- 1Interventional and Geriatric Department, The Affiliated Suqian Hospital of Xuzhou Medical University, Suqian, Jiangsu, China
- 2Endoscopy Center, Jiangsu Province (Suqian) Hospital, Suqian, Jiangsu, China
- 3School of Medicine, Jiangsu University, Zhenjiang, Jiangsu, China
- 4Oncology Department, The Affiliated Suqian Hospital of Xuzhou Medical University, Suqian, Jiangsu, China
Objective: To explore the effectiveness of prehabilitation program on elderly patients undergoing esophageal cancer surgery.
Methods: A total of 96 elderly esophageal cancer surgery patients from a tertiary hospital were selected. The control group included 48 patients treated from August to November 2023, and the prehabilitation group consisted of 48 patients treated from December 2023 to March 2024. The control group received routine care from the time of diagnosis until surgery, while the prehabilitation group received the prehabilitation program in addition to routine care. The nutritional status, hospital anxiety and depression scale (HADS), six-minute walking distance (6MWD), and quality of life (SF-36) were compared between the two groups at different time points before and after the intervention. Additionally, postoperative hospital stay, time to chest drain removal, time to first ambulation, and complications were evaluated.
Results: During the research process, in the control group, one case fell out, while two cases fell out in the prehabilitation group. The t-test and Mann Whitney U test showed that at different time points after the intervention, the indicators in the prehabilitation group were significantly better than those in the control group (P<0.05), although there was no significant difference in complications (P>0.05). Repeated measures ANOVA indicated that there were interaction effects, intervention effects, and time effects on HADS, 6MWD, and SF-36 scores at each time point in both groups (P<0.05).
Conclusion: Prehabilitation has a positive effect on improving the functional reserve, nutritional status, and psychological well-being of elderly patients undergoing esophageal cancer surgery, thus promoting postoperative recovery.
1 Introduction
Esophageal cancer is one of the common malignant tumors. The incidence and mortality of esophageal cancer in my country are much higher than those in other countries (1), and elderly patients account for more than 70% (2), putting greater pressure on society and families. Surgery is the main treatment modality, but there is a “window period” between tumor diagnosis and surgery. During this time, elderly patients face a high risk of malnutrition (3), and are prone to experiencing severe anxiety and depression, with some even developing suicidal tendencies (4). Additionally, their physical endurance declines, leading to reduced surgical tolerance and an increased risk of perioperative mortality (5). Therefore, effectively enhancing the preoperative functional status of elderly patients with esophageal cancer improves their prognosis and quality of life, which requires urgent attention.
In recent years, prehabilitation has provided a new idea to improve the perioperative condition of patients. It is a rehabilitation intervention based on accelerated rehabilitation surgery, which includes a comprehensive program of exercise, nutritional supplementation and anxiety management (6). The implementation of prehabilitation has significantly improved the nutritional and functional status, as well as the prognosis, of surgical patients. However, both domestic and international prehabilitation management lacks standardization, with low implementation rates, and it is often initiated only after hospitalization. There is also a lack of studies exploring prehabilitation practices from the time of diagnosis to the preoperative period, particularly for elderly esophageal cancer patients (7). Therefore, this study preliminarily applied a prehabilitation program, constructed based on a review of the literature and expert consultation, to elderly esophageal cancer patients immediately after diagnosis.
2 Materials and methods
2.1 Study subjects
The study included 96 elderly patients who underwent esophageal cancer surgery at a tertiary hospital. Using the first day of outpatient pathological diagnosis as the baseline, the patients were divided into two groups: 48 patients admitted between August 2023 and November 2023 were assigned to the control group, while 48 patients admitted between December 2023 and March 2024 were assigned to the prehabilitation group. All participants voluntarily took part in the study and signed the “Informed Consent Form”. The study was approved by the Ethics Committee of the Medical School of Jiangsu University (NO.20221019-5).
2.2 Inclusion, exclusion, and withdrawal criteria
2.2.1 Inclusion criteria
① Patients aged ≥60 years with mobility; ② Preoperatively diagnosed with esophageal cancer and eligible for surgery; ③ No preoperative special biological therapy; ④ Classified as American Society of Anesthesiologists (ASA) grade 1-2.
2.2.2 Exclusion criteria
① Patients with comorbid conditions such as psychiatric disorders, other malignancies, consciousness disorders, severe bronchial asthma or emphysema, severe heart failure, etc.; ② Participation in other clinical intervention studies.
2.2.3 Withdrawal criteria
① Voluntary withdrawal during the treatment period; ② Discontinuation of treatment or death.
2.3 Intervention methods
2.3.1 Intervention methods for the control group
After diagnosis, routine preoperative care is provided as follows (1): Preoperative guidance: ① Distribute health guidance manuals to familiarize patients with the basic medical process, educate them on disease-related knowledge, and encourage smoking and alcohol cessation; ② Advise patients with abnormal blood glucose or blood pressure to take their medications on time; ③ Explain the anesthesia method and fasting (food and drink) times to the patient; ④ Instruct patients on ankle pump exercises and effective coughing techniques (2). Nutritional care: Provide individualized nutritional care based on the patient’s condition and tolerance, and supplement nutritional formulations as prescribed (3). Psychological care: actively communicate with patients to alleviate concerns about the surgery (4). Pain management: Assess the patient’s pain in a timely manner and administer analgesics as needed under medical guidance.
