- Interventional Radiology, The People’s Hospital of Ganzhou, Ganzhou, Jiangxi, China
Background and Purpose: Hepatocellular carcinoma (HCC) remains a global health challenge, with hepatic artery infusion chemotherapy (HAIC) serving as a pivotal treatment for unresectable cases. Traditional transfemoral access (TFA) for HAIC is associated with significant limitations, including prolonged immobility, increased risk of deep vein thrombosis (DVT), and reduced quality of life. The distal transradial access (dTRA), emerging as a viable alternative in coronary and neurovascular interventions, offers potential advantages in HAIC. This study evaluates the feasibility, safety, and clinical outcomes of dTRA for HAIC in HCC patients, addressing the paucity of data in this specific application.
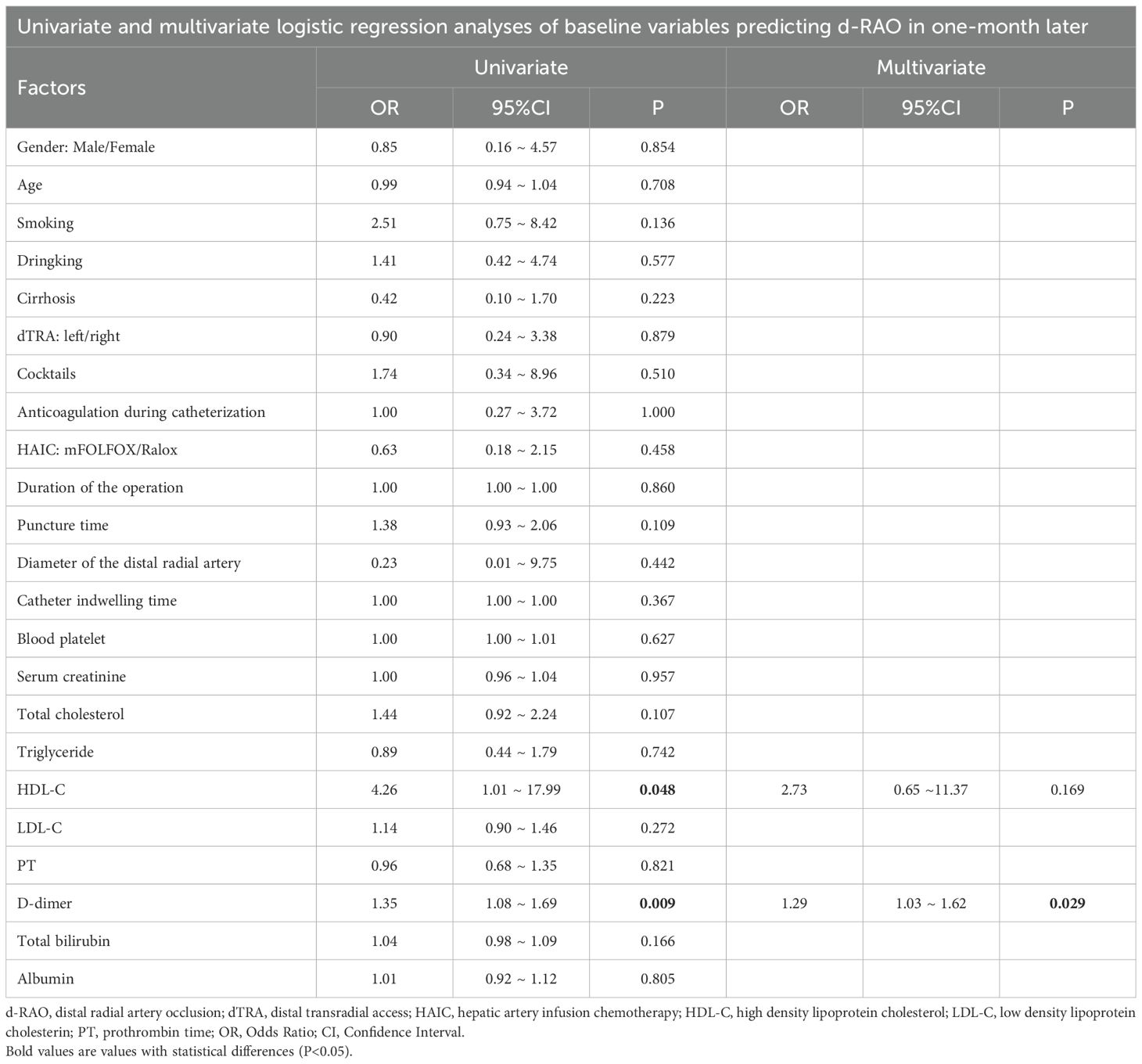
Methods: A retrospective analysis was conducted on patients who underwent dTRA-HAIC procedures for HCC between November 2023 and December 2024. The puncture time, procedural time, incidence of distal radial artery occlusion (d-RAO) and access site complications (ASC) were used to evaluate the treatment efficacy in the patients. Univariate and multivariate logistic regression analysis was performed to identify predictive factors associated with d-RAO development.
