- 1Department of Public Health, North South University, Dhaka, Bangladesh
- 2Department of Health Research Methods, Evidence, and Impact, McMaster University, Hamilton, ON, Canada
- 3Refugee Crisis Foundation, London, United Kingdom
- 4College of Health Sciences, University of Sharjah, Sharjah, United Arab Emirates
Background: Individuals with severe mental illness (SMI) experience significantly higher rates of poor oral health, including dental caries, periodontal disease, and edentulism, compared to the general population. This meta-synthesis investigates the challenges faced by individuals with SMI in managing oral health and potential solutions.
Methods: A comprehensive literature search (2010–2024) was conducted across PubMed, Web of Science, Scopus, and Google Scholar for any-language studies. The meta-synthesis involved systematic article selection, quality appraisal, and thematic data extraction/synthesis.
Results: From 1,698 records, 101 full-text articles were reviewed; 11 met the inclusion criteria. Findings consistently demonstrate a high prevalence of poor oral health outcomes (caries, tooth loss, periodontal disease) among individuals with SMI, alongside significantly lower engagement in oral hygiene (e.g., toothbrushing) and dental care-seeking behaviours. Key barriers include financial constraints, dental anxiety, medication side effects (notably xerostomia), and low oral health awareness. Stigma and inadequate dental professional training in mental health further impede access. Proposed solutions emphasise integrating oral health education into psychiatric rehabilitation, enhancing communication between dental and mental health providers, and developing tailored support systems. Evidence suggests a bidirectional relationship between oral and mental health.
Conclusion: This meta-synthesis confirms a stark oral health disparity for individuals with SMI, driven by suboptimal hygiene, medication effects, limited health literacy, and formidable access barriers compounded by financial hardship and stigma. Addressing this requires urgent, coordinated integration of mental and oral healthcare through co-located services, interdisciplinary collaboration, and tailored interventions. Future research must prioritise quantitative studies to elucidate causal pathways and long-term impacts, rigorously examining the roles of gender, geography, environment, and comorbidities. Bridging this divide is an essential public health imperative demanding systemic reform.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024516535, identifier PROSPERO [CRD42024516535].
Introduction
Mental illness significantly impacts oral health, creating a complex interplay between psychological and physical well-being. Individuals with mental disorders often experience poor oral health, which can exacerbate their overall health challenges (1, 2). People living with mental illnesses often face unique barriers to accessing and maintaining adequate oral health, resulting in disproportionately higher rates of oral diseases compared to the general population (3). These challenges are multifaceted, stemming from factors such as medication side effects, cognitive impairments, socioeconomic disparities, and stigmatization within healthcare systems (3, 4).
Mental illness encompasses a wide range of psychological conditions that affect how individuals think, feel, and behave, often leading to significant challenges in daily functioning and overall well-being. Globally, mental health disorders are highly prevalent, with conditions such as anxiety and depression affecting millions each year and contributing to substantial economic and social burdens (5, 6). For instance, it is estimated that mental illnesses account for 7.4% of disability-adjusted life years (DALYs) and 22.7% of global years lived with disability (YLDs), underscoring their role as a leading cause of disability worldwide (7). Furthermore, the prevalence of mental health disorders increased during the COVID-19 pandemic (8–10). Despite growing awareness and improved diagnostic efforts, mental health remains underreported in many regions, with systemic gaps in care and support.
An overlooked aspect of severe mental health illnesses (SMI) and their intersection with oral health. Individuals with SMI have a high risk of poor dental health due to factors such as self-neglect, adverse effects of psychotropic medications (e.g., xerostomia), substance use, and financial constraints (11–13). Poor oral health can exacerbate mental health conditions and vice versa, creating a bidirectional relationship that significantly impacts quality of life (14, 15). Quality of life declines further with advancing age and the presence of chronic diseases (16). Oral diseases such as dental caries, periodontal disease, and tooth loss are more prevalent among those with SMI compared to the general population, contributing to broader health disparities (17). This highlights the urgent need for integrated care approaches that address both mental and oral health to improve overall well-being and reduce the life expectancy gap experienced by individuals with severe mental illnesses.
Despite growing recognition of the bidirectional relationship between mental and oral health, a critical gap persists in understanding the lived experiences and specific oral healthcare needs of individuals with SMI. This qualitative meta-synthesis aims to explore and synthesize existing research to delineate the multifaceted barriers hindering access to dental care for this vulnerable population and identify underlying systemic challenges. By integrating diverse perspectives, the study seeks to inform the development of targeted interventions aimed at improving oral healthcare challenges and reducing disparities. Ultimately, this work highlights the imperative for holistic care models that concurrently address both mental and oral health needs to enhance overall well-being in individuals with SMI.
