- 1Department of Thoracic Surgery, Huzhou Central Hospital, Fifth School of Clinical Medicine of Zhejiang Chinese Medical University, Huzhou, Zhejiang, China
- 2Department of Thoracic Surgery, Huzhou Central Hospital, Affiliated Central Hospital of Huzhou University, Huzhou, Zhejiang, China
- 3Department of Central Laboratory, Huzhou Central Hospital, Fifth School of Clinical Medicine of Zhejiang Chinese Medical University, Huzhou, Zhejiang, China
- 4Department of Central Laboratory, Huzhou Central Hospital, Affiliated Central Hospital of Huzhou University, Huzhou, Zhejiang, China
Background: Anatomic basal segmentectomy is often regarded as a complex procedure, particularly in the presence of complex anatomical variations.
Case report: Herein, we present a case of a 55-year-old female patient diagnosed with invasive lung adenocarcinoma. Three-dimensional computed tomography bronchography and angiography (3D-CTBA) displayed a unique combined variation in the basal segment of right lower lobe (RLL): The medial basal subsegmental bronchi (BX7a+BX7t) originated from both the anterior and posterior segmental bronchi; The medial basal subsegmental arteries emanated from the anterior and posterior basal segmental arteries; The medial anterior segmental vein shared a trunk with both the anterior basal and lateral basal subsegmental veins. With precise preoperative planning, thoracoscopic anterior basal segmentectomy was successfully executed.
Conclusion: This case again highlights the importance of 3D-reconstruction in pulmonary segmentectomy. Detailed understanding of anatomic features of segmental bronchi and vessels is imperative for those with complex anatomical variations.
Introduction
Thoracoscopic basal segmentectomy presents formidable technical challenges for thoracic surgeons due to frequent anatomical variations (1). Preoperative understanding of segmental anatomy is crucial for surgeons to perform precise operations (2). Although numerous variations of the basal segment have been reported by Zhang M et al. (3), the type of variant in this case has rarely been previously reported. With meticulous preoperative planning and accurate intraoperative judgment, thoracoscopic right anterior basal segment (RS8) segmentectomy was successfully performed.
Case report
A 55-year-old woman was admitted to our department with a subsolid nodule in the right lower lobe (RLL), which had been under surveillance for five years following its initial detection. The high-resolution computed tomography (HRCT) revealed a 13 mm nodule in the RS8 (Figure 1A). The patient presented no history of malignant tumors, no disease symptoms, and no family history of lung cancer. No distant metastases were detected. The pulmonary function was normal. A unique variation in the right basal segment was identified via three-dimensional computed tomography bronchography and angiography (3D-CTBA). CT scan was performed using Toshiba Aquillion One 320-row Dual-Source CT, while 3D reconstruction was performed with Vitrea Extend 6.7 graphic analysis system. The prominent features including: (1) Two branches of the medial basal segmental artery, AX7a and AX7t, emanated from the anterior segmental artery (A8) and the posterior segmental artery (A10), respectively (Figure 2A). (2) The medial basal subsegmental bronchi, classified as BX7a+BX7t according to Zhang M et al., originated from both the anterior (B8) and posterior (B10) segmental bronchi (Figure 2B). (3) The medial basal segmental vein (V7) shared a trunk with the anterior basal segmental vein (V8) and the lateral basal subsegmental vein (V9a) (Figure 2C).
