- 1Multidisciplinary Treatment Cancer Center, Kurume University Hospital, Kurume, Japan
- 2Division of Gastroenterology, Department of Medicine, Kurume University School of Medicine, Kurume, Japan
- 3Department of Surgery, Kurume University School of Medicine, Kurume, Japan
- 4Department of Radiology, Kurume University School of Medicine, Kurume, Japan
Background: Central venous (CV) ports are extensively employed for the administration of chemotherapy in cancer patients owing to their safety and reliability. The rupture of a CV port catheter is an infrequent occurrence; nonetheless, it can effectuate serious complications if left untreated. In this case series, we present four cases of catheter rupture of CV ports implanted in cancer patients via the right internal jugular vein for chemotherapy administration.
Results: Our series comprised one male and three female patients, with an age range of 41–76 years (median age: 61 years). All CV ports were implanted through the right internal jugular vein using a PowerPort® MRI device and were placed for a median duration of 39 months (range: 17–45 months). In three of four instances, CV ports were inactive at the time of catheter rupture; nevertheless, one study participant continued to use the CV port even after it had ruptured. None of the patients presented with any subjective symptoms at the time of catheter rupture. Two cases were detected via subcutaneous tissue swelling during CV port utilization, and the other two were incidentally detected via imaging. The ruptured catheters were located in the right atrium-right ventricle in two patients and in the superior vena cava and left pulmonary artery in the third and fourth patients, respectively. All four devices were retrieved without complications using a snare catheter.
Conclusion: Catheter rupture of the CV port is a rare but potentially grave complication. Therefore, routine monitoring is required, considering the possibility of catheter rupture if the CV port is retained as an implant for an extended period.
1 Introduction
Long-term venous access devices, such as subcutaneously placed central venous (CV) access devices, were first introduced in 1982 and are widely used as venous access for chemotherapy in oncology patients (1). Chemotherapy should be initiated after CV port placement because it allows reliable drug delivery and safely reduces the risk of extravascular invasion with less patient distress, even among patients with difficult peripheral venous access (2, 3). Hence, the widespread use of CV ports has raised the issue of complications associated with their prolonged placement.