2.3.2 Intervention methods for the prehabilitation group
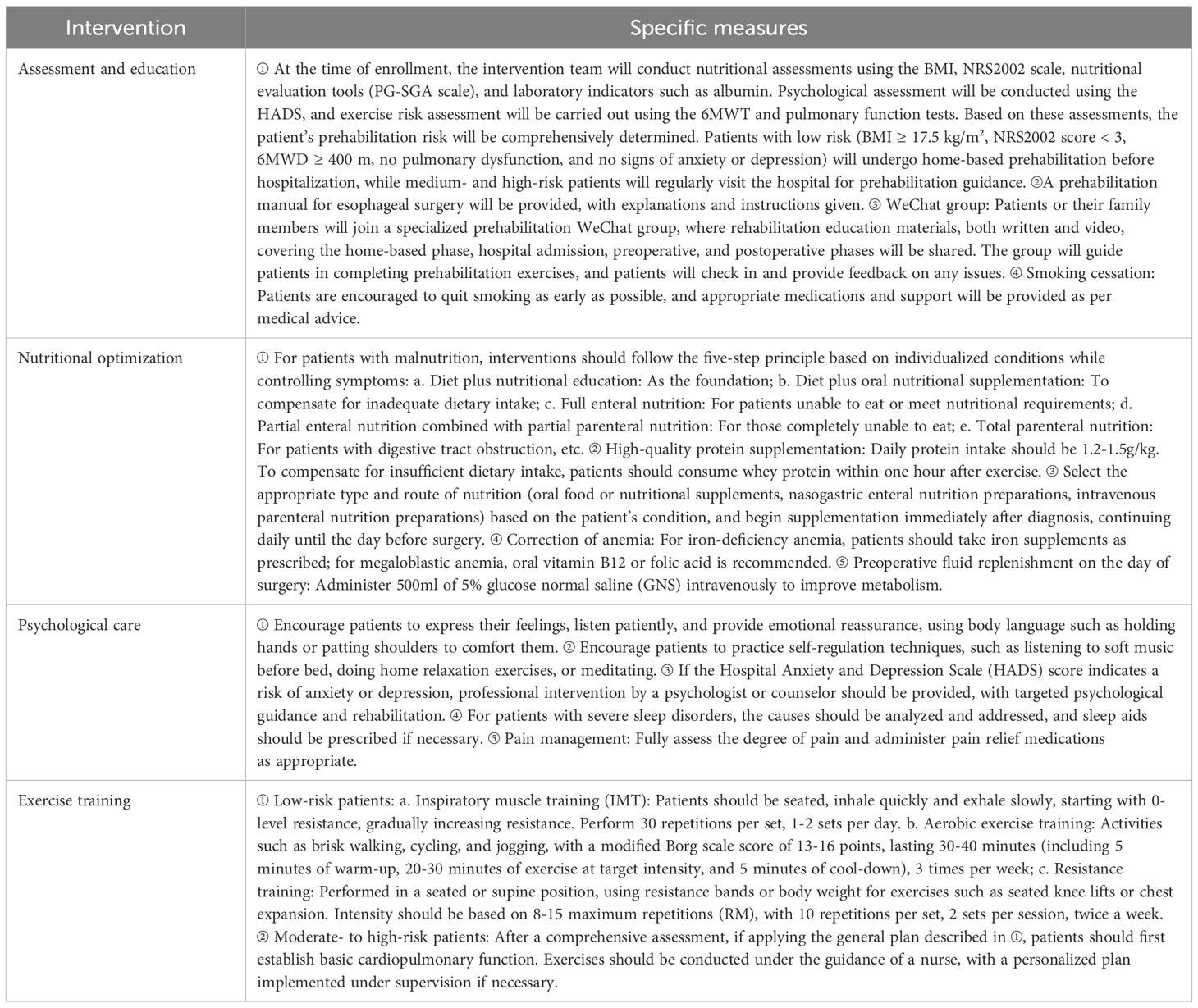
In addition to routine care, a prehabilitation protocol is implemented from the first day of diagnosis until the day before surgery, as follows:
2.3.2.1 Formation of the prehabilitation intervention team
A multidisciplinary prehabilitation team is formed, consisting of the head nurse from thoracic surgery, doctors, nurses, anesthetists, nutritionists, rehabilitation therapists, psychologists, counselors, and master’s students. The qualifications, roles, and responsibilities of the prehabilitation team members are clearly defined:① The chief nurse is responsible for developing the project plan, team training, and quality control; ② The thoracic surgeon is in charge of diagnosing and treating the disease; ③ The rehabilitation therapist and anesthetist formulate personalized exercise rehabilitation plans; ④ The nutritionist assesses the patient’s nutritional status, determines their nutritional and energy requirements, and develops a corresponding nutritional prescription; ⑤ The psychologist and counselor are responsible for psychological counseling and support; ⑥ Nurses provide guidance on diet, exercise, and psychological health, implement the plan, and assess the patient’s adherence and the effectiveness of the intervention; ⑦ The Master of nursing is responsible for collecting, organizing, and analyzing the data.
2.3.2.2 Development and implementation of the prehabilitation program
After conducting a comprehensive literature search and screening, a total of 14 studies were included, consisting of 3 guidelines (8–10), 1 expert consensus (11), 1 systematic review (12), 5 randomized controlled trials (RCTs) (13–17), and 4 quasi-experimental studies (18–21). Evidence was extracted, and based on the physiological and psychological frailties of elderly patients with esophageal cancer, an initial draft of the program was developed. Sixteen experts were invited to participate in two rounds of consultation. All experts met the following criteria: ① they were from tertiary general hospitals; ② they had been working in relevant fields for over 10 years; ③ they held senior or higher professional titles. The expert authority coefficient was 0.897, with a positive coefficient of 100%. The variation coefficient for each item was ≤0.19, and Kendall’s coefficient ranged from 0.213 to 0.384, indicating a high level of agreement and coordination among the experts, ensuring the reliability of the prehabilitation program. The specific program is detailed in Table 1.
2.4 Outcome measures evaluation
2.4.1 General patient data survey
This includes age, gender, educational level, BMI, surgical approach, time from diagnosis to surgery.
2.4.2 Serum albumin and serum prealbumin indicators
The normal ranges for serum albumin and serum prealbumin are 35–55 g/L and 18–39 g/L, respectively.
2.4.3 Hospital anxiety and depression scale score
The HADS is widely used to assess patients’ anxiety and depression levels. It consists of two subscales: the Anxiety Subscale (HADS-A) and the Depression Subscale (HADS-D), each containing 7 items. The total score for each subscale ranges from 0 to 21. A score of ≥8 indicates the presence of anxiety or depression, with higher scores reflecting greater severity.
2.4.4 Six-minute walk distance
The Six-Minute Walk Test (6MWT) measures the distance a patient can walk briskly within six minutes (22). It is a standardized method that can quickly and effectively assess cardiopulmonary function, with the result, 6MWD, serving as a good indicator of the patient’s physical functional capacity.
2.4.5 The MOS 36-item short-form health survey score
The SF-36 scale is a health survey questionnaire developed by the Health Institute in Boston, USA, based on the Medical Outcomes Study (MOS SF) created by Stewartse (23). The Chinese version of the SF-36 has been shown to have reliable validity and reliability in thoracic surgery (24).
2.4.6 The postoperative hospital stay, the time to chest tube removal, the time to first ambulation, and the complications graded according to the Clavien-Dindo classification were collected for both groups of patients
Researchers usually reflect the postoperative recovery and prognosis of patients undergoing oesophageal surgery by the postoperative hospital stay, the time to chest tube removal, the time to first ambulation, and the complications graded according to the Clavien-Dindo classification, so we also selected the above indicators as outcome measures.
2.5 Data collection method
Two nursing postgraduates (uniformly trained and not involved in the intervention implementation) were responsible for distributing questionnaires and collecting data. Data on the HADS scores, albumin and prealbumin levels, and SF-36 scores were collected for both groups at four time points: before the intervention, one day before surgery, one week after surgery, and four weeks after surgery. Additionally, the 6MWD was measured before the intervention, one day before surgery, and four weeks after surgery. Postoperative hospital stay, chest drain removal timing, first ambulation timing, and complications were also recorded.
