- 1Vanderbilt-Ingram Cancer Center, Vanderbilt University Medical Center, Nashville, TN, United States
- 2David Geffen School of Medicine at University of California, Los Angeles (UCLA), Los Angeles, CA, United States
- 3Karyopharm Therapeutics Inc., Newton, MA, United States
- 4Division of Hematologic Malignancies and Cellular Therapy, Department of Medicine, Duke University Medical Center, Durham, NC, United States
Background: Selinexor, a first-in-class, oral exportin-1 inhibitor, showed activity in penta-refractory multiple myeloma (MM) in early trial exploration; however, the side-effect profile of twice-weekly dosing led to hesitant incorporation into widespread practice. Here, our objective is to provide updated clinical evidence highlighting the preserved efficacy and improved tolerability of once-weekly selinexor at lower doses in patients with previously treated MM compared to twice-weekly regimens.
Methods: Patient-level data from the BOSTON, STOMP, STORM, and XPORT-MM-028 clinical trials were systematically evaluated to elucidate relationships between selinexor dosing schedule, regimen toxicities, and efficacy in patients with MM that had progressed after at least one prior therapy.
Results: Updated results on once-weekly selinexor in combination with other anti-MM agents showed a reduced adverse event profile and improved tolerability compared with twice-weekly selinexor regimens, without compromise in efficacy. Furthermore, new data from several regimens with weekly selinexor delivery suggest that patients who had selinexor dose reductions or were treated in cohorts with a lower selinexor starting dose had reduced rates of adverse events, and superior durations of response. Weekly selinexor in combination with pomalidomide or carfilzomib in particular showed efficacy in difficult-to-treat, multiclass relapsed/refractory MM, including MM refractory to prior BCMA-directed therapies.
