- Jiang Xi University of Traditional Chinese Medicine, Nanchang, China
Background: Acupuncture is highly controversial in enhancing the quality of sleep and the risk of emotional maladjustment in breast cancer patients. Through a comprehensive meta-analytic approach, this study intends to investigate the effects of acupuncture on enhancing sleep quality and the risk of emotional maladjustment in patients diagnosed with breast carcinoma.
Methods: Search tactics aligned with Cochrane Collaboration recommendations. Systematic electronic searches were conducted in April 2025 across several data storage, including PubMed, Embase, Web of Science, the Cochrane Library, and Scopus. The reference lists of review essay were manually searched to refine potentially eligible studies. A pair of researchers independently performed a comprehensive literature review, conducted data extraction, and assessed the risk of bias. Outcome analysis included the quality of sleep and the risk of emotional maladjustment. For continuous measures, the pooled weighted mean difference (MD) and 95% confidence interval will be estimated. The meta-analysis was conducted using the Review Manager 5.3 and Stata 16.0 statistical software platforms.
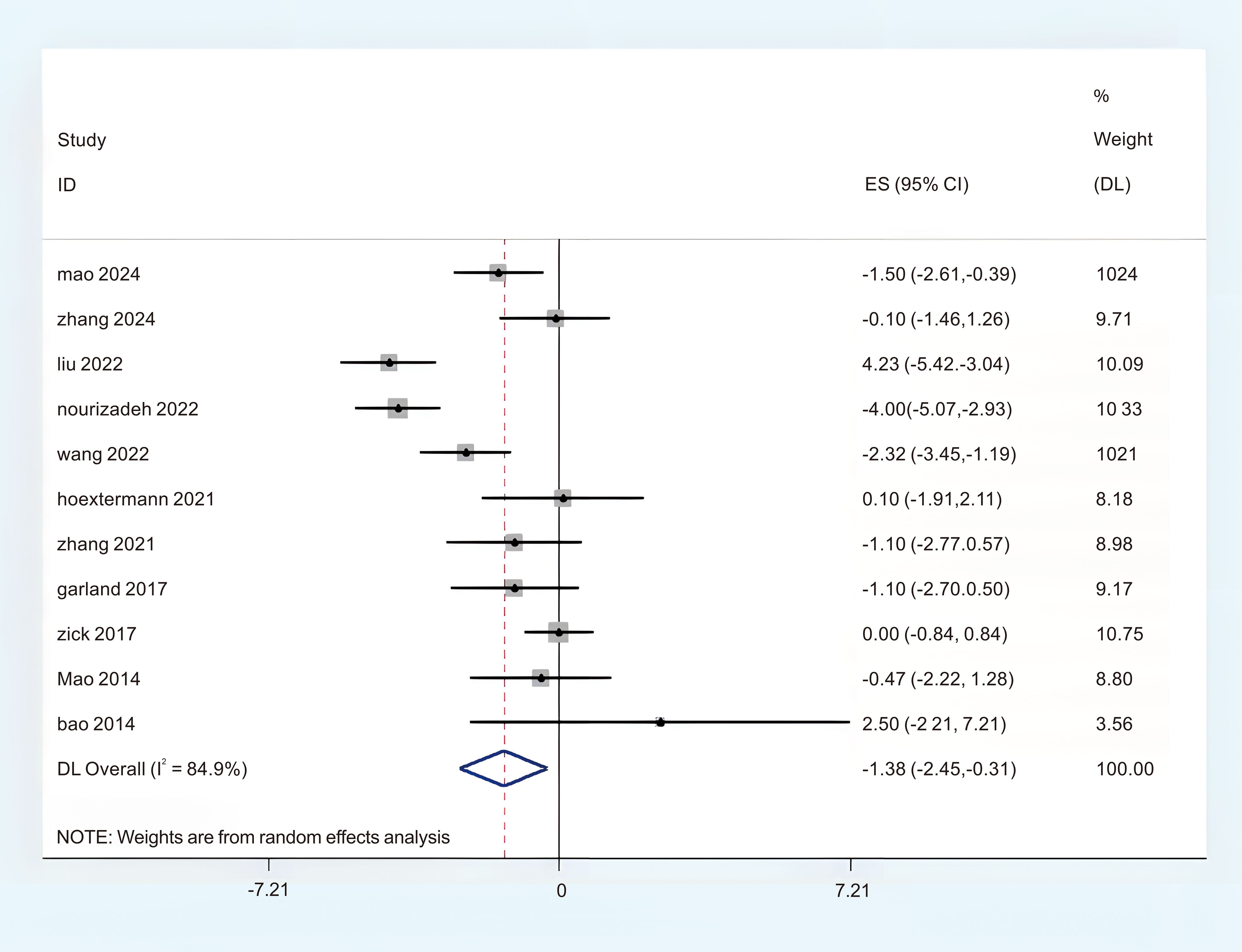
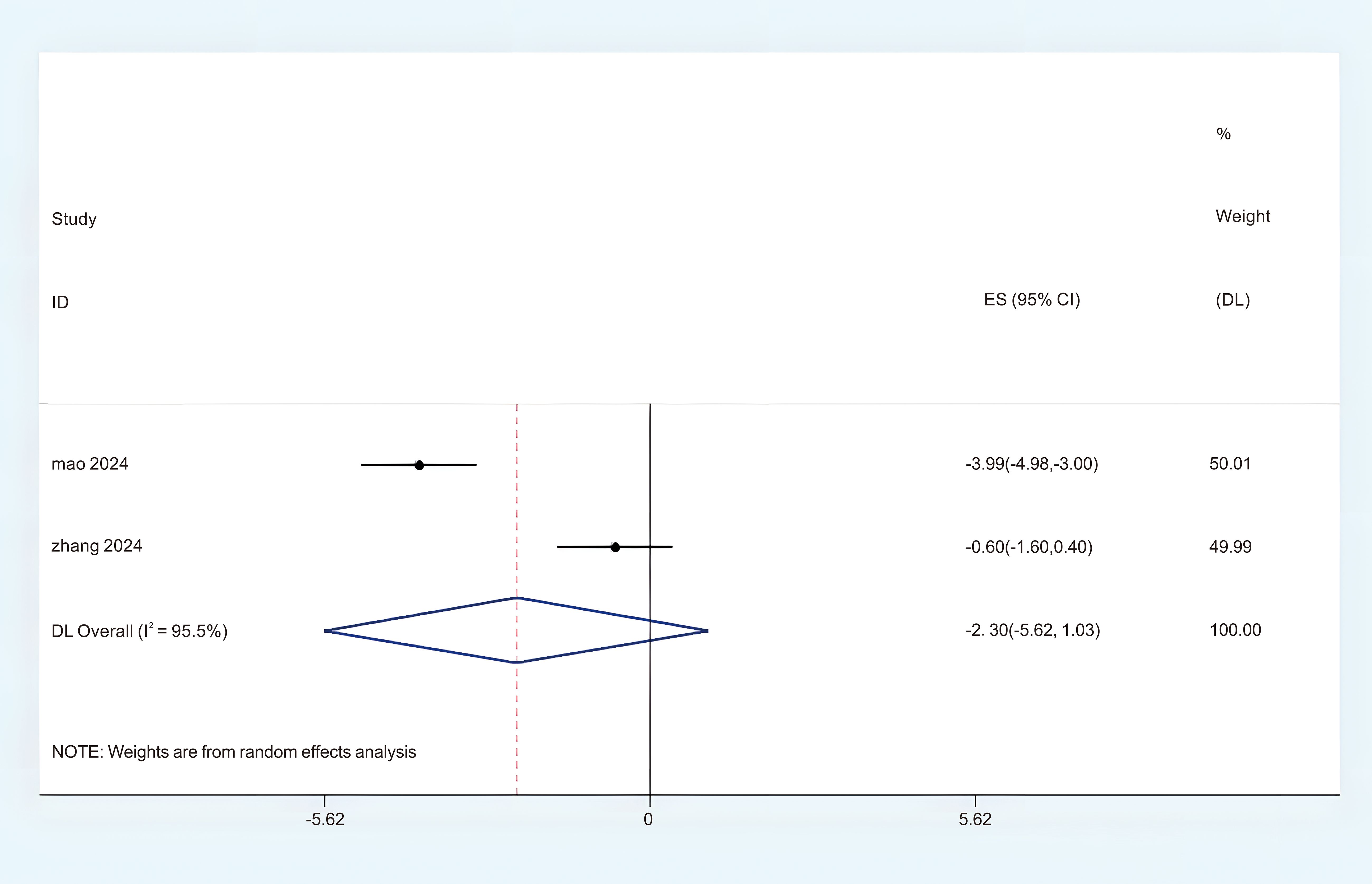
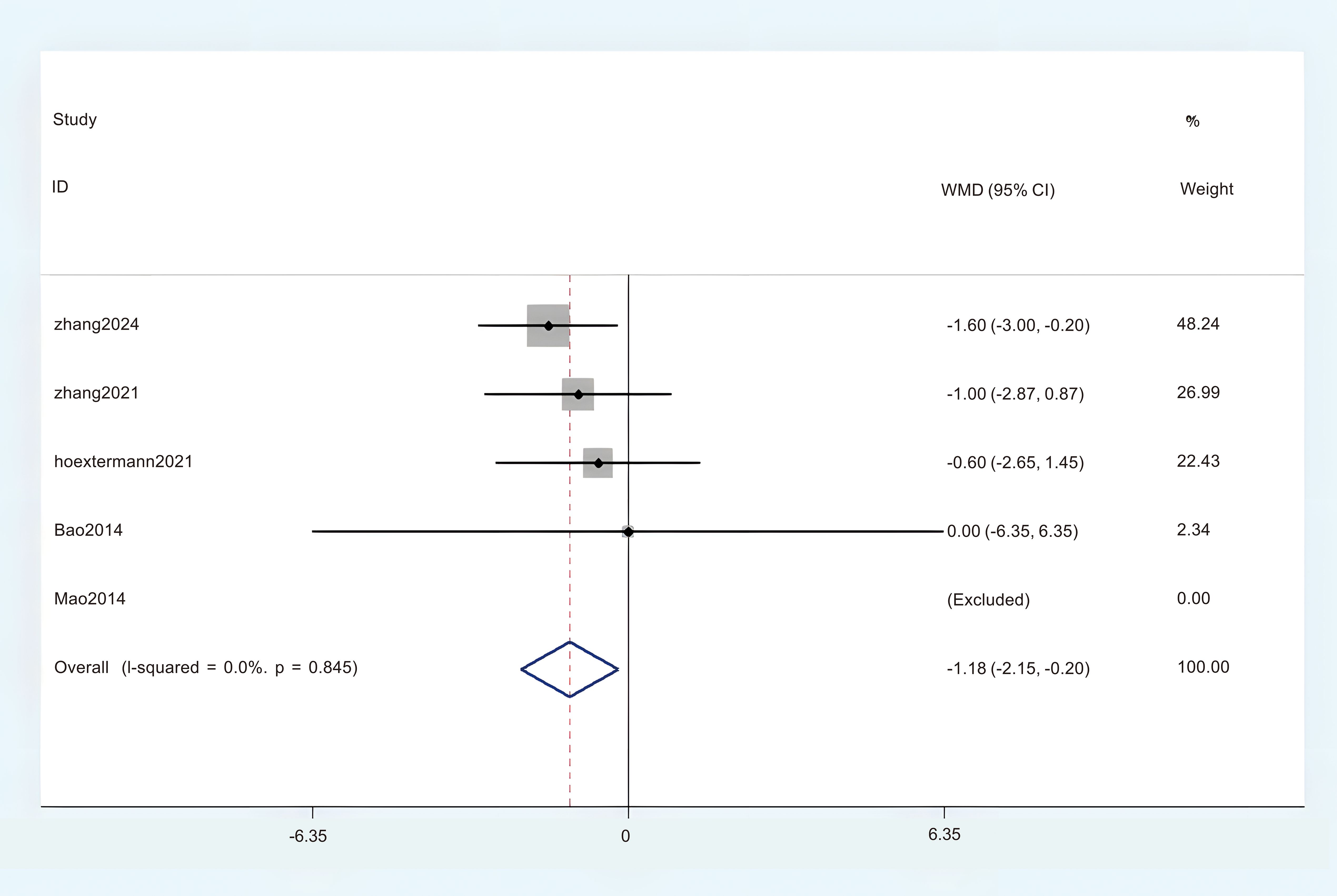
Result: A total of 11 studies involving 1116 participants were included. Statistically significant differences were found between acupuncture and control group in Pittsburgh Sleep Quality Index (PSQI) (MD = -1.38, 95%CI = -2.45 to -0.31), Insomnia Severity Index (ISI) (MD = -1.11, 95%CI = -3.68 to 1.45), Brief Fatigue Scale (BFI) score (MD = -2.30, 95%CI = -5.62 to -1.03). Acupuncture has been shown to Boost sleep quality and reducing the risk of emotional maladjustment. Specifically, it is manifested in: Hospital Anxiety and Depression Scale (HADS-A) (MD = -1.24, 95%CI = -2.41 to -0.35) and Hospital Anxiety and Depression Scale (HADS-D) (MD = -1.18, 95%CI = -2.15 to -0.20).
