- 1Urology Department of General Hospital, Ningxia Medical University, Yinchuan, China
- 2Key Laboratory of Fertility Preservation and Maintenance of Ministry of Education, Ningxia Medical University, Yinchuan, China
Synchronous multiple primary malignant neoplasms (MPMNs) involving distinct histopathological entities within the upper urinary tract represent a rare clinical phenomenon. We present a novel case of a 57-year-old male presenting with asymptomatic gross hematuria, subsequently diagnosed with three concurrent malignancies: papillary renal cell carcinoma(T1bN0M0), verrucous carcinoma of the renal pelvis (T1N0M0), and low-grade invasive urothelial carcinoma of the ureter (T2N0M0). Comprehensive imaging evaluation revealed a 5.7*5.2cm renal mass and 12cm ureteral tumor extending into the bladder. Following radical nephroureterectomy, histopathological confirmation of three distinct primary malignancies was achieved. Postoperative surveillance identified metastatic progression to adrenal, retroperitoneal, and peritoneal regions within four months, with subsequent development of bladder urothelial carcinoma. The unusual coexistence of three histologically distinct upper urinary tract malignancies, particularly the rare verrucous carcinoma variant, provides novel insights into tumor biology and clinical management paradigms for genitourinary MPMNs.
Introduction
MPMNs encompass the concurrent or consecutive emergence of two or more distinct pathological tissue types within the same organ or tissue, or across various organs or tissues within the same individual (1).Recent advancements in tumor diagnosis and treatment technology have led to a perceived rise in clinical reports documenting MPMNs (2).This case is worth mentioning because the clustering of four primary malignancies (synchronous and metachronous) is of rare occurrence in a single patient and to our knowledge, this is the first report of the combination of three synchronous primary cancers of the upper urinary tract appearing in the same patient.
In this case report, we highlight a unique patient scenario characterized by the presence of three distinct histological types of malignant neoplasms within the upper urinary tract. Specifically, the patient was diagnosed with renal papillary renal cell carcinoma, verrucous carcinoma of the renal pelvis, and low-grade uroepithelial carcinoma in the ureter.
Case report
