- Stanford Healthcare, Stanford, CA, United States
Background: Non-Hispanic Black women have a disproportionately higher breast cancer mortality rate compared to non-Hispanic white women. Structural racism embedded within societal systems plays a fundamental role in perpetuating these persistent disparities. This systematic review aims to examine the relationship between structural racism and breast cancer quality of care outcomes across various racial and ethnic groups.
Methods: Following the PRISMA guidelines, we conducted a systematic review of PubMed, Embase, and CINAHL for studies published until October 30, 2024, that examined the relationship between structural racism and breast cancer quality of care outcomes. We employed the Healthy People’s Social Determinants of Health (SDOH) framework to identify structural racism measures within these five themes: economic stability, education access, healthcare access, neighborhood and built environment, and social and community welfare. Breast cancer quality of care outcomes were assessed using the Donabedian quality of care model which encompasses three components of quality: process measures, structural measures, and outcome measures.
Results: We conducted a systematic review of 262 studies that included at least one measure of structural racism linked to a breast cancer quality of care outcome. Of these, 29 studies met the eligibility criteria for inclusion. The most frequently examined measures of structural racism were those related to residential segregation and redlining, which pertain to neighborhood and built environment SDOH domains. The predominant finding across the studies was that both residential segregation and redlining were significantly associated with adverse breast cancer outcomes. Theses outcomes included higher mortality rates, later-stage diagnoses, and suboptimal treatment. These effects exhibited variability based on race, comorbidity, and neighborhood characteristics, highlighting the complex role of structural racism in perpetuating disparities in breast cancer outcomes.
Conclusion: The complex relationship between measures of structural racism and breast cancer quality of care outcomes underscores the necessity for ongoing research to understand the pathways through which structural racism impacts health outcomes. Understanding these pathways is essential for developing targeted interventions and promoting health equity in breast cancer care.
Introduction
Breast cancer is the most common cancer diagnosis in the United States. Yet, significant disparities in survival rates persist, particularly between non-Hispanic Black and non-Hispanic White women. Non-Hispanic Black women face a 41% higher mortality rate compared to non-Hispanic white women (1). Structural racism is a likely contributor to these disparities, as it creates adverse upstream determinants of health. While there is growing recognition of the role of structural racism in health disparities, the current body of research on its relationship to breast cancer quality outcomes remains limited. Existing studies often fail to comprehensively examine the multiple dimensions of structural racism and their impact on different breast cancer quality outcomes. The objective of this study is to examine how structural racism affects disparities in quality-of-care outcomes for breast cancer among various racial and ethnic groups.
Structural racism is defined as macro-level systems, policies, and practices that institute racial discrimination in domains such as housing, education, employment, earnings, benefits, credit, healthcare, and criminal justice (2). While systemic racism refers to the racial inequalities within systems and policies, structural racism emphasizes the interconnectedness of these systems, which reinforce inequalities over time. These interlocking systems create cumulative disadvantages for racial and ethnic groups, significantly shaping the experiences and opportunities available to breast cancer survivors from marginalized backgrounds (3).
Structural racism operates through societal power dynamics-economic, political, and social-that influence social determinants of health (SDOH), such as economic stability, education access, social context, healthcare access, and neighborhood environment (4). The Healthy People framework recognizes these factors as critical to health, functioning, and overall quality of life (5). Discriminatory practices within these domains, including redlining in housing, funding disparities in education, biased hiring, wage gaps, and healthcare access barriers, collectively impact marginalized communities (8). For example, redlining and unequal housing opportunities lead to segregated and impoverished neighborhoods, predominantly affecting specific racial and ethnic communities. In education, funding disparities and unequal access to quality schools result in differential educational outcomes across racial groups. In the economic domain, employment is similarly impacted through biased hiring practices, wage gaps, and limited career advancement opportunities for racial and ethnic minorities. In the social domain, the criminal justice system contributes to disproportionate rates of incarceration among specific communities through racial profiling, biased policing, and sentencing disparities. Similarly, in healthcare access domain, structural racism is evident in barriers to access, discriminatory practices, and health outcome disparities (9).