The overall complication rate associated with CV port placement has been reported to be 7.2–12.5% (4). Port system infection is the most common complication, followed by catheter-related thrombosis (5). Catheter rupture of the CV port is an infrequent complication, with a frequency of 0.3–2.9% (6, 7). However, in these reports, the CV port was placed via the subclavian vein. Placing a CV port via the internal jugular vein is considered significantly less risky for catheter fracture than placing it via the subclavian vein (8), but this needs to be verified further. Catheter rupture is often asymptomatic but can cause serious complications; hence, removal of the ruptured catheter should always be attempted (6).
Here, we present four case studies of catheter rupture of CV ports implanted via the right internal jugular vein for the administration of chemotherapy in patients with gastrointestinal cancer. The ruptured catheter was retrieved using endovascular technique.
2 Case presentation
2.1 Case 1
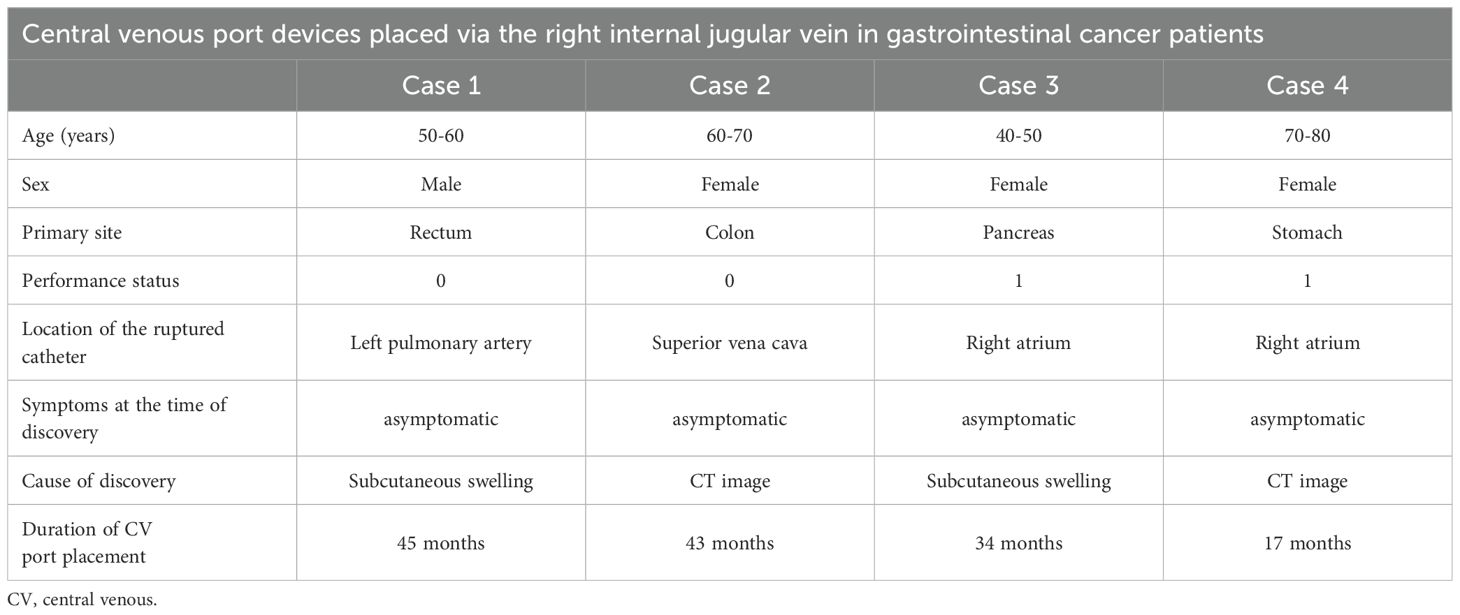
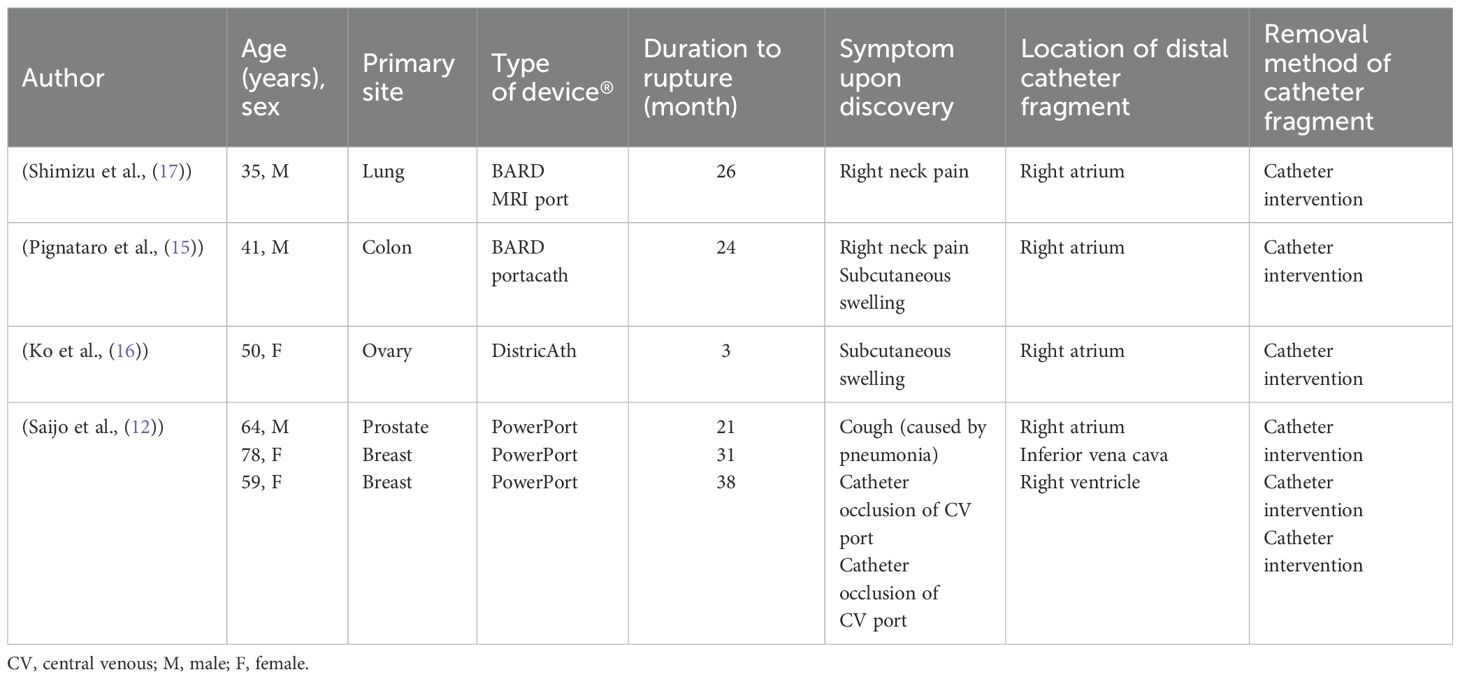
The patient was a male in his 50s, with a performance status (PS) of 0 (Table 1). He underwent laparoscopic anterior rectal resection and D3 lymph node dissection for resectable rectal cancer (pT3pN2M0 pStage IIIb). For postoperative adjuvant therapy, a CV port (PowerPort® MRI; Becton, Dickinson, and Company) was placed via the right internal jugular vein approach. The patient received CAPOX therapy following CV port placement. At the 6-month follow-up, the CV port was still in place. Eighteen months after CV port placement, peritoneal dissemination nodule recurrence was observed in the pelvis, and FOLFIRI plus bevacizumab was initiated for chemotherapy. After approximately 6 months of chemotherapy, the tumor had shrunk, and curative resection was performed (24 months after CV port placement). Forty-four months after CV port placement, peritoneal seeding nodule recurrence was identified on the anterior sacral surface, and subcutaneous swelling was observed once the CV port was used to administer chemotherapy. Catheter rupture of the CV port was suspected, and such rupture was confirmed by chest radiography and computed tomography (CT) findings. The catheter tip was located in the left pulmonary artery; however, no subjective symptoms were observed (Figures 1A, E). A snare catheter (EN Snare® 18–30 mm) was used to retrieve the torn catheter (45 months after CV port placement; Figures 2A, 3). No complications were observed. The CV port was then reinserted, and chemotherapy was restarted.
