- 1Kuwait Ministry of Health, Kuwait City, Kuwait
- 2Tufts University School of Dental Medicine, Boston, MA, United States
- 3Department of Public Health, Tufts University School of Dental Medicine, Boston, MA, United States
- 4Dasman Diabetes Institute, Kuwait City, Kuwait
- 5Division of Pediatric Dentistry, Department of Preventive Dentistry, Faculty of Dentistry, Umm Al-Qura University, Mecca, Saudi Arabia
- 6Department of Oral Health Policy and Epidemiology, Harvard School of Dental Medicine, Boston, MA, United States
Background: Human papillomavirus (HPV) infection is a significant risk factor for oropharyngeal cancer (OPC), yet dental students' knowledge of this association varies widely. Given the critical role dentists play in early detection and prevention, understanding their level of knowledge is essential. This study systematically reviews existing research to assess dental students' awareness of HPV and its link to OPC.
Methods: A systematic review and meta-analysis were conducted following PRISMA guidelines. PubMed, ProQuest, and Web of Science databases were searched for studies published up to August 2023. The Newcastle-Ottawa Scale was used to evaluate study quality. A random effects model was applied to calculate pooled prevalence with 95% confidence intervals.
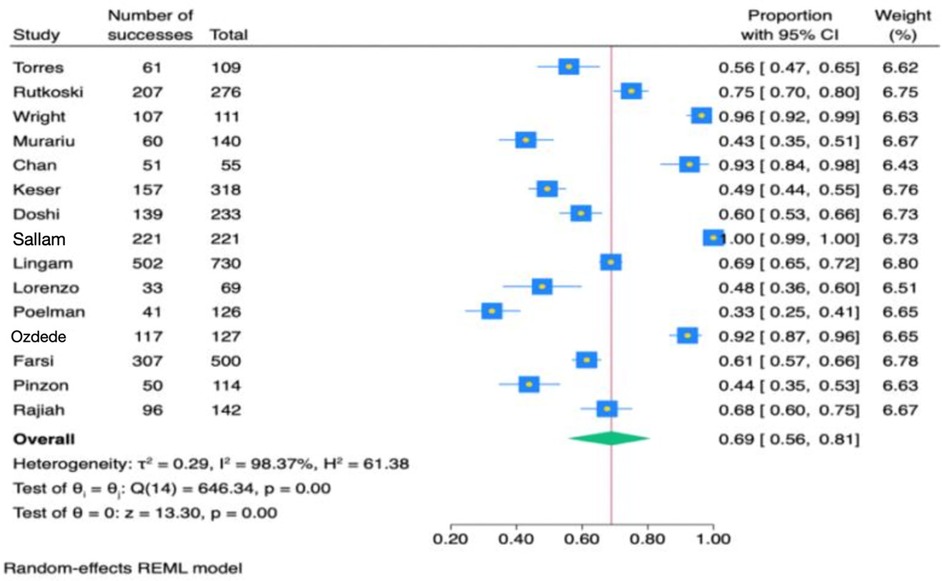
Results: Sixteen studies, comprising 6,345 participants, were included. The pooled analysis showed that 69% of dental students had general knowledge of HPV (range: 56%–96.5%; 95% CI: 0.56–0.81), while 77% recognized its association with OPC (range: 18%–96.4%; 95% CI: 0.63–0.89). Significant heterogeneity was observed across studies (Q = 646.34, P < 0.001 for HPV; Q = 804.07, P < 0.001 for HPV-OPC).
Conclusion: Knowledge gaps among dental students may hinder prevention efforts. Standardized education in dental curricula is crucial to ensure future dentists are well-prepared to address HPV-related conditions and promote early detection in clinical practice.
1 Introduction
The World Health Organization (WHO) reported that cancer ranks as the second leading cause of global mortality (1). Various risk factors for oral cancer have been suggested, involving a complex interplay of factors, including the use of betel or areca nut, tobacco, and alcohol consumption (2). Furthermore, human papillomavirus (HPV) emerges as a significant risk factor for oral cancer (3). HPV is known for its sexual transmission and can infect various body regions (4). With over 40 subtypes, high-risk variants such as HPV-16 and HPV-18 are implicated in cervical, anogenital tract, and oropharyngeal cancers (OPC) (4). Approximately 4.5% of worldwide cancer cases are attributed to HPV-related OPC, giving rise to around 630,000 new cases each year (5).
In 2023, the American Dental Association recommended that dentists routinely conduct oral and oropharyngeal cancer screenings on all patients (6). These recommendations emphasize the critical role that dentists play in the early detection of oral cancers during regular check-ups to improve treatment outcomes. Given that HPV is a risk factor for oropharyngeal cancer (3), it is imperative for dentists to have a thorough understanding of different aspects of HPV and related preventive measures like early detection and vaccination. This awareness is essential not only for the early detection of oral cancers but also for highlighting the connection between oral health and overall health, positioning dentists as key players in early detection of HPV and promoting preventive healthcare measures.