2.6 Statistical methods
Data were organized and analyzed using Excel and SPSS 26.0. Continuous variables were described using the median, standard deviation, mean, and the first and third quartiles, while categorical variables were presented as frequencies. The Mann-Whitney U test or independent sample t-test was employed to analyze continuous variables between the two groups. The chi-square test or Fisher’s exact test was used for categorical data analysis. For comparing normally distributed data across time points within a group, repeated measures analysis of variance (ANOVA) was performed. If Mauchly’s test of sphericity was met, the test results for within-subject effects were used; if not, the Greenhouse-Geisser correction was applied. Non-normally distributed data were analyzed using the generalized estimating equation (GEE).
3 Results
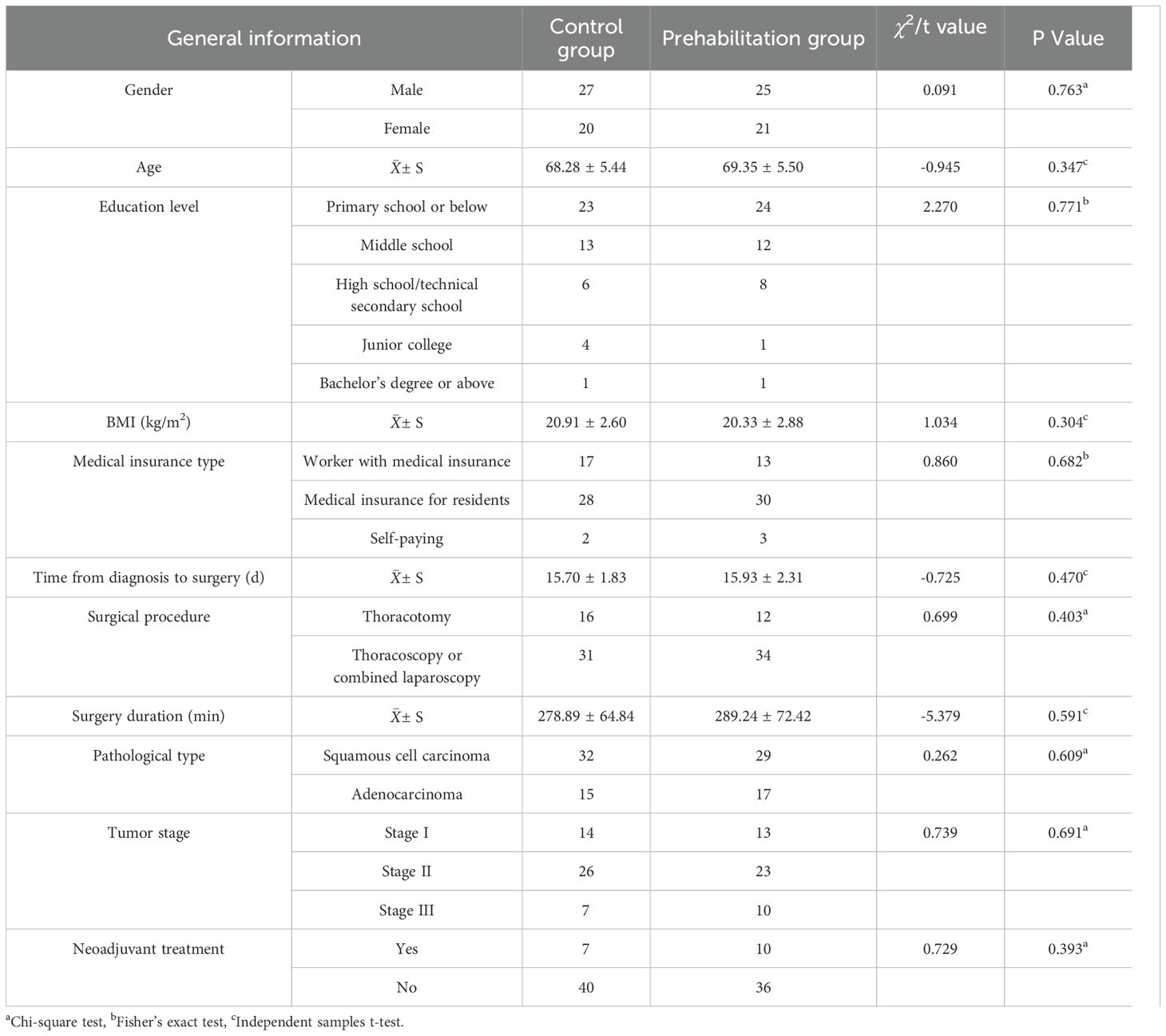
3.1 Comparison of general data between the two groups
A total of 96 patients participated in the study, with 2 patients lost to follow-up in the prehabilitation group (1 patient withdrew due to loss of contact, and 1 patient withdrew after doubting the intervention’s efficacy, assuming it would inevitably be effective). In the control group, 1 patient was lost to follow-up due to a change in contact information. Ultimately, 47 patients were included in the control group and 46 in the prehabilitation group, making a total of 93 cases.
The comparison of general data is shown in Table 2, and the baseline characteristics of the two groups are comparable.
