- 1Department of Oncology, The Second People’s Hospital of Quzhou, Quzhou, China
- 2Department of Rehabilitative, The Second People’s Hospital of Quzhou, Quzhou, China
We report a rare case of multiple primary tumors in a 67-year-old male. The patient was treated surgically for a lumbar disc herniation with intraoperative findings of L5 nerve root tumor, and postoperative pathology confirmed a diagnosis of diffuse large B-cell lymphoma (DLBCL). Three months later, the patient was further pathologically diagnosed with prostate cancer. The multidisciplinary treatment team devised a staged therapeutic strategy: firstly, 2 cycles of R-CHOP chemotherapy for DLBCL, followed by local radiotherapy for the residual lesion of lumbar spine tumor, and then 2 cycles of R-MTX-CHOP chemotherapy in sequence; after the DLBCL was controlled, the patient underwent radical prostatectomy, which was followed by adjuvant endocrine therapy and pelvic lymph node radiotherapy. Post-treatment evaluation showed complete remission (CR) in both tumors. After five years of disease-free survival, the patient presented with enlarged cervical lymph nodes in October 2022. A biopsy confirmed DLBCL recurrence. The treatment team administered six cycles of R-GemOx chemotherapy, followed by maintenance therapy with the targeted agent Orelabrutinib. Subsequent assessments confirmed a second CR. In September 2024, a colonoscopy revealed a rectal tumor, which was pathologically diagnosed as rectal cancer. The patient underwent radical surgery, and the pathological staging was determined to be stage I. According to the literature search, this is the first reported case of triple primary malignancies involving DLBCL, prostate cancer and rectal cancer, which provides valuable experience in the clinical diagnosis and treatment of such rare cases.
1 Introduction
Multiple Primary Malignant Tumors (MPMTs) refer to the occurrence of two or more histologically distinct malignant tumors in the same individual, with no evidence of recurrence, metastasis, or local spread between these tumors. Based on the time interval between the diagnosis of the second primary tumor and the first, MPMTs can be classified into simultaneous multiple primary malignancies (SMPMTs) and metachronous multiple primary malignancies (MMPMTs) (1). SMPMTs were defined as second primary tumors diagnosed within 6 months of the diagnosis of the first primary tumor, while MMPMTs were defined as second primary tumors diagnosed more than 6 months after the diagnosis of the first primary tumor (2). This case report describes a rare patient with both SMPMTs and MMPMTs. The patient was initially diagnosed with both DLBCL and prostate cancer and achieved long-term remission through standardized treatment. Approximately seven years later, the patient was diagnosed with rectal cancer, which met the diagnostic criteria for MMPMTs. This case not only exemplifies the complexity of MPMTs but also provides valuable insights into the clinical management of such rare conditions.
2 Case presentation
2.1 Initial visit and diagnosis
A 67-year-old male patient was admitted to the People’s Liberation Army No. 117 Hospital (Hangzhou, China) on December 6, 2016, presenting with “low back pain accompanied by tingling and numbness in the left lower limb persisting for over six months.” The patient had previously been in good health, with an Eastern Cooperative Oncology Group (ECOG) performance status score of 1 and a Numeric Rating Scale (NRS) pain score of 3. He denied systemic symptoms such as weight loss, night sweats, or persistent fever. There were no reported comorbidities, genetic or environmental exposure risk factors, or family history of cancer. Physical examination revealed significant limitation of lumbar movement, tenderness over the L3-L5 spinous processes and paravertebral regions (+), pain on percussion (+), radiating to the left lower limb, and a positive straight leg raising test on the left side (60°). Laboratory tests showed a normal white blood cell count and lymphocyte percentage, with negative results for human immunodeficiency virus (HIV) and Epstein-Barr virus DNA (EBV-DNA) testing. Magnetic resonance imaging (MRI) of the lumbar spine indicated lumbar disc herniation. The initial diagnosis was lumbar degenerative disease accompanied by disc herniation.
