- 1Faculty of Medicine and Health, Susan Wakil School of Nursing and Midwifery, The University of Sydney, Camperdown, NSW, Australia
- 2Sydney Institute of Women, Children and Their Families, Sydney Local Health District, NSW Health, Camperdown, NSW, Australia
- 3Translating Early Prevention of Obesity in Childhood (EPOCH-Translate) Centre of Research Excellence, The University of Sydney, Sydney, NSW, Australia
- 4Faculty of Medicine and Health, Westmead Applied Research Centre, The University of Sydney, Westmead, NSW, Australia
- 5Westmead Centre for Oral Health, Western Sydney Local Health District, NSW Health, Westmead, NSW, Australia
- 6Faculty of Medicine and Health, School of Dentistry, The University of Sydney, Camperdown, NSW, Australia
- 7Australian Centre for Integration of Oral Health, School of Nursing & Midwifery, Western Sydney University, Penrith, NSW, Australia
- 8Faculty of Health, School of Nursing and Midwifery, The University of Technology Sydney, Ultimo, NSW, Australia
- 9School of Health Sciences, Western Sydney University, Penrith, NSW, Australia
- 10Health Equity across Lifespan Research Laboratory, Campbelltown, NSW, Australia
- 11Translational Health Research Institute, Western Sydney University, Penrith, NSW, Australia
- 12Faculty of Medicine and Health, Sydney Medical School, The University of Sydney, Camperdown, NSW, Australia
- 13Oral Health Services, Sydney Local and Health District and Sydney Dental Hospital, Surry Hills, NSW, Australia
Introduction: Formula and bottle feeding behaviours can increase obesity and tooth decay (early childhood caries, ECC) in early childhood, through non-responsive feeding and prolonged exposure to sugar. Parents’ beliefs can be barriers to behaviour change for obesity and ECC prevention. Understanding these beliefs towards children's teeth and weight can address parents’ priorities and develop prevention messages. This qualitative systematic review (PROSPERO registration #CRD42022348783) aimed to identify parent or carer perspectives on obesity and ECC in children aged ≤6 years.
Methods: Database searching of CINAHL, Medline and EMBASE, with hand searching, was undertaken. Included papers were qualitative research publications, focused on parent or carer beliefs and attitudes towards overweight, obesity or ECC in infants and children. Inductive thematic analysis was undertaken to generate themes, with a strengths-based approach focused on parents’ lived experience. Quality appraisal was undertaken with the CASP Qualitative Checklist. Descriptive characteristics of the study and participants, and qualitative findings, were extracted qualitatively in NVivo.
Results: 7,365 references were identified from database and hand searching, with 98 references included for analysis. Three research themes were generated: (1) parenting to support child wellness, including healthy teeth and weight; (2) parents’ response to unwellness, including identifying symptoms, causes and protective factors for unhealthy weight and teeth; (3) information and resources needed to support healthy weight and teeth. There was high or potential risk of bias in qualitative methodology when studies did not address researcher-participant relationships or rigorous data analysis processes.
Discussion: Findings highlight the need for strength-based messages for children's teeth and weight, increased understanding of formula and bottle feeding as obesity and ECC risk factors, and holistic approaches to care by dental and primary care professionals.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42022348783, PROSPERO CRD42022348783.
1 Introduction
Overweight, obesity and dental caries (tooth decay) in early childhood are preventable conditions that share an overlapping aetiology through infant nutrition and feeding. Early childhood caries (ECC) are dental caries occurring in children aged under 6 years, with one or more primary teeth affected by tooth decay, loss or fillings (1). Overweight and obesity in children under 5 years of age is defined respectively as two and three standard deviations above the World Health Organization weight-for-height growth standard median (2). Consequences of these conditions may be extensive, such as impaired eating and nutrition from poor dentition impacting growth; and poor oral health and dental pain impacting speech development, sleep, behaviour, play, learning and later school attendance and performance (3). Increased body weight may be linked with delays in mental and motor development (4). Further, the establishment of increased body weight or unhealthy dietary patterns in infancy may increase obesity and obesogenic risk factors in childhood and adulthood (5–7), with similar increase in risk of chronic diseases such as type 2 diabetes and cardiovascular disease (8).
In addition to known dietary and behavioural risk factors of overweight, obesity and ECC (9, 10), formula and bottle feeding may contribute to overfeeding and exposure to free sugars (11). These behaviours may include feeding to soothe, instead of feeding responsively to hunger; adding fermentable carbohydrates to bottles; and ongoing use of bottles, instead of transitioning to cups (11). Health professionals report that parental beliefs can be a barrier to behavioural changes, such as the preference for infants with large body size; the value of feeding, particularly formula feeding, to encourage infant sleep; lack of concern to the health of primary teeth; and poor parental knowledge and self-efficacy to support tooth brushing and healthy eating (12–15). Whilst poor health literacy and values can overlap, some parents may value and place an emphasis of one health condition over another.
There is an opportunity to tailor health messaging towards values parents may place on one condition over another. That is, for a parent who values their child's oral health instead of weight concerns, targeted messaging focused on healthy teeth may also reduce risk factors related to their child being overweight. Understanding the beliefs and perceptions of parents and carers towards overweight, obesity or ECC will identify parental priorities in the care of their infants and children. In turn, this will inform co-design of a common risk factor intervention with consistent messaging to support best-practice formula and bottle feeding behaviours that prevent overweight, obesity and ECC.
This qualitative systematic review aimed to identify parent or carer (hereafter, referred to as “parents”) perspectives on overweight, obesity or dental caries in infants and children aged under 6 years.
2 Methods
The qualitative systematic review focused on the lived experiences of parents of infants and children aged under 6 years, and their perspectives on overweight, obesity or dental caries in early childhood. This review is reported following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 statement (16), with checklist in Supplementary Table S1, and was registered on PROSPERO (#CRD42022348783). Thematic analysis (17) was used for theme generation and analysis. A review protocol is not available.
2.1 Information sources
Reference searches were undertaken in August 2021, with a search update in January 2023 and August 2024. The database search strategy was structured using the Population/Concept/Context framework (Table 1). Databases CINAHL, Medline (via OvidSP) and EMBASE (via OvidSP) were searched with combinations of key terms for: infant or child; dental caries or overweight, obesity or excess body weight; parent or carer; beliefs, perspectives, knowledge, attitudes or culture; and qualitative research (Supplementary Tables S2–S7). All references were downloaded to Endnote 21 (Clarivate, 2013, Philadelphia, USA) for screening.
Forward and backward citation (18) was undertaken using the reference lists of included studies and citations via Google Scholar. Reviews focused on infant or child overweight, obesity or oral health were checked for relevant articles.
The literature on parental perspectives of childhood overweight and obesity is extensive. Sydney Local Health District, the authors' local health district, is a culturally and socioeconomically diverse area of New South Wales, with nearly half the population speaking a language other than English, higher rates of obesity in cultural groups, areas of extreme socioeconomic advantage and disadvantage (19, 20), and where preference for large body size is a barrier to infant obesity prevention (12), particularly amongst cultural groups. To focus the literature searched, only studies with specific reference to body size were included for analysis.
Data extracted from articles included first author, year of publication, country of data collection, data collection method, study population, population characteristics, and qualitative findings.
2.2 Thematic analysis
Thematic analysis was undertaken following the six steps outlined by Braun and Clarke (17). Thematic analysis enabled inductive theme generation and could centre the participant perspective.
Full text documents and relevant supplementary files were uploaded to NVivo version 14 (Lumivero, 2023). HC undertook familiarisation of the research by reading the articles 2–3 times. Iterative initial codes were drafted, then organised into a coding framework that was informed by the Capability-Opportunity-Motivation system of behaviour change (21), which proposes that capability, opportunity and motivation underpin behaviour and behaviour change. Following coding, thematic generation was undertaken by HC to produce themes and subthemes, which were discussed with all authors; then reviewed and refined into three final themes addressing both obesity and ECC, using a strengths-based approach towards parents' lived experience.
2.3 Quality appraisal
Critical appraisal was undertaken using the CASP Qualitative Checklist (22) to assess qualitative research methodology. Critical appraisal was summarised as tabulated data and visualisation in RevMan 5.4 (The Cochrane Collaboration, 2020).
2.4 Inter-rater reliability
Author HC undertook all Methods. Inter-rater reliability was undertaken, with a second reviewer (CR, EDW or JA) to screen full-text studies included for analysis; code ∼10% of included studies, following the coding framework; and undertake the CASP Qualitative Checklist appraisal for ∼10% of included studies.
This ensured that two reviewers determined the final studies for inclusion; supported consistent coding accuracy; and assessed critical appraisal consistently. Inter-rater reliability of CASP appraisal was scored with percentage agreement (23).
2.5 Reflexivity
Reflexivity involves critical interrogation of how knowledge production is informed by the researcher's values (17). HC is a dietitian, with a background in childhood obesity research. During familiarisation with the literature, varying perspectives between healthcare providers and parents was evident, including frustrations with health recommendations not being undertaken or difficulties faced in parenting and child rearing not being recognised. HC maintained research memos and positioned the parent perspective during coding, theme generation and analysis. The findings are focused on the parent perspective, instead of biomedical models of physiology and pathophysiology, and parent-reported resource needs, instead of researcher-inferred needs. Examples of excerpts with reflexive coding are available in Supplementary Table S8.
3 Results
3.1 Study selection
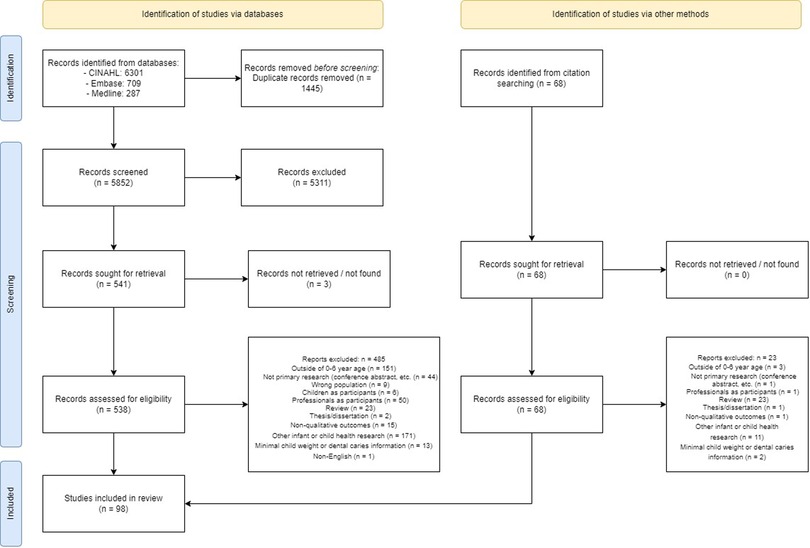
Results of the database and citation search are summarized in the PRISMA flow diagram (Figure 1). Database searching identified 7,297 references. Following duplicate removal, 5,852 references were screened for relevance based on title and abstract. 538 references were sought for full-text retrieval. Studies excluded during full-text screening included parents of children with unspecified age or outside of age range (24, 25); studies focused on feeding, nutrition and/or physical activity without context of weight, overweight/obesity or tooth decay (26, 27); weight-specific research with minimal focus on infant or child body size (28, 29); and dental research that was non-specific to feeding, nutrition and/or ECC (30, 31). Backward and forward citation searching identified 68 references. 98 articles from 91 studies were included.
