- 1Department of Thoracic Surgery, Fujian Medical University Union Hospital, Fuzhou, China
- 2Key Laboratory of Ministry of Education for Gastrointestinal Cancer, Fujian Medical University, Fuzhou, China
- 3Fujian Key Laboratory of Tumor Microbiology, Fujian Medical University, Fuzhou, China
- 4Clinical Research Center for Thoracic Tumors of Fujian Province, Fuzhou, China
- 5Key Laboratory of Cardio-Thoracic Surgery, Fujian Medical University, Fuzhou, China
Introduction: The comprehensive complication index (CCI) is a valuable index to comprehensively and systematically evaluate complication severity. This study aimed to evaluate the predictive ability of comprehensive complication index on short- and long-term overall survival(OS) in patients with esophageal squamous cell carcinoma (ESCC) undergoing Mckeown minimally invasive esophagectomy (MIE).
Methods: A total of 320 patients treated with radical MIE from 2013 to 2017 were included, and the primary outcome was OS. Firstly, the optimal cut-off value of CCI was determined by X-tile. Propensity score matching(PSM) was used to balance the baseline characteristics. Second, postoperative hospital stay and hospital costs between high- and low-CCI groups were compared. Third, the Kaplan-Meier survival curve was used to analyze survival differences. Fourth, Cox analysis was used to explore the risk factors of OS. Fifth, univariate and multivariate logistic analysis was used to determine the risk factors of high CCI.
Results: The patients with CCI > 24.2 was defined as high-CCI group, and those with CCI ≤ 24.2 were assigned to low-CCI group. The high-CCI group had more hospital costs and longer hospital stays than the low-CCI group before and after PSM (both p<0.001). The Kaplan-Meier survival curve indicated that high-CCI group had worse prognosis both before and after PSM (before matching: P<0.001; after matching: P = 0.01). CCI was determined as an independent prognostic factor (before PSM, P = 0.001; after PSM, P = 0.003).
Conclusion: The CCI could quantify postoperative complications after esophagectomy. High CCI was associated with longer postoperative hospital stays and expenses and is an independent risk factor for poor OS, holding great vlaue for reference for medical insurance, surgical quality and prognosis management.
1 Introduction
Esophageal cancer (EC) is one of the most common and challenging types of cancer, with 572,000 new cases diagnosed each year and 500,000 deaths (1). At present, due to population aging, EC mainly occurs in middle-aged and elderly people, with the average age of diagnosis being 67 years old, and about 30% of patients are over 75 years old (2, 3). For patients with EC, surgical resection is the main treatment. Although minimally invasive esophagectomy (MIE) has become a popular surgical method in recent years to reduce postoperative complications, the incidence of postoperative complications is still relatively high (4).
Postoperative complications were often considered practical indicators to evaluate surgical quality, surgical safety. Review the history of medical classification of complications, from the initial simple classification of complications into major complications and minor complications (5). Then, the Clavien-Dindo complication classification is created, and complication classification is used to evaluate the postoperative complications (6). However, surgeons often only focus on severe complications and ignore other minor complications. The lack of a comprehensive assessment of all postoperative complications in the Clavien-Dindo complication has led clinicians to propose a CCI that provides a comprehensive picture of the true overall complication profile. The CCI has been confirmed as a comprehensive prognostic factor for the short-term and long-term outcomes in patients with gastric cancer (7). The role of CCI in patients undergoing MIE for ESCC was still unclear.
Compared with open esophagectomy, MIE could accelerate the perioperative recovery of patients without affecting the long-term prognosis in patients with EC (8, 9). Postoperative complications after MIE (such as anastomotic leakage) could greatly affect the prognosis of EC (10, 11). Perioperative medical quality (especially the avoidance and management of complications) also has a profound impact on the long-term survival of patients with esophageal cancer (12). However, the impact of one specified complication for postoperative complications was still controversial. This difference was partly due to the fact that Clavien-Dindo complication grading could only provide a qualitative evaluation rather than a quantitative evaluation of postoperative complications. In this study, we aimed to investigate the predictive ability of the CCI for short-term prognosis (postoperative hospital stay and surgical cost) and long-term prognosis (overall survival, OS) in patients undergoing MIE for esophageal squamous cell carcinoma (ESCC).
2 Methods
2.1 Patient selection
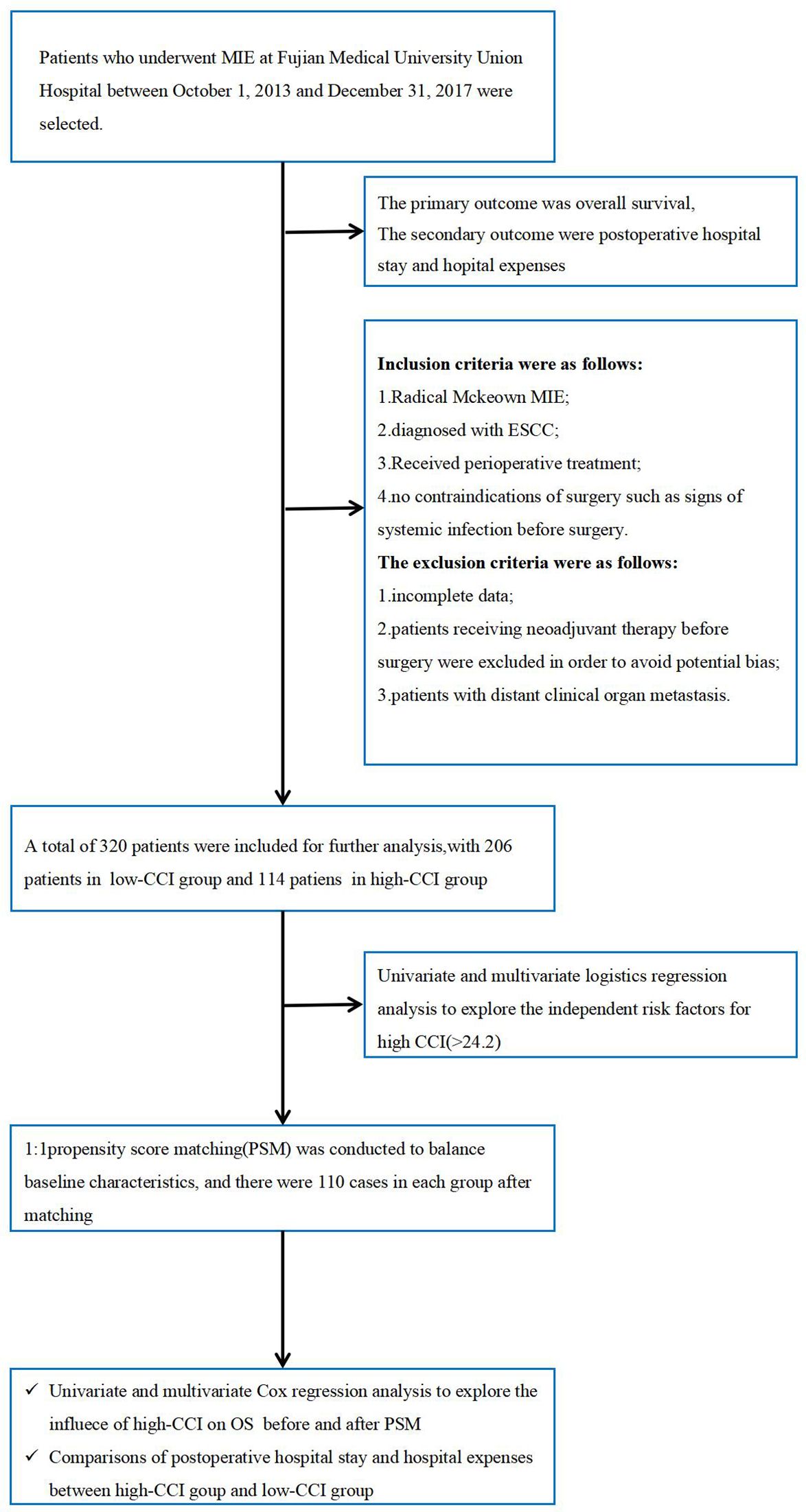
Patients who underwent MIE at Fujian Medical University between October 1, 2013 and December 31, 2017 were selected. This study was approved by the Institutional Review Board in Fujian Medical University Union Hospital(IRB number 2022YK202). Inclusion criteria were as follows: 1. Radical Mckeown MIE; 2. Diagnosed with ESCC; 3. Received perioperative treatment(including preoperative examination, operation, and postoperative nursing); 4. No contraindications of surgery. The exclusion criteria were as follows: 1. incomplete clinical data; 2. Patients who received neoadjuvant therapy were excluded due to the small sample size before 2017 and potential survival differences among regimens, to avoid bias; 3.Patients diagnosed with cM1.The details of the patient selection and analysis flowchart are presented in Figure 1.
