- 1Department of Hepatopancreatobiliary Surgery, The Affiliated Lihuili Hospital, Ningbo University, Ningbo, Zhejiang, China
- 2French Blood Establishment (EFS), National Institute of Health and Medical Research (INSERM), Joint Research Unit Regulation of Immunity for therapeutic innovation in Graft, Host, Tumoral and inflammatory associated diseases (UMR RIGHT) F-25000, Franche-Comté University, Besançon, France
- 3School of Public Health, Ningbo University Health Science Center, Ningbo, China
- 4Laboratory of the Metabolic Adaptations to Exercise Training Under Physiological and Pathological Conditions (AME2P), Clermont Auvergne University, Clermont-Ferrand, France
Introduction: This study aims to investigate the effects of Metformin on hepatocellular carcinoma cell lines, cell lines and explores the molecular mechanisms underlying.
Methods: Bel-7402 and HepG2 cells were treated with varying concentrations of Metformin and ferrostatin-1 to assess cytotoxicity using the MTT assay. Protein expression and phosphorylation changes were analyzed through a phosphoproteomics approach and further bioinformatics analysis, including Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) databases. The data from phosphoproteomics were confirmed by western blot. Metformin treatment significantly reduced cell viability in a concentration- and time-dependent manner. Phosphoproteomics analysis identified differentially expressed proteins (DEPs) primarily associated with ferroptosis and cellular metabolism. Further GO and KEGG analyses revealed the involvement of DEPs in nucleotide biosynthesis, membrane transport, and metabolic pathways. Then the bioinformatic data were verified through MTT and western blot.
Results and discussion: The results showed that ferrostatin-1 could partly reverse the inhibitory effects of Metformin, suggesting the involvement of ferroptosis. Moreover, the modulation of autophagy and ferroptosis-related proteins by Metformin was confirmed by western blot. Our findings demonstrate that Metformin induces ferroptosis in Bel-7402 and HepG2 cell lines, potentially offering a novel therapeutic strategy for the treatment of hepatocellular carcinoma. The phosphoproteomics analysis provides insights into the molecular mechanisms by which Metformin exerts its anti-cancer effects.
1 Introduction
Hepatocellular carcinoma (HCC) accounts for the majority of primary liver cancer and represents the fourth leading cause of worldwide cancer deaths (1, 2). It commonly develops through a multistep process from liver cirrhosis to low-grade dysplastic nodule, high-grade dysplastic nodule, early HCC and progressed HCC (3). Ferroptosis, a novel type of cell death due to iron-dependent phospholipid peroxidation, has received extensive attention for its lethal effect on tumor cells (4, 5). The dysregulation of ferroptosis is highly associated with the progression of HCC, and the induction of ferroptosis is also proposed as a potential promising strategy for HCC therapy (6). Accordingly, it is pertinent to elucidate the mechanisms of ferroptosis in HCC to eventually identify useful therapeutic approaches for this disease.
Metformin, a biguanide commonly used as a first-line agent for type 2 diabetes, has attracted increasing attention for its anti-cancer properties, particularly in liver-related malignancies (7, 8). Beyond its glucose-lowering activity via AMPK activation, metformin has been reported to suppress tumor progression through multiple mechanisms, including cell cycle arrest, inhibition of epithelial–mesenchymal transition (EMT), and modulation of metabolic stress (9, 10). Recent studies also demonstrate that metformin can trigger ferroptosis in HCC cells via pathways involving ATF4/STAT3 signaling or suppression of the p62–Keap1–Nrf2 antioxidant axis, thereby enhancing sensitivity to chemotherapeutic agents such as sorafenib (11, 12, (13). Additionally, ferroptosis sensitivity has been shown to be tightly regulated by the p53–SLC7A11–GPX4 axis in liver cancer cells, offering new insight into how metformin might influence this cascade (14). Notably, recent studies have highlighted the cell-line–dependent heterogeneity in ferroptosis sensitivity among HCC models. For instance, Hu et al. reported that gene expression and antioxidant capacity related to ferroptosis varied significantly between HCC cell lines, underscoring the need for parallel experimental validation across multiple models (15).
Importantly, metformin’s effects appear to intersect with autophagy and redox regulation, yet the phosphoproteomic landscape underlying these effects in HCC remains poorly defined. Protein phosphorylation plays a key role in regulating cellular signaling and is tightly linked to stress responses, metabolism, and cell death pathways (16, 17). Dysregulation of phosphorylation-mediated processes often participates in the initiation and progression of many human diseases, including cancers (18). Phosphoproteomics has evolved as a powerful tool to reveal phosphorylation sites of kinases and can provide important insights into kinases that can be targeted for therapeutic intervention; in particular, the phosphoproteomics-based approaches have been widely used to investigate cancer cells and develop personalized treatment (19, 20).
In this study, we hypothesize that metformin inhibits HCC cell proliferation by inducing ferroptosis through phosphorylation-mediated signaling networks. To test this hypothesis, we employed integrated phosphoproteomic profiling, bioinformatic pathway analysis, and in vitro validation using ferroptosis inhibitors. Our aim is to delineate the signaling events by which metformin exerts its anti-HCC effects, with the ultimate goal of identifying actionable ferroptosis-associated regulatory nodes.
2 Materials and methods
2.1 Human cell cultures
The Bel-7402 and HepG2 cell lines, both widely used for hepatocellular carcinoma research, were acquired from the American Type Culture Collection (ATCC) and cultured under sterile conditions to ensure cell viability and purity. The cells were maintained in a culture flask with Dulbecco’s Modified Eagle’s Medium (DMEM, Gibco, Cat. No. 11-965-092, USA), supplemented with 10% fetal bovine serum (FBS, Gibco, Cat. No.11560636, USA) and 1% penicillin-streptomycin (ThermoFicher Scientific, Cat. No.15323671, USA). The cultures were maintained in a humidified incubator at 37°C with 5% CO2. Passaging of the cells was carried out when the cells reached approximately 80-90% confluence, 0.25% Trypsin-EDTA (ThermoFisher Scientific, Cat. No. 25200072) was used to digest cells, the cell suspension was then transferred to new culture flasks for further experiments.
2.2 MTT assay of metformin and ferrosatin-1 treatment
To assess the cytotoxic effects of Metformin and Ferrostatin-1 on Bel-7402 and HepG2 cells, MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay was employed to determine the cell viability and proliferation. Briefly, a total of 10000 cells in 200 μL medium were pipetted into 96-well plates to grow for 24h. They were then pre-treated with 1 µM Ferrostatin-1 for 24 hours (21) before exposure to Metformin (Santa-Cruz, Cat. No. 1115-70-4) (0, 1, 2, 5, 10 and 20mM, diluted in phosphate buffer saline) for 24, 48, or 72 hours. After treatment, 20 μL of MTT reagent was added to each well, and the cells were incubated for 4 hours at 37°C. Then the medium was discarded, and formazan precipitate was dissolved in 150 μL DMSO. Absorbance at 570 nm was measured by a plate reader (Tecan Spark®, Männedorf, Switzerland). Each experimental group was conducted in triplicate.
2.3 Protein extraction and preparation
Total cellular proteins were extracted using RIPA buffer (ThermoFisher Scientific, Cat. No. 89900), supplemented with a cocktail of protease and phosphatase inhibitors (Roche) to prevent degradation and dephosphorylation of target proteins. Extracts from each sample were reduced with 2mM DTT for 1 hour at 56°C, and subsequently alkylated with sufficient iodoacetamide for 1 hour at room temperature in the dark. Then 4 times the volume of precooled acetone was mixed with samples by well vortexing and incubated at -20°C for at least 2 hours. Samples were then centrifuged and the precipitation was collected. After washing twice with cold acetone, the pellet was dissolved by dissolution buffer, which contained 0.1 M triethylammonium bicarbonate (TEAB, pH 8.5) and 6 M urea. Protein concentration was determined again by Bradford protein assay.
