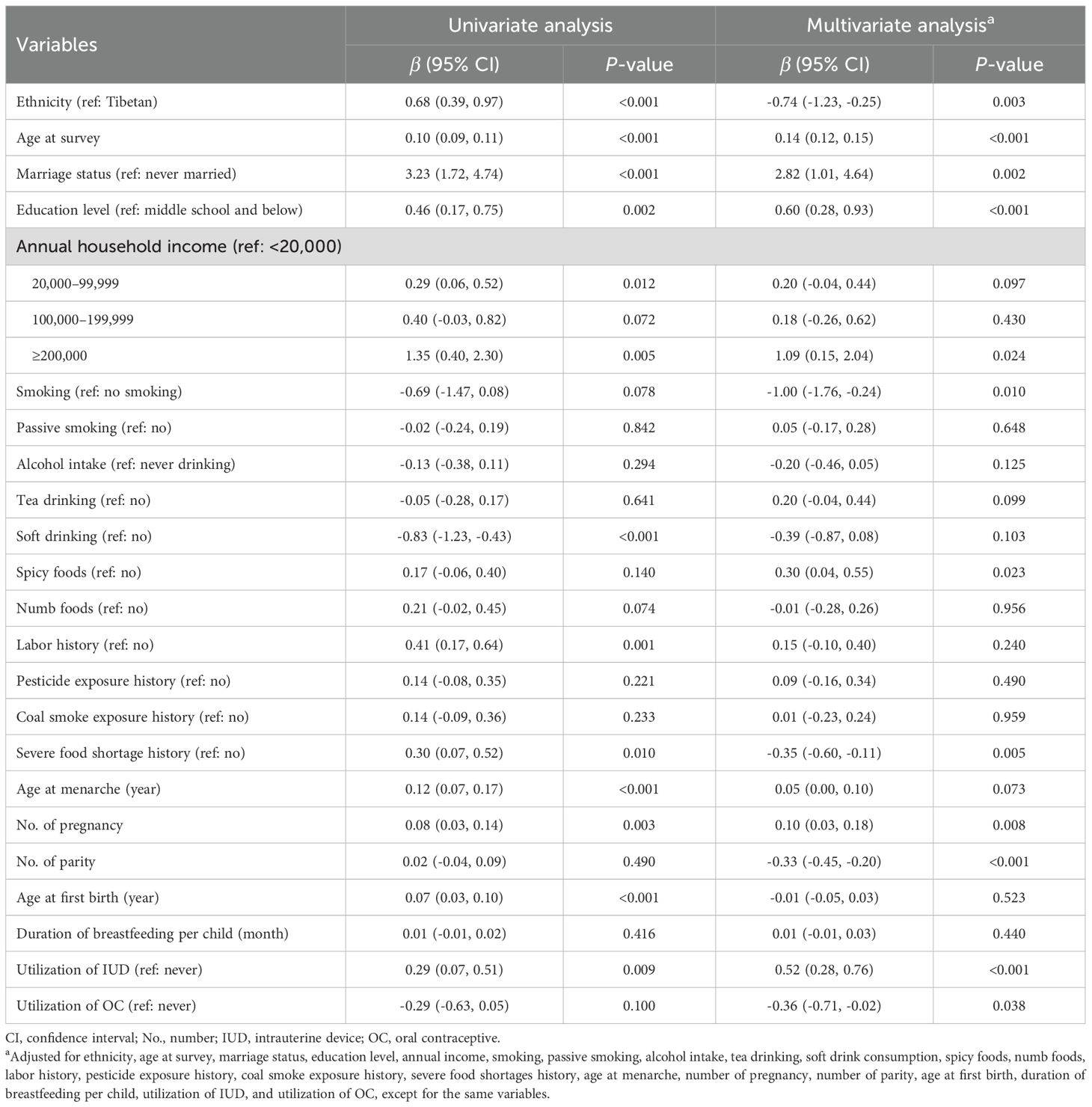
Linear regression analysis of the ANM
After adjusting the confounders, multiple linear regression analysis showed that the mean ANM of Han postmenopausal women was 0.74 year younger than Tibetan postmenopausal women (P = 0.003). Older at survey, ever married, high school and above education level, annual household income of ≥200,000 RMB, no smoking, habit of eating spicy food, never experienced severe food shortage, more gravidity, less parity, utilization of IUD, and never used OC were associated with later ANM (P < 0.05) (Table 3). The sensitivity analysis restricted to women whose age at survey was ≤75 years (n = 6,353) yielded consistent findings with the primary analysis, with no substantial changes in the effect size or significance of the association between ethnicity and the ANM (adjusted β = -0.67, 95% CI: -1.17 to -0.16, P = 0.009, Supplementary Table S2).