2.2 Data collection and outcome definition
In this study, the primary outcome was overall survival (OS), which was defined as the time from surgery to death or the last follow-up. The secondary outcomes were postoperative hospital stay and hospital costs. Postoperative complications Clavien-Dindo ≥ 3a were defined as major complications, and postoperative complications Clavien-Dindo < 3a was defined as minor complication (13). Naples score (NPS) was calculated based on the dichotomous variables of neutrophil/lymphocyte ratio, lymphocyte/monocyte ratio, serum albumin, and total cholesterol (14). NPS = 0 was defined as a low Naples score, NPS = 1 or 2 was defined as a medium Naples score, and NPS = 3 or 4 was defined as a high Naples score (15). Preoperative comorbidities were graded using the Charson comorbidities Index. Patients with a Charson index of less than or equal to 1 point were considered a low-risk group, while patients with a Charson index of more than 1 point were considered a high-risk group (16, 17).
2.3 Treatment protocol
All patients underwent MIE, including gastroesophageal replacement for digestive tract reconstruction and left cervical anastomosis (McKeown operation, 18, 19). Thoracic and abdominal lymph nodes were routinely dissected, and three-field lymph node dissection was performed for patients with suspected cervical lymph node metastasis. During the periof of 2013 to 2017, patients diagnosed with cT1–2 or cN0 were recommended to receive surgery first. Some patients with cT3 or cN+ underwent surgery first, based on surgical feasibility assessed by the surgeon and the patient’s treatment preference.
Patients were followed up every 3 to 6 months in the first and second years and every six months in the third year. The patients were followed up once a year from the fifth year after surgery.
2.4 Calculation of CCI
The CCI was calculated based on the Clavien-Dindo grading system to reflect the comprehensive severity of postoperative complications. The formula was the sum of ownership weights divided by the square root of 2 equals the CCI. The final detailed formula for the CCI was: CCI = √ (median reference value from physicians(MRVphys) × median reference value from patients(MRVpat)/2. The value of CCI was continuous, ranging from 0 (no complications) to 100 (death). We used the online calculator (http://www.assessurgery.com) to calculate CCI (20).
2.5 Statistical analysis
Categorical variables were expressed as percentages and compared with the Chi-square test/Fisher exact test. Continuous variables were represented by medians and compared by the Mann-Whitney U test. In this study, X-tile software was used to calculate the optimal cut-off value of the CCI (21, 22). The operative duration was divided into the long-and short- duration group using the receiver operating characteristic curve. First, PSM was used to match the variables with differences between the two groups. The caliper value was set as 0.02, and the matching ratio was 1:1. The paramaters includes sex, age, BMI, Charson comorbidity index, tumor location, smoking history, CEA, vascular tumor thrombus, T stage, N stage, Grade, NPS and adjuvant therapy. Secondly, the postoperative hospital stay and postoperative hospitalization cost between the two groups were compared. Third, independent risk factors were determined by univariate and multivariate Cox regression analysis (23). Statistical analysis was performed using X-tile 3.6.1 software (Yale University, USA) and R software version 4.0.5 (http://www.r-project.org). All statistical test levels considered a P value less than 0.05 to be statistically significant.
3 Results
3.1 Patient characteristics
A total of 320 patients were included in this study. 258 (80.62%) patients were ≤65 years old, and 240 (75%) were males. All patients underwent McKeown MIE, and 302 patients (94.38%) underwent 2-field lymph node dissection. The detail information of ESCC patients was shown in Supplementary Table S1.
