- 1Department of Gastrointestinal Surgery, The Sixth Affiliated Hospital, Sun Yat-sen University Yuexi Hospital, Xinyi, China
- 2Department of General Surgery (Department of Gastrointestinal Surgery), The Sixth Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 3Guangdong Provincial Key Laboratory of Colorectal and Pelvic Floor Diseases, The Sixth Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 4Biomedical Innovation Center, The Sixth Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
Situs inversus totalis (SIT) is a rare congenital condition characterized by a complete reversal of the internal organ arrangement, presenting significant surgical challenges. While previous cases of colorectal cancer in SIT patients have been reported, cases involving sigmoid colon cancer are sporadic. Here, we present the case of a 68-year-old female with sigmoid colon cancer and SIT. Following thorough preoperative preparation and a multidisciplinary team (MDT) consultation, the patient successfully underwent a laparoscopic radical sigmoidectomy. Her postoperative recovery was smooth, and she was discharged on postoperative day 10. At the 3-month follow-up, no short-term complications or signs of tumor recurrence were observed. This case highlights the importance of meticulous surgeon positioning in facilitating laparoscopic surgery for patients with SIT.
Introduction
Situs inversus totalis (SIT) is a rare congenital anatomical anomaly inherited in an autosomal recessive pattern (1). It is characterized by a complete transposition of thoracic and abdominal organs, resulting in a mirror-image arrangement compared to the typical anatomical structure (2). Studies have shown that SIT patients are more likely to have congenital abnormalities affecting the cardiovascular, gastrointestinal, and respiratory systems, along with anatomical anomalies such as polysplenia, biliary atresia, and midgut malrotation (3). The reversal of organ positions in SIT patients significantly complicates surgical assessment and procedures. In recent years, case reports have documented colorectal cancer in SIT patients, including those affecting the ascending colon, transverse colon, and descending colon (4–7). However, to the best of our knowledge, reports of SIT patients with sigmoid colon cancer undergoing laparoscopic minimally invasive surgery with comprehensive preoperative preparation, such as CT based three-dimensional vascular and colonic reconstruction, remain exceedingly rare. This report provides a detailed account of the anatomical variations observed in a case of SIT with sigmoid colon cancer and analyzes the unique aspects of the diagnostic and therapeutic approach employed.
Case presentation
In August 2024, a 68-year-old, BMI 21.3Kg/m2 female presented with a year-long history of right lower abdominal pain, initially misdiagnosed as “chronic appendicitis.” along with a two-hour history of acute abdominal pain, abdominal distension, and vomiting. The abdominal pain was intermittent and dull, occurring 4–5 times daily, without hematochezia or melena. Two hours before admission, the symptoms worsened, with increased abdominal pain, distension, and vomiting. A colonoscopy performed upon admission revealed sigmoid colon cancer with luminal stenosis, which prevented further scope advancement. A biopsy confirmed moderately differentiated adenocarcinoma. The patient had no significant past medical history or family history of cancer, and prior health examinations had documented complete situs inversus totalis (SIT).
Physical examination revealed a flat abdomen without visible gastric or intestinal peristaltic waves. Mild tenderness was present in the lower abdomen without rebound tenderness, muscle rigidity, or palpable masses. Serum tumor markers were within normal limits (CEA: 3.53 ng/ml, CA-199: 17.63 ng/ml). Laboratory tests showed elevated inflammatory markers but no evidence of anemia or hypoproteinemia. Abdominal CT imaging confirmed SIT, demonstrating the cardiac apex on the right side, the liver on the left, and the stomach and spleen on the right (Figure 1A). Chest CT confirmed dextrocardia (Figure 1B). CT colonography revealed a right-sided sigmoid colon (Figure 1C), while CT angiography detailed the abdominal vascular anatomy (Figure 1D). Contrast-enhanced abdominal CT identified a tumor in the sigmoid colon, staged as cT3N2aM0 (Figures 1E, F).
