- 1Department of Clinical Pharmacy, College of Pharmacy, King Khalid University, Abha, Saudi Arabia
- 2Department of Clinical Pharmacy, College of Pharmacy, Shaqra University, Dawadimi, Saudi Arabia
Background: Cervical cancer, mainly caused by Human Papillomavirus infection, is a growing public health concern in Saudi Arabia. Despite the availability of effective vaccination and screening programs in the country, awareness and acceptance remain limited, particularly among women in the Asir region. This study aimed to assess knowledge and attitudes toward Human Papillomavirus and cervical cancer prevention among women in the Asir region, Saudi Arabia.
Methods: A cross-sectional study was conducted from January to March 2025 among women aged 18 and older in the Asir region of Saudi Arabia. A convenience sampling method was used to recruit participants. Data were collected through an online self-administered questionnaire, and multivariable logistic regression was performed to identify factors associated with knowledge and attitudes (p < 0.05).
Results: Among the 523 participants, 66% demonstrated good knowledge of Human Papillomavirus and cervical cancer prevention, while 56% had positive attitudes. Awareness of Human Papillomavirus and the Human Papillomavirus vaccine was observed in 62.1% and 54% of women, respectively, while knowledge of screening tests remained limited at 32.7%. Only 21% of women reported being vaccinated against Human Papillomavirus. The main barriers discouraging women from practicing Pap tests were discomfort (65.4%) and lack of knowledge (63.7%). Factors significantly associated with lower odds of having good knowledge (Adjusted Odds Ratio, AOR) included older age (41–50 years: AOR = 0.479, 95% confidence interval (CI): 0.239–0.961; 51–60 years: AOR = 0.239, 95% CI: 0.113–0.505; >60 years: AOR = 0.127, 95% CI: 0.022–0.724), lower education (secondary school: AOR = 0.483, 95% CI: 0.305–0.764), and unmarried status (single: AOR = 0.562, 95% CI: 0.327–0.965; divorced/widowed: AOR = 0.413, 95% CI: 0.218–0.784). Negative attitudes were more prevalent among older women (41–50 years: AOR = 0.327, 95% CI: 0.170–0.629; 51–60 years: AOR = 0.272, 95% CI: 0.130–0.570; >60 years: AOR = 0.102, 95% CI: 0.012–0.876).
Conclusion: The study demonstrated generally good knowledge and positive attitudes toward Human Papillomavirus vaccination and cervical cancer prevention among women in the Asir region; however, awareness of screening and vaccine uptake was suboptimal. Women who were older, less educated, or unmarried had lower knowledge and more negative attitudes. Targeted educational interventions through healthcare providers, school-based programs, and social media, along with improved healthcare access, are recommended to enhance awareness, encourage regular cervical cancer screening, and reduce disease burden.
1 Introduction
Cervical cancer (CC) is one of the most common gynecological cancers worldwide and a major public health concern, with over 600,000 new cases and 340,000 deaths reported globally in 2020, predominantly affecting women aged 30–49 years (1). Persistent infection with high-risk human papillomavirus (HPV), particularly types 16 and 18, accounts for the majority of cases worldwide (2). Despite the availability of effective vaccination and screening programs globally, awareness and uptake remain suboptimal in many regions. Globally, HPV vaccination and cervical cancer screening have shown substantial benefits in reducing incidence and mortality. However, knowledge gaps and limited uptake persist in many populations, especially among adolescents and young adults, who are ideal candidates for prophylactic vaccination (3, 4). Parental willingness to vaccinate children also significantly influences vaccine coverage (5–9). In Saudi Arabia, CC is the third most prevalent gynecological cancer, following ovarian and uterine cancers (10), and ranks as the ninth most common cancer among women, with an annual incidence of 358 new cases, predominantly affecting women aged 40–49 years (11). Persistent infection with HPV remains the primary cause, with types 16 and 18 accounting for 76% of cases both nationally and globally (11, 12). The age-standardized incidence rate (ASIR) of invasive cervical cancer among Saudi women rose from 1.23 per 100,000 in 2005–2009 to 2.45 per 100,000 in 2015–2019, with intermediate rates around 2.7 per 100,000 during 2010–2014 (13, 14). Although the age-standardized mortality rate (ASMR) remains low, continuous monitoring is warranted given the rising incidence.
This incidence is considerably lower than global averages (~14.1 per 100,000 women) but similar to neighboring Gulf countries such as Kuwait (4.8), the United Arab Emirates (5.4), and Qatar (6.8), where cervical cancer also ranks among the least common malignancies (15). However, despite this relatively low burden compared with international levels, the preventable nature of the disease and the rising trend in Saudi Arabia underscore the importance of strengthening preventive strategies. Nationwide studies highlight limited awareness and preventive behaviors. Between September and November 2023, cervical cancer screening prevalence was 22.1%, with 42.4% citing the lack of a physician’s recommendation as the primary barrier. Only 7.6% of participants had received the HPV vaccine, and over 84% demonstrated low knowledge about cervical cancer (16). Another survey across multiple regions found that while 84% of women were aware of cervical cancer, only 8% had ever undergone screening. Awareness of HPV transmission, genital warts, and its link to cervical cancer was below 20%, and only 2.0% had received the HPV vaccine despite 17.7% having heard about it (17).
The Asir region has distinctive demographic and healthcare characteristics compared to other parts of Saudi Arabia. Its largely rural and mountainous geography and uneven distribution of healthcare facilities limit access to specialized gynecological and preventive services compared to major urban centers such as Riyadh and Jeddah (18). Regional studies indicate low awareness and uptake of women’s health preventive measures in Asir, including cervical cancer and breast cancer screening (19, 20). Less than half of women in the Southern Region, which includes Asir, were aware of cervical cancer, and knowledge of HPV as a causal factor was particularly low (20). A recent survey in Asir also found substantial misconceptions about cervical cancer and limited awareness of HPV vaccination (21). These findings highlight regional disparities that may affect nationwide prevention programs, and this study provides the first comprehensive assessment of knowledge and attitudes toward HPV and cervical cancer prevention among women in Asir. In Saudi Arabia, cervical cancer screening is primarily opportunistic rather than population-based. The Ministry of Health recommends Pap smear and high-risk HPV testing for women aged 21–65, with screening intervals of every three years for those aged 21–29 and every five years for those aged 30–65 (22). The HPV vaccination schedule includes one- or two-dose regimens for girls aged 9–14 and young women aged 15–20, and two doses with a six-month interval for women over 21. The HPV vaccination program, initiated in 2008, targets girls aged 9–26 and boys aged 9–21 (22, 23).
The World Health Organization (WHO) recommends the HPV vaccine for females aged 9–14, as most individuals in this age group have not yet initiated sexual activity, and sexual contact is the primary mode of HPV transmission (24). The Advisory Committee on Immunization Practices (ACIP) recommends routine HPV vaccination for males at ages 11 and 12, alongside girls, with vaccination beginning as early as age 9. For older adolescents and young adults who were not adequately vaccinated at younger ages, the vaccine is recommended up to age 21 for males and up to age 26 for females (25, 26). In March 2022, the Saudi Ministry of Health incorporated the HPV vaccine into the Saudi Immunization Schedule through a school-based program targeting seventh-grade girls in collaboration with the Ministry of Education (27). Additionally, in September 2022, the vaccine became available for females aged 9–18 upon request through primary healthcare centers (27). Parental decision-making is crucial in adolescent vaccine uptake, influencing the success of these programs (28).
The Health Belief Model (HBM) is a widely used framework for understanding health behavior change and explains the underutilization of screening and preventive interventions for asymptomatic diseases. Its key constructs include perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and cues to action (29, 30). Educating women about vaccination benefits and addressing barriers is essential to enhance cervical cancer prevention. While several studies have examined HPV knowledge and attitudes in Saudi Arabia, data from the Asir region remain limited. Therefore, this study aimed to assess the knowledge and attitudes toward HPV and cervical cancer prevention among women in the Asir region. Understanding these factors is critical for designing effective public health interventions and policies to improve vaccine uptake and reduce the burden of cervical cancer. The findings will inform healthcare strategies aimed at increasing awareness and addressing barriers to HPV vaccination, supporting national efforts to reduce cervical cancer incidence.
2 Methods and materials
2.1 Study setting, design, and period
A cross-sectional study was conducted among women aged 18 years and older residing in the Asir region of Saudi Arabia from January to March 2025.
2.2 Sample size determination
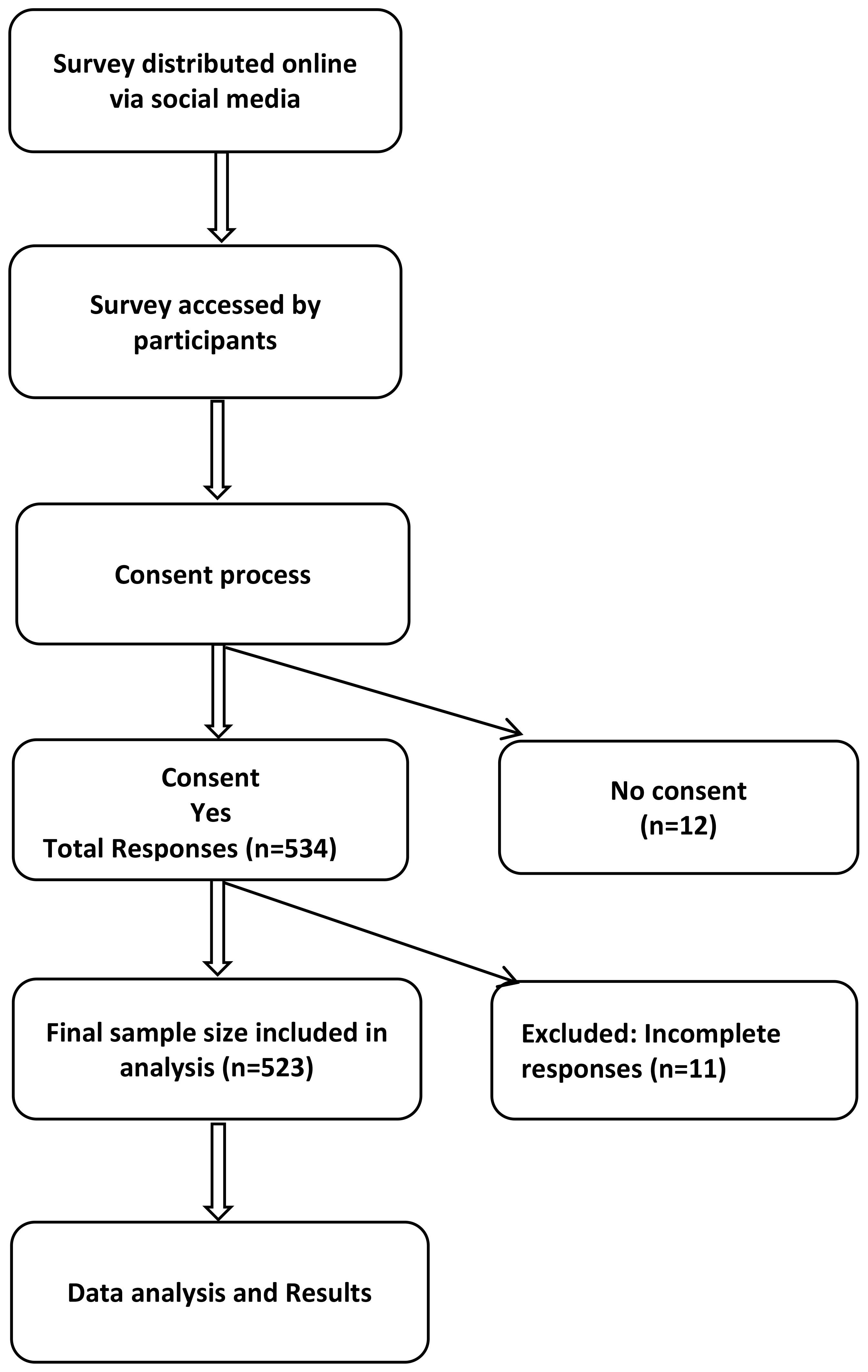
The minimum required sample size was calculated using the Raosoft online sample size calculator (Raosoft Inc., Seattle, WA, USA) (31). Considering the estimated female population of 635,234 in the Asir region (General Authority for Statistics, 2022) (32), with a 95% confidence level, 5% margin of error, and an assumed response distribution of 50%, the required sample size was 384 participants. To improve the precision and reliability of the findings, recruitment continued beyond this minimum requirement. After applying the exclusion criteria (12 participants who did not provide consent and 11 with incomplete responses), the final sample analyzed included 523 participants.