3.2 Comparison of high-CCI group and low-CCI group before and after PSM
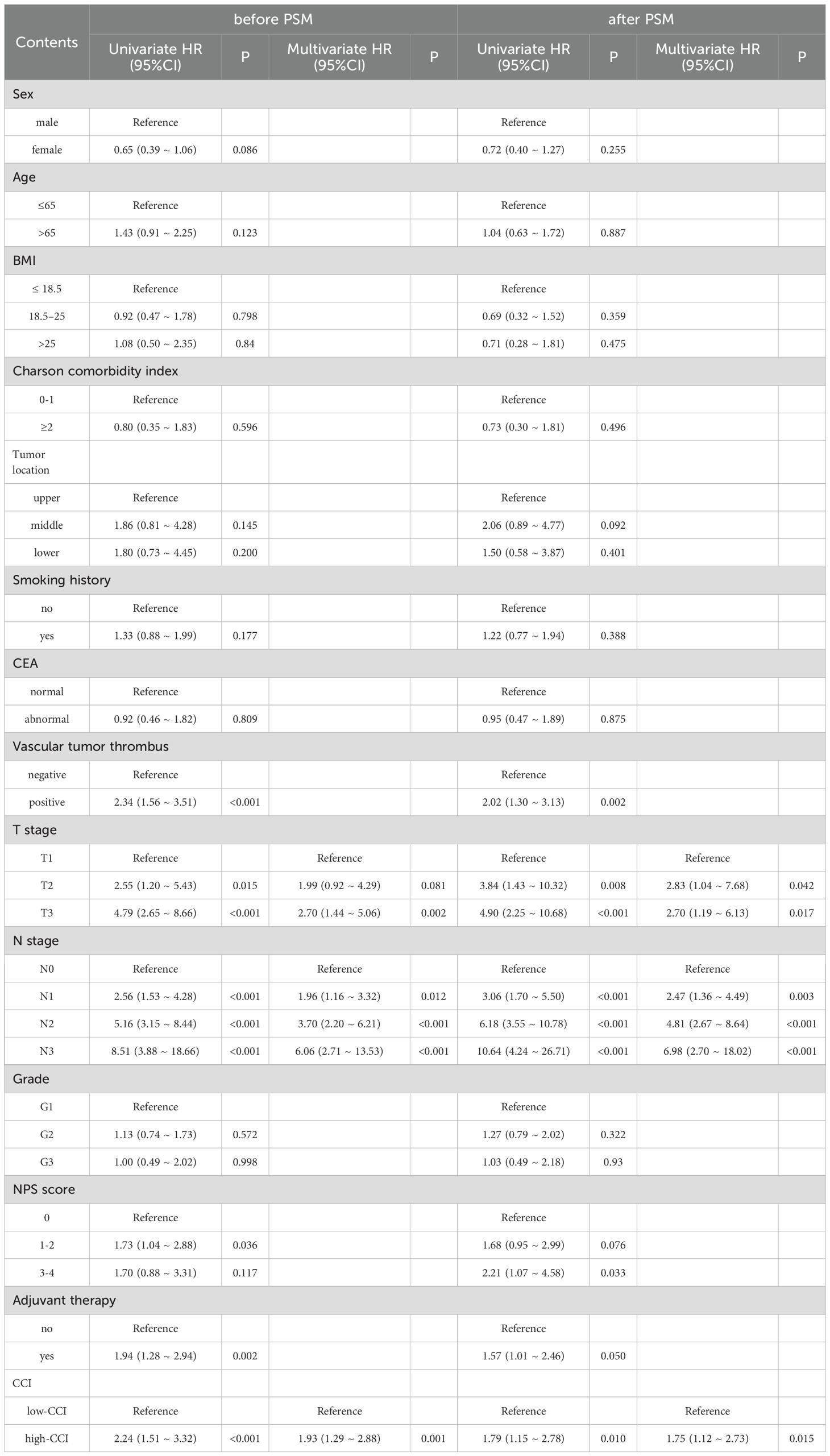
The X-tile software determined an optimal CCI cutoff of 24.2, dividing patients into high- and low-CCI groups. Before PSM, there were significant differences in T stage between the groups. After PSM, the baseline characteristics were balanced, as is shown in Table 1.
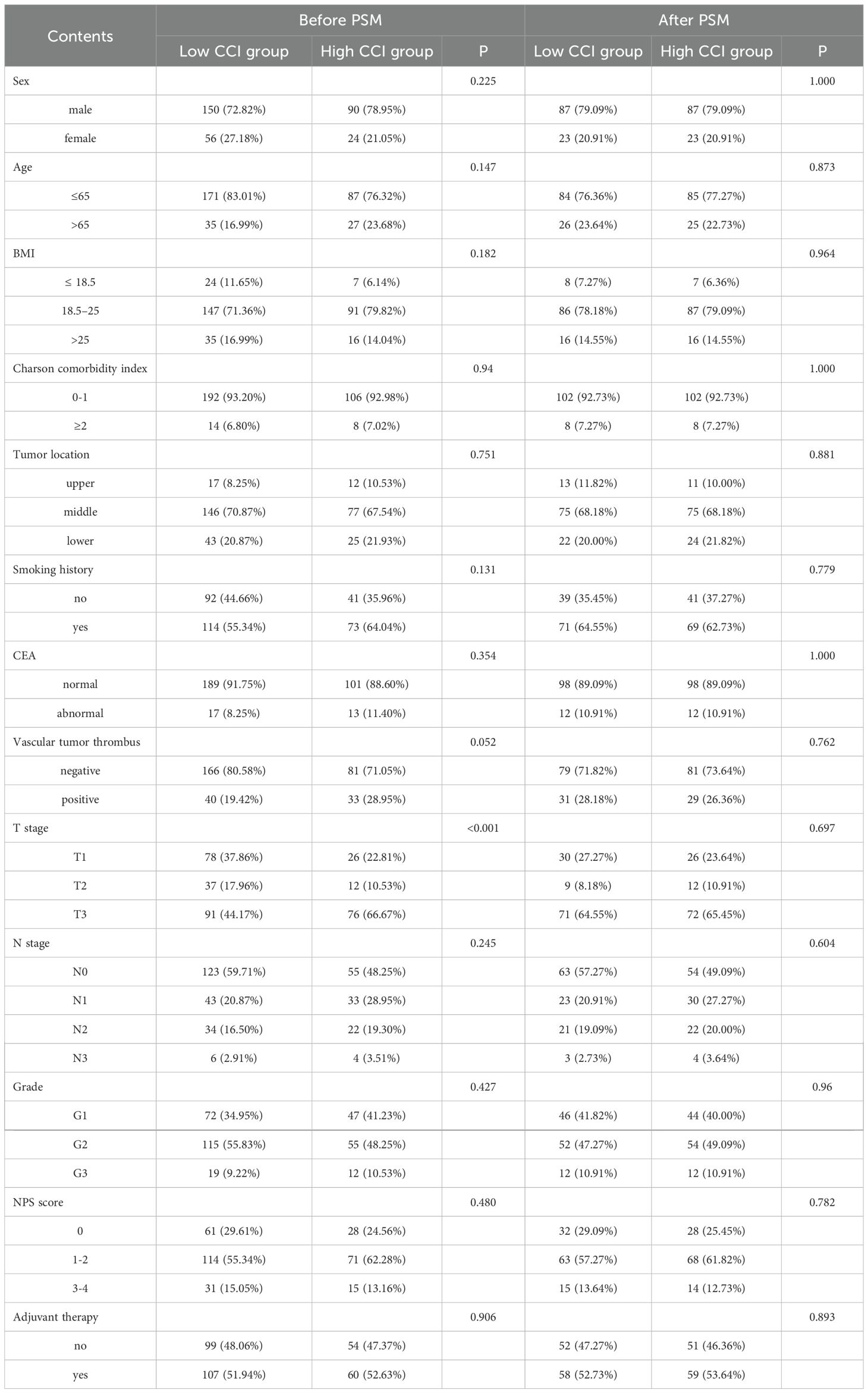
Table 1. The baseline characteristics between high CCI group and low CCI group before and after PSM.
The high CCI group had more medical expenses than the low CCI group (before PSM: 97098yuan vs. 84832yuan, P<0.001; after PSM: 99342yuan vs. 84590yuan, P<0.001) and longer hospital stays after surgery (before PSM:16 days vs. 9 days, P<0.001; after PSM: 16 days vs. 9 days, P<0.001), as is shown in Supplementary Table S2.