2.2 Initial surgery and pathological diagnosis
On December 9, 2016, the patient underwent lumbar decompression and interbody fusion with internal fixation. During the procedure, a tumor was unexpectedly discovered at the L5 nerve root, leading to additional resection of the L5 nerve root tumor. Morphological and immunohistochemical analysis suggested diffuse large B-cell lymphoma (DLBCL), non-germinal center type. The specific immunophenotypic markers included: CD45R0 (−), CD79a (+), CKpan (−), EMA (−), LCA (+), Vimentin (+), Bcl-2 (+), Bcl-6 (−), CD10 (−), CD20 (+), Ki67 (+, 75%), and MUM1 (+). Fluorescence in situ hybridization (FISH) testing was negative for BCL-6, BCL-2, and C-MYC gene rearrangements. Postoperative PET-CT (December 20, 2016) revealed thickening of the left L5 nerve root with a segmental abnormal increase in FDG uptake, indicating residual tumor. Additionally, the prostate appeared abnormally enlarged, necessitating further investigation (Figures 1A, B). The final diagnosis was DLBCL (stage IE, non-germinal center type, IPI score 3, intermediate-high risk).
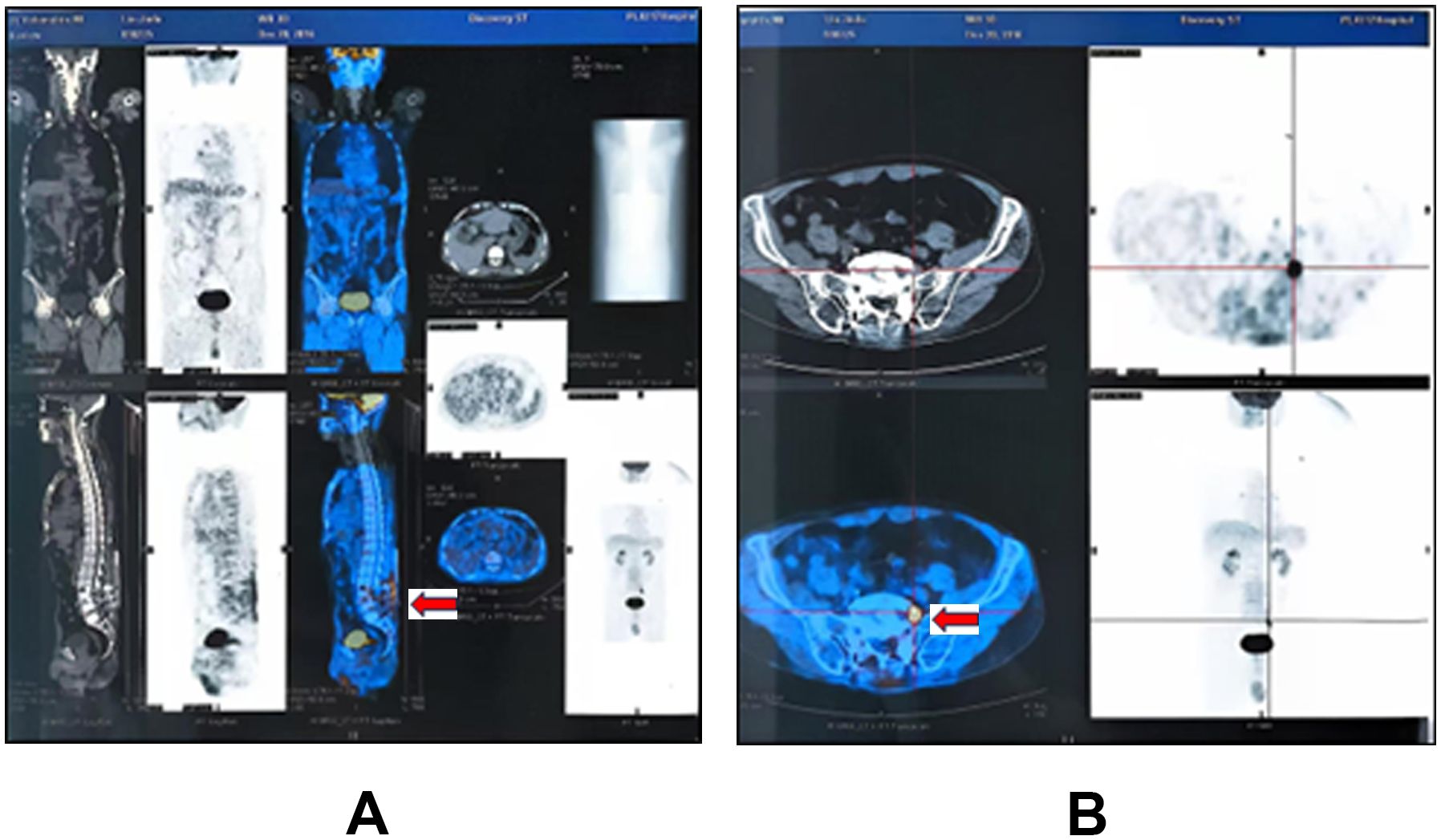
Figure 1. Postoperative PET-CT (December 2016): (A) Sagittal view showing patchy areas of moderately increased radiotracer uptake, with a maximum standardized uptake value (SUVmax) of 4.46 within the soft tissues and bone at the surgical site. (B) Axial view at the L5 level revealing thickening of the left L5 nerve root, more pronounced at the intervertebral foramen exit, with a SUVmax of 12.92.
