- 1Department of Diagnostic Innovation, Pathology Unit 2, Fondazione IRCCS Istituto Nazionale Dei Tumori, Milano, Italy
- 2Department of Oncology and Hemato-Oncology, University of Milan, Milano, Italy
- 3Department of Medical Oncology, Fondazione IRCCS Istituto Nazionale Dei Tumori, Milano, Italy
- 4Department of Pathology and Laboratory Medicine, Pathology Unit 1, Fondazione IRCCS Istituto Nazionale Dei Tumori, Milano, Italy
- 5Gynecologic Oncology Unit, Fondazione IRCCS Istituto Nazionale dei Tumori, Milano, Italy
Introduction: Ovarian cancer (OC) is one of the leading causes of cancer-related death in women worldwide. Treatment with PARP-inhibitors has significantly improved survival in patients with high-grade serous cancer (HGSC) bearing BRCA1/2 mutations (~22% of the cases), and/or homologous recombination deficiency (HRD, ~50%). Unfortunately, limited therapeutic alternatives are available for BRCA1/2 wild type/HR proficient HGSC patients, who usually exhibit resistance to standard treatments and poor prognosis.
Methods: Herein, we present the results of a comprehensive genomic profiling (CGP) analysis using the Oncomine Comprehensive Assay® (OCA) Plus in a consecutive retrospective cohort of 102 HGSC patients characterized in our institution.
Results: Genomic instability, measured by Genomic Instability Metric (GIM) >16, was found in 40% of the cases and was significantly associated with BRCA1/2 mutations (p=0.009), with a better prognosis in terms of recurrence-free survival (p=0.01). CCNE1 amplification was observed in 29% of cases and was negatively correlated with BRCA1/2 mutations (p=0.001), without any association with GIM, supporting CCNE1 as a strong and independent driver of tumorigenesis. Additionally, CCNE1 amplification was validated with fluorescent in situ hybridization (FISH), supporting the analytical robustness of NGS data (rho=0.93), and investigated by immunohistochemistry (IHC), revealing that CCNE1 protein overexpression was observed in the absence of gene amplification in 45% of cases.
Discussion: Our real-world study supports the clinical utility of the GIM metric and the analytical validity of CCNE1 amplification, a new promising biomarker for personalizing treatment in HR proficient HGSC patients. The discordance between CCNE1 amplification and protein expression raises intriguing questions about the mechanisms of CCNE1-driven tumorigenesis and warrants further investigation.
Introduction
Ovarian cancer (OC) accounts for 3% of all cancers in women and represents the deadliest gynecologic malignancy, with 294,000 new diagnoses and 198,000 deaths per year worldwide. Despite advancements in disease management, the 5-year survival rate for OC patients remains below 50% in most countries (1). This is largely attributed to the advanced stage at which the disease is typically diagnosed, the lack of solid screening tests (2), and the frequent occurrence of chemoresistance (3). Primary debulking surgery followed by platinum-based chemotherapy (CT) is the standard therapeutic approach for advanced stage disease (III and IV), while maintenance treatment with bevacizumab and/or poly (ADP-ribose) polymerase inhibitors (PARPi) is based on molecular and clinical characteristics (National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology, Version 3.2024).
OC is a highly heterogeneous disease with five major etiologically and genetically distinct histological types of ovarian carcinomas bearing specific molecular features, clinical behavior, response to treatment, and outcome (4). High-grade serous carcinoma (HGSC) is the prevalent histology (70%–75%), accounting for almost 80% of the deaths (5). HGSC harbors inactivating mutations in the tumor suppressor gene TP53 in >95% of the cases and germline or somatic BRCA1/BRCA2 gene variants, which are frequently associated with homologous recombination deficiency (HRD) in up to 22% of the cases (6). BRCA1/2 mutations represent both a prognostic factor and a predictive marker of response to platinum-based chemotherapy and to PARPi (7). Moreover, patients carrying a germline mutation in BRCA1/2 have increased cancer risk, which may also involve their relatives (8). For these reasons, the American Society of Clinical Oncology guidelines stated that germline or somatic BRCA1/2 testing should be performed in all patients with epithelial OC (8, 9). Along this line, the European Society for Medical Oncology guidelines stated that all patients with high-grade OC should be tested for germline and/or somatic BRCA1/2 mutations at diagnosis, and HRD testing is recommended in advanced cases (10). Several assays have been developed to evaluate BRCA1/2 and HR status (11). The Food and Drug Administration (FDA)-approved Myriad MyChoice CDx panel predicts HRD using a genomic instability score (GIS) computed by integrating loss of heterozygosity (LOH), large-scale state transitions (LSTs), and telomeric–allelic imbalance (TAI) (7, 11). BRCA1/2 mutation and HRD are currently the only biomarkers approved for targeted therapeutic approaches with PARPi in HGSC patients; indeed, the FDA recently approved the Myriad MyChoice assay for HRD detection (12). HRD is a multifaceted biomarker, arising from a combination of diverse genomic alterations, that requires a comprehensive and complex analysis for its accurate definition (12). Alternative tests assessing HRD through different algorithms have been recently implemented, including FoundationOne® CDx (Foundation Medicine), TruSight Oncology 500 HRD (Illumina), SOPHiA DDM HRD (SOPHiA Genetics), and AmoyDx HRD Focus Panel (AmoyDx) (13, 14). Particularly, Oncomine Comprehensive Assay Plus (Thermo Fisher Scientific) was recently implemented with HRD analysis by means of Genomic Instability Metric (GIM) computing, whose algorithm has already undergone extensive validation (14–17). In addition to HRD analysis, approximately 500 other genes are characterized for their mutational and copy number status, making OCA Plus one of the more complete target next-generation sequencing (NGS) assays available.
The mutational spectrum of HGSC also includes BRAF, NF1, ATR, ATRX, PIK3CA, RB1, CDK12, FAT3, CSMD3, and GABRA6 mutations, albeit at lower rates (1%–6%) (18, 19), with many of these alterations currently recognized as therapeutics targets in other solid tumors or under investigation in experimental clinical trials (20). In addition, HGSC is a chromosomally unstable malignancy commonly bearing amplifications in the CCNE1 (~20%), MYC (~30%), and MECOM (~25%) genes (21). CCNE1 amplification particularly represents one of the most promising targets for BRCA1/2 wild-type, HR-proficient HGSC patients (6). In this regard, AZD1775 (Adavosertib), a WEE1 kinase inhibitor operating downstream of CCNE1, or the CDK2 inhibitors INCB123667 and BLUE-222, which directly prevent the CCNE1-CDK2 complex formation, are currently under clinical investigation for anticancer activity in HGSC patients carrying CCNE1 amplification or protein overexpression (22–24). Recently, other cell-cycle inhibitors, lunresertib and azenosertib, respectively targeting PKMYT1 and WEE1, have been introduced in clinical trials concerning ovarian cancer and many other solid tumors (25–27).
Collectively, these data support the rationale for including CCNE1 among the biomarkers to be tested routinely in advanced/metastatic cancer patients.
No real-world series from clinical practice using a single Comprehensive Genomic Profiling (CGP) commercially available target DNA panel has been reported to date. For example, in 2019, Zhong et al. (28) investigated a cohort of 88 individuals using a custom panel, but they did not describe any CCNE1 amplification. Dumur et al. (16) validated the OCA Plus panel in a pan-cancer study including generically defined ovarian cancer.
In this scenario, we report a complete molecular characterization of 102 consecutive HGSC, carried out for both optimizing patients’ stratification with currently available therapies and uncovering targets for enrollment in clinical trials in the context of our institutional molecular tumor board (29).
Patients and methods
Patients and sample collection
The study comprises a cohort of 102 consecutive patients with HGSC who were tested using CGP at the Department of Diagnostics Innovation of Fondazione IRCCS Istituto Nazionale dei Tumori (Milan, Italy) from March 2022 to October 2023. The study was performed in compliance with laws and institutional guidelines and has been approved by the internal Independent Ethics Committee (protocol INT 191/24, approved on 09/17/2024). All patients signed an informed consent prior to NGS data analysis. The NGS test was usually performed at cancer diagnosis, except for patients referred to our institution at disease relapse. Outcome data were retrieved from electronic health records. For outcome analysis, the following data were collected: diagnosis date, platinum-based CT starting date, maintenance therapy, and relapse date. Tumor samples were obtained from formalin-fixed paraffin-embedded (FFPE) samples. Hematoxylin–eosin sections were revised by expert pathologists to define the tumor area and cancer cell percentage. The tumor area was manually macro-dissected when necessary. DNA was extracted as previously reported (30), DNA quality was assessed by means of the 4200 TapeStation System (Agilent, CA, United States), and DNA quantity was established using Qubit High Sensitivity dsDNA quantification assay kit (Thermo Fisher Scientific, MA, United States, catalog Q32851).