2.3 Study population and sampling procedure
Participants were eligible if they were women aged 18 years or older, residents of the Asir region, and willing to provide online consent. Women younger than 18 years, non-residents of the Asir region, or those who submitted incomplete survey responses were excluded from the study. Participants were recruited online using a convenience sampling method (Figure 1).
2.4 Data collection
Data were collected using an online self-reported questionnaire distributed via social media platforms, including X and WhatsApp (survey link: https://forms.gle/7vgFXaBNNq17p8VF6; accessed March 2, 2025). To accommodate the local population, the survey was made available in Arabic. Staff and students from King Khalid University assisted with distribution through targeted messages and posts, and outreach was also conducted at physical locations such as health clinics, universities, community centers, pharmacies, malls, parks, and religious centers using QR codes and posters to ensure broader participation. To minimize duplicate responses, the survey was configured to allow only one submission per device.
A standardized, self-administered questionnaire was developed to assess knowledge and attitudes regarding HPV, the HPV vaccine, and CC, based on previous literature (33–36). It was developed in English, translated into Arabic by bilingual experts, back-translated for accuracy, and reviewed by subject matter experts for cultural relevance and clarity. A pilot study with 50 participants assessed clarity and reliability, yielding a Cronbach’s alpha of 0.854, indicating good internal consistency. The questionnaire consisted of three sections. Section 1 collected sociodemographic data, including age, marital status, education (categorized according to the Saudi system: secondary school (grades 7–9), high school (grades 10–12), graduate (post-secondary or university), and uneducated), and employment status. Section 2: Knowledge was assessed using 10 scored questions and 2 qualitative items (Questions 11 and 12), which were not scored. Each correct answer was awarded 1 point, with a maximum possible knowledge score of 19. Questions 1–6, 9, and 10 were single-response items (yes/no or multiple-choice with one correct answer). Question 7 included 6 multiple-response items, and Question 8 included 5 multiple-response items, with each correct response receiving 1 point. Participants scoring ≥50% of the maximum were classified as having good knowledge, while those scoring <50% were classified as having poor knowledge.
Section 3 evaluated participants’ attitudes were evaluated using nine items. Questions 1–3 were single-response yes/no items, Questions 5–6 were single-response multiple-choice items (participants selected one option from several possible responses), and Questions 7–9 were single-response items with three options (Yes/No/Not sure). Each scored item was assigned 1 point for a response indicative of a positive attitude, yielding a maximum attitude score of 8. Question 4 was qualitative, assessing barriers to Pap test participation, and was not included in the scoring. Participants with scores ≥50% were classified as having a positive attitude, while those scoring <50% were classified as having a negative attitude. Question 3 assessed HPV vaccination history (for participants aged 9–26 years) and willingness to vaccinate daughters (restricted to participants with at least one daughter).
2.5 Variables
The study included both independent and dependent variables. The independent variables were demographic characteristics, including age, marital status, education level, and employment status. The dependent variables were participants’ knowledge and attitudes regarding HPV and cervical cancer prevention. Operational definitions: Women scoring ≥50% of the maximum were classified as having good knowledge or a positive attitude, while those scoring <50% were classified as having poor knowledge or a negative attitude, consistent with previous studies (37).
2.6 Statistical analysis
The survey responses collected through Google Forms were exported into Microsoft Excel and subsequently imported into SPSS for analysis. The data were cleaned, coded, and analyzed using SPSS version 18. Descriptive statistics were presented as frequencies and percentages for categorical variables. Multivariable logistic regression analysis was conducted to identify factors associated with knowledge and attitudes regarding HPV and CC prevention. Independent variables included demographic characteristics (age, employment status, education level, marital status), while dependent variables were categorized as good or poor knowledge and positive or negative attitudes. Adjusted odds ratios (AOR) with 95% confidence intervals (CI) were calculated to assess associations, and a p-value of <0.05 was considered statistically significant.
2.7 Ethical approval
Ethical approval was granted by the Institutional Review Board (IRB) of King Khalid University (ECM ≠2025-116). Participants were recruited online, and only those who provided consent were included. Confidentiality was emphasized throughout the recruitment process, and participation remained entirely voluntary. Upon clicking the survey link, participants were directed to the first page of the questionnaire on Google Forms, where they were presented with a consent form outlining the study’s objectives, voluntary participation, and confidentiality measures. Participants indicated their willingness to participate by selecting “Yes” or declined by selecting “No.” Those who declined were automatically redirected away from the questionnaire. Informed consent was therefore obtained online through this mandatory process. All data were securely stored in a password-protected database, accessible only to the principal investigator and authorized research team members, and anonymity was maintained by not collecting personally identifiable information.
3 Results
3.1 Demographics
Of the 523 women, the mean age was 34.7 ± 11.2 years, with a median of 32 years and an interquartile range (IQR) of 25–43 years. The majority were aged 18–30 years (222, 42.4%), followed by those aged 31–40 years (123, 23.5%) and 41–50 years (114, 21.8%). Participants aged 51–60 years were 56 (10.7%), while only 8 (1.5%) were above 60 years of age. Regarding employment status, 197 (37.7%) participants were employed, and 326 (62.3%) were unemployed. In terms of educational attainment, most had a graduate-level education 358 (68.5%), followed by 126 (24.1%) with secondary school education and 26 (4.9%) who completed high school. A small proportion, 13 (2.5%), were uneducated. As for marital status, 249 (47.6%) participants were single, 220 (42.1%) were married, and 54 (10.3%) were either divorced or widowed (Table 1).
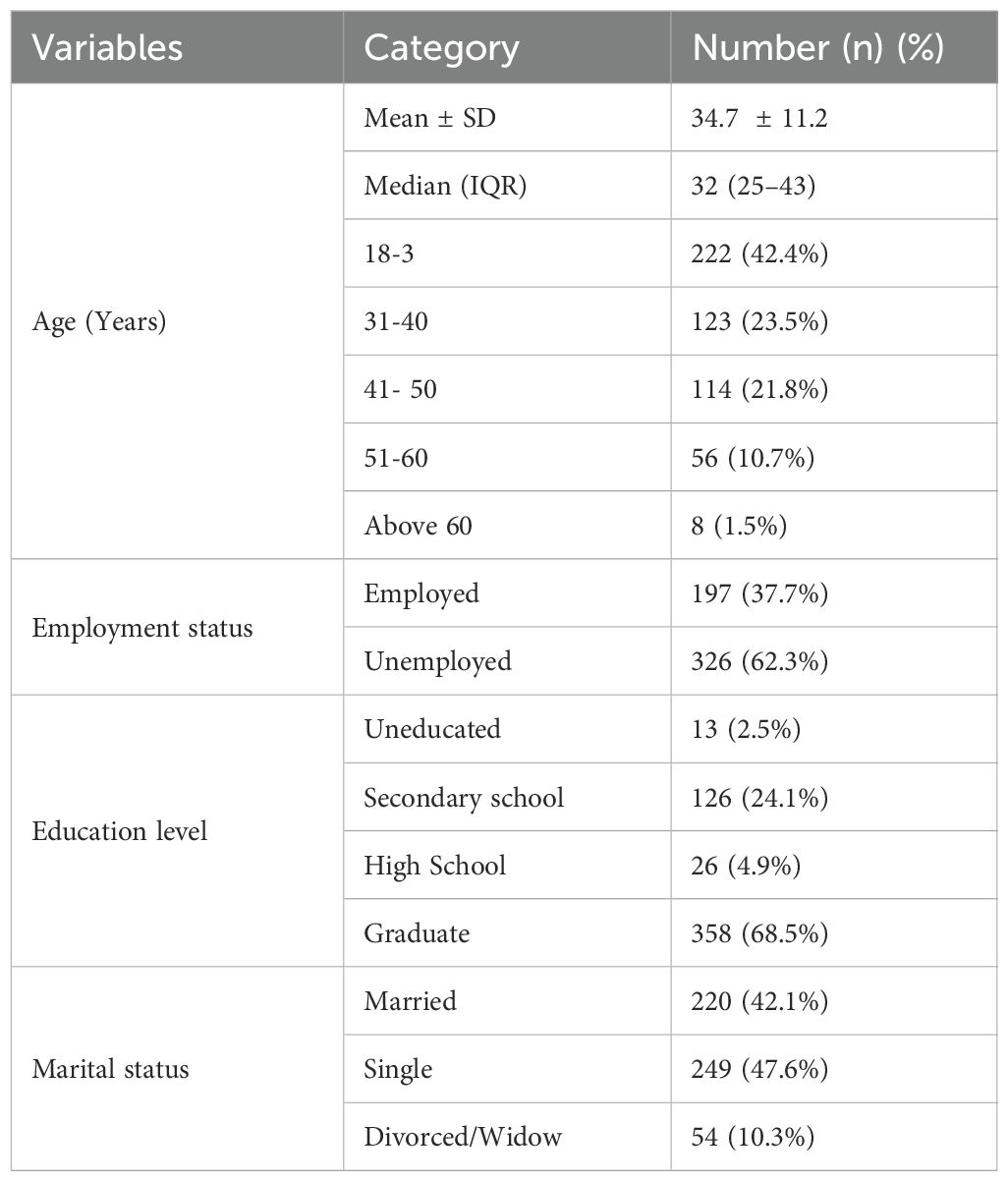
Table 1. Sociodemographic characteristics of study participants in the Asir Region, Saudi Arabia (n = 523).
