- Guang’an People’s Hospital, Gynecology Department, Guang’an, Sichuan, China
Objective: To evaluate the clinical effectiveness and prognostic outcomes of colposcopy-guided LEEP compared with cold knife conization (CKC) in the treatment of cervical intraepithelial neoplasia (CIN).
Methods: 124 patients with CIN in our hospital from January 2022 to December 2023 were chosen and classified into the control group (62 cases) and the observation group (62 cases) according to the therapeutic schedule. The observation group was treated with colposcopy combined with LEEP, while the control group underwent conventional cold knife conization (CKC). The clinical effect, surgical indicators, complications were compared. The control group underwent LEEP without colposcopic guidance, following standard clinical protocol.
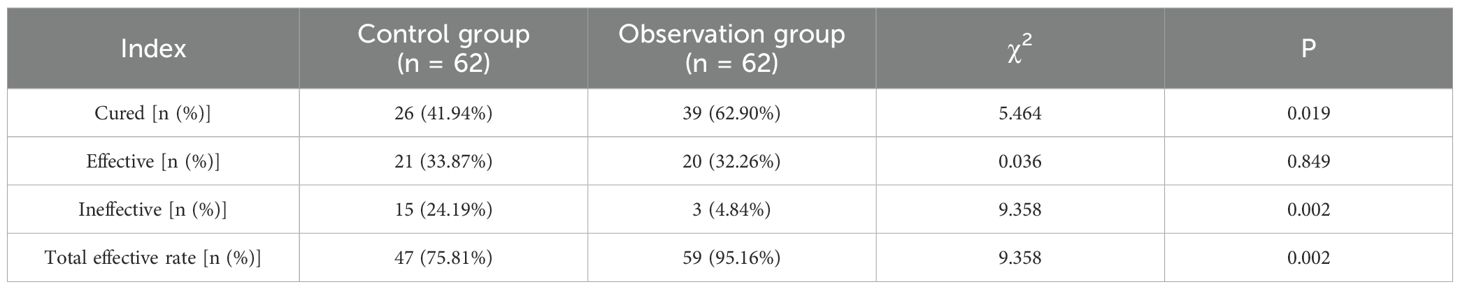
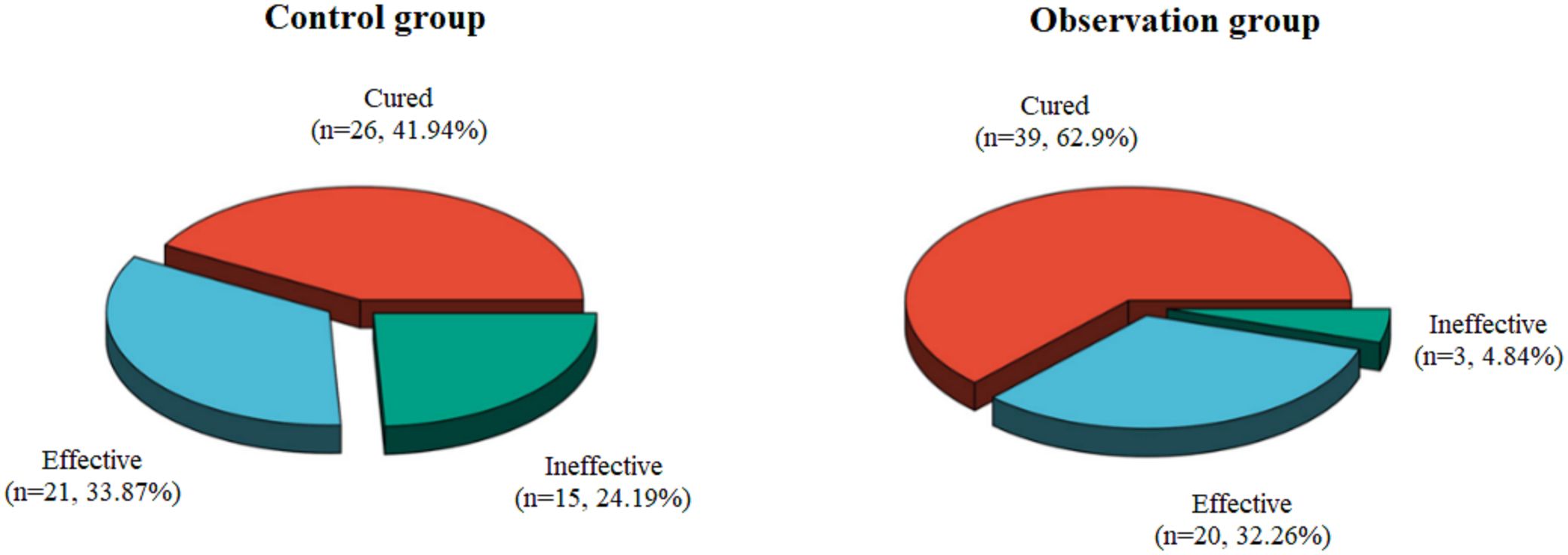
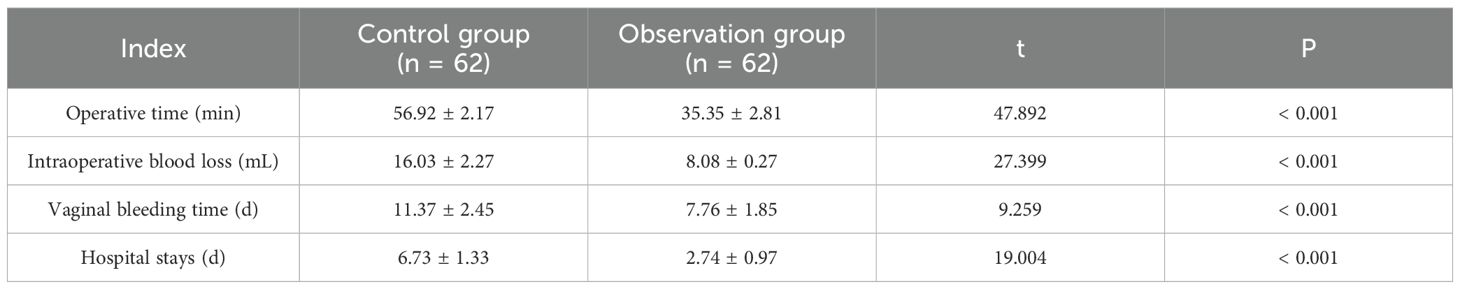
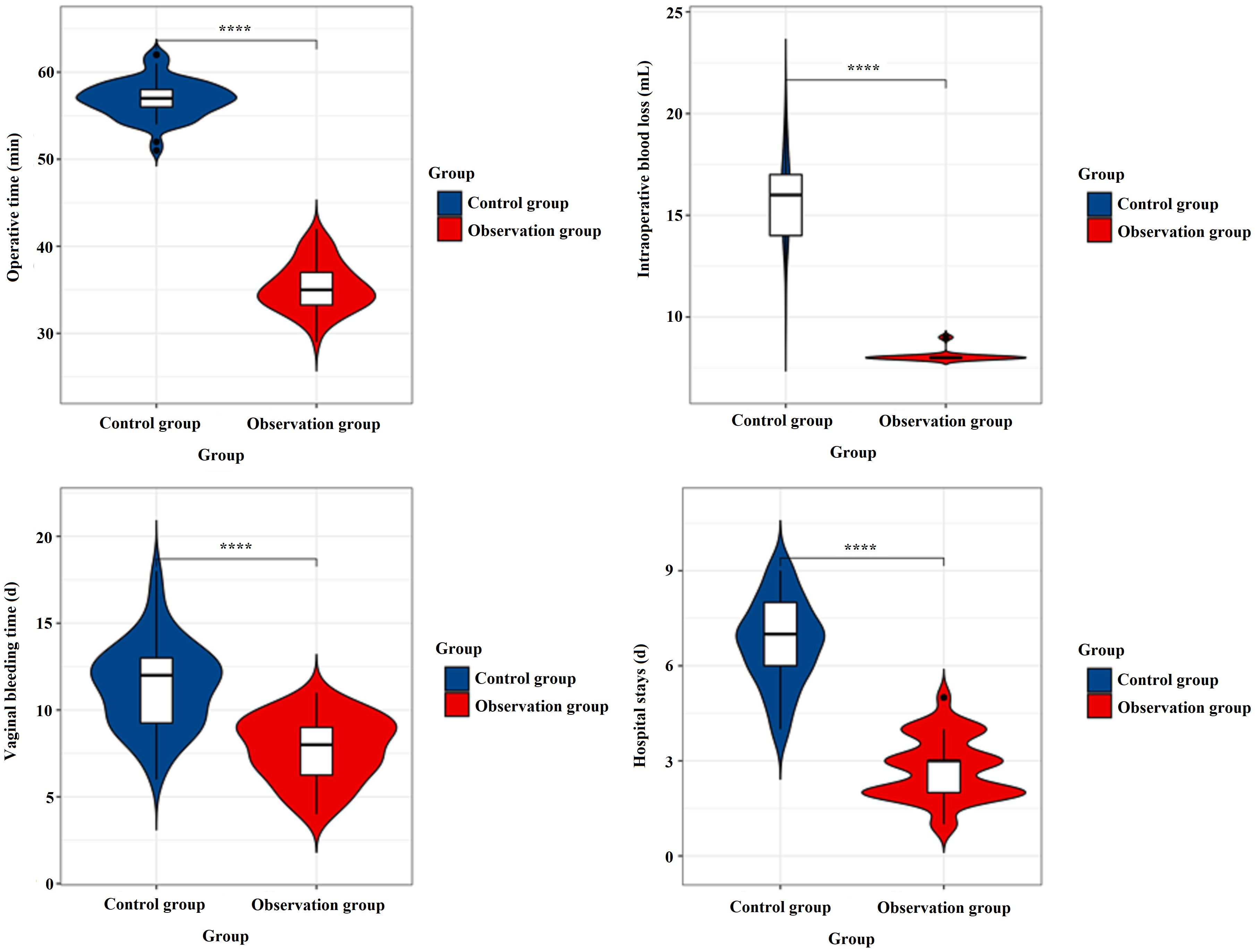
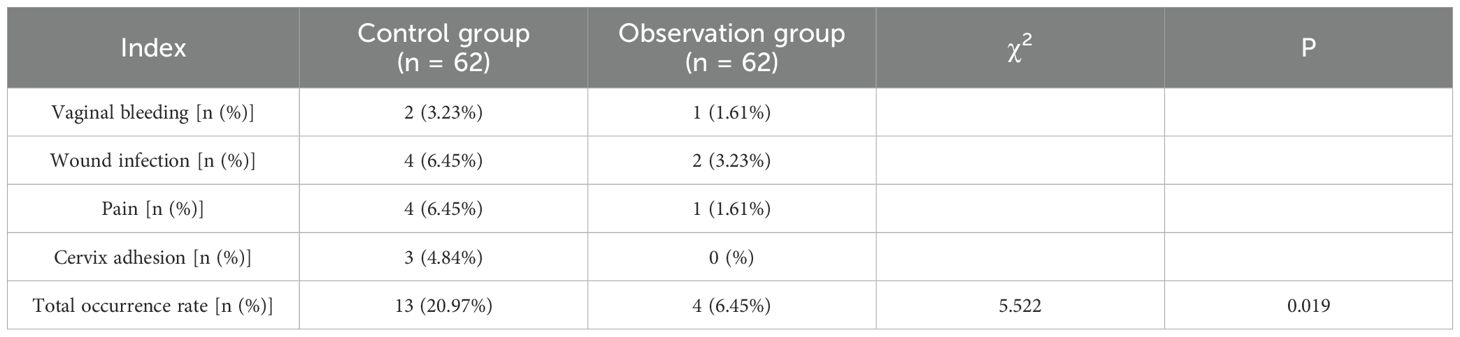
Results: The efficacy of the observation group was markedly better than that of the control group (95.16% vs. 75.81%, χ² = 9.358, P = 0.002). The operative time (35.35 ± 2.81 vs. 56.92 ± 2.17 minutes), intraoperative blood loss (8.08 ± 0.27 vs. 16.03 ± 2.27 