A 57-year-old male presented to the urology department on July 16, 2022, with asymptomatic gross hematuria. Physical examination revealed kidney percussion tenderness, while the rest of the clinical assessment was unremarkable. The patient’s medical history included hypertension, with no smoking or diabetes mellitus. Subsequent abdominal ultrasonography identified a 6.8x5.7 cm lesion in the left kidney. Computed tomography reconstruction of the urinary tract (CTU) revealed a 5.7*5.2 cm cystic, solid lesion located in the lower pole of the left kidney. Additionally, a 12 cm long mass was observed in the lower left ureter, extending into the bladder, with contrast enhancement (Figure 1).
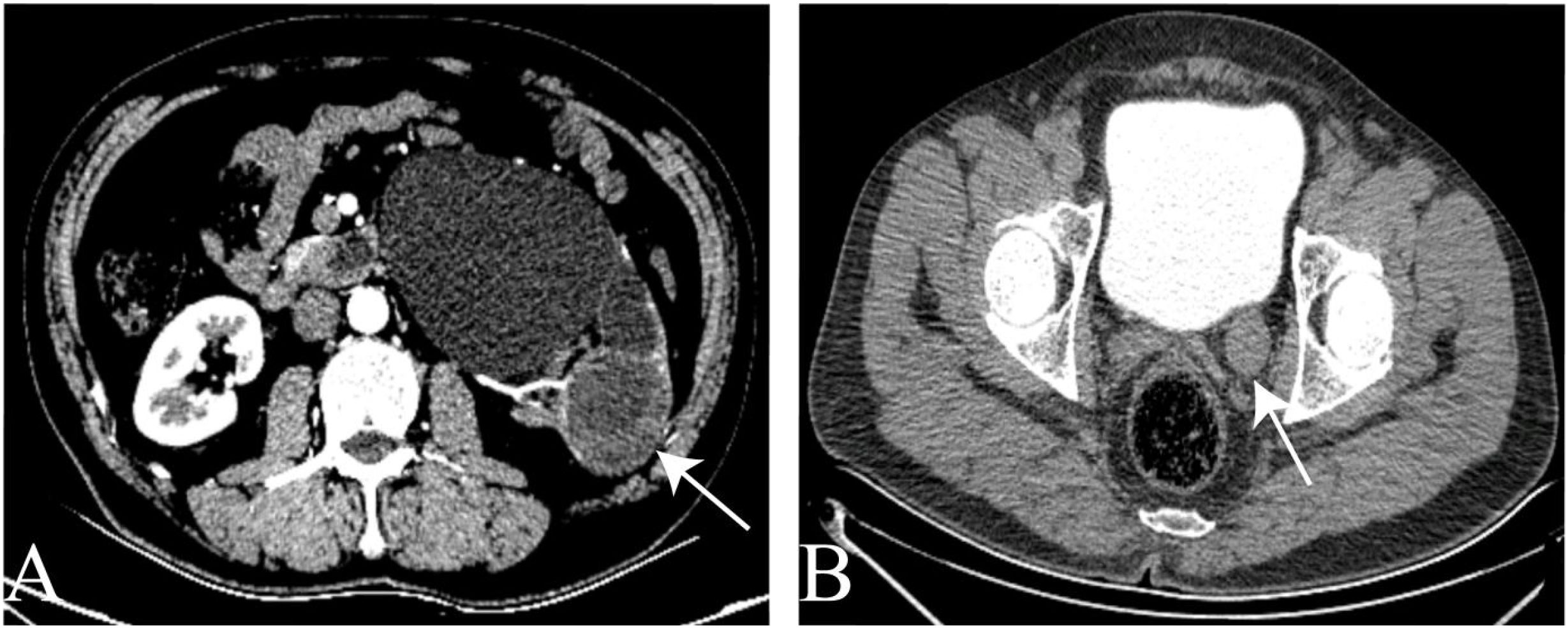
Figure 1. The CTU image. (A) space occupying lesion in the lower pole of the left kidney. (B) The tumor of the left ureter.
The CT scan showed no tumors apart from those in the ureter and kidney, and no metastases were detected. Following comprehensive auxiliary examinations, surgical intervention was conducted under general anesthesia. On July 20, 2022, a left laparoscopic nephroureterectomy was performed, resulting in the complete resection of the left kidney and left ureter, including the tumor. The surgical specimen measured 18*7*5cm (Figure 2A), and it was subsequently sent for histopathological examination. The histologic findings revealed three distinct diagnoses:1. Papillary renal cell carcinoma (type I) (Figure 2B) staged as T1bN0M0.2. Verrucous carcinoma of the renal pelvis (Figure 2C) with cancerous tissue invading the submucosa, staged as T1N0M0.3. Low-grade invasive uroepithelial carcinoma of the ureter (Figure 2D) with invasion into the smooth muscle of the ureter, staged as T2N0M0.
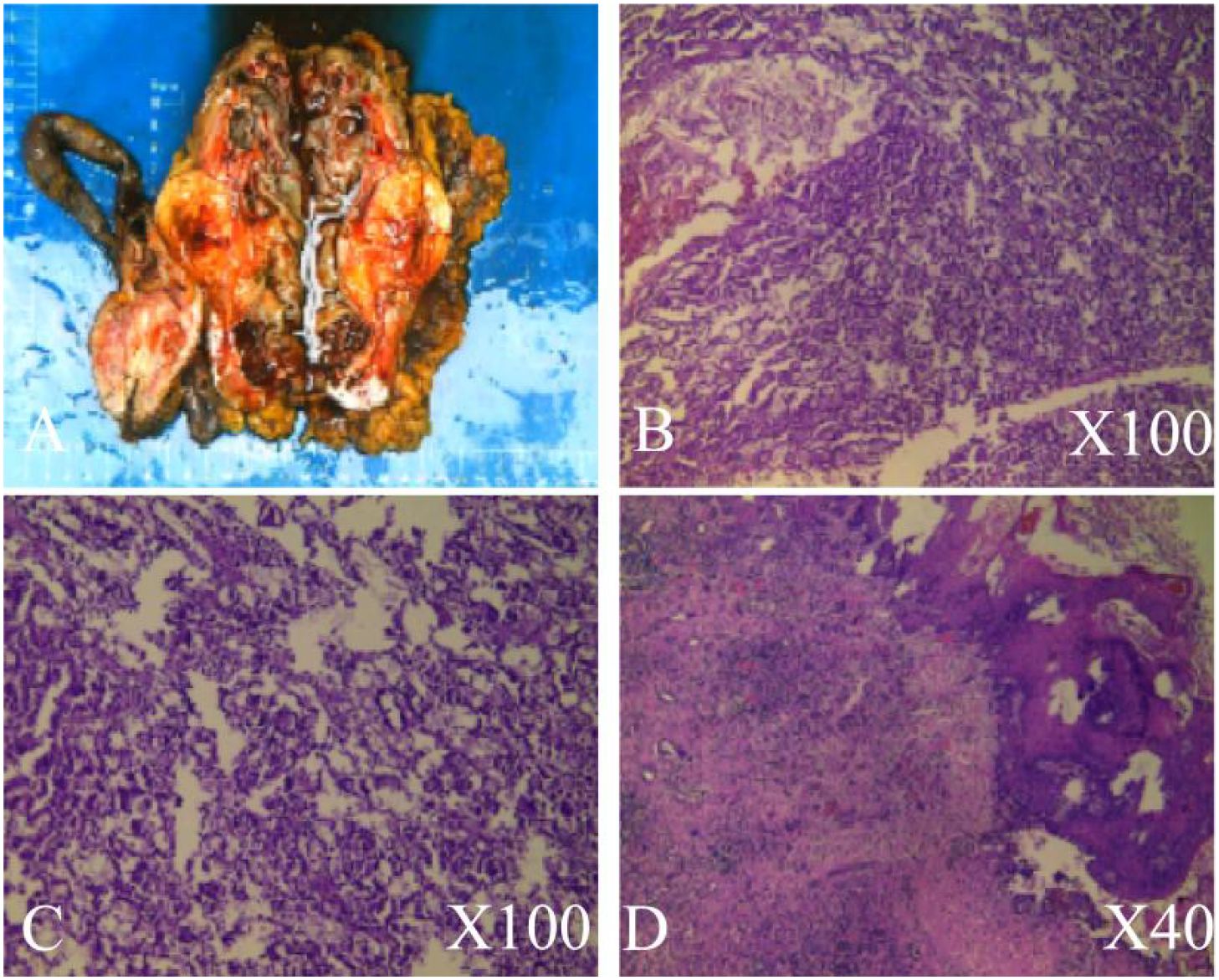
Figure 2. Histopathological examination. (A) Excised kidney tissue, kidney tumor, ureter, and perinephric fat. (B) Pathological features of papillary renal cell carcinoma. (C) Pathological features of verrucous carcinoma of the renal pelvis. (D) Pathological features of low-grade invasive uroepithelial carcinoma in the ureter.
Computed tomography of the entire abdomen was conducted every 3-6 months post-surgery. Four months later, abdominal CT imaging on November 2, 2022, revealed left adrenal metastasis (Figure 3A). Metastases were also observed in the left retroperitoneal area, peritoneum (Figure 3B), and abdominal wall (Figure 3C). One month thereafter, CTU on November 24, 2022, identified a suspicious lesion on the left bladder wall (Figure 3D).

