Abstract
Introduction:
Lip and Oral Cavity Cancer (LOCC), as a common type of malignant cancer, has become an important public health issue. This study aims to analyze and predict the trend of the LOCC burden, providing guidance for reducing the burden of LOCC.
Methods:
This study was based on the Global Burden of Disease (GBD) database 2021. We assessed the differences in LOCC among different regions and sexes from 1990 to 2021 using Age-Standardized Rates (ASR) and Estimated Annual Percentage Change (EAPC). Additionally, Bayesian Age-Period-Cohort (BAPC) model was employed to predict the Incidence, Prevalence, Death, Disability-Adjusted Life Years (DALYs), Years of Life Lost due to disease (YLLs), and Years Lived with Disability (YLDs) of LOCC globally from 2022 to 2030.
Results:
From 1990 to 2021, the global ASR of Incidence (ASIR), ASR of Prevalence (ASPR), and ASR of YLDs for LOCC had significantly increased, while the ASR of Death (ASDR), DALYs, and YLLs had decreased. The BAPC model predicted that by 2030, the ASIR and ASPR for males would decrease, while for females, an upward trend would be observed. The middle-aged and elderly population (>50 years) would still be the main patient group (accounting for over 60%).
Conclusion:
The disease burden of LOCC remains severe at present, but it is expected to show a downward trend by 2030. Therefore, it is still necessary to intensify efforts in the prevention and control of LOCC to achieve the expectation. This study provides theoretical guidance for reducing the burden of LOCC.
Introduction
Lip and oral cavity cancer (LOCC) is a malignant cancer involving the lips, tongue, gums, oral mucosa, and salivary glands, and is one of the common cancers worldwide (1). The severe impact of LOCC on patients’ speech, eating, and overall quality of life makes it an important public health issue (2). Studies have shown that smoking, alcohol consumption, chewtabaccio, betelnut, and long-term ultraviolet (UV) exposure are all significant risk factors for LOCC (3, 4). With the intensification of global population aging and the widespread presence of these risk factors, the situation of LOCC remains severe (5). Specifically, in some low- and middle-income countries, the diagnosis of LOCC is often delayed due to the lack of effective early screening and treatment methods, which leads to increased difficulty in treatment and poor prognosis (6).
Beyond its impact on the physical health of LOCC patients, it exerts a substantial economic burden on different regions. For instance, in Iran, the overall economic burden attributable to oral cancer reaches 64,245,173 USD, with the cost of late-stage treatment being five times higher than that of early-stage treatment (7). Similarly, in Australia, the average economic burden per patient with oral squamous cell carcinoma amounts to 61,128 USD (8). Therefore, understanding the current and future trends of LOCC disease burden is crucial for reducing, controlling, and preventing LOCC. It can serve as a guide for policymakers in planning and implementing effective prevention and control programs.
Based on this, our study aims to leverage the data from the Global Burden of Disease (GBD) 2021 to stratify the current and future trends in the global burden of LOCC, and to investigate the differences across genders and age groups. This endeavor is intended to provide a scientific basis for LOCC prevention and control strategies on a global level. Through the analysis of LOCC burden, we hope to offer valuable insights to public health policymakers, thereby promoting global efforts in the prevention, early diagnosis, and treatment of LOCC, and ultimately alleviating the burden of LOCC on human health.
Methods
Data source and selection
The data on LOCC in this study were sourced from the GBD 2021 database (https://vizhub.healthdata.org/gbd-results/). This database integrates data from multiple sources and provides detailed epidemiological data for 195 countries and regions worldwide, covering 359 diseases, injuries, and risk factors (9, 10). Moreover, the data utilized in this study were derived from publicly accessible datasets that have been endorsed by the University of Washington, thereby eliminating any ethical concerns (9, 10). Finally, this study focused on analyzing the current status and future projections of LOCC based on the current data, including Incidence, Prevalence, Death, Disability-Adjusted Life Years (DALYs), Years of Life Lost (YLLs) due to premature mortality, and Years Lived with Disability (YLDs).
Data processing
To characterize the LOCC burden in 2021, this study utilized Age-Standardized Rate (ASR) to mitigate the impact of population age structure, thereby enhancing the comparability of LOCC burden across different regions (9). The precision of ASR estimates was further quantified using 95% Uncertainty Intervals (UI) (9). Additionally, to assess the trend in the burden of LOCC from 1990 to 2021, the Estimate Annual Percentage Change (EAPC) was employed. EAPC is a statistical measure that quantifies the change in disease incidence or mortality over time, calculated using the formula 100×(exp(β)−1), where β represents the coefficient of the time variable in a linear regression model. The EAPC results provide the average annual percentage change, with positive values indicating an increase over time and negative values indicating a decrease (11, 12). The 95% Confidence Interval (CI) reflects the uncertainty around the EAPC estimate typically (11, 12).
Subsequently, to explore the disease burden trends of LOCC in the next nine years, we employed the Bayesian age-period-cohort (BAPC) model to project the LOCC burden up to 2030. This model integrates three principal dimensions (age effects), period effects, and cohort effects. Utilizing a Bayesian statistical framework, the BAPC model allows researchers to incorporate prior knowledge and quantify uncertainty within the model. The Bayesian approach, by combining data information with prior distributions to generate posterior distributions, provides more precise parameter estimates. The BAPC model not only describes historical trends but also predicts future disease burden. Compared with traditional epidemiological models, the BAPC model offers a more comprehensive consideration of the various factors influencing disease trends, providing a more detailed and dynamic view of disease burden. Additionally, the Bayesian nature of the model enables the quantification of uncertainty, which enhances the interpretability and credibility of the results (13, 14).
Results
The burden of LOCC from 1990 to 2021
Globally, compared to 1990, the number of LOCC cases or years in terms of Incidence, Prevalence, Death, DALYs, YLLs, and YLDs had increased several-fold in 2021. However, the number only provides a rudimentary snapshot of the LOCC burden at different time points. Therefore, this study employed ASR to compare the current burden of LOCC across different regions. In 2021, the age-standardized prevalence rate (ASPR) and the age-standardized rate of YLDs were highest in Australasia, with High-income North America and South Asia following closely behind. However, the highest age-standardized incidence rate (ASIR), age-standardized death rate (ASDR), age-standardized rate of DALYs, and YLLs were all observed in South Asia. Focusing solely on 2021, LOCC patients in three regions, including Australasia, had longer survival durations and later time points of death. Notably, the ASDR in South Asia was more than four times that of Australasia. Thus, the burden of LOCC in South Asia remains the most severe (Table 1–6).
Table 1
| Locations | 1990 Number (95% UI, cases) |
1990 Age-standardized rate (95% UI, per 100,000) | 2021 Number (95% UI, cases) |
2021 Age-standardized rate (95% UI, per 100,000) | Estimated annual percentage change (95% CI, 100%) |
|---|---|---|---|---|---|
| Both sexes | Incidence | ||||
| Global | 174077 (167404-181621) | 4.3 (4.1-4.5) | 421577 (389878-449782) | 4.9 (4.5-5.2) | 0.3981 (0.3332-0.4631) |
| High-middle SDI | 36685 (35237-38039) | 3.6 (3.5-3.8) | 75381 (68753.5-81578) | 3.9 (3.5-4.2) | 0.1374 (0.044-0.2308) |
| High SDI | 58203 (56115-59655) | 5.4 (5.3-5.6) | 104871 (97792-109602) | 5.4 (5.1-5.7) | 0.0629 (0.0028-0.1231) |
| Low-middle SDI | 35520 (31899-39325) | 5.4 (4.9-6.0) | 102039 (90115-113221) | 6.7 (6.0-7.5) | 0.6426 (0.559-0.7263) |
| Low SDI | 9501 (8202-10847) | 3.9 (3.4-4.4) | 25089 (21421-28947) | 4.6 (3.9-5.2) | 0.3313 (0.2285-0.4342) |
| Middle SDI | 33981 (31865-36099) | 3.1 (2.9-3.3) | 113857 (102889-125357) | 4.2 (3.8-4.6) | 0.8903 (0.7929-0.9877) |
| Andean Latin America | 283 (247-322) | 1.3 (1.2-1.5) | 945 (752-1166) | 1.6 (1.3-1.9) | 0.6085 (0.4407-0.7766) |
| Australasia | 1692 (1555-1832) | 7.3 (6.7-7.9) | 3469 (3088-3840) | 7.0 (6.3-7.7) | -0.1487 (-0.3425-0.0453) |
| Caribbean | 1069 (1002-1143) | 4.1 (3.8-4.4) | 2111 (1823-2406) | 3.9 (3.4-4.5) | 0.0733 (-0.0339-0.1806) |
| Central Asia | 1264 (1176-1371) | 2.6 (2.4-2.8) | 2057 (1800-2354) | 2.4 (2.1-2.7) | -0.1940 (-0.4477-0.0604) |
| Central Europe | 6364 (6075-6683) | 4.3 (4.1-4.5) | 11404 (10501-12286) | 5.6 (5.2-6.1) | 0.8003 (0.6951-0.9056) |
| Central Latin America | 1530 (1477-1576) | 1.8 (1.8-1.9) | 4442 (3946-4965) | 1.8 (1.6-2.0) | -0.2814 (-0.3885--0.1743) |
| Central Sub-Saharan Africa | 464 (357-601) | 2.0 (1.6-2.5) | 1307 (996-1674) | 2.2 (1.7-2.8) | 0.3127 (0.1506-0.475) |
| East Asia | 16020 (13746-18301) | 1.8 (1.5-2.0) | 63514 (51900-77072) | 2.9 (2.4-3.5) | 1.8681 (1.7032-2.0333) |
| Eastern Europe | 13201 (12692-13983) | 4.7 (4.6-5.0) | 21039 (19042-23091) | 6.5 (5.9-7.1) | 0.6676 (0.4681-0.8675) |
| Eastern Sub-Saharan Africa | 2582 (2247-2946) | 3.2 (2.8-3.7) | 6336 (5060-7633) | 3.4 (2.8-4.0) | 0.0284 (-0.0526-0.1095) |
| High-income Asia Pacific | 5917 (5642-6147) | 2.9 (2.8-3.1) | 18189 (15884-19823) | 4.2 (3.8-4.5) | 1.0902 (0.7726-1.4088) |
| High-income North America | 24125 (23178-24789) | 7.2 (6.9-7.4) | 36565 (34331-38154) | 5.9 (5.5-6.1) | -0.6355 (-0.7335--0.5374) |
| North Africa and Middle East | 1836 (1615-2089) | 1.1 (0.9-1.2) | 6327 (5580-7234) | 1.3 (1.2-1.5) | 0.8392 (0.7803-0.8981) |
| Oceania | 60 (43-76) | 1.9 (1.4-2.3) | 183 (135-236) | 2.2 (1.6-2.8) | 0.6785 (0.5818-0.7753) |
| South Asia | 49608 (44763-54895) | 7.9 (7.1-8.7) | 152646 (131077-170703) | 9.8 (8.5-10.9) | 0.5662 (0.4527-0.6798) |
| Southeast Asia | 9187 (8040-10245) | 3.5 (3.1-3.9) | 27647 (23814-31578) | 4.2 (3.6-4.8) | 0.4198 (0.3705-0.4691) |
| Southern Latin America | 1361 (1247-1482) | 2.9 (2.7-3.2) | 2177 (1970-2383) | 2.6 (2.3-2.8) | -0.1705 (-0.4026-0.0622) |
| Southern Sub-Saharan Africa | 1137 (877-1347) | 3.9 (3.0-4.7) | 2506 (2208-2801) | 4.1 (3.6-4.5) | -0.0300 (-0.1748-0.1151) |
| Tropical Latin America | 3438 (3267-3601) | 3.6 (3.4-3.8) | 9814 (9161-10427) | 3.8 (3.5-4.0) | 0.0724 (-0.0283-0.1733) |
| Western Europe | 31991(30658-33257) | 6.1 (5.8-6.3) | 46069 (42748-48717) | 5.6 (5.3-5.9) | -0.1889 (-0.2550--0.1228) |
| Western Sub-Saharan Africa | 940 (761-1099) | 1.0 (0.8-1.2) | 2819 (2216-3442) | 1.3 (1.1-1.6) | 0.8038 (0.7445-0.8632) |
| Female | Incidence | ||||
| Global | 55690 (52276-59041) | 2.6 (2.4-2.7) | 148660 (135703-160404) | 3.3 (3.0-3.5) | 0.6907 (0.6121-0.7695) |
| High-middle SDI | 8939 (8357-9492) | 1.6 (1.5-1.7) | 22516 (20180-24622) | 2.2 (1.9-2.4) | 0.9264 (0.8395-1.0134) |
| High SDI | 17964 (16803-18604) | 2.9 (2.8-3.0) | 36045 (31689-38609) | 3.4 (3.1-3.6) | 0.5455 (0.4696-0.6214) |
| Low-middle SDI | 13621 (11888-15392) | 4.2 (3.6-4.7) | 43158 (37580-49407) | 5.5 (4.8-6.3) | 0.8052 (0.6984-0.9121) |
| Low SDI | 3756 (3114-4364) | 3.1 (2.6-3.6) | 10593 (8941-12392) | 3.8 (3.2-4.4) | 0.4361 (0.3124-0.5598) |
| Middle SDI | 11359 (10459-12230) | 2.1 (1.9-2.2) | 36244 (32427-40239) | 2.6 (2.3-2.9) | 0.5103 (0.3879-0.633) |
| Andean Latin America | 133 (115-151) | 1.2 (1.1-1.4) | 503 (398-630) | 1.6 (1.3-2.0) | 0.8642 (0.6851-1.0437) |
| Australasia | 530 (480-568) | 4.2 (3.8-4.5) | 1194 (1042-1325) | 4.5 (4.0-5.0) | 0.2746 (0.0343-0.5155) |
| Caribbean | 324 (304-346) | 2.4 (2.2-2.6) | 598 (523-679) | 2.1 (1.8-2.4) | -0.2869 (-0.4151--0.1584) |
| Central Asia | 402 (367-443) | 1.4 (1.3-1.6) | 803 (695-912) | 1.7 (1.5-1.9) | 0.5910 (0.2850-0.8980) |
| Central Europe | 1399 (1332-1463) | 1.7 (1.6-1.8) | 3056 (2779-3306) | 2.6 (2.4-2.8) | 1.4885 (1.4116-1.5654) |
| Central Latin America | 646 (619-669) | 1.5 (1.4-1.5) | 1999 (1747-2258) | 1.5 (1.3-1.7) | -0.0801 (-0.2099-0.0499) |
| Central Sub-Saharan Africa | 193 (143-251) | 1.6 (1.1-2.1) | 546 (372-794) | 1.7 (1.2-2.6) | 0.2725 (0.1444-0.4008) |
