- 1Department of Urology, The Second Hospital of Lanzhou University, Lanzhou, China
- 2Gansu Province Clinical Research Center for Urology, Lanzhou, China
- 3Key Laboratory of Gansu Province for Urological Diseases, Lanzhou, China
Purpose: This study aimed to provide a case of scrotal hemangioma and examine its characteristics.
Methods: We presented a case report involving a sixteen-year-old male, detailing symptoms, physical examination, imaging studies, diagnosis, and treatment. We conducted a thorough literature analysis of case reports and examined their clinical characteristics, pathological categorization, recurrence, and complications.
Results: Our study comprised 21 patients with scrotal hemangioma. The average age was 27.14 years, with a range from 21 days to 84 years. 57.1% of the hemangiomas affected the organs. 61.9% of patients were situated on the right side of the scrotum. Ninety percent of patients experienced no pain. Merely 33.3% of patients exhibited additional symptoms, which encompassed azoospermia, hemorrhage, calcification, hydrocele, thrombosis, and ulceration. The predominant pathological classification was cavernous scrotal hemangioma, representing 38.1% of the cases. All patients received surgical resection, and the majority experienced neither relapse nor postoperative complications.
Conclusions: Scrotal hemangioma, an uncommon benign neoplasm in adolescents, frequently remains asymptomatic but may disrupt fertility and, in rare instances, lead to severe problems. Timely identification, diagnosis, and surgical intervention are essential for good patient outcomes.
Introduction
Hemangioma is a prevalent benign neoplasm of soft tissue resulting from vascular malformation, predominantly congenital, with a threefold higher frequency in girls compared to males (1). Hemangioma predominantly manifests in the head, neck, trunk, and limbs, along with the bladder and prostate, whereas the scrotum represents fewer than 1% of cases (2). Scrotal hemangioma can be classified into capillary, cavernous, racemose, and mixed types based on its clinical and pathological features (3). In addition to this, venous and anastomosing kinds of hemangioma also exist. The cavernous subtype of scrotal hemangiomas is the most commonly observed (4). The lesion generally manifests as thicker skin with soft lumps, along with dilated veins that resemble worms. It is bluish-purple or grayish-red, predominantly situated on the scrotum, and may impact adjacent tissues like the testicle, spermatic cord, and penis. The majority of patients with scrotal hemangioma report no pain; nevertheless, symptoms such as bleeding, ulceration, heaviness, or edema of the scrotum may occasionally manifest (5). The distinction among hemangioma, varicocele, and inguinal hernia primarily depends on imaging studies (6). Magnetic resonance imaging (MRI) is superior to ultrasound in diagnosing and differentiating scrotal hemangioma. Like vascular tumors in other regions, scrotal hemangiomas are often managed with surgical excision. Moreover, other therapeutic modalities encompass laser therapy, intervention, and sclerotherapy (7–9). This condition seldom recurs post-surgery, with little postoperative consequences. The essential factor in its therapy is the precise preoperative diagnosis and a comprehensive understanding of its anatomical interaction with adjacent tissues.
