- 1State Key Laboratory of Traditional Chinese Medicine Syndrome/Breast Disease Specialist Hospital, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangdong Provincial Hospital of Chinese Medicine, Guangdong Provincial Academy of Chinese Medical Sciences, Guangzhou, Guangdong, China
- 2The Second Clinical College of Guangzhou University of Chinese Medicine, Guangzhou, Guangdong, China
- 3Guangdong Provincial Hospital of Chinese Medicine, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, Guangdong, China
- 4Department of Breast, Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, Guangdong, China
- 5Guangdong Provincial Key Laboratory of Clinical Research on Traditional Chinese Medicine Syndrome, Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, Guangdong, China
- 6Postdoctoral Research Center, Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, Guangdong, China
- 7Chinese Medicine Guangdong Laboratory, Guangzhou, Guangdong, China
Breast cancer remains one of the most prevalent malignancies among women. Traditional Chinese Medicine (TCM) identifies Liver depression syndrome as a core clinical pattern in breast cancer; however, the absence of systematic reviews addressing this specific syndrome has constrained the development and application of TCM interventions. This systematic review searched seven Chinese and English databases, and was supplemented by published books and clinical guidelines, to identify literature documenting TCM diagnostic indicators of Liver depression syndrome in breast cancer. The collated data formed the TCM item for Liver depression syndrome in breast cancer, and descriptive statistics were applied to analyze symptom patterns. This study revealed 104 distinct clinical manifestations and 56 tongue-pulse indicators. The predominant syndrome subtypes included syndrome of qi stagnation due to Liver depression (30.5%), syndrome of phlegm congealing due to Liver depression (24.7%), syndrome of Liver qi depression (19.7%), and syndrome of Liver depression and Spleen deficiency (15.6%). Key clinical manifestations comprised distending pain in the chest and sub-costal region (68%), depression (67%), breast mass (64%), anger (52%), breast distending pain (44%), and oppression in chest (44%). The most prevalent tongue manifestation was thin white fur, while the most common pulse pattern was the stringy pulse. The current findings highlight diagnostic inconsistencies in the definition of Liver depression syndrome in breast cancer, posing challenges to clinical research and the elucidation of syndrome mechanisms. Future investigations should prioritize the standardization and objective characterization of diagnostic criteria to enhance the accuracy of syndrome recognition and facilitate scientific validation.
Systematic review registration: https://www.crd.york.ac.uk/prospero, identifier CRD42024546784.
Introduction
Breast cancer constitutes a significant contributor to cancer-related mortality among women (1), and data from China show that its incidence ranks second among cancers (2). The pathogenesis of breast cancer involves multiple mechanisms, among which emotional factors play a key role in the occurrence and progression of this disease (3). Previous studies, including systematic reviews (4), multicenter clinical studies (5), and Delphi study (6), have consistently identified Liver depression syndrome as the main clinical pattern of breast cancer. Liver depression syndrome is a general syndrome term which contains a series of syndrome subtypes centered on constrained Liver qi. Based on the common etiology, different syndrome subtypes can be divided at different stages of pathology (7).
In TCM theory, it is believed that the core pathogenesis of Liver depression syndrome is attributed to chronic emotional constraint and psychosocial stressors. Characteristic clinical manifestations encompass depression, sighing propensity, and irritability (8). In breast cancer, multiple etiological factors beyond emotional dysregulation can precipitate Liver depression. For example, breast cancer patients can suffer chronic emotional depression due to gender role stress (9). Meanwhile, modern lifestyles including lack of sleep (10), sedentary behavior (11) and high-fat diet (12) can also disrupt Liver function through multiple mechanisms. Thus, under the cumulative effect of these factors, persistent stagnation of Liver qi gradually disrupts the inter-organ coordination of the Liver, Spleen and Kidney, as well as the homeostasis of qi and blood circulation (13). This pathological state initiates a cascade of pathophysiological processes, such as qi stagnation, blood stasis, phlegm accumulation and toxin accumulation. These abnormalities accumulate in the mammary tissue, ultimately contributing to the oncogenesis of breast cancer.
While diagnostic criteria exist for subtype patterns like the Liver depression with qi stagnation and Liver depression with phlegm coagulation (7), standardized diagnostic parameters specific to breast cancer-associated Liver depression syndrome remain undefined. The standardization of syndrome diagnosis holds significant implications for TCM clinical practice and research. Establishing unified diagnostic criteria for Liver depression syndrome would not only enhance the precision of syndrome differentiation in breast cancer management but also facilitate the standardized application of TCM therapeutic approaches in breast cancer prevention and treatment. Moreover, such standardization would provide essential support for developing integrated TCM and Western medicine diagnostic frameworks and promote the international dissemination of research outcomes. Building on this, the current study systematically consolidates literature evidence and performs evidence-based medical evaluations to establish a scientific framework for developing standardized diagnostic criteria for Liver depression syndrome in the context of breast cancer.
Methods
The methods employed to identify relevant research articles were guided by the protocols outlined in the Cochrane Handbook for Systematic Reviews of Interventions. Additionally, this study was meticulously reported in strict adherence to the PRISMA guidelines. This systematic review was prospectively registered on PROSPERO (Registration ID: CRD42024546784).
Literature search strategy
Searches were conducted in the following seven electronic databases: China National Knowledge Infrastructure (CNKI), Chongqing VIP Information database (CQVIP), Wanfang Database, Chinese Biomedical Literature Service System (SinoMed), PubMed, Cochrane Library, and EMBASE. The search scope has covered all records from the inception to January 2024. Using “Liver Depression” as the core term, the search strategy targeted 18 clinically defined subtypes of Liver depression syndrome, all of the subtypes are manifestations of different pathophysiologic conditions caused by the etiology of Liver depression. Additionally, supplementary print literature sources, including textbooks, monographs, clinical guidelines, and consensus statements, were systematically reviewed to collect information from the four diagnostic methods (including inspection, auscultation, inquiry and palpation). The complete search terms and protocols are detailed in Supplementary File 1 (Chinese/English Search Terms).
