- 1Department of Breast Surgery, First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaan’xi, China
- 2School of Medicine, Xi’an Jiaotong University Health Science Center, Xi’an, Shaan’xi, China
Background: Due to the controversy in the therapeutic effect of locoregional surgery in primary tumors for patients with de novo stage IV breast cancer, the aim of this study was to evaluate the effect of locoregional surgery on overall survival in patients with de novo stage IV breast cancer.
Methods: A computer-based search of PUBMED, Embase, and American Society of Oncology (ASCO) annual meetings abstracts was conducted to identify the prospective trials of the combination of locoregional surgery in primary tumors and systemic therapy in comparison with standard systemic therapy alone for patients with de novo stage IV breast cancer. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated by universal inverse variance and combined across articles. Random-effects model and subgroup analyses were performed to ascertain the origin of this heterogeneity.
Results: A total of 2029 patients from 8 studies were included, with 1014 patients (49.98%) underwent locoregional surgery in primary tumors (surgery group) and 1015 ones (50.02%) with standard systemic therapy alone (no surgery group). Compared to patients in the no surgery group, participants with ER/PR positive breast cancer in the surgery group had improved overall survival (OS) (HR=0.77, 95%CI 0.55-0.93, P=0.01), and improved locoregional progression-free survival (HR=0.36, 95%CI 0.14-0.95, P=0.04) for all participants in the surgery group. And patients with bone-only metastases in the surgery group had insignificantly favorable OS than those in no surgery group (HR=0.70, 95%CI, 0.47-1.04, P=0.08).
Conclusion: Our study demonstrated that locoregional surgery in primary tumors was associated with improved OS for participants with ER/PR positive de novo stage IV breast cancer, and locoregional surgery in primary tumors could be worthy of clinical recommendation for patients with ER/PR positive de novo stage IV breast cancer.
Introduction
As a common malignant disease in women, approximately 6% of patients with breast cancer had distant metastases at first diagnosis (1–4), known as de novo stage IV disease (5). For such patients, systemic therapy (ST), which was determined by hormone receptor (HR) and HER2 expression status, was always recommended as a first-line treatment option by the current international guidelines (6–8). In the clinical practice, localregional treatment (LRT) (surgery or radiotherapy in primary tumors), were always performed to control tumor-related symptoms for patients with de novo stage IV breast cancer, such as pain, skin ulcers, bleeding, and infection (6, 9), although the controversy (10, 11) in the long term survival benefit of locoregional surgery in primary tumors for patients with de novo stage IV breast cancer.
Many retrospective studies have shown that the use of locoregional surgery in primary tumors could effectively improve the overall survival (OS) for patients with de novo stage IV breast cancer (12–18). However, retrospective studies were inherently subject to selection bias and other potential confounders, since younger, healthier patients who responded well to systemic therapy were more likely to undergo surgery (19). In contrast, several prospective randomized controlled trials had produced conflicting results. Many trials reported early locoregional therapy for the primary site did not improve survival in patients presenting with metastatic breast cancer (20–23). However, the MF07-01 trial showed that patients who received LRT followed by ST had a 14% higher OS benefit by the end of the 10-year follow-up compared with the patients who received only ST (16).
To determine the effect of locoregional surgery in primary tumors for de novo stage IV breast cancer patients, a comprehensive meta-analysis of prospective trials was performed to summarize the literature and evaluate the impact of surgical treatment in primary tumors on the survival rate of newly diagnosed stage IV breast cancer patients according to molecular subtype and metastatic site.
Methods
Search strategy
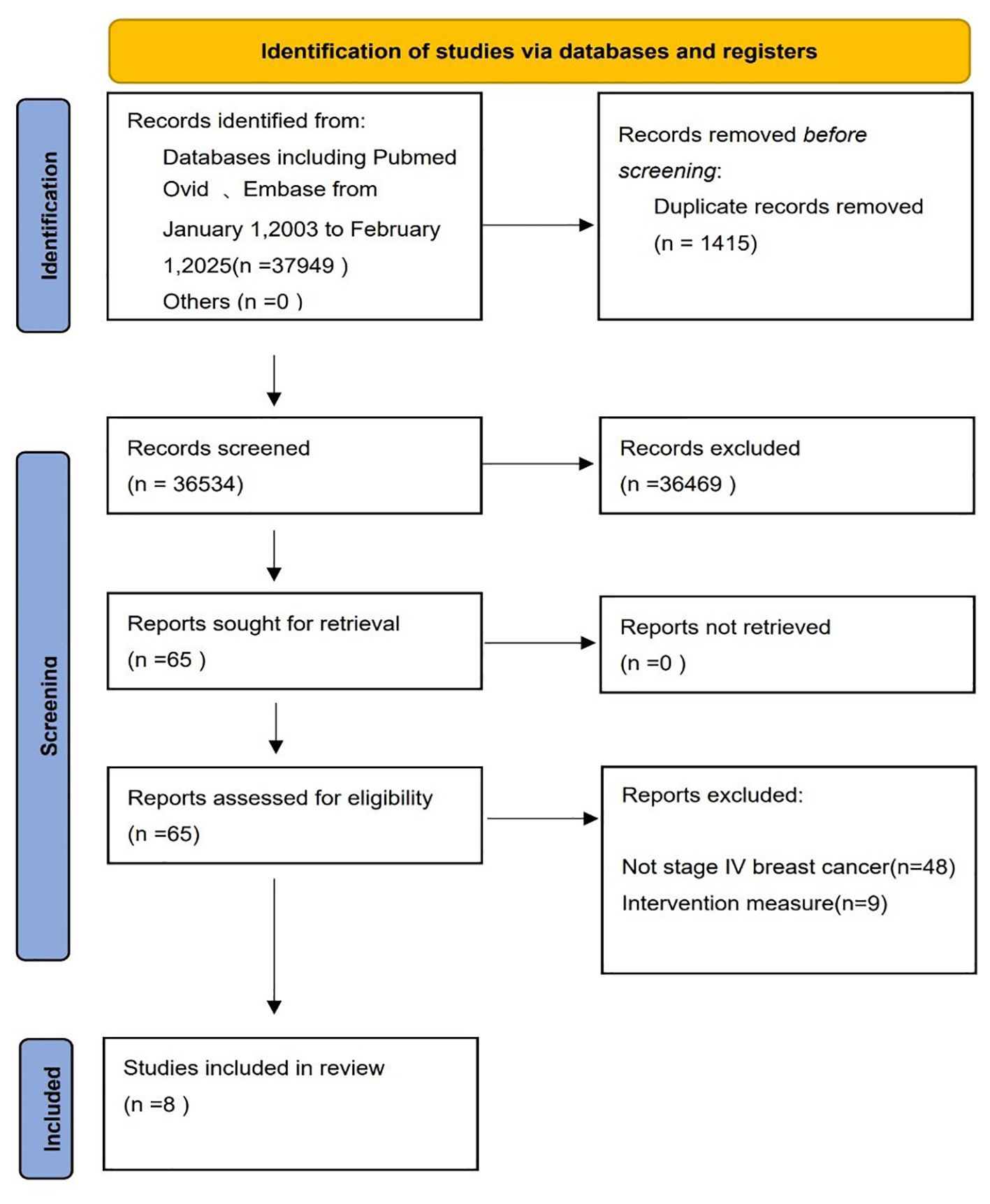
Several sources for relevant original publications were searched through Pubmed, Embase, American Society of Oncology (ASCO) annual meetings abstracts and other databases from January 1, 2003 to February 1, 2025, by the following terms as key words: (stage IV) or (de novo) or (metastatic)) AND (breast cancer) AND ((local) OR (surgery) OR (radiotherapy)), with setting filters: women, prospective trials, and adults. All search strategies were performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (24).