Besides, the comparisons of detailed complications between the two groups before and after PSM were summarized in Table 2.
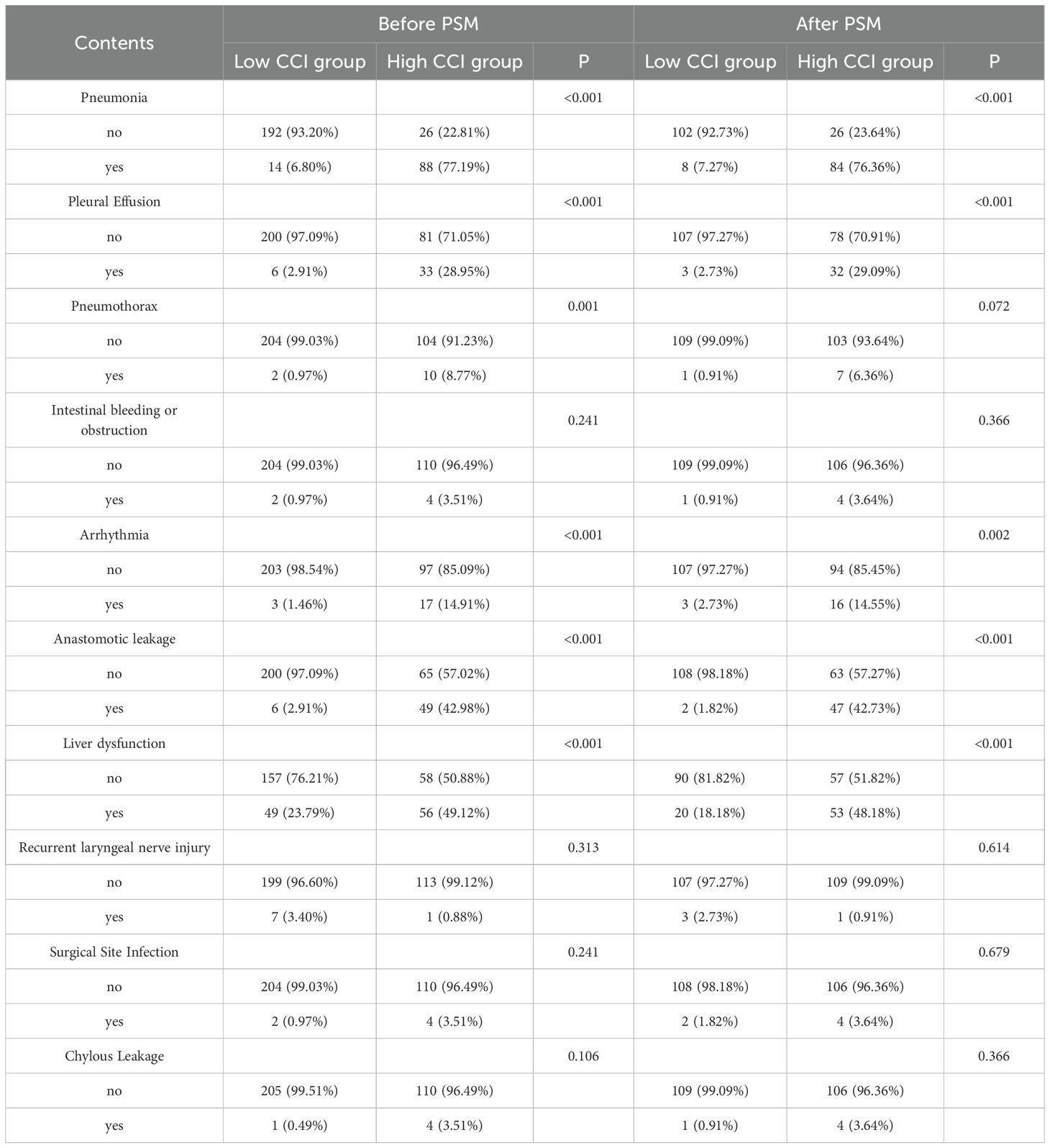
Table 2. The comparisons of detailed complications between high CCI group and low CCI group before and after PSM.
3.3 Survival analysis of CCI before and after PSM
Kaplan-Meier survival curves were analyzed for groups with high- and low- CCIs before and after PSM. Before matching, patients in the high-CCI group had worse survival outcomes than those in the low-CCI group (Figure 2A, P < 0.001). After matching, patients with the higher CCI still showed a worse prognosis (Figure 2B, P < 0.001).
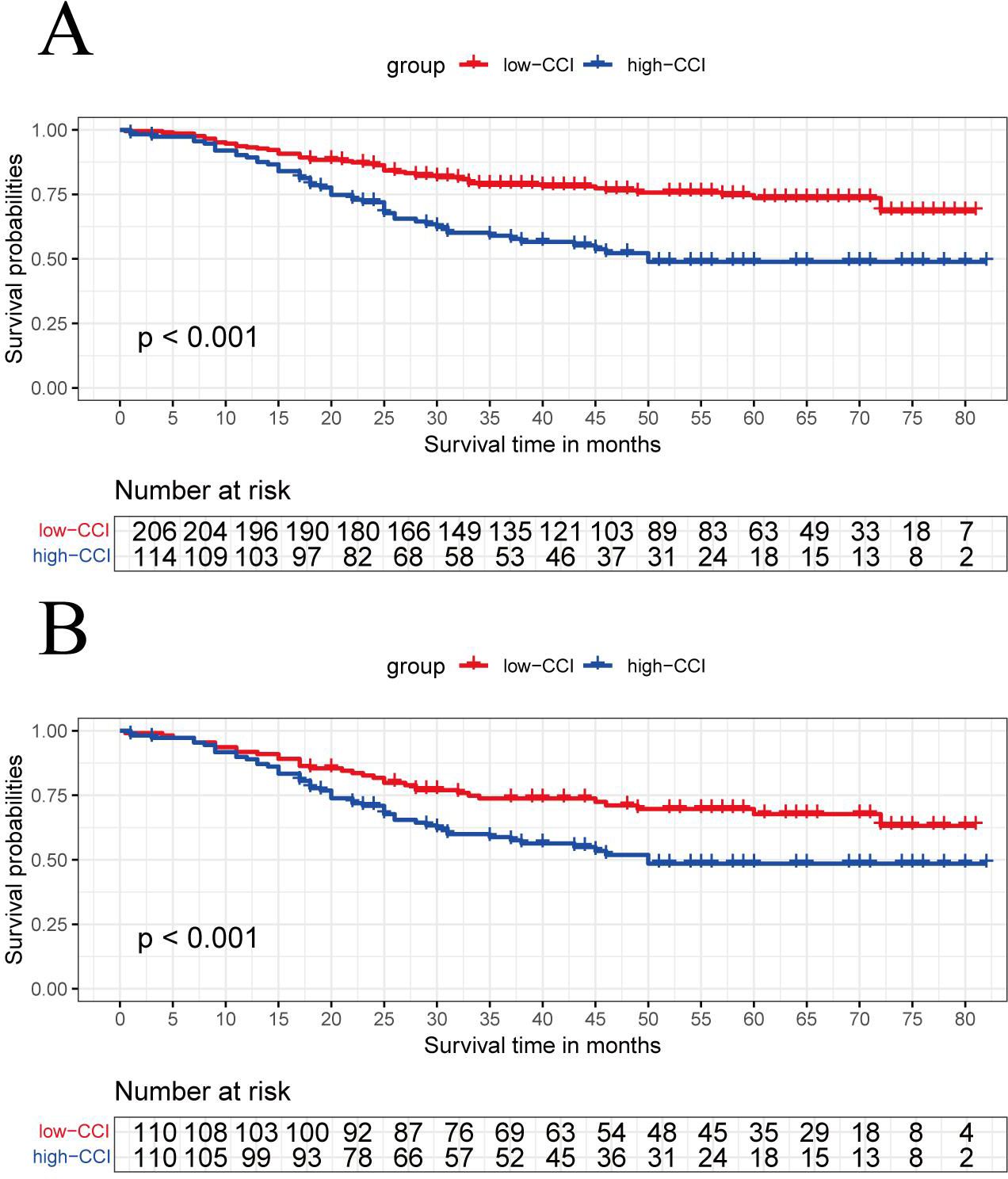
Figure 2. The Kaplan-Meier curve analysis compares the overall survival between the high-CCI group and the low-CCI group before (A) and after matching (B).