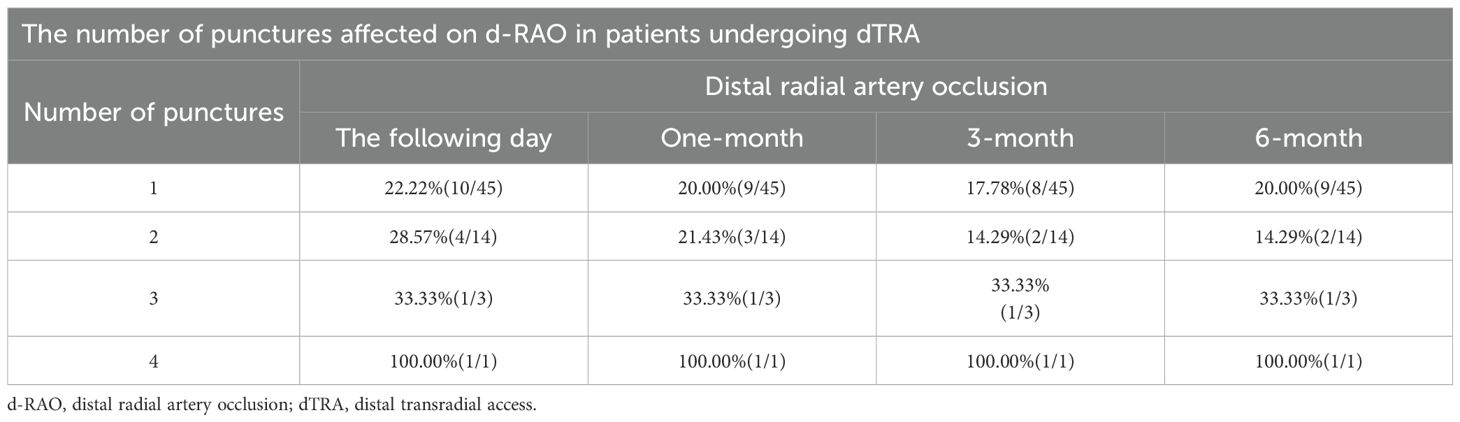
Results: The mean puncture time was 3.5 minutes (3–4.25 minutes), with a distal radial artery diameter of 1.96 ± 0.16 mm. The mean catheter indwelling time for mFOLFOX-HAIC and Ralox-HAIC were 2375 minutes (1715–3276 minutes) and 410 minutes (276, 544 minutes), respectively. Early d-RAO rates were 25.4% on postoperative day 1, declining to 20.6% at 6 months. Multivariate analysis identified preoperative D-dimer levels (p < 0.05) as significant risk factors for early d-RAO in one-month after operation. Multiple punctures may be associated with a high risk of d-RAO. No severe bleeding, hematoma, or pseudoaneurysm occurred.
Conclusion: dTRA for HAIC demonstrates high technical feasibility and acceptable safety, representing a promising alternative to TFA. Preoperative D-dimer screening and limitations on repeated punctures may optimize outcomes. Larger multicenter studies are warranted to validate these findings and refine patient selection criteria.
1 Introduction
Hepatocellular carcinoma (HCC) ranks as the sixth most common cancer globally and the third leading cause of cancer-related death, with over 90% of cases occurring in developing countries, including China (1). Especially China, with a high incidence of liver cancer, more than one-half of patients presented with stage III-IV disease (56.9%, n = 1702), precluding curative resection (2). Hepatic artery infusion chemotherapy (HAIC) has emerged as a critical treatment modality for unresectable HCC, delivering chemotherapeutic agents directly to tumor vasculature while minimizing systemic toxicity (3–6). The commonly used HAIC include mFOLFOX-HAIC (4, 7, 8), with continuous perfusion for 26–46 hours, and Ralox-HAIC, generally perfusion for 4–6 hours (9). Traditional HAIC is typically performed via the transfemoral approach (TFA), which mandates prolonged bed rest (6–12 hours), increases deep vein thrombosis (DVT) risk, and imposes significant discomfort due to groin compression (10).These limitations underscore the need for minimally invasive alternatives that preserve patient mobility and reduce vascular complications.
The transradial access (TRA) route, initially described for coronary interventions, has gained prominence for its lower bleeding risk and improved patient comfort compared to TFA (11). Distal transradial access (dTRA), targeting the radial artery at the anatomical snuffbox (distal to the superficial palmar arch), offers distinct advantages over traditional wrist-level TRA. Anatomically, the distal radial artery lies superficial to the scaphoid and trapezium bones, facilitating easier hemostasis and reducing compression time (12). Physiologically, preserving flow through the superficial palmar arch minimizes the risk of forearm radial artery occlusion (RAO), a critical concern for repeat interventions (13).
While dTRA has been validated in coronary angiography and transarterial chemoembolization (TACE) (14–16),its application in HAIC remains underinvestigated. Early studies in TACE demonstrate comparable technical success rates (86.2%-95.13%) and low major complication rates (0%-5.7%) with dTRA, highlighting its potential for hepatic interventions (17, 18). The anatomical snuffbox puncture site avoids the hypothenar motor branch and provides a straight trajectory to the aortic arch, potentially simplifying catheter navigation to the hepatic artery (19).
Despite these advancements, HAIC-specific data on dTRA are scarce. Technical feasibility, safety profiles, particularly d-RAO rates and impact of repeated punctures on radial artery patency in long-duration procedures requiring prolonged catheter retention are still key uncertainties. This study aims to address these gaps by evaluating dTRA-HAIC in a real-world HCC cohort, focusing on procedural outcomes, complication rates, and predictors of d-RAO.