Library preparation, sequencing, and analysis
CGP was performed using the commercial Oncomine Comprehensive Assay (OCA) Plus (Thermo Fisher Scientific, MA), which allows the detection of gene mutations, copy number variation (CNV), microsatellite instability (MSI), and tumor mutational burden (TMB) in 500 cancer-related genes. Libraries were generated according to the manufacturer’s instructions, quantified by the Ion Library TaqMan Quantification kit (Thermo Fisher Scientific, catalog #4468802), and diluted to a final concentration of 60 pM. Sequencing was performed on the Ion GeneStudio S5 System (Thermo Fisher Scientific) loading Ion 550 chips to obtain at least 20 million reads. Sequencing output was evaluated on the Torrent Suite 5.18.1 (Thermo Fisher Scientific) using the Coverage Analysis plugin. Library uniformity and on-target metric thresholds for quality acceptance were set to 90% and 2,000× medium coverage per case, respectively. BAM files were generated using the Variant Caller plugin of the Torrent Suite and analyzed by Ion Reporter Software (IRS) 5.20.2.0 (Thermo Fisher) with the Oncomine Comprehensive Plus 5.20 w3.1 DNA workflow (default options). The variant call format (VCFs) obtained were loaded on openCRAVAT (31), and the output variants were filtered by i) Sequence Ontology, ii) clinical significance, and iii) 1000 Genomes population frequency < 0.0001. The resulting variants were manually checked using the Integrative Genomics Viewer, Broad Institute (32), to filter out potential false-positive calls. The clinical relevance of gene variants was annotated by referring to available public databases ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/), cBioPortal (https://www.cbioportal.org/), and BRCA Exchange (https://brcaexchange.org/) and finally classified according to the American College of Medical Genetics and Genomics and the Association for Molecular Pathology (ACMG–AMP) guidelines. Pathogenic and likely pathogenic variants were considered for potential therapeutic options by standard care or targeted therapies, following the European Society of Medical Oncology (ESMO) indications (33). CNV analysis was performed on IRS (Ion Reporter Software 5.20 User Guide, MAN0028321). Copy number estimate reliability was evaluated using the Median of the Absolute values of all Pairwise Differences (MAPD > 0.5 as mandatory threshold for CNV analysis), calculated for each sample, as well as the CNV-pValue, calculated for each call. CNV calls with p-value > 0.00001 were considered not reliable (34) and then excluded.
Fluorescence in situ hybridization
Fluorescence in situ hybridization (FISH) was carried out in cases bearing CCNE1 copy number gains by NGS. The Abnova CCNE1/CEN19p dual-color FISH Probe kit, containing the Spectrum Red-labeled CCNE1 probe and the Spectrum Green-labeled Centromere 19 probe (#16032995), was used in FFPE sections. FISH slides were evaluated using a Leica DM 6000B (Wetzlar, Germany) microscope at ×100 magnification. A minimum of 50 tumor nuclei from the formalin-fixed tissue were scored. The images were captured using the CytoVision software (v. 7.0, Leica). Samples with a ratio of CCNE1 to chromosome 19 centromere signals > 2, as well as samples with multiple copies of the CCNE1 gene arranged in clusters, were considered amplified as described by Varella-Garcia et al. (35).
Immunohistochemistry
Immunohistochemistry (IHC) was carried out to investigate the protein expression beyond gene copy gain. Three-micrometer FFPE sections were placed on polarized glass slides; antigen retrieval was performed at high pH and 96°C for 15 minutes. The anti-CCNE1 antibody (clone HE12, sc-247, Santa Cruz, CA, USA) and the Dako Autostainer Link 48 were used. Testis and kidney slides were used as positive (germ cells and glomeruli, respectively) and negative (Leydig cells and tubules, respectively) controls. Staining was blindly evaluated by two pathologists and assessed using the H-score; neoplastic cells were divided into four groups (negative, weak, moderate, and strong) based on the expression level of CCNE1 in both the nucleus and cytoplasm. The H-score was calculated as a weighted average of the percentages of weak staining (weight = 1), moderate staining (weight = 2), and strong staining (weight = 3), with a range of 0–300. Discordant cases were further discussed until an agreement was reached. Based on the H-score distribution, cases were further assessed as positive or negative. The H-score threshold was set at 120 by calculating the lowest point of the bimodal distribution of H-score (120.9897) (Supplementary Figure S1).
Statistical analysis
All the associations of categorical variables (CCNE1 amplification, BRCA1/2 mutation, and GIM positivity) with numeric variables (GIM scores, %LOH, total number of SNV, TMB, total number of mutations, and CNVs in the HR gene) were evaluated using the Mann–Whitney test. Categorical variables (genomic instability status and BRCA1/2 mutation presence, CCNE1 amplification and IHC status, CCNE1, BRCA1/2 status, HRD, and disease relapse) were compared by Fisher’s test. Correlation analysis was performed using Spearman’s test. Recurrence-free survival (RFS) was analyzed using the log-rank test and the Kaplan–Meier method. Odds ratio (OR) values and their 95.5% confidence intervals were extracted from a multivariate logistic regression model fitted to individual-level data. All the analyses and visualizations were performed using R Version 4.3.1 (R Foundation for Statistical Computing).
Results
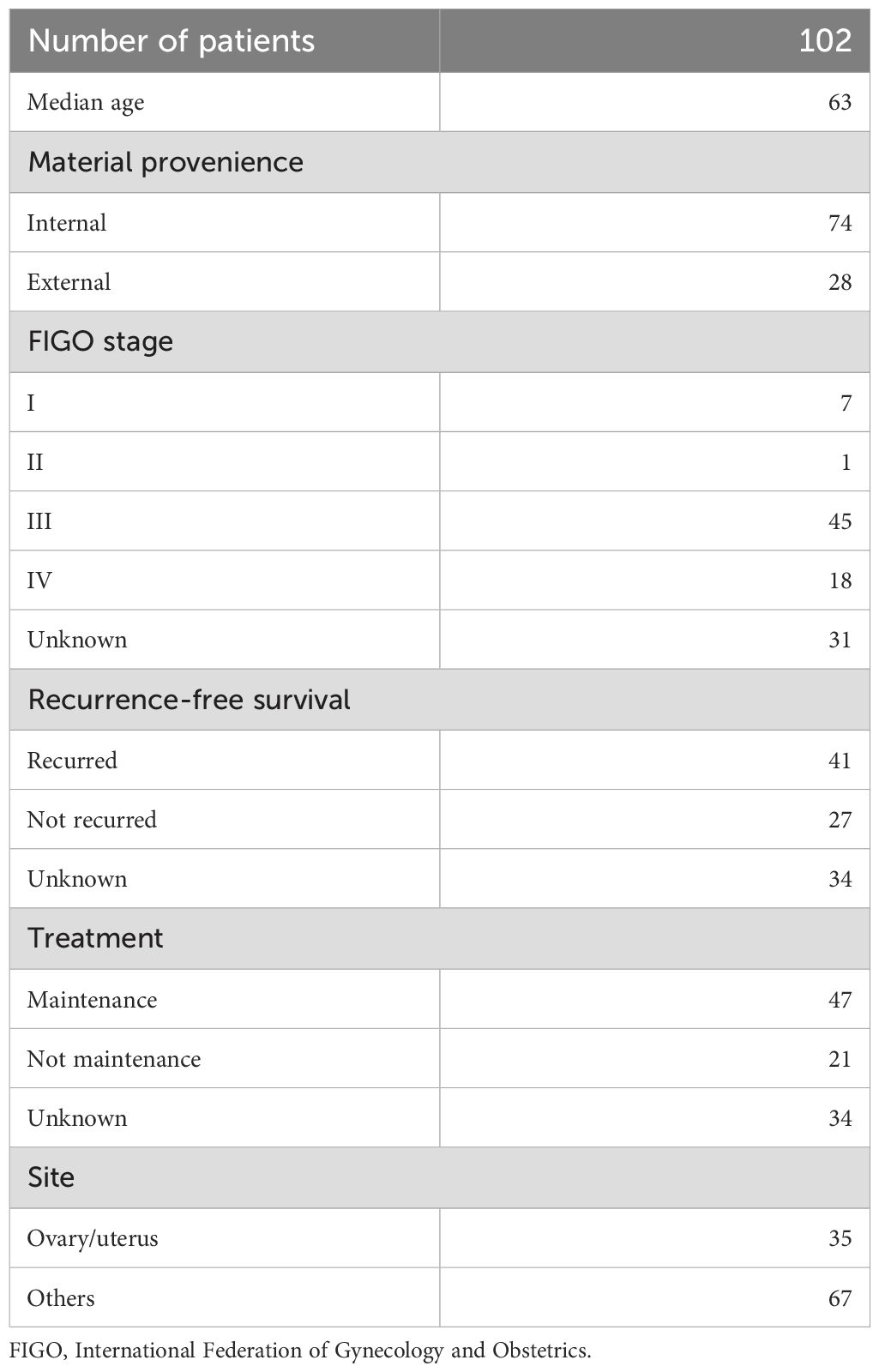
Clinico-pathological characteristics are detailed in Table 1. The median patient age was 63 years (range 36–88). According to the International Federation of Gynecology and Obstetrics (FIGO) (27) staging, 63.89% and 23.61% of the patients had stage III and stage IV diseases, respectively. Correlations between molecular data and outcome were available for 61 out of the 102 patients included in the study. Most patients (76/102, 74.51%) were diagnosed and treated in our institute, whereas the remaining (26/102, 25.49%) were outpatients who were referred for genomic profiling.
CGP analysis of HGSC confirmed high prevalence of pathogenic mutations
Figure 1 shows an overview of the mutational spectrum of the HGSC patients included in this study. Overall, 968 variants were detected in 102 cases (median, 8; range, 3–50), with a median TMB of 3.83 (range, 0–51.08). As expected, the commonest mutated genes were TP53 (94/102, 92.15%, with 81.37% pathogenic/likely pathogenic variants), BRCA1 (22/102, 21.57%, with 18/102, 17.64%, pathogenic/likely pathogenic), and BRCA2 (16/102, 15.68%, with 9/102, 8.82% pathogenic/likely pathogenic) (Figure 1). Overall, pathogenic/likely pathogenic somatic BRCA1/2 mutations were detected in 27 cases (26.47%), with 10 of them (37.07%) confirmed as germline.