Conclusions: In a rapidly evolving field of previously treated MM, lowering of selinexor dose and frequency into weekly regimens showed a more feasible and tolerable treatment with continued efficacy when compared to twice-weekly schedules, paving the path for effective management of multiclass refractory MM, including patients with very advanced disease.
1 Introduction
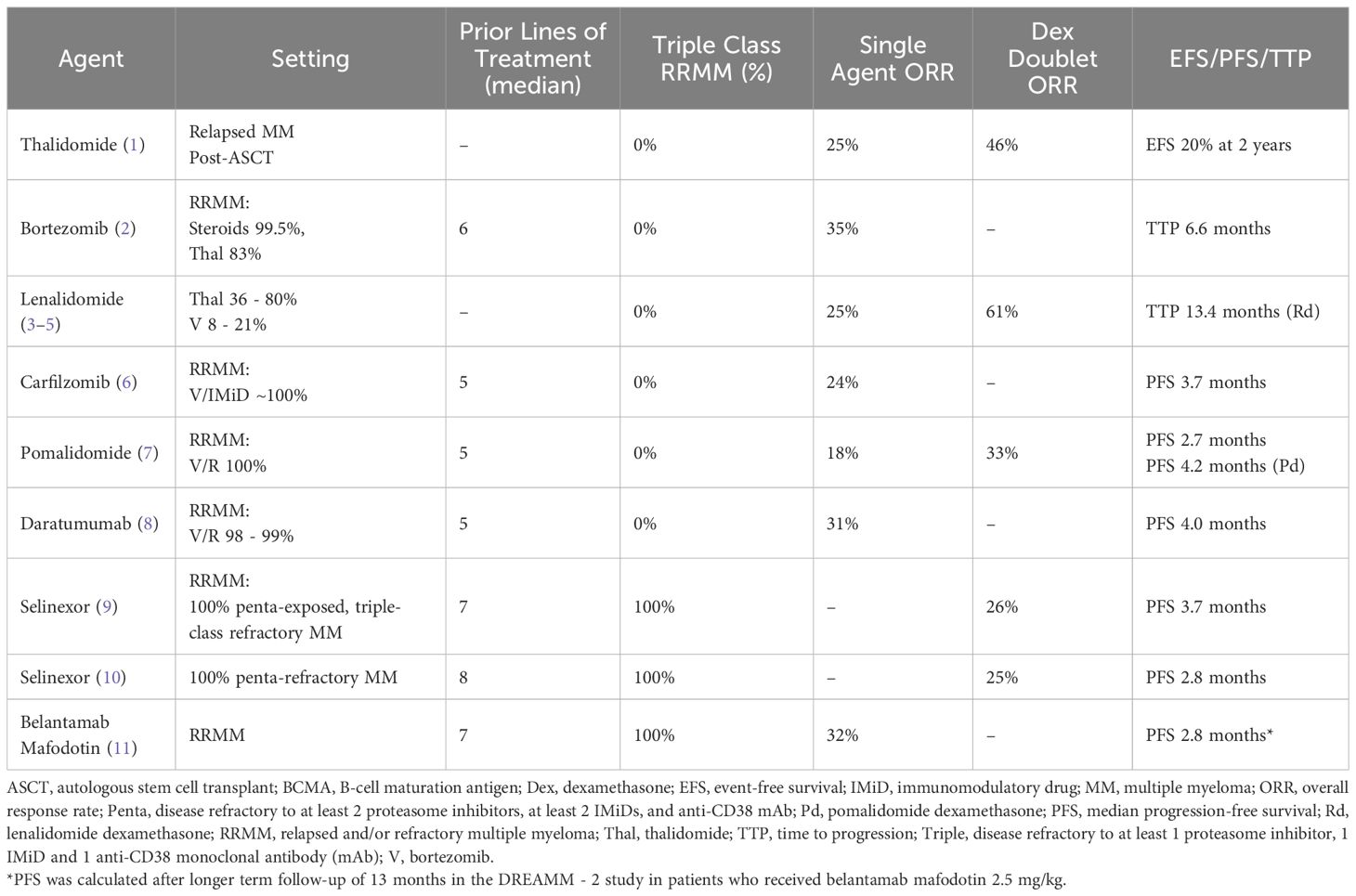
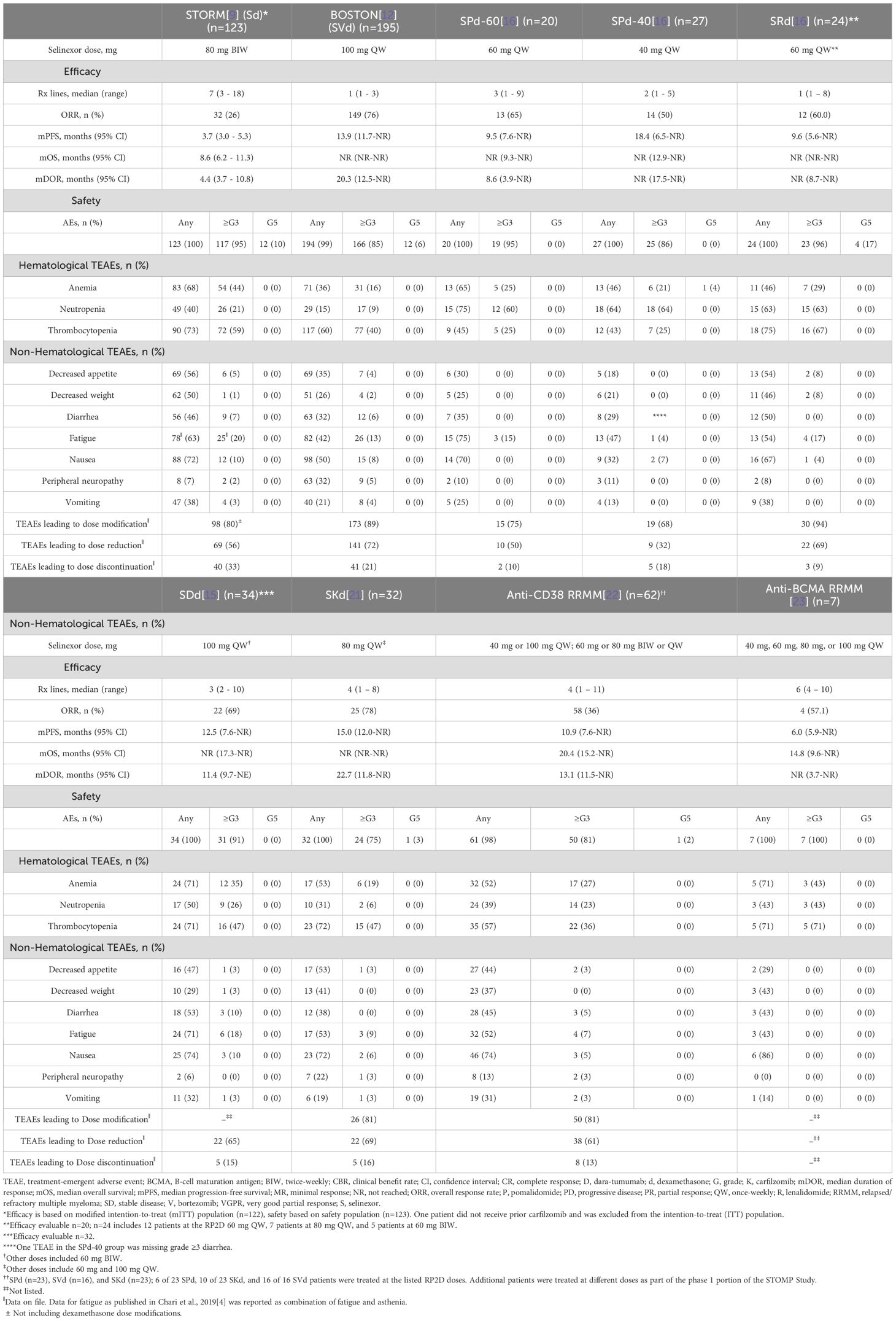
Multiple myeloma (MM) treatment is ever-evolving (Figure 1). Prior to recent advent of chimeric antigen receptor (CAR) T cell and bispecific antibodies, the single-agent overall response rates (ORRs) in previously treated MM ranged from 20%-30% (Table 1), highlighting the need to discover and combine new mechanisms of action to achieve optimal clinical responses. In 2019, selinexor (S), the first-in-class, oral XPO - 1 inhibitor, was approved in combination with dexamethasone for the treatment of heavily pre-treated relapsed/refractory myeloma. Overexpression of XPO - 1 is correlated with poor prognosis in a number of malignancies, including MM (9, 10, 12–20). Selectively targeting XPO - 1 interferes with nucleocytoplasmic transport and reactivates tumor suppressor proteins, while also blocking translation of oncogene-coding mRNAs (12). The Phase 2b Selinexor in the Treatment of Relapsed Myeloma (STORM) study (NCT02336815) evaluating the doublet combination of selinexor 80 mg plus dexamethasone 20 mg (Sd) twice-weekly showed an ORR of 26%, a median time to first response of 4.1 weeks, and a median progression free survival (PFS) of 3.7 months (9, 10, 12). Sd also showed improved overall survival (OS) in matched cohorts in community and academic settings. Yet, although it was a new option for penta-refractory MM, selinexor incorporation in everyday practice was hindered by the side effect profile of this twice-weekly combination.