2.3 Diagnosis of prostate cancer
In March 2017, the patient visited the Second People’s Hospital of Quzhou (Quzhou, China) for prostate-related examinations. Results showed a total prostate-specific antigen (tPSA) level of 12.82 ng/mL, free prostate-specific antigen (fPSA) level of 1.95 ng/mL, and a free-to-total PSA ratio of 0.15. Prostate ultrasound revealed a space-occupying lesion. Prostate needle biopsy confirmed prostate adenocarcinoma with a Gleason score of 3 + 3 = 6. At this time, the patient was diagnosed with SMPMTs: DLBCL and prostate cancer.
2.4 Treatment and remission of DLBCL
On April 7, 2017, after a multidisciplinary team (MDT) discussion, priority was given to treating the more aggressive DLBCL. The patient received 2 cycles of R-CHOP chemotherapy, specifically: rituximab (375mg/m², d0), doxorubicin (50mg/m², d1), vincristine (1.4 mg/m², d1), cyclophosphamide (750 mg/m², d1), and prednisolone (100 mg, d1-5). Subsequently, intensity-modulated radiation therapy (IMRT) (30 Gy/15 F) was administered to the residual lumbar lesion. To consolidate efficacy, the patient received 2 additional cycles of R-MTX-CHOP chemotherapy, specifically: rituximab (375 mg/m², d0), methotrexate (3 g/m², d1), doxorubicin (50 mg/m², d1), vincristine (1.4 mg/m², d1), cyclophosphamide (750 mg/m², d1),and prednisolone (100 mg, d1-5), incorporating high-dose methotrexate. On November 7, 2017, follow-up PET-CT showed complete disappearance of the lumbar residual lesion, indicating complete remission (CR) of DLBCL.
2.5 Treatment and remission of prostate cancer
On December 1, 2017, the patient underwent laparoscopic radical prostatectomy. Postoperative pathology revealed a Gleason score of 3 + 4 = 7, Grade Group 2, with a pathological stage of T3aN0M0, stage IIIB (Figure 2). Postoperatively, the patient received bicalutamide 50 mg orally once daily and triptorelin acetate 3.75 mg intramuscularly for endocrine therapy over 18 months, along with IMRT (55 Gy/25 F) to the pelvic lymph drainage area. On October 23, 2018, follow-up PET-CT confirmed CR of both prostate cancer and DLBCL, marking the transition to regular follow-up.