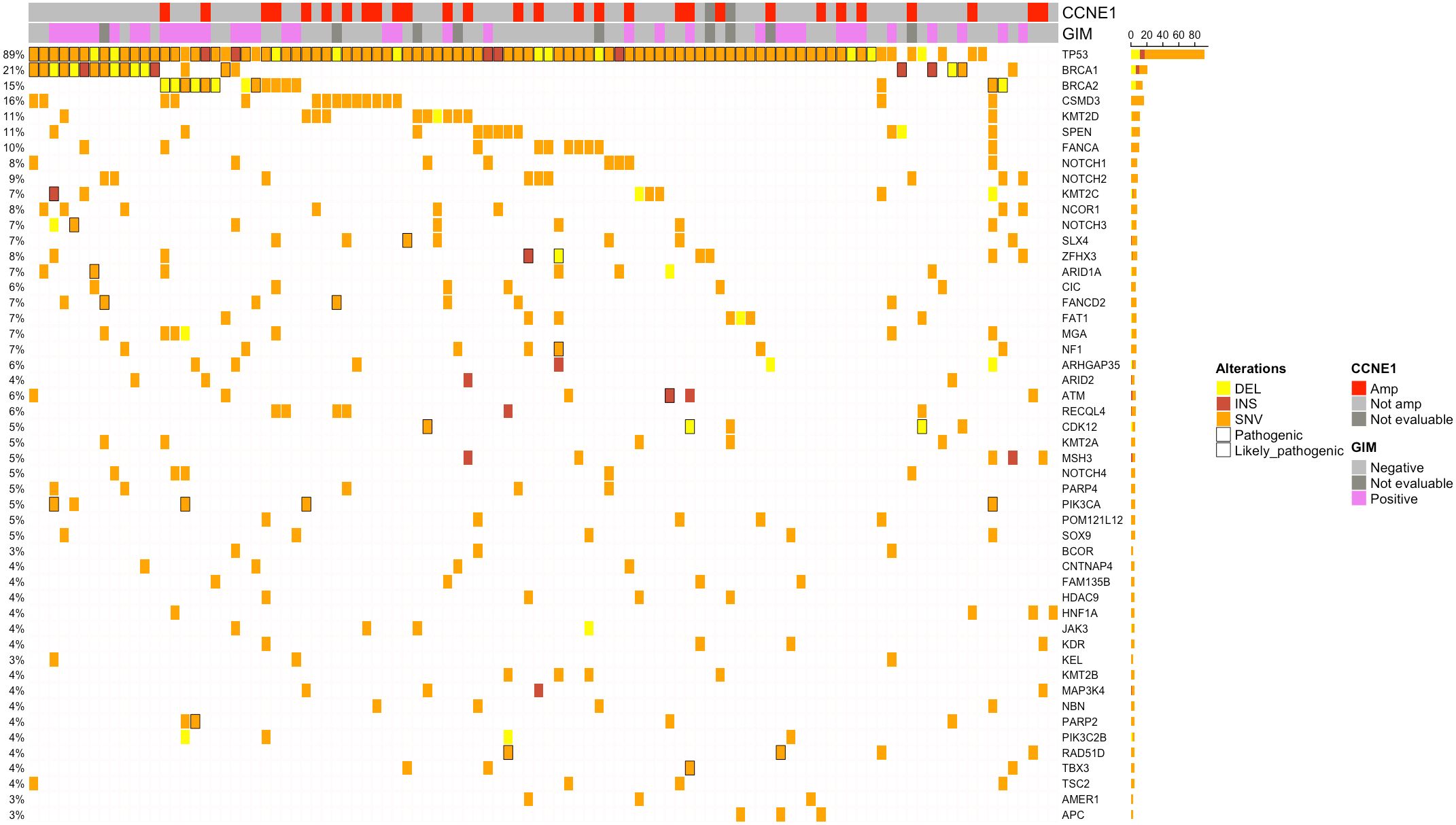
Figure 1. Oncoplots showing the top 50 altered genes by mutations. Only patients harboring alterations in selected genes are reported. Samples are represented by columns, and genes are represented by rows. Pathogenic/likely pathogenic alterations are marked in black. Indications about the Genomic Instability Metric (GIM) CCNE1 amplification status were also added. Amp, amplified; Not amp, not amplified; DEL, deletion; INS, insertion; SNV, single-nucleotide variation.
Remarkably, in 2/102 cases (1.96%), a p.Y220C variant of the TP53 gene was found. Notably, the inactivating mutation p.Y220C in p53 protein is also an emerging agnostic target, representing a potential therapeutic chance in an ongoing basket trial (19). In addition to BRCA1/2, the homologous recombination repair (HRR) genes were mutated in 23 cases (22.55%), mostly ATM (5.88%), FANCA (9.80%), NBN (3.92%), FANCD2 (6.86%), CDK12 (4.90%), and BRIP1 (2.94%). Notably, mutations were found in other potentially targetable genes, including PIK3CA (4/102, 3.92%), CDK12, PTEN, ARID1A, or BRAF (1/102 each, 0.98%).
The GIM was generated by calculating the unbalanced copy number changes in 46 genes associated with HR response, determined using genomic segmentation and yielding values ranging from 0 to 100. According to the manufacturer’s guidelines, a GIM score ≥ 16 indicates HRD as a pathogenic—and therefore druggable—condition. Sample-level LOH percentage (%LOH) is the percentage of genomic segments with LOH detected. It is calculated as the sum of the sizes of the genomic segments with LOH detected/total size of genomic segments assessed for LOH.
In 93 cases (91.17%), MAPD scores were >0.5 and were evaluable for CNV analysis as well as for GIM detection. Of these, 37 (39.78%) cases had a positive GIM score (≥16). There was a significant association between GIM score and BRCA1/2 mutation (p = 0.009142) or increased LOH percentage (p = 2.721e−05, Supplementary Figure S1). Eight BRCA1/2-mutated patients had a negative GIM score.
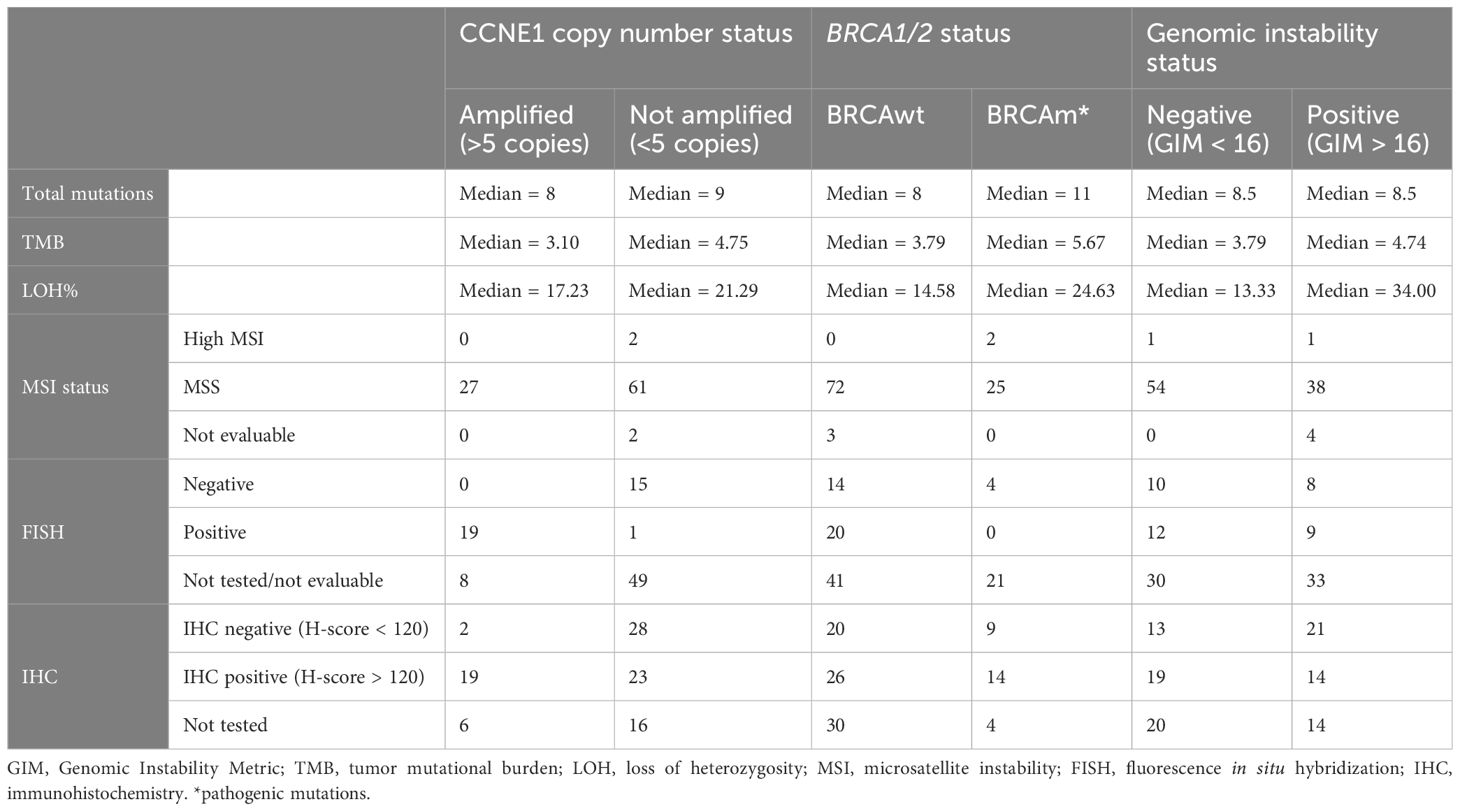
CCNE1 amplification is mutually exclusive with BRCA1/2 alteration and independent of HRD-related molecular signature
CNVs (Figure 2) occurred most frequently in the HRR genes, which represented nine of the 15 top altered genes. Copy number losses were observed in the ERAP2 (39.78%), BRCA1 (13.97%), BRCA2 (10.75%), BRIP1 (9.68%), ATM (5.37%), POLE (7.52%), CDK12 (17.20%), and POLD1 (4.3%) genes. The most common genes carrying copy number gains were CCNE1 (29.03%), MYC (26.88%), MECOM (31.18%), BARD1 (29.03%), PIK3CA (26.88%), KRAS (17.02%), JAK2 (21.50%), FAM135B (23.65%), ATR (30.10%), NOTCH3 (15.05%), CCND2 (15.05%), and ASXL1 (18.28%). Our CNV analysis was focused on genes potentially actionable with personalized treatments. CCNE1 amplification was found in 27/93 cases (29.03%, Figure 2), and it was negatively associated with BRCA1/2 mutation (p = 0.001442, Figure 3). Specifically, only two cases showed both BRCA1/2 mutations and CCNE1 amplification. The association between CCNE1 amplification and other molecular features related to genome instability, including GIM score, TMB, and LOH, was also tested: just a weak correlation between CCNE1 amplification and TMB was observed, with a median TMB of 3.10 and 4.75 in the amplified and non-amplified cases (p = 0.01813, Supplementary Figure S2).