| East Asia | 5591 (4605-6680) | 1.2 (1.0-1.5) | 15657 (12336-19421) | 1.4 (1.1-1.8) | 0.3401 (0.1486-0.532) |
| Eastern Europe | 2917 (2720-3084) | 1.7 (1.6-1.8) | 5840 (5232-6534) | 3.0 (2.7-3.4) | 1.7539 (1.5160-1.9923) |
| Eastern Sub-Saharan Africa | 969 (836-1155) | 2.4 (2.1-2.8) | 2449 (2005-2989) | 2.5 (2.1-3.0) | -0.0108 (-0.1210-0.0996) |
| High-income Asia Pacific | 2176 (2003-2313) | 2.0 (1.8-2.1) | 7229 (5701-8207) | 2.9 (2.5-3.2) | 1.2882 (0.9727-1.6046) |
| High-income North America | 8515 (7922-8845) | 4.4 (4.1-4.5) | 12620 (11417-13369) | 3.8 (3.5-4.0) | -0.5690 (-0.6747--0.4631) |
| North Africa and Middle East | 735 (640-845) | 0.9 (0.7-1.0) | 2735 (2396-3147) | 1.2 (1.0-1.3) | 1.2730 (1.1681-1.3781) |
| Oceania | 22 (16-29) | 1.4 (1.1-1.9) | 65 (49-86) | 1.7 (1.3-2.2) | 0.5348 (0.4427-0.6270) |
| South Asia | 17783 (15343-20148) | 5.9 (5.1-6.7) | 60219 (52360-69313) | 7.7 (6.7-8.8) | 0.6734 (0.5205-0.8265) |
| Southeast Asia | 3971 (3380-4511) | 2.9 (2.5-3.3) | 11125 (9383-13161) | 3.3 (2.8-3.9) | 0.0901 (0.0050-0.1753) |
| Southern Latin America | 332 (311-351) | 1.3 (1.2-1.4) | 760 (691-824) | 1.6 (1.4-1.7) | 1.0493 (0.8027-1.2965) |
| Southern Sub-Saharan Africa | 330 (271-395) | 2.0 (1.7-2.5) | 848 (749-961) | 2.5 (2.2-2.8) | 0.8037 (0.6012-1.0065) |
| Tropical Latin America | 819 (770-855) | 1.7 (1.6-1.8) | 2777 (2534-2943) | 2.0 (1.8-2.1) | 0.3208 (0.1954-0.4464) |
| Western Europe | 7366 (6906-7654) | 2.4 (2.3-2.5) | 15947 (14137-17124) | 3.5 (3.2-3.7) | 1.4558 (1.3099-1.6020) |
| Western Sub-Saharan Africa | 528 (418-631) | 1.2 (0.9-1.4) | 1681 (1300-2142) | 1.5 (1.2-1.9) | 0.8315 (0.7870-0.8761) |
| Male | Incidence | ||||
| Global | 118387 (112776-124445) | 6.2 (5.9-6.5) | 272917 (245321-296015) | 6.7 (6.0-7.2) | 0.2294 (0.1648-0.2941) |
| High-middle SDI | 27745 (26682-28937) | 6.1 (5.8-6.3) | 52865 (47657-58782) | 5.8 (5.3-6.5) | -0.2089 (-0.3050--0.1127) |
| High SDI | 40238 (38980-41402) | 8.5 (8.2-8.7) | 68826 (65517-71809) | 7.7 (7.3-8.0) | -0.2540 (-0.3085--0.1995) |
| Low-middle SDI | 21899 (18789-25089) | 6.6 (5.6-7.5) | 58881 (48621-67462) | 8.0 (6.7-9.1) | 0.5842 (0.5139-0.6546) |
| Low SDI | 5744 (4716-6786) | 4.7 (3.9-5.6) | 14496 (11581-17286) | 5.4 (4.3-6.4) | 0.2913 (0.2007-0.3819) |
| Middle SDI | 22621 (20849-24615) | 4.2 (3.9-4.6) | 77613 (66548-87891) | 5.9 (5.1-6.7) | 1.1157 (1.0162-1.2152) |
| Andean Latin America | 150 (128-176) | 1.5 (1.2-1.7) | 442 (348-558) | 1.6 (1.2-2.0) | 0.3509 (0.1690-0.5330) |
| Australasia | 1161 (1025-1307) | 10.8 (9.6-12.2) | 2274 (1965-2614) | 9.7 (8.4-11.1) | -0.3813 (-0.5588--0.2035) |
| Caribbean | 744 (685-809) | 5.9 (5.5-6.4) | 1513 (1293-1748) | 6.0 (5.1-6.9) | 0.2477 (0.1114-0.3842) |
| Central Asia | 861 (801-938) | 4.2 (3.9-4.6) | 1254 (1091-1449) | 3.3 (2.9-3.8) | -0.6827 (-0.9341--0.4307) |
| Central Europe | 4964 (4724-5251) | 7.5 (7.1-7.9) | 8348 (7598-9112) | 9.1 (8.3-10.0) | 0.5412 (0.4101-0.6726) |
| Central Latin America | 883 (847-921) | 2.2 (2.1-2.3) | 2443 (2138-2752) | 2.1 (1.9-2.4) | -0.3947 (-0.5126--0.2767) |
| Central Sub-Saharan Africa | 270 (199-399) | 2.5 (1.9-3.5) | 761 (572-993) | 2.8 (2.1-3.6) | 0.3741 (0.2004-0.5482) |
| East Asia | 10429 (8674-12391) | 2.4 (2.0-2.8) | 47856 (37470-60188) | 4.6 (3.6-5.7) | 2.4966 (2.3051-2.6885) |
| Eastern Europe | 10284 (9842-11040) | 9.3 (8.9-9.9) | 15198 (13344-17068) | 11.0 (9.7-12.4) | 0.2457 (0.0599-0.4319) |
| Eastern Sub-Saharan Africa | 1613 (1355-1864) | 4.1 (3.4-4.7) | 3887 (2987-4749) | 4.4 (3.5-5.3) | 0.1274 (0.0665-0.1882) |
| High-income Asia Pacific | 3741 (3584-3897) | 4.2 (4.0-4.4) | 10959 (9948-11869) | 5.7 (5.2-6.2) | 0.8593 (0.5371-1.1826) |
| High-income North America | 15610 (15137-16027) | 10.6 (10.2-10.8) | 23944 (22612-25016) | 8.2 (7.8-8.6) | -0.7420 (-0.8528--0.6311) |
| North Africa and Middle East | 1101 (929-1290) | 1.2 (1.0-1.5) | 3591 (3103-4115) | 1.5 (1.3-1.7) | 0.5225 (0.4813-0.5638) |
| Oceania | 38 (26-49) | 2.3 (1.6-2.9) | 118 (84-153) | 2.7 (1.9-3.5) | 0.7578 (0.6574-0.8584) |
| South Asia | 31824 (27673-36043) | 9.7 (8.3-11.0) | 92426 (73789-107477) | 12.0 (9.6-13.9) | 0.5758 (0.4880-0.6637) |
| Southeast Asia | 5216 (4461-5961) | 4.2 (3.6-4.7) | 16522 (13976-19047) | 5.2 (4.4-6.0) | 0.6546 (0.6157-0.6936) |
| Southern Latin America | 1028 (919-1148) | 4.8 (4.3-5.4) | 1416 (1235-1613) | 3.7 (3.2-4.2) | -0.6689 (-0.9129--0.4242) |
| Southern Sub-Saharan Africa | 806 (586-996) | 6.3 (4.5-7.8) | 1658 (1411-1863) | 6.2 (5.3-6.9) | -0.3475 (-0.5148--0.1799) |
| Tropical Latin America | 2618 (2473-2758) | 5.7 (5.4-6.0) | 7036 (6543-7597) | 5.9 (5.4-6.3) | 0.0427 (-0.0673-0.1529) |
| Western Europe | 24624 (23573-25815) | 10.4(10.0-10.9) | 30121 (27818-32159) | 7.9 (7.4-8.5) | -0.8810 (-0.9396--0.8224) |
| Western Sub-Saharan Africa | 411 (326-502) | 0.9 (0.7-1.0) | 1138 (868-1421) | 1.1 (0.8-1.3) | 0.6852 (0.5952-0.7753) |
Changes in lip and oral cavity cancer Incidence by regions and sexes.
Table 2
| Locations | 1990 Number (95% UI, cases) |
1990 Age-standardized rate (95% UI, per 100,000) | 2021 Number (95% UI, cases) |
2021 Age-standardized rate (95% UI, per 100,000) | Estimated annual percentage change (95% CI, 100%) |
|---|---|---|---|---|---|
| Both sexes | |||||
| Global | 97402 (92506-102361) | 2.5 (2.3-2.6) | 208379 (191288-224162) | 2.4 (2.2-2.6) | -0.1142 (-0.1675--0.0608) |
| High-middle SDI | 19478 (18676-20329) | 2.0 (1.9-2.1) | 31196 (28448-33893) | 1.6 (1.5-1.7) | -0.8570 (-0.9267--0.7872) |
| High SDI | 20812 (19950-21348) | 1.9 (1.8-2.0) | 31747 (29014-33462) | 1.5 (1.4-1.6) | -0.7532 (-0.8076--0.6988) |
| Low-middle SDI | 26672 (23882-29567) | 4.3 (3.8-4.7) | 67360 (59761-74529.) | 4.7 (4.1-5.1) | 0.1991 (0.1431-0.2551) |
| Low SDI | 7278 (6331-8263) | 3.2 (2.8-3.6) | 17333 (14819-19852) | 3.4 (2.9-3.9) | 0.0747 (-0.0083-0.1578) |
| Middle SDI | 23048 (21514-24578) | 2.3 (2.1-2.4) | 60565 (54822-66426) | 2.3 (2.1-2.5) | -0.0579 (-0.1052--0.0106) |
| Andean Latin America | 206 (179-235) | 1.0 (0.9-1.2) | 537 (426-658) | 0.9 (0.7-1.1) | -0.2902 (-0.4251--0.1552) |
| Australasia | 420 (391-448) | 1.8 (1.7-1.9) | 720 (643-793) | 1.3 (1.2-1.5) | -0.9718 (-1.2489--0.6940) |
| Caribbean | 664 (620-715) | 2.6 (2.5-2.8) | 1202 (1041-1376) | 2.2 (1.9-2.5) | -0.3013 (-0.4092--0.1932) |
| Central Asia | 894 (828-973) | 1.9 (1.7-2.0) | 1284 (1124-1460) | 1.6 (1.4-1.8) | -0.6121 (-0.7923--0.4315) |
| Central Europe | 4116 (3937-4305) | 2.8 (2.7-3.0) | 6001 (5520-6457) | 2.9 (2.7-3.1) | 0.014 (-0.0592-0.0873) |
| Central Latin America | 1052 (1014-1084) | 1.3 (1.3-1.4) | 2553 (2271-2856) | 1.0 (0.9-1.2) | -0.9621 (-1.0695--0.8546) |
| Central Sub-Saharan Africa | 366 (285-474) | 1.7 (1.4-2.1) | 951 (721-1223) | 1.8 (1.3-2.3) | 0.1094 (0.0010-0.2179) |
| East Asia | 10468 (8942-11942) | 1.2 (1.1-1.4) | 26513 (21531-32205) | 1.2 (1.0-1.5) | 0.0767 (-0.0391-0.1926) |
| Eastern Europe | 7191 (6920-7572) | 2.6 (2.5-2.7) | 9009 (8172-9925) | 2.7 (2.4-3.0) | -0.3604 (-0.5531--0.1673) |
| Eastern Sub-Saharan Africa | 2016 (1768-2307) | 2.7 (2.4-3.1) | 4492 (3620-5418) | 2.6 (2.1-3.1) | -0.198 (-0.2449--0.1511) |
| High-income Asia Pacific | 1976 (1872-2048) | 1.0 (0.9-1.0) | 5917 (4977-6492) | 1.1 (1.0-1.2) | 0.0541 (-0.2924-0.4017) |
| High-income North America | 6809 (6495-7009) | 2.0 (1.9-2.0) | 8855 (8160-9270) | 1.3 (1.2-1.4) | -1.2256 (-1.3958--1.0551) |
| North Africa and Middle East | 1201 (1048-1361) | 0.7 (0.6-0.8) | 3089 (2728-3518) | 0.7 (0.6-0.8) | -0.1222 (-0.1652--0.0791) |
| Oceania | 40 (29-51) | 1.4 (1.0-1.7) | 120 (87-155) | 1.6 (1.2-2.0) | 0.6374 (0.5483-0.7265) |
| South Asia | 36681 (32922-40660) | 6.2 (5.5-6.9) | 97154 (84355-108404) | 6.5 (5.7-7.) | 0.0274 (-0.0546-0.1095) |
| Southeast Asia | 6096 (5308-6820) | 2.5 (2.2-2.8) | 15400 (13307-17498) | 2.5 (2.2-2.8) | -0.1751 (-0.2264--0.1238) |
| Southern Latin America | 788 (723-860) | 1.7 (1.6-1.9) | 1074 (975-1170) | 1.2 (1.1-1.3) | -0.7292 (-0.9522--0.5057) |
| Southern Sub-Saharan Africa | 771 (587-923) | 2.8 (2.1-3.4) | 1605 (1417-1788) | 2.7 (2.4-3.0) | -0.2362 (-0.4675--0.0043) |
| Tropical Latin America | 2310 (2193-2425) | 2.5 (2.4-2.7) | 5714 (5312-6066) | 2.2 (2.1-2.3) | -0.4524 (-0.5593--0.3454) |
| Western Europe | 12607 (12109-13022) | 2.3 (2.2-2.4) | 14227 (12881-15084) | 1.5 (1.4-1.6) | -1.2628 (-1.3406--1.1850) |
| Western Sub-Saharan Africa | 719 (586-841) | 0.8 (0.7-2.0) | 1955 (1557-2358) | 1.0 (0.8-1.2) | 0.5845 (0.5317-0.6373) |
| Female | |||||
| Global | 30412 (28095-32661) | 1.4 (1.3-1.6) | 71488 (64699-78442) | 1.6 (1.4-1.7) | 0.1424 (0.0649-0.2199) |
| High-middle SDI | 4764 (4441-5084) | 0.9 (0.8-0.9) | 8753 (7833-9480) | 0.8 (0.7-0.9) | -0.4395 (-0.5133--0.3657) |
| High SDI | 6154 (5666-6398) | 1.0 (0.9-1.0) | 10845 (9172-11834) | 0.9 (0.8-0.9) | -0.3224 (-0.3966--0.2481) |
| Low-middle SDI | 9638 (8334-10938) | 3.2 (2.7-3.6) | 26857 (23443-30604) | 3.6 (3.2-4.1) | 0.3532 (0.2677-0.4387) |
| Low SDI | 2715 (2268-3167) | 2.4 (2.0-2.8) | 6875 (5882-8044) | 2.7 (2.3-3.1) | 0.1918 (0.0865-0.2972) |
| Middle SDI | 7112 (6553-7662) | 1.4 (1.3-1.5) | 18106 (16077-20180) | 1.3 (1.2-1.5) | -0.4032 (-0.4804--0.3259) |
| Andean Latin America | 92 (81-105) | 0.9 (0.8-1.0) | 271 (216-337) | 0.9 (0.7-1.1) | -0.1211 (-0.2697-0.0278) |
| Australasia | 135 (124-144) | 1.0 (0.9-1.1) | 251 (210-279) | 0.8 (0.7-0.9) | -0.6814 (-0.9861--0.3758) |
| Caribbean | 191 (179-204) | 1.5 (1.4-1.6) | 335 (294-384) | 1.1 (1.0-1.3) | -0.6148 (-0.7389--0.4906) |
| Central Asia | 268 (239-299) | 1.0 (0.9-1.1) | 457 (399-517) | 1.0 (0.9-1.1) | 0.0705 (-0.1610-0.3024) |
| Central Europe | 839 (801-880) | 1.0 (1.0-1.1) | 1486 (1338-1604) | 1.2 (1.1-1.3) | 0.5257 (0.4347-0.6167) |
| Central Latin America | 423 (405-439) | 1.1 (1.0-1.1) | 1083 (948-1212) | 0.8 (0.7-0.9) | -0.8609 (-1.0029--0.7187) |
| Central Sub-Saharan Africa | 145 (108-189) | 1.3 (1.0-1.7) | 379 (254-551) | 1.3 (0.9-2.0) | 0.0417 (-0.0280-0.1115) |
| East Asia | 3333 (2755-3961) | 0.8 (0.7-0.9) | 5742 (4554-7078) | 0.5 (0.4-0.6) | -1.7080 (-1.8764--1.5394) |
| Eastern Europe | 1541 (1450-1615) | 0.9 (0.8-0.9) | 2338 (2096-2604) | 1.1 (1.0-1.2) | 0.4123 (0.2722-0.5525) |
| Eastern Sub-Saharan Africa | 714 (616-854) | 1.9 (1.2-2.3) | 1622 (1340-1960) | 1.8 (1.5-2.2) | -0.2713 (-0.3419--0.2007) |
| High-income Asia Pacific | 691 (629-728) | 0.6 (0.6-0.7) | 2670 (1997-3098) | 0.8 (0.6-0.9) | 0.3256 (-0.0301-0.6825) |
| High-income North America | 2386 (2174-2497) | 1.2 (1.1-1.2) | 3011 (2628-3222) | 0.8 (0.7-0.9) | -1.2177 (-1.3831--1.0520) |
| North Africa and Middle East | 453 (390-517) | 0.6 (0.5-0.7) | 1234 (1085-1402) | 0.6 (0.5-0.7) | 0.2767 (0.1808-0.3726) |
| Oceania | 12 (9-16) | 1.0 (0.7-1.2) | 37 (28-49) | 1.1 (0.8-1.4) | 0.5564 (0.4855-0.6273) |
| South Asia | 12410 (10628-14112) | 4.5 (3.7-5.1) | 36201 (31470-41708) | 4.8 (4.2-5.6) | 0.1190 (-0.0025-0.2407) |
| Southeast Asia | 2393 (2055-2724) | 1.9 (1.7-2.2) | 5768 (4856-6823) | 1.8 (1.5-2.1) | -0.4598 (-0.5641--0.3554) |
| Southern Latin America | 197 (183-207) | 0.8 (0.7-0.8) | 382 (343-413) | 0.7 (0.7-0.8) | 0.3250 (0.0915-0.5591) |
| Southern Sub-Saharan Africa | 210 (171-255) | 1.4 (1.1-1.7) | 518 (460-584) | 1.6 (1.4-1.8) | 0.5812 (0.3059-0.8574) |
| Tropical Latin America | 539 (503-565) | 1.2 (1.1-1.3) | 1570 (1410-1677) | 1.1 (1.0-1.2) | -0.3237 (-0.4545--0.1928) |
| Western Europe | 3036 (2804-3161) | 0.9 (0.8-0.9) | 4997 (4261-5434) | 0.9 (0.8-1.0) | 0.1425 (0.0588-0.2262) |
| Western Sub-Saharan Africa | 393 (311-471) | 0.9 (0.7-1.1) | 1127 (890-1425) | 1.1 (0.9-1.4) | 0.6491 (0.5864-0.7118) |
| Male | |||||
| Global | 66990 (62782-71608) | 3.6 (3.4-3.9) | 136890 (120655-149372) | 3.4 (3.0-3.7) | -0.2789 (-0.3244--0.2334) |
| High-middle SDI | 14714 (14079-15385) | 3.4 (3.2-3.5) | 22443 (20142-24822) | 2.5 (2.3-2.8) | -1.0733 (-1.1405--1.006) |
| High SDI | 14657 (14191-15051) | 3.2 (3.0-3.2) | 20902 (19819-21889) | 2.3 (2.1-2.4) | -1.0570 (-1.1120--1.0020) |
| Low-middle SDI | 17034 (14536-19575) | 5.4 (4.6-6.2) | 40502 (33644-46284) | 5.8 (4.8-6.6) | 0.1638 (0.1226-0.2050) |
| Low SDI | 4562 (3778-5393) | 3.9 (3.3-4.7) | 10457 (8399-12440) | 4.1 (3.3-4.9) | 0.0369 (-0.0350-0.1088) |
| Middle SDI | 15935 (14660-17390) | 3.2 (2.9-3.5) | 42458 (36636-47416) | 3.3 (2.9-3.7) | 0.1388 (0.0926-0.1849) |
| Andean Latin America | 113 (96-133) | 1.2 (1.0-1.4) | 266 (211-334) | 1.0 (0.8-1.2) | -0.4436 (-0.5954--0.2915) |
| Australasia | 284 (257-313) | 2.7 (2.5-3.0) | 468 (408-529) | 1.9 (1.7-2.1) | -1.1781 (-1.4448--0.9107) |
| Caribbean | 473 (437-518) | 3.9 (3.6-4.2) | 866 (737-1007) | 3.4 (2.9-4.0) | -0.1469 (-0.2787--0.0149) |
| Central Asia | 625 (582-683) | 3.2 (3.0-3.5) | 827 (722-952) | 2.3 (2.0-2.6) | -1.0245 (-1.2088--0.8399) |