Importantly, the implementation of HPV vaccines is recommended as a strategy to reduce the incidence of HPV, given their proven efficacy against cervical and anogenital tract cancers, along with their potential to mitigate oropharyngeal cancers (4). Dentists are well-positioned to educate patients about HPV transmission risks, enhance awareness, facilitate lifestyle adjustments, and actively champion participation in HPV vaccination campaigns with the overarching aim of mitigating the escalating prevalence of HPV-related oropharyngeal cancers. A deficiency of knowledge among dentists may pose a challenge to effectively delivering preventive measures to their patients.
Previous cross-sectional studies spanning various countries have investigated the knowledge of dental students regarding HPV. In the United States, Rutkoski et al. conducted a study titled “A Multi-State Evaluation of Oral Health Students” Knowledge of Human Papillomavirus Related Oropharyngeal Cancer and HPV Vaccination” (3). The survey revealed that only 18% of participants correctly identified that HPV could cause OPC (3). In Romania, Murariu et al. explored the knowledge, practice, and awareness of oral cancer and HPV infection among dental students and residents (1). One of the survey questions focused on the transmission of HPV, with 42.8% providing the correct response (1). Additionally, a 2015 study in India by Doshi et al. assessed HPV-related knowledge among female dental students, finding that 32.19% correctly associated HPV with oral cancer (7).
The most recent systematic review conducted by Kazeminejad et al. in 2021 reported that over 80% of dental students were aware that HPV can cause oropharyngeal cancer (OPC), and more than 75% of dentists acknowledged this link (8). However, no meta-analysis to date has synthesized findings on this topic. To address this gap, the present study aimed to systematically assess the level of knowledge among dental students regarding the association between HPV and OPC, and to provide informed recommendations for incorporating HPV education into dental curricula. Guided by the PICOS framework, this review included studies involving dental students that assessed educational exposure or awareness of HPV and its link to OPC, without requiring a comparator due to its prevalence-focused nature. The primary outcome was the reported level of knowledge or awareness of HPV-related OPC, which shaped the research question and eligibility criteria.
2 Materials and methods
2.1 Protocol
The systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Eligible studies were selected for further investigation based on these criteria. The assessment of the level of knowledge regarding HPV and its association with OPC guided the systematic review and meta-analysis, shaping the selection of participants, data extraction, and the overall analytical framework of the study.
2.2 Eligibility
The Inclusion Criteria:
• Studies published up to August 2023
• Participants: Only dental students
• Study Design: Cross-sectional studies that included questions related to general knowledge about HPV and its association with OPC
Exclusion Criteria:
• Studies that included participants other than dental students
• Study designs other than cross-sectional
• Studies with questions about HPV that did not relate to general knowledge or OPC-related knowledge
2.3 Quality assessment
Each included study was independently reviewed by two investigators (K.A. and W.B.). The risk of bias was assessed using an adapted version of the Newcastle-Ottawa Scale, tailored specifically for cross-sectional studies. Any disagreements were resolved through consensus (9).
2.4 Search strategy
Databases, including PubMed, ProQuest, and Web of Science, were systematically searched for studies published up to August 2023. The search utilized terms such as “Aware*”, OR “attitude*”, OR “knowledge*”, AND “papilloma virus”, OR “human papillomavirus”, OR “HPV*”, AND “Dent*” as seen in Table 1. Additionally, a manual search was conducted to identify relevant publications. The search was restricted to English-language studies, and results were compiled into an Excel spreadsheet. Two authors independently assessed the titles and abstracts of identified studies to determine inclusion based on predefined criteria. Any discrepancies were resolved through consultation with a third author. Selected articles underwent full-text review to extract relevant information.
2.5 Data analysis
The aim of this study was to assess the knowledge of dental students regarding HPV infection and its association with oral cancer. Two forest plot graphs were constructed to present the estimated effects as prevalences with 95% confidence intervals. The analysis employed the restricted maximum likelihood method, choosing between random effects or fixed effects models based on the Q statistic to indicate study heterogeneity. Significant heterogeneity prompted verification using the random effects model. Statistical significance was set at P < 0.05. Data analysis was performed using STATA V. 16 statistical software.