Conclusion: In comparison to other standard treatment modalities, acupuncture exhibits a notable distinction in boosting the sleep quality and the risk of emotional maladjustment of breast cancer patients. However, Clinicians should exercise caution when applying these results, as the available evidence suffers from methodological biases and quality limitations.
Introduction
Breast cancer is the most prevalent form of cancer among women globally, predominantly affecting those aged between 41 and 60 years. In 2014, the National Cancer Institute reported an incidence rate of 5,609 cases per 100,000 women (1). In a document, Global Cancer Statistics 2020, Breast cancer has now overtaken lung cancer. It has 2.26 million cases (2). In female patients, Breast cancer has become the leading malignant cancer in women. With the rising standard of living, the survival rates for breast cancer are improving. His 5-year survival rate is 90% (3). Sleep quality is most prominently observed in the progression of breast cancer patients (4). A systematic review demonstrated that 62% of quality-of-life deterioration in breast cancer cases was attributable to sleep disturbances (5). In the lives of patients with breast cancer, disturbances in sleep significantly impact their life (6). The incidence of symptoms associated with breast cancer, including fatigue, anxiety, and depression, is notably high. These symptoms significantly increase the risk of emotional dysregulation (7). Therefore, sleep disorders and the risk of emotional maladjustment in breast cancer patients have increasingly attracted attention in clinical and research fields.
There are both pharmacological and non-pharmacological approaches to improving symptom of individuals with breast cancer. These methods can cause tolerance of the drug. During the treatment process of breast cancer, there is this interaction between anti-cancer drugs and sleep medications (8). Therefore, people are looking for various ways to treat sleep problems caused by breast neoplasm and boost their quality of life (9). Exercise (10), acupuncture (11), tai chi (12), yoga exercises (13). Of these methods, acupuncture works best. Acupuncture has a long history as a means of treatment, and acupuncture as a treatment has received a lot of popularity both at home and abroad (14). Acupuncture includes acupuncture and moxibustion. Acupuncture is by piercing small needles into the corresponding acupuncture points to make them “qi” (15). Acupuncture improves the body’s immune function (16). Moxibustion is a method of moxibustion that achieves a therapeutic effect through thermal stimulation of acupuncture points and acupuncture and moxibustion can be used as a treatment method that can be used in conjunction with each other, such as the combination of acupuncture and moxibustion (17). Currently, research has been conducted on the enhancement of quality of life in breast neoplasm treatment through acupuncture. Some research has indicated that acupuncture may enhance the life in breast cancer patients by promoting better sleep quality (18). Acupuncture may enhance sleep quality while concurrently alleviating distress associated with psychiatric symptoms (19). Acupuncture has been shown to be safe for sleep quality (20, 21). However, relevant studies have indicated that the clinical efficacy of acupuncture interventions for cancer-related insomnia and the risk of emotional maladjustment still requires further evidence from randomized controlled trials and systematic reviews to support its validity (22). It cannot be definitively stated that acupuncture is demonstrates efficacy in managing insomnia and emotional maladjustment associated with cancer (23).
Therefore, we conducted this meta-analysis to reevaluate the impact of acupuncture intervention on improving sleep quality and risk of emotional maladjustment in breast cancer patients. This analysis incorporates recent high-quality randomized controlled trials (RCTs) that were not included in previous studies.
Methods
Because this research is a systematic review and meta-analysis of published studies, ethical approval is not necessary. According to the guidelines established by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), we conducted a meta-analysis (24), and the guidelines for Assessing the Methodological Quality of Systematic Reviews (AMSTAR) (25). The International Prospective Register of Systematic Reviews has registered this review under CRD420251025827. For details, please refer to attachment 1 of the attached upload materials.
Search strategy
Search tactics aligned with Cochrane Collaboration recommendations. Systematic electronic searches were conducted in April 2025 across several databases, including PubMed, Embase, Web of Science, the Cochrane Library, and Scopus. Randomized controlled trials were undertaken to investigate the outcome of acupuncture on sleep quality and the risk of emotional maladjustment in breast carcinoma patients. To enhance the comprehensiveness of our review, we also conducted a manual search of the references cited in the included studies. We constructed the search formula by combining Medical Subject Headings (MeSH) with non-MeSH terms (free text). The specific keywords included “acupuncture therapy”, “breast neoplasms”, and “randomized controlled trial”. Comprehensive strategies for detailed keyword searches are obtainable in Multimedia Appendix 1.
Selection and exclusion criteria
To reduce bias, the studies that aligned with the search strategy were carefully examined and included based on the following criteria: (1) Population: Insomnia patients among breast cancer survivors; (2) Intervention: acupuncture or acupressure; (3) Comparison: No acupuncture treatment or acupressure was performed; (4) Outcome measures: sleep quality and risk of emotional maladjustment; (5) Study design: a randomized controlled trial.
Exclusion criteria: (a) Studies including Non-breast cancer patients; (b) Cases, practice guides, test protocols or reviews; (c) Experimental data are incomplete; (d) There are no full-text or non-RCTs.
Data extraction
The data extraction was conducted independently by two authors, and any Discrepancies in opinions were resolved by discussion with the third author to establish consensus. The extraction of information was conducted systematically, encompassing various elements such as the first author name, publication year, country of origin, demographic age ranges, the number of experimental and control groups, diagnostic criteria utilized, interventions applied, observed clinical outcomes, and any additional pertinent information.
Risk of bias assessment
Utilizing the Cochrane Risk of Bias tool, we analyzed the risk of bias in randomized controlled trials (RCTs) as high, low, or unclear. The components involved in bias assessment included, generation of random sequences and concealment of distribution, the implementation of a blind method for both participants, blinding of outcome assessments, selective reporting, and the management of incomplete outcome data (26). If the two authors do not reach a consensus in the process of assessing the risk, a third reviewer will resolve the assessment differences.
Quality of evidence
According to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system, the strength of evidence for each research outcome is assessed and classified into quality ratings. There were varying levels of evidence, including very low, low, moderate, and high.
Data synthesis
The research performed a meta-analysis utilizing the RevMan 5.3 software developed by the Cochrane Collaboration. For continuous data, mean differences (MD) along with their corresponding 95% confidence intervals (CI) were employed for statistical analysis. Researchers measure the odds ratio (OR) along with its 95% confidence interval (95% CI) utilizing the primary model. Heterogeneity was measured by P-values and I² statistics. When P > 0.10 and I² < 50%, it can be determined that there is no significant heterogeneity among the data sets; therefore, a fixed effects model (FEM) is employed. Conversely, when P < 0.10 and I² > 50%, which indicates significant heterogeneity, the random-effects model (REM) was utilized. In instances characterized by significant heterogeneity, we conducted sensitivity analyses or subgroup analyses to investigate the underlying sources of this heterogeneity. According to the origin of the country, it is divided into 2 subgroups: China and Unite States. According to the interventions, it is divided into 2 subgroups: acupuncture and acupressure. According to the Course of intervention, it is divided into 2 subgroups: third week and sixth week. Furthermore, when the number of included studies exceeded 10, funnel were created to identify possible publication bias in the literature reviewed.
