- 1Department of Head and Neck Surgery, Clinical Oncology School of Fujian Medical University & Fujian Cancer Hospital, Fuzhou, China
- 2Department of Anesthesiology, Clinical Oncology School of Fujian Medical University & Fujian Cancer Hospital, Fuzhou, China
- 3Department of Urological Oncology, Clinical Oncology School of Fujian Medical University & Fujian Cancer Hospital, Fuzhou, China
Objective: This study aims to compare the short-term and long-term outcomes of three surgical approaches for thyroid cancer: Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA), Gasless Unilateral Axillary Endoscopic Thyroidectomy (ETGUA), and Conventional Open Thyroidectomy (COT).
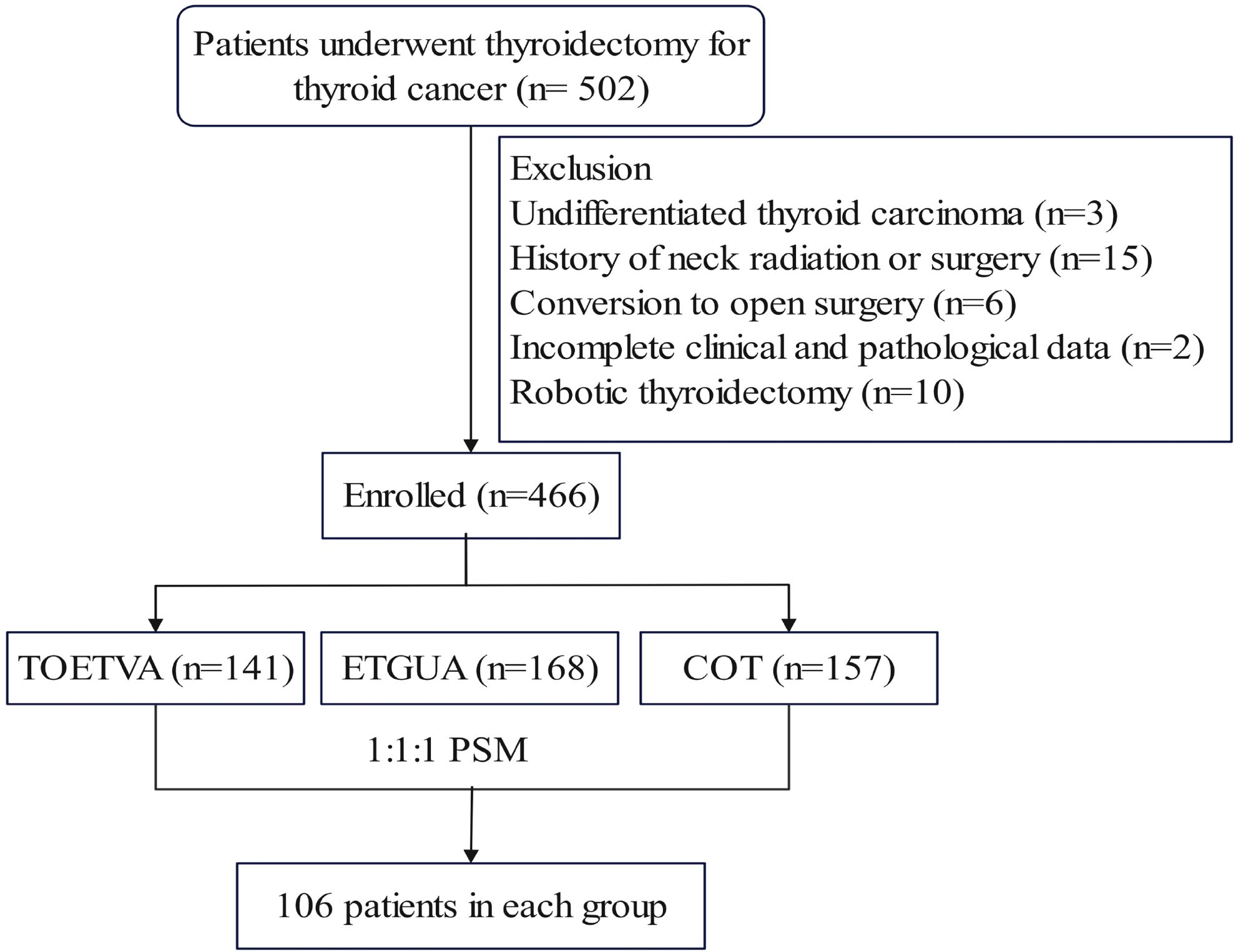
Methods: A total of 466 thyroid cancer patients who underwent surgery were initially included. After propensity score matching (PSM), 318 patients were analyzed, with 106 patients in each group (TOETVA, ETGUA, and COT). The primary outcomes compared included surgical parameters (incision length, blood loss, operation time, lymph node dissection), postoperative inflammation (WBC, CRP, IL-6), postoperative complications, postoperative pain (Visual Analog Scale, VAS), scar assessment (Vancouver Scar Scale, VSS), wound satisfaction, costs, and quality of life (36-Item Short Form Health Survey, SF-36).
Results: After matching, the operation time for TOETVA was longer than that for both ETGUA and COT. The number of lymph nodes dissected in ETGUA was fewer than in TOETVA and COT. There were no significant differences in postoperative complications, VAS scores, costs, or hospital stay among the three groups. On the first postoperative day, TOETVA and ETGUA showed higher levels of WBC and CRP than COT, but no significant differences were observed by day three. TOETVA had the shortest incision and the lowest VSS score. Wound satisfaction was significantly higher in both TOETVA and ETGUA compared to COT, with no significant difference between TOETVA and ETGUA. In terms of quality of life, some dimensions in TOETVA and ETGUA were higher than in COT. Each surgical approach has its own advantages and disadvantages.
Conclusion: TOETVA demonstrated the shortest incision and the lowest VSS score, while both TOETVA and ETGUA showed the best wound satisfaction and specific domains of quality of life. However, TOETVA had the longest operation time, and ETGUA had the fewest lymph nodes dissected.
Introduction
Thyroid cancer is one of the most common malignancies worldwide, with its incidence steadily rising over recent decades, particularly among women aged 20-29 years (1–3). As the number of younger patients increases, there is a growing emphasis on both medical and aesthetic outcomes in treatment. Fortunately, thyroid cancer generally has a good prognosis with a high survival rate, making quality of life an important consideration for both patients and healthcare providers (4, 5).
Conventional open thyroidectomy (COT) remains a key treatment approach for thyroid cancer. However, one of its major drawbacks is the visible surgical scar on the anterior neck, which can be particularly prominent in patients prone to developing hypertrophic scars (6). This can lead to significant cosmetic concerns and psychological distress (7). Consequently, improving the aesthetic outcome of surgical scars, ensuring effective tumor control, enhancing postoperative recovery, and optimizing the patient’s quality of life have become critical objectives in thyroid cancer surgery.
Laparoscopic surgery has garnered increasing attention due to its numerous advantages, such as magnification, which allows for a clearer surgical field and improved precision during surgery. Furthermore, laparoscopic approaches typically involve smaller, less noticeable incisions, providing excellent cosmetic benefits while ensuring effective treatment outcomes (8–10). As a result, laparoscopic thyroidectomy has become increasingly popular among both thyroid surgeons and patients. Various laparoscopic approaches have been developed, including the Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA) and Gasless Unilateral Axillary Endoscopic Thyroidectomy (ETGUA) (11, 12). Each of these approaches has its own set of advantages and disadvantages, and there is still no consensus on which technique is the most suitable for clinical use. This study aims to compare the short-term and long-term outcomes of three surgical approaches for thyroid cancer: TOETVA, ETGUA, and COT.