Methods
Inclusion and exclusion criteria
This review included qualitative research on adolescents and adults (15+) diagnosed with SMI, such as schizophrenia, bipolar disorder, major depression, and psychotic disorders. Studies were eligible if at least 75% of participants met the SMI criteria or if separate results were provided for this group. Research conducted in any setting, including community-based environments, psychiatric hospitals, or residential care facilities, was considered. All study designs were accepted if the articles focused on oral health care-related challenges, such as oral hygiene behaviors, access to dental care, barriers, facilitators, and impact on quality of life. Interventions aimed at improving oral health or addressing healthcare barriers were included. Only peer-reviewed, English-language studies were considered, ensuring high-quality evidence. Studies were excluded if they involved individuals without an SMI diagnosis or those under legal guardianship, lacked a focus on oral health interventions, or were non-peer-reviewed publications, editorials, conference abstracts, or non-English articles. These criteria helped maintain a clear and relevant synthesis of qualitative evidence on oral health challenges and interventions for individuals with SMI.
Search strategy
A comprehensive literature search was conducted across multiple databases, including PubMed, Web of Science, Scopus, and Google Scholar. The search strategy utilized Boolean operators and truncation to identify relevant studies on “serious mental illness” and “oral health.” Search terms included various SMI diagnoses such as “schizophrenia,” “bipolar disorder,” “major depression,” and “psychotic disorders,” combined with “oral health”-related terms like “dental care,” “oral hygiene,” and “oral health-related quality of life (OHRQoL).” Additional terms such as “focus groups,” “interviews,” “thematic analysis,” “content analysis,” “grounded theory,” and “phenomenology” were incorporated to ensure the inclusion of qualitative research. This search strategy was designed to capture a broad yet specific range of studies examining the intersection of oral health or oral diseases and mental illness through qualitative methodologies. We limited our search to articles published between January 2010 and January 2025. The study is registered under PROSPERO (CRD42024516535).
Severe mental health
Severe mental illness (SMI) is defined as a subset of mental disorders that are particularly debilitating and significantly impair an individual's ability to function in daily life. It typically includes schizophrenia and other psychotic disorders, bipolar disorder, and major depression with psychotic features. The key characteristics of SMI include:
1. Severe functional impairment in major life activities
2. Persistent and long-term nature of the illness
3. Often includes psychosis as a component
4. Higher risk for anosognosia (lack of illness insight)
5. Increased vulnerability to negative outcomes such as homelessness, hospitalization, and criminal justice involvement
Poor oral health
Oral health encompasses the condition of the mouth, teeth, and orofacial structures, impacting physical functions like eating and speaking, and mental and emotional well-being. Poor oral health commonly includes dental caries (tooth decay), periodontal (gum) disease, tooth loss, and oral cancers. According to the FDI World Dental Federation (18), oral health is defined as:
“Oral health is multifaceted and includes the ability to speak, smile, smell, taste, touch, chew, swallow, and convey a range of emotions through facial expressions with confidence and without pain, discomfort, and disease of the craniofacial complex.” Oral health care is considered a fundamental component of overall health and well-being, reflecting physiological, social, and psychological attributes essential to quality of life (18, 19). However, poor oral health not only causes pain, discomfort, and disfigurement but is also linked to broader health issues, including cardiovascular disease, diabetes complications, respiratory infections, and adverse pregnancy outcomes.
Data extraction and analysis
For this qualitative meta-synthesis, we conducted a comprehensive data extraction and analysis. Data from the included studies were systematically organized into a standardized Excel template to ensure consistency and accuracy. We categorized extracted data into key study details, including author, publication year, country, and participant demographics such as age, gender, and SMI diagnosis. Methodological aspects were also recorded, encompassing data collection methods (e.g., interviews, focus groups) and analysis approaches (e.g., thematic analysis, grounded theory). To capture the core findings, we extracted key themes related to barriers, facilitators, experiences, and the overall impact of oral health on individuals with SMI. This included both direct participant quotes and paraphrased findings. Additionally, a critical appraisal of each study was documented to assess quality and reliability.
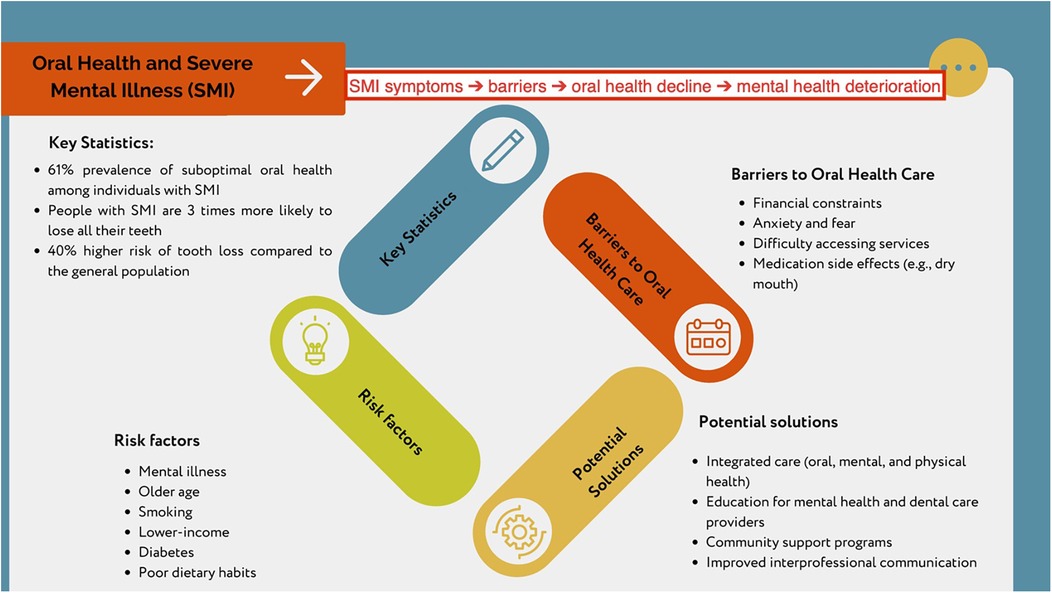
Manual coding was performed on the selected articles to identify patterns and recurring themes. Finally, we conducted a synthesis by comparing findings across studies to ensure consistency and robustness. A visual mapping approach was employed to illustrate the relationship between SMI symptoms, barriers to oral healthcare, and the subsequent deterioration of mental health, providing a clearer understanding of the interconnected challenges faced by this population.
