- 1Longhua Hospital affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 2Department of Plastic and Reconstructive Surgery, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
A 73-year-old man presented with a 20-year history of a mass in the right scapular region that had rapidly enlarged and become painful. Initially misdiagnosed as an infected sebaceous cyst, intraoperative findings revealed a solid, poorly demarcated mass. Histopathology confirmed malignant transformation of a neurofibroma into a high-grade malignant peripheral nerve sheath tumor, with positive margins. The patient underwent wide local excision with frozen-section–verified clear margins and full-thickness back flap reconstruction. On postoperative day 3, the flap developed progressive ischemic necrosis. Salvage was achieved using a novel combination of topical papaverine hydrochloride, Danhong injection, and enzymatic debridement, leading to full revascularization by day 9. The patient was discharged in stable condition on day 15. This case underscores the need for early pathological evaluation of rapidly enlarging skin masses when clinical and imaging findings are discordant. It also demonstrates the successful use of papaverine, Danhong, and enzymatic debridement as a salvage strategy for postoperative flap necrosis.
1 Introduction
MPNST is a rare and aggressive soft tissue sarcoma that accounts for 5% to 10% of soft tissue malignancies and is commonly associated with patients with NF1 or prior radiotherapy exposure (1). The aggressive nature confers a 5-year survival rate of 30%-50%, with high risks of local recurrence and distant metastasis (2–4).
2 Case description
A 73-year-old male presented with a 20-year history of a slowly enlarging right scapular region mass. Initially diagnosed as a sebaceous cyst and managed conservatively, the lesion acutely increased in size with associated pain and erythema over one week. Physical examination revealed a 6x6 cm firm, erythematous, tender mass near the right posterior axillary line at the ninth thoracic vertebra level. Color Doppler ultrasound identified an ill-defined, heterogeneous hypoechoic subcutaneous nodule (61x26 mm) with peripheral vascularity, suggestive of an infected sebaceous cyst.
Under local anesthesia, incision and drainage were attempted. Intraoperatively, no purulent material was encountered; instead, a solid subcutaneous mass was identified.
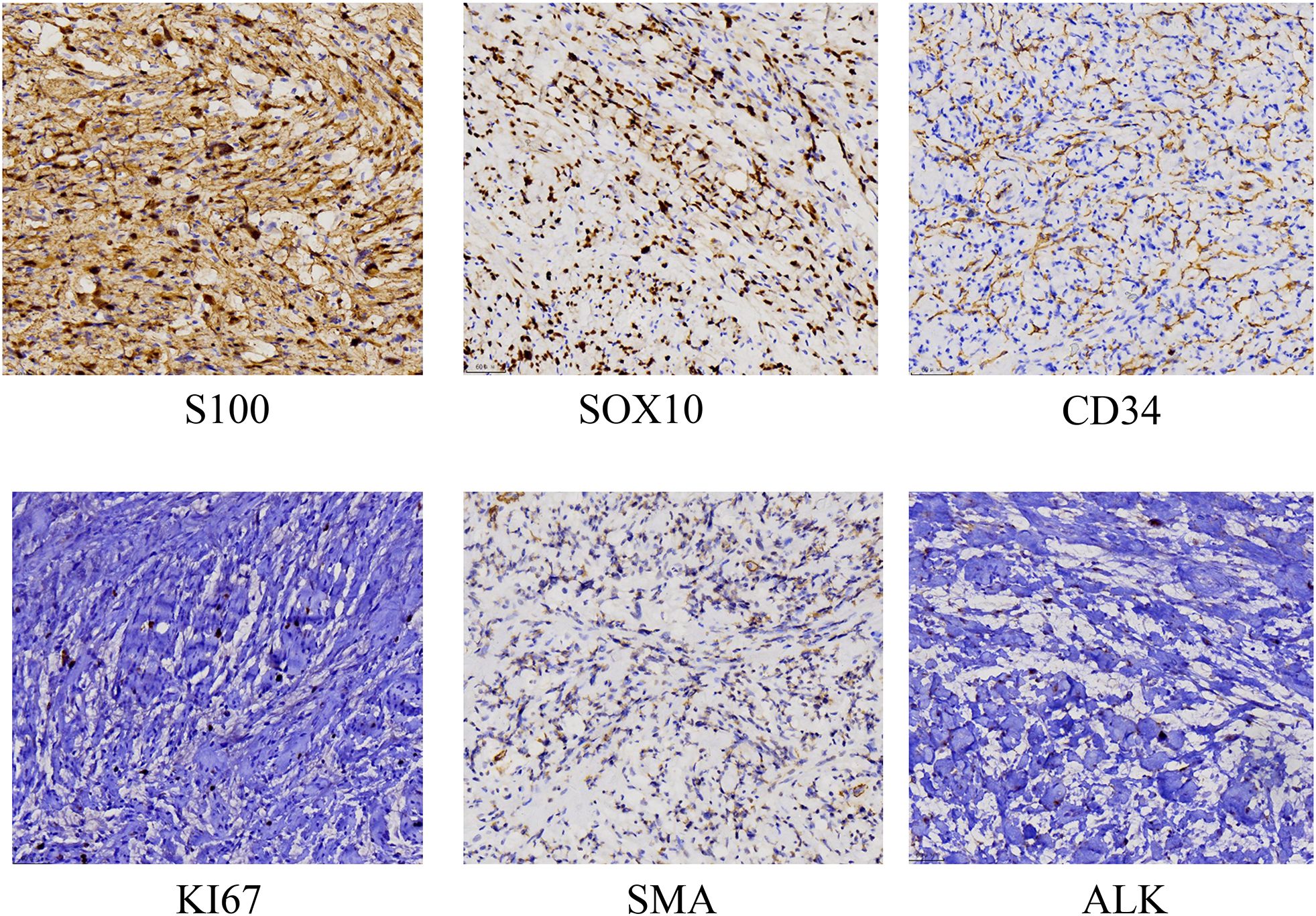
Histopathology revealed malignant transformation of a neurofibroma into a high-grade malignant peripheral nerve sheath tumor (MPNST) with involvement of lateral and deep margins. Immunohistochemistry supported the diagnosis (S-100 positive, Ki-67 10%, SMA negative, CD34 positive, ALK positive) (Figure 1). Additional imaging studies excluded distant metastasis and provided valuable information for determining the extent of surgery. Wide local excision was subsequently performed. A 2-cm