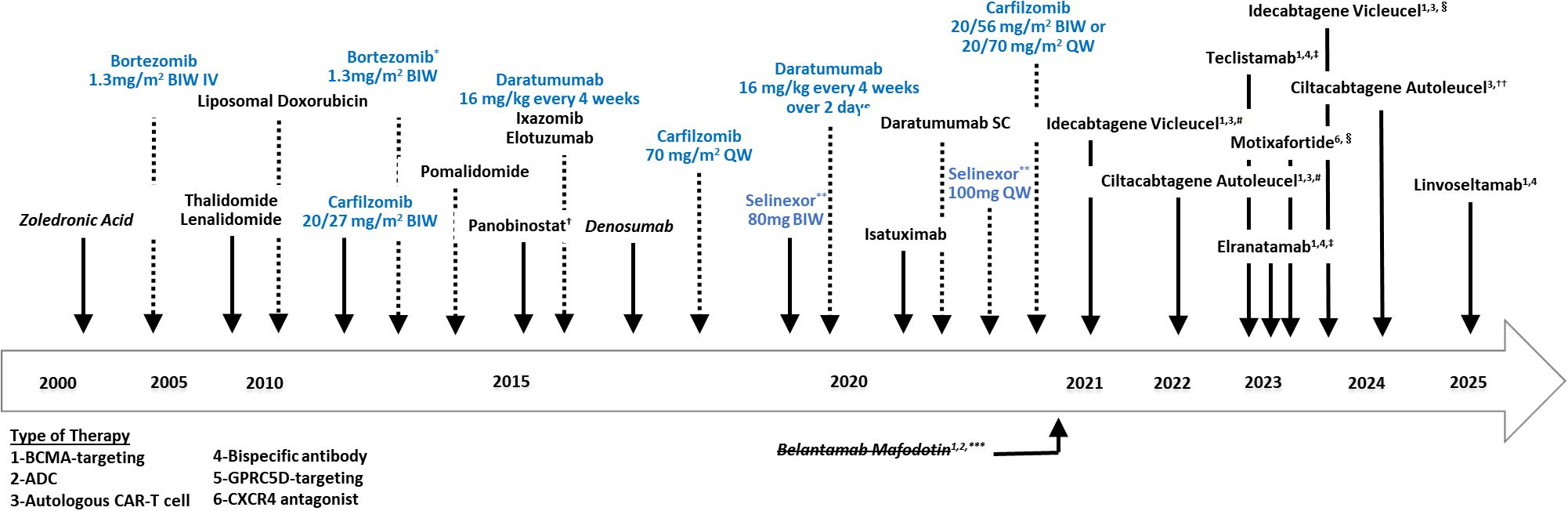
Figure 1. Two decades of multiple myeloma regulatory approvals. ADC, antibody dependent cytotoxicity; BCMA, B cell maturation antigen; BIW, twice-weekly; CAR-T, chimeric antigen receptor T-cell; CXCR4, C-X-C chemokine receptor type 4; GPRC5D, G protein-coupled receptor family C group 5 member D; SC, subcutaneous; QW, once-weekly. Drugs in blue have additional changes in doses/route of administration following drug approval. *Bortezomib dose remained the same and route of administration was updated to include sub-cutaneous in addition to intravenous. **Accelerated approval granted by the FDA in July 2019; approved in December 2020 in combination with bortezomib and dexamethasone; granted full approval by the European Medicines Agency (EMA) in May 2022. ***Accelerated approval granted by the FDA, withdrawn in November 2022 after negative results in confirmatory trial (DREAMM-3). †Approval was granted by the FDA in Nov 2023 for patients with relapsed or refractory multiple myeloma (RRMM) who have received at least 4 prior lines of therapy. ‡Conditional marketing authorization granted by the EMA and granted accelerated approval by the FDA. #Approval granted by the US FDA and conditional marketing authorization granted by the EMA. §Approval granted to include sooner after two or more lines of therapy. Originally approved for later line use ≥4 prior lines of therapy. ††Approval granted to include use at first relapse in adult patients refractory to lenalidomide after 1–3 prior lines. Originally approved for later line use ≥4 prior lines of therapy.
Here, we review the clinical efficacy and tolerability of selinexor in combination with various partner agents, with a focus on weekly versus twice-weekly dosing.
2 Material and methods
Patients with RRMM treated with selinexor were evaluated across multiple trials, including BOSTON (S-bortezomib, dexamethasone [SVd]) (12), Selinexor and Backbone Treatments of Multiple Myeloma Patients (STOMP) (NCT02343042) (S-pomalidomide, dexamethasone [SPd] (16), S-lenalidomide, dexamethasone [SRd] (13, 14), S-daratumumab, dexamethasone [SDd] (15), and S-carfilzomib, dexamethasone [SKd] (21) arms), STORM (9), and XPORT-MM-028 (NCT04414475) (SPd arm). These regimens incorporated both weekly and twice-weekly selinexor dosing schedules (Table 2). The impacts of selinexor posology on regimen toxicities, treatment duration, need for dose modifications, and efficacy in RRMM were examined.
3 Results
3.1 Lower selinexor dosing is tolerable and active
Despite the favorable response rates and clinical benefits seen in the STORM study, the 160 mg selinexor cumulative weekly dose resulted in high rates of adverse events (AEs) (Table 2) (17). The major Grade ≥3 non-hematological toxicities reported in STORM (n=202) were fatigue (22%) and nausea (9%). Tolerability, as assessed indirectly via median duration of exposure (mDOE), was 3.8 months (9, 10). Toxicities resulted in dose reductions and modifications in 80% of patients (9).
Subsequent studies evaluated lower selinexor doses and frequencies. The phase 3 BOSTON study (NCT 031110562) compared the efficacy of once-weekly (QW) selinexor 100 mg and subcutaneous bortezomib 1.3 mg/m2 combined with twice-weekly (BIW) dexamethasone 20 mg (SVd) to standard twice-weekly bortezomib and dexamethasone (Vd) in patients with MM that had progressive disease despite 1 – 3 prior lines of therapy (12). SVd received United States Food and Drug Administration (US FDA) approval in 2020 based on significantly improved PFS as determined by an independent review committee. After median follow-up of 13.2 months (SVd) and 16.5 months (Vd), median PFS was 13.93 and 9.46 months, respectively (HR 0.70 [95% CI 0.53 – 0.93], p=0.0075). The prespecified endpoint of ORR was 76.4% (SVd) versus 62.3% (Vd) (p = 0.0012), and ≥ very good partial response (VGPR) rates were 44.6% (SVd) versus 32.4% (Vd) (p=0.0082). The European Medicines Agency approved SVd in March 2021 for patients with MM who received at least one prior therapy.
