- 1College of Medicine, University of Nigeria, Ituku-Ozalla Enugu, Nigeria
- 2Harvard School of Dental Medicine, Boston, MA, United States
This article explores the transformative potential of public health policies to improve oral health outcomes through the integrated application of three fundamental pillars: sustainability, equity in healthcare access, and the reduction of oral health disease burden. By examining the interplay of these pillars, the discussion proposes strategies that not only enhance preventive measures and accessibility to dental care but also foster long-term, sustainable improvements in population oral health. The framework presented herein is intended to guide policymakers in creating evidence-based interventions that address disparities and mitigate the growing burden of oral diseases globally.
Introduction
Oral health remains a critical component of overall well-being, yet persistent disparities and a significant disease burden continues to affect diverse populations (1). The need for robust public health policies is paramount, particularly as oral diseases contribute substantially to global morbidity and socioeconomic inequities (2). This article leverages the pillars of sustainability, equity healthcare access, and oral health disease burden to frame public health policy interventions that promote prevention, improve access to care, and achieve equitable health outcomes.
To begin with, sustainability in oral health policy is essential for ensuring that interventions are not only effective in the short term but also resilient in the face of evolving public health challenges. Sustainable strategies involve the development of infrastructure that supports continuous improvement in service delivery, the implementation of preventive programs that reduce the incidence of oral diseases, and the adoption of practices that are both economically and environmentally viable (3). Prioritizing sustainability enables policymakers to build resilient health systems that can withstand future challenges while adapting to dynamic demographics and addressing the diverse needs of communities (4).
Equally important is the pillar of equitable access to oral healthcare. Despite advancements in dental care, significant gaps remain in access to quality oral health services (5). These disparities are often rooted in socioeconomic factors, geographic barriers and sometimes, cultural differences that hinder certain groups from receiving adequate care (6, 7). Policies aimed at promoting equity in care must address these issues head-on by expanding access to dental services through community outreach programs, mobile clinics, and teledentistry (8). Furthermore, investing in workforce development initiatives that ensure an adequate supply of trained dental professionals in underserved areas and removing barriers to access while ensuring that every individual receives timely and effective care allow public health policies to play a pivotal role in reducing oral health inequities (9–11).
The burden of oral diseases, including dental caries, periodontal diseases, and oral cancers, continues to escalate globally, placing an immense strain on healthcare systems (1, 2). The direct and indirect costs associated with treating advanced stages of these diseases further exacerbate the socioeconomic divide (12). Effective public health policies must therefore prioritize early intervention and prevention (13). This includes implementing evidence-based community programs, such as water fluoridation, school-based oral health education and routine screenings, which are proven to reduce the prevalence of oral diseases (9, 14). Moreover, a data-driven approach to resource allocation can help identify high-risk populations and regions, ensuring that interventions are targeted where they are most needed and that the overall burden of disease is systematically reduced (15, 16).
Sustainability: building resilient oral health systems
Sustainability in oral health also means building partnerships across sectors and disciplines to ensure a well-coordinated approach to public health challenges (17). Collaborations between government agencies, private dental care providers, academic institutions, and community organizations are essential for pooling resources, sharing best practices and fostering innovations that can lead to more resilient oral health systems (9, 18). Such partnerships facilitate the development of integrated care models that not only respond to current needs but also anticipate future challenges by incorporating emerging technologies and evolving healthcare delivery methods (19–21).
Sustainable oral health policies should embed mechanisms for regular assessment and feedback, allowing for iterative improvements in strategy and execution (22). Setting measurable goals and performance indicators enables policymakers to track progress, identify areas for improvement and ensure that investments generate long-term benefits (23). This continuous cycle of evaluation and adjustment helps maintain a dynamic system that remains responsive to changes in population demographics, disease patterns, and technological advancements (24).