Inclusion and exclusion criteria
Studies that met the following criteria were included: (1) randomized controlled trials and prospective observational studies comparing the combination of surgery in primary tumors plus systemic therapy with systemic therapy alone, (2) adults initially diagnosed with stage IV breast cancer without prior anticancer therapy, and (3) having appropriate survival data - HR and 95% confidence interval (CI) for overall survival (OS) for patients.
Studies were excluded if: (1) hazard ratios (HRs) or 95% CIs for OS were not reported, or the full text was not available for data extraction; (2) all patients underwent surgical resection of the primary tumor alone; (3) reviews, retrospective studies or meta-analyses; (4) not newly diagnosed stage IV breast cancer. This process was independently screened by two authors (Yanbo Sun and Hao Ma), and disagreements were resolved by the third author (Yingjie Li).
Data extraction
The data collected included the author's name, publication year, median follow-up time, mean age,the country for the first author, and the number and proportion of patients in the surgery group versus non-surgery group for each tumor characteristic. TNM stage, histological grade, hormone receptor status, HER2 receptor status, molecular subtype, metastatic site, and the number of metastatic sites were also extracted. For the outcome measures, hazard ratio (HR) and 95% confidence interval (CI) were extracted for overall survival (OS), local progression-free survival (LPFS), and distant progression-free survival (DPFS). Survival data according to molecular subtype and metastatic site were also extracted.
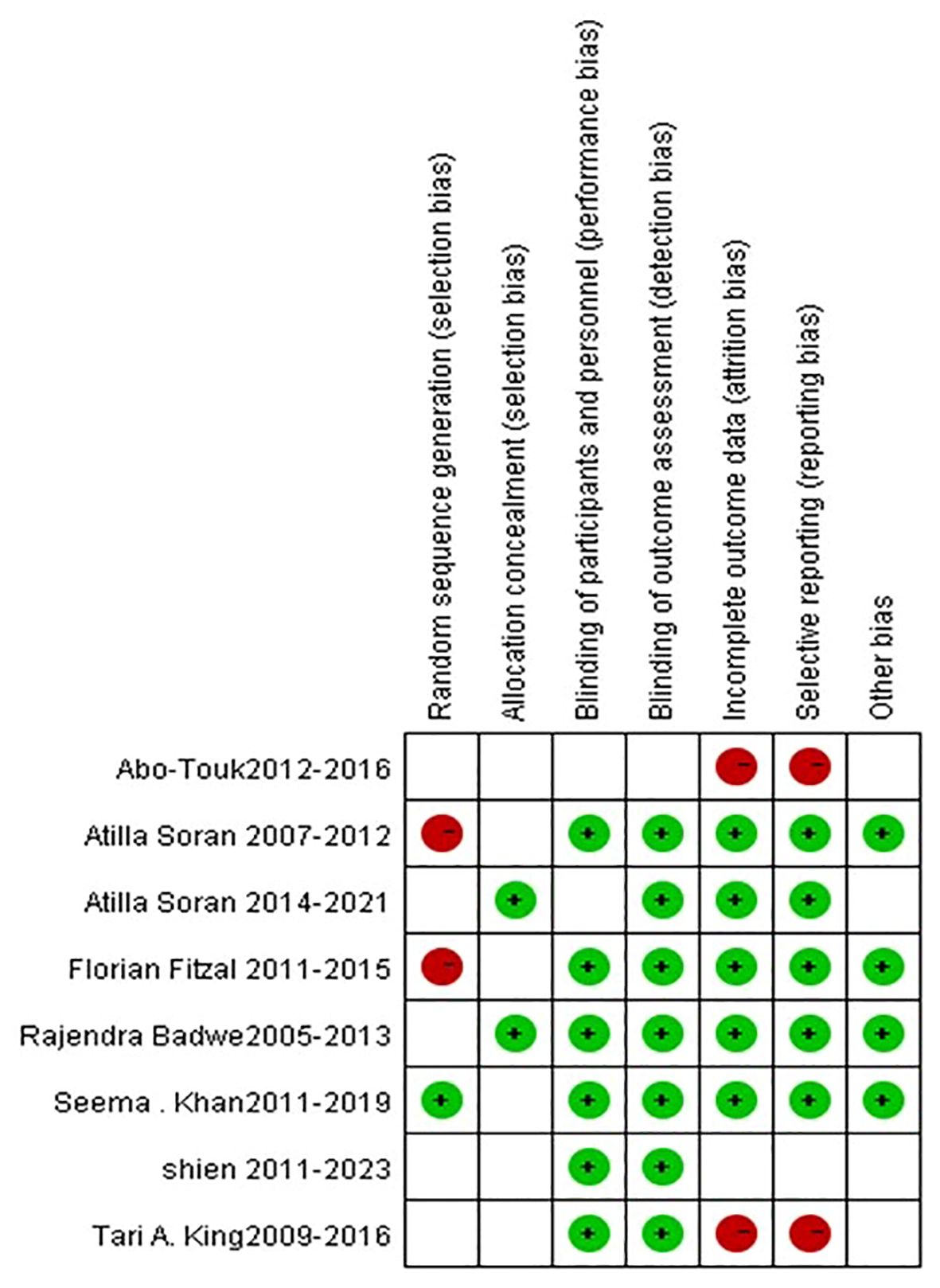
Two authors (Yanbo Sun and Hao Ma) separately used the Cochrane Risk of Bias tool to assess the risk of bias in seven domains for each study (25). For each domain, we graded the risk of bias into the following three levels: unclear risk, low risk, and high risk.
Measures of treatment effect and statistical analysis
OS was used as the primary endpoint, local progression-free survival (LPFS) and distant progression-free survival (DPFS) and hazard ratio (HR) and its 95% confidence interval (95%CI) were performed as the secondary endpoints. At the same time, subgroup analysis was performed to explore the effect of surgery on OS in different subgroups, according to tumor molecular subtype and metastatic site.