Study eligibility criteria
Inclusion criteria were: (1) Pathologically confirmed breast cancer diagnosis; (2) Records of TCM diagnosis for breast cancer (Ru Yan or breast cancer); (3) TCM syndrome differentiation confirmed as Liver depression syndrome; (4) Inclusion of comprehensive symptom descriptions and information on Chinese herbal interventions; (5) Literature addressing the etiology, pathogenesis, or clinical manifestations of Liver depression syndrome in breast cancer, including clinical observations and expert experience reports.
Exclusion criteria were: (1) Cell or animal experimental studies; (2) Duplicate publications (only one version retained); (3) Secondary analyses, including reviews and meta-analyses; (4) Clinical studies focusing on breast cancer comorbidities (e.g., postoperative lymphedema); (5) Studies involving diagnostic criteria for complex syndromes beyond Liver depression syndrome. In this study, no unpublished or original data were included.
Data extraction
Researchers systematically extracted the following variables: author information, publication year, study type, geographic region, publishing source (journal/publisher), TCM diagnostic patterns of Liver depression syndrome, signs and symptoms, pathological classification, and cancer staging. For textbook sources, entries from the same series with different editors-in-chief were consolidated as a single entry, while multiple editions by the same editors-in-chief retained only the content from the most recent edition to ensure timelines and avoid duplication.
Symptom standardization primarily referenced Clinical Terminology of Traditional Chinese Medicine Diagnosis and Treatment–Part 2: Clinical Patterns (GB/T 16751.2-2021) (7), Standardized Glossary of TCM Clinical Symptoms (14), and the Diagnostic Differentiation of TCM Symptoms (2nd Edition) (15). This standardization process provided the basis for constructing a TCM item pool for Liver depression syndrome in breast cancer, ensuring terminological precision in the systematic review.
Data analysis methodology
Literature quality assessment adhered to the hierarchical evidence grading system for TCM studies (16), which categorized sources as Level I (large-scale randomized investigations with definitive outcomes and minimal type I/II error risks), Level II (small-sample randomized studies with indeterminate results and elevated error probabilities), Level III (non-randomized concurrent controlled trials and historical expert consensus), Level IV (non-randomized historical controls and contemporary consensus statements), and Level V (case reports, uncontrolled observations, and expert opinions). Descriptive statistical analysis of TCM signs and symptoms associated with Liver depression syndrome in breast cancer was performed using SPSS 26.0, with frequency distributions calculated for all documented clinical symptoms.
Results
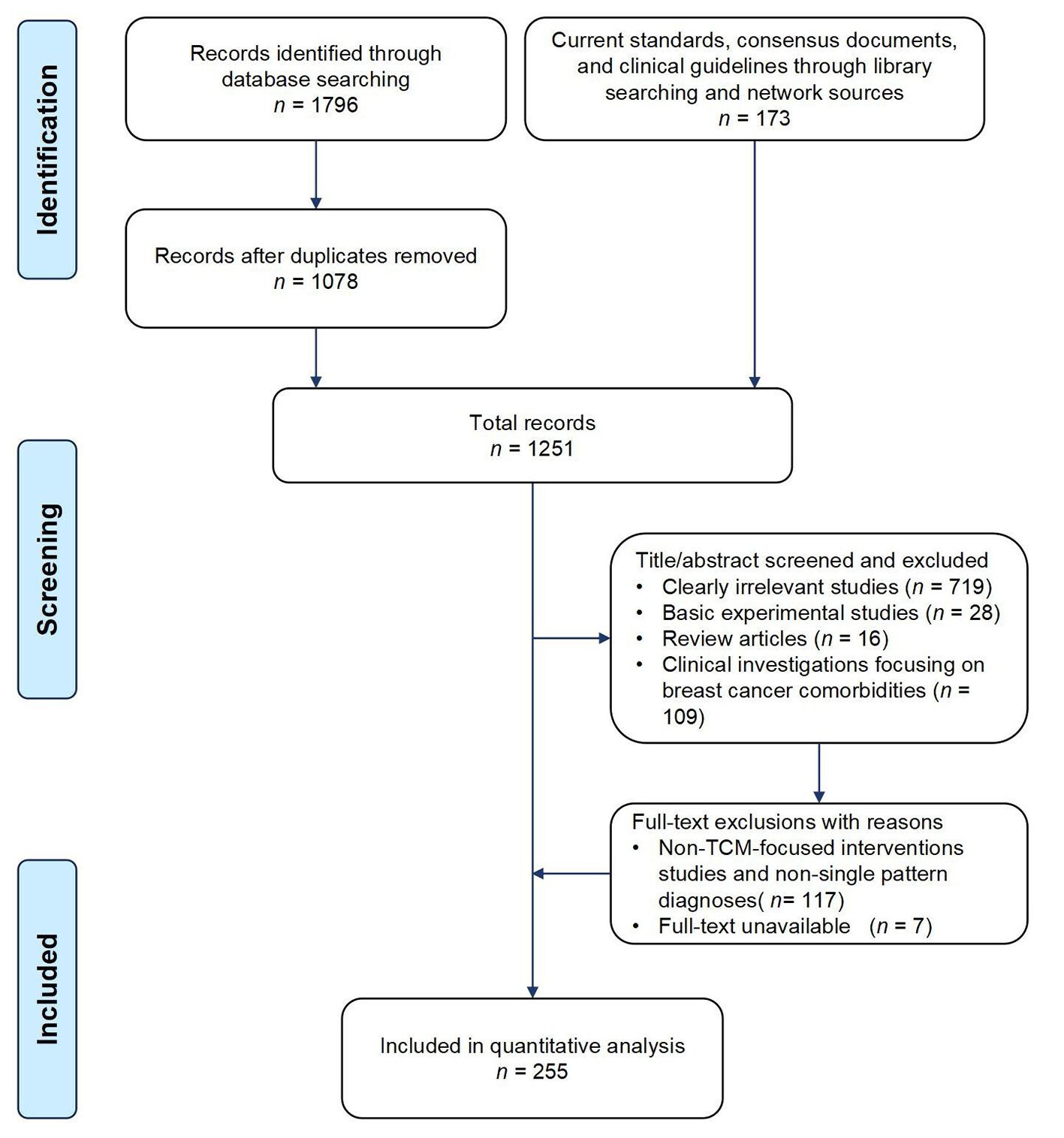
A total of 255 eligible literatures were screened, including eight expert consensus documents, 130 textbooks/monographs, 35 medical record files of renowned physicians, and 82 contemporary research articles. It was worth noting that due to the reporting of multiple subtypes of Liver depression syndrome in some literatures, thus, a total of 298 clinical entries were ultimately analyzed. The literature screening was shown in Figure 1.
