- 1Department of Urology, Bichat Claude-Bernard Hospital, Assistance Publique -Hôpitaux de Paris Nord, University Paris Cité, Paris, France
- 2Department of Urology, Comprehensive Cancer Center, Medical University of Vienna, Vienna, Austria
- 3Sorbonne University, groupe recherche clinique (GRC) 5 Predictive Onco-Urology, Assistance publique des hôpitaux de Paris (AP-HP), Urology, Pitié-Salpêtrière Hospital, Paris, France
- 4Department of Urology, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Background: Robot-assisted radical nephroureterectomy (RARNU), performed via either a multiport or single-port approach through transperitoneal or retroperitoneal routes, is an increasingly utilized surgical method for patients with upper tract urothelial carcinoma.
Materials and methods: A collaborative review of the literature available on Medline was conducted to report the perioperative outcomes of multiport or single-port, transperitoneal or retroperitoneal RARNU. A total of 31 references published between 2006 and 2023 were included.
Results: The multiport transperitoneal robotic approach has been documented in 23 studies including between 10 and 3774 RARNU. Operative times ranged from 157 to 326 minutes, intraoperative complication rates from 0% to 7.3%, estimated blood loss from 68.9 mL to 380 mL and blood transfusion rates from 1.4% to 22.7%. Overall postoperative complication ranged from 11.9% to 43.8%, with major complications occurring in 0% to 15.1% of cases. Additionally, the length of hospital stay ranged from 2.3 to 10.3 days. The single-port transperitoneal robotic approach has been documented in 3 studies including between 1 and 12 RANU. Operative time ranged from 160 to 240 minutes, with 17% of patients requiring transfusions. The length of stay varied between 3 and 7 days. Finally, five retrospective studies, including between 2 and 12 patients treated with multiport retroperitoneal RARNU and between 2 and 20 patients with single-port retroperitoneal RARNU were reported, also with satisfactory results.
Conclusion: Although prospective comparative studies are needed to confirm these results, RARNU approach, whether single-port or multi-port, transperitoneal or retroperitoneal, appears promising and safe.
Introduction
Upper tract urothelial carcinoma (UTUC) represents 5-10% of all urothelial cancers (1). Although kidney-sparing surgery emerged for selected patients with low-risk UTUC, radical nephroureterectomy (RNU) with bladder cuff excision (BCE) remains the standard treatment for those with high-risk disease (2). Historically, the open approach has been considered as the standard for RNU due to the technical challenges in accessing the kidney, ureter, and bladder, but it was associated with significant postoperative morbidity (3). Thus, laparoscopic RNU was introduced in 1991 to enhance perioperative outcomes (4). Specifically, the use of laparoscopic RNU has been shown to decrease the risk of postoperative complication and the length of stay as compared to open procedures (5), with similar oncological outcomes in several retrospective studies (6, 7). However, the complexity of laparoscopic instrumentation and the steep learning curve associated with laparoscopic BCE have prevented this technique from being widely accepted by the urological community (8).
More recently, with the increasing adoption of robotic surgery in urological cancer (9), the use of the robotic approach has been proposed to facilitate distal ureter management (10). Since, multiport or single-port, transperitoneal or retroperitoneal robot-assisted radical nephroureterectomy (RARNU) emerged as the new standard of care for patients with high-risk UTUC (11, 12). Against this backdrop, we aimed to report the latest available evidence, with a focus on perioperative outcomes, of multiport or single-port RARNU using either a transperitoneal or retroperitoneal approach for patients with UTUC.
Materials and methods
This collaborative narrative review was conducted using two separate online search engines, PubMed and Google Scholar, to identify relevant literature regarding RARNU in UTUC patients. In our research, we employed the following keywords either individually or in combination “robotic”; “radical nephroureterectomy”; “multiport”; “single-port”; “transperitoneal”; “retroperitoneal”. Articles were assessed for their relevance and methodology without any time restriction by three authors (PEG, JPS and EX). We focused exclusively on the perioperative outcomes of these four techniques, excluding oncologic results. RARNUs, with or without bladder cuff excision, were included in our review. This research excluded non-English literature, animal studies and correspondence/letters. Given the lack of available data, small series were also included in this review. In total, 31 references published between 2006 and 2023 were included in our result section.
Results
Transperitoneal RARNU
Multiport transperitoneal RARNU
The perioperative outcomes of the multiport transperitoneal RARNU approach have been documented in 23 studies, including between 10 to 3,774 patients (10, 13–34); Table 1. Regarding operative time, 18 studies (10, 13–17, 23–34) reported a mean/median duration between 157 and 326 minutes. Intraoperative complications, documented in 7 studies (10, 13, 14, 16, 18, 32, 34), ranged from 0% to 7.3%. Estimated blood loss was reported to be between 68.9 mL and 380 mL across 17 studies (10, 13–17, 24–34). Blood transfusion rates varied from 1.4% to 22.7% in 8 studies (10, 13, 15, 16, 21, 28, 31, 33). Overall postoperative complication rates ranged from 11.9% to 43.8% (10, 13–18, 21, 23, 28–30, 32–34), while major complications were reported between 0% and 15.1% (10, 13–17, 20, 23, 28, 29, 32–34). Additionally, length of hospital stay was reported in 21 studies, with durations ranging from 2.3 to 10.3 days (10, 13–22, 24, 26–34).