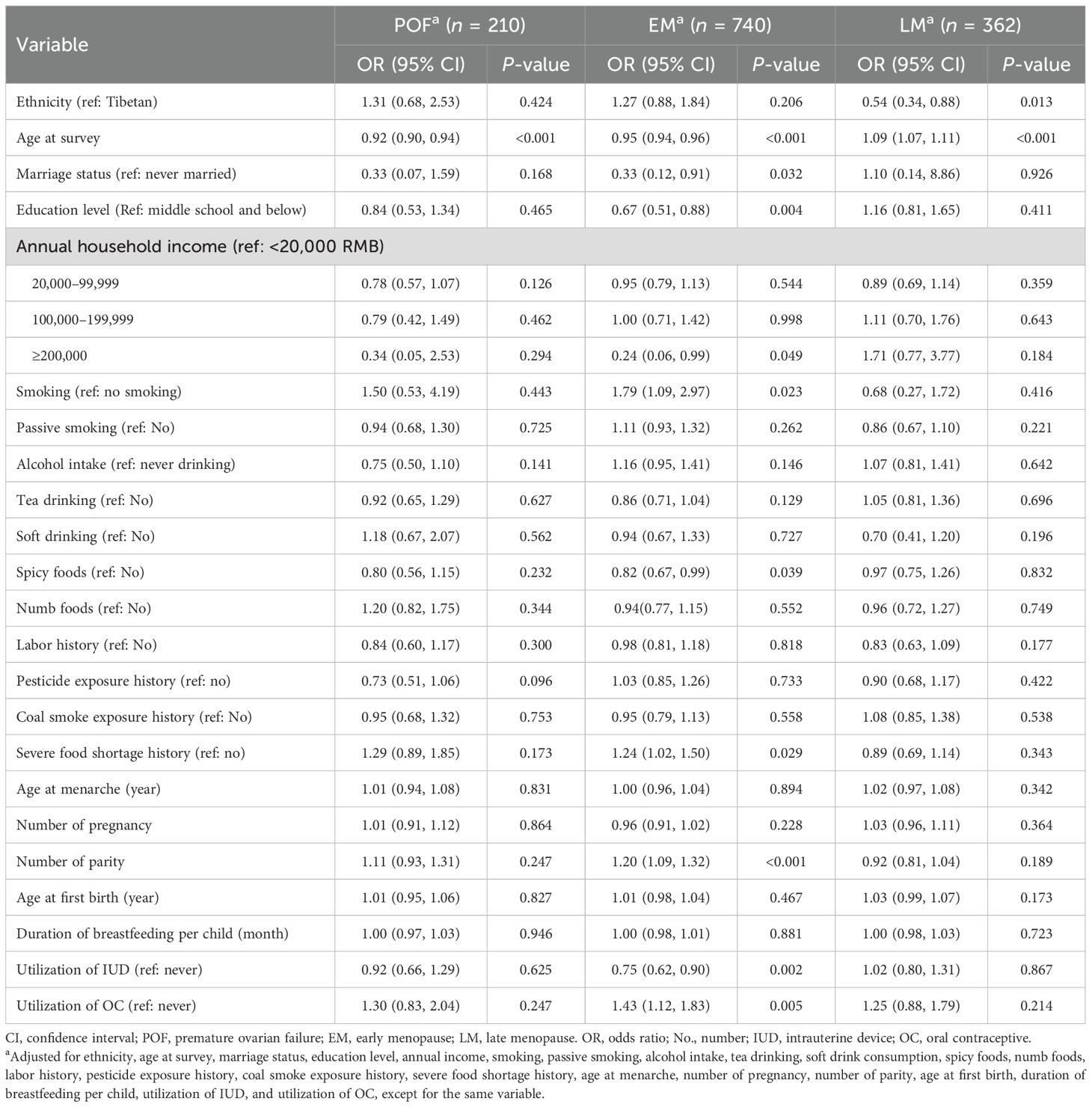
Multinomial logistic regression of the menopausal types
After adjusting for confounders, older women at survey were less likely to experience POF (OR = 0.92, 95% CI: 0.90–0.94) and EM (OR = 0.95, 95% CI: 0.94–0.96). Additionally, ever married (OR = 0.33, 95% CI: 0.12–0.91), high school and above education level (OR = 0.67, 95% CI: 0.51–0.88), annual household income ≥200,000 RMB (OR = 0.24, 95% CI: 0.06–0.99), habit of eating spicy foods (OR = 0.82, 95% CI: 0.67–0.99), and utilization of IUD (OR = 0.75, 95% CI: 0.62–0.90) were protective factors for EM. By contrast, smoking habit (OR = 1.79, 95% CI: 1.09–2.97), history of severe food shortage (OR = 1.24, 95% CI: 1.02–1.50), more parity (OR = 1.20, 95% CI: 1.09–1.32), and utilization of OC (OR = 1.43, 95% CI: 1.12–1.83) are risk factors for EM. Compared with Tibetan postmenopausal women, Han postmenopausal women were less likely to experience LM (OR = 0.54, 95% CI: 0.34–0.88). Older women at survey were more likely to experience LM (OR = 1.09, 95% CI: 1.07–1.11) (Table 4). The sensitivity analysis restricted to women whose age at survey was ≤75 years was consistent with the primary analysis (Supplementary Table S3).
Discussion
In this study, an analysis of a large size of samples has suggested that the ANM of Chinese Han postmenopausal women was earlier compared with Tibetan postmenopausal women and they were less likely to suffer LM. Older at survey, ever married, high school and above education level, annual household income ≥200,000 RMB, no smoking, habit of eating spicy foods, never experienced severe food shortage, more gravidity, less parity, utilization of IUD, and never used OC were associated with later ANM.