Before PSM, univariate Cox analysis showed that the influencing factors of OS after esophageal cancer surgery were vascular thrombus, T stage, N stage, adjuvant therapy, CCI and NPS score. In the following multivariate Cox analysis, the independent influencing factors of OS were T stage, N stage, and CCI (P < 0.001). Similarlly, after PSM, univariate and multivariate Cox analysis showed the independent influencing factors were the T stage, N stage, and CCI (P = 0.015), as is shown in Table 3.
3.4 Subgroup analysis of CCI before and after PSM
Before PSM, patients with a higher CCI exhibited significantly worse survival outcomes within the subgroups of medium and high Naples scores compared to those with a lower CCI (Figures 3B, C). However, there were no survival difference between two group in the subgroup of low Naples score (Figure 3A). Following PSM, the survival advantage of the low CCI group remained evident in the medium Naples subgroup (Figure 3E). Additionally, in the high Naples score subgroup, a trend toward improved survival was observed in low-CCI group (Figure 3F). Similarly, no survival difference was observed between two group in the subgroup of low Naples score after PSM (Figure 3D).
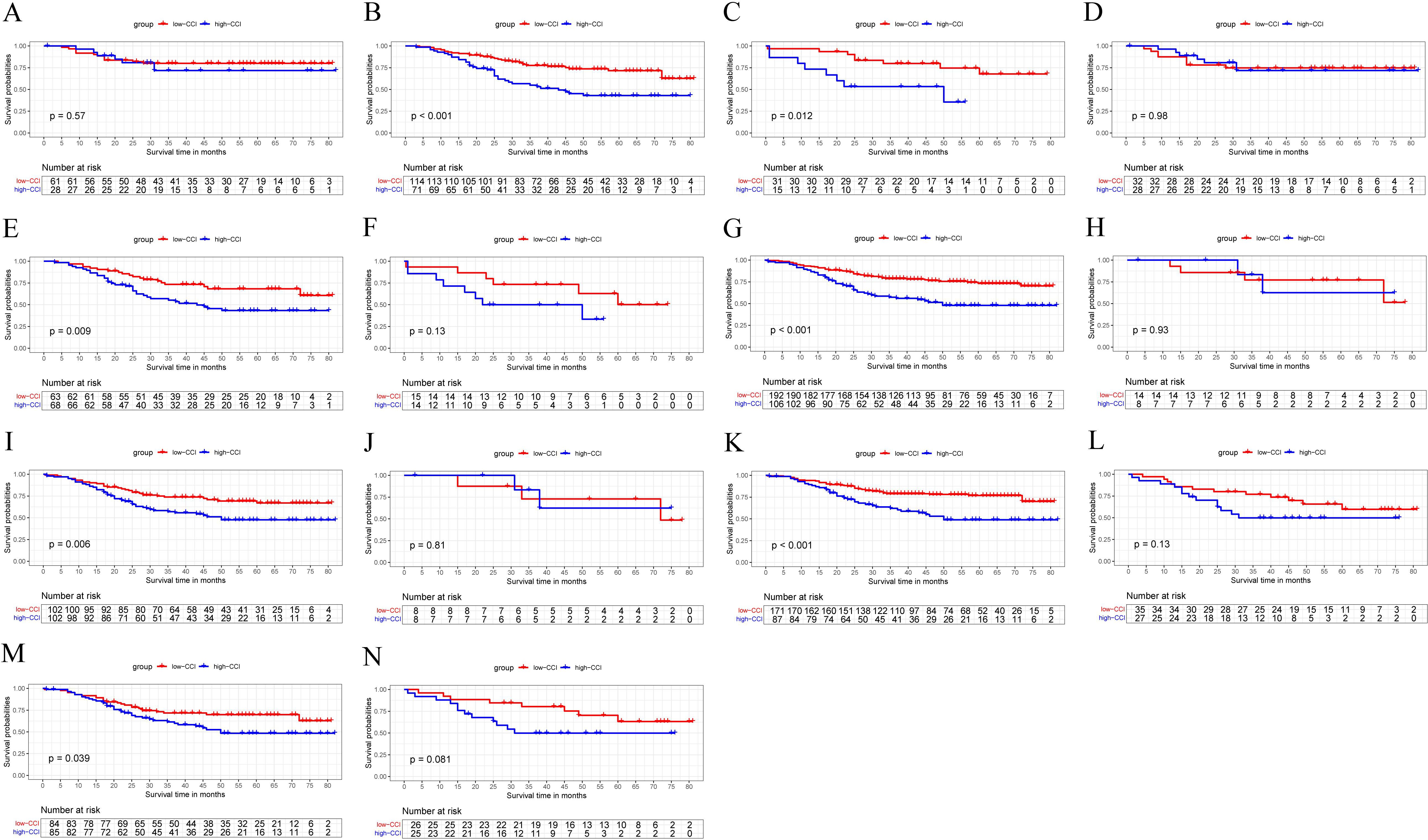
Figure 3. The Kaplan-Meier curve analysis between the high-CCI group and the low-CCI group in the subgroup of low-NPS (A, D), medium-NPS (B, E), high-NPS (C, F), low-Charlson index (G, I), high-Charlson index (H, J), age ≤ 65 (K, M) and age > 65 (L, N) before and after PSM.