Methods
Patients
This prospective non-randomized interventional study included patients who underwent surgical treatment for thyroid cancer at Fujian Cancer Hospital from March 2022 to August 2023. The inclusion criteria were: (1) histopathologically confirmed differentiated thyroid cancer; (2) no distant organ metastasis on imaging studies; and (3) complete clinical and pathological data. The exclusion criteria were: (1) a history of neck radiation, previous neck surgery, or trauma; (2) Grade III hyperthyroidism; (3) conversion from endoscopic surgery to open surgery during the procedure; (4) robotic thyroidectomy, and (5) concurrent psychiatric disorders. As shown in the flowchart (Figure 1), a total of 318 thyroid cancer patients were included, with 106 patients in each group.
Surgical technique
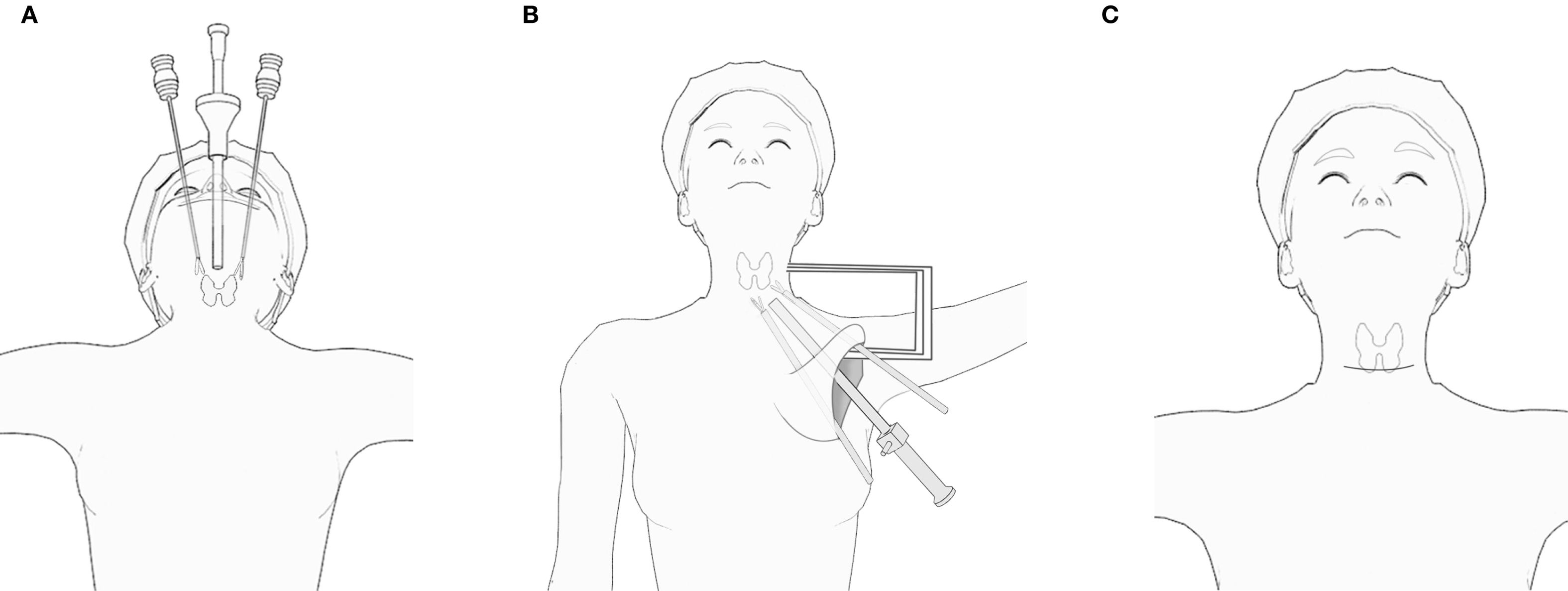
TOETVA: The patient is positioned in a supine position with hyperextension of the neck. A small horizontal incision of approximately 3-4 cm is made at the anterior vestibule of the oral cavity, just above the upper gingiva. The surgical site is prepared by injecting a solution containing adrenaline for tissue expansion in the anterior cervical subcutaneous space. This is followed by the application of CO2 insufflation to maintain the cervical space. The dissection is carried out in a subperiosteal plane, starting from the mandible and extending toward the upper margin of the sternum. The thyroid gland is exposed through this corridor, and thyroidectomy is performed.
ETGUA: The patient is placed in a supine position with the shoulders slightly elevated. A skin incision of approximately 8 cm is made along the natural axillary skin crease. The skin flap is dissected along the superficial fascia of the pectoralis major muscle. A specialized retractor is inserted into the axillary space between the sternal and clavicular heads of the sternocleidomastoid muscle. After identifying the omohyoid and hyoglossus muscles, a suspension retractor is placed to aid dissection. The thyroid gland is then exposed through this route, and thyroidectomy is performed.
COT: A skin incision of approximately 8 cm is made in a transverse direction 1-2 cm above the sternal notch, following the natural skin lines. The skin flap is dissected subcutaneously, and the strap muscles are separated along the midline (cervical line) to expose the thyroid gland. Thyroidectomy is then performed after careful dissection of surrounding structures. Figure 2 illustrates the surgical diagrams for these procedures.
Data collection and outcomes
The preoperative, postoperative day (POD1) 1, and day 3 White blood cell (WBC), serum C-reactive protein (CRP), and Interleukin-6 (IL-6) levels were measured to assess the inflammatory response.
Nonsteroidal anti-inflammatory drugs (NSAIDs) were routinely used for pain relief on postoperative days 1 and 2. The pain intensity was assessed using the Visual Analog Scale (VAS) under the guidance of a professional nurse on the morning of postoperative days 1 to 3.
The drainage tube was removed when the drainage fluid became clear and the volume of drainage was less than 20 mL per day for TOETVA and COT, and less than 50 mL for ETGUA.
A parathyroid hormone (PTH) level < 12 pg/mL at 6 hours postoperatively is considered indicative of hypoparathyroidism. At 6 months of follow-up, a PTH level ≤ 12 pg/mL or the development of clinical symptoms of permanent hypocalcemia should be considered as permanent hypoparathyroidism (13, 14).
Recurrent laryngeal nerve injury is characterized by hoarseness, dysphagia, aphonia, or dyspnea postoperatively in patients without preoperative hoarseness. Preoperative laryngoscopy reveals normal vocal cords. Following surgery, patients may experience voice changes, coughing while swallowing, loss of voice, or difficulty breathing. Permanent injury is defined as damage lasting for more than 6 months (15, 16).
The Vancouver Scar Scale (VSS) was used to assess postoperative scarring. The VSS evaluates four parameters: height, pliability, vascularity, and pigmentation, with a score range of 0 to 15. A higher score indicates more severe scarring (17). The wound satisfaction score ranges from 0 to 10, with 0 indicating very unsatisfied and 10 indicating very satisfied (18).
This study used the 36-Item Short Form Health Survey (SF-36) to assess quality of life preoperatively and at 1, 3, 6, and 12 months postoperatively. The SF-36 includes 8 dimensions: physical functioning (PF), role limitations due to physical problems (RP), bodily pain (BP), general health perceptions (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH). Each dimension’s scores range from 0 to 100, with higher scores indicating better quality of life. This scale is widely used to evaluate the quality of life in thyroid cancer patients (19–21).
