- 1Department of General Surgery, Beidahuang Group Hongxinglong Hospital, Shuangyashan, Heilongjiang, China
- 2Department of General Surgery, Linyi Maternity and Child Health Care Hospital, Linyi, Shandong, China
- 3Department of Pathology, Beidahuang Group Hongxinglong Hospital, Shuangyashan, Heilongjiang, China
- 4Department of Medical Imaging, Linyi Maternity and Child Health Care Hospital, Linyi, Shandong, China
- 5Department of Gastroenterology, Linyi People’s Hospital, Linyi, Shandong, China
Primary leiomyosarcoma of the breast is an extremely rare tumor originating from the mesenchymal tissue of the breast. The clinical data of a case of primary leiomyosarcoma of the breast admitted to our hospital on September 11, 2024 were analyzed. A 58-year-old woman had a right breast mass for a week. Physical examination revealed an irregular mass at approximately 2–3 points in the right upper quadrant of the breast. Laboratory tests showed normal results for the tumor marker CA153. Color Doppler ultrasound considered solid nodules (BI-RADS Class 4b). Modified radical mastectomy and tertiary axillary lymph node dissection was performed on 2024-9-13, and the patient underwent adjuvant chemotherapy after surgery and recovered well. Pathological findings were reported one week after surgery: breast leiomyosarcoma. This article presents the diagnosis and treatment of primary leiomyosarcoma of breast through a clinical case, which provides a reference for clinicians. This case highlights the importance of pathological examination in the diagnosis of rare tumors, and suggests the need to combine imaging, laboratory examination and pathological findings to make a comprehensive judgment of breast masses.
1 Introduction
Primary breast sarcoma is a rare tumor, accounting for less than 1% of all breast malignancies and less than 5% of all soft tissue sarcomas (1–3), while primary leiomyosarcoma of breast is an extremely rare subtype of breast sarcoma, accounting for less than 0.0006% of all breast malignancies. Fewer than 80 cases have been reported in the literature so far (4–6). There are even fewer reports in medical journals. At present, no specific treatment plan has been determined. To determine the appropriate diagnosis and treatment management plan, we evaluated this case and reviewed relevant literature to discuss its diagnosis, treatment and prognosis.