Methods
Search strategy
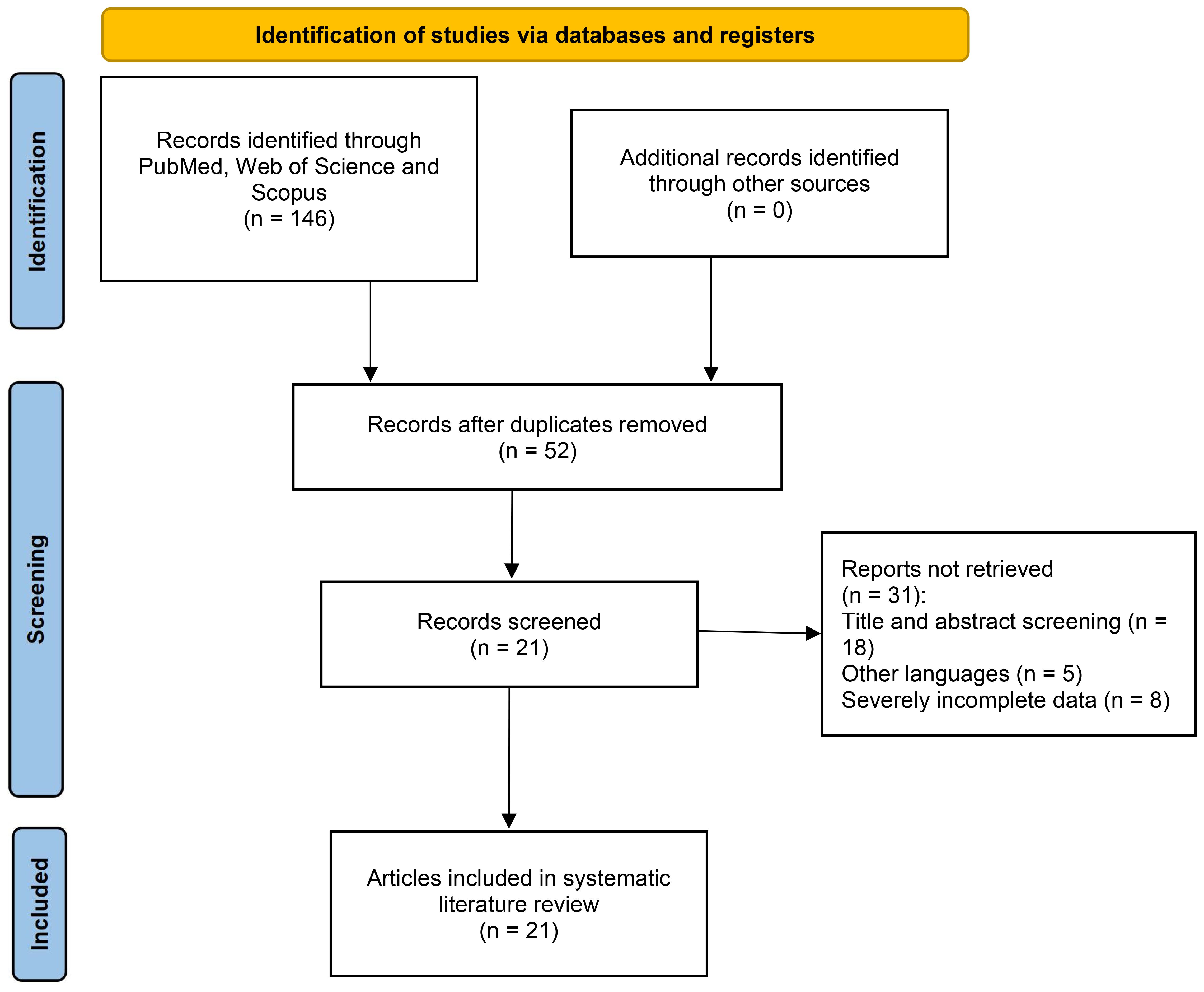
This systematic literature review was conducted independently by two reviewers following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards (CRD420251116989) to enhance understanding of the subject and provide valuable insights to the medical industry. Our investigation encompassed querying the PubMed, Web of Science, and Scopus databases. The search utilized a systematic amalgamation of phrases focusing on both the scrotum and angioma, specifically: [(Scrotum OR Scrotal) AND (Hemangioma OR Angioma OR Hemangiomas)]. The search occurred on 30 January 2025. Furthermore, the references were verified to prevent omissions (Figure 1).
Inclusion and exclusion criteria
All studies in the English language concerning scrotal hemangioma were incorporated. The hemangioma was situated in the scrotum, rather than coming from other organs, and may have involved more organs. Studies and reviews in non-English languages were removed from our research. Due to the limited number of accessible instances, we classify patients with incomplete clinical characteristics as uncertain.
Case selection, data extraction, and quality assessment
Two researchers independently assessed paper titles and abstracts utilizing established search parameters to identify studies that fulfilled the inclusion criteria. The two identical researchers evaluated the entire texts for inclusion and collected data. Subsequently, all selected cases were analyzed, and the information was gathered using Excel.
Clinical characteristics were gathered for each included case, encompassing age, tumor location, and its relation to adjacent organs, pain and other symptoms, pathological categorization, recurrence, and complications. The baseline analysis was performed on the gathered instances using R (http://www.Rproject.org).
Results
Case report
A sixteen-year-old Chinese male had a walnut-sized purple mass on the left side of his scrotum, measuring approximately 4cm by 4cm. The first lesion was discovered a week ago, and since then, its size has progressively increased, accompanied by discomfort upon palpation, without any swelling. The patient reported no history of trauma, abdominal or pelvic surgery, congenital disorders, or familial hereditary problems.