2 Methods
2.1 Study design and patient selection
This single-center retrospective cohort study included 44 patients who underwent 63 dTRA-HAIC procedures for hepatocellular carcinoma between November 2023 and December 2024. The study was approved by the institutional ethics committee (approval no. PJB2025-225-01), with informed consent waived due to its retrospective nature. In this study, important measures such as data anonymization and data access control were adopted to ensure the privacy and security of patients.
Inclusion criteria: (1) Patients with hepatocellular carcinoma (HCC) confirmed by pathology or imaging; (2) underwent hepatic artery infusion chemotherapy (HAIC) via the distal transradial access (d-TRA); (3) with complete clinical data. Exclusion criteria included: (1) concurrent severe comorbidities (e.g., severe cardiac dysfunction, renal failure); (2) preexisting occlusion or significant vascular abnormalities of the distal radial artery; (3) intraoperative conversion to alternative access routes (e.g., femoral artery approach).
2.2 Procedural technique
2.2.1 Puncture and sheath placement
Patients were positioned supine with the punctured hand resting on the lower abdomen. Under Doppler ultrasound guidance (SonoScape S70N), the distal radial artery at the anatomical snuffbox was punctured using a 21G needle (Merit Medical). Following successful blood return, a 0.018-inch guidewire was advanced, and a 4F microsheath (Merit Medical) or 4F radial sheath (APT) was deployed (Figure 1A). The sheath was flushed with a cocktail of nitroglycerin (100 μg), lidocaine (1 mL), and heparin (2000 U) to minimize spasm and thrombosis.

Figure 1. Technical procedure. (A) Transradial artery puncture, guidewire insertion and 4F radial sheath placement. (B) Catheter fixation, sheath removal, and compression with elastic bandage.
2.2.2 Catheter navigation and HAIC
A 125-cm MPA1/Ultimate1 catheter (Cordis) and 180-cm 0.035-inch guidewire (Terumo) were used to navigate through the brachial, axillary, and subclavian arteries to the hepatic artery. Angiography confirmed tumor-feeding vessels before infusing chemotherapy (mFOLFOX: oxaliplatin 85 mg/m2 intra-arterial infusion on day 1, levoleucovorin Calcium 200 mg/m2 intra-arterial infusion on day 1, and 5-fluorouracil, 400 mg/m2 bolus infusion on day 1 and 2400 mg/m2 continuous infusion over 26 or 46 h, or Ralox: oxaliplatin 100 mg/m2 for 3∼5 h, raltitrexed 3 mg/m2 in 1 h). Post-procedure, the sheath was removed, and manual compression with an elastic bandage was applied for 3 hours (Figure 1B).
2.3 Data collection and outcomes
The following data were collected: patient age, gender, tumor stages, tumor sizes, underlying medical conditions (e.g. liver cirrhosis, hypertension, diabetes mellitus, tobacco smoking, alcohol consumption, anticoagulants), procedural details of TRA (including access kit, puncture time, diameter of the distal radial artery and procedural time), incidence of distal radial artery occlusion (d-RAO) and vascular recanalization after the procedure, the preoperative baseline indicators, such as platelet count, prothrombin time (PT) and D-dimer, total cholesterol and so on just before the procedure.
The main observation indicators included: (1) the puncture time, diameter of the distal radial artery and procedural time; (2) incidence of distal radial artery occlusion (d-RAO), defined as the absence of radial artery flow on postoperative ultrasound; (3) access sites complications (bleeding, hematoma, arterial dissection, pseudoaneurysm, etc.); (4) vascular recanalization. Univariate analysis was performed to identify predictive factors associated with d-RAO development.
2.4 Statistical analysis
Categorical variables were presented as frequencies and percentages, while continuous variables were expressed as medians [interquartile range] or means ± standard deviation. Group comparisons were performed using the χ² test or Mann-Whitney U test. Preoperative variables were analyzed for associations with d-RAO using univariate and multivariate logistic regression analysis. All analyses were conducted using SPSS 26.0, with p < 0.05 considered statistically significant.
