- 1Department of Anesthesiology Department Luzhou Maternal & Child Health Hospital (Luzhou Second People's Hospital), Luzhou, Sichuan, China
- 2School of Nursing, Yingtan Health Vocational College, Yingtan, Jiangxi, China
- 3Health Care College of Yingtan Health Vocational College, Yingtan, Jiangxi, China
Background: Cancer-related fatigue (CRF) can seriously affect the quality of life of breast cancer patients. Mindfulness-based stress reduction therapy (MBSR) has been increasingly used in the treatment of breast cancer patients to reduce psychological distress and promote emotional and physical health. This review aims to provide an updated assessment of the role of MBSR in reducing CRF and sleep quality in breast cancer patients.
Objective: To evaluate the effect of MBSR on cancer-related fatigue in patients with breast cancer.
Methods: Computer search PubMed, Embase, Web of Science, Wanfang and other databases, We were able to search for articles related to CRF from MBSR in breast cancer patients from the establishment of the database to October 2023. Researchers independently screened the literature and extracted information. The meta-analysis was performed using Review Manager Software (version 5.3).
Results: A meta-analysis of 11 studies included showed that MBSR could reduce CRF in breast cancer patients (SMD = -0.86, 95%CI = −1.22 ~ −0.50). Improved sleep quality (MD = -2.54, 95%CI = −3.38 ~ −1.70).
Conclusion: Our research indicates that MBSR can reduce CRF and improve sleep quality in breast cancer patients. However, due to the moderate and significant heterogeneity in the quality of evidence observed in the included studies, these findings should be interpreted with caution.
1 Introduction
Breast cancer is the most common malignant tumour in women worldwide, posing a severe threat to women’s health and life. According to the survey on the incidence of female breast cancer in 185 countries in 2020, about 2.3 million female cases are diagnosed with milk adenocarcinoma every year, accounting for 11.7% of new cancer cases (1). However, in recent years, the emergence of neoadjuvant therapy has increased the treatment probability and improved the survival rate of patients. The global 5-year survival rate for breast cancer is currently 90% (2). Survivors are also faced with a series of physical and mental problems, such as premature menopause, body image disorder, fatigue, depression, etc (3–5). For breast cancer patients during chemotherapy, cancer-related fatigue (CRF) is the most common complication, and the incidence can be as high as 59% to 100% (6). CRF is a multidimensional concept that affects the physical (less energy and more need of sleep), cognitive (diminished concentration and attention), and affective (diminished motivation) domains (7).CRF is more severe and long-lasting than ordinary fatigue and cannot be relieved by rest and sleep. Therefore, improving CRF in breast cancer patients has been a research hotspot in recent years.
Mindfulness-Based Stress Reduction (MBSR) is an increasingly popular comprehensive psychosocial intervention, potentially through mechanisms that enhance mindfulness during meditation practice, such as sustaining moment-to-moment attention, flexibly shifting attentional focus among thoughts and sensations, and fostering non-elaborative awareness by recontextualizing negative experiences (8, 9).
Many patients with breast cancer turn to complementary therapies to deal with the symptoms of the disease (10, 11). A total of 33% to 47% of women worldwide and 48% to 80% of American women make use of such therapies, and meditation is one of complementary alternatives that positively influences the rehabilitation by reducing pain, stress, anxiety, depression, fatigue, and even the side effects caused by drug treatments (12, 13). Although meta-analysis have reported the effect of MBSR on breast cancer patients, no effect on CRF has been reported (14). Haller (15)only discussed the impact of MBSR on CRF in breast cancer patients in meta minutes, there are few pieces of literature included and a lack of reports on the effect on sleep quality. This study comprehensively collected the literature of randomized controlled studies of MBSR on CRF in breast cancer patients. The result of the intervention was verified through meta-analysis, which provided authoritative, reliable and complete evidence support for the clinical nursing work of breast cancer patients and an evidence-based basis for medical care decision-making.
2 Methods
This study was reported per the PRISMA NMA guidelines (16). The review protocol was registered with the International Prospective Register of Systematic Review (PROSPERO CRD420251130977).
2.1 Literature search
This meta-analysis followed the guidelines outlined in the systematic review and meta-analysis Preferred Reporting Program. Two independent researchers thoroughly searched multiple databases, including PubMed, Web of Science, Cochrane Library, CNKI, Wan Fang Data, and VIP. The search period was extended from the date of the establishment of the library until August 2025. Search is limited to articles published in Chinese or English. The search terms, including These searches, were performed using the following keywords: “Breast Neoplasm”, “Neoplasm, Breast,” “Breast Tumors”, “Breast Tumor”, “Tumor, Breast”, “Tumors, Breast”, “Neoplasms, Breast”, “Breast Cancer”, “Cancer, Breast”, “Mammary Cancer”, “Cancer Mammary”,”Cancers, Mammary”, “Mammary Cancers”, “Malignant Neoplasm of Breast”, “Breast Malignant Neoplasm”, “Breast Malignant Neoplasms”, “Malignant Tumor of Breast”, “Breast Malignant Tumor”, “Breast Malignant Tumors”, “Cancer of Breast”, “Cancer of the Breast”, “Fatigue”, “mindfulness-based stress reduction”, “mindfulness-based stress reduction”, “MBSR”, “mindfulness-based cognitive therapy”, “MBCT”, “mindfulness-based intervention”.
2.2 Inclusion and exclusion criteria
Study type: Randomized Controlled trial (RCT). The subjects were breast cancer patients with a definite pathological or cytological diagnosis.
Interventions: Patients used various types of MBSR
Result: CRF score, sleep quality
Exclusion criteria: Non-Chinese-English literature; Duplicate publications; Unable to obtain the required data; The index results must conform to the literature.
2.3 Data extraction
The two authors independently extracted data from all eligible studies. The following variables were removed from each study: first author name, year of publication, country, study design, sample size, age, sex ratio, and study quality score. Any disagreements are resolved through discussion or consultation with senior reviewers to reach a consensus.
2.4 Quality assessment
The authors independently assessed the risk of bias in included RCTS using the Cochrane assessment tool, which included the following seven areas: “adequate sequence generation, assignment concealment, participant and person blinding, outcome assessment blinding, incomplete outcome data, selective reporting, and other bias”.