2.4 Peptide digestion and phosphopeptide enrichment
Digestion of 5 mg of protein was performed with Trypsin Gold at a 1:50 enzyme-to-substrate ratio for 16 hours at 37°C. Peptides were desalted using a C18 cartridge and dried by vacuum centrifugation. For phosphopeptide enrichment, peptides were redissolved in 250 mM acetic acid with 30% acetonitrile, adjusted to pH 2.5-3.0, and processed using phos-select iron affinity gel according to the manufacturer’s protocol. The bounded peptides were eluted, dried and desalted using peptide desalting spin columns (Thermo Fisher, 89852).
2.5 LC-MS/MS analysis and data interpretation
Peptides were analyzed using an EASY-nLC™ 1200 UHPLC system (Thermo Fisher) coupled with an Orbitrap Q Exactive HF-X mass spectrometer (Thermo Fisher) operated in data-dependent acquisition (DDA) mode and positive polarity. Full MS scans were acquired at a resolution of 60,000 (at m/z 200) over a scan range of 350–1,500 m/z. The automatic gain control (AGC) target for MS1 was set to 3 × 106, with a maximum injection time of 50 ms. The top 20 most intense precursor ions were selected for higher-energy collisional dissociation (HCD) with a normalized collision energy (NCE) of 27%. MS/MS scans were acquired at a resolution of 15,000 (at m/z 200), using an isolation window of 1.6 m/z, an AGC target of 1 × 105, and a maximum injection time of 45 ms. Dynamic exclusion was enabled with a duration of 30 seconds to avoid repeated selection of precursor ions.
The resulting spectra were searched against a protein database using Proteome Discoverer 2.2 (PD 2.2, Thermo), with carbamidomethylation as a fixed modification, and oxidation of methionine, phosphorylation of serine (S), threonine (T), and tyrosine (Y), and N-terminal acetylation as variable modifications. Protein identification was performed at a false discovery rate (FDR) < 1.0%, and label-free quantification was applied. The protein quantitation results were statistically analyzed by the Mann–Whitney test. Differentially expressed proteins (DEPs) were defined based on fold-change (ratio > 4 or < 0.25) and statistical significance (P < 0.05).
Functional analysis of proteins and DEPs was conducted using Gene Ontology (GO), InterPro (IPR), COG (Clusters of Orthologous Groups), and KEGG (Kyoto Encyclopedia of Genes and Genomes) databases. GO and IPR analysis was conducted using the InterProScan-5 program against the non-redundant protein database (including Pfam, PRINTS, ProDom, SMART, ProSiteProfiles, and PANTHER). STRING-db (http://string.embl.de/) was used to predict potential protein–protein interactions based on related species. Motif enrichment analysis was conducted using the motif-x algorithm, focusing on a 7-amino acid window surrounding each phosphosite (occurrence > 20, P < 10−6), and visualized with WebLogo. Phosphorylation site–kinase relationships were predicted using the NetPhorest algorithm.
2.6 Western blot
Total cellular proteins were extracted using RIPA buffer (ThermoFisher Scientific, Cat. No. 89900), supplemented with a cocktail of protease and phosphatase inhibitors (Roche, Cat. No. 04693132001) to prevent degradation and dephosphorylation of target proteins. Protein concentrations were quantified using the BCA Protein Assay Kit (ThermoFisher Scientific, Cat. No. A55860), ensuring accurate loading of samples. 50 μg of each protein extract was resolved by SDS-PAGE and electrophoretically transferred onto a nitrocellulose membrane. The membranes were then incubated with primary antibodies specific for ATG9 (Abcam, ab108338, diluted 1:1000), ATG5 (Abcam, ab108327, diluted 1:1000), ATG16 (Abcam, ab188642, diluted 1:1000), P62 (Abcam, ab109012, diluted 1:10000), Beclin-1 (Abcam, ab207612, diluted 1:2000), Ic3b (Abcam, ab231078, diluted 1:1000), SLC7A (Abcam, ab236669, diluted 1:500), GPX4 (Abcam, ab125066, diluted 1:1000), ASCL4 (Abcam, ab155282, diluted 1:10000), and β-actin (Abcam, ab8227, diluted 1:1000) overnight at 4°C to ensure efficient antigen-antibody binding. After thorough washing with Tris-buffered saline with Tween (TBST) to remove unbound primary antibodies, the membranes were incubated with an HRP-conjugated secondary antibody (Bio-Rad, diluted 1:2000) for 1 hour at room temperature to amplify the signal. To visualize the immunoreactive bands, the membranes were developed using a chemiluminescent substrate (ThermoFisher Scientific, Cat. No. 34080). The luminescent signal was detected by ChemiDoc™ Imaging System (Bio-Rad) and relative expression levels normalized to β-actin were calculated
3 Results
3.1 Cellular viability response of Bel-7402 and HepG2 treated by metformin
The cell viability of two cell lines including Bel-7402 and HepG2 treated with Metformin of multiple concentrations was detected by MTT assay. The results showed that the cell viability of Bel-7402 cells indicated a negative correlation with Metformin concentration at different time points of 24, 48 and 72 hours. Among these, the Bel-7402 cells treated with 20mM Metformin at 72 hours exhibited the lowest cell viability compared with other groups, thus this concentration was selected for further experiment. Similarly, the results in HepG2 cells also represented the higher concentration of Metformin or longer duration of treatment, the lower cell viability of cells (Figure 1). These results indicated the inhibitory effect of Metformin on the proliferation of Bel-7402 and HepG2.
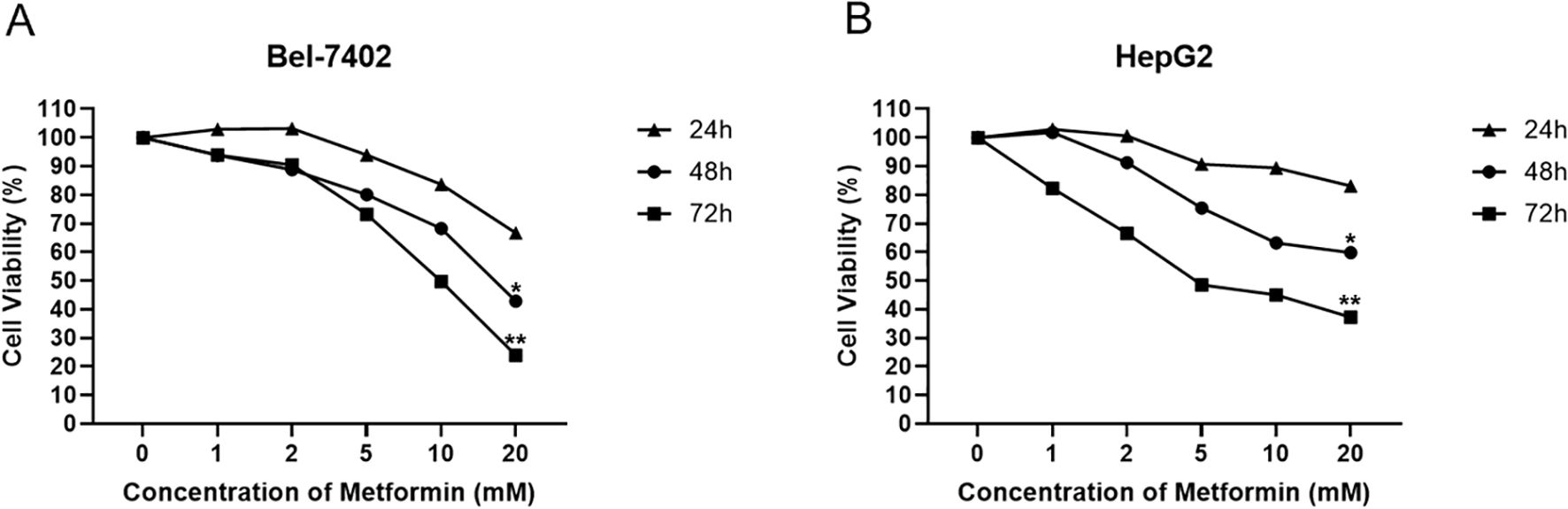
Figure 1. Cellular viability response of Bel-7402 (A) and HepG2 (B) treated by Metformin with different concentrations at 24, 48 and 72 hours using MMT assay. Data are presented as mean ± SD (n = 3). Statistical analysis was performed using one-way ANOVA followed by Tukey’s post hoc test. P< 0.05 (*) and P< 0.01 (**) indicate statistically significant differences compared to the 0 mM (control) group.
