- 1Department of Hematology and Bone Marrow Transplantation, IRCCS San Raffaele Scientific Institute, Milan, Italy
- 2Vita-Salute San Raffaele University, Milan, Italy
- 3Department of Ophthalmology, IRCCS San Raffaele Scientific Institute, Milan, Italy
- 4Pathology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy
Chronic myelomonocytic leukemia (CMML) is a rare hematological disorder characterized by variable risk of evolution to acute myeloid leukemia; to date, allogeneic stem cell transplantation is the only curative treatment. We report a case of choroidal involvement in a woman affected by CMML and presenting only with visual impairment. The patient was initially evaluated for an intensive therapeutic approach, but after biopsy the ocular lesion spontaneously regressed. Thus a “watch and wait” strategy was preferred. One year and a half after initial diagnosis, the patient is alive, with stable hematological disease and without any ocular involvement. Therefore, a close, not invasive follow up could be useful to tailor treatment for patients affected by single ocular lesions in CMML.
Introduction
Chronic myelomonocytic leukemia (CMML) is a rare hematological disorder characterized by variable risk of evolution to acute myeloid leukemia (AML). Among prognostic models, the CPSS (1) and CPSS molecular (CPSS-mol) (2) are the most frequently used in CMML, in order to predict outcome and to guide treatment. Lower risk patients can undergo vigilant observation in the absence of significant cytopenias, while the only curative treatment for high risk patients is represented so far by allogeneic stem cell transplantation (allo-SCT) (3, 4). Extramedullary localization in CMML is uncommon and organs such as spleen, liver, skin, and lymph nodes are usually involved (5–8). Ocular involvement in CMML is rare and is associated with poor prognosis and increased risk of evolution to AML (9, 10). Here we report the case of a patient with single ocular involvement by CMML who did not receive specific treatment due to spontaneous remission of the lesion.
Case report
A 65-year-old woman was referred to our hematology service in July 2020 after a severe COVID-19 infection requiring intensive care (Figure 1). The patient presented with mild monocytosis and thrombocytopenia. Her complete blood counts (CBC) were: PLT 60 x 103/µl, WBC 6 x 103/µl, ANC 3.6 x 103/µl, ALC 1.2 x 103/µl, Monocytes 1.8 x 103/µl, Hb 12 g/dl, and MCV 100.5 fL. Her physical examination was negative. After a ten month follow up showing persistent monocytosis, thrombocytopenia and macrocytosis, secondary causes were ruled out (autoimmune or infectious diseases), and a bone marrow evaluation was diagnostic for CMML-0 dysplastic type according to WHO 2016 classification in May 2021. Cytogenetics and FISH were normal, while molecular testing showed oncogenic mutations in TET2 and SRSF2 genes. CPSS and CPSS-mol risk score were low, so a watch and wait strategy was established. Soon after, the patient complained of visual loss in her left eye; the dilated fundus evaluation showed mild vitritis and a hypo-pigmented choroidal lesion with exudative retinal detachment in the mid-temporal periphery. Multimodal imaging including A- and B-scan ultrasound, dye angiography and optical coherence tomography suggested an infiltrative lesion (Figure 2 – panels 1, 2A, 3A). A retino-choroidal biopsy, performed in December 2021, disclosed substantial involvement by medium-sized mononuclear cells, immunoreactive for CD45, CD14, and CD68R. The absence of CD34 and CD117 immunoreactivity ruled out a myeloid sarcoma and the ophthalmic lesion resulted consistent with involvement by CMML. The patient was evaluated for intensive chemotherapy and subsequent consolidation with allo-SCT considering the poor prognosis associated with ocular involvement (9, 10). However, one month later (January 2022), a new ophthalmic evaluation revealed a spontaneous decrease in the lesion size. In addition, a reduction in visual acuity from 20/28 to 20/100 was reported, due to damage to the outer retinal layers resulting from subretinal exudation. CBC and marrow disease were stable and, considering the low risk according to CPSS-mol, we opted for a “watch and wait” strategy. The CMML ophthalmic lesion completely disappeared in June 2022 (Figure 2 – panels 2B and 3B). At last follow up in March 2024 the patient had stable CBC; a new bone marrow evaluation, performed in November 2023, confirmed stable chronic disease, without signs of leukemic evolution and the left choroidal lesion was in complete remission with a good vision recovery.