| Central Europe | 3277 (3119-3450) | 5.1 (4.8-5.3) | 4515 (4144-4895) | 4.9 (4.5-5.4) | -0.1864 (-0.2846--0.0881) |
| Central Latin America | 628 (602-653) | 1.6 (1.6-1.7) | 1469 (1286-1657) | 1.3 (1.1-1.5) | -0.9860 (-1.099--0.8729) |
| Central Sub-Saharan Africa | 220 (162-322) | 2.1 (1.6-3.0) | 572 (429-749) | 2.3 (1.8-2.9) | 0.2063 (0.0856-0.3272) |
| East Asia | 7135 (5907-8495) | 1.8 (1.5-2.1) | 20770 (16201-26057) | 2.1 (1.6-2.6) | 0.7324 (0.5876-0.8775) |
| Eastern Europe | 5649 (5405-6018) | 5.3 (5.1-5.7) | 6670 (5872-7520) | 4.8 (4.3-5.5) | -0.7124 (-0.9048--0.5197) |
| Eastern Sub-Saharan Africa | 1302 (1103-1522) | 3.5 (2.9-4.0) | 2869 (2234-3500) | 3.5 (2.8-4.2) | -0.0706 (-0.1045--0.0366) |
| High-income Asia Pacific | 1285 (1241.4-1327) | 1.5 (1.4-1.5) | 3246 (2971-3434) | 1.6 (1.4-1.6) | -0.2271 (-0.5713-0.1183) |
| High-income North America | 4423 (4283-4542) | 3.0 (2.9-3.1) | 5844 (5475-6103) | 2.0 (1.8-2.1) | -1.3253 (-1.5100--1.1404) |
| North Africa and Middle East | 748 (625-881) | 0.9 (0.8-1.1) | 1855 (1612-2123) | 0.8 (0.7-0.9) | -0.3956 (-0.4495--0.3417) |
| Oceania | 27 (19-36) | 1.8 (1.2-2.3) | 82 (58-108) | 2.0 (1.5-2.7) | 0.6716 (0.5714-0.7719) |
| South Asia | 24271 (21049-27547) | 7.8 (6.7-8.9) | 60952 (49383-70777) | 8.3 (6.7-9.5) | 0.0639 (0.0022-0.1255) |
| Southeast Asia | 3702 (3167-4226) | 3.2 (2.7-3.6) | 9632 (8243-11109) | 3.2 (2.8-3.7) | 0.0123 (-0.0128-0.0374) |
| Southern Latin America | 591 (528-661) | 2.9 (2.6-3.2) | 691 (609-782) | 1.8 (1.6-2.0) | -1.1603 (-1.3943--0.9256) |
| Southern Sub-Saharan Africa | 560 (405-694) | 4.6 (3.3-5.7) | 1086 (930-1218) | 4.3 (3.7-4.8) | -0.5300 (-0.776--0.2834) |
| Tropical Latin America | 1771 (1675-1867) | 4.1 (3.8-4.3) | 4143 (3858-4452) | 3.5 (3.3-3.8) | -0.4345 (-0.5494--0.3195) |
| Western Europe | 9570 (9164-9940) | 4.1 (3.9-4.2) | 9230 (8525-9803) | 2.3 (2.1-2.4) | -1.8678 (-1.9557--1.7799) |
| Western Sub-Saharan Africa | 325 (257-396) | 0.7 (0.6-0.9) | 828 (642-1033) | 0.8 (0.7-1.0) | 0.4618 (0.3889-0.5348) |
Changes in lip and oral cavity cancer Deaths by regions and sexes.
Table 3
| Locations | 1990 Number (95% UI, cases) |
1990 Age-standardized rate (95% UI, per 100,000) | 2021 Number (95% UI, cases) |
2021 Age-standardized rate (95% UI, per 100,000) | Estimated annual percentage change (95% CI, 100%) |
|---|---|---|---|---|---|
| Both sexes | |||||
| Global | 587479 (568848-605472) | 13.9 (13.4-14.3) | 1538007 (1435013-1633910) | 17.7 (16.5-18.8) | 0.8167 (0.7644-0.869) |
| High-middle SDI | 119288 (114980-123539) | 11.5 (11.1-11.9) | 291257 (266249-315946) | 15.1 (13.9-16.4) | 0.9095 (0.8257-0.9934) |
| High SDI | 265628 (256944-271581) | 25.1 (24.4-25.7) | 497975 (472450-517411) | 27.3 (26.1-28.3) | 0.3903 (0.3151-0.4656) |
| Low-middle SDI | 85381 (77410-94379) | 11.7 (10.6-12.9) | 287203 (251575-320280) | 17.7 (15.6-19.6) | 1.2932 (1.1636-1.4230) |
| Low SDI | 21900 (18812-25057) | 8.0 (6.9-9.1) | 67580 (57110-79277) | 10.8 (9.2-12.5) | 0.8007 (0.6576-0.944) |
| Middle SDI | 94680 (88988-100398) | 7.8 (7.3-8.3) | 392726 (354064-434502) | 13.9 (12.6-15.4) | 1.8834 (1.7527-2.0142) |
| Andean Latin America | 718 (625-813) | 3.1 (2.7-3.5) | 3158 (2493-3920) | 5.1 (4.0-6.4) | 1.8574 (1.6934-2.0215) |
| Australasia | 8540 (7867-9235) | 37.2 (34.3-40.3) | 19360 (17292-21470) | 40.6 (36.6-44.8) | 0.3218 (0.1694-0.4743) |
| Caribbean | 3164 (2979-3356) | 11.7 (11.0-12.4) | 7054 (6075-8094) | 13.1 (11.3-15.1) | 0.6574 (0.5381-0.7768) |
| Central Asia | 3584 (3358-3873) | 7.0 (6.6-7.6) | 6703 (5856-7588) | 7.4 (6.5-8.3) | 0.2509 (-0.0929-0.5958) |
| Central Europe | 19525 (18539-20432) | 13.2 (12.5-13.8) | 42578 (38925-46197) | 21.8 (19.9-23.7) | 1.5905 (1.4366-1.7446) |
| Central Latin America | 4135 (3997-4264) | 4.4 (4.3-4.5) | 14706 (13022-16593) | 5.7 (5.1-6.4) | 0.7209 (0.635-0.8069) |
| Central Sub-Saharan Africa | 1043 (794-1356) | 3.8 (3.0-4.9) | 3470 (2626-4487) | 5.0 (3.8-6.4) | 0.8411 (0.593-1.0898) |
| East Asia | 45700 (39379-51927) | 4.6 (3.9-5.2) | 250064 (206079-300702) | 11.4 (9.5-13.7) | 3.3177 (3.1823-3.4533) |
| Eastern Europe | 32742 (31288-35020) | 11.8 (11.3-12.7) | 61763 (55837-67693) | 19.6 (17.8-21.5) | 1.4589 (1.2156-1.7027) |
| Eastern Sub-Saharan Africa | 5856 (5113-6673) | 6.5 (5.7-7.3) | 17283 (13570-21137) | 8.0 (6.4-9.6) | 0.5903 (0.4352-0.7457) |
| High-income Asia Pacific | 20976 (20119-21796) | 10.2 (9.8-10.6) | 60153 (54034-65073) | 16.8 (15.3-18.0) | 1.7110 (1.3867-2.0363) |
| High-income North America | 123452 (119575-126380) | 37.4 (36.3-38.2) | 197418 (187715-205139) | 32.6 (31.1-33.8) | -0.3975 (-0.4695--0.3255) |
| North Africa and Middle East | 5393 (4785-6218) | 2.7 (2.4-3.1) | 24545 (21526-28272) | 4.7 (4.1-5.4) | 1.8601 (1.7726-1.9476) |
| Oceania | 178 (129-226) | 4.7 (3.4-5.9) | 562 (420-721) | 5.8 (4.4-7.4) | 0.8092 (0.6957-0.9228) |
| South Asia | 122433 (111426-135083) | 17.4 (15.8-19.1) | 447882 (382112-503421) | 26.9 (23.1-30.2) | 1.3426 (1.1874-1.498) |
| Southeast Asia | 27164 (23868-30398) | 9.2 (8.1-10.3) | 98530 (84512-113952) | 13.9 (12.0-16.1) | 1.1642 (1.0764-1.2521) |
| Southern Latin America | 4177 (3837-4538) | 8.9 (8.2-9.6) | 7874 (7116-8644) | 9.5 (8.6-10.4) | 0.4896 (0.2321-0.7476) |
| Southern Sub-Saharan Africa | 3092 (2425-3626) | 9.8 (7.6-11.6) | 7127 (6250-8030) | 10.7 (9.4-12.0) | 0.1425 (0.0827-0.2023) |
| Tropical Latin America | 9497 (9032-9936) | 9.2 (8.7-9.6) | 32002 (30163-33901) | 12.1 (11.4-12.8) | 0.7947 (0.7004-0.889) |
| Western Europe | 143929 (138625-149532) | 28.2 (27.2-29.3) | 228216 (213878-240059) | 29.7 (28.1-31.1) | 0.2621 (0.1562-0.3681) |
| Western Sub-Saharan Africa | 2170 (1735-2552) | 2.1 (1.7-2.5) | 7548 (5755-9413) | 3.1 (2.4-3.7) | 1.1718 (1.0441-1.2997) |
| Female | |||||
| Global | 850043 (783392-917046) | 38.6 (35.6-41.7) | 1846853 (1681594-2028079) | 41 (37.6-45.4) | 0.0802 (-0.0104-0.1709) |
| High-middle SDI | 31653 (29797-33536) | 5.6 (5.3-6.0) | 100068 (90014-109916) | 9.9 (9.0-10.9) | 1.9178 (1.8475-1.9881) |
| High SDI | 82592 (78596-85170) | 14.0 (13.4-14.4) | 171808 (156304-181701) | 17.8 (16.6-18.7) | 0.9036 (0.8214-0.9858) |
| Low-middle SDI | 35062 (31040-39501) | 9.7 (8.5-10.9) | 129778 (112482-149017) | 15.5 (13.5-17.8) | 1.4644 (1.3225-1.6065) |
| Low SDI | 9284 (7751-10839) | 6.8 (5.6-7.9) | 30791 (25762-36369) | 9.6 (8.1-11.2) | 0.9086 (0.7521-1.0653) |
| Middle SDI | 34878 (32314-37569) | 5.7 (5.3-6.2) | 136584 (121840-151053) | 9.5 (8.5-10.5) | 1.4919 (1.3432-1.6409) |
| Andean Latin America | 2542 (2217-2889) | 21.9 (19.0-24.8) | 6535 (5189-8182) | 20.6 (16.4-25.8) | -0.2715 (-0.4313--0.1115) |
| Australasia | 2938 (2730-3108) | 23.8 (22.1-25.2) | 4647 (4067-5090) | 17.6 (15.8-19.2) | -0.8876 (-1.1778--0.5966) |
| Caribbean | 4664 (4367-5012) | 33.7 (31.7-36.2) | 7448 (6474-8626) | 26.4 (22.9-30.6) | -0.6179 (-0.7371--0.4985) |
| Central Asia | 7278 (6745-7932) | 25.7 (23.8-28.0) | 12915 (11199-14721) | 26.7 (23.1-30.4) | 0.0732 (-0.1382-0.2850) |
| Central Europe | 19903 (19067-20726) | 24.8 (23.7-25.8) | 31147 (28431-33614) | 28.4 (26.0-30.7) | 0.5564 (0.4848-0.6280) |
| Central Latin America | 10850 (10496-11190) | 23.3 (22.5-24.1) | 25392 (22150-28696) | 18.6 (16.2-21.0) | -0.7594 (-0.8946--0.6241) |
| Central Sub-Saharan Africa | 4513 (3375-5930) | 32.9 (24.5-43.0) | 11394 (7726-16565) | 33.1 (22.2-48.2) | -0.0141 (-0.0801-0.0520) |
| East Asia | 96145 (79016-115852) | 20.1 (16.6-24.1) | 134049 (105253-166568) | 12.1 (9.5-15.1) | -1.9484 (-2.1384--1.7581) |
| Eastern Europe | 36926 (34799-38632) | 22.2 (20.8-23.2) | 56501 (50563-63297) | 30.2 (27.0-34.0) | 0.7648 (0.6266-0.9031) |
| Eastern Sub-Saharan Africa | 22374 (19071-27054) | 50.6 (43.5-60.6) | 50101 (40567-62046) | 47.3 (39.0-57.3) | -0.3689 (-0.4480--0.2898) |
| High-income Asia Pacific | 15854 (14885-16541) | 14.4 (13.6-15.1) | 37837 (30494-42511) | 15.6 (13.6-16.9) | -0.0364 (-0.3985-0.3269) |
| High-income North America | 51162 (48262-52774) | 27.4 (26.2-28.1) | 59381 (54152-62478) | 18.2 (17.0-19.1) | -1.3833 (-1.5798--1.1864) |
| North Africa and Middle East | 13138 (11503-15420) | 14.1 (12.3-16.2) | 33743 (29408-38878) | 13.9 (12.1-15.8) | 0.0876 (0.0243-0.1508) |
| Oceania | 419 (311-549) | 24.2 (18.0-31.5) | 1207 (889-1627) | 27.5 (20.7-36.5) | 0.5602 (0.4940-0.6265) |
| South Asia | 396269 (344236-449100) | 122.3 (105.3-139.3) | 1054651 (907435-1219147) | 129.5 (112.1-149.5) | 0.0254 (-0.0913-0.1423) |
| Southeast Asia | 64130 (55030-74030) | 44.3 (37.9-50.6) | 135852 (113406-161805) | 38.6 (32.4-46.0) | -0.7102 (-0.8217--0.5986) |
| Southern Latin America | 4621 (4374-4830) | 18.3 (17.3-19.1) | 7865 (7225-8415) | 16.8 (15.5-18.0) | 0.2112 (-0.0252-0.4481) |
| Southern Sub-Saharan Africa | 6201 (5133-7363) | 36.3 (29.8-43.3) | 14606 (12885-16769) | 41.0 (36.3-46.8) | 0.6459 (0.3588-0.9338) |
| Tropical Latin America | 13796 (13127-14392) | 27.1 (25.6-28.4) | 36671 (33848-38546) | 26.0 (24.0-27.3) | -0.2974 (-0.4418--0.1528) |
| Western Europe | 64889 (61781-66697) | 22.0 (21.2-22.5) | 91803 (82282-97602) | 20.8 (19.2-21.8) | -0.0522 (-0.1273-0.0228) |
| Western Sub-Saharan Africa | 11423 (8991-13685) | 24.2 (19.1-29.0) | 33098 (25282-42987) | 27.5 (21.6-35.0) | 0.4231 (0.3640-0.4823) |
| Male | |||||
| Global | 393846 (379155-408550) | 19.4 (18.7-20.2) | 968572 (879563-1049185) | 23.1 (21.0-25.0) | 0.6198 (0.5648-0.6747) |
| High-middle SDI | 87635 (84122-91341) | 18.3 (17.6-19.1) | 191189 (171647-213834) | 20.9 (18.8-23.3) | 0.4278 (0.3390-0.5168) |
| High SDI | 183036 (177656-188375) | 37.8 (36.7-38.9) | 326167 (312705-339380) | 37.3 (35.8-38.8) | 0.0827 (0.0102-0.1554) |
| Low-middle SDI | 50319 (43099-57511) | 13.7 (11.7-15.6) | 157424 (128460-181418) | 19.9 (16.4-22.9) | 1.2015 (1.0773-1.3257) |
| Low SDI | 12616 (10278-14752) | 9.2 (7.5-10.8) | 36789 (28828-44267) | 12.0 (9.5-14.5) | 0.7405 (0.6040-0.8771) |
| Middle SDI | 59802 (55137-64875) | 9.9 (9.2-10.8) | 256142 (218360-292906) | 18.6 (15.9-21.2) | 2.1410 (2.0038-2.2784) |
| Andean Latin America | 361 (309-421) | 3.2 (2.7-3.8) | 1377 (1074-1738) | 4.6 (3.6-5.8) | 1.4741 (1.2825-1.6661) |
| Australasia | 5872 (5197-6576) | 53.9 (47.7-60.4) | 12754 (10966-14724) | 55.8 (47.8-64.3) | 0.1295 (-0.0086-0.2678) |
| Caribbean | 2148 (1983-2328) | 16.5 (15.2-17.9) | 4996 (4190-5847) | 19.4 (16.4-22.7) | 0.8384 (0.6923-0.9848) |
| Central Asia | 2313 (2151-2509) | 10.5 (9.7-11.4) | 3682 (3210-4189) | 9.0 (7.9-10.2) | -0.3772 (-0.7234--0.0297) |
| Central Europe | 14912 (14116-15742) | 21.8 (20.6-23.0) | 30292 (27350-33137) | 33.5 (30.2-36.7) | 1.2858 (1.1054-1.4665) |
| Central Latin America | 2290 (2191-2391) | 5.1 (4.9-5.3) | 7601 (6616-8629) | 6.4 (5.5-7.2) | 0.4660 (0.3594-0.5727) |
| Central Sub-Saharan Africa | 575 (423-855) | 4.6 (3.4-6.7) | 1911 (1428-2531) | 5.9 (4.5-7.6) | 0.8111 (0.5499-1.0729) |
| East Asia | 27391 (23012-32267) | 5.5 (4.6-6.5) | 178396 (141151-224934) | 16.5 (13.1-20.7) | 4.0502 (3.8578-4.2428) |
| Eastern Europe | 22884 (21680-24987) | 19.8 (18.8-21.6) | 37248 (32467-42807) | 27.2 (23.8-31.2) | 0.8308 (0.6289-1.0332) |
| Eastern Sub-Saharan Africa | 3467 (2914-3992) | 7.8 (6.5-9.0) | 9953 (7486-12230) | 9.6 (7.4-11.8) | 0.6070 (0.4693-0.7449) |
| High-income Asia Pacific | 12843 (12294-13461) | 13.6 (13.0-14.2) | 36234 (32967-39522) | 21.2 (19.4-23.1) | 1.5211 (1.2095-1.8337) |
| High-income North America | 79815 (77451-81891) | 53.7 (52.1-55.1) | 129298 (123344-134767) | 45.0 (42.9-46.7) | -0.4733 (-0.5573--0.3892) |
| North Africa and Middle East | 3092 (2641-3639) | 3.1 (2.6-3.6) | 13238 (11342-15160) | 4.9 (4.3-5.6) | 1.5289 (1.456-1.6018) |
| Oceania | 101 (70-132) | 5.2 (3.6-6.6) | 332 (241-428) | 6.7 (4.8-8.5) | 0.9430 (0.8365-1.0495) |
| South Asia | 75861 (66379-85548) | 20.7 (18.0-23.3) | 260373 (206422-305435) | 31.5 (25.1-36.8) | 1.3163 (1.1803-1.4526) |
| Southeast Asia | 14271 (12192-16274) | 10.1 (8.6-11.5) | 56456 (46903-66522) | 16.3 (13.6-19.1) | 1.5000 (1.4200-1.5801) |
| Southern Latin America | 3186 (2862-3534) | 14.6 (13.1-16.1) | 5142 (4487-5871) | 13.4 (11.7-15.2) | -0.0895 (-0.3563-0.178) |
| Southern Sub-Saharan Africa | 2114 (1566-2601) | 15.1 (10.9-18.7) | 4540 (3819-5155) | 15.4 (13.1-17.3) | -0.2424 (-0.3463--0.1384) |
| Tropical Latin America | 7204 (6818-7562) | 14.4 (13.6-15.2) | 22533 (21010-24318) | 18.2 (17.0-19.7) | 0.6784 (0.5758-0.7811) |
| Western Europe | 112221 (107084-117705) | 47.6 (45.4-49.9) | 149335 (138322-159354) | 41.0 (38.2-43.7) | -0.4608 (-0.5468--0.3746) |
| Western Sub-Saharan Africa | 914 (717-1114) | 1.7 (1.3-2.1) | 2871 (2140-3617) | 2.4 (1.8-3.0) | 1.0508 (0.8960-1.2059) |
Changes in lip and oral cavity cancer Prevalence by regions and sexes.