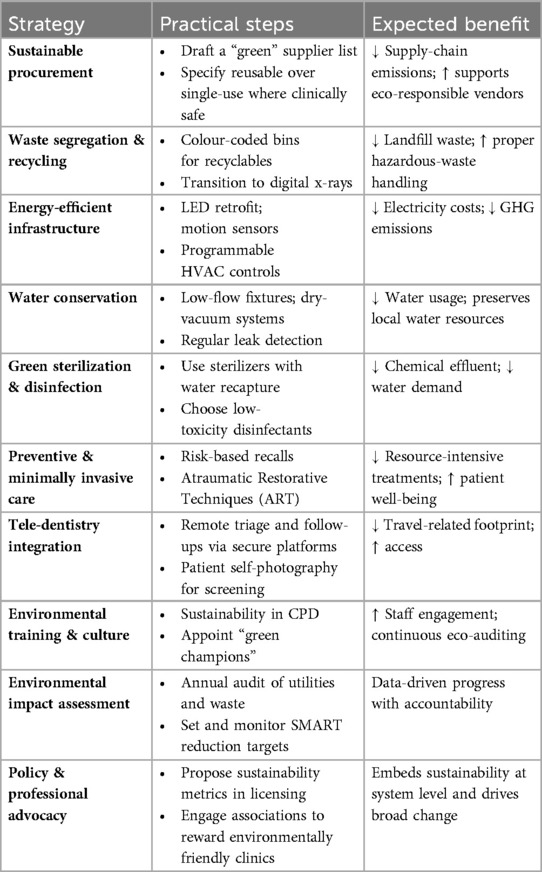
Another critical aspect is the integration of environmental stewardship into oral health initiatives. As the healthcare sector increasingly prioritizes reducing its ecological footprint, oral health policies must incorporate eco-friendly practices, from sustainable procurement of dental materials to energy-efficient clinic operations, ensuring that healthcare delivery aligns with environmental goals while remaining economically viable and socially responsible (25, 26).
Specific national policies explicitly supporting green dentistry are limited. However, organizations like the European Federation of Periodontology and the FDI World Dental Federation offer guidelines and recommendations for sustainable dental practices within the dental field. These include energy efficiency measures (e.g., LED lighting, renewable energy), water conservation (e.g., low-flow faucets), and waste management (e.g., recycling, biodegradable materials). An overview of these sustainability strategies and their operational implications is provided in Table 1.
Sustainability in oral health is not a static goal but an ongoing process that requires vision, commitment, and collaboration, and by embedding these principles into public health policies, communities can ensure accessible quality dental care, minimize environmental impacts and maintain a system agile enough to meet society's evolving needs (9, 25, 27).
Equity in access to oral healthcare: addressing disparities in oral health
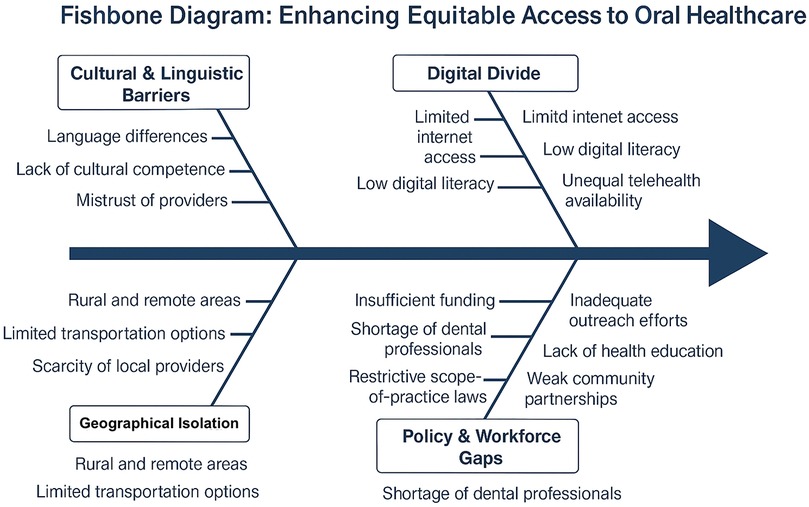
Equitable access to oral health care involves tailoring healthcare delivery to meet the unique cultural, linguistic and socioeconomic needs of diverse communities (28, 29). This multifactorial challenge is depicted in Figure 1, which outlines a Fishbone Model for Enhancing Equitable Access to Oral Healthcare. This means developing culturally competent care models that acknowledge and address specific barriers faced by minority and marginalized populations (30, 31). Such models involve training healthcare professionals in cultural sensitivity, integrating community health workers who share similar backgrounds with the target populations, and designing outreach programs that resonate with local values and practices (30, 32).
In addition, targeted policies must focus on reducing systemic barriers that limit access to quality dental care. This includes addressing financial obstacles through subsidized services or insurance schemes and overcoming logistical challenges by investing in transportation and digital connectivity for tele-dentistry initiatives (9). These strategies can bridge the gap between urban centers and rural or remote areas, ensuring that underserved populations receive the same standard of care as their more urban counterparts (33).