3.2 Phosphoproteomics of Bel-7402 and HepG2 treated by metformin
To further explore the molecular regulation mechanism of Metformin in hepatocellular carcinoma cells, phosphoproteomics and bioinformatics analysis were performed. As shown in Figure 2, the heatmap and volcano plot showed a distinct difference between the control group (Bel_0/Hep_0) and Metformin-treated groups (Bel_20/Hep_20) either in Bel-7402 or HepG2 cells. Furthermore, subcellular localization analysis revealed that the alternation of DEPs was mainly located in the nucleus, with 44.58% in Bel-7402 and 47.95% in HepG2 cells, followed by cytoplasm proteins.
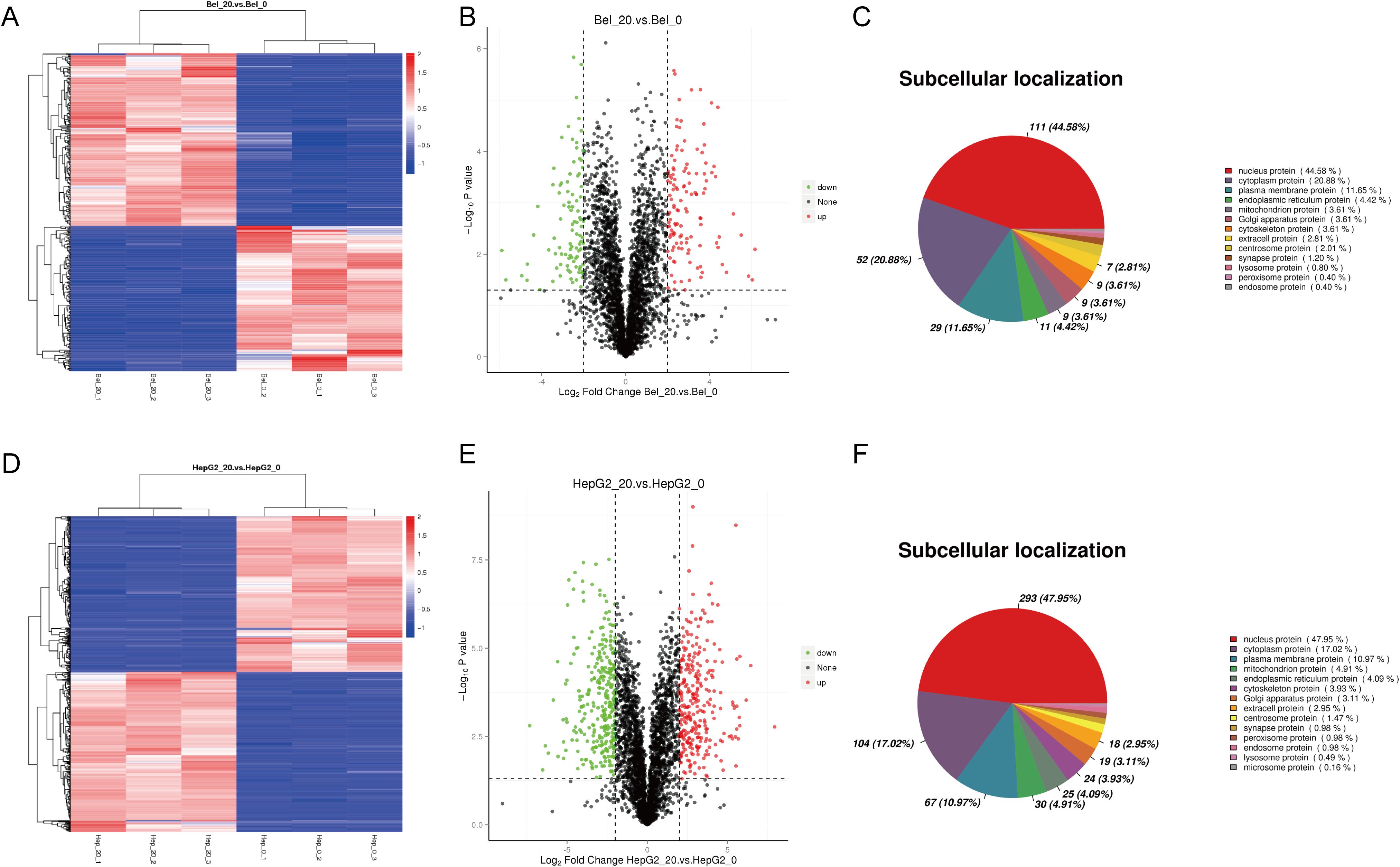
Figure 2. Phosphoproteomics of Bel-7402 and HepG2 treated by Metformin. The heatmap, volcano plot and subcellular localization analysis in Bel-7402 (A–C) and HepG2 (D–F) cell lines. Significantly altered phosphoproteins (n = 132 for Bel-7402; n = 148 for HepG2) were identified using p < 0.05 and fold-change >4 or <0.25 as cutoffs. Red and blue indicate upregulation and downregulation, respectively.
3.3 Gene ontology and KEGG analysis of phosphoproteomics
The function of DEPs between control and Metformin-treated groups in two cell groups was further analyzed by Gene Ontology analysis. Specifically, the enriched GO analysis showed that the top 5 terms in Bel-7402 cells were pyrimidine nucleotide biosynthetic process, chemical homeostasis, GTP biosynthetic process, UTP biosynthetic process and CTP biosynthetic process in Biological Process (BP); membrane region, endoplasmic reticulum, cytoplasmic part, membrane raft, whole membrane in Cellular Component (CC); and ion channel activity, protein phosphatase regulator activity, calcium ion transmembrane transporter activity, nucleoside diphosphate kinase activity, phosphatase binding in Molecular Function (MF) (Figure 3A). The KEGG pathway analysis of Bel-7402 cells suggested the significant difference in the pathway between Bel_0 and Bel_20 was mainly focused on the biosynthesis and metabolism regulation, such as Ubiquinone and other terpenoid-quinone biosynthesis, Glycine, serine and threonine metabolism, and Insulin secretion, etc (Figure 3B).