Statistical analysis
Data analysis was performed using SPSS 25.0 and R 4.4.2. Categorical variables were compared among the three groups using the Chi-square test. For continuous variables, one-way analysis of variance (ANOVA) was used when the data followed a normal distribution; otherwise, the Kruskal-Wallis H test was applied. Pairwise comparisons were conducted among the groups if the p-value was less than 0.05. To account for baseline differences across groups, propensity score matching (PSM) was performed using a caliper of 0.1 with a 1:1:1 matching ratio, utilizing the nearest neighbor matching method. Longitudinal changes between the groups were analyzed using linear mixed models (LMM). Bonferroni correction was applied to adjust for multiple comparisons. A p-value of less than 0.05 was considered statistically significant.
Results
Clinical characteristics
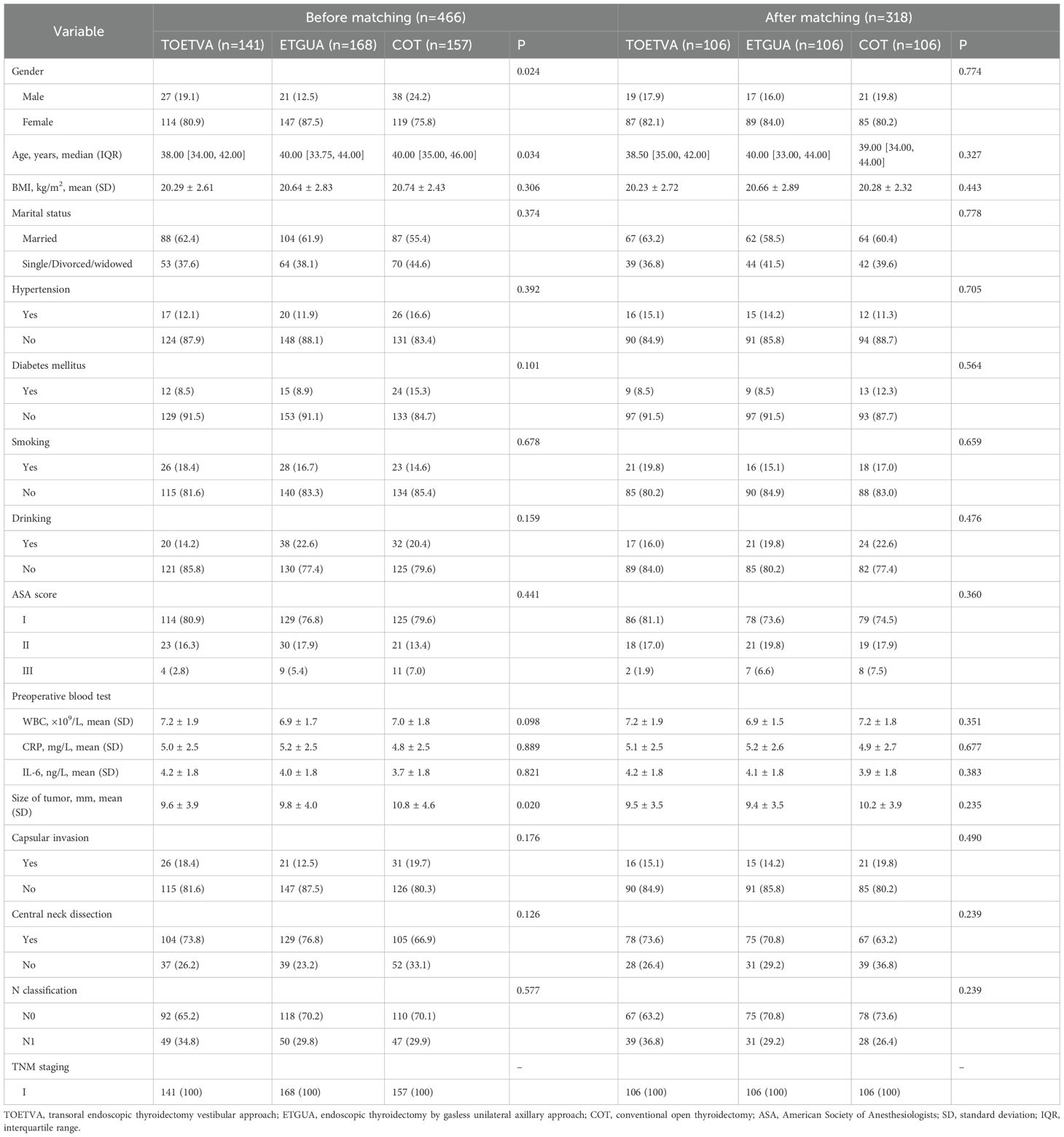
Before matching, there were imbalances in gender, age, and tumor size among the three groups. However, after performing 1:1:1 PSM, each group consisted of 106 patients, and the baseline characteristics of the three groups were well balanced, as shown in Table 1.
Short-term outcomes
The completion rate for the baseline survey was 100%, while the rates for the postoperative surveys were 95.3% at 1 month, 91.5% at 3 months, 86.7% at 6 months, and 82.3% at 12 months.
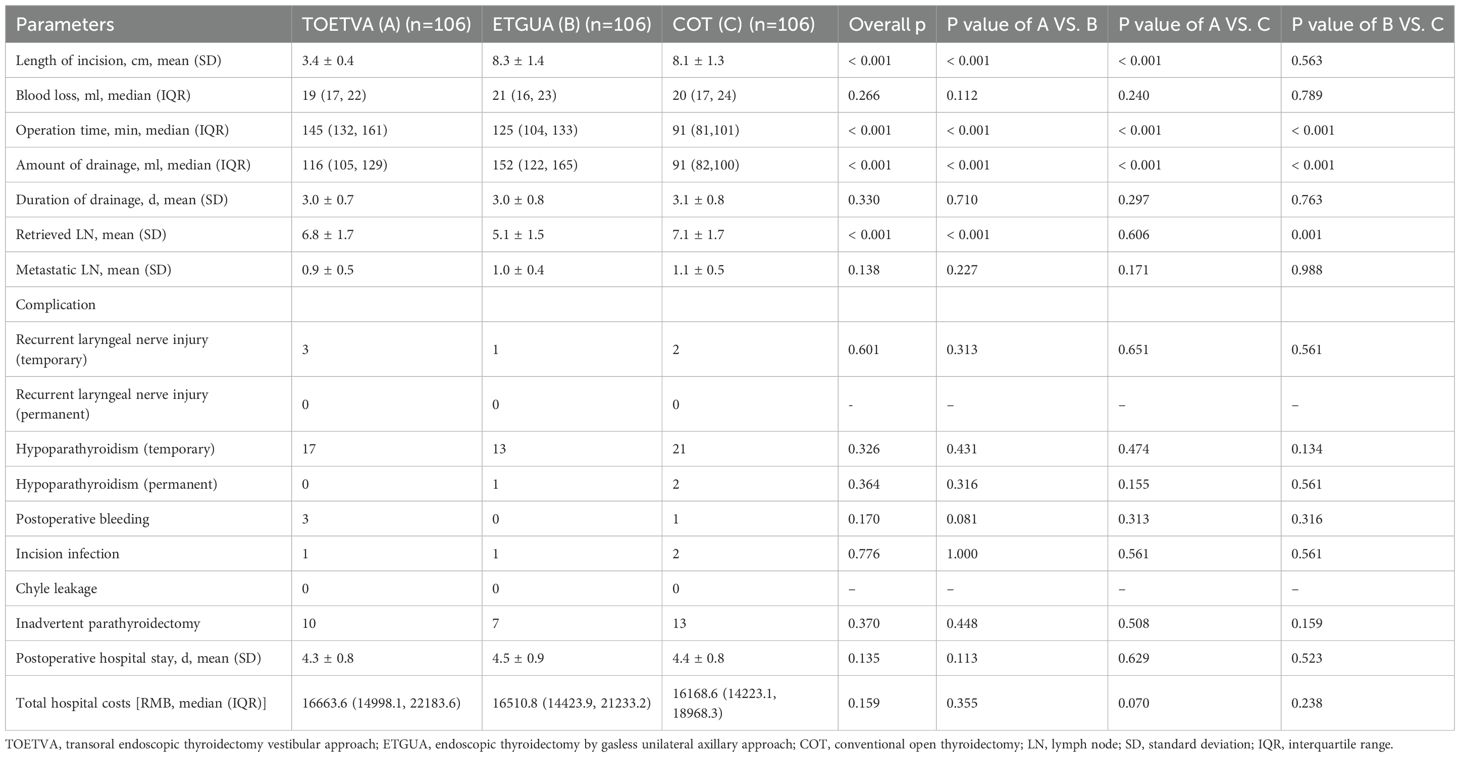
TOETVA demonstrated the shortest incision length, although it required the longest operation time. ETGUA was associated with the highest volume of postoperative drainage, as well as the fewest retrieved lymph nodes.