Whether ANM is a disparity among different ethnic groups is still controversial. Some studies indicated race/ethnicity to be a significant independent predictor for ANM (2, 3, 9, 10). A study involving five racial/ethnic groups has found that, compared with non-Latina Whites, natural menopause have occurred earlier among Latinas and later among Japanese Americans (10). A meta-analysis has indicated that the ANM has varied from 44.6 to 54.5 years across different races, with earlier menopause in women from African, Middle Eastern, some Latin American, and Asian countries and later menopause in women from Europe, Australia, Canada, and USA (3), while others have reported no racial diversity in the ANM after the confounders were controlled, including socioeconomic, lifestyle, and health conditions (11, 12).
We found more gravidity, fewer parity, and never used OC to be associated with later ANM. On the other hand, more parity and use of OC may increase the risk for EM. During gravidity, prevention of ovulation and slow depletion of the ovarian reserve may account for later menopause (22, 23). However, more parity has been associated with earlier ANM and EM in our study, which differed from other reports (10, 21–23). In our study, parity referred to the number of live birth, while for other studies this was the number of children (21) and pregnancies lasting ≥ 6 months (23). Postpartum hemorrhage and Sheehan syndrome are the risks after delivery (24, 25), which then reduced the ovarian reserve. Therefore, we propose this to be the reason for more parity and earlier ANM in our study. The relationship between OC and ANM seems to be controversial. One study has suggested that OC could delay the menopause and prolong the reproductive span (26), while (27) have found that ANM was not affected by OC after adjusting the confounders (28). They have reported that OC was associated with earlier ANM, which was consistent with our study. OC has been used not only for contraception but also in treating menstrual disorders (29). The decreased ovarian reserve in some of these patients might account for their earlier ANM. In keeping with our finding, a Dutch study has found that high-dose OC could advance the onset of menopause (28).