Quality and risk of bias assessment
Using the CASP (Critical Appraisal Skills Programme) Qualitative Checklist in this meta-synthesis ensured a rigorous assessment of study quality and potential biases (20). This tool evaluated qualitative research validity through ten key questions, covering aspects such as the appropriateness of study design, recruitment strategy alignment with research objectives, reflexivity, and ethical considerations. By systematically applying these criteria, the study maintained a high standard of evidence selection.
Studies with critical flaws, such as ethical violations or a lack of theoretical framework, were excluded to enhance reliability. The classification system—high quality (≥80% criteria met), moderate quality (50%–79%), and low quality (<50%)—helped to differentiate the strength of the included studies. This tiered approach ensured that findings were derived from well-conducted research while acknowledging variations in study rigor. All assessment decisions were documented using a PRISMA flow diagram for transparency and reproducibility, with assessment tables appended to the meta-synthesis. This methodological clarity strengthened the validity of the synthesis by allowing for independent verification and replication. By adopting a structured appraisal process, the study ensured a comprehensive and credible analysis of qualitative evidence on oral health challenges among individuals with serious mental illness.
Results
Identification of published and relevant literature
The systematic search initially identified 1,698 records, which were reduced to 155 after removing duplicates and irrelevant entries (Figure 1). The other 57 records were excluded as they comprised books, editorials, and review articles. Three articles were added manually. A total of 101 articles underwent full-text review to assess sample characteristics, qualitative methodologies, and their focus on exploring nature experiences. Of these, 18 were identified as highly relevant and further assessed using the CASP Qualitative Checklist. Seven studies were excluded due to insufficient primary data or methodological limitations, as they lacked insights grounded in participants’ perspectives. Ultimately, 11 studies were selected for synthesis, and the CASP evaluations of the articles are given in https://osf.io/fu4m6/.