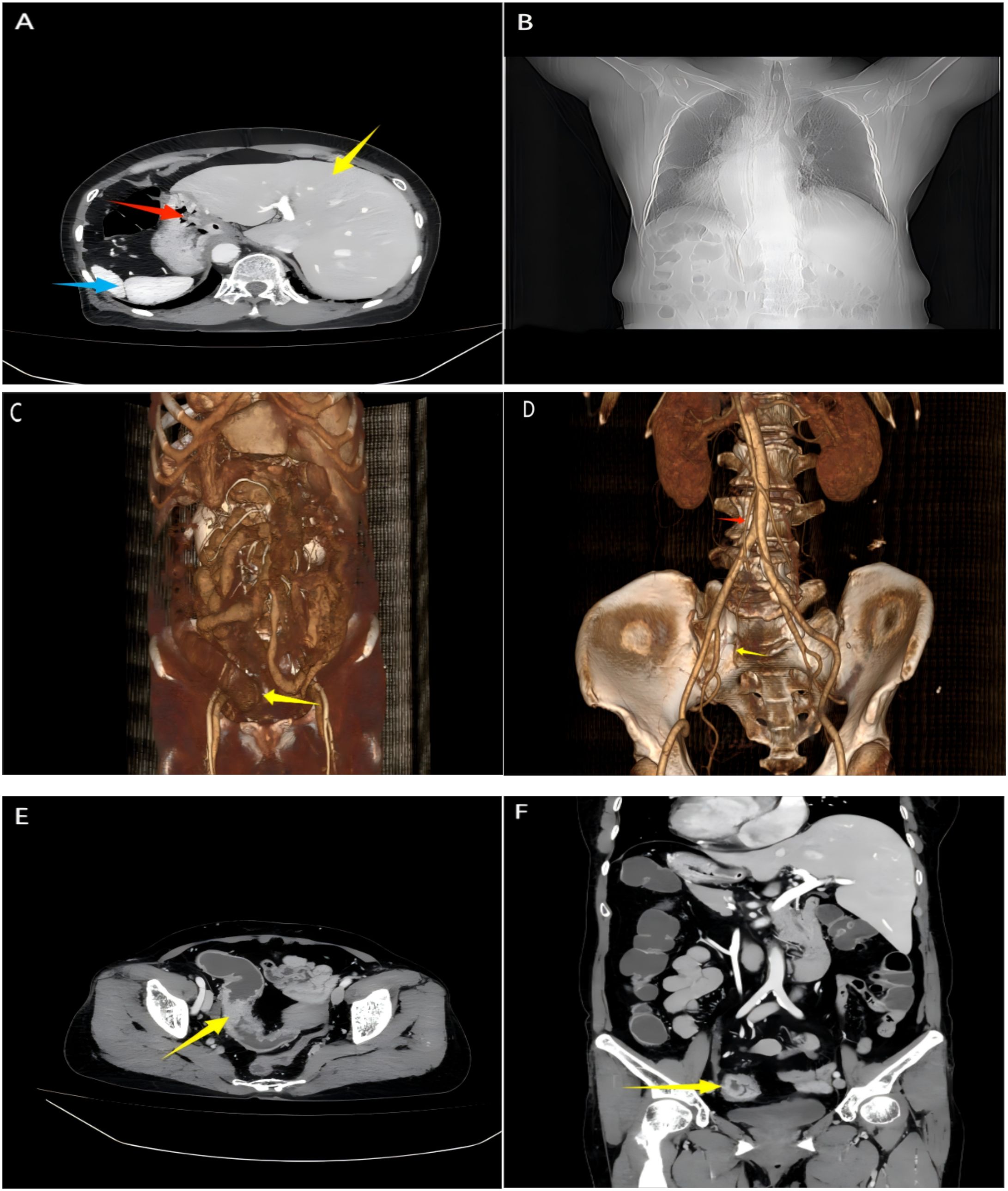
Figure 1. Images of computed tomography. (A) CT scan shows reversed positions of the liver (Red arrow), stomach (Red arrow), and spleen (blue arrow); (B) Chest CT shows dextrocardia; (C) 3D CT colonography shows a sigmoid colon tumor (yellow arrow). (D) The three-dimensional reconstruction images of CT angiography show the inferior mesenteric artery (red arrow) and sigmoid artery (yellow arrow); (E, F) CT scan cross-sectional/coronal images suggest a mass in the sigmoid colon.
Preoperative contrast-enhanced CT and 3D laparoscopy confirmed complete mirror-image transposition of the thoracic and abdominal organs, including the liver on the left and spleen on the right. Importantly, there were no features suggestive of intestinal malrotation—the duodenojejunal junction, cecum, and ascending/descending colon were all appropriately aligned, albeit mirrored.
Intraoperatively, the tumor was identified in the lower segment of the sigmoid colon, located in the right lower abdominal cavity, consistent with the preoperative imaging findings (Figure 2A). The tumor measured approximately 4.0 x 3.0 x 2.5 cm, exhibited a constricting shape and had invaded beyond the serosal layer.