2 Case description
2.1 Patient information
A 58-year-old woman presented with “a right breast mass for a week.” A week ago, the patient inadvertently found an irregular tumor on the right breast, about the size of an egg, without redness, swelling or pain, nipple discharge or nipple invagination, and normal skin on the surface of the tumor. Previously in good health. Menopause about 5 years.
2.2 Clinical findings
Physical examination: An irregular mass, about 4.0 cm × 2.0 cm × 2.0 cm in size, was visible at about 2–3 points in the upper quadrant of the right inner breast about 1.0cm from the areola, with tough quality, clear boundary, moderate motion, and no tenderness. A 1.0 cm × 1.0 cm circular mass can be found in the right axilla. Lymph node enlargement is considered.
2.3 Timeline
The patient had no family or significant past history of breast cancer.
2.4 Diagnostic assessment
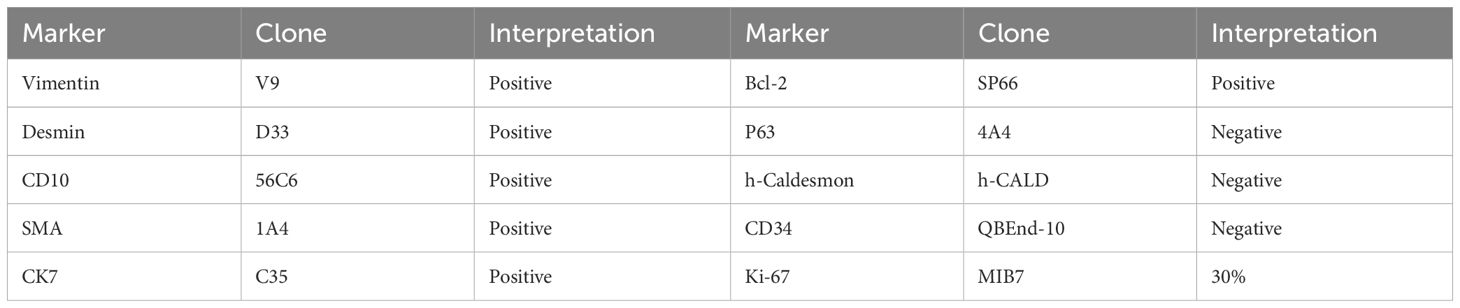
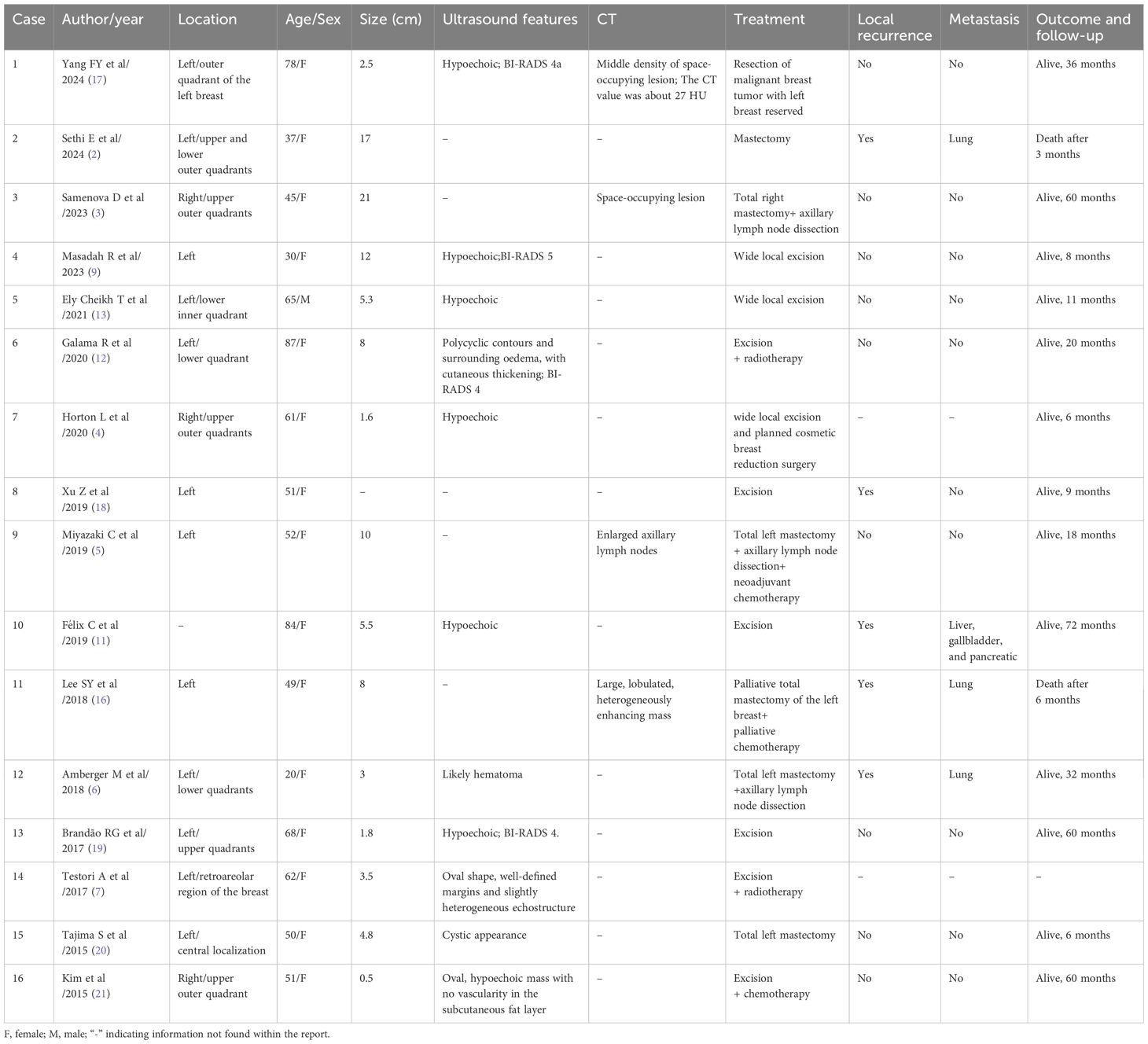
B-ultrasound examination showed that a low-echo nodule of about 3.8 cm × 2.3 cm × 2.8 cm in size was visible at about 2–3 points in the upper quadrant of the right mammary gland, with clear boundaries, uneven internal echo, irregular shape, lobed shape, and rich blood flow signals could be detected. Multiple lymph node echoes can be seen in the right axilla, with clear boundary of skin and pulp, the larger one is about 1.6 cm × 0.68 cm. Ultrasound results showed solid nodules in the upper quadrant of the right internal breast (BI-RADS 4b) (Figure 1). Preoperative completed lung CT showed that there was a tumor on the right breast, about 4.0 cm × 2.0 cm× 2.0 cm in size, with a CT value of about 17 HU, and the boundary was acceptable (Figure 2). Laboratory examination results: Blood routine: WBC 8.26 × 109/L, tumor marker CA153 5.98 U/mL. Typically, these patients do not have abnormal serological values or tumor markers, as was the case in this case (7).