Characteristics of included documents
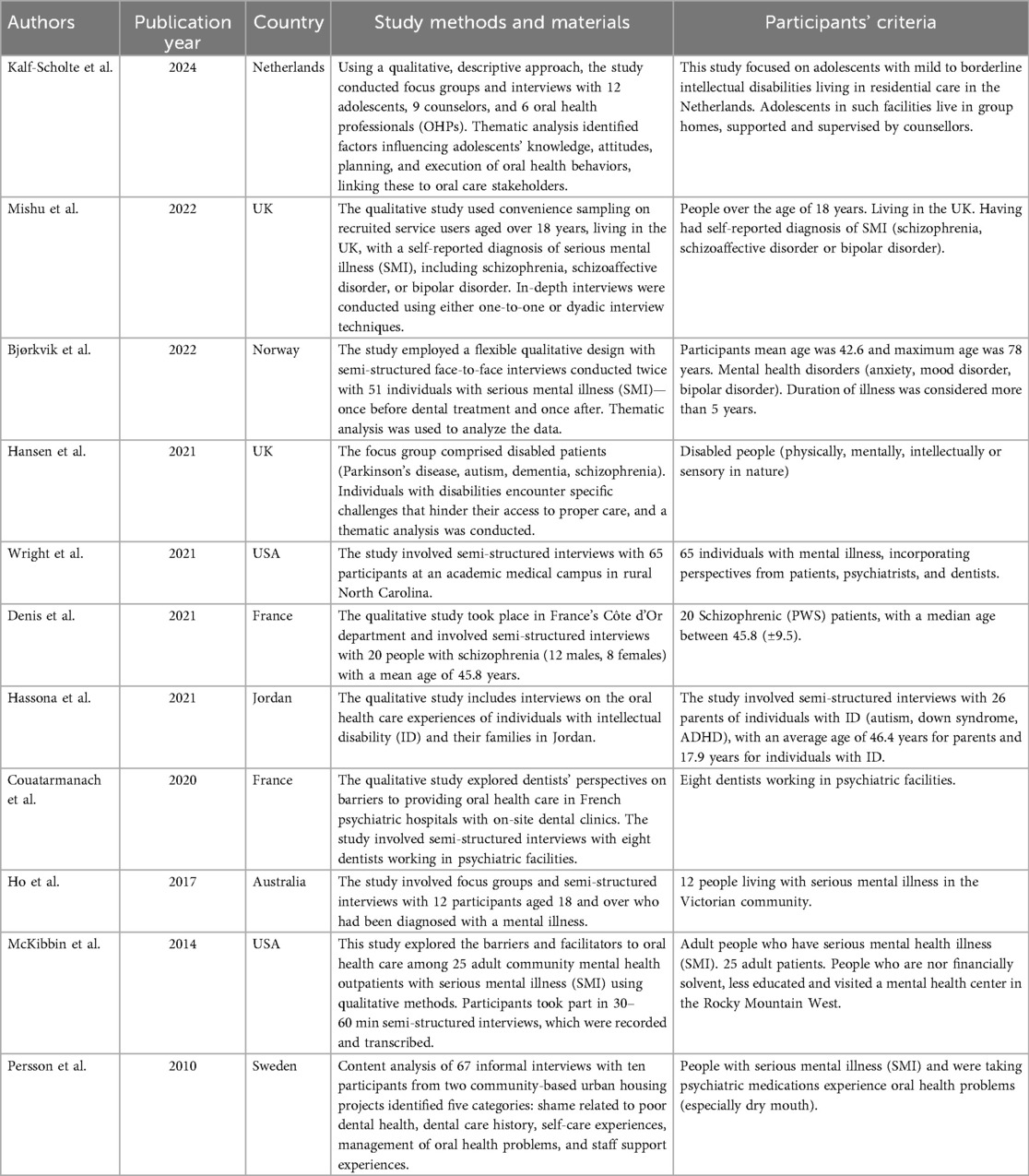
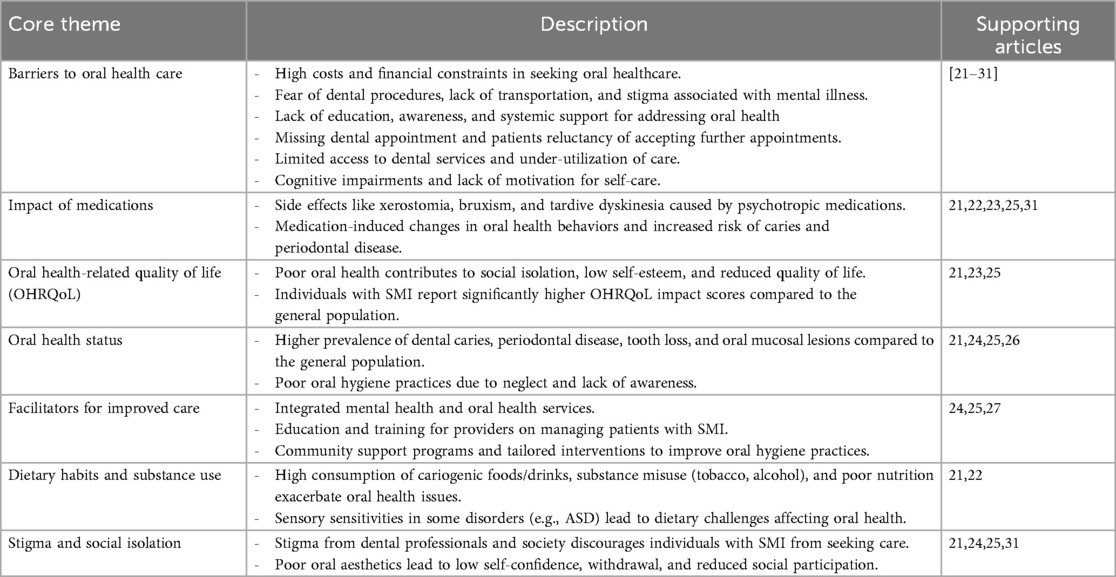
Table 1 provides an overview of the included studies published between 2010 and 2024, with the majority (8 out of 11) appearing after 2020 (21–30). Sample sizes for in-depth and key informant interviews ranged from 8 to 65 participants. The studies were conducted across eight countries: the United States (n = 2), France (n = 2), the United Kingdom (n = 2), the Netherlands (n = 1), Jordan (n = 1), Australia (n = 1), Sweden (n = 1), and Norway (n = 1). Notably, a study by Couatarmanach et al. (27) interviewed dentists as key informants to gain insight into dentists’ experiences with the lived realities of their SMI patients, particularly those affected by specific oral health challenges.
Synthesis
The studies explored various experiences, with the initial coding process providing a broad understanding of the material and highlighting key concepts. Notably, different researchers used varied interpretative language when discussing similar ideas. This meta-synthesis prioritized identifying barriers to oral health care during the coding process while also considering all extracted findings, including individual authors’ interpretations.
To structure the analysis, codes were grouped into logical clusters, leading to the identification of seven core themes: barriers to oral health care, the impact of medications, oral health-related quality of life, oral health status, facilitators for improved care, dietary habits and substance use, and stigma and social isolation. These shared and interconnected meanings are investigated under the core theme of barriers to oral health care.
Table 2 presents the thematic findings, citing source documents, followed by a detailed summary of each core theme with references to descriptive themes. However, as the primary objective of this study is to explore barriers to oral health care, the discussion focuses exclusively on the subthemes under this core theme.