Random-effects model with the inverse variance method was performed to obtain summary estimates of RR and 95% CI using Review Manager 5.4 software (Cochrane Collaboration, Oxford, United Kingdom) softwares. The value of HR lower than 1 (<1) was defined as the survival benefit of locoregional surgery in primary tumors, and P<0.05 was statistically significant. Cochran’s Q test or I2 statistic were used to estimate the size of heterogeneity, and P<0.10 or I2 greater than 50% (>50%) was considered the significant heterogeneity. To investigate the source of heterogeneity and the effect of locoregional surgery in primary tumors on OS, subgroup analyses were performed. For the sensitivity analysis, the study were removed one by one and the meta-analysis were-conducted to determine the impact of each study on the meta-analysis. In addition, a funnel plot was performed to assess the risk of publication bias, and forest plots were applied to report the results of the meta-analysis.
Results
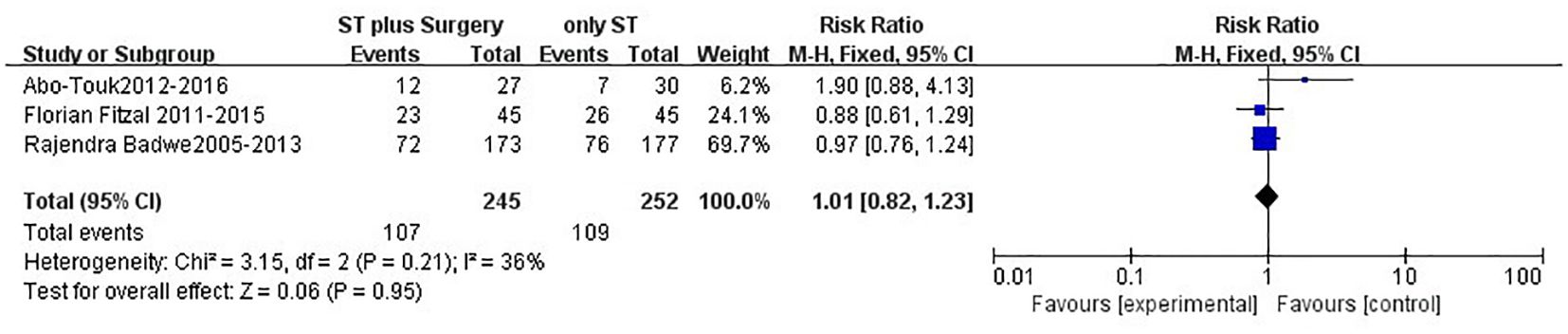
First, among the 37,949 articles found according to the search strategy, a total of 36,534 ones were left after removing the 1415 duplicates. After reading the titles and abstracts,and full texts, a total of 8 studies including 5 RCTs and 3 prospective studies and 2029 patients (17, 18, 20–23, 26, 27), were included. Totally, 1014 patients (49.98%) had underwent locoregional surgery in primary tumors (surgery group), and 1015 patients (50.02%) had no surgery (non-surgery group), as shown in Figure 1 and in Table 1. Table 1 describes the characteristics of the included studies and their patients.
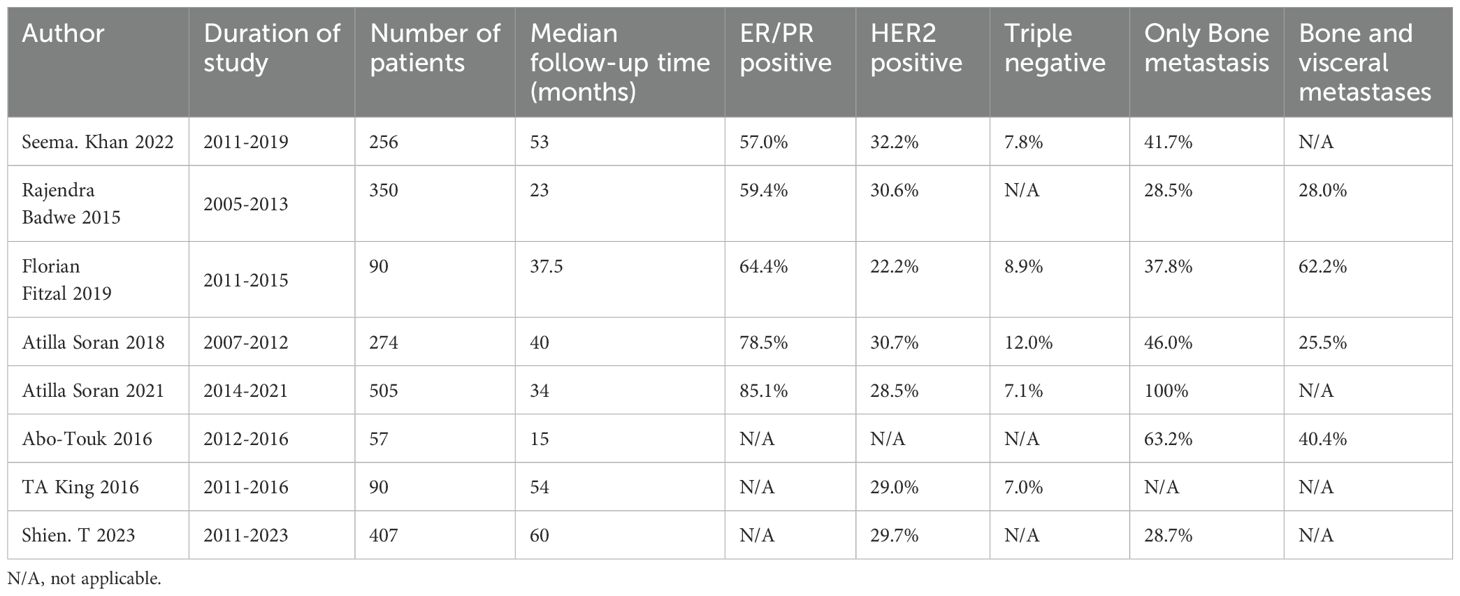