Results
Study selection and characteristics
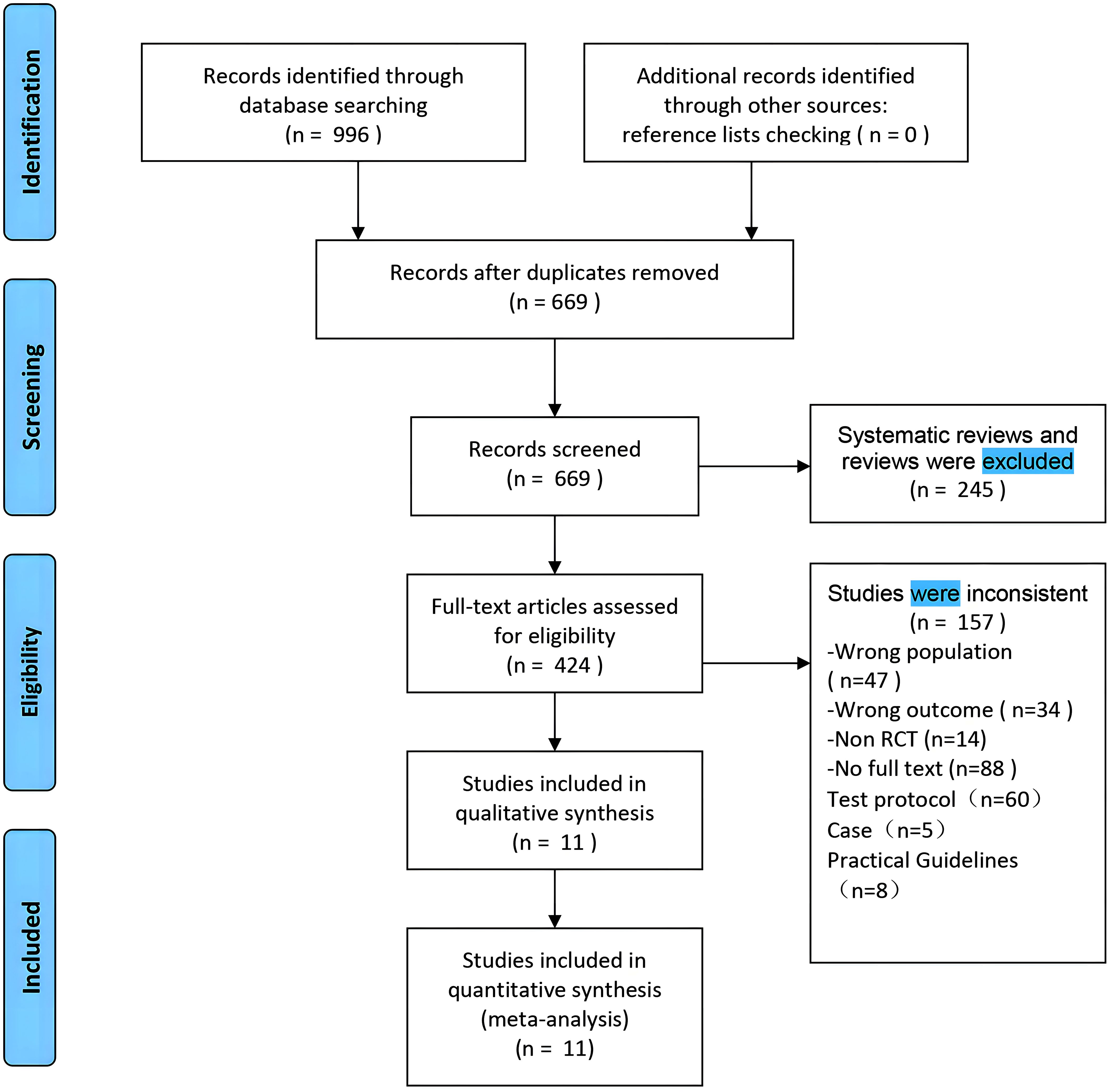
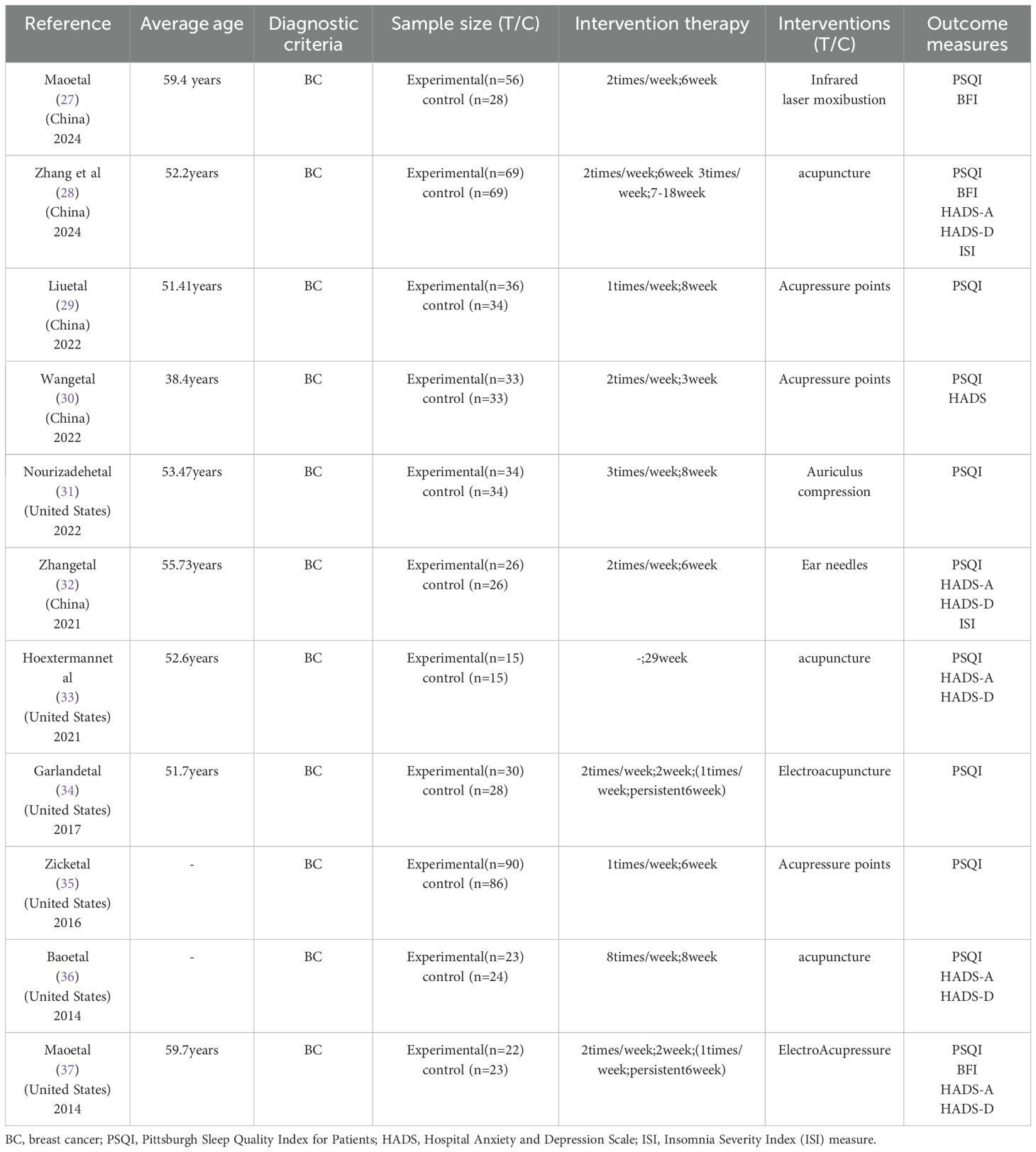
Using the search strategy, 996 articles were retrieved from the database. After removing duplicates (669 articles remained), we excluded the remaining articles: reviews, non-RCTs, no full text, trial protocols, case reports, practice guidelines, and study populations. This process resulted in 11 randomized controlled trials articles included in the meta-analysis (27–37). The process of retrieval and selection is illustrated in Figure 1. The characteristics of these literatures are concluded in Table 1. The study included a total of 836 women with breast cancer sleep disorders with an average age of about 50 years. The participants were effectively divided into 2 groups, acupuncture (n = 436) and non-acupuncture (n = 400). Regarding outcomes, Eleven studies provided Patient Pittsburgh Sleep Quality Index (PSQI) (27–37), two studies reported the Change in score of Insomnia Severity Index (ISI) (28, 32), three studies investigated the Brief Fatigue Scale (BFI) score (27, 28, 37), five studies investigated the Hospital Anxiety and Depression Scale (HADS-A) (28, 32, 33, 36, 37), five studies investigated the Hospital Anxiety and Depression Scale (HADS-D) (28, 32, 33, 36, 37).
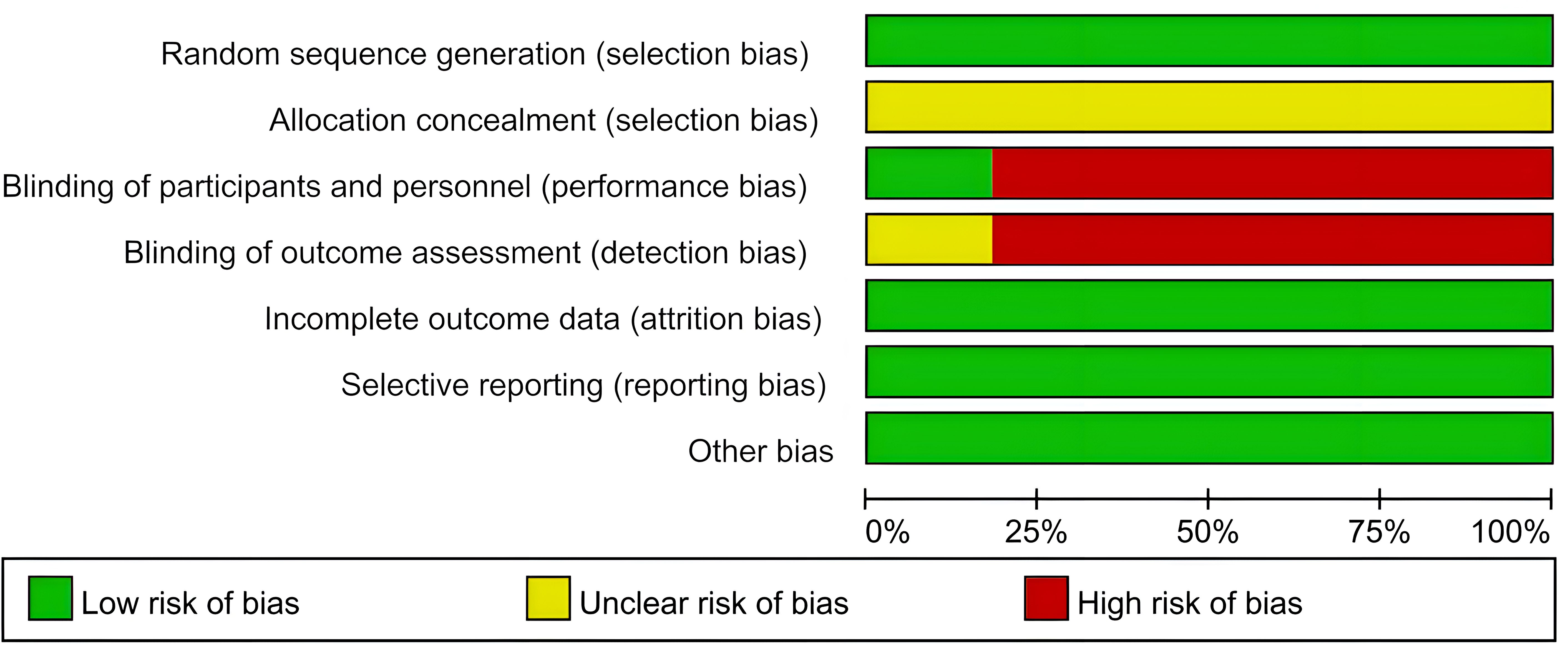
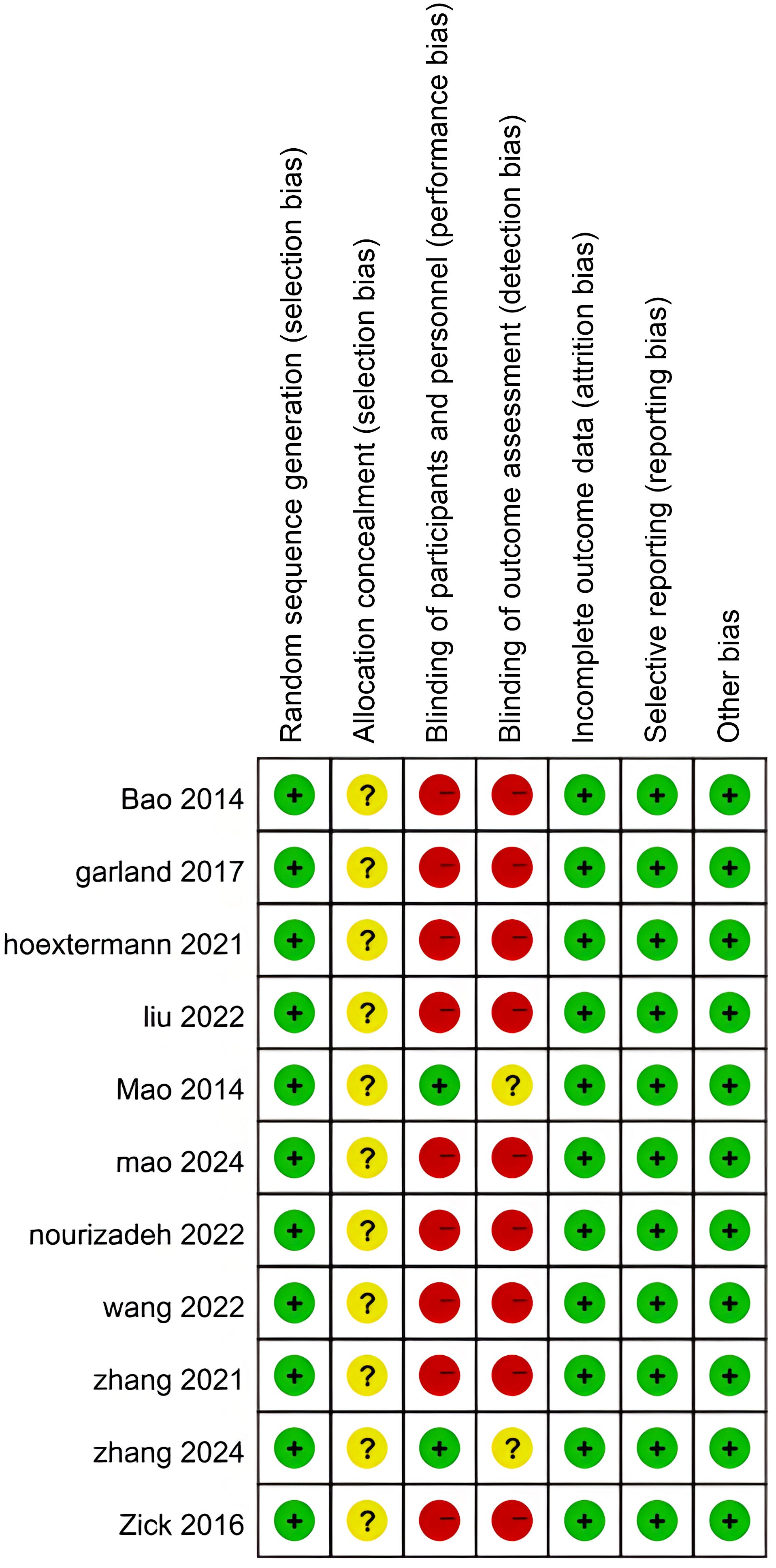
Study quality and risk of bias
The quality of the trials included in this review was assessed using the Cochrane tool. Detailed results can be found in Figures 2 and 3. In 11 studies, the description of proper random sequence generation was provided (27–37). 2 trails provided adequate blind (28, 37). All studies followed up data and the data were complete, and Detailed results are shown in Table 2.
Primary outcomes
The PSQI
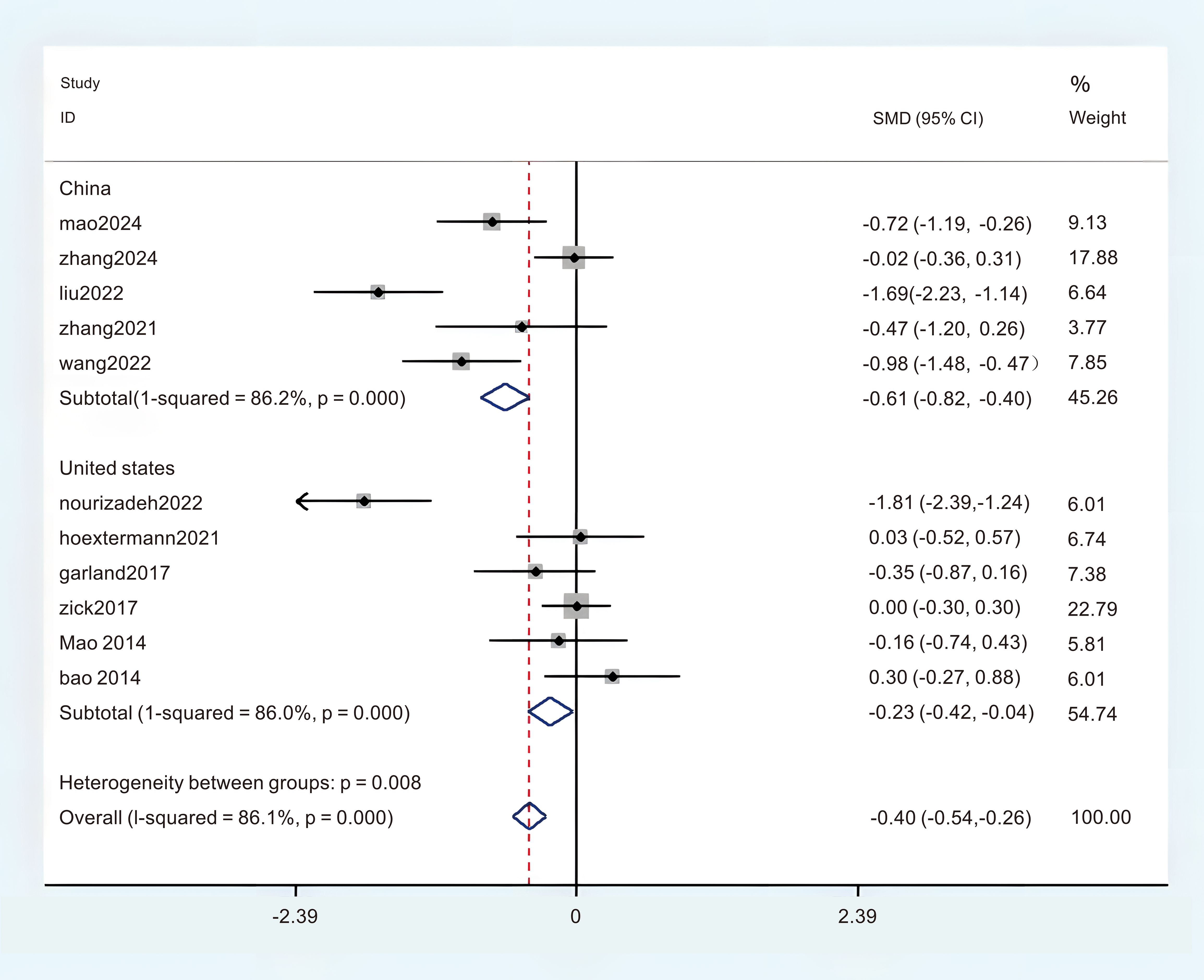
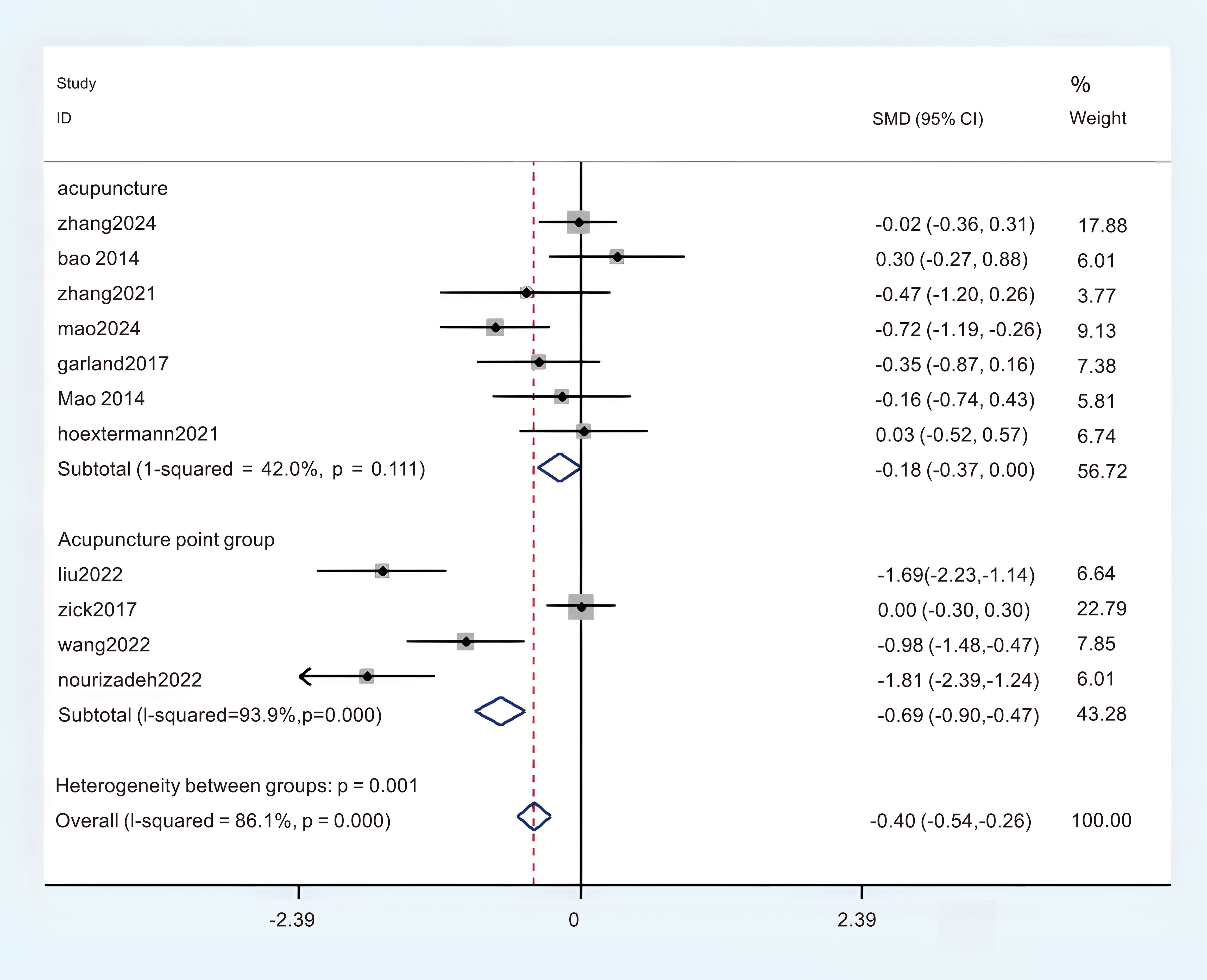