3 Results
3.1 Baseline characteristics
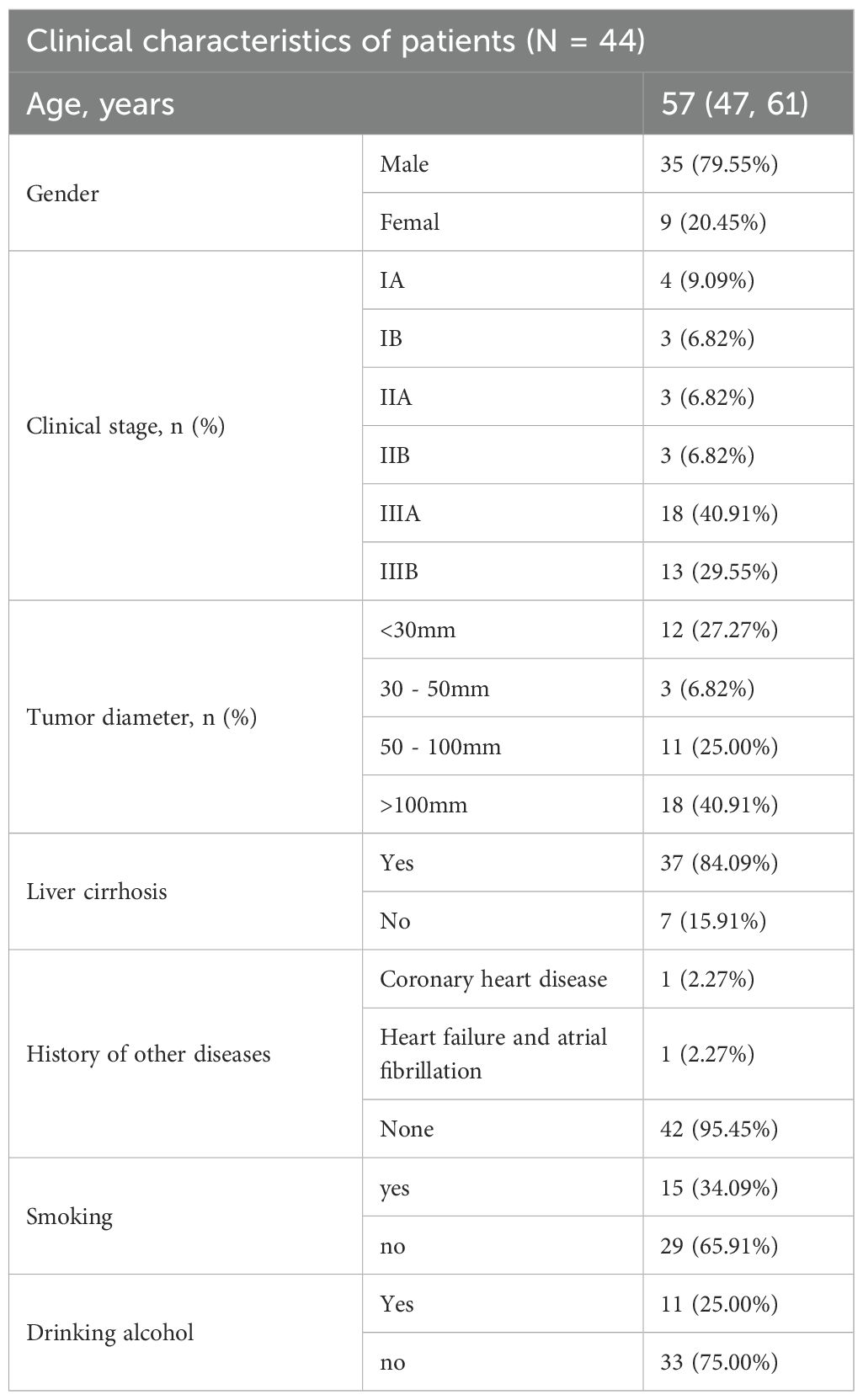
Forty-four patients (79.5% male) with a mean age of 57 years (range 47–61) were included. Most had advanced HCC (CNLC IIIA: 40.9%, IIIB: 29.5%), large tumors (>5 cm: 65.9%), and underlying cirrhosis (84.1%). Comorbidities included hypertension (54.5%) and diabetes (31.8%). Baseline demographics are detailed in Table 1.
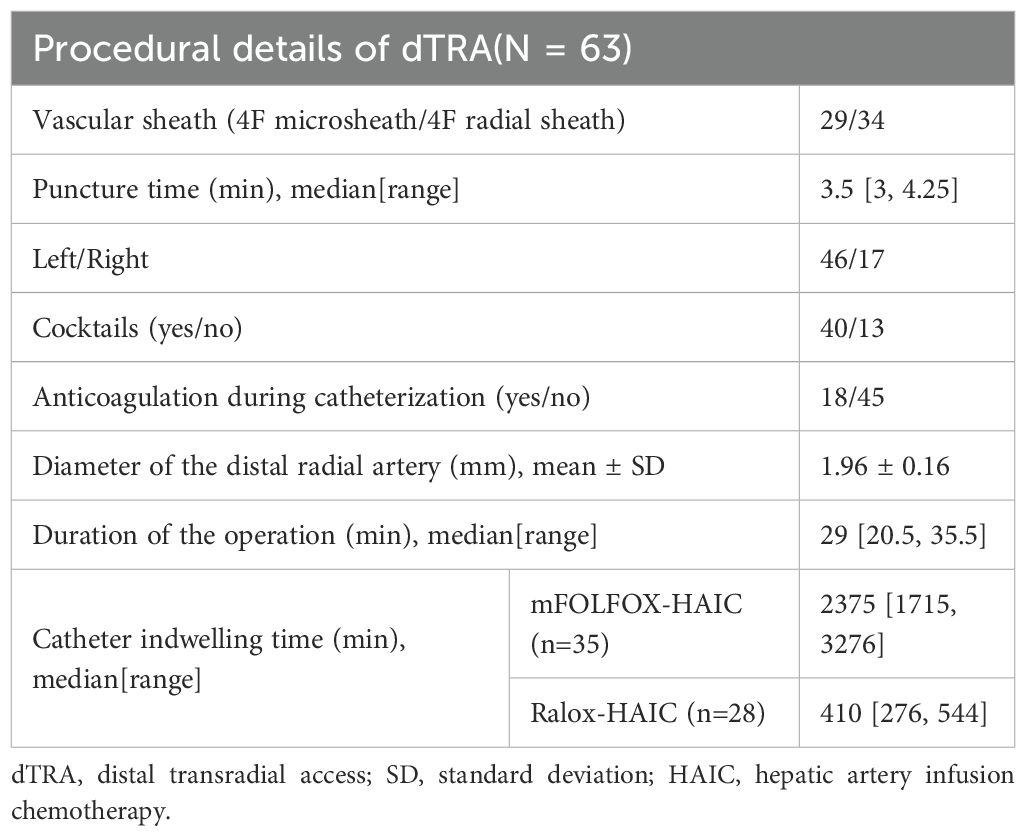
3.2 Procedural outcomes
A total of 63 procedures were performed (left dTRA: 73.0%, right dTRA: 27.0%). Technical success (defined as successful hepatic artery cannulation) was achieved in all cases. Median puncture time was 3.5 minutes (IQR 3–4.25), with a mean distal radial artery diameter of 1.96 ± 0.16 mm. The mean catheter indwelling time for mFOLFOX-HAIC and Ralox-HAIC was 2375 minutes (IQR 1715–3276 minutes) and 410 minutes (IQR 276, 544 minutes), respectively. Eighteen patients underwent repeated punctures (2–4 times), with one patient requiring four sessions (Table 2).