margin was excised down to the latissimus dorsi, and tumor-free margins were confirmed from four quadrants by intraoperative frozen sections. Due to the large defect, a rotating flap is designed under ultrasound positioning during the operation (Figures 2A–E).
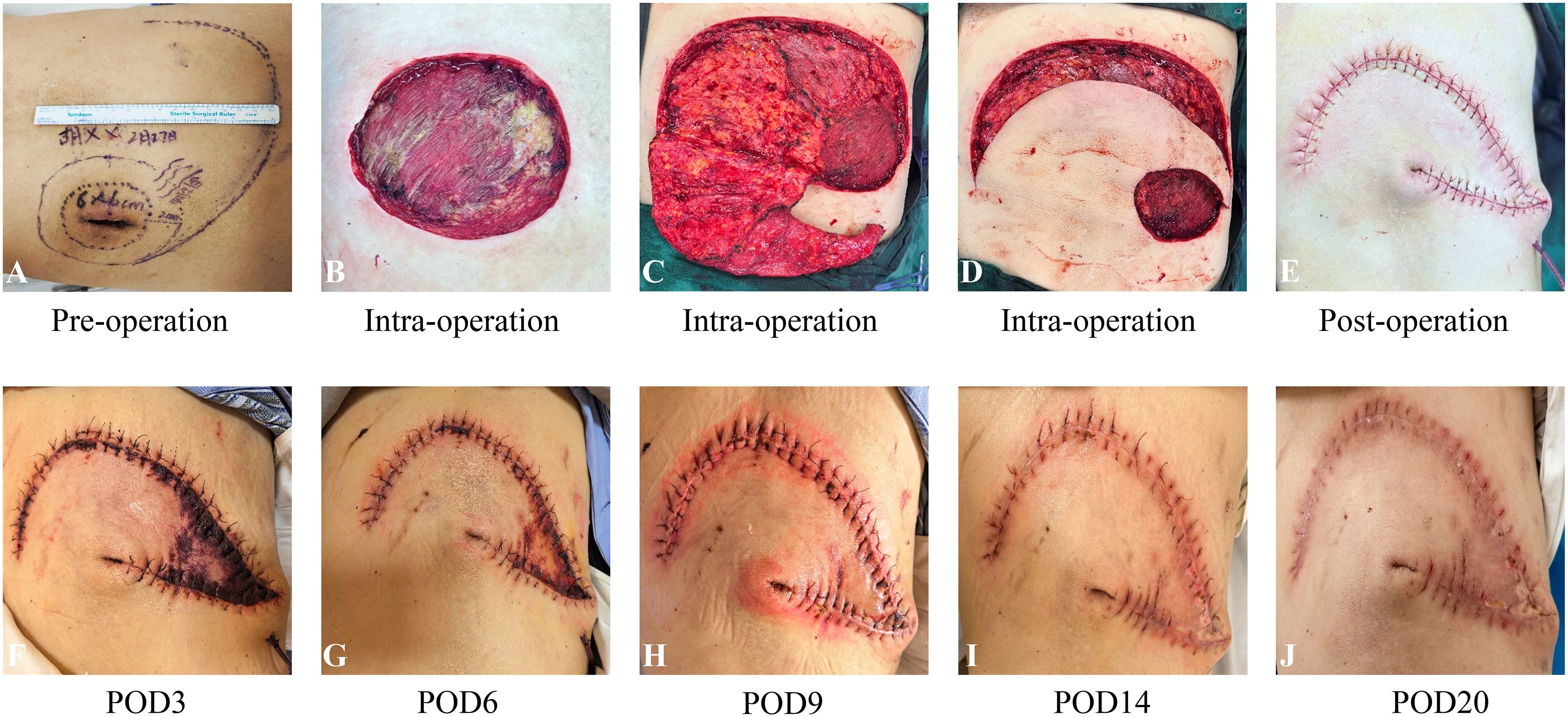
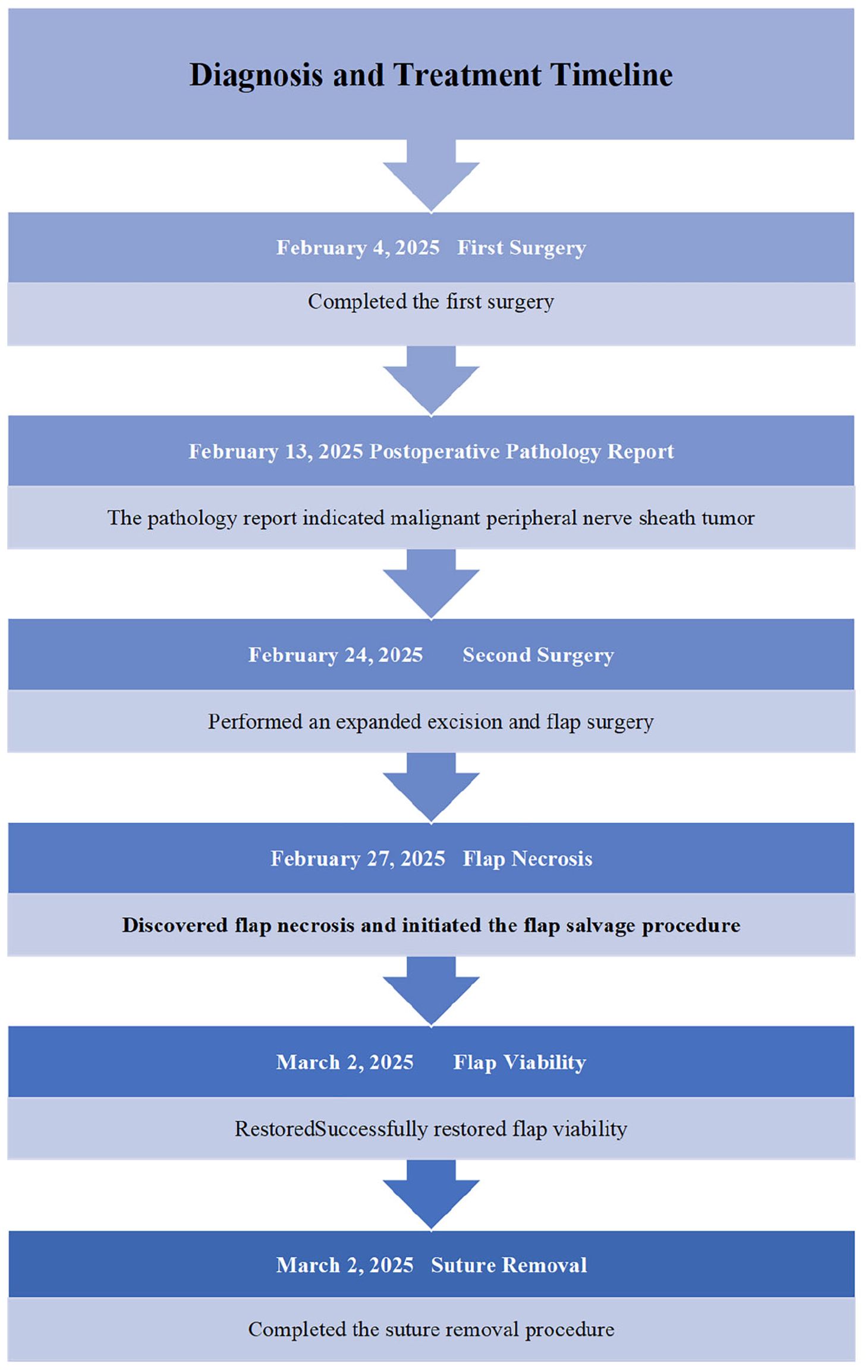
Figure 2. Skin manifestations, clinical course and timeline flap necrosis and subsequent recovery. (A) preoperative photograph. (B–D) intraoperative photographs showing flap design. (E) postoperative photograph after wound closure. (F) postoperative day 3, distal flap discoloration noted, indicating early signs of ischemia. (G–J) process of flap salvage.
On postoperative day 3, flap necrosis involving approximately 30% of the area was observed, which exhibited signs of progressive ischemic compromise, characterized by darkening of the skin, diminished capillary refill, and advancing necrosis. Salvage therapy was initiated immediately: intravenous use of papaverine hydrochloride injection (30mg tid) and Danhong injection (20ml qd) was started. At the same time, the dressing regimen was adjusted to cover the flap with a biological enzyme gauze dressing (ShaBuChuangMianFuLiao, 7.5cm×7.5cm (four layers)). On postoperative day 6, perfusion improved and 50% flap revascularization was achieved. On the 9th day, the flap demonstrated complete revascularization with restoration of normal color and turgor. On the 14th day after