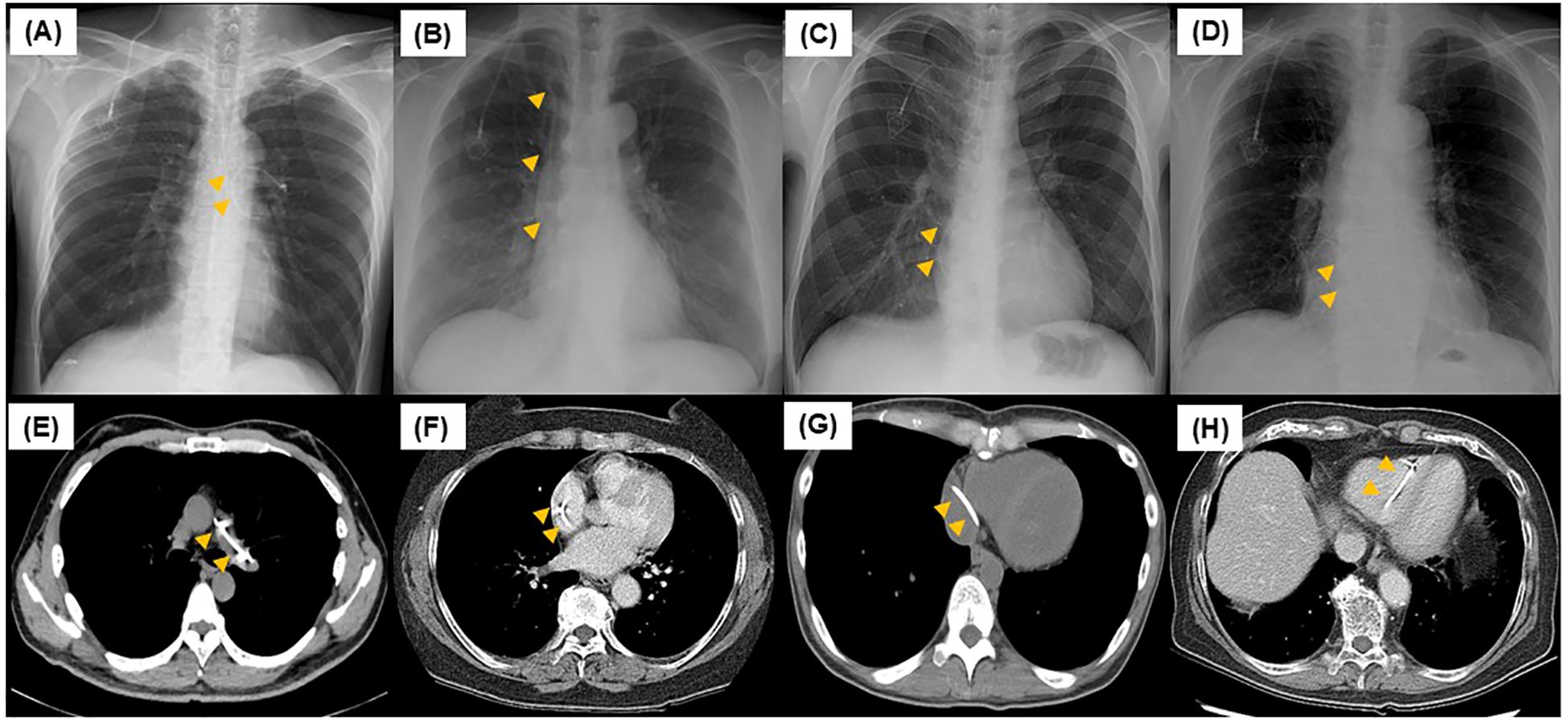
Figure 1. Chest radiography and computed tomography scan at central venous port rupture. For case 1 (A, E), the ruptured catheter was in the left pulmonary artery. For case 2 (B, F), the ruptured catheter was in the superior vena cava. For cases 3 (C, G) and 4 (D, H), the ruptured catheter was in the right atrium.