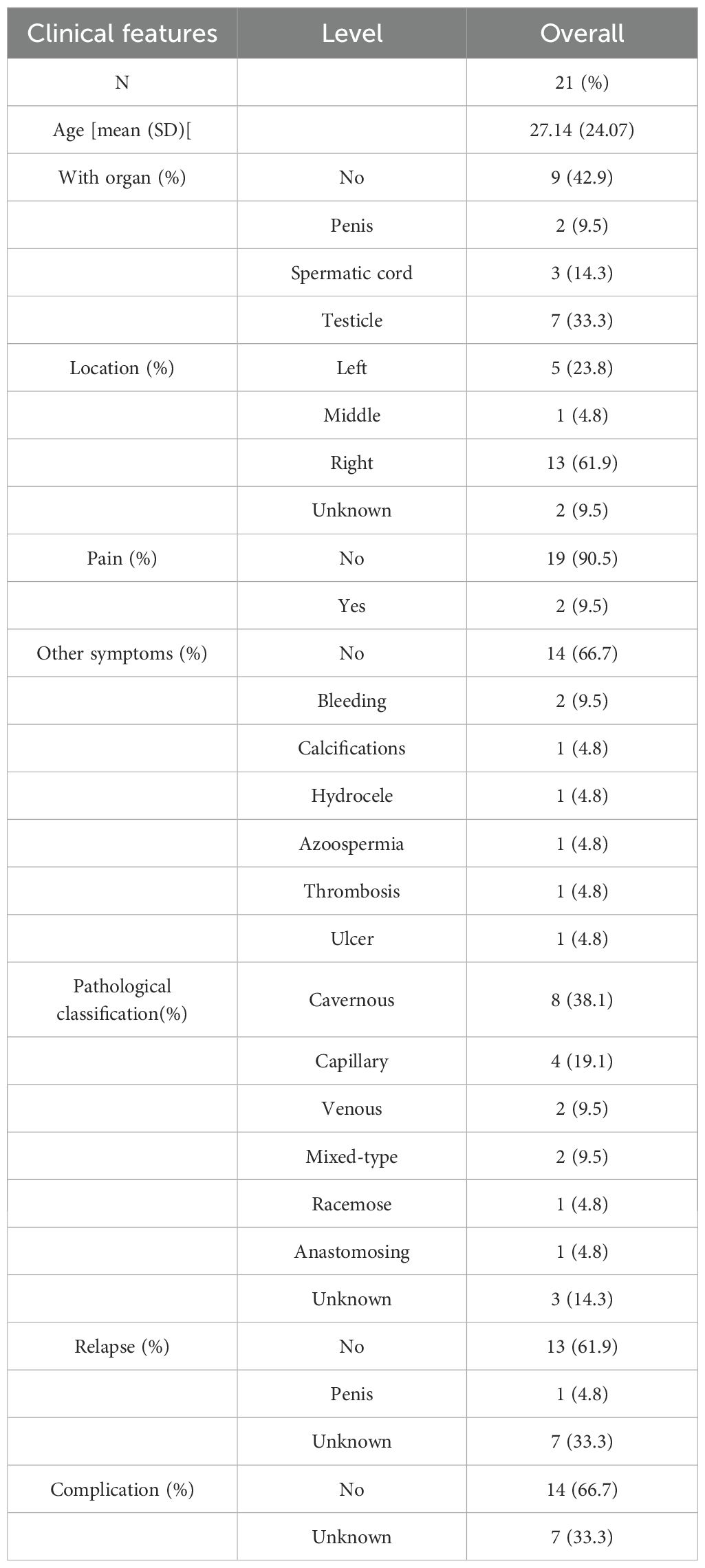
Ultrasound imaging revealed a hypo-echoic, irregularly shaped mass in the left epididymis head region, measuring 5.5 cm × 4.7 cm × 3.2 cm, characterized by distinct borders and internal hyperechoic septations, with no evident blood flow signals. A Computed Tomography (CT) scan of the pelvis indicated a lobulated soft tissue mass on the left testis, accompanied by several enlarged inguinal lymph nodes bilaterally (Figures 2A, B). The MRI demonstrated a consistently isointense T1 and hyperintense T2 signal mass with many septations in the left testicular tunica albuginea, exhibiting a strong signal on diffusion-weighted imaging (DWI) (Figures 2C, D). All laboratory tests were routine, particularly Serum Alpha-Fetoprotein (1.26 ng/ml) and Human Chorionic Gonadotropin (0.01 Miu/ml).