surgery, intermittent suture removal was started (Figures 2F–J). For 30 days after surgery, the skin healed completely. The patient was discharged in stable condition. The diagnosis and treatment timeline is shown in Table 1.
3 Discussion
3.1 MPNST diagnostic challenges and surgical management
The main clinical manifestations of MPNSTs include pain and numbness, however, these symptoms are non-specific, making it challenging to differentiate MPNSTs from other nerve-related lesions (5–8). Approximately 50% of MPNST cases are associated with neurofibromatosis type 1 (NF1), where neurofibromas, particularly plexiform neurofibromas (PNFs), have the potential to transform into MPNSTs. Additionally, around 10% of MPNST patients have a history of radiation exposure (2). PNFs and atypical neurofibromatous neoplasms of unknown biological potential (ANNUBPs) are significant high-risk factors for the development of MPNSTs. Patients with PNFs or ANNUBPs, especially those with NF1, should be closely monitored for signs of malignant transformation to ensure early detection and intervention (9). However, preoperative misdiagnosis remains common in atypical areas, such as the skin and subcutaneous tissue, where lesions may mimic benign entities like sebaceous cysts or lipomas, potentially delaying definitive management. This case underscores the critical need for pathological confirmation in patients with rapidly evolving masses in cases of clinical-imaging discordance.