Table 4
| Locations | 1990 Number (95% UI, cases) |
1990 Age-standardized rate (95% UI, per 100,000) | 2021 Number (95% UI, cases) |
2021 Age-standardized rate (95% UI, per 100,000) | Estimated annual percentage change (95% CI, 100%) |
|---|---|---|---|---|---|
| Both sexes | |||||
| Global | 2936205 (2793741-3092058) | 69.3 (65.9-73.0) | 5874069 (5326986-6347557) | 67.7 (61.3-73.2) | -0.1650 (-0.2178--0.1121) |
| High-middle SDI | 574936 (552159-599598) | 55.7 (53.7-58.1) | 834847 (764565-906224) | 43.3 (39.7-47.0) | -1.0146 (-1.0917--0.9375) |
| High SDI | 567133 (549836-582623) | 54.1 (52.5-55.6) | 739298 (698770-772933) | 40.0 (38.2-41.7) | -0.9743 (-1.0132--0.9353) |
| Low-middle SDI | 846886 (759575-940604) | 119.9 (107.2-133.0) | 2041323 (1773549-2273768) | 128.4 (112.7-142.3) | 0.1680 (0.1205-0.2155) |
| Low SDI | 231414 (200547-263401) | 87.8 (76.4-100.0) | 542181 (458550-628171) | 90.5 (77.3-104.0) | -0.0701 (-0.1498-0.0097) |
| Middle SDI | 712596 (666093-761404) | 61.0 (57.0-65.1) | 1711811 (1539968-1877702) | 61.1 (55.1-67.0) | -0.0680 (-0.1171--0.0190) |
| Andean Latin America | 5839 (5065-6626) | 25.9 (22.4-29.4) | 13748 (10902-16887) | 22.5 (17.927.7) | -0.4093 (-0.5524--0.2660) |
| Australasia | 11122 (10354-11990) | 48.7 (45.3-52.5) | 16714 (15055-18427) | 34.2 (31.1-37.6) | -1.1051 (-1.3580--0.8516) |
| Caribbean | 17267 (16040-18899) | 64.9 (60.3-70.9) | 30477 (26005-35574) | 56.6 (48.3-66.0) | -0.2204 (-0.3353--0.1053) |
| Central Asia | 27173 (25372-29367) | 53.5 (49.8-57.8) | 38199 (33257-43855) | 42.3 (36.9-48.3) | -0.8158 (-0.9764--0.6550) |
| Central Europe | 122195 (116995-127869) | 83.1 (79.6-86.8) | 158444 (145874-170984) | 82.6 (76.0-89.2) | -0.1461 (-0.2595--0.0326) |
| Central Latin America | 28302 (27434-29080) | 31.5 (30.4-32.4) | 64214 (57048-72384) | 25.1 (22.3-28.3) | -0.8990 (-1.0084--0.7895) |
| Central Sub-Saharan Africa | 11519 (8890-15029) | 44.4 (34.8-57.1) | 30186 (22815-39392) | 45.7 (34.7-58.8) | 0.0779 (-0.0296-0.1856) |
| East Asia | 315772 (267868-362039) | 33.0 (28.1-37.7) | 697683 (563154-853797) | 31.9 (25.8-38.8) | 0.0126 (-0.1046-0.1300) |
| Eastern Europe | 218629 (210259-232556) | 78.5 (75.6-83.7) | 262247 (236250-289742) | 81.7 (73.5-90.4) | -0.3580 (-0.5575--0.1582) |
| Eastern Sub-Saharan Africa | 63267 (55142-72792) | 72.6 (63.7-83.2) | 143023 (112392-174329) | 69.7 (56.0-84.1) | -0.2614 (-0.3148--0.2080) |
| High-income Asia Pacific | 53404 (51574-55281) | 26.2 (25.3-27.2) | 108024 (96340-116039) | 26.8 (24.6-28.5) | -0.2683 (-0.6213-0.0861) |
| High-income North America | 176202 (170277-181404) | 53.8 (52.1-55.3) | 208746 (198194-218647) | 34.2 (32.6-35.8) | -1.4237 (-1.5936--1.2536) |
| North Africa and Middle East | 36036 (31673-41787) | 19.0 (16.7-21.7) | 89539 (78518-102823) | 17.7 (15.6-20.2) | -0.2081 (-0.2384--0.1778) |
| Oceania | 1348 (957-1753) | 37.5 (27.1-47.9) | 4005 (2875-5239) | 43.3 (31.4-55.9) | 0.6615 (0.5762-0.7469) |
| South Asia | 1185409 (1073536-1311139) | 174.5 (156.9-193.0) | 2964855 (2541835-3330175) | 182.3 (157.1-203.7) | 0.0277 (-0.0383-0.0936) |
| Southeast Asia | 178289 (154260-200931) | 63.4 (55.1-71.0) | 422230 (365827-481879) | 61.0 (52.9-69.5) | -0.2512 (-0.3001--0.2023) |
| Southern Latin America | 21908 (20020-23803) | 46.9 (42.9-50.9) | 26651 (24190-29219) | 31.8 (28.8-34.8) | -0.9688 (-1.2010--0.7360) |
| Southern Sub-Saharan Africa | 24312 (18793-28939) | 79.7 (60.9-95.3) | 49628 (43455-55690) | 76.4 (67.3-85.4) | -0.2904 (-0.5237--0.0566) |
| Tropical Latin America | 69446 (66329-72825) | 68.8 (65.5-72.2) | 157920 (148726-167280) | 59.9 (56.3-63.4) | -0.5232 (-0.6517--0.3946) |
| Western Europe | 346859 (333307-359027) | 67.8 (65.3-70.1) | 326627 (304681-344003) | 41.5(39.1-43.5) | -1.6138 (-1.6700--1.5576) |
| Western Sub-Saharan Africa | 21898 (17650-25674) | 22.2 (18.0-25.9) | 60898. (46881-74961) | 25.9 (20.5-31.4) | 0.4910 (0.4302-0.5519) |
| Female | |||||
| Global | 870961 (803991-939990) | 39.6 (36.5-42.7) | 1904257 (1730273-2088526) | 42.6 (38.6-46.8) | 0.1010 (0.0111-0.1910) |
| High-middle SDI | 123436 (115145-132211) | 22.3 (20.8-23.9) | 206999 (188577-223727) | 20.3 (18.5-22.0) | -0.4500 (-0.5255--0.3744) |
| High SDI | 142779 (135284-147269) | 24.2 (23.0-24.9) | 214391 (191581-228823) | 20.9 (19.3-22.1) | -0.4516 (-0.5138--0.3895) |
| Low-middle SDI | 307856 (271222-348678) | 88.1 (76.8-100.1) | 795539 (689891-916633) | 97.9 (85.2-112.1) | 0.2451 (0.1589-0.3314) |
| Low SDI | 87151 (72756-101815) | 66.9 (56.1-77.9) | 213022 (180430-249562) | 70.1 (60.0-82.0) | -0.0451 (-0.1539-0.0638) |
| Middle SDI | 209045 (192476-226234) | 36.0 (33.1-38.8) | 473157 (420157-524951) | 33.2 (29.6-36.8) | -0.4605 (-0.5659--0.3549) |
| Andean Latin America | 2588 (2260-2937) | 22.3 (19.4-25.3) | 6728 (5336-8412) | 21.3 (16.9-26.6) | -0.2346 (-0.3950--0.0739) |
| Australasia | 3177 (2949-3366) | 25.7 (23.9-27.2) | 5203 (4593-5741) | 19.7 (17.8-21.6) | -0.7636 (-1.0456--0.4808) |
| Caribbean | 4781 (4478-5141) | 34.6 (32.4-37.1) | 7673 (6679-8906) | 27.2 (23.6-31.6) | -0.6022 (-0.7215--0.4829) |
| Central Asia | 7426 (6888-8102) | 26.2 (24.3-28.7) | 13232 (11450-15070) | 27.3 (23.7-31.1) | 0.0894 (-0.1241-0.3033) |
| Central Europe | 20429 (19559-21296) | 25.4 (24.3-26.5) | 32397 (29701-34903) | 29.5 (27.-31.8) | 0.5971 (0.5256-0.6687) |
| Central Latin America | 11075 (10703-11396) | 23.8 (22.9-24.6) | 26162 (22924-29589) | 19.1 (16.8-21.6) | -0.7310 (-0.8658--0.5961) |
| Central Sub-Saharan Africa | 4577 (3422-6022) | 33.4 (24.9-43.7) | 11585 (7862-16881) | 33.7 (22.6-49.0) | -0.0070 (-0.0743-0.0604) |
| East Asia | 98226 (80451-118410) | 20.5 (16.9-24.6) | 140871 (110107-175966) | 12.8 (10.0-15.9) | -1.8521 (-2.0437--1.6601) |
| Eastern Europe | 38036 (35839-39830) | 22.8 (21.4-23.9) | 58926 (52550-65875) | 31.5 (28.0-35.3) | 0.8105 (0.6702-0.9509) |
| Eastern Sub-Saharan Africa | 22696 (19342-27439) | 51.3(44.1-61.4) | 50962 (41238-62955) | 48.1 (39.6-58.2) | -0.3610 (-0.4408--0.2812) |
| High-income Asia Pacific | 16706 (15707-17482) | 15.2 (14.3-15.9) | 40420 (32648-45492) | 16.7 (14.7-18.2) | 0.0532 (-0.3040-0.4116) |
| High-income North America | 55050 (51826-57234) | 29.4 (28.0-30.5) | 65261 (59614-69022) | 20.0 (18.6-21.1) | -1.3102 (-1.4983--1.1217) |
| North Africa and Middle East | 13406 (11742-15698) | 14.4 (12.6-16.6) | 34866 (30475-40228) | 14.3 (12.5-16.4) | 0.1287 (0.0643-0.1932) |
| Oceania | 427 (316-560) | 24.7 (18.4-32.2) | 1232 (909-1657) | 28.0 (21.1-37.1) | 0.5601 (0.4935-0.6268) |
| South Asia | 402040 (348796-455621) | 124.2 (106.9-140.9) | 1075186 (924959-1242527) | 132.0 (114.2-152.3) | 0.0402 (-0.0770-0.1576) |
| Southeast Asia | 65569 (56025-75728) | 45.3 (38.7-51.9) | 140137 (117294-166986) | 39.8 (33.4-47.4) | -0.6828 (-0.7931--0.5725) |
| Southern Latin America | 4741 (4481-4967) | 18.7 (17.7-19.6) | 8162 (7516-8728) | 17.4 (16.2-18.6) | 0.2468 (0.0104-0.4837) |
| Southern Sub-Saharan Africa | 6317 (5249-7512) | 37.0 (30.5-44.2) | 14911 (13148-17131) | 41.8 (37.0-47.8) | 0.6515 (0.3666-0.9371) |
| Tropical Latin America | 14080 (13388-14689) | 27.7 (26.1-29.0) | 37707 (34750-39638) | 26.7 (24.7-28.1) | -0.2747 (-0.4181--0.1311) |
| Western Europe | 68007 (64546-70339) | 23.0 (22.1-23.7) | 98948 (88447-105655) | 22.5 (20.8-23.7) | 0.0527 (-0.0235-0.1290) |
| Western Sub-Saharan Africa | 11597 (9133-13887) | 24.6 (19.4-29.4) | 33680 (25776-43812) | 28.0 (22.1-35.7) | 0.4313 (0.3726-0.4900) |
| Male | |||||
| Global | 66990 (62782-71608) | 3.6 (3.4-3.9) | 136890 (120655-149372) | 3.4 (3.0-3.7) | -0.2789 (-0.3244--0.2334) |
| High-middle SDI | 451499 (432553-473004) | 94.5(90.5-98.9) | 627847 (561697-694420) | 68.6 (61.4-75.8) | -1.2245 (-1.3029--1.1460) |
| High SDI | 424353 (411242-436619) | 88.4 (85.6-90.9) | 524906 (501600-549228) | 60.3 (57.6-63.0) | -1.2373 (-1.2729--1.2017) |
| Low-middle SDI | 539029 (462781-617695) | 150.5 (128.7-172.3) | 1245784 (1010032-1435569) | 160.6 (131.8-184.1) | 0.1783 (0.1489-0.2076) |
| Low SDI | 144263 (119651-169530) | 108.0 (89.5-127.2) | 329159 (262644-392946) | 111.5 (89.8-132.6) | -0.0490 (-0.1134-0.0154) |
| Middle SDI | 503550 (461761-550025) | 86.4 (79.5-94.2) | 1238654 (1059945-1380995) | 90.7 (77.9-101.2) | 0.1396 (0.0968-0.1824) |
| Andean Latin America | 113 (96-133) | 1.2 (1.0-1.4) | 266 (211-334) | 1.0 (0.8-1.2) | -0.4436 (-0.5954--0.2915) |
| Australasia | 284 (257-313) | 2.7 (2.5-3.0) | 468 (408-529) | 1.9 (1.7-2.1) | -1.1781 (-1.4448--0.9107) |
| Caribbean | 473 (437-518) | 3.9 (3.6-4.2) | 866 (737-1007) | 3.4 (2.9-4.0) | -0.1469 (-0.2787--0.0149) |
| Central Asia | 625 (582-683) | 3.2 (3.0-3.5) | 827 (722-952) | 2.3 (2.0-2.6) | -1.0245 (-1.2088--0.8399) |
| Central Europe | 3277 (3119-3450) | 5.1 (4.8-5.3) | 4515 (4144-4895) | 4.9 (4.5-5.4) | -0.1864 (-0.2846--0.0881) |
| Central Latin America | 628 (602-653) | 1.6 (1.6-1.7) | 1469 (1286-1657) | 1.3 (1.1-1.5) | -0.9860 (-1.099--0.8729) |
| Central Sub-Saharan Africa | 220 (162-322) | 2.1 (1.6-3.0) | 572 (429-749) | 2.3 (1.8-2.9) | 0.2063 (0.0856-0.3272) |
| East Asia | 7135 (5907-8495) | 1.8 (1.5-2.1) | 20770 (16201-26057) | 2.1 (1.6-2.6) | 0.7324 (0.5876-0.8775) |
| Eastern Europe | 5649 (5405-6018) | 5.3 (5.1-5.7) | 6670 (5872-7520) | 4.8 (4.3-5.5) | -0.7124 (-0.9048--0.5197) |
| Eastern Sub-Saharan Africa | 1302 (1103-1522) | 3.5 (2.9-4.0) | 2869 (2234-3500) | 3.5 (2.8-4.2) | -0.0706 (-0.1045--0.0366) |
| High-income Asia Pacific | 1285 (1241-1327) | 1.5 (1.4-1.5) | 3246 (2971-3434) | 1.6 (1.4-1.6) | -0.2271 (-0.5713-0.1183) |
| High-income North America | 4423 (4283-4542) | 3.0 (2.9-3.1) | 5844 (5475-6103) | 2.0 (1.8-2.1) | -1.3253 (-1.5100--1.1404) |
| North Africa and Middle East | 748 (625-881) | 0.9 (0.8-1.1) | 1855 (1612-2123) | 0.8 (0.7-0.9) | -0.3956 (-0.4495--0.3417) |
| Oceania | 27 (19-36) | 1.8 (1.2-2.3) | 82 (58-108) | 2.0 (1.5-2.7) | 0.6716 (0.5714-0.7719) |
| South Asia | 24271 (21049-27547) | 7.8 (6.7-8.9) | 60952 (49383-70777) | 8.3 (6.7-9.5) | 0.0639 (0.0022-0.1255) |
| Southeast Asia | 3702 (3167-4226) | 3.2 (2.7-3.6) | 9632 (8243-11109) | 3.2 (2.8-3.7) | 0.0123 (-0.0128-0.0374) |
| Southern Latin America | 591 (528-661) | 2.9 (2.6-3.2) | 691 (609-782) | 1.8 (1.6-2.0) | -1.1603 (-1.3943--0.9256) |
| Southern Sub-Saharan Africa | 560 (405-694) | 4.6 (3.3-5.7) | 1086 (930-1218) | 4.3 (3.7-4.8) | -0.5300 (-0.776--0.2834) |
| Tropical Latin America | 1771 (1675-1867) | 4.1 (3.8-4.3) | 4143 (3858-4452) | 3.5 (3.3-3.8) | -0.4345 (-0.5494--0.3195) |
| Western Europe | 9570 (9164-9940) | 4.1 (3.9-4.2) | 9230 (8525-9803) | 2.3 (2.1-2.4) | -1.8678 (-1.9557--1.7799) |
| Western Sub-Saharan Africa | 325 (257-396) | 0.7 (0.6-0.9) | 828 (642-1033) | 0.8 (0.7-1.0) | 0.4618 (0.3889-0.5348) |
Changes in lip and oral cavity cancer DALYs by regions and sexes.