Compared to twice-weekly 80 mg selinexor (Sd) in the STORM trial, the once-weekly 100 mg selinexor BOSTON regimen (SVd) showed improved tolerability, with ≥ Grade 3 non-hematologic toxicities of fatigue and nausea reduced to 13% and 8%, respectively, in the BOSTON study (9, 12). Selinexor dose reductions occurred in 65% of SVd-treated patients, with a median final dose of 71.4 mg/week. Patients who had a dose reduction compared to those before dose reduction had lower duration-adjusted AE incidence rates (18). Notably, patients in the BOSTON study who had a selinexor dose reduction had a longer median PFS compared to those who did not (16.6 versus 9.2 months), suggesting that lower selinexor doses have continued activity in RRMM (18). Furthermore, SVd treatment in the BOSTON study showed that ORR was higher among patients with dose reductions compared to those without (82% versus 67%). While some caveats to the interpretation of these results can be postulated, such as more motivation to maintain a regimen with dose reduction in patients who were already responding well, or the fact that patients with stable or slowly responding disease may have had earlier discontinuation of treatment, these data showed an emerging impact of lower dose, weekly schedules of selinexor in previously treated MM (18).
Following BOSTON, the STOMP trial, a multi-arm, open-label, Phase 1b/2 study, evaluated selinexor in various triplet and quadruplet combinations in newly diagnosed and relapsed/refractory MM. S-containing triplets comprised other commonly used anti-myeloma agents such as daratumumab (D) (15), pomalidomide (P) (19), lenalidomide (R) (13), and carfilzomib (K) (20), as outlined in Table 2 (13, 15, 19, 20).
Among patients treated with SPd in STOMP (QW selinexor 40 mg [SPd-40] or 60 mg [SPd-60]) and XPORT-MM-028 (SPd-40), ORR and ≥VGPR in the SPd-40 cohort were 50% and 29%, respectively, and 65% and 30% in the SPd-60 cohort. Despite deeper responses in the SPd-60 cohort, as of June 30, 2023, mPFS was numerically longer, however did not reach statistical significance with SPd-40 (18.4 months [95% CI: 6.5, NR]) compared to SPd-60 (9.5 months [95% CI: 7.6, NR]) (16). The mDOE was also longer with SPd-40 (28 weeks) compared to SPd-60 (22 weeks). Similar to the BOSTON experience, lower selinexor dosing led to lower AE incidence, which was observed in the context of longer mDOE and mPFS for patients that were able to stay on treatment more reliably. Patients treated with SRd in STOMP (selinexor doses of 60 mg QW, 80 mg QW, and 60 mg BIW) had an ORR of 60%, PFS of 9.6 months, and OS that was not reached (Table 2), again showing activity for lower dose weekly selinexor. Overall, the total weekly selinexor dose in STORM was 1.6x higher than in BOSTON and 1.6 - 4x higher than preferred dosing in combination with other agents tested in STOMP cohorts. Taken together, lower selinexor doses, whether initiated at baseline or following dose modification, allows patients to stay on selinexor longer, thereby improving outcomes.
3.2 Weekly selinexor regimens offer value post-anti-CD38 mAb treatment
Most randomized trials evaluating second-generation proteasome inhibitors (PIs), immunomodulatory drugs (IMiDs), or agents with novel mechanisms of actions after early relapse have not included many patients with triple-class refractory (TCR) MM, largely due to trial-specific eligibility criteria (19, 20). However, with increasing use of frontline “quad” regimens, there is a growing need to address both non-responders and first-relapse patients with TCR MM. Recent studies in patients with RRMM treated with fewer prior lines of therapy have shown poor efficacy for triple-class exposed (TCE) or TCR MM treated with physician’s choice of subsequent therapy (24). Data from the LocoMMotion, MAMMOTH, and control arm of the KarMMa-3 trials, report that patients with at least TCE RRMM had PFS of 4.6, 3.4, and 4.4 months, respectively, and ORRs for the next line of treatment of 30 - 40% after anti-CD38 failure (24). These next line of treatments included different PIs, IMiDs, monoclonal antibodies, and alkylating chemotherapy regimens; selinexor-based combinations were used in < 1% of patients and therefore were not evaluated in the TCR MM context.
A retrospective analysis of 62 patients with RRMM from BOSTON and STOMP who had prior anti-CD38 exposure (median 4 prior lines), had ORRs of 52% (SPd), 56% (SVd), and 65% (SKd); only 6% of these patients received twice-weekly SPd dosing (22). Most patients were TCE and > 50% were TCR. Median PFS was 8.7 (SPd), 6.7 (SVd), and 15.0 (SKd) months and median OS was 20.4 months, with SPd at 9.6 months, SVd at 16.9 months, and SKd at 33.0 months (22). Adverse events for S-containing triplets were manageable with standard supportive care and dose modifications (Table 2). Grade ≥3 fatigue and nausea occurred in <5% of patients with SPd and SKd receiving with once-weekly dosing. Given historically poor outcomes in TCE RRMM with PIs, IMiDs, and anti-CD38 monoclonal antibodies who undergo drug-class recycling or turn to alkylator-based chemotherapy, these data suggest that once-weekly, appropriately selected S-based triplets offer a viable alternative, especially when access to T-cell-based immunotherapies is limited (22).