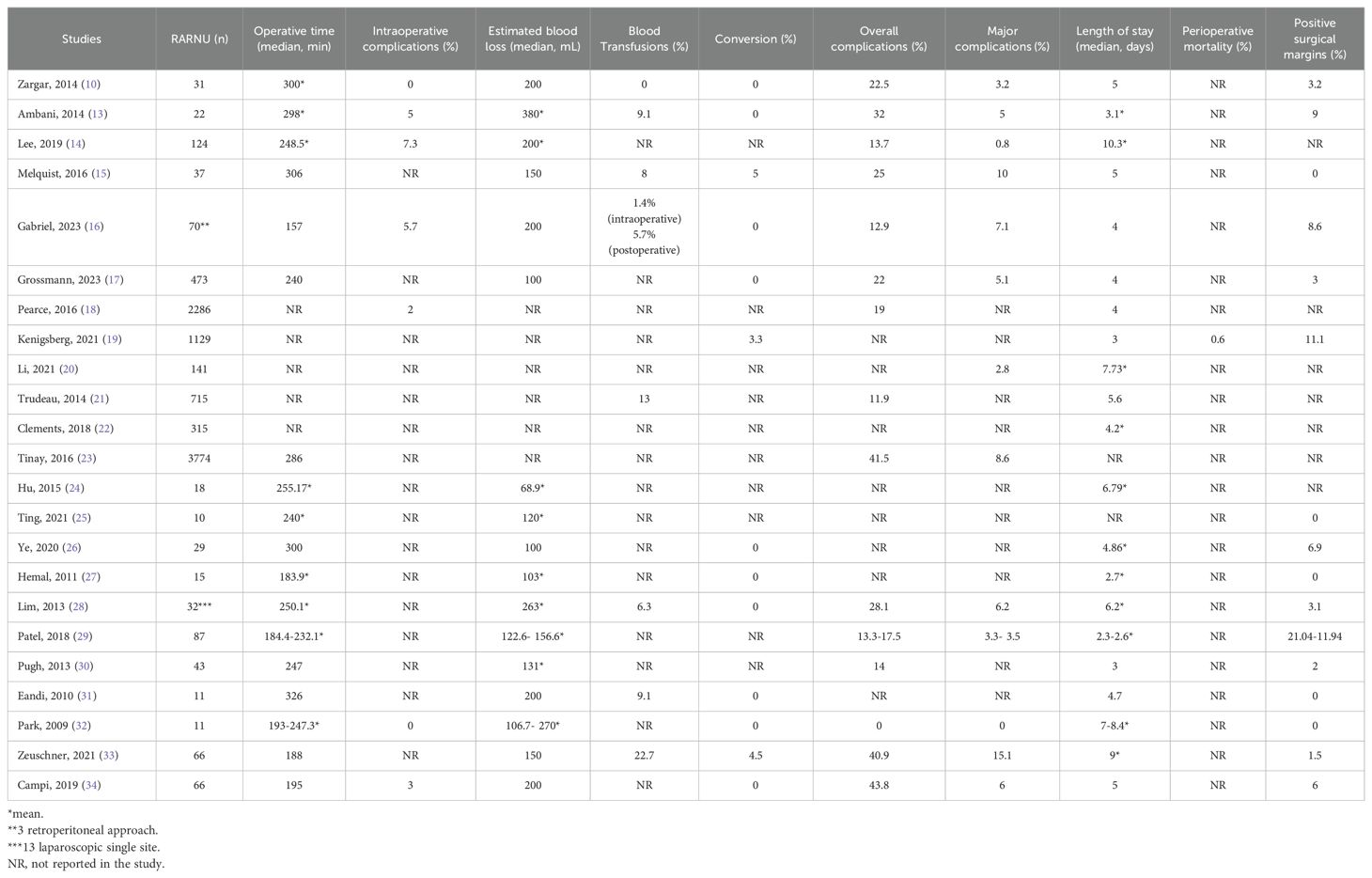
Table 1. Perioperative results of transperitoneal multiport robot assisted radical nephroureterectomy.