mL), vaginal bleeding time (7.76 ± 1.85 vs. 11.37 ± 2.45 days), and hospital stays (2.74 ± 0.97 vs. 6.73 ± 1.33 days) were all significantly shorter in the observation group (P < 0.001). The complication rate was also lower (6.45% vs. 20.97%, P = 0.019).
Conclusion: The findings suggest that this combined therapy is not only more effective but may also improve pregnancy outcomes for patients, making it a promising option for clinical application.
1 Introduction
Cervical cancer is one of the most common malignancies among women, ranking fourth after breast, colorectal, and lung cancers (1). In China alone, about 130,000 new cases and 50,000 deaths occur annually (2). In recent years, advancements in screening techniques and vaccination programs have been crucial in reducing cervical cancer incidence, although challenges remain in implementing these measures in resource-limited areas (3). Cervical intraepithelial neoplasia (CIN) represents premalignant changes in the cervical epithelium and is graded I–III based on severity (4, 5). High-grade lesions (CIN II–III) carry a 20–30% risk of progression to invasive cancer within 10–20 years, making early detection and treatment crucial (6). Persistent infection with high-risk human papillomavirus (HR-HPV) underlies most CIN cases, with HPV 16 and 18 accounting for roughly 70% of lesions (7–9). – Managing CIN effectively—by excising dysplastic tissue while preserving cervical function—is key to preventing cervical cancer, especially in women of reproductive age.
The therapy modalities of CIN main include cold knife cut method (CKC), loop electrosurgical excision procedure (LEEP), laser therapy and freezing therapy (15). LEEP knife surgery is a minimally invasive procedure commonly used in clinical practice, which can play a primary part in the therapy of cervical lesions. Compared with traditional surgery, it only requires local anesthesia or even no anesthesia, and does not require suture removal, which reduces the patients’ pain. Moreover, it can reduce the damage to the adjacent tissues of lesions, the intraoperative bleeding is less, the operation time is shorter (10, 11). A study on the efficacy of LEEP has demonstrated that it is effective in reducing cervical dysplasia and preserving cervical function, which is especially crucial for women of reproductive age (12, 13). However, one known drawback of the LEEP technique is the occurrence of thermal artifacts at the surgical margins, which may hinder accurate pathological assessment, particularly in determining margin status.