3.3 Selinexor in the new age of T-cell redirecting therapies
Chimeric antigen receptor T cell (CAR-T) and T-cell engaging bispecific antibody therapies have revolutionized our ability to manage RRMM. The single-agent activity of T-cell redirecting therapies established a new benchmark in RRMM, achieving ORR of 80 - 90% with CAR-T, and 50 - 70% with bispecific antibodies (Table 3). The two approved CAR-T cell products for MM, idecabtagene vicleucel and ciltacabtagene autoleucel, can be accessed in early lines of therapy based on the results of the KARMMA - 3 and the CARTITUDE - 4 phase 3 trials (39), while ongoing studies are generating data in the first line as well (40). This new era of MM therapeutics is welcome, however given that they are not curative, two issues must be addressed: 1) maximizing T-cell based therapy outcomes given their associated costs, logistical planning, and potential adverse effects; and 2) effectively addressing and treating a new population of RRMM that has failed bispecific antibody or CAR-T treatment. Early investigation into CAR-T efficacy has shown that factors such as T-cell exhaustion, an acquired inability for cytotoxic T-cells to target and eliminate tumors, may play a role in outcomes. A search for T-cell sparing agents to use in earlier line MM treatment to limit T-cell exhaustion and to support the efficacy of subsequent T-cell therapies is underway. IMiDs and cereblon E3 ligase modulatory drugs (CelMODs) have already been shown to increase cytotoxic T-cell activity as a downstream effect of cereblon targeting (41). Clinical data support the use of XPO - 1 inhibitors, such as low dose weekly selinexor, as potentially T-cell sparing in both the pre-apheresis stage (42) and the bridging period between apheresis and CAR-T infusion (43). Additional studies are underway to further investigate the interaction between XPO1 inhibitors, T cells, and the immune microenvironment. A retrospective study performed by the Myeloma CAR-T consortium examined the impact of various bridging regimens, as compared to no bridging, in patients with RRMM who received idecabtagene vicleucel. As reported, patients without the need for a bridge regimen to control the RRMM had the best outcomes, likely due to having more indolent disease. Amongst the patients who required bridging, those who received IMiD or S-based bridging had numerically longer PFS after CAR-T than those who received PI or alkylating chemotherapy bridging, with IMiD ± mAb combos showed comparable PFS to no-bridging (median PFS: 12.01 months vs. 11.48 months). In comparison to the IMiD ± mAb combination PFS, selinexor was 9.77 months, versus lower results with PI combos (6.41 months), and alkylator therapy (6.51 months) (43). These results suggest that S-based bridging combinations do not lead to inferior idecabtagene vicleucel outcomes, although the data specifying which doses and schedules of selinexor that were used as bridging was not reported.
A real-world evidence study reported the clinical outcomes of 45 patients treated with a selinexor regimen and subsequently received idecabtagene vicleucel, ciltacabtagene autoleucel, or another anti-BCMA CAR-T under development. The majority (75.5%) of patients received low dose selinexor (median 80mg weekly starting dose), most commonly in combination with carfilzomib (35%). The median line of selinexor exposure was seventh, while CAR-T was the ninth. An exploratory multivariate analysis determined that receiving selinexor in the line of therapy prior to CAR-T was associated with the best PFS and OS outcomes with hazard ratios of 0.4 (95% CI 0.113 – 1.09) and 0.08 (95% CI 0.02 – 0.46), respectively (42).
A report of S-containing regimens in RRMM patients who had progressed or failed anti-BCMA CAR-T showed objective responses in 6 of 7 patients, with 1 stringent complete response (treated with SKd), 3 VGPRs (2 treated with SKd and 1 with SVd), and 2 partial responses (PRs, 1 each with Sd and SVd). The ORR was 86% with a clinical benefit rate (CBR) of 100% with 1 additional minor response with SKd (44). A subsequent case series of 11 patients with progression after anti-BCMA (non-CAR-T) treatment (7 were anti-BCMA antibody drug conjugate pretreated) from the STOMP trial, all with weekly dosing of selinexor, reported ORR and CBR rates of 63.6% and 81.8%, respectively, and no cases of disease progression as a best response (23). Median DOR and PFS were not reached after median follow-up of 14.3 months and median OS was 14.8 months (Table 2). Response was >6 months for 5/7 responders and up to at least 15.6 months, with 6-month PFS probability determined to be 75%.
4 Discussion
Once-weekly SVd, SPd, SDd, and SKd, are all recommended regimen options according to the NCCN® guidelines. Lower starting doses and dose reductions during therapy have shown improved tolerability compared to twice-weekly regimens, while maintaining efficacy—even in difficult-to-treat populations such as TCR or BCMA-refractory MM. We have reviewed clinical trial data supporting the use of lower dose weekly selinexor to maintain efficacy while lowering toxicity. Whether a lower starting dose of selinexor is more effective than higher doses remains to be tested in prospective randomized trials or pharmacokinetic simulation models.
In the BOSTON trial, patients who had a dose reduction had longer PFS, DOR, and time-to-next-treatment, reduced rates of AEs, and improved QoL, suggesting that a strategic dose reduction could optimize selinexor treatment in patients with RRMM (18). Similarly, a retrospective observational study showed that patients with RRMM receiving selinexor-based regimens administered with a lower starting dose and antiemetic support had reduced treatment failure, longer treatment duration, and fewer dose-related toxicities (45). In the STOMP study, lower-dose selinexor maintained anti-MM activity with manageable toxicity, even in heavily pretreated patients.
Spearheaded by anti-CD38 mAbs and the anticipated transition of novel therapies including BCMA targeting CAR-T and bispecifics into earlier treatment lines, patients may be TCR after only a few lines of treatment. Additionally, anti-BCMA refractory MM represents an emerging niche where novel mechanisms of action may provide clinical value. Phase 3 trials enriched for these patients are needed to gain appropriate insights into the sequencing of therapies. The EMN29 study (NCT05028348) is evaluating the SPd-40 triplet in TCE MM with progression of disease after an anti-CD38 antibody in the immediate prior line of treatment. Given that both selinexor and a cereblon E3 ligase modulator such as mezigdomide impact T-cell fitness and support T-cell health) an additional arm of the STOMP trial is underway to evaluate the all-oral triplet combination of selinexor, mezigdomide, and dexamethasone in patients with RRMM who have progressed after either bispecific or CAR-T therapy.