A total of 11 studies provided adequate data on the Pittsburgh Sleep Quality Index (PSQI), which were obtained in the meta-analysis. There was a notable degree of heterogeneity observed, leading to the selection of the REM (P < 0.1, I2 = 84.9%). The findings from the random effects meta-analysis indicated that acupuncture demonstrated a more pronounced effect on enhancing sleep quality compared to the experimental comparison group. (MD = -1.38; 95%CI = -2.45 to -0.31; Figure 4). To identify the sources of heterogeneity and assess the correlation of the Pittsburgh Sleep Quality Index (PSQI) across different countries, we categorized the PSQI results into two subgroups based on these nations. There were five studies conducted in China that provided data on the Pittsburgh Sleep Quality Index (PSQI), revealing a notable variability in the aggregated outcomes (P < 0.05, I2 = 86.2%), and six studies provided the Pittsburgh Sleep Quality Index (PSQI) data from the United States, revealing a notable variability in the aggregated outcomes (P < 0.05, I2 = 86.0%). In this subgroup analysis, a random effects model (REM) was employed as the statistical method. The results of the synthesis across subgroups are presented as follows: (1) in China (MD = -0.61; 95% CI = -0.82 to -0.40; Figure 5); (2) in Unite states (MD = -0.23; 95% CI = -0.29 to 0.25; Figure 5); In order to clarify the sources of heterogeneity and assess the relationship between PSQI and intervention models, we categorized the PSQI results into two subgroups based on two distinct intervention models. There were seven studies that utilized the Pittsburgh Sleep Quality Index (PSQI) in acupuncture research, revealing no substantial heterogeneity present within the aggregated data (P < 0.05, I2 = 42.0%). The Finite Element Method (FEM) was employed in the analysis of this subgroup. Four studies administered the Pittsburgh Sleep Quality Index (PSQI) in relation to acupressure, revealing a significant heterogeneity among the pooled data (P < 0.05, I2 = 93.9%), The REM was employed for this subgroup analysis. The results of the synthesis across subgroups are presented as follows: (1) acupuncture (MD = -0.18; 95% CI = -0.37 to 0.00; Figure 6); (2) acupressure (MD = -0.69; 95% CI = -0.90 to -0.47; Figure 6). The overall certainty of this evidence was assessed to be moderate to very low.