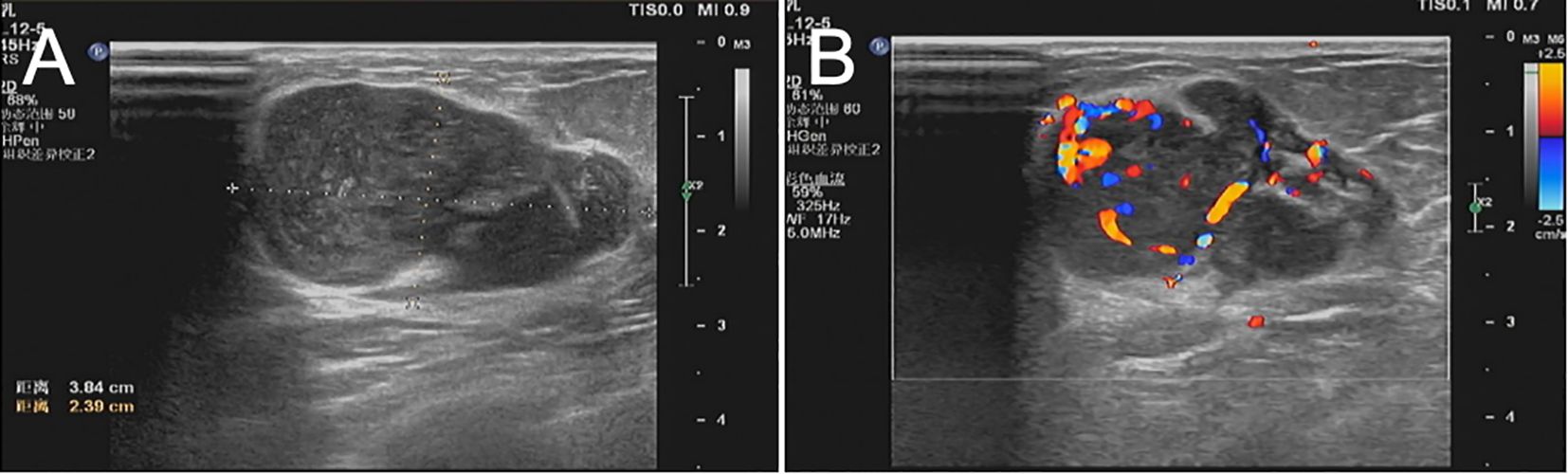
Figure 1. (A, B) Ultrasonography showed that the hypoechoic nodules of 3.8 cm × 2.3 cm × 2.8 cm in size were visible at about 2–3 points in the upper quadrant of the right mammary gland, with clear boundaries, less uniform internal echo, irregular shape, lobed shape, and rich blood flow signals could be detected. It was classified via ultrasonography in Breast Imaging-Reporting and Data System (BI-RADS 4b) category.