Effect of local surgery on overall survival (OS)
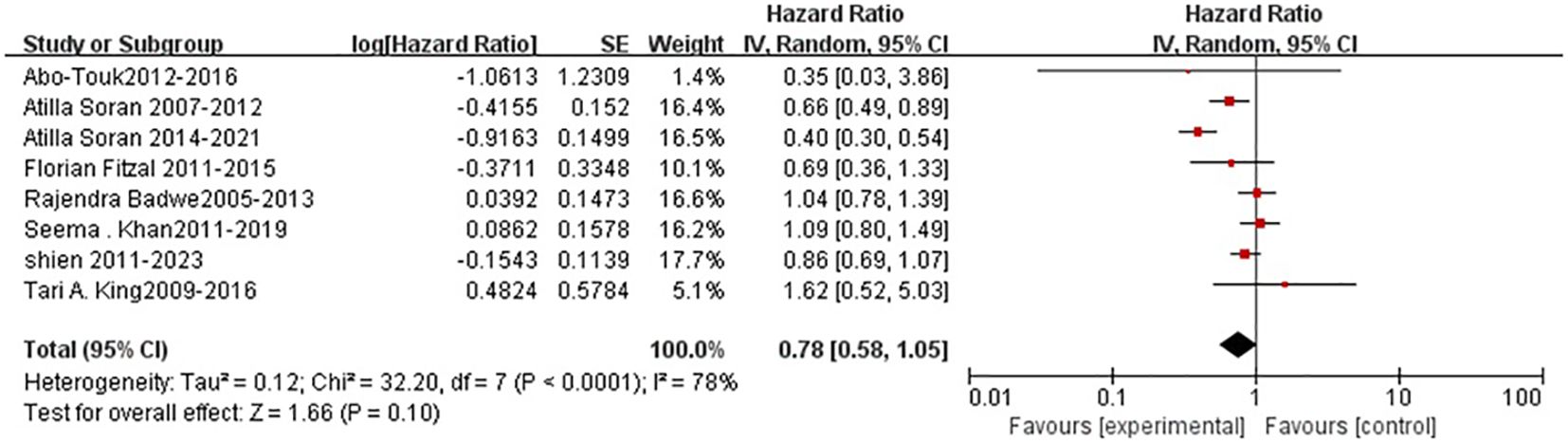
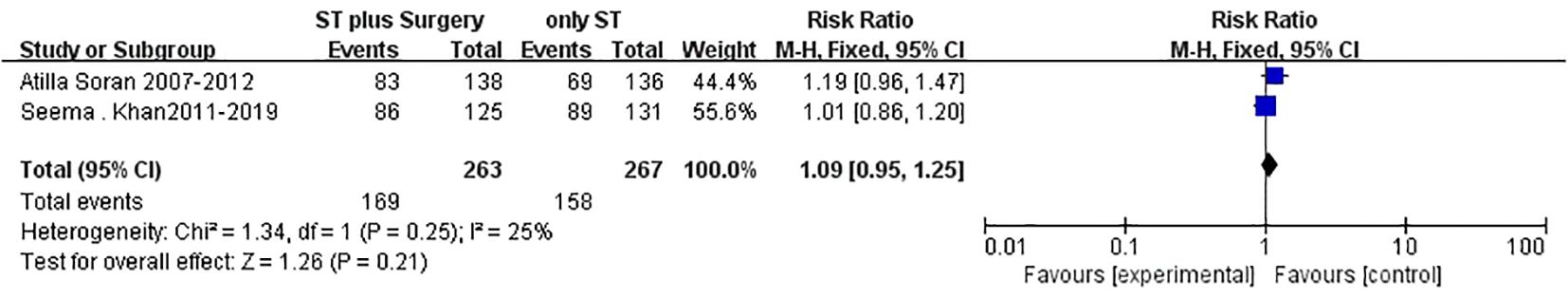
After a median follow-up time of 40 months, patients in the surgery group had a insignificantly statistically (P=0.10) higher overall survival (OS) rate than those in the non-surgery group (HR=0.75; 95%CI, 0.58-1.05) (Figure 2), although there was statistically significant heterogeneity (P<0.0001, I2=78%). Besides, no benefit of 2-year OS (relative risk [RR] = 1.01; 95 % CI 0.82–1.23, P = 0.95; Figure 3), or 3-year OS (RR = 1.09; 95 % CI 0.95–1.25, P = 0.21; Figure 4) were found for patients in the surgery group.
Effect of local surgery on local progression-free survival and distant progression-free survival
Totally, 3 trials reported HR data on LPFS after primary tumor resection. Patients in the surgery group had significantly (P=0.04) improved LPFS than those in the no-surgery group (HR=0.36, 95%CI,0.14-0.95, Figure 5), although there was statistically significant heterogeneity among the trials (P =0.002, I2=85%, Figure 5). Moreover, for distant progression-free survival (DPFS), only 2 trials reported the relevant HR data, and the pooled HR of 0.95 (95%CI,0.41-2.22) showed that patients in the surgery group had similar DPFS to those in the non-surgery group (P=0.91, Figure 6).
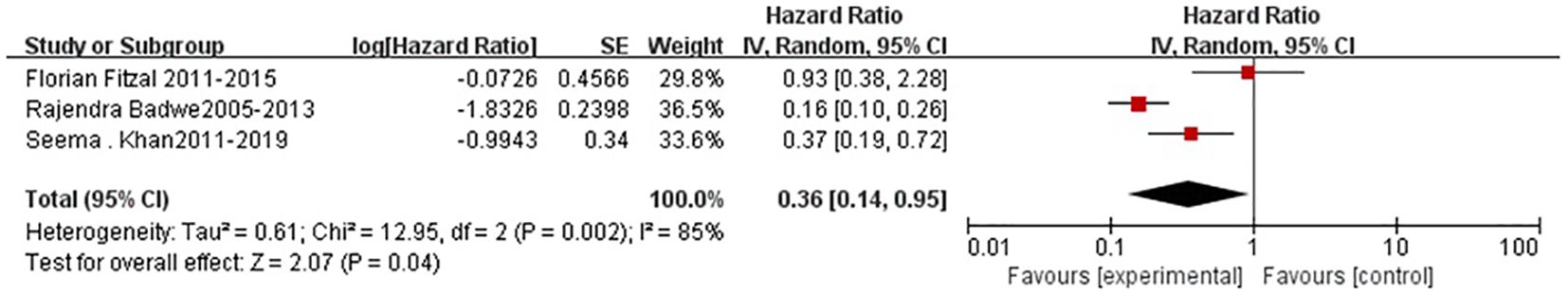
Figure 5. Results of the meta-analysis of local progression-free survival among patients with de novo stage IV breast cancer.
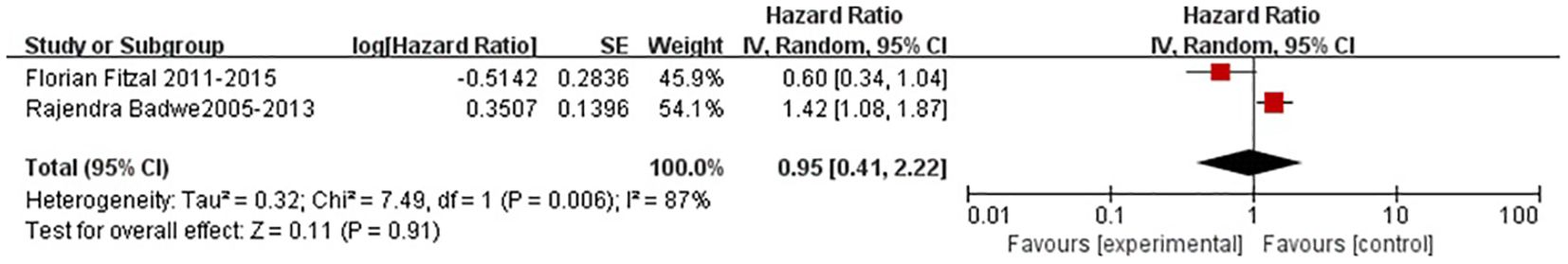
Figure 6. Meta-analysis of distant progression-free survival among patients with de novo stage IV breast cancer.
