- 1Department of Preventive Dental Science, Dr. Gerald Niznick College of Dentistry, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada
- 2Children’s Hospital Research Institute of Manitoba, Winnipeg, MB, Canada
- 3Department of Pediatrics and Child Health and Department of Community Health Sciences, Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada
- 4Shared Health Inc., Winnipeg, MB, Canada
- 5Department of Oral Biology, Dr. Gerald Niznick College of Dentistry, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada
Introduction: The Interim Canada Dental Benefit (CDB), introduced in 2022, provided financial assistance to families with children <12 years. This study analyzed data from the Canada Revenue Agency (CRA) during the program's entirety.
Methods: Data were accessed from the CRA for applicants and covered both the first (October 1, 2022–June 30, 2023) and second (July 1, 2023–June 30, 2024) periods. Rates of participation and 95% confidence intervals (CIs) were calculated using population data from Statistics Canada. Adjusted rates were calculated based on the proportion of children without private dental insurance, and without private or public insurance.
Results: Over the 21 months of the Interim CDB, 408,240 regular applications were made and $401M distributed to Canadian families. More applications were made during period 1 (P1) than period 2 (P2), but more funding distributed in P2; $197M for 204,270 applications in P1 and $203M for 203,970 applications in P2. Overall, 321,000 children received the Interim CDB in P1 and 328,040 in P2. Provinces with highest rates of child participation included Manitoba, Ontario, Nova Scotia, and Saskatchewan. The highest adjusted rates based on the proportion of children without private or public insurance were Nova Scotia (673.3/1,000, 95% CI: 658.5–688.4 P1 and 717.8/1,000, 95% CI: 702.5–733.3 P2), Northwest Territories (618.4/1,000, 95% CI: 560–681.3 P1 and 573.2/1,000, 95% CI: 517–633.8 P2), and Saskatchewan (495.1/1,000 P1, 95% CI: 486.5–503.7 and 528.3/1,000, 95% CI: 519.5–537.2 P2)
Conclusions: Regions with access to care challenges had higher rates uptake of the Interim CDB when adjusting for the lack of private or public insurance. Findings from this study may help inform policy decisions and reach of the CDCP.
1 Introduction
Oral health is a significant determinant of overall health, yet disparities in dental care access are prevalent across Canada. These disparities are particularly common among children from priority populations who often experience a higher caries prevalence (1). Historically, the Canadian healthcare system did not include dental care (2, 3). Until recently, oral health remained largely outside of Canada's publicly funded healthcare system (4).
The limited public funding in Canada for dental care targets specific groups (4). The federal government provides funding for dental services to specific population groups (e.g., registered First Nations and Inuit Peoples, Canadian Armed Forces) (5). Provincial governments also fund dental care, particularly for low-income children, social welfare recipients, individuals with disabilities, and those with craniofacial disorders (5). Additionally, some municipalities often share costs for dental care for low-income children and social welfare recipients with provinces, and they independently provide care for low-income seniors (5).
Despite these government investments, access to oral health care remains a challenge for many Canadians. Vulnerable groups, including low-income households, children, seniors, Indigenous populations, and individuals with disabilities, face barriers to dental care, such as financial constraints, transportation issues, and limited services in rural and remote regions (6). Statistics show that while three-quarters of Canadians visit a dental professional annually, many still lack consistent access, largely due to cost (7).
The Interim Canada Dental Benefit (CDB), introduced in October 2022, was a critical first step in addressing these access barriers for children under 12 years from low-income families (8, 9). The Interim CDB was implemented as a precursor to the Canadian Dental Care Plan (CDCP), providing eligible families of children <12 years of age with financial support towards their children's dental expenses.
Families earning under $90,000 annually were eligible to receive the Interim CDB for children under 12 years. Families with private insurance or employer-sponsored plans were ineligible. Applicants needed to have filed income taxes for the previous year. However, applicants who received government dental benefits, such as the Non-Insured Health Benefits (for registered First Nations and Inuit Peoples) or Employment and Income Assistance (i.e., social assistance), were also eligible for the Interim CDB if their child's dental expenses were not fully reimbursed. Based on family income, financial support ranged from $260 to $650 per eligible child, with payments managed by the Canada Revenue Agency (CRA) (8–10). The Period 1 (P1) of the Interim CDB covered eligible dental treatment between October 1, 2022, and June 30, 2023, and Period 2 (P2) covered treatment from July 1, 2023, to June 30, 2024.
As the Interim CDB ended June 30, 2024, a new chapter in Canadian dental care began with applications for the CDCP on June 27, 2024. The CDCP, with its expanded coverage to a broader range of uninsured Canadians with family incomes of less than $90,000, represents a significant policy shift towards more inclusive universal dental coverage. This transition is a testament to the continuous improvement and evolution of dental care policy in Canada. The purpose of this study was to analyze aggregated data from the Government of Canada on applications made and accepted during the entire 21 months of the Interim CDB, to evaluate its reach to gain insights into dental care needs and barriers faced by low-income Canadian families.
2 Methods
The study used aggregated data from the CRA regarding approved applications, unique applicants, and total funds distributed from October 2022 to June 2024. Public data were accessed from the Government of Canada Open Data Portal: https://open.canada.ca/data/en/dataset/69035265-2714-4ffa-af3f-fa850209b616 and https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1310092001. Ethics approval was not required as it involved exclusively de-identified aggregated data publicly accessible from the government of Canada. The hypothesis was that Interim CDB uptake would be highest among lower-income families and regions with lower rates of private or public dental insurance coverage.
Data for this study were accessed from the CRA for applicants as of June 30, 2024, and assessed as of July 26, 2024. Data covered the entire first period (October 1, 2022–June 30, 2023) and 12 months of the second period (July 1, 2023–June 30, 2024). Data were segmented into four periods: Period 1 (P1), Period 2 (P2), Additional Period 1 (AP1), and Additional Period 2 (AP2). P1 includes applicants who applied, received the Interim CDB and sought dental care for their child(ren) between October 1, 2022, and June 30, 2023 (16). The P2 data include applicants who had dental treatment, applied, received the benefit, and sought dental care for their child(ren) between July 1, 2023, and June 30, 2024. AP1 data include applicants whose children had dental treatment with costs that exceeded $650 between October 1, 2022 and June 30, 2023. These applicants were eligible to apply and receive an additional $650 within the second pay period but would not be eligible to apply for the P2 of the Interim CDB. AP2 data include applicants who had children whose cost for dental treatment exceeded $650 between July 1, 2023, and June 30, 2024. They qualified to apply and receive an additional $650 within the second period, granted they had not applied for and received the Interim CDB within P1.
The analysis considered provincial/territorial variations, rates of child participation, and family net income distributions. New data for this follow-up also included additional metrics, such as changes in child participation levels and financial trends over the program's lifetime. Descriptive statistics were calculated using Microsoft Excel, with data visualizations highlighting changes across all population segments.
The Canada Dental Benefit file provided the number of applications and the applicant's province/territory of residence. Each unique applicant represented an individual, potentially applying for multiple children. Residence was determined as of the application date. All amounts were rounded to the nearest thousand dollars and counts to the nearest ten.