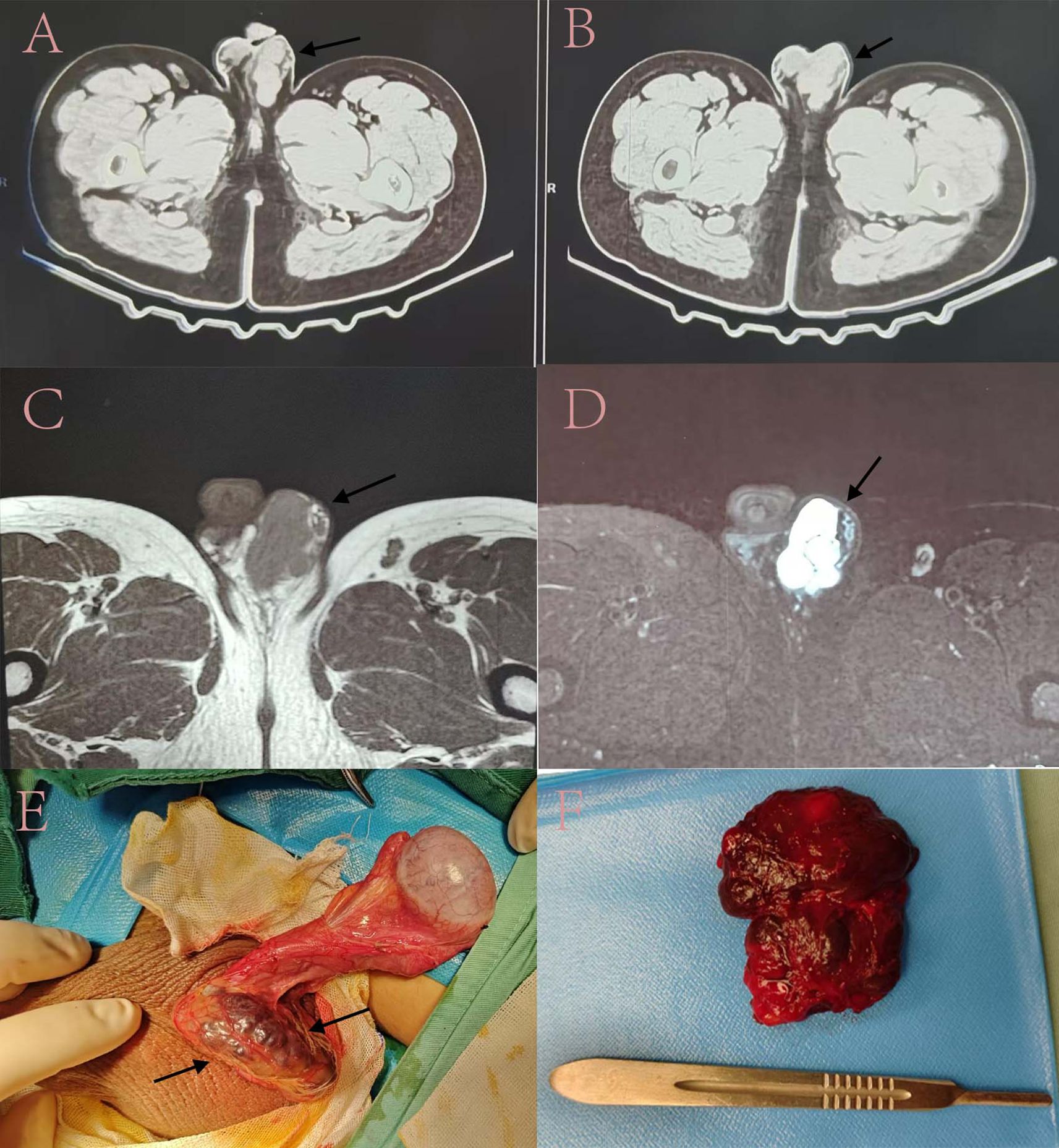
Figure 2. Imaging assessment and intraoperative observations. (A, B). The results of Pelvic Computed Tomography; (C, D). The results of magnetic resonance imaging; (E, F). The tumor’s position during the surgical procedure and the subsequent specimen obtained postoperatively. Numerous black arrows denote the tumor’ s position.
