- 1Drug Development, EpicentRx, Torrey Pines, CA, United States
- 2Department of Translational Neuroscience, University of Queensland Centre for Clinical Research, Brisbane, QLD, Australia
- 3Department of Bioengineering, University of California at San Diego, La Jolla, CA, United States
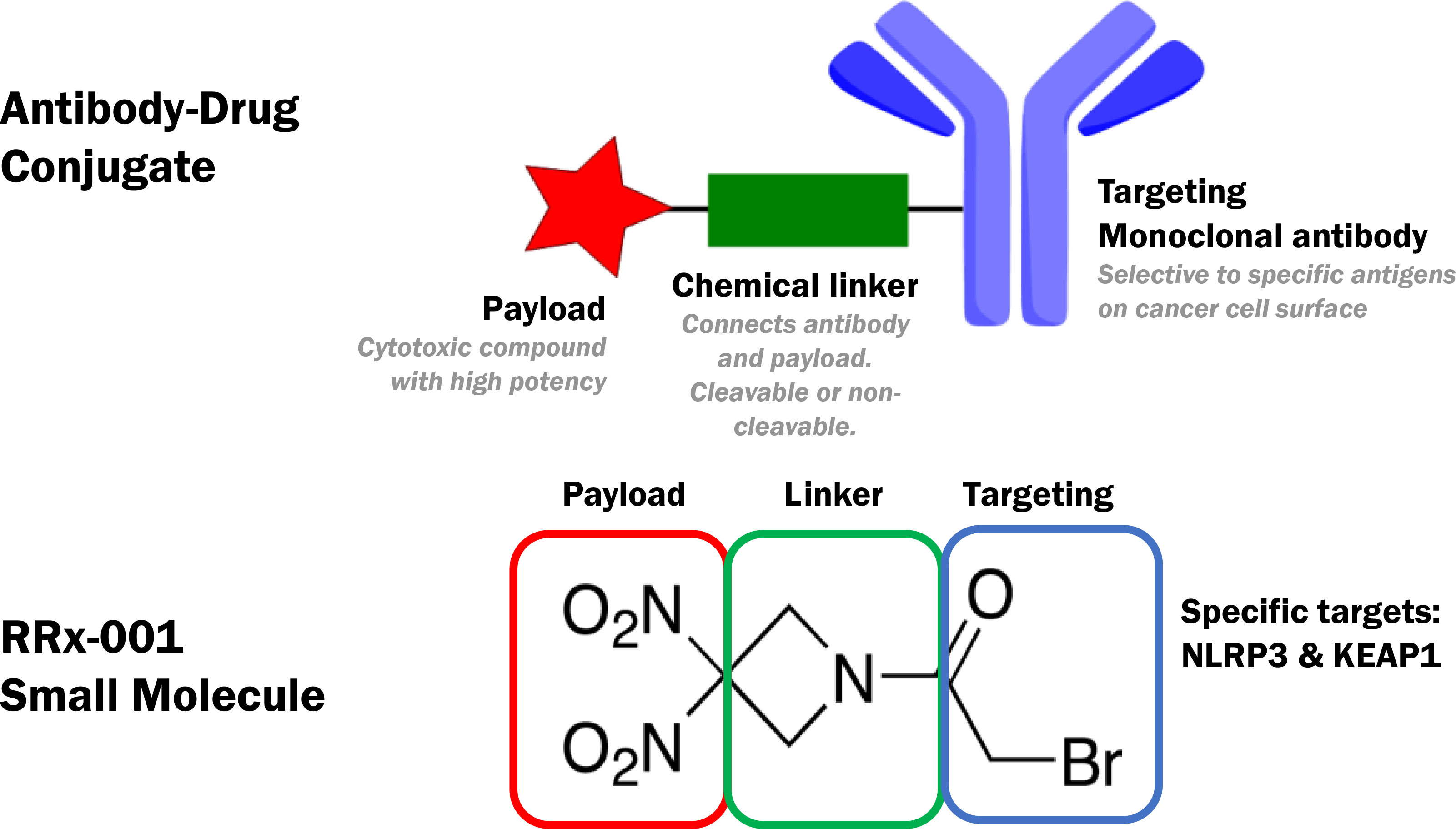
RRx-001 is a shape shifting small molecule with Fast Track designation for the prevention/amelioration of chemoradiation-induced severe oral mucositis (SOM) in newly diagnosed Head and Neck cancer. It has been intentionally developed or “engineered” as a chimeric single molecular entity that targets multiple redox-based mechanisms. Like an antibody drug conjugate (ADC), RRx-001 contains, at one end a “targeting” moiety, which binds to the NLRP3 inflammasome and inhibits it as well as Kelch-like ECH-associated protein 1 (KEAP1), the negative regulator of Nrf2, and, at the other end, a conformationally constrained, dinitro containing 4 membered ring, which fragments under conditions of hypoxia and reduction to release therapeutically active metabolites i.e., the payload. This “payload”, which is delivered specifically to hypoperfused and inflamed areas, includes nitric oxide, nitric oxide related species and carbon-centered radicals. As observed with ADCs, RRx-001 contains a backbone amide “linker” attached to a binding site, which correlates with the Fab region of an antibody, and to the dinitroazetidine payload, which is microenvironmentally activated. However, unlike ADCs, whose large size impacts their pharmacokinetic properties, RRx-001 is a nonpolar small molecule that easily crosses cell membranes and the blood brain barrier (BBB) and distributes systemically. This short review is organized around the de novo design and in vivo pro-oxidant/pro-inflammatory and antioxidant/anti-inflammatory activity of RRx-001, which, in turn, depends on the reduced to oxidized glutathione ratio and the oxygenation status of tissues.
1 Introduction
This short review covers the de novo design of the chimeric or hybrid therapy, RRx-001, also referred to by its chemical acronym, ABDNAZ, for alpha bromodinitroazetidine, and its United States Adopted Names (USAN) generic, non-proprietary, first-in-class name, nibrozetone.
Increasingly, it has become clear that many disorders especially progressive ones like several types of cancer, neurodegenerative diseases, congestive heart failure, diabetes, and kidney disease are too complex and too multifactorial to be successfully treated by a single medication or therapy (1). This provides support for polypharmacology of which perhaps the most successful example is the triple therapy cocktail for human immunodeficiency virus (HIV). However, combination therapies are potentially subject to drug-drug interactions, additive toxicities, and the development of resistance, which limit their usefulness.
An alternative to combination of two or more therapies administered separately is multi-targeted drugs particularly those obtained through conjugation of two or more pharmacophores having specific pharmacological activities and rendered potentially more effective and less toxic than in isolation due to the avoidance of different bioavailabilities, pharmacokinetics, metabolism, and drug-drug interactions (2). Several small molecule chimeric drugs are in development; however, to best knowledge, one of the most clinically advanced is RRx-001 on which this review focuses.
RRx-001 amalgamates two pharmacophores with mixed and diametrically opposed biological functions: the targeting moiety is (mostly) anti-inflammatory/anti-oxidative and the payload moiety, depending on whether conditions are redox-reduced and hypoxic, is (mostly) pro-inflammatory/pro-oxidative. These two pharmacophores are an acyl bromide and a dinitroazetidine, which are conjugated through a stable i.e., non-cleavable amide linker. This design intentionally resembles that of an antibody drug conjugate (ADC), as shown below in Figure 1.