3.2 Knowledge and attitudes
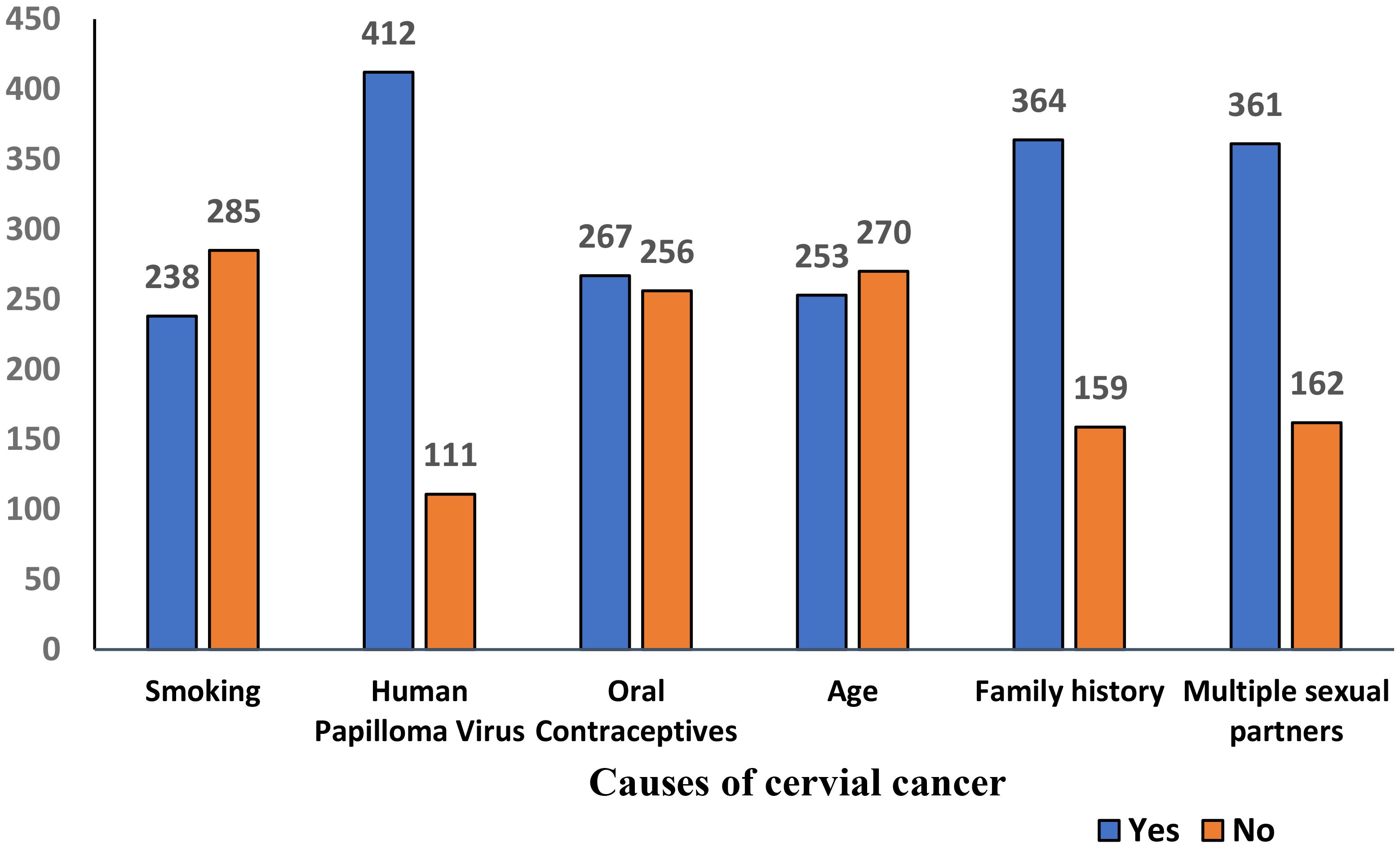
Based on the predefined threshold of ≥50% of the maximum score (as described in the Methods), participants scoring ≥50% were classified as having good knowledge or a positive attitude, while those scoring below 50% were considered to have poor knowledge or a negative attitude. Good knowledge was demonstrated by 347 (66%) women, while 176 (34%) had poor knowledge. Positive attitudes were observed in 292 (56%) women, while 231 (44%) had negative attitudes (Table 2, Figure 2). Awareness of HPV was reported by 325 (62.1%) women, while 282 (54%) were aware of the HPV vaccine. Knowledge of screening tests for cervical cancer was limited, with only 171 (32.7%) aware of them. A majority 385 (68.5%) believed cervical cancer is preventable, while 138 (26.4%) disagreed. Awareness of the Pap smear test was reported by 241 (46.1%) women Regarding perceived causes of cervical cancer, 412 (78.8%) correctly identified HPV, while substantial proportions also reported family history 364 (69.6%) and multiple sexual partners 361 (69.0%) as risk factors. Other reported causes included smoking 238 (45.5%), oral contraceptives 267 (51.0%), and increasing age 253 (48.4%) (Figure 3). When asked about signs and symptoms of cervical cancer, most participants recognized pelvic pain or pain during intercourse 410 (78.4%), postcoital or intermenstrual vaginal bleeding 403 (77.1%), and foul-smelling watery or bloody vaginal discharge 368 (70.4%). Weight loss 304 (58.1%) and dyspareunia 373 (71.3%) were less frequently reported but still noted by more than half of the respondents. (Table 3, Figure 4). Regarding vaccination attitudes, 404 (77.2%) believed that women vaccinated against HPV still need a Pap test; however, only 110 (21%) were vaccinated against HPV. Among participants with at least one daughter (n=253), 180 (71.1%) expressed willingness to vaccinate their daughters, while 73 (28.9%) were not willing (Table 4).
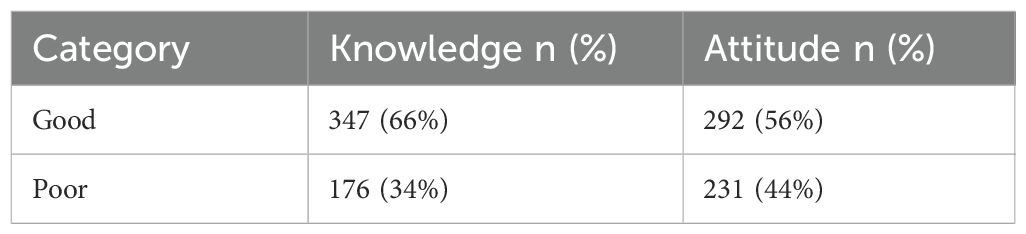
Table 2. Scores of knowledge and attitudes toward human papillomavirus (HPV) and cervical cancer among women in the Asir Region, Saudi Arabia (n = 523).
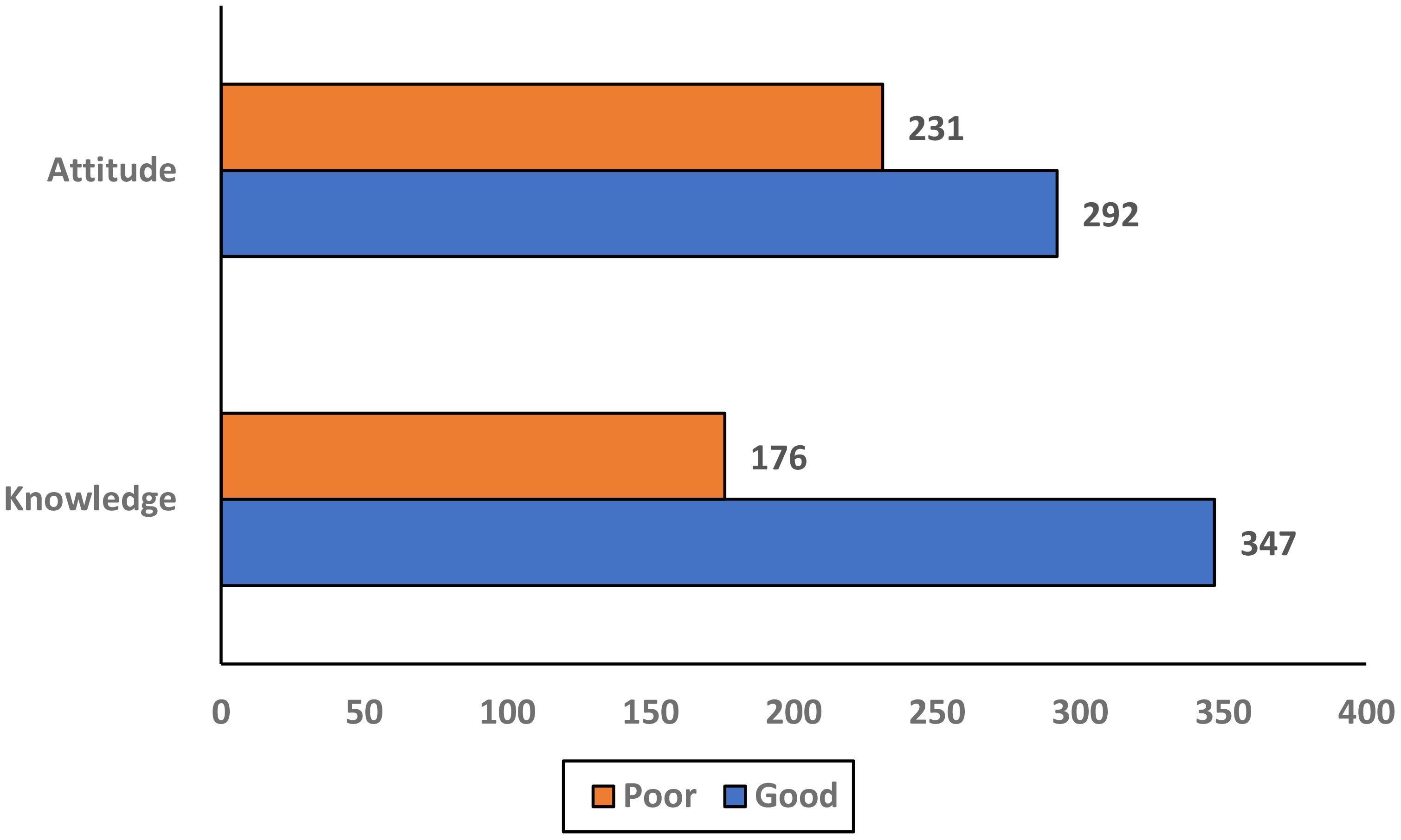
Figure 2. Scores of knowledge and attitudes toward human papillomavirus (HPV) and cervical cancer among women in the Asir Region, Saudi Arabia (n = 523).