2.5 Data synthesis and analysis
RevMan 5.3 software was used for analysis. If there was no statistical significance in the heterogeneity among the results (P≥ 0.1, I2 < 50%), a fixed effect model was used for meta-analysis. If the heterogeneity among the findings was statistically significant (P < 0.1, I2 ≥50%), the random-effects model was used for meta-analysis after the influence of apparent clinical heterogeneity was excluded. For continuous data, Weighted Mean Difference (WMD) was used to analyze results obtained with the same measurement tools. Standardized Mean Difference (SMD) was used to analyze the same variables when different measurement tools were used. 95%CI was calculated for all analyses.
3 Results
3.1 Study selection
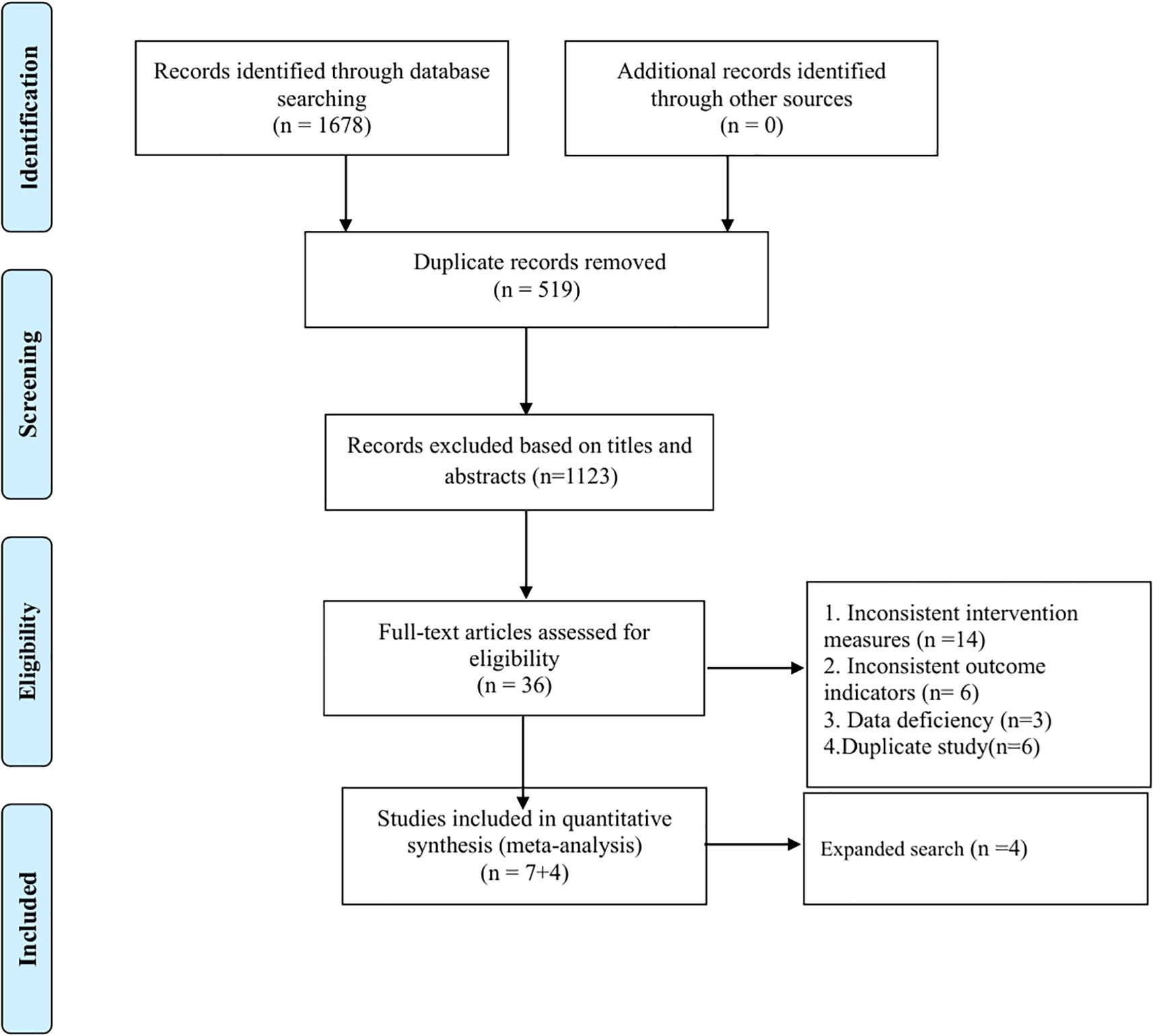
The literature search yielded 1678 results, most of which were excluded because they were replicates or because they were not relevant to our meta-analysis. Then, the full text of 36 articles is reviewed. Finally, 11 literatures were included in this study. See Figure 1. Flow chart.