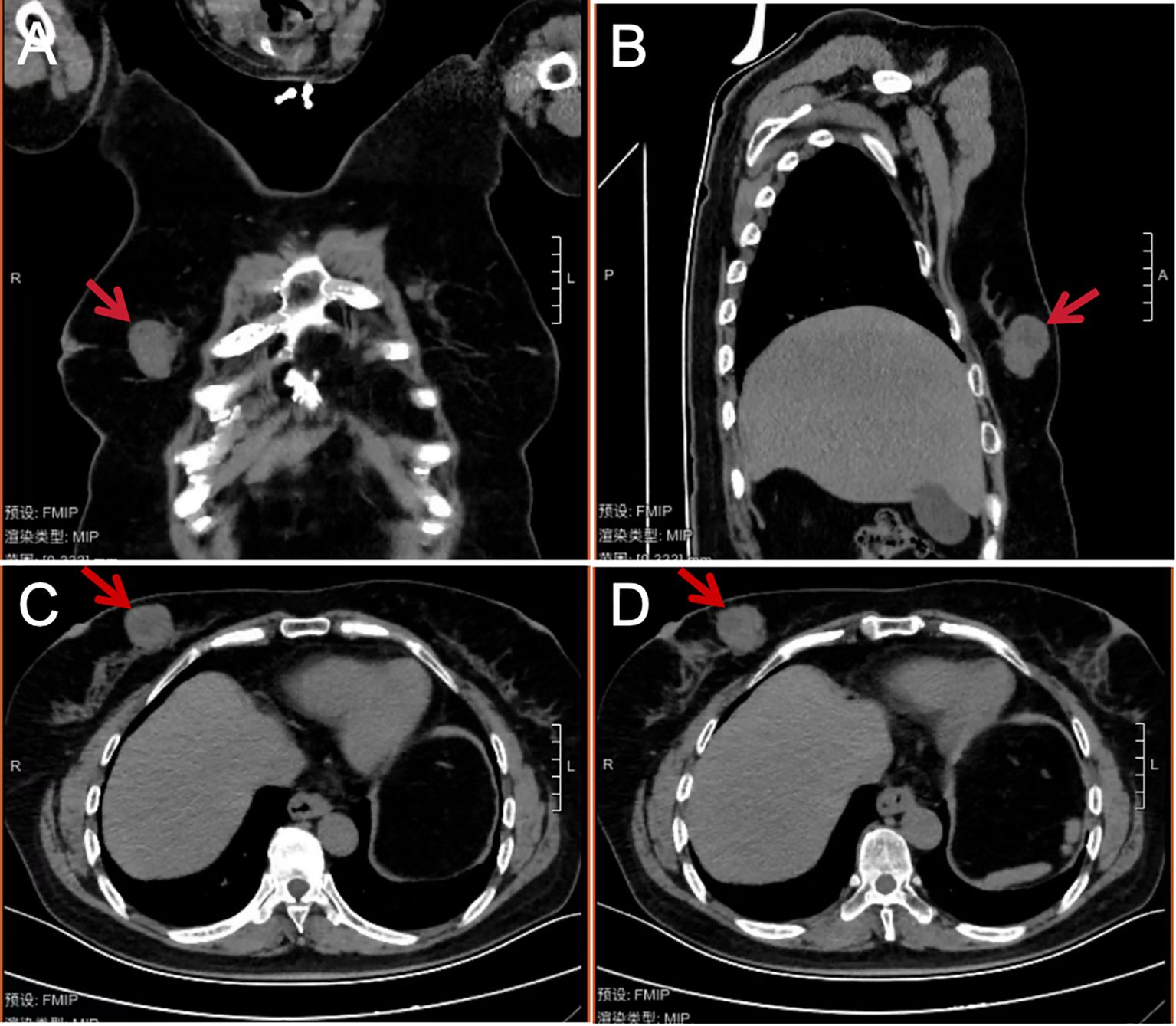
Figure 2. Coronal (A), sagittal (B), and cross-sectional (C, D) chest CT images of the patient in mediastinal window view before breast tumor resection. A soft tissue mass (shown by the red arrow at about 3 points) can be seen on the medial side of the right mammary gland. The density is not uniform, the shape is not regular, the lobulated mass can be seen, the size is about 4.0 cm × 2.0 cm × 2.0 cm, the CT value is about 17 HU, and the boundary is clear.
2.5 Therapeutic intervention
After improving the preoperative examination, the patient met the surgical indications and had no obvious contraindications. The patient underwent surgical treatment on the third day after admission and underwent resection of breast masses. The rapid pathological return during the operation was malignant tumor of the mesenchymal tissue of the breast. Combined with the preoperative ultrasound report of the patient, multiple swollen lymph nodes in the right axilla were evaluated, and modified radical mastectomy and tertiary axillary lymph node dissection were performed. Ensure that the width of the cutting edge is at least 3 cm. Two indwelling drainage tubes.
2.6 Follow-up and outcomes
Conventional treatment was given after surgery. Postoperative pathological findings: The tumor cells were arranged in parallel, fascicular-like interwoven arrangement, accompanied by mucoid degeneration and more nuclear division. The tumor section was grayish white, and the nipple and incisal margin were negative. Diagnosis: Right breast leiomyosarcoma, highly differentiated tumor volume 5.0 cm × 2.0 cm × 1.0 cm, accompanied by mucinous degeneration, nuclear fission image 24/10 HPE, no clear invasion of vascular and divine realm. Right subaxillary lymph node 0/26 (–) (Figure 3).