We conducted a surgical excision for the patient. A clear demarcation was noted between the hemangioma and the testis during the surgical investigation. Therefore, the choice was made to retain the testis while excising solely the hemangioma (Figures 2E, F). The postoperative pathology report indicated a cavernous hemangioma. The tumor displays a lobulated architecture consisting of several proliferating tiny blood vessels with thin walls (Figure 3). Post-operation, the patient exhibited no discernible discomfort at the surgical site and had satisfactory recovery. Telephone follow-up at nine months post-surgery revealed the patient experienced no postoperative problems or recurrence.
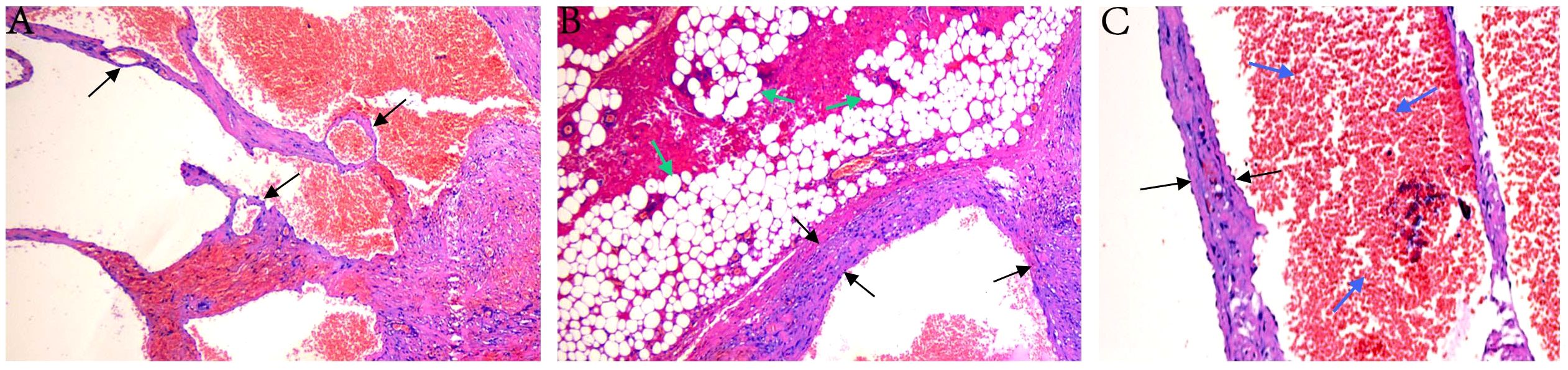
Figure 3. Histopathological images. (A) Large, dilated vascular channels containing red blood cells (RBCs) within their lumina. (B) Dilated, thick-walled blood vessels surrounded by mature adipose tissue. (C) High-power view showing dilated blood vessels with intraluminal RBCs and prominent endothelial lining. The black arrows indicate vessel walls, green arrows indicate adipocytes, and blue arrows indicate RBCs.
Result of baseline analysis
Our investigation comprised a total of 21 patients with scrotal hemangioma (2, 5, 10–28). The age varied from 21 days to 84 years, with a mean age of 27.14 years. In 57.1% of instances, the hemangioma affected genital structures, including the penis, spermatic cord, or testicle. Sixty-one point nine percent of patients were situated on the right side of the scrotum. Ninety percent of patients experienced no pain. 33.3% of patients exhibited additional symptoms or complications, including azoospermia, hemorrhage, calcification, hydrocele, thrombosis, and ulceration. The predominant pathological classification was cavernous scrotal hemangioma, comprising 38.1% of the cases, followed by capillary hemangioma at 19.1%. Despite the application of alternative therapeutic modalities, all patients underwent surgical resection. The majority of patients experienced neither recurrence nor surgical complications (Table 1).
