- 1Department of Orthopedics, The Second Affiliated Hospital of Zhejiang University, Hangzhou, Zhejiang, China
- 2Orthopedics Research Institute of Zhejiang University, Hangzhou, Zhejiang, China
- 3Department of orthopedics, Yunhe County People’s Hospital, Lishui, Zhejiang, China
- 4School of Nursing and Midwifery, University of Technology Sydney, NSW, Australia
Background: This study aimed to evaluate surgical resection techniques for primary malignant tumors of the distal radius and to examine the reconstruction strategies employed for resulting large bone defects.
Methods: A retrospective analysis was conducted on 11 cases involving the resection and reconstruction of primary malignant tumors in the distal radius. Complete medical records and follow-up data from December 2013 to December 2022 were reviewed. Oncological outcomes were assessed, with specific focus on the extent of tumor invasion, surgical resection techniques, and reconstruction strategies.
Results: The follow-up period ranged from 5 to 118 months, with a mean duration of 41.6 months. At the final follow-up, local recurrence was observed in three patients, six died due to disease progression, and five were alive. For tumors confined to the distal radius, resection of the distal radius follow by joint-preserving reconstruction using either autologous fibular grafts or 3D-printed prostheses. For tumors involving the distal radius, proximal carpal bones, and/or distal ulna, wrist arthrodesis are chose using either autologous fibular grafts or ipsilateral ulnar transposition with arthrodesis For tumors involving more than half of the distal radius, reconstruction strategies include ulnar-only fixation or wrist arthrodesis with ipsilateral ulnar transposition.
Conclusions: Primary malignant tumors of the distal radius are rare and associated with a poor prognosis. Selection of resection and reconstruction techniques is primarily influenced by the extent of tumor invasion, with joint-preserving strategies feasible in selected cases and arthrodesis required for more extensive bone involvement.
1 Introduction
Primary malignant tumors of the distal radius are rare, with giant cell tumors more frequently reported in the literature. Large segmental resection of the distal radius is the main treatment approach, and achieving a wide surgical margin is essential for malignant tumors. In certain cases, resection of the distal radius alone may be inadequate, necessitating removal of the proximal carpal bones and/or adjacent segments of the ulna, depending on the extent of tumor involvement. The choice of reconstruction techniques is influenced by variability in resection approaches. As primary malignant tumors in the distal radius are rare, only a limited number of case reports pertaining to osteosarcoma, chondrosarcoma, and angiosarcoma are available in the literature (1–4). The scarcity of cases has led to a lack of consensus on optimal resection and reconstruction strategies for extensive segmental defects. Available reconstruction options include joint-preserving techniques such as autologous fibular grafts, allograft distal radius bone transplantation, and the use of 3D-printed prostheses. When joint preservation is not feasible, wrist arthrodesis may be performed using autologous iliac bone grafts, autologous fibular grafts, 3D-printed prostheses, or ipsilateral ulnar transposition with arthrodesis (5).
Given the limited literature on primary malignant tumors in the distal radius, a comprehensive analysis of resection methods and reconstruction techniques remains lacking. In this study, 11 cases of primary malignant tumors in the distal radius were retrospectively analyzed using complete medical records and follow-up data from a hospital. Oncological outcomes were summarized, and the extent of tumor involvement, resection methods, and the choice of reconstruction strategies were analyzed.
2 Methods
2.1 General information
2.1.1 Inclusion and exclusion criteria
2.1.1.1 Inclusion criteria
The following cases were included in the study: (1) primary malignant tumor of the distal radius; (2) No metastasis occurred during treatment; (3) Surgical treatment was performed; (4) availability of complete medical records and follow-up data.
2.1.1.2 Exclusion criteria
The following cases were excluded: (1) giant cell tumors; (2) metastatic tumors; (3) tumor invasion of vital blood vessels and nerves; and (4) lost to follow-up cases.
2.1.2 Study sample
A retrospective analysis was conducted on 11 patients with primary malignant tumors in the distal radius treated at a hospital between December 2013 and December 2022. This sample consisted of 6 males and 5 females, aged 7 to 74 years (mean age: 43.2 years). Diagnoses included osteosarcoma (n = 4 cases), undifferentiated sarcoma (n = 2), angiosarcoma (n = 1), chondrosarcoma (n = 1), leiomyosarcoma (n = 1), carcinosarcoma (n = 1), and malignant giant cell tumor (n = 1).
This study was approved by the hospital’s ethics committee, and informed consent was obtained from the families of all patients.