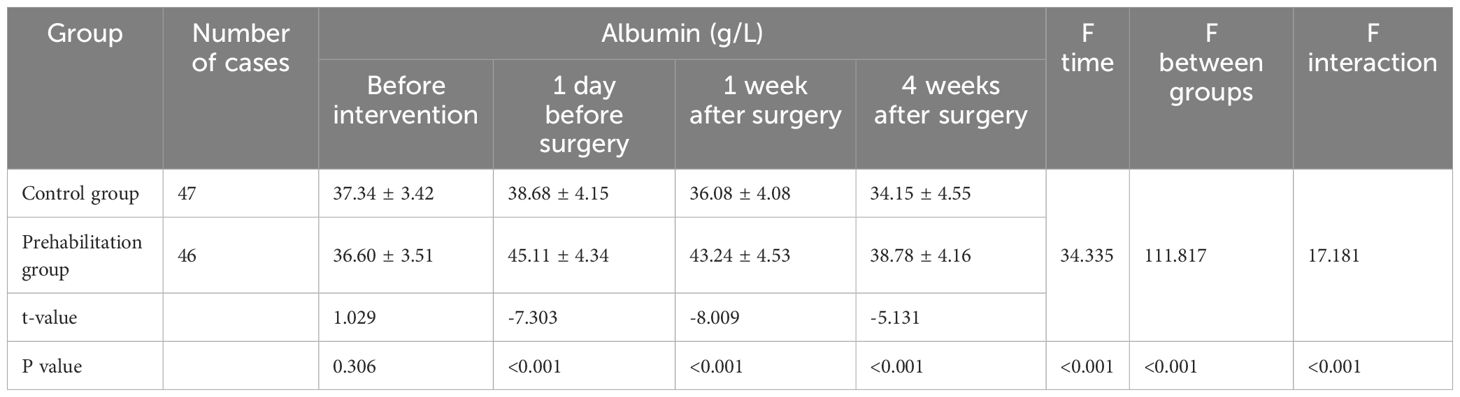
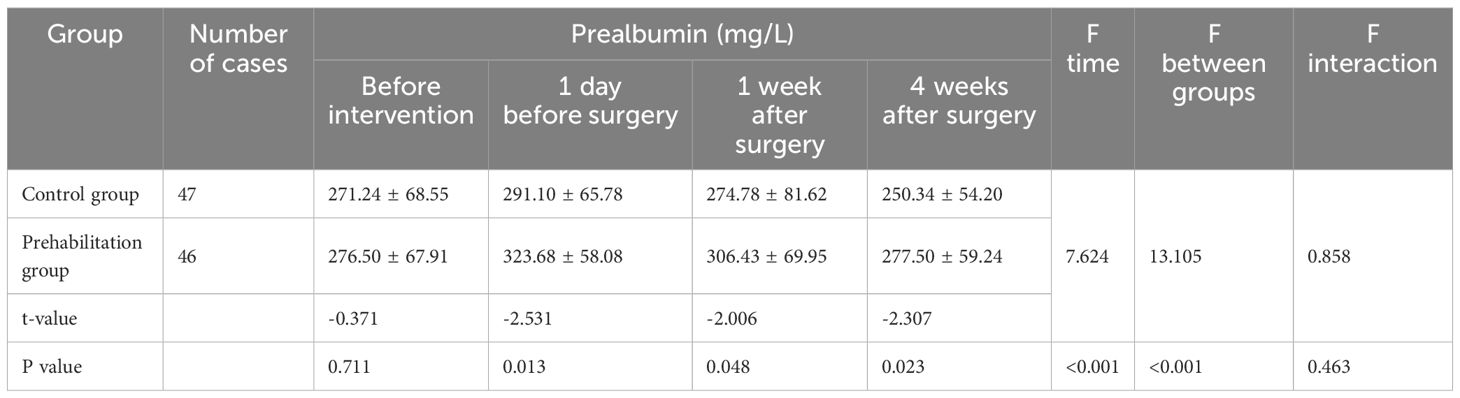
3.2 Comparison of serum albumin and prealbumin between the two groups
The two groups were comparable before the intervention. At each time point after the intervention, the prehabilitation group had higher levels than the control group (P < 0.05). The albumin results showed a time effect, intervention effect, and interaction effect (P < 0.05). For prealbumin, there were time and intervention effects (P < 0.05), but no interaction effect (P > 0.05). This indicates a significant difference in albumin and prealbumin levels between the two groups due to differences in the rehabilitation care plans. Additionally, the nutritional indicators of the prehabilitation group remained more stable postoperatively. See Tables 3 and 4 for details.
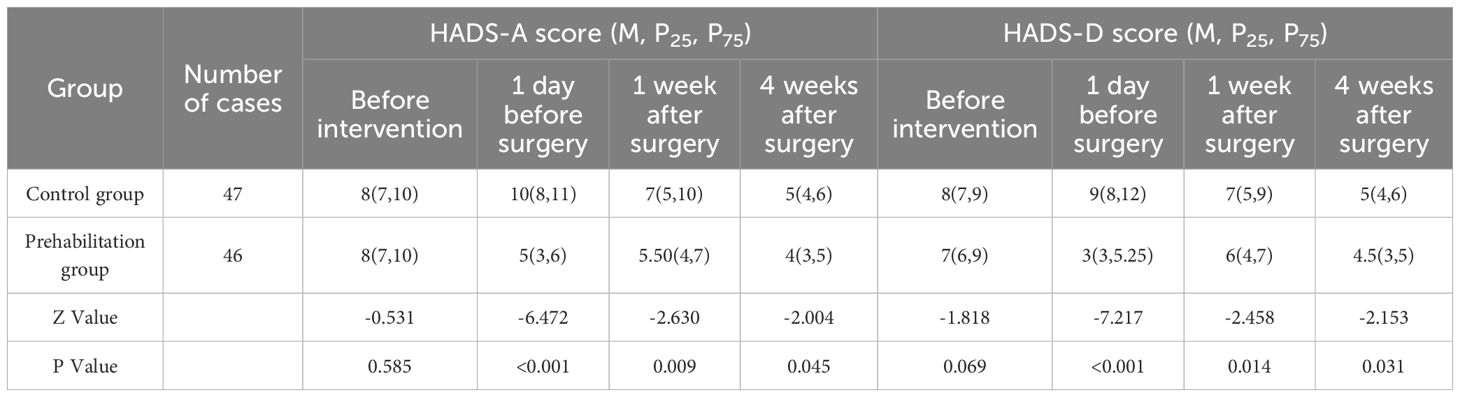
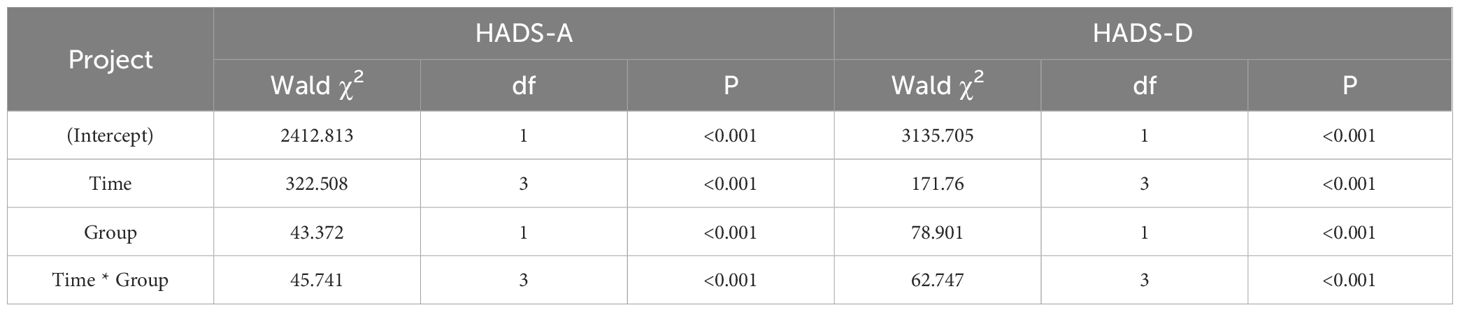
3.3 Comparison of psychological states between the two groups
Before the intervention, the HADS-A and HADS-D scores of both groups were comparable (P > 0.05). After the intervention, the prehabilitation group had significantly lower scores at each time point compared to the control group (P < 0.05). GEE analysis indicated significant intervention effects, time effects, and interaction effects between the two groups (P < 0.05), demonstrating that the HADS scores of the two groups showed significant differences due to the variations in rehabilitation nursing plans. For details, see Tables 5 and 6.