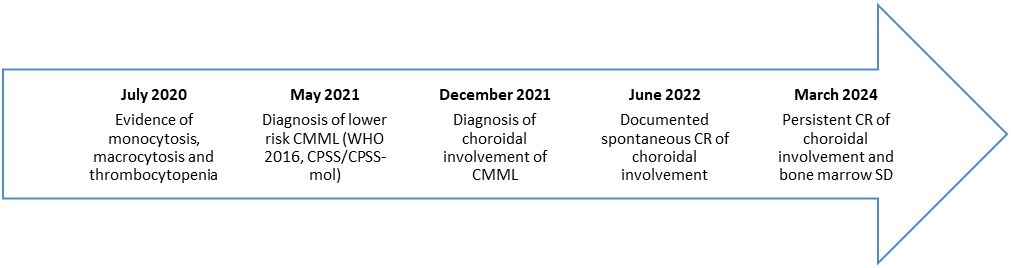
Figure 1 Timeline of relevant clinical data. CMML, chronic myelomonocytic leukemia; CPSS, CMML-specific prognostic scoring system; CPSS-mol, CMML-specific prognostic scoring system – molecular; CR, complete remission; SD, stable disease.
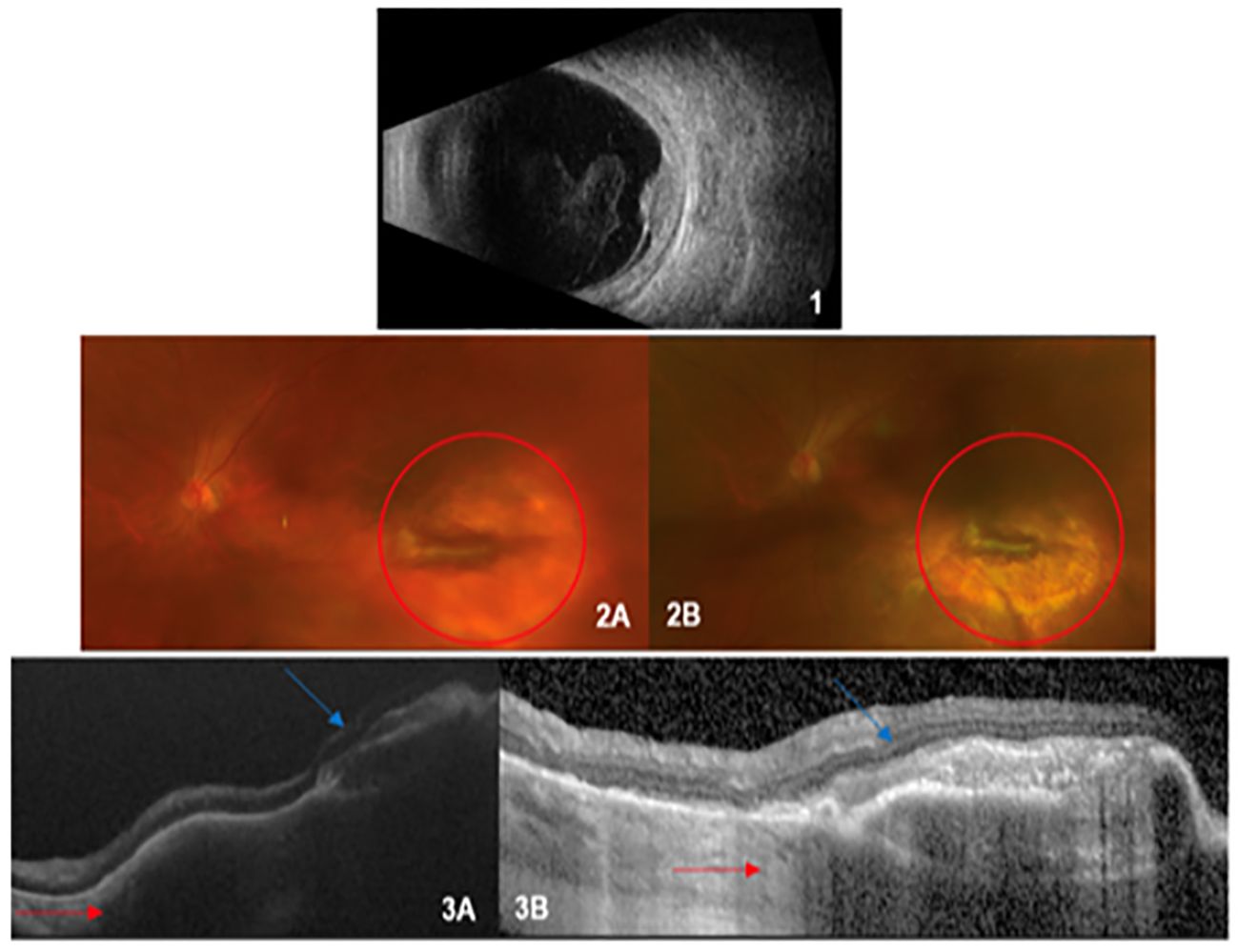
Figure 2 1) Scan Echography: raised lesion in the retinal plane with medium-low internal reflectivity with inferior exudate retinal detachment and mild vitritis. 2) Ultra-wide field retinography (baseline and follow-up): on the left (2A), a scarring lesion surrounded by a shaded retinal area (red circle); on the right (2B), disappearance of the shaded area around the permanent scar. 3) Optical Coherence Tomography (baseline and follow up): voluminous hyporeflective area under the retinal layer in the left image (3A), dramatically reduced after follow up in the right one (red arrow, 3B); the scarring lesion has remained stable (blue arrow).
Discussion
Extramedullary localization in CMML is uncommon and its prognostic value is unclear; a retrospective study by Mayo clinic demonstrated that non hepatosplenic extramedullary disease in patients affected by CMML did not impact on both overall and leukemia free survival (11). Ophthalmic localizations are rare but associated with poor prognosis (9, 10) and can lead to aggressive therapeutic approaches, particularly in young patients. In our case, the spontaneous remission of the single ocular lesion together with a favorable molecular risk score, prompted us to opt for a “watch and wait” approach. This resulted in preservation of a good health related quality of life, without signs of disease progression at last follow up. In conclusion, our case report describes a spontaneous remission of choroidal involvement by CMML, suggesting that a close, not invasive follow up could be useful to tailor treatment for patients affected by single ocular lesions in CMML.