3 Results
3.1 Literature search
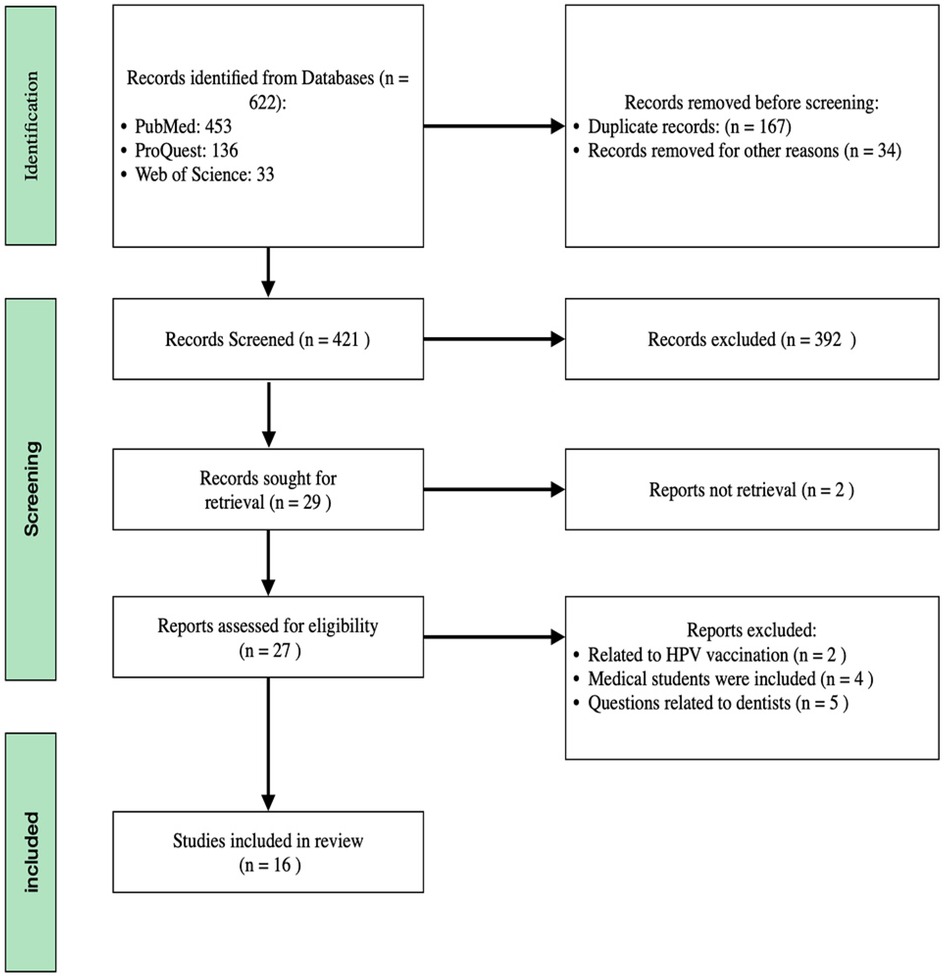
The literature search conducted on PubMed, ProQuest, and Web of Science identified 453, 136, and 33 titles, respectively. Subsequent evaluation of these titles led to the selection of 29 relevant articles. However, upon further analysis, it was found that 11 articles did not meet the inclusion criteria, and two articles were unretrievable. Therefore, the review ultimately incorporated 16 articles. The rationale for the exclusion of specific studies and the methodology employed for article selection are visually represented in Figure 1. The category labeled “other reasons” includes exclusions due to factors such as duplicate records, irrelevance to the topic based on title and abstract screening, lack of access to full text, and article types that did not meet the inclusion criteria. Additionally, Figures 2, 3 demonstrate funnel plot analysis to assess publication bias among the included studies. Visual inspection of the plots suggested potential asymmetry in both outcomes. Egger's test confirmed statistically significant publication bias for studies reporting general HPV knowledge among dental students (P = 0.0005) and for those assessing knowledge of the HPV–oropharyngeal cancer (OPC) association (P = 0.0007). Of the 16 included studies, 15 addressed general questions regarding HPV among students, while 13 discussed the relationship between HPV and OPC.
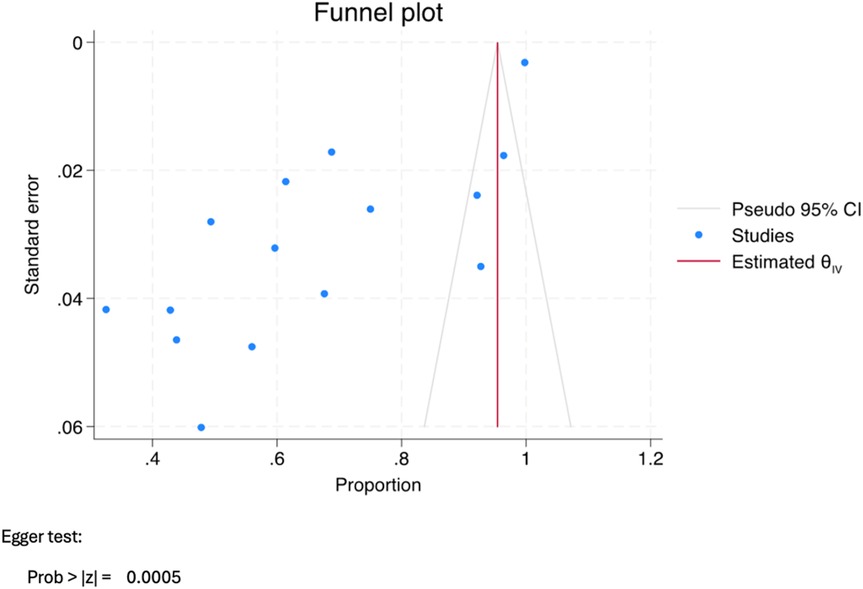
Figure 2. Funnel plot assessing publication bias for studies reporting general knowledge of HPV among dental students.