Single-port transperitoneal RARNU
The single-port transperitoneal robotic approach has been documented in 3 studies including between 1 and 12 RANU (Table 2). Lee et al. reported satisfactory perioperative outcomes in a retrospective cohort of 68 patients who underwent robot-assisted surgery using a single-port technique, including 12 RARNU procedures. The mean operative time was 227 minutes, with an estimated blood loss of 248 mL, a perioperative transfusion rate of 17%, and a mean hospital stay of 4 days (35). Additionally, Kim et al. share their experience with single-port robotic surgery performed by a single surgeon in a second retrospective study. Among 120 urological procedures, 5 patients underwent transperitoneal single-port RARNU. In this study, the operative time ranged from 160 to 240 minutes, blood loss between 100 and 200 mL, and hospital stay varied from 3 to 7 days (36). Finally, Abaza et al. describe, in a third retrospective study from 2021, their first 100 single-port robotic surgeries, including 59 prostatectomies, 18 partial nephrectomies, 12 pyeloplasties, 4 nephrectomies, 4 adrenalectomies, 2 partial cystectomies, and 1 transperitoneal RNU. Although specific perioperative outcomes for UTUC are not detailed, the overall results were promising, highlighting the feasibility and potential benefits of a single-port approach (37).
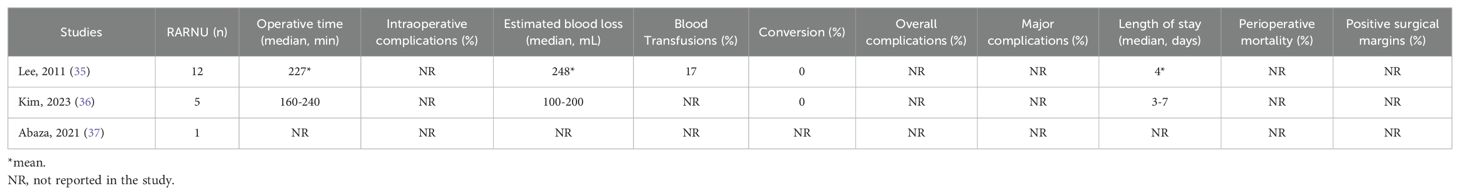
Table 2. Perioperative results of transperitoneal single-port robot assisted radical nephroureterectomy.
Retroperitoneal RARNU
While the transperitoneal approach remains the traditional route (3), there is increasing interest in the retroperitoneal approach for RARNU due to its potential benefits. Thus, Sparwasser et al. conducted in 2023 the first direct comparison between retroperitoneal and transperitoneal RARNU. The analysis included perioperative patient data from 24 transperitoneal RNU and 12 retroperitoneal RNU cases. While intraoperative (16.4% vs 0%, p = 0.35) and postoperative (25% vs 12.5%, p = 0.64) complications showed no significant differences, retroperitoneal route was significantly associated with reduced surgery time (p < 0.05) and shorter length of stay (p < 0.05) compared to transperitoneal RNU (38). Regarding the surgical technique, retroperitoneal RNU has been described using both multiport and single-port robotic techniques.
Multiport retroperitoneal RARNU
To date, there have been very few reported cases of complete RARNU with BCE using the multiport retroperitoneal approach (Table 3). In 2006, Rose et al. reported in a retrospective study the first experience including 2 patients treated by robotic retroperitoneoscopic RNU using the Da Vinci Surgical System. Both procedures were successfully completed with the robot without conversion. Mean operative time was 182.5 min and estimated blood loss was 75 ml. In this study, postoperative recovery was uneventful (39). More recently, a retrospective analysis reported five patients who underwent RARNU with BCE exclusively within the retroperitoneal space. In this study, UTUC was localized to the distal ureter in two cases and to the kidney in three. None of the patients with UTUC had positive surgical margins. Regarding perioperative outcomes, no intraoperative adverse events of grade ≥2 were reported, and the median estimated blood loss was 150 ml. Additionally, no patients experienced postoperative complications classified as Clavien–Dindo grade ≥ 3a. The median hospital stay was 5.4 days, with no readmissions within 30 days. It is worth mentioning that the authors noted that intraoperative redocking was required for managing the distal ureter, which took 7 minutes (40). Finally, Sparwasser et al. reported a series of 12 RARNU. In the study, the mean operative time was 192 minutes, with a perioperative transfusion rate of 8.3%, and a mean hospital stay of 5.75 days (38).
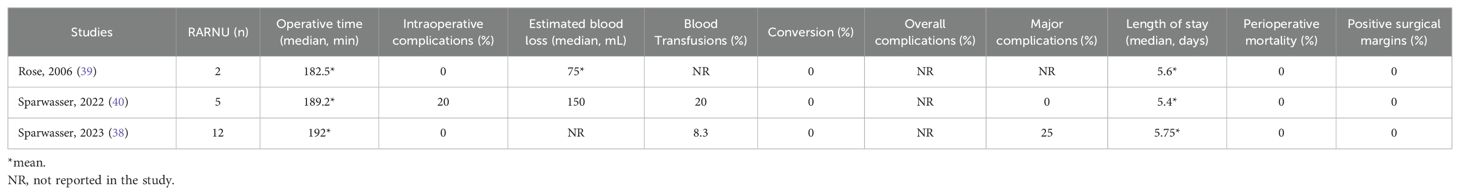
Table 3. Perioperative results of retroperitoneal multiport robot assisted radical nephroureterectomy.