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ED: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Investigation, Validation. GC: Writing – original draft. MC: Investigation, Validation, Writing – original draft, Writing – review & editing, Conceptualization. AD: Writing – original draft. SM: Writing – review & editing. LV: Writing – review & editing. ML: Writing – review & editing. MB: Writing – review & editing. MP: Writing – original draft, Writing – review & editing. FC: Supervision, Validation, Writing – review & editing. MC: Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Such E, Germing U, Malcovati L, Cervera J, Kuendgen A, Della Porta MG, et al. Development and validation of a prognostic scoring system for patients with chronic myelomonocytic leukemia. Blood. (2013) 121:3005–15. doi: 10.1182/blood-2012-08-452938
2. Elena C, Galli A, Such E, Meggendorfer M, Germing U, Rizzo E, et al. Integrating clinical features and genetic lesions in the risk assessment of patients with chronic myelomonocytic leukemia. Blood. (2016) 128:1408–17. doi: 10.1182/blood-2016-05-714030
3. Robin M, de Wreede LC, Padron E, Bakunina K, Fenaux P, Koster L, et al. Role of allogeneic transplantation in chronic myelomonocytic leukemia: an international collaborative analysis. Blood. (2022) 140:1408–18. doi: 10.1182/blood.2021015173
4. Liu HD, Ahn KW, Hu ZH, Hamadani M, Nishihori T, Wirk B, et al. Allogeneic hematopoietic cell transplant for adult chronic myelomonocytic leukemia. Biol Blood Marrow Transplant. (2017) 23:767–75. doi: 10.1016/j.bbmt.2017.01.078
5. Bowen JM, Perry AM, Quist E, Akhtari M. Extramedullary hematopoiesis in a sentinel lymph node as an early sign of chronic myelomonocytic leukemia. Case Rep Pathol. (2015) 2015:594970. doi: 10.1155/2015/594970
6. Bradford CR, Smith SR, Wallis JP. Pericardial extramedullary hemopoiesis in chronic myelomonocytic leukemia. J Clin. Pathol. (1993) 46:674–5. doi: 10.1136/jcp.46.7.674