As structure dictates activity, the design of RRx-001 serves as a jumping off point to describe its paradoxical antioxidant/pro-oxidant and anti-inflammatory/proinflammatory properties in vivo.
Parenterally administered RRx-001 is currently in a Phase 3 trial with a platinum doublet (etoposide + carboplatin/cisplatin or EP) for the treatment of third line and beyond small cell lung cancer (SCLC) called REPLATINUM (3) and in a Phase 2b radioprotective trial called KEVLARx in newly diagnosed head and neck cancer. As an uncharged (albeit non-lipid soluble) small molecule, RRx-001 and its metabolites are cell membrane permeable (4) and cross the highly restrictive blood brain barrier (BBB) (5), which otherwise excludes 98% of small molecule drugs and ~100% of biologics (6, 7); this BBB permeability and encouraging evidence of clinical activity against brain metastases (5) and glioma (8, 9) prompted the preclinical assessment of RRx-001 in various neurodegenerative diseases, including Alzheimer’s, Parkinson’s, and ALS/MND where it has, to date, demonstrated genuine disease modifying potential (10).
It may seem counterintuitive that RRx-001, as a prooxidant, which reverses resistance to chemotherapy protects against the progression of neurodegenerative diseases in preclinical models since already elevated levels of inflammation and reactive oxygen and nitrogen species (RONS) are thought to underlie them. However, a common misconception is that RONS are universally harmful and that so-called “antioxidants” must scavenge them to be effective. In fact, like RRx-001, most antioxidants are either prooxidants that generate reactive species and/or electrophiles, which form covalent adducts with proteins. This is the case, for example, with physical exercise and several phytochemicals including curcumin from turmeric, diallyl sulfide from garlic, resveratrol from grapes, epicatechin from cocoa or green tea and sulforaphane from cruciferous vegetables like broccoli, cauliflower, and kale (11), all of which generate a mild oxidative stress that, in turn, upregulates endogenous antioxidant defense systems, such as reduced glutathione (12). This is also the case with dimethyl fumarate (DMF), an electrophilic compound, which has been approved for the treatment of relapsing multiple sclerosis in the United States and Europe, and which is under investigation in cancer and other neurodegenerative diseases like Alzheimer’s, and Parkinson’s (13). Like RRx-001, DMF induces an initial oxidative burst through alkylation of thiols and depletion of glutathione (GSH) that activates Nrf2 and ultimately increases GSH levels (14).
Structure activity relationships have demonstrated that analogs of RRx-001, which do not contain the inflammatory payload are minimally active.
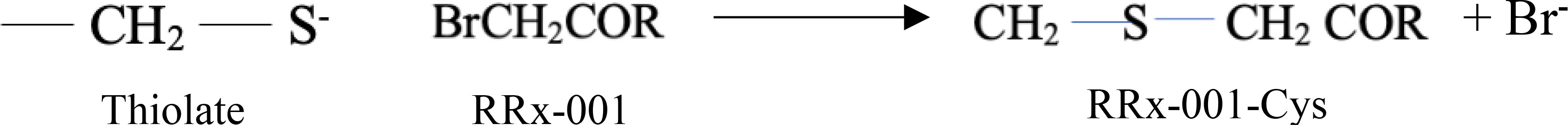
The α-bromoacetamide moiety of RRx-001 selectively and rapidly alkylates/derivatizes available thiolate anions (R-S-) through nucleophilic substitution (SN2) which displaces the leaving group, bromide (15), as shown in Figure 2. A thiolate is much more nucleophilic and reactive than a neutral thiol (16). The stability of the thiolate residues to which RRx-001 preferentially binds depends on the presence and proximity of cationic amino acids or specific hydrogen bonds that depress their pKa value and, hence, increase reactivity (4).
Depending on the cysteine thiolate residues that it alkylates, RRx-001 irreversibly inhibits the function of proteins. Because RRx-001 binds covalently, its half-life is effectively equivalent to the resynthesis half-life of the bound protein, which impacts the dosing frequency. Accordingly, RRx-001 is administered on a weekly or monthly basis, depending on the disease indication. The fact that RRx-001 only reacts with a few select thiolates (17) based on metabolism and disposition studies (18) probably accounts for the absence of dose limiting toxicities, and drug-related serious adverse events (SAEs) in over 350 patients treated with it to date. Also, a maximal tolerated dose (MTD) has never been reached (19). The main adverse event associated with RRx-001 is an infusion-related superficial thrombophlebitis-like venous inflammation and pain (20), which is treated, if it is treated at all, with non-steroidal anti-inflammatory drugs. RRx-001 is administered in an ex vivo device with an aliquot of anticoagulated blood to improve patient discomfort and to prevent more serious complications and sequelae such as infection or progression to deep vein thrombosis. However, typical chemotherapy-like hematologic and non-hematologic adverse events such as nausea/vomiting, alopecia, weight loss, fatigue, stomatitis, diarrhea, and myelosuppression are never encountered with it. In addition to venous inflammation, another common side effect with RRx-001 is tumor pseudoprogression, in which decreased tumor burden follows transient tumor growth due to edema and immune infiltration (21). Pseudoprogression mimics true early progression, which is potentially problematic because it may lead to premature discontinuation from treatment with RRx-001 (22).