Rates of children with the Interim CDB per 1,000 were calculated by dividing the number of children with the benefit by the number of Canadians aged 0–11, by province or territory, based on census 2021 data available from Statistics Canada (8, 9, 11). Additionally, we calculated adjusted rates of children without private dental insurance who received the Interim CDB per 1000. Provincial data on the percentage of children 0–17 years with private dental insurance was obtained from the Canadian Oral Health Survey (COHS) 2023–2024: Statistics Canada Table 13-10-0920-01 Selected indicators of dental insurance coverage by age group and gender, released October 23, 2024. This permitted us to calculate the percentage of children 0–17 years in each province without private insurance, which was then used to calculate adjusted rates for the total population of children 0–11 years of age in each province to reflect those without private insurance. Additionally, we determined the percentage of children 0–17 years with private or public dental insurance in each province to calculate adjusted rates for uninsured children 0–11 years (i.e., no private or public insurance). Data on private dental and public insurance for children in the three territories came from the Canadian Health Survey on Children and Youth (CHSCY) 2019, which was used to calculate the adjusted rates among the uninsured. Additionally, 95% confidence intervals (CIs) for rates were calculated using the Medcalc.org online statistical software (https://www.medcalc.org/calc/rate_ci.php). Differences between provinces and territories were likely to exist if there was no overlap of 95% CIs. Maps were generated using MapChart© (https://www.mapchart.net/canada.html).
Lastly, based on published results of Interim CDB applications data for first three quarters of P2, the actual number of applications, number of unique applicants, number of children receiving the benefit and total amount dispersed for the Interim CDB during the entirety of P2 were compared to projected values based on the first 9 months of the program's second year (8).
3 Results
Over the 21 months of the Interim CDB, 452,460 applications were made, and $440.7M was distributed to families. A total of 408,240 were regular applications with $401M dispersed through that route while the remainder of applications were for AP1 and AP2. More applications were made during P1 than P2, but more funding was distributed in P2; $197M for 204,270 applications in P1 and $203M for 203,970 applications in P2. Overall, 321,000 children received the Interim CDB in P1, and 328,040 children received the Interim CDB in P2 (Table 1).
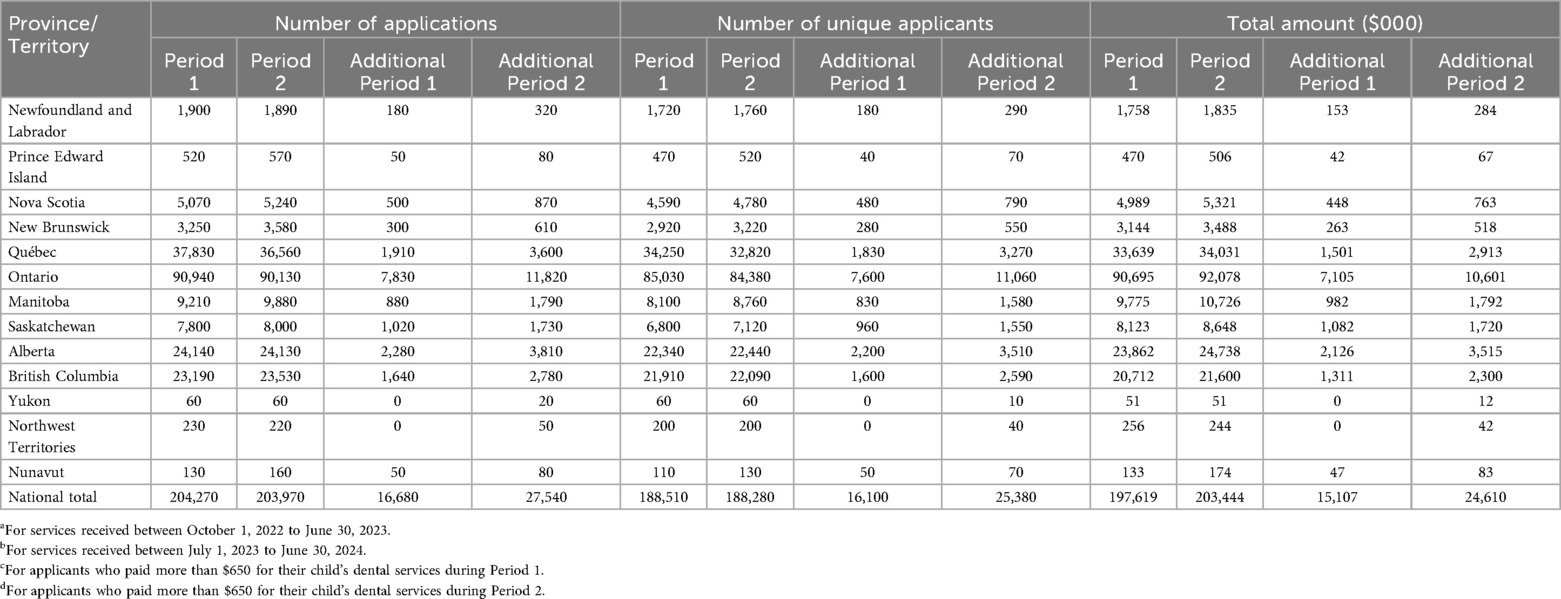
Table 1. Number of approved interim CDB applications, unique applicants, and total amount distributed (in $000) by province/territory during Period 1a, Period 2b, Additional Period 1c, and Additional Period 2d.
Ontario, Quebec, Alberta, and British Columbia had the highest number of approved applications and participants (Table 1), reflecting their larger populations and potentially greater need for dental benefits. Ontario consistently accounted for the most approved applications across all periods, reflecting its population size. The total approved amount was $90.6M and $92.0M for P1 and P2, respectively. Quebec reported a decline in the number of applications between the periods, from 37,830 in P1 to 36,560 in P2, while the amount distributed decreased accordingly. Meanwhile, the fewest applications came from the territories: Yukon, Nunavut, and the Northwest Territories (Table 1).
Data on the number of applications and amount distributed during AP1 and AP2 appear in Table 1. Overall, there were 16,680 applications made for additional funding in P1 and 27,540 in P2, with 24,660 and 39,300 children approved, respectively. The total amount distributed through this additional funding was $15.1M in AP1 and $24.6M in AP2. The majority of additional applications were from residents of Ontario (46.9% in AP1 and 42.9% in AP2) followed by Alberta (9.8% in AP1 and 10.1% in AP2). Similarly, most additional funds dispersed were highest in Ontario (47.0% in AP1 and 43.1% in AP2), followed by Alberta (14.1% in AP1 and 14.3% in AP2). Likewise, of all the children approved for additional funding, most were from Ontario (46.8% in AP1 and 42.8% in AP2), followed by Alberta (14.2% in AP1 and 14.4% in AP2).