Discussion
Hemangioma, specifically cavernous hemangioma, is an uncommon congenital condition in the scrotum. Scrotal hemangiomas predominantly manifest in youngsters, with 70%-90% of instances occurring before the age of 7 (29). Nevertheless, a limited number of patients with the illness display significant symptoms or consequences, especially when the lesion is diminutive and progresses gradually. Attracting patients’ early attention is challenging unless a mass is identified during inspection. The individuals identified and treated are, in fact, adolescents or even adults. The lesion manifests as a pliable mass under the scrotal skin or as many engorged veins creating a serpentine mass with a bluish-purple or gray hue. It is frequently noted in the scrotal wall or within the scrotum. This illness may be readily misinterpreted as varicocele, lymphangioma, or arteriovenous malformation (27, 30). Hemangiomas generally present unilaterally and, when substantial in size, may involve the spermatic cord, testis, penis, and spread to the perineum and buttocks (28). It is essential to differentiate scrotal hemangioma from benign and malignant malignancies of these organs.
Patients may exhibit varying tumor-related abnormalities or other symptoms based on the location, size, and level of hemangioma involvement. A deep scrotal hemangioma exhibiting ulceration, pruritus, and hemorrhage was documented (31), and thrombosis was identified within the scrotal hemangioma (12). Some patients may present with additional findings such as calcifications or associated hydroceles (18, 21). A patient with scrotal hemangioma had azoospermia resulting from testicular injury induced by elevated temperatures associated with the condition (5).
Imaging examination, as the primary diagnostic instrument, is essential for enabling doctors to diagnose hemangiomas accurately. This method not only aids in the detection of hemangiomas but also assists in excluding alternative differential diagnoses. Ultrasound is a fundamental assessment that can initially ascertain the characteristics and dimensions of scrotal malignancies. Manifestations encompass robust blood flow signs and a variable arterial spectrum (26). Nevertheless, because of the ambiguous presentation of the tumors, the precision of ultrasound is limited, and at times, it is challenging to differentiate them from varicoceles. CT is essential for assessing hemangiomas with calcification or venous calculi. MRI imaging provides exceptional clarity for malignancies, especially soft tissue tumors, facilitating the identification of anatomical relationships between tumors and adjacent tissues to determine suitable surgical approaches (6). Pathological examination is unequivocally the gold standard for diagnosis.
Surgical excision is generally selected for the management of scrotal hemangioma. When the tumor infiltrates the internal organs of the scrotum, the surgical approach is determined by the extent of this infiltration. Some people have undergone orchiectomy, and although the contralateral testicle is preserved, it still affects the patient. Consequently, partial testicular resection may be deemed appropriate. In addition, there are also treatments including arteriosclerosis (8, 9), laser (32, 33)and medication such as propranolol (34). In young patients, these methods carry significant risks of recurrence and consequences, and their application is not prevalent. A patient with a congenital hemangioma on the penis and scrotum underwent interventional embolization and achieved a favorable prognosis. In contrast to malignant tumors, scrotal hemangiomas, being benign, exhibit little invasive potential and recurrence, with the majority of patients experiencing a favorable prognosis.
Conclusions
This study presents a case report of a 16-year-old boy with scrotal hemangioma, outlining the diagnostic procedure and treatment management. Furthermore, we executed an exhaustive examination of 21 previously documented instances from the literature and analyzed their demographic and clinical attributes. These findings offer critical insights to aid clinicians in the early diagnosis and appropriate treatment of this illness.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Medical Ethics. Committee of the Second Hospital of Lanzhou University (Project Number: 2024A-014). The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from primarily isolated as part of your previous study for which ethical approval was obtained. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the minor(s)’ legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZC: Investigation, Writing – original draft. JM: Writing – review & editing. JW: Writing – review & editing. HG: Investigation, Visualization, Writing – review & editing. JN: Data curation, Investigation, Writing – review & editing. LY: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This paper is supported by The Special Fund Project for Central Guiding Local Science and Technology Development(24ZYQA050), and Key Research and Development Plan of the Science and Technology Department of Gansu Province (22YF7FA090).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MRI, magnetic resonance imaging; CT, Pelvis Computed Tomography; DWI, Diffusion weighted imaging.