3.2 Basic characteristics of included studies
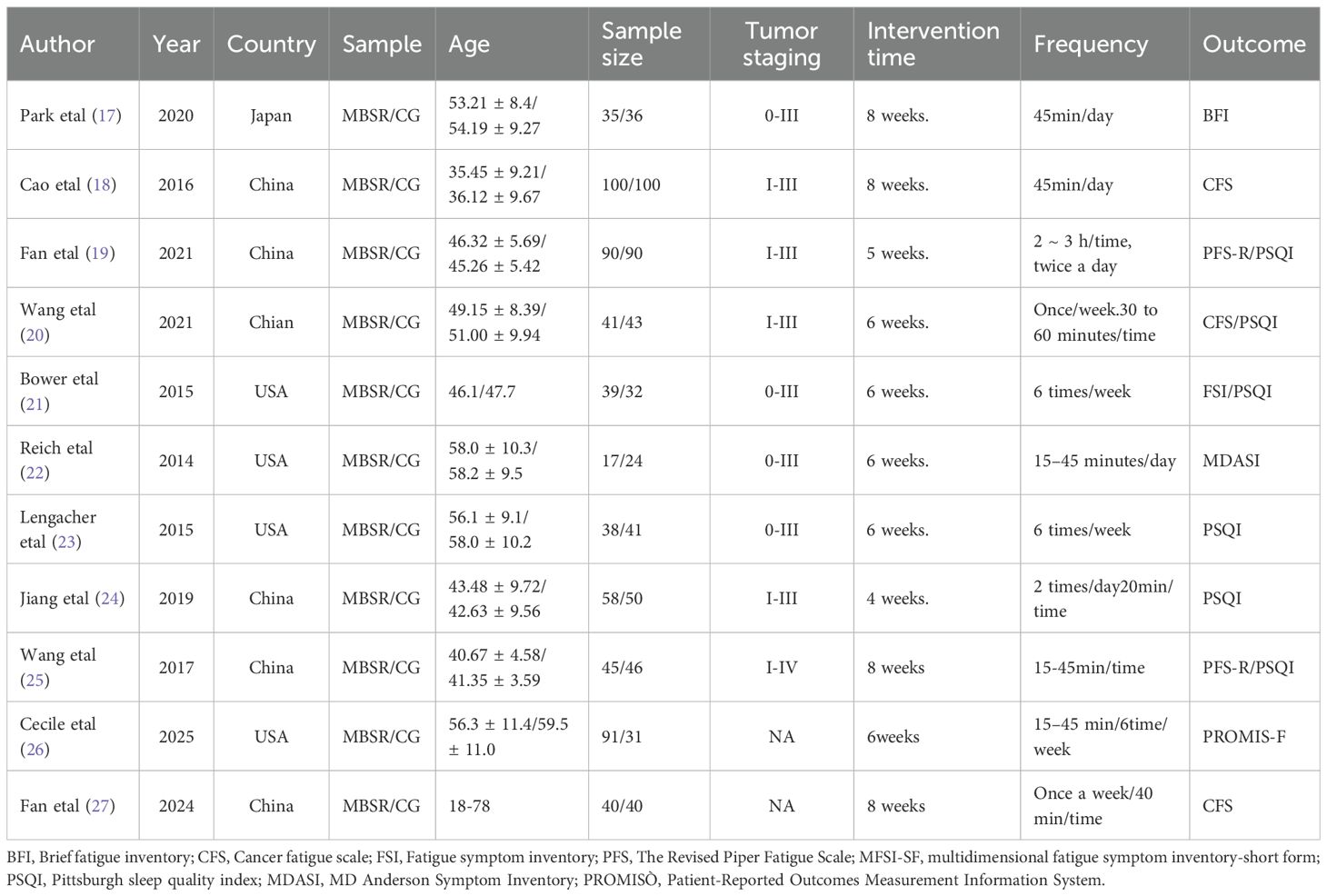
Our research included a total of 11 studies, among which 6 were from China, 4 from the USA, and 1 from Japan. Other characteristics are detailed in Table 1.
3.3 Methodological quality assessment
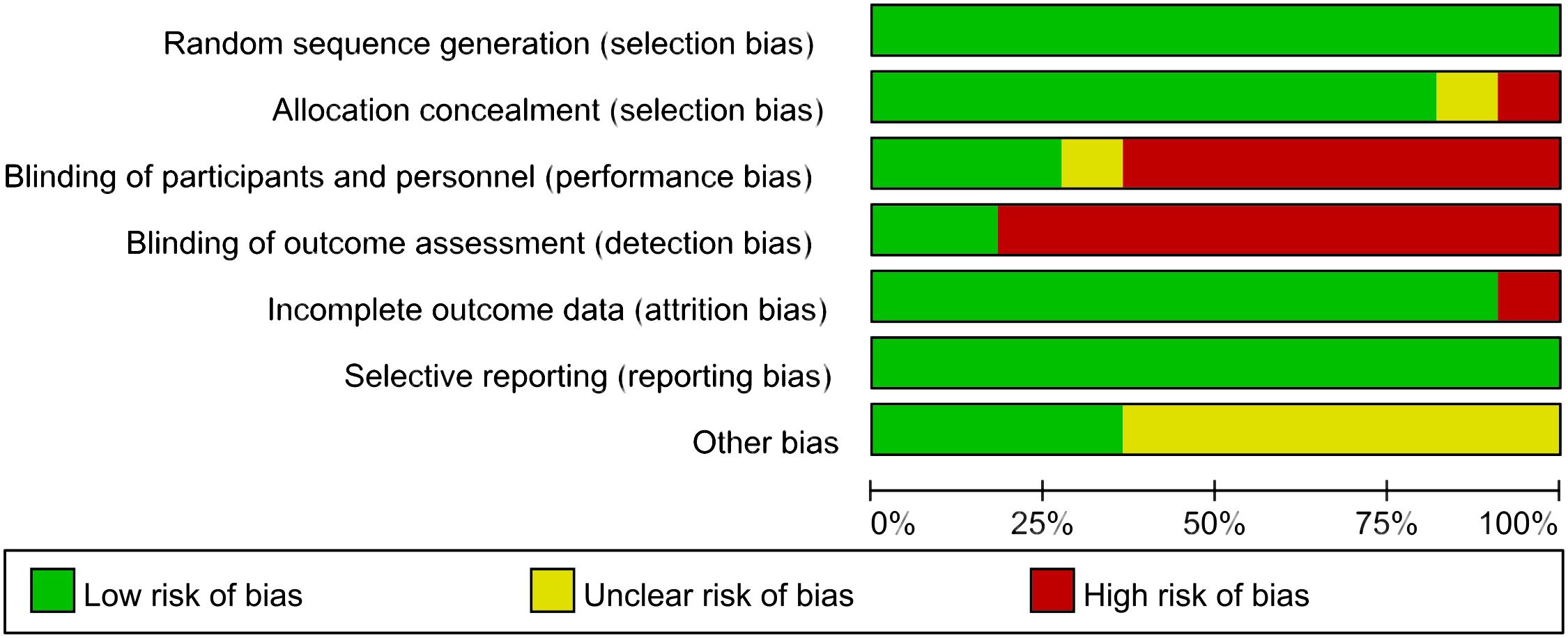
The methodological quality of the included 11 articles was evaluated. The summary of the risk of bias assessment is shown in Figure 2.