3.2 Inter-rater reliability
Author HC independently undertook all Methods, including reference searching and screening; data extraction; study coding; and quality appraisal.
A second researcher, CR or JA, screened all full-text studies, against the inclusion and exclusion criteria. Disagreements were resolved by author EDW, with 98 articles included for analysis.
To ensure consistency in coding, eight articles were coded by EDW following the coding framework. Discussion between HC and EDW indicated high consistency in coding decisions.
Eleven studies were randomly selected for CASP assessment with a second reviewer, EDW or JA. There was high inter-rater reliability, with an overall 93.6% percentage agreement, and high agreement across all ten CASP checklist items (23) (Supplementary Table S9).
3.3 Included studies
Descriptive characteristics of the 98 articles are summarised in Supplementary Table S10. Most participants were mothers. Fifty-nine articles included infants and children with overweight, obesity or ECC, diagnosed by health professionals or self-reported by parents. Eighty-six articles involved populations at increased risk of overweight, obesity or ECC, relating to relative social disadvantage (low income; low education; refugees, migrants, immigrants or cultural minority populations; Indigenous populations), countries in economic transition, or parents with overweight/obesity. Most articles were from the USA (47), followed by European countries (12) and Australia (9). Studies from each continent were represented, mostly from North America (55), then Asia (13), Europe and Oceania (12 each), with fewer in South America (5) and Africa (1). All studies undertook qualitative research through focus groups (55) or interviews (56), barring one which used Photovoice.
3.4 Quality appraisal
CASP findings are summarised in Supplementary Table S11 and Figure S1. Overall, articles had good qualitative research quality: studies had clear research aims (n = 98); appropriate use of qualitative methodology (n = 98); results were valuable in relation to current practice or policy, transferability to other populations, or relevance to new areas of research (n = 96); and clearly stated findings for explicitness, credibility or relation to the research question (n = 82). Studies were at high or unclear risk of bias for not considering or explicitly reporting on the researcher-participant relationship (n = 64), the use of informed consent or sufficient explanation of the research process to participants (n = 44), and rigorous data analysis processes (n = 39).
3.5 Thematic analysis
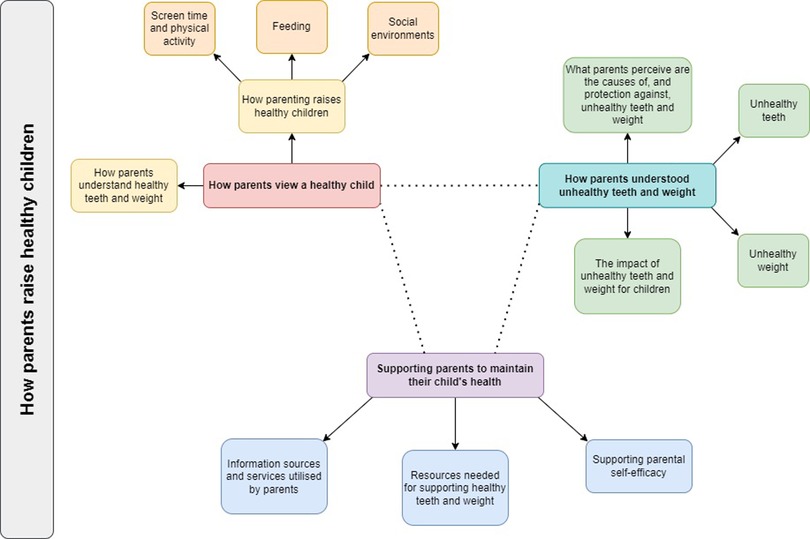
Themes are conceptualised in Figure 2. Findings are grouped by how parents: value child wellness, including healthy teeth and weight, and the parenting practices supporting this (Theme 1); respond to unwellness, including identifying symptoms, causal factors and protective factors (Theme 2); and identify resources needed to support healthy teeth and weight (Theme 3). Our findings demonstrate that although parents valued wellness, they tended to respond and seek resources only when children were unwell. This is consistent with existing literature around parental responses to health promotion when children are asymptomatic. Representative quotes are reported in Supplementary Table S12.
3.6 Theme 1: how parents view a healthy child
Good health for children was determined by observable physical, cognitive and emotional development, including happiness; self-esteem; good appetite, activity and play; life opportunities; growth and attaining developmental milestones; absence of illness and disease; learning ability; behaviour and temperament (32–43).
3.6.1 How parents understand healthy teeth and weight
Good oral health was defined by the absence of disease: aesthetically pleasing teeth were white, straight, evenly spaced, without pain, holes, decay or discoloration; pink gums and attractive smiles (13, 41, 44–50). However, parents’ views on the health of primary and permanent teeth differed. Parents valued primary teeth if they believed it would impact the health of permanent teeth (47, 48, 51–53). Conversely, only permanent teeth were valued when these were viewed as having more long-term importance than primary teeth (49, 54–56).
Healthy or desirable body weight was determined by size or shape, appetite and physical activity. Many parents considered largeness or heaviness to demonstrate adequate nutrition and growth, energy reserves, physical strength, and contentment (35, 37, 39, 57–65). Parents considered good appetite and dietary intake, lack of fussiness around food, and physical activity or play without signs of overexertion or developmental delay, as signs of children having healthy weight, receiving adequate nutrition, and being sufficiently active (33, 35, 38, 39, 42, 43, 57–60, 62, 65–72). Largeness or heaviness, which demonstrated growth and nutrition, were distinct from overweight or obesity as disease conditions. This was conceptualised as “solid”, “thick”, or “fresh”, “baby fat”, “plumpness”, “chubbiness”, “muscled” or “chunkiness”, and could be informed by cultural beliefs and norms (32, 35, 38, 42, 43, 60, 62–66, 73, 74). Few studies found positive beliefs towards smaller body weight, and could be mitigated by health provider advice (67, 75) or beliefs about breastfeeding benefits (76).
Few parents viewed the use of growth charts as a clinical method of identifying healthy body weight positively (36, 40, 70, 77). However, parents also viewed high growth chart trajectories or percentiles positively when this was reported or viewed as healthy, “normal”, or showing increasing body weight (65, 78, 79).
3.6.2 How parenting raises healthy children
Parents valued their ability to meet their children's wants and needs (43), and provide a safe family and household environment (33, 80, 81). These beliefs informed perspectives regarding feeding, activity and play, and screen time.
3.6.2.1 Screen time and physical activity
Parents felt screen use could interfere with eating, appetite regulation and parent-infant bonding (58, 61, 71, 74, 82, 83). Screen use was associated with children being “lazy” or “inactive”, independent of health outcomes (33, 35, 60). However, screen time was believed to support learning, digital skill development and exposure to healthy foods (58, 84), and enabled children to behave indoors (61, 82, 85).
Parents felt physical activity was intrinsic in growth and development, with infants being naturally inclined to be active when they reached developmental milestones, such as crawling and walking (58, 86). Therefore, parents did not need to encourage play and activity. Similarly, for older children, parents only felt responsible for providing transport or safe play options (34, 87, 88). Parents felt they only needed to support physical activity if their child had overweight or obesity (69, 89).
3.6.2.2 Feeding
Values towards healthy eating by children and feeding decisions from parents overlapped. While healthy eating supported physical and mental growth and contributed to a good appearance (37, 54, 58, 77, 90), this could include forced feeding or pressure feeding practices to ensure children were fed, regardless of hunger or appetite (36, 71, 74, 75, 77). Likewise, while feeding also demonstrated parental affection and the ability to meet children's physical and emotional needs (42, 62, 83, 91), this also meant offering cariogenic and/or obesogenic food being important to provide enjoyable eating experiences (74, 81) and to diversify a child's diet (53, 92). Denying this would deprive children of opportunities to enjoy food and learn self-regulation (54, 93). Early introduction of solid food to infants before six months broadened the taste palate to prevent fussy eating (70, 74).
3.6.2.3 Social environments
Parenting approaches and the family environment supported oral hygiene and healthy eating, through supervising and/or modelling routine tooth brushing and food choices, making food purchasing decisions, ensuring healthy foods were available, limiting availability of unhealthy foods in the household, and avoiding pressuring children to eat foods they did not enjoy (33, 35, 37, 38, 41, 42, 45, 46, 49, 50, 52, 53, 61, 65, 67, 75, 77, 83, 84, 94–107).
Most parents considered their child's oral hygiene and dietary behaviours to be their responsibility. Broader social support were equally important, such as from other parents, older siblings and family members (84, 98–101, 103, 104, 107), with schools and healthcare providers also being responsible for teaching tooth brushing or providing healthy food environments (50, 67, 84, 87, 88, 96, 103, 107–109).
3.7 Theme 2: how parents understood unhealthy teeth and weight
Poor health and illness were defined by symptoms and health consequences that interfere with wellbeing, while early indicators of disease—such as white spots in ECC, or growth charts showing risk of overweight or obesity—could be overlooked or dismissed.
3.7.1 Unhealthy teeth
Parents identified poor oral health through symptomatic disease and unattractive teeth. Few parents used medical terms, such as “tooth decay” or “cavities”—instead, this was reported as visible decay, including holes, “rot” and “black spots”; fractured or cracked teeth; tooth discoloration; tooth loss and extraction; pain, distress, poor behaviour and mood; bad breath; inability to eat and sleep; visible fillings; and swollen gums (36, 41, 44, 45, 48–51, 55, 100, 110–114).
3.7.2 Unhealthy weight
Parents believed that smallness or thinness in children indicated undernutrition; poor growth and development; or illnesses, like anaemia and tapeworms. These beliefs could be informed by health provider assessment when children did not follow a standardised growth trajectory (32, 78) or in populations with poverty or socioeconomic disadvantage (33, 77, 96). Thinness was also associated with parental neglect or inability to meet nutritional needs (40, 66, 77, 96).
Parents considered infants or children to be at an unhealthy weight when their appearance or behaviour appeared unattractive; when they appeared “larger” than their peers; or when they required larger clothing sizes (35, 40, 59, 60, 62, 65, 66, 84, 89, 115, 116). While parents may acknowledge that their child had a clinical diagnosis of overweight or obesity, few parents felt this meant their child's weight was unhealthy unless physical and emotional consequences were experienced, which is discussed separately in theme 2.4.
Notably, there were opposing views on the suitability of standardised growth charts to identify healthy weight and growth. Few parents felt that growth charts were suitable for identifying overweight or obesity (35, 60, 67, 84, 115). Parents demonstrated uncertainty towards the purpose of growth charts (63, 70, 79). When growth charts identified a clinical diagnosis of overweight/obesity that was incongruent with parental expectations, parents viewed growth charts negatively or being incompatible with a child's unique growth trajectory (32, 35, 42, 79, 89).