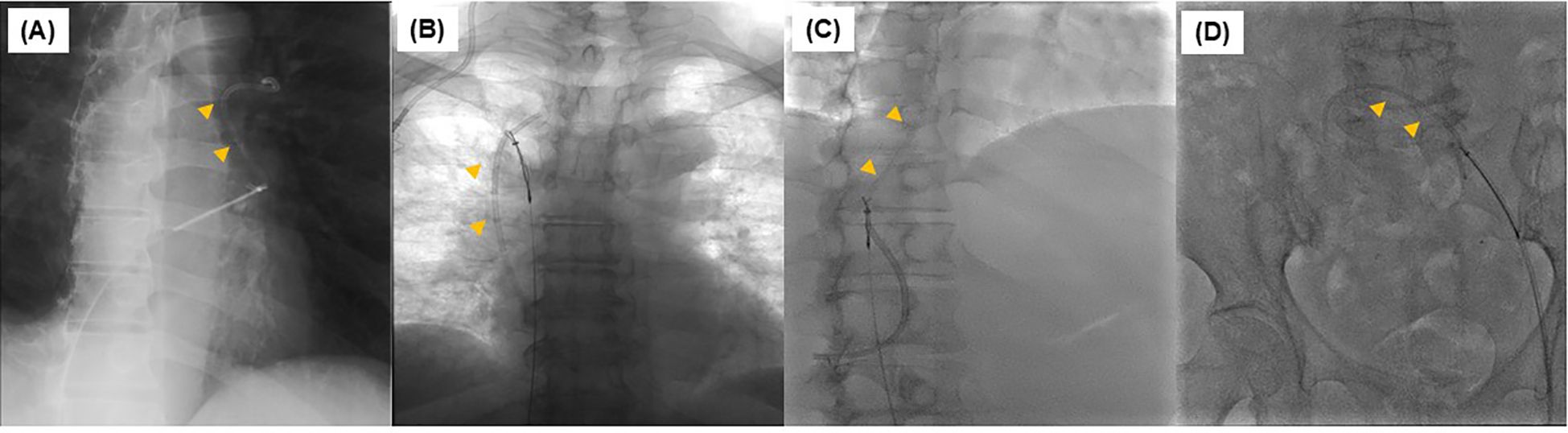
Figure 2. Removal of torn catheter using a snare catheter during an interventional procedure. In all cases from Case 1 to 5 (A–D), all ruptured catheters were removed with a snare catheter.
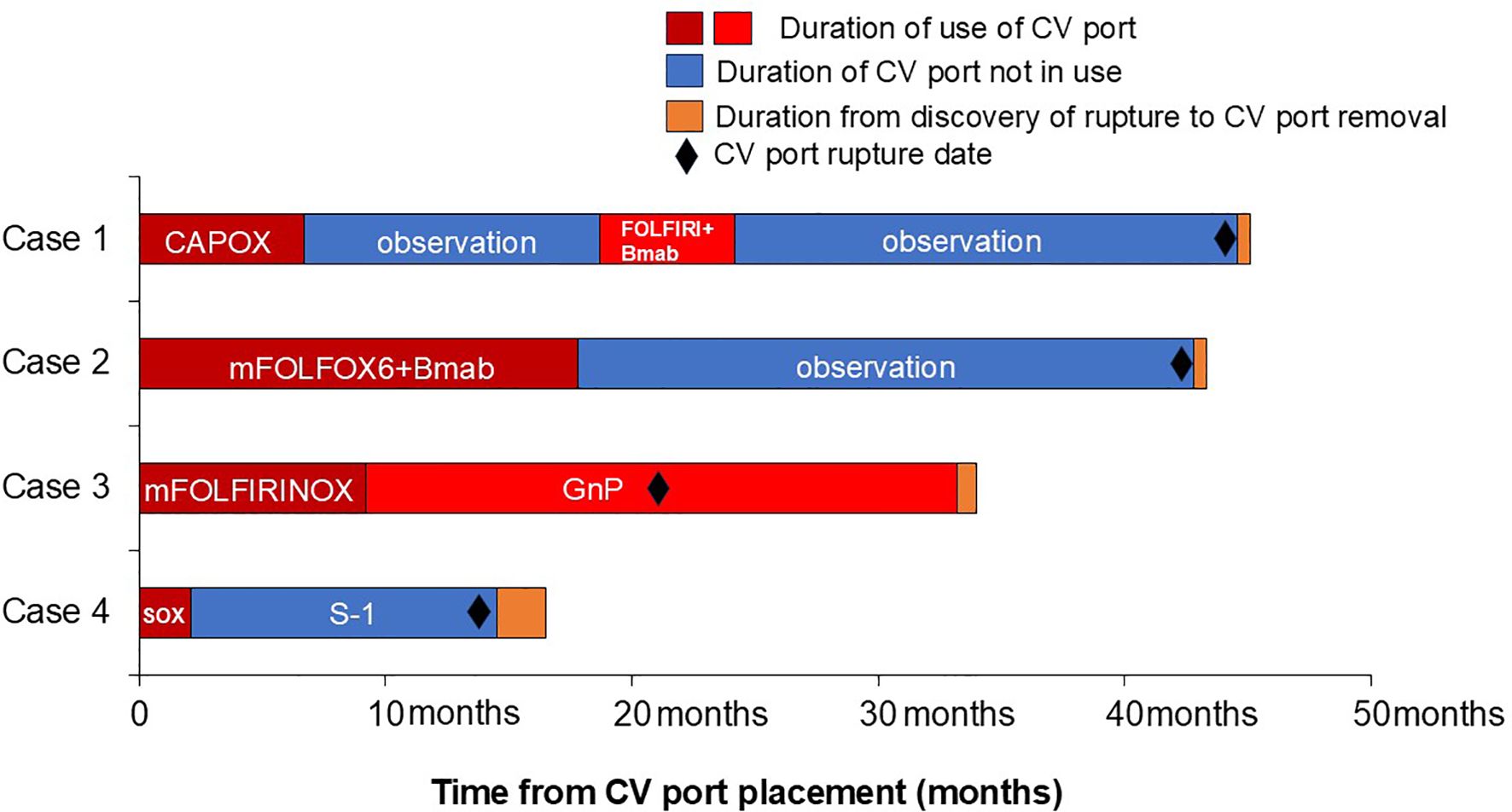
Figure 3. Duration of time between placement of CV port and retrieval of ruptured CV port. CAPOX; capecitabine plus oxaliplatin; FOLFIRI+Bmab; fluorouracil, leucovorin, and irinotecan plus bevacizumab; mFOLFOX6+Bmab; fluorouracil, leucovorin, and oxaliplatin plus bevacizumab; mFOLFIRINOX; fluorouracil, leucovorin, oxaliplatin, and irinotecan; GnP; gemcitabine and nab-paclitaxel; SOX, S-1 plus oxaliplatin.
2.2 Case 2
The patient was a female in her 60s, with a PS of 0 (Table 1). She underwent CV port placement via the right internal jugular approach for postoperative recurrence of ascending colon cancer (PowerPort® MRI). Chemotherapy was initiated with mFOLFOX6 plus bevacizumab therapy after CV port placement. Eighteen months after placing the CV port, the tumor was assessed to be in complete response, and she was followed up without further chemotherapy. Forty-four months after CV port placement, CT scan revealed catheter rupture of the CV port. The catheter tip was in the right atrium; however, no subjective symptoms were observed (Figures 1B, F). A snare catheter (EN Snare® 18–30 mm) was used to retrieve the torn catheter (43 months after CV port placement; Figures 2B, 3). No complications were observed. The patient was followed up without CV port reinsertion.
2.3 Case 3
The patient was a female in her 40s, with a PS of 1 (Table 1). She was diagnosed with unresectable pancreatic cancer (cT4N1M1 cStage IV) and underwent CV port placement via the right internal jugular vein approach (PowerPort® MRI). Chemotherapy was initiated with mFOLFIRINOX therapy after CV port placement. Nine