For MPNST treatment, achieving R0 resection is crucial (10). While complete surgical resection is the primary treatment for MPNST it is often hindered by the large size of tumors, their proximity to complex nerve networks, and a low rate of negative resection margins. In this case, quadrant-based specimen orientation combined with intraoperative frozen section analysis enabled targeted excision until histologically negative margins were achieved. Preoperative ultrasound mapping of perforator vessels facilitated flap design while preserving vascular integrity. This integrated approach supports complex reconstruction while maintaining optimal oncologic safety.
3.1 Flap necrosis salvage: mechanistic rationale
Flap surgery is a crucial surgical technique for the repair of tissue defects resulting from tumor excision, trauma, vascular ulcers of the lower extremities, or skin loss due to diabetes, which plays a vital role in restoring both the structure and function of the affected area. However, it is associated with various complications, such as flap necrosis and wound dehiscence, with an incidence of up to around 50% (11). The primary mechanisms underlying flap necrosis are inadequate blood perfusion, impaired venous return, and ischemia-reperfusion injury (12). When the extent of ischemia exceeds the tissue’s tolerance threshold within a short period, and no intervention is made, the ischemic tissue will undergo irreversible necrosis.
Postoperative flap necrosis involving approximately 30% of the surface area on postoperative day (POD) 3 was managed using an integrative multimodal regimen combining Western pharmacotherapy and traditional Chinese medicine, alongside targeted local therapy. Papaverine is a non-opioid vasodilator that induces vasodilation by inhibiting cAMP/cGMP phosphodiesterase, increasing intracellular cyclic nucleotide levels to relieve microvascular spasm and enhance perfusion. Therefore, papaverine is especially important for flaps in ischemic conditions, as it can effectively improve tissue oxygenation and nutrient supply. In addition, papaverine alleviates ischemia-reperfusion injury by reducing the production of free radicals, decreasing intracellular calcium concentrations, and inhibiting inflammatory responses, further promoting flap survival and repair (13).
To augment its effects, we incorporated Danhong injection—a standardized traditional Chinese medicine formulation derived from Salvia and safflower—known for vasodilatory, anti-inflammatory, and pro-angiogenic properties in cardiovascular and cerebrovascular disorders (14–16). We think that the combination produces synergistic improvement in microcirculation. Externally, a biological enzyme gauze dressing was applied to maintain a moist wound-healing environment and promote tissue revitalization. Wet healing theory has been widely recognized in clinical practice and applied to wound treatment. Bioenzyme dressings have the ability to inhibit, stop bleeding, and promote wound healing due to their good biocompatibility, biodegradability, and biological functions. Conventional salvage strategies, including surgical revascularization, endovascular intervention, and systemic anticoagulation, primarily aim to restore macroscopic blood flow (17, 18). These methods are effective in restoring macroscopic blood flow but may be limited in cases with microvascular compromise, diffuse disease, or patients unsuitable for invasive interventions. Conventional techniques are considered the cornerstone of flap salvage. When inadequate perfusion is identified, correction of mechanical factors is generally prioritized, including suture release, hematoma evacuation, and surgical re-exploration when indicated. Adjunctive measures such as warming, administration of antispasmodic agents, and anticoagulant or antiplatelet therapy can be applied. These interventions are primarily directed at resolving vascular compromise and are regarded as first-line management.
This comprehensive treatment regimen achieved complete flap recovery by POD 9—substantially faster than typical recovery times reported with conventional therapy. We think that this regimen not only focuses on mechanical restoration of blood supply but also emphasizes microcirculatory regulation and wound bed optimization. To our knowledge, this is the first documented use of Danhong injection in postoperative flap salvage, representing an innovative application of combined Chinese and Western medical approaches to optimize microcirculatory restoration and reconstructive outcomes. Notably, the dosage and treatment duration should be adjusted on a case-by-case basis in accordance with patient-specific factors.
