- 1University Hospital for Urology, Klinikum Oldenburg, Department of Human Medicine, School of Medicine and Health Sciences, Carl von Ossietzky University Oldenburg, Oldenburg, Germany
- 2University Institute for Diagnostic and Interventional Radiology, Klinikum Oldenburg, Department of Human Medicine, School of Medicine and Health Sciences, Carl von Ossietzky University Oldenburg, Oldenburg, Germany
Invasive lymph node (LN) staging is crucial for survival in penile cancer (PeCa) patients. To lower patient morbidity associated with radical inguinal lymphadenectomy, sentinel node biopsy (SNB) is recommended. Application of conventional radioactive/fluorescent tracers for sentinel node (SN) labelling is limited to centers with nuclear medicine or lacks pre-operative imaging. We introduce a radiation-free fluorescent magnetic hybrid tracer for bimodal inguinal SN imaging in PeCa patients. In three consecutive PeCa patients, the fluorescent magnetic hybrid tracer (50 µl indocyanine green, 5 mg/ml, in 1 ml superparamagnetic iron oxide nanoparticles) was peritumorally injected. SNs were visualized by magnetic resonance imaging (MRI). Intra-operatively, SNs were detected using a handheld magnetometer and a fluorescence camera. Concordance was determined between MRI and magnetometer-guided SNB and between magnetic and fluorescent SN labelling. MRI revealed 29 SNs (median 4.5, range 0–8 SNs/groin). Twenty-five LNs (median 4.5, range 0–9 LNs/groin) were resected, including 16 magnetically active and 17 fluorescent SNs (median 3, range 0–6 SNs/groin, either mode). MRI and magnetometer-guided SNB had 66% concordance, magnetic and fluorescence SN labelling 96%. The diagnostic accuracy of our approach has to be evaluated in larger patient cohorts. Our radiation-free SNB technique is feasible without the need for nuclear medicine, its associated additional effort and regulations.
1 Introduction
In penile cancer (PeCa) patients, early and correct inguinal lymph node (LN) staging is crucial for prognosis and therapy planning as it directly affects the patients’ survival (1). Invasive LN staging is the preferred option (2) as imaging techniques lack sensitivity for detecting inguinal metastases smaller than 10 mm (1). Still, up to 55% of PeCa patients are subjected to post-operative morbidity with the number of resected LNs as main predictor for complications (1). European guidelines (1) therefore highly recommend sentinel node biopsy (SNB) for inguinal LN staging. The concept behind SNB is that sentinel nodes (SN) represent the first lymphatic drainage stations of a tumor bearing organ and carry thus the highest risk of LN invasion (LNI) (1). Hence, by identification and targeted resection of SNs a high staging accuracy can be achieved while reducing the risk of post-surgical complications. In PeCa, SNB has developed to a safe and reliable LN staging technique, particularly when using an indocyanine green-99mTechnetium (ICG-99mTc) hybrid tracer for SN marking combined with pre-operative lymphoscintigraphy as well as single-photon emission computed tomography/CT (SPECT/CT) (3, 4). The addition of ICG to the conventional tracer has been found to be especially helpful due to intra-operative optical SN detection (3). This procedure carries, however, the disadvantage of radioactivity and its general application may therefore be limited to specialized centers with nuclear medicine infrastructure. Radiation-free inguinal SN marking can be achieved by superparamagnetic iron oxide nanoparticles (SPION) (5). Pre-operative imaging and surgical planning can be realized via magnetic resonance imaging (MRI) (6). A combination of ICG and SPIONs for inguinal SN imaging and surgery has already been introduced in animal models (7). After successful application in prostate cancer patients (8), we present first results of the use of a fluorescent magnetic hybrid tracer for bimodal inguinal SN imaging in PeCa patients.