Figure 3. Funnel plot assessing publication bias for studies evaluating dental students’ knowledge of the association between HPV and oropharyngeal cancer (OPC).
3.2 Study characteristics
The characteristics of the studies included in this meta-analysis are presented in Table 2. A total of 16 cross-sectional studies were included, with 14 addressing general HPV knowledge and 13 focusing on HPV and OPC (1, 3–5, 7, 10–20). The sample sizes ranged from 55 to 730 participants, and the studies were conducted across various countries. Specifically, this systematic review included four studies from the United States conducted between 2020 and 2022, with sample sizes ranging from 55 to 276 participants. The assessment of HPV knowledge in these studies revealed percentages ranging from 56% to 96.5%. The studies also evaluated the awareness of the relationship between HPV and OPC, with awareness percentages ranging from 18% to 96.4%.
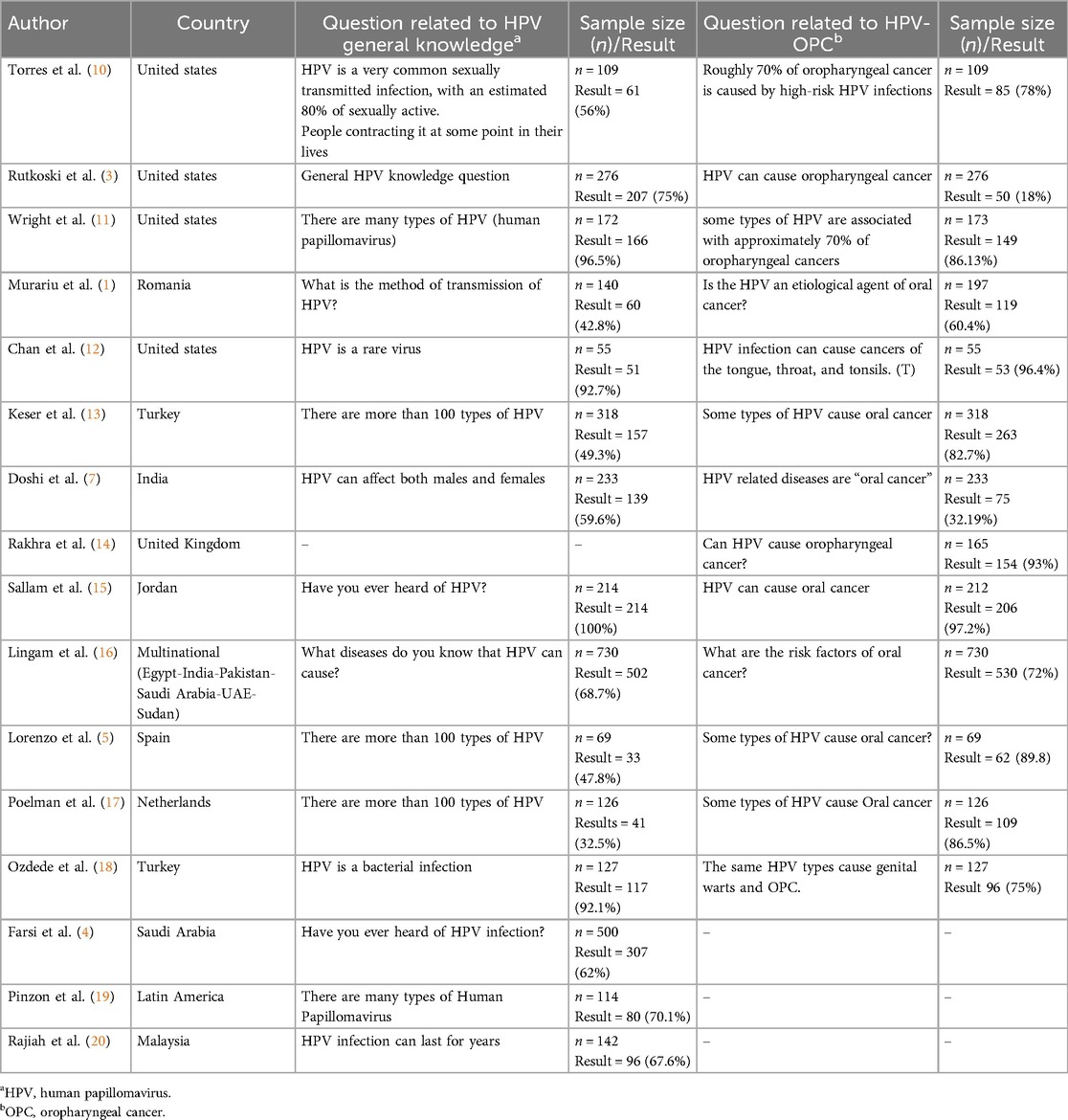
Table 2. Characteristics and Key findings of studies evaluating dental students’ knowledge of human papillomavirus and oropharyngeal cancer.