Moreover, fostering strong partnerships with community organizations, faith-based groups, and local leaders is crucial in disseminating health information and building trust (34). Community engagement not only increases awareness about the importance of preventive dental care but also encourages collective action toward creating supportive environments for oral health (9, 35).
Oral health disease burden: prioritizing high-impact interventions that is population specific
The global burden of oral diseases, such as dental caries, periodontal diseases, and oral cancers, places immense pressure on healthcare systems worldwide. Among children and adolescents, dental caries remains the most prevalent condition, calling for preventive strategies such as school-based fluoride varnish programs, water fluoridation, and sugar intake regulation. In working-age adults, periodontal diseases dominate, requiring policies that promote oral hygiene education, smoking cessation initiatives, and early periodontal screening within workplaces and community health centers. For older adults, particularly in populations with high rates of tobacco and alcohol consumption, oral cancers present a significant threat, emphasizing the need for systematic oral cancer screenings embedded in primary care services (1, 2). Targeted policies for specific burdens and populations ensure that interventions are aligned with the actual patterns of disease, allowing for efficient resource allocation and greater public health impact. Effective public health policies must focus on targeted interventions backed by robust epidemiological research and demonstrated success (36). To identify and prioritize these burdens accurately, epidemiological data must be systematically gathered through comprehensive needs assessments which captures disease prevalence and service gaps through continuous surveillance systems that monitor oral health trends over time. Following this, implementing population-based preventive measures becomes imperative (37). In addition to prevention, early detection plays a critical role in mitigating the severity of oral diseases (1, 9). Integrating routine oral health screenings into general health check-ups allows for the early identification of potential issues, enabling prompt intervention before conditions escalate into more severe or life-threatening stages (38, 39). This proactive approach not only improves individual outcomes but also reduces the long-term economic burden on healthcare systems by preventing costly treatments and hospitalizations associated with advanced oral diseases (40).
Furthermore, the strategic allocation of resources based on robust epidemiological data is essential for targeting interventions effectively (41). This targeted approach ensures that preventive programs and treatment facilities are established in high-risk areas, thus maximizing the impact of interventions and promoting a more equitable distribution of healthcare services (4, 6, 40).
High-impact interventions should also incorporate innovative solutions such as community-based screening programs, mobile dental clinics, and tele-dentistry services (42). These innovations extend the reach of traditional healthcare systems, particularly in underserved rural and remote communities where access to dental care is limited (9). Tele dentistry's platforms enable early screening, risk stratification and remote triage while shifting care toward preventive and minimally invasive interventions, and reducing travel barriers and clinic congestion. When linked to epidemiological data and underpinned by public private partnerships, these digital services allow precise, scalable resource allocation that promotes equity and significantly lowers the overall oral disease burden.
Additionally, public-private partnerships can bolster these efforts, fostering collaborations that leverage diverse expertise and financial resources to implement scalable, sustainable solutions (43).
Policy recommendations
Drawing on the pillars of sustainability, equality, and the reduction of the oral health disease burden, comprehensive policy recommendations can be advanced to transform the delivery of oral health services within public health systems (44). A foundational element of these recommendations is the development of integrated health models that seamlessly incorporate oral health into the broader framework of public healthcare (39). By doing so, oral health becomes an intrinsic component of overall health management, allowing for more coordinated care that recognizes the interconnectedness of dental conditions with chronic diseases such as diabetes and cardiovascular disorders (9, 45). Such integration not only streamlines service delivery but also facilitates the early detection and management of oral diseases within routine health check-ups, thus mitigating the progression to more severe conditions and reducing long-term healthcare costs (39, 46).
Collaboration among governmental agencies, educational institutions, community organizations, and the private sector is vital to mobilizing the necessary resources and expertise (47, 48). Cross-sector partnerships enable the pooling of knowledge, technology, and financial resources, which can be leveraged to establish comprehensive care networks, especially in underserved regions (6, 20). These collaborations can also foster the development of multidisciplinary training programs that prepare healthcare professionals to address the unique challenges of oral health in diverse communities (18). These interlinked strategies are synthesized in Figure 2, which illustrates a Framework for Targeted Oral Health Interventions linking Needs Assessment to Sustainable and Equitable Outcomes. Through shared responsibility and joint initiatives, the collective expertise of these stakeholders can drive innovation in service delivery, ensuring that policies are both responsive and adaptable to evolving public health needs (4, 20).