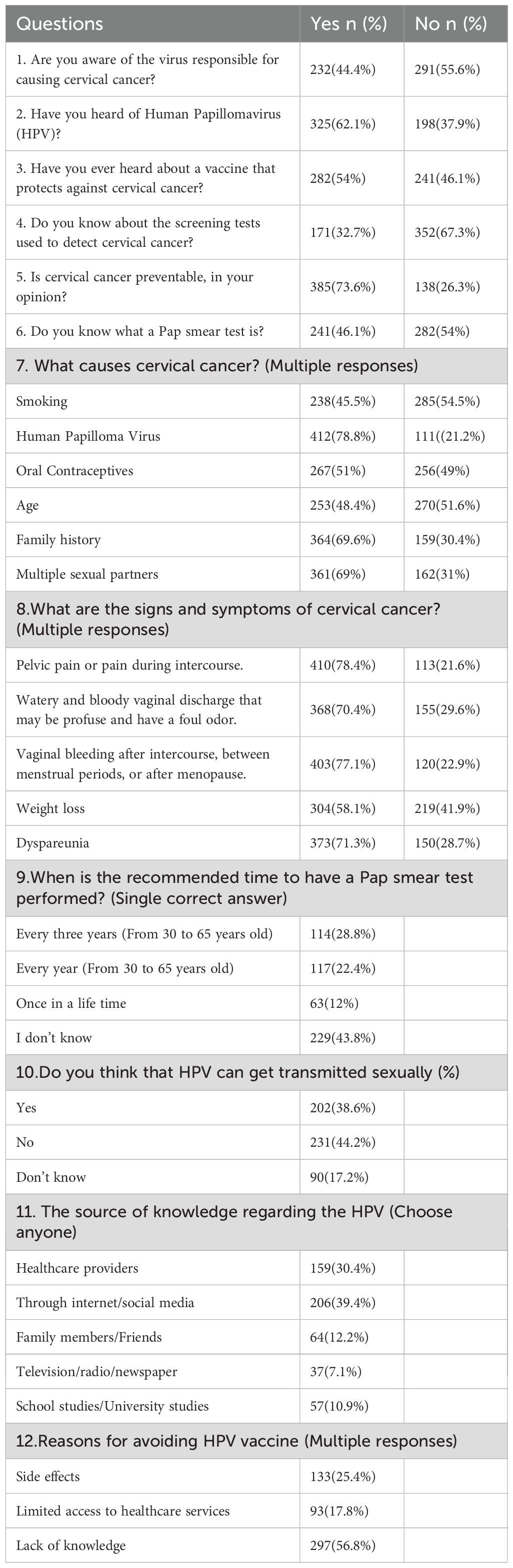
Table 3. Knowledge of human papillomavirus (HPV) and cervical cancer prevention among women in the Asir Region, Saudi Arabia (n = 523).
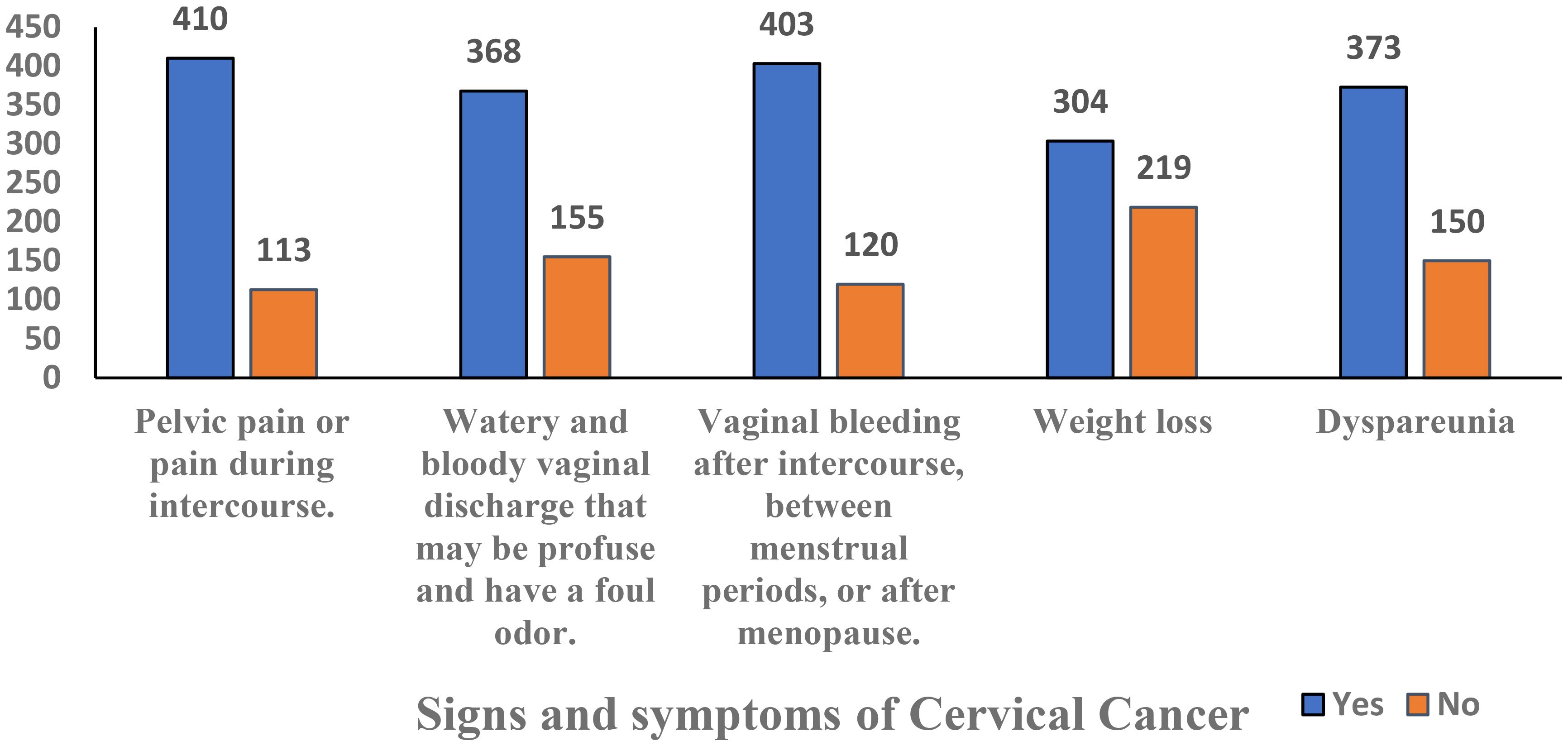
Figure 4. Signs and symptoms of cervical cancer prevention among women in the Asir Region, Saudi Arabia (n = 523).
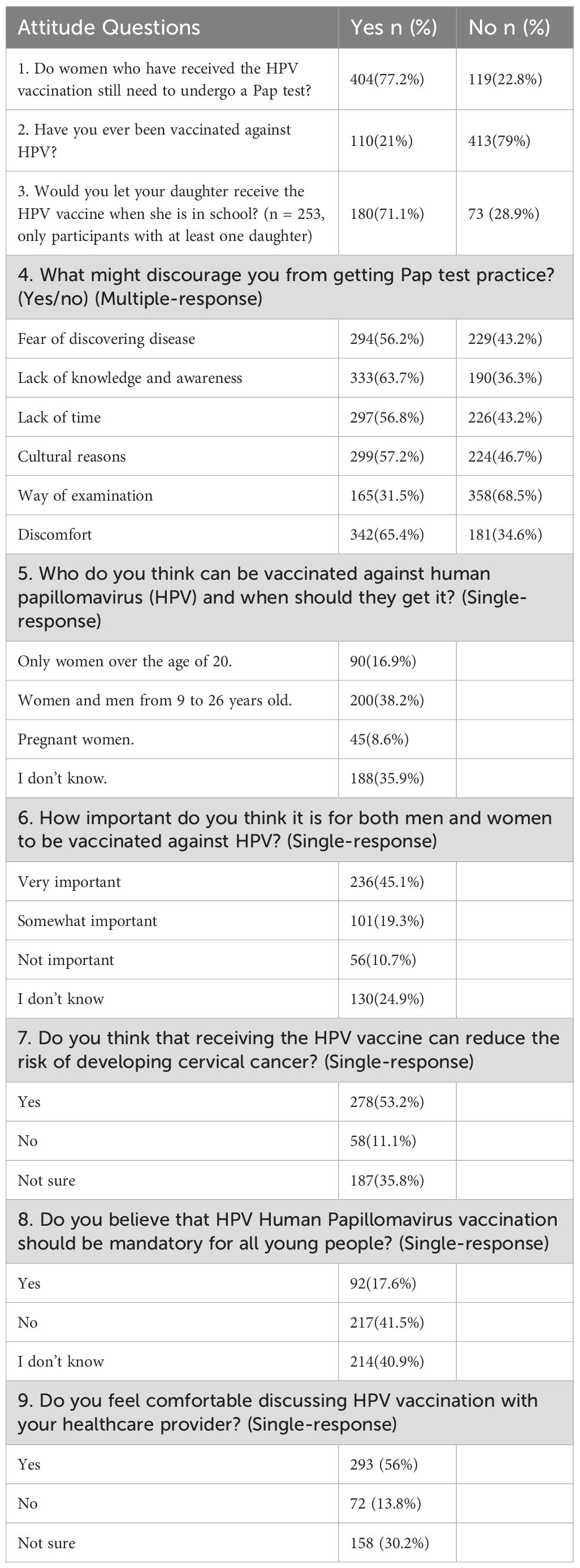
Table 4. Attitudes regarding human papillomavirus (HPV) vaccination and cervical cancer prevention among women in the Asir Region, Saudi Arabia (n = 523).
3.3 Barriers and sources of information
The most common sources of knowledge were the internet/social media 206 (39.4%), and healthcare providers 159 (30.4%) (Table 3, Figure 5). Discomfort 342 (65.4%) and lack of awareness 333 (63.7%) were the main barriers to Pap test practice (Table 4, Figure 6). In this study, discomfort was defined as both physical and emotional unease associated with undergoing a Pap test, encompassing physical pain, embarrassment, and anxiety related to the intimate nature of the procedure.