High costs and financial constraints on oral health care
The studies highlighted significant barriers to oral healthcare access for individuals with mental illness, with cost being a central issue. Patients, psychiatrists, and dentists were interviewed across multiple studies, revealing that financial constraints often prevent individuals from seeking preventative or follow-up dental care. Many patients only visit dentists during emergencies due to high treatment costs, lack of affordable insurance, and limited availability of public dentists accepting health coverage (23, 24). Low income, unemployment, and higher living costs exacerbate these challenges, with indirect expenses like transportation and wage loss further limiting access (3, 21, 22, 29).
Participants frequently cited difficulty finding dentists who accept public insurance, particularly in remote areas, and expressed concerns about unpredictable eligibility for free care (3, 29). Fear of high costs and uncertainty about payment also deterred individuals from seeking timely treatment, with some choosing to endure pain rather than incur expenses (28). Patients emphasized the need for transparent information about fees, payment plans, and discounts to alleviate financial anxieties and improve access to care (30). These findings underscore the need for systemic changes to address economic barriers and ensure equitable oral healthcare for individuals with mental illness. A participant from a study stated the reason for not getting continued dental care was fear of not having enough money to pay for services.
“Haven't been to the dentist for a few years because of financial reasons.” [Article from Ho et al., 2017 (28)]
Fear of dental procedures and stigma associated with mental illness
Dental anxiety and fear are significant barriers to care, often heightened by psychological stress and past negative experiences (22, 24, 29). Low confidence about oral health can reduce social interaction and worsen mental health, leading to isolation (30). The stigma surrounding mental illness and intellectual disabilities further discourages individuals and families from seeking dental care, with some avoiding public spaces due to societal judgement (26, 28). Additionally, the invasive nature of dental procedures and lack of trust in dental professionals contribute to reluctance to seek treatment (22, 28, 30). Moreover, parents of children with intellectual disabilities reported societal stigma, which limits their ability to seek care and participate in social life (23). Furthermore, parents of disabled children with exacerbated dental disease reported late-stage presentations due to pain or swelling. They often received reactive care without preventive advice, leading to a cycle of medication and referrals (23). One of the study participants described the scenario highlighted in the research:
“I experience shame more than anxiety at the dentist and expect to be ridiculed or criticized. I have been bullied before, and I always expect it to happen again. Trust is difficult.” [Article from Bjørkvik et al., 2021 (3)]
Another article stated the same scenario from a patient:
“I have anxiety attacks at the dentist’s office… I do not take things easily and feel stressed when I have dental pain… I am afraid to go to the dentist… I have difficulties in managing my visit to the dentist.” [Article from Denis et al., 2021 (25)]
Lack of education, awareness, and systemic support for addressing oral health
Both dentists and psychiatrists identified gaps in their education, with dentists lacking training on the link between oral and mental health and psychiatrists requiring additional training on the importance of oral health screening (24). Patients’ lack of dental insurance and awareness about the importance of oral health further deterred them from seeking care (24). Many delayed treatments until emergencies arose, opting for extractions over prolonged procedures (30). Poor dietary habits and stress-related behaviours, like excessive snacking, negatively impact oral health (25). While some patients with better oral health literacy sought regular care, others delayed treatment until experiencing severe pain or swelling, often receiving reactive rather than preventive care (26, 29). Communication barriers, including complex dental terminology, further hindered understanding and effective care (28). One dentist from a hospital stated that
“There are 30%–40% of the patients who refuse dental care; they say, ‘No, I’m OK, like that, don’t touch my mouth”, and the nurse called us to say that he’s not going to come to the appointment, and we’re not going to force him to come.” [Article from Wright et al, 2021 (24)]
These findings highlight the need for improved education, preventive strategies, and clearer communication in oral healthcare for both patients and doctors.
Missing dental appointments and patient experiences
Dental providers face challenges in managing high caseloads and often refer patients who miss appointments, while patients struggle to find accessible and timely care due to overburdened services (22, 23). Some patients with severe mental illness value their independence and perceive reminders or offers of assistance as patronizing, preferring to manage their oral care without external support (30). Cognitive impairments affect oral hygiene routines. One of the patients from a study highlighted,
“On days when I feel hopeless and think of ending life, I forget both to brush my teeth and to go to the dental clinic.” [Article from Bjørkvik et al., 2021 (3)]
These issues highlight the need for better resource allocation and patient-centered approaches in dental care, especially for people with mental illness.
Limited access to dental services and underutilization of care
Limited access to dental services, whether through the National Health Service or private providers, discourages health-seeking behaviours across all demographics, with long waiting lists and high demand being significant barriers (22, 23). Balancing adequate care with efficient use of public funds remains a challenge, requiring careful planning by healthcare commissioners. The social model of disability is highlighted as a better framework for understanding the barriers faced by individuals with disabilities in accessing healthcare (23).
Overview of findings
Figure 2 presents a four-step cycle, illustrating the significant oral health challenges faced by individuals with severe mental illness. Key statistics show a 61% prevalence of suboptimal oral health, a threefold likelihood of losing all teeth, and a 40% higher risk of tooth loss than the general population (3). Risk factors include mental illness, old age, smoking, lower income, diabetes, and unhealthy dietary habits. Barriers to care include financial constraints, anxiety, difficulty accessing services, and medication side effects, for example, xerostomia. Potential solutions proposed are integrated care, improved provider education, community support programs, and enhanced interprofessional communication.