2.2 Treatment methods
All 11 patients underwent limb-salvage surgery. The choice of resection and reconstruction techniques was based on the extent of tumor involvement:
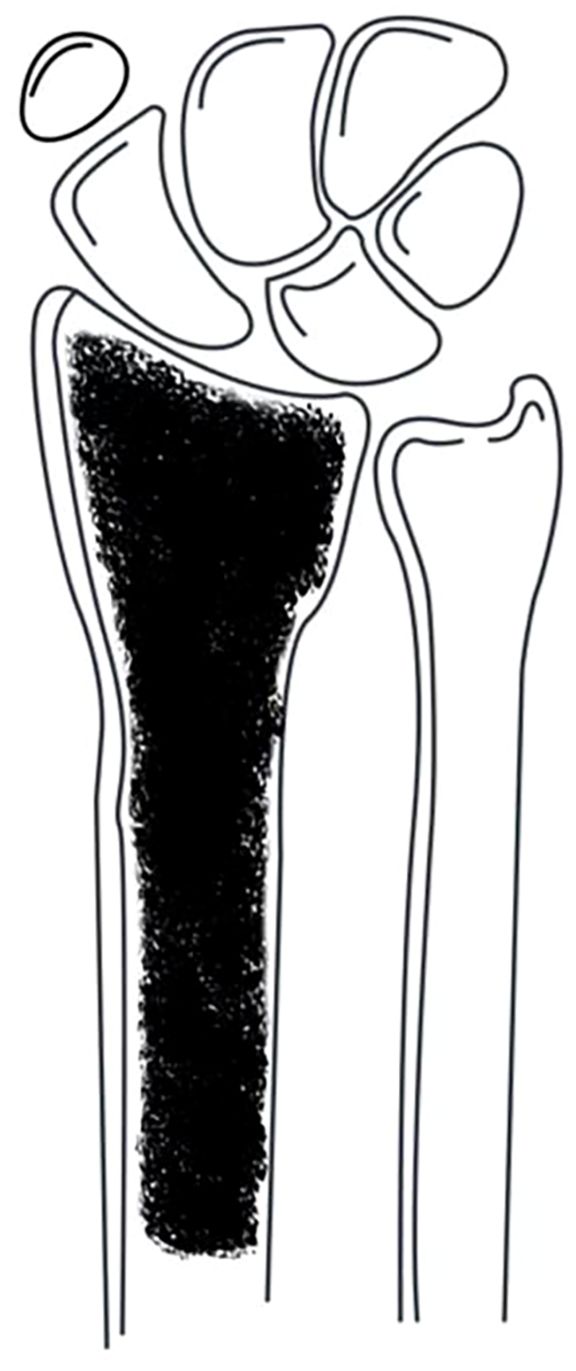
Tumors confined to the distal radius (Figure 1): Resection of the distal radius followed by joint-preserving reconstruction using either autologous fibular grafts or 3D-printed prostheses.
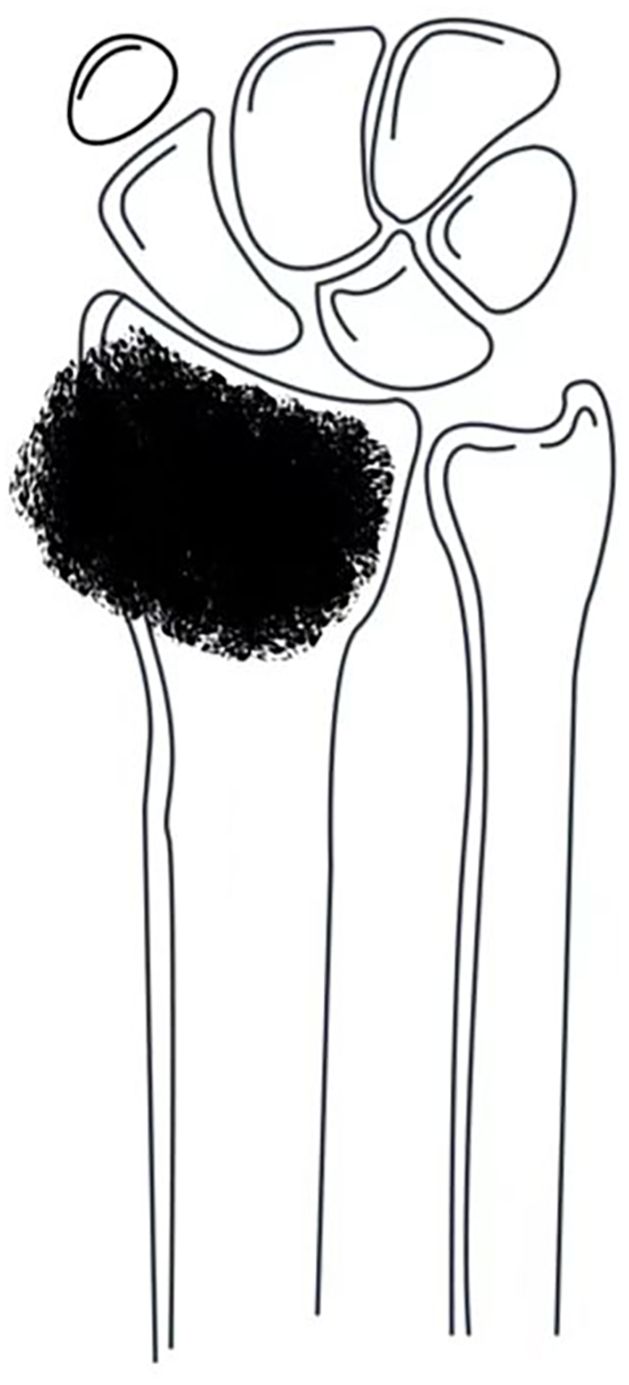
Figure 1. Tumor confined to the distal radius without involvement of the distal radioulnar joint or distal carpal bones.
Tumors involving the distal radius, proximal carpal bones, and/or distal ulna (Figure 2): Resection of the involved structures, followed by wrist arthrodesis using either autologous fibular grafts or ipsilateral ulnar transposition with arthrodesis.