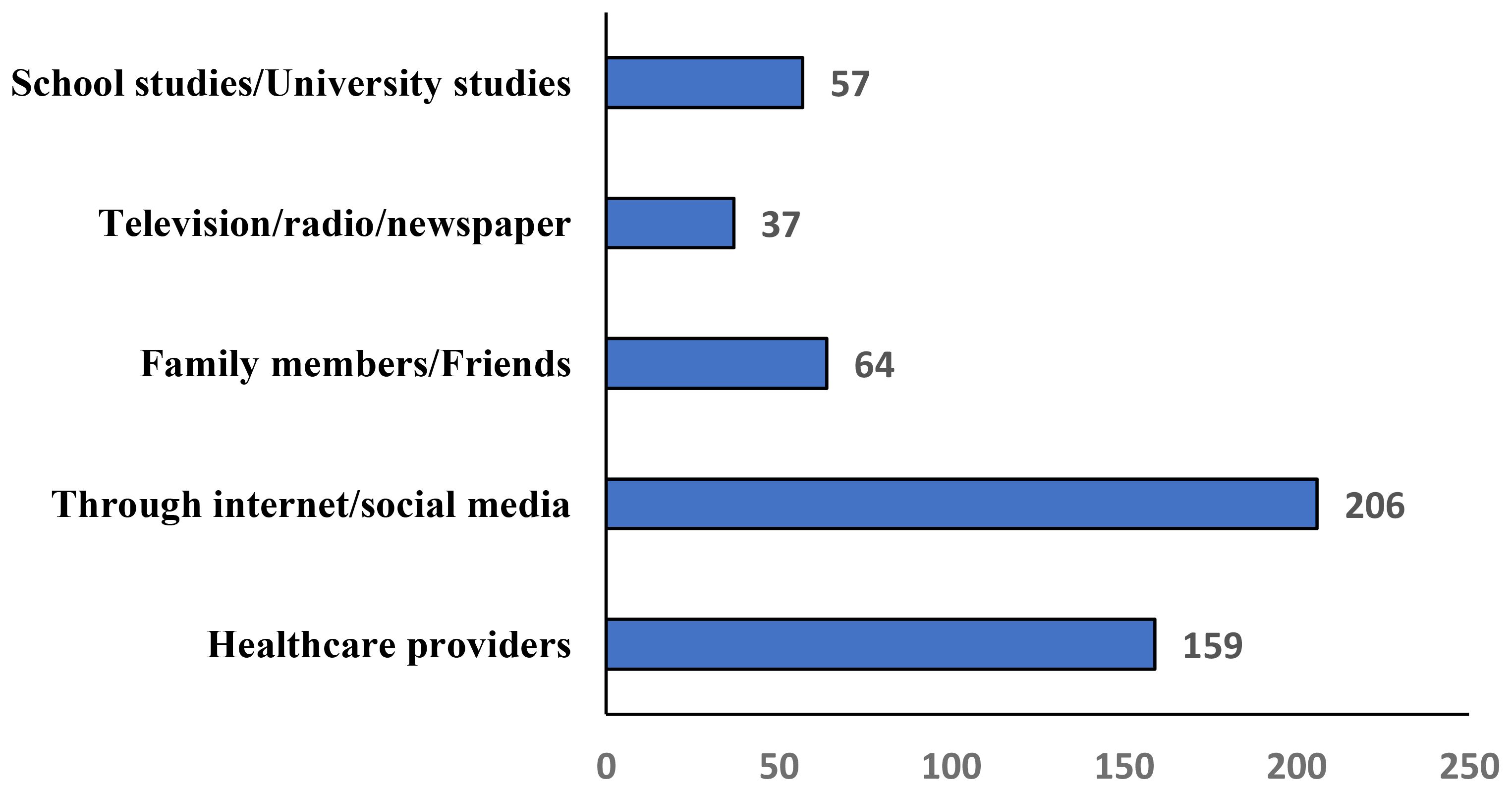
Figure 5. Sources of knowledge regarding human papillomavirus (HPV) and cervical cancer prevention among women in the Asir Region, Saudi Arabia (n = 523).
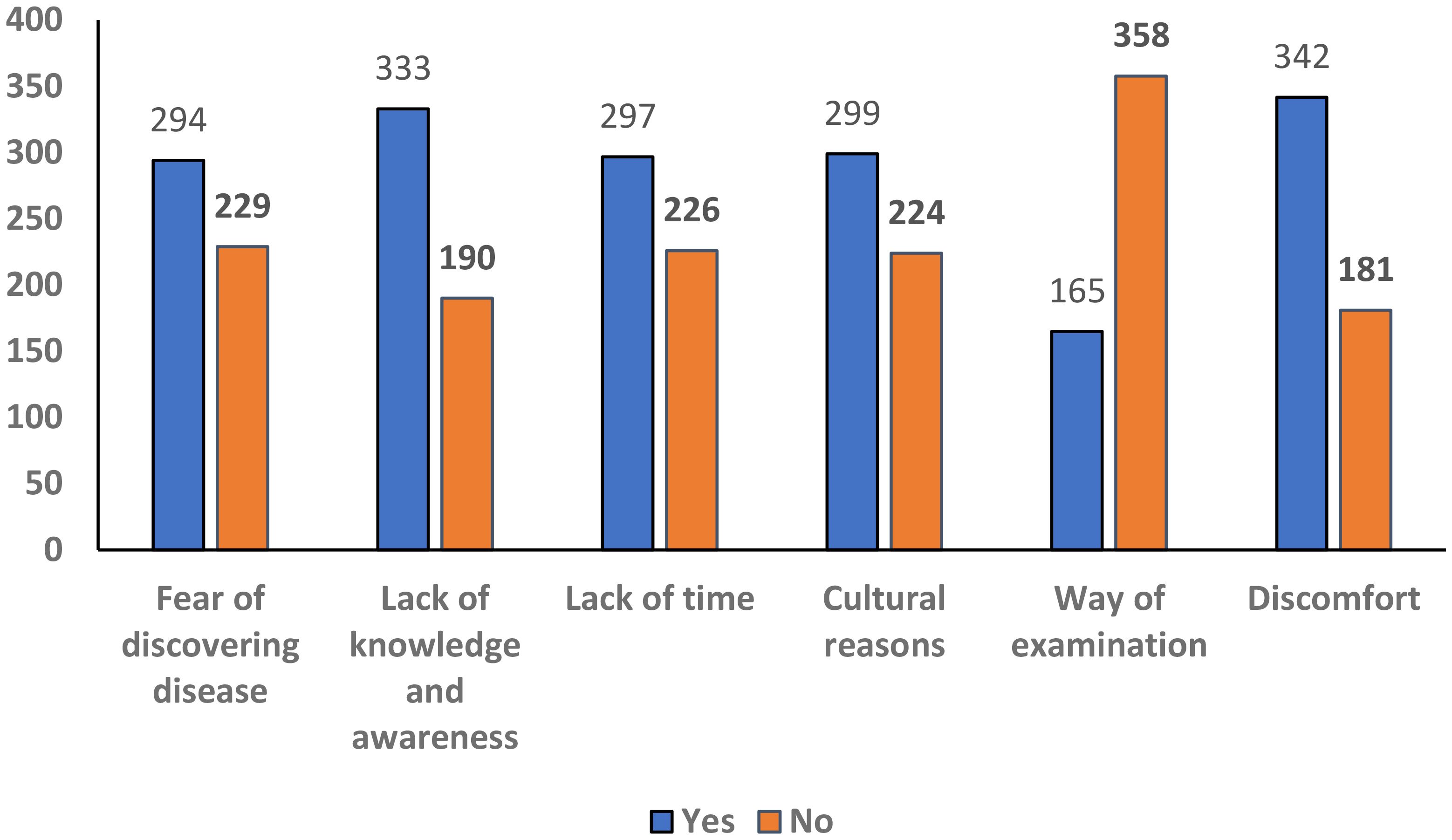
Figure 6. Factors discouraging women from undergoing Pap test in the Asir Region, Saudi Arabia (n = 523).
3.4 Regression analysis
The multivariable logistic regression analysis was performed to examine factors associated with knowledge and attitudes regarding HPV and cervical cancer prevention. Women aged 41–50 years had significantly lower knowledge (adjusted odds ratio (AOR) = 0.479, 95% confidence interval (CI): 0.239–0.961, p = 0.038), and those aged 51–60 years (AOR = 0.239, 95% CI: 0.113–0.505, p = 0.001) and above 60 years (AOR = 0.127, 95% CI: 0.022–0.724, p = 0.020) were even less likely to have adequate knowledge. Regarding education, women who had completed secondary school were less knowledgeable compared to graduates (AOR = 0.483, 95% CI: 0.305–0.764, p = 0.002), while other education levels and employment status were not significantly associated with knowledge. Marital status also influenced knowledge, with single women (AOR = 0.562, 95% CI: 0.327–0.965, p = 0.037) and divorced/widowed women (AOR = 0.413, 95% CI: 0.218–0.784, p = 0.007) showing lower knowledge than married women. For attitudes, older age was the only significant predictor of negative attitudes. Women aged 41–50 years had lower odds of positive attitudes (AOR = 0.327, 95% CI: 0.170–0.629, p = 0.001), with further decreases in the 51–60 years (AOR = 0.272, 95% CI: 0.130–0.570, p = 0.001) and above 60 years groups (AOR = 0.102, 95% CI: 0.012–0.876, p = 0.037). Employment, education, and marital status were not significantly associated with attitudes. Overall, older age, lower education, and being single or divorced/widowed were significantly associated with lower knowledge, while older age was the main factor associated with negative attitudes toward HPV and cervical cancer prevention (Table 5).
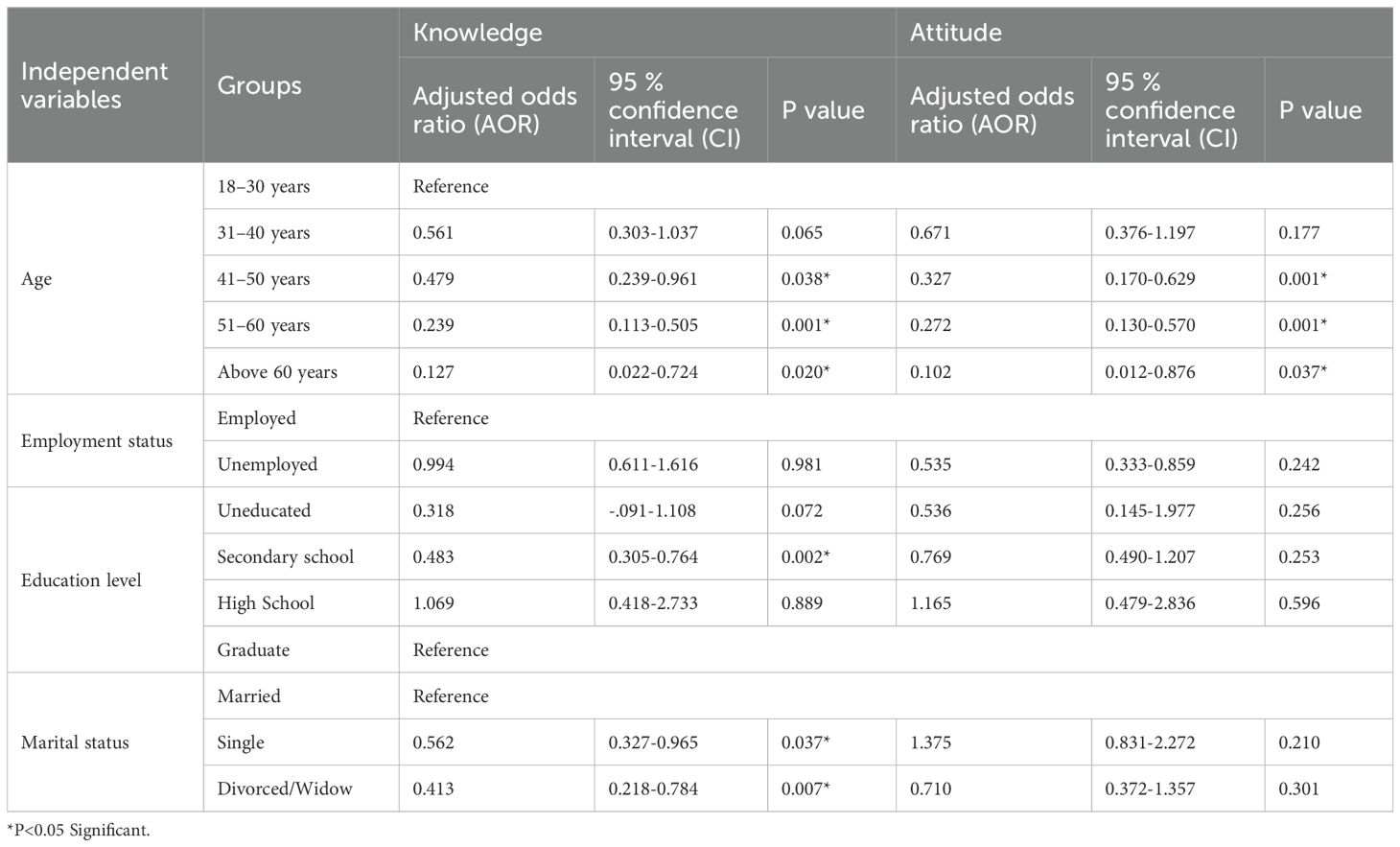
Table 5. Multivariable logistic regression of factors associated with knowledge and attitudes regarding HPV and cervical cancer among women in the Asir Region, Saudi Arabia (n = 523).