5 Conclusions
Most anti-tumor therapies undergo an evolution as experience grows in dosing and schedule - Selinexor is no exception from this posology refinement. S-containing triplets with weekly administration schedules delivered have showed reduced toxicity profiles, improved tolerance and durability of disease response in difficult to manage patient populations. As such, they represent a proven alternative and/or companion class of agent to PIs, IMiDs, and anti-CD38 monoclonal antibodies in heavily pretreated MM. Anti-tumor activity is observed even at low doses of weekly S-containing triplets, where the toxicities of a combination therapy do not exacerbate the AEs expected with the partner drug in a combination. Further research in strategic therapeutic sequencing of selinexor in rational combinations with other classes of anti-MM agents with a focus on optimizing T-cell fitness may facilitate our ability to achieve even better outcomes in multi-class RRMM, which remains area of unmet need.
Author contributions
MB: Writing – original draft, Writing – review & editing, Formal analysis, Investigation, Visualization, Data curation, Conceptualization. GS: Writing – review & editing, Writing – original draft. TM: Writing – original draft, Writing – review & editing. DV: Writing – review & editing, Formal analysis, Writing – original draft. CG: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was supported by research funding from Karyopharm Therapeutics, Inc.
Acknowledgments
JetPub Scientific Communications LLC, supported by Karyopharm Therapeutics, assisted in the preparation of this manuscript.
Conflict of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: MB has worked for an independent review committee for Parexel; advisory boards for Janssen Research, BMS/Celgene, Sanofi-Genzyme, and Pfizer; and consulting for Pfizer and AbbVie. TM and DV are employees of Karyopharm Therapeutics Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor GM declared a past co-authorship with the author CG.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Weber D. Thalidomide and its derivatives: new promise for multiple myeloma. Cancer Control. (2003) 10:375–83. doi: 10.1177/107327480301000504
2. Richardson PG, Barlogie B, Berenson J, Singhal S, Jagannath S, Irwin D, et al. A phase 2 study of bortezomib in relapsed, refractory myeloma. New Engl J Med. (2003) 348:2609–17. doi: 10.1056/nejmoa030288
3. Richardson P. Management of the relapsed/refractory myeloma patient: strategies incorporating lenalidomide. Semin Hematol. (2005) 42:S9–15. doi: 10.1053/J.SEMINHEMATOL.2005.10.004
4. Richardson PG, Blood E, Mitsiades CS, Jagannath S, Zeldenrust SR, Alsina M, et al. A randomized phase 2 study of lenalidomide therapy for patients with relapsed or relapsed and refractory multiple myeloma. Blood. (2006) 108:3458–64. doi: 10.1182/BLOOD-2006-04-015909
5. Dimopoulos MA, Chen C, Spencer A, Niesvizky R, Attal M, Stadtmauer EA, et al. Long-term follow-up on overall survival from the MM-009 and MM-010 phase III trials of lenalidomide plus dexamethasone in patients with relapsed or refractory multiple myeloma. Leukemia. (2009) 23:2147–52. doi: 10.1038/LEU.2009.147
6. Siegel DS, Martin T, Wang M, Vij R, Jakubowiak AJ, Lonial S, et al. A phase 2 study of single-agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma. Blood. (2012) 120:2817. doi: 10.1182/BLOOD-2012-05-425934
7. Richardson PG, Siegel DS, Vij R, Hofmeister CC, Baz R, Jagannath S, et al. Pomalidomide alone or in combination with low-dose dexamethasone in relapsed and refractory multiple myeloma: a randomized phase 2 study. Blood. (2014) 123:1826–32. doi: 10.1182/BLOOD-2013-11-538835
8. Usmani SZ, Weiss BM, Plesner T, Bahlis NJ, Belch A, Lonial S, et al. Clinical efficacy of daratumumab monotherapy in patients with heavily pretreated relapsed or refractory multiple myeloma. Blood. (2016) 128:34–44. doi: 10.1182/BLOOD-2016-03-705210
9. Chari A, Vogl DT, Gavriatopoulou M, Nooka AK, Yee AJ, Huff CA, et al. Oral selinexor–dexamethasone for triple-class refractory multiple myeloma. New Engl J Med. (2019) 381:727–38. doi: 10.1056/nejmoa1903455
10. Karyopharm Therapeutics Inc. XPOVIO® (selinexor), package insert (2022). Available online at: https://www.karyopharm.com/wp-content/uploads/2019/07/NDA-212306-SN-0071-Prescribing-Information-01July2019.pdf (Accessed March 20, 2022).