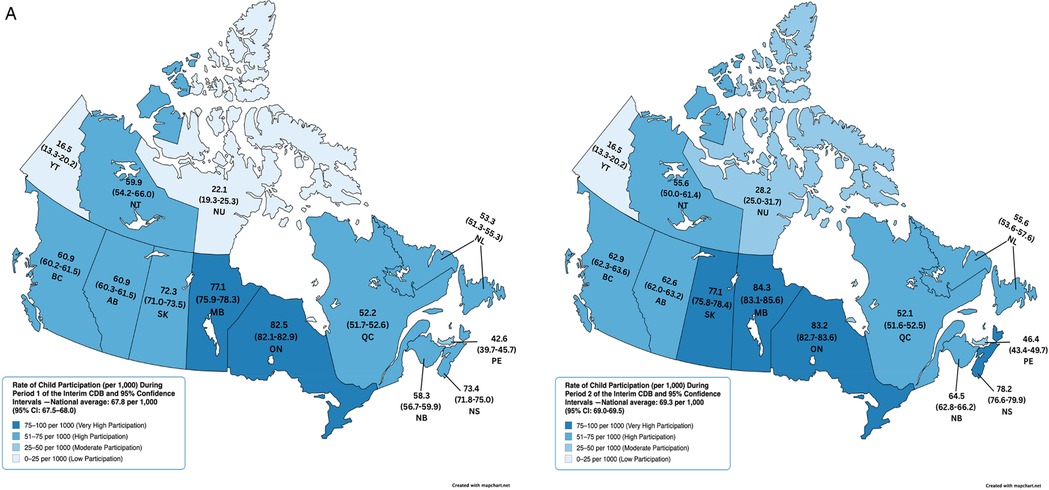
Table 2 reports the number of children receiving the Interim CDB and the rate of child participation by province and territory during P1, P2, AP1, and AP2. Provinces with the highest rates of child participation included Ontario, Manitoba, Nova Scotia, and Saskatchewan (Figure 1A). Interestingly, three of these provinces demonstrated an increase in rates from P1 to P2: Manitoba (77.1/1,000, 95% CI: 75.9–78.3 in P1 and 84.3/1000 95% CI: 83.1–85.6 in P2), Nova Scotia (73.4/1,000, 95% CI: 71.8–75.0 in P1 and 78.2/1000 95% CI: 76.6–79.9 in P2), and Saskatchewan (72.3/1,000, 95% CI: 71.0–73.5 in P1 and 77.1/1000 95% CI: 75.8–78.4 in P2) (Table 2 and Figure 1A).
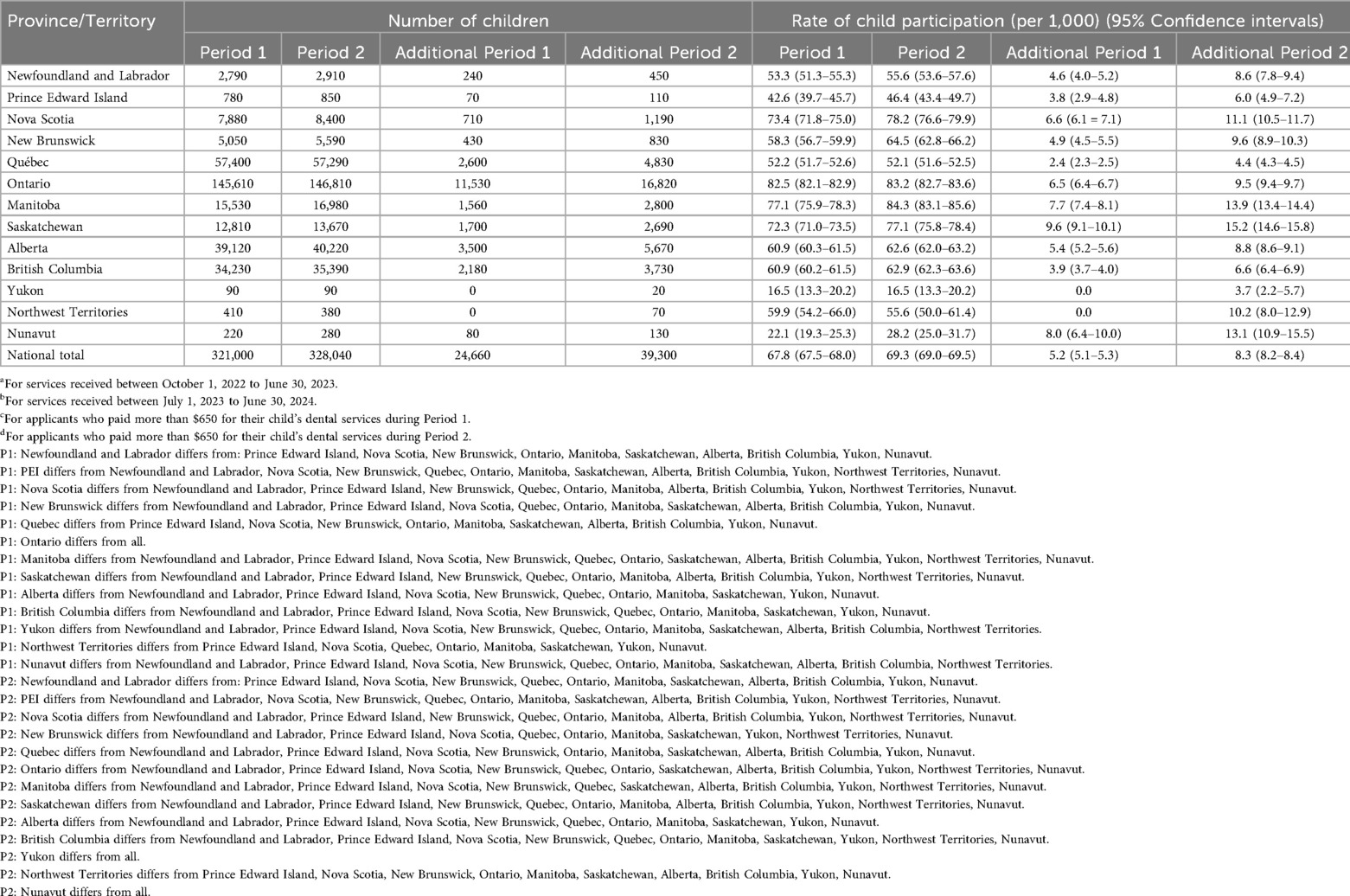
Table 2. Number of approved interim CDB children and rate of child participation by province/territory during the Period 1a, Period 2b, Additional Period 1c, and Additional Period 2d.