Figure 3. Computed tomography of the abdomen. (A) Left adrenal mass. (B) Mass in the left retroperitoneum and peritoneum. (C) Mass in the abdominal wall. (D) Mass in the bladder.
The patient underwent Transurethral Resection of Bladder Tumour (TURBT) on December 1, 2022, for suspected recurrent bladder tumors. Multiple cauliflower-like tumors were observed scattered throughout the bladder during surgery. The bladder tumor was completely excised and submitted for histopathological examination. The histological analysis revealed low-grade uroepithelial carcinoma, staged as cT2bN1M1 (Figure 4).
Two weeks post-surgery, the patient commenced chemotherapy at the standard dosage: gemcitabine (1.8g) and cisplatin (150mg) administered every three weeks. Regular follow-up visits were scheduled, including hematological assessments, ultrasonographic examinations, and abdominal CT scans. Clinical chemistry parameters, renal and liver function tests, urinalysis, as well as vital signs such as height and weight, were diligently monitored. Enhanced abdominal CT imaging conducted on March 13, 2023, revealed a soft tissue shadow measuring 6.8 x 5.4 x 3.4 cm with uneven density enhancement in the left kidney area. Additionally, a soft tissue mass approximately 8.6 x 6.1 cm was observed in the left abdominal wall, accompanied by enlarged lymph nodes around the abdominal aorta region. By April 2023, the patient reported experiencing pain and hematuria during regular follow-up evaluations.
Discussion
The occurrence of multiple primary malignant tumors in the urinary tract is a rare phenomenon in clinical practice, presenting significant technical challenges in treatment. The incidence of such occurrences in the urinary system is reported to be approximately 6.31% in international studies (3).MPMNs originate from various organs and systems. The location of predilection varies according to the distribution of tumor occurrence in each region and is usually related to the patient’s environment (4),family history (5),genetic (6)and tobacco smoking (7) (7).However, it’s noteworthy that the patient in this case had no history of smoking, no significant past medical history, and no family history of carcinomas. Particularly, there was no family history of malignancies with young onset among any family members.