3.3 Safety and complications
3.3.1 Distal radial artery occlusion
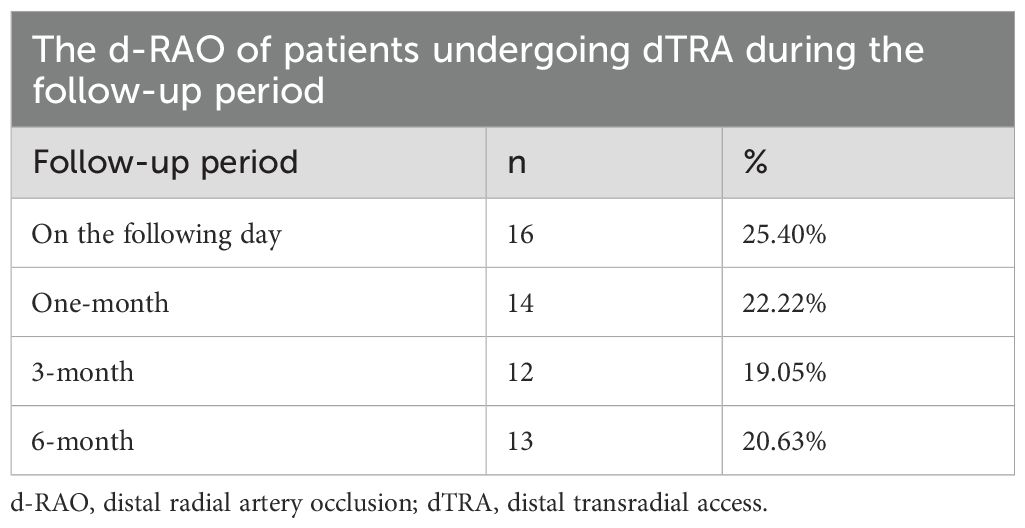
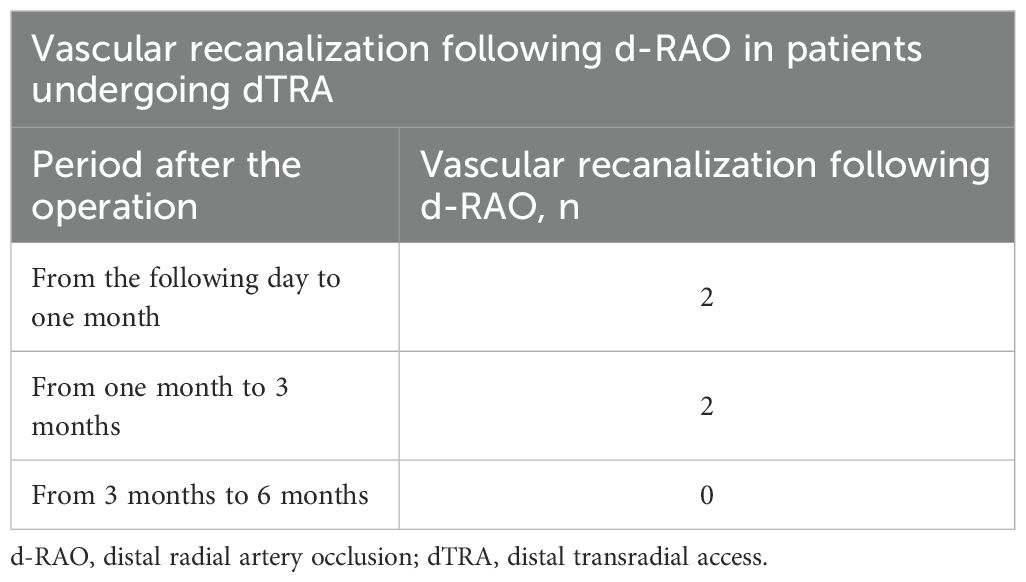
The d-RAO incidence decreased over time: 25.4% (16/63) on day 1, 22.2% (14/63) at 1 month, 19.1% (12/63) at 3 months, and 20.6% (13/63) at 6 months (Table 3). Vascular recanalization occurred in 4 cases (6.3%): 2 within 1 month and 2 between 1–3 months. No recanalization was observed after 3 months (Table 4).
3.3.2 Risk Factors for d-RAO
Univariate analysis revealed that D-dimer was significantly associated with an increased risk of d-RAO (OR = 1.35, 95% CI: 1.08-1.69, p = 0.009) (Table 5). After adjusting for potential confounders (including smoking, operation time, catheter indwelling time and so on), multivariate analysis demonstrated that D-dimer remained an independent risk factor for d-RAO (adjusted OR = 1.29, 95% CI: 1.03-1.62, p = 0.029) (Table 5). This suggests that D-dimer provides independent prognostic value for predicting d-RAO in the first post-operation month. Notably, the sole patient with four punctures developed persistent d-RAO at all time points (Table 6).