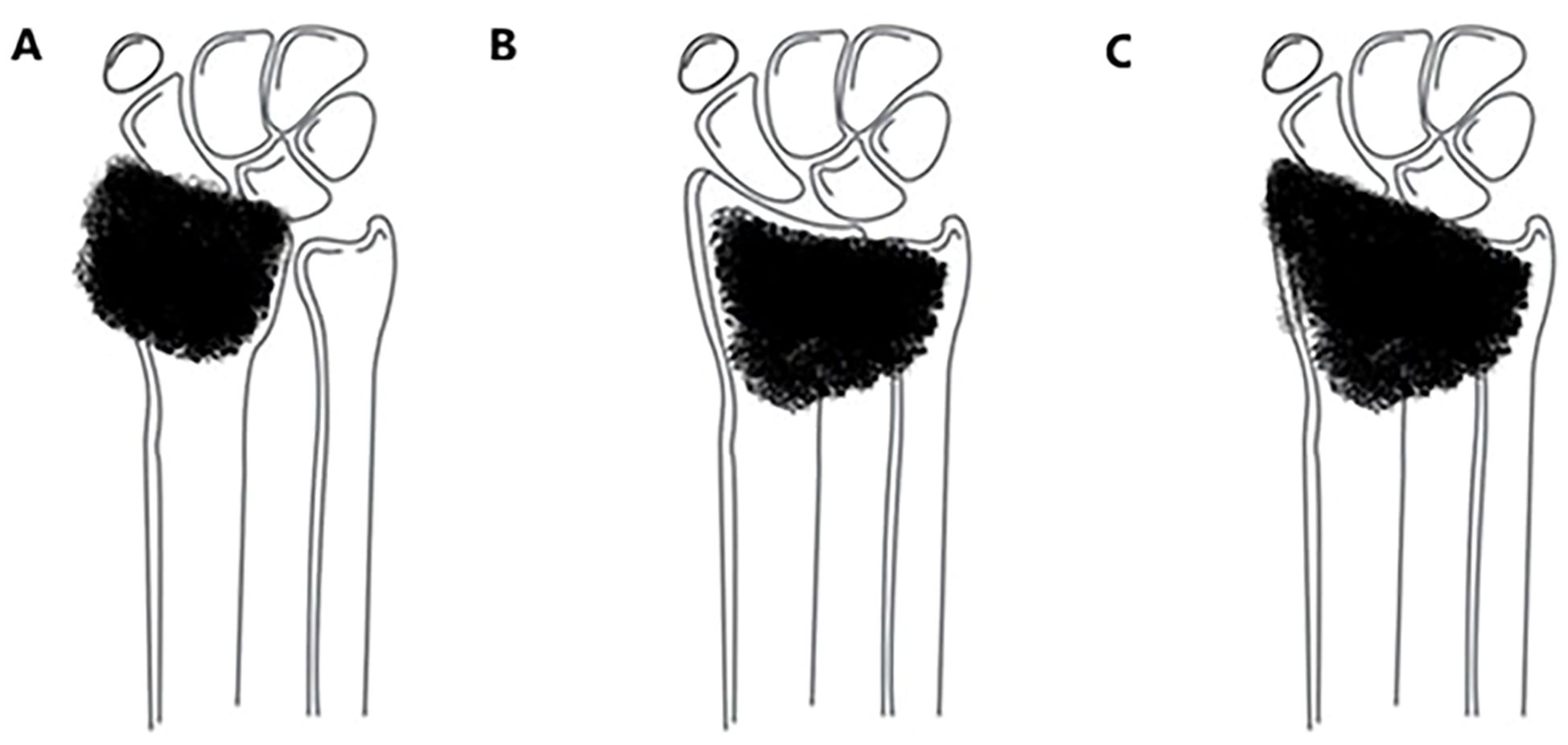
Figure 2. Tumor involving the distal radius with extension to the distal carpal bones and/or the distal radioulnar joint: (A) involving only the distal carpal bones; (B) involving only the distal radioulnar joint; (C) involving both the distal carpal bones and the distal radioulnar joint.
Tumors involving more than half of the distal radius (Figure 3): Reconstruction strategies included ulnar-only fixation and wrist arthrodesis.
Additionally, three patients received adjuvant chemotherapy, while four received neoadjuvant chemotherapy.
2.3 Observation indicators
Postoperative data were collected through telephone interviews and outpatient follow-ups. Survival time was defined as the duration from the date of diagnosis to the date of death or the last follow-up. Follow-up assessments included verification of patient demographics (sex, age), clinical information, and surgical details, as well as monitoring for complications, recurrence, metastasis, survival status, and functional outcomes using the Musculoskeletal Tumor Society (MSTS) scoring system (6).
3 Results
3.1 Oncological prognosis
The 11 patients were followed up for periods ranging from 5 to 118 months, with an average follow-up of 41.6 months. At the final follow-up, three patients had a recurrence, six had succumbed to the disease, and five remained alive (Figure 4).
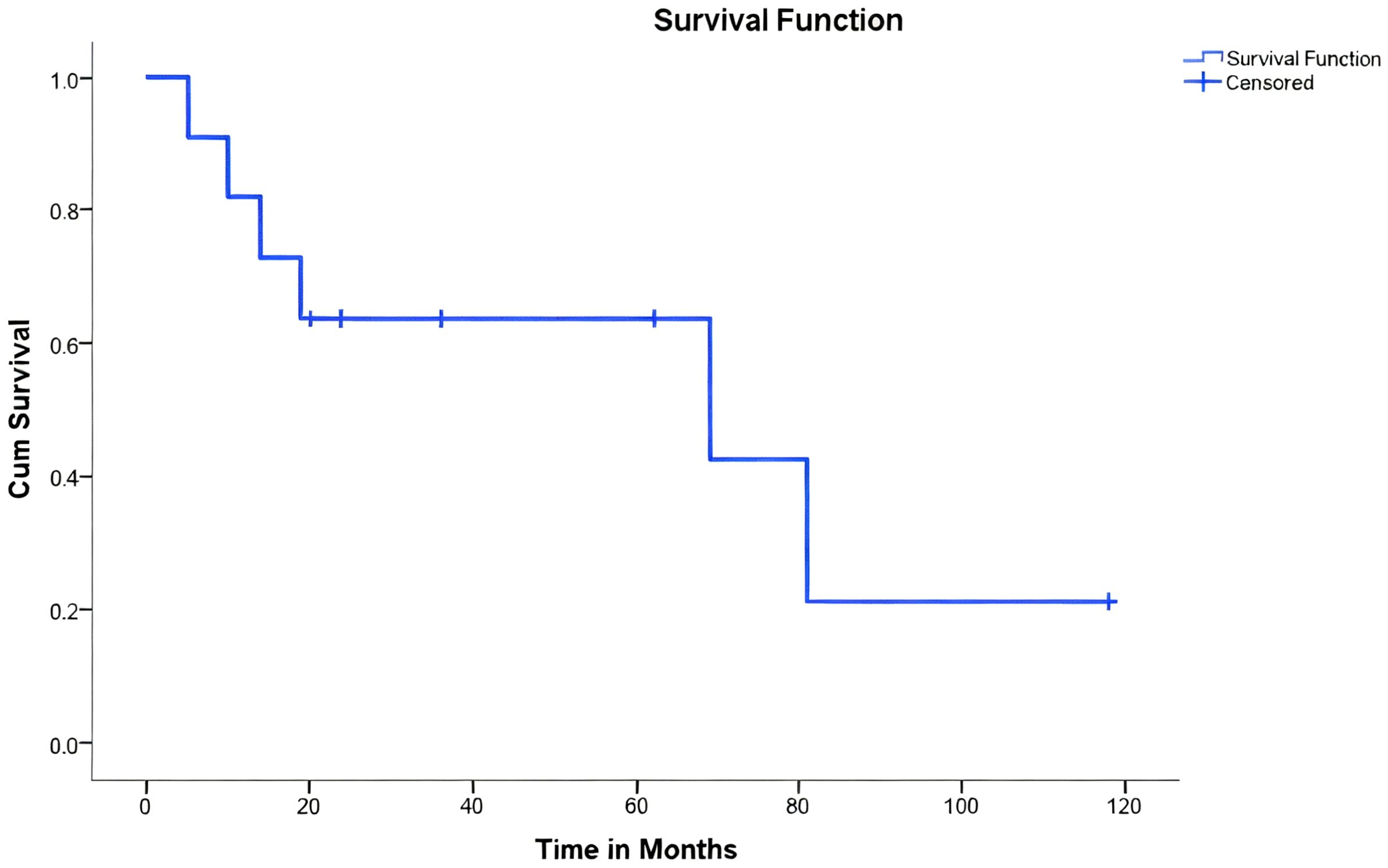