Colposcopy provides real-time visualization of cervical lesions and may improve the precision of LEEP procedures. While cold knife conization (CKC) remains a standard treatment for CIN, it is a more invasive procedure, requiring general anesthesia and often resulting in higher complication rates. By contrast, LEEP, especially when performed with colposcopic guidance, offers a less invasive and potentially more precise method of lesion excision. However, limited evidence is available comparing clinical outcomes between CKC with colposcopic guidance and conventional LEEP in terms of surgical success, complication rates, and fertility-related prognosis. Therefore, this study aims to evaluate the clinical and prognostic impact of colposcopy-guided LEEP compared to CKC in the treatment of CIN, particularly in populations with fertility concerns.
2 Materials and methods
2.1 General information about patients
A total of 124 patients diagnosed with CIN and admitted to our hospital between January 2022 and December 2023 were included in this study. The patients were divided into the control group (n=62) and the observation group (n=62) based on a predefined therapeutic schedule, according to the treatment protocol followed at our institution. The allocation to either the control group (cold knife conization, CKC) or the observation group (colposcopy-guided LEEP) was not influenced by clinical urgency, patient preference, or the severity of the condition.
The control group was 26–58 years old, with a mean of 35.68 ± 6.53 years. The duration of the disease ranged from 5 months to 2 years, with a mean of 1.21 ± 0.39 years. The results of physical examination were cervical smooth in 26 cases and cervical erosion in 36 cases. The CIN classification included 34 Grade II and 28 Grade III. The patients in observation group ranged in age from 25 to 56 years, with a mean of 34.78 ± 6.68 years. The duration of disease ranged from 3 months to 2 years, with a mean of 1.29 ± 0.41 years. The results of physical examination showed that 29 cases had a normal cervical appearance, while 33 cases exhibited cervical erosion. The classification of CIN was Grade II (36 cases) and Grade III (26 cases). There was no obvious difference in the general data between the two groups (P > 0.05). This study has been reviewed and approved by the hospital Ethics committee, and all patients have given their informed consent.
Sample size estimation: The minimum required sample size was calculated using a power analysis based on our previous experience, assuming a difference in total effective rate of 20% between groups, with α = 0.05 and power (1 − β) = 0.80. The calculation yielded a required sample size of at least 56 patients per group, which was exceeded in this study.
2.2 Inclusion and exclusion criteria
Inclusion criteria: (1) Patients who meet the diagnostic criteria for CIN in the Standardized Diagnosis and Treatment Guidelines for Cervical Cancer and Precancerous Lesions (Trial); (2) Patients confirmed by colposcopy, thin-prep cytology test (TCT), or HPV testing; (3) Patients with histologically confirmed CIN II-III on cervical biopsy; (4) Patients who are married or have a sexual history; (5) Primary patients; (6) Patients with no history of antitumor therapy; (7) Patients with good compliance and can cooperate with follow-up.
Exclusion criteria: (1) Patients with reproductive tract infection, cervical inflammation and other gynecological diseases; (2) Patients diagnosed with cervical carcinoma in situ or with ovarian tumors; (3) Patients with dysfunction of vital organs; (4) Patients with history of pelvic or hysterectomy; (5) Patients with coagulation and immune dysfunction; (6) Patients with mental illness or communication disorders; (7) Patients who are lactating or pregnant.
2.3 Methods
The observation group was treated with colposcopy combined with LEEP. The operation was performed between the 4th and 7th day after the end of menstruation. Patients were instructed to assume the bladder lithotomy position. The vulva and cervix were fully exposed after routine disinfection, and a speculum was inserted to visualize the vaginal vault and cervix. Colposcopy (OPTOMIC; Model: OP-C5) was then used to examine the cervical area. Acetic acid and iodine staining tests were performed to assess the cervical morphology and delineate the extent of lesions, which were marked accordingly. Following this assessment, local anesthesia was administered using a 1% lidocaine hydrochloride injection (Hebei Tiancheng Pharmaceutical Co., Ltd.) to facilitate the subsequent surgical procedure. And the scope and grade of lesions were further confirmed to select the appropriate LEEP cutter head (Beijing Yakokunda Medical Technology Co., LTD.) to excise the lesions. The specific operating criteria: the electric cutting power was set at 30–50 W, the incision made from 0.3 - 0.5cm away from the uncolored margin of the cervix, and the moving electrode rotated clockwise to remove the lesion in a circular manner. The excision range should exceed the lesion margin by 0.3 - 0.5mm, and the cutting depth should be determined according to the lesion grade (the depth of CIN II grade is 0.5 - 1.0 cm, the depth of CIN III grade is 1.0 - 1.5 cm). After colposcopic observation to ensure clean excision and electrocoagulation to stop bleeding, the excised lesions were sent for examination. Treatment success was defined as complete lesion excision with negative pathological margins and no visible residual lesion under follow-up colposcopy at 3 months. Postoperative care included routine cleaning, disinfection, and anti-infection treatment. Patients were advised to avoid sexual activity, vaginal medication, and douching for 4–6 weeks, and were monitored regularly during follow-up.
The control group underwent CKC. Patients were positioned and prepared similarly to those in the observation group. Using a scalpel, a cone-shaped excision was performed by making a circumferential incision at the 12 o’clock position on the cervical mucosa. The incision was directed obliquely at a 45° angle toward the cervical canal, with a depth of approximately 15 mm to ensure complete removal of the lesion. Hemostasis was achieved through direct pressure with sterile gauze.