Previous studies have highlighted structural racism as a fundamental driver of health disparities among breast cancer survivors by influencing the broader landscape of SDOH (6). Individuals from marginalized racial and ethnic backgrounds often face multiple barriers to timely, high-quality healthcare (7), including disparities in early detection, diagnosis, and treatment, which leads to delayed interventions and worse outcomes (8). Structural racism also leads to unequal socioeconomic opportunities, further affecting access to supportive care and post-treatment services (9, 10). The cumulative effects of discrimination, stress, and limited access to healthcare contribute to higher levels of psychological distress among minority breast cancer survivors (11, 12). These findings underscore the urgent need to examine how structural racism influences breast cancer care outcomes and to implement targeted policy interventions that address the root causes of these disparities (13).
This review aims to map existing evidence on structural racism’s role in breast cancer disparities and outline areas for future research to inform policies aimed at mitigating these disparities. By examining a wide range of structural factors guided by the Healthy People 2030 SDOH framework, we seek to capture the complex interplay between various determinants of health. This holistic approach allows us to identify patterns and associations that may not be evident when focusing on isolated factors. Our study highlights areas where research is lacking. directing future research efforts toward understanding the nuanced effects of structural racism on breast cancer outcomes. By addressing structural racism and its impact on social determinants of health, we can better understand the pathways through which it contributes to adverse outcomes for breast cancer survivors from marginalized groups and develop strategies to improve equity in cancer care.
Methods
Data source and search strategy
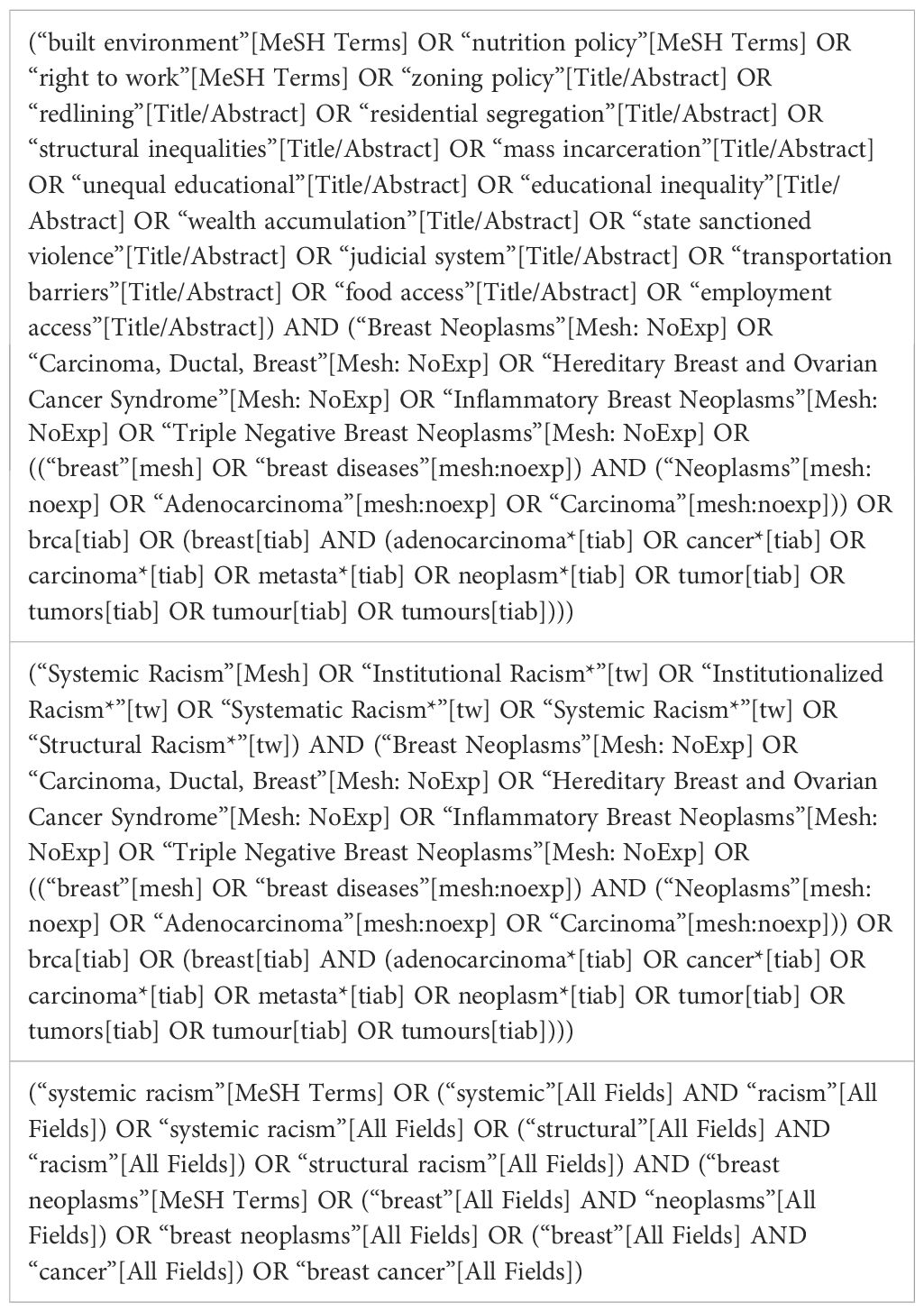
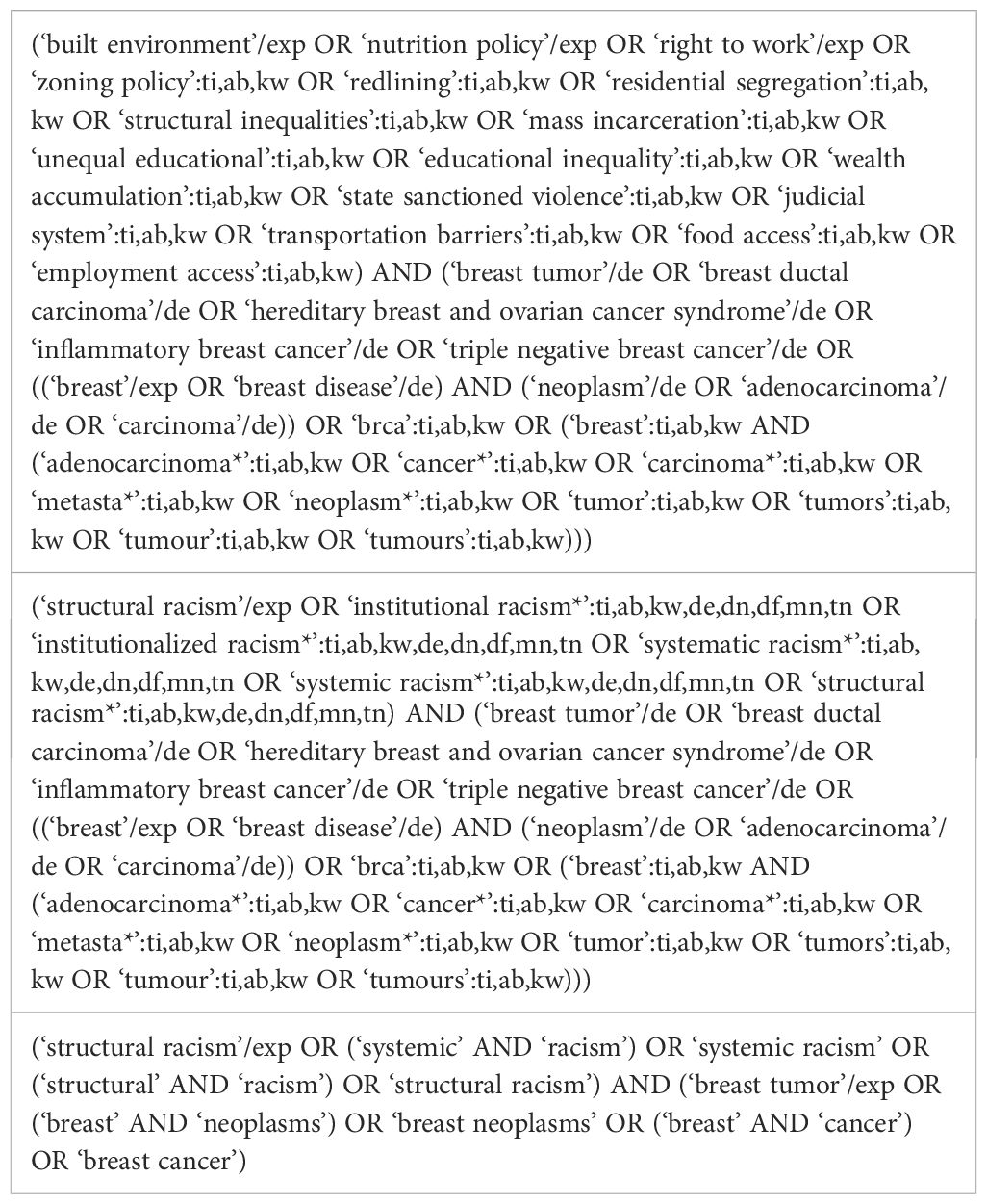
In adhering to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines (50), we searched three databases: PubMed, Embase, and CINAHL for English-language, peer-reviewed studies on structural racism and breast cancer outcomes till October 2024. Guided by the Healthy people’s 2030 SDOH framework, we searched for studies that measured and examined structural racism, which includes social and community context, economic stability, education access, healthcare access, neighborhood and built environment domains.
These aspects were considered in relation to quality-of-care outcome measures, process measures and structural measures. These measures include mortality, survival rates, treatment, biomarkers, and incidence rates, screening rates, as well as other quality of care measures We identified specific Medical Subject Heading (MeSH) terms and keywords that encapsulated the concept of structural racism and structural inequalities related to breast cancer outcomes.
Study selection: inclusion and exclusion criteria
Studies met inclusion criteria if they (1): published in English, (2) had a data sources within the United States, (3) fall into one of the following designs: cross-sectional, cohort, randomized clinical trial (RCT), quasi-experimental, or pre-post study design, (4) consist of adults aged 18 years or older, (5) had to encompass a racial or ethnic minority group or multiple racial and ethnic groups, (6) measure at least one breast cancer outcome such as a) outcome measures b) process measures, or c) structural measures, (7) measure one of the structural factors, as defined by the Healthy People’s SDOH framework, including a) Economic, b) Social, c) Healthcare access, d) build environment, or e)education.
We excluded studies that (1) examined racism only at the individual level and did not examine structural measures including systems, policies, and practices, (2) Studies with Abstract only, (3) Qualitative and review studies.
Data extraction and assessment of bias
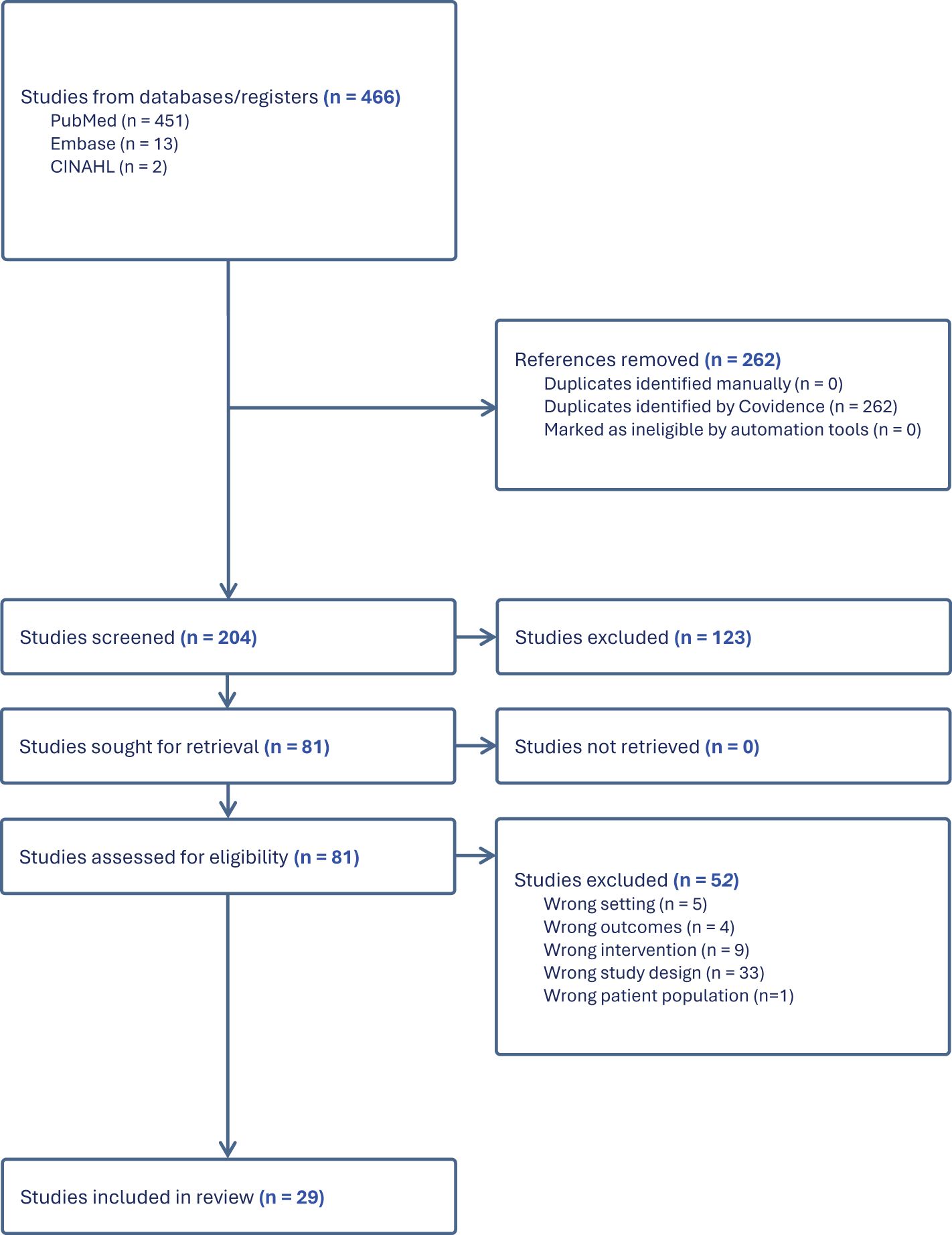
Two independent reviewers (OA and AY) screened all the results to determine eligibility for this review. Studies were evaluated for bias and quality using the Joanna Briggs Institute (JBI) Checklist. Figure 1 provides an overview of the study selection process. We began by reviewing the titles and abstracts of potential studies to examine their alignment with our inclusion criteria. To maintain consistency, a checklist was utilized, encompassing our eligibility criteria, to make the determination of whether a study should be included or excluded. Any studies that did not meet the eligibility criteria were excluded from further consideration. Following this initial assessment of titles and abstracts, full-text articles that met our initial inclusion criteria proceeded to a more comprehensive synthesis. Both the initial and full-text reviews were conducted independently and then collaboratively finalized by all authors, using the platform Covidence (14). This collaborative use of the checklist ensured uniform decision-making processes for each article under review. Upon the completion of full-text synthesis, articles that did not meet the inclusion criteria were excluded, and the rationale for their exclusion was documented. During the data extraction phase, we captured critical information, including study design, study population, sample size, and the specific outcomes assessed.
Search, study selection, and data collection
Figure 1 shows the PRISMA diagram with the results for study identification, screening, eligibility, and final selection, along with details of studies excluded and retained at each phase. After searching PubMed, Embase, and CINAHL, 466 studies were identified. The search strategies are included in Table 1A in the Appendix. Following the removal of duplicates, 262 articles remained for title and abstract screening, using the inclusion criteria listed above.
There were eighty-one articles that met the inclusion criteria and underwent a full article review. Of the eighty-one articles that initially met our inclusion criteria, 52 were subsequently excluded due to reasons such as inappropriate study design. This led to a final inclusion of 29 articles for our synthesis. The articles included for data extraction are shown in Table 1.