Figure 2. Oncoplots showing the top 50 altered genes by copy number variations. Only patients harboring alterations in selected genes are reported. Samples are represented by columns, and genes are represented by rows. Pathogenic/likely pathogenic alterations are marked in black. Indications about Genomic Instability Metric (GIM) and BRCA1/2 status were also added. Amp, amplified; Not amp, not amplified; DEL, deletion; INS, insertion; SNV, single-nucleotide variation.
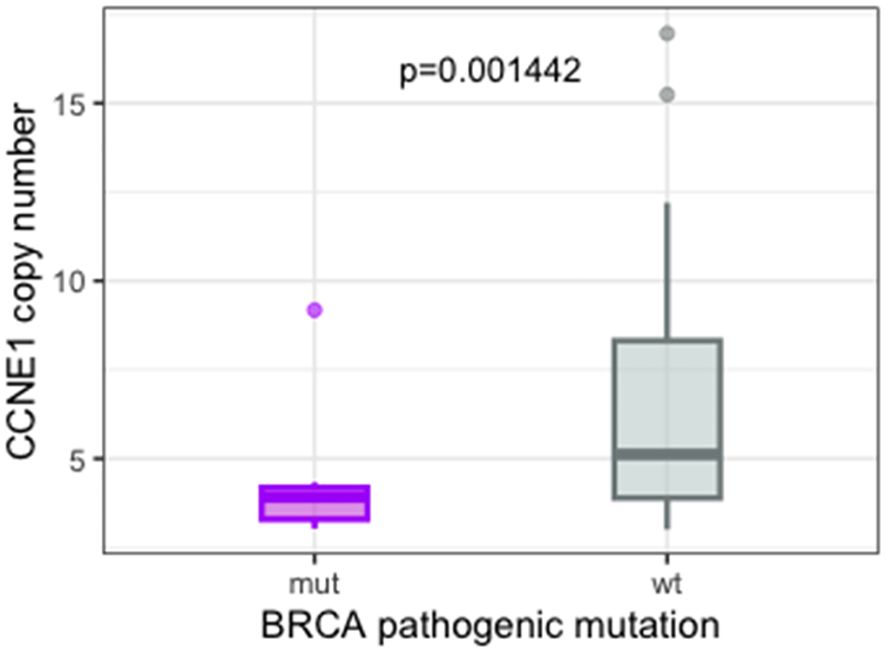
Figure 3. Boxplot showing the inverse correlation between pathogenic BRCA1/2 mutation and CCNE1 amplification detected by NGS. NGS, next-generation sequencing.
Altered actionable genes behind BRCA1/2 or CCNE1 were rare, appeared to be more often altered in the HRD setting, and most rarely co-occurred with CCNE1 amplification (2/38 HRD-positive PIK3CA-mutated, 1/38 HRD-positive BRAF-mutated, 1/38 HRD-positive CDK12-mutated, 1/27 CCNE1-positive PIK3CA-mutated, and 1/27 CCNE1-positive CDK12-mutated). Finally, pathogenic or likely pathogenic mutations in potentially actionable genes were also rare among CCNE1-negative/HR-proficient cases, being identified in eight out of 50 cases (16%). Specifically, these included two CDK12 mutations, one BRAF mutation, one KRAS mutation, two PIK3CA mutations, one NF1 mutation, and one PTEN mutation.
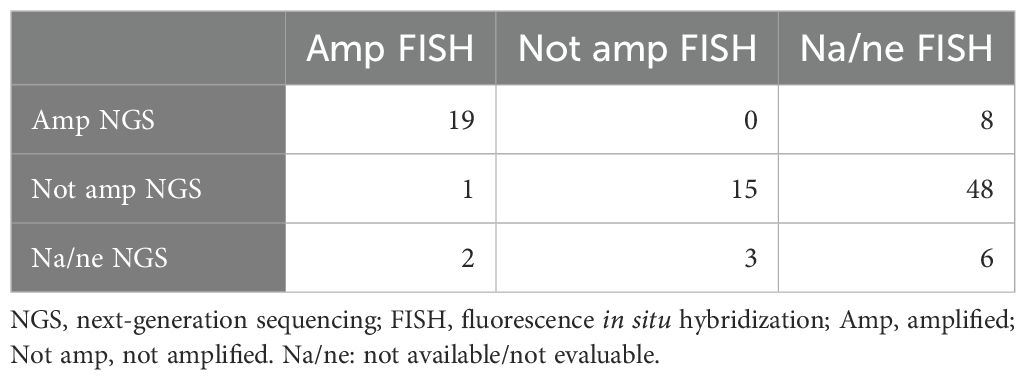
CCNE1 amplification by NGS is robustly validated by fluorescence in situ hybridization
Given the clinical interest regarding the CCNE1 gene as an emerging therapeutic target, CCNE1 NGS data were validated using FISH (Figure 4). FISH was carried out in 42 cases, including 21/27 NGS amplified cases, 15/64 NGS non-amplified cases, and 6/9 cases for which CNV NGS analysis had failed. In all but one of the 35 cases analyzable and evaluable with both techniques, FISH confirmed the NGS results.
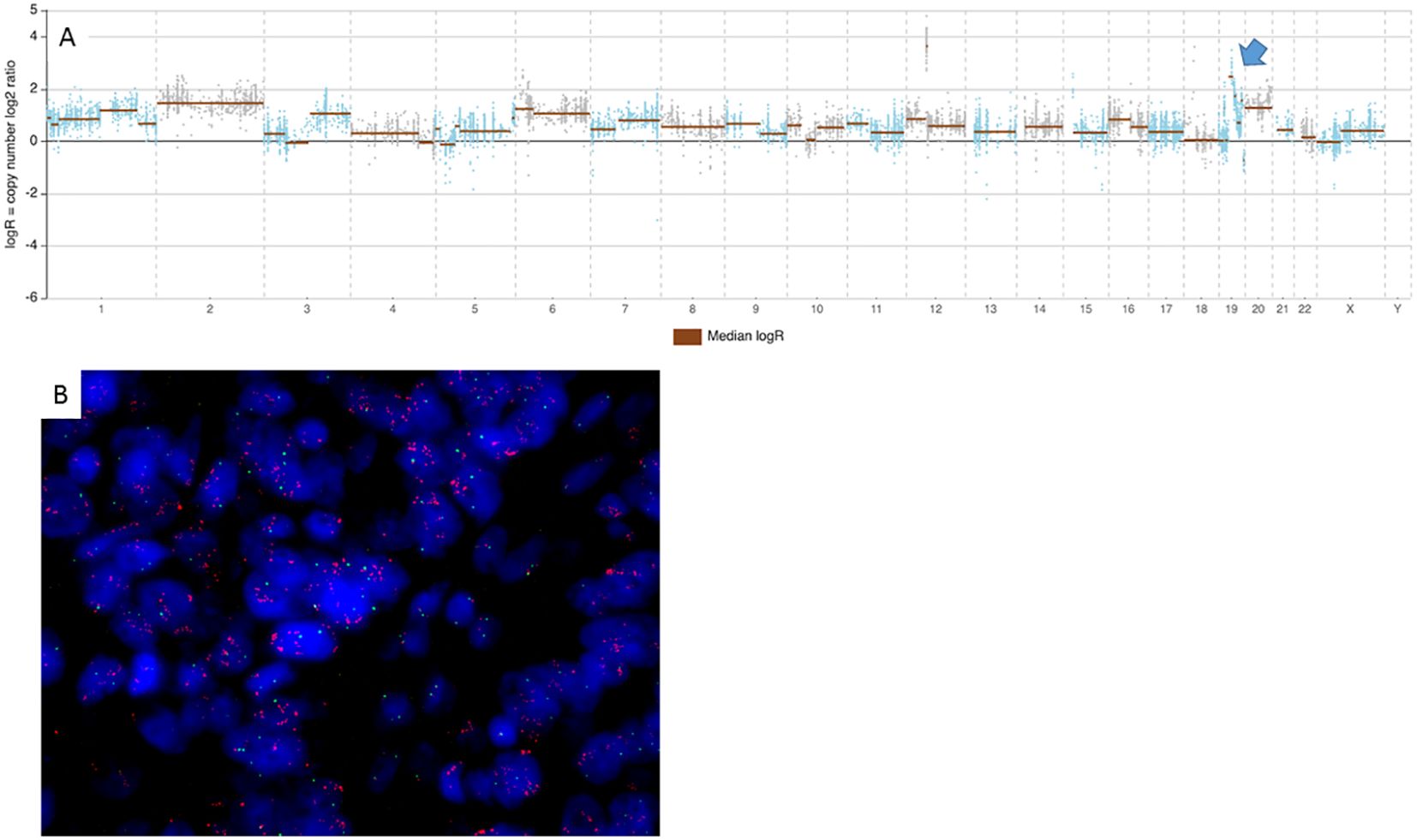
Figure 4. NGS and FISH CCNE1 pattern in an amplified case. (A) Top panels showing log2 ratios of the copy number estimates by NGS assay for each amplicon (blue and brown points). Brown horizontal bars represent genomic segmentation resulting from amplicons with similar log2 ratios clustered together. The blue arrow indicates the segment localized on CytoBand 19q12, corresponding to CCNE1 gene amplicons. The image shows a case with focal amplification of CCNE1, confirmed by FISH in the picture below (B), where green and red signals refer to centromere and CCNE1 gene, respectively. NGS, next-generation sequencing; FISH, fluorescence in situ hybridization.