3.7.3 What parents perceive are the causes of, and protection against, unhealthy teeth and weight
Parents generally were able to identify certain causal and protective factors in ECC, overweight, obesity or weight gain. These findings are focused on the parental perspective, instead of biomedical models of pathophysiology.
For ECC, causal factors included insufficient tooth brushing, dietary sugar intake (particularly sweets, fruit juice and milk), and bottle feeding (13, 36, 44–53, 55, 76, 82, 85, 91, 95, 97, 99, 101, 103, 105, 107, 108, 110, 113, 117–119). Protective factors included regular tooth brushing or gum cleaning, limiting dietary sugar intake, limiting bottle use, and routine dental check-ups (41, 44, 46, 47, 49, 50, 52, 53, 98, 100, 103, 104, 107). Few parents identified night-time breastfeeding, cariogenic bacteria transmission, or carbohydrous foods, as causes of ECC (50, 53, 91, 95, 101, 105, 110); or the role of fluoride in ECC prevention (46, 47, 100, 104, 120).
For weight gain, causal factors included dietary intake of high fat and/or high sugar foods, overeating, early introduction of solid foods for infants, prolonged bottle or formula feeding, and physical inactivity or sedentary behaviour (35, 37, 60, 62, 65–67, 75, 77, 78, 82, 85, 86, 89, 90). Protective factors included breastfeeding, healthy eating, decreased intake of energy-dense unhealthy foods, physical activity, and infants reaching developmental milestones, such as walking (32, 42, 58, 60, 82, 89).
Dental attendance was not consistently seen as a protective factor against ECC. Many parents considered accessing dental care only for symptom treatment (36, 45, 48, 49, 53, 54, 81, 94, 97, 98, 102, 104, 114, 120–122). Parents who valued preventative dental care may only do so after negative experiences of ECC from their families and communities (52, 54, 56, 94, 97, 111).
Genetic susceptibility to ECC or higher body weight was frequently discussed as being intrinsic. Therefore, ECC, overweight, or obesity was inevitable or untreatable, even with preventative behaviours, such as regular dental attendance or lifestyle behaviours (33, 35, 38, 39, 42, 43, 46–51, 57, 60, 61, 65, 66, 68, 69, 71, 77, 86–89, 94, 95, 98, 99, 105, 112, 115, 118, 123).
Some beliefs reflect unclear understanding of biological causes of ECC or overweight and obesity. This included ECC being caused by poor tooth formation from undernutrition, e.g., insufficient milk or calcium during pregnancy or infancy (46, 55, 95, 103, 112, 118), or use of antibiotics (49, 110); and overweight and obesity being caused by metabolism, poor sleep, stress from bullying, and hormones in animal production (35, 60, 65–67, 77). Parents also believed mouth washing was sufficient for oral hygiene, especially when feeding to sleep made tooth-brushing difficult (36, 76, 91). For parents who misunderstood the causes of ECC, cariogenic risk factors could be maintained—for example, parents who believed that chewing or sucking of bottle teats caused ECC (46, 95, 117, 118) replaced bottles with cups during feeding to sleep.
The cariogenicity and obesogenicity of foods and drinks could be poorly understood, as demonstrated through beliefs on: the healthiness of fruit juice, fruit drink and soft drinks; dilution of sugary drinks with water being protective against ECC; or use of unrefined sugars, such as jaggery or honey (49, 52, 54, 60, 61, 85, 91, 92, 94, 95, 112, 117, 120). Some parents were unaware that certain foods or drinks—such as candy, chocolate, cookies, potato chips, or ice cream—were cariogenic or obesogenic (49, 72, 81, 91, 95) or felt that certain foods, while cariogenic, remained nourishing (36, 54, 81, 94).
3.7.4 The impact of unhealthy teeth and weight for children
For parents, unhealthy teeth and weight was defined by consequential impacts. Understanding the life course trajectory of overweight, obesity and ECC could inform how parents responded to these conditions. However, there were notable differences in perceptions on ECC, compared to overweight and obesity. Fewer parents proactively discussed prevention, while those who did could be informed by experiences in their family and community, such as their childhood or the care of other children (38, 39, 41, 45, 75, 82, 84, 85, 94–96, 101, 107).
The consequences of ECC related to the permanence of primary and permanent teeth. Parents reacted to poor health in primary teeth when it impacted nutrition, speaking, child mood and behaviour, or when it was believed to impact the health of permanent teeth (36, 47, 48, 51–53, 94, 99, 100, 114). While asymptomatic ECC, such as white spots, did not prompt health seeking by some parents, parents also reported being dismissed and unsupported by health professionals when seeking advice on asymptomatic ECC (36, 46, 48, 111, 112, 114). Parents' views on primary teeth was related to its impermanence, and varied from apathy to concern (13, 36, 44, 47–50, 53, 56, 94, 98, 102, 113, 121). For some parents, the health of primary teeth appeared unrelated to the health of permanent teeth, and primary teeth were “practice” for oral hygiene behaviours for permanent teeth (13, 48, 49, 53, 111). Subsequently, dental care reflected a focus on acute symptom treatment, such distress and poor behaviour from dental pain, with minimal focus on ECC prevention (94, 112, 114, 124). Longer-term dental care behaviours varied after experiences of ECC: for some, the resolution of symptoms after removal of decayed teeth led to dental care behaviours not being maintained, while others were motivated to maintain dental care behaviours (49, 94, 95, 99, 101, 106, 110, 111).
Consistent with this, overweight and obesity—either as a present diagnosis or a future risk—was not seen as significant if children appeared asymptomatic (40, 43, 67, 84, 89, 125). Overweight or obesity was detrimental when it was consequential, such as parental back pain when carrying a heavy infant; physical incapacity, including delays in reaching developmental milestones, shortness of breath, and tiredness during play; and teasing or bullying that impacted children's mental health and self-esteem (32–35, 37–39, 42, 43, 60, 61, 64–67, 77, 82–84, 87–89, 96, 116).
Understanding the life course trajectory of overweight or obesity meant that some parents anticipated the risk of future weight-related health problems and the normalization of obesogenic lifestyle behaviours into adulthood (32, 33, 37, 39, 43, 60, 64–66, 75, 77, 82, 84, 85, 87–89). However, despite significant health consequences, overweight or obesity were unimportant at present, and would only be a problem beyond infancy or school age (58, 65, 68, 69, 78, 87). Subsequently, parents believed that obesogenic behaviours could be addressed later, or that body weight would self-resolve when child height or physical activity intrinsically increased (58, 64–66, 69, 83, 84, 87, 89, 116).
3.8 Theme 3: supporting parents to maintain their child's health
While there were distinctions in framing their needs for promoting children's oral health and healthy eating, and preventing ECC, overweight or obesity, parents' need for information and resources was consistent. Parents discussed their ability to successfully support healthy teeth and eating being based on internal and external loci of control.
3.8.1 Information sources and services utilised by parents
Parents utilised professional and non-professional sources for information about children's health, such as medical, nursing, dentistry, allied health professionals and government programs, and family, friends, peers and advertising, respectively. Teachers, early childhood educators and social workers were also important non-health professional sources of information (45, 46, 49, 55, 76, 88, 97, 101, 103, 104, 108, 117, 126). Attitudes towards these sources were dependent on being aligned with parents’ expectations. Parents' satisfaction with professional sources was impacted by expectations of care, agreement with information received, comprehensiveness of education, quality of services, and the parent-provider relationship, particularly a clinician's competence when working with children (13, 32, 35, 38, 49, 53, 58, 60, 63, 75–78, 81, 82, 84, 87, 89, 90, 92, 94, 97–99, 103, 107, 111, 113, 114, 120, 122, 123, 126). The use of non-professional sources of information varied: many parents trusted the advice and experiences of other parents and family members (13, 35–37, 46, 48, 58, 76, 83, 87, 92, 93, 96), while few parents felt this information did not align with professional advice (74, 87, 99, 114). Notably, information from health professionals could impact how parents perceived the severity or significance of ECC, overweight or obesity (32, 46, 48, 58, 65, 84, 86, 89, 112) – and parents were confused when received conflicting information from trusted sources or were advised by health professionals that further health care seeking was not needed (35, 53, 54, 76, 84, 89, 99, 111, 114, 121, 125).
Parents reported difficulty accessing health providers being a barrier to accessing information or care to support their child's health. This included actual or perceived cost of services; time barriers; inability to receive specialist referrals; attendance to service locations, related to transport challenges and isolation of rural, regional and remote areas; language barriers; and refusal of dental services for children reportedly too young for care (13, 43–46, 50, 52–54, 56, 81, 82, 94, 98–100, 111–114, 117, 120).
3.8.2 Resources needed for supporting healthy teeth and weight
Parents identified information and resource needs based on gaps in care, which may indicate that routine well-child services were not meeting parent needs, or that parents were not accessing health services. These topics included breastfeeding and introduction of solid foods, healthy eating, physical activity, sleep, understanding growth charts, oral health and care, and general parenting, such as responding to infant cues, and child development. Information also needed to be specific, factual and practical (32–34, 47, 50, 53, 58, 62–64, 70, 74, 76, 78, 80–84, 87, 88, 90, 96, 102, 103, 108, 111–113, 115–117, 120, 125, 126).
Parents offered suggestions on community- or school-based programs that could be available, such as parent groups, playgroups, education programs with peer learning, dental outreach, and activity programs (33, 48, 50, 53, 58, 80, 88, 96, 109, 125). To be accessible, these programs needed to be free, provide childcare, and involve children in age-appropriate education (34, 125). Resources also needed to be proactive instead of reactive, such as the establishment of food assistance programs or food co-ops with healthy food, and the provision of dental care supplies, like toothbrushes and toothpaste, through community services (34, 45, 50, 87, 100, 108).
Parents wanted improved access to dental care for children, such as affordable, subsidised or free dental care; alignment of dental services with medical services; or access to paediatric dentists (45, 53, 54, 98, 99, 106, 108, 113). While free or subsidized dental care could be available in countries with public healthcare, this was not broadly known, or was perceived as poorer quality compared to private health services (44, 51, 53, 54).
Resources were needed to meet diverse language needs, such as low literacy resources, access to interpreters, and increased language diversity (38, 44, 48, 53, 63, 87, 90, 102, 113). Resources in different formats or modes were required, varying from print resources; digital resources, such as electronic newsletters, internet and social media websites; and in-person resources, such as parenting classes, and community health workers to link parents to services (44, 48, 63, 87, 90, 120, 125).
3.8.3 Supporting parental self-efficacy
Parents identified practices to raise a healthy child in theme 1.2. However, internal and external factors limit their efficacy in doing this.
While parents considered tooth brushing as important, they experienced barriers, including self-efficacy, lack of time, and responding to a resistant child (13, 36, 48–50, 53, 80, 81, 94, 95, 97, 99–105, 110, 122). Some parents reported teeth cleaning that was not best-practice, such as unsupervised tooth brushing before 7 years of age, mouth rinsing or cleaning with cloth instead of tooth brushing, delayed tooth brushing initiation, or suboptimal tooth brushing time (44, 49, 53, 97, 101, 103, 110, 119, 120, 122).