Our study has also found that lower educational level and income may also contribute to earlier menopause, which is in keeping with previously reported data (9, 15, 22). Low socioeconomic status (SES) has been associated with an elevated risk of unhealthy behaviors (such as early initiation of smoking, high-energy food, and low physical activity), while high socioeconomic status was associated with healthy diet (such as suitable consumption of fruits, vegetables, and dairy products, regular breakfast) and active lifestyle (such as appropriate physical exercise) (30). As a result, living and eating habits are related with the ANM. In keeping with others’ reports (10, 31), we found smoking habit to be associated with earlier ANM and EM. The components of smoke may cause demise of oocytes by reactive oxygen species (ROS) and activating pro-apoptotic proteins [Bcl-2 and Bcl-2-associated X protein (BAX) proteins] (32, 33). Interestingly, we found that the habit of eating spicy foods could delay ANM by approximately 3.6 months, and the reason might be the antioxidant, anti-inflammatory, and immunomodulatory effects of chili pepper (34, 35). Furthermore, women who had experienced severe food shortage are more likely to experience EM, which was in keeping with previous reports (36, 37).
In this study, we found that older at survey was associated with later ANM, less POF and EM, and more LM. Other studies also reported that the long-term trend of ANM may be non-linear (38). In China, the policy of family planning, educational level, economic status, and food supply have differed between different generations (39)—for instance, the great famine during 1959–1961 (40). Since the reform in 1978, economy has progressed remarkably in China (41), which may have induced the connection between ANM and the age at survey.
After adjusting for the abovementioned confounders, the ANM of Han women was 0.74 year earlier than that of Tibetan women. The discrepancy may be attributed to the genetic background of the two ethnic groups. A number of genes have been associated with the ANM, with the range of effect ranging from 3.5 to 74 weeks (42). Ethnic heterogeneity of genes, such as FRMD5 and GPRC5B, has been associated with the ANM among Asian and African women but not in Hispanic and Latino (Fernández-Rhodes et al., 2018). Another study has revealed differences in allelic frequencies of eight genes associated with the ANM, including 10q24.1/CCNJ, 3q21.3/H1FX, 4p11/ZAR1, 8p21.2/GNRH1, 18q21.33/ZCCHC2, 8q24.11/RAD21, 4q23/EIF4E, and 14q24.2/DCAF4 between Japanese and European populations (43).
It should be acknowledged that many studies investigating ANM determinants have included BMI as a potential confounding factor in their regression models (3, 12). However, given the time-dependent variable of BMI which may fluctuate substantially over decades, to use postmenopausal BMI measurements (collected years or even decades after menopause) as an approximation for premenopausal BMI could introduce a significant measurement error (10). Furthermore, many studies examining the association between ANM and BMI have reported no significant correlation between them (3). For these methodological and evidence-based considerations, we have prudently chosen not to include BMI as a covariate in our analysis.
Several limitations of this study should be acknowledged. First, the retrospective assessment of ANM may be subject to recall bias, particularly among older participants. Although our sensitivity analysis excluding women aged >75 years yielded consistent results, residual misclassification cannot be completely ruled out. Second, while we adjusted for numerous covariates, unmeasured confounding factors such as genetic predisposition and detailed hormonal profiles may influence the observed ethnic differences. Third, due to the cross-sectional nature of design, causal relationships between identified factors and ANM cannot be established. Prospective studies with accurate ANM and more information on confounders should be carried out to uncover the relationship between the ANM and ethnicity.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Sichuan University Medical Ethical Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SC: Formal analysis, Methodology, Software, Validation, Writing – original draft. LY: Conceptualization, Visualization, Writing – original draft. FC: Data curation, Investigation, Writing – review & editing. YQ: Data curation, Investigation, Writing – review & editing. JZ: Writing – review & editing. JL: Writing – review & editing. QL: Conceptualization, Data curation, Investigation, Project administration, Resources, Writing – review & editing. YG: Conceptualization, Funding acquisition, Project administration, Resources, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Key Research and Development Program of China (2017YFC0907304), Science and Technology Innovation Program of Sichuan Maternal and Child Health Care Association (22FXZD01), Scientific Research Program of Sichuan Medical Association (S22015), Scientific Research Program of Chengdu Municipal Health Commission (2022155), National Center for Women and Children’s Health, China CDC “Maternal and Infants Nutrition and Health Research Programs” (2023FYH012), and Natural Science Foundation of Sichuan Province (2024NSFSC0695).