Table 5
| Locations | 1990 Number (95% UI, cases) |
1990 Age-standardized rate (95% UI, per 100,000) | 2021 Number (95% UI, cases) |
2021 Age-standardized rate (95% UI, per 100,000) | Estimated annual percentage change (95% CI, 100%) |
|---|---|---|---|---|---|
| Both sexes | |||||
| Global | 2871519 (2733328-3026295) | 67.7 (64.4-71.3) | 5713196 (5183525-6171742) | 65.9 (59.7-71.2) | -0.1832 (-0.2361--0.1302) |
| High-middle SDI | 561447 (539389-585862) | 54.4 (52.3-56.8) | 804832 (738906-874361) | 41.8 (38.3-45.3) | -1.0591 (-1.1369--0.9811) |
| High SDI | 541955 (526962-553673) | 51.8 (50.3-52.9) | 693410 (656939-723548) | 37.6 (36.0-39.1) | -1.0385 (-1.0781--0.9988) |
| Low-middle SDI | 835581 (749392-929025) | 118.2 (105.9-131.3) | 2007285 (1746697-2238461) | 126.2 (111.0-140.1) | 0.1577 (0.1105-0.2048) |
| Low SDI | 228405 (197877-260046) | 86.6 (75.4-98.5) | 533868 (451292-619265) | 89.1 (76.0-102.3) | -0.0778 (-0.1575-0.0019) |
| Middle SDI | 700957 (655320-747947) | 60.0 (56.0-64.0) | 1669323 (1502850-1830781) | 59.6 (53.7-65.3) | -0.0960 (-0.1437--0.0482) |
| Andean Latin America | 5742 (4973-6524) | 25.4 (22.0-28.9) | 13390 (10588-16439) | 22.0 (17.4-26.9) | -0.4410 (-0.5831--0.2987) |
| Australasia | 10356 (9674-11065) | 45.4 (42.4-48.5) | 15063 (13630-16529) | 30.8 (28.0-33.8) | -1.214 (-1.4747--0.9527) |
| Caribbean | 16889 (15691-18442) | 63.5 (59.0-69.2) | 29691 (25404-34636) | 55.1 (47.2-64.3) | -0.2334 (-0.3486--0.1181) |
| Central Asia | 26728 (25022-28953) | 52.6 (49.0-56.9) | 37426 (32549-42919) | 41.4 (36.1-47.3) | -0.8312 (-0.9899--0.6723) |
| Central Europe | 119896 (114789-125465) | 81.6 (78.1-85.2) | 153996.9393 (141726.3-166548.6) | 80.4 (73.9-87.0) | -0.1752 (-0.2890--0.0613) |
| Central Latin America | 27773 (26934-28544) | 30.9 (29.9-31.8) | 62534 (55474-70281) | 24.5 (21.7-27.5) | -0.9226 (-1.0322--0.8129) |
| Central Sub-Saharan Africa | 11365 (8773-14853) | 43.7 (34.3-56.4) | 29735 (22464-38796) | 44.9 (34.1-57.8) | 0.0723 (-0.0341-0.1789) |
| East Asia | 310076 (263236-355895) | 32.3 (27.6-36.9) | 671860 (545021-826267) | 30.7 (25.0-37.6) | -0.0524 (-0.1684-0.0637) |
| Eastern Europe | 214353 (206458-227104) | 77.7 (74.2-81.7) | 254977 (229147-281922) | 79.4 (71.4-87.7) | -0.3891 (-0.5900--0.1878) |
| Eastern Sub-Saharan Africa | 62428 (54364-71641) | 71.6 (62.7-81.9) | 140859 (110404-171902) | 68.6 (55.0-82.9) | -0.2676 (-0.3205--0.2146) |
| High-income Asia Pacific | 51129 (49542-52724) | 25.1 (24.3-25.9) | 101422 (90072-109007) | 25.1 (23.2-26.7) | -0.3531 (-0.7107-0.0059) |
| High-income North America | 165135 (160216-168807) | 50.5 (49.1-51.5) | 191630 (181247-198978) | 31.4 (30.0-32.6) | -1.4922 (-1.6690--1.3152) |
| North Africa and Middle East | 35373 (31070-40913) | 18.7 (16.4-21.3) | 86975 (76178-99608) | 17.2 (15.1-19.6) | -0.2432 (-0.2734--0.2130) |
| Oceania | 1326 (941-1722) | 36.9 (26.7-47.1) | 3938 (2827-5161) | 42.5 (30.9-55.0) | 0.6608 (0.5756-0.7460) |
| South Asia | 1169596 (1058465-1292454) | 172.1 (154.7-190.7) | 2913399 (2493288-3275522) | 179.1 (154.1-200.3) | 0.0152 (-0.0501-0.0806) |
| Southeast Asia | 175044 (151362-197602) | 62.2 (54.0-69.8) | 411679 (356094-470571) | 59.4 (51.6-67.7) | -0.2727 (-0.3221--0.2233) |
| Southern Latin America | 21408 (19584-23345) | 45.9 (42.0-49.9) | 25787 (23468-28210) | 30.7 (28.0-33.6) | -0.9987 (-1.2316--0.7652) |
| Southern Sub-Saharan Africa | 23926 (18500-28431) | 78.4 (60.0-93.8) | 48750 (42680-54547) | 75.0 (66.0-83.8) | -0.2968 (-0.5323--0.0608) |
| Tropical Latin America | 68268 (65125-71560) | 67.6 (64.3-70.9) | 154326 (145322-163365) | 58.5 (55.0-61.9) | -0.5410 (-0.6705--0.4113) |
| Western Europe | 333109 (321050-343632) | 65.3 (62.9-67.2) | 305822 (286439-321093) | 38.9 (36.8-40.7) | -1.7016 (-1.7595--1.6437) |
| Western Sub-Saharan Africa | 21588 (17400-25352) | 21.8 (17.7-25.6) | 59926 (46200-73546) | 25.5 (20.2-30.8) | 0.4846 (0.4236-0.5455) |
| Female | |||||
| Global | 850043 (783392-917046) | 38.6 (35.6-41.7) | 1846853 (1681594-2028079) | 41.3 (37.6-45.4) | 0.0802 (-0.0104-0.1709) |
| High-middle SDI | 119984 (112275-129049) | 21.7 (20.3-23.3) | 197409 (179757-213284) | 19.4 (17.7-20.9) | -0.5168 (-0.5923--0.4412) |
| High SDI | 134989 (127968-138741) | 22.9 (21.9-23.4) | 198695 (177901-211359) | 19.4 (17.9-20.4) | -0.5292 (-0.5935--0.4649) |
| Low-middle SDI | 303425 (267186-343458) | 86.8 (75.8-98.4) | 780947 (678258-899360) | 96.1 (83.7-109.9) | 0.2330 (0.1468-0.3192) |
| Low SDI | 85939 (71743-100350) | 65.9 (55.2-76.8) | 209454 (177431-245607) | 68.9 (58.9-80.5) | -0.0544 (-0.1632-0.0544) |
| Middle SDI | 205030 (189232-222063) | 35.3 (32.5-38.1) | 459239 (408646-510473) | 32.2 (28.7-35.8) | -0.4936 (-0.5980--0.389) |
| Andean Latin America | 2542 (2217-2889) | 21.9 (19.0-24.8) | 6535 (5189-8182) | 20.6 (16.4-25.8) | -0.2715 (-0.4313--0.1115) |
| Australasia | 2938 (2730-3108) | 23.8 (22.1-25.2) | 4647 (4067-5090) | 17.6 (15.8-19.2) | -0.8876 (-1.1778--0.5966) |
| Caribbean | 4664 (4367-5012) | 33.7 (31.8-36.2) | 7448 (6474-8626) | 26.4 (22.8-30.6) | -0.6179 (-0.7371--0.4985) |
| Central Asia | 7278 (6745-7932) | 25.7 (23.8-28.0) | 12915 (11199-14721) | 26.7 (23.1-30.4) | 0.0732 (-0.1382-0.2850) |
| Central Europe | 19903 (19067-20726) | 24.8 (23.7-25.8) | 31147 (28431-33614) | 28.4 (26.0-30.7) | 0.5564 (0.4848-0.6280) |
| Central Latin America | 10850 (10496-11190) | 23.3 (22.5-24.1) | 25392 (22150-28696) | 18.6 (16.2-21.0) | -0.7594 (-0.8946--0.6241) |
| Central Sub-Saharan Africa | 4513 (3375-5930) | 32.9 (24.5-43.0) | 11394 (7726-16565) | 33.1 (22.2-48.2) | -0.0141 (-0.0801-0.0520) |
| East Asia | 96145 (79016-115852) | 20.1 (16.6-24.1) | 134049 (105253-166568) | 12.1 (9.5-15.1) | -1.9484 (-2.1384--1.7581) |
| Eastern Europe | 36926 (34799-38632) | 22.2 (20.8-23.2) | 56501 (50563-63297) | 30.2 (27.0-34.0) | 0.7648 (0.6266-0.9031) |
| Eastern Sub-Saharan Africa | 22374 (19071-27054) | 50.6 (43.5-60.6) | 50101 (40567-62046) | 47.3 (39.0-57.3) | -0.3689 (-0.448--0.2898) |
| High-income Asia Pacific | 850043 (783392-917046) | 38.6 (35.6-41.7) | 1846853 (1681594-2028079) | 41.3 (37.6-45.4) | 0.0802 (-0.0104-0.1709) |
| High-income North America | 15854 (14885-16541) | 14.4 (13.6-15.1) | 37837 (30494-42511) | 15.6 (13.6-16.9) | -0.0364 (-0.3985-0.3269) |
| North Africa and Middle East | 51162 (48262-52774) | 27.4 (26.2-28.1) | 59381 (54152-62478) | 18.2 (17.0-19.1) | -1.3833 (-1.5798--1.1864) |
| Oceania | 13138 (11503-15420) | 14.1 (12.3-16.2) | 33743 (29408-38878) | 13.9 (12.1-15.8) | 0.0876 (0.0243-0.1508) |
| South Asia | 419 (311-549) | 24.2 (18.0-31.5) | 1207 (889-1627) | 27.5 (20.7-36.5) | 0.5602 (0.4940-0.6265) |
| Southeast Asia | 396269 (344236-449100) | 122.4 (105.3-139.3) | 1054651 (907435-1219147) | 129.5 (112.1-149.5) | 0.0254 (-0.0913-0.1423) |
| Southern Latin America | 64130 (55030-74030) | 44.3 (37.9-50.6) | 135852 (113406-161805) | 38.6 (32.4-46.0) | -0.7102 (-0.8217--0.5986) |
| Southern Sub-Saharan Africa | 4621 (4374-4830) | 18.3 (17.3-19.1) | 7865 (7225-8415) | 16.8 (15.5-18.0) | 0.2112 (-0.0252-0.4481) |
| Tropical Latin America | 6201 (5133-7363) | 36.3 (29.8-43.3) | 14606 (12885-16769) | 41.0 (36.3-46.8) | 0.6459 (0.3588-0.9338) |
| Western Europe | 13796 (13127-14392) | 27.1 (25.6-28.4) | 36671 (33848-38546) | 26.0 (24.0-27.3) | -0.2974 (-0.4418--0.1528) |
| Western Sub-Saharan Africa | 64889 (61781-66697) | 22.0 (21.2-22.5) | 91803 (82282-97602) | 20.8 (19.2-21.8) | -0.0522 (-0.1273-0.0228) |
| Male | |||||
| Global | 2021476 (1890182-2164947) | 99.18230972 (92.7-106.0) | 3866342 (3359573-4249613) | 92.1 (80.1-101.1) | -0.3118 (-0.352--0.2716) |
| High-middle SDI | 441463 (422991-462502) | 92.4 (88.5-96.6) | 607422 (544621-672649) | 66.3 (59.5-73.4) | -1.2608 (-1.3401--1.1814) |
| High SDI | 406966 (395136-417536) | 84.8 (82.2-87.0) | 494715 (473677-515990) | 56.9 (54.5-59.3) | -1.2944 (-1.3305--1.2583) |
| Low-middle SDI | 532156 (456088-609659) | 148.5 (127.0-170.1) | 1226338 (996720-1411527) | 158.0 (129.9-181.3) | 0.1693 (0.1405-0.1982) |
| Low SDI | 142465 (118094-167504) | 106.6 (88.4-125.6) | 324414 (258682-387374) | 109.8 (88.4-130.7) | -0.0556 (-0.1199-0.0088) |
| Middle SDI | 495927 (454970-541872) | 85.0 (78.2-92.7) | 1210083 (1034867-1349833) | 88.6 (76.0-98.8) | 0.1131 (0.0713-0.1548) |
| Andean Latin America | 3200 (2728-3753) | 29.1 (24.5-34.3) | 6854 (5399-8506) | 23.3 (18.4-29.1) | -0.5879 (-0.7400--0.4355) |
| Australasia | 7418 (6700-8149) | 68.9 (62.6-75.5) | 10416 (9125-11826) | 44.9 (39.5-50.8) | -1.3601 (-1.6152--1.1042) |
| Caribbean | 12225 (11173-13598) | 95.0 (87.0-105.4) | 22243 (18833-26309) | 86.6 (73.4-102.2) | -0.0737 (-0.2079-0.0606) |
| Central Asia | 19449 (18098-21006) | 87.9 (81.8-95.8) | 24511 (21343-28361) | 59.6 (52.0-68.8) | -1.2718 (-1.4308--1.1124) |
| Central Europe | 99992 (95232-105268) | 147.1 (140.2-154.7) | 122849 (112686-133423) | 137.9 (126.4-149.9) | -0.3801 (-0.5197--0.2403) |
| Central Latin America | 16922 (16260-17568) | 38.9 (37.3-40.4) | 37141 (32335-42096) | 31.3 (27.2-35.4) | -0.9819 (-1.1005--0.8633) |
| Central Sub-Saharan Africa | 6852 (5015-10184) | 56.0 (41.3-81.5) | 18340 (13582-24308) | 58.6 (44.4-76.1) | 0.1199 (-0.0031-0.2430) |
| East Asia | 213931 (176567-255648) | 45.2 (37.5-53.7) | 537810 (418440-678690) | 50.4 (39.6-63.2) | 0.6045 (0.4634-0.7458) |
| Eastern Europe | 177426 (169726-190212) | 154.9 (148.4-165.8) | 198475 (174246-224154) | 143.5 (126.1-161.8) | -0.7113 (-0.9161--0.506) |
| Eastern Sub-Saharan Africa | 40054 (33862-46904) | 92.8 (78.6-108.0) | 90757 (69153-112318) | 91.8 (71.2-112.0) | -0.149 (-0.1879--0.1100) |
| High-income Asia Pacific | 35275 (34249-36520) | 37.7 (36.5-39.0) | 63585 (59033-67230) | 35.3 (32.8-37.5) | -0.5945 (-0.949--0.2386) |
| High-income North America | 113973 (111048-116708) | 77.7 (75.7-79.5) | 132249 (126103-137395) | 46.2 (44.2-48.0) | -1.6012 (-1.7812--1.4208) |
| North Africa and Middle East | 22234 (18732-26422) | 23.0 (19.3-27.2) | 53231 (46117-61103) | 20.4 (17.7-23.4) | -0.4565 (-0.4997--0.4133) |
| Oceania | 907 (622-1217) | 48.6 (33.7-64.0) | 2731 (1905-3605) | 56.5 (39.7-74.0) | 0.7029 (0.6069-0.7991) |
| South Asia | 773326 (672874-876143) | 216.9 (188.3-245.7) | 1858748 (1483108-2166194) | 229.3 (184.5-266.7) | 0.0903 (0.0499-0.1307) |
| Southeast Asia | 110914 (94809-126783) | 81.8 (7.0-93.7) | 275827 (233449-318325) | 82.0 (69.8-94.3) | -0.0379 (-0.0594--0.0163) |
| Southern Latin America | 16787 (14985-18722) | 77.6 (69.3-86.4) | 17921 (15649-20224) | 46.6 (40.8-52.6) | -1.4110 (-1.6583--1.1632) |
| Southern Sub-Saharan Africa | 17725 (13084-21874) | 129.8 (94.3-160.6) | 34143 (28807-38729) | 118.2 (100.8-133.0) | -0.5918 (-0.8527--0.3301) |
| Tropical Latin America | 54472 (51795-57463) | 111.9 (105.9-118.0) | 117654 (109572-126187) | 95.7 (89.2-102.6) | -0.5513 (-0.6904--0.4121) |
| Western Europe | 268219 (256502-278708) | 114.2 (109.3-118.8) | 214018 (200137-227173) | 58.2 (54.6-61.7) | -2.2452 (-2.3112--2.1791) |
| Western Sub-Saharan Africa | 10165 (8026-12399) | 19.4 (15.4-23.7) | 26828 (20207-34029) | 23.1 (17.8-28.9) | 0.5209 (0.4409-0.6009) |
Changes in lip and oral cavity cancer YLLs by regions and sexes.