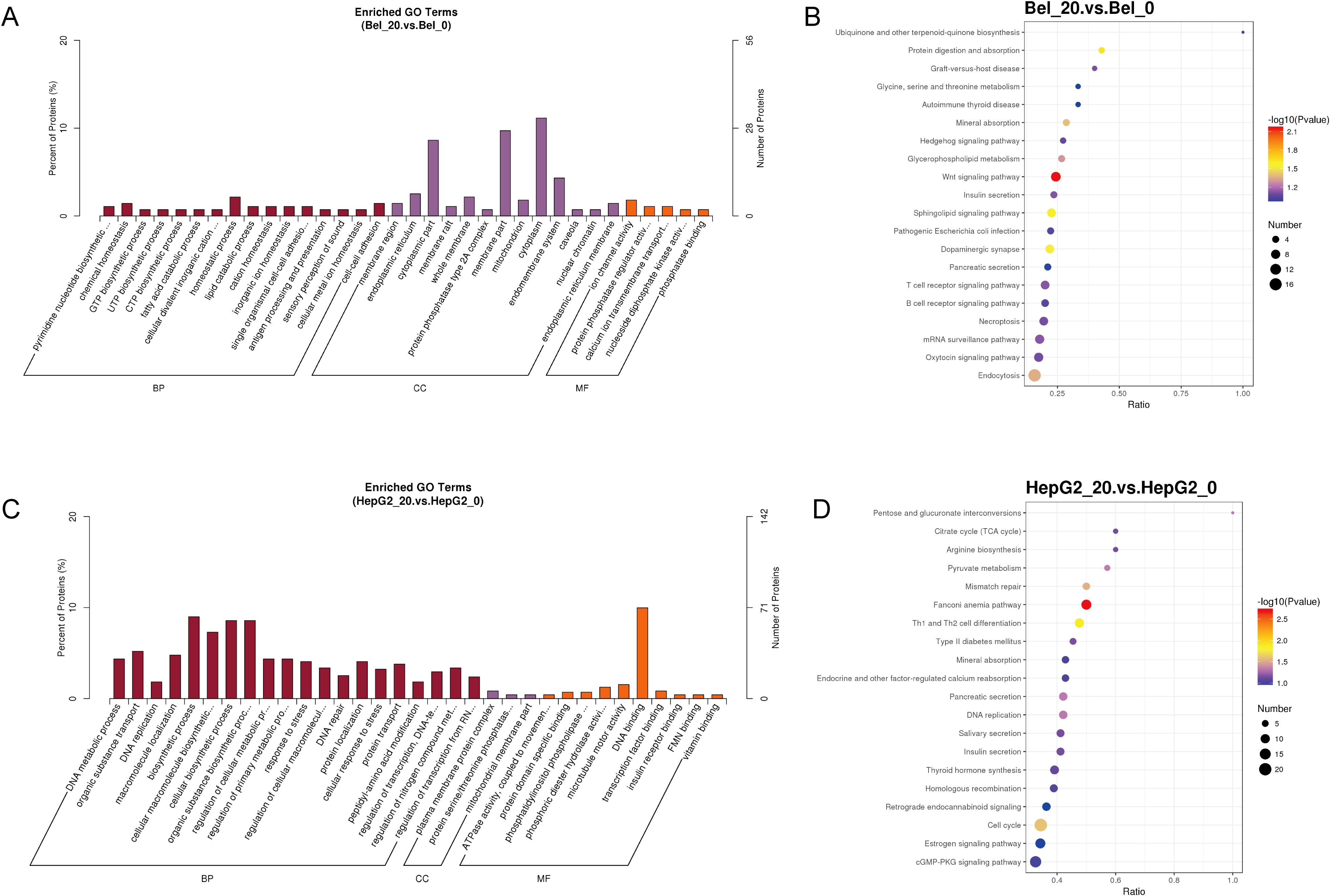
Figure 3. Gene ontology analysis of phosphoproteomics. The Enriched GO Terms and KEGG pathway analyses in Bel-7402 (A, B) and HepG2 (C, D) cell lines.
As for HepG2 cells, the top 5 enriched terms analyzed by GO were DNA metabolic process, organic substance transport, DNA replication, macromolecule localization and biosynthetic process in BP; plasma membrane protein complex, protein serine/threonine phosphatase complex, mitochondrial membrane part, clathrin coat of trans-Golgi network vesicle, clathrin coat of coated pit in CC; and ATPase activity, protein domain specific binding, phosphatidylinositol phospholipase C activity, phosphoric diester hydrolase activity and microtubule motor activity in MF (Figure 3C). Moreover, the KEGG pathway analysis of HepG2 cells suggested Pentose and glucuronate interconversions, Citrate cycle (TCA cycle), Arginine biosynthesis, Pyruvate metabolism and mismatch repair, suggested a primary alternation of biosynthesis and metabolism regulation in HepG2_0 and HepG2_20, similarly to the GO data in Bel-7402 cells (Figure 3D).
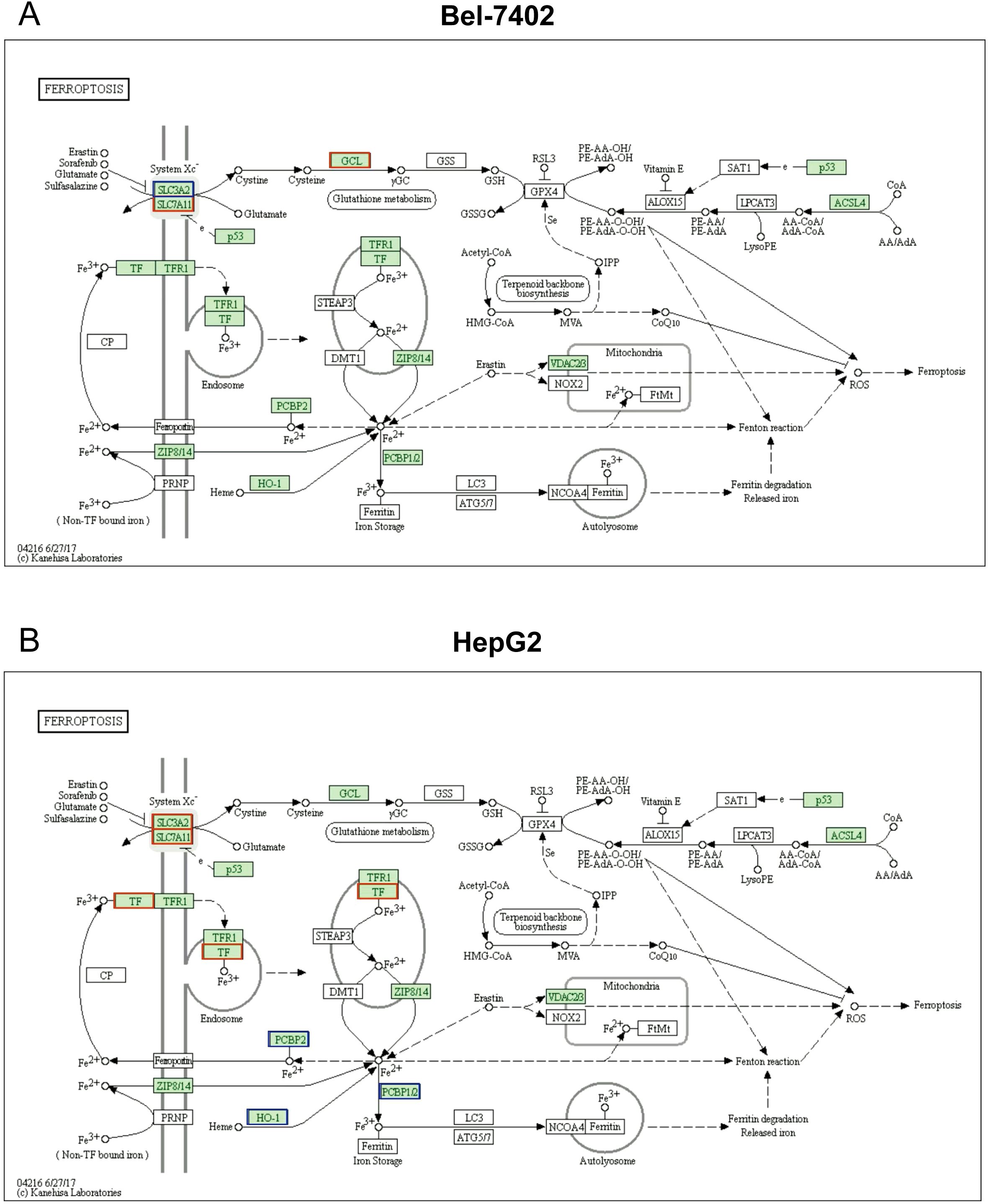
3.4 Ferroptosis pathway analysis based on KEGG in two cell lines
Notably, KEGG analysis revealed that differentially expressed protein enriched in ferroptosis pathway, as well. Furthermore, several studies shown that ferroptosis is closely interconnected with various molecular pathways and cellular processes, including immunological signaling, transcription factors, other cell death modalities, and metabolic pathways, which were all mentioned in our phosphoproteomics results above (Figure 3). This complex network of interactions highlights that ferroptosis is a key molecular process involved in the Metformin inhibitory effect on hepatocellular carcinoma (22–24).