3.4 Results of the meta-analysis
3.4.1 CRF
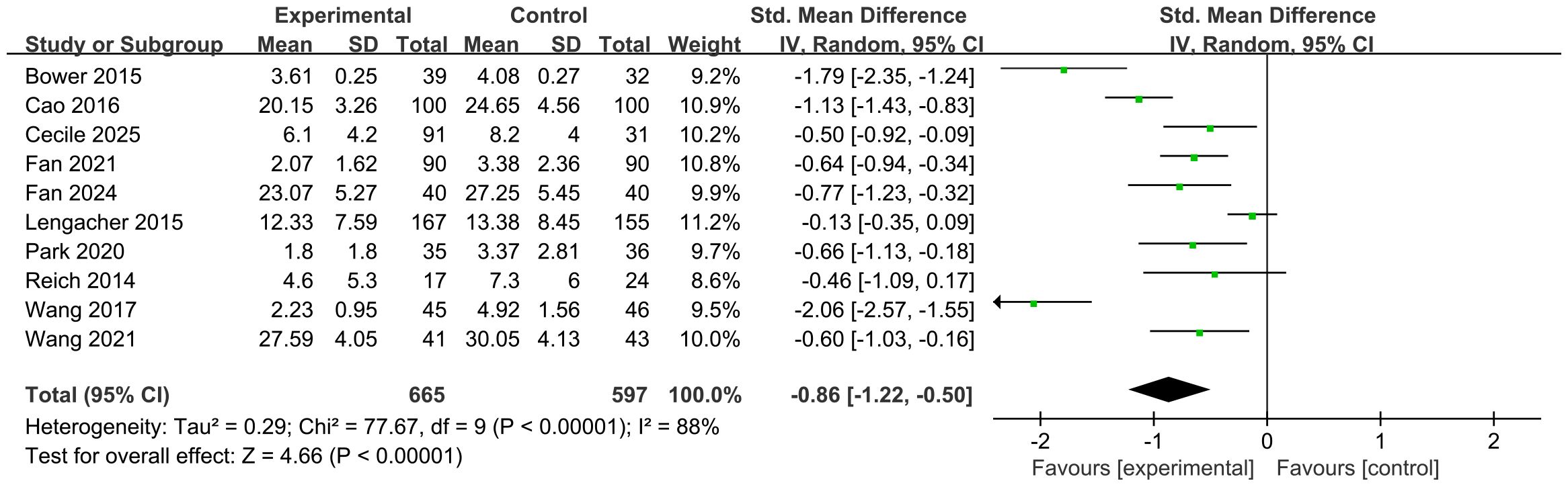
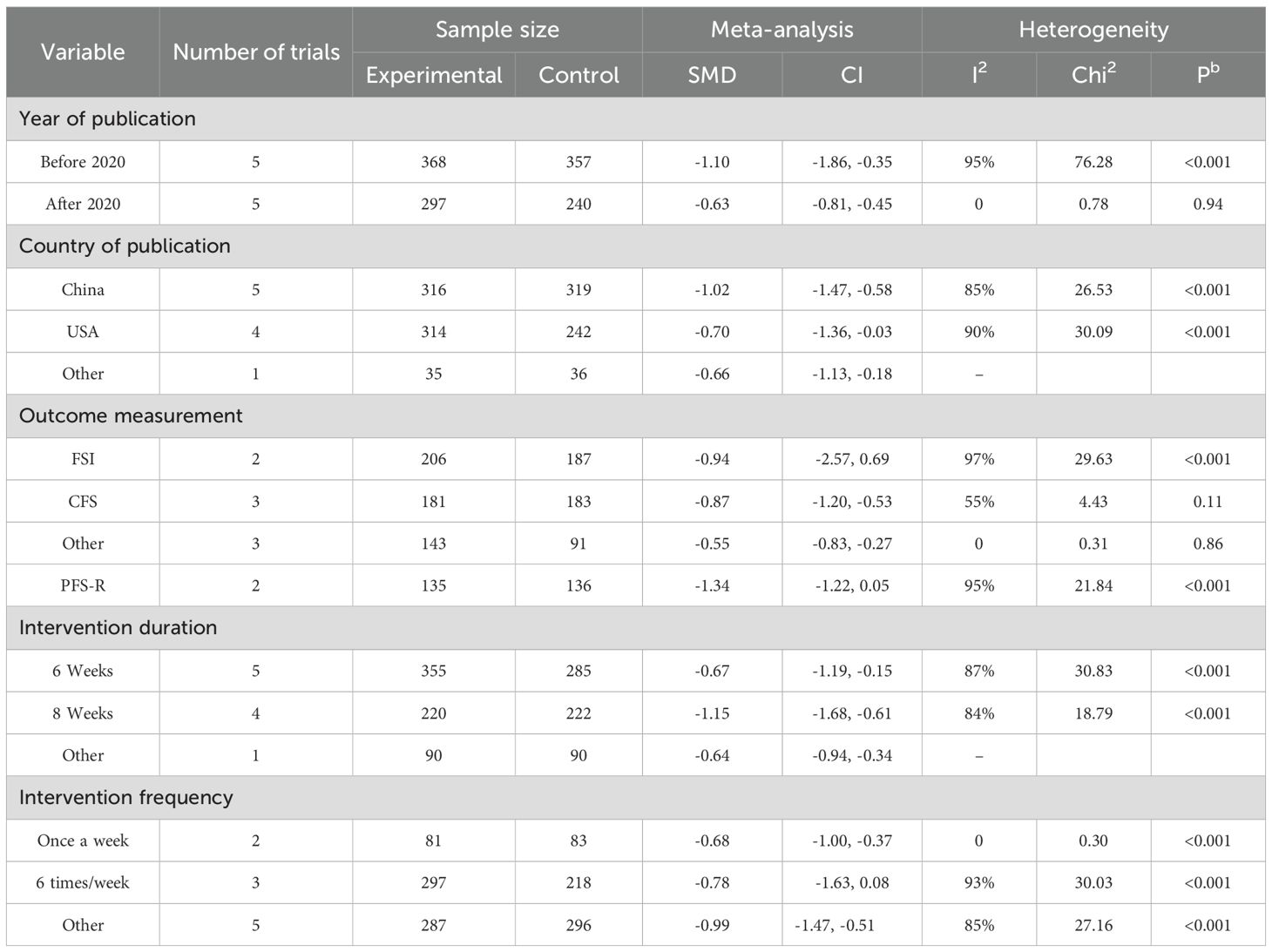
The efficacy of MBSR was compared with that of the control group. A meta-analysis of 10 studies was conducted, and the overall results are presented in Figure 3. Compared to the control group, MBSR significantly alleviated CRF [SMD = –0.86, 95% CI (–1.22, –0.50), p < 0.001], with significant heterogeneity observed (I² = 88%, p < 0.001). Sensitivity analysis was performed by sequentially excluding each study, yet substantial heterogeneity persisted. Therefore, subgroup analysis was conducted to explore potential sources of heterogeneity; detailed results are provided in Table 2 and the Supplementary Materials.