This review also included six studies from Europe conducted between 2018 and 2022. Four of these studies assessed both HPV knowledge and the relationship between HPV and OPC, while the remaining two focused exclusively on the HPV and OPC relationship. The sample sizes for these studies ranged from 69 to 318 participants. The percentage of HPV knowledge ranged from 32.5% to 49.3%, while awareness of the HPV and OPC connection ranged from 60.4% to 93%.
Furthermore, six studies conducted between 2015 and 2022 from various countries, including those in Asia, Africa, and one in Latin America, were reviewed. Half of these studies assessed both HPV knowledge and the HPV and OPC relationship, whereas the other half focused solely on HPV knowledge. For the studies on HPV knowledge, the sample sizes ranged from 114 to 730 participants, with knowledge levels between 59.16% and 100%. For the studies addressing the HPV and OPC relationship, the sample sizes ranged from 233 to 730 participants, with awareness percentages ranging from 32.19% to 97.2%.
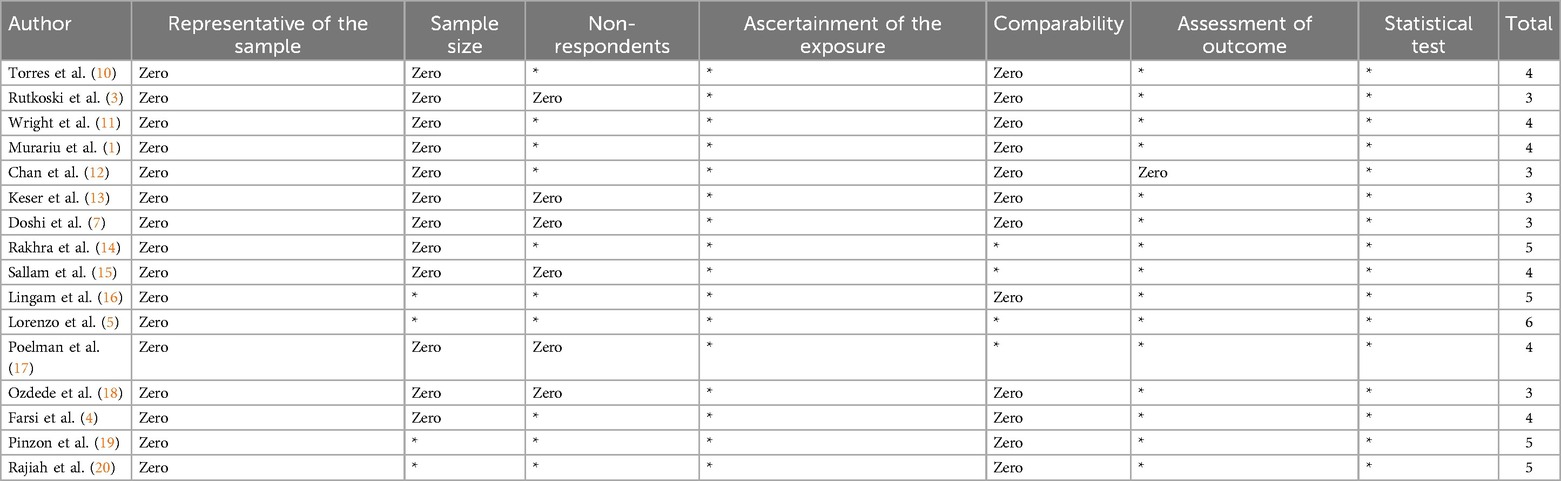
3.3 Quality assessment
Among the 16 articles included in the two meta-analyses, the quality assessment revealed that 11 articles scored 4 or less out of 9 on the NOS scale. Four studies scored 5, and only one study achieved a score of 6. The scores for each study are summarized in Table 3.