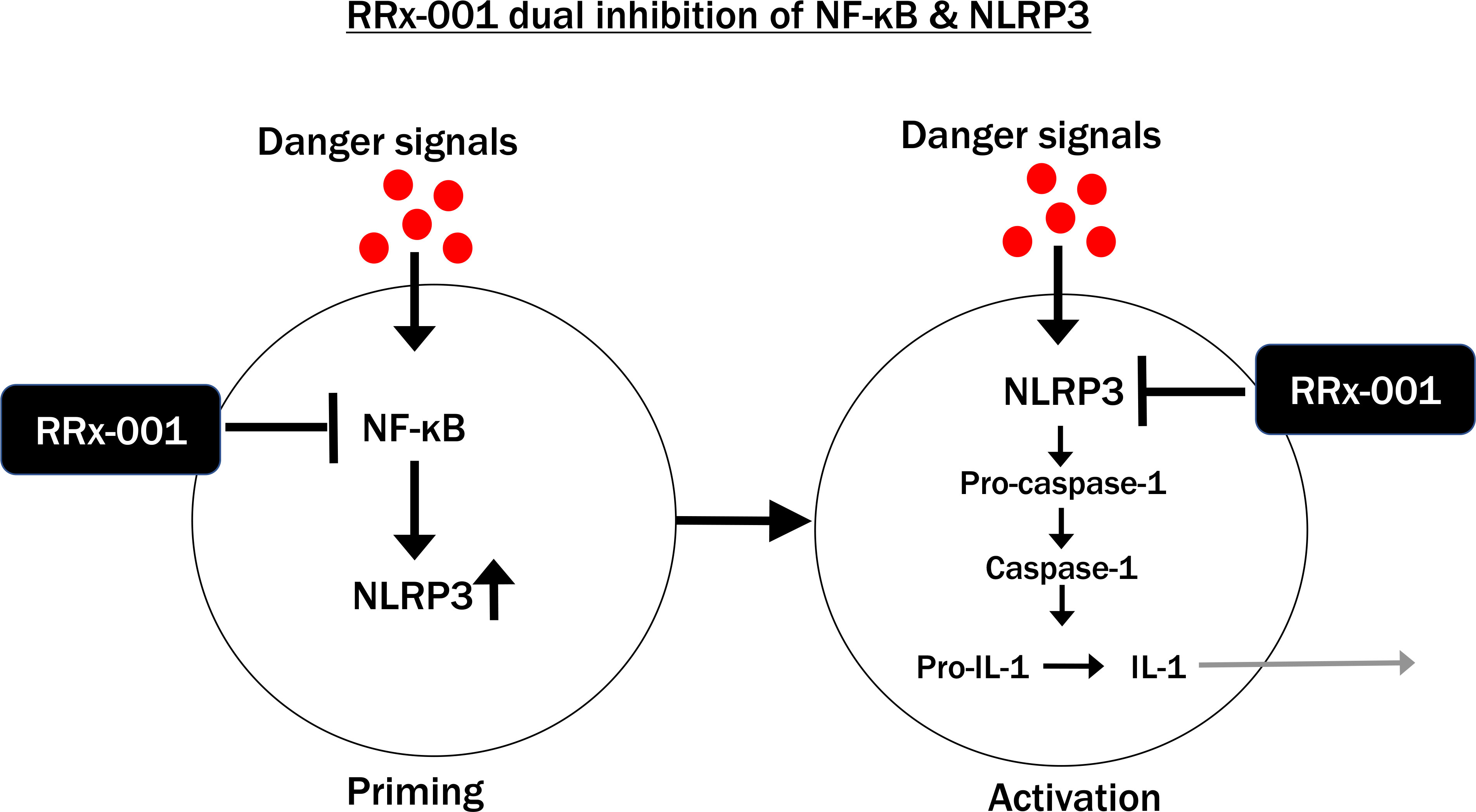
One of the most important targets of RRx-001 is the nucleotide-binding oligomerization domain, leucine-rich repeat, and pyrin domain containing 3 (NLRP3) inflammasome. RRx-001 is a double inhibitor of the NLRP3 inflammasome, firstly because it selectively binds to cysteine 409 on the central NACHT domain of NLRP3 (14, 15), which prevents its assembly and, secondly, because it inhibits nuclear factor kappa B (NF-κB) (23).
2 Targeting moiety
2.1 Double inhibition of the NLRP3 inflammasome by RRx-001
The NLRP3 inflammasome is an intracellular multiprotein complex that activates in response to harmful stimuli, such as dead cells, irritants, or pathogens. This activation mediates an inflammatory response through the production and release of IL-1β, IL-18, and gasdermin D (GSDMD).
Inflammation is the first line of defense against infection, which makes NLRP3 inflammasome activation beneficial and homeostatic, provided that the duration of the subsequent inflammatory response is short-lived i.e., days to weeks, and resolution quickly follows removal of the noxious stimulus (24). However, if the inflammatory response is inadequate or if the noxious stimulus persists, chronicity develops, which is pathologic and maladaptive, because of the overproduction of reactive oxygen species (ROS) and cytokines from ongoing inflammasome activation and immune cell infiltration (25). A malicious cycle of chronic inflammation, oxidative stress, and destruction of healthy cells and tissues ensues, which over time i.e., months to years leads to disease, end-organ damage, and even mortality.
NLRP3 inflammasome activation is canonically a two-step process involving NF-κB priming from a range of pathogen-associated molecular patterns (PAMPs) such as viral and bacterial components and damage-associated molecular patterns (DAMPs) (Step 1) and protein complex assembly (Step 2), also involving a range of PAMPs and DAMPs, which are also known as “danger signals” (26). As shown in Figure 3, RRx-001 inhibits both steps, due to its repression of TAK1, which activates NF-κB, and NLRP3 assembly. The non-canonical NLRP3 pathway involves human caspase-4 and caspase-5 from gram-negative bacterial infection (27).
Aberrant activation of the NLRP3 inflammasome is associated with the onset and progression of many diseases including metabolic syndrome, type 2 diabetes, non-alcoholic fatty liver disease, cardiovascular disease, chronic kidney disease, cancer, depression, neurodegenerative and autoimmune diseases, and endometriosis. For this reason, NLRP3 inflammasome inhibitors are used to treat a range of diseases from cancer to neurodegenerative conditions like Parkinson’s and Alzheimer’s (28).
Indeed, outside of cancer, RRx-001, the most clinically advanced of the direct NLRP3 inhibitors, including MCC950, which is no longer in development, has received FDA Fast Track status (29) as a radioprotector to prevent/ameliorate severe oral mucositis based on the results of a randomized Phase 2 clinical trial called PREVLAR (30) and is also under preclinical study in Parkinson’s Disease and amyotrophic lateral sclerosis (ALS)/motor neuron disease with grants awarded from the Michael J. Fox Foundation (MJFF) and Fight MND, respectively. The second most clinically advanced NLRP3 inflammasome inhibitor is OLT-1177 (Dapsutrile), having completed at least three Phase 2 trials in gout, osteoarthritis, and heart failure (31). On top of NF-κB and NLRP inhibition, RRx-001 directly and indirectly upregulates the master antioxidant transcription factor, nuclear factor (erythroid-derived 2)-like 2 (Nrf2), which differentiates RRx-001 from other rationally designed, unimechanistic direct NLRP3 inhibitors like selnoflast, dapsutrile, DFV890 (IFM-2427), and ZYIL1 (32). Besides NLRP3 inhibition and Nrf2 induction, other established mechanisms of action for RRx-001 including epigenetic modulation (33), tumor associated macrophage repolarization (34), and vascular normalization (6), which may play greater or lesser roles depending on the disease indication, are not discussed herein since this review was solicited specifically for a redox-based article collection.
2.2 Double upregulation of Nrf2 by RRx-001
Because RRx-001 reacts with glutathione and cysteine (preferentially in their thiolate forms), it induces oxidative stress (OS) (30). In response to OS, which damages cellular components such as proteins, DNA and lipids the constitutive inhibitor of Nrf2, Kelch-like ECH-associated protein 1 (KEAP1), physically dissociates from Nrf2, leading to the nuclear translocation of Nrf2, and transcription of a detoxifying battery of antioxidant response element (ARE) genes such as reduced glutathione (GSH), glutathione S-transferase Ya, NAD(P)H oxidoreductase (NQO1) and heme oxygenase-1 (HO-1) (35). In addition to oxidation of specific cysteine residues in KEAP1, RRx-001 is thought to form adducts with these residues, presumably leading to the ubiquitination and subsequent proteasome-dependent degradation of KEAP1.
The preclinical and clinical radio- and chemoprotective effects of RRx-001 that have been observed both preclinically and clinically are attributable not only to NLRP3 inflammasome inhibition but also to Nrf2 induction (18, 36, 37). RRx-001 is such a strong activator of Nrf2 that it significantly induces the transcription of target genes including heme oxygenase-1 (HO-1) even in the presence of N-acetyl-l-cysteine or glutathione (GSH) (37–39). This hyperactivation of Nrf2 raises the question whether RRx-001 administration has the potential to protect tumors both from chemotherapeutic agents and radiation-induced damage since Nrf2 is possibly protumorigenic. Preclinical data have established that, in fact, RRx-001 selectively kills Caco-2, A2780 (ovarian cancer), and UWB1 (BRCA1-null human ovarian cancer) cells but not CRL-1459/CCD-18Co normal fibroblast colon cells (35) and clinical data support the anticancer activity of RRx-001 both alone (19) and in combination with chemotherapy (40), immunotherapy (41), and radiation (42). Separate from all that, however, it is persistent, long-term activation of Nrf2 that seems to protect cancer cells from genotoxic chemo- and radiotherapies, and to make them refractory to treatment, not controlled, intermittent activation from a small molecule Nrf2 inducer like RRx-001 (43). Also, Nrf2 is thought to suppress carcinogenesis especially at early stages, owing to its detoxifying activity (44).