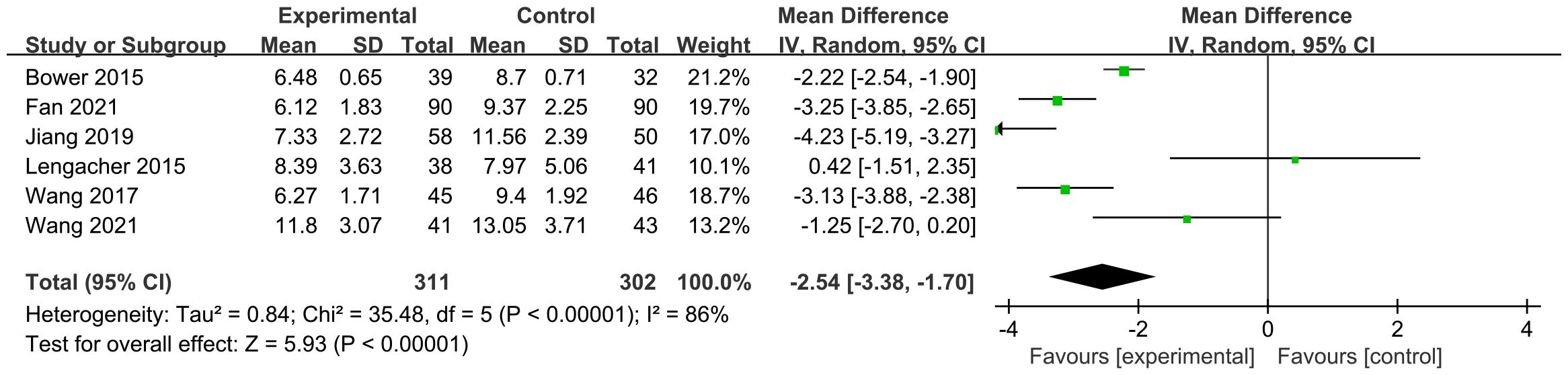
3.4.2 PSQI
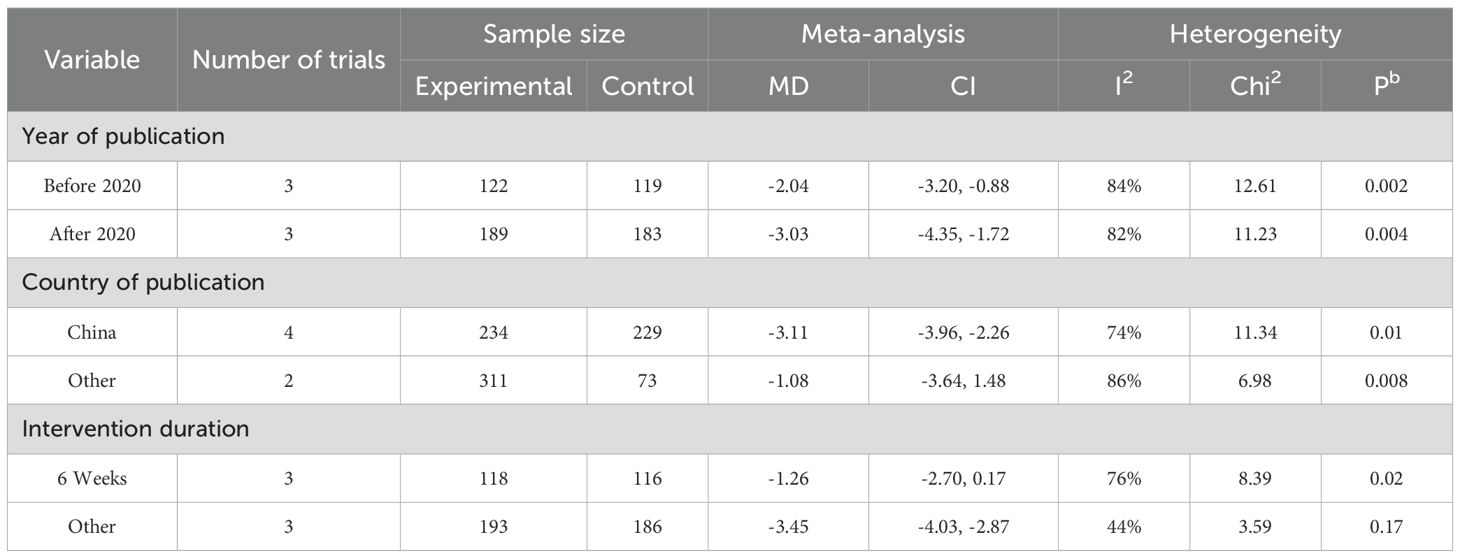
The efficacy of MBSR was compared with that of a control group. A meta-analysis of six studies was performed, and the overall findings are illustrated in Figure 4. Compared with the control group, MBSR resulted in a significant improvement in sleep quality among breast cancer patients [MD = –2.54, 95% CI (–3.38, –1.70), p < 0.001], with significant heterogeneity detected (I² = 86%, p < 0.001). Sensitivity analysis conducted by sequentially excluding individual studies showed that substantial heterogeneity remained. Therefore, subgroup analyses were carried out to explore potential sources of heterogeneity; detailed results are presented in Table 3 and the Supplementary Materials.