As represented in Figure 4, the downregulation of SLC3A2, and the upregulations of SLC7A11 and GCL signals were found to participate in the ferroptosis process, these proteins were also found to be a significant difference between Bel_0 and Bel_20 groups. Consistently, several DEPs related to ferroptosis were also determined in HepG2_0 and HepG2_20, such as the overexpression of SLC3A2, SLC7A11, TF, and downregulation of PCBP2 and HO-1.
3.5 The role of ferroptosis in metformin-mediated inhibition of hepatocellular carcinoma
MTT assay demonstrated that metformin could significantly suppress the cell viability of Bel-7402, while its inhibitory role could be partly reversed by ferrostatin-1 (all p<0.05) (Figure 5A), also known as Fer-1, a potent and selective inhibitor of ferroptosis. In line with Bel-7402 cells, there is a dramatic difference between Fer-1 and Metformin treatment groups in HepG2 cells (p<0.05), and the suppressive impact of Metformin could be partly eliminated by Fer-1 (p<0.05), as shown in Figure 5B.
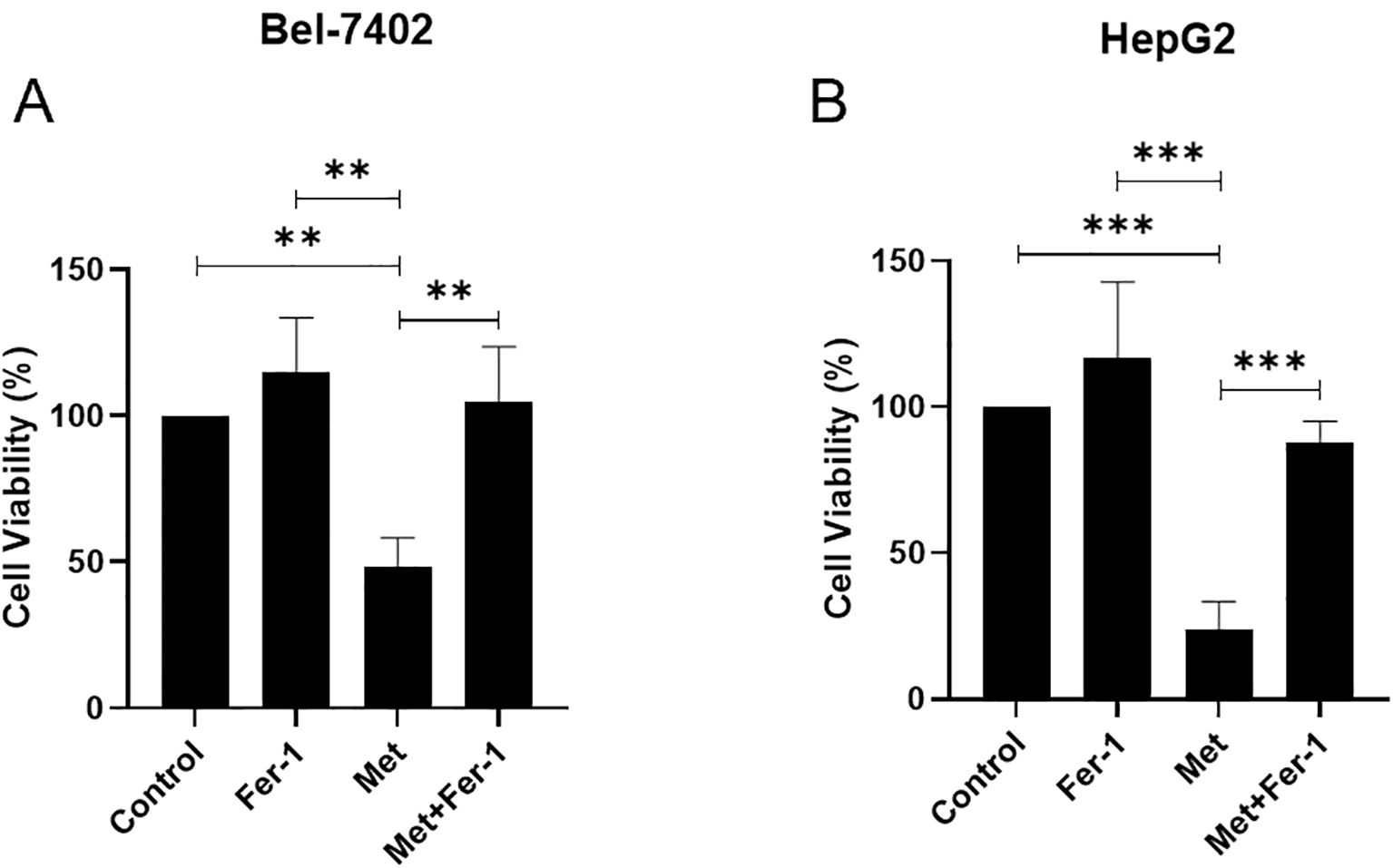
Figure 5. The cell viability is affected by Metformin through ferroptosis in Bel-7402 (A) and HepG2 (B) cell lines. Fer-1, ferrostatin-1; Met, Metformin. P<0.01(**), P<0.001 (***).
3.6 The ferroptosis and autophagy-related protein expressions affected by metformin
Based on the partially reversed MTT results and the fact that ferroptosis closely interacts with autophagy (24), WB was performed to detect the ferroptosis and Autophagy-related protein expressions in HepG2 and Bel-7402 cells. The expression levels in HepG2 were shown in Figures 6A, C, the data showed that the Autophagy-related proteins including ATG9, ATG5, P62 were decreased in Metformin group, and could be recused by Fer-1, while ATG16 and Ic3b did not show an obvious rescue effect after Fer-1 intervention in Metformin-treated HepG2 cells. The ferroptosis proteins such as SLC7A and GPX4 showed a significant inhibition after Metformin treatment, and could be upregulated after Fer-1 intervention. No significant change was noticed in ASCL4 between Metformin and Metformin+Fer-1 groups.