Acknowledgments
We thank all of the participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1584267/full#supplementary-material
References
1. World Health Organization. Research on the menopause in the 1990s: Report of a WHO scientific group. (Geneva: World Health Organization) (1996).
2. Daan NM and Fauser BC. Menopause prediction and potential implications. Maturitas. (2015) 82:257–65. doi: 10.1016/j.maturitas.2015.07.019
3. Schoenaker DA, Jackson CA, Rowlands JV, and Mishra GD. Socioeconomic position, lifestyle factors and age at natural menopause: A systematic review and meta-analyses of studies across six continents. Int J Epidemiol. (2014) 43:1542–62. doi: 10.1093/ije/dyu094
4. Zhu D, Chung H-F, Dobson AJ, Pandeya N, Giles GG, Bruinsma F, et al. Age at natural menopause and risk of incident cardiovascular disease: A pooled analysis of individual patient data. Lancet Public Health. (2019) 4:e553–e64. doi: 10.1016/S2468-2667(19)30155-0
5. Bae LG, Eun NG, Wonsock K, Byoungduck H, Hwan CK, Mee KS, et al. Association between premature menopause and cardiovascular diseases and all-cause mortality in Korean women. J Am Heart Assoc. (2023) 12:e030117. doi: 10.1161/JAHA.123.030117
6. Jones AR, Enticott J, Ebeling PR, Mishra GD, Teede HT, and Vincent AJ. Bone health in women with premature ovarian insufficiency/early menopause: A 23-year longitudinal analysis. Hum Reprod. (2024) 39:1013–22. doi: 10.1093/humrep/deae037
7. Ryoko K, Motoki I, Krull AS, Rashedul IM, Shafiur RM, Eiko S, et al. Reproductive factors and endometrial cancer risk among women. JAMA Netw Open. (2023) 6:e2332296. doi: 10.1001/jamanetworkopen.2023.32296
8. Das A and Destouni A. Novel insights into reproductive ageing and menopause from genomics. Hum Reprod. (2022) 38:195–203. doi: 10.1093/humrep/deac256
9. Team IS. Variations in reproductive events across life: A pooled analysis of data from 505–147 women across 10 countries. Hum Reprod. (2019) 34:881–93. doi: 10.1093/humrep/dez015
10. Henderson KD, Bernstein L, Henderson B, Kolonel L, and Pike MC. Predictors of the timing of natural menopause in the Multiethnic Cohort Study. Am J Epidemiol. (2008) 167:1287–94. doi: 10.1093/aje/kwn046
11. Gold EB, Crawfold SL, Avis NE, Crandall CJ, Mattews KA, Waetjen LE, et al. Factors related to age at natural menopause: Longitudinal analyses from SWAN. Am J Epidemiol. (2013) 178:70–83. doi: 10.1093/aje/kws421
12. Sievert LL, Huicochea-Gómez L, Cahuich-Campos D, Whitcomb BW, and Brown DE. Age at menopause among rural and urban women in the state of Campeche, Mexico. Menopause. (2021) 28:1358–68. doi: 10.1097/GME.0000000000001886
13. Song L, Shen L, Li H, Liu B, Zheng X, Zhang L, et al. Age at natural menopause and hypertension among middle-aged and older Chinese women. J Hypertens. (2018) 36:594–600. doi: 10.1097/HJH.0000000000001585
14. Wang M, Gan W, Kartsonaki C, Guo Y, Lv J, Chen Z, et al. Menopausal status, age at natural menopause and risk of diabetes in China: a 10-year prospective study of 300,000 women. Nutr Metab. (2022) 19:7. doi: 10.1186/s12986-022-00643-x
15. Li L, Wu J, Pu D, Zhao Y, Wan C, Sun L, et al. Factors associated with the age of natural menopause and menopausal symptoms in Chinese women. Maturitas. (2012) 73:354–60. doi: 10.1016/j.maturitas.2012.09.008
16. Xu Q, Ren S, Er Xiding AS, Xu L, Guo L, Zha Y, et al. Menopause age and influencing factors among Uyghur and Han women in Urumqi City. Chin J Prev Med. (1995) 29:322.