Single-port retroperitoneal RARNU
Currently, there is also limited literature on RNU with BCE using the single-port robotic system, and the available studies involve a small number of patients (Table 4). Thus, in 2023, Pellegrino et al. presented results for 18 patients treated using a supine anterior retroperitoneal access technique with the da Vinci Single-Port robotic platform, which included 2 RNU with BCE. The findings suggested that this approach was feasible and safe, with low complication rates, reduced postoperative pain, and earlier discharge (41). Additionally, Bang et al. reported perioperative outcomes in 20 patients who underwent single-port RARNU with BCE. In this retrospective study, the median console time was 106 minutes and 40 seconds, with expected blood loss of 122.50 ± 75.18 mL. Postoperative outcomes were also satisfactory, as none of these 20 patients experienced complications according to the Clavien-Dindo scale (42).
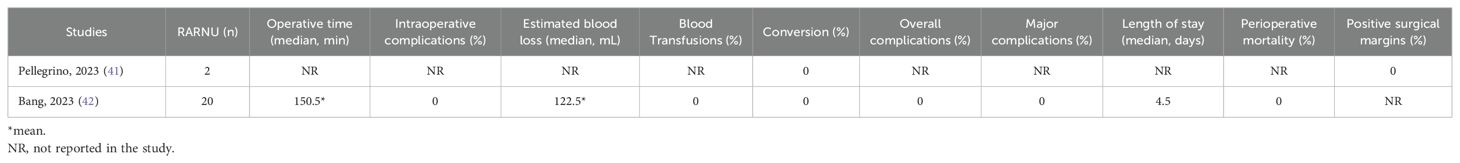
Table 4. Perioperative results of retroperitoneal single-port robot assisted radical nephroureterectomy.
Discussion
Given the widespread adoption of robotic in the surgical management of urological cancers, we compiled in this narrative review the perioperative results of multiport transperitoneal RARNU. We also incorporated data on single-port transperitoneal procedures and retroperitoneal techniques (both multiport and single-port). Overall, our analysis shows that the multiport transperitoneal approach is well documented and associated with satisfactory perioperative outcomes, supporting its large-scale adoption compared to laparoscopic techniques. These findings are further supported by comparative analyses. The perioperative outcomes of multiport transperitoneal RARNU have been compared to those of laparoscopic RNU in a recent meta-analysis and systematic review. Thus, O’Sullivan et al., reported in a meta-analysis including 10 studies and employing the fixed-effects model of Mantel-Haenszel no significant difference between the two techniques in terms of overall postoperative morbidity, including major complications, operative time, estimated blood loss, intraoperative complications, and postoperative surgical margins. However, a slight reduction in length of stay and perioperative mortality was observed in favor of the RARNU group (43). Additionally, a systematic review including a total of 8,470 patients who underwent RARNU and 19,872 patients who underwent laparoscopic RNU analyzed data from 12 comparative original studies. Although the robotic procedure was linked to a longer operative time, the results indicated that it was associated with fewer overall complications and a shorter hospital stay compared to laparoscopic RNU (44).
With regards to other robotic techniques, the currently available data consist only of a few small retrospective series. Compared to transperitoneal multiport RARNU, the transperitoneal single-port route has also demonstrated satisfactory perioperative outcomes, with the potential advantage of reducing postoperative pain due to the single incision and facilitating early discharge. The retroperitoneal approach, whether multiport or single-port, may be a preferable option for patients with a history of abdominal surgery to avoid intraperitoneal adhesions (45). However, the difficulty of this access route lies in working within a confined space, which significantly limits the triangulation of multiport instruments and dexterity (46). Moreover, a major hurdle to this approach is the challenge of instrument placement and the potential conflicts that may arise, making the procedure complex and difficult to replicate (41). In any case, the optimal approach needs to be adapted to each patient, and the choice must take into account the medical history, the tumor characteristics, and the surgical expertise.
In addition to perioperative benefits, the robotic approach offers several advantages for both the surgeon and the procedure, including enhanced ergonomics, greater precision, elimination of tremors, the ability to operate in 3D vision, and increased degrees of freedom in instrument mobility, enabling fine and accurate movements (47). These features may contribute to better oncological outcomes and account for the satisfactory perioperative results reported in this review. With regards to the surgical procedure, the robotic approach simplifies endoscopic excision of the bladder cuff, whereas laparoscopic procedures often require an iliac incision. In fact, a multicenter study involving data from 17 centers and 276 patients (185 robotic, 91 laparoscopic) demonstrated that patients undergoing RARNU were significantly more likely to have BCE endoscopically (81% vs. 63.7%, P = 0.003), providing strong evidence in favor of promoting robotic surgery for the management of RNU (48).