3.4 Access site complications
No major complications (arterial dissection, pseudoaneurysm, or severe bleeding) were observed. Minor ecchymosis occurred in 5 cases (7.9%), resolving within 48 hours without intervention.
4 Discussion
HAIC, as an important interventional therapy for advanced HCC, can effectively control intrahepatic tumors, increase objective response rate, prolong overall survival, and improve quality of life. TFA, as the conventional approach of HAIC, has the remarkable limitation of restricting activities. This study demonstrates that dTRA is technically feasible for HAIC, with a 100% cannulation success rate and median puncture time of 3.5 minutes, comparable to reported TACE data (17, 20). The anatomical snuffbox provides a stable puncture site with direct access to the radial artery, avoiding the tortuosity often encountered in proximal TRA. The use of 4F sheaths and hydrophilic guidewires minimized vascular trauma, while ultrasound guidance improved first-pass success, particularly in patients with small artery diameters (mean 1.96 mm). These findings align with prior studies showing that dTRA puncture success rates exceed 85% with operator experience (21).
The absence of major ASC (e.g., bleeding, pseudoaneurysm) highlights the safety of dTRA in HAIC. This contrasts with TFA, which reports hematoma rates of 2–5% and pseudoaneurysm rates of 0.3–1.0% (22). However, the incidence of bruisin/hematoma during HAIC via TFA ranges from 9.6% to 18.2% (23, 24). The superficial location of the distal radial artery allows efficient manual compression, reducing hemostasis time to 3 hours—significantly shorter than the 6–12 hours required for TFA (25). Secondly, dTRA reduces bed rest, avoids femoral vein compression, eliminating the risk of DVT, a critical advantage in immobile HCC patients with coagulation abnormalities. Additionally, dTRA is particularly suitable for obese patients or those with groin pathologies, expanding the treatable population (12).
The observed d-RAO rate (25.4% early, 20.6% at 6 months) is higher than rates reported in coronary studies (5.7–13%) (13, 26), but lower than traditional wrist-level TRA (up to 30%) (27). This discrepancy may reflect prolonged procedure duration during HAIC, which often requires extended catheter placement (always 6 hours or 46 hours) and increases endothelial injury and thrombus formation, as well as the unique coagulopathy profile in cirrhotic HCC patients, who exhibit both hypocoagulable (low platelets) and hypercoagulable (elevated D-dimer) states, complicating hemostasis (28). Consistently, previous study revealed RAO for HAIC by TRA access occurred more frequently, up to 33%-37.5% (24), which is much higher than our results. Additionally, repeated punctures contribute to cumulative vascular damage, with ≥4 punctures showing a 100% occlusion rate in our cohort. Therefore, for patients requiring multiple HAIC sessions, strategies such as vascular protection or alternating bilateral radial artery use should be considered. Notably, d-RAO rates declined over time, possibly due to spontaneous recanalization or collateral development via the palmar arch. Early recanalization (within 3 months) was observed in 6.3% of cases, underscoring the importance of early Doppler ultrasound surveillance.
Preoperative D-dimer levels emerged as a significant predictor of d-RAO, reflecting systemic endothelial dysfunction and hypercoagulability in HCC (29). Elevated D-dimer may indicate microvascular injury, increasing susceptibility to thrombosis (18). Clinically, this suggests routine D-dimer screening to identify high-risk patients, who may benefit from intensified anticoagulation (e.g., higher heparin doses) or alternative access sites.
dTRA provides significant advantages for HCC patients, including improved comfort through early ambulation, preservation of femoral access for repeat interventions, and technical benefits such as easier catheter navigation via the left dTRA’s shorter path to the celiac trunk (30). Patient quality of life (QOL) measure was not provided in this study. Previous studied showed TRA to HAIC was associated with greater improvement in the quality of life associated with the procedure compared with TFA (24, 31). Furthermore, for patients with advanced liver malignancies undergoing HAIC treatment, TRA significantly outperformed TFA in terms of patient satisfaction and average hospital stay (23). Based on this, it can be inferred that HCC patients treated with the dTRA approach for HAIC may achieve higher comfort and better quality of life compared to those treated with the TFA approach.
However, its adoption is limited by factors such as the single-center retrospective nature of current study, no control groups, relatively small sample size and the need for longer-term patency data beyond six months. Future research should focus on prospective comparisons between dTRA and TFA for HAIC, as well as the development of vascular protection strategies like optimized antiplatelet regimens or drug-eluting sheaths. Additionally, refining patient selection through biomarker assessment—such as D-dimer and platelet function testing—could further enhance outcomes and minimize complications.
5 Conclusion
Distal transradial access for hepatic artery infusion chemotherapy is a feasible and safe alternative to traditional transfemoral access, with acceptable d-RAO rates and minimal major complications. Preoperative D-dimer screening and limitations on repeated punctures may optimize outcomes. However, large-scale prospective cohort studies are warranted to validate these findings and refine patient selection criteria.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ganzhou people’s hospital ethics committee. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because The research carried out meets the following conditions: it is a study that utilizes the medical records obtained from previous clinical diagnoses and treatments, and meets all of the following conditions: The purpose of the research is important. 2. Waiving informed consent will not have an adverse impact on the rights and health of the subjects. 3. The privacy and personal identity information of the subjects are protected.