A statistically significant difference in survival outcomes between the high and low CCI groups was observed both before and after PSM in the subgroup of patients with a low charlson comorbidity score (Figures 3G, I). Similarly, a significant survival disparity between these two groups was also present in the subgroup of patients aged≤65 years, as is shown in Figures 3K, M. While, the low CCl group had similar survival with the high CCI group in terms of patients with high charlson score (Figures 3H, J)and patients aged over 65 (Figures 3L, N).
3.5 Univariate and multivariate logistic analysis of high CCI
By the receiver operating characteristic curve, the operative time was divided into long duration group (≥278.5mins) and short duration group(<278.5mins). Univariate logistics indicated that clinical T stage, clinical N stage, intraoperative blood loss, and operation time were potential risk factors for high CCI(P<0.05). Further multivariate logistic analysis using the forward method confirmed that intraoperative bleeding (P = 0.003) was independent risk factors of high CCI, as is shown in Supplementary Table S4.
4 Discussion
Early postoperative complications reflect short-term outcomes and may negatively affect the long-term prognosis by prolonging inflammation and increasing immunosuppression, thus promoting tumor recurrence and metastasis (24–26). Studies have shown that maintaining strong cellular immunity and controlling excessive catecholamine and prostaglandin responses during the perioperative period can reduce immune suppression, tumor recurrence, benefiting both short- and long-term survival (27). However, the link between postoperative complications and long-term survival in EC patients remains unclear (28–30). While complications generally harm long-term survival, the system of Clavien-Dindo grades have not shown significant prognostic differences in ESCC (31, 32). This may be due to the low sensitivity of Clavien-Dindo grading in predicting survival outcomes. Recently, the concept of textbook outcome has been introduced as a new way to assess complications and predict prognosis in ESCC (33). However, textbook outcome still relies on Clavien-Dindo grading, which may not fully capture the complexity of complications. Previous studies suggested that the CCI was more sensitive than traditional classifications (34–36). Therefore, this study aimed to evaluate the value of CCI in predicting both short- and long-term outcomes in ESCC patients.
Our results showed that the survival outcomes between higg-CCI group and low-CCI group were statistically different. The Kaplan-Meier survival analysis indicated that patients with high CCI had worse prognosis both before and after PSM. Cox analysis further confirmed that CCI was an independent risk factor of OS. This was consistent with the report from Kudo T et al. (37). However, therer are several advantages of our study. First, the larger sample size strengthened the reliability of our findings. Second, surgical approaches for esophageal cancer differ in their impact on postoperative complications; therefore, we focused on patients who underwent the McKeown procedure to minimize confounding. Third, subgroup analysis confirmed the prognostic value of CCI. Notably, this value was evident not only in patients with moderate to high Naples scores, but also in those with low Charlson index scores and in younger patients. This suggests that CCI-based assessment of complications provides independent prognostic information that complements existing risk stratification tools, even in traditionally low-risk groups.
Thoerically, CCI could provide a more comprehensive evaluation of postoperative complications, more accurately reflecting the severity of postoperative complications and the influence of postoperative complications on the level of systemic inflammatory response and degree of immunosuppression (38). For example, for patients experiencing one Clavien-Dindo grade 2 complication or combined with two grade 1 postoperative complications, the CCI score does not exceed 24.2. In contrast, for patients with at least one complication of Clavien-Dindo grade 3 or higher (severe complications), the CCI score exceeds 24.2. When the Clavien-Dindo classification system is used to evaluate the impact of postoperative complications on prognosis, the assessment typically considers only the most severe complication, thereby overlooking the contribution of less severe events. Therefore, utilizing the CCI for a comprehensive evaluation of postoperative complications allows for a more holistic understanding of their impact on long-term patient outcomes.
Compared with other complication grading methods, CCI is more strongly correlated with length of stay and cost of stay (39). This study supported that the high-CCI group had longer hospital stays and higher surgical costs. Longer hospital stays and higher medical costs were a huge economic and psychological burden for patients and their families, which suggested that we should actively prevent and effectively treat complications. Meanwhile, given the strong correlation between CCI and postoperative hospitalization costs, CCI may be a potential reference index for insurance settlement.
T stage and N stage were aslo identified as independent risk factors of OS, which is similar with other studies (40). In this study, the Naples score and Charlson status were not identified as independent risk factors. This outcome may be attributed to the fact that these two measures primarily reflect short-term nutritional status and, consequently, are insufficient to comprehensively capture long-term nutritional conditions (16). Current evidence suggests that the clinical benefits of adjuvant therapy may vary depending on the patient’s condition. Adjuvant therapy is associated with survival benefits in patients with lymph node positivity (41), but not in those without lymph node metastasis (42). Therefore, when developing individualized treatment strategies, it is important to evaluate the patient’s clinical status, the risk of postoperative complications, and the potential benefits of adjuvant therapy to support more precise and tailored decisions. Smoking status is not identified as an independent risk factor for OS, and this finding aligns with previous research (43). This study also found more intraoperative blood loss were associated with high CCI, which was similar with previous study (44).
This study has several limitations. Despite the establishment of stringent criteria, certain limitations inherent to retrospective matched analyses were unavoidable. Additionally, treatment approaches for similar postoperative complications may differ across centers or groups due to variations in clinical experience, potentially increasing heterogeneity among studies. Consequently, future research should aim to develop a standardized protocol for the evaluation and treatment of complications, based on multicenter studies, to enhance the assessment of prognostic impacts and facilitate cross-center comparisons. Moreover, due to the relatively small population of patients with esophageal adenocarcinoma (EAC), this study included only ESCC patients. As a result, the applicability of CCI in EAC patients requires further validation. Furthermore, this study excluded patients who underwent surgical treatment following neoadjuvant therapy, necessitating additional validation of the CCI scoring system’s applicability in this specific patient population. Future studies with larger sample sizes are essential to confirm our findings.
5 Conclusion
The CCI has the capability to quantify postoperative complications following esophagectomy. Before and after PSM, a high CCI is correlated with extended postoperative hospital stays and increased hospital costs. Furthermore, it serves as an independent risk factor for poor OS, holding significant potential as a reference tool for insurance claims and offers valuable evaluation indicators for clinicians concerning surgical quality control and patient prognosis management.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Institutional Review Board of the Fujian Medical University Union Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the requirement for informed consent was waived by the review board due to the retrospective nature of the study.
Author contributions
XW: Data curation, Formal analysis, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. JY: Data curation, Methodology, Validation, Writing – original draft. SX: Data curation, Methodology, Validation, Writing – original draft. YL: Data curation, Writing – original draft. PZ: Methodology, Validation, Writing – original draft. LG: Conceptualization, Writing – review & editing, Methodology, Formal analysis. ZH: Data curation, Methodology, Supervision, Writing – review & editing. MK: Conceptualization, Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was sponsored by the National Natural Science Foundation of China (Grant No. 82372680& 82302904), Joint Funds for the innovation of Science and Technology, Fujian Province (Grant No. 2023Y9168&2024Y9321), Clinical Research Center for Thoracic Tumors of Fujian Province (Grant No. 2024YGPT001) and Startup Fund for scientific research,Fujian Medical University (Grant No. 2024QH1030).