2.4 Observation indicators
Evaluated based on intraoperative findings, postoperative pathology, and follow-up at 3 months after treatment. All excised specimens were sent for histopathological examination. The involvement of surgical margins (positive/negative) was recorded. Recurrence was defined as histologically confirmed CIN II or higher on follow-up.
1. Clinical effect: The evaluation was based on histological examination (biopsy). Cure was defined as complete epithelialization of the cervix and absence of residual lesions. Effective referred to ≥75% improvement in lesion healing as observed during follow-up. Cases showing less than 75% improvement were deemed ineffective. Total effective rate = (Cured cases + Effective cases)/Total cases × 100%.
2. Surgical indicators: Intraoperative blood loss, operative time, vaginal bleeding time and hospital stays were compared.
3. Complications: Postoperative complications such as vaginal bleeding, wound infection, pain and cervix adhesion were compared between the two groups.
2.5 Statistical methods
SPSS 27.0 analysis software was applied. All continuous variables were tested for normality before t-tests, and the Shapiro-Wilk test was used to assess whether the data conformed to normal distribution. If the data did not conform to normal distribution, nonparametric tests (such as the Mann-Whitney U test) were used for comparison. The measurement data expressed by (), and t-test was adopted. The count data were statistically described by percentages, and the comparison of rates between groups was performed using the chi-square test, with P < 0.05 indicating that the difference was statistically significant.
3 Results
3.1 Results of clinical efficacy
As shown in Table 1 and Figure 1, the observation group achieved a significantly higher total effective rate (95.16%) compared to the control group (75.81%) (χ² = 9.358, P = 0.002).
3.2 Results of clinical surgical indexes
The mean operative time in the observation group was 35.35 ± 2.81 minutes, significantly shorter than 56.92 ± 2.17 minutes in the control group (t = 47.892, P < 0.001). Intraoperative blood loss was markedly reduced in the observation group (8.08 ± 0.27 mL) compared to the control group (16.03 ± 2.27 mL) (t = 27.399, P < 0.001). Vaginal bleeding time was also shorter in the observation group (7.76 ± 1.85 days) versus the control group (11.37 ± 2.45 days) (t = 9.259, P < 0.001). Additionally, hospital stays were significantly reduced in the observation group (2.74 ± 0.97 days) compared to the control group (6.73 ± 1.33 days) (t = 19.004, P < 0.001). As shown in Table 2 and Figure 2.
3.3 Results of the occurrence of complications
As shown in Table 3, the total complication rate in the observation group was significantly lower than in the control group (6.45% vs. 20.97%, χ² = 5.522, P = 0.019). Specifically, the rates of vaginal bleeding (1.61% vs. 3.23%), wound infection (3.23% vs. 6.45%), pain (1.61% vs. 6.45%), and cervix adhesion (0% vs. 4.84%) were all lower in the observation group compared to the control group.
4 Discussion
The occurrence and progression of cervical cancer is thought to be a multi-factor, multi-step, multi-stage dynamic development of the pathological process, which is from normal cervical-HPV infection to CIN to cervical cancer progression, which is a relatively long process, about ten years or even decades (14, 15). CIN is the precancerous stage of cervical cancer, the prevalence of CIN I resolves naturally, only a small percentage of lesions persist or develop into CIN II - CIN III, and roughly 10 - 20% of CIN II - CIN III ultimately develop into cervical cancer (16). Since it is necessary to go through a relatively long stage of precancer to develop cervical cancer, timely diagnosis and correct therapy of patients at the stage of precancer are likely to potentially reduce the occurrence and mortality for cervical cancer. Recently, the occurrence of CIN has shown an obvious trend of rejuvenation, and more CIN patients require the preservation of reproductive function (17, 18). Therefore, it is particularly vital to maximize the preservation of the reproductive potential of young patients with CIN. In recent years, LEEP has become the main therapy method for CIN. It is a therapeutic means of conical excision of suspected diseased cervical tissues by using an electric knife with a circular or triangular metal ring, which is passed through a high-frequency electric current (19). Through the high-frequency current can quickly generate ultra-high frequency radio waves, in contact with the human soft tissue that can generate impedance to generate a large amount of heat energy, so that the cells instantly become explosive dehydrated tissue. The various operations such as cutting and hemostasis are accomplished without affecting the pathological examination of the organisms at the margins of the incision (20, 21).