Regarding oncological outcomes, several previous studies investigated the impact of the surgical RNU approaches on survival outcomes and found similar progression-free survival (PFS), cancer-specific survival (CSS), and overall survival (OS) among the three approaches (open, laparoscopic and multiport transperitoneal robotic), despite variations in statistical methods, cohort sizes, and study designs (14, 17, 22, 49). Additionally, the most recent meta-analysis by Vecchia et al., which investigated the effect of the surgical technique on PFS and CSS in approximately 87,000 patients, observed no significant difference (12). However, the primary concern with the robotic approach relates to the risk of intravesical recurrence. In fact, Grossmann et al. reported in a recent multicenter study, which involved 756 patients and used propensity score matching, that although Kaplan–Meier and log-rank analyses found similar RFS, CSS, and OS across transperitoneal multiport RARNU, LRNU, and ORNU groups, the intravesical RFS was significantly higher with open surgery. Additionally, using multivariable regression analyses, LRNU and RARNU were independently associated with worse intravesical RFS (HR 1.66, 95% CI 1.22–2.28, p = 0.001 and HR 1.73, 95%CI 1.22–2.47, p = 0.002, respectively) (17). Thus, the latest EAU guidelines advise caution, given the potentially higher risk of intravesical recurrence associated with both laparoscopic and robotic RNU compared to the open approach (2). However, further comparative studies are needed to confirm this precaution.
Finally, beyond perioperative and oncological outcomes, cost considerations remain another key factor influencing the widespread adoption of robotic surgery. Although the initial costs for acquiring and maintaining robotic systems are substantial, some indirect benefits—such as shorter hospital stays and fewer complications (43, 44)—may help offset these expenses. However, a recent study by Di Bello et al., including 1,138 RNU procedures, found that RARNU was significantly associated with higher hospital costs compared to open surgery ($64,761 vs. $54,768, p<0.001). Additionally, even after adjusting for multiple variables, RARNU remained an independent predictor of increased hospital costs (HR: 1.13; P<0.001), which likely represents the main obstacle to its large-scale implementation (50). However, the widespread adoption of robotic procedures across all surgical specialties, as well as the entry of new competitors and the standardization of consumables, are expected to further reduce the overall costs of these procedures.
As a narrative review, our report has certain limitations, including reliance on retrospective studies, heterogeneity in study designs and outcome measures, and small sample sizes in certain surgical approaches. Future research is needed to better evaluate and compare these four techniques, particularly through multicenter prospective studies assessing long-term oncologic outcomes, as well as cost-effectiveness analyses and the impact on patient quality of life associated with the use of these new approaches.
Conclusion
This narrative review compiled the perioperative outcomes of RARNU performed via transperitoneal or retroperitoneal approaches, using either single-port or multi-port techniques in patients with UTUC. We found that the multi-port transperitoneal technique is well-documented, safe, and should be part of the surgical arsenal for high-risk UTUC patients. Regarding the single-port transperitoneal approach and the retroperitoneal approach with either single-port or multi-port techniques, the current number of available studies is limited. Further research involving a larger number of patients is needed to better assess these surgical options.
Author contributions
P-EG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. SS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing. MR: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Writing – review & editing. JS: Conceptualization, Data curation, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. EX: Conceptualization, Data curation, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Soria F, Shariat SF, Lerner SP, Fritsche HM, Rink M, Kassouf W, et al. Epidemiology, diagnosis, preoperative evaluation and prognostic assessment of upper-tract urothelial carcinoma (UTUC). World J Urol. (2017) 35:379−87. doi: 10.1007/s00345-016-1928-x