Characteristics of included studies
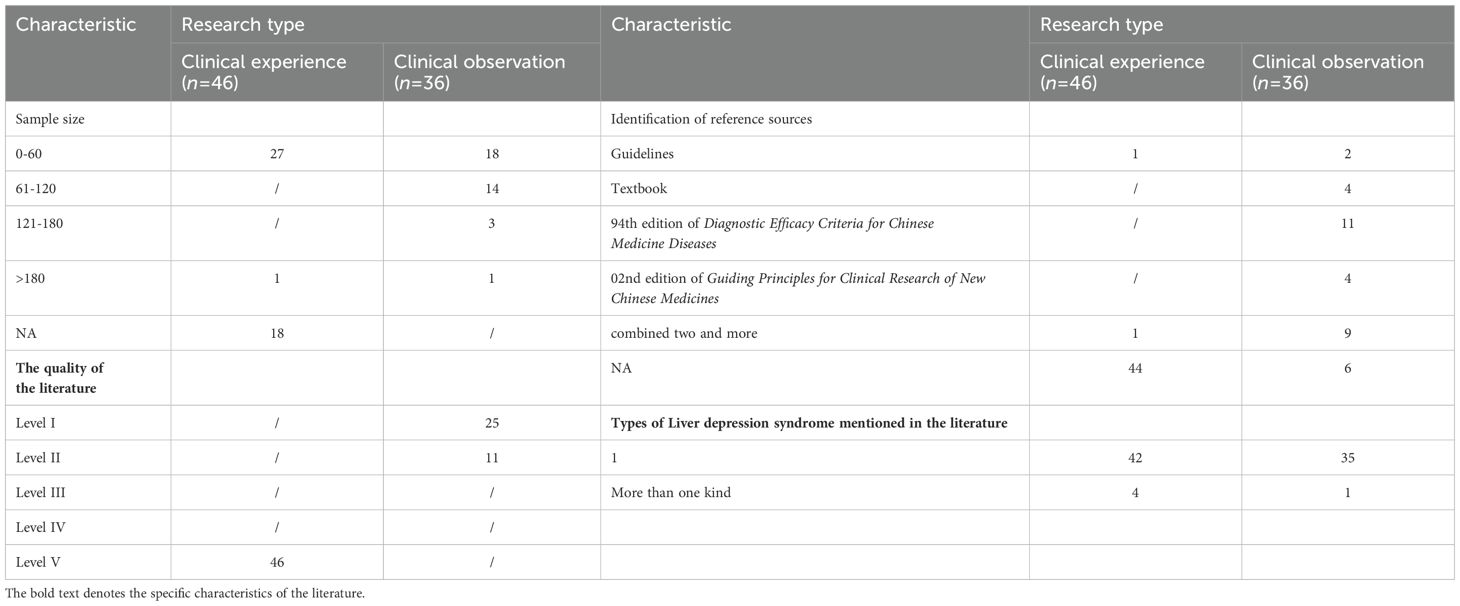
Among the 82 included studies, 46 were clinical experience summaries and 36 were clinical observations. Level V literature accounted for 56.1% (46/82), Level I literature accounted for 30.5% (25/82), and Level II literature accounted for 13.4% (11/82). These studies were classified as Level V literature because they were non-controlled studies, such as experience summaries and case reports. Table 1 presents the basic characteristics of the literature.
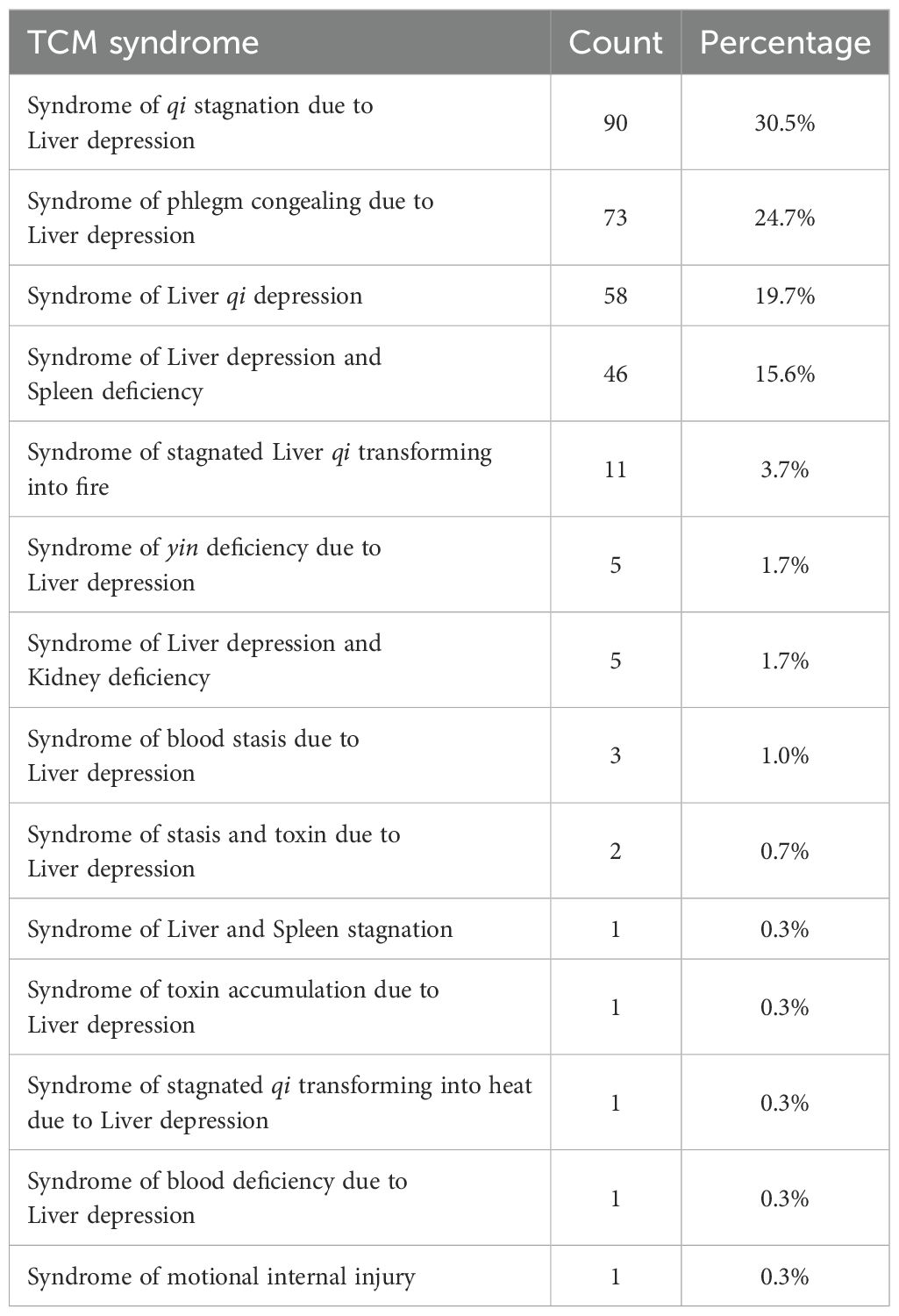
Frequency of syndrome results
Analysis of 298 clinical entries revealed 25 distinct subtypes of Liver depression syndrome. Due to terminological variations across medical literature and practitioners, semantically equivalent subtypes were consolidated. The top five syndromes were: qi stagnation due to Liver depression (30.5%), phlegm congealing due to Liver depression (24.7%), Liver qi depression (19.7%), Liver depression and Spleen deficiency (15.6%) and stagnated Liver qi transforming into fire (3.7%). Table 2 shows the main subtypes of Liver depression syndrome in breast cancer literature.