Effect of local surgery on subgroup analysis
Subgroup analyses were performed according to molecular subtyps and site of metastasis. A total of 6 trials reported the HR data on overall survival (OS) by molecular subtypes. The pooled HR of 0.71 (95%CI,0.55-0.93, Figure 7) indicated that the primary tumor resection could significantly statistically improve the overall survival for candidates with ER/PR positive diseases (P=0.01, Figure 7)., although statistically significant heterogeneity existed among the trials (P=0.04, I2=58%, Figure 7). However, for triple-negative or HER2-positive diseases, no OS benefit were found after the adminstration of locoregional surgery in primary tumors (Figure 7).
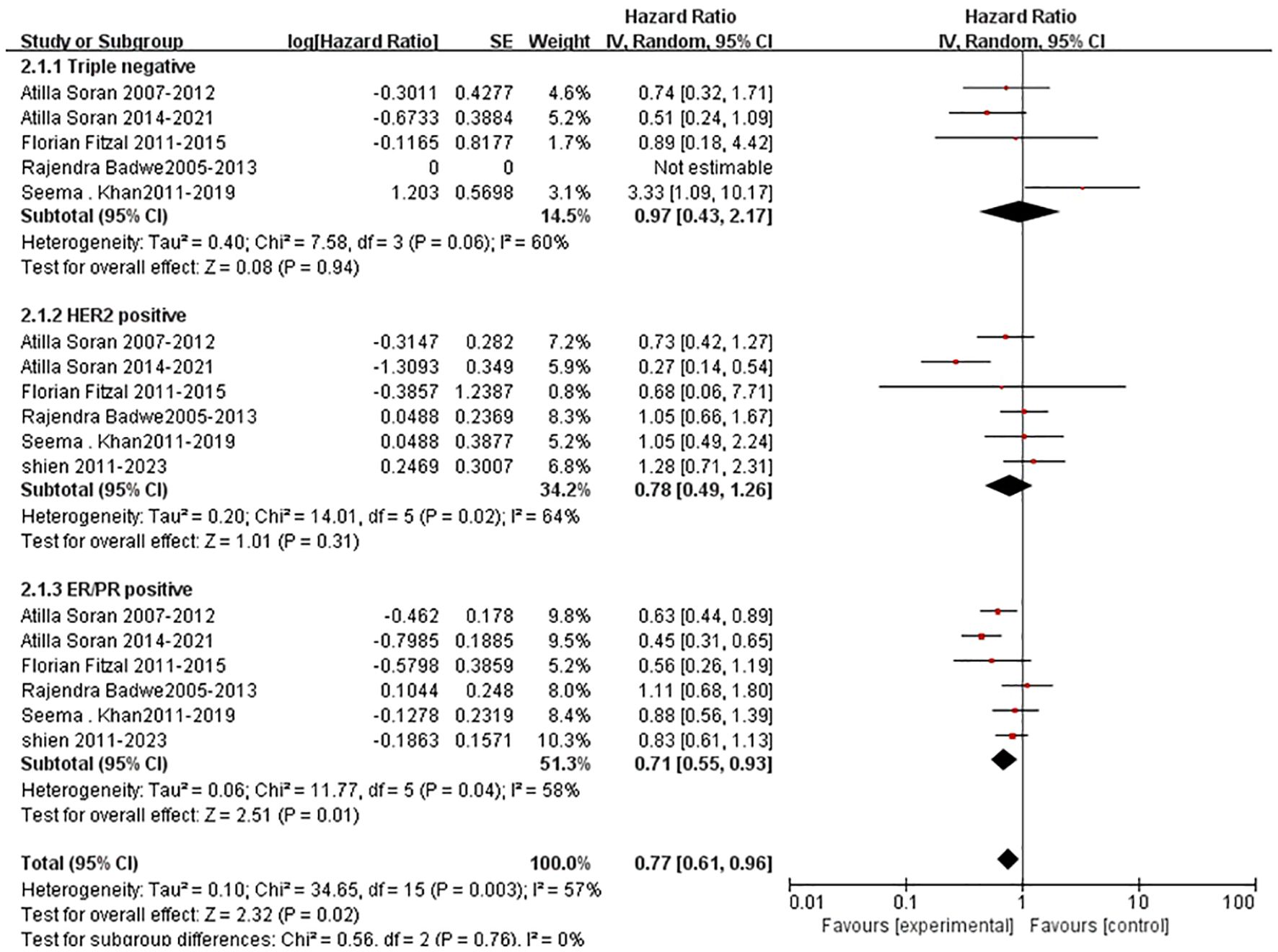
Figure 7. Results of subgroup analysis of overall survival by molecular subtype for surgical versus nonsurgical comparison.
Six trials reported the survival data for patients with bone metastases only, and three trials reported the survival data for patients with both bone and visceral metastases. For women with bone-only metastases as well as those with both bone and visceral metastases, patients in the surgery group had statistically insignificantly improved overall survival than those in the no-surgery group (bone-only metastases: HR=0.70, 95%CI,0.47-1.04; Bone and visceral metastasis: HR=0.93, 95%CI,0.76-1.15, Figure 8), although there was statistically significant heterogeneity between trials (Figure 8).