Discussion
The meta-synthesis reveals systemic barriers to oral health care for individuals with serious mental illness (SMI), with financial constraints, fear/stigma, and fragmented care systems emerging as critical challenges. These findings align with existing literature while highlighting the unique challenges faced by this population. Below, we contextualize these barriers using evidence from the reviewed studies.
High costs and limited insurance coverage were consistently cited as prohibitive factors, forcing many individuals with SMI to delay or avoid dental care until emergencies arise. For example, five studies from the meta-synthesis found that participants avoided dental visits due to unaffordable fees. In contrast, another study noted that only 40% of psychiatrists screened patients for oral health due to perceived irrelevance in mental health care. This aligns with broader findings that individuals with SMI have a 60% higher odds of tooth loss compared to their peers without mental health issues (31). Another study found that perceived poor mental health correlates with a 1.90% increase in the likelihood of complete tooth loss (32). Financial constraints are a major barrier to accessing dental care for individuals with SMI, particularly in low- and middle-income countries (LMICs) (33). The lack of public dental services accepting subsidized insurance exacerbates inequities, particularly in rural or underserved areas.
Dental anxiety, compounded by societal stigma toward mental illness, creates a cycle of avoidance and worsening oral health. The synthesis found individuals avoid care due to fear of judgement, and there's a relationship between poor oral health, shame, and social withdrawal. Mental health stigma also discourages families of individuals with intellectual disabilities from seeking care, as reported. Many individuals experience dental anxiety due to fear of pain and negative past experiences, leading to avoidance of dental care (34). This anxiety is influenced by intrapersonal, interpersonal, and societal factors, including personal traits, past encounters, and societal stigma toward mental illness, which can deter individuals from seeking help and worsen their oral health over time (34, 35). Notably, the invasive nature of dental procedures and distrust in providers further heighten anxiety, particularly among those with psychiatric conditions.
Dental and mental health professionals reported insufficient training to address the interplay between oral health and SMI. The meta-synthesis explored that dentists cited poor communication with psychiatric staff while psychiatrists lacked awareness of oral health screening protocols. The finding is consistent with other studies (36, 37). For example, many dental professionals lack formal training in mental health, leading to communication challenges and treatment hesitancy (36). A survey of dental students highlighted fear and discomfort in treating patients with SMI, underscoring the need for improved education (37). Additionally, medication side effects and dietary habits contribute to poor oral hygiene, further worsening mental health.
Access to dental care for individuals with severe mental illness (SMI) is hindered by systemic and socioeconomic barriers, exacerbating oral health disparities. Long waiting lists and overburdened public health systems delay treatment, often leading to the progression of untreated dental conditions. Quantitative studies also evaluated these and found similar results (38, 39). Geographic disparities further restrict access, particularly in rural or underserved areas where specialized dental services are scarce (40). For those with SMI, these financial obstacles compound existing challenges, making regular dental visits difficult to maintain (31, 32).
The synthesis noted that patients with SMI often miss dental appointments and may not recognize the severity of their oral health issues due to various barriers. Additionally, cognitive impairments associated with SMI, such as apathy, executive dysfunction, and disorganized thinking, further reduce adherence to oral hygiene routines. Individuals may struggle with daily brushing and flossing, miss dental appointments, or fail to recognize the severity of their oral health issues. One study mentioned that individuals with SMI face challenges such as managing complex life circumstances, psychological and physical difficulties, and a lack of motivation or awareness regarding oral health (41). This neglect creates a cycle in which poor oral health exacerbates physical discomfort and social withdrawal, ultimately worsening overall well-being and mental health outcomes. Accessibility and availability of dental services are also significant issues, with many patients experiencing lower rates of dental service utilization compared to the general population (42).
The relevance of these findings to low- and middle-income countries (LMICs) warrants careful consideration, as differences in healthcare infrastructure, socioeconomic conditions, and cultural contexts significantly shape outcomes. In LMICs, the already high prevalence of oral health problems such as dental caries and periodontal disease among individuals with SMI is likely exacerbated by limited access to preventive and curative dental services (particularly in rural areas where dentists are scarce), a higher burden of malnutrition and systemic illnesses like diabetes, and pervasive stigma surrounding mental illness (43–47). These challenges are compounded by fragmented health systems with minimal integration between mental health and dental services, a shortage of dental professionals trained to care for individuals with SMI, and substantial financial barriers, including the absence of universal health coverage and heavy reliance on out-of-pocket payments.
Strengths and limitations of the study
This review synthesizes qualitative research to provide a comprehensive view of oral health challenges in individuals with severe mental illness (SMI). It captures lived experiences, highlighting key themes such as barriers to care, medication side effects, stigma, and systemic challenges. Common issues include financial constraints, lack of mental health training among dental professionals, and medication-induced xerostomia. Stigma and social isolation further hinder access to care. While enhancing the generalizability of insights, the study also suggests solutions like integrated care models and interdisciplinary collaboration. However, the following limitations should be considered in broader applications of this meta-synthesis.