Frequency of signs and symptoms of liver depression syndrome in breast cancer
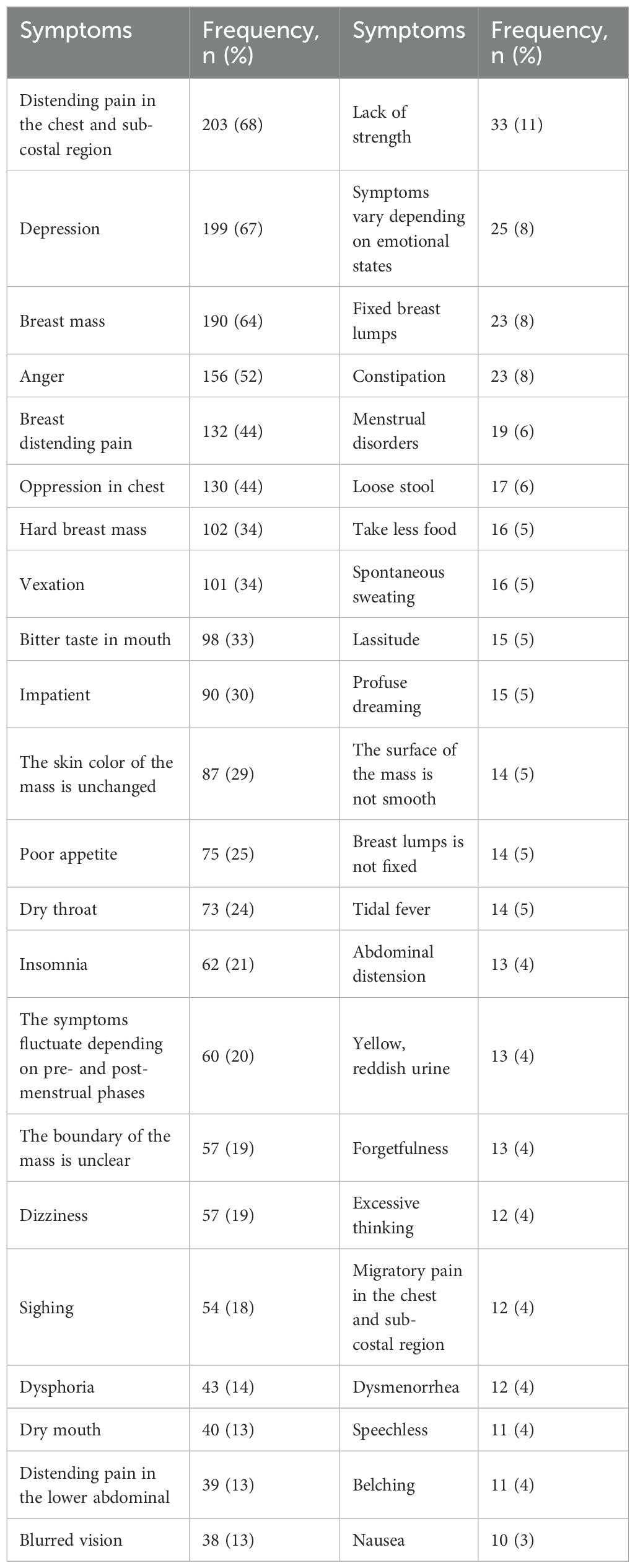
A total of 104 signs and symptoms associated with Liver depression syndrome in breast cancer were identified through systematic data curation. The top ten signs and symptoms were: distending pain in the chest and sub-costal region (68%), depression (67%), breast mass (64%), anger (52%), breast distending pain (44%), oppression in chest (44%), hard breast mass (34%), vexation (34%), bitter taste in mouth (33%), impatient (30%) (detailed in Table 3).
In terms of tongue and pulse, this systematic review identified a total of 54 entries associated with Liver depression syndrome in breast cancer. The five most common tongue manifestations were: thin and white fur (48%), thin and yellow fur (28%), red tongue (23%), thin fur (17%), pale tongue (14%). The five most pulse conditions were: stringy pulse (41%), stringy and slippery pulse (28%), stringy and thready pulse (14%), stringy and deep pulse (7%), stringy and strong pulse (6%). Table 4 presents the frequency distribution of tongue and pulse of Liver depression syndrome in breast cancer.