Figure 4. Kaplan-Meier survival analysis of 11 patients undergoing limb-salvage surgery for primary bone tumors of the radius. The Kaplan-Meier curve illustrates the overall survival probability of the patient cohort. The X-axis represents time in months post-surgery. The Y-axis represents the cumulative survival probability. A drop in the curve indicates a patient death event. Tick marks (+) on the curve represent censored data (patients who were alive at the last follow-up).
Among the three patients with recurrence, one developed a local soft tissue recurrence and underwent a second resection, while the other two required amputation. Among the six patients who succumbed to the disease, five died due to metastatic progression, while one patient with osteosarcoma passed away due to immunosuppression and subsequent varicella infection post-chemotherapy.
Of the five surviving patients, four had an average MSTS functional score of 26.5 (range: 24–28). One patient did not undergo MSTS assessment due to amputation.
3.2 Summary of resection and reconstruction methods for primary malignant tumors of the distal radius
The 11 cases of primary malignant tumors in the distal radius were treated as follows (Table 1):
3.2.1 Isolated distal radius resection
Six cases involved isolated resection of the distal radius. Of these, five underwent joint-preserving reconstruction—four with autologous fibular grafts and one with a 3D-printed prosthesis (Figure 5). In one case, where tumor involvement exceeded 50% of the radial length, reconstruction was performed using ulnar-only fixation and ulnar-wrist arthrodesis (Figure 6).
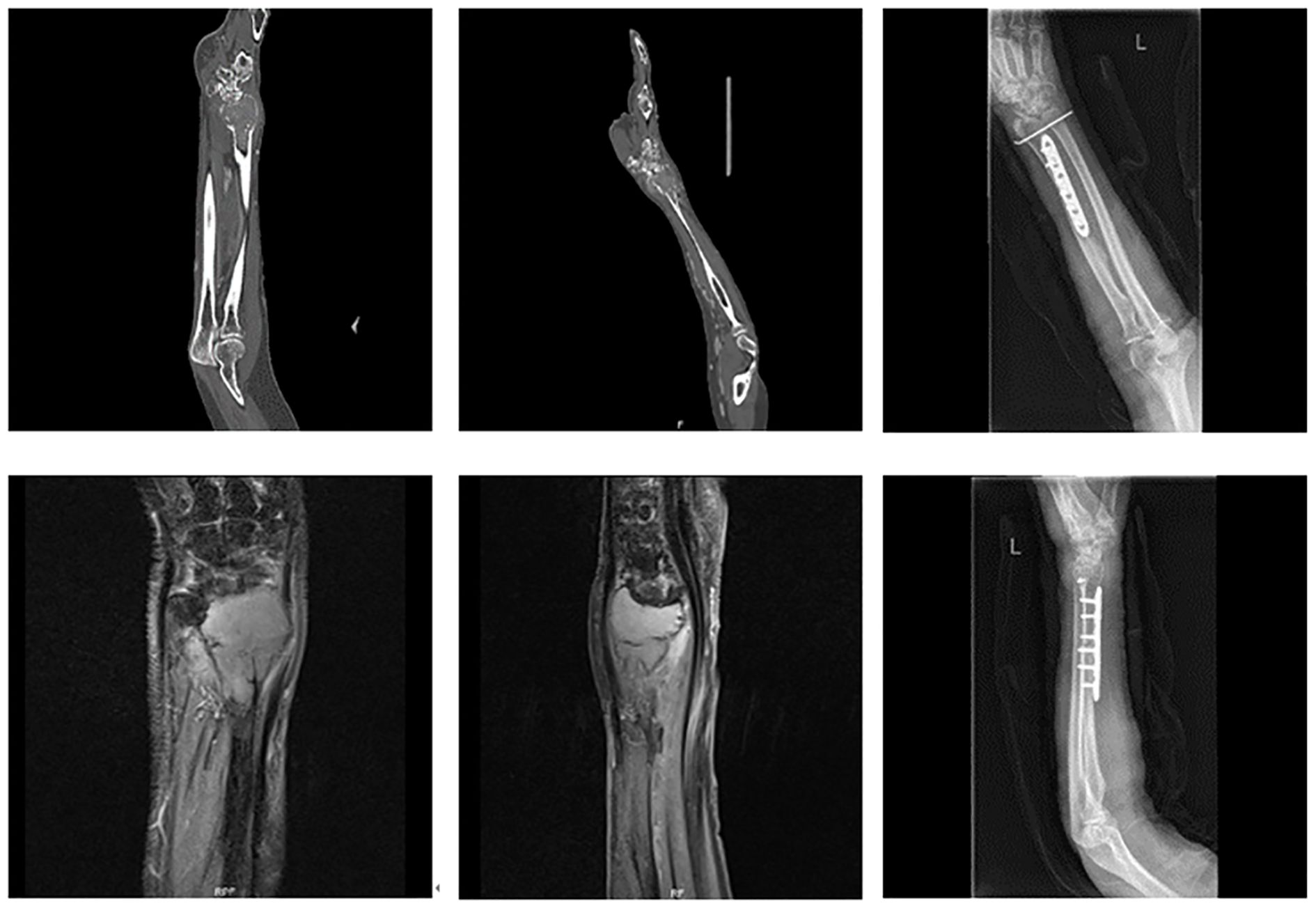
Figure 5. A 69-year-old female with undifferentiated sarcoma of the left distal radius. The patient underwent large segmental resection and reconstruction with an autologous fibular graft.