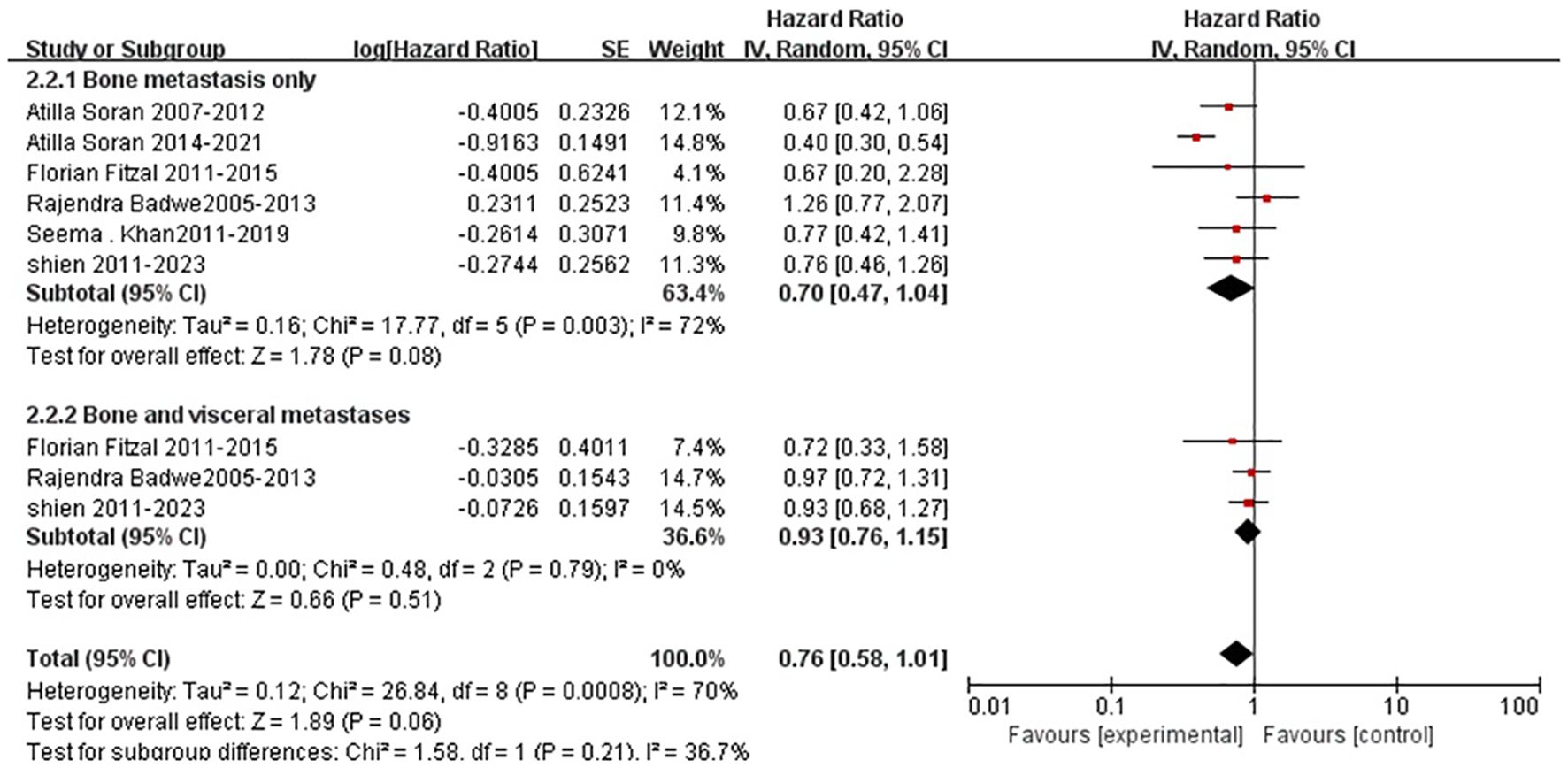
Figure 8. Results of subgroup analysis comparing overall survival of metastatic sites with surgery and without surgery.
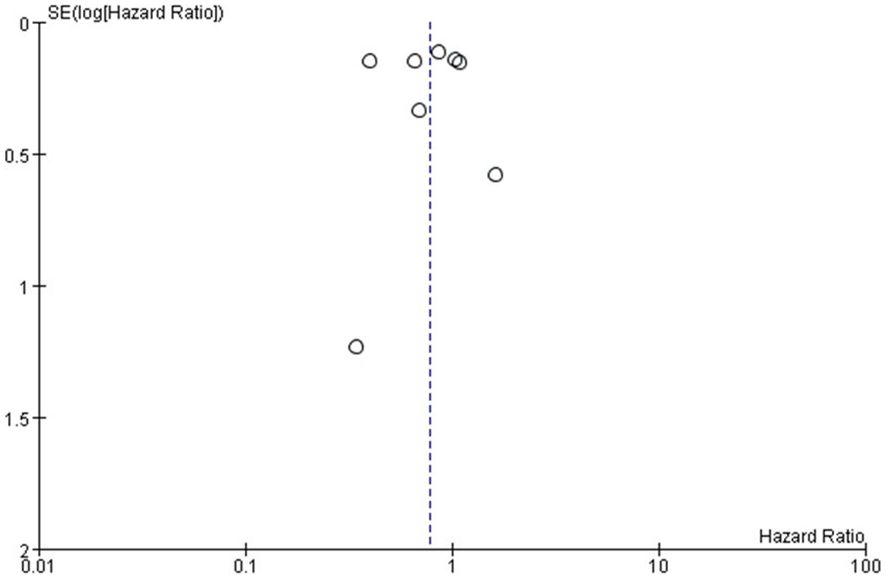
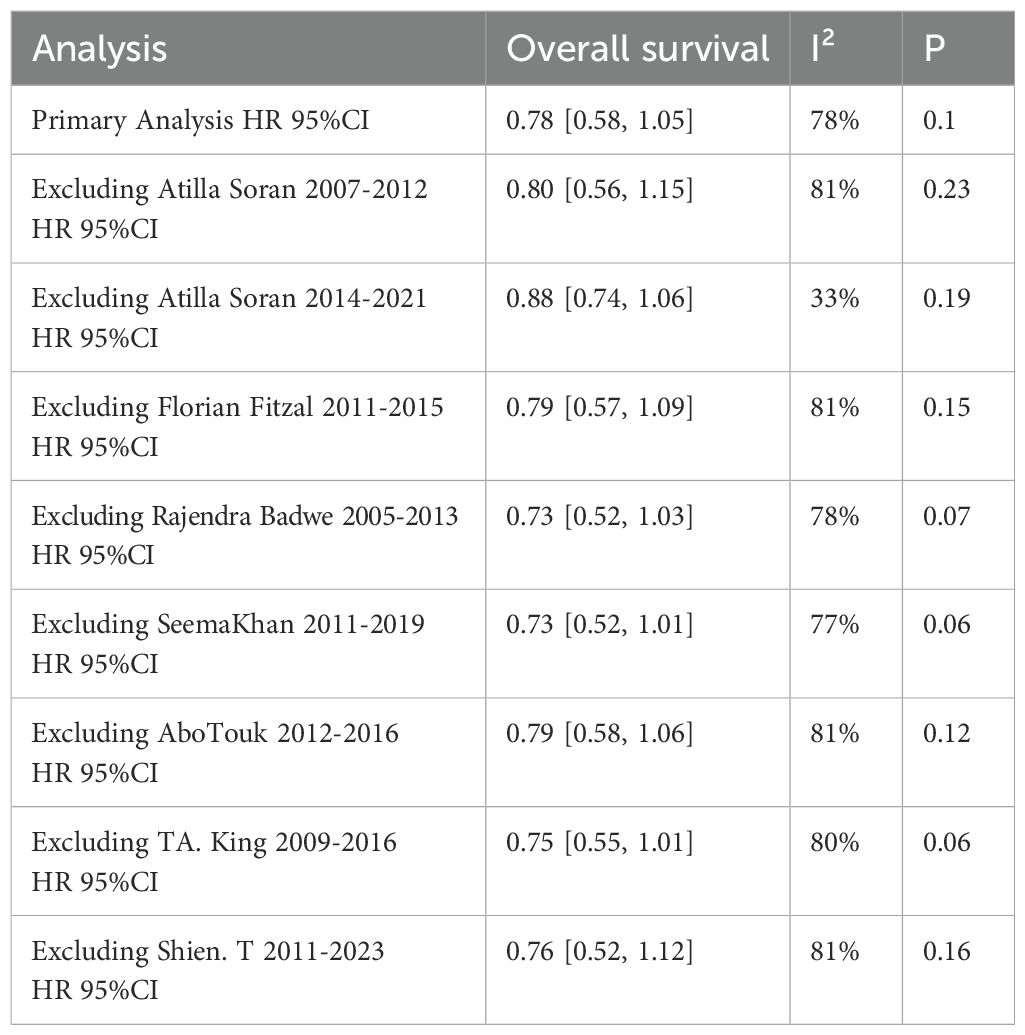
Bias analysis and sensitivity analysis
For all the eight studies included in the meta-analysis, the Cochrane Risk of Bias tool was used to assess the risk of bias (Figure 9). The funnel plot performed to assess the publication bias, as shown in Figure 10, indicated no publication bias being found in the included studies. The sensitivity analysis was conducted by deleting each study one by one and re-conducting the meta-analysis, as shown in Table 2. and The results of all the sensitivity analyses were consistent with the original analysis.