The BFI
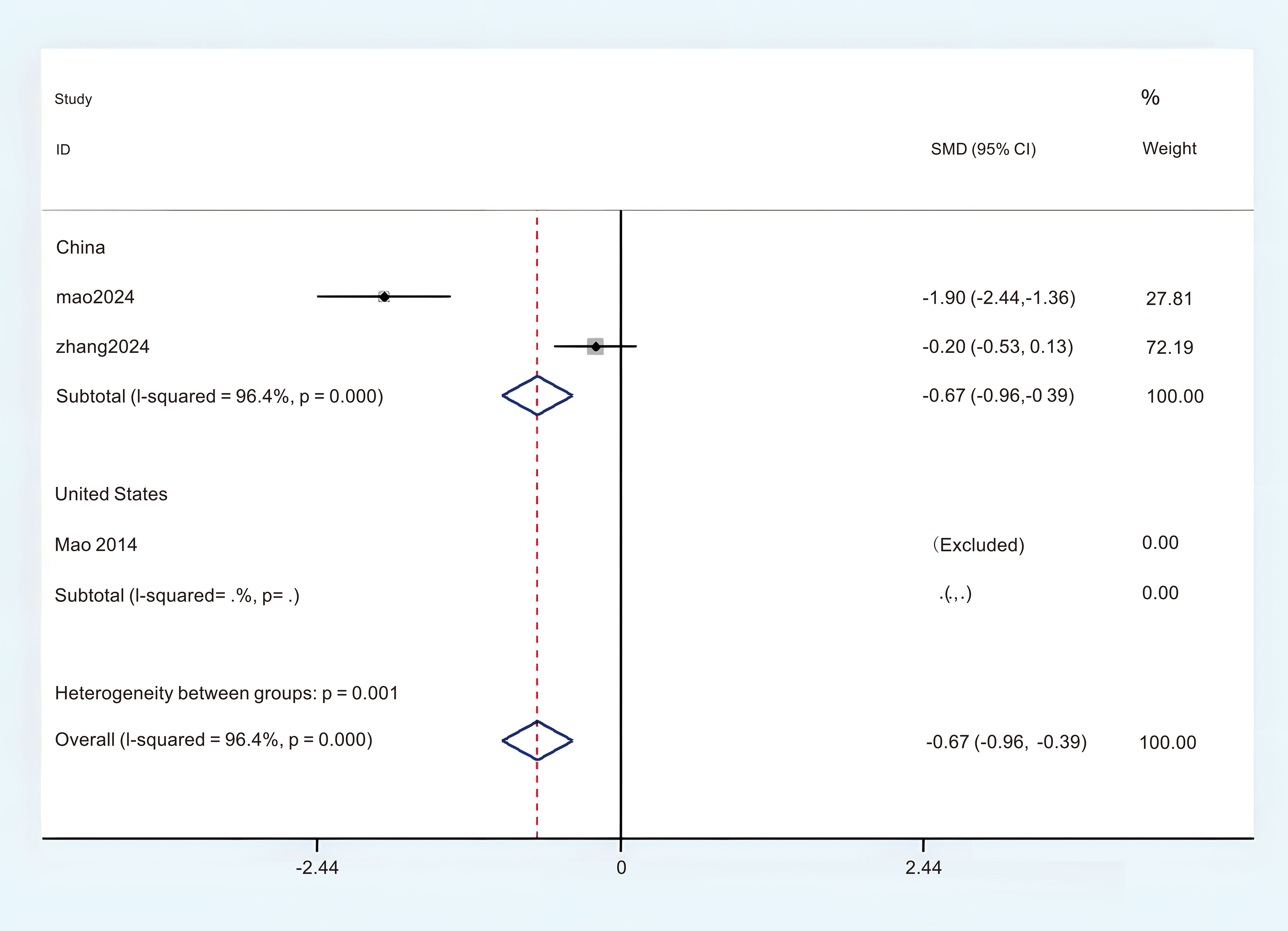
Three studies provided sufficient data regarding BFI for this meta-analysis. Based on the observed significant heterogeneity, a random effects model (REM) was determined to be appropriate (P < 0.05, I2 = 95.5%). The findings from the random effects meta-analysis indicated that acupuncture demonstrated a significantly greater impact on the enhancement of BFI compared to the control group. (MD = -2.30; 95%CI = -5.62 to -1.03; Figure 7). In order to investigate the sources of heterogeneity and assess the relationship of BFI across different countries, we classified the BFI results into two subgroups based on the circumstances of these two nations. There were two studies that administered the BFI in China, revealing a notable variability in the aggregated outcomes (P < 0.05, I2 = 96.4%). In this analysis, a random effects model (REM) was employed. The results of the subgroup synthesis are presented as follows: (1) in China (MD = -0.67; 95% CI = -0.96 to -0.39; Figure 8). The overall certainty of this evidence was assessed to be moderate to very low.
The ISI
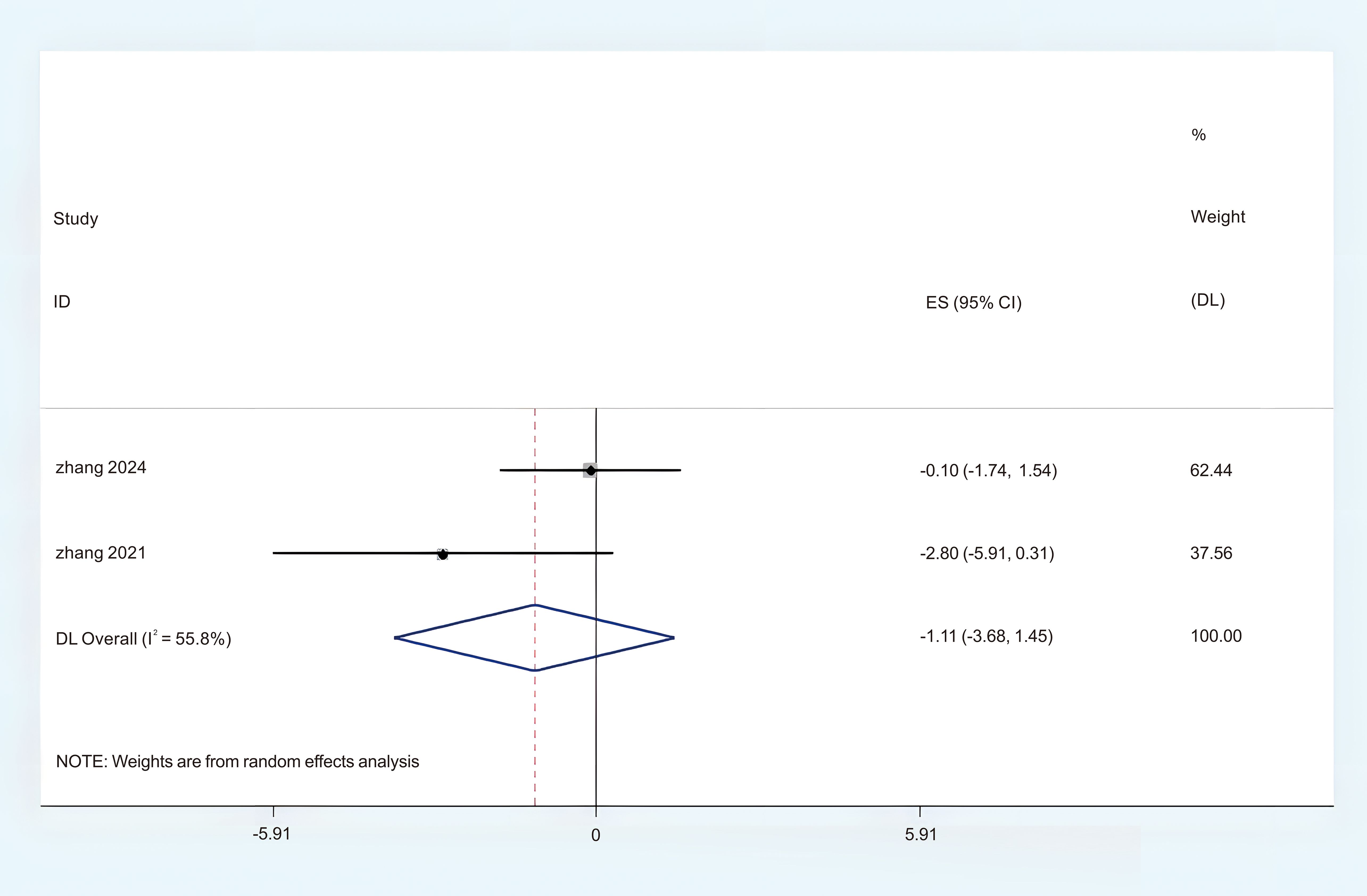
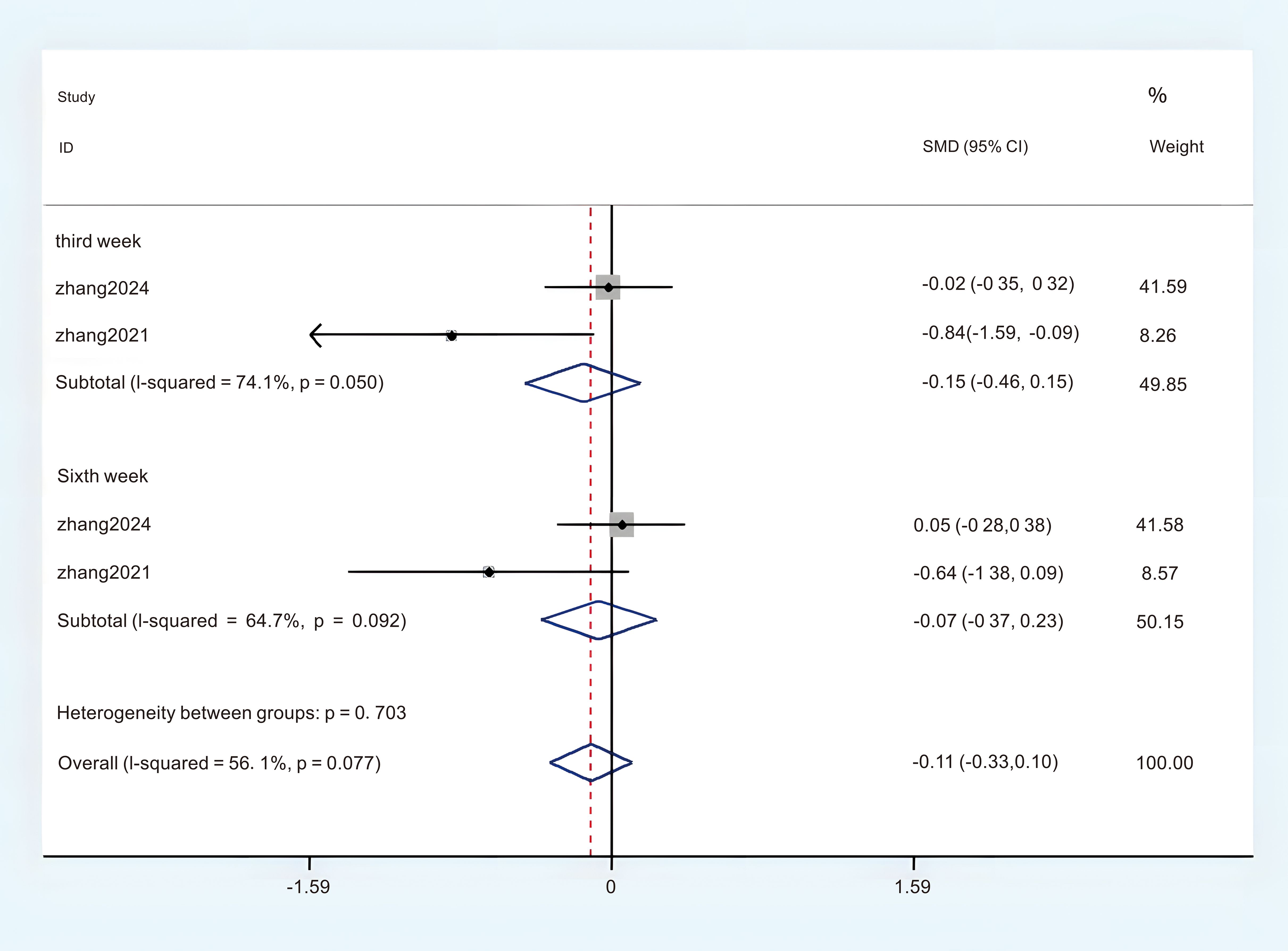
Two studies provided sufficient ISI data, which can be incorporated into this meta-analysis. Significant heterogeneity was observed, prompting the selection of a Random Effects Model (REM) (P < 0.05, I2 = 55.8%). The results of the meta-analysis given by random effects showed that acupuncture had a more significant effect on the improvement of ISI than the control group. (MD = -1.11; 95%CI = -3.68 to 1.45; Figure 9). Subgroup analyses were conducted to investigate potential sources of heterogeneity and examine the relationship between ISI scores and intervention sessions. The results stratified by intervention session duration demonstrated: (1) third week (MD = -0.15; 95% CI = -0.46 to -0.15; Figure 10); (2) sixth week (MD = -0.07; 95% CI = -0.37 to -0.23; Figure 10). The overall certainty of this evidence was assessed to be moderate to very low.
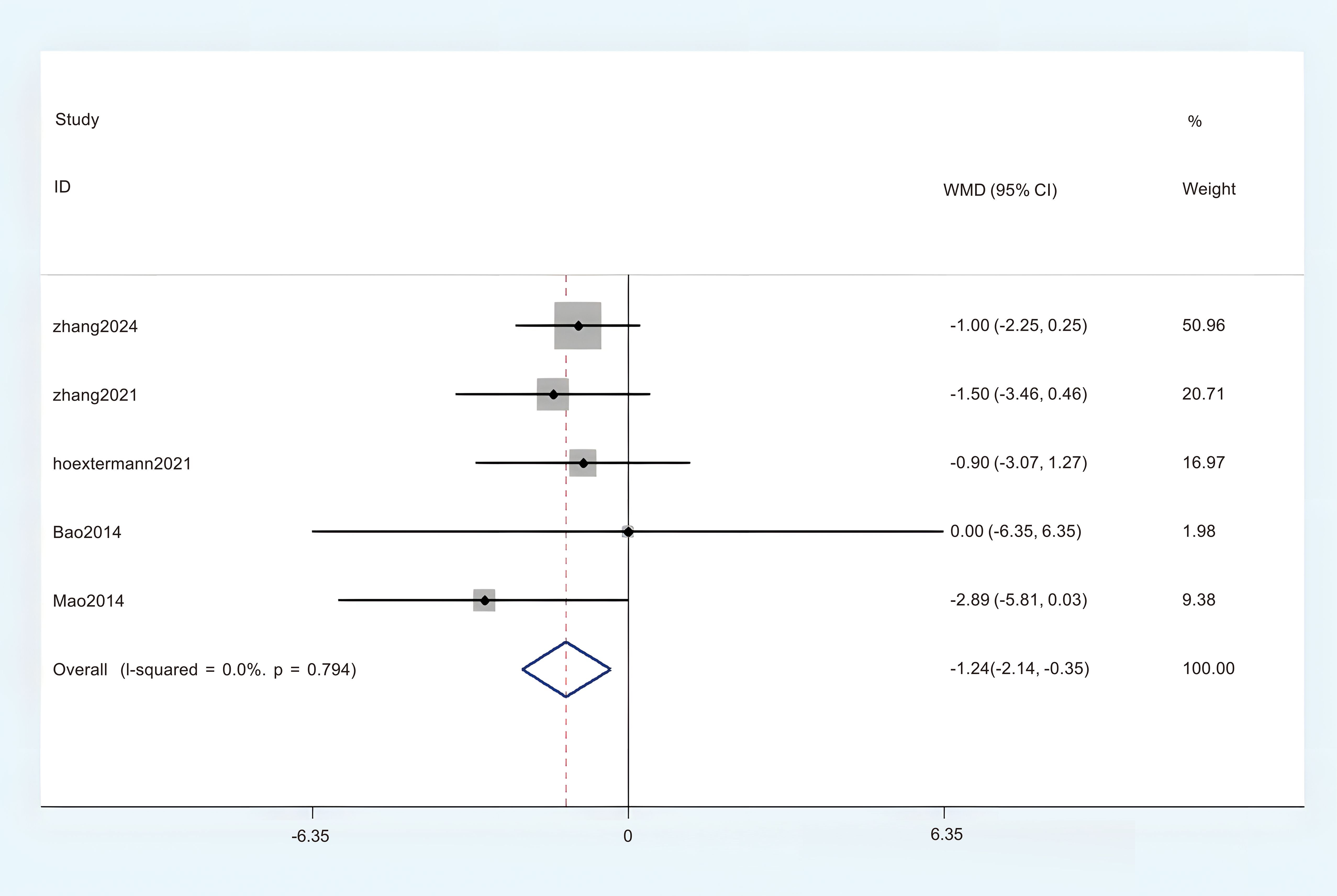
The HADS-A
Five studies provided sufficient data on the Hospital Anxiety and Depression Scale - Anxiety subscale (HADS-A) for this meta-analysis. No significant heterogeneity was observed, and a fixed-effects model (FEM) was employed (P < 0.1, I2 = 0%). The aggregated results revealed a statistically significant difference between the acupuncture group and the comparison group. (MD = -1.24; 95% CI = -2.41 to -0.35; Figure 11). The overall certainty of this evidence was assessed to be moderate to very low.
The HADS-D
A total of five studies contributed sufficient data on the Hospital Anxiety and Depression Scale-Depression (HADS-D) for this meta-analysis. The analysis revealed no significant heterogeneity, leading to the utilization of a Fixed Effects Model (FEM). (P < 0.1, I2 = 0%). The aggregated findings revealed a statistically significant difference between the acupuncture group and the control group. (MD = -1.18; 95% CI = -2.15 to -0.2; Figure 12). The overall certainty of this evidence was assessed to be moderate to very low.