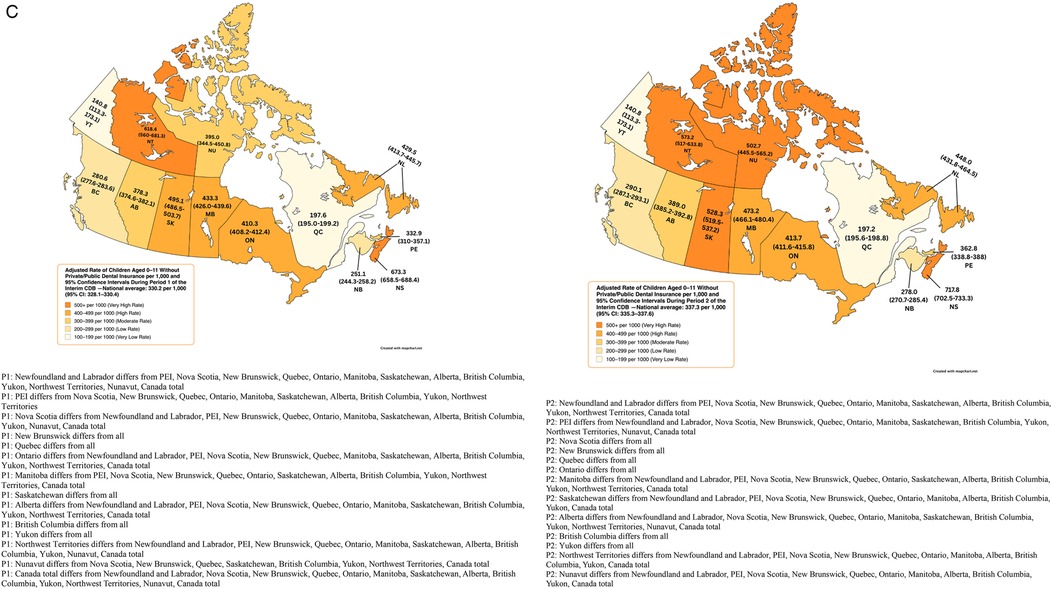
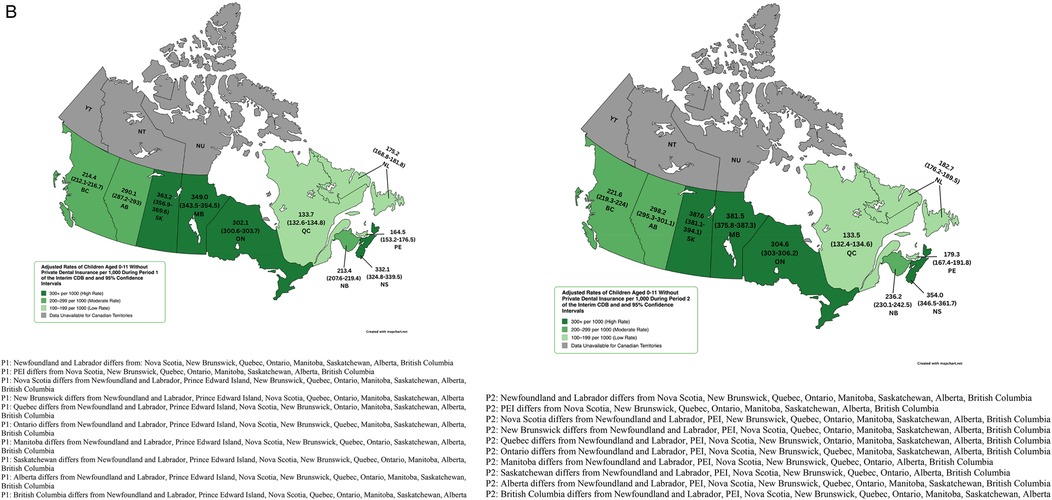
Figure 1. (A) Rate of child participation (per 1,000) during period 1 and 2 of the interim CDB and 95% confidence intervals. (B) Adjusted rates of children aged 0–11 without Private Dental Insurance per 1,000 During Period 1 and 2 of the Interim CDB and 95% Confidence Intervals. (C) Adjusted Rate of Children Aged 0–11 Without Private/Public Dental Insurance per 1,000 and 95% Confidence Intervals During Period 1 and 2 of the Interim CDB.
Adjusted rates of child participation limited to those without private dental insurance (obtained from the Canadian Oral Health Survey) revealed that Saskatchewan (363.2/1,000, 95% CI: 356.9–369.6) had the highest uptake in P1, followed by Manitoba (349.0/1,000, 95% CI: 343.5–354.5), Nova Scotia (332.1/1,000, 95% CI: 324.8–339.5), and Ontario (302.1/1,000, 95% CI: 300.6–303.7) (Figure 1B). Adjusted rates in P2 were higher; Saskatchewan (387.6/1,000, 95% CI: 381.1–394.1), Manitoba (381.5/1,000, 95% CI: 375.8–387.3), Nova Scotia (354.0/1,000, 95% CI: 346.5–361.7), and Ontario (304.6/1,000, 95% CI: 303–306.2) (Figure 1B).
Adjusted rates of participation among those without private or public dental insurance (obtained from the Canadian Oral Health Survey for provinces and from the Canadian Health Survey on Children and Youth (CHSCY) 2019 for territories) revealed that the Canadian average rate of uptake was 330.2/1,000 (95% CI: 328.1–330.4) in P1 and 337.3/1,000 (95% CI: 335.3–337.6) in P2. Nova Scotia had the highest uptake rate in P1 (673.3/1,000, 95% CI: 658.5–688.4) followed by the Northwest Territories (618.4/1,000, 95% CI: 560–681.3), Saskatchewan (495.1/1,000, 95% CI: 486.5–503.7), Manitoba (433.3/1,000, 95% CI: 426.0–439.6), and Newfoundland and Labrador (429.5/1,000, 95% CI: 413.7–445.7) (Figure 1C). Six provinces saw an increase in the rate of uninsured children receiving the Interim CDB from P1 to P2 (Nova Scotia, New Brunswick, Manitoba, Saskatchewan, Alberta, and British Columbia). Nova Scotia had the highest rate of uptake among uninsured children in P2 (717.8/1,000, 95% CI: 702.5–733.3), followed by the Northwest Territories (573.2/1,000, 95% CI: 517–633.8), Saskatchewan (528.3/1,000, 95% CI: 519.5–537.2), Nunavut (502.7/1,000, 95% CI: 445.5–565.2), and Manitoba (473.7/1,000, 95% CI: 466.1–480.4) (Figure 1C). Yukon on Quebec had the lowest adjusted rates of participation (Figure 1C).
Adjusted rates and 95% CIs for those without private or public dental insurance appeared to differ between some provinces and territories (Figure 1C). For instance, Nova Scotia differed from Newfoundland and Labrador, PEI, New Brunswick, Quebec, Ontario, Manitoba, Saskatchewan, Alberta, British Columbia, Yukon, Nunavut, and the Canadian total in P1 and from all provinces and territories in P2. Adjusted rates for the Northwest Territories differed from Newfoundland and Labrador, PEI, New Brunswick, Quebec, Ontario, Manitoba, Saskatchewan, Alberta, British Columbia, Yukon, Nunavut, and the Canadian total in P1. In P2, adjusted rates for the Northwest Territories differed from Newfoundland and Labrador, PEI, Nova Scotia, New Brunswick, Quebec, Ontario, Manitoba, Alberta, British Columbia, Yukon, and the Canadian total. Meanwhile, Saskatchewan differed from all other provinces or territories in P1 and all except for the Northwest Territories and Nunavut in P2. In both periods, adjusted rates among those without private or public dental insurance differed from all other provinces and territories.