RRx-001 is only behind dimethyl fumarate (DMF, BG-12, Tecfidera®) and omaveloxolone (Skyclaris®), which are approved for the treatment of remitting-relapsing multiple sclerosis (RRMS) and psoriasis (DMF), and Friedrich’s ataxia (omaveloxolone) in terms of its clinical advancement (45). Like RRx-001, omaveloxolone is well tolerated and so is DMF except for one rare serious adverse event, progressive multifocal leukoencephalopathy (PML), an opportunistic and often fatal infection of the brain (46).
As previously stated, because of its reactivity with the thiolate forms of cysteine and glutathione, RRx-001 significantly induces oxidative stress (OS), at least initially, which is a double-edged sword, because RRx-001 may exacerbate already high baseline OS levels in older individuals and/or those with chronic diseases like cancer, heart failure, and diabetic nephropathy before the compensatory expression of Nrf2-related cytoprotective enzymes such as catalase, glutathione S-transferases, glutathione reductases, glutathione peroxidase-1 (GPx), heme oxygenase-1, superoxide dismutase (SOD), thioredoxin, and quinone oxidoreductases occurs (47).
2 Non-cleavable linker
In antibody drug conjugates (ADCs) a linker connects the targeting moiety with the payload. Linkers are classified as cleavable and non-cleavable. The amide linker in RRx-001 is stable to external enzymatic cleavage. The comparative advantage of a non-cleavable linker over a cleavable one in this case is increased plasma stability so that the dinitroazetidine payload is not prematurely released or released in normal cells.
3 Payload moiety
It is perhaps misleading to only refer to the highly strained dinitroazetidine end of RRx-001 as the “payload” given the enhanced biologic activity of the “targeting moiety” against NF-κB/NLRP3 inflammasome and KEAP1, the negative regulator of Nrf2. Nevertheless, the strain in the 4-membered dinitroazetidine and its reactivity with GSH makes it susceptible to nucleophilic ring opening and strain release transformations in vivo under ischemic/hypoxic conditions. Cleavage of C-C and C-NO2 bonds has the potential to generate carbon-centered radicals and nitric oxide (NO) or NO-related species, such as the nitrosonium ion (NO+) or the nitroxyl anion (NO-), respectively, which underlie the anticancer DNA damaging effects of RRx-001. X-ray crystal structure analysis on RRx-001 demonstrates that the azetidine ring is puckered to reduce steric and electronic repulsions, which favors ring opening to relieve strain (48).
Preclinical and clinical data have demonstrated that RRx-001 is an ‘on-demand’ nitric oxide (NO) donor and superagonist, meaning that, unlike the organic nitrates, which are commonly used in the treatment of cardiovascular disease, and other nitric oxide donors such as furoxans, benzofuroxans, NONOates, and S-nitrosothiols, NO is released from RRx-001 at high levels not systemically, but locally and only where ischemia/hypoxia is present, that is in the right time and right place (49, 50). This local release obviates the toxicities such as hypotension, methemoglobinemia, dizziness, nausea, and headache that are associated with these other nitric oxide donors. In solid tumors, where hypoxia is common, RRx-001-mediated NO donation has been shown preclinically and clinically to dilate the vasculature (51) and to augment the delivery of oxygen (52), other anticancer drugs (6), and effector cells as a result (53). Also, in tumors with high levels of oxidative stress, nitric oxide, a highly diffusible and reactive free radical, combines with superoxide to form the powerful oxidant, peroxynitrite (ONOO-) (47), which induces DNA damage; peroxynitrite is also associated with macrophage cytotoxicity since immune myeloid cells, like macrophages, produce both nitric oxide and superoxide to generate it (54). Preclinical data have demonstrated that the application of hyperthermia also increases NO production from RRx-001.
In addition, RRx-001 derivatizes deoxyhemoglobin and displaces nitric oxide from its binding site on beta cysteine 93; this adds to the local overproduction of NO since these RRx-001-derivatized red cells preferentially adhere to hypoxic/ischemic vasculature (55–57).
In addition to cancer (58), nitric oxide insufficiency/deficiency is a characteristic of several disease states (59) including pulmonary hypertension, hyperlipidemia, and non-alcoholic steatohepatitis (NASH) (60), COVID-19 (61, 62), chronic kidney disease, myocardial infarction (63), cerebral malaria and stroke (64), ischemia reperfusion injury (65), hemorrhagic shock (66), and sickle cell disease (67) where RRx-001 has demonstrated activity, although not all this data is publicly available.
However, the effects of nitric oxide are not one-sided in terms of its pro-oxidant properties, as NO also induces transcriptional upregulation of Nrf2-related protective genes and activation of the tumor suppressor, p53 (68, 69).
4 Conclusion and future directions
The paradox of RRx-001, and what separates it from other NLRP3 inflammasome inhibitors and Nrf2 inducers, several of which are rationally designed to only inhibit the NLRP3 inflammasome or KEAP1, for example, is that RRx-001 switches between pro-oxidant/proinflammatory activity and antioxidant/anti-inflammatory activity depending on the redox potential of the cellular environment and the presence or absence of hypoxia. Such plasticity is rarely, if ever, seen because small molecules do not tend to alter their mechanism of action from one tissue to another. Thus, as a rule, a protective drug universally protects, no matter the tissue type, and the same is true for a cytotoxic one, which damages diseased and healthy cells alike. Chemotherapy may appear to preferentially target cancer cells but that is only because rapidly dividing cells are more sensitive to its toxic effects. In fact, chemotherapy is non-specific; it acts on rapidly dividing cancer cells and rapidly dividing normal ones, like those in the hair follicles, the gastrointestinal tract, and the bone marrow; hence the common side effects from chemotherapy of hair loss, vomiting and/or diarrhea, and myelosuppression.
The plasticity of RRx-001 is design-driven: the dinitroazetidine ring is stable under normoxia but under hypoxic, reductive conditions where vasodilation is needed most to increase local blood flow and oxygenation the ring fragments and releases nitric oxide via a radical process. Under mild hyperthermia, RRx-001 also increases NO production (70). See Figure 4 below. In hypoxic tumors where high levels of superoxide anion are an observed hallmark, NO outcompetes the enzyme superoxide dismutase (SOD), which breaks down superoxide into oxygen and hydrogen peroxide, and readily combines with to produce the cytotoxic and genotoxic radical, peroxynitrite, as follows: (71, 72). In turn, peroxynitrite decomposes to nitrogen dioxide (NO2) and hydroxyl radicals (·OH), two very potent oxidants with significant cytotoxic potential.

Figure 4 Dinitroazetidine Ring Fragmentation and Release of Nitric Oxide Under Reductive Conditions in Hypoxic Tissues.