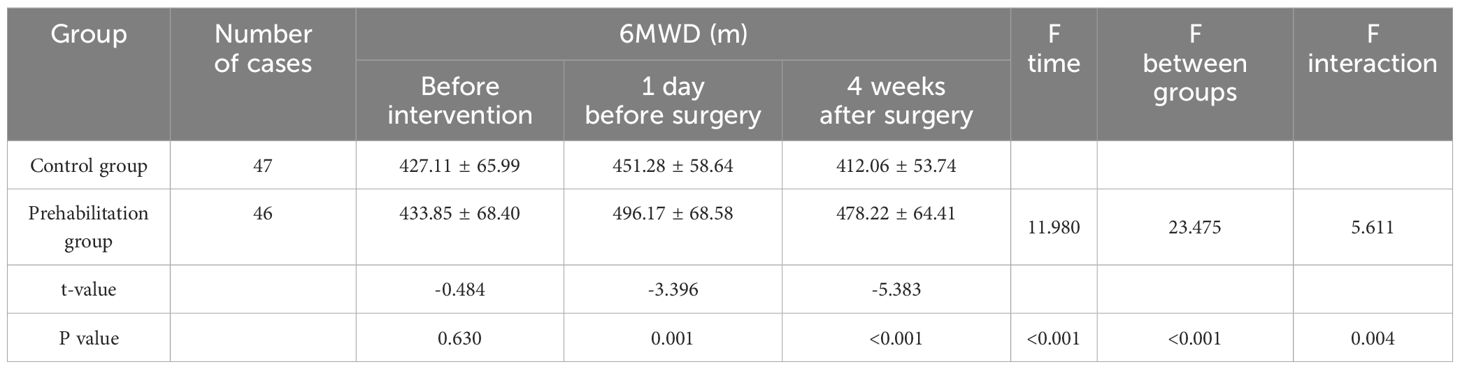
3.4 Comparison of 6MWD between two groups
Before the intervention, the 6MWD of both groups was comparable (P > 0.05). Compared to the control group, the prehabilitation group showed higher 6MWD at all time points after the intervention (P < 0.05). A time effect, intervention effect, and interaction effect were observed between the two groups (P < 0.05), indicating significant differences in 6MWD due to the different rehabilitation care programs. Details are shown in Table 7.
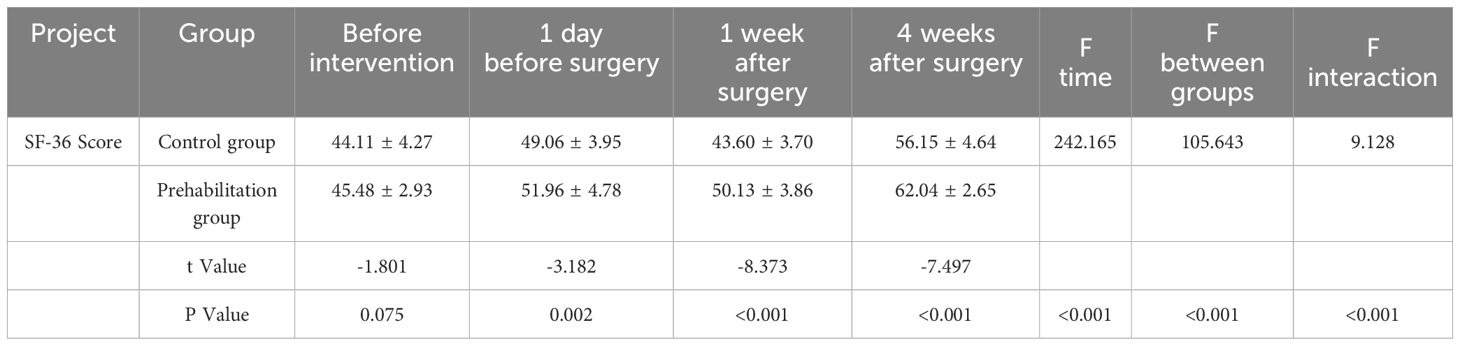
3.5 Comparison of quality of life between two groups
Before the intervention, there was no significant difference in the SF-36 scores between the two groups (P > 0.05). After the intervention, at each time point, the SF-36 scores of the experimental group were higher than those of the control group (P < 0.05). There was a time effect, intervention effect, and interaction effect between the two groups’ SF-36 scores (P < 0.05), as detailed in Table 8.
3.6 Comparison of postoperative hospitalization, chest drain removal, time to first ambulation, and complications between two groups
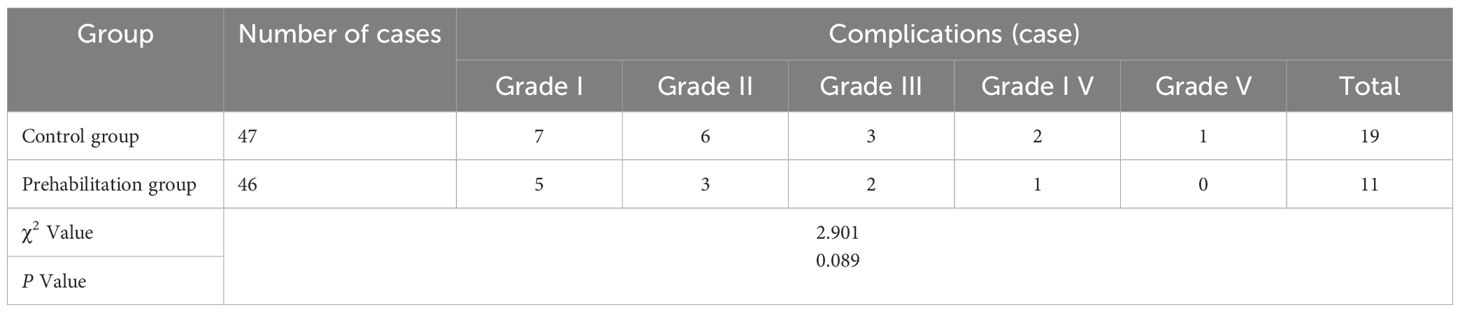
(1) The prehabilitation group had significantly shorter postoperative hospitalization, chest drain removal, and time to first ambulation compared to the control group (P < 0.05), as shown in Table 9. (2) Complications occurred in 19 cases in the control group and 11 cases in the prehabilitation group (P>0.05), as shown in Table 10.