Table 6
| Locations | 1990 Number (95% UI, cases) |
1990 Age-standardized rate (95% UI, per 100,000) | 2021 Number (95% UI, cases) |
2021 Age-standardized rate (95% UI, per 100,000) | Estimated annual percentage change (95% CI, 100%) |
|---|---|---|---|---|---|
| Both sexes | |||||
| Global | 64685 (47399-83186) | 1.6 (1.1-2.0) | 160873 (118043-210399) | 1.9 (1.4-2.4) | 0.5507 (0.4933-0.6081) |
| High-middle SDI | 13488 (9811-17519) | 1.3 (1.0-1.7) | 30015 (21934-39119) | 1.5 (1.1-2.0) | 0.4801 (0.3928-0.5675) |
| High SDI | 25177 (18804-32767) | 2.4 (1.8-3.1) | 45887 (34195-59876) | 2.4 (1.8-3.2) | 0.1937 (0.1324-0.2551) |
| Low-middle SDI | 11304 (8374-14840) | 1.7 (1.2-2.2) | 34038 (24696-45279) | 2.2 (1.6-2.9) | 0.8412 (0.7418-0.9407) |
| Low SDI | 3008 (2159-3943) | 1.2 (0.9-1.6) | 8312 (6030-11290) | 1.4 (1.0-1.9) | 0.4584 (0.3437-0.5732) |
| Middle SDI | 11638 (8433-15167) | 1.0 (0.7-1.3) | 42487 (30295-56024) | 1.5 (1.1-2.0) | 1.2793 (1.1687-1.3899) |
| Andean Latin America | 96 (67-125) | 0.4 (0.3-0.6) | 358 (237-506) | 0.6 (0.4-0.8) | 1.0618 (0.8929-1.2309) |
| Australasia | 765 (552-1035) | 3.3 (2.4-4.5) | 1650 (1165-2169) | 3.4 (2.4-4.5) | 0.0754 (-0.0909-0.2420) |
| Caribbean | 378 (279-493) | 1.4 (1.1-1.9) | 785 (566-1029) | 1.5 (1.1-1.9) | 0.3131 (0.2045-0.4218) |
| Central Asia | 444 (321-577) | 0.9 (0.6-1.2) | 772 (549-1039) | 0.9 (0.6-1.2) | 0.0051 (-0.2696-0.2805) |
| Central Europe | 2299 (1670-2999) | 1.6 (1.1-2.0) | 4447 (3262-5844) | 2.2 (1.6-2.9) | 1.1166 (0.9997-1.2337) |
| Central Latin America | 529 (385-694) | 0.6 (0.4-0.9) | 1680 (1196-2272) | 0.7 (0.5-0.9) | 0.1153 (0.0194-0.2112) |
| Central Sub-Saharan Africa | 153 (104-216) | 0.6 (0.4-0.9) | 451 (303-656) | 0.7 (0.5-1.1) | 0.4503 (0.2655-0.6355) |
| East Asia | 5695 (3950-7685) | 0.6 (0.4-0.8) | 25823 (17762-34761) | 1.2 (0.8-1.6) | 2.4282 (2.2812-2.5755) |
| Eastern Europe | 4275 (3092-5539) | 1.5 (1.1-2.0) | 7270 (5304-9484) | 2.3 (1.6-3.0) | 0.9698 (0.7618-1.1783) |
| Eastern Sub-Saharan Africa | 838 (598-1125) | 1.0 (0.7-1.4) | 2164 (1526-2993) | 1.1 (0.8-1.5) | 0.1533 (0.0514-0.2553) |
| High-income Asia Pacific | 2275 (1675-2977) | 1.1 (0.8-1.5) | 6601 (4785-8670) | 1.7 (1.2-2.2) | 1.3111 (1.008-1.6152) |
| High-income North America | 11067 (8299-14552) | 3.3 (2.5-4.7) | 17116 (12825-22545) | 2.8 (2.1-3.7) | -0.5433 (-0.6226--0.464) |
| North Africa and Middle East | 662 (479-899) | 0.4 (0.3-0.5) | 2564 (1851-3502) | 0.5 (0.4-0.7) | 1.2400 (1.1677-1.3124) |
| Oceania | 21 (14-31) | 0.6 (0.4-0.9) | 66 (44-97) | 0.8 (0.5-1.1) | 0.7034 (0.6023-0.8045) |
| South Asia | 15812 (11498-20715) | 2.4 (1.7-3.1) | 51455 (36749-67858) | 3.2 (2.3-4.2) | 0.8283 (0.6997-0.9570) |
| Southeast Asia | 3244 (2322-4331) | 1.2 (0.7-1.6) | 10550 (7625-14134) | 1.5 (1.1-2.1) | 0.7181 (0.656-0.7802) |
| Southern Latin America | 499 (353-663) | 1.1 (0.8-1.4) | 864 (616-1164) | 1.0 (0.7-1.3) | 0.1042 (-0.1187-0.3276) |
| Southern Sub-Saharan Africa | 386 (262-533) | 1.3 (0.9-1.8) | 877 (634-1164) | 1.4 (1.0-1.8) | 0.0851 (-0.0221-0.1924) |
| Tropical Latin America | 1177 (862-1521) | 1.2 (0.9-1.5) | 3594 (2608-4715) | 1.4 (1.0-1.8) | 0.3554 (0.2639-0.4470) |
| Western Europe | 13750 (10161-17969) | 2.6 (2.0-3.5) | 20804 (15171-27077) | 2.6 (1.9-3.4) | 0.0347 (-0.0451-0.1145) |
| Western Sub-Saharan Africa | 310 (222-421) | 0.3 (0.2-0.4) | 971 (679-1363) | 0.4 (0.3-0.6) | 0.9009 (0.8225-0.9793) |
| Female | |||||
| Global | 20918 (15331-27162) | 1.0 (0.7-1.2) | 57404 (42494-75994) | 1.3 (0.9-1.7) | 0.8532 (0.7828-0.9236) |
| High-middle SDI | 3451 (2490-4610) | 0.6 (0.4-0.8) | 9590 (6970-12721) | 0.9 (0.8-1.2) | 1.3445 (1.2666-1.4225) |
| High SDI | 7790 (5764-10292) | 1.3 (0.9-1.7) | 15696 (11636-20912) | 1.5 (1.1-2.1) | 0.6858 (0.6129-0.7588) |
| Low-middle SDI | 4431 (3116-5779) | 1.3 (0.9-1.7) | 14591 (10387-19621) | 1.8 (1.3-2.4) | 0.9786 (0.8613-1.0960) |
| Low SDI | 1211 (838-1637) | 1.0 (0.7-1.3) | 3567 (2562-4870) | 1.2 (0.9-1.6) | 0.5484 (0.4155-0.6814) |
| Middle SDI | 4014 (2887-5276) | 0.7 (0.5-0.9) | 13917 (9944-18535) | 1.0 (0.7-1.3) | 0.8959 (0.7613-1.0307) |
| Andean Latin America | 45 (33-60) | 0.4 (0.3-0.5) | 192 (130-270) | 0.6 (0.4-0.9) | 1.3518 (1.1792-1.5247) |
| Australasia | 239 (170-323) | 1.9 (1.4-2.6) | 556 (393-753) | 2.1 (1.5-2.9) | 0.4530 (0.2501-0.6563) |
| Caribbean | 117 (86-152) | 0.8 (0.6-1.1) | 224 (157-307) | 0.8 (0.6-1.1) | -0.0349 (-0.1651-0.0956) |
| Central Asia | 147 (104-194) | 0.5 (0.4-0.7) | 316 (218-439) | 0.7 (0.5-0.9) | 0.8189 (0.4924-1.1465) |
| Central Europe | 526 (385-699) | 0.6 (0.5-0.9) | 1250 (928-1652) | 1.1 (0.8-1.5) | 1.8697 (1.7867-1.9528) |
| Central Latin America | 224 (166-292) | 0.5 (0.4-0.6) | 769 (549-1048) | 0.6 (0.4-0.8) | 0.3752 (0.2618-0.4887) |
| Central Sub-Saharan Africa | 64 (43-93) | 0.5 (0.3-0.7) | 191 (115-307) | 0.6 (0.3-0.9) | 0.4323 (0.2820-0.5829) |
| East Asia | 2081 (1446-2803) | 0.4 (0.3-0.6) | 6821 (4507-9544) | 0.6 (0.4-0.9) | 1.0169 (0.8483-1.1859) |
| Eastern Europe | 1109 (797-1471) | 0.7 (0.5-0.9) | 2424 (1760-3284) | 1.3 (0.9-1.7) | 2.1236 (1.8549-2.3930) |
| Eastern Sub-Saharan Africa | 322 (224-437) | 0.8 (0.5-1.0) | 861 (603-1198) | 0.8 (0.6-1.1) | 0.1284 (-0.0047-0.2615) |
| High-income Asia Pacific | 852 (618-1126) | 0.8 (0.6-1.0) | 2583 (1843-3499) | 1.2 (0.8-1.6) | 1.4833 (1.1693-1.7983) |
| High-income North America | 3888 (2880-5118) | 2.0 (1.5-2.7) | 5880 (4399-7760) | 1.8 (1.3-2.4) | -0.4753 (-0.5674--0.3832) |
| North Africa and Middle East | 267 (189-363) | 0.3 (0.2-0.4) | 1122 (804-1583) | 0.5 (0.3-0.7) | 1.6728 (1.5645-1.7812) |
| Oceania | 8 (5-12) | 0.5 (0.3-0.7) | 24 (16-35) | 0.6 (0.4-0.8) | 0.5553 (0.4520-0.6587) |
| South Asia | 5770 (4100-7533) | 1.8 (1.3-2.4) | 20535 (14811-27535) | 2.5 (1.8-3.4) | 0.9211 (0.7554-1.0871) |
| Southeast Asia | 1439 (1030-1892) | 1.0 (0.7-1.3) | 4284 (3046-5696) | 1.2 (0.9-1.6) | 0.3454 (0.2535-0.4375) |
| Southern Latin America | 120 (83-158) | 0.5 (0.3-0.6) | 296 (213-395) | 0.6 (0.5-0.8) | 1.3881 (1.1322-1.6447) |
| Southern Sub-Saharan Africa | 115 (81-161) | 0.7 (0.5-1.0) | 304 (220-403) | 0.9 (0.6-1.1) | 0.9308 (0.7521-1.1099) |
| Tropical Latin America | 283 (206-373) | 0.6 (0.4-0.7) | 1035 (747-1361) | 0.7 (0.5-1.0) | 0.662 (0.5437-0.7804) |
| Western Europe | 3118 (2290-4109) | 1.0 (0.8-1.4) | 7145 (5273-9554) | 1.6 (1.2-2.2) | 1.7274 (1.5516-1.9035) |
| Western Sub-Saharan Africa | 174 (119-241) | 0.4 (0.3-0.5) | 581 (400-833) | 0.5 (0.3-0.7) | 0.9196 (0.8629-0.9764) |
| Male | |||||
| Global | 43767 (32062-55845) | 2.2 (1.6-2.8) | 103468 (74778-135007) | 2.5 (1.8-3.2) | 0.3842 (0.3258-0.4427) |
| High-middle SDI | 10036 (7262-12946) | 2.2 (1.6-2.8) | 20424 (14902-26931) | 2.2 (1.6-3.0) | 0.0839 (-0.0069-0.1748) |
| High SDI | 17387 (12949-22598) | 3.6 (2.7-4.7) | 30191 (22495-39272) | 3.4 (2.5-4.5) | -0.1142 (-0.1708--0.0576) |
| Low-middle SDI | 6873 (4948-9169) | 2.0 (1.4-2.6) | 19446 (13485-26219) | 2.6 (1.8-3.4) | 0.7941 (0.7045-0.8838) |
| Low SDI | 1797 (1266-2471) | 1.4 (2.0-1.9) | 4744 (3326-6475) | 1.7 (1.2-2.3) | 0.4251 (0.3211-0.5293) |
| Middle SDI | 7623 (5464-9960) | 1.4 (1.0-1.8) | 28570 (20188-38092) | 2.1 (1.5-2.8) | 1.5119 (1.3985-1.6255) |
| Andean Latin America | 50 (34-67) | 0.5 (0.3-0.6) | 165 (107-234) | 0.6 (0.4-0.8) | 0.7623 (0.5731-0.9519) |
| Australasia | 526 (377-717) | 4.9 (3.5-6.6) | 1093 (742-1496) | 4.7 (3.2-6.4) | -0.1186 (-0.276-0.0391) |
| Caribbean | 261 (192-346) | 2.0 (1.5-2.7) | 560 (401-744) | 2.2 (1.6-2.9) | 0.4831 (0.3448-0.6216) |
| Central Asia | 297 (214-385) | 1.4 (1.0-1.8) | 455 (322-623) | 1.2 (0.8-1.6) | -0.5130 (-0.7779--0.2474) |
| Central Europe | 1773 (1291-2318) | 2.6 (1.9-3.4) | 3197 (2336-4222) | 3.5 (2.6-4.6) | 0.8323 (0.6911-0.9738) |
| Central Latin America | 304 (220-401) | 0.7 (0.5-1.0) | 910 (639-1232) | 0.8 (0.5-1.1) | -0.0501 (-0.1610-0.0609) |
| Central Sub-Saharan Africa | 88 (55-137) | 0.8 (0.5-1.2) | 260 (169-375) | 0.9 (0.6-1.3) | 0.4817 (0.2837-0.6801) |
| East Asia | 3614 (2504-4932) | 0.8 (0.5-1.1) | 19002 (12778-26105) | 1.8 (1.2-2.4) | 3.0525 (2.8699-3.2354) |
| Eastern Europe | 3165 (2305-4104) | 2.8 (2.0-3.6) | 4846 (3432-6379) | 3.5 (2.5-4.6) | 0.4724 (0.2872-0.6579) |
| Eastern Sub-Saharan Africa | 516 (366-698) | 1.3 (0.9-1.7) | 1303 (896-1842) | 1.4 (1.0-1.9) | 0.2334 (0.1530-0.3139) |
| High-income Asia Pacific | 1422 (1039-1847) | 1.5 (1.1-2.0) | 4018 (2911-5258) | 2.2 (1.6-2.9) | 1.1186 (0.8210-1.4171) |
| High-income North America | 7178 (5379-9471) | 4.8 (3.6-6.4) | 11235 (8360-14729) | 3.9 (2.9-5.1) | -0.6398 (-0.7302--0.5492) |
| North Africa and Middle East | 394 (281-534) | 0.4 (0.3-0.6) | 1441 (1027-1975) | 0.6 (0.4-0.8) | 0.9217 (0.8663-0.9772) |
| Oceania | 13 (8-19) | 0.7 (0.5-1.1) | 41 (27-62) | 0.9 (0.6-1.4) | 0.7902 (0.6888-0.8917) |
| South Asia | 10042 (7133-13333) | 2.9 (2.1-3.9) | 30919 (20956-41641) | 3.9 (2.7-5.2) | 0.8407 (0.7358-0.9457) |
| Southeast Asia | 1805 (1266-2414) | 1.4 (1.0-1.8) | 6265 (4483-8462) | 1.9 (1.4-2.5) | 0.9882 (0.9359-1.0404) |
| Southern Latin America | 379 (264-506) | 1.8 (1.2-2.4) | 567 (396-768) | 1.5 (1.0-2.0) | -0.4149 (-0.6425--0.1869) |
| Southern Sub-Saharan Africa | 270 (174-385) | 2.0 (1.3-2.9) | 573 (407-775) | 2.0 (1.5-2.7) | -0.2540 (-0.3898--0.1179) |
| Tropical Latin America | 894 (655-1149) | 1.9 (1.4-2.4) | 2558 (1866-3344) | 2.1 (1.5-2.7) | 0.2982 (0.1985-0.3981) |
| Western Europe | 10632 (7818-13717) | 4.5 (3.3-5.8) | 13659 (9911-17862) | 3.7 (2.7-4.8) | -0.6584 (-0.7233--0.5934) |
| Western Sub-Saharan Africa | 135 (95-187) | 0.3 (0.2-0.4) | 389 (268-556) | 0.4 (0.2-0.5) | 0.7845 (0.6760-0.8932) |
Changes in lip and oral cavity cancer YLDs by regions and sexes.