Even though RRx-001 mediates nitro-oxidative stress and is cytotoxic to tumors through the formation of ONOO− and carbon- and nitrogen-centered radicals, it also protects against ischemia reperfusion injury (IRI) in several organs, including the heart and the kidneys, as preclinical data have demonstrated (73). One of the likely mechanisms behind this protective effect is NO release from RRx-001, which is thought to suppress superoxide generation through S-nitrosylation (SNO) of mitochondrial complex I. As a gas, nitric oxide, which passively diffuses through mitochondrial membranes, reversibly S-nitrosates cysteine 39 on the ND3 subunit of mitochondrial complex I (NADH:ubiquinone oxidoreductase); complex I is a dynamic enzyme, which transitions between active (-A) and deactivated (-D) states. During ischemia, complex I deactivates (-D state), which exposes the ND3 subunit Cys39 residue and makes it susceptible to modification. During reperfusion, complex I reactivates (-A state), which leads to an oxidative burst. S-nitrosylation of ND3 cysteine 39 temporarily inhibits complex I activity and delays mitochondrial recovery at the onset of reperfusion, hence attenuating excessive reactive oxygen species (ROS) production and oxidative damage (74).
The bromoacetyl end of the RRx-001 molecule inhibits the NLRP3 inflammasome, which is responsible for the release of proinflammatory cytokines, and KEAP1, which sequesters the antioxidant powerhouse, Nrf2, and targets it for degradation. NLRP3 inflammasome inhibition and Nrf2 induction are also related to the protective effects of RRx-001.
RRx-001 arose from a collaboration between the biopharmaceutical company, EpicentRx, (formerly RadioRx) and chemists from the aerospace and defense industry; the intent of this collaboration was to translate the well-known phrase, “the whole is greater than the sum of its parts” through a chimeric ADC-like small molecule, which combined independent chemical pharmacophores that were (and are) used in the aerospace and defense industry. Structure activity relationship (SAR) studies demonstrate that this is the case since the activity of the parent molecule significantly exceeds that of its individual pharmacophores or close analogs in which these pharmacophores are replaced (4).
Accordingly, RRx-001 is an entirely new molecular entity (NME) without precedent in the pharmaceutical space, which warrants the new USAN name, bromonitrozidine, reflective of its first-in-class mechanisms of action and its lack of belonging to any other pharmacological groups; the closest relative of RRx-001 is the high density, melt-castable explosive 1,3,3-Trinitroazetidine (TNAZ), which has been proposed as a replacement for dynamite (75). Like TNAZ, RRx-001 is extremely energetic, which makes it hazardous to manufacture, requiring special safety measures (76). These measures include the use of proper facilities in isolated areas well away from any habitation, and the need for substantial personal protective equipment and emergency procedures on site. Fortunately, the addition of solvents such as DMSO or polyethylene glycol (PEG) desensitizes RRx-001 and renders it safe for transport and use.
In summary, then, RRx-001 is a chimeric, CNS-penetrant (77), thiolate-reactive molecule that undergoes a physical change in response to an intrinsic, chemical trigger, reductive hypoxia (78). A potential second trigger is the application of mild hyperthermia. RRx-001 is active in cancer with a half maximal inhibitory concentration (IC50) in the subnanomolar range and synergizes with (79) and resensitizes to chemotherapies, immunotherapies, targeted therapies, and radiation (33, 80, 81). It is also a potential medical countermeasure against the effects of high dose, whole-body radiation exposure in radiological or nuclear incidents and has demonstrated preclinical neuroprotective effects in Parkinson’s and Alzheimer’s Diseases, Multiple Sclerosis, and Amyotrophic Lateral Sclerosis/Motor Neuron Disease.
In addition to RRx-001, co-crystals of RRx-001 and other dinitroazetidine-based small molecules with multi-indication potential are under development as is an oral formulation since in some disease indications, not necessarily cancer, the p.o. route is a more acceptable and economical method of administration despite the potential loss of bioavailability. A future patent-protected strategy (81) to increase the nitric oxide generation of RRx-001 (82–84), which takes advantage of its thermal sensitivity, is to apply mild hyperthermia noninvasively to the organs or tissues of interest during RRx-001 administration.
Author contributions
Conceptualization, BO and TR. Methodology, BO and TR. Writing—original draft preparation, BO and TR. Review and editing, all authors. All authors contributed to the article and approved the submitted version.
Conflict of interest
Authors BO, TR, and SC are employees of EpicentRx.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Iyengar R. Complex diseases require complex therapies. EMBO Rep (2013) 14(12):1039–42. doi: 10.1038/embor.2013.177
2. Bawa P, Pradeep P, Kumar P, Choonara YE, Modi G, Pillay V. Multi-target therapeutics for neuropsychiatric and neurodegenerative disorders. Drug Discovery Today (2016) 21:1886–914. doi: 10.1016/j.drudis.2016.08.001
3. Oronsky B, Reid TR, Larson C, Caroen S, Quinn M, Burbano E, et al. REPLATINUM phase III randomized study: RRx-001 + platinum doublet versus platinum doublet in third-line small cell lung cancer. Future Oncol (2019) 15(30):3427–33. doi: 10.2217/fon-2019-0317
4. Oronsky B, Guo X, Wang X, Cabrales P, Sher D, Cannizzo L, et al. Discovery of RRx-001, a myc and CD47 downregulating small molecule with tumor targeted cytotoxicity and healthy tissue cytoprotective properties in clinical development. J Med Chem (2021) 64(11):7261–71. doi: 10.1021/acs.jmedchem.1c00599
5. Kim MM, Parmar H, Cao Y, Pramanik P, Schipper M, Hayman J, et al. Whole brain radiotherapy and RRx-001: two partial responses in radioresistant melanoma brain metastases from a phase I/II clinical trial: a TITE-CRM phase I/II clinical trial. Transl Oncol (2016) 9(2):108–13. doi: 10.1016/j.tranon.2015.12.003
6. Oronsky B, Reid T, Cabrales P. Vascular priming with RRx-001 to increase the uptake and accumulation of temozolomide and irinotecan in orthotopically implanted gliomas. J Drug Targeting (2021) 29(9):998–1003. doi: 10.1080/1061186X.2021.1904248
7. Pardridge WM. The blood-brain barrier: bottleneck in brain drug development. NeuroRx (2005) 2(1):3–14. doi: 10.1602/neurorx.2.1.3
8. Oronsky B. Profile EpicentRx, inc. Hum Vaccin Immunother. (2023) 19(1):2184963. doi: 10.1080/21645515.2023.2184963
9. Oronsky B, Reid TR, Oronsky A, Sandhu N, Knox SJ. A review of newly diagnosed glioblastoma. Front Oncol (2021) 10:574012. doi: 10.3389/fonc.2020.574012