References
1. Siu WS, Chen YC, and Ding DC. Vulvar hemangioma: A review. Diagnost (Basel). (2025) 15:1270. doi: 10.3390/diagnostics15101270
2. Lin CY, Sun GH, Yu DS, Wu CJ, Chen HI, and Chang SY. Intrascrotal hemangioma. Arch Androl. (2002) 48:259–65. doi: 10.1080/01485010290031565
3. Marino F, Lorusso G, Gandi C, Ragonese M, Pierconti F, and Sacco E. Epithelioid (Histiocytoid) hemangioma of the testis: A case report and literature review of a rare benign tumor. Urologia. (2025) 92:169–73. doi: 10.1177/03915603241292838
4. Munteanu IR, Novaconi RC, Merce AP, Dima CN, Falnita LS, Manzur AR, et al. Cardiac hemangiomas: A five-year systematic review of diagnosis, treatment, and outcomes. Cancers (Basel). (2025) 17:1532. doi: 10.3390/cancers17091532
5. Gotoh M, Tsai S, Sugiyama T, Miyake K, and Mitsuya H. Giant scrotal hemangioma with azoospermia. Urology. (1983) 22:637–9. doi: 10.1016/0090-4295(83)90315-1
6. Zahran MF and Yuri P. A rare pediatric scrotal hemangioma: A case report and comprehensive analysis of n Bloc Excision as definitive treatment. Int J Surg Case Rep. (2024) 116:109347. doi: 10.1016/j.ijscr.2024.109347
7. Wang C, Wu F, Peng W, and Jiang H. A case study regarding treating the congenital hemangioma over penis and scrotum by interventional embolization. Asian J Surg. (2023) 46:4553–5. doi: 10.1016/j.asjsur.2023.05.004
8. Movassaghi M, Wu J, and Carpenter CP. Pediatric penile non-involuting congenital hemangioma with an associated pyogenic granuloma: surgical management of a rare vascular anomaly. Urology. (2021) 158:197–9. doi: 10.1016/j.urology.2021.09.012
9. Ergin G, Kopru B, Ebiloglu T, Kirac M, Kibar Y, Fuat Cicek A, et al. Unusual intrascrotal lesions in adults in urological practice. Arch Esp Urol. (2019) 72:955–64.
10. Laarif S, Trabelsi F, Daïb A, Ben Abdallah R, Hellal Y, and Kaabar N. Inguinoscrotal hernia revealing a testicular hemangioma: Report of a neonatal case. Urol Case Rep. (2023) 50:102491. doi: 10.1016/j.eucr.2023.102491
11. Moneir WM and AlShammari A. Excision of an ulcerated scrotal hemangioma in a four-month-old boy: A case report and review of literature. Cureus. (2022) 14:e25844. doi: 10.7759/cureus.25844
12. Iafrate M, Leone N, Tiengo C, and Zattoni F. Surgical treatment of large hemangioma of the scrotum in a young adult male. Arch Ital Urol Androl. (2020) 92:53–4. doi: 10.4081/aiua.2020.1.53
13. Gangkak G, Mishra A, Priyadarshi S, and Tomar V. Large genital cavernous hemangioma: A rare surgically correctable entity. Case Rep Urol. (2015) 2015:950819. doi: 10.1155/2015/950819
14. Białek W, Rudzki S, and Wronecki L. Capillary hemangioma of the testis. A case report of a rare benign tumor. J Ultrason. (2016) 16:87–93. doi: 10.15557/JoU.2016.0009
15. Zaidi SN and Fathaddin AA. Testicular capillary hemangioma–a case report of a rare tumor. Indian J Pathol Microbiol. (2012) 55:557–9. doi: 10.4103/0377-4929.107815
16. Vavallo A, LaFrancesChina F, Lucarelli G, Bettocchi C, Ditonno P, Battaglia M, et al. Capillary hemangioma of the scrotum mimicking an epididymal tumor: case report. Arch Ital Urol Androl. (2014) 86:395–6. doi: 10.4081/aiua.2014.4.395
17. Ergün O, Ceylan BG, Armagan A, Kapucuoglu N, Ceyhan AM, and Perk H. A giant scrotal cavernous hemangioma extending to the penis and perineum: a case report. Kaohsiung J Med Sci. (2009) 25:559–61. doi: 10.1016/S1607-551X(09)70549-2
18. Jeon YS, Cho SG, Kim WH, and Choi SJ. Cavernous haemangioma of the spermatic cord in a child. Pediatr Radiol. (2006) 36:1323–5. doi: 10.1007/s00247-006-0325-9
19. Mitsuhashi M, Harima M, Kobayakawa H, and Asakawa M. Racemose hemangioma of the scrotum: a case report. Hinyokika Kiyo. (2002) 48:503–6.