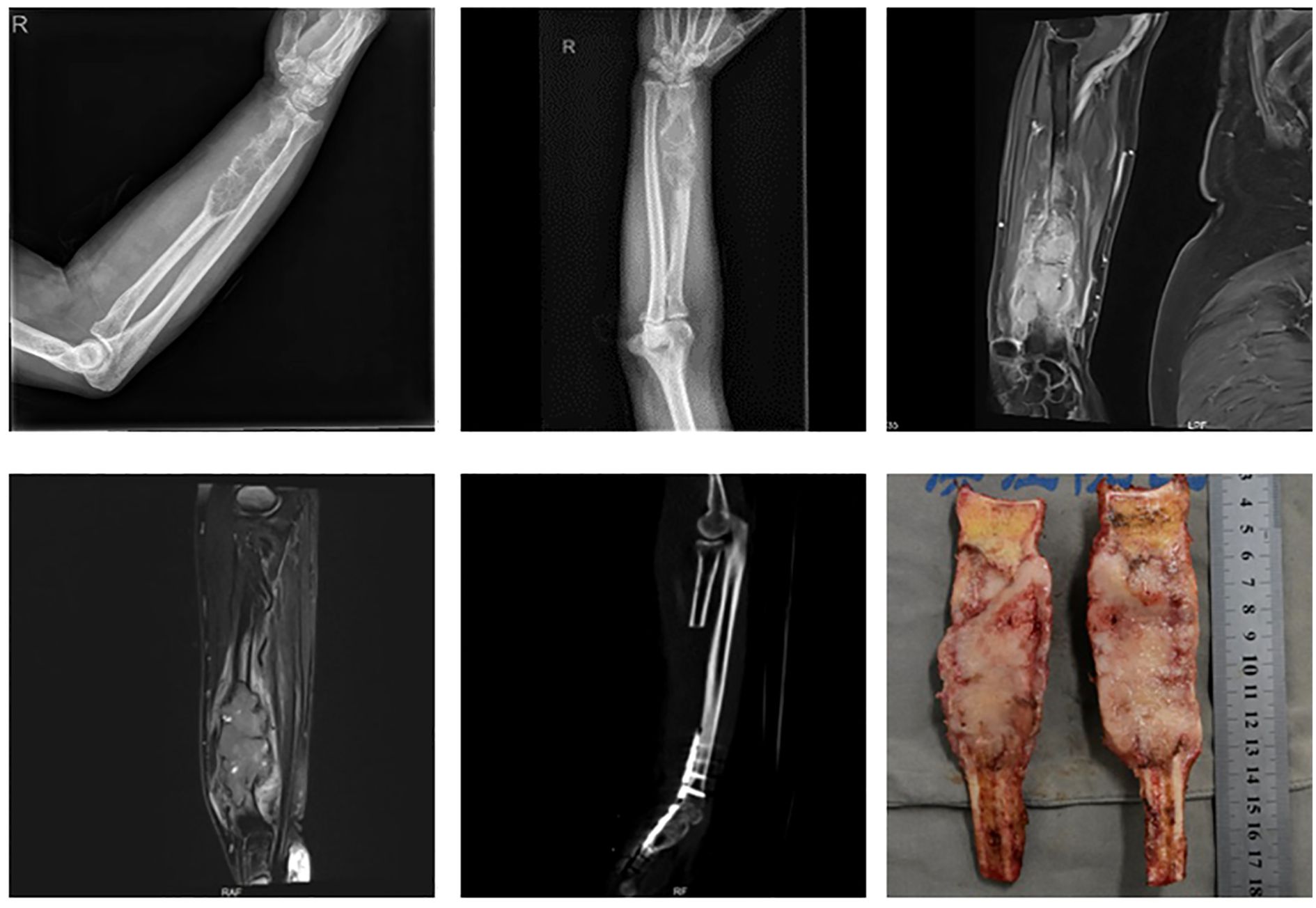
Figure 6. A 74-year-old male with carcinosarcoma of the distal right radius involving more than half of the bone. The patient underwent large segmental resection followed by ulnar-wrist arthrodesis.
3.2.2 Resection of the distal radius and additional structures
Five cases involved extended resections: one case of distal radius and distal ulna resection, one case of distal radius and proximal carpal bone resection, and three cases involving resection of the distal radius, distal ulna, and proximal carpal bones. All cases were reconstructed with wrist arthrodesis—three using autologous fibular grafts and two using ipsilateral ulnar transposition with arthrodesis (Figure 7).