No statistically significant differences were found among the three groups regarding blood loss, duration of drainage, number of metastatic lymph nodes, overall complications, inadvertent parathyroidectomy, postoperative hospital stay, or total hospital costs, as shown in Table 2.
On POD1, both TOETVA and ETGUA showed higher levels of WBC and CRP when compared to COT; however, by POD3, no significant differences were observed among the three groups. No differences in IL-6 or VAS scores were found among the groups postoperatively, as shown in Figure 3.
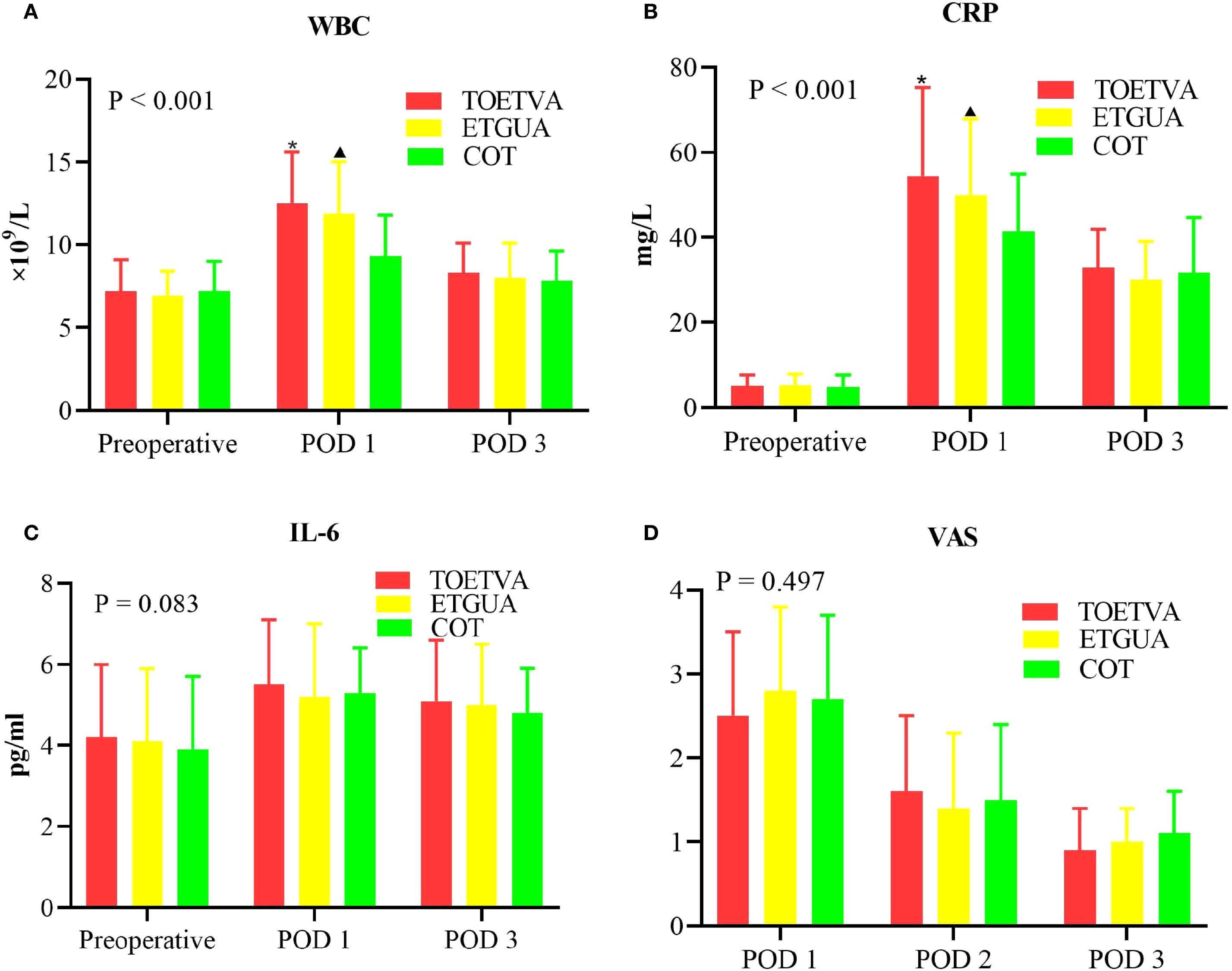
Figure 3. Postoperative inflammatory response and pain intensity. (A) WBC; (B) CRP; (C) IL-6; (D) VAS. *indicates a statistically significant difference (p < 0.05) between TOETVA and COT; ▴indicates a statistically significant difference (p < 0.05) between ETGUA and COT.
Long-term outcomes
TOETVA had the lowest VSS score, indicating the best scar appearance. However, no significant difference was observed between TOETVA and ETGUA in terms of wound satisfaction, with both approaches demonstrating higher satisfaction compared to COT, as shown in Figure 4.