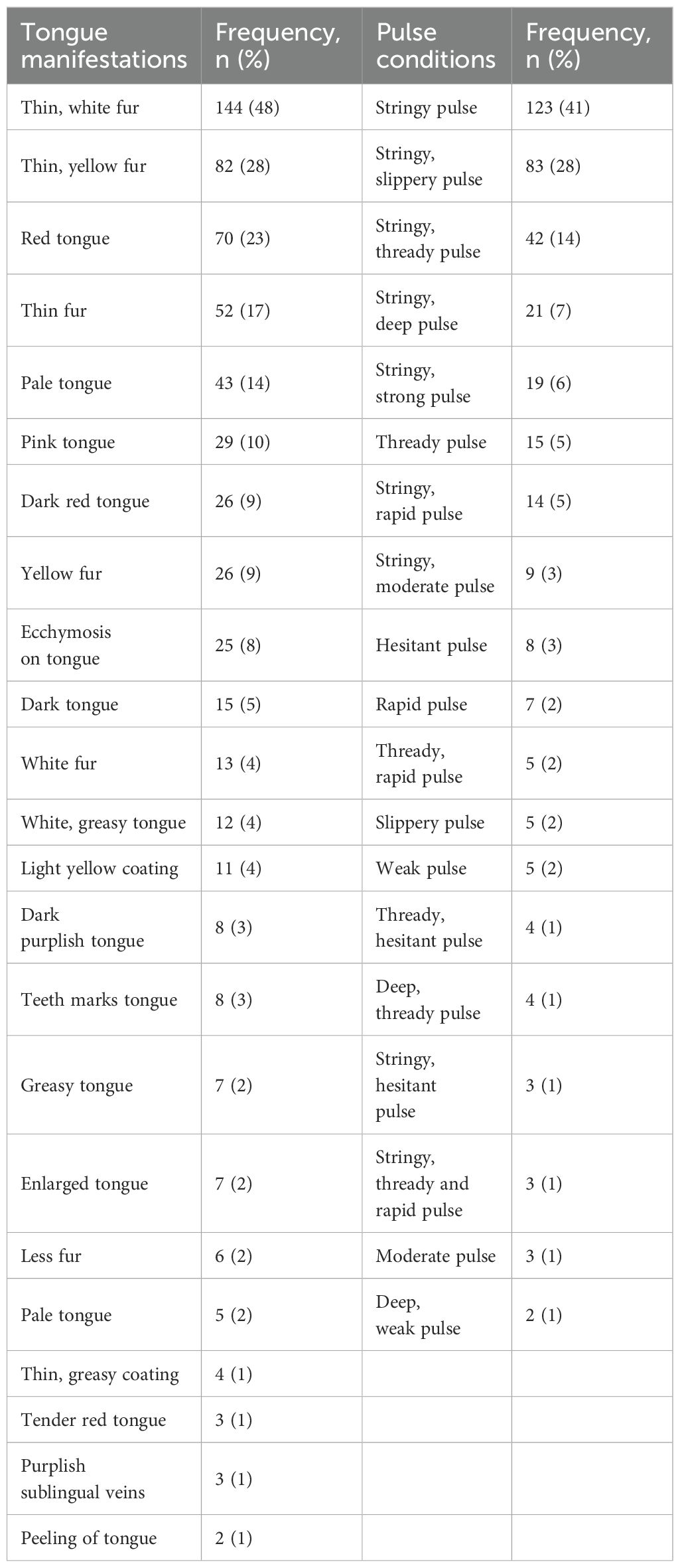
Table 4. The frequency of tongue manifestations and pulse conditions of Liver depression syndrome evidence in breast cancer.
Discussion
Traditional Chinese Medicine demonstrates therapeutic potential in breast cancer, with studies indicating its efficacy in alleviating side effects and improving quality of life (17–19). While Liver depression syndrome is a key clinical syndrome in breast cancer pathogenesis, the lack of standardized diagnostic criteria has hindered scientific understanding and TCM intervention development. This study systematically synthesizes literature to outline its clinical characteristics, dominant symptoms, and tongue–pulse diagnostic indicators, facilitating precise syndrome characterization and supporting TCM oncology theory refinement. Our study indicates that breast cancer patients with Liver depression syndrome exhibit six main symptom clusters: breast-related abnormalities, emotional disturbances, Liver meridian pathway manifestations, chest-abdominal discomfort, menstrual irregularities, and bowel/bladder dysfunction. Emotional symptoms, such as depression, anger, vexation, often fluctuating alongside emotional states.
The results of this study indicate that Liver depression syndrome in breast cancer presents with a variety of tongue and pulse manifestations. Across all literature related to Liver depression syndrome, thin white fur and stringy pulse are the most frequently observed. Tongue and pulse are critical diagnostic parameters in TCM syndromes. Previous studies have established several criteria for Liver depression syndrome across various diseases, yet tongue manifestations are seldom mentioned. For instance, tongue signs were not included in the diagnostic criteria for Liver depression and Liver qi depression syndromes (20, 21), suggesting that experts consider tongue signs to lack specificity for these patterns. In the criteria for Liver depression syndrome, the tongue description “pale tongue with thin white fur” represents normal physiological findings (22). This may reflect the TCM theory that tongue coating reflects Stomach qi transformation, while Liver depression primarily disrupts qi movement without directly inducing dampness or heat accumulation, leading to subtle tongue coating changes and reduced diagnostic value. In contrast, pulse conditions play a crucial role in the diagnosis of Liver depression syndrome. The stringy pulse is the only consistent indicator across criteria, aligning with our literature review findings.
TCM deeply understands Liver depression syndrome, identifying various causes such as external pathogens, emotional stress, and phlegm accumulation that disrupt the flow of vital energy qi. In breast cancer, Liver depression is both a common pattern and a crucial factor. TCM believes breast tissue is connected to the Liver meridian system, and breast health depends on the Liver and Stomach working together. Chronic emotional suppression or sudden anger can cause Liver qi stagnation, impairing Spleen function and nutrient processing. Combined with a diet high in rich or fatty foods, this can lead to internal phlegm-dampness buildup. When these harmful elements gather in breast tissue, they create the conditions for cancer to develop. Besides, emotional factors play a dominant role in Liver regulation, and Liver depression is linked to tumorigenesis in multiple ways. The Liver meridian traverses the throat, and prolonged Liver depression can generate fire-toxin. This fire-toxin scorches body fluids into phlegm, contributing to thyroid cancer (referred to as “gall tumors” in TCM) (23). Additionally, Liver depression and repressed anger induce qi stagnation and blood stasis, which are the pathological mechanisms underlying liver cancer (24).