months after CV port placement, she had difficulty continuing treatment due to gastrointestinal toxicity, and the treatment was shifted to gemcitabine and nab-paclitaxel therapy. Twenty-one months after CV port placement, a CT scan revealed catheter rupture of the CV port. The catheter tip was located in the right atrium; however, no subjective symptoms were observed (Figures 1C, G). Despite catheter rupture of the CV port, chemotherapy was continued using the CV port without rupture detection because the catheter rupture was localized within the central venous tract. Thirty-three months after CV port placement, subcutaneous swelling was observed when the CV port was used, and catheter rupture of the CV port was identified. A snare catheter (Atrieve Vascular Snare Kit, 27–45 mm) was used to retrieve the torn catheter (34 months after CV port placement; Figures 2C, 3). No complications were observed. She continued chemotherapy via peripheral infusion without CV port reinsertion.
2.4 Case 4
The patient was a female in her 70s, with a PS of 1 (Table 1). She underwent CV port placement via the right internal jugular vein approach (PowerPort® MRI) for recurrent peritoneal dissemination after advanced gastric cancer surgery (pT3N0M0 pStage IIA). Chemotherapy was initiated with SOX therapy after CV port placement. Two months after CV port placement, oxaliplatin was discontinued due to gastrointestinal toxicity and was shifted to oral S1 therapy. Fourteen months after CV port placement, a CT scan revealed catheter rupture of the CV port; the catheter tip was located in the right atrium, but no subjective symptoms were observed (Figures 1D, H). A snare catheter (EN Snare® 18–30 mm) was used to retrieve the torn catheter (17 months after CV port placement; Figures 2D, 3). No complications were observed. The patient was followed up without CV port reinsertion.