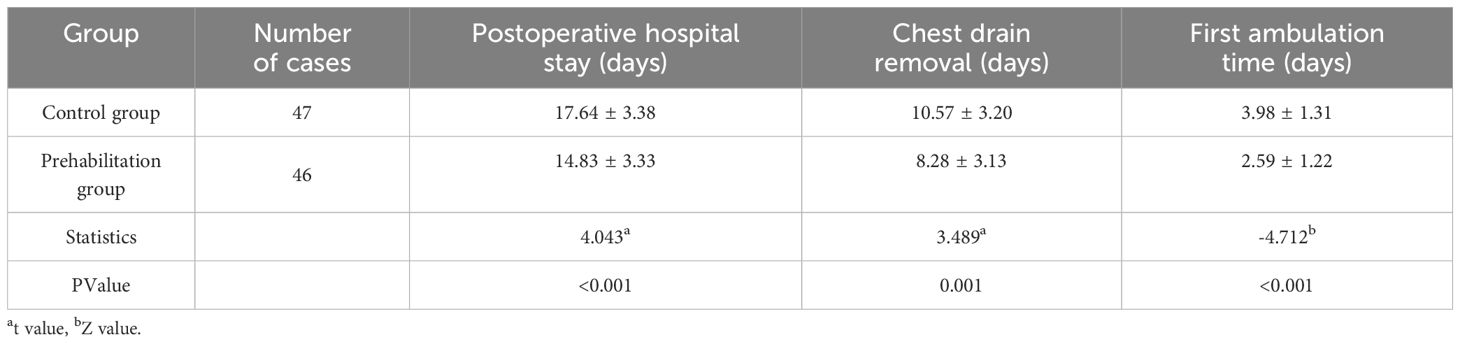
Table 9. Comparison of postoperative hospitalization, chest drain removal, and time to first ambulation between two groups.
4 Discussion
4.1 The effect of prehabilitation programs on the nutritional status of elderly esophageal cancer patients
Studies have shown that the incidence of malnutrition in esophageal cancer patients is as high as 50% to 76% (25), and patients with a high risk of malnutrition tend to have worse prognoses, higher complication rates, and poorer outcomes. Preoperative nutritional support can promote wound healing, prevent complications, and enhance immune function.
In this study, the prehabilitation group underwent nutritional screening and assessment prior to surgery and received personalized nutritional support. After the intervention, the perioperative nutritional indicators of the prehabilitation group were superior to those of the control group, with more stable changes in the prehabilitation group, facilitating better postoperative nutritional recovery. This finding is consistent with the results of Chen et al. (26), which demonstrated that postoperative patients, with sufficient nutritional support and coordinated exercise, successfully transitioned through the catabolic phase and experienced accelerated recovery.
4.2 Effect of the prehabilitation program on the psychological state of elderly patients with esophageal cancer
The incidence of esophageal cancer is higher among the elderly, and these patients tend to have more complications and higher mortality rates. Emotional disorders such as depression and anxiety are common, and some patients may develop autonomic dysfunction, all of which negatively affect postoperative recovery (27). Preoperative psychological interventions aimed at improving patients’ mental state, along with encouragement and support for prehabilitation exercises and nutritional planning, can be beneficial.
In both groups, preoperative HADS-A and HADS-D scores were greater than 8, indicating that elderly esophageal cancer patients experienced anxiety and depression prior to surgery. Psychological support provided to elderly patients may influence hormone secretion through the hypothalamic-pituitary-adrenal axis, thereby enhancing immune function and promoting physical recovery. The results showed that the HADS-A and HADS-D scores in the prehabilitation group were significantly lower than those in the control group during the perioperative period (P<0.05), with significant time effects, intervention effects, and interaction effects (P<0.05). This suggests that the prehabilitation program is effective in alleviating anxiety and depression in patients. A study by Zhou X et al (28) on the impact of prehabilitation on depression scores in elderly patients undergoing laryngeal surgery also demonstrated that prehabilitation effectively alleviates depression, consistent with the findings of this study.
4.3 Effects of prehabilitation programs on perioperative functional status and physical capacity in elderly patients with esophageal cancer
Elderly patients with esophageal cancer often experience increased metabolism, more complications, and an elevated physical and mental burden due to treatment, which frequently leads to greater consumption of energy and a significant decline in functional capacity (29). These factors negatively impact postoperative recovery, leading to more adverse events, extended hospital stays, and delayed rehabilitation. Exercise prehabilitation can trigger physiological stress, promoting adaptive responses in tissues and organs, which enhances the patient’s ability to cope with surgical stress (29).In this study, the prehabilitation group underwent a comprehensive assessment of functional status, and personalized exercise plans were developed based on each patient’s condition, ensuring safety while improving physical function. The results showed that implementing the prehabilitation program was beneficial in increasing patients’ 6MWD during the perioperative period, as well as improving functional status and physical capacity. This is consistent with the findings of Moorthy et al. (30), where systematic prehabilitation exercise training increased patients’ preoperative functional reserve, enhancing endurance and physical fitness, and resulting in faster and better recovery compared to conventional care after surgery.
4.4 Effect of prehabilitation program on quality of life of elderly patients with esophageal cancer
Elderly patients with esophageal cancer are often affected by cachexia, which reduces physiological reserves. When combined with surgical trauma, this results in poor quality of life (31). In this study, the SF-36 scale was used to explore the impact of the prehabilitation program on quality of life. The results showed that the implementation of the prehabilitation program was effective in improving patients’ overall quality of life. This finding is similar to that of Allen et al. (13), and may be related to the improvement of both physiological reserves and psychological well-being as a result of prehabilitation.
4.5 Effect of prehabilitation program on postoperative hospitalization, chest drain removal, first ambulation, and complications in elderly patients with esophageal cancer
Patients in the prehabilitation group ambulated earlier, had their chest drains removed sooner, and experienced shorter postoperative hospital stays, consistent with the findings of Swaminathan et al. (32). This suggests that the prehabilitation program, which provides psychological, nutritional, and exercise support, contributes to improving patients’ mental health, enhancing muscle mass and mobility, and facilitating the recovery of their functional status and ability to ambulate. It also helps shorten the time needed for chest drain removal and hospital stay.
Although some studies (33)indicate that prehabilitation can reduce the incidence of postoperative complications by improving patients’ physical and psychological reserves, other research shows that prehabilitation does not effectively lower the complication rate (30), which aligns with the findings of this study. This discrepancy may be related to the complexity and difficulty of treating elderly esophageal cancer patients. Therefore, future studies could consider conducting more rigorous, large-scale, multicenter randomized controlled trials to further evaluate the effect of prehabilitation on complications in elderly patients with esophageal cancer.