In TCM, a classical view holds that Liver depression is a key pathogenic factor in breast cancer oncogenesis (25). However, since Liver depression syndrome comprises multiple subtypes, it remains unclear whether all subtypes contribute to breast cancer development. This uncertainty warrants further investigation. These subtypes reflect the progression of Liver depression through distinct pathological stages. TCM emphasizes “transformation of pathogenesis”, indicating that syndromes are not static but can evolve as the disease progress. Literature and textbooks (26, 27) show that in the early stage of breast cancer, Liver depression with qi stagnation is the main syndrome. Without timely intervention, it may gradually evolve into Liver depression transforming into fire, followed by Liver depression with blood stasis and phlegm coagulation. Prolonged Liver depression can damage Spleen function, leading to Spleen deficiency. Therefore, Liver depression with qi stagnation serves as the pathological foundation, while other syndrome manifestations are results of pathological evolution. Each subtype is not independently pathogenic but is jointly triggered by the pathological chain of “qi stagnation–phlegm stasis–toxic accumulation–vital deficiency”.
In terms of treatment, TCM focuses on getting the body’s energy qi flowing smoothly again by regulating the Liver. A prime example is the classic TCM formula Chaihu Shugan San, which relieves Liver congestion and improves emotional well-being and quality of life (28–30). With modern technological advancements, we can investigate specific effector pathways and molecular targets associated with Liver depression syndrome in breast cancer using histological and omics techniques (31). Our goal is to uncover the syndrome’s microscopic and molecular signatures. Additionally, using our team’s established Liver depression syndrome breast cancer mouse model, we can assess the efficacy of TCM interventions on key signaling nodes. This will provide a solid basis for precisely targeting Liver depression syndrome in breast cancer therapy.
Depressive symptoms in breast cancer patients are a significant public health issue (32–34), with a 30.2% prevalence globally in 2023 (35). There are significant clinical and pathophysiological links between TCM’s Liver depression syndrome and Western-defined depression in these patients. Modern biomedical research recognizes chronic stress as fundamentally analogous to TCM’s “Liver constraint” (Liver qi stagnation), as shown by preclinical studies using chronic stress models to induce Liver depression syndrome (36–38). Chronic psychological stress activates the sympathetic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis, releasing substances that promote cancer progression (39) and impair immune surveillance (40), thereby increasing breast cancer susceptibility (41, 42). Additionally, experimental data show that chronic psychological stress accelerates mammary tumor growth and metastasis in mouse models, while the TCM formula Sini San counteracts these effects by reducing stress-induced aerobic glycolysis (43). The TCM pathomechanism of “qi stagnation” aligns with depression-associated dysregulation of the neuroendocrine-immune network. In TCM theory, the Liver regulates qi flow and emotions, and therapies that restore Liver qi dynamics likely exert multi-mechanistic effects: simultaneously normalizing qi circulation, alleviating emotional distress, and enhancing immune surveillance (44–46).
This study systematically maps the literature on Liver depression syndrome in breast cancer, but limitations exist. Most studies (56.1%) were Level V non-controlled, reflecting the current dominance of observational and case-based evidence in this field. Though valuable for clinical insights, their retrospective design and lack of control groups limit causal inference. Future research should focus on establishing standardized diagnostic criteria for Liver depression syndrome in breast cancer to enhance diagnostic accuracy and consistency. Utilizing advanced multi-omics technologies like metabolomics and spatial transcriptomics can help elucidate the syndrome’s biological mechanisms and identify key molecular events related to clinical depression. Integration of artificial intelligence (AI) and big data analytics will aid in developing objective biomarkers and early detection tools, advancing TCM syndrome standardization. Multicenter clinical trials are needed to validate the effects of Liver qi-regulating therapies on the tumor microenvironment and optimize herbal formulas. These efforts will promote the development of integrative TCM-Western treatment models to improve breast cancer prognosis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author contributions
PW: Conceptualization, Methodology, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. SYM: Data curation, Writing – original draft. QZ: Data curation, Writing – review & editing. QG: Conceptualization, Supervision, Writing – review & editing. QJC: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the National Natural Science Foundation of China( 82305234 and, 82474504, and 82405608); Guangzhou Science and Technology Plan Project (NO.2024A03J0850, SL2024A04J3296 and SL2025A04J4201); Incubation Program for the Science and Technology Development of Chinese Medicine Guangdong Laboratory (HQL2024PZ023); Project of Guangdong Provincial Key Laboratory of Clinical Research on Traditional Chinese Medicine Syndrome (YN2023ZH10); Autonomous Project of State Key Laboratory of Traditional Chinese Medicine Syndrome(QZ2023ZZ13).National Demonstration Pilot Project for the Inheritance and Development of Traditional Chinese Medicine -Construction project between Guangzhou University of Chinese Medicine and Zhongshan Hospital of Traditional Chinese Medicine(No.GZYZS2024XKG05); Guangdong Hospital of Traditional Chinese Medicine Special Research Project on Traditional Chinese Medicine Science and Technology (YN2022QN32, and YN2022QN01); Autonomous Project of State Key Laboratory of Traditional Chinese Medicine syndrome (SKLKY2024B0009, SKLKY2024B0017 and SKLKY2025C0001) and 2024 Guangdong Provincial Administration of Traditional Chinese Medicine Research Project (Special Fund for Scientific Research Platforms) (Grant No. 20244029).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1614903/full#supplementary-material
References
1. Siegel RL, Kratzer TB, Giaquinto AN, Sung H, and Jemal A. Cancer statistics, 2025. CA: A Cancer J Clin. (2025) 75:10–45. doi: 10.3322/caac.21871
2. Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, et al. Cancer incidence and mortality in China, 2022. J Natl Cancer Cent. (2024) 4:47–53. doi: 10.1016/j.jncc.2024.01.006
3. Zimmaro LA, Sorice KA, Handorf EA, Daly MB, and Reese JB. Understanding clinical communication about mood disturbance symptoms among breast cancer patients: A mixed methods analysis. Patient Educ Couns. (2022) 105:2089–95. doi: 10.1016/j.pec.2022.02.004
4. Guo Q, Chen Q, Xue CC, Zhang AL, and Coyle ME. Chinese medicine syndromes and stages of early breast cancer: hierarchical cluster analysis and implication for clinical practice. J Altern Complement Med. (2021) 27:904–14. doi: 10.1089/acm.2021.0055
5. Guo Q, Coyle ME, Zhang AL, Xue X, Bian W, Song A, et al. Chinese medicine syndrome differentiation for early breast cancer: A multicenter prospective clinical study. Front Oncol. (2022) 12:914805. doi: 10.3389/fonc.2022.914805
6. Guo Q and Chen Q. Standardization of syndrome differentiation defined by traditional chinese medicine in operative breast cancer: A modified delphi study. ScientificWorldJournal 2015. (2015) p:820436. doi: 10.1155/2015/820436
7. Terminology of Chinese medicine clinical diagnosis and treatment Part 2: Evidence. In: National technical committee for standardization of traditional chinese medicine. Beijing: National Technical Committee for Standardization of Traditional Chinese Medicine.