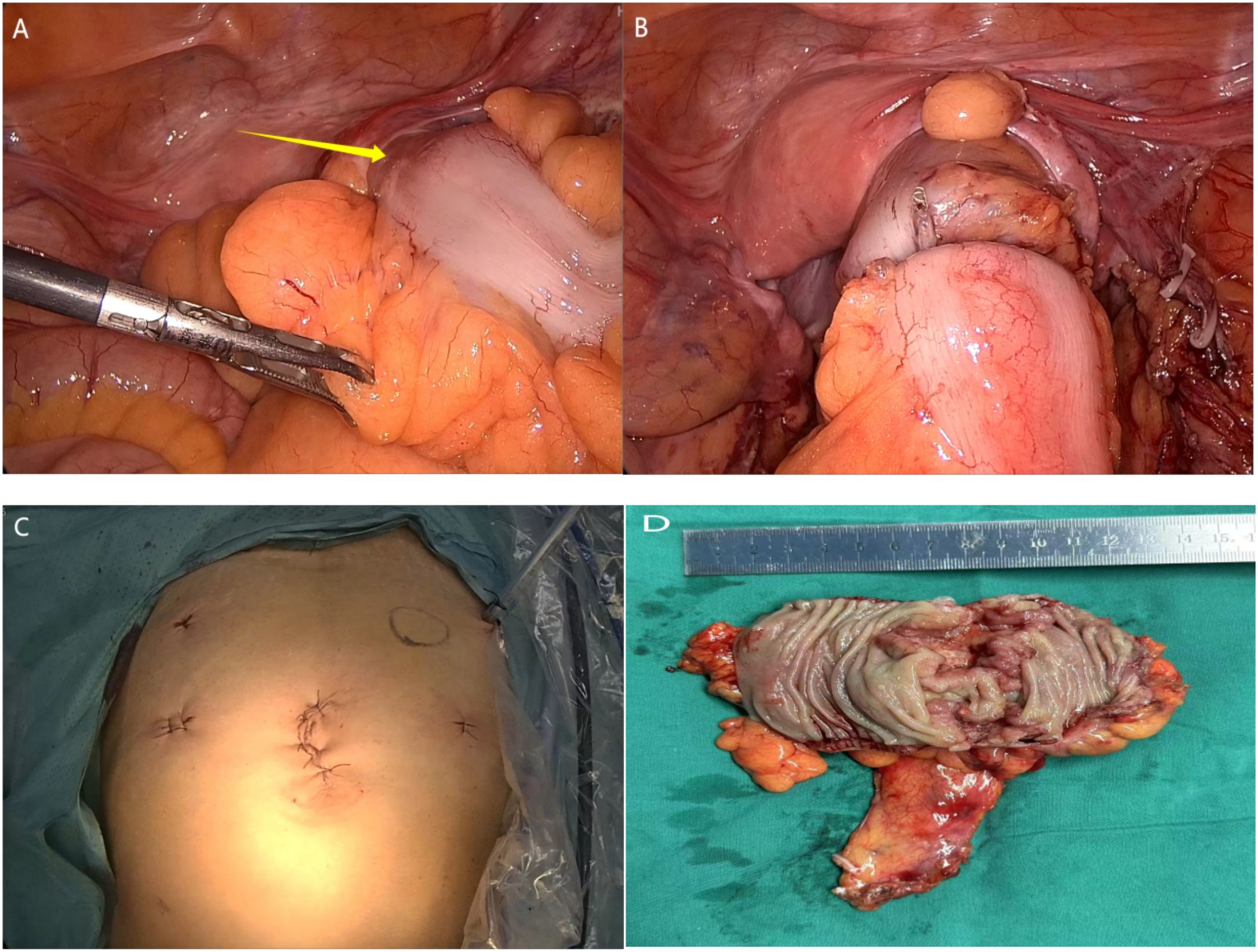
Figure 2. Images of operation and histopathological examination. (A) Laparoscopy revealed a lesion in the distal sigmoid colon.; (B) Laparoscopic tumor resection followed by colonic anastomosis reconstruction; (C) Postoperative abdominal photograph following minimally invasive surgery; (D) The sigmoid colon tumor after complete excision (view of the opened bowel wall).