11. Lonial S, Lee HC, Badros A, Trudel S, Nooka AK, Chari A, et al. Longer term outcomes with single-agent belantamab mafodotin in patients with relapsed or refractory multiple myeloma: 13-month follow-up from the pivotal DREAMM-2 study. Cancer. (2021) 127:4198–212. doi: 10.1002/CNCR.33809
12. Grosicki S, Simonova M, Spicka I, Pour L, Kriachok I, Gavriatopoulou M, et al. Once-per-week selinexor, bortezomib, and dexamethasone versus twice-per-week bortezomib and dexamethasone in patients with multiple myeloma (BOSTON): a randomized, open-label, phase 3 trial. Lancet. (2020) 396:1563–73. doi: 10.1016/S0140-6736(20)32292-3
13. White DJ, Lentzsch S, Gasparetto C, Bahlis N, Chen CI, Lipe BC, et al. Safety and efficacy of the combination of selinexor, lenalidomide and dexamethasone (SRd) in patients with newly diagnosed multiple myeloma. Blood. (2019) 134:3165–5. doi: 10.1182/blood-2019-124370
14. White DJ, LeBlanc R, Baljevic M, Bahlis NJ, Lentzsch S, Venner CP, et al. Selinexor, lenalidomide and dexamethasone (SRd) for patients with relapsed/refractory and newly diagnosed multiple myeloma. Blood. (2020) 136:45–6. doi: 10.1182/BLOOD-2020-140141
15. Gasparetto C, Lentzsch S, Schiller G, Callander N, Tuchman S, Chen C, et al. Selinexor, daratumumab, and dexamethasone in patients with relapsed or refractory multiple myeloma. EJHaem. (2021) 2:56–65. doi: 10.1002/JHA2.122
16. White D, Schiller GJ, Madan S, Lentzsch S, Chubar E, Lavi N, et al. Efficacy and safety of once weekly selinexor 40 mg versus 60 mg with pomalidomide and dexamethasone in relapsed and/or refractory multiple myeloma. Front Oncol. (2024) 14:1352281. doi: 10.3389/fonc.2024.1352281
17. Nooka AK, Costa LJ, Gasparetto CJ, Richardson PG, Siegel DS, Chari A, et al. Guidance for use and dosing of selinexor in multiple myeloma in 2021: consensus from international myeloma foundation expert roundtable. Clin Lymphoma Myeloma Leuk. (2022) 22:e526–31. doi: 10.1016/j.clml.2022.01.014
18. Jagannath S, Delimpasi S, Grosicki S, Van Domelen DR, Bentur OS, Špička I, et al. Association of selinexor dose reductions with clinical outcomes in the BOSTON study. Clin Lymphoma Myeloma Leuk. (2023) 23:917–923.e3. doi: 10.1016/j.clml.2023.08.018
19. Dimopoulos M, Quach H, Mateos MV, Landgren O, Leleu X, Siegel D, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): results from a randomized, multicenter, open-label, phase 3 study. Lancet. (2020) 396:186–97. doi: 10.1016/S0140-6736(20)30734-0
20. Richardson PG, Oriol A, Beksac M, Liberati AM, Galli M, Schjesvold F, et al. Pomalidomide, bortezomib, and dexamethasone for patients with relapsed or refractory multiple myeloma previously treated with lenalidomide (OPTIMISMM): a randomized, open-label, phase 3 trial. Lancet Oncol. (2019) 20:781–94. doi: 10.1016/S1470-2045(19)30152-4
21. Gasparetto C, Schiller GJ, Tuchman SA, Callander NS, Baljevic M, Lentzsch S, et al. Once weekly selinexor, carfilzomib and dexamethasone in carfilzomib non-refractory multiple myeloma patients. Br J Cancer. (2022) 126:718–25. doi: 10.1038/S41416-021-01608-2
22. Schiller GJ, Lipe BC, Bahlis NJ, Tuchman SA, Bensinger WI, Sutherland HJ, et al. Selinexor-based triplet regimens in patients with multiple myeloma previously treated with anti-CD38 monoclonal antibodies. Clin Lymphoma Myeloma Leuk. (2023) 23:e286–e296.e4. doi: 10.1016/J.CLML.2023.06.001
23. Baljevic M, Gasparetto C, Schiller GJ, Tuchman SA, Callander NS, Lentzsch S, et al. Selinexor-based regimens in patients with multiple myeloma after prior anti-B-cell maturation antigen treatment. EJHaem. (2022) 3:1270–6. doi: 10.1002/JHA2.572
24. Gandhi UH, Cornell RF, Lakshman A, Gahvari ZJ, McGehee E, Jagosky MH, et al. Outcomes of patients with multiple myeloma refractory to CD38-targeted monoclonal antibody therapy. Leukemia. (2019) 33:2266–75. doi: 10.1038/s41375-019-0435-7
25. Anderson Larry D Jr, Munshi NC, Shah N, Jagannath S, Berdeja JG, Lonial S, et al. Idecabtagene vicleucel (ide-cel, bb2121), a BCMA-directed CAR T cell therapy, in relapsed and refractory multiple myeloma: Updated KarMMa results. J Clin Oncol. (2021) 39:8016. doi: 10.1200/JCO.2021.39.15_suppl.8016
26. Lin Y, Martin TG, Usmani SZ, Berdeja JG, Jakubowiak AJ, Agha ME, et al. CARTITUDE-1 final results: Phase 1b/2 study of ciltacabtagene autoleucel in heavily pretreated patients with relapsed/refractory multiple myeloma. J. Clin. Oncol. (2023) 41:8009–9. doi: 10.1200/JCO.2023.41.16_SUPPL.8009
27. Martin T, Usmani SZ, Berdeja JG, Jakubowiak A, Agha M, Cohen AD, et al. Updated results from CARTITUDE-1: phase 1b/2Study of ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T cell therapy, in patients with relapsed/refractory multiple myeloma. Blood. (2021) 138:549–9. doi: 10.1182/BLOOD-2021-146060
28. Costello CL, Cohen AD, Patel KK, Ali SS, Berdeja JG, Shah N, et al. Phase 1/2 study of the safety and response of P-BCMA-101 CAR-T cells in patients with relapsed/refractory (r/r) multiple myeloma (MM) (PRIME) with novel therapeutic strategies. Blood. (2020) 136:29–30. doi: 10.1182/BLOOD-2020-142695
29. Moreau P, Garfall AL, van de Donk NWCJ, Nahi H, San-Miguel JF, Oriol A, et al. Teclistamab in relapsed or refractory multiple myeloma. N Engl J Med. (2022) 387:495–505. doi: 10.1056/NEJMOA2203478