Results
Study design, sample characteristics, and settings
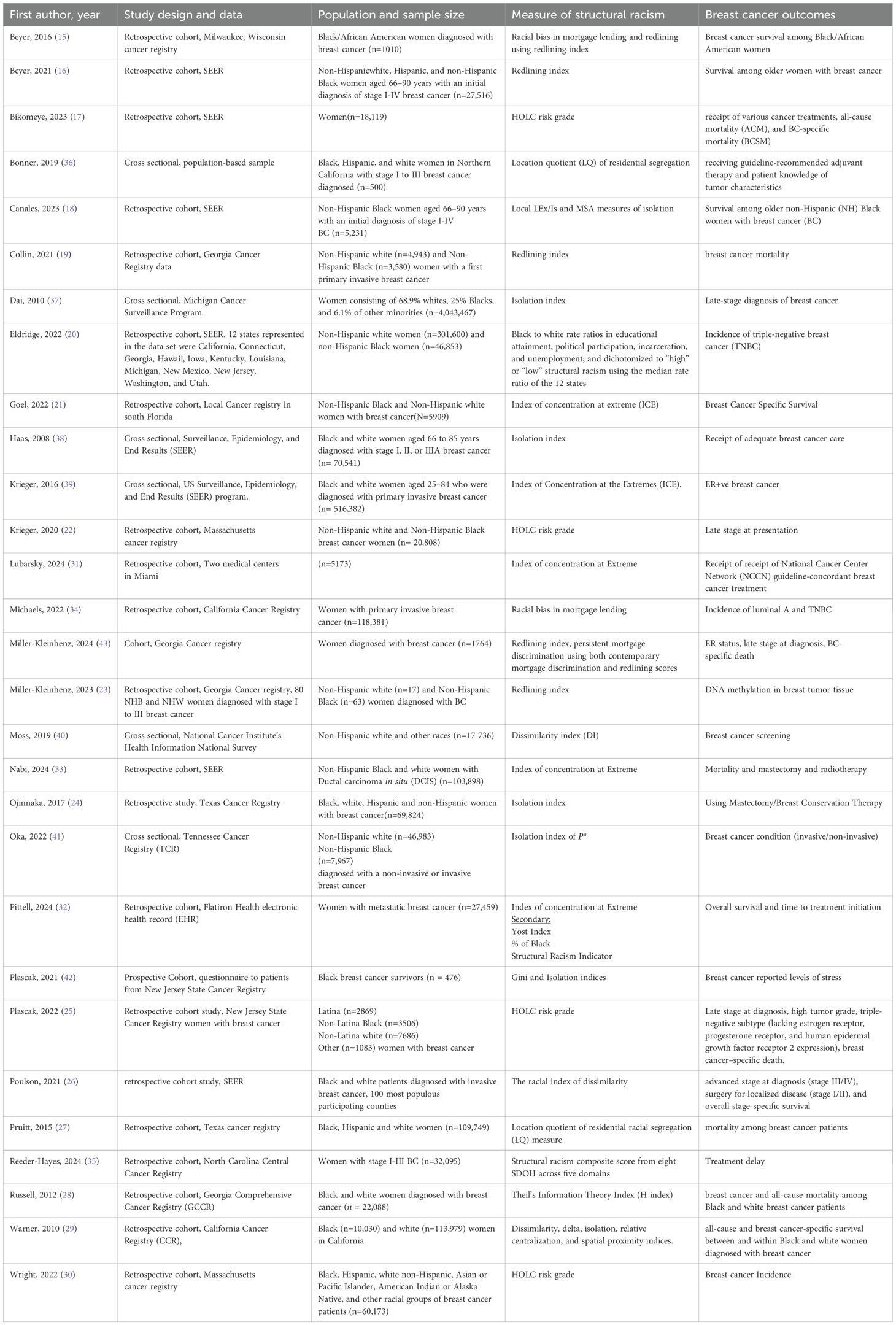
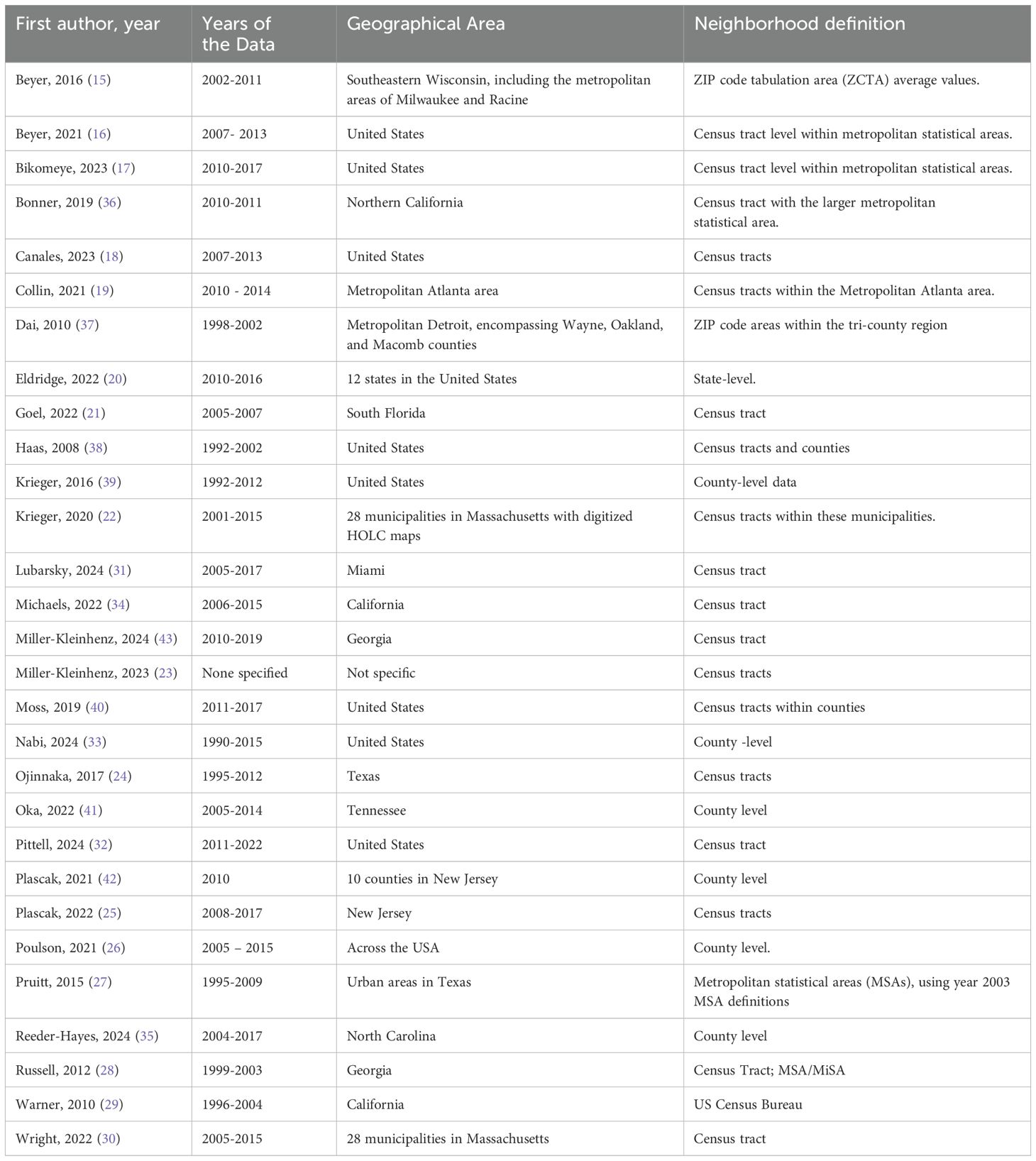
The characteristics of the twenty-nine studies included in this review are summarized in Table 1 and 2. Out of the 29 studies reviewed, 21 were retrospective cohort studies (15–35), while the remaining study designs included 6 cross-sectional studies (36–41) and 2 prospective cohort study (42, 43). The samples comprised adult women aged >18 years, diagnosed with breast cancer, and representing at least one racial minority group.
In terms of settings, most of the studies utilized secondary data from national and state cancer registries, such as the US Surveillance, Epidemiology, and End Results (SEER) program, as well as cancer registries in Massachusetts, California, Georgia, Tennessee, Michigan, South Florida, New Jersey, Milwaukee Wisconsin, North Carolina, Miami, Florida, and Texas (Table 2).