2 Methods
To demonstrate clinical tracer applicability, we included three consecutive PeCa patients with ≥ pT1a G2 tumors who were scheduled for inguinal SNB according to the European guidelines (1) at our center in 2023. We peritumorally injected the ICG-SPION hybrid tracer consisting of 50 µl ICG solution (25 mg ICG powder (Verdye, Diagnostic Green, Aschheim-Dornach, Germany) dissolved in 5 ml sterile water) and 1 ml SPION (Magtrace, Endomag, Cambridge, UK) one to three days before surgery. All patients were informed orally and in writing about the procedure and possible associated risks and all patients gave written informed consent. Abdominal transversal T1-, T2-, and T2*-weighted MRI sequences (6) were recorded for pre-operative inguinal SN visualization at four to seven hours before surgery. A radiologist well-experienced in magnetic sentinel diagnostics using MRI evaluated the scans and counted SNs for each groin separately. During SNB, each groin was systematically searched for magnetic as well as fluorescence signal using a handheld magnetometer probe (Sentimag, Endomag, Cambridge, UK) and a near-infrared fluorescence imaging (FI) system (Quest SPECTRUM 3, Olympus, Hamburg, Germany), respectively. LNs closely adjacent to SNs or suspicious LNs identified by the surgeon were resected, too. All resected LNs were documented, re-measured ex vivo for magnetic activity as well as for fluorescence, and sent to conventional histopathology as individual samples.
3 Results
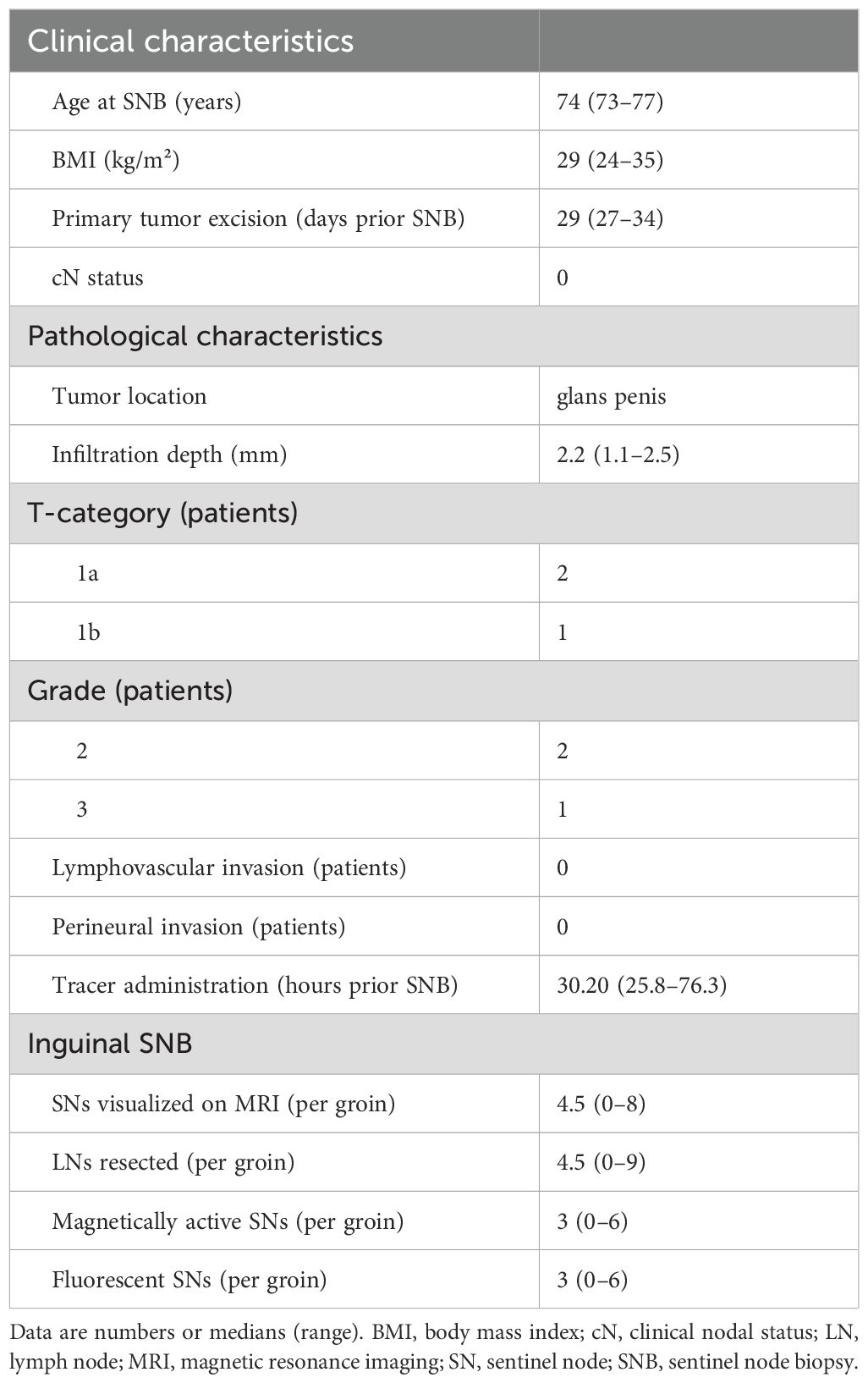
Clinical patient characteristics as well as therapeutic data are summarized in Table 1. On pre-operative inguinal MRI scans (Figures 1a, b), 29 LNs (Table 1) with SPION uptake have been identified. Overall, 25 LNs have been resected during inguinal SNB of which 16 LNs were magnetically active (Table 1). Concordance between pre-operative inguinal MRI scans and magnetometer-guided SNB was 66%. FI revealed, in total, 17 fluorescent LNs (Figures 1c, d; Table 1). All but one fluorescent LNs were magnetically active as well (Figures 1e, f). The resulting concordance between magnetometer-guided and FI-guided SNB was 96%. An example of a resected fluorescent as well as magnetically active SN is shown in Figure 1f. All resected LNs were histopathologically negative.