4.6 Artificial intelligence influence on perioperative management
In our research, all indicators of the prehabilitation group were better than those of the control group, except for complications. Maybe there are other variables which were not studied such as stage of the disease the stage of training of the operating surgeon even the time when the operation was carried out first on the list or second on the list. We notice that deep learning used in AI can help identify such variables even with small sample size, deep learning using neural networks can be used instead of basic statistics (34, 35). And AI can be used in enhancing perioperative care and even intraoperative experience such as using Deepseek to answer some questions from patients about prehabilitation (36). In future research, we can attempt to explore the use of AI to manage patients who participated in prehabilitation, in order to improve the scientific and rigorous nature of prehabilitation management.
5 Conclusion
This study suggests that implementing a prehabilitation program for elderly esophageal cancer patients holds significant value. It can improve patients’ nutritional status, enhance physical endurance and quality of life, and to some extent, alleviate perioperative anxiety and depression, as well as shorten postoperative recovery time. However, it does not reduce the incidence of complications which maybe related to other variables, in future research, we can introduce AI to control variables and strengthen communication with patients. Compared to younger individuals, elderly patients have weaker physiological and psychological vulnerabilities, so a comprehensive monitoring of all patient indicators should be conducted throughout the prehabilitation process for safety reasons. Furthermore, as this was a single-center study with a relatively small sample size, potential biases may exist, and future large-scale multicenter trials are needed to further verify its scientific validity and feasibility.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Medical School of Jiangsu University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KZ: Supervision, Validation, Data curation, Formal Analysis, Visualization, Conceptualization, Investigation, Writing – original draft, Resources, Writing – review & editing. FC: Project administration, Methodology, Visualization, Supervision, Writing – review & editing, Investigation, Writing – original draft, Resources. XS: Writing – original draft, Software, Investigation, Writing – review & editing, Validation, Project administration. CL: Project administration, Methodology, Validation, Writing – original draft, Writing – review & editing. ZL: Writing – review & editing, Funding acquisition, Supervision, Visualization, Resources, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Mechanism and clinical value of LncRNA FOXD3-AS1 in the progression of esophageal cancer, K202204, Science and Technology Bureau of Sucheng District.
Acknowledgments
The research team thank all the individuals with esophageal cancer who agreed to participate in this study and gave their time to attend all data collection appointments and the intervention.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Liu ZC, Li ZX, Zhang Y, Zhou T, Zhang JY, You WC, et al. Interpretation on the report of global cancer statistics 2020. J Multidiscip Cancer Manage (Electronic Version). (2021) 7:1–14. doi: 10.12151/JMCM.2021.02-0
2. Zhou JC, Zheng RS, Zhang SW, Chen R, Wang SM, Sun KX, et al. Analysis on the trend of esophageal cancer incidence and age change in cancer registration areas of China, 2000 to 2015. Chin J Cancer Prev Treat. (2020) 27:1437–42. doi: 10.16073/j.cnki.cjcpt.2020.18.01
3. Zhu L, Gao J, Bai DX, Liang Y, Yang Z, Liu RR, et al. Prevalence of nutritional risk in patients with esophageal cancer in China: A meta-analysis. Modern Prev Med. (2020) 47:4447–51. doi: 10.20043/j.cnki.mpm.2020.24.009
4. Heinrich M, Hofmann L, Baurecht H, Kreuzer PM, Knüttel H, Leitzmann MF, et al. Suicide risk and mortality among patients with cancer. Nat Med. (2022) 28:852–9. doi: 10.1038/s41591-022-01745-y
5. Kamarajah SK, Gujjuri RR, Elhadi M, Umar H, Bundred JR, Subramanya MS, et al. Elderly patients have increased perioperative morbidity and mortality from oesophagectomy for oesophageal cancer: A systematic review and meta-analysis. Ejso. (2021) 47:1828–35. doi: 10.1016/j.ejso.2021.02.030
6. Maria ME, Guillaume B-D, Rashami A, Celena S-B, and Francesco C. Multimodal prehabilitation improves functional capacity before and after colorectal surgery for cancer: a five-year research experience. Acta Oncol. (2017) 56(2):295–300. doi: 10.1080/0284186X.2016.1268268
7. Dai XJ and Wu Q. Review on application of Trimodal Prehabilitation in gastrointestinal cancer patients undergoing elective surgery. Chin J Pract Nurs. (2021) 37:317–21. doi: 10.3760/cma.j.cn211501-20200426-02055
8. Low DE, Allum W, De Manzoni G, Ferri L, Immanuel A, Kuppusamy M, et al. Guidelines for perioperative care in esophagectomy: enhanced recovery after surgery (ERAS(®)) society recommendations. World J Surg. (2019) 43:299–330. doi: 10.1007/s00268-018-4786-4
9. Cao H, Chen YJ, Gu XP, Min S, Peng SL, Wang DX, et al. Clinical practice guidelines for enhanced recovery after surgery in China(2021 edition). Chin J Pract Surg. (2021) 41:961–92. doi: 10.19538/j.cjps.issn1005-2208.2021.09.01
10. Ajani JA, D'Amico TA, Bentrem DJ, Chao J, Corvera C, Das P, et al. Esophageal and esophagogastric junction cancers, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. (2019) 17:855–83. doi: 10.6004/jnccn.2019.0033
11. Liu ZJ, Zhang L, Liu HS, Cang J, Wang TL, Min S, et al. Expert consensus on prehabilitation management for enhanced recovery in patients undergoing thoracic surgery (2022). Med J Peking Union Med Coll Hosp. (2022) 13:387–401. doi: 10.12290/xhyxzz.2022-0178
12. Bolger JC, Loughney L, Tully R, Cunningham M, Keogh S, McCaffrey N, et al. Perioperative prehabilitation and rehabilitation in esophagogastric Malignancies: a systematic review. Dis Esophag. (2019) 32(9):doz058. doi: 10.1093/dote/doz058
13. Allen SK, Brown V, White D, King D, Hunt J, Wainwright J, et al. Multimodal prehabilitation during neoadjuvant therapy prior to esophagogastric cancer resection: effect on cardiopulmonary exercise test performance, muscle mass and quality of life—A pilot randomized clinical trial. Ann Surg Oncol. (2022) 29:1839–50. doi: 10.1245/s10434-021-11002-0