7. Mathew RA, Bennett JM, Liu JJ, Komrokji RS, Lancet JE, Naghashpour M, et al. Cutaneous manifestations in CMML: indication of disease acceleration or transformation to AML and review of the literature. Leuk. Res. (2012) 36:72–80. doi: 10.1016/j.leukres.2011.05.003
8. Hu L, Zheng B, Fu L, Hu M. Chronic myelomonocytic leukemia (CMML)-0 with pleural effusion as first manifestation. Medicine (2020) 99(44):e23030. doi: 10.1097/MD.0000000000023030
9. Ohkoshi K, Tsiaras WG. Prognostic importance of ophthalmic manifestations in childhood leukemia. Br J Ophthalmol. (1992) 76:651–5. doi: 10.1136/bjo.76.11.651
10. Kezuka T, Usui N, Suzuki E, Wakasugi K, Usui M. Ocular complications in myelodysplastic syndromes as preleukemic disorders. Jpn. J Ophthalmol. (2005) 49:377–83. doi: 10.1007/s10384-005-0228-6
Keywords: chronic myelomonocytic leukemia, ocular involvement, personalized medicine, multimodal imaging analysis, watch and wait approach
Citation: Diral E, Catalano G, Cicinelli MV, Distefano A, Mastaglio S, Vago L, Lupo Stanghellini MT, Bernardi M, Ponzoni M, Ciceri F and Carrabba MG (2024) Spontaneous remission of choroidal involvement by chronic myelomonocytic leukemia: a case report. Front. Oncol. 14:1399894. doi: 10.3389/fonc.2024.1399894
Received: 12 March 2024; Accepted: 19 April 2024;
Published: 02 May 2024.
Edited by:
Pasquale Niscola, Sant’Eugenio Hospital of Rome, ItalyReviewed by:
Na Wang, Shandong Provincial Hospital, ChinaHannes Becker, Tübingen University Hospital, Germany
Copyright © 2024 Diral, Catalano, Cicinelli, Distefano, Mastaglio, Vago, Lupo Stanghellini, Bernardi, Ponzoni, Ciceri and Carrabba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elisa Diral, ZGlyYWwuZWxpc2FAaHNyLml0
 Elisa Diral
Elisa Diral Gloria Catalano
Gloria Catalano Maria Vittoria Cicinelli
Maria Vittoria Cicinelli Andrea Distefano
Andrea Distefano Sara Mastaglio
Sara Mastaglio Luca Vago
Luca Vago Maria Teresa Lupo Stanghellini
Maria Teresa Lupo Stanghellini Massimo Bernardi
Massimo Bernardi Maurilio Ponzoni
Maurilio Ponzoni Fabio Ciceri
Fabio Ciceri Matteo G. Carrabba
Matteo G. Carrabba