2. Masson-Lecomte A, Birtle A, Pradere B, Capoun O, Compérat E, Domínguez-Escrig JL, et al. European association of urology guidelines on upper urinary tract urothelial carcinoma: summary of the 2025 update. Eur Urol. (2025) 87(6):697–716. doi: 10.1016/j.eururo.2025.02.023
3. Barton GJ, Tan WP, and Inman BA. The nephroureterectomy: a review of technique and current controversies. Transl Androl Urol. (2020) 9:3168−90. doi: 10.21037/tau.2019.12.07
4. Clayman RV, Kavoussi LR, Figenshau RS, Chandhoke PS, and Albala DM. Laparoscopic nephroureterectomy: initial clinical case report. J Laparoendosc Surg. (1991) 1:343−9. doi: 10.1089/lps.1991.1.343
5. Correia J, Mendes G, Texeira B, Madanelo M, Fraga A, and Silva-Ramos M. Perioperative and oncological outcomes of laparoscopic and open radical nephroureterectomy for locally advanced upper tract urothelial carcinoma: a single-center cohort study. Cent Eur J Urol. (2022) 75:257−64. doi: 10.5173/ceju.2022.103
6. Peyronnet B, Seisen T, Dominguez-Escrig JL, Bruins HM, Yuan CY, Lam T, et al. Oncological outcomes of laparoscopic nephroureterectomy versus open radical nephroureterectomy for upper tract urothelial carcinoma: an european association of urology guidelines systematic review. Eur Urol Focus. (2019) 5:205−23. doi: 10.1016/j.euf.2017.10.003
7. Piszczek R, Nowak Ł, Krajewski W, Chorbińska J, Poletajew S, Moschini M, et al. Oncological outcomes of laparoscopic versus open nephroureterectomy for the treatment of upper tract urothelial carcinoma: an updated meta-analysis. World J Surg Oncol 21 avr. (2021) 19:129. doi: 10.1186/s12957-021-02236-z
8. Steinberg JR and Matin SF. Laparoscopic radical nephroureterectomy: dilemma of the distal ureter. Curr Opin Urol. (2004) 14:61−5. doi: 10.1097/00042307-200403000-00003
9. Bignante G, Orsini A, Lasorsa F, Lambertini L, Pacini M, Amparore D, et al. Robotic-assisted surgery for the treatment of urologic cancers: recent advances. Expert Rev Med Devices. (2024) 21:1165−77. doi: 10.1080/17434440.2024.2435546
10. Zargar H, Krishnan J, Autorino R, Akca O, Brandao LF, Laydner H, et al. Robotic nephroureterectomy: a simplified approach requiring no patient repositioning or robot redocking. Eur Urol. (2014) 66:769−77. doi: 10.1016/j.eururo.2014.02.060
11. Pellegrino AA, Mima M, and Crivellaro S. Application of the single-port robotic platform during radical nephroureterectomy for upper tract urothelial carcinoma: feasibility of the single-port robot in the multi-quadrant setting. Transl Androl Urol. (2023) 12:1469−74. doi: 10.21037/tau-23-48
12. Veccia A, Antonelli A, Francavilla S, Simeone C, Guruli G, Zargar H, et al. Robotic versus other nephroureterectomy techniques: a systematic review and meta-analysis of over 87,000 cases. World J Urol. (2020) 38:845−52. doi: 10.1007/s00345-019-03020-1
13. Ambani SN, Weizer AZ, Wolf JS, He C, Miller DC, and Montgomery JS. Matched comparison of robotic vs laparoscopic nephroureterectomy: an initial experience. Urology. (2014) 83:345−9. doi: 10.1016/j.urology.2013.07.079
14. Lee H, Kim HJ, Lee SE, Hong SK, and Byun SS. Comparison of oncological and perioperative outcomes of open, laparoscopic, and robotic nephroureterectomy approaches in patients with non-metastatic upper-tract urothelial carcinoma. PloS One. (2019) 14:e0210401. doi: 10.1371/journal.pone.0210401
15. Melquist JJ, Redrow G, Delacroix S, Park A, Faria EE, Karam JA, et al. Comparison of single-docking robotic-assisted and traditional laparoscopy for retroperitoneal lymph node dissection during nephroureterectomy with bladder cuff excision for upper-tract urothelial carcinoma. Urology. (2016) 87:216−23. doi: 10.1016/j.urology.2015.07.070
16. Gabriel PE, Pinar U, Lenfant L, Parra J, Vaessen C, Mozer P, et al. Perioperative, renal function and oncological outcomes of robot-assisted radical nephroureterectomy for patients with upper tract urothelial carcinoma. World J Urol. (2023) 41(11):3001–3007. doi: 10.1007/s00345-023-04590-x
17. Grossmann NC, Soria F, Juvet T, Potretzke AM, Djaladat H, Ghoreifi A, et al. Comparing Oncological and Perioperative Outcomes of Open versus Laparoscopic versus Robotic Radical Nephroureterectomy for the Treatment of Upper Tract Urothelial Carcinoma: A Multicenter, Multinational, Propensity Score-Matched Analysis. Cancers. (2023) 15:1409. doi: 10.3390/cancers15051409
18. Pearce SM, Pariser JJ, Patel SG, Steinberg GD, Shalhav AL, and Smith ND. The effect of surgical approach on performance of lymphadenectomy and perioperative morbidity for radical nephroureterectomy. Urol Oncol mars. (2016) 34:121.e15–21. doi: 10.1016/j.urolonc.2015.09.008