Parents recognised the difficulty in supporting children's healthy eating in obesogenic and cariogenic environments. Parents felt their attempts to encourage healthy eating were undermined by other carers and children's peers (13, 37, 42, 44, 49, 50, 53, 56, 60, 61, 64, 66, 67, 78, 81–84, 93, 99, 104, 111, 115, 127). Similar to tooth brushing, parents experienced barriers to providing healthy foods, including self-efficacy, children's food preferences, financial and time costs of providing healthy food, and the convenience and inexpensive nature of unhealthy foods (13, 34, 35, 50, 60–62, 66, 74, 77, 81, 82, 84, 85, 88, 96, 99, 100, 116, 117, 125, 126).
Parents' use of food, or response to signs of hunger, indicated these were barriers to healthy eating. Parents reported the use of persuasive feeding to pressure children into eating healthy foods, reduce disruptive behaviour, or to reward good behaviour (13, 37, 38, 42, 49, 57, 64, 75, 77, 81, 83, 85, 87, 126). Parents felt unable to deny food requests, challenge food refusal, or address resistance from children, even during food introduction for infants (35, 36, 38, 44, 49, 61, 64, 71, 75, 83, 85, 91–94, 97, 98, 115, 123). This awareness of foods being unhealthy while also feeling children could not be refused is distinct from theme 1.2.2, where food should not be denied and should be provided to encourage diverse food experiences.
Ensuring infants and children were fed, particularly “fussy” or “picky” eaters, could lead to prolonged bottle feeding (36, 42, 49, 90). Likewise, parents' concerns that children's refusal to use drinking cups or eat healthy foods would cause undernutrition led to encouragement or maintenance of cariogenic or obesogenic feeding behaviours (35, 49, 61, 76, 81, 90, 93, 95, 97, 99). Parents did not feel confident to deny food for children who reported being hungry (32, 35, 42, 60, 61, 97, 109, 115), which was similar to parents feeling that feeding to soothe was the only behaviour that could settle crying, tantrums or fussiness (13, 57, 64, 80, 123).
4 Discussion
This qualitative systematic review of 98 publications centres the lived experiences of parents of infants and children, which focus on valuing child wellness, and responding to unwellness when unhealthy weight or ECC symptoms were experienced. Parents valued messages about healthy weight and teeth, but not messages about preventing obesity or ECC. Parents had reactive responses to overweight, obesity or ECC – such as dental attendance for ECC treatment but not routine check-ups for prevention, or limiting obesogenic foods after overweight or obesity was clinically diagnosed. Parents reported information needs from professional sources on nutrition, dental care and responsive parenting, which may indicate gaps in well-child visits where this information is typically provided.
These review findings are consistent with previous qualitative research, where there was poor understanding of cariogenic risk from formula, bottle or night-time feeding; the addition of foods into bottles being obesogenic and cariogenic; cultural preferences for larger or heavier infants and children; and low self-efficacy in tooth brushing or responsive child feeding (128–131). This is congruent with questionnaires which demonstrate varying levels of parental knowledge on bottle use and preventative dental care on ECC risk (132–134) – however, knowledge of bottle use may not affect ECC status or use of obesogenic feeding behaviours (134, 135). Key messages on formula and bottle feeding as causal factors of obesity and ECC were not recalled: parents were largely unaware of the association, with some only becoming aware after unhealthy weight gain or ECC occurred (13, 36, 48, 49, 53, 76, 86, 94, 95, 117, 118); and few were aware that frequency of feeding could result in overnutrition or sugar exposure as obesity and ECC risk factors (75, 97, 105). Community and primary health care-based interventions for parents can improve bottle use behaviours and routine preventative dental care (11, 133, 136–138), which emphasises the importance of education and support on dental care and nutrition throughout pregnancy and early childhood.
These findings indicate the need for communication that address parent priorities and support self-efficacy. This has implications for health messages and behaviour change technique-informed strategies in program design, such as strength-based messages (i.e., healthy teeth and growth) instead of messages about obesity or ECC prevention. Healthy teeth were prioritised for aesthetic appearance, including attractive smiles, while the function of teeth for eating was only discussed as a consequence of ECC. In contrast, healthy weight was prioritised for the aesthetics of size demonstrating adequate growth, and the function of weight reflecting good dietary intake and ability to play. Impairments in these, along with bullying or teasing, indicated children at an unhealthy weight. These differences were also seen when interpreting the life-course trajectory of ECC, overweight or obesity. While parents could identify the immediate consequences of ECC, few identified the long-term risk of dental caries in permanent teeth. Conversely, while parents could identify chronic conditions associated with unhealthy weight, these were considered to be relevant only if overweight or obesity occurred beyond infancy and childhood. Even where parents could identify cariogenic or obesogenic risk factors, they experienced challenges in health-promoting behaviours and ceasing cariogenic or obesogenic risk behaviours, such as settling child crying with feeding. Responsive parenting supports parents to interact with infants and children to develop child regulation and autonomy—the INSIGHT trial demonstrated improved maternal structured feeding practices (139) and modestly improved child weight outcomes at 3 years age (140), while the Sleep Strong African American Families trial demonstrated improvements in maternal responsive feeding (141) and reduced odds of infant rapid weight gain at 16 weeks age (142). Communication to parents should include: strength-based messaging and strategies to build parental self-efficacy; emphasize the relevance of health-promoting behaviours from infancy; and identify how rapidly ECC and overweight or obesity can occur, even in infancy and childhood.
These findings also indicate resource needs and the potential for co-design in program delivery. Parents identified the use or need for community- or school-based resources; distribution of dental health products, like toothbrushes or toothpaste; and education, workshops or health screening in schools and community venues. Specific focus was given towards affordable access to dental care, including services for children, by participants internationally and across socioeconomic statuses. Financial accessibility for medical treatment, particularly dental care, require health service restructure and may not be feasible to address without system-level change—however, strategies to increase access to care may include public health messaging about dental service eligibility, which may not be widely known (94), and preventative care delivery or home visiting with community health workers (143–146). Many articles in this review (86 of 98) involved vulnerable populations with social disadvantage or changing food environments during economic transition—therefore, co-design and community partnership can support equity in program reach and address upstream social determinants of health (147). Community stakeholder involvement in program design may support uptake and sustainability, such as the currently ongoing Healthy Smile Happy Child dental health program (148) and Whanau Pakari early childhood obesity program (149).
Experiences recalled by parents also indicate the need for changes in health provider practice. Parents reported confusion or frustration from health providers who dismissed or normalised obesity or ECC diagnosis or symptoms (84, 111, 114); refused to provide referrals for allied health or dental care (82, 111); or would not provide dental services for children under three years age (111, 121). This demonstrates the need for clear dissemination of up-to-date practice guidelines, which encourage dental attendance at one year age to establish preventative health behaviours and routine check-ups (150, 151), as well as continuing practice development for providers on early identification of obesity and ECC, such as using growth charts to identify unhealthy weight gain or addressing ECC from white spot identification (152, 153). Targeted or tailored messages and services by community health workers, especially for high-risk populations, may increase dental service uptake (143, 154). There are opportunities to integrate oral health into primary health care by non-dental practitioners (155) or oral health practitioners to discuss obesity prevention (156, 157), especially where obesogenic and cariogenic behaviours overlap. A common risk factor approach to obesity and ECC, across child health professional roles, can be supported with inclusion in tertiary education curricula, interdisciplinary collaboration, continuing practice development, and use of best-practice resources—such as screening tools and client-facing resources—to undertake screening, behaviour change counselling, and referral to services (157–159).
Quality appraisal with the CASP Qualitative Checklist indicated that articles tended to have good methodological quality. All articles had clear research aims and appropriate use of qualitative research methods. Many articles had clearly stated findings, with results linked to current practice, transferability to other populations or relevance to further areas of research. However, there could be unclear or high risk of bias in not explicitly reporting the researcher-participant relationship, details of informed consent or explanation of the research process for participants, or rigorous data analysis processes, as these aspects tended by briefly or not reported. As the use of social science research expands in health disciplines, it is important that future research addresses rigorous qualitative research methodology, and reflexivity and power relations between researchers and participants (17).
This review has several strengths. First, it integrates research from separate health disciplines for two conditions that share overlapping aetiologies—notably, a common finding when discussing both obesity and ECC was low parental self-efficacy to respond to children's unsettled behaviour and to address unhealthy feeding behaviours by other carers. Second, the findings of the included studies were broad, with 98 articles identified from nearly 6,000 references, which indicate a comprehensive search. Many qualitative studies on overweight, obesity or obesogenic behaviours in early childhood were excluded due to lack of focus on body weight or size. However, this refined the focus of this review as the body of literature on paediatric obesity is extensive and the inclusion of further studies would not have expanded findings. Third, the use of reflexive thematic analysis centred the parental perspective, particularly on child feeding, teeth and weight, and why cariogenic and obesogenic feeding behaviours may be valued. This, in turn, can inform program design which addresses community values or uses a strength-based approach to support behaviour change.
Limitations of this review relate to techniques to enhance trustworthiness and credibility of data analysis. One reviewer, HC, undertook database searching; study screening for inclusion and exclusion; coding in NVivo; and generation of the primary findings using thematic analysis. Study screening, NVivo coding and thematic analysis in duplicate would improve credibility of findings. However, inter-rater reliability was undertaken with a second reviewer to confirm full-text studies included for analysis; compare coding; and compare critical appraisal of qualitative methodology—the inter-rater reliability between reviewers was high and indicate that the work undertaken by HC is trustworthy and credible. Further, final themes and subthemes were finalised with discussion across co-authors. Diverse populations were included in this review, with 50 of 77 studies from Western countries (United States, Australia, Canada, New Zealand, western Europe) involving cultural minorities or Indigenous populations, and the remaining 21 studies including cultural majority populations across South America, Mexico and Asia. While preferences for larger or heavier child body size of weight cannot be generalisable across diverse populations, this perspective was observed across cultural groups in 13 included studies—and similar perspectives are demonstrated towards the lack of importance of primary teeth compared to permanent teeth by participants across different cultural groups in 13 included studies. However, few included studies involved populations or diaspora from African countries (one study, South Africa (43); one study, West Indies (53); Black American or British parents, 15 studies (35, 39, 40, 42, 57, 70, 72, 78, 79, 87, 89, 102, 111, 117, 121); migrants from African countries and the Caribbean (37, 44, 48–50, 58, 63, 113, 127), 9 studies), indicating underrepresentation in research.
This systematic qualitative review of 98 articles suggests the need for a holistic approach to prevention of obesity and dental caries in early childhood, and to address overlapping dietary behaviours. By using a focus on parents' lived experience, it identifies the need for strength-based communication and opportunities to improve understanding of formula and bottle feeding as cariogenic and obesogenic risk factors. Findings also demonstrate the need for continuing practice development for health professionals to identify and address early symptoms of obesity and ECC, including referral to dental care, and holistic approaches to dental and obesity prevention care by primary care and oral health practitioners.
Understanding these parent perspectives on healthy teeth and weight in early childhood will support the development of health promotion initiatives, including education resources and messages to support behaviour change. These findings will inform community stakeholder engagement, including focus groups and co-design workshops to develop an obesity and ECC prevention intervention through changing formula and bottle feeding behaviours.