Discussion
Through analyzing the eight prospective studies (5 RCTs and 3 prospective studies) including more than 2000 patients, we found that the administration of locoregional surgery in primary tumors helped improving the local progression-free survival, other than the overall survival or distant progression-free survival in patients with de novo stage IV breast cancer. More interesting, based on the subgroup analyses on tumor subtype and metastatic site, the benefit of locoregional surgery in OS were found for patients with ER/ PR-positive diseases, bone-only metastasis. To our knowledge, this was the largest prospective study-based research to assess the impact of locoregional surgery in primary tumors on longterm OS.
It had been debatable whether or not the use of locoregional surgery in primary tumors, including breast-conserving surgery or mastectomy, axillary lymph dissection, or sentinel lymph node biopsy with or without radiotherapy, could help improve OS for patients with de novo stage IV breast cancer (28). Consequently, the indications of locoregional surgery in primary tumors were always considered as the followings: (1) symptomatic primary site (with the aim to control local symptoms); (2) progression of the primary tumor after controlled distant disease is controlled; (3) no evidence of disease except in the primary tumor (7, 8). In the current study, nearly half of the population included had underwent locoregional surgery in primary tumors. The result demonstrated indirectly the anxiety regarding the choice of therapeutic schedule in clinical work.
Survival of cancer patients, especially progression-free survival, distant progression-free survival, overall survival, important reliable, objective and easily accessible indicators, had been widely used in the evaluation and analysis of long-term prognosis of breast cancer patients. In our study, based on analysis of a large cohort of 2029 patients from 8 studies, the efficacy of locoregional surgery in primary tumors in prolonging the local progression-free survival was established, suggesting that locoregional surgery in primary tumors should not be omitting indiscriminately in patients with de novo stage IV breast cancer
As expectedly, in the current study, we found that locoregional surgery in primary tumors was associated with prolonging overall survival (OS) for patients with ER/PR positive breast cancer. The result was partly consistent to MF 07-01 trial, which concluded that after locoregional surgery and long-term follow-up, patients with de novo stage IV breast cancer had impvoed OS. The underlying reasons might be the low incidence of triple-negative and high incidence of ER/PR positive and isolated bone metastases rather than visceral metastases disease. However, due to no information on the association between surgical margin and outcomes, the choice of detailed surgical approaches for patients with de novo stage IV breast cancer remained ambiguous and vague. Some researchers found that total mastectomy and partial mastectomy with a definite negative margin were similar in the OS rate (28, 29). A meta- analysis (30) of 216 066 patients with de novo stage IV breast cancer also showed that both partial mastectomy and total mastectomy with negative margins can be used as local management options for patients with de novo stage IV breast cancer. Therefore, both breast- conserving surgery with negative margin and total mastectomy could be used as an alternative surgical procedure for patients with de novo stage IV breast cancer.
Moreover, this meta-analysis had certain limitations. First, there were differences in the experimental protocols of the included studies, such as the timing of surgery and different surgical methods, which could influence the overall survival of patients. Second, there was significant heterogeneity among the participants in the trials, and the different characteristics of the patients might affect the overall survival. Third, some trials did not show the complete outcome data or subgroup analyses, and some trials were showed in abstract form.
Conclusion
Our study demonstrated that locoregional surgery in primary tumors was associated with improved OS for participants with ER/PR positive de novo stage IV breast cancer, and locoregional surgery in primary tumors could be worthy of clinical recommendation for patients with ER/PR positive de novo stage IV breast cancer. And, more prospective and randomized controlled trials of higher quality are needed to provide more convincing results.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
YS: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Methodology, Supervision. HM: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing, Funding acquisition, Software, Project administration. YL: Formal analysis, Resources, Writing – original draft, Writing – review & editing. CZ: Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing, Conceptualization, Project administration.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The work was supported by Clinical Research Fund of Wu Jiaping Medical Foundation (Grant No: 320.6750.2022-19-76) and Beijing Kechuang Medical Development Foundation(Grant No: KC2021-JF-0167-18).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. (2020) 70:7–30. doi: 10.3322/caac.21590
2. Boman C, Edman Kessler L, Bergh J, Matikas A, Foukakis T. Women with short survival after diagnosis of metastatic breast cancer: a population-based registry study. Breast Cancer Res Treat. (2022) 194(1):49–56. doi: 10.1007/s10549-022-06591-7
3. Gnerlich J, Jeffe DB, Deshpande AD, Beers C, Zander C, Margenthaler JA. Surgical removal of the primary tumor increases overall survival in patients with metastatic breast cancer: analysis of the 1988-2003 SEER data. Ann Surg Oncol. (2007) 14(8):2187–94. doi: 10.1245/s10434-007-9438-0
4. Daily K, Douglas E, Romitti PA, Thomas A. Epidemiology of de novo metastatic breast cancer. Clin Breast Cancer. (2021) 21(4):302–8. doi: 10.1016/j.clbc.2021.01.017
5. Lee JS, Toktas O, Soran A. Role of locoregional treatment in de novo stage IV breast cancer. Clin Med Insights Oncol. (2020) 14:1179554920942440. doi: 10.1177/1179554920942440