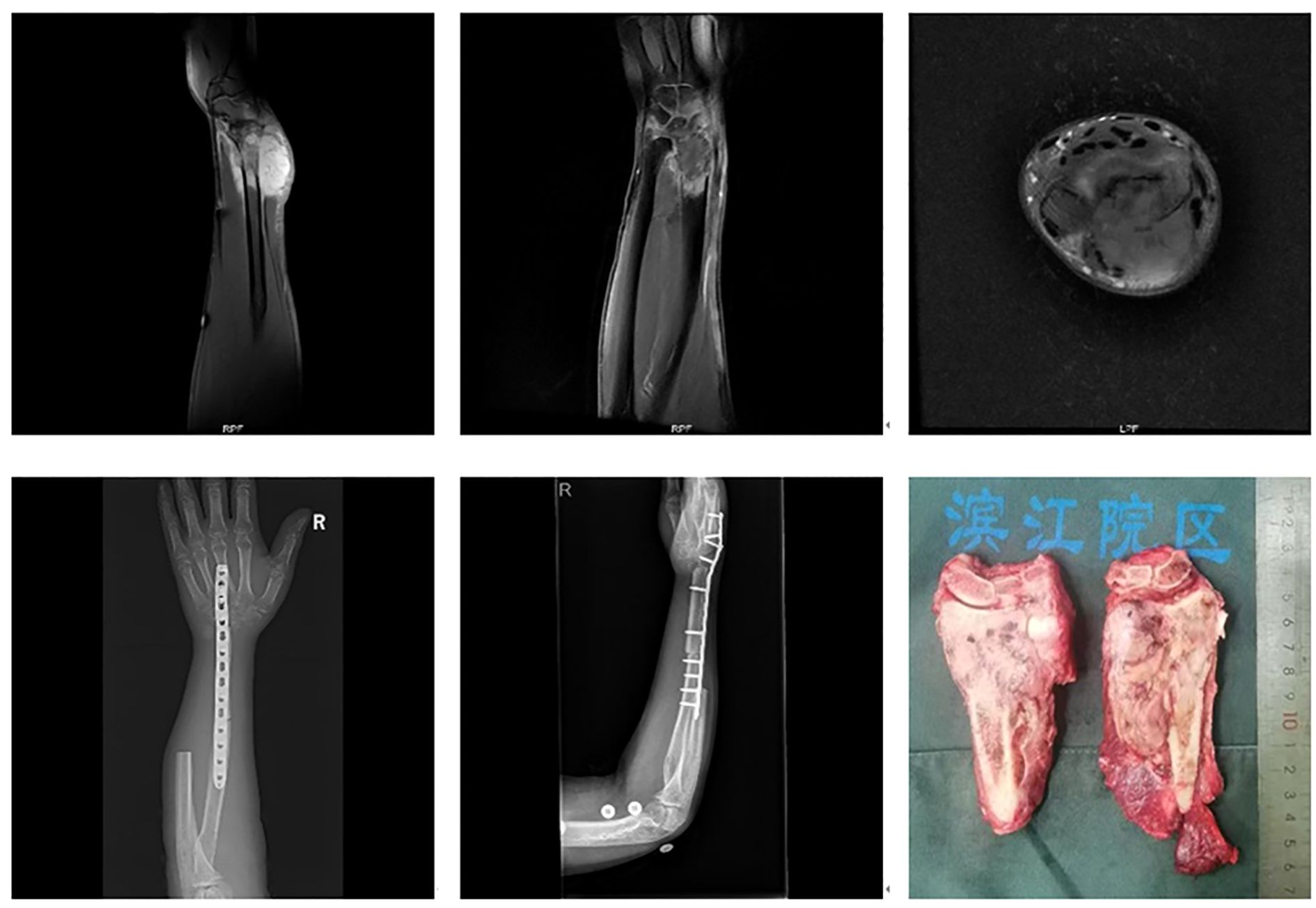
Figure 7. A 46-year-old male with leiomyosarcoma of the right distal radius, with tumor involvement extending to the distal radius, proximal carpal bones, and the distal ulnar-radial joint. The patient underwent resection of the distal radius, distal ulna, and proximal carpal bones, followed by ipsilateral ulnar transposition with arthrodesis.
4 Discussion
Primary malignant tumors of the distal radius are rare, with only case reports available and no large series studies to provide comprehensive data. This lack of extensive research has resulted in limited understanding among surgeons regarding treatment strategies and prognosis (7–9). In this study, the oncological outcomes of 11 cases of primary malignant tumors in the distal radius were summarized. It was seen that local resection and reconstruction yielded satisfactory functional outcomes, with an average MSTS score of 26.5. However, the overall survival prognosis was poor, with six patient deaths, more than half of which were due to metastatic disease. As a non-weight-bearing bone, the distal radius often presents with no early symptoms, resulting in delayed diagnoses that allow extensive tumor invasion and an increased risk of pulmonary metastasis.
Reconstruction methods for distal radius bone defects primarily include joint-preserving techniques and wrist arthrodesis. The aim of using joint-preserving approaches is to maintain wrist function, but this may lead to complications such as joint instability, deformity, and chronic pain. Common reconstruction options include autologous fibular grafts, allografts, and prosthetic implants. Allografts, while effective, require a suitable donor and are associated with various complications such as fractures, non-union, infection, and immune rejection. Complication rates ranging from 5.9% to 26.7% have been reported, with non-union rates as high as 42.9% (10–13), which has led to a decline in their use.
Autologous fibular grafts remain a common choice for reconstruction following distal radius resection, with favorable outcomes indicated in studies (14, 15). The anatomical shape of the fibular head closely resembles that of the distal radius, facilitating effective bone healing and biological reconstruction. However, the use of autologous fibular grafts for reconstructing large bone defects following the resection of primary malignant tumors in the distal radius needs careful evaluation of the patient’s prognosis. This is particularly relevant for individuals with high-grade tumors and a poor survival outlook, as the fibular head necessitates additional surgical morbidity.