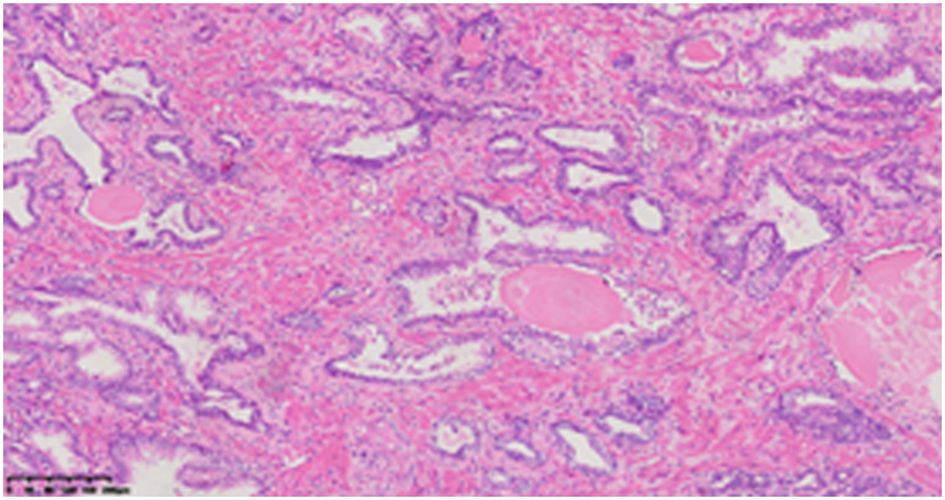
Figure 2. Histopathological examination (HE staining, ×10 magnification): Prostatic Adenocarcinoma (Acinar Type), Gleason Score 3 + 4 = 7: The tumor involves both lobes of the prostate, with perineural invasion and tumor infiltration close to the peripheral surgical margin.
2.6 DLBCL recurrence and treatment
In October 2022 (5 years later), routine follow-up revealed multiple enlarged lymph nodes in the right submandibular, deep cervical group along the medial border of the sternocleidomastoid muscle, and right supraclavicular fossa. PET-CT showed significantly increased FDG uptake, suggesting lymphoma infiltration (Figure 3). A needle biopsy of the cervical lymph nodes (Figure 4) with immunohistochemistry results included: CK (-), CD3 scattered (+), CD20 (+), CD21 (−), Bcl-2 (+), CyclinD1 (−), CD56 (−), CD138 scattered (+), CD10 (−), MUM1 scattered (+), EBER (−), and Ki-67 (+, 60%). These findings confirmed DLBCL recurrence. The patient subsequently received 6 cycles of R-GemOx chemotherapy, specifically: rituximab (375 mg/m², d0), gemitabine (1000 mg/m², d1), and oxaliplatin (100 mg/m², d1). After chemotherapy, orelabrutinib was administered as targeted maintenance therapy.

Figure 3. PET-CT Findings (October 2022): Multiple enlarged lymph nodes were observed in the right submandibular region, along the medial border of the sternocleidomastoid muscle in the deep cervical group, and in the right supraclavicular fossa. The largest node measured approximately 2.7 cm in short-axis diameter, with an average SUVmax of 6.5 and a maximum SUVmax of 7.5. These findings are suggestive of lymphoma infiltration.
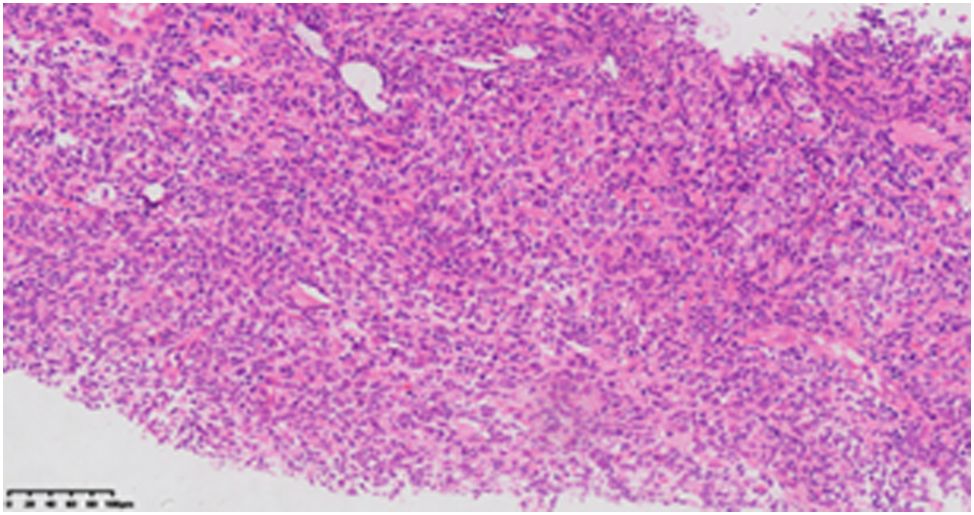
Figure 4. Cervical lymph node biopsy histopathological examination (HE staining, ×10 magnification) reveals diffuse abnormal hyperplastic lesions of lymphoid tissue, suggestive of lymphoma.