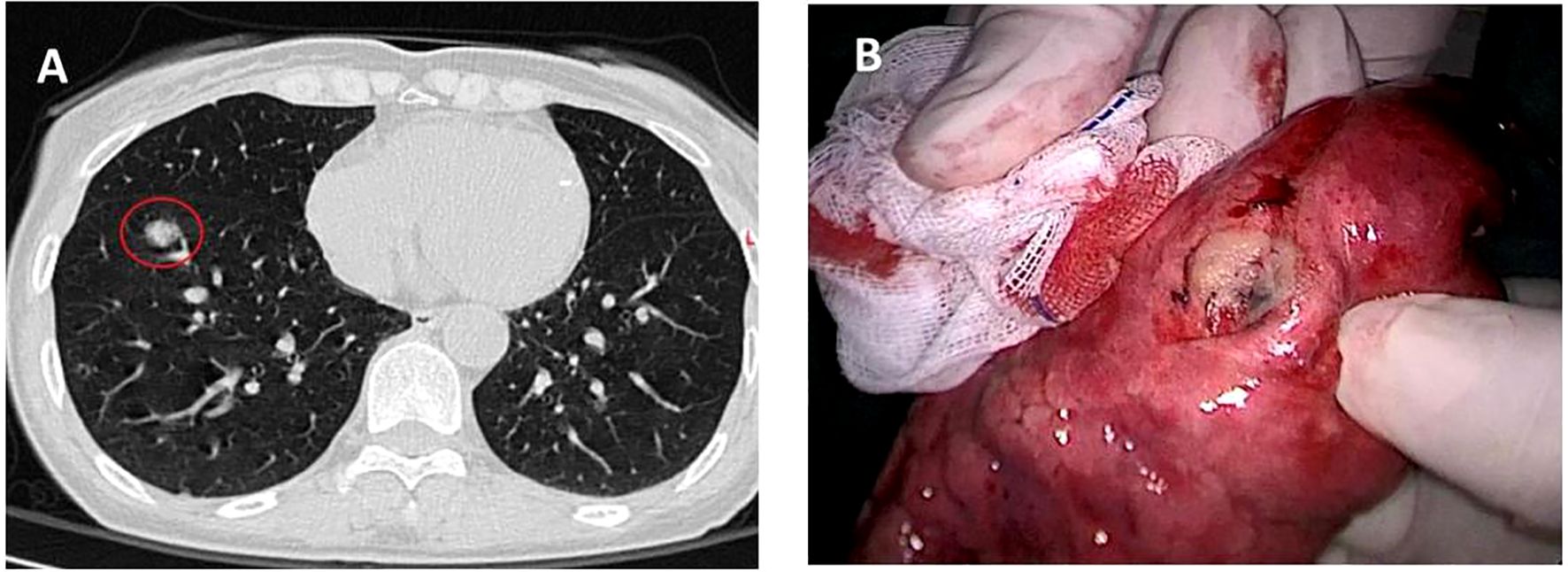
Figure 1. Preoperative chest CT scan and the intraoperative specimen. (A) A 13 mm-diameter subsolid nodule in the anterior basal segment of right lower lobe. (B) The tumor was 2.5 cm away from the incisal margin.
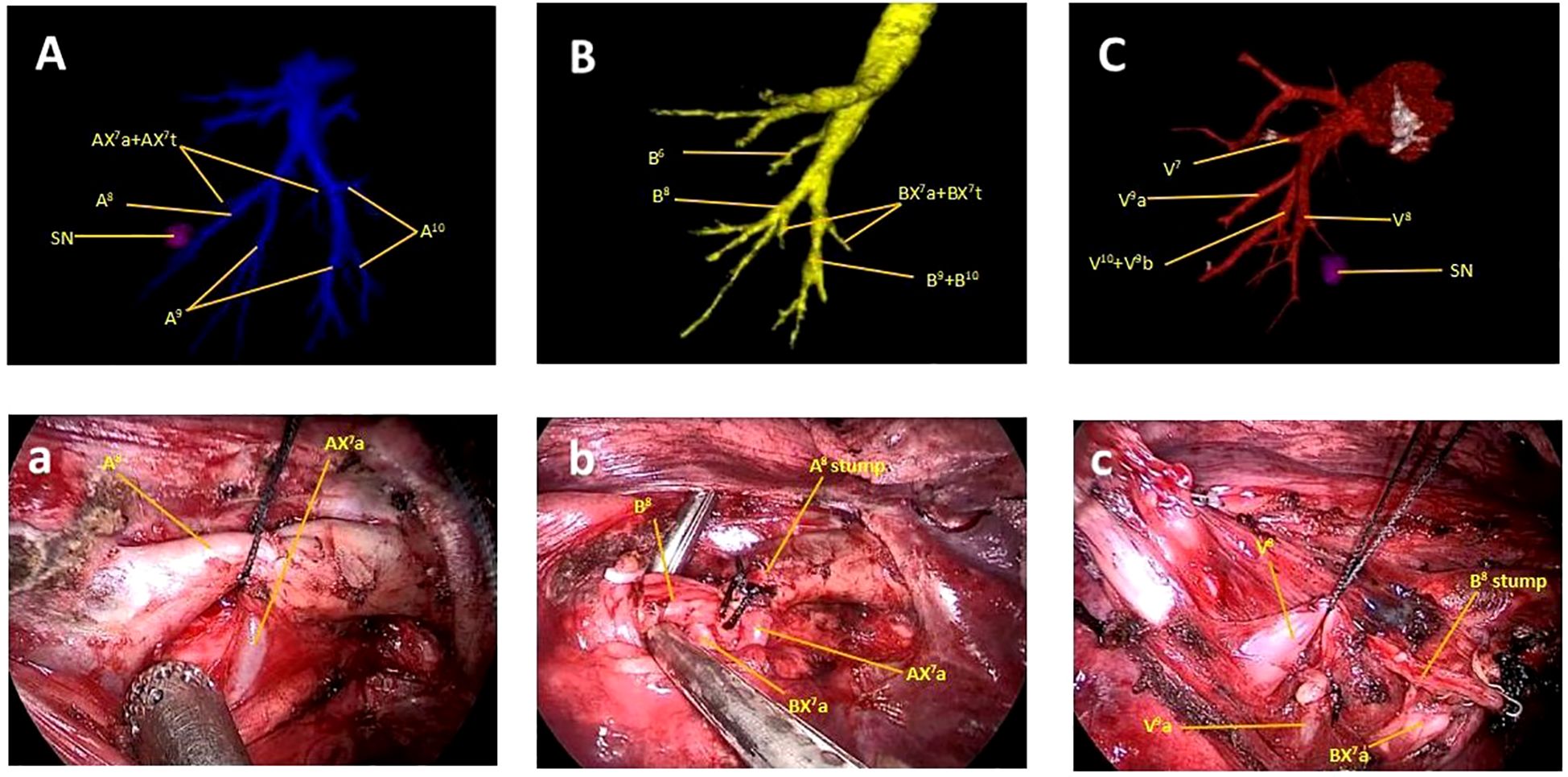
Figure 2. Preoperative 3D-CTBA of the right lower lobe and intraoperative findings. (A, a) The AX7a emanated from the A8. (B, b) BX7a originated from the B. (C, c) The V7 shared a trunk with the V8 and the V9a.
The tumor was diagnosed as stage cIA2 (cT1bN0M0). Anatomical pulmonary segmentectomy was the preferred protocol according to the National Comprehensive Cancer Network (NCCN) lung cancer guidelines (V2.2024). Based on detailed preoperative planning, thoracoscopic RS8 segmentectomy was performed precisely. Initially, the A8 and AX7a were clearly exposed after opening the interlobar fissure; the A8 was dissected using silk, while the AX7a was preserved (Figure 2A). Subsequently, after removing the lymph nodes surrounding the bronchi, the B8 was dissected using a stapler, and the BX7a was protected (Figure 2B). Thereafter, the V8 locating posterior to the B8 was exposed and ligated with silk (Figure 2C). Finally, the RS8 was divided using endostaplers, with the RS7a being successfully retained. The tumor was located 2.5 cm away from the incisal margin (Figure 1B). Intraoperative pathology analysis identified invasive adenocarcinoma, with intrapulmonary lymph nodes and surgical margins negative. Postoperative pathology analysis confirmed invasive adenocarcinoma with no involvement of the surrounding lymph nodes. The immunohistochemistry revealed that the Ki-67 index was 15%, which suggests slower tumor growth and more favorable prognosis. Additionally, the TTF-1 expression was strong positivity (+++), which supports the diagnosis of adenocarcinoma and indicates a higher likelihood of responsiveness to targeted therapies, should they be required in the future. The surgical process can be obtained via scanning the QR code (Figure 3). Following discharge, the patient underwent regular follow-up evaluations at six-month intervals. As of the most recent assessment in March 2025, there was no evidence of tumor recurrence or complications related to the surgery.