Rates of child participation for the additional funding streams, AP1 and AP2 were also calculated (Table 2). Saskatchewan (9.6/1,000, 95% CI: 9.1–10.1 in AP1 and 15.2/1,000, 95% CI: 14.6–15.8 in AP2), Manitoba (7.7/1,000, 95% CI: 7.4–8.1 in AP1 and 13.9/1,000, 95% CI: 13.4–14.4 in AP2), Nunavut (8.0/1,000, 95% CI: 6.4–10.0 in AP1 and 13.1/1,000, 95% CI: 10.9–15.8 in AP2), and Nova Scotia (6.6/1,000, 95% CI: 6.1–7,1 in AP1 and 11.1/1,000, 95% CI: 10.5–11.7 in AP2) had the highest rates of applications for additional funding to cover the costs of their children's dental care.
Figure 2 presents the distribution of children approved along with the total funds dispersed for the various periods according to age of the child. The greatest number of children with the Interim CDB in P1 and P2 were among those six years of age, while the highest amounts dispersed were to those five years of age and above (Figure 2A). The number of infants who received the Interim CDB increased from P1 to P2; 19.8% increase among those <12 months of age (11,730–14,620) and 7.1% increase among one-year olds. There was also a 5.4% and 4.9% increase among two- and three-year-olds, respectively. Similarly, there was an increase in the amount of funding dispersed from P1 to P2 among infants; 20.1% increase among those <12 months of age ($7,386M to $9.245M) and 8.6% increase among one-year olds ($11.7M to $12.7M). There was also a 5.8% and 5.5% increase among two- and three-year-olds, respectively. Meanwhile, there was a 4.7% decrease in the number of 11-year-olds who received the Interim CDB in P2 than in P1 (28,230–26,910) and a 4.2% decrease in the amount of funding provided to 11-year-olds ($17.2M to $16.5M). Figure 2B presents the distribution of the number of children approved and the total funds dispersed during AP1 and AP2. Overall, there was a 59.4% increase in the total number of approved children, rising from 24,660 in AP1 to 39,300 in AP2. Similarly, the total funding dispersed increased by 62.9%, from $15.1M to $24.6M. This upward trend was generally consistent across most age groups. However, there was a 51.1% decrease in the number of 11-year-olds approved (5,420 in AP1 to 2,650 in AP2). Additionally, the total funding for this age group declined from $3.4M to $1.6M.
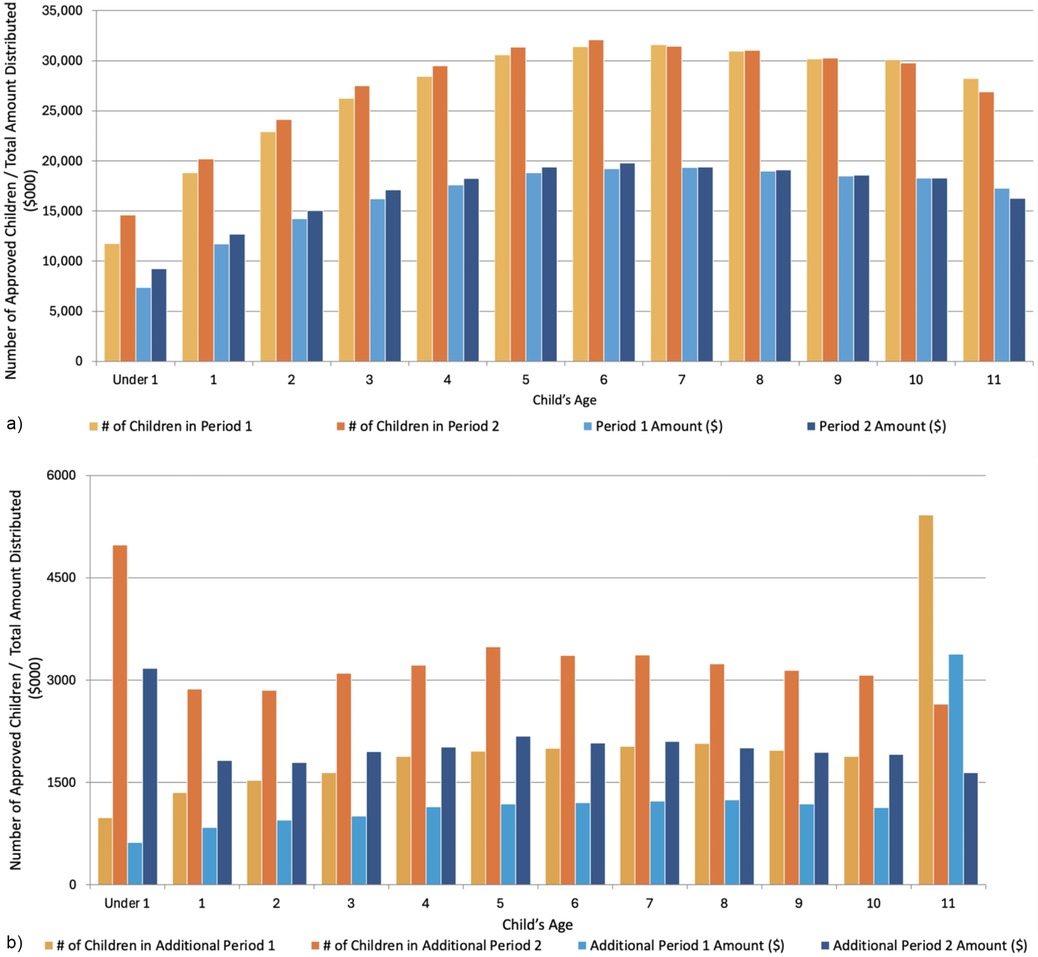
Figure 2. Total number of approved children and total amount distributed (in $000) during period 1, period 2, additional period 1, and additional period 2 of the interim CDB. (a) Number of approved children and total amount distributed ($000) by age during Period 1 and Period 2 of the interim CDB. (b) Number of approved children and total amount distributed ($000) by age during Period 1 and Period 2 of the interim CDB.
Table 3 reports the number of approved Interim CDB applications, unique applicants, children, and the total amount (in $000) by adjusted annual net family income during P1, P2, AP1, and AP2. In P1, 46.9% of approved children came from families with adjusted net incomes <$30,000. 44.5% were from families earning between $30,000 and $69,999, and only 8.9% were from families earning ≥$70,000. During P2, the percentage of children from lower-income families (<$30,000) increased to 55.2%, while 37.6% were from families earning between $30,000 and $69,999, and 7.4% were from families earning ≥$70,000. More than half of children (51.8%) approved in AP1 were from households earning <$30,000, which increased to 63.5% during AP2.