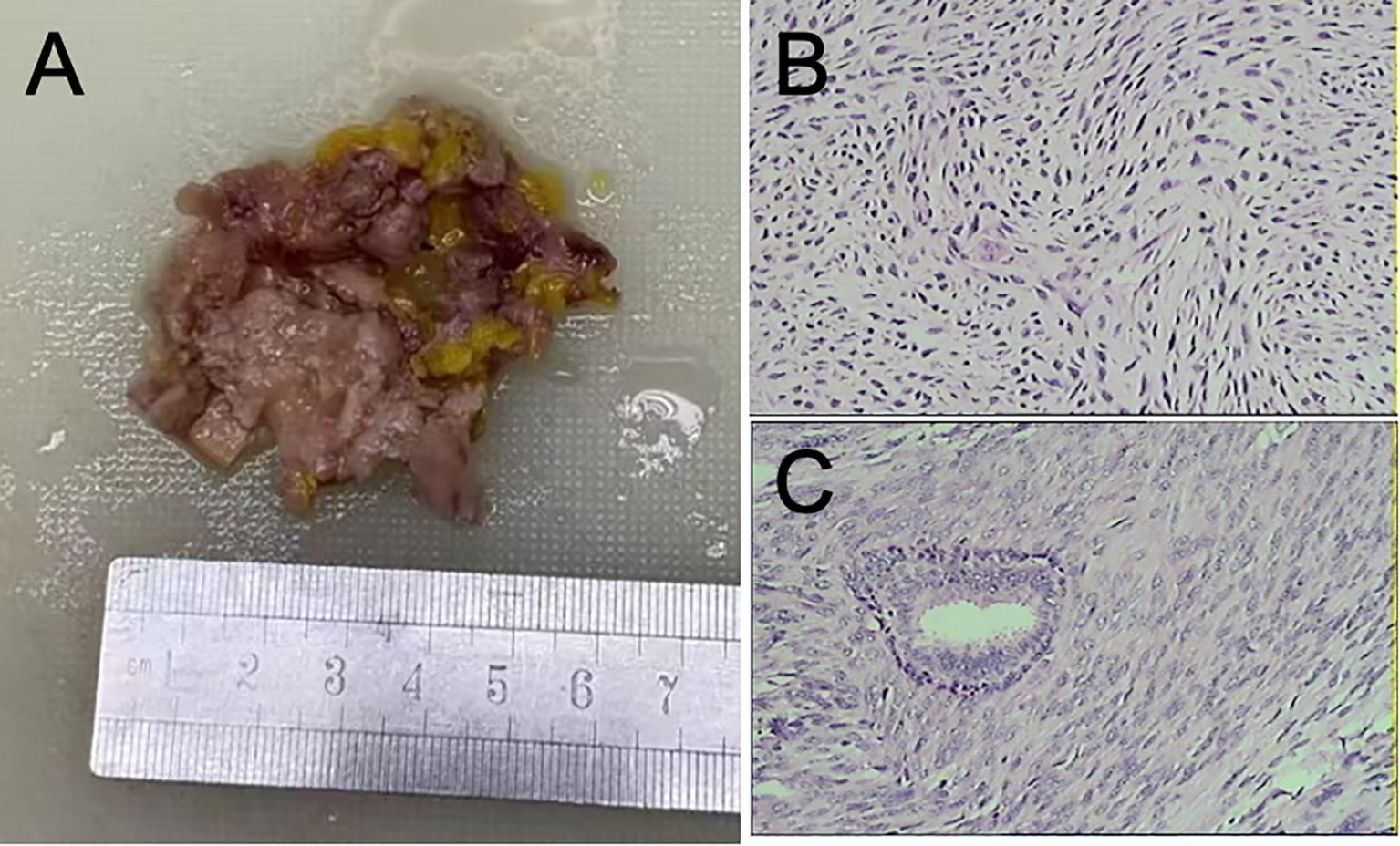
Figure 3. (A) Right breast mass, volume: 6.0 × 5.0 × 1.2 cm3, section gray, intraoperative freeze pathology. (B, C) Photomicrographs of the tumor. The tumor cells were arranged in parallel, fascicular interlace, accompanied by mucoid degeneration and more nuclear division. Pathological diagnosis: right breast leiomyosarcoma, highly differentiated, tumor volume 5.0 cm × 2.0 cm × 1.0 cm3, accompanied by mucinous degeneration, mitotic image 24/10 HPE, no clear invasion of vascular and divine realm. Right subaxillary lymph node 0/26 (HE, 40×).