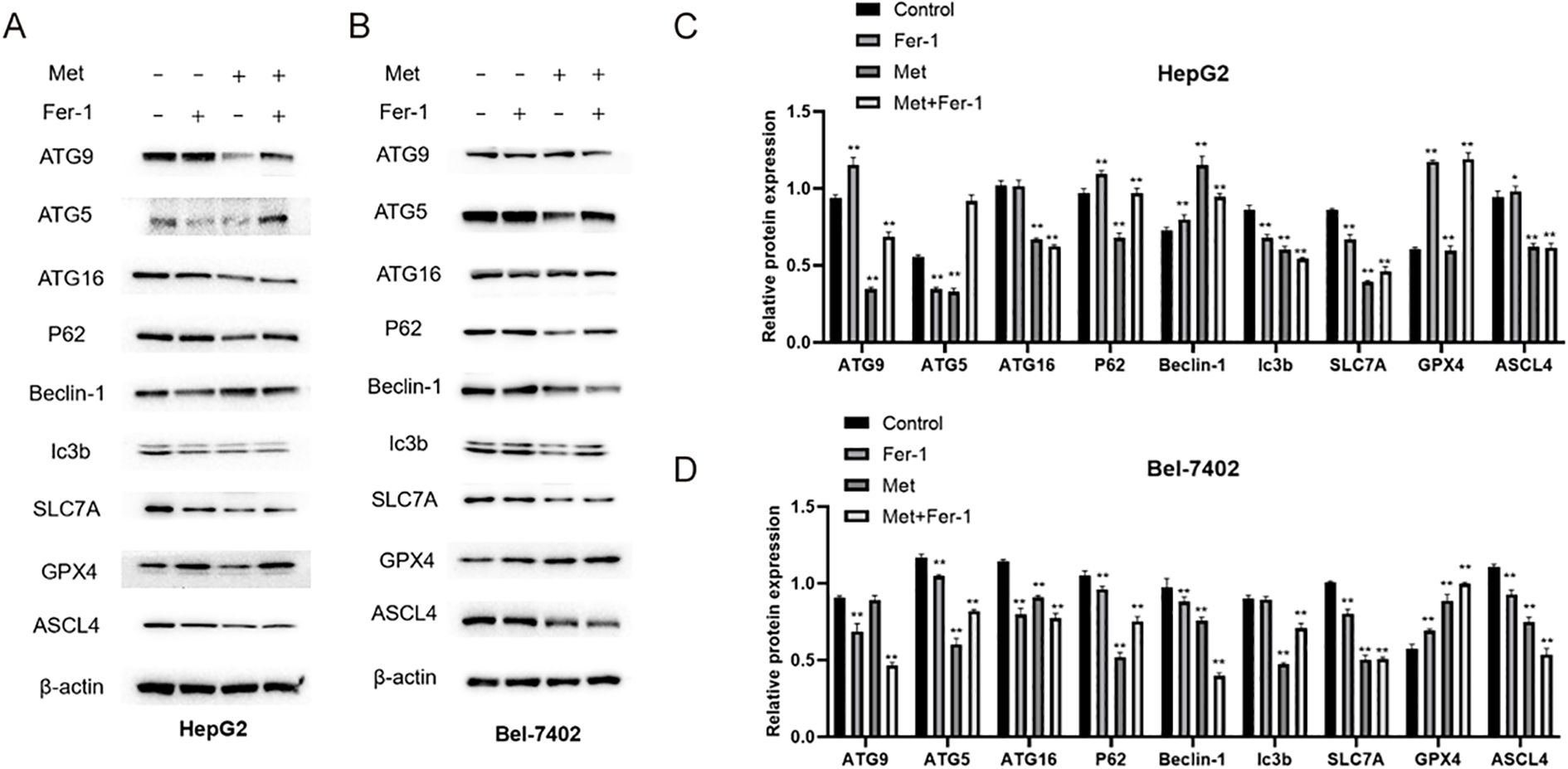
Figure 6. The protein expressions of ferroptosis and Autophagy-related protein detected by WB in HepG2 (A, C) and Bel-7402 (B, D) cell lines. Fer-1, ferrostatin-1; Met, Metformin. Statistical analysis was performed using one-way ANOVA followed by Tukey’s post hoc test. P< 0.05 (*) and P< 0.01 (**) indicate statistically significant differences compared to the 0 mM (control) group.
As for Bel-7402 cell line, its expression results were shown in Figures 6B, D, the protein expressions of ATG5, P62, Ic3b were downregulated in Metformin group, and were rescued by Fer-1 treatment. However, ATG9 and ATG16 showed opposite results that the Metformin could elevate their expression whereas this effect could be partly reversed by Fer-1 intervention. Intriguingly, ferroptosis-relevant proteins including SLC7A, GPX4 and ASCL4 showed different tendencies in Bel-7402 cells, indicating an intrinsic interaction of the ferroptosis process.
4 Discussion
Phosphoproteomics is a powerful approach for the identification and quantitation of phosphorylation sites at the system level, paving the way toward deeper understanding of the regulatory mechanisms underlying cancers (25, 26). Importantly, the current study employed phosphoproteomics approach in combination with bioinformatics analysis and in vitro studies and revealed the underlying mechanisms by which metformin acts in HCC. Metformin treatment decelerated the proliferation of HCC cells via ferroptosis induction, consequently suppressing the progression of HCC.
Several studies have shown that metformin acts as a therapeutic drug for the treatment of HCC as it can regulate biological functions of cancer cells, including proliferation, migration, invasion, angiogenesis, colony formation, apoptosis, and autophagy (27–29). Here, in this study, we adopted metformin treatment for in vitro assay and demonstrated that metformin could dramatically impede the proliferation in HCC cells in a dose- and time-dependent manner. This finding is in agreement with a previous study which shows that HCC cells treated with metformin exhibit significantly reduced cell proliferative, migratory and invasive capacities, during which alternative splicing of LGR4 plays a central role (30). Another study has documented that metformin counteracts HCC cell proliferation markedly via increasing cells arrested at the G2/M phase, dependent on the suppressing effect of miR-378 on CDK1 expression (31). Additionally, use of metformin contributes to repression of hepatoma cell proliferation and promotion of cell cycle arrest at the G0/G1 phase in a dose-dependent manner through AMP-activated protein kinase and its upstream kinase LKB1 to elevate p21/Cip1 and p27/Kip1 and decline cyclin D1 (32).
Metformin is believed to exert its anti-cancer effect by both direct cellular and indirect systemic mechanisms of actions; in the direct model, metformin inhibits mitochondrial respiration in cancer cells, downregulates ATP levels, and activates AMPK, triggering inhibition of mTORC1, and ultimately inhibiting cell growth. In the indirect model, metformin enhances insulin sensitivity, and increases the uptake of glucose in the cell, diminishing circulating levels of insulin (an essential factor for cell growth promotion), and thus impairing cell proliferation (12, 33, 34). Notably, subsequent results of this study demonstrated that the ability of metformin to induce ferroptosis may be a mechanism underlying its anti-proliferative effect in HCC cells, based on phosphoproteomics, bioinformatics analysis and in vitro studies. In much accordance to our results, a recent study has documented that metformin can augment the anti-proliferative effect of sorafenib on HCC cells HepG2 and Huh-7 through ferroptosis induction by blocking the p62-Keap1-Nrf2/HO1 signaling pathway (11). In vitro experiments combined with bioinformatics data vindicated that Fer-1 could partially abolish the inhibitory effects of metformin in HCC. To the best of our knowledge, this study is the first to offer evidence in support of this claim.
As a kind of regulated cell death, ferroptosis is directly triggered through three possible mechanisms: denaturation of relevant proteins on the cellular membrane; damage of the integrity of the cellular membrane; and increase of the permeability of the cellular membrane (35, 36). It is well known that ferroptosis is characterized by iron-dependent lipid peroxidation. The occurrence of lipid peroxidation and accumulation of intracellular iron can result in over-production of reactive oxygen species, which causes cellular damage, ultimately leading to cell death and tumor growth inhibition (37, 38). Indeed, there is increasing evidence that the induction of ferroptosis is a promising therapeutic option for HCC therapy due to its abrogating role in the growth and proliferation of HCC cells (15, 39, 40). GPX4 and SLC7A11 are important ferroptosis markers; downregulation of their expression can sensitize cells to ferroptosis (14, 41). In the present study, SLC7A11 and GPX4 expression showed a significant drop in HCC cells after metformin treatment, while this drop could be annulled by Fer-1 intervention. These results are supported by a previous report by Deng et al. (13). In light of these results, it can be plausible that metformin may be a potential target for ferroptosis-mediated HCC treatment.
Moreover, emerging evidence suggests that metformin may also influence ferroptosis indirectly through the autophagy pathway. Metformin activates AMPK, which inhibits the mTOR pathway and promotes autophagy (42, 43). Autophagy, particularly ferritinophagy—a selective degradation of ferritin—can increase intracellular labile iron levels and promote lipid peroxidation, thereby enhancing ferroptosis (44, 45). In support of this, recent studies in HCC have shown that agents activating AMPK, such as nicotinamide mononucleotide (NMN), induce both autophagy and ferroptosis via phosphorylation-mediated signaling cascades, resulting in tumor suppression (46).
Based on these findings, we propose that metformin may exert its ferroptosis-inducing effect not only through direct modulation of ferroptosis-related proteins such as SLC7A11 and GPX4, but also through autophagy-regulated iron and lipid metabolism pathways. This dual regulatory mechanism may contribute to its anti-proliferative efficacy in HCC. Further studies are needed to validate this hypothesis using autophagy inhibition or AMPK/mTOR modulation models (47–53).