8. Chen JX and Wilson JF. International standard libraryof chinese medicine: diagnostics in chinese medicine (Second edition). Beijing: People’s Health Publishing House (2019).
9. Liu JK, Kaji AH, Roth KG, Hari DM, Yeh JJ, Dauphine C, et al. Determinants of psychosocial distress in breast cancer patients at a safety net hospital. Clin Breast Cancer. (2022) 22:43–8. doi: 10.1016/j.clbc.2021.06.011
10. Hwang Y and Knobf MT. Sleep health in young women with breast cancer: a narrative review. Supportive Care Cancer. (2022) 30:6419–28. doi: 10.1007/s00520-022-06953-3
11. Lee J, Lee J, Lee D-W, Kim H-R, and Kang M-Y. Sedentary work and breast cancer risk: A systematic review and meta-analysis. J Occup Health. (2021) 63:e12239. doi: 10.1002/1348-9585.12239
12. Wang X, Liu X, Jia Z, Zhang Y, Wang S, and Zhang H. Evaluation of the effects of different dietary patterns on breast cancer: monitoring circulating tumor cells. Foods. (2021) 10(9):2223. doi: 10.3390/foods10092223
13. Chen H, Pei X, and Chen Q. Practical chinese breast disease. Beijing: China Traditional Chinese Medicine Press Co (2023).
14. Li J and Ma L. Glossary of clinical symptoms in chinese medicine. In: Clinical terminology of common symptoms in chinese medicine. Beijing: China Medical Science Press (2005).
15. Yao N. Differential diagnosis of symptoms in chinese medicine. In: Differential diagnosis of symptoms in chinese medicine. Beijing: The People's Health Press (2000).
16. Wang S, Yu S, Zhao X, Dai Q, Chen Z, and Xu S. Current status and strategies of research on evidence-based clinical diagnosis and treatment guidelines in traditional chinese medicine. Chin J Traditional Chin Med. (2012) 27:2759–63.
17. Yu Q, Xu C, Song J, Jin Y, and Gao X. Mechanisms of traditional chinese medicine/natural medicine in HR-positive breast cancer: a comprehensive literature review. J Ethnopharmacology. (2024) 319(Pt 3):117322. doi: 10.1016/j.jep.2023.117322
18. Zhao X, Luo T, Qiu Y, Yang Z, Wang D, Wang Z, et al. Mechanisms of traditional Chinese medicine overcoming of radiotherapy resistance in breast cancer. Front Oncol. (2024) 14. doi: 10.3389/fonc.2024.1388750
19. Wang W, Yuan J, Zhu Y, and Li R, and Zhang J-G. Traditional Chinese Medicine (TCM) enhances the therapeutic efficiency of Gemcitabine-loaded injectable hydrogel on postoperative breast cancer through modulating microenvironment. J Materials Chem B. (2025) 13(16):4864–78. doi: 10.1039/D4TB02776K
20. Chen J, Xu H, Zhao X, Hu L, Wan X, and Zhi N. A bibliometric study on the macro-differentiation standards of liver depression syndrome. J Beijing Univ Chin Med. (2004) 04):1–4.
21. Liu X, Chen Z, and Guo Q. A preliminary study on the symptom scale of liver qi stagnation syndrome. J Hunan Univ Traditional Chin Med. (2007) 01):48–51.
22. Fang G, Zhou X, Chen J, Li X, Fan X, Liao X, et al. Construction of a diagnostic scale for liver depression and qi stagnation certificate based on delphi method and hierarchical analysis. J Traditional Chin Med. (2022) 63:1525–31.
23. Niu J and Dai J. Progress in the study of traditional Chinese medicine diagnosis and treatment of thyroid cancer. Chin J Basic Chin Med. (2020) 26:1739–42.
24. Li X and Yuan H. Improving the efficacy of traditional Chinese medicine in the treatment of primary hepatocellular carcinoma from the perspective of etiology and pathogenesis. J Clin Hepatobiliary Dis. (2021) 37:2001–4.
25. Chen S. Surgery: A series of ancient books on chinese medicine. Beijing: Chinese Ancient Books Publishing House (1999).
26. Yang J, Gao W, and Huang J. Exploration of the identification ideas and treatment experience of breast cancer. Chin J Traditional Chin Med. (2024) 39:2945–8.
27. Lin H. Guidelines for chinese medicine treatment of Malignant tumors. Beijing: People’s Health Publishing House (2014).
28. Zhang Z and Liu L. Exploration of the potential molecular mechanism of the treatment of triple-negative breast cancer with Free San based on single-cell RNA sequencing and network pharmacology approach. New Chin Medicines Clin Pharmacol. (2022) 33:1519–27.