MPMNs were initially described by Bilroth in 1889 (8). In 1932, Warren and Gates proposed three criteria for the diagnosis of a second primary cancer: i) each tumor must present a definite clinical and histological picture of malignancy; ii) each tumor must be histologically distinct; and iii) the probability that one was a metastatic lesion from the other must be excluded (9).
Synchronous malignancies are defined as those occurring within 6 months of the diagnosis of a previous malignant neoplasm, while metachronous malignancies are those that occur more than 6 months apart (10), heterochronous malignancies comprise the majority of cases. In this instance, the patient initially presented with asymptomatic gross hematuria accompanied by kidney percussion pain. At the first visit, three concurrent upper urinary tract cancers were identified. Four months later, bladder tumors and metastases developed. Thorough histopathological examination and adequate sectioning facilitated the successful diagnosis of three distinct primary malignancies within the upper urinary tract. Consequently, the patient is classified as having MPMNs.
The genitourinary system is the preferred site for MPMNs, with bladder and prostate cancers being the most commonly observed (11).However, the proportion of renal and ureteral cancers combined with MPMNs is even lower. It has been reported in the literature that renal cancer accounted for 2% of the first MPMN cancers and 2.4% of the second primary cancers (12).In this case, the occurrence of renal verrucous carcinoma is particularly rare. Verrucous carcinoma, a distinctive variant of squamous cell carcinoma (SCC), is uncommon but notable. It was first described by Lauren Ackerman in 1948 (13).Verrucous carcinoma can manifest at various sites, including the upper aerodigestive tract, skin, bladder, and genitalia (14).The renal tumor in this case exhibits typical features of verrucous carcinoma. Verrucous carcinoma refers to a distinct histologic appearance characterized by well-differentiated squamous cell carcinoma with localized infiltration and minimal propensity for metastasis to regional lymph nodes or distant sites, as observed in our tumor. Although bladder metastases developed post-surgery, they did not exhibit verrucous carcinoma characteristics. Additional histologic features include extensive keratinization with exophytic or papillomatous extension into the stroma and a lack of significant cellular anaplasia (15). Verrucous carcinoma is recognized as a warty variant of squamous cell carcinoma, featuring predominantly exophytic growth of well-differentiated keratinizing epithelium with minimal atypia. It typically exhibits locally destructive pushing margins at its interface with underlying connective tissue and does not invade the lamina propria. The tumor cells demonstrate little atypia, although faint invasion foci may be observed in verrucous carcinomas (16).
There is limited literature available nationally and internationally regarding verrucous carcinoma. Additionally, upper urothelial carcinoma is considered a relatively rare condition, accounting for approximately 5–10% of all urothelial cancers (17). In Western countries, the incidence of upper urothelial carcinoma is low, estimated at approximately 1–2 cases per 100,000 individuals. It is predominantly diagnosed in older male patients (18). In this case, the patient presented with a combination of three urological tumors, representing simultaneous MPMNs. Instances of three or more primary upper urinary malignancies are rare, with few reports documented in the literature.
An early diagnosis of MPMNs holds the potential to facilitate timely administration of anticancer treatments, including surgery, chemoradiotherapy, and immunotherapy, thereby improving overall survival and progression-free survival rates. However, there are currently no established guidelines for the treatment of MPMNs, and management typically relies on the primary cancer that appears at different times. Nevertheless, in cases of multiple primary malignancies of the urinary tract, surgery is often prioritized in treatment approaches. For elderly patients with multiple primary malignancies of the urinary tract who are in poor health, non-operative treatment may be considered if surgery is deemed too risky. Therefore, the development of reasonable chemoradiotherapy regimens and cycles is crucial in such cases to improve prognosis and enhance the 5-year survival rate. In the present case, radical surgery was chosen as the initial treatment option. Unfortunately, four months later, the patient developed bladder tumors and metastases. Depending on the overall condition of the patient and the specific pathology of the bladder, an individualized treatment plan involving chemotherapy and molecular targeted therapy may be considered.