4 Discussion
This study assessed the knowledge and attitudes of 523 women in Saudi Arabia regarding HPV and CC prevention. The findings showed that 66% of participants had a good level of understanding, while 34% demonstrated limited awareness. In terms of attitudes, 56% expressed a positive outlook, whereas 44% were less inclined to support preventive measures. These results underscore the need to strengthen public health initiatives to bridge knowledge gaps and promote HPV vaccination and CC screening. A significant portion of women in Saudi Arabia showed awareness of CC and HPV. Specifically, 44.4% of participants knew that HPV is responsible for causing CC, and 62.1% had heard of HPV. These findings align with previous research in Saudi Arabia (38, 39), which reported moderate levels of awareness. A prior study indicated that 60.85% of participants had heard about HPV, showing relatively similar trends (40). However, earlier studies highlighted poor understanding of CC (53.05%), HPV (51.79%), and the vaccine (34.09%) (40–42). Although awareness levels appear to be improving, many women still lack comprehensive knowledge about HPV and its link to CC, emphasizing the need for targeted educational interventions. Akkour et al. reported that 84.0% of respondents had heard about CC, and 61.7% of women acknowledged that early diagnosis leads to a better prognosis. However, only 18.1% knew that HPV causes CC, and just 21.1% understood the route of HPV transmission (40). In comparison, our study found that 44.4% of women were aware of the virus responsible for CC, indicating relatively higher awareness regarding the causal link between HPV and CC. This difference may reflect improvements in public health campaigns, greater availability of health information through digital platforms, and the younger age distribution of our participants (35, 41). The observed improvement in HPV awareness and vaccine uptake may reflect recent national health initiatives in Saudi Arabia, including school-based immunization programs and public health campaigns (43). Greater access to information via digital platforms and healthcare providers likely contributed to higher awareness, highlighting the need for sustained, culturally sensitive education to further enhance vaccination coverage, promote regular screening, and reduce cervical cancer burden (44).
Our study found that 73.6% of participants believed CC is preventable, while 26.3% disagreed. Knowledge of Pap smear testing remained limited, as only 46.1% were familiar with it, while 54% were unaware. Although 79.5% expressed a positive attitude toward screening, only 21.4% had undergone a Pap smear, revealing a gap between awareness and participation. Despite this high willingness, actual uptake remains low, reflecting a clear intention–behavior gap. This mismatch is primarily driven by lack of knowledge, cultural sensitivities, fear of diagnosis, and logistical constraints. Addressing these barriers through targeted educational campaigns, provider engagement, and accessible screening services is essential to convert willingness into action and improve cervical cancer prevention (45). National and regional data indicate low cervical cancer screening coverage in Saudi Arabia. Al Khudairi et al. (46) reported that 75.2% of women in Riyadh had never undergone a Pap smear, and 75.5% had never received a physician recommendation, with 82–93.9% unaware of appropriate screening timing. Similarly, Al Ghamdi found that only 21.1% of adult Saudi women had undergone the test (47). Low participation reflects gaps in awareness, physician engagement, cultural sensitivities, misconceptions about cervical cancer risk, fear of diagnosis, and geographic barriers, particularly in rural areas. The differences in Pap smear awareness and uptake between studies may also be due to participant characteristics such as urban vs. rural residence, educational level, and accessibility of healthcare facilities, as well as variations in study methodology (online surveys vs. in-person interviews) (48).
These findings align with previous studies in Saudi Arabia and the region. Alharbi et al. (49) reported good CC knowledge among women in Makkah, yet our study found that only 32.7% were aware of screening, and just 13.8% knew about Pap smears. Similarly, Al Khudairi et al. (50) found that nearly half of Saudi women were unaware of Pap smears, and over 75% had never undergone one. Alsous et al. assessed women aged 18–60 years across four Arabic-speaking countries (Jordan, Saudi Arabia, Egypt, and Lebanon) and reported poor HPV awareness, with better knowledge among younger, educated women, particularly healthcare professionals (51).
According to the present study, 21% of Saudi women had received the HPV vaccine, compared to 8.25% reported in another Saudi study (35). Similarly, previous study found that only 2.0% of adult Saudi women had been vaccinated against HPV (40), and Yang et al. reported comparable findings in adult populations (52). Khulud et al. reported an HPV vaccination rate of just 10.9% among adult Saudi women (53). These differences may be explained by variations in age distribution, regional contexts, timing of vaccination initiatives, cultural factors, and healthcare access. For instance, our study included women aged 18 years and above, with 42% aged 18–30, which may partly explain the relatively higher vaccination rate observed (54–56). A study conducted in Abha also found that sociodemographic factors significantly influenced HPV vaccine acceptance among young and adolescent females (56). Recent systematic reviews have shown that narrative-based education on the benefits of the HPV vaccine can enhance vaccination uptake, emphasizing the role of healthcare providers in promoting it (57, 58). Recent Saudi studies indicate that physicians’ knowledge and recommendations significantly influence HPV vaccine uptake (59), while parental and teacher attitudes affect schoolgirls’ vaccination decisions (60). Strengthening policy interventions and provider engagement is crucial for improving HPV vaccine coverage. Implementing culturally sensitive strategies can enhance vaccine acceptance and support CC prevention in Saudi Arabia. These findings reinforce the importance of targeted education, school-based programs, and active healthcare provider engagement to improve HPV awareness and vaccination coverage in Saudi Arabia. Similarly, Al-Naggar et al. (61) reported that young women’s perceptions and opinions significantly influenced their willingness to receive HPV vaccination, highlighting the importance of understanding cultural and personal beliefs when designing educational interventions). Strengthening policy interventions and provider engagement is crucial for improving HPV vaccine coverage. Implementing culturally sensitive strategies can enhance vaccine acceptance and support CC prevention in Saudi Arabia. In Saudi Arabia, HPV prevention faces challenges such as cultural sensitivities, low awareness, and misconceptions (62, 63). Despite the availability of screening, uptake remains low. Many women in this study reported discomfort (65.4%), lack of knowledge (63.7%), cultural concerns (57.2%), time constraints (56.8%), and fear of diagnosis (56.2%) as key barriers to Pap smear testing, while 31.5% avoided the exam itself. Addressing these barriers through culturally sensitive education and awareness campaigns is essential to improving screening uptake and HPV prevention (63, 64).
Only 38.2% of Saudi participants correctly identified that HPV vaccinations are available for both men and women aged 9 to 26, consistent with other studies showing low vaccine knowledge among adults (65). In contrast, 71% of respondents in a Canadian survey knew men could also be vaccinated (66). Enhancing access and awareness for both genders could improve vaccination uptake, particularly among males (67). Numerous health behavior theories emphasize the importance of awareness and knowledge as essential components for adopting health-protective behaviors (68). Previous research has shown a positive correlation between vaccine uptake and levels of HPV knowledge (69). Although the HPV vaccine is generally safe, mild side effects such as soreness, redness, swelling, fever, nausea, or muscle/joint pain may occur (70). In this study, 25.4% of women avoided vaccination due to concerns about side effects, aligning with Radwan et al., where 27.7% reported similar hesitations (71). Healthcare providers must proactively address misconceptions to strengthen confidence, improve acceptance, and enhance CC prevention.
Our study identified the internet and social media (39.4%) and healthcare providers (30.4%) as the primary sources of knowledge. Similarly, another study reported internet/social media (69%) as the main source of awareness, followed by healthcare workers (29.8%) (47). Turki et al. also found online platforms as the primary information source (72). In this study, only ~30% of women identified healthcare providers as their main source of HPV information. Prior Saudi studies have reported barriers such as time constraints, limited provider recommendations, discomfort discussing sexual health, and training gaps (59, 60). Addressing these challenges through provider education, routine counseling, and culturally sensitive communication could strengthen providers’ role as trusted sources (45). Additionally, 77% of respondents associated vaginal bleeding after intercourse, between menstrual cycles, or after menopause with CC, consistent with Zahid et al. (73) and Easwaran et al. (74). A study in India reported that 79.9% of participants were willing to vaccinate their daughters (75).
Overall, these findings highlight that older age, lower education, and being single or divorced/widowed were significant predictors of lower knowledge, while older age was associated with negative attitudes toward HPV and CC prevention. Targeted educational interventions, culturally sensitive awareness campaigns, healthcare provider engagement, and digital platforms can further enhance vaccination rates and CC screening uptake.
4.1 Limitations
This study has several limitations. First, its cross-sectional design limits the ability to establish causal relationships between knowledge, attitudes, and preventive practices related to HPV and CC. Additionally, the data relied on self-reported responses, which may be subject to recall and social desirability biases, potentially leading to inaccurate reporting of awareness and attitudes. This study also relied on an online self-administered survey, which may have led to overrepresentation of younger and more educated women. The cross-sectional study with online, social media-based recruitment strategy may have introduced selection bias, potentially underrepresenting women without internet access or those less active on social media, such as older, rural, or less-educated populations. Despite efforts to reach diverse participants through multiple channels including health clinics, community centers, pharmacies, malls, parks, and religious centers the sample may not fully represent the broader female population in the Asir region. Future studies should use probability-based or mixed-method sampling to improve generalizability.
Sampling bias may be present, as the study primarily included accessible and willing participants, and the convenience sampling method may limit the generalizability of the findings to the broader Saudi population. Moreover, the study’s regional focus may not fully capture cultural variations across the country. Furthermore, the study lacked qualitative insights to explore reasons behind low vaccination and screening rates and did not thoroughly examine potential confounding variables such as socioeconomic status and healthcare access. Lastly, the absence of longitudinal follow-up limits the ability to assess changes in knowledge, attitudes, and practices over time following awareness interventions.