30. Bahlis NJ, Raje NS, Costello C, Dholaria BR, Solh MM, Levy MY, et al. Efficacy and safety of elranatamab (PF-06863135), a B-cell maturation antigen (BCMA)-CD3 bispecific antibody, in patients with relapsed or refractory multiple myeloma (MM). J Clin Oncol. (2021) 39:8006–6. doi: 10.1200/JCO.2021.39.15_SUPPL.8006
31. Minnema MC, Krishnan AY, Berdeja JG, Rocafiguera AO, van de Donk NWCJ, Rodríguez-Otero P, et al. Efficacy and safety of talquetamab, a G protein-coupled receptor family C group 5 member D x CD3 bispecific antibody, in patients with relapsed/refractory multiple myeloma (RRMM): Updated results from MonumenTAL-1. J. Clin. Oncol. (2022) 40:8015–5. doi: 10.1200/JCO.2022.40.16_SUPPL.8015
32. Cohen A, Harrison S, Krishnan A, Fonseca R, Forsberg P, and Spencer A. Initial clinical activity and safety of BFCR4350A, a fcRH5/CD3 T-cell-engaging bispecific antibody. In: Relapsed/Refractory Multiple Myeloma, Blood (2020) 136(Supplement 1):42–43. doi: 10.1182/blood-2020-136985
33. Madduri D, Rosko A, Brayer J, Zonder J, Bensinger WI, and Li J. REGN5458, a BCMA x CD3 Bispecific Monoclonal Antibody, Induces Deep and Durable Responses in Patients with Relapsed/Refractory Multiple Myeloma (RRMM), Blood. (2020) 136, (Supplement 1):41–42. doi: 10.1182/blood-2020-139192
34. D’Souza A, Shah N, Rodriguez C, Voorhees PM, Weisel K, Bueno OF, et al. A phase I first-in-human study of ABBV-383, a B-cell maturation antigen × CD3 bispecific T-cell redirecting antibody, in patients with relapsed/refractory multiple myeloma. J Clin Oncol. (2022) 40:3576–86. doi: 10.1200/JCO.22.01504
35. Chen W, Fu C, Fang B, Liang A, Xia Z, He Y, et al. Phase II Study of fully human BCMA-targeting CAR-T cells (Zevorcabtagene autoleucel) in patients with relapsed/refractory multiple myeloma. Blood. (2022) 140:4564–5. doi: 10.1182/BLOOD-2022-168610
36. Frigault M, Rosenblatt J, Dhakal B, Raje N, Cook D, Gaballa MR, et al. Phase 1 study of CART-ddbcma for the treatment of subjects with relapsed and/or refractory multiple myeloma. Blood. (2022) 140:7439–40. doi: 10.1182/BLOOD-2022-163827
37. Bumma N, Richter J, Jagannath S, Lee HC, Hoffman JE, Suvannasankha A, et al. Linvoseltamab for treatment of relapsed/refractory multiple myeloma. J Clin Oncol. (2024) 42:2702–12. doi: 10.1200/JCO.24.01008
38. Sperling AS, Derman BA, Nikiforow S, Im S-Y, Ikegawa S, Prabhala RH, et al. Updated phase I study results of PHE885, a T-Charge manufactured BCMA-directed CAR-T cell therapy, for patients (pts) with r/r multiple myeloma (RRMM). J Clin Oncol. (2023) 41:8004–4. doi: 10.1200/JCO.2023.41.16_SUPPL.8004
39. San-Miguel J, Dhakal B, Yong K, Spencer A, Anguille S, Mateos M-V, et al. Cilta-cel or standard care in lenalidomide-refractory multiple myeloma. New Engl J Med. (2023) 389:335–47. doi: 10.1056/NEJMOA2303379
40. Dytfeld D, Dhakal B, Agha M, Manier S, Delforge M, Kuppens S, et al. Bortezomib, lenalidomide and dexamethasone (VRd) followed by ciltacabtagene autoleucel versus vrd followed by lenalidomide and dexamethasone (Rd) maintenance in patients with newly diagnosed multiple myeloma not intended for transplant: A randomized, phas. Blood. (2021) 138:1835–5. doi: 10.1182/blood-2021-146210
41. Colley A, Brauns T, Sluder AE, Poznansky MC, and Gemechu Y. Immunomodulatory drugs: a promising clinical ally for cancer immunotherapy. Trends Mol Med. (2024) 30:765–80. doi: 10.1016/J.MOLMED.2024.05.001
42. Dima D, Rossi A, Costa B, Mark T, Ijioma S, Ray D, et al. P-408 survival analysis of selinexor-exposed relapsed/refractory multiple myeloma (RRMM) treated with chimeric antigen receptor T-cell (CAR-T) therapy: A real-world exploratory analysis. Clin Lymphoma Myeloma Leuk. (2024) 24:S270. doi: 10.1016/S2152-2650(24)02310-3
43. Afrough A, Hashmi H, Hansen DK, Sidana S, Ahn C, Peres LC, et al. Real-world impact of bridging therapy on outcomes of ide-cel for myeloma in the U.S. Myeloma Immunotherapy Consortium. Blood Cancer J. (2024) 14:1–5. doi: 10.1038/s41408-024-00993-0
44. Chari A, Vogl DT, Jagannath S, Jasielec J, Unger TJ, DeCastro A, et al. Selinexor-based regimens for the treatment of myeloma refractory to chimeric antigen receptor T cell therapy. Br J Hematol. (2020) 189:e126–30. doi: 10.1111/bjh.16550
Keywords: selinexor, multiple myeloma, drug administration schedules, exportin 1, antagonists, inhibitors, combination drug therapy, clinical efficacy
Citation: Baljevic M, Schiller G, Mark TM, Van Domelen DR and Gasparetto C (2025) Lower dose and weekly schedules of selinexor in multiple myeloma - updated evidence on safety and efficacy. Front. Oncol. 15:1649493. doi: 10.3389/fonc.2025.1649493
Received: 18 June 2025; Accepted: 22 August 2025;
Published: 22 September 2025.
Edited by:
Gabor Mikala, Central Hospital of Southern Pest, HungaryReviewed by:
Gergely Varga, Semmelweis University, HungaryCopyright © 2025 Baljevic, Schiller, Mark, Van Domelen and Gasparetto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muhamed Baljevic, bXVoYW1lZC5iYWxqZXZpY0B2dW1jLm9yZw==
 Muhamed Baljevic
Muhamed Baljevic Gary Schiller
Gary Schiller Tomer M. Mark3
Tomer M. Mark3