19. Kenigsberg AP, Smith W, Meng X, Ghandour R, Rapoport L, Bagrodia A, et al. Robotic nephroureterectomy vs laparoscopic nephroureterectomy: increased utilization, rates of lymphadenectomy, decreased morbidity robotically. J Endourol. (2021) 35:312−8. doi: 10.1089/end.2020.0496
20. Li CC, Chang CH, Huang CP, Hong JH, Huang CY, Chen IHA, et al. Comparing oncological outcomes and surgical complications of hand-assisted, laparoscopic and robotic nephroureterectomy for upper tract urothelial carcinoma. Front Oncol. (2021) 11:731460. doi: 10.3389/fonc.2021.731460
21. Trudeau V, Gandaglia G, Shiffmann J, Popa I, Shariat SF, Montorsi F, et al. Robot-assisted versus laparoscopic nephroureterectomy for upper-tract urothelial cancer: A population-based assessment of costs and perioperative outcomes. Can Urol Assoc J. (2014) 8:E695–701. doi: 10.5489/cuaj.2051
22. Clements MB, Krupski TL, and Culp SH. Robotic-assisted surgery for upper tract urothelial carcinoma: A comparative survival analysis. Ann Surg Oncol. (2018) 25:2550−62. doi: 10.1245/s10434-018-6557-8
23. Tinay I, Gelpi-Hammerschmidt F, Leow JJ, Allard CB, Rodriguez D, Wang Y, et al. Trends in utilisation, perioperative outcomes, and costs of nephroureterectomies in the management of upper tract urothelial carcinoma: a 10-year population-based analysis. BJU Int. (2016) 117:954−60. doi: 10.1111/bju.13375
24. Hu CY, Yang CK, Huang CY, Ou YC, Hung SF, Chung SD, et al. Robot-assisted laparoscopic nephroureterectomy versus hand-assisted laparoscopic nephroureterectomy for upper urinary tract urothelial carcinoma: A matched comparison study. BioMed Res Int. (2015) 2015:918486. doi: 10.1155/2015/918486
25. Ting HK, Cha TL, Tsai YT, Liu SY, Wu ST, Meng E, et al. Effects of robot-assisted versus hand-assisted nephroureterectomy on circulating tumor cells for upper urinary tract urothelial carcinoma. Sci Rep. (2021) 11:19499. doi: 10.1038/s41598-021-99092-4
26. Ye H, Feng X, Wang Y, Chen R, Zhang C, Zhang W, et al. Single-docking robotic-assisted nephroureterectomy and extravesical bladder cuff excision without intraoperative repositioning: The technique and oncological outcomes. Asian J Surg. (2020) 43:978−85. doi: 10.1016/j.asjsur.2019.11.009
27. Hemal AK, Stansel I, Babbar P, and Patel M. Robotic-assisted nephroureterectomy and bladder cuff excision without intraoperative repositioning. Urology. (2011) 78:357−64. doi: 10.1016/j.urology.2010.12.075
28. Lim SK, Shin TY, Kim KH, Chung BH, Hong SJ, Choi YD, et al. Intermediate-term outcomes of robot-assisted laparoscopic nephroureterectomy in upper urinary tract urothelial carcinoma. Clin Genitourin Cancer. (2013) 11:515−21. doi: 10.1016/j.clgc.2013.04.027
29. Patel MN and Hemal AK. Does advancing technology improve outcomes? Comparison of the da vinci standard/S/si to the xi robotic platforms during robotic nephroureterectomy. J Endourol. (2018) 32:133−8. doi: 10.1089/end.2017.0477
30. Pugh J, Parekattil S, Willis D, Stifelman M, Hemal A, and Su LM. Perioperative outcomes of robot-assisted nephroureterectomy for upper urinary tract urothelial carcinoma: a multi-institutional series. BJU Int. (2013) 112:E295–300. doi: 10.1111/bju.12163
31. Eandi JA, Nelson RA, Wilson TG, and Josephson DY. Oncologic outcomes for complete robot-assisted laparoscopic management of upper-tract transitional cell carcinoma. J Endourol. (2010) 24:969−75. doi: 10.1089/end.2009.0340
32. Park SY, Jeong W, Ham WS, Kim WT, and Rha KH. Initial experience of robotic nephroureterectomy: a hybrid-port technique. BJU Int. (2009) 104:1718−21. doi: 10.1111/j.1464-410X.2009.08671.x
33. Zeuschner P, Vollmer SG, Linxweiler J, Wagenpfeil G, Wagenpfeil S, Saar M, et al. Robot-assisted versus open radical nephroureterectomy for urothelial carcinoma of the upper urinary tract: A retrospective cohort study across ten years. Surg Oncol. (2021) 38:101607. doi: 10.1016/j.suronc.2021.101607
34. Campi R, Cotte J, Sessa F, Seisen T, Tellini R, Amparore D, et al. Robotic radical nephroureterectomy and segmental ureterectomy for upper tract urothelial carcinoma: a multi-institutional experience. World J Urol. (2019) 37:2303−11. doi: 10.1007/s00345-019-02790-y
35. Won Lee J, Arkoncel FRP, Rha KH, Choi KH, Yu HS, Chae Y, et al. Urologic robot-assisted laparoendoscopic single-site surgery using a homemade single-port device: a single-center experience of 68 cases. J Endourol. (2011) 25:1481−5. doi: 10.1089/end.2010.0656