17. Wan L, Gu W, Zhao M, Liu F, and Liu J. Relationship between age of menopause and fertility, disease and life expectancy in elderly women. Chin J Popul Sci. (2002) 2:70–4.
18. Zeng L and Zhou X. Analysis of the affecting natural menopausal age of Han and Miao nationalities in Guiyang. Chin Health Stand Manage. (2016) 7:4–6. doi: 10.3969/j.issn.1674-9316.2016.09.003
19. Li S, Li Y, Wang W, Jiao J, Degen AA, Zhang T, et al. Dietary habits of pastoralists on the Tibetan plateau are influenced by remoteness and economic status. Food Res Int. (2023) 174:113627. doi: 10.1016/j.foodres.2023.113627
20. Zhao X, Hong F, Yin J, Tang W, Zhang G, Liang X, et al. Cohort profile: the China Multi-Ethnic cohort (CMEC) study. Int J Epidemiol. (2021) 50:721–721l. doi: 10.1093/ije/dyaa185
21. Mishra GD, Pandeya N, Dobson AJ, Chung H-F, Anderson D, Kuh D, et al. Early menarche, nulliparity and the risk for premature and early natural menopause. Hum Reprod. (2017) 32:679–86. doi: 10.1093/humrep/dew350
22. Wang M, Gong W-W, Hu R-Y, Wang H, Guo Y, Bian Z, et al. Age at natural menopause and associated factors in adult women: findings from the China Kadoorie Biobank study in Zhejiang rural area. PLoS One. (2018) 13:e0195658. doi: 10.1371/journal.pone.0195658
23. Langton CR, Whitcomb BW, Purdue-Smithe AC, Sievert LL, Hankinson SE, Manson JE, et al. Association of parity and breastfeeding with risk of early natural menopause. JAMA Netw Open. (2020) 3:e1919615. doi: 10.1001/jamanetworkopen.2019.19615
24. Patek K and Friedman P. Postpartum hemorrhage - Epidemiology, risk factors, and causes. Clin Obstet Gynecol. (2023) 66:344–56. doi: 10.1097/GRF.0000000000000782
25. Diri H, Karaca Z, Tanriverdi F, Unluhizarci K, and Kelestimur F. Sheehan’s syndrome: New insights into an old disease. Endocrine. (2016) 51:22–31. doi: 10.1007/s12020-015-0726-3
26. Roman Lay AA, do Nascimento CF, Horta BL, and Dias Porto Chiavegatto Filho A. Reproductive factors and age at natural menopause: A systematic review and meta-analysis. Maturitas. (2020) 131:57–64. doi: 10.1016/j.maturitas.2019.10.012
27. Langton CR, Whitcomb BW, Purdue-Smithe AC, Sievert LL, Hankinson SE, Manson JE, et al. Association of oral contraceptives and tubal ligation with risk of early natural menopause. Hum Reprod. (2021) 36:1989–98. doi: 10.1093/humrep/deab054
28. de Vries E, den Tonkelaar I, van Noord PA, van der Schouw YT, te Velde ER, and Peeters PH. Oral contraceptive use in relation to age at menopause in the DOM cohort. Hum Reprod. (2001) 16:1657–62. doi: 10.1093/humrep/16.8.1657
29. Gynecologic Endocrinology Subgroup CSoOaG, Chinese Medical Association. Guideline on diagnosis and treatment of abnormal uterine bleeding: 2022 revisions. Chin J Obstet Gynecol. (2022) 57:481–90. doi: 10.3760/cma.j.cn112141-20220421-00258
30. Gautam N, Dessie G, Rahman MM, and Khanam R. Socioeconomic status and health behavior in children and adolescents: A systematic literature review. Front Public Health. (2023) 11:1228632. doi: 10.3389/fpubh.2023.1228632
31. Ruth KS, Perry JR, Henley WE, Melzer D, Weedon MN, and Murray A. Events in early life are associated with female reproductive ageing: A UK biobank study. Sci Rep. (2016) 6:24710. doi: 10.1038/srep24710
32. Cheng SF, Qin XS, Han ZL, Sun XF, Feng YN, Yang F, et al. Nicotine exposure impairs germ cell development in human fetal ovaries cultured in vitro. Aging (Albany NY). (2018) 10:1556–74. doi: 10.18632/aging.101492