A camera port was placed at the umbilicus, and three working ports were positioned at the right McBurney’s point (5 mm), left McBurney’s point (12 mm), and suprapubic region slightly left of midline (5 mm) as the operating surgeon was right handed standing on the left side of the patient. There were no peritoneal deposits. Initially, the peritoneum was incised along the root of the sigmoid mesocolon, and dissection proceeded cephalad to identify the origin of the inferior mesenteric artery (IMA). The IMA was carefully isolated and divided at its base (preserving the “left colic artery branch”). The sigmoid mesocolon was then mobilized distally to the rectosigmoid junction, with meticulous preservation of both ureters and the hypogastric nerve plexus. The splenic flexure was fully mobilized to ensure tension-free anastomosis. The proximal rectum was transected using a linear stapler. The specimen was extracted through the 12-mm left lower quadrant port, and the anvil of a circular stapler was introduced into the proximal colon. After re-establishing pneumoperitoneum, the stapler was inserted transanally, and an end-to-end anastomosis was performed. The anastomosis was inspected for adequate blood supply and absence of tension, and an air leak test confirmed its integrity (Figure 2B).
A pelvic drainage tube was placed postoperatively, and the incision was closed in layers following the original structure (Figures 2C, D). The procedure lasted 115 minutes, with an estimated blood loss of 20 ml.
Postoperative laboratory tests showed mild leukocytosis (WBC 10,690/mm³, neutrophils 8,940/mm³), likely due to surgical stress. Prophylactic antibiotics were administered, and the patient remained asymptomatic without fever or abdominal pain. Drain output was minimal (30 ml/day initially, decreasing to <30 ml/day by postoperative Day 6) and serosanguinous before removal. The patient resumed enteral intake after flatus passage by Day 4. The patient was discharged on postoperative day 10.
The final pathological diagnosis was moderately differentiated adenocarcinoma, staged as T3N0M0 (Stage IIA). The total number of lymph nodes retrieved were 15. The proximal and distal resection margins were free of tumor.
At the 10-month follow-up, no evidence of short-term complications or tumor recurrence was observed. No adjuvant therapy was given to the patient.
Discussion
The exact mechanism underlying situs inversus totalis (SIT) remains unclear. Some researchers propose that it may be linked to fetal heterotopia during embryonic development and chromosomal abnormalities. The incidence of SIT is estimated to range from approximately 1 in 8,000 to 1 in 20,000 (8). Most individuals with SIT show no significant differences in physiological functions, including digestion, circulation, and respiration, compared to those with typical anatomical structures.
The unique anatomical variations associated with SIT present significant challenges in diagnosis and treatment, particularly in surgical interventions, where procedural complexity is heightened (9). Even for experienced gastrointestinal surgeons, minimally invasive surgery in SIT patients is a technically demanding, with the primary difficulty being the accurate identification of vascular structures. In such cases, preoperative vascular reconstruction s critical for clearly delineating the primary blood supply to the intestines, thereby enhancing surgical success.
In recent years, the number of reports documenting laparoscopic surgery for colorectal cancer in SIT patients has steadily increased (5, 7, 10, 11). These studies consistently highlight the importance of thorough preoperative assessment and meticulous surgical planning. When possible, angiography is recommended prior to surgery to identify anatomical variations. Abdominal 3D CT angiography and CT colonography provide detailed anatomical insights, particularly regarding the colon’s vascular branching patterns, enabling surgeons to identify potential anomalies preoperatively. This facilitates precise ligation of the tumor’s blood supply, minimizing intraoperative bleeding and reducing the risk of hematogenous metastasis, while also shortening operative time.
Others, robotic-assisted surgery offers significant advantages in colorectal cancer treatment, particularly in enhancing precision and minimizing vessel sacrifice. The safety and feasibility of robotic vessel-sparing sigmoidectomy and robotic-sewn intracorporeal anastomosis have been well-documented, further supporting the growing role of robotic surgery in achieving oncological radicality while preserving critical vascular structures (12, 13). These advancements not only improve surgical outcomes but also pave the way for more efficient and minimally invasive approaches in colorectal cancer management.
In addition to standard evaluations such as chest X-rays, laboratory tests, and contrast-enhanced abdominal CT scans, preoperative echocardiography is essential for SIT patients to detect cardiac anomalies that may influence prognosis (14). In this case, preoperative color Doppler ultrasonography of the heart and lower limb vessels ruled out other cardiovascular anomalies that could affect the patient’s prognosis.