This meta-synthesis has several limitations that should be considered when interpreting its findings. First, the study is based on participants with serious mental illness (SMI) in the Global North, limiting the generalizability of results to other clinical or geographic populations. While efforts were made to conduct comprehensive sampling, the scarcity of relevant literature resulted in a small sample size (n = 11). Another challenge lies in the heterogeneity of study designs, populations, and interventions, making direct comparisons difficult. The included studies also exhibited methodological limitations, such as researcher reflexivity, which may influence confirmability and introduce bias in recruitment and research procedures. The synthesis prioritized participants’ raw data (direct quotes) to enhance credibility, ensuring interpretations remained close to their lived experiences. Additionally, detailed documentation of search procedures and quality appraisals was maintained to uphold rigour and transparency.
A further limitation is the potential for researcher bias in interpreting and synthesizing qualitative data, which can influence the conclusions. Lastly, the lack of longitudinal studies prevents an assessment of long-term changes in oral health behaviours and the sustained impact of interventions over time. Future research should address these gaps by incorporating diverse populations, minimizing methodological inconsistencies, and conducting long-term follow-up studies to evaluate intervention effectiveness.
Conclusion
This meta-synthesis highlights the profound and pervasive burden of poor oral health among individuals with SMI, marked by significantly elevated rates of dental caries, tooth loss and periodontal disease. Key drivers—including suboptimal oral hygiene, limited health literacy, the adverse effects of long-term psychotropic medication (notably xerostomia), and formidable barriers to accessing dental care—converge to create a stark health disparity. Financial hardship, inadequate training of dental professionals in mental health, pervasive stigma, and social isolation further compound this inequity. Addressing this crisis demands coordinated action: the integration of mental and oral healthcare through co-located services, robust interdisciplinary collaboration, and the implementation of tailored, accessible interventions is imperative. Future research must prioritise quantitative studies to elucidate causal pathways and long-term impacts, rigorously examining the roles of gender, geography, environmental factors, and comorbid physical conditions. Bridging this divide is not merely a dental concern but an urgent public health imperative, requiring systemic reform to uphold the fundamental health rights of this vulnerable population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
TA: Writing – review & editing, Conceptualization, Writing – original draft, Data curation. JB: Validation, Resources, Writing – review & editing. KZ: Writing – review & editing, Data curation. MA: Writing – review & editing, Data curation. MN: Conceptualization, Writing – review & editing, Formal analysis. MDH: Writing – review & editing, Data curation. AH: Resources, Writing – review & editing, Formal analysis, Writing – original draft, Data curation, Methodology, Supervision, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kalaigian A, Chaffee B. Mental health and oral health in a nationally representative cohort. J Dent Res. (2023) 102:1007–14. doi: 10.1177/00220345231171108
2. Kisely S, Baghaie H, Lalloo R, Siskind D, Johnson N. A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom Med. (2015) 77:83–92. doi: 10.1097/PSY.0000000000000135
3. Bjørkvik J, Quintero D, Vika M, Nielsen G, Virtanen J. Barriers and facilitators for dental care among patients with severe or long-term mental illness. Scand J Caring Sci. (2021) 36:27–35. doi: 10.1111/scs.12960
4. Slack-Smith L, Hearn L, Scrine C, Durey A. Barriers and enablers for oral health care for people affected by mental health disorders. Aust Dent J. (2017) 62:6–13. doi: 10.1111/adj.12429
5. Yang X, Fang Y, Chen H, Zhang T, Yin X, Man J, et al. Global, regional and national burden of anxiety disorders from 1990 to 2019: results from the Global Burden of Disease Study 2019. Epidemiol Psychiatr Sci. (2021) 30:e36. doi: 10.1017/S2045796021000275
6. Ashbaugh D, Santomauro D, Herrera A, Shadid J, Zheng P, Ashbaugh C, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
7. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. (2022) 9(2):137–50. doi: 10.1016/S2215-0366(21)00395-3
8. Ali M, Uddin Z, Ahsan NF, Haque MZ, Bairagee M, Khan SA, et al. Prevalence of mental health symptoms and its effect on insomnia among healthcare workers who attended hospitals during COVID-19 pandemic: a survey in Dhaka city. Heliyon. (2021) 7(5):e06985. doi: 10.1016/j.heliyon.2021.e06985
9. Chowdhury SR, Sunna TC, Das DC, Kabir H, Hossain A, Mahmud S, et al. Mental health symptoms among the nurses of Bangladesh during the COVID-19 pandemic. Middle East Curr Psychiatry. (2021) 28(1):23. doi: 10.1186/s43045-021-00103-x