Figure 3. QR code for the surgical video. The surgical process can be obtained via scanning the QR code.
Discussion
Recently, anatomic pulmonary segmentectomy has been widely performed for early-stage non-small cell lung cancer, in accordance to the National Comprehensive Cancer Network (NCCN) lung cancer guidelines (4). Understanding the anatomical structure of the pulmonary segments is essential for surgery, while 3D-CTBA technology has been proved to be highly beneficial in facilitating anatomic pulmonary segmentectomy. As reported by Chen H et al. (5), 3D-CTBA guided surgery demonstrates a reduction in both operation time and surgery-related complications compared to 2D-CT. In addition to that, Zhang M et al. (3) analyzed the economic impact of 3D-CTBA in thoracic surgeries, concluding that its ability to reduce surgical errors offsets the initial costs associated with imaging technology. Segmentectomy of the S8 tends to be considered more simple than other types of basal segmentectomies (6). However, it can also present a major challenge for surgeon when complex anatomical variations involved. This case reported a rare and complex anatomical variation in the basal segment of the RLL. To the best of our knowledge, such variation has rarely been reported. The success of this operation lies in resecting the RS8 precisely while preserving the RS7a.
The RS7 has the smallest volume of all pulmonary segments, but the anatomical structure of RS7 has been reported more complicated. Nagashima T et al. (7) classified the branching pattern of the B7 into four types:(B7a), (B7b), (B7ab) and (BX7). In this classification, the B7 is designated as BX7 when it does not originate from the base of the basal bronchus. Similarly, the branching pattern of the A7 has been divided into four types:(A7a), (A7b), (A7ab) and (AX7). Shimizu K et al. (8) reported that the incidence of such combined variant was 5.6%(15out of 270 cases). Zhang M et al. (3) firstly proposed an alternative classification for B7, identifying six distinct types: B7a, B7p, B7o, B7t, BX7a, and BX7t. When BX7 originates from B8, it is designated as BX7a, while when it derives from B10, it is referred to as BX7t. According to this classification, our case was categorized as the type of BX7a and BX7t. However, the variant we reported was more complex than previously documented. Two branches, designated as BX7a and BX7t, concurrently exist and originate from B8 and B10, respectively. The BX7a traversed anterior to the inferior pulmonary vein (IPV) and shared a trunk with B8, whereas BX7t passed through the IPV and originated from B10. Intraoperatively, (B8+ BX7a) can be easily mistaken for B8 because of such unique anatomical variation.