Exposure and outcome measures
Exposure measures: structural racism measures
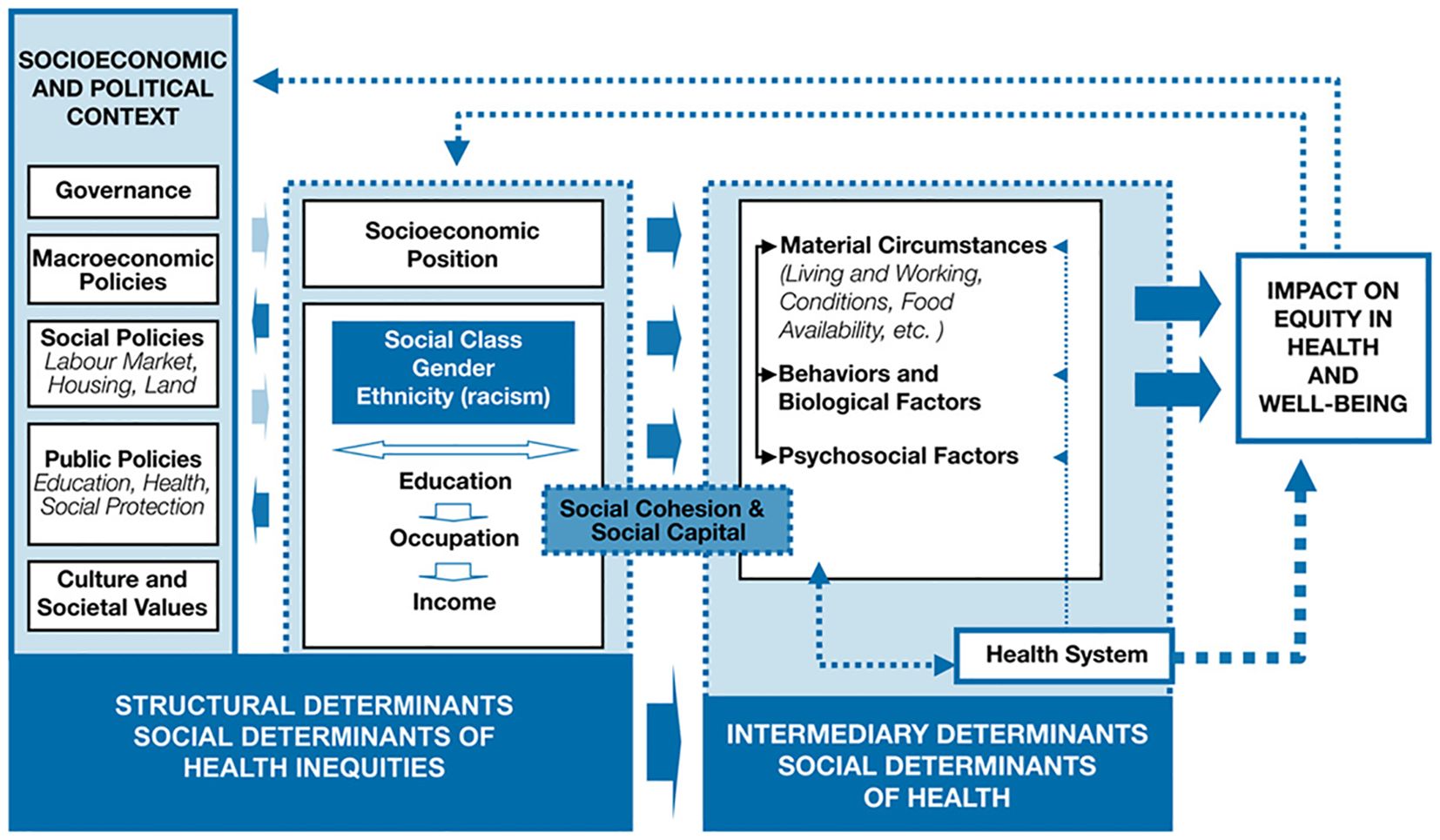
Based on Healthy people framework’s social determinates of health, the neighborhood and build environment domain has been the focus of most studies examining the impact of structural racism on breast cancer outcomes. Specifically, fourteen studies investigated residential segregation, and eight studies examined redlining, which refers to discriminatory mortgage lending practices based on racial composition of neighborhood and financial disinvestment in predominantly Black neighborhoods (often referred to as “red zones”). In contrast, only one study examined structural racism in the domain of education, social and community context, and economic stability based on the Black-to-white ratio in educational attainment, political participation, incarceration, and unemployment. Notably, while many studies assessed healthcare access—such as insurance coverage and disparities in breast cancer outcomes—none specifically investigated the association between structural racial discrimination in healthcare access and breast cancer outcomes (Figure 2).
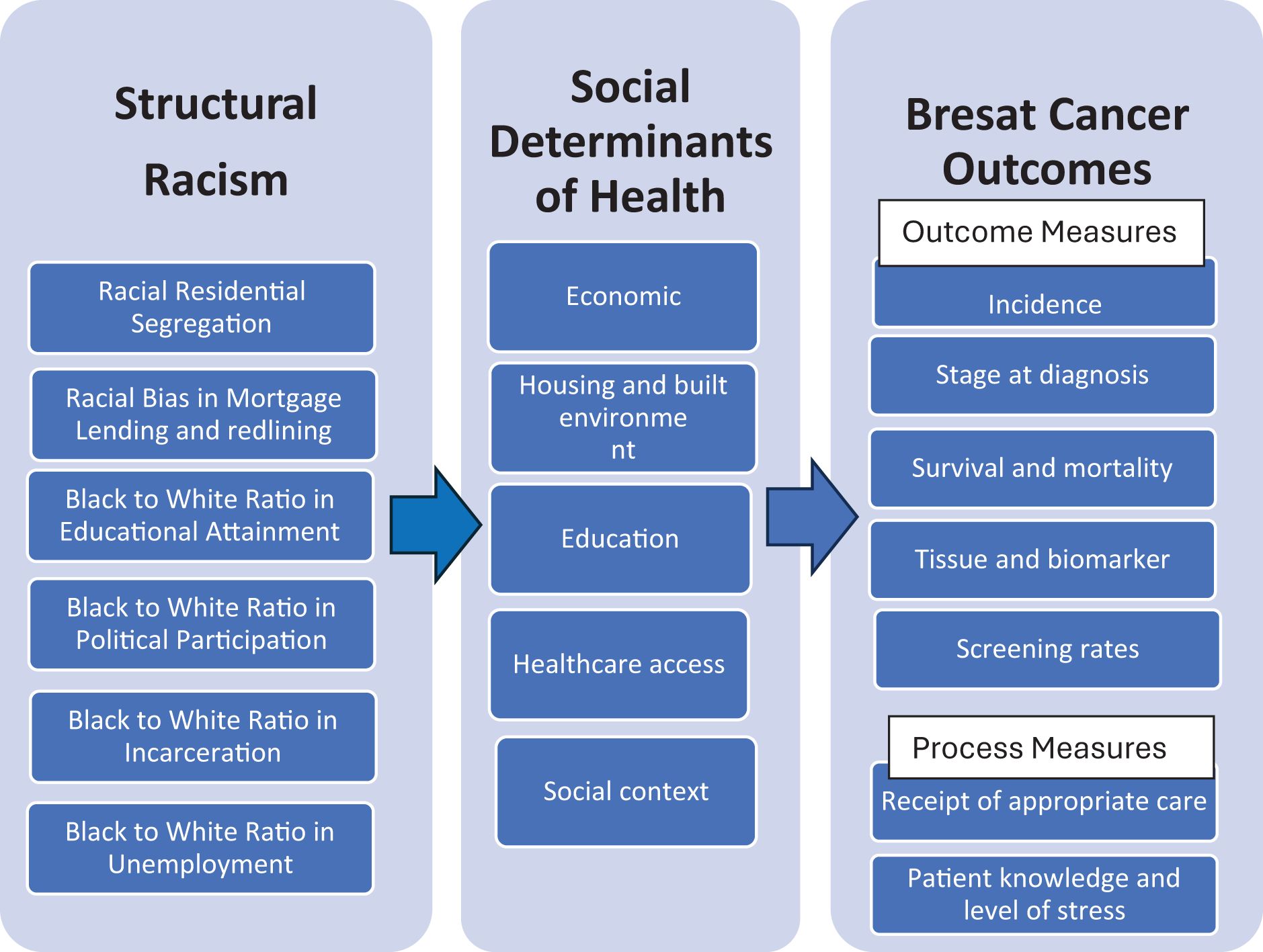
Figure 2. Structural racism impact breast cancer quality of care through Influence on SDOH. Structural racism as fundamental mediator for impact of SDOH on breast cancer outcomes.
Below are specific measures of structural racism utilized in the studies:
1- Residential Segregation Measures (17 studies):
Location Quotient: This measure compares the proportion of a specific racial group in a neighborhood to the proportion of that group in a larger area, indicating the degree of concentration or segregation. (2 studies) (27, 36) Index of Concentration at Extreme: This index quantifies the extent to which a neighborhood is dominated by a single racial group, highlighting extreme segregation. (5 studies) (21, 31–33, 39).
Isolation measures: These measures assess the degree to which members of a racial group are isolated from other groups within a neighborhood (7 studies) (18, 24, 29, 37, 38, 41, 42) Delta: This measure captures changes in segregation over time, providing insights into trends in residential patterns. (1 study) (29).
Relative Centralization: This measure evaluates the centrality of a racial group within a metropolitan area, indicating how concentrated or dispersed the group is. (1 study) (29).
Spatial Proximity: This measure assesses the physical distance between different racial groups within a neighborhood, reflecting the level of integration or segregation. (1 study) (29) Dissimilarity Index: This index measures the evenness of racial distribution across neighborhoods, indicating how evenly different racial groups are spread out. (3 studies) (26, 29, 40).
Theil’s Information Theory Index (H index): This index quantifies the level of segregation by considering the distribution of racial groups across different areas. (1 study) (28).
Gini index: A common measure of segregation that assesses the evenness of racial distribution within a population. (1 study) (42).
2-Redlining and Mortgage Bias Measures (10 studies):
HOLC Risk Grade (grades A, B, C, D): This grading system, developed by the Homeowners’ Loan Corporation, categorized neighborhoods based on perceived investment risk, often disadvantaging Black neighborhoods. (4 studies) (17, 22, 25, 30).
Redlining Index: This index quantifies the extent of redlining practices in specific areas, highlighting the impact of discriminatory lending on neighborhood development. (5 studies) (15, 16, 19, 23, 43).
Racial Bias in Mortgage Lending Against Black Residents Regardless of Neighborhood redlining: This measure examines discriminatory lending practices targeting Black individuals, irrespective of their neighborhood’s redlining status. (2 study) (15, 34).
3-Black to white Ratio in Educational Attainment, Political Participation, Incarceration, and Unemployment Measure: This measure assesses disparities in these domains by comparing the educational attainment, political participation, incarceration, and economic outcomes of Black individuals to those of white individuals within same neighborhood. Educational attainment ratio measured as the relative proportion of Black individuals to White individuals over the age of 15 who hold a bachelor’s degree or higher. Employment ration assessed as the relative state-level unemployment rate ratio between Black and White individuals. Incarceration measured as the relative proportion of Black individuals to White individuals incarcerated in jails and prisons, as well as the disenfranchisement rates of Black individuals due to felony convictions. Political participation evaluated as the relative proportion of Black individuals to White individuals aged 18 and over who were registered to vote and who participated in elections. (1 study) (20).
4- Racial Gaps in SDOH Composite Score Measure: From eight SDOH across five domains, this composite score ranked from 0–100 minimum-maximum scale for racial gap in SDOH factors at the county level. (1 study) (35).