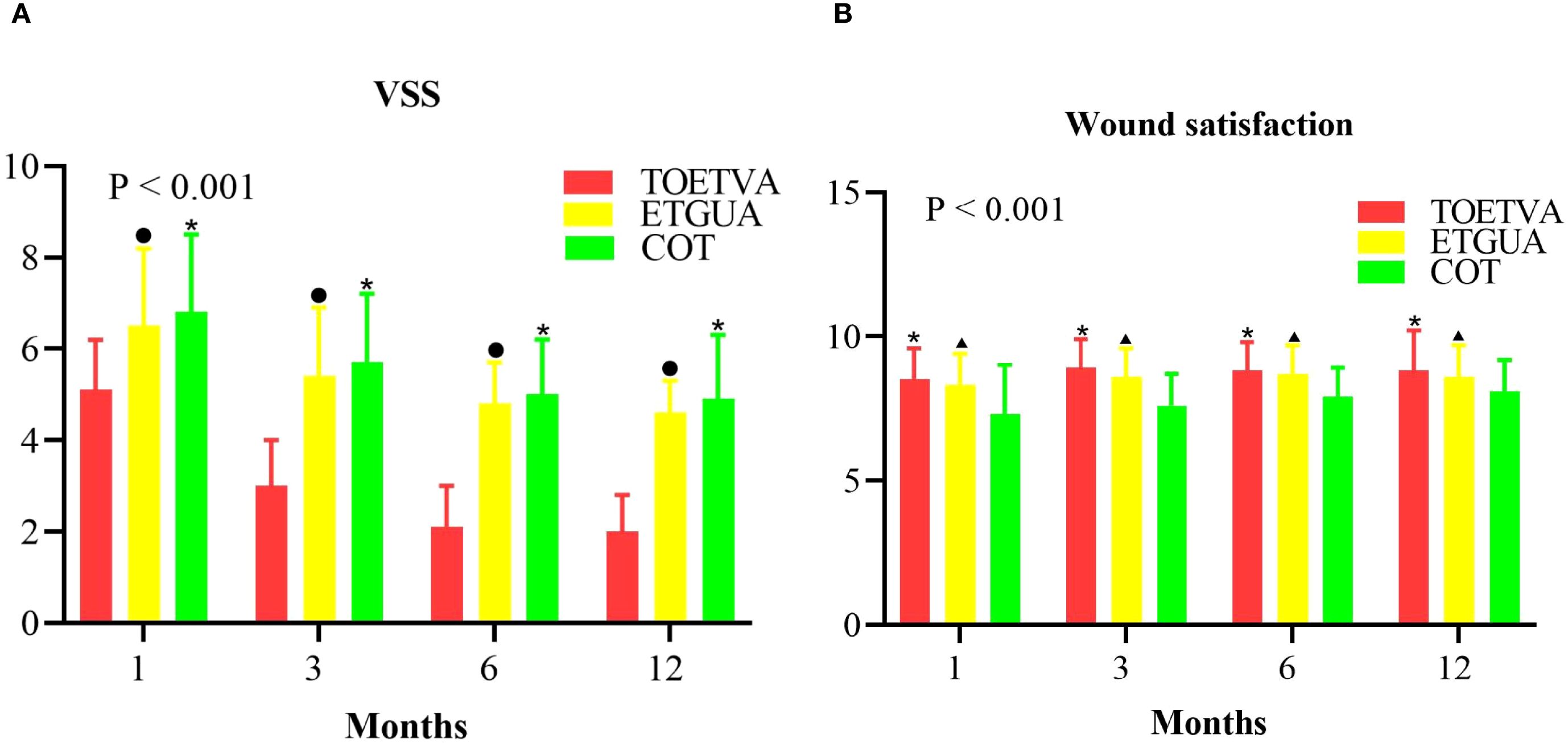
Figure 4. Comparison of postoperative scarring and wound satisfaction. (A) VSS; (B) Wound Satisfaction. •indicates a statistically significant difference (p < 0.05) when comparing TOETVA and ETGUA; *indicates a statistically significant difference (p < 0.05) between TOETVA and COT; ▴indicates a statistically significant difference (p < 0.05) when comparing ETGUA and COT.
Regarding quality of life, there were no significant differences among the three groups in the dimensions of PF, RP, BP, GH, or VT. For SF, at 3 months postoperatively, ETGUA showed higher scores than COT. At 6 and 12 months, both TOETVA and ETGUA had higher SF scores compared to COT. In RE, at 3 months postoperatively, TOETVA showed higher scores than COT, and at 6 and 12 months, both TOETVA and ETGUA demonstrated higher scores compared to COT. For MH, both TOETVA and ETGUA showed higher scores than COT at 6 and 12 months postoperatively, as shown in Figure 5.
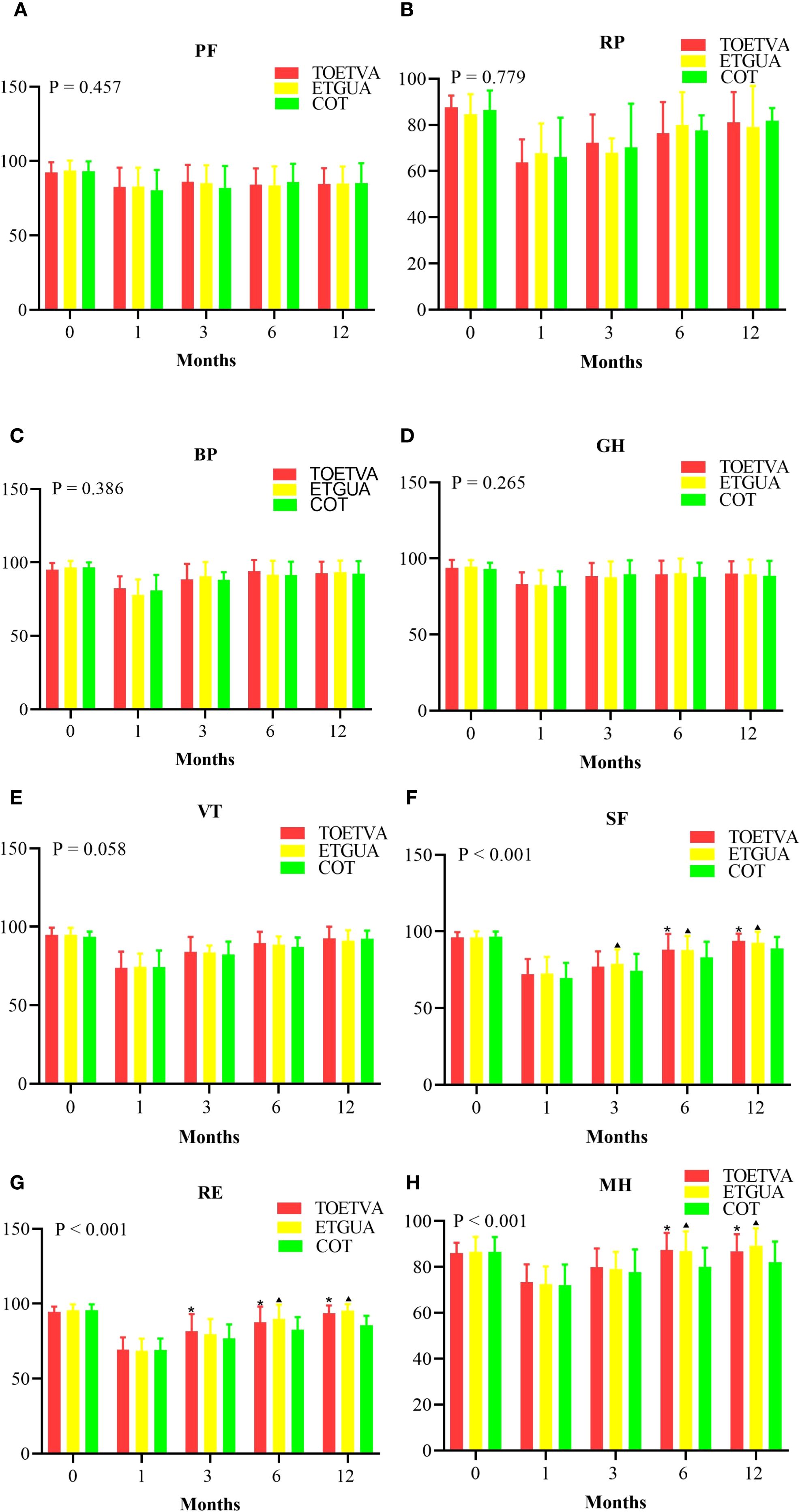
Figure 5. Comparison of Quality of Life Among the Three Patient Groups. (A) Physical functioning, (B) Role limitations due to physical problems, (C) Bodily pain, (D) General health perceptions, (E) Vitality, (F) Social functioning, (G) Role limitations due to emotional problems, (H) Mental health. *indicates a statistically significant difference (p < 0.05) between TOETVA and COT; ▴indicates a statistically significant difference (p < 0.05) when comparing ETGUA and COT.