5 Conclusion
This qualitative systematic review centred the perspectives of parents on overweight, obesity and dental caries in early childhood. Parents are focused on child wellness and value messages on healthy teeth and weight. Parents react to health conditions, such as ECC or obesity, once children experience symptoms that interfere with wellbeing—however, they may not undertake preventative behaviours, such as routine dental check-ups, or limiting obesogenic foods before overweight or obesity is clinically diagnosed. Parents identified information needs that highlight the importance of supporting parental self-efficacy for tooth brushing, healthy eating and responsive parenting. These findings also highlight the importance of health providers in early identification of ECC and obesity, and provision of accurate, tailored and up-to-date information and advice.
Data availability statement
The data presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Author contributions
HC: Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. RC: Methodology, Writing – review & editing. BC: Methodology, Writing – review & editing. JA: Formal analysis, Writing – review & editing. AA: Supervision, Writing – review & editing. ED-W: Investigation, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. HC receives a PhD student scholarship from the EPOCH-Translate Centre of Research Excellence, which is funded by the National Health and Medical Research Council grant award GA189596.
Acknowledgments
The authors thank Chris Rossiter for her assistance in reference screening and Professor Louise Baur for her support as postgraduate research supervisor.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/froh.2025.1524715/full#supplementary-material
References
1. World Health Organization. Ending Childhood Dental Caries: WHO Implementation Manual. Geneva, Switzerland: World Health Organisation (2019). Available at: https://apps.who.int/iris/handle/10665/330643
2. World Health Organization. Obesity and Overweight. Geneva, Switzerland: World Health Organisation (2020). Available at: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight [Accessed October 30 2020].
3. Casamassimo PS, Thikkurissy S, Edelstein BL, Maiorini E. Beyond the dmft: the human and economic cost of early childhood caries. J Am Dent Assoc. (2009) 140(6):650–57. doi: 10.14219/jada.archive.2009.0250
4. Cataldo R, Huang J, Calixte R, Wong AT, Bianchi-Hayes J, Pati S. Effects of overweight and obesity on motor and mental development in infants and toddlers. Pediatric Obes. (2016) 11(5):389–96. doi: 10.1111/ijpo.12077
5. Luque V, Escribano J, Closa-Monasterolo R, Zaragoza-Jordana M, Ferré N, Grote V, et al. Unhealthy dietary patterns established in infancy track to mid-childhood: the EU childhood obesity project. J Nutr. (2018) 148(5):752–59. doi: 10.1093/jn/nxy025
6. Druet C, Stettler N, Sharp S, Simmons RK, Cooper C, Smith GD, et al. Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatr Perinat Epidemiol. (2012) 26(1):19–26. doi: 10.1111/j.1365-3016.2011.01213.x
7. Lucas K, James P, Choh AC, Lee M, Czerwinski SA, Demerath EW, et al. The positive association of infant weight gain with adulthood body mass index has strengthened over time in the fels longitudinal study. Pediatric Obes. (2018) 13(8):476–84. doi: 10.1111/ijpo.12271
8. Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circ. (2005) 111(15):1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10
9. Hooley M, Skouteris H, Boganin C, Satur J, Kilpatrick N. Parental influence and the development of dental caries in children aged 0–6 years: a systematic review of the literature. J Dentistry. (2012) 40(11):873–85. doi: 10.1016/j.jdent.2012.07.013
10. Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med. (2016) 50(6):761–79. doi: 10.1016/j.amepre.2015.11.012
11. Cheng H, Chen R, Milosevic M, Rossiter C, Arora A, Denney-Wilson E. Interventions targeting bottle and formula feeding in the prevention and treatment of early childhood caries, overweight and obesity: an integrative review. Int J Environ Res Public Health. (2021) 18(23):12304. doi: 10.3390/ijerph182312304
12. Cheng H, Eames-Brown R, Tutt A, Laws R, Blight V, McKenzie A, et al. Promoting healthy weight for all young children: a mixed methods study of child and family health nurses’ perceptions of barriers and how to overcome them. BMC Nurs. (2020) 19(1):84. doi: 10.1186/s12912-020-00477-z
13. Elwell K, Camplain C, Kirby C, Sanderson K, Grover G, Morrison G, et al. A formative assessment of social determinants of health related to early childhood caries in two American Indian communities. Int J Environ Res Public Health. (2021) 18(18):9838. doi: 10.3390/ijerph18189838
14. Horowitz AM, Kleinman DV, Child W, Radice SD. Perceptions of dental hygienists and dentists about preventing early childhood caries: a qualitative study. J Dent Hyg. (2017) 91(4):29–36.29118081
15. Veale M, Ajwani S, Johnson M, Nash L, Patterson T, George A. The early childhood oral health program: a qualitative study of the perceptions of child and family health nurses in south western Sydney, Australia. BMC Oral Health. (2016) 16:1–10. doi: 10.1186/s12903-016-0213-0
16. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10(1):89. doi: 10.1186/s13643-021-01626-4
18. Cooper C, Booth A, Varley-Campbell J, Britten N, Garside R. Defining the process to literature searching in systematic reviews: a literature review of guidance and supporting studies. BMC Med Res Methodol. (2018) 18(1):85. doi: 10.1186/s12874-018-0545-3
19. Sydney Local Health District. Culturally and Linguistically Diverse Health Strategic Plan 2022–2026. Sydney, NSW: Sydney Local Health District (2022). Available at: https://www.slhd.nsw.gov.au/pdfs/SLHD-Culturally-and-Linguistically-Diverse-Health-Strategic-Plan-2022-2026.pdf [AccessedAugust 14, 2023].
20. Sydney Local Health District. Planning Tools. Sydney, NSW: Sydney Local Health District (2023). Available at: https://slhd.health.nsw.gov.au/planning/tools [Accessed August 14, 2023].
21. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
22. CASP UK. Qualitative Checklist. Oxford: Critical Appraisal Skills Programme (2018). Available at: https://casp-uk.net/casp-tools-checklists/ [Accessed June 6 2022].
23. Stemler SE. A comparison of consensus, consistency, and measurement approaches to estimating interrater reliability. Pract Assess Res Eval. (2004) 9:4.
24. Aljafari AK, Gallagher JE, Hosey MT. Failure on all fronts: general dental practitioners’ views on promoting oral health in high caries risk children–a qualitative study. BMC Oral Health. (2015) 15:45. doi: 10.1186/s12903-015-0032-8
25. Krstic S, Dennis S, Southcombe F, Denney-Wilson E. What do parents think about child’s routine height and weight measures? A qualitative study. Aust J Prim Health. (2024) 30(1):1–8. doi: 10.1071/PY23017
26. Taverno Ross SE, Macia L, Documét PI, Escribano C, Kazemi Naderi T, Smith-Tapia I. ‘Latino parents’ perceptions of physical activity and healthy eating: at the intersection of culture, family, and health. J Nutr Educ Behav. (2018) 50(10):968–76. doi: 10.1016/j.jneb.2017.12.010
27. Petrunoff NA, Wilkenfeld RL, King LA, Flood VM. ‘Treats’, ’sometimes foods’, ‘junk': a qualitative study exploring ‘extra foods’ with parents of young children. Public Health Nutr. (2014) 17(5):979–86. doi: 10.1017/S1368980012005095
28. Kuswara K, Laws R, Kremer P, Hesketh KD, Campbell KJ. The infant feeding practices of Chinese immigrant mothers in Australia: a qualitative exploration. Appetite. (2016) 105:375–84. doi: 10.1016/j.appet.2016.06.008
29. Lakshman R, Landsbaugh JR, Schiff A, Cohn S, Griffin S, Ong KK. Developing a programme for healthy growth and nutrition during infancy: understanding user perspectives. Child Care Health Dev. (2012) 38(5):675–82. doi: 10.1111/j.1365-2214.2011.01283.x
30. Peralta E, Tallman TJ, Scala CA, Scala BN, Dahl ZT, Weyant RJ, et al. Maternal perceptions of assisting preschool-aged children with toothbrushing. JADA. (2024) 155(7):597–604. doi: 10.1016/j.adaj.2024.04.005
31. Hoeft KS, Barker JC, Masterson EE. Maternal beliefs and motivations for first dental visit by low-income Mexican American children in California. Pediatr Dent. (2011) 33(5):392–98.22104706
32. Bentley F, Swift JA, Cook R, Redsell SA. I would rather be told than not know”—a qualitative study exploring parental views on identifying the future risk of childhood overweight and obesity during infancy. BMC Public Health. (2017) 17(1):684. doi: 10.1186/s12889-017-4684-y
33. Crawford PB, Gosliner W, Anderson C, Strode P, Becerra-Jones Y, Samuels S, et al. Counseling Latina mothers of preschool children about weight issues: suggestions for a new framework. J Am Diet Assoc. (2004) 104(3):387–94. doi: 10.1016/j.jada.2003.12.018
34. Glover M, Wong SF, Taylor RW, Derraik JGB, Fa'alili-Fidow J, Morton SM, et al. The complexity of food provisioning decisions by māori caregivers to ensure the happiness and health of their children. Nutrients. (2019) 11(5):994. doi: 10.3390/nu11050994
35. Hughes CC, Sherman SN, Whitaker RC. How low-income mothers with overweight preschool children make sense of obesity. Qual Health Res. (2010) 20(4):465–78. doi: 10.1177/1049732310361246
36. Karasz A, Patel V, Ranasinghe S, Chaudhuri K, McKee D. Preventing caries in young children of immigrant Bangladeshi families in New York: perspectives of mothers and paediatricians. Community Dent Health. (2014) 31(2):80–4. doi: 10.1922/CDH_3234Karasz
37. Lindsay AC, Sussner KM, Greaney ML, Peterson KE. ‘Latina Mothers’ beliefs and practices related to weight Status, feeding, and the development of child overweight. Public Health Nurs. (2011) 28(2):107–18. doi: 10.1111/j.1525-1446.2010.00906.x
38. Lindsay A, Wallington S, Greaney M, Hasselman M, Machado M, Mezzavilla R, et al. Sociocultural and environmental influences on Brazilian immigrant Mothers’ beliefs and practices related to child feeding and weight Status. Matern Child Health J. (2017) 21(5):1085–94. doi: 10.1007/s10995-016-2207-6
39. Rich SS, DiMarco NM, Huettig C, Essery EV, Andersson E, Sanborn CF. Perceptions of health status and play activities in parents of overweight hispanic toddlers and preschoolers. Fam Community Health. (2005) 28(2):130–41. doi: 10.1097/00003727-200504000-00005
40. Thompson AL, Adair L, Bentley ME. Whatever average is”: understanding African American Mothers’ perceptions of infant weight, growth, and health. Curr Anthropol. (2014) 55(3):348–55. doi: 10.1086/676476
41. Poirier BF, Hedges J, Smithers LG, Moskos M, Jamieson LM. Aspirations and worries: the role of parental intrinsic motivation in establishing oral health practices for indigenous children. Int J Environ Res Public Health. (2021) 18(21):11695. doi: 10.3390/ijerph182111695
42. Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don't low-income mothers worry about their preschoolers being overweight? Pediatrics. (2001) 107(5):1138–46. doi: 10.1542/peds.107.5.1138
43. Klingberg S, van Sluijs EMF, Draper CE. The thing is, kids don't grow the same": parent perspectives on preschoolers’ weight and size in Soweto, South Africa. PLoS One. (2020) 15(4):e0231094. doi: 10.1371/journal.pone.0231094
44. Amin M, Perez A. Is the wait-for-patient-to-come approach suitable for African newcomers to Alberta, Canada? Community Dent Oral Epidemiol. (2012) 40(6):523–31. doi: 10.1111/j.1600-0528.2012.00698.x
45. Athavale P, Khadka N, Roy S, Mukherjee P, Chandra Mohan D, Turton BB, et al. Early childhood junk food consumption, severe dental caries, and undernutrition: a mixed-methods study from Mumbai, India. Int J Environ Res Public Health. (2020) 17(22):8629. doi: 10.3390/ijerph17228629
46. López del Valle LM, Riedy CA, Weinstein P. Rural puerto rican women’s views on children’s oral health: a qualitative community-based study. J Dent Child. (2005) 72(2):61–6.