Conclusion
This case involves a patient with sigmoid colon cancer and SIT who successfully underwent laparoscopic sigmoid colectomy with radical lymphadenectomy. It underscores the critical role of comprehensive preoperative imaging and meticulous surgical planning. Despite the challenges associated with laparoscopic surgery in SIT patients, this approach proves to be a safe and effective minimally invasive treatment option when supported by appropriate strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
C-YZ: Writing – original draft. JH: Data curation, Writing – original draft. L-CH: Writing – original draft, Data curation. LC: Writing – original draft, Investigation. HP: Writing – review & editing, Conceptualization. CY: Writing – review & editing. YP: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1613470/full#supplementary-material
References
1. Iwamura T, Shibata N, Haraguchi Y, Hisashi Y, Nishikawa T, Yamada H, et al. Synchronous double cancer of the stomach and rectum with situs inversus totalis and polysplenia syndrome. J Clin Gastroenterol. (2001) 33:148–53. doi: 10.1097/00004836-200108000-00012
2. Gentile BA and Tighe DA. Situs inversus totalis. N Engl J Med. (2019) 380:e45. doi: 10.1056/NEJMicm1811002
3. Guo CX, Chen W, Yao WY, Li GG, Zhang Q, Chen YW, et al. The first report of laparoscopic pancreaticoduodenectomy for primary duodenal carcinoma in a patient with situs inversus totalis: report of a rare case. Surg Laparosc Endosc Percutan Tech. (2019) 29:e29–33. doi: 10.1097/SLE.0000000000000659
4. Xu Q, Liu W, Lin C, Dang Y, and Lin C. Transverse colon cancer with obstruction in a patient with situs inversus totalis: A case report and review of literature. Asian J Surg. (2020) 43:1186–8. doi: 10.1016/j.asjsur.2020.09.003
5. Hu JL, Li QY, and Wu K. Ascending colon cancer and situs inversus totalis - altered surgeon position for successful laparoscopic hemicolectomy: A case report. World J Clin Oncol. (2022) 13:848–52. doi: 10.5306/wjco.v13.i10.848
6. Feng J, Niu W, Zhang J, Ding Y, Li Z, Zhang J, et al. Pathological complete response after monotherapy with immune checkpoint inhibitors for bifocal colon cancer in a patient with lynch syndrome and situs inversus totalis: a case report. Front Immunol. (2025) 16:1571607. doi: 10.3389/fimmu.2025.1571607
7. Cheng L, Feng YG, He L, Xie JB, Zhou CJ, Liu JJ, et al. Descending colon cancer in a patient with situs inversus totalis: a case report and literature review. J Surg Case Rep. (2022) 2022:rjab568. doi: 10.1093/jscr/rjab568
8. Burn J. Disturbance of morphological laterality in humans. Ciba Found Symp. (1991) 162:282–96; discussion 96-9. doi: 10.1002/9780470514160.ch16
9. Eitler K, Bibok A, and Telkes G. Situs inversus totalis: A clinical review. Int J Gen Med. (2022) 15:2437–49. doi: 10.2147/IJGM.S295444
10. Fujiwara Y, Fukunaga Y, Higashino M, Tanimura S, Takemura M, Tanaka Y, et al. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J Gastroenterol. (2007) 13:5035–7. doi: 10.3748/wjg.v13.i37.5035
11. Takeda T, Haraguchi N, Yamaguchi A, Uemura M, Miyake M, Miyazaki M, et al. Laparoscopic sigmoidectomy in a case of sigmoid colon cancer with situs inversus totalis. Asian J Endosc Surg. (2019) 12:111–3. doi: 10.1111/ases.12483
12. Huscher CGS, Cobellis F, and Lazzarin G. Preserving vascular integrity during totally robotic sigmoidectomy: unleashing the power of vessel-sparing precision. Langenbecks Arch Surg. (2024) 409:46. doi: 10.1007/s00423-023-03218-3
13. Huscher CGS, Lazzarin G, Marchegiani F, and Marks J. Robotic right colectomy with robotic-sewn anastomosis: a pilot case series. J Robot Surg. (2023) 17:427–34. doi: 10.1007/s11701-022-01435-4
Keywords: sigmoid colon cancer, situs inversus totalis, laparoscopy, surgery, technology
Citation: Zhang C-Y, He J, Huang L-C, Chen L, Pan H, Chen Y-L and Peng Y (2025) Minimally invasive surgical treatment for sigmoid colon cancer in a patient with situs inversus totalis: a case report. Front. Oncol. 15:1613470. doi: 10.3389/fonc.2025.1613470
Received: 17 April 2025; Accepted: 25 July 2025;
Published: 20 August 2025.
Edited by:
Rahul Gupta, Synergy Institute of Medical Sciences, IndiaCopyright © 2025 Zhang, He, Huang, Chen, Pan, Chen and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong-Le Chen, Y2hlbnlsZTNAbWFpbC5zeXN1LmVkdS5jbg==; Yi Peng, MzE1MTUxMTAyQHFxLmNvbQ==
†These authors have contributed equally to this work
 Chao-Yue Zhang
Chao-Yue Zhang Jing He1†
Jing He1† Yong-Le Chen
Yong-Le Chen Yi Peng
Yi Peng