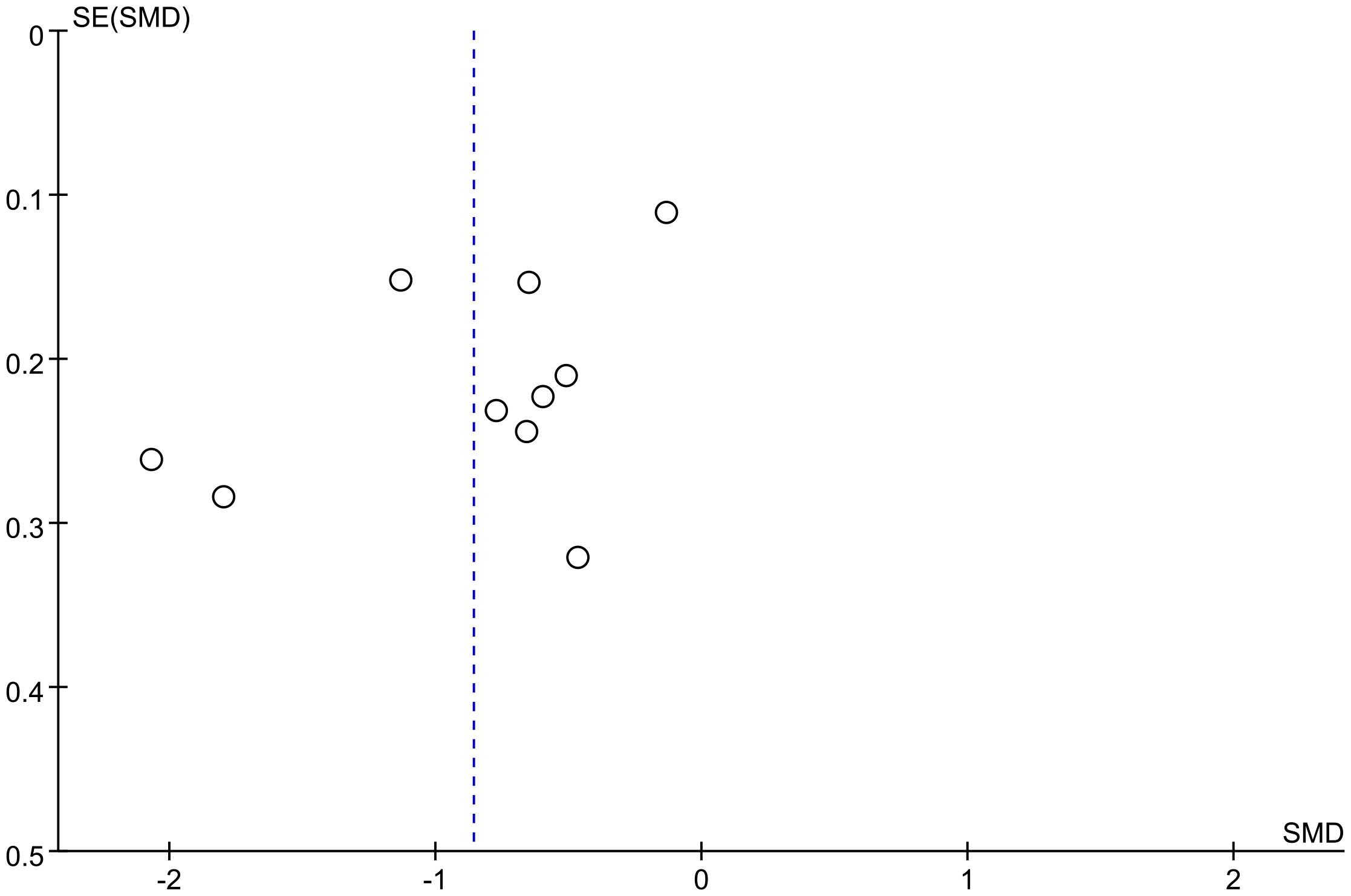
3.4.3 Publication bias
The funnel plot showed potential publication bias (Figure 5). The slight asymmetry observed in the funnel plot suggests the possible presence of publication bias among the included studies.
4 Discussions
CRF not only restricts the normal physiological function of breast cancer patients but also harms the mental health of patients, seriously reduces the quality of life of patients, and ultimately affects the progress of cancer treatment. This study found that the use of MBSR in women with breast cancer was associated with improved sleep quality in breast cancer patients by reducing CRF.
Xie (28) discussed the impact of MBSR on CRF in cancer patients in her study. results found that MBSR could reduce CRF in cancer patients, but the effects of MBSR on CRF were not apparent. In our study, MBSR reduced CRF in breast cancer patients. Our findings are identical to those of the Castanhel (29) study. The neural mechanism of MBSR is that long-term mindfulness training can enhance the activity of theta waves in the frontal lobe of the brain, stimulate the activity levels of related brain regions such as attention and emotion, and increase the gray matter density in regions such as the left superior temporal gyrus and the right hippocampus (30, 31). Furthermore, Research has found that when breast cancer patients undergo MBSR training, the interleukin-4 (IL-4), a product of T cells, increases in their bodies. This cytokine plays a crucial regulatory role in the differentiation and maturation of immune cells, which may be the neuroimmunological basis for enhancing the body’s immunity through MBSR (32). The psychological mechanism by which MBSR improves CRF may involve positive changes in an individual’s awareness and attention towards things and related experiences, enhancing the response to external stimuli, strengthening self-regulation functions, reducing fatigue, and promoting physical and mental health (33). CRF can trigger a decline in physical function in breast cancer patients (34)and is a significant problem during breast cancer treatment (35). Armes et al. (36)emphasize that no medication for fatigue exists. However, interventions should focus on psychological, educational, social, and group support therapies designed to allow individuals to explain fatigue, cope with symptoms with positive thinking, and return to daily activities. The main components of MBSR include sitting and walking meditation, yoga practice, and mindfulness relaxation techniques. MBSR can improve patients’ cortisol and blood pressure, reduce the subjective pain and immune response caused by stress, and enhance and activate the structure of brain regions involved in emotional processing (37). Thus, it is beneficial to improve patients’ CRF.