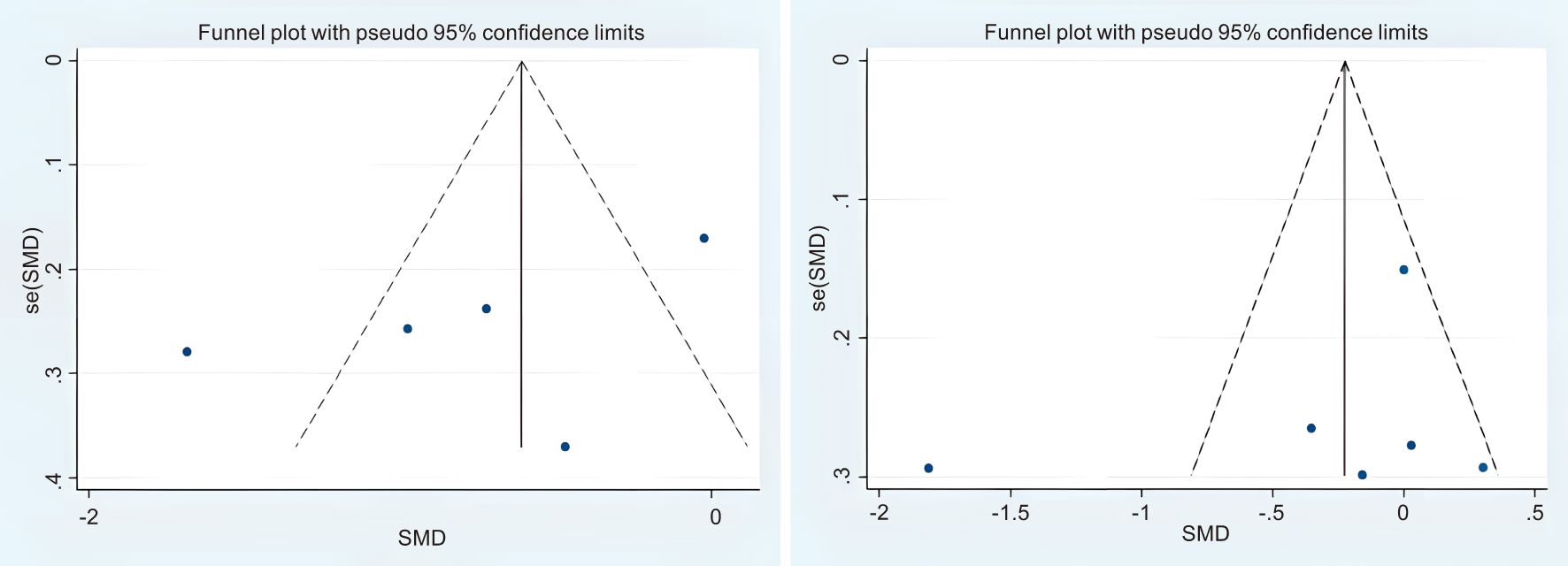
Publication bias the funnel plot method was employed to assess publication bias (Figure 13), which indicated that there was no evidence of publication bias in the study.
Discussion
The study conducted by Thompson et al (38) indicates that sleep disorders can lead to an increase in the secretion of inflammatory biomarkers, specifically including tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and C-reactive protein (CRP). This is concomitant with a decrease in cortisol levels within the body. According to the traditional Chinese medicine, sleep quality disorders and emotional maladjustment are primarily attributed to imbalances in qi and blood, and they are also associated with the dysfunction of internal organs (39). Sleep disturbances and mood disorder, a typical and chronic symptom of breast cancer patients, can cause patient discomfort and diminish life. According to modern medicine, sleep disorders are caused by the excitement of autonomic nervous system. Therefore, research has demonstrated that acupuncture can enhance the treatment of sleep disorders and emotional disorder by stimulating the body’s parasympathetic nervous system (40). Relevant studies have indicated that inadequate sleep is linked to the use of sleep aids, anxiety disorders, and metastatic diseases (41). Acupuncture plays an important role as a traditional medical treatment, but its impact on research on the treatment of insomnia and emotional maladjustment in patients with breast cancer is controversial. Moreover, relevant studies have not clearly stated that acupuncture plays a good role in the treatment of breast cancer patients (19). Nighttime light exposure (such as staying up late or working night shifts) inhibits melatonin secretion, which has antioxidant effects, inhibits estrogen synthesis and regulates immunity. Its reduction may promote tumorigenesis. Although acupuncture can promote the stimulation of the body’s righteous qi, there remain numerous controversies regarding the management of sleep disorders and mood disorder in patients with breast cancer. In this study, we searched for randomized controlled trials of acupuncture to improve sleep quality and risk of emotional maladjustment of breast cancer patients abroad. In terms of improving sleep quality and enhancing the risk of emotional maladjustment for patients with breast cancer, acupuncture demonstrates significant differences when compared to other standard treatments.
Furthermore, subgroup analyses were conducted to enhance the validation of the findings from the study. We performed subgroup analyses based on various interventions and comparison group. The results indicated that acupuncture has a significant positive effect on improving the sleep quality of breast cancer patients when compared to standard care, pharmacological treatments, and sham compressions. Subgroup analyses were conducted for different countries and the results showed that acupuncture did considerably improve sleep quality in breast cancer patients compared with the control group. However, the subgroup analysis did not markedly reduce the heterogeneity present in the study. This discrepancy may arise from the variations in measurement methods employed between the intervention and control groups. In the study of the control group, it also played a therapeutic role, and this result is likely to be related to the psychological comfort given by medical staff (42). Therefore, there is an urgent need to conduct more high-quality randomized controlled trials in the future to compare the correlations between various intervention regimens and their respective effects. Additionally, these studies should aim to optimize the dose-response relationship to provide more substantial evidence supporting the research findings. For the ISI, BFI, the pooled results of our study indicated a high degree of heterogeneity between the acupuncture and control groups in the treatment of patients with insomnia disorder related to breast cancer. Therefore, we performed subgroup analyses but were unable to explore sources of heterogeneity, possibly due to inconsistencies in sample characteristics and intervention regimens across studies. Considering the limitations of existing research in both qualitative and quantitative aspects, as well as the potential influence of confounding factors, it is advisable to exercise caution when interpreting these subgroup results. For the included literature, there is bias in the quality of the currently included studies, which may lead to low quality of the research evidence, so it is suggested that the clinical design of acupuncture and moxibustion research should be standardized. In terms of outcome measures, no more comprehensive indicators were considered to comprehensively assess the overall efficacy of acupuncture therapy for breast cancer treatment. For the HADS-A, HDAS-D, the pooled results of our study indicated that no significant differences were observed between the acupuncture group and the control group in the treatment of emotional dysregulation associated with breast cancer. It is essential to recognize that the standard for selection and positioning of acupuncture in the studies included were not consistent. The accuracy of acupuncture localization has been recognized as a crucial determinant in achieving therapeutic efficacy. Future research adopt the standard acupuncture point chart of China to enhance the accuracy of locating and identifying acupuncture points. Descriptive analyses of objective sleep parameters have shown varying results across different studies. These discrepancies may arise from the differences in precision and sensitivity among various devices used to measure these parameters, potentially leading to inconsistent findings and introducing biases. Repetitive testing will be essential in the future to ensure further validation. Modifications in physiological biomarkers are imperative to furnish scientifically credible evidence. Consequently, it is imperative that future research endeavors account for these variables to the greatest extent feasible. Wang et al (43) showed that the application of acupuncture has been shown to enhance sleep quality and mood regulation by reducing heart rate and increasing heart rate variability; However, None of the studies included in this review examined these physiological parameters; therefore, additional evidence is required to establish a connection between alterations in physiological parameters and sleep promotion. In the majority of studies included in this review, the questionnaire survey serves as a tool for measuring outcomes. Given the subjective nature of sleep quality and mood regulation, patient reports play a crucial role in assessing prognosis, monitoring and managing symptoms, as well as guiding clinical decision-making. coincidentally, questionnaires are regarded as a cost-effective and easily accessible method, which contributes to their widespread application in clinical practice. However, by measuring sleep quality and risk of emotional maladjustment, We can minimize subjective biases from participants and evaluators, thereby gaining a deeper understanding of the changes in sleep architecture and circadian rhythms. In the future, a combination of subjective and objective assessment tools can be employed to evaluate sleep quality and risk of emotional maladjustment, facilitating the analysis of the correlation between objective monitoring data and patient-reported outcomes.
This meta-analysis also had a few limitations which should be stated. We conducted a comprehensive search of foreign databases and identified the absence of current meta-analyses examining the efficacy of acupuncture in enhancing sleep quality and risk of emotional maladjustment among patients diagnosed with breast cancer. Although there are many meta-sections on acupuncture to improve breast cancer, none of them involve the clinical heterogeneity analysis of the sleep quality and the risk of emotional maladjustment of patients with breast cancer, and no reasonable subgroup analysis is conducted, which has limited clinical guidance value. The meta-analysis of this paper summarized the latest evidence, analyzed the effect of acupuncture on the improvement of the sleep and emotion patients with breast cancer from the perspective of the largest sleep quality disorder and the risk of emotional maladjustment affecting breast cancer patients, and carried out a reasonable clinical heterogeneity and subgroup analysis. Only 11 articles were included in this study, with small sample size, low quality, large heterogeneity, low quality evidence for the results, and lack of evaluation of endpoint indicators. This article did not search Chinese databases, and the external validity conclusion was poor.