The mechanism of LEEP is the principle of high heat, which can improve the surgical accuracy and reduce the damage to normal tissue (22). At the same time, the operation can preserve the fertility function and meet the fertility needs of patients. In our study, colposcopy combined with LEEP was used to make full use of the role of colposcopy, which could improve the surgical field of view, promote the grasp of the disease information, and maximize the removal of diseased tissue, thus improving the clinical effect (23–25). Our study revealed that the efficacy of the observation group was better than the control group (P < 0.05), indicating that the combined application of colposcopy and LEEP can enhance the therapeutic effect and promote clinical efficacy, and has good application value. Because colposcopy combined with LEEP can achieve complementary advantages, colposcopy provides a good operating field, combined with arc resection can achieve complete resection of lesions. It is conducive to hemostasis, so as to effectively improve clinical therapy effect (26). At the same time, our results indicated the operative time, vaginal bleeding time, intraoperative blood loss and hospital stays in the observation group were lower (P < 0.001), suggesting that colposcopy combined with LEEP could shorten the operation time and discharge time, reduce the amount of intraoperative blood loss. The reason may be that the use of colposcopy can more clearly observe the cervical lesions, especially the relationship between the lesion and the normal tissue, so as to promote the complete removal of the lesion (27). Meanwhile, a good surgical field is conducive to the refinement and accurate operation of the operation, thus effectively shortening the operation time, reducing the trauma to the patient, and providing favorable conditions for a good postoperative recovery (28).
Our results presented the occurrence of complications in the observation group was markedly reduced (P < 0.05), indicating that the above combined therapy regimen could prevent complications, not only improve the safety of LEEP, but also promote a good prognosis. We analyzed that the combined application of colposcopy and LEEP could maximize the resection of the lesion and facilitate the observation of normal tissues around the lesion, thus reducing unnecessary damage and preventing the occurrence of cervical adhesion and bleeding (29, 30). “In addition to the immediate clinical outcomes, the long-term recurrence of HPV-related lesions remains a key concern in the management of CIN. Several studies have explored the long-term risk factors for recurrence after surgical interventions such as conization. For example, a retrospective multi-institutional study highlighted the role of HPV vaccination in reducing the recurrence risk of cervical dysplasia after conization (31). Although the study did not find a statistically significant reduction in recurrence, it suggested that vaccination slightly lowers the risk of recurrent disease, particularly in patients who had at least one negative examination between conization and the diagnosis of recurrent lesions. This finding underscores the importance of integrating vaccination strategies in cervical dysplasia management to potentially reduce the risk of recurrence over time. Thus, while colposcopy-guided LEEP is effective in the short term, additional interventions, including vaccination, should be considered to further reduce the risk of recurrence and improve long-term patient prognosis. It is essential for future research to assess the cost-effectiveness and broader application of HPV vaccination, particularly in women undergoing conization for CIN”.
This study has several limitations. As a retrospective, single-center design, it is subject to selection bias and observer bias, which may affect the generalizability of the results. The small sample size further limits the external applicability of our findings. The lack of randomization in this study, with allocation based on therapeutic schedule, could have introduced selection bias. The lack of colposcopy in the control group may have introduced detection bias. Moreover, the follow-up period for lesion recurrence was limited to only 3 months, which may not be sufficient for assessing long-term CIN outcomes. While we controlled for some confounding factors, unmeasured variables could still influence outcomes. To confirm our findings, prospective, multicenter, and larger-scale studies with randomized designs are needed to minimize biases and improve the reliability of the results.
5 Conclusion