Author contributions
YW: Investigation, Methodology, Formal Analysis, Writing – original draft, Data curation. CY: Data curation, Validation, Writing – review & editing. XL: Validation, Data curation, Writing – review & editing. BZ: Data curation, Validation, Writing – review & editing. DZ: Data curation, Validation, Writing – review & editing. YT: Project administration, Supervision, Funding acquisition, Writing – review & editing, Investigation, Conceptualization.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was supported by grants from Health Commission of Ganzhou Municipality for Interventional Clinical Specialty Capacity Building Plan and Bureau of Science and Technology of Ganzhou Municipality (NO.GZ2022ZSF087). The funders had no role in study design, data collection, data analysis, interpretation or writing of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Shan T, Ran X, Li H, Feng G, Zhang S, Zhang X, et al. Disparities in stage at diagnosis for liver cancer in China. J Natl Cancer Center. (2023) 3:7–13. doi: 10.1016/j.jncc.2022.12.002
3. Lyu N, Wang X, Li JB, Lai JF, Chen QF, Li SL, et al. Arterial chemotherapy of oxaliplatin plus fluorouracil versus sorafenib in advanced hepatocellular carcinoma: A biomolecular exploratory, randomized, phase III trial (FOHAIC-1). J Clin Oncol. (2022) 40:468–80. doi: 10.1200/JCO.21.01963
4. Li QJ, He MK, Chen HW, Fang WQ, Zhou YM, Xu L, et al. Hepatic arterial infusion of oxaliplatin, fluorouracil, and leucovorin versus transarterial chemoembolization for large hepatocellular carcinoma: A randomized phase III trial. J Clin Oncol. (2022) 40:150–60. doi: 10.1200/JCO.21.00608
5. Feng G, Feng Y, Yao S, Huang X, Peng Z, Tang Y, et al. Transcatheter arterial chemoembolization combined with hepatic arterial infusion chemotherapy versus transcatheter arterial chemoembolization for unresectable hepatocellular carcinoma: A systematic review and meta-analysis. Turk J Gastroenterol. (2024) 35:266–79. doi: 10.5152/tjg.2024.23228
6. Zhang W, Ouyang D, Huang Z, and Che X. Hepatic arterial infusion chemotherapy versus sorafenib for advanced hepatocellular carcinoma with portal vein tumor thrombus: An updated meta-analysis and systematic review. Front Oncol. (2023) 13:1085166. doi: 10.3389/fonc.2023.1085166
7. Lai Z, Huang Y, Wen D, Lin X, Kan A, Li Q, et al. One day versus two days of hepatic arterial infusion with oxaliplatin and fluorouracil for patients with unresectable hepatocellular carcinoma. BMC Med. (2022) 20:415. doi: 10.1186/s12916-022-02608-6
8. Lyu N, Kong Y, Mu L, Lin Y, Li J, Liu Y, et al. Hepatic arterial infusion of oxaliplatin plus fluorouracil/leucovorin vs. sorafenib for advanced hepatocellular carcinoma. J Hepatol. (2018) 69:60–9. doi: 10.1016/j.jhep.2018.02.008
9. Zang M, Hu X, Yuan G, Li R, Li W, Pang H, et al. Tyrosine kinase inhibitors, immune checkpoint inhibitors combined with hepatic arterial infusion of oxaliplatin and raltitrexed versus oxaliplatin, 5-fluorouracil and leucovorin for intermediate and advanced hepatocellular carcinoma: A retrospective study. Int Immunopharmacol. (2023) 125:111019. doi: 10.1016/j.intimp.2023.111019
10. Seol SM, Kim PH, Shin JH, Chun SY, Lee MY, Kim KM, et al. The safety and efficacy of haemostasis with a catechol-conjugated, chitosan-based haemostatic dressing versus a chitosan-based haemostatic dressing after transfemoral approach for transcatheter arterial chemoembolization: a randomized controlled trial. Pol J Radiol. (2021) 86:e685–91. doi: 10.5114/pjr.2021.112327
11. Kiemeneij F. Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI). EuroIntervention. (2017) 13:851–7. doi: 10.4244/EIJ-D-17-00079
12. Sgueglia GA, Di Giorgio A, Gaspardone A, and Babunashvili A. Anatomic basis and physiological rationale of distal radial artery access for percutaneous coronary and endovascular procedures. JACC Cardiovasc Interv. (2018) 11:2113–9. doi: 10.1016/j.jcin.2018.04.045
13. Li F, Shi GW, Zhang BF, Yu XL, Huang HM, Xiao JQ, et al. Recanalization of the occluded radial artery via distal transradial access in the anatomic snuffbox. BMC Cardiovasc Disord. (2021) 21:67. doi: 10.1186/s12872-021-01890-1
14. Jiang F, Fan WL, Zheng W, Wu X, and Hu H. Distal radial artery access is a safe and feasible technique in the anatomical snuffbox for visceral intervention. Med (Baltimore). (2023) 102:e33987. doi: 10.1097/MD.0000000000033987
15. Wang X, Xian L, Zhang W, Xu Y, Zhao D, and Wang X. Feasibility and safety of transarterial chemoembolization in patients with liver cancer via the distal radial approach: a single-center retrospective cohort study. Transl Cancer Res. (2024) 13:4500–6. doi: 10.21037/tcr-24-1231
16. Rashid M, Kwok CS, Pancholy S, Chugh S, Kedev SA, Bernat I, et al. Radial artery occlusion after transradial interventions: A systematic review and meta-analysis. J Am Heart Assoc. (2016) 5:e002686. doi: 10.1161/JAHA.115.002686
17. Li J, Xian L, Wang X, Wang X, Wang D, and Zhang W. Hepatic artery chemoembolization with distal transradial access for primary hepatocellular carcinoma: a novel interventional therapy for peripheral tumors. Am J Transl Res. (2023) 15:5791–6.