Breast cancer quality of care outcome measures
We used the Donabedian model (2005) for quality-of-care classifications into three categories: outcome measures, process measures, and structural measures. For the quality of care outcome measures, a total of 15 studies included measures of survival and mortality (15–19, 21, 25–29, 32, 33), incidence measure is included in 2 study (30 ,34), stage at diagnosis is included in 6 studies (22, 26, 37, 41–43), tissue and biomarker measures are included in 5 studies (20, 23, 25, 39, 43), and patient-centric measures are included in two studies (36, 42). For the quality of care process measures, receipt of appropriate cancer care measures are included in 9 studies (17, 24, 26, 31–33, 35, 36, 38), and a measure of breast cancer screening is included in one study (40). None of the studies investigated quality of care structural measures.
Study findings: evidence of impact of structural racism
Residential segregation and redlining emerged as the most frequently employed measures of structural racism, showing positive associations with multiple adverse breast cancer outcomes including high mortality rates, late stage at diagnoses, and lower quality of care.
However, the influence of structural racism varies, affected not only by individual characteristics such as race and ethnicity, comorbidity, but also by neighborhood features and their interactions.
Residential segregation
Studies focusing on residential segregation and mortality rates have consistently found a significant impact of residential segregation on mortality.
Correlation with mortality rates varied based on neighborhood measures
Canales et al. (18) observed that women residing in areas with high local isolation faced increased mortality from breast cancer, particularly among those with two or more comorbidities HR = 1.20 (95%CI: 1.08-1.33). However, local isolation was not associated with higher mortality when it was linked with a high level of segregation in the Metropolitan Statistical Area (MSA). Protective ethnic density may play a role in attenuating this effect. Goel et al. (21) identified higher hazards of death in predominantly non-Hispanic Black and Hispanic segregated neighborhoods especially in low-income communities HR= 2.43 (95%CI: 1.72- 3.43) and HR= 1.99 (95%CI: 1.39- 2.84). Poulson et al. (26) noted a 29% RR=1.29 (95% CI: 1.04- 1.60) increased hazard of death with rising Index of Dissimilarity (IoD) for Black patients over 50, while white patients showed no significant difference. Pruitt et al. (27) found associations between elevated Black segregation and higher all-cause mortality HR= 1.31 (95% CI: 1.26-1.37), but the association disappeared after controlling for race and ethnicity. Russell et al. (28) highlighted the significant impact of tract-level percent Black on breast cancer-specific mortality and observed an interaction between race and MSA/MiSA area segregation. Among Black but not white, as the segregation increase the mortality increased HR = 2.20 (95% CI: 1.09- 4.45) On the other hand, Warner and Gomez (29) found that living in neighborhoods with a higher proportion of Black residents was associated with lower all-cause and breast cancer-specific mortality among Black women HR = 0.86 (95% CI: 0.76–0.97) but higher mortality among white women HR = 1.07 (95% CI: 1.02–1.13). Hass et al. (38) found that although Blacks experienced greater breast cancer mortality than whites, segregation did not substantially mediate this disparity.
Correlation with late stage at diagnosis
Dai (37) identified a positive correlation between Black residential segregation and the late-stage breast cancer presentation, even after accounting for primary care access, mammography access, economic advantages, and sociocultural barriers mean=0.109 (p<0.01). Poulson et al. (26) revealed that increasing segregation is associated with a higher risk of advanced-stage presentation in Black patients aged over 50 RR= 1.49 (95%CI: 1.27- 1.74). Warner and Gomez (29) noted that neighborhood racial composition and metropolitan segregation did not explain differences in cancer stage or survival between Black and white women. Additionally, Oka et al. (41) found no association between county-level Black isolation and invasive breast cancer.
Correlation with receiving treatment
Haas et al. (38) revealed that increased Black segregation was associated with a reduced likelihood of both Black and white women receiving adequate breast cancer care OR=0.73 (95% CI: 0.64-0.82), with 8.9% explaining a notable portion of the Black-white disparity. Hispanic-white disparities initially observed disappeared when accounting for residential segregation. Ojinnaka et al. (24) found that higher racial residential segregation decreased the likelihood of receiving mastectomy/breast-conserving treatment, particularly affecting African American individuals OR=0.56 (95% CI: 0.36-0.88). While Nabi et al. (33) found that women with DCIS in less privileged counties measured by ICE higher odds of mastectomy vs radiotherapy and breast conservative surgery OR = 1.51; (95%CI: 1.35–1.69) (33). Polsun et al. (51) reported a 3% lower likelihood of surgical resection for localized disease with a rising Index of Dissimilarity (IoD). In contrast, Bonner et al. (36) found a higher likelihood of receiving adjuvant hormonal therapy in participants with higher residential segregation measured by the Black Location Quotient (LQ) OR= 4.06 (95% CI: 1.26-12.93), emphasizing the nuanced and multifaceted nature of the relationship between residential segregation and breast cancer care outcomes. Lubarsky (31), found that non-Hispanic Black less likely to receive guidelines breast cancer treatment compared to non-Hispanic whites regardless the status of residential segregation (31). Pittel et al. (32) found that, compared to women in more privileged women form less privileged neighborhoods measured as more segregated had longer time to treat (38 vs 31 days) and less survival rate HR=0.91, (95% CI 0.86- 0.95) (31).
Correlation with screening rates
For breast cancer screening and segregation, Moss et al. (40) revealed that breast cancer screening rates were lower in rural compared to urban areas. This difference was not linked to segregation among breast cancer patients.
Correlation with perceived stress
Regarding perceived stress and segregation, Plascak et al. (42) found weak positive correlations with Black segregation (Gini index), body mass index, and perceived stress.
Correlation with biomarkers
Similar to redlining, studies have found that residential segregation impacts the biological and tissue markers of breast cancer characteristics. Krieger et al. (39) found higher odds ratios for ER+ versus ER− tumors in women living in the top versus bottom quintile of counties, with adjustments for income and ICE measures attenuating racial/ethnic odds ratios for being ER+.
Redlining and mortgage bias
The correlation between redlining, mortgage bias, and increased mortality rates in breast cancer outcomes exhibited variations based on race/ethnicity and comorbidity.
Correlation with mortality rates vary based on race
Beyer et al. (15) noted that while mortgage lending bias had an increase in mortality hazard rates for all cause HR=1.16 (1.04-1.29) and for breast cancer specific HR=1.12 (95%CI: 0.98-1.28), the redlining index reduced these rates HR=0.73 (0.59-0.90) for all cause morality and HR=0.76 (95%CI: 0.59 to 0.98) for breast cancer-specific mortality for Black women. Collin et al. (19) found that increased redlining metrics were associated with higher estimated breast cancer mortality rates, and these outcomes varied among racial/ethnic groups. Notably, they observed a significant positive association HR= 1.39 (95% CI: 1.09-1.78) in Non-Hispanic white women, while there was no significant association HR = 1.13 (95% CI: 0.90-1.42) detected in Non-Hispanic Black women.
Correlation with Mortality Rates vary based on Comorbidities: Beyer et al. (16) found a significant increase in mortality for non-Hispanic Black race in redlined zones compared to non-Hispanic whites HR =1.25 (95%CI: 1.08-1.46). While the hazard rate was lower for women with comorbidity in the relined zones for all races HR=0.82 (95%CI: 0.69 to 0.98). Additionally, Bikomeye et al. (17) demonstrated that historical redlining is a significant predictor of poorer survival after breast cancer diagnosis, affecting all-cause HR= 1.09 (95% CI: 1.03 - 1.15) and breast cancer–specific mortality likelihood HR= 1.26 (95% CI: 1.13 - 1.41). This relation was mediated by comorbidities as a significant contributor for mortality hazard for all races. HR= 1.16 (95%CI 1.09 - 1.23) with no comorbidities versus HR=1.09 (95% CI: 1.03 - 1.15) after adjusting for comorbidities.
Correlation with late stage at diagnosis
Recent research by Krieger et al. (22) also reveals elevated risks of late-stage cancer diagnosis among women with breast cancer residing in redlined areas risk ratio (RR)= 1.07 (95%CI: 0.98- 1.17). In-depth analyses of the residual disparity indicate that, even following a hypothetical intervention aimed at equalizing the distribution of census tract segregation (CT ICE), disparities in late-stage cancer risk associated with redlining, as measured by HOLC area, would persist RR=1.03 (95% CI: 0.95- 1.12).
Plascak et al. (25) discovered race and ethnicity-dependent variations in breast cancer outcomes associated with HOLC grades. Living in areas designated as “best” by the HOLC was linked to reduced chances of being diagnosed at a late stage OR=0.34 (95% CI: 0.22-0.53).
Correlation with receiving treatment
Bikomeye et al. (17) found that historical redlining was correlated with a decreased probability of undergoing surgery OR = 0.74 (95% CI: 0.66 - 0.83) and an increased probability of receiving palliative care OR = 1.41: (95% CI= 1.04 - 1.91) for all races.
Correlation with biomarkers
Additionally, studies have found that redlining impacts the biological and tissue markers of breast cancer characteristics. Miller-Kleinhenz et al. (23) identified a positive correlation between redlining and methylation in breast cancer. Miller-Kleinhenz et al. (43) found that living in historically redlining areas linked to increased odds of ER-ve breast cancer among non-Hispanic Black women (odds ratio [OR], 1.62 [95% CI, 1.01-2.60]) (43).
Correlation with incidence varied based on associated recent segregation
Micheals et al. (34) found no association between mortgage bias and incidence of Luminal A breast cancer (IRRadj = 0.92, 95% CI = 0.85, 1.00) (34) Studies suggest that examining historical redlining in conjunction with current residential segregation measures can provide a better understanding of the impact of structural racism. For example, Wright et al. (30) found that the highest incidence occurred in areas with the best HOLC grade and privileged contemporary characteristics, particularly for ER-positive and PR-positive breast cancer, while the lowest incidence was in areas with concentrated racialized economic deprivation and no HOLC grade.