47. Momeni Z, Sargeran K, Yazdani R, Sighaldeh SS. Perception of Iranian mothers about oral health of their school-children: a qualitative study. J Dent (Tehran). (2017) 14(4):180–90.29285028
48. Prowse S, Schroth RJ, Wilson A, Edwards JM, Sarson J, Levi JA, et al. Diversity considerations for promoting early childhood oral health: a pilot study. Int J Dent. (2014) 2014:175084. doi: 10.1155/2014/175084
49. van Nes KA, Veerkamp JSJ, Reis R. Barriers and opportunities to oral health in Dutch-Moroccan children in The Netherlands: a narrative report. Eur Arch Paediatr Dent. (2018) 19(5):353–64. doi: 10.1007/s40368-018-0367-3
50. Balasooriyan A, van der Veen MH, Bonifácio CC, Dedding C. Understanding parental perspectives on young children’s oral health (≤4 years) growing up in a disadvantaged neighbourhood of Amsterdam, The Netherlands: an exploratory study. BMC Public Health. (2024) 24(1):627. doi: 10.1186/s12889-024-18073-0
51. Amin MS, Harrison RL, Weinstein P. A qualitative look at parents’ experience of their child’s dental general anaesthesia. Int J Paediatr Dent. (2006) 16(5):309–19. doi: 10.1111/j.1365-263X.2006.00750.x
52. Finlayson TL, Beltran NY, Becerra K. Psychosocial factors and oral health practices of preschool-aged children: a qualitative study with hispanic mothers. Ethn Health. (2019) 24(1):94–112. doi: 10.1080/13557858.2017.1315366
53. Naidu R, Nunn J, Forde M. Oral healthcare of preschool children in trinidad: a qualitative study of parents and caregivers. BMC Oral Health. (2012) 12(1):27–40. doi: 10.1186/1472-6831-12-27
54. Hashim R, Fitzgerald RP, Schafer CT, Thomson WM. Mothers’ understanding of dental-caries related feeding practices and children’s use of dental care in Ajman. Soc Sci Dent. (2010) 1(2):97–107.
55. Rivera Y, Boyd LD, Libby L. Hispanic seasonal farmworker Caregivers’ beliefs and perceptions of early childhood caries. J Dent Hyg. (2020) 94(5):14–21.33008945
56. Roguski M, McBride-Henry K. Insights into the oral health crisis amongst pre-schoolers in aotearoa/New Zealand: a discourse analysis of parent/caregiver experiences. BMC Oral Health. (2020) 20(1):182. doi: 10.1186/s12903-020-01173-9
57. Baughcum AE, Burklow KA, Deeks CM, Powers SW, Whitaker RC. Maternal feeding practices and childhood obesity: a focus group study of low-income mothers. Arch Pediatr Adolesc Med. (1998) 152(10):1010–14. doi: 10.1001/archpedi.152.10.1010
58. Bektas G, Boelsma F, Baur VE, Seidell JC, Dijkstra SC. Parental perspectives and experiences in relation to lifestyle-related practices in the first two years of a child’s life: a qualitative study in a disadvantaged neighborhood in The Netherlands. Int J Environ Res Public Health. (2020) 17(16):5838. doi: 10.3390/ijerph17165838
59. Keenan J, Stapleton H. Bonny babies? Motherhood and nurturing in the age of obesity. Health Risk Soc. (2010) 12(4):369–83. doi: 10.1080/13698571003792926
60. Do LM, Larsson V, Tran TK, Nguyen HT, Eriksson B, Ascher H. Vietnamese Mother’s conceptions of childhood overweight: findings from a qualitative study. Glob Health Action. (2016) 9(1):30215. doi: 10.3402/gha.v9.30215
61. Safaiyan A, Zarei F, Moghaddam HR, Maasoumi N, Matlabi H. How do mothers explain the causes of childhood obesity? Community-based approach in preschool centers. Child Care Pract. (2021) 30(3):247–60. doi: 10.1080/13575279.2021.1946012
62. Small L, Melnyk BM, Anderson-Gifford D, Hampl JS. Exploring the meaning of excess child weight and health: shared viewpoints of Mexican parents of preschool children. Pediatr Nurs. (2009) 35(6):357–66.20166465
63. Steinman L, Doescher M, Keppel GA, Pak-Gorstein S, Graham E, Haq A, et al. Understanding infant feeding beliefs, practices and preferred nutrition education and health provider approaches: an exploratory study with Somali mothers in the USA. Matern Child Nutr. (2010) 6(1):67–88. doi: 10.1111/j.1740-8709.2009.00185.x
64. Wu Y, Ma X, Fraser WD, Li M, Wang W, Huang H, et al. Caregivers’ perceptions, challenges and service needs related to tackling childhood overweight and obesity: a qualitative study in three districts of Shanghai, China. BMC Public Health. (2021) 21(1):768. doi: 10.1186/s12889-021-10744-6
65. Eli K, Howell K, Fisher PA, Nowicka P. A little on the heavy side”: a qualitative analysis of parents’ and grandparents’ perceptions of preschoolers’ body weights. BMJ Open. (2014) 4(12):e006609. doi: 10.1136/bmjopen-2014-006609
66. Guendelman S, Fernald LC, Neufeld LM, Fuentes-Afflick E. Maternal perceptions of early childhood ideal body weight differ among Mexican-origin mothers residing in Mexico compared to California. J Am Diet Assoc. (2010) 110(2):222–29. doi: 10.1016/j.jada.2009.10.033
67. Guerrero A, Slusser W, Barreto P, Rosales N, Kuo A. Latina Mothers’ perceptions of healthcare professional weight assessments of preschool-aged children. Matern Child Health J. (2011) 15(8):1308–15. doi: 10.1007/s10995-010-0683-7
68. Syrad H, Falconer C, Cooke L, Saxena S, Kessel AS, Viner R, et al. Health and happiness is more important than weight': a qualitative investigation of the views of parents receiving written feedback on their child’s weight as part of the national child measurement programme. J Hum Nutr Diet. (2015) 28(1):47–55. doi: 10.1111/jhn.12217
69. Cave TL, Derraik JGB, Willing EJ, Hofman PL, Anderson YC. Caregiver perceptions of weight in preschool children, and determinants of engagement in a multidisciplinary intervention service for weight issues. Obes Res Clin Pract. (2021) 15(3):262–67. doi: 10.1016/j.orcp.2021.03.002
70. Valencia A, Thomson C, Duncan B, Arthur A. Evaluating Latino WIC Mothers’ perceptions of infant’s healthy growth: a formative assessment. Matern Child Health J. (2016) 20(3):525–33. doi: 10.1007/s10995-015-1850-7
71. Suprawoto DN, Hayati H, Rachmawati IN, Wanda D. Fat kids are adorable”: the experiences of mothers caring for overweight children in Indonesia. Compr Child Adolesc Nurs. (2019) 42(sup1):226–33. doi: 10.1080/24694193.2019.1594454
72. Porter L, Shriver L, Ramsay S. Maternal perceptions related to eating and obesity risk among low-income African American preschoolers. Matern Child Health J. (2016) 20(12):2565–72. doi: 10.1007/s10995-016-2082-1
73. Rachmi CN, Hunter CL, Mu L, Baur LA. Perceptions of overweight by primary carers (mothers/grandmothers) of under five and elementary school-aged children in bandung, Indonesia: a qualitative study. Int J Behav Nutr Phys Act. (2017) 14:1–13. doi: 10.1186/s12966-017-0556-1
74. Lakhanpaul M, Benton L, Lloyd-Houldey O, Manikam L, Rosenthal DM, Allaham S, et al. Nurture early for optimal nutrition (NEON) programme: qualitative study of drivers of infant feeding and care practices in a British-Bangladeshi population. BMJ Open. (2020) 10(6):e035347. doi: 10.1136/bmjopen-2019-035347
75. Beck AL, Hoeft KS, Takayama JI, Barker JC. Beliefs and practices regarding solid food introduction among Latino parents in Northern California. Appetite. (2018) 120:381–87. doi: 10.1016/j.appet.2017.09.023
76. Suprabha BS, Shenoy R, Mahabala KY, Nayak AP, Rao A, D’Souza V. Early feeding and weaning practices of Indian children with early childhood caries: a qualitative exploration. JDR Clin Trans Res. (2022) 8(2):131–38. doi: 10.1177/23800844221083645
77. Lindsay AC, Machado MT, Sussner KM, Hardwick CK, Kerr LR, Peterson KE. Brazilian Mothers’ beliefs, attitudes and practices related to child weight status and early feeding within the context of nutrition transition. J Biosoc Sci. (2009) 41(1):21–37. doi: 10.1017/S0021932008003039
78. Redsell SA, Atkinson P, Nathan D, Siriwardena AN, Swift JA, Glazebrook C. Parents’ beliefs about appropriate infant size, growth and feeding behaviour: implications for the prevention of childhood obesity. BMC Public Health. (2010) 10:711. doi: 10.1186/1471-2458-10-711
79. Woolford SJ, Clark SJ, Lumeng JC, Williams DR, Davis MM. Maternal perspectives on growth and nutrition counseling provided at preschool well-child visits. J Natl Med Assoc. (2007) 99(2):153–58.17366952
80. Hoeft KS, Rios SM, Pantoja Guzman E, Barker JC. Using community participation to assess acceptability of “contra caries”, a theory-based, promotora-led oral health education program for rural Latino parents: a mixed methods study. BMC Oral Health. (2015) 15:103. doi: 10.1186/s12903-015-0089-4
81. Poirier B, Hedges J, Smithers L, Moskos M, Jamieson L. What are we doing to our babies’ teeth?” barriers to establishing oral health practices for indigenous children in South Australia. BMC Oral Health. (2021) 21(1):1–12. doi: 10.1186/s12903-021-01791-x
82. Cespedes E, Andrade GOM, Rodríguez-Oliveros G, Perez-Cuevas R, González-Unzaga MA, Trejo AB, et al. Opportunities to strengthen childhood obesity prevention in two Mexican health care settings. Int J Paediatr Dent. (2012) 2(3):496–504. doi: 10.5750/ijpcm.v2i3.194
83. Galvez EP, Vizcarra M, Molina P, Coloma MJ, Stecher MJ, Bost K, et al. Exploring parents’ perspectives on feeding their young children: a qualitative study using photo-elicitation in Chile. Public Health Nutr. (2022) 25(9):2415–25. doi: 10.1017/S1368980022000428
84. McDonald S. The lived experiences of Mexican-heritage mothers caring for overweight preschool children. Qual Rep. (2015) 20(4):431–50. doi: 10.46743/2160-3715/2015.2119
85. Rodríguez-Oliveros G, Haines J, Ortega-Altamirano D, Power E, Taveras EM, González-Unzaga MA, et al. Obesity determinants in Mexican preschool children: parental perceptions and practices related to feeding and physical activity. Arch Med Res. (2011) 42(6):532–39. doi: 10.1016/j.arcmed.2011.10.006
86. Dinkel D, Snyder K, Kyvelidou A, Molfese V. He’s just content to sit: a qualitative study of mothers’ perceptions of infant obesity and physical activity. BMC Public Health. (2017) 17:1–10. doi: 10.1186/s12889-017-4503-5
87. McGarvey EL, Collie KR, Fraser G, Shufflebarger C, Lloyd B, Oliver MN. Using focus group results to inform preschool childhood obesity prevention programming. Ethn Health. (2006) 11(3):265–85. doi: 10.1080/13557850600565707