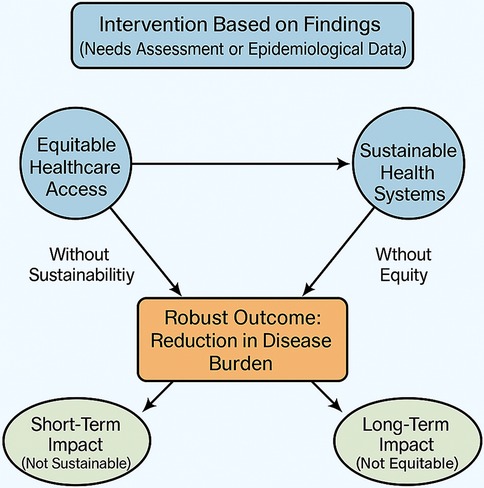
Figure 2. Framework for targeted oral health interventions linking needs assessment to sustainable and equitable outcomes.
Investment in research and innovation is crucial for developing new preventive strategies, diagnostic tools, and sustainable treatment modalities, with robust initiatives exploring emerging technologies such as digital diagnostics and tele-dentistry, which have the potential to revolutionize oral health care delivery, particularly in resource-limited settings (49). This commitment to innovation not only enhances the precision of early diagnosis but also supports the creation of interventions that are tailored to the socioeconomic contexts of various populations (4). Designing community-centered programs that are attuned to local needs further underscores the importance of equality in public health policy (50). Involving community members in the planning and execution of oral health initiatives fosters a sense of ownership and ensures that the programs address specific cultural, geographic, and socioeconomic barriers to care (20). These initiatives might include local education campaigns, the deployment of mobile dental units, and the establishment of tele-dentistry services that reach remote areas (51).
Finally, the establishment of robust monitoring and evaluation systems is essential for ensuring that policy interventions are having their intended impact and for identifying areas where continuous improvement is necessary (52, 53). Comprehensive data collection and analysis allow for real-time feedback on program effectiveness, facilitating adjustments that can optimize resource allocation and improve outcomes over time (15). Such systems not only provide accountability but also enable the dissemination of best practices across different regions and contexts (4). Regular evaluation of policy performance ensures that initiatives remain aligned with the overarching goals of sustainability, equality, and the reduction of the oral health disease burden, ultimately fostering a dynamic and responsive public health system (44, 54).
Framework for Targeted Oral Health Interventions linking Needs Assessment to Sustainable and Equitable Outcomes.
Conclusion
Integrating the pillars of sustainability, equality, and targeted interventions against the oral health disease burden provides a robust framework for strengthening public health policies. By focusing on long-term, equitable, and high-impact strategies, policymakers can substantially enhance oral health outcomes, reduce disparities, and create resilient systems capable of addressing the future challenges of oral healthcare. This approach not only benefits individual communities but also contributes to the overall strengthening of global health systems, fostering a future where equitable oral health is within reach for all.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
CA: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. CO: Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. Artificial Intelligence (AI) was utilized to enhance the language and grammar of the manuscript by improving clarity, coherence, and academic precision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Oral health. Geneva: World Health Organization (2025). Available at: https://www.who.int/news-room/fact-sheets/detail/oral-health (Accessed March 20, 2025).
2. Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet. (2019) 394(10194):249–60. doi: 10.1016/S0140-6736(19)31146-8
3. Foláyan MO, Ishola AG, Bhayat A, El Tantawi M, Ndembi N. Strengthening health systems to tackle oral diseases in Africa: Africa centers for disease control and prevention’s role. Front Public Health. (2025) 13:1539805. doi: 10.3389/fpubh.2025.1539805
4. Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. (2018) 6(11):e1196–252. doi: 10.1016/S2214-109X(18)30386-3
5. Northridge ME, Kumar A, Kaur R. Disparities in access to oral health care. Annu Rev Public Health. (2020) 41:513–35. doi: 10.1146/annurev-publhealth-040119-094318
6. Hoagland A, Kipping S. Challenges in promoting health equity and reducing disparities in access across new and established technologies. Can J Cardiol. (2024) 40(6):1154–67. doi: 10.1016/j.cjca.2024.02.014
7. World Health Organization. Health inequalities and their causes. Geneva: World Health Organization (2025). Available at: https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (Accessed March 26, 2025).