Black to white rate ratios in educational attainment, political participation, incarceration, and unemployment
Correlation with incidence varied by race
Eldridge and Berrigan (20) found that Black women residing in states with high levels of structural racism across the domains of educational attainment, judicial treatment, and political participation were more likely to be diagnosed with triple-negative breast cancer (TNBC) compared to those in states with low disparities. Interactions between indicators of structural racism and race were significant for educational attainment, employment, disenfranchisement, and voting practices, revealing that the impact of these measures on TNBC diagnosis significantly differs between Black and white women. Disparities in educational attainment were positively associated with TNBC for both groups but were significantly weaker for white women OR=1.17 (95% CI: 1.10-1.23) compared to Black women OR=1.50 (95%CI: 1.27-1.77). In contrast, the positive association between disparities in voting practices and TNBC was observed only among Black women, being null for white women.
Racial gaps in SDOH
Correlation with treatment
Reed et al., 2024 found that living in counties with high racial gaps in eight SDOH across five domains was associated with increased odds of treatment delay among Black women with breast cancer Adjusted OR=1.2 (95% CI: 1.08 - 1.45) (35).
Discussion
This systematic review synthesizes current evidence on the impact of structural racism on disparities in quality-of-care outcomes for breast cancer. The findings highlight that residential segregation and redlining are critical contributors to disparities in survival rates among breast cancer patients, as identified in multiple studies. Structural racism also contributes to inequities across other breast cancer outcomes, including incidence rates, stage at diagnosis, tumor biomarker profiles, and patient-centered quality of care measures. The relationship between structural racism and breast cancer outcomes is often influenced by interplay of multiple factors, including sample characteristics, such as race and ethnicity, comorbidities, neighborhood attributes, and the geographic scope of measurement (e.g., local census tract versus broader metropolitan statistical areas). These interactions underscore the complex interplay of factors shaping disparities in breast cancer care.
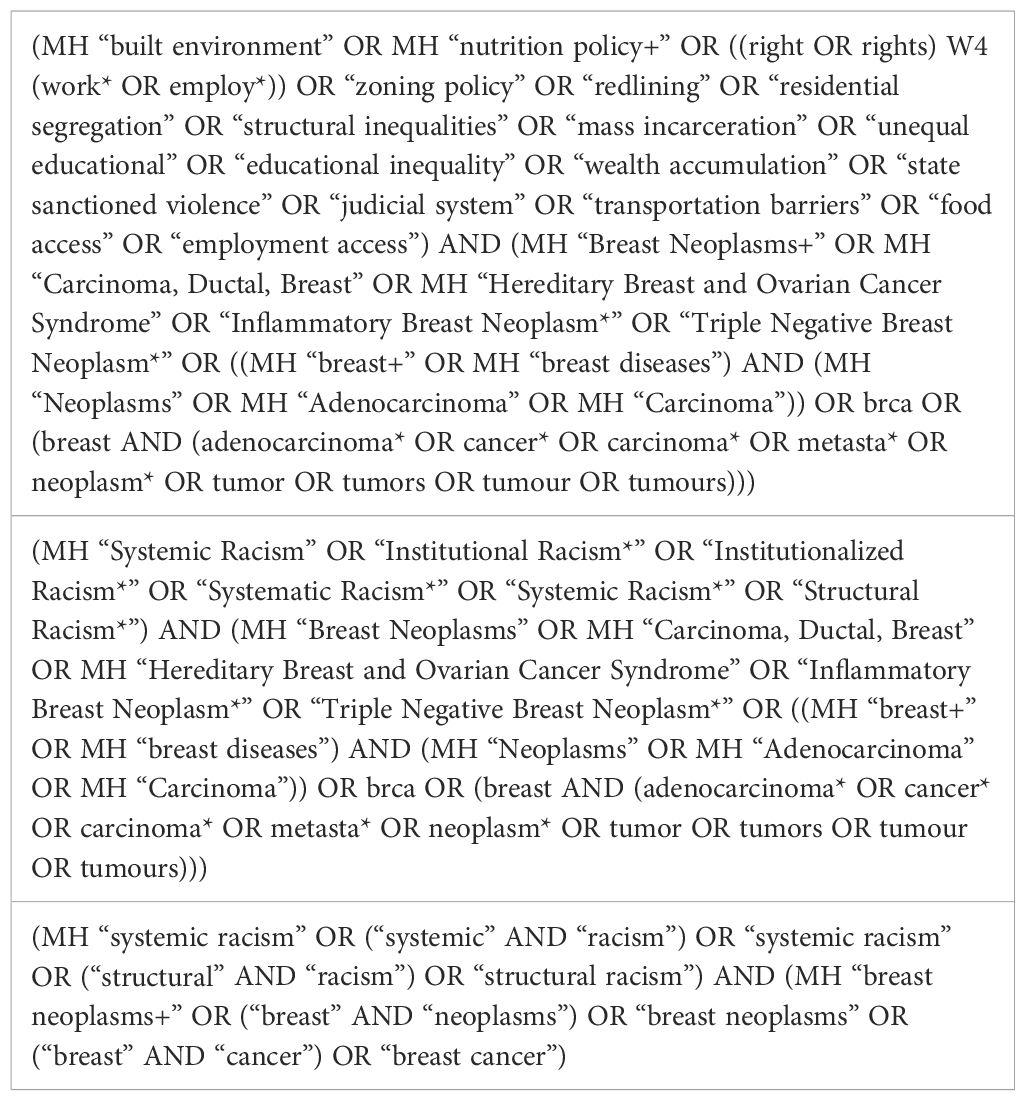
Structural racism functions at the macrolevel, encompassing multiple systems and creating widespread disparities The World Health Organization’s (WHO) framework of social determinants of health, (See Appendix Figure A), highlights the impact of structural racism on these determinants, which ultimately shapes disparities in health outcomes for marginalized communities, including those affected by breast cancer. It emphasizes the multifaceted factors that influence health outcomes, including individual, social, economic, and environmental conditions. Structural racism exerts profound influence through policies and practices such as residential segregation and redlining, which systematically disadvantage certain racial groups across multiple domains of SDOH. For example, redlining, which is a macrolevel policy, has long restricted material circumstances such as economic opportunities, educational resources, and access to quality healthcare in predominantly Black neighborhoods, which in turn contributes to adverse health outcomes such as delayed detection, diagnosis, and treatment for cancer survivors. These structural inequities result in poorer prognoses for breast cancer across multiple racial groups.
Structural racism is the overarching form of racism that encompasses various lower-level forms of racism. One prominent example is systematic racism, which operates within specific systems, such as healthcare or criminal justice, and contributes to cross-system inequalities. Disparities in healthcare coverage, underfunded schools in Black neighborhoods, and the over-policing of communities of color serve as examples of systematic racism. In contrast, institutional racism is more narrowly defined, affecting individuals within specific institutions or corporate policies. Historical practices like literacy tests for voting and criminal background checks for employment disproportionately impact African Americans are examples of this form of racism and lead to compounding disparities in healthcare. Experiencing racism across these multiple levels leads to health disparities through pathways including increased exposure to environmental pollution (44), restricted healthcare access (45), targeted marketing of harmful products (e.g., tobacco) (46), and biological effects from chronic stress, such as inflammation, and accelerated cellular aging (i.e., telomere shortening) (47).
Studies revealed varying impacts of structural racism on breast cancer outcomes. For example, racial bias in mortgage lending was associated with increased all-cause mortality hazard rates for Black women (15). Structural racism also affects non-Black women, such as increased odds of TNBC among both Black and white women in high-structural racism environments, though the impact was greater for Black women (20). In some cases, structural racism profoundly affects white communities as study by Collin et al. (19) found that the increased redlining was significantly associated with breast cancer mortality among non-Hispanic white women but less so among non-Hispanic Black women.
The relation between structural racism and breast cancer outcomes often depends on interacting factors such as race, ethnicity, neighborhood composition, and segregation levels. For instance, while Hispanic-white disparities in care diminished after adjusting for residential segregation (38), other studies, like Warner and Gomez (9), found no explanatory power of neighborhood racial composition and metropolitan segregation on cancer stage or survival differences between Black and white women. This underscores the complexity of structural racism’s impact on breast cancer quality of care, requiring an understanding of how multiple moderators interact. For example, Russell et al. (28) highlighted the significant impact of the interaction between race and MSA/MiSA area segregation on breast cancer-specific mortality rates.
This study has several limitations: First, the broad scope of measures leads to a lack of depth in understanding the impact mechanisms of each measure; however, this systematic review was able at identifying evidence for relationship between structural racism and breast cancer care outcomes. Second, we did not include assessments of bias for the studies included as many of the studies did not include it. Third, while this study may not provide the best framework for clinical guidelines, it directs attention to necessary future research.
Utilizing established frameworks, such as the Donabedian model for quality of care and the Healthy People 2030 SDOH framework, provides a structured approach to our analysis. This allows us to categorize and assess the various measures systematically. Our goal is to provide a comprehensive overview that can inform future empirical research and policy interventions. We recognize that our findings may prompt further investigation into specific mechanisms of action. By presenting a broad analysis, we hope to encourage researchers to delve deeper into individual factors and their interactions, ultimately leading to a more nuanced understanding of how structural racism affects breast cancer outcomes.
Recommendation and future research direction
Considering the substantial impact of residential segregation and redlining on breast cancer disparities, it is imperative to implement policy interventions that address housing and economic inequities (48). These interventions should focus on dismantling discriminatory lending practices, investing in marginalized communities, and expanding access to affordable housing. Additionally, community-based initiatives, educational programs, and economic empowerment strategies can play a crucial role in alleviating the healthcare barriers that contribute to these disparities.
Within the healthcare system, policy changes are essential for dismantling structural racism. It is critical to ensure equitable access to care, facilitate early detection, and provide high-quality treatment. Furthermore, promoting diversity in the healthcare workforce and implementing culturally competent care practices are essential components of a comprehensive strategy to address these disparities (49).
Future research should aim to enhance our understanding of how structural racism influences breast cancer outcomes, considering the complex interplay of individual and neighborhood factors. Moreover, investigations into other discriminatory social determinants of health (SDOH), including economic and educational disparities, are necessary to elucidate the root causes of breast cancer outcome disparities. This multidimensional approach will be vital for informing effective interventions and advancing health equity in breast cancer care.