In most of the amplified cases, FISH CCNE1 signals were arranged in clusters, which makes it impossible to precisely enumerate the CCNE1 copy number by calculating a ratio CCNE1/cen19. In those cases, an estimate based on the size of the clusters was offered: smaller clusters were estimated to contain five to eight gene copies, and large clusters contained >10 or >20 copies according to their size (Supplementary Table S1).
FISH copy number values, thus estimated, together with NGS ones, are reported in Supplementary Table S2. A robust linear association was observed between NGS and FISH copy number values as assessed by Spearman’s correlation test (rho = 0.93, p = 7.261e−15) (Table 2).
Immunohistochemistry for CCNE1 unravels CCNE1 expression in the absence of amplification and irrespective of NGS copy number
Forty-three out of the 73 (58.9%) cases analyzed by IHC (Table 3) were classified as positive based on the threshold described above. A statistically significant correlation was found between CCNE1 amplification and positivity by IHC (p = 7.999e−5, Figure 5A). In particular, most CCNE1 amplified cases were positive by IHC (19/21, 90.5%). In contrast, high levels of CCNE1 immunoreactivity were found in 23/51 of non-amplified cases (45%, Figure 5B). These results were confirmed by Spearman’s rank correlation analysis conducted between NGS copy number and H-score values, showing a moderate but statistically significant positive association (rho = 0.50, p = 7.887e−05). Then, the behavior of CCNE1 expression assessed by IHC in patients showing low-level CCNE1 gains (three to five copies) was tested, and 8/12 cases (67%) were found, actually resembling the percentage observed in patients showing normal CCNE1 copy number (17/27, 63%). No significant differences in terms of BRCA1/2 mutations, GIM score, or other markers present were observed between CCNE1-expressing and non-expressing groups.
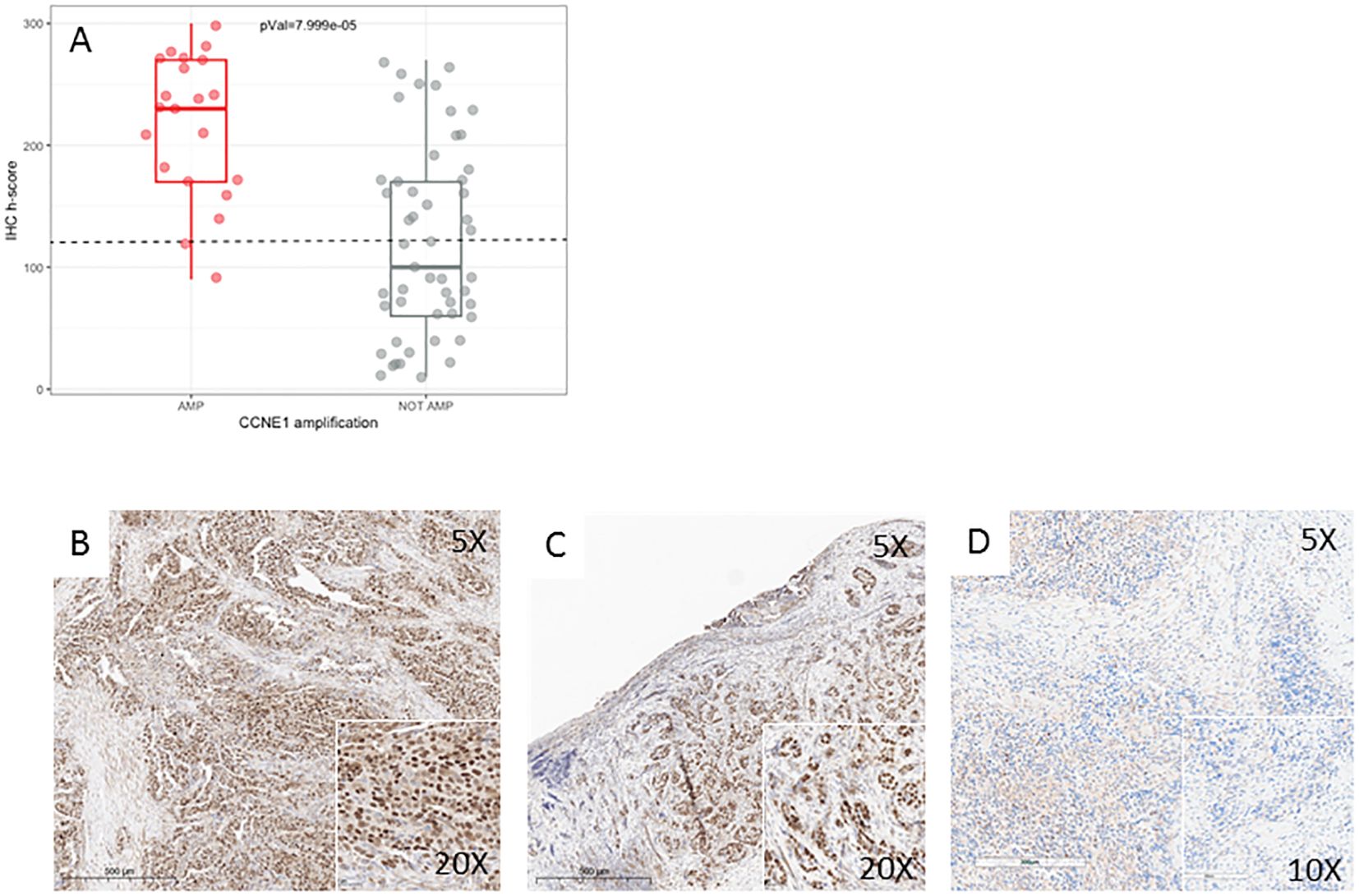
Figure 5. CCNE1 immunohistochemistry. (A) Boxplot showing the positive correlation between CCNE1 amplification results, detected by both NGS and FISH, and protein expression, detected by IHC. (B–D) Representative IHC staining of CCNE1 in three HGSC cases. (B) HGSC with CCNE1 amplification and positive IHC. (C) HGSC with no CCNE1 amplification and positive IHC. (D) HGSC with no CCNE1 amplification and a negative IHC. Original magnification: ×5 main image and ×20–×10 boxes. HGSC, high-grade serous ovarian carcinoma; IHC, immunohistochemistry; NGS, next-generation sequencing; FISH, fluorescence in situ hybridization.
GIM effective proxy for outcome prediction
Follow-up data were available in 68 patients (66.67%). All but one of these patients were treated with first-line platinum-based CT, which was referred to as best supportive care for poor performance status and thus excluded from further analyses. Two patients were indeed excluded from the survival analysis for having stage I and II disease. After completing CT, maintenance therapy was administered in 47 patients (69.11%), with bevacizumab (9/68 cases, 13.23%), PARPi (27/68, 39.70%), or both (11/68, 16.18%). In 10 patients, maintenance therapy was not administered due to disease progression or death while receiving CT, none of them carrying a BRCA1/2 pathogenic mutation or positive GIM. Among the 19 patients with pathogenic/likely pathogenic BRCA1/2 mutations, maintenance therapy was administered in 15 (78.95%), with PARPi (13) or PARPi plus bevacizumab (2). Among the 49 BRCA1/2 wild-type patients, maintenance therapy was administered in 32 (65.30%), with PARPi (14), PARPi plus bevacizumab (9), and bevacizumab (9). Median follow-up was 27.60 months. NGS testing was performed at disease onset in 66/68 cases (97.1%), whereas the remaining two cases (2.9%) were profiled at relapse following platinum-based CT.
HGSC patients carrying BRCA1/2 mutation and treated with platinum-based CT showed a better RFS (p = 0.038, Figure 6A). Interestingly, patients with a positive GIM score had a similar outcome (p = 0.003, Figure 6B). Likewise, BRCA1/2 mutations (OR = 0.30, CI = 0.098–0.913) and GIM score (OR = 0.13, CI = 0.040–0.408) were significantly associated with a lower risk of disease recurrence. Patients with GIM-positive high-grade serous ovarian carcinoma (HGSOC) had a similar outcome independent of BRCA1/2 mutation status, with median RFS of 18.73 and 58.12 months for positive and negative GIM, respectively. GIM negative/BRCA1–2 wild-type patients had a worse PFS compared to both BRCA1/2-mutated and GIM-positive patients (p = 0.0094, OR for recurrence = 0.19, CI = 0.062–0.557, Figure 6C). Moreover, in the BRCA1/2 wild-type cohort, no difference in RFS was observed according to maintenance regimen (PARPi, bevacizumab, or both; Supplementary Figure S5).