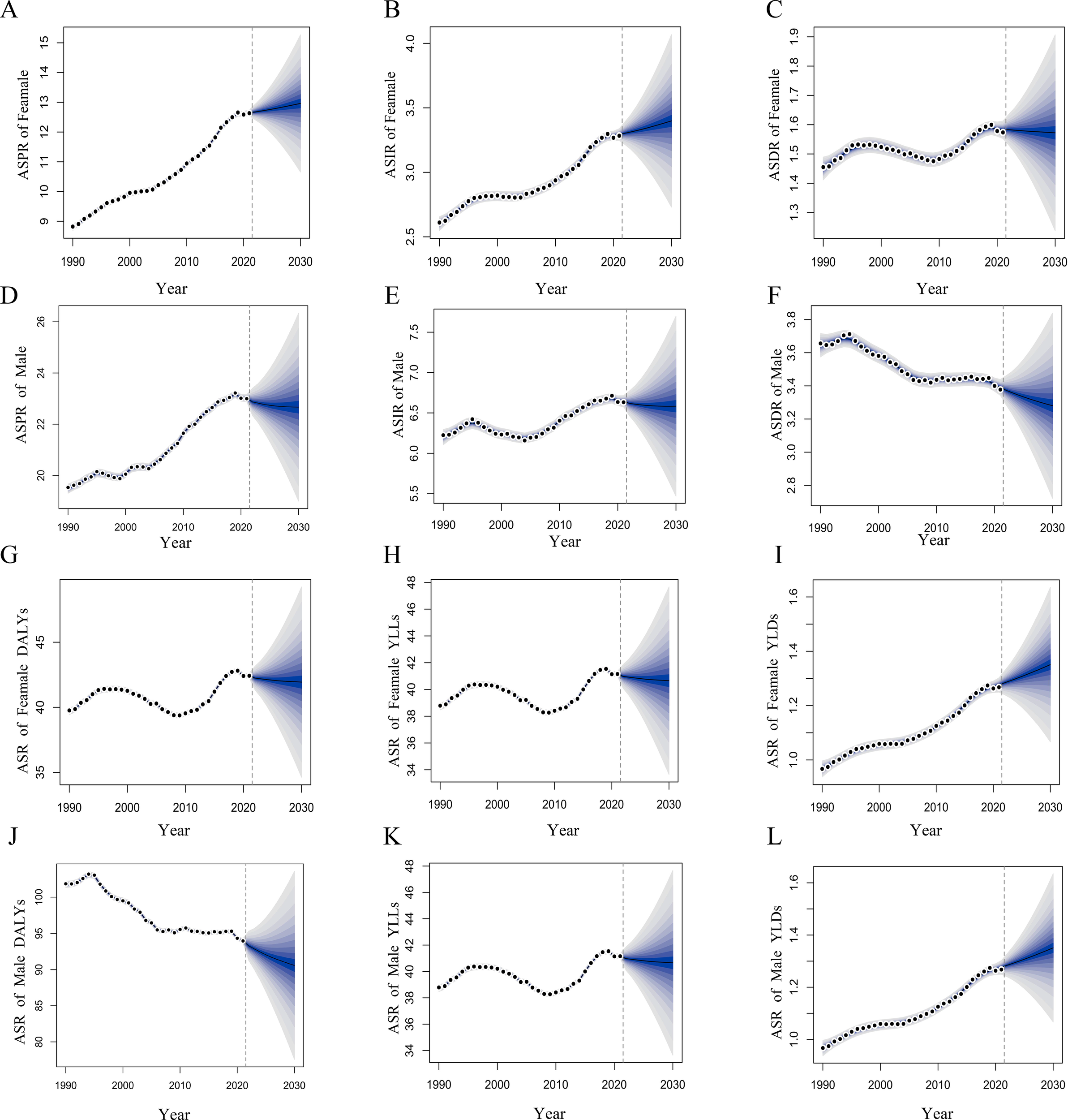
Regarding the trends in changes, from 1990 to 2021, ASIR, ASPR, and ASR of YLDs for LOCC exhibited an estimate annual increasing trend (EAPC, 0.3981 [95% CI, 0.3332 to 0.4631]; 0.8167 [95% CI, 0.7644 to 0.8690]; 0.5507 [95% CI, 0.4933 to 0.6081]) globally (Figures 1A, C, F). Among the 21 GBD regions, East Asia had the highest estimate annual increase in ASIR, ASPR, and ASR of YLDs (EAPC, 1.8681 [95% CI, 1.7032 to 2.0333]; 3.3177 [95% CI, 3.1823 to 3.4533]; 2.4282 [95% CI, 2.2812 to 2.5755]) (Table 1–6). In contrast to the aforementioned trends, the ASDR, ASR of DALYs, and YLLs caused by LOCC all exhibited an estimate annual decreasing trend (EAPC, -0.1142 [95% CI, -0.1675 to -0.0608]; -0.1650 [95% CI, -0.2178 to -0.1121]; -0.1832 [95% CI, -0.2361 to -0.1302]) (Figures 1B, D, E). Ultimately, Western Europe exhibited the most substantial estimate annual decline in ASDR, ASR of DALYs, and YLLs (EAPC, -1.2628 [95% CI, -1.3406 to -1.1850]; -1.6138 [95% CI, -1.6700 to -1.5576]; -1.7016 [95% CI, -1.7595 to -1.6437]). Notably, the region where all LOCC burden indicators showed a marked increase was Oceania.
Figure 1

Trends in the disease burden of lip and oral cavity cancer (LOCC) by gender from 1990 to 2021. (A–F) represent the incidence, death, prevalence, years lived with disability (YLDs), years of life lost (YLLs) and disability-adjusted life years (DALYs), respectively.
In terms of sex differences, a notable observation is that among males in East Asia, the highest annual percentage increases were seen in ASIR, ASPR, and the ASR of YLDs (EAPC, 2.4966 [95% CI, 2.3051 to 2.6885]; 4.0502 [95% CI, 3.8578 to 4.2428]; 3.0525 [95% CI, 2.8699 to 3.2354]). Conversely, among females in East Asia, ASPR, ASDR, the ASR of DALYs, and YLLs all exhibited a marked annul decreasing trend (EAPC, -1.9484 [95% CI, -2.1384 to -1.7581]; -1.7080 [95% CI, -1.8764 to -1.5394]; -1.8521 [95% CI, -2.0437 to -1.6601]; -1.9484 [95% CI, -2.1384 to -1.7581]) (Table 1-6).
Projections of the burden of LOCC from 2022 to 2030
Based on the BAPC predictive model, this study found that the global burden of LOCC will exhibit significant sex differences from 2022 to 2030. Specifically, the ASIR and ASPR among males are projected to decline, whereas the opposite trend is anticipated for females. Moreover, by 2030, both sexes are expected to experience a decrease in the ASDR, ASR of DALYs, and YLLs. However, the ASR of YLDs is projected to increase for both sexes (Figure 2).
Figure 2
Projections of the burden of lip and oral cavity cancer (LOCC) by gender from 2022 to 2030 based on the Bayesian Age-Period-Cohort (BAPC) model. (A–C) depict the forecasted age-standardized prevalence rate (ASPR), age-standardized incidence rate (ASIR), and age-standardized death rate (ASDR) for females, respectively. (D–F) present the corresponding projections for males. (G-I) illustrate the predicted age-standardized rates of disability-adjusted life years (DALYs), years of life lost (YLLs), and years lived with disability (YLDs) for females, while Panels (J-L) show these predictions for males.
Specifically, compared to the Incidence of LOCC in males in 2021, the number of cases or years is projected to increase by 17.3% by 2030, the number of Death by 12.1%, the Prevalence by 17.4%, the number of DALYs by 14.7%, the number of YLLs by 14.6%, and the number of YLDs by 9.1%. Except for the ASR of YLDs in males, all other indicators were expected to show a downward trend. Specifically, the ASIR was projected to decrease from 6.65 to 6.58, the ASDR from 3.39 to 3.28, the ASPR from 23.02 to 22.66, the ASR of DALYs from 93.98 to 90.58, and the ASR of YLLs from 91.50 to 88.16, while the ASR of YLDs is expected to increase from 2.49 to 2.51, with all rates expressed per 100,000 population. Additionally, by 2030, the Incidence of LOCC in females was projected to increase by 18.3%, Death by 7.9%, Prevalence by 23.2%, DALYs by 18.6%, YLLs by 18.2%, and YLDs by 5.7%. The ASIR in females was expected to rise from 3.29 to 3.39, the ASPR from 12.65 to 12.96, and the ASR of YLDs from 1.28 to 1.35. Conversely, the ASDR is projected to decrease from 1.58 to 1.57, the ASR of DALYs from 42.43 to 41.93, and the ASR of YLLs from 41.16 to 40.65, with all rates expressed per 100,000 population. These projections suggest that, compared to 2021, the life milestones of LOCC patients of both sexes in 2030 will likely see a delay in the time of death and an increase in survival duration.
Moreover, this study also compared the LOCC disease burden among different age groups of males and females in 2021 and 2030. The findings revealed that, for both sexes, the ASR and the number of cases increase with age, particularly in middle-aged and elderly populations, where this trend is more pronounced. Specifically, patients aged over 50 years are projected to constitute the majority of all LOCC patients (Figure 3). This indicates that middle-aged and elderly LOCC patients will continue to pose a significant challenge in the efforts to reduce the LOCC disease burden in the future.
Figure 3
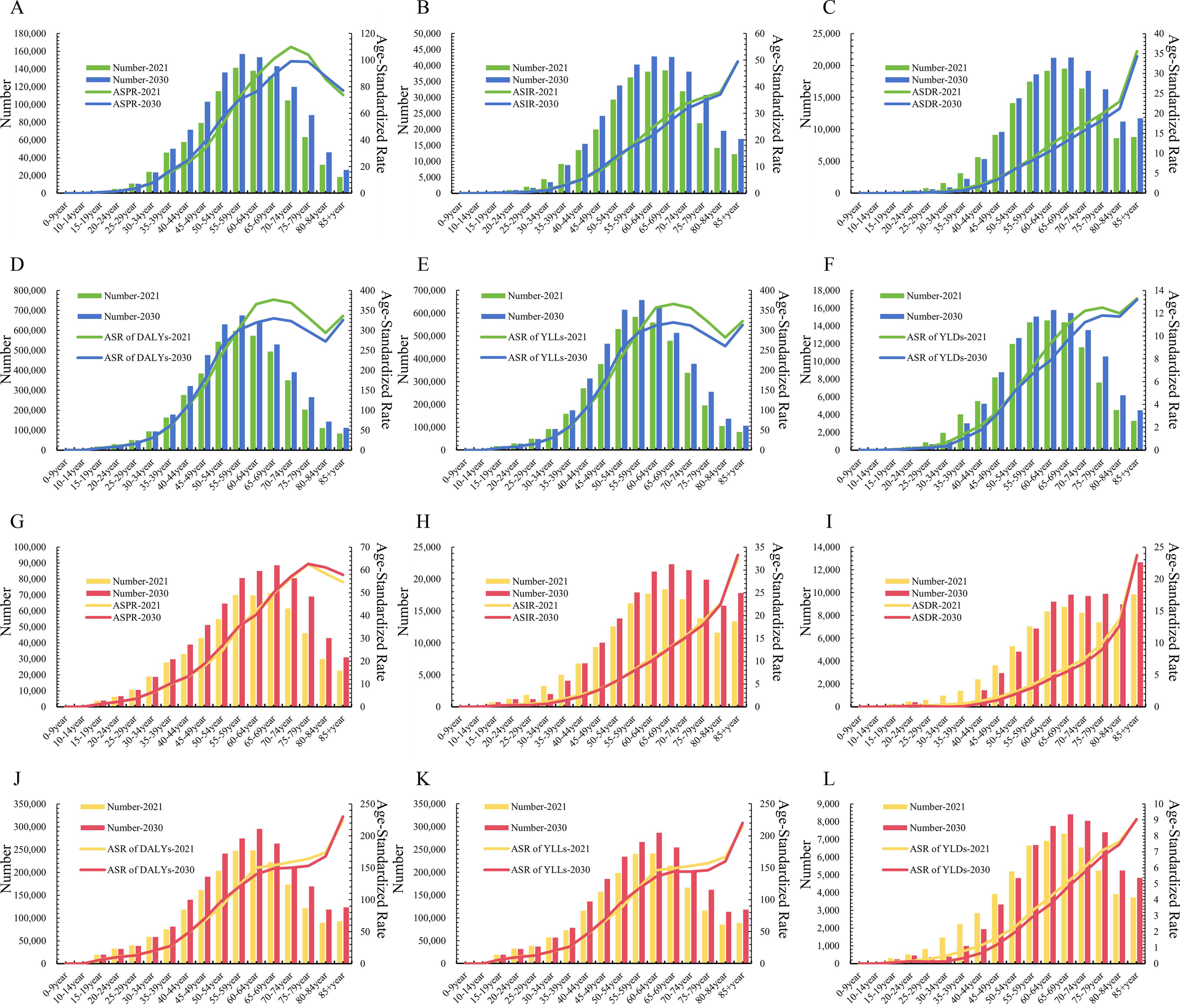
Comparison of projected burden of lip and oral cavity cancer (LOCC) across different age groups for the years 2022 and 2030 based on the Bayesian Age-Period-Cohort (BAPC) model. (A–F) represent the prevalence, incidence, deaths, disability-adjusted life years (DALYs), years of life lost (YLLs), and years lived with disability (YLDs) for males, respectively. Panels (G-L) depict the corresponding metrics for females.