Discussion
Laparoscopic thyroidectomy has become a widely adopted surgical technique for treating thyroid cancer, offering several advantages over traditional open surgery (22–25). However, within the field of laparoscopic surgery, multiple approaches exist, each with distinct benefits and limitations. At our institution, laparoscopic thyroid surgery was first extensively implemented in 2020, which facilitated the development of expertise and the standardization of procedures. This study focused on patients who underwent surgery starting in 2022, thereby minimizing the impact of the learning curve, which could otherwise introduce bias into outcome comparisons (26, 27).
In this study, TOETVA was associated with the longest operative time among the three techniques. This can be attributed to the confined working space of the oral vestibule and the complex surrounding anatomy, which demands enhanced surgical precision. The restricted space limits instrument maneuverability, often resulting in challenging dissection and prolonged operation time (28–30). While prolonged operative time is a known risk factor for complications due to extended anesthesia exposure (31), and while the transoral approach converts a naturally clean (Class I) incision into a potentially contaminated (Class II) one—theoretically increasing infection risk—no statistically significant differences were observed in overall complication rates across the groups. This discrepancy can be explained by several factors. First, all three surgical techniques are well-established at our institution, with standardized procedures implemented since 2020, thereby minimizing the impact of the learning curve and ensuring consistency and proficiency in surgical execution. Second, strict perioperative protocols were uniformly applied, including aseptic techniques, continuous intraoperative monitoring, and systematic postoperative care, helping to mitigate risks associated with prolonged surgery. Additionally, the minimally invasive nature of TOETVA may itself reduce infection risk (29, 32, 33). Moreover, although TOETVA was the only approach in which prophylactic antibiotics were administered throughout the perioperative period, the standardized surgical and antiseptic protocols (such as strict aseptic techniques and consistent postoperative wound care) applied across all groups likely also contributed to maintaining low and comparable infection rates.
ETGUA was associated with the highest volume of postoperative drainage; however, there were no differences in the duration of drainage among the three groups. This technique involves creating a surgical access pathway through a subcutaneous tunnel from the axillary incision to the neck. The operative space is relatively spacious, the pathway is longer, and the procedure requires significant traction and dissection of surrounding tissues. These factors contribute to an increased accumulation of interstitial fluid postoperatively, resulting in greater drainage. The axillary incision site, which involves relatively thick skin and subcutaneous tissue, is also rich in blood vessels and lymphatic channels. The surgical manipulation in this area can disrupt these vessels, leading to fluid accumulation in the surgical region (34, 35). Although elevated drainage volumes are often indicative of greater tissue trauma and may theoretically increase the risk of seroma or delayed wound healing (36), no statistically significant differences were observed in rates of postoperative bleeding, incision infection, or chyle leakage among the groups. This suggests that the increased drainage did not correlate with a higher incidence of adverse clinical events. Furthermore, although TOETVA and ETGUA were associated with elevated WBC and CRP levels on POD1—reflecting a more pronounced initial inflammatory response likely due to more extensive dissection and access route establishment (37)—these values normalized by POD3. No significant intergroup differences were found in WBC, CRP, or IL-6 levels at that time. The absence of differences in IL-6, a sensitive and short-half-life marker of surgical stress (38, 39), further indicates that the inflammatory response was transient and well-controlled.
Previous studies have shown that while performing contralateral thyroid lobectomy via a unilateral axillary approach presents certain technical challenges, experienced surgeons have demonstrated that total thyroidectomy and bilateral central compartment lymph node dissection through a single axillary incision are feasible (40–43). However, in this study, ETGUA was associated with the fewest retrieved lymph nodes (LN). The limited visibility of the contralateral central compartment lymph nodes, due to obstruction from the trachea, larynx, and cricoid cartilage, restricts access to these nodes, leading to fewer lymph nodes being dissected. Therefore, in cases where contralateral lymph node enlargement is suspected, careful consideration should be given to the selection of ETGUA as the surgical approach.
In this study, TOETVA demonstrated the shortest incision length and the lowest VSS score, indicating the best scar appearance among the three surgical approaches. The moist environment of the oral cavity and its rich vascular supply contribute to rapid wound healing and scar fading. TOETVA utilizes a transoral approach, which avoids visible external incisions, offering excellent cosmetic outcomes (18, 44, 45). Interestingly, no significant difference in wound satisfaction was observed between TOETVA and ETGUA, despite TOETVA having the lowest VSS score. The ETGUA incision is located within the axillary fold, providing a concealed surgical site that does not affect the aesthetic result (46, 47).
In this study, we also evaluated the total hospital costs associated with TOETVA, ETGUA, and COT, as cost is an important factor in the selection of surgical techniques. No statistically significant differences were observed in total hospital costs among the three groups. This suggests that, despite differences in operative time and technical complexity, the overall financial burden of these procedures is comparable, making them equally viable options from a cost perspective when considering other clinical and cosmetic outcomes.
In this study, overall, no significant differences were observed between the groups in the dimensions of PF, RP, BP, GH, or VT. These dimensions reflect general physical health and functioning, suggesting that, despite the differences in surgical techniques, all three approaches may yield similar physical outcomes in the early postoperative period. However, TOETVA and ETGUA demonstrated superior long-term benefits in the SF, RE, and MH domains. Both TOETVA and ETGUA contributed to reduced visible scarring, which enhanced patients’ overall mental health and body image. These improvements may, in turn, promote better emotional well-being and self-esteem (48–50).
This study has several limitations. First, it was conducted at a single center, which may limit the generalizability of the results to other institutions or patient populations. Second, this study did not assess long-term recurrence or survival outcomes due to the relatively short follow-up period. Future studies with extended follow-up are needed to evaluate the oncological efficacy of TOETVA, ETGUA, and COT. Finally, while robotic surgery has become increasingly prevalent in clinical practice (51), our institution initiated robotic surgery relatively recently, having performed only 10 cases at the time of the study. To minimize potential bias associated with the learning curve effect, robotic surgery was excluded from this analysis.
Conclusions
Each surgical approach has its own advantages and limitations. TOETVA and ETGUA demonstrate superior outcomes in terms of incision satisfaction and specific dimensions of quality of life, providing significant benefits compared to COT. However, the selection of the surgical method should be individualized, considering both oncological effectiveness and the patient’s cosmetic and functional preferences.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The study adhered to the principles outlined in the Declaration of Helsinki. It was reviewed and approved by the Ethics Committee of Fujian Cancer Hospital. Written informed consent was obtained from all participants for the purpose of research. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CB: Conceptualization, Writing – review & editing, Writing – original draft. ZL: Writing – review & editing, Investigation, Data curation. MY: Writing – review & editing. SW: Investigation, Data curation, Writing – review & editing. CX: Formal Analysis, Data curation, Writing – review & editing. WP: Formal Analysis, Writing – review & editing, Investigation. CH: Investigation, Writing – review & editing. GF: Writing – review & editing, Data curation, Formal Analysis, Investigation, Conceptualization.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the Startup Fund for scientific research, Fujian Medical University (2022QH1158, 2022QH1654); Natural Science Foundation of Fujian Province (2024J011094, 2024J011083); Sponsored by Fujian Provincial Health Technology Project (2024QNA051, 2024QNA055).