Given the morphological diagnosis of sarcoma, a large immunohistochemistry (IHC) panel was applied to reach a definitive diagnosis (Table 1). Vimentin, Desmin, and CD10 were strongly positive in tumor cells, and SMA, CK7, and Bcl-2 showed patchy strong positivity. P63, h-Caldesmon, and CD34 were negative. The Ki67 proliferation index was 30% (Figure 4). The clinical stage of this case follows the standard TNM stage of breast malignancy (6, 8), which is T2N0M0.
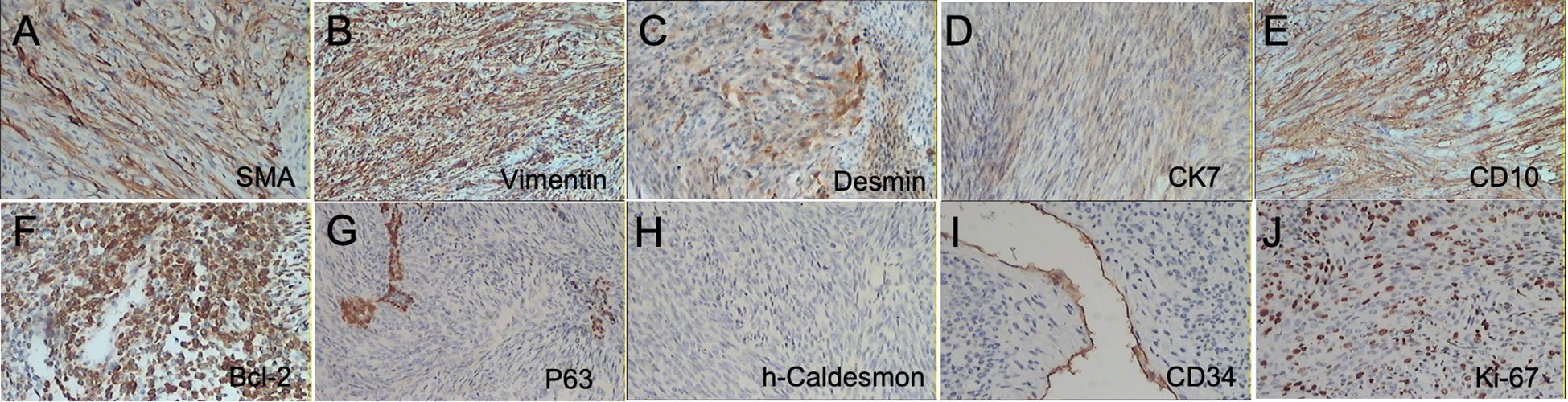
Figure 4. Immunohistochemical staining was positive for SMA, Vimentin, Desmin, CK7, CD10, and Bcl-2 (A–F) and negative for P63, h-Caldesmon, and CD34 (G–I), respectively. (J) Ki67 -30% (10×).
Postoperative follow-up was conducted on the patient, and the patient recovered well after surgery. The drainage tube was removed and stitches were removed on the 15th day after surgery. There was no dysfunction or numbness in the affected upper limb, and the muscle strength was normal. Chemotherapy is recommended.
3 Discussion
Breast leiomyosarcoma is an uncommon tumor. They may originate from smooth muscle cells or stromal mesenchymal cells in the lining of blood vessels. In histopathological evaluation, immunohistochemical staining as an adjunct is essential to distinguish leiomyosarcoma from other tumors and soft tissue sarcomas. These tumors are usually Desmin and SMA positive and S100 and CKpan negative (6, 9–11). In the treatment options for primary leiomyosarcoma, surgery is generally considered to be the main treatment option (12). Previous studies recommend at least 3 cm negative incisal margin for optimal results (4, 9, 13). Since there have been no reported cases of lymphatic metastasis via hematogenous route, axillary lymph node dissection is not necessary if leiomyosarcoma can be confirmed before or during surgery (6, 8, 9, 14, 15). In this case, lymph node enlargement was considered by preoperative ultrasound, and metastasis could not be clearly ruled out, so lymph node dissection was performed. So we did not use a wide local excision. However, postoperative pathology reported that lymph nodes showed increased reactivity and no metastasis. Such diseases are often further treated with radiotherapy and chemotherapy after surgery. The patient went to the oncology department for chemotherapy after surgery. AC chemotherapy regimen, including doxorubicin and cyclophosphamide, was administered every 21 days for a total of 4 courses. Nevertheless, the patient did not complain of discomfort, and there were no adverse and unanticipated events during the treatment. The patient had been followed up for six months, and no recurrence or metastasis had been detected. Long-term follow-up of this disease is important because a proportion of these tumors have been reported to recur after treatment (2, 16). We reviewed the cases reported in the English literature in the past 10 years, as shown in Table 2.