2.7 Rectal cancer and treatment
During routine follow-up in September 2024, colonoscopy revealed a rectal lesion, and pathological examination confirmed adenocarcinoma (Figure 5A). The patient subsequently underwent laparoscopic radical rectal surgery. Postoperative pathology indicated moderately differentiated adenocarcinoma, with a pathological stage of pT2N0M0, Stage I (Figure 5B).
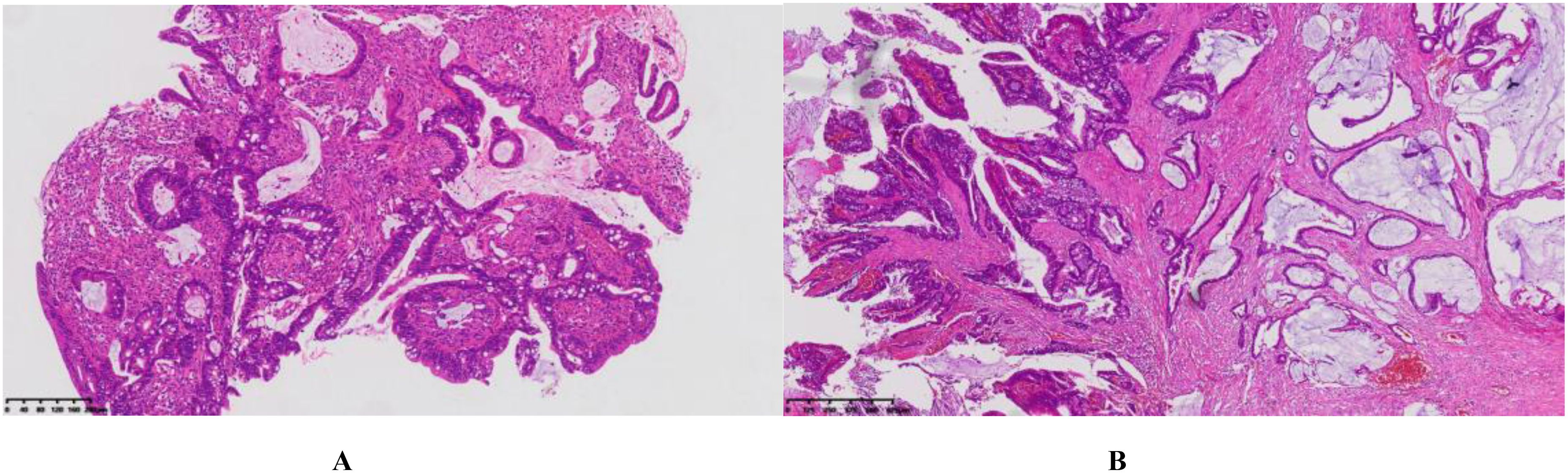
Figure 5. (A) Colonoscopy and histopathological examination (HE staining, ×10 magnification) (B) Postoperative pathological examination (HE staining, ×4 magnification): Moderately differentiated adenocarcinoma with partial mucinous adenocarcinoma. The tumor measures approximately 1.5 cm × 1 cm × 0.5 cm, infiltrates the deep muscular layer, and shows no clear evidence of vascular or perineural invasion.
In October 2024, the PET-CT showed no signs of tumor recurrence or metastasis. The treatment efficacy was assessed as CR. Currently, the patient continues maintenance therapy with orelabrutinib. The patient is in good general condition, with an ECOG performance status score of 1, and maintains a good quality of life.