Few studies have focused on the effect of MBSR on sleep quality in breast cancer patients. Good sleep benefits the human spirit, emotion, immune function, cell growth and repair. The disturbance of sleep patterns and the decline of sleep quality will affect patients’ cognitive function, immune function and quality of life. Breast cancer patients often worry about their disease, and their sleep quality decreases. In addition, chemotherapy causes hair loss, gastrointestinal reactions, bone marrow suppression, anxiety and depression, and other problems that aggravate patients’ sleep disorders. Breast cancer patients have a higher incidence of sleep disorders during chemotherapy, up to 80% (38). MBSR is a mindfulness-based stress management therapy that aims to pass mindfulness-based meditation. The self-management mode of training can reduce the pressure on the subject and effectively manage the subject’s emotions (39). When MBSR is applied to breast cancer patients, it can regulate the quality of sleep by relieving their mental state of anxiety and depression and improving their emotional regulation ability.
5 Limitations and future implications
This study has several limitations. Only literature published in Chinese and English was included, and the search was limited to a finite number of databases, which may have resulted in an incomplete retrieval of relevant studies. Variations in intervention protocols, session durations, and outcome measures across the included studies may have introduced heterogeneity and potential bias. The long-term effects of mindfulness-based interventions on CRF and sleep quality in breast cancer patients remain to be further investigated. Additionally, the relatively small number of included studies, coupled with insufficient reporting of blinding and allocation concealment procedures, may compromise the methodological quality and limit the robustness of the conclusions. Future research should involve more rigorous, high-quality randomized controlled trials with larger sample sizes to further evaluate the efficacy of mindfulness-based stress reduction in improving CRF and sleep outcomes in this population.
6 Conclusion
Our combined findings suggest that MBSR reduces CRF and improves sleep quality in breast cancer patients. Given some limitations of this meta-analysis, well-designed studies with larger sample sizes and more detailed outcome measures are needed.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
XW: Resources, Funding acquisition, Supervision, Writing – review & editing. LG: Conceptualization, Data curation, Investigation, Software, Writing – original draft, Writing – review & editing. YP: Formal analysis, Writing – original draft, Writing – review & editing, Data curation, Investigation, Validation. TH: Formal analysis, Funding acquisition, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Pinto BM, Frierson GM, Rabin C, Trunzo JJ, and Marcus BH. Home-based physical activity intervention for breast cancer patients. J Clin Oncol. (2005) 23:3577–87. doi: 10.1200/JCO.2005.03.080
3. Avis NE, Crawford S, and Manuel J. Quality of life among younger women with breast cancer. J Clin Oncol. (2005) 23:3322–30. doi: 10.1200/JCO.2005.05.130
4. Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR, et al. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. (2000) 18:743–53. doi: 10.1200/JCO.2000.18.4.743
5. Ganz PA. Monitoring the physical health of cancer survivors: a survivorship-focused medical history. J Clin Oncol. (2006) 24:5105–11. doi: 10.1200/JCO.2006.06.0541
6. Salvo EM, Ramirez AO, Cueto J, Law EH, Situ A, Cameron C, et al. Risk of recurrence among patients with HR-positive, HER2-negative, early breast cancer receiving adjuvant endocrine therapy: A systematic review and meta-analysis. Breast. (2021) 57:5–17. doi: 10.1016/j.breast.2021.02.009
7. Ruiz-Casado A, Álvarez-Bustos A, De Pedro CG, Méndez-Otero M, and Romero-Elías M. Cancer-related fatigue in breast cancer survivors: A review. Clin Breast Cancer. (2021) 21:10–25. doi: 10.1016/j.clbc.2020.07.011
8. Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. (1990). Delta Trade Paperback/Bantam Dell.
9. Chambers R, Lo BCY, and Allen NB. The impact of intensive mindfulness training on attentional control, cognitive style, and affect. Cogn Ther Res. (2008) 32:303–22. doi: 10.1007/s10608-007-9119-0
10. Cramer H, Lauche R, Paul A, and Dobos G. Mindfulness-based stress reduction for breast cancer-a systematic review and meta-analysis. Curr Oncol. (2012) 19:e343–352. doi: 10.3747/co.19.1016
11. Brahmi SA, El FZ, Benbrahim Z, Akesbi Y, Amine B, Nejjari C, et al. Complementary medicine use among Moroccan patients with cancer: a descriptive study. Pan Afr Med J. (2011) 10:36.
12. Greenlee H, Balneaves LG, Carlson LE, Cohen M, Deng G, Hershman D, et al. Clinical practice guidelines on the use of integrative therapies as supportive care in patients treated for breast cancer. J Natl Cancer Inst Monogr. (2014) 2014:346–58. doi: 10.1093/jncimonographs/lgu041
13. Lamothe M, Rondeau É, Malboeuf-Hurtubise C, Duval M, and Sultan S. Outcomes of MBSR or MBSR-based interventions in health care providers: A systematic review with a focus on empathy and emotional competencies. Complement Ther Med. (2016) 24:19–28. doi: 10.1016/j.ctim.2015.11.001
14. Jing S, Zhang A, Chen Y, Shen C, Currin-Mcculloch J, Zhu C, et al. Mindfulness-based interventions for breast cancer patients in China across outcome domains: a systematic review and meta-analysis of the Chinese literature. Support Care Cancer. (2021) 29:5611–21. doi: 10.1007/s00520-021-06166-0
15. Haller H, Winkler MM, Klose P, Dobos G, Kümmel S, Cramer H, et al. Mindfulness-based interventions for women with breast cancer: an updated systematic review and meta-analysis. Acta Oncol. (2017) 56:1665–76. doi: 10.1080/0284186X.2017.1342862
16. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
17. Park S, Sato Y, Takita Y, Tamura N, Ninomiya A, Kosugi T, et al. Mindfulness-based cognitive therapy for psychological distress, fear of cancer recurrence, fatigue, spiritual well-being, and quality of life in patients with breast cancer-A randomized controlled trial. J Pain Symptom Manage. (2020) 60:381–9. doi: 10.1016/j.jpainsymman.2020.02.017
18. Xin C, Huan Z, and Ling L. A study of mindfulness training intervention on cancer-related fatigue in breast cancer patients after chemotherapy. Chongqing Med Sci. (2016) 45:2953–5.