Acknowledgments
We appreciate the support by Figdraw.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1661797/full#supplementary-material
References
1. Lu L, Mullins CS, Schafmayer C, Zeißig S, and Linnebacher M. A global assessment of recent trends in gastrointestinal cancer and lifestyle-associated risk factors. Cancer Commun (London England). (2021) 41:1137–51. doi: 10.1002/cac2.12220
2. GBD 2019 Adolescent Mortality Collaborators. Global, regional, and national mortality among young people aged 10–24 years, 1950-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London England). (2021) 398:1593–618. doi: 10.1016/S0140-6736(22)00320-8
3. Partridge L, Deelen J, and Slagboom PE. Facing up to the global challenges of aging. Nature. (2018) 561:45–56. doi: 10.1038/s41586-018-0457-8
4. Yoshida N, Yamamoto H, Miyata H, and Baba H. Response to comment on "Can minimally invasive esophagectomy replace open esophagectomy for esophageal cancer? Latest analysis of 24,233 esophagectomies from the Japanese national clinical database. Ann Surg. (2019) 270:e110–1. doi: 10.1097/SLA.0000000000003337
5. Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multi-center randomized controlled trial (KLASS-01). Ann Surg. (2016) 263:28–35. doi: 10.1097/SLA.0000000000001346
6. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. (2009) 250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2
7. Kim TH, Suh YS, Huh YJ, Son YG, Park JH, Yang JY, et al. The comprehensive complication index (CCI) is a more sensitive complication index than the conventional Clavien-Dindo classification in radical gastric cancer surgery. Gastric cancer: Off J Int Gastric Cancer Assoc Japanese Gastric Cancer Assoc. (2018) 21:171–81. doi: 10.1007/s10120-017-0728-3
8. Kalff MC, Gottlieb-Vedi E, Verhoeven RHA, van Laarhoven HWM, Lagergren J, Gisbertz SS, et al. Presentation, treatment, and prognosis of esophageal carcinoma in a nationwide comparison of Sweden and the Netherlands. Ann Surg. (2021) 274:743–50. doi: 10.1097/SLA.0000000000005127
9. Kalff MC, Fransen LFC, de Groot EM, Gisbertz SS, Nieuwenhuijzen GAP, Ruurda JP, et al. Long-term survival after minimally invasive versus open esophagectomy for esophageal cancer: A nationwide propensity-score matched analysis. Ann Surg. (2022) 276:e749–57. doi: 10.1097/SLA.0000000000004708
10. Fransen LFC, Berkelmans GHK, Asti E, van Berge Henegouwen MI, Berlth F, Bonavina L, et al. The effect of postoperative complications after minimally invasive esophagectomy on long-term survival: an international multi-center cohort study. Ann Surg. (2021) 274:e1129–37. doi: 10.1097/SLA.0000000000003772
11. Saunders JH, Yanni F, Dorrington MS, Bowman CR, Vohra RS, Parsons SL, et al. Impact of postoperative complications on disease recurrence and long-term survival following oesophagogastric cancer resection. Br J Surg. (2020) 107:103–12. doi: 10.1002/bjs.11318
12. Hallet J, Jerath A, Turgeon AF, McIsaac DI, Eskander A, Zuckerman J, et al. Association between anesthesiologist volume and short-term outcomes in complex gastrointestinal cancer surgery. JAMA Surg. (2021) 156:479–87. doi: 10.1001/jamasurg.2021.0135
13. Wang D, Zhang J, Bai Z, Yang Y, Wang T, Jin L, et al. Associations of postoperative complications assessed by clavien-dindo classification and comprehensive complication index with long-term overall survival in elderly patients after radical CRC resection. Clin Interventions Aging. (2020) 15:1939–49. doi: 10.2147/CIA.S271969
14. Li J, Yang W, Yuan Y, Zuo M, Li T, Wang Z, et al. Preoperative Naples prognostic score is a reliable prognostic indicator for newly diagnosed glioblastoma patients. Front Oncol. (2022) 12:775430. doi: 10.3389/fonc.2022.775430
15. Xiong J, Hu H, Kang W, Liu H, Ma F, Ma S, et al. Prognostic impact of preoperative naples prognostic score in gastric cancer patients undergoing surgery. Front Surg. (2021) 8:617744. doi: 10.3389/fsurg.2021.617744
16. Kubo Y, Tanaka K, Yamasaki M, Yamashita K, Makino T, Saito T, et al. Influences of the charlson comorbidity index and nutrition status on prognosis after esophageal cancer surgery. Ann Surg Oncol. (2021) 28:7173–82. doi: 10.1245/s10434-021-09779-1
17. Yamashita K, Watanabe M, Mine S, Fukudome I, Okamura A, Yuda M, et al. The impact of the Charlson comorbidity index on the prognosis of esophageal cancer patients who underwent esophagectomy with curative intent. Surg Today. (2018) 48:632–9. doi: 10.1007/s00595-018-1630-2
18. Sun HB, Li Y, Liu XB, Zhang RX, Wang ZF, Lerut T, et al. Early oral feeding following mcKeown minimally invasive esophagectomy: an open-label, randomized, controlled, noninferiority trial. Ann Surg. (2018) 267:435–42. doi: 10.1097/SLA.0000000000002304
19. Wee JO and Morse CR. Minimally invasive Ivor Lewis esophagectomy. J Thorac Cardiovasc Surg. (2012) 144:S60–2. doi: 10.1016/j.jtcvs.2011.12.051
20. Slankamenac K, Graf R, Puhan MA, and Clavien PA. Perception of surgical complications among patients, nurses and physicians: a prospective cross-sectional survey. Patient Saf Surg. (2011) 5:30. doi: 10.1186/1754-9493-5-30
21. Shimizu S, Saito H, Kono Y, Murakami Y, Shishido Y, Miyatani K, et al. The prognostic significance of the comprehensive complication index in patients with gastric cancer. Surg Today. (2019) 49:913–20. doi: 10.1007/s00595-019-01828-3
22. Whooley BP, Law S, Murthy SC, Alexandrou A, and Wong J. Analysis of reduced death and complication rates after esophageal resection. Ann Surg. (2001) 233:338–44. doi: 10.1097/00000658-200103000-00006
23. Haas M, Huber T, Pickl C, van Rhijn BWG, Gužvić M, Gierth M, et al. The comprehensive complication index is associated with a significant increase in complication severity between 30 and 90 days after radical cystectomy for bladder cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. (2021) 47:1163–71. doi: 10.1016/j.ejso.2020.09.040
24. Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, and Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg. (2015) 261:497–505. doi: 10.1097/SLA.0000000000000854