3 Discussion
Long-term placement of CV ports results in complications such as catheter-related bloodstream infections, local infections, thrombosis, and catheter damage. The incidence of catheter rupture of CV ports placed via the subclavian vein is reported to be 0.5–1.5% (9, 10), and the mechanism is thought to be pinch-off syndrome caused by compression between the clavicle and first rib (11). Saijo et al. (12) observed catheter rupture in 3 (4.5%) of 66 patients who had a CV port placed via the internal jugular vein. Furthermore, in our previous study of 184 cases of CV port placement for advanced colorectal cancer, the CV port was placed through the internal jugular vein in 180 (98%) patients; of these, 5 (2.7%) experienced catheter injury, including 1 (0.5%) case of CV port rupture (13). Busch reported that the frequency of catheter rupture in 533 patients with CV ports placed in the upper arm was 1.8% (14). Thus, catheter rupture occurs regardless of which vein is used for CV port placement.
Previous studies have reported cases of catheter damage, both complete rupture and partial damage, in CV ports placed via multiple venous approaches. We found six cases of complete rupture of CV port catheters placed via the right internal jugular vein in the literature (12, 15–17) (Table 2). CV port placement via the internal jugular vein approach reportedly has a higher success rate and fewer complications than the subclavian vein approach (18). Additionally, recent reports have suggested the usefulness of CV port placement via the innominate vein or brachiocephalic vein (19, 20). While no conclusive evidence has been established regarding which approach is most preferable, we currently opt for ultrasound-guided CV port placement via the internal jugular vein.
We report four cases (0.6%) of catheter rupture among 726 patients who underwent CV port placement via the right internal jugular vein. The cause of catheter rupture was thought to be stress that weakened the catheter. Another possible reason was the use of the Groshong CV port. Groshong catheters, made of silicone, are considered more vulnerable than open-ended polyurethane catheters (21). Furthermore, the median duration of CV port implantation in the four patients was 39 months, which is relatively long. Thus, the risk of rupture should be considered when implanting a grossing-type CV port for a long period; the type of CV port needs to be considered carefully when it is required for long-term use.
Among the four patients with catheter rupture in the current series, in one patient, the rupture went unnoticed, and the ruptured CV port continued being used. The delay in detecting catheter rupture occurred because the ruptured part was distally located and remained in the intravascular region. Furthermore, the physicians in charge did not assess the position of the catheter tip in CT images. In fact, by the time the rupture was detected, 13 months had elapsed, and five CT scans were performed during this period. We were preoccupied with the tumor size and missed the catheter rupture. To our knowledge, while no study has reported serious complications from continued use of ruptured catheters and no serious complications occurred in our patients, imaging scans, even in asymptomatic cases, must be assessed for the possibility of catheter rupture to prevent complications. Further, the CV ports were not being used in three patients after initial therapy. Catheter rupture of the CV port is an infrequent complication associated with long-term placement of CV ports, and it can have serious sequela. Hence, the CV port must be removed when no longer required.
In all four cases with ruptured CV ports, the ruptured catheters were retrieved using an interventional technique, with no complications. Most patients with torn catheters are asymptomatic, but in rare cases, cardiac perforation, arrhythmias, and thromboembolism may occur; hence, their retrieval is advisable (22). A torn catheter can be retrieved by several methods, including interventional methods and surgical, open-chest approaches; the less invasive interventional approach is popular (6). In fact, intravascular catheterization has a retrieval rate of approximately 94–98% of torn catheters (23, 24).
In one of our patients in whom the torn catheter had remained in the right atrium for a long period, the catheter was removed without any granulation tissue, although we suspected that catheter removal would be difficult owing to adhesion to the surrounding tissue. The interventional technique is effective in retrieving torn catheters owing to the high probability of retrieval and low complication rate. Huang et al. (25) noted that while technical advancements have reduced complications associated with CV ports, international guidelines on this procedure are still lacking. They emphasize the need for multicenter prospective trials to validate optimal insertion vessels, catheter tip positioning, and catheter management during CV port placement.
This case series has several limitations. Our series included only four cases at a single institution. Although we mentioned the possible causes of catheter rupture, we have not been able to prove a definitive causal relationship. Further multicenter studies with a larger number of cases are, thus, needed.