5 Conclusion
This study highlights that while many women in the Asir region have good knowledge and positive attitudes toward HPV vaccination and preventive measures, awareness and participation in cervical cancer screening remain limited. Older, less-educated, and unmarried or divorced/widowed women showed gaps in knowledge and more negative attitudes, whereas younger, more educated, and married women were more knowledgeable and proactive. These findings emphasize the need for targeted educational interventions, enhanced healthcare access, and school-based vaccination programs. Leveraging healthcare providers and social media as communication channels can further strengthen preventive practices. Future research should focus on evaluating the effectiveness of such interventions and identifying additional barriers to HPV vaccination and screening uptake.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was granted by the Institutional Review Board (IRB) of King Khalid University (ECM ≠2025-116). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GK: Methodology, Writing – original draft, Data curation, Conceptualization, Software, Funding acquisition, Writing – review & editing, Project administration. KO: Validation, Supervision, Investigation, Methodology, Resources, Conceptualization, Project administration, Writing – original draft. ES: Writing – review & editing, Investigation, Conceptualization, Writing – original draft, Supervision, Funding acquisition, Data curation, Project administration, Resources, Formal analysis, Methodology. AA: Data curation, Visualization, Methodology, Conceptualization, Investigation, Funding acquisition, Project administration, Formal analysis, Writing – review & editing, Writing – original draft. TA: Methodology, Investigation, Software, Funding acquisition, Formal analysis, Data curation, Writing – original draft, Writing – review & editing, Resources. HS: Methodology, Writing – original draft, Formal analysis, Visualization, Data curation, Software, Supervision, Resources, Validation, Writing – review & editing, Investigation.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. The authors extend their appreciation to the Deanship of Research and Graduate studies at King Khalid University for funding this work through large Research Project under grant number RGP2/44/46.
Acknowledgments
The authors extend their appreciation to the Deanship of Research and Graduate studies at King Khalid University for funding this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction note
A correction has been made to this article. Details can be found at: 10.3389/fonc.2025.1726725.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Singh D, Kesharwani P, Thakur S, Gupta R, Patel S, Sharma S, et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob Health. (2023) 11:e197–208. doi: 10.1016/S2214-109X(22)00501-0
2. World Health Organization. Cervical cancer (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer.
3. Kim JJ, Ortendahl J, and Goldie SJ. Cost-effectiveness of human papillomavirus vaccination and CC screening in women older than 30 years in the United States. Ann Intern Med. (2009) 151:538–45. doi: 10.7326/0003-4819-151-8-200910200-00007
4. Cates JR, Ortiz R, Shafer A, Romocki LS, and Coyne-Beasley T. Designing messages to motivate parents to get their preteenage sons vaccinated against human papillomavirus. Perspect Sex Reprod Health. (2012) 44:39–47. doi: 10.1363/4403912
5. Bair RM, Mays RM, Sturm LA, and Zimet GD. Acceptability of the human papillomavirus vaccine among Latina mothers. J Pediatr Adolesc Gynecol. (2008) 21:329–34. doi: 10.1016/j.jpag.2008.02.007
6. Lenselink CH, Gerrits MM, Melchers WJ, Massuger LF, van Hamont D, Bekkers RL, et al. Parental acceptance of Human Papillomavirus vaccines. Eur J Obstet Gynecol Reprod Biol. (2008) 137:103–7. doi: 10.1016/j.ejogrb.2007.02.012
7. Ogilvie GS, Remple VP, Marra F, McNeil SA, Naus M, Pielak Karen L, et al. Parental intention to have daughters receive the human papillomavirus vaccine. Cmaj. (2007) 177:1506–12. doi: 10.1503/cmaj.071022
8. Sperber NR, Brewer NT, and Smith JS. Influence of parent characteristics and disease outcome framing on HPV vaccine acceptability among rural, Southern women. Cancer Causes Control. (2008) 19:115–8. doi: 10.1007/s10552-007-9013-7
9. Woodhall SC, Lehtinen M, Verho T, Huhtala H, Hokkanen M, Kosunen E, et al. Anticipated acceptance of HPV vaccination at the baseline of implementation: a survey of parental and adolescent knowledge and attitudes in Finland. J Adolesc Health. (2007) 40:466–9. doi: 10.1016/j.jadohealth.2007.01.005
10. International Agency for Research on Cancer. Saudi Arabia Fact Sheet 2022 . Available online at: https://gco.iarc.who.int/media/globocan/factsheets/populations/682-saudi-arabia-fact-sheet.pdf (Accessed March 10, 2024).
11. ICO/IARC Information Centre on HPV and Cancer. Human Papillomavirus and Related Cancers, Saudi Arabia Fact Sheet 2023 . Available online at: https://hpvcentre.net/statistics/reports/SAU.pdf (Accessed March 10, 2024).
12. Centers for Disease Control and Prevention. Basic Information About CC 2023 . Available online at: https://www.cdc.gov/cancer/cervical/basic_info/index.htm (Accessed March 10, 2024).
13. Saudi Cancer Registry. Invasive cervical cancer incidence trends in Saudi Arabia (2005–2019): ASIRs across three periods (2005–2009, 2010–2014, 2015–2019). East Mediterr Health J. (2025) 31:380–92.
14. Alkhalawi E. Cervical cancer in Saudi Arabia: trends and regional disparities in incidence and survival (2005–2016) Jeddah, Saudi Arabia: King Abdulaziz University (2021).
16. Alkhamis FH, Alabbas ZAS, Al Mulhim JE, Alabdulmohsin FF, Alshaqaqiq MH, and Alali EA. Prevalence and predictive factors of cervical cancer screening in Saudi Arabia: A nationwide study. Cureus. (2023) 15:e49331. doi: 10.7759/cureus.49331
17. Akkour K, Alghuson L, Benabdelkamel H, Alhalal H, Alayed N, AlQarni A, et al. Cervical cancer and human papillomavirus awareness among women in Saudi Arabia. Medicina. (2021) 57:1373. doi: 10.3390/medicina57121373
18. Aljohani B, Donnelly SW, Al Sumaih B, and O’Neill C. The relationship between region of residence, socio-demographic factors, and healthcare utilization among Saudi citizens: insights from the 2013 Saudi Health Interview Survey. Front Med. (2023) 10:1252340. doi: 10.3389/fmed.2023.1252340
19. Alqahtani T, Alqahtani AM, Alshahrani SM, Orayj K, Almanasef M, Alamri AH, et al. Assessment of knowledge and practice of mammography and breast self-examination among the general female population in Asir Region of KSA. Eur Rev Med Pharmacol Sci. (2021) 25:7231–7. doi: 10.26355/eurrev_202112_27416
20. Alsaleem MA, Alkhairi L, Alsaleem SA, Alsabaani A, Asiri A, Alqahtani A, et al. Knowledge, attitudes, and practices of women in the Southern Region of Saudi Arabia regarding cervical cancer and the Pap smear test. Saudi Med J. (2019) 40:1157–63. doi: 10.31557/apjcp.2019.20.4.1177
21. Alfayi MS. Cervical cancer and human papillomavirus vaccine among females in Asir Region of Saudi Arabia: assessing knowledge and awareness. JJHS. (2024) 12:34–42. doi: 10.4103/KKUJHS.KKUJHS_26_24
22. Saudi Cancer Registry. Cancer incidence report Saudi Arabia 2015. Riyadh, Saudi Arabia: Ministry of Health, Saudi Arabia (2018). Available online at: https://shc.gov.sa/Arabic/NCC/Activities/AnnualReports/2015%20E%20SCR%20final%206%20NOV.pdf.
23. de Martel C, Plummer M, Vignat J, and Franceschi S. Global burden of cancers attributable to infections in 2018: A worldwide incidence analysis. Lancet Glob Health. (2021) 9:e180–90. doi: 10.1016/S2214-109X(19)30488-7
24. World Health Organization. (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer (Accessed March 10, 2024).
25. Meites E, Kempe A, and Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination - updated recommendations of the advisory committee on immunization practices. MMWR. (2019) 65:1405–8. doi: 10.15585/MMWR.MM6549A5
26. Centers for Disease Control and Prevention. HPV vaccine administration 2021 . Available online at: https://www.cdc.gov/vaccines/vpd/hpv/hcp/administration.html (Accessed March 10, 2024).
27. Nada M. The director of the department of prevention of CC and human papilloma virus (HPV), the preventive health assistant deputyship, the public health deputyship, Saudi moH, personal communication. (2023).
28. Brabin L, Roberts SA, Farzaneh F, and Kitchener HC. Future acceptance of adolescent human papillomavirus vaccination: a survey of parental attitudes. Vaccine. (2006) 24:3087–94. doi: 10.1016/j.vaccine.2006.01.048
29. Hou SI. Health education: theoretical concepts, effective strategies and core competencies. Health Promot Pr. (2014) 15:619–21. doi: 10.1177/1524839914538045
30. Feng GC, Lin Z, Ou W, Su X, and Yan Q. A model-based meta-analysis of willingness to participate in cancer screening. Int J Environ Res Public Health. (2021) 18:2580. doi: 10.3390/ijerph18052580
31. Raosoft Inc. Raosoft sample Size Calculator . Available online at: http://www.raosoft.com/samplesize.html (Accessed January 2025).
32. General Authority for Statistics, Kingdom of Saudi Arabia. Population by Region 2010–2022. Riyadh: General Authority for Statistics (2022). Available online at: https://www.stats.gov.sa/en/w/%D8%A7%D9%84%D8%B3%D9%83%D8%A7%D9%86-2010%D9%85-2022%D9%85-1.
33. Sait KH. Attitudes, knowledge, and practices in relation to CC and its screening among women in Saudi Arabia. Saudi Med J. (2009) 30:1208–12.
34. Alghalyini B, Zaidi ARZ, Meo SA, Faroog Z, Rashid M, Alyousef SS, et al. Awareness and knowledge of human papillomavirus, vaccine acceptability and CC among college students in Saudi Arabia. Hum Vaccin Immunother. (2024) 20:2403844. doi: 10.1080/21645515.2024.2403844
35. Alqarni SS, Alshehri SM, Alkhateeb MA, and Alsudias LS. Assessing Saudi women's awareness about human papillomavirus (HPV) and their susceptibility to receive the vaccine. Hum Vaccin Immunother. (2024) 20:2395086. doi: 10.1080/21645515.2024.2395086
36. Alolayan1 SA, Qureshey AK, Alsaedi JR, Alazmi EA, Alkhlaqi HA, and Almutairi M. Knowledge and attitude towards screening and vaccination for CC among females in Jeddah, Saudi Arabia. Int J Med Developing Countries. (2024) 8:1906–16. doi: 10.24911/IJMDC.51-1717755201
37. Mekonnen BA, Anagaw YK, Kassahun BA, and Worku MC. Evaluation of female university students' knowledge, attitudes, and practices toward human papillomavirus infection and vaccination. Multicenter cross-sectional study BMC Womens Health. (2024) 24:437. doi: 10.1186/s12905-024-03279-6
38. Osman TMA, Keshk EA, Mohamed OMOI, Alomari HAS, Alshanini FAM, Alghamdi DGSI, et al. Knowledge, attitude, and practice toward CC and its screening among women from Al-Baha Area, Saudi Arabia. IJMDC. (2025) 9:381–7. doi: 10.24911/IJMDC.51-1736338766
39. Malibari SS. Knowledge about CC among women in Saudi Arabia. Egypt J Hosp Med. (2018) 70:1823–5. doi: 10.12816/0044760
40. Akkour K, Alghuson L, Benabdelkamel H, Alhalal H, Alayed N, AlQarni A, et al. CC and human papillomavirus awareness among women in Saudi Arabia. Medicina. (2021) 57:1373. doi: 10.3390/medicina57121373
41. Alherz FA, Alamri AA, Aljbreen A, and Alwallan N. Knowledge of CC, human papillomavirus (HPV), and acceptance of the HPV vaccine among parents of daughters in Riyadh, Saudi Arabia. J Infection Public Health. (2024) 17:789–94. doi: 10.1016/j.jiph.2024.03.014
42. Almehmadi MM, Salih MM, and Al-Hazmi AS. Awareness of human papillomavirus infection complications, CC, and vaccine among the Saudi population. Saudi Med J. (2019) 40:555–9. doi: 10.15537/SMJ.2019.6.24208
43. Algaadi SA, Aldhafiri HJ, Almulhim YA, Alsubhi RS, Almakrami MH, and Aljamaan NH. Public acceptance of human papillomavirus (HPV) vaccination in Saudi Arabia. J Pioneering Med Sci. (2024) 30:e1–8. doi: 10.61091/jpms202413409
44. Sabin Vaccine Institute. Advocating for Women's Health in Saudi Arabia (2025). Available online at: https://www.sabin.org/resources/advocating-for-womens-health-in-saudi-arabia/.