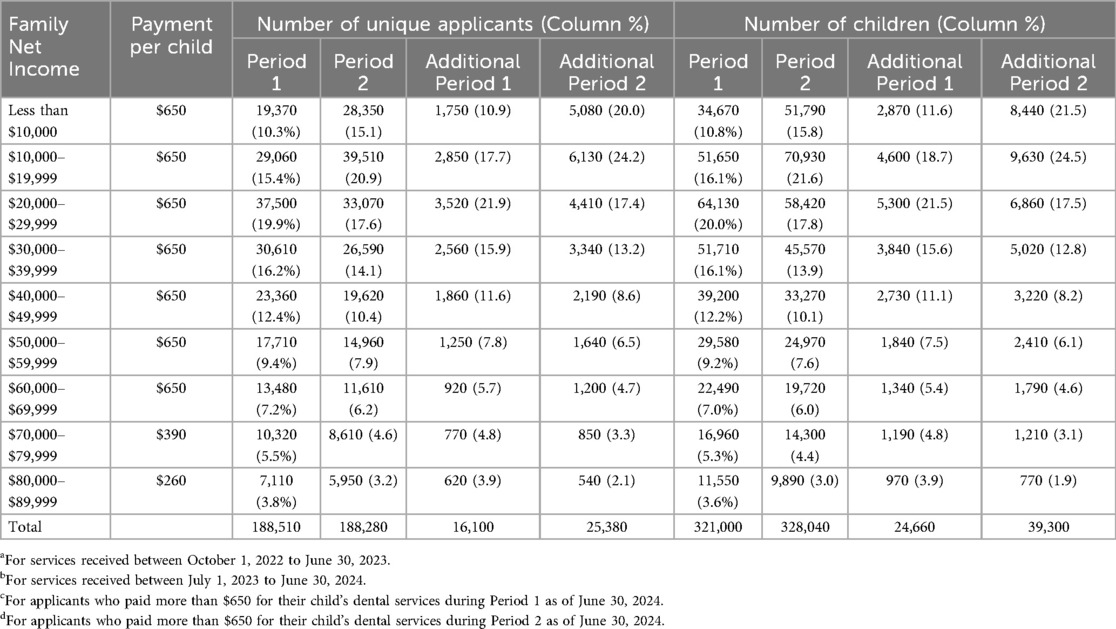
Table 3. Number of approved interim CDB applications, unique applicants, children, and total amount (in $000) by adjusted net family income during Period 1a, 2b, Additional Period 1c, and Additional Period 2d.
Information on the age grouping and place of residence of applicants appears in Table 4. The total number of applicants remained stable over the two periods, with 188,510 in P1 and 188,280 in P2 although P1 only consisted of 9 months while P2 was a 12-month span. Most approved applicants belonged to the 25–34 year old (36.5% P1 and 38.6% P2) and 35–44 year old (47.2% P1 and 46.1% P2) groups. This distribution was exhibited in all the provinces and territories. For example, in Ontario, 36.6% of parents in P1 were aged 25–34, increasing to 38.4% in P2, while those aged 35–44 accounted for 47.4% and 46.6%, respectively. In contrast, individuals <25 and those aged ≥65 made up a minimal portion of applicants. For instance, in Newfoundland and Labrador, those under 25 comprised 6.4% in P1 and 5.1% in P2, while those aged 65 and older represented less than 1% across most provinces.
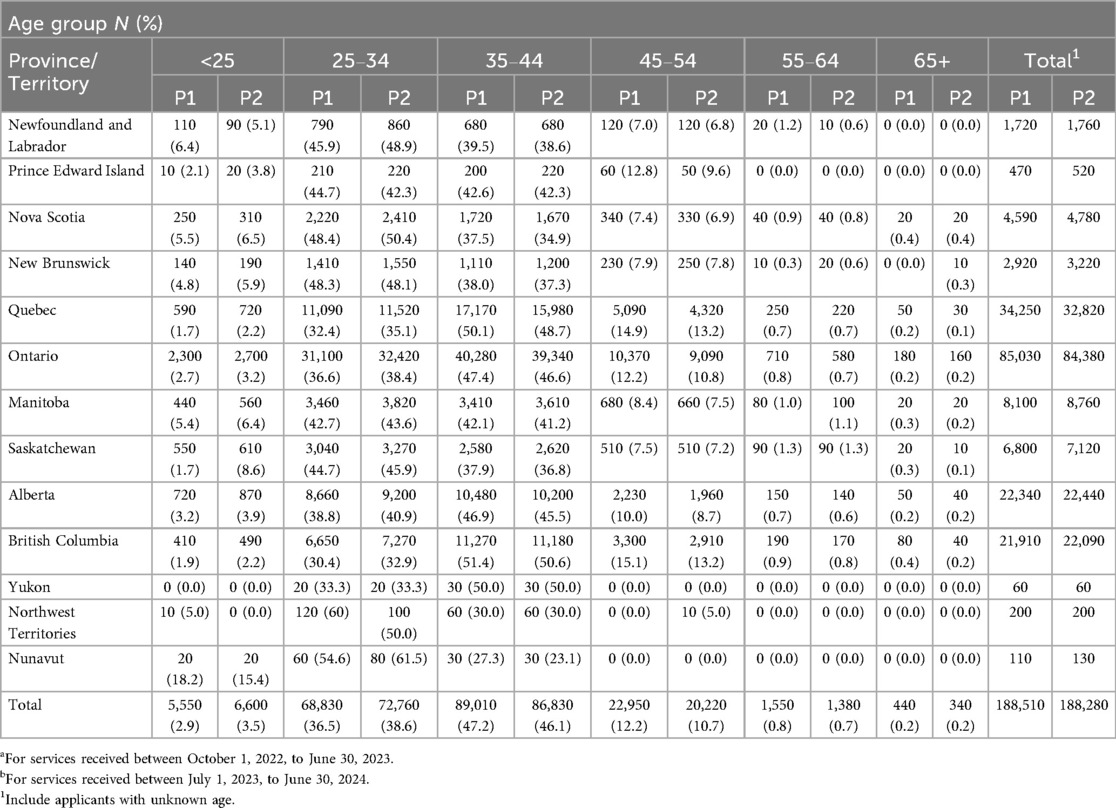
Table 4. Number of approved interim CDB unique applicants by province and territory, and age group during the Period 1a and Period 2b.
The actual number of applications, number of unique applicants, number of children receiving the benefit and total amount dispersed for the Interim CDB during the entirety of P2 were compared to projected values based on the first 9 months of the program's second year (8). Overall, the actual number of applications and unique applicants at the end of P2 fell short of projections (Table 5), with 26,910 fewer applications and 26,747 fewer unique applicants. Similarly, 48,133 fewer children received the Interim CDB and $30.4M less dispersed than projected in P2.
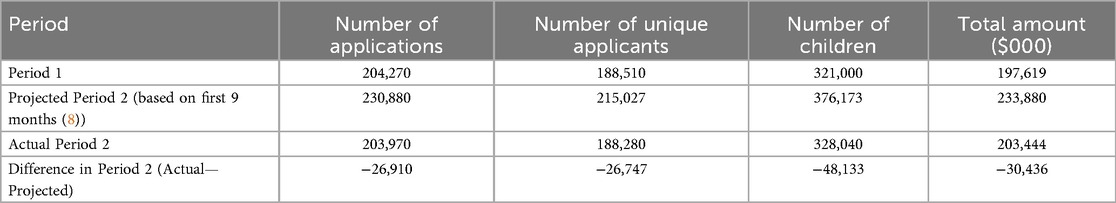
Table 5. Total number of approved interim CDB applications, unique applicants, number of children, and total amount distributed (in $000) during the period 1, and period 2, additional period 1, and additional period 2 (October 1, 2022 to June 30, 2024).