Discussion
Drawing on the GBD 2021 database, this study conducted a analysis of the global burden of LOCC from 1990 to 2021 and employed the BAPC model to forecast the trends of LOCC from 2022 to 2030. Globally, South Asia emerged as the GBD region with the most severe LOCC burden in 2021. Between 1990 and 2021, the global ASIR, ASPR, and ASR of YLDs for LOCC exhibited a marked upward trend, whereas the ASDR, ASR of DALYs, and ASR of YLLs showed a downward trajectory. Notably, East Asia and Western Europe experienced more pronounced annual changes in LOCC burden. By 2030, the DALYs and YLLs are projected to decline, likely due to a reduction in death and an extension in survival duration among LOCC patients, while the ASR of YLDs is expected to rise. Overall, the burden of LOCC remains a significant global concern.
Numerous factors contribute to the severe burden of LOCC. Among these, lifestyle habits exert a particularly significant influence on LOCC (15). Specifically, the practice of chewing betel quid can directly damage the oral mucosa and induce genetic mutations, thereby triggering oral cavity cancer (15, 16). China, Myanmar, India, and Bangladesh, as major global producers of betel nut, also exhibit extremely high levels of betel nut consumption (17, 18). Moreover, approximately half of the oral cavity cancer cases reported in East Asian countries are attributed to betel nut chewing (19). This is likely one of the reasons for the prominent EAPC of LOCC in East Asia and the ASDR in South Asia. Furthermore, ultraviolet (UV) radiation serves as a critical risk factor for the development of lip cancer (20). UV rays have the capacity to disrupt DNA within skin and mucosal cells, thereby inducing genetic mutations and elevating the likelihood of lip cancer (21, 22). Our research has identified a marked escalation in the burden of LOCC within Oceania, a trend potentially linked to the region’s geographical context. The disparity in solar radiation exposure across regions, attributable to their latitudinal positions and variations in the ozone layer, plays a significant role (23). Regions including South Asia, Oceania, and Australasia et.al, are commonly subjected to higher intensities of UV radiation, which is likely a principal factor underlying the substantial burden of lip cancer in these locales (24, 25). Consequently, the adoption of prudent sun protection strategies is instrumental in mitigating the risk of lip cancer. It is essential to initiate preventive initiatives aimed at enhancing the awareness of utilizing sunscreen and hats, especially within countries with strong UV.
The global ASDR of LOCC has shown a gradual decline (with a negative EAPC), and projections for 2022–2030 indicate a downward trend in the ASDR, ASR of DALYs, and YLLs due to LOCC worldwide. These positive shifts are likely due to significant advancements in the global LOCC healthcare sector. In terms of early diagnostic techniques, oral exfoliative cytology enables the detection of potential cancer cells in the oral cavity by analyzing cells collected from the oral mucosa, particularly in patients with submucosal fibrosis (10). Innovations in surgical techniques have also led to improved treatment outcomes for LOCC patients (26, 27). Targeted radiotherapy technologies can precisely focus high doses of radiation on tumor sites, enhancing local tumor control rates and improving the survival duration of LOCC patients (28–31). However, there were notable differences in the changes of ASDR across different regions. Western Europe has experienced the most significant average annual decline in ASDR, with a marked decrease observed in males, which may be associated with its comprehensive and advanced healthcare system. In Western Europe, efficient cancer screening networks have been established, facilitating more accurate early detection of cancer (3, 32). Meanwhile, the decline in the burden of LOCC in Australasia and High-income North America, including Australia and the United States, may be related to a decrease in the number of people working outdoors and an increase in primary prevention of solar radiation by outdoor workers using sunscreen and protective clothing and headgear (4). Therefore, we advocate that early screening for LOCC should draw inspiration from Western Europe, aiming to refine and establish an effective early detection system for cancers.
This study projects that between 2022 and 2030, the ASIR and ASPR of LOCC will exhibit a declining trend in males globally, whereas an upward trend is anticipated in females. Moreover, the burden of LOCC is particularly severe among middle-aged and elderly populations, with older females being disproportionately affected. This phenomenon may be closely linked to a lack of awareness regarding oral health among the elderly (33). Many seniors fail to implement timely and effective personal oral care in their daily routines, leading to a gradual accumulation of oral health issues (34, 35). the phenomenon of delayed medical treatment within the elderly population also contributes to the failure to effectively control oral diseases at early stages, thereby exacerbating the overall LOCC burden (34). As the population continues to age, the LOCC burden among middle-aged and elderly individuals will face even more formidable challenges in the future. Furthermore, the ASIR and ASPR of female LOCC were higher than those of males, which may be attributed to changes in consumption patterns of cigarette smoking (4). Scholars have pointed out that the impact of smoking on the historical trends of oral cavity cancer is reflected in its similarity to the trends of lung cancer two decades later; in several European countries, the incidence of lung cancer among male continues to decline, while it rises among female, which coincides with the lag time of cigarette smoking consumption (4). Consequently, there is an urgent need to develop more targeted diagnostic and treatment measures, enhance educational efforts on lip and oral cavity health for the elderly, elevate their awareness of lip and oral cavity health, and optimize the allocation of medical service resources to address the growing burden of LOCC. At the same time, it is also necessary to strengthen publicity about the hazards of smoking consumption to LOCC and raise public awareness regarding this risk factor.
From a disease control and prevention strategy perspective, the findings of this study provide direction for global LOCC management. For regions experiencing rapid increases in Incidence rates, such as East Asia, it is essential to widely disseminate health knowledge related to LOCC and enhance the public’s awareness of the disease. Concurrently, establishing a robust screening system, increasing investment in oral healthcare facilities, training specialized oral screening personnel, and promoting regular oral examinations are crucial, especially for high-risk groups such as long-term betel nut chewers, who should have shorter intervals between check-ups to facilitate early detection and treatment. For regions where the ASDR was not significantly declining or still rising, such as Oceania and some parts of Sub-Saharan Africa, in addition to strengthening health education and screening efforts, we advocate for increased investment in medical resources, improving primary healthcare facilities, and introducing advanced oral examination equipment and LOCC treatment technologies to areas with a high burden of LOCC.
Lastly, this study also has certain limitations. Issues such as non-standardized data collection methods and insufficient sample representativeness may lead to some variation in data quality, potentially interfering with the accuracy of the analytical results to a certain extent. For instance, some developing countries may experience underreporting or misreporting due to a lack of comprehensive disease registration systems and professional data collectors, affecting an accurate assessment of the local LOCC burden. Thus, we suggest integrating and strengthen cancer registry data to mitigate this limitation in future studies. Furthermore, as this study was based on existing data and models for analysis and forecasting, there may be unforeseen factors impacting the burden of LOCC.
Conclusion
The LOCC burden remains severe at present, but it is anticipated to exhibit a downward trend by 2030. Consequently, it is imperative to intensify efforts in the prevention and control of LOCC to meet these expectations. This study offers theoretical guidance for mitigating the burden of LOCC. In light of the findings, we should enhance control and preventive measures against LOCC, focusing on aspects such as regulating betel nut consumption, promoting lip and oral cavity sun protection, and ensuring timely access to medical services. These targeted interventions are crucial for reducing the incidence and improving the prognosis of LOCC, thereby contributing to a decrease in the overall disease burden. By prioritizing these areas, we can work towards a future where the impact of LOCC on global health is significantly diminished.
Statements
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://vizhub.healthdata.org/gbd-results/.
Author contributions
Q-YM: Data curation, Resources, Conceptualization, Methodology, Writing – review & editing, Writing – original draft, Software. M-L: Formal Analysis, Writing – review & editing. S-WC: Software, Writing – original draft, Visualization. S-RT: Resources, Writing – review & editing, Formal Analysis, Software, Visualization, Writing – original draft, Data curation, Conceptualization, Validation, Project administration, Methodology, Supervision, Investigation.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Howard A Agrawal N Gooi Z . Lip and oral cavity squamous cell carcinoma. Hematol Oncol Clin North Am. (2021) 35:895–911. doi: 10.1016/j.hoc.2021.05.003
2
Schüller M Gosau M Müller S Gerken M Rohrmeier C Legal S et al . Long-term outcome and subjective quality of life after surgical treatment of lower lip cancer. Clin Oral Investig. (2015) 19:1093–9. doi: 10.1007/s00784-014-1327-x
3
Hashim D Genden E Posner M Hashibe M Boffetta P . Head and neck cancer prevention: from primary prevention to impact of clinicians on reducing burden. Ann Oncol. (2019) 30:744–56. doi: 10.1093/annonc/mdz084
4
Miranda-Filho A Bray F . Global patterns and trends in cancers of the lip, tongue and mouth. Oral Oncol. (2020) 102:104551. doi: 10.1016/j.oraloncology.2019.104551
5
Roghanizadeh L Atarbashi-Moghadam S Masaebi F Baghban AA . Lip and oral cavity cancer in Iran from 1990 to 2019 based on the global burden of disease study. Sci Rep. (2025) 15:7389. doi: 10.1038/s41598-025-92090-w
6
Ghanem AS Tóth Á Nagy AC . Socio-demographic disparities in global trends of lip and oral cavity neoplasms from 1990 to 2021. Sci Rep. (2025) 15:4230. doi: 10.1038/s41598-025-88684-z
7
Rezapour A Jahangiri R Olyaeemanesh A Kalaghchi B Nouhi M Nahvijou A . The economic burden of oral cancer in Iran. PloS One. (2018) 13:e0203059. doi: 10.1371/journal.pone.0203059
8
Pollaers K Massingham I Friedland PL Farah CS . The economic burden of oral squamous cell carcinoma in Australia. J Oral Pathol Med. (2019) 48:588–94. doi: 10.1111/jop.12907
9
GBD . 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2100–32. doi: 10.1016/S0140-6736(24)00367-2
10
GBD . 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2133–61. doi: 10.1016/S0140-6736(24)00757-8
11
Cen J Wang Q Cheng L Gao Q Wang H Sun F . Global, regional, and national burden and trends of migraine among women of childbearing age from 1990 to 2021: insights from the Global Burden of Disease Study 2021. J Headache Pain. (2024) 25:96. doi: 10.1186/s10194-024-01798-z
12
Han L Zhao T Zhang R Hao Y Jiao M Wu Q et al . Burden of nutritional deficiencies in China: findings from the global burden of disease study 2019. Nutrients. (2022) 14:3919. doi: 10.3390/nu14193919
13
Wang F Ma B Ma Q Liu X . Global, regional, and national burden of inguinal, femoral, and abdominal hernias: a systematic analysis of prevalence, incidence, deaths, and DALYs with projections to 2030. Int J Surg. (2024) 110:1951–67. doi: 10.1097/JS9.0000000000001071
14
Bai Z Wang H Shen C An J Yang Z Mo X . The global, regional, and national patterns of change in the burden of nonmalignant upper gastrointestinal diseases from 1990 to 2019 and the forecast for the next decade. Int J Surg. (2025) 111:80–92. doi: 10.1097/JS9.0000000000001902
15
Chamoli A Gosavi AS Shirwadkar UP Wangdale KV Behera SK Kurrey NK et al . Overview of oral cavity squamous cell carcinoma: Risk factors, mechanisms, and diagnostics. Oral Oncol. (2021) 121:105451. doi: 10.1016/j.oraloncology.2021.105451
16
Warnakulasuriya S Chen THH . Areca nut and oral cancer: evidence from studies conducted in humans. J Dent Res. (2022) 101:1139–46. doi: 10.1177/00220345221092751
17
Chen Q Hu X Li D Huang X . Areca nut and oral cancer: warnings and prevention in China. Br Dent J. (2025) 238:10–1. doi: 10.1038/s41415-025-8282-6
18
Arora S Squier C . Areca nut trade, globalisation and its health impact: perspectives from India and South-east Asia. Perspect Public Health. (2019) 139:44–8. doi: 10.1177/1757913918785398
19
Warnakulasuriya S Chen THH . Areca nut and oral cancer: evidence from studies conducted in humans. J Dent Res. (2022) 101:1139–46. doi: 10.1177/00220345221092751
20
Huang J Chan SC Ko S Lok V Zhang L Lin X et al . Disease burden, risk factors, and trends of lip, oral cavity, pharyngeal cancers: A global analysis. Cancer Med. (2023) 12:18153–64. doi: 10.1002/cam4.6391
21
Shield KD Ferlay J Jemal A Sankaranarayanan R Chaturvedi AK Bray F et al . The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012. CA Cancer J Clin. (2017) 67:51–64. doi: 10.3322/caac.21384
22
D’souza S Addepalli V . Preventive measures in oral cancer: An overview. BioMed Pharmacother. (2018) 107:72–80. doi: 10.1016/j.biopha.2018.07.114
23
Khalid A van Essen P Crittenden TA Dean NR . The anatomical distribution of non-melanoma skin cancer: a retrospective cohort study of 22 303 Australian cases. ANZ J Surg. (2021) 91:2750–6. doi: 10.1111/ans.17030
24
Unsal AA Unsal AB Henn TE Baredes S Eloy JA . Cutaneous squamous cell carcinoma of the lip: A population-based analysis. Laryngoscope. (2018) 128:84–90. doi: 10.1002/lary.26704
25
Silva LVO de Arruda JAA Abreu LG Ferreira RC da Silva LP Pelissari C et al . Demographic and clinicopathologic features of actinic cheilitis and lip squamous cell carcinoma: a Brazilian multicentre study. Head Neck Pathol. (2020) 14:899–908. doi: 10.1007/s12105-020-01142-2
26
de Wit JG van Schaik JE Voskuil FJ Vonk J de Visscher SAHJ Schepman KP et al . Comparison of narrow band and fluorescence molecular imaging to improve intraoperative tumour margin assessment in oral cancer surgery. Oral Oncol. (2022) 134:106099. doi: 10.1016/j.oraloncology.2022.106099
27
Chellappan B Obanigba G Hoyer P Ross L . Lip reconstruction after mohs micrographic surgery: A guide on flaps. Cutis. (2023) 111:205–9. doi: 10.12788/cutis.0743
28
Quinlan-Davidson SR Mohamed ASR Myers JN Gunn GB Johnson FM Skinner H et al . Outcomes of oral cavity cancer patients treated with surgery followed by postoperative intensity modulated radiation therapy. Oral Oncol. (2017) 72:90–7. doi: 10.1016/j.oraloncology.2017.07.002
29
Huang SH Hahn E Chiosea SI Xu ZY Li JS Shen L et al . The role of adjuvant (chemo-)radiotherapy in oral cancers in the contemporary era. Oral Oncol. (2020) 102:104563. doi: 10.1016/j.oraloncology.2019.104563
30
Hosni A Chiu K Huang SH Xu W Huang J Bayley A et al . Non-operative management for oral cavity carcinoma: Definitive radiation therapy as a potential alternative treatment approach. Radiother Oncol. (2021) 154:70–5. doi: 10.1016/j.radonc.2020.08.013
31
Merfeld EC Witek ME Francis DM Burr AR Wallace CR Kuczmarska-Haas A et al . Interstitial brachytherapy for lip cancer: technical aspects to individualize treatment approach and optimize outcomes. Pract Radiat Oncol. (2023) 13:340–5. doi: 10.1016/j.prro.2023.01.004
32
Maver PJ Poljak M . Primary HPV-based cervical cancer screening in Europe: implementation status, challenges, and future plans. Clin Microbiol Infect. (2020) 26:579–83. doi: 10.1016/j.cmi.2019.09.006
33
Batchelor P . The changing epidemiology of oral diseases in the elderly, their growing importance for care and how they can be managed. Age Ageing. (2015) 44:1064–70. doi: 10.1093/ageing/afv148
34
Varela-Centelles P Seoane J Lopez-Cedrun JL Fernandez-Sanroman J García-Martin JM Takkouche B et al . The length of patient and primary care time interval in the pathways to treatment in symptomatic oral cancer. A quantitative systematic review. Clin Otolaryngol. (2018) 43:164–71. doi: 10.1111/coa.12919
35
Metzger K Moratin J Horn D Pilz M Ristow O Hoffmann J et al . Treatment delay in early-stage oral squamous cell carcinoma and its relation to survival. J Craniomaxillofac Surg. (2021) 49:462–7. doi: 10.1016/j.jcms.2021.02.007
Summary
Keywords
lip and oral cavity cancer, global burden of disease, estimated annual percentage change, bayesian age-period-cohort model, prevention
Citation
Mu Q-Y, Min-Li, Chen S-W and Tang S-R (2025) Current and future burden trends of lip and oral cavity cancer based on estimated annual percentage change and the Bayesian age-period-cohort model: a study based on the global burden of disease 2021. Front. Oncol. 15:1674054. doi: 10.3389/fonc.2025.1674054
Received
27 July 2025
Accepted
29 September 2025
Published
22 October 2025
Volume
15 - 2025
Edited by
Sven Eric Niklander, Universidad Andres Bello, Chile
Reviewed by
Sebastiaan De Visscher, University Medical Center Groningen, Netherlands
René Andrés Martinez-Flores, Universidad Andrés Bello, Chile
Updates
Copyright
© 2025 Mu, Min-Li, Chen and Tang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheng-Rong Tang, shengrongt2025@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.