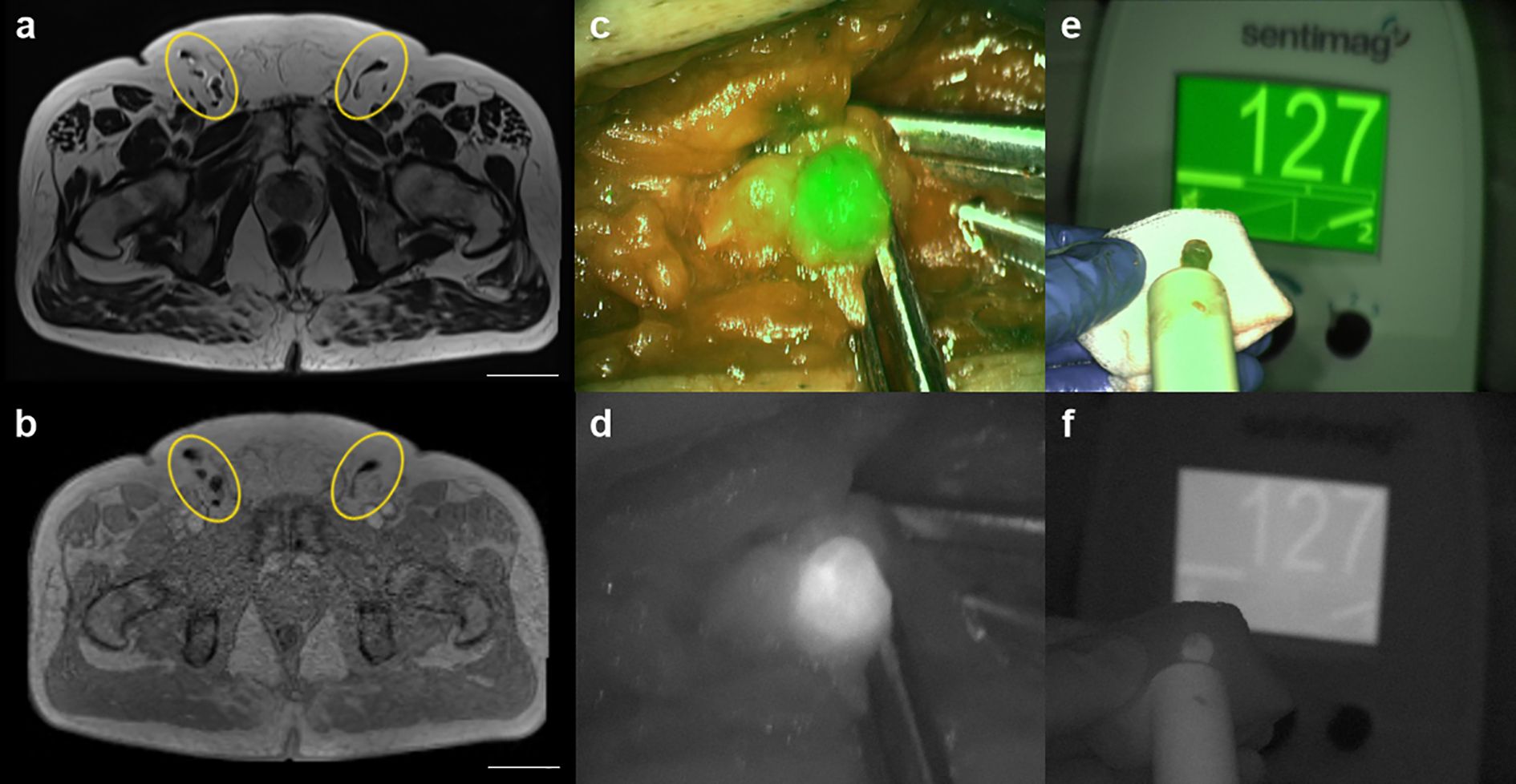
Figure 1. Pre- and intra-operative bimodal inguinal sentinel node (SN) imaging. (a, b) transversal abdominal T2- and T2*-weighted MRI scans (scale 50 mm) for pre-operative inguinal SN visualization (yellow circles). (c, d) intra-operative optical SN detection using a fluorescence imaging (FI) system; (c) overlay, (d) laser light. (e, f) resected fluorescent and magnetically active SN recorded by handheld magnetometer probe and FI; (e) overlay, (f) laser light.
None of the patients showed adverse reactions to tracer injection. No post-operative wound complications, such as seroma, infection or dehiscence, have been observed.
4 Discussion
These are the first results of radiation-free bimodal inguinal SN imaging using the new fluorescent and magnetic hybrid tracer in PeCa patients. The SPION component of the hybrid tracer enables pre-operative inguinal SN visualization and surgical planning via MRI as wells as intra-operative SN detection using a handheld magnetometer. The moderate concordance rates between MRI and intra-operative SN detection as observed in this pilot study could be partly explained by the high spatial resolution of MRI and its high sensitivity to very small concentrations of SPION. Pre-operative MRI might thus overestimate the actual SN number as we have reported previously for prostate cancer (8). To improve comparability between pre- and intra-operative SN detection and between future studies as well, we recommend to set up uniform definitions to distinguish magnetic SNs from other magnetic activity as they are used for the radioactive procedure (10).
The ICG component of our new hybrid tracer enables optical SN identification during surgery and thus, meticulous SN resection. Concordance between fluorescence and magnetic SN labelling was 96%. Due to its small molecule size, free ICG tends to label not only SNs but also higher echelon nodes (9). As observed in the ICG-99mTc hybrid tracer, the non-covalent binding of ICG to SPION might thus avoid unnecessary LN resection (10). This is