10. Reid T, Oronsky B, Caroen S, Cabrales P. The direct NLRP3 inhibitor and Phase 3 small molecule anticancer agent, RRx-001, protects aged triple transgenic Alzheimer’s disease model mice from CNS degeneration and cognitive decline. Alzheimer's Dement (2022) 18:e061516. doi: 10.1002/alz.061516
11. Forman HJ, Davies KJ, Ursini F. How do nutritional antioxidants really work: nucleophilic tone and para-hormesis versus free radical scavenging in vivo. Free Radic Biol Med (2014) 66:24–35. doi: 10.1016/j.freeradbiomed.2013.05.045
12. Halliwell B. The antioxidant paradox: less paradoxical now? Br J Clin Pharmacol (2013) 75(3):637–44. doi: 10.1111/j.1365-2125.2012.04272.x
13. Scuderi SA, Ardizzone A, Paterniti I, Esposito E, Campolo M. Antioxidant and anti-inflammatory effect of Nrf2 inducer dimethyl fumarate in neurodegenerative diseases. Antioxidants (2020) 9(7):630. doi: 10.3390/antiox9070630
14. Satoh T, Lipton S. Recent advances in understanding NRF2 as a druggable target: development of pro-electrophilic and non-covalent NRF2 activators to overcome systemic side effects of electrophilic drugs like dimethyl fumarate. F1000Res (2017) 6:2138. doi: 10.12688/f1000research.12111.1
15. Oronsky BT, Reid T, Knox SJ, Scicinski JJ. The scarlet letter of alkylation: a mini review of selective alkylating agents. Transl Oncol (2012) 5(4):226–9. doi: 10.1593/tlo.12187
16. Poole LB. The basics of thiols and cysteines in redox biology and chemistry. Free Radic Biol Med (2015) 80:148–57. doi: 10.1016/j.freeradbiomed.2014.11.013
17. Scicinski J, Oronsky B, Cooper V, Taylor M, Alexander M, Hadar R, et al. Development of methods for the bioanalysis of RRx-001 and metabolites. Bioanalysis (2014) 6(7):947–56. doi: 10.4155/bio.13.331
18. Scicinski J, Oronsky B, Taylor M, Luo G, Musick T, Marini J, et al. Preclinical evaluation of the metabolism and disposition of RRx-001, a novel investigative anticancer agent. Drug Metab Dispos (2012) 40(9):1810–6. doi: 10.1124/dmd.112.046755
19. Reid T, Oronsky B, Scicinski J, Scribner CL, Knox SJ, Ning S, et al. Safety and activity of RRx-001 in patients with advanced cancer: a first-in-human, open-label, dose-escalation phase 1 study. Lancet Oncol (2015) 16(9):1133–42. doi: 10.1016/S1470-2045(15)00089-3
20. Caroen S, Oronsky B, Reid T, Pandher K, Lopez A. Superficial venous-associated inflammation from direct IV administration of RRx-001 in rats. Int J Med Sci (2022) 19(11):1628–30. doi: 10.7150/ijms.76615
21. Abrouk N, Oronsky B, Caroen S, Ning S, Knox S, Peehl D. A note on improved statistical approaches to account for pseudoprogression. Cancer Chemother Pharmacol (2018) 81(3):621–6. doi: 10.1007/s00280-018-3529-4
22. Brzezniak C, Schmitz BA, Peterson PG, Degesys A, Oronsky BT, Scicinski JJ, et al. RRx-001-Induced tumor necrosis and immune cell infiltration in an EGFR mutation-positive NSCLC with resistance to EGFR tyrosine kinase inhibitors: a case report. Case Rep Oncol (2016) 9(1):45–50. doi: 10.1159/000443605
23. Coll RC, Schroder K, Pelegrín P. NLRP3 and pyroptosis blockers for treating inflammatory diseases. Trends Pharmacol Sci (2022) 43(8):653–68. doi: 10.1016/j.tips.2022.04.003
24. Jayabalan N, Oronsky B, Cabrales P, Reid T, Caroen S, Johnson AM, et al. A review of RRx-001: a late-stage multi-indication inhibitor of NLRP3 activation and chronic inflammation. Drugs (2023) 83(5):389–402. doi: 10.1007/s40265-023-01838-z
25. Fang J, She J, Lin F, Wu JC, Han R, Sheng R, et al. RRx-001 exerts neuroprotection against LPS-induced microglia activation and neuroinflammation through disturbing the TLR4 pathway. Front Pharmacol (2022) 13:889383. doi: 10.3389/fphar.2022.889383
26. Oronsky B, Caroen S, Reid T. What exactly is inflammation (and what is it not)? Int J Mol Sci (2022) 23(23):14905. doi: 10.3390/ijms232314905
27. Zhang N, Andresen BT, Zhang C. Inflammation and reactive oxygen species in cardiovascular disease. World J Cardiol (2010) 2(12):408–10. doi: 10.4330/wjc.v2.i12.408
28. Sharma M, de Alba E. Structure, activation and regulation of NLRP3 and AIM2 inflammasomes. Int J Mol Sci (2021) 22(2):872. doi: 10.3390/ijms22020872
29. Available at: https://www.prnewswire.com/news-releases/epicentrx-receives-fast-track-designation-from-the-us-fda-for-lead-asset-rrx-001-to-preventattenuate-chemotherapy-and-radiation-treatment-induced-severe-oral-mucositis-301784214.html.
30. Bonomi M, Blakaj DM, Kabarriti R, Colvett K, Takiar V, Biagioli M, et al. PREVLAR: phase 2a randomized trial to assess the safety and efficacy of RRx-001 in the attenuation of oral mucositis in patients receiving head and neck chemoradiotherapy. Int J Radiat Oncol Biol Phys (2023) 14:S0360–3016(22)03683-5. doi: 10.1016/j.ijrobp.2022.12.031
31. Wohlford GF, Van Tassell BW, Billingsley HE, Kadariya D, Canada JM, Carbone S, et al. Phase 1B, randomized, double-blinded, dose escalation, single-center, repeat dose safety and pharmacodynamics study of the oral NLRP3 inhibitor dapansutrile in subjects with NYHA II-III systolic heart failure. J Cardiovasc Pharmacol (2020) 77(1):49–60. doi: 10.1097/FJC.0000000000000931
32. Zhang X, Wang Z, Zheng Y, Yu Q, Zeng M, Bai L, et al. Inhibitors of the NLRP3 inflammasome pathway as promising therapeutic candidates for inflammatory diseases (Review). Int J Mol Med (2023) 51(4):35. doi: 10.1007/s00894-022-05405-3
33. Zhao H, Ning S, Scicinski J, Oronsky B, Knox SJ, Peehl DM. Epigenetic effects of RRx-001: a possible unifying mechanism of anticancer activity. Oncotarget (2015) 6(41):43172–81. doi: 10.18632/oncotarget.6526
34. Cabrales P. RRx-001 acts as a dual small molecule checkpoint inhibitor by downregulating CD47 on cancer cells and SIRP-α on Monocytes/Macrophages. Transl Oncol (2019) 12:626–32. doi: 10.1016/j.tranon.2018.12.001
35. Oronsky B, Scribner C, Aggarwal R, Cabrales P. RRx-001 protects normal tissues but not tumors via Nrf2 induction and bcl-2 inhibition. J Cancer Res Clin Oncol (2019) 145(8):2045–50. doi: 10.1007/s00432-019-02958-4
36. Baird L, Dinkova-Kostova AT. The cytoprotective role of the Keap1-Nrf2 pathway. Arch Toxicol (2011) 85(4):241–72. doi: 10.1007/s00204-011-0674-5
37. Jurgensen KJ, Skinner WKJ, Oronsky B, Abrouk ND, Graff AE, Landes RD, et al. RRx-001 radioprotection: enhancement of survival and hematopoietic recovery in gamma-irradiated mice. Front Pharmacol (2021) 12:676396. doi: 10.3389/fphar.2021.676396
38. Villa A, Sonis ST. Radiotherapy-induced severe oral mucositis: pharmacotherapies in recent and current clinical trials. Expert Opin Investig Drugs (2023) 22:1–10. doi: 10.1080/13543784.2023.2193324
39. Ning S, Sekar TV, Scicinski J, Oronsky B, Peehl DM, Knox SJ, et al. Nrf2 activity as a potential biomarker for the pan-epigenetic anticancer agent, RRx-001. Oncotarget (2015) 6(25):21547–56. doi: 10.18632/oncotarget.4249
40. Reid TR, Abrouk N, Caroen S, Oronsky B, Stirn M, Larson C, et al. ROCKET: phase II randomized, active-controlled, multicenter trial to assess the safety and efficacy of RRx-001 + irinotecan vs. single-agent regorafenib in Third/Fourth line colorectal cancer. Clin Colorectal Cancer. (2023) 22(1):92–9.