Conclusion
The efficacy of acupuncture in enhancing sleep quality and risk of emotional maladjustment among breast cancer patients was significantly distinct from that of other standard treatments. However, because of the risk of bias and low quality of the evidence in the primary literature included in this study, the specific facts should be considered when applying it clinically.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author contributions
YY: Writing – original draft. HW: Conceptualization, Supervision, Writing – review & editing. ZC: Supervision, Writing – review & editing. QT: Data curation, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to thank Feilong Zhu for excellent technical support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1617818/full#supplementary-material
References
1. Giron PS, Haddad CA, Lopes de Almeida Rizzi SK, Nazário AC, and Facina G. Effectiveness of acupuncture in rehabilitation of physical and functional disorders of women undergoing breast cancer surgery. Supportive Care Cancer. (2016) 24(6):2491–6. doi: 10.1007/s00520-015-3054-5
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020:GLOBAL estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca-Cancer J Clin. (2021) 71:5. doi: 10.3322/caac.21660
3. Siegel RL, Miller KD, Fuchs HE, and Jemal A. Cancer statistics. Ca-Cancer J Clin. (2022) 72:7–33. doi: 10.3322/caac.21708
4. Wu HS, Gao F, and Given C. Living as a survivor: sleep disturbance, fatigue, depressive mood, and cognitive dysfunction after breast cancer treatment. Cancer Nurs. (2024) 47(3):221-8. doi: 10.1097/NCC.0000000000001200
5. Cheng WH, Teo RH, Cheng LJ, Lau Y, and Lau ST. Global prevalence of sleep disturbances among breast cancer survivors: a systematic review with metaanalysis. Sleep Health. (2023) 9:704–16. doi: 10.1016/j.sleh.2023.04.004
6. Schroeck JL, Ford J, Conway EL, Kurtzhalts KE, Gee ME, Vollmer KA, et al. Review of safety and efficacy of sleep medicines in older adults, Clin. Therapeut. (2016) 38:2340–72. doi: 10.1016/j.clinthera.2016.09.010
7. Lu WL, Li HX, Qian BY, Wang Y, Jansen L, Huang GW, et al. The clinical characteristics and prognosis of Chinese early stage breast cancer patients:a retrospective study. Breast J. (2010) 16(3):331. doi: 10.1111/j.1524-4741.2010.00903.x
8. Murphy CC, Fullington HM, Alvarez CA, Betts AC, Lee S, Haggstrom DA, et al. Polypharmacy and patterns of prescription medication use among cancer survivors. Cancer. (2018) 124:2850–7. doi: 10.1002/cncr.31389
9. Ma Y, Hall DL, Ngo LH, Liu Q, Bain PA, and Yeh GY. Efficacy of cognitive behavioral therapy for insomnia in breast cancer: a meta-analysis, Sleep Med. Rev. (2021) 55:101376. doi: 10.1016/j.smrv.2020.101376
10. Yang H, Yang Z, Pan H, and Zhou Q. Effects of physical activity on sleep problems in breast cancer survivors: a meta-analysis, Support. Care Cancer. (2021) 29:4023–32. doi: 10.1007/s00520-020-05914-y
11. Zhang J, Qin Z, So TH, Chang TY, Yang S, Chen H, et al. Acupuncture for chemotherapy-associated insomnia in breast cancer patients: an assessor participant blinded, randomized, sham-controlled trial. Breast Cancer Res. (2023) 25:49. doi: 10.1186/s13058-023-01645-0
12. Yang P, Hu Q, Zhang L, Shen A, Zhang Z, Wang Q, et al. Effects of non-pharmacological interventions on cancer-related cognitive impairment in patients with breast cancer: A systematic review and network meta-analysis. Eur J Oncol Nurs. (2025) 75:102804. doi: 10.1016/j.ejon.2025.102804
13. Zhu J, Chen X, Zhen X, Zheng H, Chen H, Chen H, et al. Meta-analysis of effects of yoga exercise intervention on sleep quality in breast cancer patients, Front. Oncol. (2023) 13:1146433. doi: 10.3389/fonc.2023.1146433
14. Schapira MM, Mackenzie ER, Lam R, Casarett D, Seluzicki CM, Barg FK, et al. Breast cancer survivors willingness to participate in an acupuncture clinical trial: a qualitative study. Support Care Cancer. (2014) 22:1207–15. doi: 10.1007/s00520-013-2073-3 [DOI] [PMC free article] [PubMed] [Google Scholar
15. Joshi N and Araque H. Neurophysiologic basis for the relief of human pain by acupuncture. Acupunct Electrother Res. (2009) 34:165–74. doi: 10.3727/036012909803861022
16. Filshie J, Bolton T, Browne D, and Ashley S. Acupuncture and self acupuncture for long-term treatment of vasomotor symptoms in cancer patients—audit and treatment algorithm. Acupunct Med. (2005) 23:171–80. doi: 10.1136/aim.23.4.171
17. Mao JJ, Tan T, Li SQ, Meghani SH, Glanz K, and Bruner D. Attitudes and barriers towards participation in an acupuncture trial among breast cancer patients: a survey study. BMC Complement Altern Med. (2014) 14:7. doi: 10.1186/1472-6882-14-7
18. Weng Y, Ren X, Zu Z, Xiao L, and Chen M. Efficacy and safety of acupuncture for the treatment of insomnia in breast cancer patients: a systematic review and meta-analysis. Complementary therapies Med. (2024) 86:103087. doi: 10.1016/j.ctim.2024.103087
19. Zhang J, Zhang Z, Huang S, Qiu X, Lao L, Huang Y, et al. Acupuncture for cancer-related insomnia: A systematic review and meta-analysis. Phytomedicine. (2022) 102:154160. doi: 10.1016/j.phymed.2022.154160
20. Fu C, Zhao N, Liu Z, Yuan LH, Xie C, Yang WJ, et al. Acupuncture improves peri-menopausal insomnia: a randomized controlled trial. Sleep. (2017) 40(11):5. doi: 10.1093/sleep/zsx153
21. Liu Y, Feng H, Liu W, Mao H, Mo Y, Yin Y, et al. Regulation action and nerve electrophysiology mechanism of acupuncture on arousal state in patients of primary insomnia. Zhongguo Zhen Jiu. (2017) 37(1):19–23. doi: 10.13703/j.0255-2930.2017.01.004
22. Zhao H, Liu C, Ye H, Shi K, Yao Y, and Wang M. Advancements in the physiopathological study of acupuncture treatment for insomnia: A review. Med (Baltimore). (2024) 103:e38476. doi: 10.1097/MD.0000000000038476
23. Eriksen WT, Singerman L, Romero SAD, Bussell J, Barg FK, and Mao JJ. Understanding the use of acupuncture for insomnia among cancer survivors: A qualitative study. J Altern Complement Med. (2018) 24:962–7. doi: 10.1089/acm.2018.0156
24. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Bmj. (2009) 339:b2700. doi: 10.1136/bmj.b2700
25. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj. (2017) 358:j4008. doi: 10.1136/bmj.j4008
26. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj. (2011) 343:d5928. doi: 10.1136/bmj.d5928
27. Mao H, Jin M, Xie L, Mao N, Shen X, Chen J, et al. Infrared laser moxibustion for cancer-related fatigue in breast cancer survivors: a randomized controlled trial. Breast Cancer Res. (2024) 26.1:80. doi: 10.1186/s13058-024-01838-1
28. Zhang J, Qin Z, So TH, Chang TY, Yang S, Chen H, et al. Acupuncture for chemotherapy-associated insomnia in breast cancer patients: an assessor-participant blinded, randomized, sham-controlled trial. Breast Cancer Res. (2023) 25.1:49. doi: 10.1186/s13058-023-01645-0
29. Liu Q, Wang C, Wang Y, Xu W, Zhan C, Wu J, et al. Mindfulness-based stress reduction with acupressure for sleep quality in breast cancer patients with insomnia undergoing chemotherapy: a randomized controlled trial. Eur J Oncol Nurs. (2022) 61:1022195. doi: 10.1016/j.ejon.2022.102219
30. Wang Y, Li X, Ji X, Wu J, Li J, Zheng W, et al. Adaptive auricular point acupressure for sleep disturbance in women with breast cancer: a randomized controlled trial. Evidence-Based Complementary Altern Med. (2022) 2022:8637386. doi: 10.1155/2022/8637386
31. Nourizadeh R, Khanipour S, Zamiri RE, Namin MS, Khalili A, and Hakimi S. A comparison of the effects of self-acupressure and aerobic exercises on sleep disorders of breast cancer survivors: a controlled randomized clinical trial. Med Acupuncture. (2022) 34.2:131–6. doi: 10.1089/acu.2020.1515
32. Zhang J, Qin Z, So TH, Chen H, Lam WL, Yam LL, et al. Electroacupuncture plus auricular acupressure for chemotherapy-associated insomnia in breast cancer patients: a pilot randomized controlled trial. Integr Cancer therapies. (2021) 20:153473542110191035. doi: 10.1177/15347354211019103
33. Höxtermann MD, Buner K, Haller H, Kohl W, Dobos G, Reinisch M, et al. Efficacy and safety of auricular acupuncture for the treatment of insomnia in breast cancer survivors: a randomized controlled trial. Cancers. (2021) 13(16):4082. doi: 10.3390/cancers13164082
34. Garland SN, Xie SX, Li Q, Seluzicki C, Basal C, and Mao JJ. Comparative effectiveness of electro-acupuncture versus gabapentin for sleep disturbances in breast cancer survivors with hot flashes: a randomized trial. Menopause. (2017) 24.5:517–23. doi: 10.1097/GME.0000000000000779
35. Zick SM, Sen A, Wyatt GK, Murphy SL, Arnedt JT, Harris RE, et al. Investigation of 2 types of self-administered acupressure for persistent cancer-related fatigue in breast cancer survivors: a randomized clinical trial. JAMA Oncol. (2016) 2(11):1470–6. doi: 10.1001/jamaoncol.2016.1867
36. Bao T, Cai L, Snyder C, Betts K, Tarpinian K, Gould J, et al. Patient-reported outcomes in women with breast cancer enrolled in a dual-center, double-blind, randomized controlled trial assessing the effect of acupuncture in reducing aromatase inhibitor-induced musculoskeletal symptoms. Cancer. (2014) 120(3):381–9. doi: 10.1002/cncr.28352
37. Mao JJ, Farrar JT, Bruner D, Zee J, Bowman M, Seluzicki C, et al. Electroacupuncture for fatigue, sleep, and psychological distress in breast cancer patients with aromatase inhibitor-related arthralgia: a randomized trial. Cancer. (2014) 120(23):3744–51. doi: 10.1002/cncr.28917
38. Thompson KI, Chau M, Lorenzetti MS, Hill LD, Fins AI, and Tartar JL. Acute sleep deprivation disrupts emotion, cognition, inflammation, and cortisol in young healthy adults, Front, Behav. Neurosci. (2022) 16:945661. doi: 10.3389/fnbeh.2022.945661
39. Yang T, Wang S, Zhang X, Liu L, Liu Y, and Zhang C. Efficacy of auricular acupressure in maintenance haemodialysis patients: a systematic review and meta- analysis. J Clin Nurs. (2022) 31:508–19. doi: 10.1111/jocn.15966
40. Pei M, Chen J, Dong S, Yang B, Yang K, Wei L, et al. Auricular acupressure for insomnia in patients with maintenance hemodialysis: a systematic review and meta-analysis, Front. Psychiatr. (2021) 12:576050. doi: 10.3389/fpsyt.2021.576050
41. Faiz SA, Knox AS, Fellman B, Jaumally BA, Pacheco GN, Das A, et al. Sleep disturbances based on patient reported outcomes in patients with breast cancer. Sleep Breathing. (2024) 28(6):2491–500. doi: 10.1007/s11325-024-03150-w
42. Wang T, Tan JB, Yao LQ, Huilin C, Zhao I, Eliseeva S, et al. Effects of somatic acupoint stimulation on anxiety and depression in cancer patients: an updated systematic review of randomized controlled trials, Compl. Ther Clin Pract. (2023) 51:101735. doi: 10.1016/j.ctcp.2023.101735
Keywords: acupuncture, breast cancer, risk of emotional maladjustment, meta-analysis, sleep quality
Citation: Yang Y, Wang H, Chen ZZ and Teng QR (2025) Effects of acupuncture on improving sleep quality and the risk of emotional maladjustment of breast cancer patients: a systematic review and meta-analysis. Front. Oncol. 15:1617818. doi: 10.3389/fonc.2025.1617818
Received: 29 April 2025; Accepted: 10 June 2025;
Published: 26 June 2025.
Edited by:
Xu Zhai, China Academy of Chinese Medical Sciences, ChinaReviewed by:
Paulo Sargento, Escola Superior de Saúde Ribeiro Sanches, PortugalPaula O. Carvalho, Superior School of Health North of the Portuguese Red Cross, Portugal
Copyright © 2025 Yang, Wang, Chen and Teng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Yang, MTI0NDk1NDY5N0BxcS5jb20=; Hong Wang, MjkyNzMyMzQzOUBxcS5jb20=
†ORCID: Hong Wang, orcid.org/0009-0008-0109-7250
 Yi Yang
Yi Yang Hong Wang
Hong Wang Zai Zhao Chen
Zai Zhao Chen