88. Patino-Fernandez AM, Hernandez J, Villa M, Delamater A. School-based health promotion intervention: parent and school staff perspectives. J Sch Health. (2013) 83(11):763–70. doi: 10.1111/josh.12092
89. Goodell LS, Pierce MB, Bravo CM, Ferris AM. Parental perceptions of overweight during early childhood. Qual Health Res. (2008) 18(11):1548–55. doi: 10.1177/1049732308325537
90. Brotanek JM, Schroer D, Valentyn L, Tomany-Korman S, Flores G. Reasons for prolonged bottle-feeding and iron deficiency among Mexican-American toddlers: an ethnographic study. Acad Pediatr. (2009) 9(1):17–25. doi: 10.1016/j.acap.2008.10.005
91. Shrikrishna Suprabha B, Shenoy R, Mahabala Karuna Y, Nayak AP, Rao A, D’Souza V. Dietary practices among children with early childhood caries and the associated factors: a qualitative study. Int J Paediatr Dent. (2022) 32(2):176–84. doi: 10.1111/ipd.12842
92. Chaidez V, Townsend M, Kaiser LL. Toddler-feeding practices among Mexican American mothers. A qualitative study. Appetite. (2011) 56(3):629–32. doi: 10.1016/j.appet.2011.02.015
93. Cheney AM, Nieri T, Davis E, Prologo J, Valencia E, Anderson AT, et al. The sociocultural factors underlying Latina Mothers’ infant feeding practices. Glob Qual Nurs Res. (2019) 6:2333393618825253. doi: 10.1177/2333393618825253
94. Arora A, Lucas D, To M, Chimoriya R, Bhole S, Tadakamadla SK, et al. How do mothers living in socially deprived communities perceive oral health of young children? A qualitative study. Int J Environ Res Public Health. (2021) 18(7):3521. doi: 10.3390/ijerph18073521
95. Hoeft KS, Barker JC, Masterson EE. Urban Mexican-American mothers’ beliefs about caries etiology in children. Community Dent Oral Epidemiol. (2010) 38(3):244–55. doi: 10.1111/j.1600-0528.2009.00528.x
96. Lindsay AC, Ferarro M, Franchello A, Barrera Rde L, Machado MM, Pfeiffer ME, et al. Child feeding practices and household food insecurity among low-income mothers in Buenos Aires, Argentina. Cien Saude Colet. (2012) 17(3):661–69. doi: 10.1590/S1413-81232012000300012
97. Tiwari T, Rai N, Colmenero E, Gonzalez H, Castro M. A community-based participatory research approach to understand urban latino parent’s oral health knowledge and beliefs. Int J Dent. (2017) 2017:9418305. doi: 10.1155/2017/9418305
98. Momeni Z, Sargeran K, Yazdani R, Shahbazi Sighaldeh S. Perceived barriers to the preservation and improvement of children’s oral health among Iranian women: a qualitative study. Eur Arch Paediatr Dent. (2019) 20(2):95–103. doi: 10.1007/s40368-018-0395-z
99. Amin MS, Harrison RL. Understanding parents’ oral health behaviors for their young children. Qual Health Res. (2009) 19(1):116–27. doi: 10.1177/1049732308327243
100. Collins CC, Villa-Torres L, Sams LD, Zeldin LP, Divaris K. Framing young childrens oral health: a participatory action research project. PLoS One. (2016) 11(8):e0161728. doi: 10.1371/journal.pone.0161728
101. Finlayson TL, Cabudol M, Liu JX, Garza JR, Gansky SA, Ramos-Gomez F. A qualitative study of the multi-level influences on oral hygiene practices for young children in an early head start program. BMC Oral Health. (2019) 19(1):166. doi: 10.1186/s12903-019-0857-7
102. Mofidi M, Zeldin LP, Rozier RG. Oral health of early head start children: a qualitative study of staff, parents, and pregnant women. Am J Public Health. (2009) 99(2):245–51. doi: 10.2105/AJPH.2008.133827
103. Suprabha BS, D’Souza V, Shenoy R, Karuna YM, Nayak AP, Rao A. Early childhood caries and parents’ challenges in implementing oral hygiene practices: a qualitative study. Int J Paediatr Dent. (2021) 31(1):106–14. doi: 10.1111/ipd.12696
104. Tiwari T, Rai NK, Wilson AR, Gansky SA, Albino J. What can we learn from parents of caries-free and caries-active hispanic children? JDR Clin Trans Res. (2021) 6(1):47–58. doi: 10.1177/2380084420904043
105. Virgo-Milton M, Boak R, Hoare A, Gold L, Waters E, Gussy M, et al. An exploration of the views of Australian mothers on promoting child oral health. Aust Dent J. (2016) 61(1):84–92. doi: 10.1111/adj.12332
106. Lee J, Schroth RJ, Lawrence HP. Nishtam Niwiipitan (my first teeth): oral health digital stories from urban indigenous parents. JDR Clin Trans Res. (2022) 8(4):326–36. doi: 10.1177/23800844221117143
107. Poirier BF, Hedges J, Smithers LG, Moskos M, Jamieson LM. Child-, family-, and community-level facilitators for promoting oral health practices among indigenous children. Int J Environ Res Public Health. (2022) 19(3):1150. doi: 10.3390/ijerph19031150
108. Butten K, Johnson NW, Hall KK, Toombs M, King N, O'Grady KF. Yarning about oral health: perceptions of urban Australian aboriginal and torres strait islander women. BMC Oral Health. (2020) 20(1):35. doi: 10.1186/s12903-020-1024-x
109. Ek A, Nordin K, Nyström CD, Sandvik P, Eli K, Nowicka P. Responding positively to “children who like to eat": parents’ experiences of skills-based treatment for childhood obesity. Appetite. (2020) 145:104488. doi: 10.1016/j.appet.2019.104488
110. Custodio NB, Schardosim LR, Piovesan CP, Hochscheidt L, Goettems ML. Maternal perception of the impact of anterior caries and its treatment on children: a qualitative study. Int J Paediatr Dent. (2019) 29(5):642–49. doi: 10.1111/ipd.12501
111. Isong IA, Luff D, Perrin JM, Winickoff JP, Ng MW. Parental perspectives of early childhood caries. Clin Pediatr (Phila). (2012) 51(1):77–85. doi: 10.1177/0009922811417856
112. Masterson E, Barker J, Hoeft K, Hyde S. Shades of decay: the meanings of tooth discoloration and deterioration to Mexican immigrant caregivers of young children. Hum Organ. (2014) 73(1):82–93. doi: 10.17730/humo.73.1.861831136642q074
113. Nicol P, Al-Hanbali A, King N, Slack-Smith L, Cherian S. Informing a culturally appropriate approach to oral health and dental care for pre-school refugee children: a community participatory study. BMC Oral Health. (2014) 14:69. doi: 10.1186/1472-6831-14-69
114. Suprabha BS, Shenoy R, Mahabala KY, Nayak AP, Rao A, D’Souza V. Early childhood caries and dental care utilization in mangalore, India: parents’ perceptions. JDR Clin Trans Res. (2024) 9:337–45. doi: 10.1177/23800844231225193
115. Toftemo I, Glavin K, Lagerløv P. Parents’ views and experiences when their preschool child is identified as overweight: a qualitative study in primary care. Fam Pract. (2013) 30(6):719–23. doi: 10.1093/fampra/cmt056
116. Ziser K, Decker S, Stuber F, Herschbach A, Giel KE, Zipfel S, et al. Barriers to behavior change in parents with overweight or obese children: a qualitative interview study. Front Psychol. (2021) 12:631678. doi: 10.3389/fpsyg.2021.631678
117. Horowitz AM, Kleinman DV, Child W, Maybury C. Perspectives of Maryland adults regarding caries prevention. Am J Public Health. (2015) 105(5):e58–64. doi: 10.2105/AJPH.2015.302565
118. Horton S, Barker JC, Horton S, Barker JC. Rural latino immigrant caregivers’ conceptions of their children’s oral disease. J Public Health Dent. (2008) 68(1):22–9. doi: 10.1111/j.1752-7325.2007.00078.x
119. Riggs E, Gibbs L, Kilpatrick N, Gussy M, van Gemert C, Ali S, et al. Breaking down the barriers: a qualitative study to understand child oral health in refugee and migrant communities in Australia. Ethn Health. (2015) 20(3):241–57. doi: 10.1080/13557858.2014.907391
120. Horowitz A, Canto M, Goodman H, Child W. Perceptions and practices of dental caries prevention by Maryland latinas: a qualitative study. J Dent Oral Care Med. (2016) 2(2):205. doi: 10.15744/2454-3276.2.205
121. Hilton IV, Stephen S, Barker JC, Weintraub JA. Cultural factors and children’s oral health care: a qualitative study of carers of young children. Community Dent Oral Epidemiol. (2007) 35(6):429–38. doi: 10.1111/j.1600-0528.2006.00356.x
122. Weinstein P, Troyer R, Jacobi D, Moccasin M. Dental experiences and parenting practices of native American mothers and caretakers: what we can learn for the prevention of baby bottle tooth decay. ASDC J Dent Child. (1999) 66(2):120–26.10431622
123. McFarren H, Vazquez C, Jacobs EA, Dela Tejera G, Gray M. Understanding feeding practices of latinx mothers of infants and toddlers at risk for childhood obesity: a qualitative study. Matern Child Nutr. (2020) 16(3):1–9. doi: 10.1111/mcn.12983
124. Horton S, Barker JC. Rural Mexican immigrant parents’ interpretation of children’s dental symptoms and decisions to seek treatment. Community Dent Health. (2009) 26(4):216–21.20088219
125. Nicely S, Miller ME, Craviotto M-T. Parents’ perceptions of 5210 nutrition messaging and child weight Status. J Nutr Educ Behav. (2019) 51(5):629–35. doi: 10.1016/j.jneb.2019.01.023
126. Hardy K, Hooker L, Ridgway L, Edvardsson K. Australian Parents’ experiences when discussing their child’s overweight and obesity with the maternal and child health nurse: a qualitative study. J Clin Nurs. (2019) 28(19/20):3610–17. doi: 10.1111/jocn.14956
127. Sussner K, Lindsay A, Greaney M, Peterson K. The influence of immigrant status and acculturation on the development of overweight in latino families: a qualitative study. J Immigr Minor Health. (2008) 10(6):497–505. doi: 10.1007/s10903-008-9137-3
128. Heinig MJ, Follett JR, Ishii KD, Kavanagh-Prochaska K, Cohen R, Panchula J. Barriers to compliance with infant-feeding recommendations among low-income women. J Hum Lact. (2006) 22(1):27–38. doi: 10.1177/0890334405284333
129. Higgins B. Puerto rican cultural beliefs: influence on infant feeding practices in western New York. J Transcult Nurs. (2000) 11(1):19–30. doi: 10.1177/104365960001100105
130. Wong D, Perez-Spiess S, Julliard K. Attitudes of Chinese parents toward the oral health of their children with caries: a qualitative study. Pediatr Dent. (2005) 27(6):505–12.16532893
131. Gussy M, Waters E, Riggs E, Kilpatrick N. Mother’s perceptions of mainstream dental health messages for their children: a qualitative study. ADOHTA J. (2010):20–7.