4 Conclusion
Catheter rupture of the CV port is an infrequent complication, and breakage rates are expected to decrease as catheter materials improve. Nevertheless, since catheter rupture can lead to serious complications, routine monitoring is required, regardless of the vein into which they are inserted, and the possibility of catheter rupture should also be considered if the CV port is left in situ for an extended period.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Kurume University Hospital Ethics Committee Approval Number 2025-02. The studies were conducted in accordance with the local legislation and institutional requirements. In principle, written consent is obtained. However, it is difficult to obtain written consent directly for subjects who are not currently seen at the hospital. Therefore, as an alternative to obtaining informed consent, we notify research subjects, etc. via our website and notices posted in the hospital, etc., and, in principle, ensure that subjects have the opportunity to refuse participation in the research without any disadvantage to their future medical treatment, etc. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
TT: Writing – original draft, Writing – review & editing. FM: Data curation, Investigation, Writing – review & editing. SN: Data curation, Investigation, Writing – review & editing. AK: Data curation, Investigation, Writing – review & editing. MK: Data curation, Investigation, Writing – review & editing. ST: Data curation, Supervision, Writing – review & editing. FF: Data curation, Supervision, Writing – review & editing. TK: Data curation, Supervision, Writing – review & editing. KM: Conceptualization, Data curation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
This study was partly supported by an award from the Michel Mitsuo Yokoyama Foundation for the Promotion of Immunology Science.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Niederhuber JE, Ensminger W, Gyves JW, Liepman M, Doan K, and Cozzi E. Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery. (1982) 92:706–12.
2. Teichgräber UK, Kausche S, Nagel SN, and Gebauer B. Outcome analysis in 3,160 implantations of radiologically guided placements of totally implantable central venous port systems. Eur Radiol. (2011) 21:1224–32. doi: 10.1007/s00330-010-2045-7
3. Tabatabaie O, Kasumova GG, Eskander MF, Critchlow JF, Tawa NE, and Tseng JF. Totally Implantable venous access devices: a review of complications and management strategies. Am J Clin Oncol. (2017) 40:94–105. doi: 10.1097/COC.0000000000000361
4. Machat S, Eisenhuber E, Pfarl G, Stübler J, Koelblinger C, Zacherl J, et al. Complications of central venous port systems: a pictorial review. Insights Imaging. (2019) 10:86. doi: 10.1186/s13244-019-0770-2
5. Nakamura T, Sasaki J, Asari Y, Sato T, Torii S, and Watanabe M. Complications after implantation of subcutaneous central venous ports (PowerPort®). Ann Med Surg (Lond). (2017) 17:1–6. doi: 10.1016/j.amsu.2017.03.014
6. Ayx I, Goessmann H, Hubauer H, Uller W, Wiesinger I, Uhl C, et al. Interventional removal of intravascular medical devices: methods and technical success. Rofo. (2016) 188:566–73. doi: 10.1055/s-0042-104204
7. Biffi R, Corrado F, de Braud F, de Lucia F, Scarpa D, Testori A, et al. Long-term, totally implantable central venous access ports connected to a Groshong catheter for chemotherapy of solid tumours: experience from 178 cases using a single type of device. Eur J Cancer. (1997) 33:1190–4. doi: 10.1016/S0959-8049(97)00039-7
8. Wu C-Y, Fu J-Y, Feng P-H, Kao T-C, Yu S-Y, Li H-J, et al. Catheter fracture of intravenous ports and its management. World J Surg. (2011) 35:2403–10. doi: 10.1007/s00268-011-1200-x
9. Ilhan BM, Sormaz İC, and Türkay R. Pinch-off syndrome, a rare complication of totally implantable venous access device implantation: a case series and literature review. Korean J Thorac Cardiovasc Surg. (2018) 51:333–7. doi: 10.5090/kjtcs.2018.51.5.333
10. Biffi R, de Braud F, Orsi F, Pozzi S, Mauri S, Goldhirsch A, et al. Totally implantable central venous access ports for long-term chemotherapy. A prospective study analyzing complications and costs of 333 devices with a minimum follow-up of 180 days. Ann Oncol. (1998) 9:767–73. doi: 10.1023/A:1008392423469
11. Aitken DR and Minton JP. The “pinch-off sign”: a warning of impending problems with permanent subclavian catheters. Am J Surg. (1984) 148:633–6. doi: 10.1016/0002-9610(84)90340-4