6. Merloni F, Palleschi M, Gianni C, Casadei C, Curcio A, Romeo A, et al. Locoregional treatment of de novo stage IV breast cancer in the era of modern oncology. Front Oncol. (2023) 13:1083297. doi: 10.3389/fonc.2023.1083297
7. Cardoso F, Paluch-Shimon S, Schumacher-Wulf E, Matos L, Gelmon K, Aapro MS, et al. 6th and 7th International consensus guidelines for the management of advanced breast cancer (ABC guidelines 6 and 7). Breast. (2024) 76:103756. doi: 10.1016/j.breast.2024.103756
8. Gradishar WJ, Moran MS, Abraham J, Abramson V, Aft R, Agnese D, et al. Breast cancer, version 3.2024, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. (2024) 22(5):331–57. doi: 10.6004/jnccn.2024.0035
9. Yoshimura M. Radiation therapy for primary tumor of de novo stage IV breast cancer. Transl Cancer Res. (2020) 9(8):5108–16. doi: 10.21037/tcr.2020.02.54
10. Falkson G, Holcroft C, Gelman RS, Tormey DC, Wolter JM, Cummings FJ. Ten-year follow-up study of premenopausal women with metastatic breast cancer: an Eastern Cooperative Oncology Group study. J Clin Oncol. (1995) 13(6):1453–8. doi: 10.1200/JCO.1995.13.6.1453
11. Bernard-Marty C, Cardoso F, Piccart MJ. Facts and controversies in systemic treatment of metastatic breast cancer. Oncologist. (2004) 9(6):617–32. doi: 10.1634/theoncologist.9-6-617
12. Harris E, Barry M, Kell MR. Meta-analysis to determine if surgical resection of the primary tumour in the setting of stage IV breast cancer impacts on survival. Ann Surg Oncol. (2013) 20:2828–34. doi: 10.1245/s10434-013-2998-2
13. Warschkow R, Güller U, Tarantino I, Cerny T, Schmied BM, Thuerlimann B, et al. Improved survival after primary tumor surgery in metastatic breast cancer: A propensity-adjusted, population-based SEER trend analysis. Ann Surg. (2016) 263(6):1188–98. doi: 10.1097/SLA.0000000000001302
14. Danna EA, Sinha P, Gilbert M, Clements VK, Pulaski BA, Ostrand-Rosenberg S. Surgical removal of primary tumor reverses tumor-induced immunosuppression despite the presence of metastatic disease. Cancer Res. (2004) 64(6):2205–11. doi: 10.1158/0008-5472.CAN-03-2646
15. Norton L, Massagué J. Is cancer a disease of self-seeding? Nat Med. (2006) 12(8):875–8. doi: 10.1038/nm0806-875
16. Petrelli F, Barni S. Surgery of primary tumors in stage IV breast cancer: an updated meta-analysis of published studies with meta-regression. Med Oncol. (2012) 29:3282–90. doi: 10.1007/s12032-012-0310-0
17. Soran A, Dogan L, Isik A, Ozbas S, Trabulus DC, Demirci U, et al. The effect of primary surgery in patients with de novo stage IV breast cancer with bone metastasis only (Protocol BOMET MF 14-01): A multi-center, prospective registry study. Ann Surg Oncol. (2021) 28(9):5048–57. doi: 10.1245/s10434-021-09621-8
18. Soran A, Ozmen V, Ozbas S, Karanlik H, Muslumanoglu M, Igci A, et al. Randomized trial comparing resection of primary tumor with no surgery in stage IV breast cancer at presentation: protocol MF07-01. Ann Surg Oncol. (2018) 25(11):3141–9. doi: 10.1245/s10434-018-6494-6
19. Khan SA. Primary tumor resection in stage IV breast cancer: consistent benefit, or consistent bias? Ann Surg Oncol. (2007) 14(12):3285–7. doi: 10.1245/s10434-007-9547-9
20. Fitzal F, Bjelic-Radisic V, Knauer M, Steger G, Hubalek M, Balic M, et al. Impact of breast surgery in primary metastasized breast cancer: outcomes of the prospective randomized phase III ABCSG-28 POSYTIVE trial. Ann Surg. (2019) 269(6):1163–9. doi: 10.1097/SLA.0000000000002771
21. Badwe R, Hawaldar R, Nair N, Kaushik R, Parmar V, Siddique S, et al. Locoregional treatment versus no treatment of the primary tumour in metastatic breast cancer: an open-label randomised controlled trial. Lancet Oncol. (2015) 16(13):1380–8. doi: 10.1016/S1470-2045(15)00135-7
22. Shien T, Nakamura K, Shibata T, Kinoshita T, Aogi K, Fujisawa T, et al. A randomized controlled trial comparing primary tumour resection plus systemic therapy with systemic therapy alone in metastatic breast cancer (PRIM-BC): Japan Clinical Oncology Group Study JCOG1017. Jpn J Clin Oncol. (2012) 42(10):970–3. doi: 10.1093/jjco/hys120
23. Abo-Touk NA, Fikry AA, Fouda EY. The benefit of locoregional surgical intervention in metastatic breast cancer at initial presentation. Cancer Res J. (2016) 4:32–2. doi: 10.11648/j.crj.20160402.12
24. Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. (2021) 372:n71.
25. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50(4):1088–101. doi: 10.2307/2533446
26. Khan SA, Zhao F, Goldstein LJ, Cella D, Basik M, Golshan M, et al. Early local therapy for the primary site in de novo stage IV breast cancer: results of a randomized clinical trial (EA2108). J Clin Oncol. (2022) 40(9):978–87. doi: 10.1200/JCO.21.02006
27. King TA, Lyman JP, Gonen M, Voci A, De Brot M, Boafo C, et al. Prognostic impact of 21-gene recurrence score in patients with stage IV breast cancer: TBCRC 013. J Clin Oncol. (2016) 34(20):2359–65. doi: 10.1200/JCO.2015.63.1960
28. Khan SA, Stewart AK, Morrow M. Does aggressive local therapy improve survival in metastatic breast cancer? Surgery. (2002) 132(4):620–6;discussion 626-7.
29. Pockaj BA, Wasif N, Dueck AC, Wigle DA, Boughey JC, Degnim AC, et al. Metastasectomy and surgical resection of the primary tumor in patients with stage IV breast cancer: time for a second look? Ann Surg Oncol. (2010) 17(9):2419–26. doi: 10.1245/s10434-010-1016-1
Keywords: locoregional surgery, overall survival, meta-analysis, de novo stage IV breast cancer, ER/PR-positive
Citation: Sun Y, Ma H, Li Y and Zhou C (2025) Effect of locoregional surgery in primary tumors on overall survival in patients with de novo stage IV breast cancer: a systematic review and meta-analysis. Front. Oncol. 15:1590246. doi: 10.3389/fonc.2025.1590246
Received: 09 March 2025; Accepted: 14 April 2025;
Published: 13 May 2025.
Edited by:
Matteo Ghilli, Pisana University Hospital, ItalyReviewed by:
Lorenzo Scardina, Agostino Gemelli University Polyclinic (IRCCS), ItalyMarina Bortul, University of Trieste, Italy
Copyright © 2025 Sun, Ma, Li and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Can Zhou, emhvdWNhbnoyMDA1QDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
 Yanbo Sun
Yanbo Sun Hao Ma
Hao Ma Yingjie Li
Yingjie Li Can Zhou
Can Zhou