36. Kim KH, Ahn HK, Kim M, and Yoon H. Technique and perioperative outcomes of single-port robotic surgery using the da Vinci SP platform in urology. Asian J Surg. (2023) 46:472−7. doi: 10.1016/j.asjsur.2022.05.128
37. Abaza R, Murphy C, Bsatee A, Brown DH, and Martinez O. Single-port robotic surgery allows same-day discharge in majority of cases. Urology. (2021) 148:159−65. doi: 10.1016/j.urology.2020.08.092
38. Sparwasser P, Frey L, Fischer ND, Thomas A, Dotzauer R, Surcel C, et al. First comparison of retroperitoneal versus transperitoneal robot-assisted nephroureterectomy with bladder cuff: A single center study. Ann Surg Oncol. (2023) 30:4531−9. doi: 10.1245/s10434-023-13363-0
39. Rose K, Khan S, Godbole H, Olsburgh J, Dasgupta P, and GUY’S and St. Thomas’ Robotics Group. Robotic assisted retroperitoneoscopic nephroureterectomy – first experience and the hybrid port technique. Int J Clin Pract. (2006) 60:12−4. doi: 10.1111/j.1368-5031.2006.00703.x
40. Sparwasser P, Epple S, Thomas A, Dotzauer R, Boehm K, Brandt MP, et al. First completely robot-assisted retroperitoneal nephroureterectomy with bladder cuff: a step-by-step technique. World J Urol. (2022) 40:1019−26. doi: 10.1007/s00345-021-03920-1
41. Pellegrino AA, Chen G, Morgantini L, Calvo RS, and Crivellaro S. Simplifying retroperitoneal robotic single-port surgery: novel supine anterior retroperitoneal access. Eur Urol. (2023) 84:223−8. doi: 10.1016/j.eururo.2023.05.006
42. Bang S, Cho HJ, Ha US, Lee JY, and Hong SH. Retroperitoneal single-port robot-assisted nephroureterectomy with bladder cuff excision: initial experience and description of the technique. J Clin Med. (2023) 12:6091. doi: 10.3390/jcm12186091
43. O’Sullivan NJ, Naughton A, Temperley HC, and Casey RG. Robotic-assisted versus laparoscopic nephroureterectomy; a systematic review and meta-analysis. BJUI Compass. (2023) 4:246−55. doi: 10.1002/bco2.208
44. Ji R, He Z, Fang S, Yang W, Wei M, Dong J, et al. Robot-assisted vs. laparoscopic nephroureterectomy for upper urinary tract urothelial carcinoma: a systematic review and meta-analysis based on comparative studies. Front Oncol. (2022) 12:964256. doi: 10.3389/fonc.2022.964256
45. Arora S, Heulitt G, Menon M, Jeong W, Ahlawat RK, Capitanio U, et al. Retroperitoneal vs transperitoneal robot-assisted partial nephrectomy: comparison in a multi-institutional setting. Urology. (2018) 120:131−7. doi: 10.1016/j.urology.2018.06.026
46. Anderson BG, Wright AJ, Potretzke AM, and Figenshau RS. Retroperitoneal access for robotic renal surgery. Int Braz J Urol Off J Braz Soc Urol. (2018) 44:200−1. doi: 10.1590/s1677-5538.ibju.2016.0633
47. Reddy K, Gharde P, Tayade H, Patil M, Reddy LS, and Surya D. Advancements in robotic surgery: A comprehensive overview of current utilizations and upcoming frontiers. Cureus. (2023) 15:e50415. doi: 10.7759/cureus.50415
48. Veccia A, Carbonara U, Djaladat H, Mehazin R, Eun DD, Reese AC, et al. Robotic vs Laparoscopic Nephroureterectomy for Upper Tract Urothelial Carcinoma: A Multicenter Propensity-Score Matched Pair « tetrafecta » Analysis (ROBUUST Collaborative Group). J Endourol. (2022) 36:752−9. doi: 10.1089/end.2021.0587
49. Rodriguez JF, Packiam VT, Boysen WR, Johnson SC, Smith ZL, Smith ND, et al. Utilization and outcomes of nephroureterectomy for upper tract urothelial carcinoma by surgical approach. J Endourol. (2017) 31:661−5. doi: 10.1089/end.2017.0086
Keywords: robot assisted radical nephroureterectomy, multiport, single-port, transperitoneal, retroperitoneal
Citation: Gabriel P-E, Shariat SF, Rouprêt M, Sfakianos JP and Xylinas E (2025) Perioperative outcomes of multiport or single-port, transperitoneal or retroperitoneal robot assisted radical nephroureterectomy: a narrative review. Front. Oncol. 15:1655703. doi: 10.3389/fonc.2025.1655703
Received: 28 June 2025; Accepted: 23 September 2025;
Published: 06 October 2025.
Edited by:
Hanan Goldberg, Upstate Medical University, United StatesReviewed by:
Murat Akand, University Hospitals Leuven, BelgiumLingxiao Zhang, The First Affiliated Hospital of Hainan Medical University, China
Copyright © 2025 Gabriel, Shariat, Rouprêt, Sfakianos and Xylinas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Evanguelos Xylinas, ZXZhbmd1ZWxvcy54eWxpbmFzQGFwaHAuZnI=
 Pierre-Etienne Gabriel
Pierre-Etienne Gabriel Shahrokh F. Shariat2
Shahrokh F. Shariat2