3.4 Forest plots
Figure 4 presents a meta-analysis of 15 studies assessing general HPV knowledge among dental students. The findings indicate that 69% of students had general knowledge (95% CI: 0.56–0.81). Due to significant heterogeneity (Q = 646.34, P < 0.001), a random effects model was applied. Figure 5 presents a meta-analysis of 13 studies evaluating HPV-related knowledge specific to oropharyngeal cancer (OPC) among dental students. The results showed that 77% of dental students were aware of the association between HPV and OPC (95% CI: 0.63–0.89). Due to significant heterogeneity (Q = 804.07, P < 0.001), a random effects model was applied.
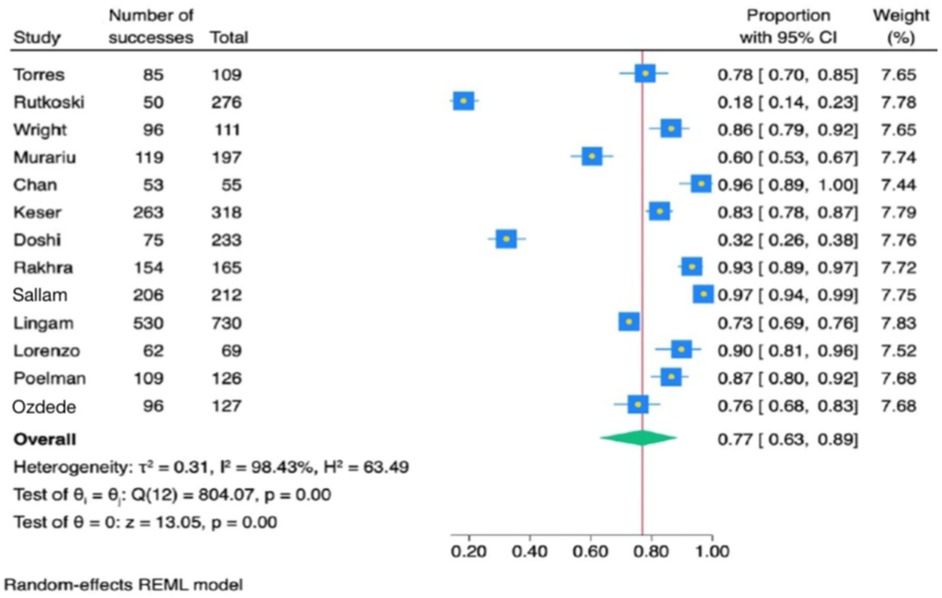
Figure 5. Forest plot diagram of the estimate effect of the association of human papillomavirus and oropharyngeal cancers questions.
4 Discussion
This systematic review and meta-analysis study was conducted to assess the level of knowledge among dental students concerning HPV and its link to OPC. The results showed that dental students had a 69% knowledge level about HPV and a 77% understanding of HPV's association with OPC. However, the previously published systematic review which evaluated awareness of HPV-related oral cancers among both dentists and dental students, found that more than 80% of dental students are aware that HPV can cause OPC (8). Furthermore, over 75% of dentists acknowledge HPV as a causative factor in oral cancer (8). The difference between the findings in our meta-analysis and the previous systematic review might be attributed to the fact that our meta-analysis included only dental students, while the other review included both dentists and dental students. Additionally, the range of questions included in this meta-analysis varied widely. For example, 96% of the dental students chose the correct answer for the statement “There are many types of HPV”, however, knowledge on the mode of HPV transmission was lower, with only 42.8% of responses being correct.
Similarly, geographical differences and the diversity of educational systems globally might have an impact on the results observed in studies assessing dental students' knowledge about HPV and its association with OPC. For instance, in Turkey, only 49% of participants correctly answered a general question about HPV types (13). In Italy, a 47% accuracy for a similar question was reported (5). In contrast, in the United States, 96% of participants correctly identified HPV types (11). Studies conducted in the U.S. generally indicate a higher level of awareness among dental students regarding the connection between HPV and OPC (3, 11). This variation highlighted the influence of geographical location and educational frameworks on students' understanding of critical health issues, emphasizing the need for tailored educational interventions to bridge knowledge gaps worldwide.
The Commission on Dental Accreditation (CODA), which accredits dental education programs in the United States, has implemented a mandatory standard (standard 2.24-part b) (21), requiring graduates to be competent in providing oral health care within the scope of general dentistry, including screening and risk assessment for head and neck cancer (21). Thus, dental schools must develop and update their curricula to meet these national standards. These standards also have the potential to ensure comprehensive dental education that integrates HPV knowledge and enhances early detection of head and neck cancers globally. Integrating a standardized component into dental curricula is essential to ensure that all dental students gain comprehensive knowledge about HPV and learn to apply this knowledge in their clinical practice. This should include training on oral cancer screening, patient education about HPV, and the importance of vaccination. By enhancing both the theoretical and practical aspects of dental education to include thorough information on HPV and its health implications, we can better prepare dental students with the skills and expertise necessary to diagnose, understand, and manage HPV-related conditions effectively in their professional careers (3, 4, 11, 7, 13, 15).