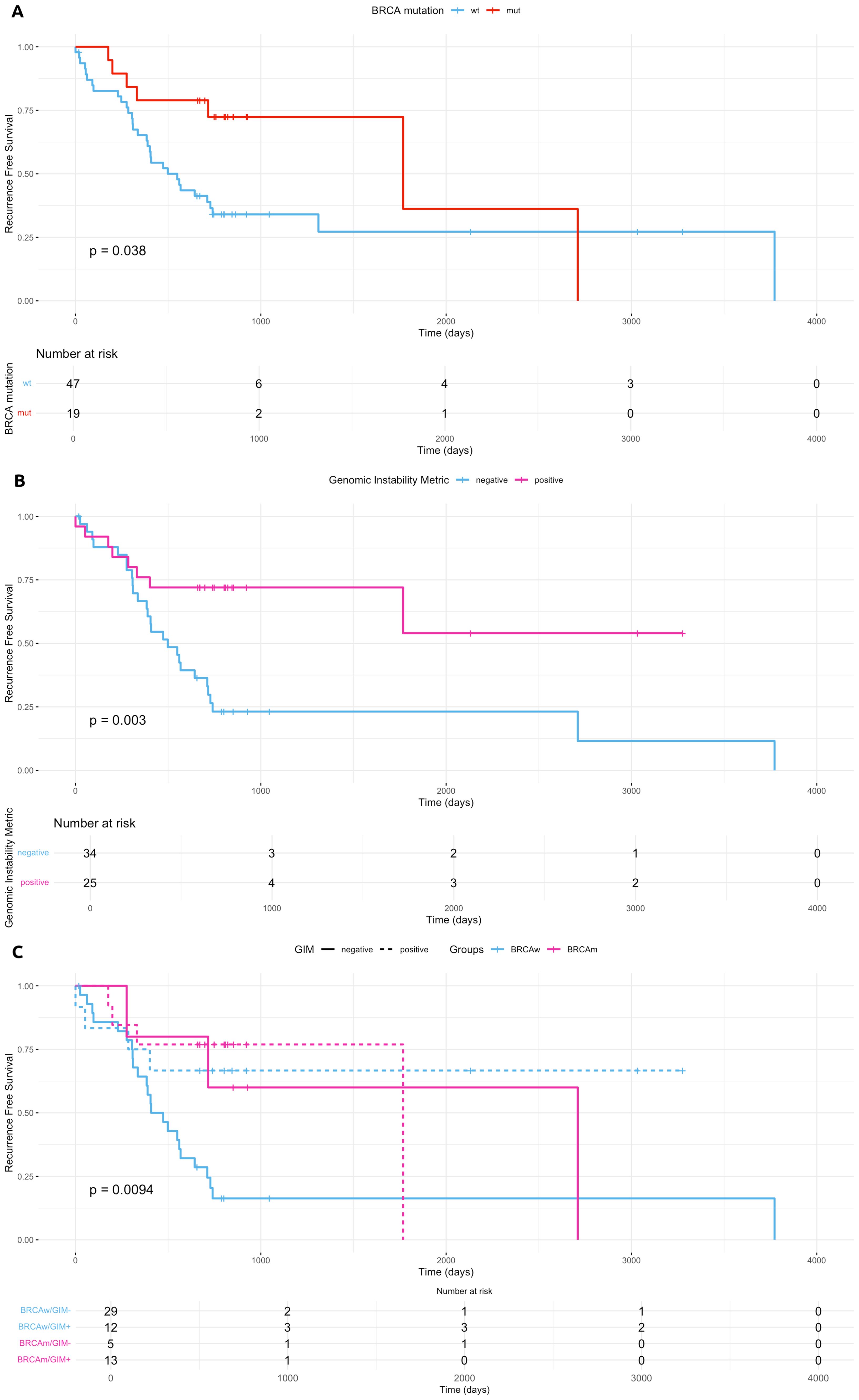
Figure 6. Clinical outcomes. (A–C) Kaplan–Meier estimates of recurrence-free survival according to BRCA1/2 mutational status (A), homologous recombination status calculated with GIM score (B), and both (C). Panel (C) confirms that patients with GIM-positive scores had a similar outcome independent of BRCA1/2 mutation presence. wt, wild type; mut, mutated; BRCAm, BRCA1/2 mutated; BRCAwt, BRCA1/2 wild type; GIM, Genomic Instability Metric.
CCNE1 status was not associated with platinum-based CT RFS (p = 0.9 for amplification by NGS and FISH, Supplementary Figure S4; p = 0.17 for overexpression by IHC, Supplementary Figure S4). Similarly, no association was found between RFS and CCNE1 amplification or overexpression.
Discussion
We report an extensive genomic analysis of a real-world cohort of HGSC patients carried out with the Thermo Fisher Oncomine Comprehensive Plus panel (OCA Plus). Among the different analyses, OCA Plus provides a calculation of the level of HRD (the GIM score), particularly important since it has recently become a target for PARPi therapy. Previous studies have performed a technical validation of the GIM score (15): Shejbel et al. found a concordance of 89% (60% in samples with an estimated tumor fraction < 30%) between OCA Plus and Myriad tests in a cohort of 80 HGSC patients. In our cohort, the OCA Plus GIM score was positive in 40% of cases, with half of them (20% of the overall cohort) carrying BRCA1/2 pathogenic mutations as expected (p = 0.009). We found that GIM-positive patients bore alterations in several HRR genes, with BRCA1/2, BRIP1, ATM, POLE, POLD1, CDK12, PPP2R2, NBN, RAD54L, RAD51C, and RAD51B being the most frequent. Notably, GIM-positive cases also had a high LOH, further sustaining the link between genomic instability and high LOH levels. LOH percentage measurement is closely aligned with the LOH score calculated using FoundationOne Assay, which was used for assessing HRD status and PARPi treatment in the ARIEL2 phase 2 clinical trial (36).
In our cohort, eight patients (29.63% of BRCA1/2-mutated) carrying pathogenic variants in BRCA1/2 had a negative GIM value. Although these cases represent a minority, they are particularly noteworthy, as HRD is primarily associated with BRCA1/2 mutations (6), making their negative GIM scores an unexpected and biologically relevant observation. While HRD can frequently occur in the absence of BRCA1/2 mutations, the opposite—BRCA1/2 mutations without detectable HRD—is considered much rarer, further highlighting the peculiarity of these cases. As proposed by Shejbel et al. (15), this finding could have potential technical explanations, mainly related to tumor fraction estimates or values very close to the positivity threshold. However, alternative biological mechanisms may also be involved, including epigenetic mechanisms (reversion of methylated promoters or overexpression of miRNA) or the activation of alternative pathways (37). As mentioned, data on the technical validation of the GIM score have already been extensively published in the literature, but its clinical validity is less well documented. Consistently, our real-world clinical data showed comparable RFS trends in HRD patients to those obtained with the reference test Myriad, further supporting its utility in informing therapeutic decisions for HGSC patients. Similarly, with the limitation due to the short median follow-up of our series (28 months) compared to the PAOLA1 trial (60 months), we showed that BRCA1/2 wt-HR-proficient patients, as determined by OCA Plus or Myriad assays, had similar RFS. The interchangeability of different tests for HRD suggests that there is an urgent need to harmonize these assays in pathology laboratories.
We found CCNE1 amplification in 29% of our cases, negatively correlated with BRCA1/2 mutations. When present, CCNE1 amplification is an early genomic event in HGSC that is maintained throughout the clinical course of the disease (38), and the high prevalence of this alteration in our cohort, particularly in tumors lacking BRCA1/2 mutations, underscores its potential role as an independent oncogenic driver. HGSCs harboring CCNE1 amplification are typically associated with chemoresistance and poor prognosis (39); however, this alteration is increasingly recognized as a promising predictive biomarker for emerging molecularly targeted therapies (22–24).
While we found a high concordance between NGS- and FISH-detected amplification, in testing CCNE1 expression by IHC, we observed, surprisingly, high levels of immunoreactivity in nearly half of the cases in the absence of gene amplification. These data were confirmed by a significant but mild correlation between NGS copy numbers and IHC H-score values, which could be caused, in our opinion, by the large number of non-amplified CCNE1-expressing cases. This behavior has been previously reported in literature (40, 41) and has been proposed to be caused by mutations or methylation in ubiquitin–proteasome pathway genes, which impair protein degradation, eventually resulting in CCNE1 accumulation. Our data confirmed that no molecular differences seemed to exist between non-amplified CCNE1-expressing and non-expressing patients. We considered the possibility that the protein enrichment observed in non-amplified samples could be related to low-level CCNE1 gains. However, this hypothesis was not confirmed by our data, leading us to believe that an alternative mechanism at the transcriptional or epigenetic level may actually account for this phenomenon. These findings are, in our opinion, one of the most promising results of this study because they underline the importance of implementing IHC, possibly integrated with RNA sequencing, in the clinical assessment of CCNE1 alterations for molecularly driven therapies. Notably, the phase I clinical trial NCT05238922, recruiting patients who are positive for CCNE1 by IHC, is currently active in several countries (42). Preliminary results from trials enrolling patients based on either amplification or immunohistochemistry data suggest that response appears to correlate more strongly with protein expression than with gene amplification. These findings indicate that relying solely on CCNE1 amplification may underestimate the population of patients potentially sensitive to the drug (43). In our view, this could be partly explained by the particular behavior of the protein discussed above. However, as CCNE1 is a relatively new biomarker, the issue remains unresolved. Currently, neither the antibody nor the IHC cut-off values are standardized and are still under evaluation, and the degree to which amplification serves as a reliable surrogate for protein expression is still unclear.
Targetable mutations rarely appeared with BRCA1/2 alterations, HRD, or CCNE1 amplification. Therefore, it was not possible to formulate hypotheses or perform meaningful statistical analyses regarding co-occurring alterations. On the contrary, we observed that approximately 8/50 of CCNE1-negative HR-proficient patients (7.84 overall) carried pathogenic alterations in the PTEN, PIK3CA, BRAF, KRAS, or CDK12 genes, being potentially eligible for off-label treatments.