20. Konya E, Uejima S, Ohnishi N, Sugiyama T, and Kurita T. Venous hemangioma of the scrotum: a case report. Hinyokika Kiyo. (2000) 46:731–3.
21. Tada M, Takemura S, Takimoto Y, and Kishimoto T. A case of cavernous hemangioma of the testis. Hinyokika Kiyo. (1989) 35:1969–71.
22. Kuraoka T, Taguchi K, Hosokawa S, Shimada K, Mori Y, Ikoma F, et al. A case of capillary hemangioma of the testis in a child. Hinyokika Kiyo. (1994) 40:361–3.
23. Komeda H, Horie M, and Isogai K. A case report of scrotal hemangioma. Hinyokika Kiyo. (1989) 35:911–2.
24. Senoh H, Ichikawa Y, Okuyama A, Takaha M, and Sonoda T. Cavernous hemangioma of scrotum and penile shaft. Urol Int. (1986) 41:309–11. doi: 10.1159/000281225
25. Zhang ZY, Hong P, Deng SH, Tang SY, Liu Z, He HY, et al. Spermatic cord anastomosing hemangioma mimicking a Malignant inguinal tumor: A case report and literature review. Front Surg. (2022) 9:930160. doi: 10.3389/fsurg.2022.930160
26. Chavan D and Javalgi AP. Scrotal hemangioma: a case report. J Clin Diagn Res. (2014) 8:ND03–4. doi: 10.7860/JCDR/2014/9777.5264
27. Tromp EE, Kouwenhoven ST, Quint KD, Gmelig Meijling KA, and Genders RE. Unilateral scrotal angiomas: An expression of underlying varicocele. Scand J Urol. (2016) 50:88–9. doi: 10.3109/21681805.2015.1064471
28. Eastridge RR, Carrion HM, and Politano VA. Hemangioma of scrotum, perineum, and buttocks. Urology. (1979) 14:61–3. doi: 10.1016/0090-4295(79)90216-4
29. Ye D, Ma X, and Yang X. Scrotal calcinosis: a case report and literature review. Am J Clin Exp Urol. (2022) 10:194–8.
30. Aslan S, Eryuruk U, Ogreden E, Tasdemir MN, Cınar I, and Bekci T. Intrascrotal extratesticular schwannoma: A rare cause of scrotal mass. Curr Med Imaging. (2023) 19:1210–3. doi: 10.2174/1573405618666220930151519
31. Dejman B, Makarem A, Ahmed F, and Askarpour M. Scrotal cavernous hemangioma presented with pruritus in a teenager: A case report. Clin Case Rep. (2023) 11:e7315. doi: 10.1002/ccr3.7315
32. Canu D, Mary-Prey S, and Leauté-Labreze C. Diagnosis and management of infantile hemangiomas: Tremendous advances over the last 15 years. Presse Med. (2025) 54:104291. doi: 10.1016/j.lpm.2025.104291
33. Dubar P, Mathis T, Hucteau E, Thariat J, Nhari M, Maschi C, et al. A fast protocol for photodynamic therapy in exudative choroidal circumscribed hemangioma: Early laser irradiance after end of verteporfin infusion. Acta Ophthalmol. (2025). doi: 10.1111/aos.17513
Keywords: scrotum hemangioma, scrotum tumor, cavernous hemangioma, surgical treatment, diagnosis and prognosis
Citation: Chang Z, Man J, Wang J, Gui H, Niu J and Yang L (2025) Scrotal hemangioma: a case report and systematic literature review. Front. Oncol. 15:1586677. doi: 10.3389/fonc.2025.1586677
Received: 03 March 2025; Accepted: 05 August 2025;
Published: 20 August 2025.
Edited by:
Fabio Grizzi, Humanitas Research Hospital, ItalyReviewed by:
Alessandro Boscarelli, Institute for Maternal and Child Health Burlo Garofolo (IRCCS), ItalySumanta Das, Fortis Memorial Research Institute, India
Copyright © 2025 Chang, Man, Wang, Gui, Niu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Yang, ZXJ5X3lhbmdsaUBsenUuZWR1LmNu
†These authors have contributed equally to this work
 Zhe Chang1,2,3†
Zhe Chang1,2,3† Jirong Wang
Jirong Wang Li Yang
Li Yang