A systematic review assessed healthcare providers' knowledge of HPV, with sample sizes ranging from 172 to 194, revealing that knowledge levels varied between 21% and 84% (22). Comparatively, dental students in this study showed an average knowledge level of 69%, ranging from 56% to 96.5%. Moreover, the review examined the understanding of the link between HPV and oropharyngeal squamous cell carcinoma, noting knowledge levels among providers ranged from 22% to 100%. In contrast, dental students demonstrated an average knowledge level of 77% on questions pertaining to HPV and OPC (3, 4, 11).
While this meta-analysis provides valuable insights into dental students' knowledge of HPV and its association with OPC, it is important to consider several limitations. Primarily, the effect estimates are derived from cross-sectional studies, which inherently carry risks of bias, including selection, information, and recall biases. These biases could compromise the accuracy and applicability of the findings (3, 4). The quality of the included studies was evaluated using the Newcastle-Ottawa Scale (NOS), which revealed low scores on quality indicators (8). Another significant limitation is the representativeness of the study samples; none of the analyzed studies included samples that were fully representative of the target population, thereby limiting the generalizability of the findings to the broader population of dental students (16). Additionally, only four out of the sixteen studies reviewed had sample sizes that were deemed adequate and satisfactory, potentially restricting the validity of the meta-analysis outcomes (19). Most studies in this meta-analysis did not control for confounding factors, which could skew the true effect of the relationship between dental students' knowledge of HPV and its implications for oral health (3, 4). Lastly, it is important to acknowledge that each study used different questions, which may have been perceived differently by participants across studies and countries. This variability in survey instruments and question wording may have contributed to the heterogeneity between studies observed in the meta-analysis. To address this, we employed a random-effects model to account for the heterogeneity.
Given these limitations, the findings of this meta-analysis should be interpreted with caution. Future research should aim to address these limitations by conducting studies with more rigorous designs, larger and more representative samples, and comprehensive controls for confounding variables to provide more reliable and generalizable results (1, 8, 14).
5 Conclusions
This study underscores disparities in HPV-related knowledge across dental student cohorts. While certain students exhibit a robust comprehension of HPV and its clinical ramifications, others display substantial knowledge gaps. These findings underscore the imperative to implement structured educational interventions within dental curricula. Such initiatives are essential to equip future dentists with the requisite proficiency in early detection, prevention, and management of HPV-related oral health conditions.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: N/A.
Author contributions
KA: Writing – original draft, Writing – review & editing. BM: Writing – original draft, Writing – review & editing. WB: Writing – original draft, Writing – review & editing. YB: Writing – original draft, Writing – review & editing. HA: Writing – original draft, Writing – review & editing. HA: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Murariu A, Baciu E-R, Bobu L, Diaconu-Popa D, Zetu I, Gelețu G, et al. Knowledge, practice, and awareness of oral cancer and HPV infection among dental students and residents: a cross-sectional study. Medicina (Kaunas). (2022) 58(6):806. doi: 10.3390/medicina58060806
2. Kumar M, Nanavati R, Modi TG, Dobariya C. Oral cancer: etiology and risk factors. J Cancer Res Ther. (2016) 12(2):458–63. doi: 10.4103/0973-1482.186696
3. Rutkoski H, Tay DL, Dixon BL, Pinzon LM, Mooney R, Winkler JD, et al. A multi-state evaluation of oral health Students’ knowledge of human papillomavirus-related oropharyngeal cancer and HPV vaccination. J Dent Educ. (2020) 35(5):1017–25. doi: 10.1007/s13187-019-01561-y
4. Farsi NJ, Al Sharif S, Al Qathmi M, Merdad M, Marzouki H, Merdad L. Knowledge of human papillomavirus (HPV) and oropharyngeal cancer and acceptability of the HPV vaccine among dental students. Asian Pac J Cancer Prev. (2020) 21(12):3595–603. doi: 10.31557/APJCP.2020.21.12.3595
5. Lorenzo-Pouso AI, Gándara-Vila P, Banga C, Gallas M, Pérez-Sayáns M, García A, et al. Human papillomavirus-related oral cancer: knowledge and awareness among Spanish dental students. J Cancer Educ. (2019) 34(4):782–8. doi: 10.1007/s13187-018-1373-1
6. Clinical dentistry and oral cancer screening. Available at: https://maplespub.com/article/clinical-dentistry-and-oral-cancer-screening (Accessed January 20, 2025).