In conclusion, based on phosphoproteomics, bioinformatics analysis and in vitro studies, the current research validated the mechanism by which metformin regulated the proliferation of HCC cells. These findings may provide valuable insights into the pathogenesis and therapeutic target of HCC. However, the molecular mechanism of how metformin affects ferroptosis and the resultant cell proliferation in HCC needs to be clarified by further experimental studies. Moreover, the potential of metformin-mediated modulation of autophagy warrants further investigation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author contributions
JS: Conceptualization, Writing – original draft. XY: Data curation, Methodology, Writing – original draft. YS: Formal analysis, Methodology, Writing – original draft. MD: Resources, Software, Writing – review & editing. AG: Investigation, Methodology, Supervision, Writing – original draft. CL: Conceptualization, Visualization, Writing – original draft. SM: Formal analysis, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the Ningbo Major Research and Development Plan Project (Grant Nos. 2024Z179 and 2023Z160), the Ningbo Natural Science Foundation (2024J393), and Ningbo Top Medical and Health Research Program (2024020818).
Acknowledgments
The authors would like to express their gratitude to Professor Lina Zhang for her invaluable support and guidance throughout the course of this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1531420/full#supplementary-material
References
1. Vogel A, Meyer T, Sapisochin G, Salem R, and Saborowski A. Hepatocellular carcinoma. Lancet. (2022) 400:1345–62. doi: 10.1016/S0140-6736(22)01200-4
2. Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, and Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. (2019) 16:589–604. doi: 10.1038/s41575-019-0186-y
3. Jee BA, Choi JH, Rhee H, Yoon S, Kwon SM, Nahm JH, et al. Dynamics of genomic, epigenomic, and transcriptomic aberrations during stepwise hepatocarcinogenesis. Cancer Res. (2019) 79:5500–12. doi: 10.1158/0008-5472.CAN-19-0991
4. Jiang X, Stockwell BR, and Conrad M. Ferroptosis: mechanisms, biology and role in disease. Nat Rev Mol Cell Biol. (2021) 22:266–82. doi: 10.1038/s41580-020-00324-8
5. Tang B, Zhu J, Wang Y, Chen W, Fang S, Mao W, et al. Targeted xCT-mediated Ferroptosis and Protumoral Polarization of Macrophages Is Effective against HCC and Enhances the Efficacy of the Anti-PD-1/L1 Response. Adv Sci (Weinh). (2023) 10:e2203973. doi: 10.1002/advs.202203973
6. Ajoolabady A, Tang D, Kroemer G, and Ren J. Ferroptosis in hepatocellular carcinoma: mechanisms and targeted therapy. Br J Cancer. (2023) 128:190–205. doi: 10.1038/s41416-022-01998-x
7. LaMoia TE and Shulman GI. Cellular and molecular mechanisms of metformin action. Endocr Rev. (2021) 42:77–96. doi: 10.1210/endrev/bnaa023
8. Wang K, Zhang K, Zhang X, Chen D, and Jiang S. Recent insights of metformin on hepatocellular carcinoma (HCC). Mini Rev Med Chem. (2023) 23:1154–66. doi: 10.2174/1389557522666220623150717
9. Ferretti AC, Hidalgo F, Tonucci FM, Almada E, Pariani A, Larocca MC, et al. Metformin and glucose starvation decrease the migratory ability of hepatocellular carcinoma cells: targeting AMPK activation to control migration. Sci Rep. (2019) 9:2815. doi: 10.1038/s41598-019-39556-w
10. Zhao D, Xia L, Geng W, Xu D, Zhong C, Zhang J, et al. Metformin suppresses interleukin-22 induced hepatocellular carcinoma by upregulating Hippo signaling pathway. J Gastroenterol Hepatol. (2021) 36:3469–76. doi: 10.1111/jgh.v36.12
11. Tang K, Chen Q, Liu Y, Wang L, and Lu W. Combination of metformin and sorafenib induces ferroptosis of hepatocellular carcinoma through p62-Keap1-Nrf2 pathway. J Cancer. (2022) 13:3234–43. doi: 10.7150/jca.76618
12. Hua Y, Zheng Y, Yao Y, Jia R, Ge S, and Zhuang A. Metformin and cancer hallmarks: shedding new lights on therapeutic repurposing. J Transl Med. (2023) 21:403. doi: 10.1186/s12967-023-04263-8
13. Deng C, Xiong L, Chen Y, Wu K, and Wu J. Metformin induces ferroptosis through the Nrf2/HO-1 signaling in lung cancer. BMC Pulm Med. (2023) 23:360. doi: 10.1186/s12890-023-02655-6
14. Zeng C, Lin J, Zhang K, Ou H, Shen K, Liu Q, et al. SHARPIN promotes cell proliferation of cholangiocarcinoma and inhibits ferroptosis via p53/SLC7A11/GPX4 signaling. Cancer Sci. (2022) 113:3766–75. doi: 10.1111/cas.v113.11
15. Hu G, Huang X, Zhang B, Gao P, Wu W, and Wang J. Identify an innovative ferroptosis-related gene in hepatocellular carcinoma. J Clin Lab Anal. (2022) 36:e24632. doi: 10.1002/jcla.24632
16. Hunter T. A journey from phosphotyrosine to phosphohistidine and beyond. Mol Cell. (2022) 82:2190–200. doi: 10.1016/j.molcel.2022.05.007
17. Zittlau K, Nashier P, Cavarischia-Rega C, Macek B, Spat P, and Nalpas N. Recent progress in quantitative phosphoproteomics. Expert Rev Proteomics. (2023) 20:469–82. doi: 10.1080/14789450.2023.2295872
18. Zhou H, Albuquerque CP, Liang J, Suhandynata RT, and Weng S. Quantitative phosphoproteomics: New technologies and applications in the DNA damage response. Cell Cycle. (2010) 9:3479–84. doi: 10.4161/cc.9.17.13152
19. Abe Y, Hirano H, Shoji H, Tada A, Isoyama J, Kakudo A, et al. Comprehensive characterization of the phosphoproteome of gastric cancer from endoscopic biopsy specimens. Theranostics. (2020) 10:2115–29. doi: 10.7150/thno.37623
20. Qi Y, Zhang X, Seyoum B, Msallaty Z, Mallisho A, Caruso M, et al. Kinome profiling reveals abnormal activity of kinases in skeletal muscle from adults with obesity and insulin resistance. J Clin Endocrinol Metab. (2020) 105:644–59. doi: 10.1210/clinem/dgz115
21. Li S, Zhou C, Zhu Y, Chao Z, Sheng Z, Zhang Y, et al. Ferrostatin-1 alleviates angiotensin II (Ang II)- induced inflammation and ferroptosis in astrocytes. Int Immunopharmacol. (2021) 90:107179. doi: 10.1016/j.intimp.2020.107179
22. Zhang X, Hu Y, Wang B, and Yang S. Ferroptosis: Iron-mediated cell death linked to disease pathogenesis. J BioMed Res. (2024) 38:1–23. doi: 10.7555/JBR.38.20240172
23. Li M, Jin S, Zhu X, Xu J, Cao Y, and Piao H. The role of ferroptosis in central nervous system damage diseases. PeerJ. (2024) 12:e16741. doi: 10.7717/peerj.16741
24. Rabitha R, Shivani S, Showket Y, and Sudhandiran G. Ferroptosis regulates key signaling pathways in gastrointestinal tumors: Underlying mechanisms and therapeutic strategies. World J Gastroenterol. (2023) 29:2433–51. doi: 10.3748/wjg.v29.i16.2433