Our data suggest that using CGP in OC patients is effective in capturing BRCA1/2 status and complex metrics like HRD, as well as in identifying biomarkers exploitable in clinical trials for BRCA wild-type and HR-proficient patients. We therefore believe that performing a comprehensive NGS test that includes all actionable biomarkers at an early stage could indeed represent an advantageous up-front strategy, offering improved clinical management, time saving, and tissue preservation for patients, as well as cost-effectiveness for healthcare systems. Neverthless, the primary aim remains to achieve a more refined and accurate stratification of HGSC patients, enabling better clinical decision-making, and in this context, molecular tumor boards (MTBs) represent the ideal tool for governing modern precision oncology (29, 44). Indeed, the compliance with MTB recommendations has been associated with a better outcome for women with gynecological cancers and breast cancer (45, 46).
In conclusion, we demonstrated the utility of CGP for patients with HGSC in a real-world setting, highlighting its analytical validity and the potential to reliably identify new biomarkers for novel molecularly driven treatments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Comitato Etico Territoriale Lombardia 4 (INT 191/24, approved on 09/17/2024). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EC: Conceptualization, Data curation, Formal analysis, Investigation, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. DL: Conceptualization, Data curation, Investigation, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. EM: Data curation, Resources, Writing – original draft. LA: Formal analysis, Software, Supervision, Validation, Writing – review & editing. MD: Conceptualization, Data curation, Supervision, Writing – review & editing. MG: Methodology, Validation, Writing – review & editing. BB: Methodology, Validation, Writing – review & editing. MP: Data curation, Supervision, Writing – review & editing. MMa: Data curation, Supervision, Writing – review & editing. SD: Conceptualization, Data curation, Supervision, Writing – review & editing. AD: Data curation, Formal analysis, Software, Validation, Writing – review & editing. RC: Methodology, Validation, Writing – review & editing. AA: Methodology, Validation, Writing – review & editing. FB: Methodology, Validation, Writing – review & editing. GD: Methodology, Validation, Writing – review & editing. NC: Methodology, Validation, Writing – review & editing. AG: Methodology, Validation, Writing – review & editing. AB: Data curation, Formal analysis, Writing – review & editing. IC: Data curation, Formal analysis, Writing – review & editing. AP: Data curation, Project administration, Software, Writing – review & editing. ET: Supervision, Writing – review & editing. FP: Supervision, Writing – review & editing. MMi: Supervision, Writing – review & editing. BP: Data curation, Supervision, Validation, Writing – review & editing. AV: Supervision, Writing – review & editing. FR: Supervision, Writing – review & editing. FB: Supervision, Writing – review & editing. GP: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by Ministry of Health, Ricerca Corrente funds.
Conflict of interest
Authors LA and FP are consultant for Roche.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1633410/full#supplementary-material
Supplementary Figure 1 | barplot showing the distribution of CCNE1 staining H-score used for the discriminating threshold assessment.
Supplementary Figure 2 | Boxplot showing the positive correlation between a positive value of genomic instability metric (GIM) and LOH percentage.
Supplementary Figure 3 | Visualizing of the correlations between the principal molecular markers. Boxplots showing the comparisons of Ccne1 amplification status with molecular markers detected by NGS in OCA plus panel. Respectively: TMB (tumor mutational burden), total mutations number detected per sample, GIM and LOH%.
Supplementary Figure 4 | Clinical outcomes. (A, B) Kaplan-Meier estimates of recurrence free survivals according to Ccne1 amplification (A) and expression (B) status.
Supplementary Figure 5 | Clinical outcomes. Kaplan-Meier estimates of recurrence free survivals in the three different maintenance treatment groups. Bev: Bevacizumab; Bev-PARPi: Bevacizumab plus PARP-inhibitors; PARPi: PARP-inhibitors.
Supplementary Table 1 | The copy numbers values estimed respectively for NGS and FISH. NGS values were calculated by Ion Reporter Software, FISH values have been approximated according to estimates calculated as described in Result section and in ref 35.
References
1. Nag S, Aggarwal S, Rauthan A, and Warrier N. Maintenance therapy for newly diagnosed epithelial ovarian cancer- a review. J Ovarian Res. (2022) 15:88. doi: 10.1186/s13048-022-01020-1
2. Jayson GC, Kohn EC, Kitchener HC, and Ledermann JA. Ovarian cancer. Lancet. (2014) 384:1376–88. doi: 10.1016/S0140-6736(13)62146-7
3. DiSilvestro P and Secord AA. Maintenance treatment of recurrent ovarian cancer: Is it ready for prime time? Cancer Treat Rev. (2018) 69:53–65. doi: 10.1016/j.ctrv.2018.06.001
4. Webb PM and Jordan SJ. Global epidemiology of epithelial ovarian cancer. Nat Rev Clin Oncol. (2024) 21:389–400. doi: 10.1038/s41571-024-00881-3
5. Wang Y, Duval AJ, Adli M, and Matei D. Biology-driven therapy advances in high-grade serous ovarian cancer. J Clin Invest. (2024) 134:e174013. doi: 10.1172/JCI174013
6. Bell D, Berchuck A, Birrer M, Chien J, Cramer D, Dao F, et al. Integrated genomic analyses of ovarian carcinoma TCGA Network. Nature. (2011) 474:609. doi: 10.1038/nature10166.
7. Konstantinopoulos PA and Matulonis UA. Clinical and translational advances in ovarian cancer therapy. Nat Cancer. (2023) 4:1239–57. doi: 10.1038/s43018-023-00617-9
8. Konstantinopoulos PA, Norquist B, Lacchetti C, Armstrong D, Grisham RN, Goodfellow PJ, et al. Germline and somatic tumor testing in epithelial ovarian cancer: ASCO guidelines. JCO. (2020) 38:1222–45. doi: 10.1200/JCO.19.02960
9. Azzollini J, Capone I, Duca M, Vingiani A, Piccolo A, Agnelli L, et al. Is tumour sequencing effective for the identification of germline BRCA1/2 pathogenic variant carriers? Tumori J. (2024). Online ahead of print. doi: 10.1177/03008916241280127
10. González-Martín A, Harter P, Leary A, Lorusso D, Miller RE, Pothuri B, et al. Newly diagnosed and relapsed epithelial ovarian cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. (2023) 34:833–48. doi: 10.1016/j.annonc.2023.07.011
11. Stover EH, Fuh K, Konstantinopoulos PA, Matulonis UA, and Liu JF. Clinical assays for assessment of homologous recombination DNA repair deficiency. Gynecol Oncol. (2020) 159:887–98. doi: 10.1016/j.ygyno.2020.09.029
12. Konstantinopoulos PA, Ceccaldi R, Shapiro GI, and D’Andrea AD. Homologous recombination deficiency: exploiting the fundamental vulnerability of ovarian cancer. Cancer Discov. (2015) 5:1137–54. doi: 10.1158/2159-8290.CD-15-0714
13. Quesada S, Penault-Llorca F, Matias-Guiu X, Banerjee S, Barberis M, Coleman RL, et al. Homologous recombination deficiency in ovarian cancer: Global expert consensus on testing and a comparison of companion diagnostics. Eur J Cancer. (2025) 215:115169. doi: 10.1016/j.ejca.2024.115169
14. Roma C, Abate RE, Sacco A, Califano D, Arenare L, and Bergantino F. Harmonization of homologous recombination deficiency testing in ovarian cancer: Results from the MITO16A/MaNGO-OV2 trial. Eur J Cancer. (2024) 206:114127. doi: 10.1016/j.ejca.2024.114127
15. Schejbel L, Poulsen TS, Vestergaard LK, et al. Evaluation of the oncomine comprehensive assay plus NGS panel and the oncoScan CNV assay for homologous recombination deficiency detection. Mol Diagn Ther. (2025) 29:117–27. doi: 10.1007/s40291-024-00745-7
16. Dumur CI, Krishnan R, Almenara JA, Brown KE, Dugan KR, Farni C, et al. Analytical validation and clinical utilization of the oncomine comprehensive assay plus panel for comprehensive genomic profiling in solid tumors. J Mol Pathol. (2023) 4:109–27. doi: 10.3390/jmp4020012
17. Pfarr N, von Schwarzenberg K, Zocholl D, Merkelbach-Bruse S, Siemanowski J, Mayr EM, et al. High concordance of different assays in the determination of homologous recombination deficiency-associated genomic instability in ovarian cancer. JCO Precis Oncol. (2024) 8:e2300348. doi: 10.1200/PO.23.00348
18. Santana dos Santos E, Lallemand F, Petitalot A, Caputo SM, and Rouleau E. HRness in breast and ovarian cancers. Int J Mol Sci. (2020) 21:3850. doi: 10.3390/ijms21113850