33. Matikainen T, Perez GI, Jurisicova A, Pru JK, Schlezinger JJ, Ryu H-Y, et al. Aromatic hydrocarbon receptor-driven Bax gene expression is required for premature ovarian failure caused by biohazardous environmental chemicals. Nat Genet. (2001) 28:355–60. doi: 10.1038/ng575
34. Azlan A, Sultana S, Huei CS, and Razman MR. Antioxidant, anti-obesity, nutritional and other beneficial effects of different chili pepper: A review. Molecules. (2022) 27:898. doi: 10.3390/molecules27030898
35. Chen L, Ding R, Luo Q, Tang X, Ding X, Yang X, et al. Association between spicy food and hypertension among Han Chinese aged 30–79 years in Sichuan Basin: a population-based cross-sectional study. BMC Public Health. (2023) 23:1663. doi: 10.1186/s12889-023-16588-6
36. Yarde F, Broekmans FJ, van der Pal-de Bruin KM, Schönbeck Y, te Velde ER, Stein AD, et al. Prenatal famine, birthweight, reproductive performance and age at menopause: the Dutch hunger winter families study. Hum Reprod. (2013) 28:3328–36. doi: 10.1093/humrep/det331
37. Wang N, Huang Y, Wen J, Su Q, Huang Y, Cai L, et al. Early life exposure to famine and reproductive aging among Chinese women. Menopause. (2019) 26:463–8. doi: 10.1097/GME.0000000000001259
38. Gottschalk MS, Eskild A, Hofvind S, Gran JM, and Bjelland EK. Temporal trends in age at menarche and age at menopause: A population study of 312 656 women in Norway. Hum Reprod. (2020) 35:464–71. doi: 10.1093/humrep/dez288
39. Wang Y, Fan H, and Guo C. Trend and factors of population fertility changes from the perspective of economics and education - China, 1949-2020. China CDC Wkly. (2021) 3:599–603. doi: 10.46234/ccdcw2021.159
40. Kim S, Fleisher B, and Sun JY. The long-term health effects of fetal malnutrition: Evidence from the 1959–1961 China Great Leap Forward Famine. Health Econ. (2017) 26:1264–77. doi: 10.1002/hec.3397
41. Lu Y, Zhang Y, Cao X, Wang C, Wang Y, Zhang M, et al. Forty years of reform and opening up: China’s progress toward a sustainable path. Sci Adv. (2019) 5:eaau9413. doi: 10.1126/sciadv.aau9413
42. Ruth KS, Day FR, Hussain J, Martínez-Marchal A, Aiken CE, Azad A, et al. Genetic insights into biological mechanisms governing human ovarian ageing. Nature. (2021) 596:393–7. doi: 10.1038/s41586-021-03779-7
Keywords: ethnicity, Chinese Han, Chinese Tibetan, postmenopausal, age at natural menopause
Citation: Chen S, Yang L, Chen F, Qiu Y, Zhang J, Li Ling J, Liu Q and Gong Y (2025) The age at natural menopause of Chinese Han and Tibetan women. Front. Endocrinol. 16:1584267. doi: 10.3389/fendo.2025.1584267
Received: 27 February 2025; Accepted: 10 July 2025;
Published: 01 August 2025.
Edited by:
Sonam Verma, Washington University in St. Louis, United StatesReviewed by:
Sylvia Kirchengast, University of Vienna, AustriaGautam Anand, Washington University in St. Louis, United States
Victor Manuel Vargas-Hernandez, Academia Mexicana de Cirugia, Academia Nacional de Medicina de Mexico, Mexico
Copyright © 2025 Chen, Yang, Chen, Qiu, Zhang, Li Ling, Liu and Gong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Gong, Z29uZ3lhbjA2MTlAMTYzLmNvbQ==; Qiaolan Liu, bGl1cWlhb2xAc2N1LmVkdS5jbg==
†These authors have contributed equally to this work
 Shiqi Chen
Shiqi Chen Liangbo Yang
Liangbo Yang Furui Chen3,4
Furui Chen3,4 Jing Zhang
Jing Zhang Qiaolan Liu
Qiaolan Liu Yan Gong
Yan Gong