4 Conclusion
Primary Leiomyosarcoma of the Breast is an extremely rare malignant tumor of the breast, usually originating in blood vessels, papillary smooth muscle or leiomyoma malignant transformation, mainly through blood metastasis, local lymph node involvement is rare. Pathological examination is the key to diagnosis, typical manifestations are spindle cells, nuclear atypia, and more mitotic signs, and the expression of immunohistochemical markers such as SMA and Desmin is helpful to distinguish from other tumor types.
Surgical resection is the primary treatment, with a negative margin and usually without axillary lymph node dissection. The role of chemotherapy and radiotherapy is unclear and needs to be evaluated on an individual basis. Although the prognosis is superior to other breast sarcomas, the risk of local recurrence and distant metastasis still requires long-term follow-up. At present, there is no uniform diagnosis and treatment standard, and the prognostic factors are not fully defined. Since the cases are rare and mostly reported as individual cases, further accumulation and analysis of patient data are needed to optimize treatment strategies, clarify disease characteristics, and provide a more powerful guidance basis for clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The requirement of ethical approval was waived by The Ethics Committee of the Linyi Maternity and Child Health Care Hospital for the studies on humans because written informed consent was obtained from the minor’s legal guardian, for the publication of any potentially identifiable images or data included in this article. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. The human samples used in this study were acquired from a by- product of routine care or industry. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HL: Writing – original draft, Writing – review & editing. HR: Conceptualization, Data curation, Formal analysis, Writing – original draft. SZ: Data curation, Formal analysis, Methodology, Writing – original draft. GD: Methodology, Writing – original draft. PT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are also very thankful for the editors’ and reviewers’ valuable suggestions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Palassini E, Baldi GG, Ciniselli CM, Gennaro M, Gronchi A, Sangalli C, et al. Outcome improvement with chemotherapy and radiotherapy in primary, localized, radiation-associated angiosarcoma of the breast region: a retrospective case series analysis. Esmo Open. (2024) 9:103474. doi: 10.1016/j.esmoop.2024.103474
2. Sethi E, Misra S, and Ahuja A. Primary leiomyosarcoma with osteosarcomatous differentiation of the breast. Autops Case Rep. (2024) 14:e2024476. doi: 10.4322/acr.2024.476
3. Samenova D, Midlenko A, Khamzina Y, Kaldybayev M, and Khamzina S. Primary leiomyosarcoma of the breast: a successful surgical treatment in a 45-year-old woman. Am J Case Rep. (2023) 24:e939437. doi: 10.12659/AJCR.939437
4. Horton L, Wohlfeil M, Al-Kourainy N, and Choi L. Rare case of primary leiomyosarcoma of the breast treated with wide local excision and planned cosmetic breast reduction surgery. BMJ Case Rep. (2020) 13:e236013. doi: 10.1136/bcr-2020-236013
5. Miyazaki C, Shiozawa M, Koike R, Ogihara K, Sasaki Y, Shiba S, et al. Neoadjuvant chemotherapy for primary sarcoma of the breast: a case report. J Med Case Rep. (2019) 13:289. doi: 10.1186/s13256-019-2197-2
6. Amberger M, Park T, Petersen B, and Baltazar GA. Primary breast leiomyosarcoma with metastases to the lung in a young adult: case report and literature review. Int J Surg Case Rep. (2018) 47:34–7. doi: 10.1016/j.ijscr.2018.04.010