crucial especially in intermediate risk (pT1a G2) patients for whom the risk of LN metastasis as well as the risks associated with surgical staging have to be carefully balanced (1). Our study is limited by its small sample size. While the number of only three patients is adequate to address the clinical application of our new hybrid tracer in this rare tumor entity, our results regarding the diagnostic accuracy of the new technique are only preliminary. The diagnostic accuracy as well as safety of the fluorescent magnetic hybrid tracer have to be confirmed in multicentric studies including larger patient series. In order to acknowledge possible undetected false negative procedures, future studies assessing the diagnostic accuracy of our new technique should also implement an oncological follow-up schedule for at least two years from surgery. Nevertheless, our radiation-free approach for SNB can easily be transferred to centers without nuclear medicine infrastructure and might help to improve surgical inguinal LN staging while reducing post-surgical morbidity in PeCa patients.
Data availability statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics statement
This study was performed in line with the principles of the Declaration of Helsinki. Patients included in this analysis were a sub-cohort from another, larger study approved by the Medical Ethics Committee of the University of Oldenburg, Germany (approval no.: 2020-186, date: 2021/04/16).
Author contributions
BM: Conceptualization, Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. SE: Conceptualization, Formal Analysis, Investigation, Writing – review & editing. MO: Investigation, Writing – review & editing. MM: Writing – review & editing. FW: Writing – review & editing. AW: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Brouwer OR, Tagawa ST, Albersen M, Ayres B, Crook J, van der Heijden MS, et al. EAU-ASCO guidelines on penile cancer. Arnhem, The Netherlands: EAU Guidelines Office (2024). Available at: https://uroweb.org/guidelines/penile-cancer (Accessed July 15, 2024).