Acknowledgments
We express our sincere gratitude to all the patients and investigators who participated in this study for their valuable contributions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Gong Y, Jiang Q, Zhai M, Tang T, and Liu S. Thyroid cancer trends in China and its comparative analysis with G20 countries: Projections for 2020-2040. J Glob Health. (2024) 14:04131. doi: 10.7189/jogh.14.04131
3. Douglas EH, Rhoads A, Thomas A, Aloi J, Suhl J, Lycan T Jr, et al. Incidence and survival in reproductive-aged women with differentiated thyroid cancer: United States SEER 18 2000-2016. Thyroid. (2020) 30:1781–91. doi: 10.1089/thy.2020.0152
4. Ulisse S, Baldini E, Lauro A, Pironi D, Tripodi D, Lori E, et al. Papillary thyroid cancer prognosis: an evolving field. Cancers (Basel). (2021) 13:5567. doi: 10.3390/cancers13215567
5. Legrand A, Bernier MO, Bressand A, Buffet C, Mandin C, Menegaux F, et al. Health-related quality of life and radioiodine therapy in thyroid cancer patients: a before-and-after study. Qual Life Res. (2024) 33:2721–31. doi: 10.1007/s11136-024-03721-0
6. Kim W, Yu HW, Kim SJ, Chai YJ, Choi JY, and Lee KE. The anterior neck scar outcomes of conventional thyroidectomy using a wound protector: a multicenter double-blinded randomized controlled trial. Int J Surg. (2024) 110:3425–32. doi: 10.1097/JS9.0000000000001288
7. Zhu P, Zhang H, Gu X, Ding Y, Qian M, Wang W, et al. Quality of life in chinese youth following open thyroid surgery: A qualitative study. Cancer Nurs. (2023) 48(5):378–84. doi: 10.1097/NCC.0000000000001314
8. Jongekkasit I, Jitpratoom P, Sasanakietkul T, and Anuwong A. Transoral endoscopic thyroidectomy for thyroid cancer. Endocrinol Metab Clin North Am. (2019) 48:165–80. doi: 10.1016/j.ecl.2018.11.009
9. Zheng D, Yang Q, Wu J, Zhou Z, Cai J, Chen L, et al. Global trends in research of endoscopic thyroidectomy from 2013 to 2022: a scientometric and visualization analysis. Front Endocrinol (Lausanne). (2023) 14:1199563. doi: 10.3389/fendo.2023.1199563
10. Chen YH, Chao WP, Wang SH, Huang YT, and Ng SC. Transoral endoscopic and robotic thyroidectomy for thyroid cancer: the mid-term oncological outcome. Surg Endosc. (2023) 37:7829–38. doi: 10.1007/s00464-023-10339-9
11. Fernandez-Ranvier G, Lieberman B, Guevara D, Voogd A, Matsuda ME, Eck K, et al. Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA) learning curve: a regression analysis of complication rates and severity. Surg Endosc. (2022) 36:4839–44. doi: 10.1007/s00464-021-08832-0
12. Ge JN, Yu ST, Sun BH, Wei ZG, Zhang ZC, Chen WS, et al. A novel anatomy-based five-settlement method for endoscopic thyroid lobectomy and ipsilateral central compartment neck dissection via gasless unilateral axillary approach: a preliminary report. Front Endocrinol (Lausanne). (2023) 14:1147313. doi: 10.3389/fendo.2023.1147313
13. Privitera F, Centonze D, La Vignera S, Condorelli RA, Distefano C, Gioco R, et al. Risk factors for hypoparathyroidism after thyroid surgery: A single-center study. J Clin Med. (2023) 12:1956. doi: 10.3390/jcm12051956
14. Granata R, Zanghì A, Scribano M, Riccioli G, Privitera F, La Vignera S, et al. Incidental parathyroidectomy after thyroid surgery: A single-center study. Biomedicines. (2024) 12:2372. doi: 10.3390/biomedicines12102372
15. Lee MJ, Oh MY, Lee JM, Sun J, and Chai YJ. Comparative surgical outcomes of transoral endoscopic and robotic thyroidectomy for thyroid carcinoma: a propensity score-matched analysis. Surg Endosc. (2023) 37:1132–9. doi: 10.1007/s00464-022-09636-6
16. Lee JH, Choi HJ, Woo JW, and Jung EJ. Robotic versus endoscopic transoral thyroidectomy in papillary thyroid cancer: A comparative analysis of surgical outcomes in 240 consecutive patients. Head Neck. (2023) 45:827–37. doi: 10.1002/hed.27295
17. Choi WK, Shin HY, Park YJ, Lee SH, Lee AY, and Hong JS. Analysis of trends and status of evaluation methods in thyroid scar. Heliyon. (2024) 10:e29301. doi: 10.1016/j.heliyon.2024.e29301
18. Zhang G, Li B, Zhang G, Lin Y, Chen Y, and Gao J. Pros and cons of transoral endoscopic thyroidectomy via vestibular approach: A comparative study. Surg Laparosc Endosc Percutan Tech. (2020) 31:331–6. doi: 10.1097/SLE.0000000000000875
19. Changchien TC, Yen YC, and Lu YC. Mental health and quality of life of patients with differentiated thyroid cancer pre and post radioactive iodine treatment: A prospective study. J Clin Med. (2024) 13:5472. doi: 10.3390/jcm13185472
20. Winter J, Axelsson E, Björkhem-Bergman L, Ihre Lundgren C, and Hedman C. Five-year follow-up of health-related quality of life in differentiated thyroid cancer patients treated with total thyroidectomy and radioiodine in Sweden: A nationwide prospective cohort study. Thyroid. (2024) 34:713–22. doi: 10.1089/thy.2023.0691
21. Watt T, Christoffersen T, Brogaard MB, Bjorner JB, Bentzen J, Hahn CH, et al. Quality of life in thyroid cancer. Best Pract Res Clin Endocrinol Metab. (2023) 37:101732. doi: 10.1016/j.beem.2023.101732
22. Liu Z, Li Y, Wang Y, Xiang C, Yu X, Zhang M, et al. Comparison of the transoral endoscopic thyroidectomy vestibular approach and open thyroidectomy: A propensity score-matched analysis of surgical outcomes and safety in the treatment of papillary thyroid carcinoma. Surgery. (2021) 170:1680–6. doi: 10.1016/j.surg.2021.06.032
23. Lira RB, De Cicco R, Rangel LG, Bertelli AA, Duque Silva G, de Medeiros Vanderlei JP, et al. Transoral endoscopic thyroidectomy vestibular approach: Experience from a multicenter national group with 412 patients. Head Neck. (2021) 43:3468–75. doi: 10.1002/hed.26846
24. Piromchai P. Comparison of quality of life between patients undergoing submental endoscopic thyroidectomy and conventional thyroidectomy: A prospective controlled clinical trial. J Clin Med. (2022) 11:4802. doi: 10.3390/jcm11164802
25. Dabsha A, Khairallah S, Elkharbotly I, Hossam E, Hanafy A, Kamel M, et al. Learning curve and volume outcome relationship of endoscopic trans-oral versus trans-axillary thyroidectomy; A systematic review and meta-analysis. Int J Surg. (2022) 104:106739. doi: 10.1016/j.ijsu.2022.106739
26. Lira RB, Ramos AT, Nogueira R, de Carvalho GB, Russell JO, Tufano RP, et al. Transoral thyroidectomy (TOETVA): Complications, surgical time and learning curve. Oral Oncol. (2020) 110:104871. doi: 10.1016/j.oraloncology.2020.104871
27. Razavi CR, Vasiliou E, Tufano RP, and Russell JO. Learning curve for transoral endoscopic thyroid lobectomy. Otolaryngol Head Neck Surg. (2018) 159:625–9. doi: 10.1177/0194599818795881