25. Jiang Y, Sun A, Zhao Y, Ying W, Sun H, Yang X, et al. Proteomics identifies new therapeutic targets of early-stage hepatocellular carcinoma. Nature. (2019) 567:257–61. doi: 10.1038/s41586-019-0987-8
26. Li H and Guan Y. Machine learning empowers phosphoproteome prediction in cancers. Bioinformatics. (2020) 36:859–64. doi: 10.1093/bioinformatics/btz639
27. Abd El-Fattah EE and Zakaria AY. Metformin modulate immune fitness in hepatocellular carcinoma: Molecular and cellular approach. Int Immunopharmacol. (2022) 109:108889. doi: 10.1016/j.intimp.2022.108889
28. Abdelhamid AM, Saber S, Youssef ME, Gaafar AGA, Eissa H, Abd-Eldayem MA, et al. Empagliflozin adjunct with metformin for the inhibition of hepatocellular carcinoma progression: Emerging approach for new application. BioMed Pharmacother. (2022) 145:112455. doi: 10.1016/j.biopha.2021.112455
29. Shen Z, Zhou H, Li A, Wu T, Ji X, Guo L, et al. Metformin inhibits hepatocellular carcinoma development by inducing apoptosis and pyroptosis through regulating FOXO3. Aging (Albany NY). (2021) 13:22120–33. doi: 10.18632/aging.203464
30. Zhuo H, Miao S, Jin Z, Zhu D, Xu Z, Sun D, et al. Metformin suppresses hepatocellular carcinoma through regulating alternative splicing of LGR4. J Oncol. (2022) 2022:1774095. doi: 10.1155/2022/1774095
31. Zhou J, Han S, Qian W, Gu Y, Li X, and Yang K. Metformin induces miR-378 to downregulate the CDK1, leading to suppression of cell proliferation in hepatocellular carcinoma. Onco Targets Ther. (2018) 11:4451–9. doi: 10.2147/OTT.S167614
32. Chen HP, Shieh JJ, Chang CC, Chen TT, Lin JT, Wu MS, et al. Metformin decreases hepatocellular carcinoma risk in a dose-dependent manner: population-based and in vitro studies. Gut. (2013) 62:606–15. doi: 10.1136/gutjnl-2011-301708
33. Pernicova I and Korbonits M. Metformin–mode of action and clinical implications for diabetes and cancer. Nat Rev Endocrinol. (2014) 10:143–56. doi: 10.1038/nrendo.2013.256
34. Soliman PT, Zhang Q, Broaddus RR, Westin SN, Iglesias D, Munsell MF, et al. Prospective evaluation of the molecular effects of metformin on the endometrium in women with newly diagnosed endometrial cancer: A window of opportunity study. Gynecol Oncol. (2016) 143:466–71. doi: 10.1016/j.ygyno.2016.10.011
35. Cong T, Luo Y, Fu Y, Liu Y, Li Y, and Li X. New perspectives on ferroptosis and its role in hepatocellular carcinoma. Chin Med J (Engl). (2022) 135:2157–66. doi: 10.1097/CM9.0000000000002327
36. Liao H, Shi J, Wen K, Lin J, Liu Q, Shi B, et al. Molecular targets of ferroptosis in hepatocellular carcinoma. J Hepatocell Carcinoma. (2021) 8:985–96. doi: 10.2147/JHC.S325593
37. Fu B, Shao R, Wang H, Chen G, Bai S, and Wang H. Integrated assessment of the clinical and biological value of ferroptosis-related genes in multiple myeloma. Cancer Cell Int. (2022) 22:326. doi: 10.1186/s12935-022-02742-4
39. Jiang Y, Hui D, Pan Z, Yu Y, Liu L, Yu X, et al. Curcumin promotes ferroptosis in hepatocellular carcinoma via upregulation of ACSL4. J Cancer Res Clin Oncol. (2024) 150:429. doi: 10.1007/s00432-024-05878-0
40. Yuan Z, Liu T, Huo X, Wang H, Wang J, and Xue L. Glutamine transporter SLC1A5 regulates ionizing radiation-derived oxidative damage and ferroptosis. Oxid Med Cell Longev. (2022) 2022:3403009. doi: 10.1155/2022/3403009
41. Chen Q, Zheng W, Guan J, Liu H, Dan Y, Zhu L, et al. SOCS2-enhanced ubiquitination of SLC7A11 promotes ferroptosis and radiosensitization in hepatocellular carcinoma. Cell Death Differ. (2023) 30:137–51. doi: 10.1038/s41418-022-01051-7
42. Zhang CS, Li M, Ma T, Zong Y, Cui J, Feng JW, et al. Metformin activates AMPK through the lysosomal pathway. Cell Metab. (2016) 24:521–2. doi: 10.1016/j.cmet.2016.09.003
43. Kalender A, Selvaraj A, Kim SY, Gulati P, Brule S, Viollet B, et al. Metformin, independent of AMPK, inhibits mTORC1 in a rag GTPase-dependent manner. Cell Metab. (2010) 11:390–401. doi: 10.1016/j.cmet.2010.03.014
44. Gao M, Monian P, Pan Q, Zhang W, Xiang J, and Jiang X. Ferroptosis is an autophagic cell death process. Cell Res. (2016) 26:1021–32. doi: 10.1038/cr.2016.95
45. Hou W, Xie Y, Song X, Sun X, Lotze MT, Zeh HJ 3rd, et al. Autophagy promotes ferroptosis by degradation of ferritin. Autophagy. (2016) 12:1425–8. doi: 10.1080/15548627.2016.1187366
46. Sun Z, Liu L, Liang H, and Zhang L. Nicotinamide mononucleotide induces autophagy and ferroptosis via AMPK/mTOR pathway in hepatocellular carcinoma. Mol Carcinog. (2024) 63:577–88. doi: 10.1002/mc.23673
47. de Oliveira S, Houseright RA, Graves AL, Golenberg N, Korte BG, Miskolci V, et al. Metformin modulates innate immune-mediated inflammation and early progression of NAFLD-associated hepatocellular carcinoma in zebrafish. J Hepatol. (2019) 70:710–21. doi: 10.1016/j.jhep.2018.11.034
48. Dutta S, Shah RB, Singhal S, Dutta SB, Bansal S, Sinha S, et al. Metformin: A review of potential mechanism and therapeutic utility beyond diabetes. Drug Des Devel Ther. (2023) 17:1907–32. doi: 10.2147/DDDT.S409373
49. Kamarudin MNA, Sarker MMR, Zhou JR, and Parhar I. Metformin in colorectal cancer: molecular mechanism, preclinical and clinical aspects. J Exp Clin Cancer Res. (2019) 38:491. doi: 10.1186/s13046-019-1495-2
50. Lv Z and Guo Y. Metformin and its benefits for various diseases. Front Endocrinol (Lausanne). (2020) 11:191. doi: 10.3389/fendo.2020.00191
51. Seok SH. Structural insights into protein regulation by phosphorylation and substrate recognition of protein kinases/phosphatases. Life (Basel). (2021) 11. doi: 10.3390/life11090957
52. Tseng HH, Chen YZ, Chou NH, Chen YC, Wu CC, Liu LF, et al. Metformin inhibits gastric cancer cell proliferation by regulation of a novel Loc100506691-CHAC1 axis. Mol Ther Oncolytics. (2021) 22:180–94. doi: 10.1016/j.omto.2021.08.006
Keywords: metformin, hepatocellular carcinoma, ferroptosis, phosphoproteomics, cell viability
Citation: Sun J, Yu X, Shan Y, Dai M, Gaucherot A, Lu C and Mao S (2025) Metformin inhibits the proliferation of hepatocellular carcinoma cells through inducing ferroptosis analyzed by phosphoproteomics. Front. Oncol. 15:1531420. doi: 10.3389/fonc.2025.1531420
Received: 20 November 2024; Accepted: 13 May 2025;
Published: 30 May 2025.
Edited by:
Liang Qiao, The University of Sydney, AustraliaReviewed by:
Keith R. Laderoute, Laderoute Consulting, LLC, United StatesQin Li, Shanghai General Hospital, China
Copyright © 2025 Sun, Yu, Shan, Dai, Gaucherot, Lu and Mao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caide Lu, MXkzMTlAMTYzLmNvbQ==; Shuqi Mao, bW1tYW9zaHVxaUAxNjMuY29t
 Jihan Sun
Jihan Sun Xi Yu1
Xi Yu1 Yuying Shan
Yuying Shan Caide Lu
Caide Lu Shuqi Mao
Shuqi Mao