However, the follow-up period was limited to 3 months, which does not allow for assessment of long-term oncological safety, durability of flap survival, or recurrence risk. In addition, the comprehensive treatment regimen lacks standardized protocols, which may affect reproducibility and comparability. Although the treatment was well tolerated in this patient, potential drug interactions, adverse effects, and cost considerations warrant further evaluation. From the patient’s perspective, the treatment was reported as tolerable and acceptable, with subjective improvement in comfort and confidence during recovery; nevertheless, systematic incorporation of patient-reported outcomes will be important in future studies.
4 Conclusion
This case illustrates the diagnostic pitfalls of subcutaneous MPNSTs masquerading as infected cysts. The case highlights two key points (1): Clinicians are warned to expand the scope of differential diagnosis for subcutaneous masses that suddenly enlarge in elderly patients, especially when imaging is inconsistent with clinical manifestations, pathological examination should be performed as soon as possible to avoid misdiagnosis. If the mass is discovered during surgery, it is recommended to do frozen pathological examination in time (2). For evolving flap ischemia, we need timely multimodal intervention. The successful reversal of significant flap necrosis using triple therapy (papaverine, Danhong injection, and enzymatic debridement) offers a reference for wound management after similar plastic flap surgery. Further studies should explore the synergistic mechanisms of this pharmacologic approach in reconstructive surgery. This case contributes new insights and addresses an existing gap in the literature regarding similar instances.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Longhua Hospital, Shanghai University of Traditional Chinese Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
LC: Visualization, Writing – original draft, Writing – review & editing. XW: Writing – review & editing. FL: Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by Natural Science Foundation of China (grant nos.82474506).
Acknowledgments
We thank the patient for permitting us to use his data to complete this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1689834/full#supplementary-material
References
1. Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, and Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. (1986) 57:2006–21. doi: 10.1002/1097-0142(19860515)57:10<2006::aid-cncr2820571022>3.0.co;2-6
2. Stucky CC, Johnson KN, Gray RJ, Pockaj BA, Ocal IT, Rose PS, et al. Malignant peripheral nerve sheath tumors (MPNST): the Mayo Clinic experience. Ann Surg Oncol. (2012) 19:878–85. doi: 10.1245/s10434-011-1978-7
3. Wong WW, Hirose T, Scheithauer BW, Schild SE, and Gunderson LL. Malignant peripheral nerve sheath tumor: analysis of treatment outcome. Int J Radiat oncology biology physics. (1998) 42:351–60. doi: 10.1016/S0360-3016(98)00223-5
4. Zou C, Smith KD, Liu J, Lahat G, Myers S, Wang WL, et al. Clinical, pathological, and molecular variables predictive of Malignant peripheral nerve sheath tumor outcome. Ann surgery. (2009) 249:1014–22. doi: 10.1097/SLA.0b013e3181a77e9a
5. Reilly KM, Kim A, Blakely J, Ferner RE, Gutmann DH, Legius E, et al. Neurofibromatosis type 1-associated MPNST state of the science: outlining a research agenda for the future. J Natl Cancer Institute. (2017) 109. doi: 10.1093/jnci/djx124
6. Mowery A and Clayburgh D. Malignant peripheral nerve sheath tumors: Analysis of the national cancer database. Oral Oncol. (2019) 98:13–9. doi: 10.1016/j.oraloncology.2019.09.010