2. Protzel C, Alcaraz A, Horenblas S, Pizzocaro G, Zlotta A, Hakenberg OW. Lymphadenectomy in the surgical management of penile cancer. Eur Urol. (2009) 55:1075–88. doi: 10.1016/j.eururo.2009.02.021
3. Dell’Oglio P, de Vries HM, Mazzone E, KleinJan GH, Donswijk ML, van der Poel HG, et al. Hybrid indocyanine green-99mTc-nanocolloid for single-photon emission computed tomography and combined radio- and fluorescence-guided sentinel node biopsy in penile cancer: Results of 740 inguinal basins assessed at a single institution. Eur Urol. (2020) 78:865–72. doi: 10.1016/j.eururo.2020.09.007
4. Torbrand C, Warnolf Å, Glombik D, Davidsson S, Carlsson J, Baseckas G, et al. Sentinel node identification with hybrid tracer-guided and conventional dynamic sentinel node biopsy in penile cancer: A prospective study in 130 patients from the two national referral centres in Sweden. Eur Urol Oncol. (2022) 5:704–11. doi: 10.1016/j.euo.2022.09.004
5. Cleaveland P, Lau M, Parnham A, Murby B, Ashworth D, Manohoran P, et al. Testing the feasibility of SentiMag/Sienna+ for detecting inguinal sentinel nodes in penile cancer (SentiPen): An eUROGEN and national cancer research institute trial. Eur Urol. (2019) 76:874–5. doi: 10.1016/j.eururo.2019.09.007
6. Winter A, Kowald T, Engels S, Wawroschek F. Magnetic resonance sentinel lymph node imaging and magnetometer-guided intraoperative detection in penile cancer, using superparamagnetic iron oxide nanoparticles: first results. Urol Int. (2020) 104:177–80. doi: 10.1159/000502017
7. Azargoshasb S, Molenaar L, Rosiello G, Buckle T, van Willigen DM, van de Loosdrecht MM, et al. Advancing intraoperative magnetic tracing using 3D freehand magnetic particle imaging. Int J CARS. (2022) 17:211–8. doi: 10.1007/s11548-021-02458-2
8. Michalik B, Engels S, Otterbach MC, Frerichs J, Suhrhoff PE, van Oosterom MN, et al. A new bimodal approach for sentinel lymph node imaging in prostate cancer using a magnetic and fluorescent hybrid tracer. Eur J Nucl Med Mol Imaging. (2024) 51:2922–8. doi: 10.1007/s00259-023-06522-8
9. Ohnishi S, Lomnes SJ, Laurence RG, Gogbashian A, Mariani G, Frangioni JV. Organic alternatives to quantum dots for intraoperative near-infrared fluorescent sentinel lymph node mapping. Mol Imaging. (2005) 4:172–81. doi: 10.1162/15353500200505127
10. Wit EMK, KleinJan GH, Berrens AC, van Vliet R, van Leeuwen PJ, Buckle T, et al. A hybrid radioactive and fluorescence approach is more than the sum of its parts; outcome of a phase II randomized sentinel node trial in prostate cancer patients. Eur J Nucl Med Mol Imaging. (2023) 50:2861–71. doi: 10.1007/s00259-023-06191-7
Keywords: fluorescence imaging, hybrid tracer, ICG, penile cancer, sentinel lymph nodes, SPION
Citation: Michalik B, Engels S, Otterbach MC, Maurer MH, Wawroschek F and Winter A (2025) Bimodal inguinal sentinel lymph node imaging using a radiation-free fluorescent magnetic hybrid tracer in penile cancer patients. Front. Oncol. 15:1523038. doi: 10.3389/fonc.2025.1523038
Received: 05 November 2024; Accepted: 18 April 2025;
Published: 09 May 2025.
Edited by:
Lothar Bergmann, University Hospital Frankfurt, GermanyReviewed by:
David González Calatayud, Autonomous University of Madrid, SpainMatthias May, St. Elisabeth-Hospital Straubing, Germany
Copyright © 2025 Michalik, Engels, Otterbach, Maurer, Wawroschek and Winter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexander Winter, d2ludGVyLmFsZXhhbmRlckBrbGluaWt1bS1vbGRlbmJ1cmcuZGU=
 Bianca Michalik1
Bianca Michalik1 Alexander Winter
Alexander Winter