19. Fanbenben. Effects of mindfulness-based stress reduction therapy on cancer-related fatigue and sleep quality in patients with breast cancer undergoing chemotherapy. Chin School Doctor. (2021) 35:111–3.
20. Jinmei W, Huiyuan M, and Yalan S. Effects of mindfulness relaxation training on fear of cancer recurrence, cancer-related fatigue and sleep quality in patients with breast cancer. Oncol Clin Rehabil China. (2021) 28:228–33. doi: 10.13455/j.cnki.cjcor.2021.02.26
21. Bower JE, Crosswell AD, Stanton AL, Crespi CM, Winston D, Arevalo J, et al. Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer. (2015) 121:1231–40. doi: 10.1002/cncr.29194
22. Reich RR, Lengacher CA, Kip KE, Shivers SC, Schell MJ, Shelton MM, et al. Baseline immune biomarkers as predictors of MBSR(BC) treatment success in off-treatment breast cancer patients. Biol Res Nurs. (2014) 16:429–37. doi: 10.1177/1099800413519494
23. Lengacher CA, Reich RR, Paterson CL, Ramesar S, Park JY, Alinat C, et al. Examination of broad symptom improvement resulting from mindfulness-based stress reduction in breast cancer survivors: A randomized controlled trial. J Clin Oncol. (2016) 34:2827–34. doi: 10.1200/JCO.2015.65.7874
24. Jiangzhen W and Maoxueping. Effects of mindfulness-based stress reduction training on perceived stress and cancer-related fatigue in patients with advanced breast cancer. Clin Educ Gen Pract. (2019) 17:575–6. doi: 10.13558/j.cnki.issn1672-3686.2019.06.033
25. Kun W, Changying C, Jiansai A, Yang Z, and Lixia Q. The effects of mindfulness-based stress reduction on fatigue and sleep quality for breast cancer patients undergoing chemotherapy. Chin J Nurs. (2017) 52:518–23.
26. Lengacher CA, Reich RR, Rodriguez CS, Nguyen AT, Park JY, Meng H, et al. Efficacy of mindfulness-based stress reduction for breast cancer (MBSR(BC)) a treatment for cancer-related cognitive impairment (CRCI): A randomized controlled trial. J Integr Complement Med. (2025) 31:75–91. doi: 10.1089/jicm.2024.0184
27. Xu F, Zhang J, Xie S, and Li Q. Effects of Mindfulness-Based Cancer Recovery training on anxiety, depression, post-traumatic stress disorder, and cancer-related fatigue in breast neoplasm patients undergoing chemotherapy. Med (Baltimore). (2024) 103:e38460. doi: 10.1097/MD.0000000000038460
28. Xie C, Dong B, Wang L, Jing X, Wu Y, Lin L, et al. Mindfulness-based stress reduction can alleviate cancer- related fatigue: A meta-analysis. J Psychosom Res. (2020) 130:109916. doi: 10.1016/j.jpsychores.2019.109916
29. Castanhel FD and Liberali R. Mindfulness-Based Stress Reduction on breast cancer symptoms: systematic review and meta-analysis. Einstein (Sao Paulo). (2018) 16:eRW4383. doi: 10.31744/einstein_journal/2018RW4383
30. Shapiro SL, Carlson LE, Astin JA, and Freedman B. Mechanisms of mindfulness. J Clin Psychol. (2006) 62:373–86. doi: 10.1002/jclp.20237
31. Takahashi T, Murata T, Hamada T, Omori M, Kosaka H, Kikuchi M, et al. Changes in EEG and autonomic nervous activity during meditation and their association with personality traits. Int J Psychophysiol. (2005) 55:199–207. doi: 10.1016/j.ijpsycho.2004.07.004
32. Carlson LE and Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. (2005) 12:278–85. doi: 10.1207/s15327558ijbm1204_9
33. Vago DR and Silbersweig DA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Front Hum Neurosci. (2012) 6:296. doi: 10.3389/fnhum.2012.00296
34. Hoffman AJ, Brintnall RA, and Cooper J. Merging technology and clinical research for optimized post-surgical rehabilitation of lung cancer patients. Ann Transl Med. (2016) 4:28. doi: 10.3978/j.issn.2305-5839.2016.01.10
35. Minton O and Stone P. How common is fatigue in disease-free breast cancer survivors? A systematic review of the literature. Breast Cancer Res Treat. (2008) 112:5–13. doi: 10.1007/s10549-007-9831-1
36. Armes J, Chalder T, Addington-Hall J, Richardson A, and Hotopf M. A randomized controlled trial to evaluate the effectiveness of a brief, behaviorally oriented intervention for cancer-related fatigue. Cancer. (2007) 110:1385–95. doi: 10.1002/cncr.22923
37. Yinxia T, Ping W, Lihua L, and Hui C. The role of short-term mindfulness training in the care of advanced lung cancer patients. Shanghai Nurs. (2017) 17:20–3.
38. Matthews EE, Berger AM, Schmiege SJ, Cook PF, Mccarthy MS, Moore CM, et al. Cognitive behavioral therapy for insomnia outcomes in women after primary breast cancer treatment: a randomized, controlled trial. Oncol Nurs Forum. (2014) 41:241–53. doi: 10.1188/14.ONF.41-03AP
Keywords: MBSR, breast cancer, cancer-related fatigue, meta-analysis, fatigue
Citation: Wang X, Gao L, Pang Y and Huang T (2025) Effect of mindfulness-based stress on cancer-related fatigue in breast cancer patients: a systematic review and meta-analysis. Front. Oncol. 15:1585383. doi: 10.3389/fonc.2025.1585383
Received: 20 March 2025; Accepted: 09 September 2025;
Published: 29 September 2025.
Edited by:
Mohamed Shehata, Midway College, United StatesReviewed by:
Semra Bulbuloglu, Istanbul Aydın University, TürkiyeAhmad Gebreil, University of Louisville, United States
Copyright © 2025 Wang, Gao, Pang and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Gao, Z2FvbGVpQHMuZGx1LmVkdS5jbg==
 Xiong Wang1
Xiong Wang1 Lei Gao
Lei Gao Yuqi Pang
Yuqi Pang