7. Doshi D, Reddy BS, Karunakar P, Deshpande K. HPV, cervical cancer and pap test related knowledge among a sample of female dental students in India. Asian Pac J Cancer Prev. (2015) 16(13):5415–20. doi: 10.7314/apjcp.2015.16.13.5415
8. Kazeminejad E, Mirzaei F, Ghasemi S, Dashti M, Esmaily M. Knowledge and awareness about HPV-related oral cancer among dentists and dental students: a systematic review. J Oral Health Oral Epidemiol. (2023) 12(1):14–20. doi: 10.34172/johoe.2023.03
9. Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. (2013) 13:1–7.23280303
10. Torres E, Richman A, Wright W, Wu Q. Assessing dental students’ HPV health literacy and intention to engage in HPV-related oropharyngeal cancer prevention. J Cancer Educ. (2022) 37(4):950–6. doi: 10.1007/s13187-020-01905-z
11. Wright M, Pazdernik V, Luebbering C, Davis JM. Dental students’ knowledge and attitudes about human papillomavirus prevention. Vaccines (Basel). (2021) 9(8):888. doi: 10.3390/vaccines9080888
12. Chan WY, Hanano C, Wu Y, Kritz-Silverstein D. Human papillomavirus knowledge and recommendation practices among conference attendees. Pediatr Dent. (2022) 44(3):181–5.35799337
13. Keser G, Yılmaz G, Pekiner FN. Assessment of knowledge level and awareness about human papillomavirus among dental students. J Cancer Educ. (2021) 36(4):664–9. doi: 10.1007/s13187-019-01683-3
14. Rakhra D, Walker TWM, Hall S, Fleming CA, Thomas SJ, Kerai A, et al. Human papillomavirus (HPV) and its vaccine: awareness and opinions of clinical dental students in a UK dental school. Br Dent J. (2018) 225(10):976–81. doi: 10.1038/sj.bdj.2018.1024
15. Sallam M, Al-Fraihat E, Dababseh D, et al. Dental students’ awareness and attitudes toward HPV-related oral cancer: a cross-sectional study at the University of Jordan. BMC Oral Health. (2019) 19:171. doi: 10.1186/s12903-019-0864-8
16. Lingam AS, Koppolu P, Alhussein SA, Abdelrahim RK, Abusalim GS, ElHaddad S, et al. Dental students’ perception, awareness, and knowledge about HPV infection, vaccine, and its association with oral cancer: a multinational study. Infect Drug Resist. (2022) 15:3711–24. doi: 10.2147/IDR.S365715
17. Poelman MR, Brand HS, Forouzanfar T, Daley EM, Jager DHJ. Prevention of HPV-related oral cancer by dentists: assessing the opinion of Dutch dental students. J Cancer Educ. (2018) 33(6):1347–54. doi: 10.1007/s13187-017-1257-9
18. Özdede M, Bağcı N, Gündüz T, Peker İ. Evaluation of knowledge and awareness of dentists and dental students about human papillomavirus vaccination and oropharyngeal cancer relationship. Clin Exp Health Sci. (2020) 10(3):309–15.
19. Pinzon LM, Velazquez A, Rutkoski H, Tay DL, Martel L, Drury C, et al. Cross-cultural adaptation of a Spanish version of a previously validated HPV survey that evaluates dental students’ knowledge, perception, and clinical practices in Latin America. BMC Oral Health. (2022) 22(1):72. doi: 10.1186/s12903-022-02108-2
20. Rajiah K, Maharajan MK, Num F, S K, Koh H, C R. Knowledge about human papillomavirus and cervical cancer: predictors of HPV vaccination among dental students. Asian Pac J Cancer Prev. (2017) 18(6):1573–9. doi: 10.22034/APJCP.2017.18.6.1573
21. Coda accreditation standards [Internet]. Available at: https://coda.ada.org/standards (Accessed January 20, 2025).
Keywords: human papillomavirus, oropharyngeal cancer, dental students, knowledge assessment, HPV-related cancers, HPV awareness, dental education
Citation: Albusairi K, Mandani B, Bouresly W, Brahmbhatt Y, Alqaderi H and Alhazmi H (2025) Knowledge of HPV and its association with oropharyngeal cancer among dental students: a systematic review and meta-analysis. Front. Oral Health 6:1604925. doi: 10.3389/froh.2025.1604925
Received: 2 April 2025; Accepted: 12 May 2025;
Published: 22 May 2025.
Edited by:
Chandrashekar Janakiram, Amrita Vishwa Vidyapeetham University, IndiaReviewed by:
Adrien Boillot, Assistance Publique Hopitaux De Paris, FranceHope M. Amm, University of Alabama at Birmingham, United States
Copyright: © 2025 Albusairi, Mandani, Bouresly, Brahmbhatt, Alqaderi and Alhazmi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hesham Alhazmi, SGFhaGF6bWlAdXF1LmVkdS5zYQ==
 Khaled Albusairi
Khaled Albusairi Badriyah Mandani1
Badriyah Mandani1 Yash Brahmbhatt
Yash Brahmbhatt Hend Alqaderi
Hend Alqaderi Hesham Alhazmi
Hesham Alhazmi