132. Sahin E, Hazar Bodrumlu E. Relationship between early childhood caries and parents’ knowledge and attitudes towards primary teeth. Pediatr Dent J. (2024) 34(2):70–6. doi: 10.1016/j.pdj.2024.05.001
133. Dudovitz R, Teutsch C, Holt K, Herman A. Improving parent oral health literacy in head start programs. J Public Health Dent. (2020) 80(2):150–58. doi: 10.1111/jphd.12361
134. Schroth RJ, Brothwell DJ, Moffatt MEK. Caregiver knowledge and attitudes of preschool oral health and early childhood caries (ECC). Int J Circumpolar Health. (2007) 66(2):153–67. doi: 10.3402/ijch.v66i2.18247
135. Kavanagh KF, Cohen RJ, Heinig MJ, Dewey KG. Educational intervention to modify bottle-feeding behaviors among formula-feeding mothers in the WIC program: impact on infant formula intake and weight gain. J Nutr Educ Behav. (2008) 40(4):244–50. doi: 10.1016/j.jneb.2007.01.002
136. Menegaz AM, de Ávila Quevedo L, Muniz LC, Finlayson TL, Ayala GX, Cascaes AM. Changes in young children’s oral health-related behaviours and caregiver knowledge: a cluster randomized controlled trial in Brazil. Community Dent Oral Epidemiol. (2020) 48(1):81–7. doi: 10.1111/cdoe.12507
137. Watt RG, Tull KI, Hardy R, Wiggins M, Kelly Y, Molloy B, et al. Effectiveness of a social support intervention on infant feeding practices: randomised controlled trial. J Epidemiol Community Health. (2009) 63(2):156–62. doi: 10.1136/jech.2008.077115
138. Savage JS, Hohman EE, Marini ME, Shelly A, Paul IM, Birch LL. INSIGHT Responsive parenting intervention and infant feeding practices: randomized clinical trial. Int J Behav Nutr Phys Act. (2018) 15(1):64. doi: 10.1186/s12966-018-0700-6
139. Ruggiero CF, Hohman EE, Birch LL, Paul IM, Savage JS. INSIGHT Responsive parenting intervention effects on child appetite and maternal feeding practices through age 3 years. Appetite. (2021) 159:105060. doi: 10.1016/j.appet.2020.105060
140. Paul IM, Savage JS, Anzman-Frasca S, Marini ME, Beiler JS, Hess LB, et al. Effect of a responsive parenting educational intervention on childhood weight outcomes at 3 years of age: the INSIGHT randomized clinical trial. JAMA. (2018) 320(5):461–68. doi: 10.1001/jama.2018.9432
141. Hernandez E, Lavner JA, Moore AM, Stansfield BK, Beach SRH, Smith JJ, et al. Sleep SAAF responsive parenting intervention improves mothers’ feeding practices: a randomized controlled trial among African American mother-infant dyads. Int J Behav Nutr Phys Act. (2022) 19(1):129. doi: 10.1186/s12966-022-01366-1
142. Lavner JA, Savage JS, Stansfield BK, Beach SRH, Marini ME, Smith JJ, et al. Effects of the sleep SAAF responsive parenting intervention on rapid infant weight gain: a randomized clinical trial of African American families. Appetite. (2022) 175:106080. doi: 10.1016/j.appet.2022.106080
143. Harrison RL, Wong T. An oral health promotion program for an urban minority population of preschool children. Community Dent Oral Epidemiol. (2003) 31(5):392–99. doi: 10.1034/j.1600-0528.2003.00001.x
144. Lawrence HP, Romanetz M, Rutherford L, Cappel L, Binguis D, Rogers JB. Effects of a community-based prenatal nutrition program on the oral health of aboriginal preschool children in northern Ontario. Probe (Adelaide). (2004) 38(4):172–88.
145. Kyoon-Achan G, Schroth RJ, Sanguins J, Campbell R, Demaré D, Sturym M, et al. Early childhood oral health promotion for first nations and métis communities and caregivers in Manitoba. Health Promot Chronic Dis Prev Can. (2021) 41(1):14–24. doi: 10.24095/hpcdp.41.1.02
146. Smithers LG, Lynch J, Hedges J, Jamieson LM. Diet and anthropometry at 2 years of age following an oral health promotion programme for Australian aboriginal children and their carers: a randomised controlled trial. Br J Nutr. (2017) 118(12):1061–69. doi: 10.1017/S000711451700318X
147. Wild CEK, Cave TL, Willing EJ, Derraik JGB, Grant CC, Hofman PL, et al. Correspondence: systematic reviews do not always capture context of real-world intervention programmes for childhood obesity (response to littlewood, et al., 2020 in BMC public health). BMC Public Health. (2021) 21(1):501. doi: 10.1186/s12889-021-10486-5
148. Kyoon-Achan G, Schroth R, DeMaré D, Sturym M, Sanguins J, Chartrand F, et al. Healthy smile, happy child: partnering with Manitoba first nations and metis communities for better early childhood oral health. AlterNative. (2021) 17(2):265–74. doi: 10.1177/11771801211016873
149. Anderson YC, Wynter LE, Moller KR, Cave TL, Dolan GMS, Grant CC, et al. The effect of a multi-disciplinary obesity intervention compared to usual practice in those ready to make lifestyle changes: design and rationale of Whanau Pakari. BMC Obes. (2015) 2(1):41. doi: 10.1186/s40608-015-0068-y
150. Dickson-Swift V, Kenny A, Gussy M, McCarthy C, Bracksley-O’Grady S. The knowledge and practice of pediatricians in children’s oral health: a scoping review. BMC Oral Health. (2020) 20(1):211. doi: 10.1186/s12903-020-01198-0
151. Long CM, Quinonez RB, Rozier RG, Kranz AM, Lee JY. Barriers to Pediatricians’ adherence to American academy of pediatrics oral health referral guidelines: North Carolina general dentists’ opinions. Pediatr Dent. (2014) 36(4):309–15.25197996
152. Rossiter C, Cheng H, Denney-Wilson E. Primary healthcare professionals’ role in monitoring infant growth: a scoping review. J Child Health Care. (2023) 28(4):880–97. doi: 10.1177/13674935231165897
153. US Preventive Services Task Force. Screening and interventions to prevent dental caries in children younger than 5 years: uS preventive services task force recommendation statement. JAMA. (2021) 326(21):2172–78. doi: 10.1001/jama.2021.20007
154. Senturia K, Fiset L, Hort K, Huebner C, Mallott E, Milgrom P, et al. Dental health aides in Alaska: a qualitative assessment to improve paediatric oral health in remote rural villages. Community Dent Oral Epidemiol. (2018) 46(4):416–24. doi: 10.1111/cdoe.12385
155. Christian B, George A, Veginadu P, Villarosa A, Makino Y, Kim WJ, et al. Strategies to integrate oral health into primary care: a systematic review. BMJ Open. (2023) 13(7):e070622. doi: 10.1136/bmjopen-2022-070622
156. Arora A, Poudel P, Manohar N, Bhole S, Baur LA. The role of oral health care professionals in preventing and managing obesity: a systematic review of current practices and perceived barriers. Obes Res Clin Pract. (2019) 13(3):217–25. doi: 10.1016/j.orcp.2019.03.005
157. Bhoopathi V, Tripicchio G. Childhood dental caries and obesity: opportunities for interdisciplinary approaches to prevention. Obes Sci Pract. (2024) 10(1):e740. doi: 10.1002/osp4.740
158. Villarosa AR, George D, Ramjan LM, Srinivas R, George A. The role of dental practitioners in addressing overweight and obesity among children: a scoping review of current interventions and strategies. Obes Res Clin Pract. (2018) 12(5):405–15. doi: 10.1016/j.orcp.2018.07.002
159. George A, Sousa MS, Kong AC, Blinkhorn A, Patterson Norrie T, Foster J, et al. Effectiveness of preventive dental programs offered to mothers by non-dental professionals to control early childhood dental caries: a review. BMC Oral Health. (2019) 19(1):172. doi: 10.1186/s12903-019-0862-x
Keywords: dental caries, obesity, health knowledge, attitude and practice, child health, child nutrition sciences
Citation: Cheng H, Chen R, Christian B, Appleton J, Arora A and Denney-Wilson E (2025) Carer perspectives on overweight, obesity and dental caries in early childhood: findings from a systematic qualitative review. Front. Oral Health 6:1524715. doi: 10.3389/froh.2025.1524715
Received: 8 November 2024; Accepted: 21 May 2025;
Published: 18 June 2025.
Edited by:
Iole Vozza, Sapienza University of Rome, ItalyReviewed by:
Denise Corridore, Sapienza University of Rome, ItalyMorenike Oluwatoyin Folayan, Nigerian Institute of Medical Research (NIMR), Nigeria
Abedelmalek Kalefh Tabnjh, University of Gothenburg, Sweden
Giulia Zumbo, Sapienza University of Rome, Italy
Copyright: © 2025 Cheng, Chen, Christian, Appleton, Arora and Denney-Wilson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heilok Cheng, amVzc2ljYS5jaGVuZ0BzeWRuZXkuZWR1LmF1
†Present Address: Amit Arora, ARCED Foundation, Dhaka, Bangaledesh
 Heilok Cheng
Heilok Cheng Rebecca Chen4,5,6
Rebecca Chen4,5,6 Amit Arora
Amit Arora Elizabeth Denney-Wilson
Elizabeth Denney-Wilson