28. Wang D, Wang Y, Zhou S, Liu X, Wei T, Zhu J, et al. Transoral thyroidectomy vestibular approach versus non-transoral endoscopic thyroidectomy: a comprehensive systematic review and meta-analysis. Surg Endosc. (2022) 36:1739–49. doi: 10.1007/s00464-021-08836-w
29. Wang Y, Zhou S, Liu X, Rui S, Li Z, Zhu J, et al. Transoral endoscopic thyroidectomy vestibular approach vs conventional open thyroidectomy: Meta-analysis. Head Neck. (2021) 43:345–53. doi: 10.1002/hed.26486
30. Oh MY, Chai YJ, Yu HW, Kim SJ, Choi JY, and Lee KE. Transoral endoscopic thyroidectomy vestibular approach as a safe and feasible alternative to open thyroidectomy: a systematic review and meta-analysis. Int J Surg. (2023) 109:2467–77. doi: 10.1097/JS9.0000000000000444
31. Guidolin K, Spence RT, Azin A, Hirpara DH, Lam-Tin-Cheung K, Quereshy F, et al. The effect of operative duration on the outcome of colon cancer procedures. Surg Endosc. (2022) 36:5076–83. doi: 10.1007/s00464-021-08871-7
32. Russell JO, Razavi CR, Shaear M, Liu RH, Chen LW, Pace-Asciak P, et al. Transoral thyroidectomy: safety and outcomes of 200 consecutive North American cases. World J Surg. (2021) 45:774–81. doi: 10.1007/s00268-020-05874-8
33. Arikan M, Riss P, and European TOETVA Study Group. Transoral thyroidectomy: initial results of the European TOETVA study group. World J Surg. (2023) 47:1201–8. doi: 10.1007/s00268-023-06932-7
34. Li SL, Du P, Lv T, Lu DN, Shao CY, Zhang YN, et al. Quantitative comparison of three thyroidectomy approaches in neck muscles, voice, and swallowing functions. Asian J Surg. (2024) 47:1734–9. doi: 10.1016/j.asjsur.2023.12.085
35. Zhang X, Yu J, Zhu J, Wei H, Meng N, Hu M, et al. A meta-analysis of unilateral axillary approach for robotic surgery compared with open surgery for differentiated thyroid carcinoma. PloS One. (2024) 19:e0298153. doi: 10.1371/journal.pone.0298153
36. Xin Y, Yang L, Xie Q, Li D, Tian Z, Li Y, et al. Clinical factors influencing postoperative drainage volume in papillary thyroid carcinoma: A retrospective analysis. Curr Probl Surg. (2025) 68:101776. doi: 10.1016/j.cpsurg.2025.101776
37. ÜnlÜ MT, Aygun N, Serin E, and Uludag M. Comparison of transoral endoscopic thyroidectomy vestibular approach and open conventional thyroidectomy regarddec inflammatory responses, pain, and patient satisfaction: a prospective study. Front Surg. (2023) 10:1281093. doi: 10.3389/fsurg.2023.1281093
38. Wirtz DC, Heller KD, Miltner O, Zilkens KW, and Wolff JM. Interleukin-6: a potential inflammatory marker after total joint replacement. Int Orthop. (2000) 24:194–6. doi: 10.1007/s002640000136
39. Roch PJ, Ecker C, Jäckle K, Meier MP, Reinhold M, Klockner FS, et al. Interleukin-6 as a critical inflammatory marker for early diagnosis of surgical site infection after spine surgery. Infection. (2024) 52:2269–77. doi: 10.1007/s15010-024-02271-4
40. Tae K, Ji YB, Song CM, and Ryu J. Robotic and endoscopic thyroid surgery: evolution and advances. Clin Exp Otorhinolaryngol. (2019) 12:1–11. doi: 10.21053/ceo.2018.00766
41. Yu ST, Ge JN, Sun BH, Wei ZG, Zhang ZC, Chen WS, et al. A modified, single-incision, gasless, endoscopic thyroidectomy and bilateral central neck dissection via axillary approach technique for bilateral papillary thyroid microcarcinoma: A preliminary report. Heliyon. (2024) 10:e24802. doi: 10.1016/j.heliyon.2024.e24802
42. Kim EY, Lee KH, Park YL, Park CH, Lee CR, Jeong JJ, et al. Single-incision, gasless, endoscopic trans-axillary total thyroidectomy: A feasible and oncologic safe surgery in patients with papillary thyroid carcinoma. J Laparoendosc Adv Surg Tech A. (2017) 27:1158–64. doi: 10.1089/lap.2016.0669
43. Sung ES, Ji YB, Song CM, Yun BR, Chung WS, and Tae K. Robotic thyroidectomy: comparison of a postauricular facelift approach with a gasless unilateral axillary approach. Otolaryngol Head Neck Surg. (2016) 154:997–1004. doi: 10.1177/0194599816636366
44. Yan X, Zhu C, Wu W, Geng X, Ding Y, and Li Y. Transoral endoscopic thyroidectomy vestibular approach for papillary thyroid microcarcinoma: an analysis of clinical outcomes. Am J Transl Res. (2022) 14:7907–15. doi: 10.62347/JOTR145173
45. Mirghani HO and Albalawi IA. A comparison between transoral endoscopic thyroidectomy vestibular approach and transareolar thyroidectomy regarding postoperative pain and cosmetic outcomes: A systematic review and meta-analysis. Pak J Med Sci. (2024) 40:2726–31. doi: 10.12669/pjms.40.11.9712
46. Sun Y, Zhou S, and Zhou G. Safety and cosmesis of gasless endoscopic thyroidectomy: a retrospective study. Updates Surg. (2024) 76:1955–62. doi: 10.1007/s13304-024-01938-9
47. Magnoni F, Galimberti V, Corso G, Intra M, Sacchini V, and Veronesi P. Axillary surgery in breast cancer: An updated historical perspective. Semin Oncol. (2020) 47:341–52. doi: 10.1053/j.seminoncol.2020.09.001
48. Xu T, Qin X, Zhang Y, Li P, Ran Y, Fan Y, et al. A prospective study comparing the gasless endoscopic thyroidectomy trans-axillary approach to conventional open thyroidectomy: health and quality of life outcomes. Surg Endosc. (2024) 38:1995–2009. doi: 10.1007/s00464-024-10689-y
49. Huang JK, Ma L, Song WH, Lu BY, Huang YB, and Dong HM. Quality of life and cosmetic result of single-port access endoscopic thyroidectomy via axillary approach in patients with papillary thyroid carcinoma. Onco Targets Ther. (2016) 9:4053–9. doi: 10.2147/OTT.S99980
50. Altedlawi Albalawi IA and Mirghani HO. The quality of life after trans oral video-assisted thyroidectomy and cervical thyroidectomy: a systematic review and meta-analysis. Front Surg. (2023) 10:1116473. doi: 10.3389/fsurg.2023.1116473
Keywords: thyroid cancer, transoral endoscopic thyroidectomy vestibular approach, gasless unilateral axillary endoscopic thyroidectomy, open thyroidectomy, wound satisfaction, quality of life
Citation: Bian C, Lin Z, Yan M, Weng S, Xie C, Pan W, Huang C and Fang G (2025) Comparative short- and long-term outcomes of TOETVA, ETGUA, and COT in thyroid cancer: a propensity score-matched study. Front. Oncol. 15:1606568. doi: 10.3389/fonc.2025.1606568
Received: 05 April 2025; Accepted: 22 September 2025;
Published: 08 October 2025.
Edited by:
Erika Crosetti, San Giovanni Bosco Hospital, ItalyReviewed by:
Rafael De Cicco, Doctor Arnaldo Cancer Institute, BrazilHasan Zafer Acar, Girne American University, Cyprus
Copyright © 2025 Bian, Lin, Yan, Weng, Xie, Pan, Huang and Fang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guiren Fang, MTM1MDkzOTIzMjRAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Cong Bian
Cong Bian Zhenmeng Lin
Zhenmeng Lin Mingfang Yan
Mingfang Yan Shaokun Weng3
Shaokun Weng3