3 Discussion
The incidence of MPMTs has significantly increased with advancements in cancer diagnosis and treatment, as well as prolonged patient survival. The reported incidence of MPMTs ranges from 0.73% to 11.7% (3). The treatment principles for MPMTs require individualized planning based on the stage, pathological type of each tumor, and the patient’s overall condition. When pathologically confirmed, each tumor should be evaluated and staged independently. Given the potential for confusion between MPMTs and metastatic cancer, multidisciplinary team (MDT) discussions are crucial for challenging cases. Generally, tumors with a greater impact on patient survival or quality of life should be prioritized. We present a representative case of MPMTs, involving the concurrent diagnoses of DLBCL and prostate cancer, followed by a diagnosis of rectal cancer 7 years later. In this case, PET-CT and pathological biopsies were used to establish the diagnosis, and an individualized treatment plan was tailored according to the tumor type and stage.
3.1 Analysis of treatment strategies
The R-CHOP regimen, as a first-line chemotherapy for DLBCL, achieved significant efficacy in this case. Combined with local radiotherapy, the patient achieved a 5-year disease-free remission. Upon relapse, the R-GemOx regimen was employed as second-line therapy, followed by orelabrutinib maintenance treatment.
Orelabrutinib, a second-generation BTK inhibitor, has shown potential clinical efficacy in chronic lymphocytic leukemia (CLL), small lymphocytic lymphoma (SLL), mantle cell lymphoma (MCL), and relapsed or refractory Waldenström macroglobulinemia (4–6). However, its role in DLBCL remains exploratory. Retrospective studies suggest high response rates with orelabrutinib combined with chemotherapy in both untreated and relapsed patients (7, 8). To date, no data exists on orelabrutinib maintenance therapy in DLBCL. The successful treatment of this patient provides valuable insights into its potential application in DLBCL maintenance.
3.2 Analysis of potential factors in MPMTs
3.2.1 Genetic factors
Genetic factors play a central role in MPMTs. Known hereditary cancer syndromes, such as Lynch Syndrome, BRCA1/2 mutations, and TP53 mutations, are closely associated with the development of multiple malignancies (9–11). Lynch Syndrome, which is caused by mutations in DNA mismatch repair genes (e.g., MLH1, MSH2, MSH6, PMS2), significantly increases the risk of colorectal, endometrial, and other cancers. Similarly, BRCA1/2 mutations are linked not only to breast and ovarian cancers but also to prostate and pancreatic cancers (11–13). Although comprehensive genetic testing was not performed in this case, the sequential diagnoses of DLBCL, prostate cancer, and rectal cancer suggest the possibility of an unrecognized hereditary cancer syndrome. Therefore, comprehensive genetic testing and family history investigation are recommended for patients with MPMTs to identify potential hereditary etiologies.
3.2.2 Immune system and tumor microenvironment
The immune system plays a critical role in cancer development and progression. Chronic inflammation and immunosuppression may promote tumorigenesis, while abnormal immune activation can impair immune surveillance, increasing cancer risk (14). Immune cells in the tumor microenvironment play a key role in cancer development and progression (15). For instance, M1/M2 macrophage polarization and tumor-associated macrophages (TAMs) promote tumor growth through cell proliferation, immune suppression, and angiogenesis (16). The initial diagnosis of DLBCL in this patient indicates B-cell dysfunction, which may have contributed to the development of other tumors due to immune dysregulation. Therefore, immune system assessment and modulation are essential in MPMTs management.
3.2.3 Treatment-related factors
Radiotherapy and chemotherapy, as primary cancer treatments, increase the risk of secondary primary malignancies through various mechanisms due to their long-term side effects (17, 18). Studies show a significantly elevated risk of rectal cancer in patients who received radiotherapy (OR: 1.45, 95% CI: 1.07-1.97, P = 0.02) (19), consistent with this case. Certain chemotherapeutic agents (e.g., alkylating agents, anthracyclines) may also increase secondary tumor risk through DNA damage or immune suppression (20). Thus, treatment plans should balance therapeutic benefits with long-term risks to minimize MPMTs occurrence.
3.2.4 Environmental and lifestyle factors
Chronic exposure to carcinogens (e.g., tobacco, alcohol, chemical pollutants) and unhealthy lifestyle habits (e.g., high-fat diet, physical inactivity) may increase the risk of multiple cancers (21, 22). For example, smoking is associated with lung cancer and may also elevate the risk of bladder and pancreatic cancers (23). For MPMTs patients, a detailed investigation of lifestyle and occupational exposures is necessary.