Conclusion
The relationship between structural racism measures and breast cancer outcomes is inherently complex and require comprehensive models. It is crucial to extend the scope beyond current measures, encompassing a diverse range of structural determinants of health such as education, incarceration, and healthcare access. Additionally, there is a pressing need for models that address survivorship experiences, psychological distress, and the quality of care. Moreover, accounting for individual characteristics like race, ethnicity, and comorbidity and considering both small local and broader measures, and understanding their interactions, is essential. Furthermore, studies should delve into moderators of effect and elucidate the mechanisms through which structural measures impact outcomes, both socially and biologically. Lastly, there is a critical need for studies that rigorously test structural racism policy interventions to evaluate their impact on breast cancer outcomes. This comprehensive approach is necessary to address the multifaceted and interconnected factors contributing to disparities in breast cancer outcomes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
OA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MW: Writing – original draft, Writing – review & editing. AY: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. DeSantis CE, Ma J, Goding Sauer A, Newman LA, and Jemal A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. (2017) 67:439–48. doi: 10.3322/caac.21412, PMID: 28972651
2. Best AL, Roberson ML, Plascak JJ, Peterson CE, Rogers CR, Hastert TA, et al. Structural racism and cancer: calls to action for cancer researchers to address racial/ethnic cancer inequity in the United States. Cancer Epidemiol biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. (2022) 31:1243–6. doi: 10.1158/1055-9965.EPI-21-1179, PMID: 35642391
3. Braveman PA, Arkin E, Proctor D, Kauh T, and Holm N. Systemic and structural racism: definitions, examples, health damages, and approaches to dismantling. Health Aff (Millwood). (2022) 41:171–8. doi: 10.1377/hlthaff.2021.01394, PMID: 35130057
4. Social determinants of health - healthy people 2030. health.gov. https://health.gov/healthypeople/priority-areas/social-determinants-health.
5. Bailey ZD, Feldman JM, and Bassett MT. How structural racism works — Racist policies as a root cause of U.S. Racial health inequities. N Engl J Med. (2021) 384:768–73. doi: 10.1056/NEJMms2025396, PMID: 33326717
6. Geneviève LD, Martani A, Shaw D, Elger BS, and Wangmo T. Structural racism in precision medicine: leaving no one behind. BMC Med Ethics. (2020) 21:17. doi: 10.1186/s12910-020-0457-8, PMID: 32075640
7. Radley DC, Baumgartner JC, Collins SR, Zephyrin L, and Schneider EC. Achieving racial and ethnic equity in US health care. New York, NY: The Commonwealth Fund. (2021).
8. Gallicchio L, Tonorezos E, de Moor JS, Elena J, Farrell M, Green P, et al. Evidence gaps in cancer survivorship care: A report from the 2019 national cancer institute cancer survivorship workshop. J Natl Cancer Inst. (2021) 113:1136–42. doi: 10.1093/jnci/djab049, PMID: 33755126
9. Health, income, & Poverty: where we are & what could help. Health Affairs Health Policy Brief. doi: 10.1377/hpb20180817.901935
10. Pager D and Shepherd H. The sociology of discrimination: racial discrimination in employment, housing, credit, and consumer markets. Annu Rev Sociol. (2008) 34:181–209. doi: 10.1146/annurev.soc.33.040406.131740, PMID: 20689680
11. Polanco-Roman L, Danies A, and Anglin DM. Racial discrimination as race-based trauma, coping strategies and dissociative symptoms among emerging adults. Psychol Trauma Theory Res Pract Policy. (2016) 8:609–17. doi: 10.1037/tra0000125, PMID: 26963957
12. Vines AI, Ward JB, Cordoba E, and Black KZ. Perceived racial/ethnic discrimination and mental health: a review and future directions for social epidemiology. Curr Epidemiol Rep. (2017) 4:156–65. doi: 10.1007/s40471-017-0106-z, PMID: 28920011
13. Bonilla-Silva E. Rethinking racism: toward a structural interpretation. Am Sociol Rev. (1997) 62:465–80. doi: 10.2307/2657316
14. Covidence. Covidence - Better systematic review management. Available online at: https://www.covidence.org/ (Accessed December 15, 2023).
15. Beyer KMM, Zhou Y, Matthews K, Bemanian A, Laud PW, and Nattinger AB. New spatially continuous indices of redlining and racial bias in mortgage lending: links to survival after breast cancer diagnosis and implications for health disparities research. Health Place. (2016) 40:34–43. doi: 10.1016/j.healthplace.2016.04.014, PMID: 27173381
16. Beyer KMM, Zhou Y, Laud PW, McGinley EL, Yen TWF, Jankowski C, et al. Mortgage lending bias and breast cancer survival among older women in the United States. J Clin Oncol. (2021) 39:2749–57. doi: 10.1200/JCO.21.00112, PMID: 34129388
17. Bikomeye JC, Zhou Y, McGinley EL, Canales B, Yen TWF, Tarima S, et al. Historical redlining and breast cancer treatment and survival among older women in the United States. JNCI J Natl Cancer Inst. (2023) 115:652–61. doi: 10.1093/jnci/djad034, PMID: 36794919
18. Canales B, Laud PW, Tarima S, Zhou Y, Bikomeye JC, McGinley EL, et al. Isolation and survival: The impact of local and MSA isolation on survival among non-Hispanic Black women diagnosed with breast cancer in the United States using a SEER-Medicare cohort. Health Place. (2023) 83:103090. doi: 10.1016/j.healthplace.2023.103090, PMID: 37531804
19. Collin LJ, Gaglioti AH, Beyer KM, Zhou Y, Moore MA, Nash R, et al. Neighborhood-level redlining and lending bias are associated with breast cancer mortality in a large and diverse metropolitan area. Cancer Epidemiol Biomarkers Prev. (2021) 30:53–60. doi: 10.1158/1055-9965.EPI-20-1038, PMID: 33008873
20. Eldridge L and Berrigan D. Structural racism and triple-negative breast cancer among black and white women in the United States. Health Equity. (2022) 6:116–23. doi: 10.1089/heq.2021.0041, PMID: 35261938
21. Goel N, Westrick AC, Bailey ZD, Hernandez A, Balise RR, Goldfinger E, et al. Structural racism and breast cancer-specific survival: impact of economic and racial residential segregation. Ann Surg. (2022) 275:776. doi: 10.1097/SLA.0000000000005375, PMID: 35081560
22. Krieger N, Wright E, Chen JT, Waterman PD, Huntley ER, and Arcaya M. Cancer stage at diagnosis, historical redlining, and current neighborhood characteristics: breast, cervical, lung, and colorectal cancers, massachusetts, 2001–2015. Am J Epidemiol. (2020) 189:1065–75. doi: 10.1093/aje/kwaa045, PMID: 32219369
23. Miller-Kleinhenz JM, Moubadder L, Beyer KM, Zhou Y, Gaglioti AH, Collin LJ, et al. Redlining–associated methylation in breast tumors: the impact of contemporary structural racism on the tumor epigenome. Front Oncol. (2023) 13:1154554. doi: 10.3389/fonc.2023.1154554, PMID: 37621676
24. Ojinnaka CO, Luo W, Ory MG, McMaughan D, and Bolin JN. Disparities in surgical treatment of early-stage breast cancer among female residents of Texas: the role of racial residential segregation. Clin Breast Cancer. (2017) 17:e43–52. doi: 10.1016/j.clbc.2016.10.006, PMID: 27889438
25. Plascak JJ, Beyer K, Xu X, Stroup AM, Jacob G, and Llanos AAM. Association between residence in historically redlined districts indicative of structural racism and racial and ethnic disparities in breast cancer outcomes. JAMA Netw Open. (2022) 5:e2220908. doi: 10.1001/jamanetworkopen.2022.20908, PMID: 35802373
26. Poulson MR, Beaulieu-Jones BR, Kenzik KM, Dechert TA, Ko NY, Sachs TE, et al. Residential racial segregation and disparities in breast cancer presentation, treatment, and survival. Ann Surg. (2021) 273(1):3–9. doi: 10.1097/SLA.0000000000004451, PMID: 32889878
27. Pruitt SL, Lee SJC, Tiro JA, Xuan L, Ruiz JM, and Inrig S. Residential racial segregation and mortality among black, white, and Hispanic urban breast cancer patients in Texas, 1995 to 2009. Cancer. (2015) 121(11):1845–55. doi: 10.1002/cncr.29282, PMID: 25678448
28. Russell EF, Kramer MR, Cooper HLF, Gabram-Mendola S, Senior-Crosby D, and Jacob Arriola KR. Metropolitan area racial residential segregation, neighborhood racial composition, and breast cancer mortality. Cancer Causes Control. (2012) 23:1519–27. doi: 10.1007/s10552-012-0029-4, PMID: 22825071
29. Warner ET and Gomez SL. Impact of neighborhood racial composition and metropolitan residential segregation on disparities in breast cancer stage at diagnosis and survival between black and white women in California. J Community Health. (2010) 35:398–408. doi: 10.1007/s10900-010-9265-2, PMID: 20358266
30. Wright E, Waterman PD, Testa C, Chen JT, and Krieger N. Breast cancer incidence, hormone receptor status, historical redlining, and current neighborhood characteristics in Massachusetts, 2005-2015. JNCI Cancer Spectr. (2022) 6:pkac016. doi: 10.1093/jncics/pkac016, PMID: 35603845
31. Lubarsky M, Hernandez AE, Collie BL, Westrick AC, Thompson C, Kesmodel SB, et al. Does structural racism impact receipt of NCCN guideline-concordant breast cancer treatment? Breast Cancer Res Treat. (2024) 206(3):509–17. doi: 10.1007/s10549-024-07245-6, PMID: 38809304
32. Pittell H, Calip GS, Pierre A, Ryals CA, and Guadamuz JS. Racialized economic segregation and inequities in treatment initiation and survival among patients with metastatic breast cancer. Breast Cancer Res Treat. (2024) 206:411–23. doi: 10.1007/s10549-024-07319-5, PMID: 38702585
33. Nabi O, Liu Y, Struthers J, and Lian M. The role of residential segregation in treatment and outcomes of ductal carcinoma in situ of the breast. Cancer Epidemiol Biomarkers Prev. (2024) 33(12):1633–9. doi: 10.1158/1055-9965.EPI-24-0488/749112/The-Role-of-Residential-Segregation-in-Treatment?redirectedFrom=fulltext, PMID: 39292206
34. Michaels EK, Canchola AJ, Beyer KMM, Zhou Y, Shariff-Marco S, and Gomez SL. Home mortgage discrimination and incidence of triple-negative and Luminal A breast cancer among non-Hispanic Black and non-Hispanic White females in California, 2006–2015. Cancer Causes Control. (2022) 33:727–35. doi: 10.1007/s10552-022-01557-y, PMID: 35113296