The progressive development of prosthetic implants has contributed to their increasing use in distal radius reconstruction. Although prosthetic complications, such as subluxation and aseptic loosening, have been reported in approximately 60% of cases, severe complications remain relatively rare (16). Artificial prostheses, including 3D-printed implants, are increasingly being used in reconstructive surgery due to their potential to reduce prosthesis loosening (17). In this study, autologous fibular grafts were used in four out of five cases involving isolated distal radius resection, while a 3D-printed prosthesis was used in one case. Both techniques appear suitable for cases requiring simple distal radius resection. Given the poor prognosis associated with malignant tumors of the distal radius, prosthetic solutions—especially 3D-printed implants—may become increasingly important in future reconstruction strategies.
Wrist arthrodesis techniques for distal radius reconstruction include the use of autologous iliac bone grafts, autologous fibular head grafts, ipsilateral ulnar transposition, and prosthetic arthrodesis. Arthrodesis is generally preferred in cases of joint instability, particularly when resection involves the proximal carpal bones and/or the distal ulna (18, 19). While autologous fibular head grafting is effective, it necessitates fibular harvesting, thereby increasing surgical complexity. In contrast, ipsilateral ulnar transposition eliminates the need for fibular grafting and has been associated with favorable outcomes and reduced complication rates. This method, first described by Seradge in 1982, has since been widely adopted for distal radius reconstruction (20–22).
In this study, one patient underwent resection of the distal radius and proximal carpal bones, another required distal radius and distal ulna resection, and three underwent resection of the distal radius, distal ulna, and proximal carpal bones. Autologous fibular head arthrodesis was employed in earlier cases; however, ipsilateral ulnar transposition with arthrodesis was favored in more recent cases due to its lower complication rate. Prosthetic arthrodesis was used less frequently, given its associated risks, while autologous fibular head grafts remained a viable option for high-grade tumors but required careful patient selection.
Additionally, one patient with extensive distal radius involvement (> 50% of the bone length) underwent ulnar-only fixation with wrist arthrodesis. This approach, first reported by Sayre in 1893 for pediatric radial deformities (23), has since been applied in cases of failed distal radius reconstruction (24, 25). Given the extent of bone loss in this particular case, ulnar-only fixation with wrist arthrodesis was a viable reconstructive option.
4.1 Limitations
The limitations of this study include the following: 1) As a retrospective study, it is subject to potential biases that may affect the accuracy of the data; 2) the small sample size may limit the generalizability of the findings; and 3) the long study period introduces variability in treatment approaches and outcome assessments.
In future research, the focus should be on expanding the sample size, refining classification criteria, and establishing standardized guidelines to enhance clinical decision-making.
4.2 Conclusion
Primary malignant tumors of the distal radius are rare and often associated with poor prognoses. Treatment strategies, including resection and reconstruction, should be individualized based on the extent of tumor involvement to optimize functional and oncological outcomes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Human Research Ethics Committee of the Second Affiliated Hospital, Zhejiang University School of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
Q-HG: Writing – original draft, Writing – review & editing, Conceptualization, Data curation. WW: Writing – original draft, Investigation, Writing – review & editing, Formal Analysis. Z-MYa: Project administration, Writing – review & editing, Methodology, Writing – original draft. Y-JQ: Writing – review & editing, Resources, Writing – original draft. J-DW: Writing – original draft, Writing – review & editing, Software. K-YW: Writing – original draft, Supervision, Writing – review & editing. H-MT: Validation, Writing – review & editing, Writing – original draft. Z-MYe: Writing – original draft, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, and/or publication of this article.
Acknowledgments
Junyan Xie, Acquisition of data, analysis and interpretation of the data. Bing Liu, Acquisition of data, critical revision of the manuscript for intellectual content. Libin Jin, Acquisition of data, critical revision of the manuscript for intellectual content. Nong Lin, Acquisition of data, critical revision of the manuscript for intellectual content.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MSTS, Musculoskeletal Tumor Society scoring.
References
1. Mavrogenis AF, Galanopoulos J, Vottis C, Megaloikonomos PD, Palmerini E, and Kokkalis ZT. Osteoarticular allograft reconstruction for an Angiosarcoma of the distal radius. J Long Term Eff Med Implants. (2016) 26:79–87. doi: 10.1615/JLongTermEffMedImplants.2016013008
2. Higuchi T, Yamamoto N, Hayashi K, Takeuchi A, Abe K, Taniguchi Y, et al. Successful joint preservation of distal radius osteosarcoma by en bloc tumor excision and reconstruction using a tumor bearing frozen autograft: a case report. BMC Surg. (2018) 18:12. doi: 10.1186/s12893-018-0346-y
3. Ichihara S, Hidalgo-Diaz JJ, Facca S, and Liverneaux P. Unicompartmental isoelastic resurfacing prosthesis for Malignant tumor of the distal radius: a case report with a 3-year follow-up. Orthop Traumatol Surg Res. (2015) 101:969–71. doi: 10.1016/j.otsr.2015.09.020
4. van de Sande MA, van Geldorp NH, Dijkstra PD, and Taminiau AH. Surgical technique: tibia cortical strut autograft interposition arthrodesis after distal radius resection. Clin Orthop Relat Res. (2013) 471:803–13. doi: 10.1007/s11999-012-2555-5
5. Liu W, Wang B, Zhang S, Li Y, Hu B, and Shao Z. Wrist reconstruction after en bloc resection of bone tumors of the distal radius. Orthop Surg. (2021) 13:376–83. doi: 10.1111/os.12737
6. Enneking WF, Dunham W, Gebhardt MC, Malawar M, and Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. (1993) 286:241–6. doi: 10.1097/00003086-199301000-00035
7. Niu X, Xu H, Inwards CY, Li Y, Ding Y, Letson GD, et al. Primary Bone Tumors: Epidemiologic Comparison of 9200 Patients Treated at Beijing Ji Shui Tan Hospital, Beijing, China, With 10–165 Patients at Mayo Clinic, Rochester, Minnesota. Arch Pathol Lab Med. (2015) 139:1149–55. doi: 10.5858/arpa.2014-0432-OA
8. Picci P, Manfrini M, Fabbri N, Gambarotti M, and Vanel D. Atlas of Musculoskeletal Tumors and Tumor like Lesions, The Rizzoli Case Archive. Switzerland: Springer (2014).