12. Saijo F, Mutoh M, Tokumine J, Yoshinobu O, Hama H, Namima T, et al. Late fracture of Groshong ports: A report of the three cases. J Vasc Access. (2019) 20:563–6. doi: 10.1177/1129729819834512
13. Shigyo H, Suzuki H, Tanaka T, Moriyama E, Shimotsuura Y, Nagasu S, et al. Safety of early bevacizumab administration after central venous port placement for patients with colorectal cancer. Cancers (Basel). (2023) 15:2264. doi: 10.3390/cancers15082264
14. Busch JD, Vens M, Herrmann J, Adam G, and Ittrich H. Material failure of silicone catheter lines: a retrospective review of partial and complete ruptures in 553 patients. AJR Am J Roentgenol. (2017) 208:464–9. doi: 10.2214/AJR.16.16540
15. Pignataro BS, Nishinari K, Wolosker N, and Bomfim GA. Fracture and migration into the coronary sinus of a totally implantable catheter introduced via the right internal jugular vein. BMJ Case Rep. (2014) 2014:bcr2014207276. doi: 10.1136/bcr-2014-207276
16. Ko SY, Park SC, Hwang JK, and Kim SD. Spontaneous fracture and migration of catheter of a totally implantable venous access port via internal jugular vein–a case report. J Cardiothorac Surg. (2016) 11:50. doi: 10.1186/s13019-016-0450-y
17. Shimizu T, Mekata E, Murata S, Yamamoto T, and Tani T. A case of catheter fracture of a totally implantable access port introduced through the right internal jugular vein. J Surg Oncol. (2011) 103:460–1. doi: 10.1002/jso.21758
18. Yip D and Funaki B. Subcutaneous chest ports via the internal jugular vein. A retrospective study of 117 oncology patients. Acta Radiol. (2002) 43:371–5. doi: 10.1034/j.1600-0455.2002.430405.x
19. Sun X, Xu J, Xia R, Wang C, Yu Z, Zhang J, et al. Efficacy and safety of ultrasound-guided totally implantable venous access ports via the right innominate vein in adult patients with cancer: Single-centre experience and protocol. Eur J Surg Oncol. (2019) 45:275–8. doi: 10.1016/j.ejso.2018.07.048
20. Sun X, Bai X, Zhang Y, Xu L, Yu Z, Jin Y, et al. Perioperative and postoperative complications of ultrasound-guided totally implantable venous access ports via the brachiocephalic vein in patients with cancer: a prospective study. J Cancer. (2021) 12:1379–85. doi: 10.7150/jca.55343
21. Kojima S, Hiraki T, Gobara H, Iguchi T, Fujiwara H, Matsui Y, et al. Fracture of totally implanted central venous access devices: a propensity-score-matched comparison of risks for Groshong silicone versus polyurethane catheters. J Vasc Access. (2016) 17:535–41. doi: 10.5301/jva.5000606
22. Li Y, Chen J, Li Z, Lu H, Ren K, Ren J, et al. Successful percutaneous transvenous retrieval of intravascular fractured port catheter: a single center experience. J Cardiothorac Surg. (2020) 15:101. doi: 10.1186/s13019-020-01131-0
23. Egglin TK, Dickey KW, Rosenblatt M, and Pollak JS. Retrieval of intravascular foreign bodies: experience in 32 cases. AJR Am J Roentgenol. (1995) 164:1259–64. doi: 10.2214/ajr.164.5.7717243
24. Cheng CC, Tsai TN, Yang CC, and Han CL. Percutaneous retrieval of dislodged totally implantable central venous access system in 92 cases: experience in a single hospital. Eur J Radiol. (2009) 69:346–50. doi: 10.1016/j.ejrad.2007.09.034
Keywords: central venous port, catheter rupture, chemotherapy, complications, gastrointestinal cancer, internal jugular vein
Citation: Tanaka T, Masaru F, Nagasu S, Kuhara A, Koganemaru M, Tanoue S, Fujita F, Kawaguchi T and Miwa K (2025) Case Report: Catheter rupture of central venous port devices placed via the right internal jugular vein for chemotherapy in gastrointestinal cancer patients: a four-case series. Front. Oncol. 15:1620952. doi: 10.3389/fonc.2025.1620952
Received: 30 April 2025; Accepted: 11 August 2025;
Published: 03 September 2025.
Edited by:
Genti Xhepa, Ente Ospedaliero Cantonale (EOC), SwitzerlandReviewed by:
Apurva Patel, Gujarat Cancer & Research Institute, IndiaXingwei Sun, Second Affiliated Hospital of Soochow University, China
Huseyin Kemal Rasa, Anadolu Medcal Center Hospital, Türkiye
Cherry Bansal, Tantia University, India
Copyright © 2025 Tanaka, Masaru, Nagasu, Kuhara, Koganemaru, Tanoue, Fujita, Kawaguchi and Miwa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Keisuke Miwa, bWl3YV9rZWlzdWtlQG1lZC5rdXJ1bWUtdS5hYy5qcA==
 Toshimitsu Tanaka
Toshimitsu Tanaka Fukahori Masaru1,2
Fukahori Masaru1,2 Fumihiko Fujita
Fumihiko Fujita Takumi Kawaguchi
Takumi Kawaguchi Keisuke Miwa
Keisuke Miwa