In summary, colposcopy combined with LEEP is an effective therapy for high-grade CIN, particularly CIN II and CIN III. This approach can improve clinical outcomes, reduce intraoperative blood loss, shorten operation time, and minimize hospital stays. These advantages highlight the potential of colposcopy combined with LEEP as a valuable treatment option for high-grade CIN. However, the retrospective nature, single-center design, and small sample size of this study limit the generalizability of the findings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by This study was approved by the Ethics Committee of the Guang’an People’s Hospital (Approval number: 2023-Ethical review-15). Informed consent was obtained from all the participants. All methods were carried out in accordance with Declaration of Helsinki. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FJ: Conceptualization, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. LW: Conceptualization, Data curation, Formal Analysis, Software, Visualization, Writing – review & editing. ZS: Investigation, Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Global Health. (2020) 8:e191–203. doi: 10.1016/S2214-109X(19)30482-6
2. Ji L, Chen M, and Yao L. Strategies to eliminate cervical cancer in China. Front Oncol. (2023) 13:1105468. doi: 10.3389/fonc.2023.1105468
3. Palumbo M, Lavitola G, Di Filippo C, Foreste V, Granata M, Imperatore O, et al. Impact of Human papillomavirus 9-valent vaccine on viral clearance after surgical treatment: A single-center retrospective observational study. Eur J Obstet Gynecol Reprod Biol. (2025) 310:113994. doi: 10.1016/j.ejogrb.2025.113994
4. Kalliala I, Athanasiou A, Veroniki AA, Salanti G, Efthimiou O, Raftis N, et al. Incidence and mortality from cervical cancer and other Malignancies after treatment of cervical intraepithelial neoplasia: a systematic review and meta-analysis of the literature. Ann Oncol. (2020) 31:213–27. doi: 10.1016/j.annonc.2019.11.004
5. Loopik DL, Bentley HA, Eijgenraam MN, IntHout J, Bekkers RL, and Bentley JR. The natural history of cervical intraepithelial neoplasia grades 1, 2, and 3: a systematic review and meta-analysis. J Lower Genital Tract Dis. (2021) 25:221–31. doi: 10.1097/LGT.0000000000000604
6. Loopik DL, IntHout J, Ebisch RMF, Melchers WJG, Massuger LFAG, Siebers AG, et al. The risk of cervical cancer after cervical intraepithelial neoplasia grade 3: A population-based cohort study with 80,442 women. Gynecol Oncol. (2020) 157:195–201. doi: 10.1016/j.ygyno.2020.01.023
7. Barra F, Della Corte L, Noberasco G, Foreste V, Riemma G, Di Filippo C, et al. Advances in therapeutic vaccines for treating human papillomavirus-related cervical intraepithelial neoplasia. J Obstet Gynaecol Res. (2020) 46:989–1006. doi: 10.1111/jog.14276
8. Spinillo A, Dominoni M, Boschi AC, Sosso C, Fiandrino G, Cesari S, et al. Clinical significance of the interaction between human papillomavirus (HPV) type 16 and other high-risk human papillomaviruses in women with cervical intraepithelial neoplasia (CIN) and invasive cervical cancer. J Oncol. (2020) 2020:6508180. doi: 10.1155/2020/6508180
9. Lazare C, et al. Evaluation of cervical intraepithelial neoplasia occurrence following the recorded onset of persistent high-risk human papillomavirus infection: a retrospective study on infection duration. Front Oncol. (2019) 9:976. doi: 10.3389/fonc.2019.00976
10. Hurtado-Roca Y, Becerra-Chauca N, and Malca M. Efficacy and safety of cryotherapy, cold cone or thermocoagulation compared to LEEP as a therapy for cervical intraepithelial neoplasia: Systematic review. Rev Saude Publ. (2020) 54:27. doi: 10.11606/s1518-8787.2020054001750
11. Bogani G, DI Donato V, Sopracordevole F, Ciavattini A, Ghelardi A, Lopez S, et al. Recurrence rate after loop electrosurgical excision procedure (LEEP) and laser Conization: A 5-year follow-up study. Gynecol Oncol. (2020) 159:636–41. doi: 10.1016/j.ygyno.2020.08.025
12. Curty G, de Carvalho PS, and Soares MA. The role of the cervicovaginal microbiome on the genesis and as a biomarker of premalignant cervical intraepithelial neoplasia and invasive cervical cancer. Int J Mol Sci. (2019) 21:222. doi: 10.3390/ijms21010222
13. Zhang X, Tong J, Ma X, Yu H, Guan X, Li J, et al. Evaluation of cervical length and optimal timing for pregnancy after cervical conization in patients with cervical intraepithelial neoplasia: A retrospective study. Med (Baltimore). (2020) 99:e23411. doi: 10.1097/MD.0000000000023411
14. Skoulakis A, Fountas S, Mantzana-Peteinelli M, Pantelidi K, and Petinaki E. Prevalence of human papillomavirus and subtype distribution in male partners of women with cervical intraepithelial neoplasia (CIN): a systematic review. BMC Infect Dis. (2019) 19:1–11. doi: 10.1186/s12879-019-3805-x
15. Xue H, Gao H, Zheng J, Chen Y, Chen J, Pan D, et al. Use of extended HR-HPV Genotyping in improving the Triage Strategy of 2019 ASCCP recommendations in Women with positive HR-HPV diagnosis and Simultaneous LSIL Cytology Results. J Cancer. (2021) 12:4332. doi: 10.7150/jca.55826
16. Zhao D, Zhang L, Xie F, Peng D, Wei J, Jiang L, et al. Outcomes of prior cervical cytology and HR-HPV testing in women subsequently diagnosed with CIN1, CIN2/3, and invasive cervical cancer: a 4-year routine clinical experience after implementation of systematic training and quality control programs. BMC Cancer. (2020) 20:1–10. doi: 10.1186/s12885-020-07321-2