4 Discussion
The Interim CDB was a temporary program providing financial relief to cover dental expenses for children <12 years of age while the federal government planned the new CDCP. Our analyses of aggregate data for the entirety of the program reveals several key insights into the program's uptake and impact on accessibility for dental care. As reported in our publications on the first 9 and 18 months of the program (8, 9), significant regional and socio-economic variability exist, highlighting successes and areas for further improvement.
Ontario, Quebec, Alberta, and British Columbia had the highest number of approved applications, reflecting their population sizes and potentially greater socio-economic challenges. To control for the size differences in provinces and territories, rates of child participation were calculated to facilitate comparisons between provinces and territories. Those provinces and territories with the highest unadjusted uptake rates during the entirety of the Interim CDB included Manitoba, Ontario, Nova Scotia, and Saskatchewan, which confirms what we reported after reviewing data after the first 9 and 18 months of the program (8, 9). The higher participation in Manitoba and Saskatchewan may be due to reported poorer access to dental services as compared to other provinces (8, 12). These two provinces were identified as having more notable access to oral health care challenges according to national surveys (13).
After adjusting for the lack of private or public insurance, two provinces and one territory had the highest rates in both P1 and P2, namely Nova Scotia, Northwest Territories, and Saskatchewan. Manitoba also had higher rates of uptake than the other remaining provinces and territories. Rates in Nova Scotia, the Northwest Territories, and Saskatchewan were 2.0 times, 1.8 times, and 1.5 times the Canadian average, respectively. Uptake rates also increased in Nunavut from P1 (395.0/1,000) to P2 (502.7/1,000) suggesting that targeted outreach efforts may have contributed to enhanced access in more remote locations. The high rates from Nova Scotia were surprising considering that the province has a legislated children's dental public health program (14). However, the high rates of uptake from the Northwest Territories, Saskatchewan, and Manitoba may be attributed to the absence of provincial or territorial dental programs for children (14). According to data provided by Statistics Canada for this study, the estimated proportion of children 0–17 years of age without private and/or public dental insurance is 10.9% in Nova Scotia, 9.7% in the Northwest Territories, 14.6% in Saskatchewan, and 17.8% in Manitoba. Quebec and Yukon had the lowest uptake rates, 3.4 and 4.7 times lower than Nova Scotia's and 1.7 and 2.4 times lower than the Canadian average after adjusting for uninsured children. Both regions offer public dental health programs for children (14). Data provided by Statistics Canada for this study reveal provincial and territorial differences in private and public insurance coverage among children aged 0–17. For instance, only 73.6% of children in Quebec had private and/or public dental insurance while over 85% or more of the pediatric populations in Saskatchewan, Yukon, Nova Scotia, Northwest Territories, and Nunavut had private or public dental insurance. This proportion of children with private and/or public dental coverage was also below 80% in New Brunswick, British Columbia, and Ontario. Quebec's lower uptake rates were surprising and may signify potential challenges in awareness or accessibility along with the potential need for improved dialogue and cooperation between the federal and provincial governments in the oral health realm.
Income levels significantly influenced the uptake of the Interim CDB. Overall, as family income increased, the number of applicants fell sharply revealing that the Interim CDB primarily supported lower-income families. Families earning less than <$30,000 represented the majority of approved applicants across all periods, with participation increasing over time. Conversely, participation among high-income families ($70,000+) was consistently lower, indicating that the Interim CDB primarily supported those with the greatest need. However, lower uptake among higher-income families may also point to a perceived lack of necessity for the benefit among these groups. It raises an important question of whether families in this income bracket require government support for dental care.
Overall, the number of approved applications remained stable between P1 and P2, indicating steady demand for the Interim CDB. Regional shifts were evident, with Ontario and Quebec reporting the highest participation but a slight decline in Quebec from 18.2% in P1 to 17.4% in P2. The steady distribution amounts between periods highlight consistent support provided to families across Canada. One unique finding was the spike in AP2 for children under 1 year, as the number of children under one who received the AP2 payment for the Interim CDB is slightly higher than other age groups. Infant dental care is often more preventative than curative. It does not result in inordinately higher expenses—the most likely explanation is that children eligible for the benefit could only receive a maximum of two payments. Many children <1 year would not have qualified for either the P1 or AP1 payments, increasing the likelihood of them applying for the AP2 additional payment to receive their maximum of two payments. For older children who had the option of receiving a P1 payment, there would be a reduced likelihood of applying for a P2 additional payment, as they were more likely to have exhausted the maximum number of payments before getting to AP2. Legislatively, children under 1 were eligible for the P2 additional if they met the other criteria. It appears that many young children in Canada may have benefited from the Interim CDB. The encouraging uptake of the intervention among parents with infants indicates early progress in improving oral health outcomes and may represent an important step toward reducing the burden of early childhood caries in Canada.
The discrepancies between projected and actual numbers of children and funds distributed in the second year of the Interim CDB underline significant policy implications. Actual applications, unique applicants, children receiving benefits, and total funds dispersed during P2 fell short of projections based on data from the first 18 months of the program (8). This is most likely because the new CDCP was being promoted for children under 18 years during the final quarter of the Interim CDB, leading parents to possibly wait to apply for CDCP instead. The fact that the actual figures for AP2 exceeded projections suggests a higher-than-expected demand for the benefit. This emphasizes the need for adaptive funding policies that effectively respond to fluctuating needs. Lower participation rates among higher-income families suggests a lack of awareness. Targeted campaigns could help ensure that all eligible families are informed about and can access the available support. Higher-income families are often more likely to possess employer-based dental benefits, resulting in eligibility disqualifications. The program might have been less relevant for wealthier households with needs beyond the plan, such as orthodontic services.
The limited nature of the data accessible through the CRA's data portal prevented any further analysis on the potential influence of sociodemographic factors and geography on uptake of the Interim CDB by Canadian families. Due to the nature of data available on the Interim CDB, this study's limitations include a lack of specific insights on overarching trends and broad utilization due to high aggregation and low dataset granularity. Specifically, within-province inequities may stem from urban/rural differences in dental networks, Interim CDB program enrolment, and accessibility for remote populations. Further, based on the limited data provided, there was no ability to look at urban/rural differences in uptake of the Interim CDB in each province or territory.
The two time periods being investigated were not of the same lengths with period 1 only being nine months and period 2 was a full 12 months, limiting statistical comparisons between the periods. Since the Interim CDB was a benefit paid to families, no data exist on dental treatments provided to children, their costs, and reimbursement details, which limits a deeper understanding of the benefit's impact. Participation rates were calculated from the under–12 population using the 2021 census. Migration and differing fertility rates over the subsequent three years may have influenced the analysis. Insurance coverage rates were calculated specifically for children aged 0–11 based on data originally collected for children aged 0–17. Thus, assuming a uniform distribution of insurance coverage across these age groups may have introduced inaccuracies. Data from the COHS 2023–2024 and CHSCY 2019 permitted the calculation of adjusted rates of uptake of the Interim CDB for those without private and public dental insurance. Considering these population surveys were completed at different timepoints may have resulted in some over or underestimation of the true status of dental insurance for children in some provinces and territories. Actual coverage rates for younger children may have differed from these estimates, potentially affecting the precision of the analyses. However, the use of these COHS and CHSCY data sets was recommended following consultation and engagement with Health Canada's Oral Health Branch overseeing the implementation and evaluation of the Interim CDB, whose staff are knowledge users on our evaluation research studies.