4 Conclusion
We report a case of MPMTs involving concurrent DLBCL and prostate cancer, with a subsequent diagnosis of rectal cancer 7 years later. The patient achieved complete remission at all stages following systematic treatment. The successful use of orelabrutinib in DLBCL maintenance therapy provides valuable insights for future research. The occurrence of MPMTs may be related to genetic factors, immune dysfunction, long-term side effects of radiotherapy and chemotherapy, as well as environmental and lifestyle factors. For patients with MPMTs, comprehensive genetic testing and family history investigation are crucial, and optimizing treatment strategies is essential for reducing the risk of secondary tumors. Furthermore, enhanced long-term follow-up and preventive measures are essential.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by ethics committee of the Second People’s Hospital of Quzhou. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HQ: Project administration, Validation, Writing – review & editing. YZ: Formal Analysis, Methodology, Writing – review & editing. XZ: Conceptualization, Data curation, Formal Analysis, Writing – original draft. SZ: Software, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank the patient for his cooperation and support for academic communication, and thank the department of pathology for providing diagnostic support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhai C, Cai Y, Lou F, Liu Z, Xie J, Zhou X, et al. Multiple primary Malignant tumors - A clinical analysis of 15,321 patients with Malignancies at a single center in China. J Cancer. (2018) 9:2795–801. doi: 10.7150/jca.25482
2. Moertel CG, Dockerty MB, and Baggenstoss AH. Multiple primary Malignant neoplasms. I. Introduction and presentation of data. Cancer. (1961) 14:221–30. doi: 10.1002/1097-0142(196103/04)14:2<221::AID-CNCR2820140202>3.0.CO;2-6
3. Demandante CG, Troyer DA, and Miles TP. Multiple primary Malignant neoplasms: case report and a comprehensive review of the literature. Am J Clin Oncol. (2003) 26:79–83. doi: 10.1097/00000421-200302000-00015
4. Cao XX, Jin J, Fu CC, Yi SH, Zhao WL, Sun ZM, et al. Evaluation of orelabrutinib monotherapy in patients with relapsed or refractory Waldenstrom’s macroglobulinemia in a single-arm, multicenter, open-label, phase 2 study. EClinicalMedicine. (2022) 52:101682. doi: 10.1016/j.eclinm.2022.101682
5. Dhillon S. Orelabrutinib: first approval. Drugs. (2021) 81:503–7. doi: 10.1007/s40265-021-01482-5
6. Xu W, Zhou K, Wang T, Yang S, Liu L, Hu Y, et al. Orelabrutinib in relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma patients: Multi-center, single-arm, open-label, phase 2 study. Am J Hematol. (2023) 98:571–9. doi: 10.1002/ajh.26826
7. Wei R, Wu Y, Jiang S, Zhang A, Zhang L, Liu L, et al. Efficacy and safety of Orelabrutinib-based regimens in diffuse large B-cell lymphoma: a single-center retrospective analysis. Clin Exp Med. (2023) 23:4609–21. doi: 10.1007/s10238-023-01231-w
8. Yin H, Hua W, Shen HR, Wu JZ, Li Y, Wang L, et al. Efficacy and safety analysis of the OR-CHOP regimen for the treatment of MCD subtype diffuse large B cell lymphoma in the real-world setting. Zhonghua Xue Ye Xue Za Zhi. (2024) 45:827–31. doi: 10.3760/cma.j.cn121090-20240607-00212
9. Shiseki M, Nishikawa R, Yamamoto H, Ochiai A, Sugimura H, Shitara N, et al. Germ-line p53 mutation is uncommon in patients with triple primary cancers. Cancer Lett. (1993) 73:51–7. doi: 10.1016/0304-3835(93)90187-e
10. Hampel H, Frankel W, Panescu J, Lockman J, Sotamaa K, Fix D, et al. Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients. Cancer Res. (2006) 66:7810–7. doi: 10.1158/0008-5472.CAN-06-1114
11. Petrucelli N, Daly MB, and Pal T. BRCA1- and BRCA2-Associated Hereditary Breast and Ovarian Cancer. [Review; Book Chapter]. Seattle (WA): University of Washington, Seattle: GeneReviews® [Internet]. (1993).