41. Reid T, Oronsky B, Caroen S, Quinn M, Williams J, Cabrales P, et al. Phase 1 pilot study of RRx-001 + nivolumab in patients with advanced metastatic cancer (PRIMETIME). Front Immunol (2023) 14:1104753. doi: 10.3389/fimmu.2023.1104753
42. Kim MM, Parmar HA, Schipper M, Devasia T, Aryal MP, Kesari S, et al. BRAINSTORM: a multi-institutional phase 1/2 study of RRx-001 in combination with whole brain radiation therapy for patients with brain metastases. Int J Radiat Oncol Biol Phys (2020) 107(3):478–86. doi: 10.1016/j.ijrobp.2020.02.639
43. Rojo delaVM, Chapman E, Zhang DD. NRF2 and the hallmarks of cancer. Cancer Cell (2018) 34(1):21–43. doi: 10.1016/j.ccell.2018.03.022
44. Vargas-Mendoza N, Morales-González Á, Morales-Martínez M, Soriano-Ursúa MA, Delgado-Olivares L, Sandoval-Gallegos EM, et al. Flavolignans from silymarin as Nrf2 bioactivators and their therapeutic applications. Biomedicines (2020) 8(5):122. doi: 10.3390/biomedicines8050122
45. Dinkova-Kostova AT, Copple IM. Advances and challenges in therapeutic targeting of NRF2. Trends Pharmacol Sci (2023) 44(3):137–49. doi: 10.1016/j.tips.2022.12.003
46. Jordan AL, Yang J, Fisher CJ, Racke MK, Mao-Draayer Y. Progressive multifocal leukoencephalopathy in dimethyl fumarate-treated multiple sclerosis patients. Mult Scler. (2022) 28(1):7–15. doi: 10.1177/1352458520949158
47. George S, Abrahamse H. Redox potential of antioxidants in cancer progression and prevention. Antioxidants (2020) 9(11):1156. doi: 10.3390/antiox9111156
48. Jeffrey R, Deschamps, Louis F, Cannizzo, Straessler. NA. Structure of 1-tert-Butyl-3-hydroxymethyl-3-nitroazetidine and 1-Bromoacetyl-3,3-dinitroazetidine, an investigative anticancer agent derived from energetic materials. J Chem Crystallogr (2013) 43(6):306–9.
49. Fens MH, Cabrales P, Scicinski J, Larkin SK, Suh JH, Kuypers FA, et al. Targeting tumor hypoxia with the epigenetic anticancer agent, RRx-001: a superagonist of nitric oxide generation. Med Oncol (2016) 33(8):85. doi: 10.1007/s12032-016-0798-9
50. Scicinski J, Oronsky B, Ning S, Knox S, Peehl D, Kim MM, et al. NO to cancer: the complex and multifaceted role of nitric oxide and the epigenetic nitric oxide donor, RRx-001. Redox Biol (2015) 6:1–8. doi: 10.1016/j.redox.2015.07.002
51. Oronsky BT, Scicinski JJ, Reid T, Knox S. Beyond antiangiogenesis: vascular modulation as an anticancer therapy-a review. Transl Oncol (2012) 5(3):133–40. doi: 10.1593/tlo.12118
52. Oronsky B, Scicinski J, Cabrales P, Minchinton A. RRx-001, an epigenetic-based radio- and chemosensitizer, has vascular normalizing effects on SCCVII and U87 tumors. Clin Epigenetics. (2016) 8:53. doi: 10.1186/s13148-016-0220-7
53. Lee MJ, Tomita Y, Yuno A, Lee S, Abrouk NE, Oronsky B, et al. Results from a biomarker study to accompany a phase II trial of RRx-001 with reintroduced platinum-based chemotherapy in relapsed small cell carcinoma. Expert Opin Investig Drugs (2021) 30(2):177–83. doi: 10.1080/13543784.2021.1863947
54. Oronsky BT, Knox SJ, Scicinski J. Six degrees of separation: the oxygen effect in the development of radiosensitizers. Transl Oncol (2011) 4(4):189–98. doi: 10.1593/tlo.11166
55. Cirrik S, Ugurel E, Aksu AC, Oronsky B, Cabrales P, Yalcin O. Nitrite may serve as a combination partner and a biomarker for the anti-cancer activity of RRx-001. Biorheology (2019) 56(4):221–35. doi: 10.3233/BIR-190213
56. Jani VP, Asaro R, Oronsky B, Cabrales P. RRx-001 increases erythrocyte preferential adhesion to the tumor vasculature. Int J Mol Sci (2021) 22(9):4713. doi: 10.3390/ijms22094713
57. Cabrales P, Scicinski J, Reid T, Kuypers F, Larkin S, Fens M, et al. A look inside the mechanistic black box: are red blood cells the critical effectors of RRx-001 cytotoxicity? Med Oncol (2016) 33(7):63. doi: 10.1007/s12032-016-0775-3
58. Oronsky B, Fanger GR, Oronsky N, Knox S, Scicinski J. The implications of hyponitroxia in cancer. Transl Oncol (2014) 7(2):167–73. doi: 10.1016/j.tranon.2014.02.001
59. Smeda M, Kieronska A, Adamski MG, Proniewski B, Sternak M, Mohaissen T, et al. Nitric oxide deficiency and endothelial-mesenchymal transition of pulmonary endothelium in the progression of 4T1 metastatic breast cancer in mice. Breast Cancer Res (2018) 20(1):86. doi: 10.1186/s13058-018-1013-z
60. Caroen S, Reid T, Oronsky B, Cabrales P. The NLRP3 inhibitor and Nrf2 agonist, RRx-001, ameliorates non-alcoholic fatty liver disease in rats. J Clin Lipidol. (2022) 16(3):e69. doi: 10.1016/j.jacl.2022.05.053
61. Oronsky B, Knox S, Cabrales P, Oronsky A, Reid TR. Desperate times, desperate measures: the case for RRx-001 in the treatment of COVID-19. Semin Oncol (2020) 47(5):305–8. doi: 10.1053/j.seminoncol.2020.07.002
62. Hammond TC, Lee RC, Oronsky B, Reid TR, Caroen S, Juarez TM, et al. Clinical course of two patients with COVID-19 respiratory failure after administration of the anticancer small molecule, RRx-001. Int Med Case Rep J (2022) 15:735–8. doi: 10.2147/IMCRJ.S389690
63. Oronsky B, Ao-Ieong ESY, Yalcin O, Carter CA, Cabrales P. Cardioprotective effect of phase 3 clinical anticancer agent, RRx-001, in doxorubicin-induced acute cardiotoxicity in mice. Mol Pharm (2019) 16(7):2929–34. doi: 10.1021/acs.molpharmaceut.9b00150