45. Kirubarajan A, Leung S, Li X, et al. Barriers and facilitators for cervical cancer screening among adolescents and young people: a systematic review. BMC Women's Health. (2021) 21:122. doi: 10.1186/s12905-021-01264-x
46. Al Khudairi H, Abu-Zaid A, Alomar O, and Salem H. Public awareness and knowledge of Pap smear as a screening test for cervical cancer among Saudi population in Riyadh City. Cureus. (2017) 9:e984. doi: 10.7759/cureus.984
47. Al Ghamdi and Nada H. Knowledge of human papilloma virus (HPV), HPV-vaccine and pap smear among adult Saudi women. J Family Med Primary Care. (2022) 11:2989–99. doi: 10.4103/jfmpc.jfmpc_2094_21
48. Tsekpetse P, Salu S, Otoo DM, Dushime Joy Flora, Shiuma Joshua, Oloo Betty, et al. Rural-urban disparities in cervical cancer screening uptake and its predictors among women aged 30–49 years in Ghana: a multivariate decomposition analysis. BMC Women's Health. (2025) 25:396. doi: 10.1186/s12905-025-03962-2
49. Alharbi HS, Jokhdar HA, Garout MA, Al Falogy EH, Zahrany RA, Al-Harbi WS, et al. Assessment of knowledge, awareness and attitude about CC and its screening among women in Makkah, Saudi Arabia, in: 4th International Conference &Exhibition on Surgery, Dubai, UAE.
50. Al Khudairi H, Abu-Zaid A, Alomar O, and Salem H. Public awareness and knowledge of Pap smear as a screening test for CC among Saudi population in Riyadh City. Cureus. (2017) 9:e984. doi: 10.7759/cureus.984"10.7759/cureus.984
51. Alsous MM, Ali AA, Al-Azzam SI, Abdel Jalil MH, Al-Obaidi HJ, Al-abbadi EI, et al. Knowledge and awareness about human papillomavirus infection and its vaccination among women in Arab communities. Sci Rep. (2021) 11:786. doi: 10.1038/s41598-020-80834-9
52. Yang J, Nolte FS, Chajewski OS, Lindsey KG, Houser PM, Pellicier J, et al. Cytology and high risk HPV testing in CC screening program: outcome of 3-year follow-up in an academic institute. Diagn Cytopathol. (2018) 46:22–7. doi: 10.1002/dc.23843
53. Barnard M, Cole AC, Ward L, Gravlee E, Cole ML, and Compretta C. Interventions to increase uptake of the human papillomavirus vaccine in unvaccinated college students: a systematic literature review. Prev Med Rep. (2019) 14:100884. doi: 10.1016/j.pmedr.2019.100884
54. Alghalyini B, Alqarni SS, Alkhateeb MA, and Alsudias LS. Awareness and knowledge of human papillomavirus, vaccine acceptability and cervical cancer among college students in Saudi Arabia. Hum Vaccin Immunother. (2024) 20:2403844. doi: 10.1080/21645515.2024.2403844
55. Alsulami FT. Exploring the impact of knowledge about the human papillomavirus and its vaccine on perceived benefits and barriers to human papillomavirus vaccination among adults in the Western region of Saudi Arabia. Healthcare (Basel). (2024) 12:1451. doi: 10.3390/healthcare12141451
56. Alshahrani MN, Almutairi D, Zahrani Y, Alsabaani A, Alraey Y, and Alshahrani SM. Barriers associated with the parental acceptance of human papillomavirus (HPV) vaccination of minors in Asir, Saudi Arabia: A cross-sectional study. Hum Vaccin Immunother. (2025) 21:2513708. doi: 10.1080/21645515.2025.2513708
57. Mavundza EJ, Iwu-Jaja CJ, Wiyeh AB, Gausi B, Abdullahi LH, Halle-Ekane G, et al. A systematic review of interventions to improve HPV vaccination coverage. Vaccines (Basel). (2021) 9:687. doi: 10.3390/vaccines9070687
58. Alshehri S and Sallam M. Vaccine conspiracy association with higher COVID-19 vaccination side effects and negative attitude towards booster COVID-19, influenza and monkeypox vaccines: a pilot study in Saudi universities. Hum Vaccin Immunother;. (2023) 19:2275962. doi: 10.1080/21645515.2023.2275962
59. Alosaimi B, Fallatah DI, Abd ElHafeez S, Saleeb Mohamed, Alshanbari Huda M, Awadalla Maaweya, et al. Predictors of human papillomavirus (HPV) vaccine acceptability among physicians, their knowledge on cervical cancer, and factors influencing their decision to recommend it. J Multidiscip Healthc. (2024) 17:5177–88. doi: 10.2147/JMDH.S484534
60. Fallatah DI, Khalil MA, Abd ElHafeez S, Gouda Salma, Alshanbari Huda M, Awadalla Maaweya, et al. Factors influencing human papillomavirus vaccine uptake among parents and teachers of schoolgirls in Saudi Arabia: a cross-sectional study. Front Public Health. (2024) 12:1403634. doi: 10.3389/fpubh.2024.1403634
61. Al-Naggar RA, Al-Jashamy K, and Chen R. Perceptions and opinions regarding human papilloma virus vaccination among young women in Malaysia. Asian Pac J Cancer Prev. (2010) 11:1515–21.
62. Alhamlan FS, Khayat HH, Ramisetty-Mikler S, Al-Muammar TA, Tulbah AM, Al-Badawi IA, et al. Sociodemographic characteristics and sexual behavior as risk factors for human papillomavirus infection in Saudi Arabia. Int J Infect Dis. (2016) 46:94–9. doi: 10.1016/j.ijid.2016.04.004
63. Tobaiqy MA, Mehdar SA, Altayeb TI, Saad TM, and Alqutub ST. Parental knowledge, views, and perceptions of human papilloma virus infection and vaccination-cross-sectional descriptive study. J Fam Med Prim Care. (2023) 12:556–60. doi: 10.4103/jfmpc.jfmpc_1673_22
64. Heena H, Durrani S, AlFayyad I, Riaz M, Tabasim R, Parvez G, et al. Knowledge, Attitudes, and Practices towards CC and Screening amongst Female Healthcare Professionals: A Cross-Sectional Study. J Oncol. (2019) 2019:5423130. doi: 10.1155/2019/5423130
65. Davis EN and Doyle PC. An assessment of young adults’ Awareness and knowledge related to the human papillomavirus (HPV), oropharyngeal cancer, and the HPV vaccine. Cancers. (2025) 17:344. doi: 10.3390/cancers17030344
66. Sadry SA, De Souza LR, and Yudin MH. The impact of ethnicity on awareness and knowledge of and attitudes towards the human papillomavirus and vaccine among adult women. J Obstet Gynaecol Can. (2013) 35:995–1003. doi: 10.1016/S1701-2163(15)30787-8
67. Ragan KR, Bednarczyk RA, Butler SM, and Omer SB. Missed opportunities for catch-up human papillomavirus vaccination among university undergraduates: Identifying health decision-making behaviors and uptake barriers. Vaccine. (2018) 36:331–41. doi: 10.1016/j.vaccine.2017.07.041
68. Heimbecker V, Bordini SC, Rodrigues AC, de Alencar NM, Blanco NS, Fitz F, et al. Gender differences on the awareness of human papillomavirus infection and vaccination. J Cancer Educ. (2024) 39:611–7. doi: 10.1007/s13187-024-02516-8
69. Barnard M, George P, Perryman ML, and Wolff LA. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: Implications from the Precaution Adoption Process Model. PloS One. (2017) 12:e0182266. doi: 10.1371/journal.pone.0182266
70. Everything You Need to Know About the HPV Vaccine . Available online at: https://www.gavi.org/vaccineswork/everything-you-need-know-about-hpv-vaccine (Accessed October 23, 2024).
71. Radwan A, Sabban H, Alsobhi R, Alsayed N, Alharthi T, and Alzanbaqi M. Awareness and knowledge of human papillomavirus (HPV) infection and vaccine among women: A cross-sectional study in Jeddah, Saudi Arabia. Cureus. (2023) 15:e45400. doi: 10.7759/cureus.45400
72. Turki YM and Alqurashi J. Knowledge, attitudes, and perceptions towards human papillomavirus (HPV) vaccination among adult women in primary health care centers in Makkah, Saudi Arabia. Cureus. (2023) 15:e44157. doi: 10.7759/cureus.44157
73. Zahid HM, Qarah AB, Alharbi AM, Alomar AE, and Almubarak SA. Awareness and practices related to CC among females in Saudi Arabia. Int J Environ Res Public Health. (2022) 19:1455. doi: 10.3390/ijerph19031455
74. Easwaran V, Shorog EM, Alshahrani AA, Mohammad AA, Sadiq MM, Alavudeen SS, et al. Knowledge, attitudes, and practices related to CC prevention and screening among female pharmacy students at a public University in a Southern Region of Saudi Arabia. Healthcare (Basel). (2023) 11:2798. doi: 10.3390/healthcare11202798
Keywords: cervical cancer, human papilloma virus, knowledge, attitude, women
Citation: Kandasamy G, Orayj K, Shorog E, Alshahrani AM, Alanazi TS and Algorman HS (2025) Knowledge and attitudes toward human papillomavirus and cervical cancer prevention among women in the Asir Region, Saudi Arabia: a cross-sectional study. Front. Oncol. 15:1608568. doi: 10.3389/fonc.2025.1608568
Received: 29 May 2025; Accepted: 29 September 2025;
Published: 16 October 2025; Corrected: 27 October 2025.
Edited by:
Monika Rucinska, University of Warmia and Mazury in Olsztyn, PolandReviewed by:
Karim A. Mohamed Al-Jashamy, SEGi University, MalaysiaMaaweya Awadalla, King Fahd Medical City, Saudi Arabia
Copyright © 2025 Kandasamy, Orayj, Shorog, Alshahrani, Alanazi and Algorman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Geetha Kandasamy, Z2xha3NobWlAa2t1LmVkdS5zYQ==
 Geetha Kandasamy
Geetha Kandasamy Khalid Orayj1
Khalid Orayj1 Eman Shorog
Eman Shorog Tahani S. Alanazi
Tahani S. Alanazi