The simultaneous occurrence of primary malignant neoplasms in the renal, ureteral, and urinary bladder regions poses diagnostic and therapeutic challenges. Distinguishing synchronous primaries from metastatic disease is crucial for guiding appropriate treatment strategies and prognostication. In this case, thorough clinical evaluation, imaging studies, and histopathological analysis facilitated accurate diagnosis and informed multidisciplinary management. The successful outcome underscores the importance of a comprehensive approach involving urological, oncological, and radiological expertise in addressing complex oncological presentations. Furthermore, this case highlights the need for heightened awareness of synchronous primary malignancies in clinical practice, particularly in regions with a high incidence of genitourinary malignancies such as China. In addition, multidisciplinary treatment and individualized precision treatment strategies may help improve the prognosis of MPMNs (19).The exceptional nature of this case underscores the imperative for systematic data collection on analogous instances in future investigations, coupled with comprehensive research into molecular mechanisms to elucidate the underlying pathophysiological determinants of such rare co-occurrences. Regrettably, we were unable to acquire the freshly procured clinical specimens from the patient, thereby precluding the implementation of genetic screening. Had the genetic screening been feasible, it would have facilitated a comprehensive elucidation of potential genetic predisposition and somatic mutation-driven molecular pathways associated with the disease. This would have enabled the provision of personalized genetic counseling and early cancer risk assessment for the patient’s familial cohort.
Conclusions
This case report illustrates a rare occurrence of synchronous primary malignant neoplasms affecting the renal, ureteral, and urinary bladder regions in a Chinese male patient. Through detailed clinical description and analysis, we emphasize the importance of comprehensive evaluation and multidisciplinary management in addressing complex oncological presentations. Heightened awareness of synchronous primary malignancies is essential for guiding optimal treatment strategies and improving patient outcomes. Further research is warranted to elucidate the underlying mechanisms and risk factors associated with the development of synchronous primary malignancies in the genitourinary tract.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Ethics Committee of the University of Ningxia Medical. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from General Hospital of Ningxia Medical University. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
BH: Writing – original draft, Writing – review & editing, Data curation, Resources. WY: Writing – original draft, Writing – review & editing, Data curation, Resources. MAA: Writing – review & editing, Data curation. HT: Writing – review & editing, Data curation, Resources, Writing – original draft. MZ: Writing – review & editing, Data curation, Writing – original draft. JZ: Writing – original draft, Writing – review & editing. CD: Writing – review & editing, Data curation. NL: Writing – review & editing, Data curation. RH: Writing – review & editing. GL: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to acknowledge the National Natural Science Foundation of China for their support in this project. The authors would also like to acknowledge the General Hospital of Ningxia Medical University for their helpful assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Correction note
This article has been corrected with minor changes. These changes do not impact the scientific content of the article.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhao YX, Yang Z, Ma LB, Dang JY, and Wang HY. Synchronous gastric cancer complicated with chronic myeloid leukemia (multiple primary cancers): A case report. World J Clin cases. (2022) 10:11146–54. doi: 10.12998/wjcc.v10.i30.11146, PMID: 36338220
2. Ma XY, Tian K, and Sun PF. Multiple primary Malignant neoplasm: Case report and comprehensive literature review. Front Oncol. (2022) 12:1090634. doi: 10.3389/fonc.2022.1090634, PMID: 36686734
3. Inci O, Kaya E, Alagol B, Atakan IH, Aydin S, and Ereselli H. Multiple primary Malignant neoplasms in urologic patients. Int Urol Nephrol. (2004) 36:1–4. doi: 10.1023/b:urol.0000032673.34011.7d, PMID: 15338662