64. Yalcin O, Oronsky B, Carvalho LJ, Kuypers FA, Scicinski J, Cabrales P. From METS to malaria: RRx-001, a multi-faceted anticancer agent with activity in cerebral malaria. Malar J (2015) 14:218. doi: 10.1186/s12936-015-0720-5
65. Cabrales P, Caroen S, Oronsky A, Carter C, Trepel J, Summers T, et al. The macrophage stimulating anti-cancer agent, RRx-001, protects against ischemia-reperfusion injury. Expert Rev Hematol (2017) 10(6):575–82. doi: 10.1080/17474086.2017.1324779
66. Brouse C, Ortiz D, Su Y, Oronsky B, Scicinski J, Cabrales P. Impact of hemoglobin nitrite to nitric oxide reductase on blood transfusion for resuscitation from hemorrhagic shock. Asian J Transfus Sci (2015) 9(1):55–60. doi: 10.4103/0973-6247.150952
67. Fens HAM, Larkin SK, Fitch WL, Scicinski J, Oronsky B, Kuypers FA. Treatment with a novel dinitroazetidine, abdnaz, improves nitrite reductase activity of sickle red blood cells. Blood (2012) 120(21):3246. doi: 10.1182/blood.V120.21.3246.3246
68. Oronsky BT, Knox SJ, Scicinski JJ. Is nitric oxide (NO) the last word in radiosensitization? a review. Transl Oncol (2012) 5(2):66–71. doi: 10.1593/tlo.11307
69. Das DS, Ray A, Das A, Song Y, Tian Z, Oronsky B, et al. A novel hypoxia-selective epigenetic agent RRx-001 triggers apoptosis and overcomes drug resistance in multiple myeloma cells. Leukemia (2016) 30(11):2187–97. doi: 10.1038/leu.2016.96
70. Fens MH, Larkin SK, Oronsky B, Scicinski J, Morris CR, Kuypers FA. The capacity of red blood cells to reduce nitrite determines nitric oxide generation under hypoxic conditions. PloS One (2014) 9(7):e101626. doi: 10.1371/journal.pone.0101626
71. Wang Y, Branicky R, Noë A, Hekimi S. Superoxide dismutases: dual roles in controlling ROS damage and regulating ROS signaling. J Cell Biol (2018) 217(6):1915–28. doi: 10.1083/jcb.201708007
72. Virág L, Szabó E, Gergely P, Szabó C. Peroxynitrite-induced cytotoxicity: mechanism and opportunities for intervention. Toxicol Lett (2003) 140-141:113–24. doi: 10.1016/S0378-4274(02)00508-8
73. Oronsky B, Scicinski J, Ning S, Peehl D, Oronsky A, Cabrales P, et al. RRx-001, a novel dinitroazetidine radiosensitizer. Invest New Drugs (2016) 34(3):371–7. doi: 10.1007/s10637-016-0326-y
74. Babot M, Birch A, Labarbuta P, Galkin A. Characterisation of the active/de-active transition of mitochondrial complex I. Biochim Biophys Acta (2014) 1837(7):1083–92. doi: 10.1016/j.bbabio.2014.02.018
75. Oronsky B, Scicinski J, Ning S, Peehl D, Oronsky A, Cabrales P, et al. Rockets, radiosensitizers, and RRx-001: an origin story part I. Discovery Med (2016) 21(115):173–80.
76. Kanter J, Oronsky B, Reid T, Caroen S, Stirn M, Brinkhaus F, et al. Explosive hazards identified during the manufacture and transportation of 1-Bromoacetyl-3,3-dinitroazetidine (RRx-001). Organic Process Res Dev (2022) 26(11):3010–4. doi: 10.1021/acs.oprd.2c00109
77. Oronsky BT, Oronsky NC, Fanger GR, Oronsky AL, Lybeck MMC, Lybeck HE, et al. A review of two promising radiosensitizers in brain metastases: rrx-001 and 2-deoxyglucose. J Cancer Sci Ther (2015) 7:137–41. doi: 10.4172/1948-5956.1000338
78. Oronsky B, Carter CA, Caroen S, Scribner C, Oronsky A, Reid TR. RRx-001, a first-in-class small molecule inhibitor of MYC and a downregulator of CD47, is an “erythrophagoimmunotherapeutic”. Oncoimmunology (2020) 9(1):1746172. doi: 10.1080/2162402X.2020.1746172
79. Oronsky B, Reid TR, Oronsky A, Caroen S, Carter CA, Cabrales P. Brief report: RRx-001 is a c-myc inhibitor that targets cancer stem cells. Oncotarget (2018) 9(34):23439–42. doi: 10.18632/oncotarget.25211
80. Oronsky BT, Oronsky AL, Lybeck M, Oronsky NC, Scicinski JJ, Carter C, et al. Episensitization: defying time’s arrow. Front Oncol (2015) 5:134. doi: 10.3389/fonc.2015.00134
81. Oronsky B, Scicinski J, Reid T, Oronsky A, Carter C, Oronsky N, et al. RRx-001, a novel clinical-stage chemosensitizer, radiosensitizer, and immunosensitizer, inhibits glucose 6-phosphate dehydrogenase in human tumor cells. Discovery Med (2016) 21(116):251–65.
82. Oronsky B, Oronsky N, Cabrales P. Platelet inhibitory effects of the phase 3 anticancer and normal tissue cytoprotective agent, RRx-001. J Cell Mol Med (2018) 22(10):5076–82. doi: 10.1111/jcmm.13791
83. Oronsky B, Caroen S, Brinkhaus F, Reid T, Stirn M, Kumar R. Patent and marketing exclusivities 101 for drug developers. Recent Pat Biotechnol (2023) 17(3):257–70. doi: 10.2174/1872208317666230111105223
Keywords: RRx-001, NLRP3 inflammasome, Nrf2, KEAP1, nitric oxide, antibody drug conjugate (ADC), NFkB
Citation: Oronsky B, Takahashi L, Gordon R, Cabrales P, Caroen S and Reid T (2023) RRx-001: a chimeric triple action NLRP3 inhibitor, Nrf2 inducer, and nitric oxide superagonist. Front. Oncol. 13:1204143. doi: 10.3389/fonc.2023.1204143
Received: 11 April 2023; Accepted: 18 May 2023;
Published: 29 May 2023.
Edited by:
Barbara Marengo, University of Genoa, ItalyReviewed by:
Lisa Bouchier-Hayes, Baylor College of Medicine, United StatesKirtikar Shukla, Wake Forest University, United States
Copyright © 2023 Oronsky, Takahashi, Gordon, Cabrales, Caroen and Reid. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bryan Oronsky, Ym9yb25za3lAZXBpY2VudHJ4LmNvbQ==
 Bryan Oronsky
Bryan Oronsky Lori Takahashi1
Lori Takahashi1 Pedro Cabrales
Pedro Cabrales Scott Caroen
Scott Caroen