8. Lehnert L, Thakur Y. Alternative pathways in dentistry: mobile dental clinics, illustration of implementation in San Mateo and Santa Clara county through federally qualified health center. J Calif Dent Assoc. (2024) 52(1). doi: 10.1080/19424396.2024.2320945
9. National Institutes of Health. Section 4 Oral Health Workforce, Education, Practice and Integration. In: Oral Health in America: Advances and Challenges. Bethesda, MD: National Institute of Dental and Craniofacial Research(US) (2021). Available at: https://www.ncbi.nlm.nih.gov/books/NBK578298/
10. National Institutes of Health. Section 1 Effect of Oral Health on the Community, Overall Well-Being, and the Economy. In: Oral Health in America: Advances and Challenges. Bethesda, MD: National Institute of Dental and Craniofacial Research(US) (2021). Available at: https://www.ncbi.nlm.nih.gov/books/NBK578297/
11. Gizaw Z, Astale T, Kassie GM. What improves access to primary healthcare services in rural communities? A systematic review. BMC Primary Care. (2022) 23(1):313. doi: 10.1186/s12875-022-01919-0
12. Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. (2014) 20(4):327–37. doi: 10.3350/cmh.2014.20.4.327
13. Frieden TR. Six components necessary for effective public health program implementation. Am J Public Health. (2014) 104(1):17–22. doi: 10.2105/AJPH.2013.301608
14. Alshammari FR, Alsayed AA, Albakry M, Aljohani M, Kabbi H, Alamri H. Evidence based recommendations to improve the children’s oral health in Saudi Arabia. Saudi Dent J. (2022) 34(6):431–44. doi: 10.1016/j.sdentj.2022.06.003
15. Cascini F, Santaroni F, Lanzetti R, Failla G, Gentili A, Ricciardi W. Developing a data-driven approach in order to improve the safety and quality of patient care. Front Public Health. (2021) 9:667819. doi: 10.3389/fpubh.2021.667819
16. Chao K, Sarker MNI, Ali I, Firdaus RBR, Azman A, Shaed MM. Big data-driven public health policy making: potential for the healthcare industry. Heliyon. (2023) 9(9):e19681. doi: 10.1016/j.heliyon.2023.e19681
17. de Lara JVI, Frazão P. Oral health guidelines in the primary care policies of five selected countries: an integrative review. Health Policy OPEN. (2021) 2:100042. doi: 10.1016/j.hpopen.2021.100042
18. Glick M, Urquhart O, Bhosale AS, Carrasco-Labra A, Edelson JT. A unified voice to drive global improvements in oral health. BMC Glob Public Health. (2023) 1(1):19. doi: 10.1186/s44263-023-00019-0
19. Junaid SB, Imam AA, Balogun AO, De Silva LC, Surakat YA, Kumar G, et al. Recent advancements in emerging technologies for healthcare management systems: a survey. Healthcare (Basel). (2022) 10(10):1940. doi: 10.3390/healthcare10101940
20. Alderwick H, Hutchings A, Briggs A, Mays N. The impacts of collaboration between local health care and non-health care organizations and factors shaping how they work: a systematic review of reviews. BMC Public Health. (2021) 21(1):753. doi: 10.1186/s12889-021-10630-1
21. Kreuter MW, Thompson T, McQueen A, Garg R. Addressing social needs in health care settings: evidence, challenges, and opportunities for public health. Annu Rev Public Health. (2021) 42:329–44. doi: 10.1146/annurev-publhealth-090419-102204
22. Simpson DD. A framework for implementing sustainable oral health promotion interventions. J Public Health Dent. (2011) 71(s1):S84–94. doi: 10.1111/j.1752-7325.2011.00234.x
23. Sreedharan J, Subbarayalu AV, Kamalasanan A, Albalawi I, Krishna GG, Alahmari AD, et al. Key performance indicators: a framework for allied healthcare educational institutions. Clinicoecon Outcomes Res. (2024) 16:173–85. doi: 10.2147/CEOR.S446614
24. Tulchinsky TH, Varavikova EA. Measuring, monitoring, and evaluating the health of a population. New Public Health. (2014):91–147. doi: 10.1016/B978-0-12-415766-8.00003-3