35. Reeder-Hayes KE, Jackson BE, Kuo TM, Baggett CD, Yanguela J, LeBlanc MR, et al. Structural racism and treatment delay among black and white patients with breast cancer. J Clin Oncol. (2024) 42:3858–66. doi: 10.1200/JCO.23.02483, PMID: 39106434
36. Bonner SN, Clark C, Keating NL, Kouri EM, and Freedman RA. Examining associations of racial residential segregation with patient knowledge of breast cancer and treatment receipt. Clin Breast Cancer. (2019) 19:178–87.e3. doi: 10.1016/j.clbc.2018.12.001, PMID: 30685264
37. Dai D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place. (2010) 16:1038–52. doi: 10.1016/j.healthplace.2010.06.012, PMID: 20630792
38. Haas JS, Earle CC, Orav JE, Brawarsky P, Keohane M, Neville BA, et al. Racial segregation and disparities in breast cancer care and mortality. Cancer. (2008) 113:2166–72. doi: 10.1002/cncr.23828, PMID: 18798230
39. Krieger N, Singh N, and Waterman PD. Metrics for monitoring cancer inequities: residential segregation, the Index of Concentration at the Extremes (ICE), and breast cancer estrogen receptor status (USA, 1992–2012). Cancer Causes Control. (2016) 27:1139–51. doi: 10.1007/s10552-016-0793-7, PMID: 27503397
40. Moss JL, Ehrenkranz R, Perez LG, Hair BY, and Julian AK. Geographic disparities in cancer screening and fatalism among a nationally representative sample of US adults. J Epidemiol Community Health. (2019) 73:1128–35. doi: 10.1136/jech-2019-212425, PMID: 31615890
41. Oka M, Williams F, and Whiteside M. Comparing proxy and formal measures of county-level racial isolation in race-stratified models: A case study in Tennessee, 2005–2014. SSM - Popul Health. (2022) 19:101146. doi: 10.1016/j.ssmph.2022.101146, PMID: 35756544
42. Plascak JJ, Llanos AAM, Qin B, Chavali L, Lin Y, Pawlish KS, et al. Visual cues of the built environment and perceived stress among a cohort of black breast cancer survivors. Health Place. (2021) 67:102498. doi: 10.1016/j.healthplace.2020.102498, PMID: 33383367
43. Miller-Kleinhenz JM, Barber LE, Maliniak ML, Moubadder L, Bliss M, Streiff MJ, et al. Historical redlining, persistent mortgage discrimination, and race in breast cancer outcomes. JAMA Netw Open. (2024) 7:e2356879. doi: 10.1001/jamanetworkopen.2023.56879, PMID: 38376843
44. Morello-Frosch R and Lopez R. The riskscape and the color line: Examining the role of segregation in environmental health disparities. Environ Res. (2006) 102:181–96. doi: 10.1016/j.envres.2006.05.007, PMID: 16828737
45. McGee-Avila JK, Richmond J, Henry KA, Stroup AM, and Tsui J. Disparities in geospatial patterns of cancer care within urban counties and structural inequities in access to oncology care. Health Serv Res. (2023) 58:152–64. doi: 10.1111/1475-6773.14182, PMID: 37208901
46. Yerger VB, Przewoznik J, and Malone RE. Racialized geography, corporate activity, and health disparities: tobacco industry targeting of inner cities. J Health Care Poor Underserved. (2007) 18:10–38. doi: 10.1353/hpu.2007.0120, PMID: 18065850
47. Williams DR and Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. (2009) 32:20–47. doi: 10.1007/s10865-008-9185-0, PMID: 19030981
48. Fan Q, Nogueira L, Yabroff KR, Hussaini SMQ, and Pollack CE. Housing and cancer care and outcomes: A systematic review. JNCI J Natl Cancer Inst. (2022) 114:1601–18. doi: 10.1093/jnci/djac173, PMID: 36073953
49. Pallok K, Maio FD, and Ansell DA. Structural racism — A 60-year-old black woman with breast cancer. N Engl J Med. (2019) 380:1489–93. doi: 10.1056/NEJMp1811499, PMID: 30995369
50. Moher D, Liberati A, Tetzlaff J, Altman DG, and PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6(7):e1000097. doi: 10.1371/journal.pmed.1000097, PMID: 19621072
51. Poulson M, Neufeld MY, Dechert T, Allee L, and Kenzik KM. Historic redlining, structural racism, and firearm violence: A structural equation modeling approach. Lancet Reg Health Am. (2021) 3:100052. doi: 10.1016/j.lana.2021.100052, PMID: 34888540
Appendix
Summary of Residential segregation measures
The assessment of residential segregation in these studies employed diverse measures including the five traditional dimensions of residential segregation: evenness, exposure, clustering, concentration, and centralization as well as new small area measures such as Location Quotient measure, the Index of Concentration at Extreme and the local exposure and isolation measures.
Six studies used the Isolation Index which is an exposure measure and one used local isolation measure. The isolation index measures the degree of potential contact between groups within neighborhoods of a city. The Isolation Index evaluates the exposure of minority members to either only other minority members or to members of the majority group. Index values range from 0 to 1, with exposure representing the average probability of contact between Blacks and whites at the neighborhood level.
One study used the Delta Index, which is a component of the Concentration Index, represents the relative amount of physical space occupied by a minority group in each geographic area. The Concentration Index assesses the population density of Blacks across the metropolitan area relative to the density of white. The index measures the relative amount of physical space occupied by a minority group in the urban environment. The Index of Concentration at Extreme measures the extent to which minority members are exposed exclusively to other minority members or to members of the majority group. Index values range from 0 to 1, indicating the proportion of minority members that would need to move across neighborhoods to achieve a uniform density.
One study used Spatial Proximity which is a clustering index. The index measures the extent to which areas inhabited by minority members adjoin one another in space. Spatial Proximity, or clustering, measures the degree to which minority residential areas are adjacent to one another in physical space. Index values range from 1.0 (no difference in clustering) to greater than 1.0 (minority group members living closer to each other than to majority members). Clustering assesses the effect of “ghettoization” or the degree to which predominantly Black neighborhoods are contiguous to predominantly white neighborhoods.
Three studies utilized the Dissimilarity Index, one study employed Theil’s Information Theory Index (H index), and one study utilized Gini, all of which are measures assessing the ‘evenness’ of residential segregation. These indices refer to the unequal distribution of social groups across areal units of an urban area. The Racial Dissimilarity Index measures the proportion of minority members that would need to change residence for each unit of analysis to have the same distribution as the larger overall area, ranging from 0 (no segregation) to 1 (complete segregation). Evenness assesses the degree to which each neighborhood mirrors the distribution of Blacks to whites as in the metropolitan area overall. Another measure is the Theil’s Information Theory Index (H index). This index gauges local and regional diversity, evaluating the evenness of racial group distribution across neighborhoods, ranging from 0 (completely even or integrated distribution) to 1 (completely segregated). It approximates the proportion of the minority group that would need to relocate to achieve an even distribution within the region.
One study used Relative Centralization. Relative Centralization indicates the proportion of the minority population that would need to change residence to match the centralization level of the majority group. Index values range between −1.0 and 1.0, with positive values indicating that minority group members reside closer to the city center than majority members. The centralization measures the degree to which a group is located near the center of an urban area. Centralization measures how predominantly Black neighborhoods are in relation to the metropolitan area’s center versus its suburbs. Additionally, three studies used the Location Quotient measure.
The Location Quotient (LQ) for racial residential segregation is a comparative measure, assessing the relative proportions of a minority group within a census tract compared to the proportion of that group in the larger Metropolitan Statistical Area (MSA), facilitating the evaluation of disparities in the racial composition of an individual’s neighborhood in relation to the broader MSA.
Redlining measures:
Two measures have been used for redlining: the redlining index and Homeowners’ Loan Corporation (HOLC) grade classification. The redlining index was created by expanding adaptive spatial filters until at least five Black and five white mortgage applicants were identified. Instead of calculating solely within the filter, the odds of mortgage application denial were estimated for individuals inside versus outside the filter. The resulting index, centered around 1, indicates whether an area is equally likely (1), more likely (>1), or less likely (<1) to face mortgage denials compared to other regions in the study area. The original HOLC maps were used to compute the percentage of area in the original maps of each city that were graded A, B, C, or D (corresponding to green = “Best”; blue = “Still Desirable”; yellow = “Declining”; and red = “Hazardous” designations, respectively).
Table A: Search Strategy-PubMed.
Table B: Search Strategy-Embase.
Table C: Search Strategy-CINAHL.
Keywords: breast cancer, structural racism, SDOH, quality of care, cancer care
Citation: Abdelhadi O, Williams M and Yan A (2025) Structural racism as a leading cause of racial disparities in breast cancer quality of care outcomes: a systematic review. Front. Oncol. 15:1562672. doi: 10.3389/fonc.2025.1562672
Received: 17 January 2025; Accepted: 19 June 2025;
Published: 16 July 2025.
Edited by:
Nabil Adam, Rutgers, The State University of New Jersey, United StatesReviewed by:
Saber A. Amin, University of Nebraska Medical Center, United StatesFouad Nahhat, Mayo Clinic Arizona, United States
Copyright © 2025 Abdelhadi, Williams and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ola Abdelhadi, b2FiZGVsaGFkaUB1Y2RhdmlzLmVkdQ==
 Ola Abdelhadi
Ola Abdelhadi Michelle Williams
Michelle Williams