7. Testori A, Meroni S, Voulaz E, Alloisio M, De Sanctis R, Bossi P, et al. Primary breast leiomyosarcoma and synchronous homolateral lung cancer: a case report. J Thorac Dis. (2017) 9:E1054–9. doi: 10.21037/jtd.2017.10.98
8. Fujita N, Kimura R, Yamamura J, Akazawa K, Kasugai T, and Tsukamoto F. Leiomyosarcoma of the breast: a case report and review of the literature about therapeutic management. Breast. (2011) 20:389–93. doi: 10.1016/j.breast.2011.03.001
9. Masadah R, Anwar F, Nelwan BJ, and Faruk M. Primary leiomyosarcoma of the breast: a case report and literature review. Int J Surg Case Rep. (2023) 106:108290. doi: 10.1016/j.ijscr.2023.108290
10. Singh G, Sharma D, and Goyal S. Primary leiomyosarcoma of breast presenting with metastasis: an atypical presentation with dismal prognosis. Indian J Med Paediatr Oncol. (2017) 38:535–7. doi: 10.4103/ijmpo.ijmpo_139_16
11. Felix C, Bispo M, and Chagas C. Pancreatic metastasis from primary leiomyosarcoma of the breast. Ge Port J Gastroenterol. (2019) 26:223–5. doi: 10.1159/000489866
12. Galama R, Matoso J, Capela G, Boto C, Duarte C, and Mendes AR. A rare etiology of a large tumoral mass of the breast - case report primary leiomyosarcoma and osteosarcoma of the breast. Int J Surg Case Rep. (2021) 78:201–3. doi: 10.1016/j.ijscr.2020.12.050
13. Ely CT, Hamza K, Hicham B, Fatiha EM, Hajar EO, Mustapha B, et al. Leiomyosarcoma of the male breast: case report. Ann Med Surg (Lond). (2021) 67:102495. doi: 10.1016/j.amsu.2021.102495
14. Karabulut Z, Akkaya H, and Moray G. Primary leiomyosarcoma of the breast: a case report. J Breast Cancer. (2012) 15:124–7. doi: 10.4048/jbc.2012.15.1.124
15. Chinen LT, Mello CA, Abdallah EA, Ocea LM, Buim ME, Breve NM, et al. Isolation, detection, and immunomorphological characterization of circulating tumor cells (ctcs) from patients with different types of sarcoma using isolation by size of tumor cells: a window on sarcoma-cell invasion. Onco Targets Ther. (2014) 7:1609–17. doi: 10.2147/OTT.S62349
16. Lee SY and Lee NR. Positive response of a primary leiomyosarcoma of the breast following salvage hyperthermia and pazopanib. Korean J Intern Med. (2018) 33:442–5. doi: 10.3904/kjim.2015.242
17. Yang FY, Wang X, Lu SY, Zhao YJ, and Ren WW. Initial experience using ultrasound, automated breast volume scanner, and elastography for primary leiomyosarcoma of the breast: a rare case report. Heliyon. (2024) 10:e33475. doi: 10.1016/j.heliyon.2024.e33475
18. Xu Z, Gu J, Zhang S, Zhang Z, and Fang W. Leiomyosarcoma with osteoclast-like (lms-ogc) giant cells the breast: a report of a rare case. Thorac Cancer. (2019) 10:2054–6. doi: 10.1111/1759-7714.13190
19. Brandao RG, Elias S, Pinto NA, Alcoforado AM, Esposito PC, and Facina G. Leiomyoma of the breast parenchyma: a case report and review of the literature. Sao Paulo Med J. (2018) 136:177–81. doi: 10.1590/1516-3180.2016.0253040117
20. Tajima S, Koda K, and Fukayama M. Primary leiomyosarcoma of the breast with prominent osteoclastic giant cells: a case expressing receptor activator of nf-kappab ligand (rankl). Pathol Int. (2015). doi: 10.1111/pin.12328
Keywords: breast, primary leiomyosarcoma, sarcoma, breast malignancy, mastectomy
Citation: Lv H, Ren H, Zhang S, Ding G and Tian P (2025) Case Report: Primary leiomyosarcoma of the breast. Front. Oncol. 15:1571029. doi: 10.3389/fonc.2025.1571029
Received: 04 February 2025; Accepted: 29 April 2025;
Published: 22 May 2025.
Edited by:
Robert Wesolowski, The Ohio State University, United StatesReviewed by:
Ahmed Farag El-Kased, University of Menoufia, EgyptYichang Hao, Peking University Third Hospital, China
Copyright © 2025 Lv, Ren, Zhang, Ding and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ping Tian, dHAxMjQ1OTA3NjkzQDEyNi5jb20=
 Haoqiang Lv1
Haoqiang Lv1 Ping Tian
Ping Tian