25. Martin N, Mulligan S. Environmental sustainability through good-quality oral healthcare. Int Dent J. (2022) 72(1):26–30. doi: 10.1016/j.identj.2021.06.005
26. Martínez-Peláez R, Ochoa-Brust A, Rivera S, Félix VG, Ostos R, Brito H, et al. Role of digital transformation for achieving sustainability: mediated role of stakeholders, key capabilities, and technology. Sustainability. (2023) 15(14):11221. doi: 10.3390/su151411221
27. Varzakas T, Antoniadou M. A holistic approach for ethics and sustainability in the food chain: the gateway to oral and systemic health. Foods. (2024) 13(8):1224. doi: 10.3390/foods13081224
28. Garcia RI, Cadoret CA, Henshaw M. Multicultural issues in oral health. Dent Clin North Am. (2008) 52(2):319–vi. doi: 10.1016/j.cden.2007.12.006
29. Foláyan MO, Bernard OT, Titus OS, Alade O, Aliyu TK, Bhayat A, et al. Cultural practices, oral health service utilisation and oral health policy and guidelines development in Africa: insights from the Yorùbá ethnic group. Front Oral Health. (2025) 6:1539827. doi: 10.3389/froh.2025.1539827
30. Nair L, Adetayo OA. Cultural competence and ethnic diversity in healthcare. Plastic and reconstructive surgery. Glob Open. (2019) 7(5):e2219. doi: 10.1097/GOX.0000000000002219
31. Stubbe DE. Practicing cultural competence and cultural humility in the care of diverse patients. Focus (Am Psychiatr Publ). (2020) 18(1):49–51. doi: 10.1176/appi.focus.20190041
32. Singh H, Fulton J 4th, Mirzazada S, Saragosa M, Uleryk EM, Nelson MLA. Community-based culturally tailored education programs for black communities with cardiovascular disease, diabetes, hypertension, and stroke: systematic review findings. J Racial Ethn Health Disparities. (2023) 10(6):2986–3006. doi: 10.1007/s40615-022-01474-5
33. Chen X, Orom H, Hay JL, Waters EA, Schofield E, Li Y, et al. Differences in rural and urban health information access and use. J Rural Health. (2019) 35(3):405–17. doi: 10.1111/jrh.12335
34. Gwathmey TM, Williams KL, Caban-Holt A, Starks TD, Foy CG, Mathews A, et al. Building a community partnership for the development of health ministries within the African American community: the triad pastors network. J Community Health. (2024) 49(3):559–67. doi: 10.1007/s10900-023-01315-4
35. Molete MM, Malele-Kolisa Y, Thekiso M, Lang AY, Kong A, George A. The role of community health workers in promoting oral health at school settings: a scoping review. J Public Health Dent. (2024) 84(2):175–86. doi: 10.1111/jphd.12612
36. Thomson K, Hillier-Brown F, Todd A, McNamara C, Huijts T, Bambra C. The effects of public health policies on health inequalities in high-income countries: an umbrella review. BMC Public Health. (2018) 18:869. doi: 10.1186/s12889-018-5677-1
37. Shahzad M, Upshur R, Donnelly P, Bharmal A, Wei X, Feng P, et al. A population-based approach to integrated healthcare delivery: a scoping review of clinical care and public health collaboration. BMC Public Health. (2019) 19:708. doi: 10.1186/s12889-019-7002-z
38. Betts KJ, Moravec L. Integration of oral health screening, intervention, and referral into the pediatric well-child visit. J Pediatr Health Care. (2023) 37(6):609–15. doi: 10.1016/j.pedhc.2023.05.007
39. Prasad M, Manjunath C, Murthy AK, Sampath A, Jaiswal S, Mohapatra A. Integration of oral health into primary health care: a systematic review. J Family Med Prim Care. (2019) 8(6):1838–45. doi: 10.4103/jfmpc.jfmpc_286_19
40. AbdulRaheem Y. Unveiling the significance and challenges of integrating prevention levels in healthcare practice. J Prim Care Community Health. (2023) 14:21501319231186500. doi: 10.1177/21501319231186500