The anatomical variation of pulmonary vessels often coexists with bronchial variation, thereby complicating segmentectomy procedures, as reported by Gossot D et al. (9). This aligns with the current case, where such variations required precise surgical techniques. In this particular case, the A7 was composed of AX7a and AX7t, originating from A8 and A10, while V8 shared a trunk with V7 and V9a. Intraoperatively, such variations can be confusing for surgeons, potentially leading to the inadvertent transection of AX7a and V9a. The unique anatomical variation reported in this case, specifically the coexistence of BX7a and BX7t originating from B8 and B10 respectively, increases surgical difficulty due to the complexity of identifying and preserving critical structures like AX7a and V9a during segmentectomy. Misidentification of BX7a as part of B8 intraoperatively can lead to inadvertent transection of vital vessels or bronchi, emphasizing the need for meticulous preoperative 3D-CTBA planning and intraoperative judgment. In conclusion, this case presented a unique variation of bronchus and pulmonary vessels in the basal segment of the RUL. With the guidance of detailed preoperative planning, thoracoscopic RS8 segmentectomy was performed accurately.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
TL: Writing – original draft. SH: Writing – original draft. JZ: Writing – review & editing. LJ: Methodology, Writing – review & editing. QS: Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the Joint Funds of the Zhejiang Provincial Natural Science Foundation of China under Grant No. LBY22H200006.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhang J, Li H, Yu C, and Zhu Y. Thoracoscopic segmentectomy for right upper lobe with unique anatomic variation. Ann Thorac Surg. (2022) 114:e201–3. doi: 10.1016/j.athoracsur.2021.11.052
2. Akdeniz A and Kara E. Determining tracheobronchial tree with anatomical dissection: 204 cases. Turk Thorac J. (2021) 22:124–9. doi: 10.5152/TurkThoracJ.2021.18111
3. Zhang M, Liu X, and Ge M. Prevalence and anatomical characteristics of medial-basal segment in right lung. Eur J Cardiothorac Surg. (2023) 64:ezad342. doi: 10.1093/ejcts/ezad342
4. Riely GJ, Wood DE, Ettinger DS, Aisner DL, Akerley W, Bauman JR, et al. Non-small cell lung cancer, version 2. 2024, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. (2024) 22:249–74. doi: 10.6004/jnccn.2204.0023
5. Chen H, Lin K, Xiao G, Tang G, Huang Y, Chen C, et al. A study on the efficacy of three-dimensional CT bronchial angiography in thoracoscopic precision resection of lung segments. Altern Ther Health Med. (2023) 29:335–9. doi: AT8652
6. Igai H, Matsuura N, and Kamiyoshihara M. Uniportal thoracoscopic right anterior basal (S8) segmentectomy using unidirectional dissection. Multimed Man Cardiothorac Surg. (2021) 2021. doi: 10.1510/mmcts.2021.021
7. Nagashima T, Shimizu K, Ohtaki Y, Obayashi K, Nakazawa S, Mogi A, et al. Analysis of variation in bronchovascular pattern of the right middle and lower lobes of the lung using three-dimensional CT angiography and bronchography. Gen Thorac Cardiovasc Surg. (2017) 65:343–9. doi: 10.1007/s11748-017-0754-4
8. Shimizu K, Nagashima T, Yajima T, Ohtaki Y, Obayashi K, Nakazawa S, et al. Thoracoscopic medial-basal segment segmentectomy. Ann Thorac Surg. (2017) 104:e403–6. doi: 10.1016/j.athoracsur.2017.07.006
Keywords: three-dimensional computed tomography bronchography and angiography, anatomical variation, basal segment, anatomic segmentectomy, lung cancer
Citation: Liu T, Huang S, Zhang J, Jin L and Shen Q (2025) Thoracoscopic right anterior basal segmentectomy with unique anatomic variation: a case report and literature review. Front. Oncol. 15:1562303. doi: 10.3389/fonc.2025.1562303
Received: 17 January 2025; Accepted: 05 June 2025;
Published: 26 June 2025.
Edited by:
Lizza E. L. Hendriks, Maastricht University Medical Centre, NetherlandsReviewed by:
Andrea De Vico, Azienda Usl Teramo, ItalyAli Bilal Ulas, Atatürk University, Türkiye
Yu-Wei Liu, Kaohsiung Medical University Hospital, Taiwan
Copyright © 2025 Liu, Huang, Zhang, Jin and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianbin Zhang, ZmlzaGluZzExQDE2My5jb20=; Qibin Shen, c3FiMDA0NkAxNjMuY29t
†These authors have contributed equally to this work
 Tiancheng Liu1,2†
Tiancheng Liu1,2† Jianbin Zhang
Jianbin Zhang