25. Baba Y, Yoshida N, Shigaki H, Iwatsuki M, Miyamoto Y, Sakamoto Y, et al. Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: A retrospective single-institution study. Ann Surg. (2016) 264:305–11. doi: 10.1097/SLA.0000000000001510
26. Saeki H, Tsutsumi S, Tajiri H, Yukaya T, Tsutsumi R, Nishimura S, et al. Prognostic significance of postoperative complications after curative resection for patients with esophageal squamous cell carcinoma. Ann Surg. (2017) 265:527–33. doi: 10.1097/SLA.0000000000001692
27. Goldfarb Y, Sorski L, Benish M, Levi B, Melamed R, and Ben-Eliyahu S. Improving postoperative immune status and resistance to cancer metastasis: a combined perioperative approach of immunostimulation and prevention of excessive surgical stress responses. Ann Surg. (2011) 253:798–810. doi: 10.1097/SLA.0b013e318211d7b5
28. Lindner K, Fritz M, Haane C, Senninger N, Palmes D, and Hummel R. Postoperative complications do not affect long-term outcome in esophageal cancer patients. World J Surg. (2014) 38:2652–61. doi: 10.1007/s00268-014-2590-3
29. Lerut T, Moons J, Coosemans W, Van Raemdonck D, De Leyn P, Decaluwé H, et al. Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Ann Surg. (2009) 250:798–807. doi: 10.1097/SLA.0b013e3181bdd5a8
30. Sachidananda S, Timsina L, Namburi N, and Birdas TJ. Esophagectomy complications impact long-term survival: A national cancer database analysis. Ann Surg. (2023) 277:437–41. doi: 10.1097/SLA.0000000000005093
31. Li KK, Wang YJ, Liu XH, Tan QY, Jiang YG, and Guo W. The effect of postoperative complications on survival of patients after minimally invasive esophagectomy for esophageal cancer. Surg endoscopy. (2017) 31:3475–82. doi: 10.1007/s00464-016-5372-1
32. Nathan H, Yin H, and Wong SL. Postoperative complications and long-term survival after complex cancer resection. Ann Surg Oncol. (2017) 24:638–44. doi: 10.1245/s10434-016-5569-5
33. Xu SJ, Lin LQ, Chen C, Chen TY, You CX, Chen RQ, et al. Textbook outcome after minimally invasive esophagectomy is an important prognostic indicator for predicting long-term oncological outcomes with locally advanced esophageal squamous cell carcinoma. Ann Trans Med. (2022) 10:161. doi: 10.21037/atm-22-506
34. Tu RH, Lin JX, Li P, Xie JW, Wang JB, Lu J, et al. Comprehensive complication index predicts cancer-specific survival of patients with postoperative complications after curative resection of gastric cancer. Gastroenterol Res Pract. (2018) 2018:4396018. doi: 10.1155/2018/4396018
35. Kowalewski KF, Müller D, Mühlbauer J, Hendrie JD, Worst TS, Wessels F, et al. The comprehensive complication index (CCI): proposal of a new reporting standard for complications in major urological surgery. World J Urol. (2021) 39:1631–9. doi: 10.1007/s00345-020-03356-z
36. Tirotta F, Parente A, Richardson T, Almonib A, Evenden C, Max Almond L, et al. Comparison of comprehensive complication index and Clavien-Dindo classification in patients with retroperitoneal sarcoma. J Surg Oncol. (2021) 124:1166–72. doi: 10.1002/jso.26612
37. Kudo T, Oshikiri T, Goto H, Harada H, Urakawa N, Hasegawa H, et al. Comprehensive complication index as a prognostic factor in minimally invasive esophagectomy for esophageal squamous cell carcinoma. Esophagus: Off J Japan Esophageal Soc. (2022) 19:410–6. doi: 10.1007/s10388-022-00911-y
38. Tsujimoto H, Ichikura T, Ono S, Sugasawa H, Hiraki S, Sakamoto N, et al. Impact of postoperative infection on long-term survival after potentially curative resection for gastric cancer. Ann Surg Oncol. (2009) 16:311–8. doi: 10.1245/s10434-008-0249-8
39. Llàcer-Millán E, Pavel MC, Memba R, Coronado D, González S, Achalandabaso M, et al. Comparison between Comprehensive Complication Index (CCI®) and Clavien-Dindo Classification for laparoscopic single-stage treatment of choledocholithiasis with concomitant cholelithiasis. Langenbeck's Arch Surg. (2023) 408:100. doi: 10.1007/s00423-023-02840-5
40. Hou B, Yuan J, Kang S, Yang Y, Huang X, Xu H, et al. Positive lymph node ratio is an important index to predict long-term survival for advanced esophageal squamous carcinoma patients (II∼III) with R0 resection–a SEER-based analysis. Heliyon. (2023) 9:e22600. doi: 10.1016/j.heliyon.2023.e22600
41. Raman V, Jawitz OK, Farrow NE, Voigt SL, Rhodin KE, Yang CJ, et al. The relationship between lymph node ratio and survival benefit with adjuvant chemotherapy in node-positive esophageal adenocarcinoma. Ann Surg. (2022) 275:e562–7. doi: 10.1097/SLA.0000000000004150
42. Pasquer A, Gronnier C, Renaud F, Duhamel A, Théreaux J, Carrere N, et al. Impact of Adjuvant Chemotherapy on Patients with Lymph Node-Positive Esophageal Cancer who are primarily Treated with Surgery. Ann Surg Oncol. (2015) 22 Suppl 3:S1340–9. doi: 10.1245/s10434-015-4658-1
43. Kamarajah SK, Madhavan A, Chmelo J, Navidi M, Wahed S, Immanuel A, et al. Impact of smoking status on perioperative morbidity, mortality, and long-term survival following transthoracic esophagectomy for esophageal cancer. Ann Surg Oncol. (2021) 28:4905–15. doi: 10.1245/s10434-021-09720-6
Keywords: overall survival, comprehensive complication index, Clavein-Dindo classification, minimally invasive esophagectomy, esophageal squamous cell carcinoma
Citation: Wang X, Yu J, Xie S, Lin Y, Zhang P, Gao L, Hong Z and Kang M (2025) High comprehensive complication index after minimally invasive esophagectomy associated with poor short-term and long-term outcome: a propensity score matching analysis. Front. Oncol. 15:1661797. doi: 10.3389/fonc.2025.1661797
Received: 13 July 2025; Accepted: 22 September 2025;
Published: 28 October 2025.
Edited by:
Airazat M. Kazaryan, Østfold Hospital, NorwayReviewed by:
Paolo Mercantini, Sapienza University of Rome, ItalyShagen Danielian, Armenian National Institute of Health (NIH), Armenia
Copyright © 2025 Wang, Yu, Xie, Lin, Zhang, Gao, Hong and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingqiang Kang, a2FuZ21pbmdxaWFuZzA3OTlAMTYzLmNvbQ==; Zhinuan Hong, aG9uZ3poaW51YW5AMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Xiaoqing Wang
Xiaoqing Wang Jingchuan Yu1,2,3†
Jingchuan Yu1,2,3† Ye Lin
Ye Lin Peipei Zhang
Peipei Zhang Zhinuan Hong
Zhinuan Hong