41. Fairchild G, Tasseff B, Khalsa H, Generous N, Daughton AR, Velappan N, et al. Epidemiological data challenges: planning for a more robust future through data standards. Front Public Health. (2018) 6:336. doi: 10.3389/fpubh.2018.00336
42. Niknam F, Sharifian R, Bashiri A, Mardani M, Akbari R, Tuffaha H, et al. Tele-dentistry, its trends, scope, and future framework in oral medicine; a scoping review during January 1999 to December 2021. Arch Public Health. (2023) 81:104. doi: 10.1186/s13690-023-01128-w
43. Strasser S, Stauber C, Shrivastava R, Riley P, O'Quin K. Collective insights of public-private partnership impacts and sustainability: a qualitative analysis. PLoS One. (2021) 16(7):e0254495. doi: 10.1371/journal.pone.0254495
44. Abodunrin OR, Olagunju MT, Alade OT, Foláyan MO. Relationships between oral health and the sustainable development goals: a scoping review. BioMed. (2023) 3(4):460–70. doi: 10.3390/biomed3040037
45. Fu D, Shu X, Zhou G, Ji M, Liao G, Zou L. Connection between oral health and chronic diseases. MedComm. (2025) 6(1):e70052. doi: 10.1002/mco2.70052
46. Amaya A, Medina I, Mazzilli S, D'Arcy J, Cocco N, Van Hout MC, et al. Oral health services in prison settings: a global scoping review of availability, accessibility, and model of delivery. J Community Psychol. (2024) 52(8):1108–37. doi: 10.1002/jcop.23081
47. Rajabi M, Ebrahimi P, Aryankhesal A. Collaboration between the government and nongovernmental organizations in providing health-care services: a systematic review of challenges. J Educ Health Promot. (2021) 10:242. doi: 10.4103/jehp.jehp_1312_20
48. Obi C, Ojiakor I, Etiaba E, Onwujekwe O. Collaborations and networks within communities for improved utilization of primary healthcare centers: on the road to universal health coverage. Int J Public Health. (2024) 69:1606810. doi: 10.3389/ijph.2024.1606810
49. de Carvalho LFDCES, Zanatta RF. Editorial: technological innovations for improved prevention and diagnosis of oral disease. Front Oral Health. (2024) 5:1481890. doi: 10.3389/froh.2024.1481890
50. Yuan M, Lin H, Wu H, Yu M, Tu J, Lü Y. Community engagement in public health: a bibliometric mapping of global research. Arch Public Health. (2021) 79:6. doi: 10.1186/s13690-021-00525-3
51. Bala R, Sargaiyan V, Rathi SA, Mankar SS, Jaiswal AK, Mankar SA. Mobile dental clinic for oral health services to underserved rural Indian communities. Bioinformation. (2023) 19(13):1383–7. doi: 10.6026/973206300191383
52. Danforth K, Ahmad AM, Blanchet K, Khalid M, Means AR, Memirie ST, et al. Monitoring and evaluating the implementation of essential packages of health services. BMJ Glob Health. (2023) 8(Suppl 1):e010726. doi: 10.1136/bmjgh-2022-010726
53. de Cola MA, Chestnutt EG, Richardson S, Baudry M, Nnaji C, Ibinaiye T, et al. From efficacy to effectiveness: a comprehensive framework for monitoring, evaluating and optimizing seasonal malaria chemoprevention programmes. Malar J. (2024) 23:39. doi: 10.1186/s12936-024-04860-y
Keywords: oral health policy, sustainability, health equity, disease burden, preventive strategies
Citation: Anyikwa CL and Ogwo CE (2025) Enhancing oral health outcomes through public health policy reform. Front. Oral Health 6:1604465. doi: 10.3389/froh.2025.1604465
Received: 1 April 2025; Accepted: 12 May 2025;
Published: 9 June 2025.
Edited by:
Praveen S. Jodalli, Manipal College of Dental Sciences, IndiaReviewed by:
Shimaa Hussein Kotb, Sphinx University, EgyptPriyanga Chandrasekaran, Sri Balaji Vidyapeeth (Deemed to be) University, India
Copyright: © 2025 Anyikwa and Ogwo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chukwuemeka L. Anyikwa, YW55aWt3YWVtZWthQGdtYWlsLmNvbQ==
†ORCID:
Chukwuebuka E. Ogwo
orcid.org/0000-0002-9325-0126
 Chukwuemeka L. Anyikwa
Chukwuemeka L. Anyikwa Chukwuebuka E. Ogwo2,†
Chukwuebuka E. Ogwo2,†