Now that the Interim CDB has sunset, policy-makers responsible for implementation and administration of the CDCP need to consider whether the families who are in greatest need of improved access to oral health care are in fact applying for and receiving the benefit. Promotional materials about the CDCP along with community engagement activities should specifically target those residing in rural and remote regions of the country, First Nations, Métis, and Inuit Peoples of Canada, those living in poverty, and those with language barriers. They must also ensure that aggregated data made available to researchers is stratified by area of residence (e.g., residing in rural, remote and urban areas) to evaluate whether the uptake of the new program is equitable.
5 Conclusion
The Interim Canada Dental Benefit (CDB) has increased dental care access for low-income families with children under 12, particularly in high-need areas. However, uptake disparities persist across regions, income levels, and age groups, necessitating further interventions. Enhancing accessibility and tailoring strategies to regional needs will be vital for equitable distribution. Building on this, the CDCP aims to expand coverage for up to nine million uninsured Canadians, easing financial barriers and reducing disparities for vulnerable groups (14). These initiatives mark a significant shift in Canada's dental health policy, targeting underserved communities with critical funding. Ensuring resources meet increased demand, particularly in underserved areas and during benefit periods, is essential for the program's effectiveness and reach.
Data availability statement
The original data utilized for this study were accessed from the links provided in the Methods section. Further inquiries can be directed to the corresponding author.
Author contributions
RS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. CY: Writing – original draft, Writing – review & editing, Formal analysis, Visualization. VC: Writing – original draft, Writing – review & editing. OO: Formal analysis, Writing – original draft, Writing – review & editing. VL: Formal analysis, Writing – original draft, Writing – review & editing. SG: Formal analysis, Writing – original draft, Writing – review & editing. EK: Writing – original draft, Writing – review & editing. AM: Conceptualization, Investigation, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Operating funds for this study were provided by RS's Canadian Institutes of Health Research Applied Public Health Chair Award in “Public Health Approaches to Improve Access to Oral Health Care and Oral Health Status for Young Children in Canada (Application Number #516947; Competition Number 202310CH4; Funding Reference Number CH4 192589)”.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Allison PJ. Canada’s oral health and dental care inequalities and the Canadian Dental Care Plan. Can J Public Health (2023) 114(4):530–33. doi: 10.17269/s41997-023-00800-6
2. Menon A, Schroth RJ, Hai-Santiago K, Yerex K, Bertone M. The Canadian Dental Care Plan and the senior population. Front Oral Health. (2024) 5:1385482. doi: 10.3389/froh.2024.1385482
3. Martin D, Miller AP, Quesnel-Vallée A, Caron NR, Vissandjée B, Marchildon GP. Canada’s universal health-care system: achieving its potential. Lancet. (2018) 391(10131):1718–35. doi: 10.1016/S0140-6736(18)30181-8
4. Levy BB, Goodman J, Eskander A. Oral healthcare disparities in Canada: filling in the gaps. Can Public Health. (2023) 114(1):139–45. doi: 10.17269/s41997-022-00692-y
5. Quinonez C. Why was dental care excluded from Canadian medicare? NCOHR Work Pap Ser. (2013) (1(1)):1–5. Available online at: http://ncohr-rcrsb.ca/knowledge-sharing/working-paper-series/content/quinonez.pdf
6. FDI World Dental Federation. Access to oral healthcare for vulnerable and underserved populations: adopted by the general assembly: September 2019, San Francisco, United States of America. Int Dent J. (2020) 70(1):15–6. doi: 10.1111/idj.12556
7. Statistics Canada. More than one-third of Canadians reported they had not visited a dental professional in the previous 12 months, 2022. The Daily (2023). Available online at: https://www150.statcan.gc.ca/n1/en/daily-quotidien/231106/dq231106a-eng.pdf?st=gIrSZjLD
8. Goubran S, Cruz de Jesus V, Menon A, Olatosi OO, Schroth RJ. Uptake of the interim Canada dental benefit: an investigation of data from the first 18 months of the program. Front Oral Health. (2024) 5:1481423. doi: 10.3389/froh.2024.1481423
9. Schroth RJ, Cruz de Jesus V, Menon A, Olatosi OO, Lee VH, Yerex K, et al. An investigation of data from the first year of the interim Canada dental benefit for children <12 years of age. Front Oral Health. (2023) 4:1328491. doi: 10.3389/froh.2023.1328491
10. Nadeau M. Helping create health smiles across Canada. Learn more about the Canada dental benefit and the upcoming Canadian Dental Care Plan. CDA Essentials. (2023) 10(5):2. Available online at: https://www.cda-adc.ca/en/services/essentials/2023/issue5/8/
11. Statistics Canada. Table 98-10-0020-01. In: Canada S, editor. Age (in Single Years), Average age and Median age and Gender: Canada, Provinces and Territories, Census Metropolitan Areas and Census Agglomerations with Parts. Ottawa: Statistics Canada (2021).
12. Menon A, Cruz de Jesus V, Virtanen JI, Schroth RJ. Parents’ views on access to dental care and the interim Canada dental benefit. JDR Clin Trans Res. (2025):23800844251323169. doi: 10.1177/23800844251323169
13. Health Canada. Canada Dental Benefit Baseline Survey. Final Report. Ottawa: Health Canada (2023).
Keywords: insurance dental, oral health, health policy, public health dentistry, access to care, universal health care
Citation: Schroth RJ, Youssef C, Cruz de Jesus V, Olatosi OO, Lee VHK, Goubran S, Khan E and Menon A (2025) An investigation of the reach of the interim Canada dental benefit for children under 12 years of age. Front. Oral Health 6:1611815. doi: 10.3389/froh.2025.1611815
Received: 14 April 2025; Accepted: 10 September 2025;
Published: 1 October 2025.
Edited by:
Alex Douglas McMahon, University of Glasgow, United KingdomReviewed by:
Raghad Obeidat, Texas A&M University, United StatesAmin Vahdati, The University of Manchester, United Kingdom
Copyright: © 2025 Schroth, Youssef, Cruz de Jesus, Olatosi, Lee, Goubran, Khan and Menon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Robert J. Schroth, cm9iZXJ0LnNjaHJvdGhAdW1hbml0b2JhLmNh
 Robert J. Schroth
Robert J. Schroth Carol Youssef
Carol Youssef Vivianne Cruz de Jesus
Vivianne Cruz de Jesus Olubukola O. Olatosi
Olubukola O. Olatosi Victor H. K. Lee1,2
Victor H. K. Lee1,2 Saif Goubran
Saif Goubran Eefa Khan
Eefa Khan Anil Menon
Anil Menon