14. Guo Z, Ji SG, Xu Y, Cong ZZ, and Hu LW. The effect of preoperative prehabilitation on nutritional status and body composition of patients with esophageal cancer after operation. Parent Enteral Nutr. (2018) 25:156–60. doi: 10.16151/j.1007-810x.2018.03.008
15. Valkenet K, Trappenburg JCA, Ruurda JP, Guinan EM, Reynolds JV, Nafteux P, et al. Multicentre randomized clinical trial of inspiratory muscle training versus usual care before surgery for oesophageal cancer. Br J Surg. (2018) 105:502–11. doi: 10.1002/bjs.10803
16. Minnella EM, Awasthi R, Loiselle S-E, Agnihotram RV, Ferri LE, and Carli F. Effect of exercise and nutrition prehabilitation on functional capacity in esophagogastric cancer surgery: A randomized clinical trial. JAMA Surg. (2018) 153:1081–9. doi: 10.1001/jamasurg.2018.1645
17. Yamana I, Takeno S, Hashimoto T, Maki K, Shibata R, Shiwaku H, et al. Randomized controlled study to evaluate the efficacy of a preoperative respiratory rehabilitation program to prevent postoperative pulmonary complications after esophagectomy. Digest Surg. (2015) 32:331–7. doi: 10.1159/000434758
18. Christensen JF, Simonsen C, Brack-Petersen A, Thorsen-Streit S, Herrstedt A, Djurhuus SS, et al. Safety and feasibility of preoperative exercise training during neoadjuvant treatment before surgery for adenocarcinoma of the gastro-oesophageal junction. Bjs Open. (2019) 3:74–84. doi: 10.1002/bjs5.50110
19. Li HC, Tong F, Ying YH, Pan HH, and Zhao W. Prehabilitation program in perioperative period for patients with esophageal cancer. Zhejiang Med J. (2019) 41:1301–4. doi: 10.12056/j.issn.1006-2785.2019.41.12.2017-1041
20. Xie Q, Wang Q, Lei M, Liu XB, and Zhao MR. Effect of preoperative prehabilitation on nutritional indicators, body composition, blood glucose, inflammatory response and immune function of patients with esophageal cancer after operation. Clin Misdiagn Misther. (2019) 32:87–93. doi: 10.3969/j.issn.1002-3429.2019.12.019
21. Li L, Zhang YH, Huang YL, and Li SM. Effect of preoperative prehabilitation in patients receiving surgical treatment for adenocarcinoma of the esophagogastric junction. J Nurs Sci. (2021) 36:80–3. doi: 10.3870/j.issn.1001-4152.2021.20.080
22. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. (2002) 166:111–7. doi: 10.1164/ajrccm.166.1.at1102
23. Ying W, Min QW, Lei T, Na ZX, Li L, Jing L, et al. The health effects of Baduanjin exercise (a type of Qigong exercise) in breast cancer survivors: A randomized, controlled, single-blinded trial. Eur J Oncol Nurs. (2019) 39:90–7. doi: 10.1016/j.ejon.2019.01.007
24. Song ZF, Han ZJ, Lin L, and Che GW. Reliability and validity of SF-36 scale for evaluating quality of life of thoracic surgery patients. Chin J Clin Thorac Cardiovasc Surg. (2014) 21:164–7.
25. Cao J, Xu H, Li W, Guo Z, Lin Y, Shi Y, et al. Nutritional assessment and risk factors associated to malnutrition in patients with esophageal cancer. Curr Probl Cancer. (2021) 45:100638. doi: 10.1016/j.currproblcancer.2020.100638
26. Chen J, Luo AL, Yang L, Wang W, Zhou X, and Yang M. Nutrition management by a multidisciplinary team for prevention of nutritional deficits and morbidity following esophagectomy. Braz J Med Biol Res. (2023) 56:e12421. doi: 10.1590/1414-431X2023e12421
27. Housman B, Flores R, and Lee DS. Narrative review of anxiety and depression in patients with esophageal cancer: underappreciated and undertreated. J Thorac Dis. (2021) 13:3160–70. doi: 10.21037/jtd-20-3529
28. Zhou X, Jin L, Zhao J, and Liu XM. Application of multimodal rehabilitation intervention in elderly patients undergoing partial laryngectomy. Chin J Gerontol. (2022) 42:5383–6. doi: 10.3969/j.issn.1005-9202.2022.21.062
29. Zhou YB. Prehabilitation for gastrointestinal cancer patients. Chin J Gastrointest Surg. (2021) 24:122–7. doi: 10.3760/cma.j.cn.441530-20200318-00152
30. Moorthy K, Halliday LJ, Noor N, Peters CJ, Wynter-Blyth V, and Urch CE. Feasibility of implementation and the impact of a digital prehabilitation service in patients undergoing treatment for oesophago-gastric cancer. Curr Oncol (Toronto Ont). (2023) 30:1673–82. doi: 10.3390/curroncol30020128
31. Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, and Kumbhani DJ. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. (2005) 242:326–41. doi: 10.1097/01.sla.0000179621.33268.83
32. Swaminathan N, Kundra P, Ravi R, and Kate V. ERAS protocol with respiratory prehabilitation versus conventional perioperative protocol in elective gastrectomy- a randomized controlled trial. Int J Surg (Lond Engl). (2020) 81:149–57. doi: 10.1016/j.ijsu.2020.07.027
33. Liu K, Ji S, Xu Y, Diao Q, Shao C, Luo J, et al. Safety, feasibility, and effect of an enhanced nutritional support pathway including extended preoperative and home enteral nutrition in patients undergoing enhanced recovery after esophagectomy: a pilot randomized clinical trial. Dis Esophag. (2020) 33(2):doz030. doi: 10.1093/dote/doz030
34. Antonio Vittorino G and Marialuisa L. Telemedicine: a unique, univocal, and shared definition for everyone. Artif Intell Surg. (2024) 4:37–43. doi: 10.20517/ais.2024.03
35. Valentina B, Matteo P, and Elena Giovanna B. The health technology assessment in the artificial intelligence era: the AI surgical department. Artif Intell Surg. (2024) 4:44–7. doi: 10.20517/ais.2024.10
Keywords: elderly, esophageal cancer, prehabilitation, surgery, program application
Citation: Zhou K, Cai F, Shao X, Luo C and Liu Z (2025) Application of prehabilitation program in elderly patients undergoing esophageal cancer surgery. Front. Oncol. 15:1605647. doi: 10.3389/fonc.2025.1605647
Received: 03 April 2025; Accepted: 23 June 2025;
Published: 11 July 2025.
Edited by:
Savvas Lampridis, Imperial College London, United KingdomReviewed by:
Andras Papp, University of Pecs, HungaryHeba Taher, Cairo University, Egypt
Kulbhushan Thakur, University of Delhi, India
Ester Oneda, Fondazione Poliambulanza Istituto Ospedaliero, Italy
Copyright © 2025 Zhou, Cai, Shao, Luo and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao Shao, c2hhb3NtaWxlQDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
 Kun Zhou1†
Kun Zhou1† Xiao Shao
Xiao Shao Zihao Liu
Zihao Liu