12. Peltomaki P, Nystrom M, Mecklin JP, and Seppala TT. Lynch syndrome genetics and clinical implications. Gastroenterology. (2023) 164:783–99. doi: 10.1053/j.gastro.2022.08.058
13. Cheng HH, Shevach JW, Castro E, Couch FJ, Domchek SM, Eeles RA, et al. BRCA1, BRCA2, and associated cancer risks and management for male patients: A review. JAMA Oncol. (2024) 10:1272–81. doi: 10.1001/jamaoncol.2024.2185
14. Ostrand-Rosenberg S. Immune surveillance: a balance between protumor and antitumor immunity. Curr Opin Genet Dev. (2008) 18:11–8. doi: 10.1016/j.gde.2007.12.007
15. Barbosa AM, Gomes-Goncalves A, Castro AG, and Torrado E. Immune system efficiency in cancer and the microbiota influence. Pathobiology. (2021) 88:170–86. doi: 10.1159/000512326
16. Boutilier AJ and Elsawa SF. Macrophage polarization states in the tumor microenvironment. Int J Mol Sci. (2021) 22(13):6995. doi: 10.3390/ijms22136995
17. Berrington DGA, Curtis RE, Kry SF, Gilbert E, Lamart S, Berg CD, et al. Proportion of second cancers attributable to radiotherapy treatment in adults: a cohort study in the US SEER cancer registries. Lancet Oncol. (2011) 12:353–60. doi: 10.1016/S1470-2045(11)70061-4
18. Travis LB, Ng AK, Allan JM, Pui CH, Kennedy AR, Xu XG, et al. Second Malignant neoplasms and cardiovascular disease following radiotherapy. Health Phys. (2014) 106:229–46. doi: 10.1097/HP.0000000000000013
19. Nugent TS, Low EZ, Fahy MR, Donlon NE, McCormick PH, Mehigan BJ, et al. Prostate radiotherapy and the risk of secondary rectal cancer-a meta-analysis. Int J Colorectal Dis. (2022) 37:437–47. doi: 10.1007/s00384-021-04075-6
20. Spratt JJ and Hoag MG. Incidence of multiple primary cancers per man-year of follow up: 20-year review from the Ellis Fischel State Cancer Hospital. Ann Surg. (1966) 164:775–84. doi: 10.1097/00000658-196611000-00001
21. Yamamoto S, Yoshimura K, Ri S, Fujita S, Akasu T, and Moriya Y. The risk of multiple primary Malignancies with colorectal carcinoma. Dis Colon Rectum. (2006) 49:S30–6. doi: 10.1007/s10350-006-0600-8
22. Gallagher RP, Bajdik CD, Fincham S, Hill GB, Keefe AR, Coldman A, et al. Chemical exposures, medical history, and risk of squamous and basal cell carcinoma of the skin. Cancer Epidemiol Biomarkers Prev. (1996) 5:419–24.
Keywords: multiple primary malignant tumors, DLBCL, prostate cancer, rectal cancer, solid tumors
Citation: Zhang X, Zhou S, Zhou Y and Qiu H (2025) Diffuse large B-cell lymphoma combined with two solid tumors: a case report. Front. Oncol. 15:1561923. doi: 10.3389/fonc.2025.1561923
Received: 16 January 2025; Accepted: 27 May 2025;
Published: 17 June 2025.
Edited by:
Yi Zhang, The First Affiliated Hospital of Zhengzhou University, ChinaReviewed by:
Xinfeng Chen, First Affiliated Hospital of Zhengzhou University, ChinaNelly Elshafie, Purdue University, United States
Rahma Daoud, University of Sfax, Tunisia
Copyright © 2025 Zhang, Zhou, Zhou and Qiu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuqiao Zhou, MTUwNzAxNjgyMzRAMTYzLmNvbQ==; Huiqing Qiu, MTMyODU3MDk1NjZAMTYzLmNvbQ==
 Xiufang Zhang1
Xiufang Zhang1 Huiqing Qiu
Huiqing Qiu