19. Bhamidipati D and Schram AM. Emerging tumor-agnostic molecular targets. Mol Cancer Ther. (2024) 23:1544–54. doi: 10.1158/1535-7163.MCT-23-0725
20. Bogani G, Chiappa V, Bini M, Ronzulli D, Indini A, Conca E, et al. BYL719 (alpelisib) for the treatment of PIK3CA-mutated, recurrent/advanced cervical cancer. Tumori J. (2022) 109:244–8. doi: 10.1177/03008916211073621
21. Mittempergher L. Genomic characterization of high-grade serous ovarian cancer: dissecting its molecular heterogeneity as a road towards effective therapeutic strategies. Curr Oncol Rep. (2016) 18:44. doi: 10.1007/s11912-016-0526-9
22. Fu S, Yao S, Yuan Y, Previs RA, Elias AD, Carvajal RD, et al. Multicenter phase II trial of the WEE1 inhibitor adavosertib in refractory solid tumors harboring CCNE1 amplification. JCO. (2023) 41:1725–34. doi: 10.1200/JCO.22.00830
23. House NC, Brown VE, Chen M, Yuan L, Moore SL, Guo J, et al. Profiling the activity of the potent and highly selective CDK2 inhibitor BLU-222 reveals determinants of response in CCNE1-aberrant ovarian and endometrial tumors. Cancer Res. (2025) 85(7):1297–309. doi: 10.1158/0008-5472.28721807
24. Wee S, Ye M, Lo Y, Hansbury M, Shin N, Weber M, et al. Discovery of INCB123667, a potent and selective cyclin-dependent kinase 2 (CDK2) inhibitor for the treatment of cyclin E dysregulated cancers. Eur J Cancer. (2022) 174:S79. doi: 10.1016/S0959-8049(22)01010-3
25. Wainberg ZA, Bent AH, Moreno V, Pedregal M, Mehta R, Chen EX, et al. 504MO Phase I study of the PKMYT1 inhibitor lunresertib (lunre) in combination with FOLFIRI in advanced gastrointestinal (GI) cancers (MINOTAUR study). Ann Oncol. (2024) 35:S201. doi: 10.1016/j.annonc.2024.05.419
26. Li M, Lulla AR, Wang Y, Tsavaschidis S, Wang F, Karakas C, et al. Low-molecular weight cyclin E confers a vulnerability to PKMYT1 inhibition in triple-negative breast cancer. Cancer Res. (2024) 84:3864–80. doi: 10.1158/0008-5472.CAN-23-4130
27. Ma J, Liu W, Li J, Kim D, Kim S, Levy A, et al. Azenosertib is a potent and selective WEE1 kinase inhibitor with broad antitumor activity across a range of solid tumors. Mol Cancer Ther. (2025). Online ahead of print. doi: 10.1158/1535-7163.MCT-24-1194
28. Zhong F, Zhu T, Pan X, Zhang Y, Yang H, Wang X, et al. Comprehensive genomic profiling of high-grade serous ovarian carcinoma from Chinese patients identifies co-occurring mutations in the Ras/Raf pathway with TP53. Cancer Med. (2019) 8:3928–35. doi: 10.1002/cam4.2243
29. Vingiani A, Agnelli L, Duca M, Lorenzini D, Damian S, Proto C, et al. Molecular tumor board as a clinical tool for converting molecular data into real-world patient care. JCO Precis Oncol. (2023) 7:e2300067. doi: 10.1200/PO.23.00067
30. Azzollini J, Vingiani A, Agnelli L, Tamborini E, Perrone F, Conca E, et al. Management of BRCA tumour testing in an integrated molecular tumour board multidisciplinary model. Front Oncol. (2022) 12:857515. doi: 10.3389/fonc.2022.857515
31. Pagel KA, Kim R, Moad K, Busby B, Zheng L, Tokheim C, et al. Integrated informatics analysis of cancer-related variants. JCO Clin Cancer Inform. (2020) 4:310–7. doi: 10.1200/CCI.19.00132
32. Robinson J, Thorvaldsdóttir H, Winckler W, Guttman M, Lander ES, Getz G, et al. Integrative genomics viewer. Nat Biotechnol. (2011) 29:24–6. doi: 10.1038/nbt.1754
33. Mateo J, Chakravarty D, Dienstmann R, Jezdic S, Gonzalez-Perez A, Lopez-Bigas N, et al. A framework to rank genomic alterations as targets for cancer precision medicine: the ESMO Scale for Clinical Actionability of molecular Targets (ESCAT). Ann Oncol. (2018) 29:1895–902. doi: 10.1093/annonc/mdy263
34. Bozzi F and Conca E. Silvestri, M. et al. Detecting gene copy number alterations by Oncomine Comprehensive genomic profiling in a comparative study on FFPE tumor samples. Sci Rep. (2025) 15:4314. doi: 10.1038/s41598-025-88494-3
35. Varella-Garcia M. Stratification of non-small cell lung cancer patients for therapy with epidermal growth factor receptor inhibitors: the EGFR fluorescence in situ hybridization assay. Diagn Pathol. (2006) 1:19. doi: 10.1186/1746-1596-1-19
36. Swisher EM, Kwan TT, Oza AM, et al. Molecular and clinical determinants of response and resistance to rucaparib for recurrent ovarian cancer treatment in ARIEL2 (Parts 1 and 2). Nat Commun. (2021) 12:2487. doi: 10.1038/s41467-021-22582-6
37. Mekonnen N, Yang H, and Shin YK. Homologous recombination deficiency in ovarian, breast, colorectal, pancreatic, non-small cell lung and prostate cancers, and the mechanisms of resistance to PARP inhibitors. Front Oncol. (2022) 12:880643. doi: 10.3389/fonc.2022.880643
38. Margolis B, Dao F, Licciardi M, Misirlioglu S, Olvera N, Ramaswami S, et al. CCNE1 amplification among metastatic sites in patients with gynecologic high-grade serous carcinoma. Gynecol Oncol Rep. (2021) 37:100850. doi: 10.1016/j.gore.2021.100850
39. Gorski JW, Ueland FR, and Kolesar JM. CCNE1 amplification as a predictive biomarker of chemotherapy resistance in epithelial ovarian cancer. Diagn (Basel). (2020) 10:279. doi: 10.3390/diagnostics10050279
40. Aziz D, Etemadmoghadam D, Caldon CE, Au-Yeung G, Deng N, Hutchinson R, et al. 19q12 amplified and non-amplified subsets of high grade serous ovarian cancer with overexpression of cyclin E1 differ in their molecular drivers and clinical outcomes. Gynecol Oncol. (2018) 151:327–36. doi: 10.1016/j.ygyno.2018.08.039
41. Willis SE, Jones NG, Shaan G, Jones EV, Raymond A, Nuttal B, et al. Large scale multi-omics concordance study of cyclin E1 identifies high expressing tumors lacking CCNE1 gene alterations across multiple tumor indications. Cancer Res. (2024) 84:1649–9. doi: 10.1158/1538-7445.AM2024-1649
42. Simonelli M, Lorusso D, Homicsko K, Seguy F, Kinder M, Liu Q, et al. 617MO Safety and tolerability of INCB123667, a selective CDK2 inhibitor, in patients (pts) with advanced solid tumors: A phase I study. Ann Oncol. (2024) 35:S495. doi: 10.1016/j.annonc.2024.08.684
43. Damian S, Lorusso D, Simonelli M, Homicsko K, Colombo I, Cassier PA, et al. Safety and preliminary efficacy from a phase 1 study of INCB123667, a selective CDK2 inhibitor, in patients with advanced platinum-resistant and refractory ovarian cancer (OC). JCO. (2025) 43:5514–4. doi: 10.1200/JCO.2025.43.16_suppl.5514
44. Sessa C, Travado L, Calaminus G, Cunha TM, Delgado Bolton RC, van Driel W, et al. European Cancer Organisation Essential Requirements for Quality Cancer Care for ovarian cancer: Focus on the multidisciplinary team. Tumori J. (2024) 111:11–9. doi: 10.1177/03008916241303022
45. Kato S, Kim KH, Lim HJ, Boichard A, Nikanjam M, Weihe E, et al. Real-world data from a molecular tumor board demonstrates improved outcomes with a precision N-of-One strategy. Nat Commun. (2020) 11:4965. doi: 10.1038/s41467-020-18613-3
Keywords: high-grade serous ovarian cancer (HGSC), comprehensive genomic profiling (CGP), homologous recombination deficiency (HRD) score, CCNE1 amplification, precision oncology cancer
Citation: Conca E, Lorenzini D, Minna E, Agnelli L, Duca M, Gentili M, Bodini B, Polignano M, Mantiero M, Damian S, Devecchi A, Dagrada G, Carminati R, Ardore A, Barbetta F, Da Chuna NB, Guerrizio A, Busico A, Capone I, Piccolo A, Tamborini E, Perrone F, Milione M, Paolini B, Vingiani A, Raspagliesi F, De Braud F and Pruneri G (2025) Genomic instability and CCNE1 amplification as emerging biomarkers for stratifying high-grade serous ovarian cancer. Front. Oncol. 15:1633410. doi: 10.3389/fonc.2025.1633410
Received: 22 May 2025; Accepted: 30 June 2025;
Published: 06 August 2025.
Edited by:
Wenbo Ma, Southern Medical University, ChinaReviewed by:
Raffaella Ergasti, Agostino Gemelli University Polyclinic (IRCCS), ItalyRaphael Leman, Centre François Baclesse, France
Copyright © 2025 Conca, Lorenzini, Minna, Agnelli, Duca, Gentili, Bodini, Polignano, Mantiero, Damian, Devecchi, Dagrada, Carminati, Ardore, Barbetta, Da Chuna, Guerrizio, Busico, Capone, Piccolo, Tamborini, Perrone, Milione, Paolini, Vingiani, Raspagliesi, De Braud and Pruneri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giancarlo Pruneri, Z2lhbmNhcmxvLnBydW5lcmlAaXN0aXR1dG90dW1vcmkubWkuaXQ=
†These authors have contributed equally to this work and share first authorship
 Elena Conca1†
Elena Conca1† Emanuela Minna
Emanuela Minna Luca Agnelli
Luca Agnelli Matteo Duca
Matteo Duca Marco Gentili
Marco Gentili Gianpaolo Dagrada
Gianpaolo Dagrada Adele Busico
Adele Busico Elena Tamborini
Elena Tamborini Federica Perrone
Federica Perrone Massimo Milione
Massimo Milione Filippo De Braud
Filippo De Braud Giancarlo Pruneri
Giancarlo Pruneri