29. Xu S, Li R, and Liu L. Reversal of energy metabolism reprogramming in MDA-MB-231 cells of breast cancer by serum containing Dang jia wu shan. Chin J Exp Formulas. (2022) 28:8–14.
30. Liu L, Ni Y, and Yin F. Efficacy of Chai Hu Shu Hepatosan plus reduction combined with CAF regimen in the treatment of stage III breast cancer and its effect on serum MMPs, estrogen levels and tumor markers. Chin herbal Med. (2020) 43:220–3.
31. Wang W, Yang L, Li W, Sun Y, Sun H, Chen Y, et al. Multi-omics driven paradigm for construction of traditional Chinese Medicine Zheng (syndrome) diagnosis and treatment model, taking Shi Zheng (syndrome of dampness) as an example. Chin Med. (2025) 20(1):33. doi: 10.1186/s13020-025-01085-2
32. Starostin RA, Kuzmina SV, and Gataullin IG. Prevalence of depressive disorders in breast cancer patients. Eur Psychiatry. (2024) 67:S70–0. doi: 10.1192/j.eurpsy.2024.190
33. Sadaqa D, Farraj A, Naseef H, Alsaid H, Al-Shami N, and AbuKhalil AD. Risk of developing depression among breast cancer patients in Palestine. BMC Cancer. (2022) 22(1):295. doi: 10.1186/s12885-022-09420-8
34. Peña-Vargas C, del Río-Rodriguez P, Rosario LP, Laporte-Estela G, Torres-Blasco N, Rodriguez-Castro Z, et al. Losses related to breast cancer diagnosis: the impact on grief and depression symptomatology within the context of hispanic/latina patients with breast cancer. Healthcare. (2025) 13(6):624. doi: 10.3390/healthcare13060624
35. Weng C-H, Javan Biparva A, Raoofi S, Rafiei S, Masoumi M, Doustmehraban M, et al. Global depression in breast cancer patients: Systematic review and meta-analysis. PloS One. (2023) 18(7):e0287372. doi: 10.1371/journal.pone.0287372
36. Tong Y, Zhao G, Shuang R, Wang H, and Zeng N. Saikosaponin a activates tet1/dll3/notch1 signalling and promotes hippocampal neurogenesis to improve depression-like behavior in mice. J Ethnopharmacology. (2024) 319(Pt 3):117289. doi: 10.1016/j.jep.2023.117289
37. Wang B, Lu S, Zhang C, Zhu L, Li Y, Bai M, et al. Quantitative proteomic analysis of the liver reveals antidepressant potential protein targets of Sinisan in a mouse CUMS model of depression. Biomedicine Pharmacotherapy. (2020) 130:110565. doi: 10.1016/j.biopha.2020.110565
38. Zhou Z, Wang Y, Sun S, Zhang K, Wang L, Zhao H, et al. Paeonia lactiflora Pall. Polysaccharide alleviates depression in CUMS mice by inhibiting the NLRP3/ASC/Caspase-1 signaling pathway and affecting the composition of their intestinal flora. J Ethnopharmacology. (2023) 316:116716. doi: 10.1016/j.jep.2023.116716
39. Gosain R, Gage-Bouchard E, Ambrosone C, Repasky E, and Gandhi S. Stress reduction strategies in breast cancer: review of pharmacologic and non-pharmacologic based strategies. Semin Immunopathology. (2020) 42:719–34. doi: 10.1007/s00281-020-00815-y
40. Yu S, Li W, Tang L, Fan X, Yao S, Zhang X, et al. Depression in breast cancer patients: Immunopathogenesis and immunotherapy. Cancer Lett. (2022) 536:215648. doi: 10.1016/j.canlet.2022.215648
41. Ma W, Liu P, Zheng J, Lü J, Zhao Q, Li D, et al. Immune and nonimmune mechanisms mediate the mental stress-induced tumor growth in a xenograft model of breast cancer. Cell Death Dis. (2021) 12(11):987. doi: 10.1038/s41419-021-04280-9
42. Zheng Y, Wang N, Wang S, Zhang J, Yang B, and Wang Z. Chronic psychological stress promotes breast cancer pre-metastatic niche formation by mobilizing splenic MDSCs via TAM/CXCL1 signaling. J Exp Clin Cancer Res. (2023) 42(1):129. doi: 10.1186/s13046-023-02696-z
43. Zheng Y, Zhan D, Hong S, Wang N, and Wang Z. Study on the mechanism of action of Si-Ni San in regulating glycolysis to inhibit chronic psychological stress-mediated breast cancer progression. J Traditional Chin Med Oncol. (2022) 4:50–9.
44. Wang Y-T, Wang X-L, Wang Z-Z, Lei L, Hu D, and Zhang Y. Antidepressant effects of the traditional Chinese herbal formula Xiao-Yao-San and its bioactive ingredients. Phytomedicine. (2023) 109:154558. doi: 10.1016/j.phymed.2022.154558
45. Tang K-R, Mo X-W, Zhou X-Y, Chen Y-Y, Liu D-D, He L-L, et al. Xiaoyao San, a Chinese herbal formula, ameliorates depression-like behavior in mice through the AdipoR1/AMPK/ACC pathway in hypothalamus. J Integr Med. (2022) 20:442–52. doi: 10.1016/j.joim.2022.07.003
Keywords: breast cancer, liver depression syndrome, systematic review, Chinese medicine syndrome, clinical application
Citation: Wu P, Mao S, Zuo Q, Guo Q and Chen Q (2025) A systematic review and exploration of clinical application of liver depression syndrome in breast cancer. Front. Oncol. 15:1614903. doi: 10.3389/fonc.2025.1614903
Received: 20 April 2025; Accepted: 23 July 2025;
Published: 11 August 2025.
Edited by:
Zhi-Xiang Xu, University of Alabama at Birmingham, United StatesCopyright © 2025 Wu, Mao, Zuo, Guo and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qianqian Guo, Z3VvcWlhbnFpYW5AZ3p1Y20uZWR1LmNu; Qianjun Chen, Y3FqNTVAMTYzLmNvbQ==
 Peng Wu
Peng Wu Siying Mao
Siying Mao Qian Zuo
Qian Zuo Qianqian Guo
Qianqian Guo Qianjun Chen
Qianjun Chen