17. Park J, Kim Y, Kim J, Kang S, Kim K, Kim JH, et al. Health-related quality of life of patients with cervical cancer according to the duration of treatment and cancer progression. Asian Pac J Cancer Prevent: APJCP. (2022) 23:1945. doi: 10.31557/APJCP.2022.23.6.1945
18. Casajuana-Pérez A, Ramírez-Mena M, Ruipérez-Pacheco E, Gil-Prados I, García-Santos J, Bellón-Del Amo M, et al. Effectiveness of prophylactic human papillomavirus vaccine in the prevention of recurrence in women conized for HSIL/CIN 2-3: The VENUS study. Vaccines. (2022) 10:288. doi: 10.3390/vaccines10020288
19. Naaman M, Omenge O, Ann M, Victor O, Tao L, Edwin S, et al. LEEP more effective than cryotherapy as effective treatment for CIN lesions in women living with HIV and without HIV in western Kenya (2129). Gynecol Oncol. (2023) 176:S215. doi: 10.1016/j.ygyno.2023.06.254
20. Zhou Q, Hu X, Zhou J, Zhao M, Zhu X, and Zhu X. Human papillomavirus DNA in surgical smoke during cervical loop electrosurgical excision procedures and its impact on the surgeon. Cancer Manage Res. (2019) 11:3643–54. doi: 10.2147/CMAR.S201975
21. Foggiatto AI, de Carvalho NS, Fonseca FV, and Maestri CA. Recurrence in cervical high-grade squamous intraepithelial lesion: the role of the excised endocervical canal length—Analysis of 2,427 patients. J Lower Genital Tract Dis. (2023) 27:1–6. doi: 10.1097/LGT.0000000000000708
22. Cai H, Ma T, Che Y, Wang Y, Wang C, and Yin G. Loop electrosurgical excision procedure followed by 5-aminolevulinic acid photodynamic therapy for cervical intraepithelial neoplasia, a report of six cases. Photodiagnosis Photodyn Ther. (2020) 29:101650. doi: 10.1016/j.pdpdt.2020.101650
23. Kim SI, Kim SJ, Suh DH, Kim K, No JH, and Kim YB. Pathologic discrepancies between colposcopy-directed biopsy and loop electrosurgical excision procedure of the uterine cervix in women with cytologic high-grade squamous intraepithelial lesions. J Gynecol Oncol. (2020) 31:e13. doi: 10.1016/j.ygyno.2020.04.043
24. Costa-Fagbemi M, Yakubu M, Meggetto O, Moffatt J, Walker MJ, Koné AP, et al. Risk of cervical dysplasia after colposcopy care and risk-informed return to population-based screening: a systematic review. J Obstet Gynaecol Canada. (2020) 42:607–24. doi: 10.1016/j.jogc.2019.05.017
25. Godiwala PN, Amelia G, Tierney O'K, Lena G, Karen O'K, Casey O'K, et al. Using a new hand-held colposcope in combination with cryotherapy and LEEP in a see-and-treat cervical cancer screening program. EJMO. (2019) 3:257–262. doi: 10.14744/ejmo.2019.50315
26. Kahramanoglu I, Demirkiran F, Turan H, Bese T, Yilmaz N, Ilvan S, et al. The use of colposcopic punch biopsy in the management of abnormal cervical cytology: A 5–year retrospective audit. J Obstet Gynaecol. (2019) 39:110–4. doi: 10.1080/01443615.2018.1468740
27. Xie H, Morton R, Balendran J, Philp S, Saidi S, Farrell R, et al. The impact of primary human papillomavirus screening on negative loop excision histology following biopsy-proven high-grade cervical intra-epithelial lesions: A review from a large tertiary colposcopy unit. Aust New Z J Obstet Gynaecol. (2021) 61:941–8. doi: 10.1111/ajo.13426
28. Kim J-H, Kim J, Kim K, No JH, Kim YB, and Suh DH. Risk factor and treatment of vaginal intraepithelial neoplasia after hysterectomy for cervical intraepithelial neoplasia. J Lower Genital Tract Dis. (2022) 26:147–51. doi: 10.1097/LGT.0000000000000664
29. González González V, Ramírez Mena M, Calvo Torres J, Herráiz Martínez MÁ, and Serrano García I. and P. Coronado, “Analysis of new colposcopy techniques in the diagnosis and evolution of SIL/CIN: comparison of colposcopy with the DSI system (COLPO-DSI study). J Personalized Med. (2023) 13:1605. doi: 10.3390/jpm13111605
30. Koner S, Bose C, Sen A, and Mukhopadhyay A. Evaluation of colposcopy and loop electrosurgical excision procedure (LEEP) in A rural mobile cervical cancer screening unit in west Bengal, India. Ann Oncol. (2012) 23:ix471. doi: 10.1016/S0923-7534(20)34012-6
31. Bogani G, Raspagliesi F, Sopracordevole F, Ciavattini A, Ghelardi A, Simoncini T, et al. Assessing the Long-Term Role of Vaccination against HPV after Loop Electrosurgical Excision Procedure (LEEP): A Propensity-Score Matched Comparison. Vaccines (Basel). (2020) 8:717. doi: 10.3390/vaccines8040717
Keywords: colposcopy, LEEP, CIN, clinical efficacy, prognostic effect
Citation: Jin F, Wang L and Su Z (2025) Clinical and prognostic outcomes of colposcopy-guided LEEP versus cold knife conization in the management of cervical intraepithelial neoplasia. Front. Oncol. 15:1627024. doi: 10.3389/fonc.2025.1627024
Received: 12 May 2025; Accepted: 21 July 2025;
Published: 07 August 2025.
Edited by:
Tullio Golia D’Augè, Sapienza University of Rome, ItalyReviewed by:
Mario Palumbo, Federico II University Hospital, ItalyOttavia D’Oria, Sapienza University of Rome, Italy
Copyright © 2025 Jin, Wang and Su. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhan Su, d2pqXzBfMEAxNjMuY29t
 Fengying Jin
Fengying Jin Zhan Su
Zhan Su