9. Muramatsu K, Ihara K, Yoshida K, Tominaga Y, Hashimoto T, and Taguchi T. Musculoskeletal sarcomas in the forearm and hand: standard treatment and microsurgical reconstruction for limb salvage. Anticancer Res. (2013) 33:4175–82.
10. Szabo RM, Anderson KA, and Chen JL. Functional outcome of en bloc excision and osteoarticular allograft replacement with the Sauve-Kapandji procedure for Campanacci grade 3 giant-cell tumor of the distal radius. J Handb Surg Am. (2006) 31:1340–8. doi: 10.1016/j.jhsa.2006.06.004
11. Asavamongkolkul A, Waikakul S, Phimolsarnti R, and Kiatisevi P. Functional outcome following excision of a tumour and reconstruction of the distal radius. Int Orthop. (2009) 33:203–9. doi: 10.1007/s00264-007-0441-7
12. Duan H, Zhang B, Yang HS, Liu YH, Zhang WL, Min L, et al. Functional outcome of en bloc resection and osteoarticular allograft reconstruction with locking compression plate for giant cell tumor of the distal radius. J Orthop Sci. (2013) 18:599–604. doi: 10.1007/s00776-013-0394-1
13. Scoccianti G, Campanacci DA, Beltrami G, Caldora P, and Capanna R. The use of osteo-articular allografts for reconstruction after resection of the distal radius for tumour. J Bone Joint Surg. (2010) 92:1690–4. doi: 10.1302/0301-620X.92B12.25121
14. Humail SM, Ghulam MK, and Zaidi IH. Reconstruction of the distal radius with non-vascularised fibular graft after resection of Giant cell tumour of bone. J Orthop Surg. (2014) 22:356–9. doi: 10.1177/230949901402200318
15. Barik S, Jain A, Ahmad S, and Singh V. Functional outcome in giant cell tumor of distal radius treated with excision and fibular arthoplasty: a case series. Eur J Orthop Surg Traumatol. (2020) 30:1109–17. doi: 10.1007/s00590-020-02679-2
16. Wang B, Wu Q, Liu J, Chen S, Zhang Z, and Shao Z. What are the functional results, complications, and outcomes of using a custom unipolar wrist Hemiarthroplasty for treatment of grade III Giant cell tumors of the distal radius? Clin Orthop Relat Res. (2016) 474:2583–90. doi: 10.1007/s11999-016-4975-0
17. Gulati K, Prideaux M, Kogawa M, Lima-Marques L, Atkins GJ, Findlay DM, et al. Anodized 3D-printed titanium implants with dual micro- and nano-scale topography promote interaction with human osteoblasts and osteocyte-like cells. J Tissue Eng Regener Med. (2017) 11:3313–25. doi: 10.1002/term.2239
18. Qu H, Guo W, Li D, Yang Y, Wei R, and Xu J. Functional results of wrist arthrodesis versus arthroplasty with proximal fibula following giant cell tumour excision of the distal radius. J Handb Surg Eur Vol. (2019) 44:394–401. doi: 10.1177/1753193418809785
19. Nassr A, Khan MH, Ali MH, Espiritu MT, Hanks SE, Lee JY, et al. Donor-site complications of autogenous nonvascularized fibula strut graft harvest for anterior cervical corpectomy and fusion surgery: experience with 163 consecutive cases. Spine J. (2009) 9:893–8. doi: 10.1016/j.spinee.2009.04.020
20. Seradge H. Distal ulnar translocation in the treatment of giant-cell tumors of the distal end of the radius. J Bone Joint Surg Am. (1982) 64:67–73. doi: 10.2106/00004623-198264010-00011
21. Gundavda MK, Agarwal MG, Reddy R, Katariya A, and Bhadiyadra R. Does a modified technique to achieve arthrodesis of the wrist after resection of the distal radius and translocating the ipsilateral ulna as a vascularized graft to reconstruct the defect improve grip strength and outcomes scores? Clin Orthop Relat Res. (2021) 479:1285–93. doi: 10.1097/CORR.0000000000001604
22. Chalidis BE and Dimitriou CG. Modified ulnar translocation technique for the reconstruction of giant cell tumor of the distal radius. Orthopedics. (2008) 31:608. doi: 10.3928/01477447-20080601-05
24. Bhargava P, Ajmera A, Nagariya S, and Chatrath V. Centralisation of ulna for recurrence in reconstructed lower end radius giant cell tumor. J Orthop. (2008) 5:e3. doi: 10.1016/S0972-978X(08)00094-4
Keywords: bone defect, distal radius, malignancy, resection, reconstruction
Citation: Guo Q-H, Wang W, Yang Z-M, Qiu Y-J, Wu J-D, Wang K-Y, Tao H-M and Ye Z-M (2025) Reconstruction strategies for extensive bone defects following resection of primary malignant tumors in the distal radius. Front. Oncol. 15:1644295. doi: 10.3389/fonc.2025.1644295
Received: 10 June 2025; Accepted: 29 September 2025;
Published: 20 October 2025.
Edited by:
Joseph M. Escandón, Wyckoff Heights Medical Center, United StatesReviewed by:
Nianzhe Sun, Central South University, ChinaGuolong Bin, Guangxi Medical University Cancer Hospital, China
Copyright © 2025 Guo, Wang, Yang, Qiu, Wu, Wang, Tao and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng-Ming Yang, MjIwMDAxM0B6anUuZWR1LmNu
†These authors have contributed equally to this work
 Qing-He Guo1,2†
Qing-He Guo1,2† Zheng-Ming Yang
Zheng-Ming Yang