4. Ye X, Liu X, Yin N, Song W, Lu J, Yang Y, et al. Successful first-line treatment of simultaneous multiple primary Malignancies of lung adenocarcinoma and renal clear cell carcinoma: A case report. Front Immunol. (2022) 13:956519. doi: 10.3389/fimmu.2022.956519, PMID: 35979370
5. Wang Y and Wu XT. Stomach carcinoma presenting with a synchronous liver cancer: a case report and literature review. Case Rep Gastrointest Med. (2014) 2014:970293. doi: 10.1155/2014/970293, PMID: 25328726
6. Hursting SD, Digiovanni J, Dannenberg AJ, Azrad M, Leroith D, Demark-Wahnefried W, et al. Obesity, energy balance, and cancer: new opportunities for prevention. Cancer Prev Res (Phila). (2012) 5:1260–72. doi: 10.1158/1940-6207.CAPR-12-0140, PMID: 23034147
7. Mukaiyama Y, Suzuki M, Morikawa T, Mori Y, Takeshima Y, Fujimura T, et al. Multiple primary Malignant neoplasms of the glottis, renal pelvis, urinary bladder, oral floor, prostate, and esophagus in a Japanese male patient: a case report. World J Surg Oncol. (2014) 12:294. doi: 10.1186/1477-7819-12-294, PMID: 25245383
8. Bagga N, Khera S, Choudhary GR, and Tuteja RK. Urothelial carcinoma of the renal pelvis with synchronous ipsilateral papillary renal cell carcinoma. Indian J Pathol Microbiol. (2020) 63:497–8. doi: 10.4103/IJPM.IJPM_617_18, PMID: 32769353
9. Kim DH, Kim SM, Choi MG, Sohn TS, Bae JM, and Kim S. Multiple primary Malignancies in patients with multiple early gastric cancer. J Gastric Cancer. (2017) 17:154–61. doi: 10.5230/jgc.2017.17.e19, PMID: 28680720
10. Pan SY, Huang CP, and Chen WC. Synchronous/metachronous multiple primary Malignancies: review of associated risk factors. Diagn (Basel). (2022) 12. doi: 10.3390/diagnostics12081940, PMID: 36010291
11. Chun TY. Coincidence of bladder and prostate cancer. J Urol. (1997) 157:65–7. doi: 10.1016/S0022-5347(01)65281-9, PMID: 8976217
12. Feller A, Matthes KL, Bordoni A, Bouchardy C, Bulliard JL, Herrmann C, et al. The relative risk of second primary cancers in Switzerland: a population-based retrospective cohort study. BMC Cancer. (2020) 20:51. doi: 10.1186/s12885-019-6452-0, PMID: 31964352
13. Baseskioglu B, Yenilmez A, Acikalin M, Can C, and Donmez T. Verrucous carcinoma of the renal pelvis with a focus of conventional squamous cell carcinoma. Urol Int. (2012) 88:115–7. doi: 10.1159/000330906, PMID: 21968520
14. Sheaff M, Fociani P, Badenoch D, and Baithun S. Verrucous carcinoma of the renal pelvis: case presentation and review of the literature. Virchows Arch. (1996) 428:375–9. doi: 10.1007/BF00202204, PMID: 8797941
15. Kansal NS, Rosenberg G, Han M, and Richter F. Verrucous carcinoma of the renal pelvis. Urology. (2001) 58:105. doi: 10.1016/s0090-4295(01)01133-5, PMID: 11445495
16. Sellami-Boudawara T, Gouiaa N, Makni S, Sellami A, Bahri I, Mhiri MN, et al. Verrucous carcinoma of the kidney: report of 2 cases. Ann Urol (Paris). (2001) 35:198–202. doi: 10.1016/s0003-4401(01)00025-0, PMID: 11496593
17. Gust KM, Resch I, D’Andrea D, and Shariat SF. Update on systemic treatment of upper tract urothelial carcinoma: a narrative review of the literature. Transl Androl Urol. (2021) 10:4051–61. doi: 10.21037/tau-21-47, PMID: 34804847
18. Soria F, Shariat SF, Lerner SP, Fritsche HM, Rink M, Kassouf W, et al. Epidemiology, diagnosis, preoperative evaluation and prognostic assessment of upper-tract urothelial carcinoma (UTUC). World J Urol. (2017) 35:379–87. doi: 10.1007/s00345-016-1928-x, PMID: 27604375
Keywords: synchronous, MPMN, urinary, verrucous carcinoma, kidney
Citation: Huang B, Yin W, Al-Qaisi MA, Tian H, Zhao M, Zhang J, Deng C, Li N, He R and Li G (2025) Multiple synchronous primary malignant neoplasms of renal, ureter and urinary bladder: a case report. Front. Oncol. 15:1576764. doi: 10.3389/fonc.2025.1576764
Received: 14 February 2025; Accepted: 27 June 2025;
Published: 24 July 2025; Corrected: 12 August 2025.
Edited by:
Ronald M Bukowski, Cleveland Clinic, United StatesReviewed by:
Sri Manjari K, Osmania University, IndiaRajesh Kumar, Kerala University of Health Sciences, India
Copyright © 2025 Huang, Yin, Al-Qaisi, Tian, Zhao, Zhang, Deng, Li, He and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guangyong Li, Z3Vhbmd5b25nbGkxOTc5QGhvdG1haWwuY29t; Rui He, cnVpaGU1MTVAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Bincheng Huang
Bincheng Huang Wenhui Yin1†
Wenhui Yin1† Jin Zhang
Jin Zhang Rui He
Rui He Guangyong Li
Guangyong Li