18. Xu D, Liu Y, Xu C, Liu X, Chen Y, Feng C, et al. Factors affecting radial artery occlusion after right transradial artery catheterization for coronary intervention and procedures. Ther Clin Risk Manage. (2023) 19:525–33. doi: 10.2147/TCRM.S403410
19. Babunashvili A and Dundua D. Recanalization and reuse of early occluded radial artery within 6 days after previous transradial diagnostic procedure. Catheter Cardiovasc Interv: Off J Soc Cardiac Angiogr Interventions. (2011) 77:530–6. doi: 10.1002/ccd.22846
20. Valgimigli M, Gagnor A, Calabró P, Frigoli E, Leonardi S, Zaro T, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. Lancet. (2015) 385:2465–76. doi: 10.1016/S0140-6736(15)60292-6
21. Valsecchi O, Vassileva A, Cereda AF, Canova P, Satogami K, Fiocca L, et al. Early clinical experience with right and left distal transradial access in the anatomical snuffbox in 52 consecutive patients. J Invasive Cardiol. (2018) 30:218–23.
22. Koutouzis M, Kontopodis E, Tassopoulos A, Tsiafoutis I, Katsanou K, Rigatou A, et al. Distal versus traditional radial approach for coronary angiography. Cardiovasc Revasc Med: Including Mol Interventions. (2019) 20:678–80. doi: 10.1016/j.carrev.2018.09.018
23. Lyu TY, Li M, He JA, Sun QF, Wang L, Qin H, et al. Analysis of the experience and procedural complications of trans-radial access versus trans-femoral access for hepatic arterial perfusion chemotherapy in patients with advanced hepatic Malignancies:a retrospective study. Zhonghua Nei Ke Za Zhi. (2024) 63:183–91. doi: 10.3760/cma.j.cn112138-20230827-00087
24. Wan Y, Chen B, Li N, Yang JY, Dai HT, Tang KY, et al. Transradial versus transfemoral access for patients with liver cancer undergoing hepatic arterial infusion chemotherapy: patient experience and procedural complications. J Vasc Interv Radiol. (2022) 33:956–963.e1. doi: 10.1016/j.jvir.2022.04.024
25. Pancholy SB and Patel TM. Effect of duration of hemostatic compression on radial artery occlusion after transradial access. Catheter Cardiovasc Interv. (2012) 79:78–81. doi: 10.1002/ccd.22963
26. Tuncez A, Kaya Z, Aras D, Yıldız A, Gül EE, Tekinalp M, et al. Incidence and predictors of radial artery occlusion associated transradial catheterization. Int J Med Sci. (2013) 10:1715–9. doi: 10.7150/ijms.7087
27. Uhlemann M, Möbius-Winkler S, Mende M, Eitel I, Fuernau G, Sandri M, et al. The Leipzig prospective vascular ultrasound registry in radial artery catheterization: impact of sheath size on vascular complications. JACC Cardiovasc Interventions. (2012) 5:36–43. doi: 10.1016/j.jcin.2011.08.011
28. Tripodi A and Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med. (2011) 365:147–56. doi: 10.1056/NEJMra1011170
29. Wang Y, Liu Z, Wu Y, Li Z, Wang Y, Wang S, et al. Early prevention of radial artery occlusion via distal transradial access for primary percutaneous coronary intervention. Front Cardiovasc Med. (2022) 9:1071575. doi: 10.3389/fcvm.2022.1071575
30. Shah RM, Patel D, Abbate A, Cowley MJ, and Jovin IS. Comparison of transradial coronary procedures via right radial versus left radial artery approach: A meta-analysis. Catheter Cardiovasc Interv: Off J Soc Cardiac Angiogr Interventions. (2016) 88:1027–33. doi: 10.1002/ccd.26519
Keywords: hepatocellular carcinoma, distal transradial access (dTRA), hepaticartery infusion chemotherapy, feasibility, safety
Citation: Wu Y, Yu C, Li X, Zhong B, Zeng D and Tian Y (2025) Feasibility and safety of hepatic artery infusion chemotherapy via the distal transradial access for hepatocellular carcinoma. Front. Oncol. 15:1644296. doi: 10.3389/fonc.2025.1644296
Received: 10 June 2025; Accepted: 08 October 2025;
Published: 22 October 2025.
Edited by:
Ganesan Ramamoorthi, Moffitt Cancer Center, United StatesReviewed by:
Zhao Xiao-Hui, Tianjin Medical University Cancer Institute and Hospital, ChinaAbhirup Bagchi, Children’s Hospital of Philadelphia, United States
Copyright © 2025 Wu, Yu, Li, Zhong, Zeng and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunfei Tian, amllcnV3eTAxQDEyNi5jb20=
 Yi Wu
Yi Wu Chunlin Yu
Chunlin Yu Yunfei Tian
Yunfei Tian