7. Le Guellec S, Decouvelaere AV, Filleron T, Valo I, Charon-Barra C, Robin YM, et al. Malignant peripheral nerve sheath tumor is a challenging diagnosis: A systematic pathology review, immunohistochemistry, and molecular analysis in 160 patients from the french sarcoma group database. Am J Surg pathology. (2016) 40:896–908. doi: 10.1097/PAS.0000000000000655
8. Zhou HY, Jiang S, Ma FX, and Lu H. Peripheral nerve tumors of the hand: Clinical features, diagnosis, and treatment. World J Clin cases. (2020) 8:5086–98. doi: 10.12998/wjcc.v8.i21.5086
9. Yao C, Zhou H, Dong Y, Alhaskawi A, Hasan Abdullah Ezzi S, Wang Z, et al. Malignant peripheral nerve sheath tumors: latest concepts in disease pathogenesis and clinical management. Cancers. (2023) 15. doi: 10.3390/cancers15041077
10. Boswell-Smith V, Spina D, and Page CP. Phosphodiesterase inhibitors. Br J Pharmacol. (2006) 147 Suppl 1:S252–7. doi: 10.1038/sj.bjp.0706495
11. Fischer JP, Sieber B, Nelson JA, Cleveland E, Kovach SJ, Wu LC, et al. Comprehensive outcome and cost analysis of free tissue transfer for breast reconstruction: an experience with 1303 flaps. Plast reconstructive surgery. (2013) 131:195–203. doi: 10.1097/PRS.0b013e318277856f
12. van den Heuvel MG, Buurman WA, Bast A, and van der Hulst RR. Review: Ischaemia-reperfusion injury in flap surgery. J plastic reconstructive aesthetic surgery: JPRAS. (2009) 62:721–6. doi: 10.1016/j.bjps.2009.01.060
13. De Takats G. Papaverine: use and toxicity. New Engl J Med. (1970) 282:225. doi: 10.1056/NEJM197001222820416
14. Ma Y, Deng K, Liu J, Ma B, Mei F, Hui W, et al. The add-on effects of Danhong injection among patients with ischemic stroke receiving Western medicines: A systematic review and meta-analysis. Front Pharmacol. (2022) 13:937369. doi: 10.3389/fphar.2022.937369
15. Yang S, Wang Y, Shen H, Chen T, and Du H. Efficacy and safety of Danhong injection for treating myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Front Pharmacol. (2024) 15:1371959. doi: 10.3389/fphar.2024.1371959
16. Du H, He Y, Pan Y, Zhao M, Li Z, Wang Y, et al. Danhong injection attenuates cerebral ischemia-reperfusion injury in rats through the suppression of the neuroinflammation. Front Pharmacol. (2021) 12:561237. doi: 10.3389/fphar.2021.561237
17. Mirzamohammadi F, Nnamani Silva ON, Leaf RK, Eberlin KR, and Valerio IL. Chemoprophylaxis and management of venous thromboembolism in microvascular surgery. Semin Plast surgery. (2023) 37:57–72. doi: 10.1055/s-0042-1760381
18. Üstün GG, Öztürk S, and Koçer U. Standardization of the rat dorsal random pattern (McFarlane) flap model and evaluation of the pharmacological agents aiming to salvage partial flap necrosis: A systematic review and a meta-analysis. Ann Plast surgery. (2021) 87:e145–e52. doi: 10.1097/SAP.0000000000002919
Keywords: malignant peripheral nerve sheath tumor, misdiagnosis, flap necrosis, wound repair, Chinese medicine
Citation: Chen L, Wu X and Li F (2025) Salvage of necrotic flap following malignant peripheral nerve sheath tumor excision using multimodal pharmacotherapy: a case report. Front. Oncol. 15:1689834. doi: 10.3389/fonc.2025.1689834
Received: 21 August 2025; Accepted: 30 September 2025;
Published: 15 October 2025.
Edited by:
Margaret Ottaviano, G. Pascale National Cancer Institute Foundation (IRCCS), ItalyReviewed by:
Pasquale Tammaro, Fondazione IRCCS Istituto Nazionale dei Tumori, ItalyGraciella Wahjoe Pramono, Universitas Pelita Harapan Fakultas Kedokteran, Indonesia
Copyright © 2025 Chen, Wu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lili Chen, MTE2MTI4NDc0OUBxcS5jb20=; Feng Li, MTM5MTYzMzUwMTBAMTYzLmNvbQ==
 Lili Chen
Lili Chen Xiangyi Wu2
Xiangyi Wu2