10. Ali M, Ahsan GU, Khan R, Khan HR, Hossain A. Immediate impact of stay-at-home orders to control COVID-19 transmission on mental well-being in Bangladeshi adults: patterns, explanations, and future directions. BMC Res Notes. (2020) 13(1):494. doi: 10.1186/s13104-020-05345-2
11. Santhosh Kumar S, Cantillo R, Ye D. The relationship between oral health and schizophrenia in advanced age—a narrative review in the context of the current literature. J. Clin. Med. (2023) 12:6496. doi: 10.3390/jcm12206496
12. Chen R-J, Lai K-H, Lee C-H, Lin H-Y, Lin C-C, Chen C-H, et al. Exploring the link between xerostomia and oral health in mental illness: insights from autism spectrum disorder, depression, bipolar disorder, and schizophrenia. Healthcare. (2024) 12:2018. doi: 10.3390/healthcare12202018
13. Frigaard J, Hynne H, Randsborg K, Mellin-Olsen T, Young A, Rykke M, et al. Exploring oral health indicators, oral health-related quality of life and nutritional aspects in 23 medicated patients from a short-term psychiatric ward. Front. Public Health. (2023) 11:1083256. doi: 10.3389/fpubh.2023.1083256
14. Khairunnisa Z, Siluvai S, Kanakavelan K, Agnes L, Indumathi K, Krishnaprakash G. Mental and oral health: a dual frontier in healthcare integration and prevention. Cureus. (2024) 16(12):e76264. doi: 10.7759/cureus.76264
15. Ohi T, Murakami T, Komiyama T, Miyoshi Y, Endo K, Hiratsuka T, et al. Oral health-related quality of life is associated with the prevalence and development of depressive symptoms in older Japanese individuals: the Ohasama study. Gerodontology. (2022) 39(2):204–12. doi: 10.1111/ger.12557
16. Hossain A, Hasan M, Rahman T, Almarzooqi A, Rahman SA, Hijazi H, et al. Palliative care needs and quality of life among adults with advanced chronic illnesses in low-income communities of Bangladesh. BMC Palliat Care. (2025) 24(1):18. doi: 10.1186/s12904-024-01643-9
17. Tiwari T, Kelly A, Randall CL, Tranby E, Franstve-Hawley J. Association between mental health and oral health status and care utilization. Front Oral Health. (2022) 2:732882. doi: 10.3389/froh.2021.732882
18. Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI world dental federation opens the door to a universal definition of oral health. Int Dent J. (2016) 66(6):322–4. doi: 10.1111/idj.12294
19. Foley MA, Lalloo R, Spencer AJ, Do LG. What are “health” and “oral health”? J Global Oral Health. (2022) 5:110–8. doi: 10.25259/JGOH_23_2022
20. Critical Appraisal Skills Programme UK. CASP qualitative studies checklist (2024). Available online at: https://casp-uk.net/casp-tools-checklists/qualitative-studies-checklist/ (Accessed on May 03, 2025)
21. Kalf-Scholte SM, van Zoonen R, Sijperda-Abdul D, Algra H, Valkenburg C. Factors influencing the oral health behaviour of Dutch adolescents with mild to borderline intellectual disabilities living in residential care: a qualitative study. J Appl Res Intellect Disabil. (2024) 37(3):e13220. doi: 10.1111/jar.13220
22. Mishu MP, Faisal MR, Macnamara A, Sabbah W, Peckham E, Newbronner L, et al. A qualitative study exploring the barriers and facilitators for maintaining oral health and using dental service in people with severe mental illness: perspectives from service users and service providers. Int J Environ Res Public Health. (2022) 19(7):4344. doi: 10.3390/ijerph19074344
23. Hansen C, Curl C, Geddis-Regan A. Barriers to the provision of oral health care for people with disabilities. BDJ In Pract. (2021) 34:30–4. doi: 10.1038/s41404-021-0675-x
24. Wright WG, Averett PE, Benjamin J, Nowlin JP, Lee JGL, Anand V. Barriers to and facilitators of oral health among persons living with mental illness: a qualitative study. Psychiatr Serv. (2021) 72(2):156–62. doi: 10.1176/appi.ps.201900535
25. Denis F, Siu-Paredes F, Maitre Y, Amador G, Rude N. A qualitative study on experiences of persons with schizophrenia in oral-health-related quality of life. Braz Oral Res. (2021) 35:e050. doi: 10.1590/1807-3107bor-2021.vol35.0050
26. Hassona Y, Aljafari A, Atef A, Abdalfattah L, Hosey MT. Failure on all fronts: qualitative analysis of the oral health care experience in individuals with intellectual disability. Spec Care Dentist. (2021) 41(2):235–43. doi: 10.1111/scd.12550
27. Couatarmanach A, Sherlaw W, Prigent P-M, Harpet C, Bertaud V. Dentists’ perspectives on barriers to providing oral health care in French psychiatric hospitals with on-site dental clinics. Community Dent Oral Epidemiol. (2020) 48(4):296–301. doi: 10.1111/cdoe.12532.hal-02532849
28. Ho HD, Satur J, Meldrum R. Perceptions of oral health by those living with mental illnesses in the victorian community - the consumer’s perspective. Int J Dent Hyg. (2018) 16(2):e10–6. doi: 10.1111/idh.12278
29. McKibbin CL, Kitchen-Andren KA, Lee AA, Wykes TL, Bourassa KA. Oral health in adults with serious mental illness: needs for and perspectives on care. Community Ment Health J. (2015) 51(2):222–8. doi: 10.1007/s10597-014-9758-z
30. Persson K, Olin E, Ostman M. Oral health problems and support as experienced by people with severe mental illness living in community-based subsidised housing–a qualitative study. Health Soc Care Community. (2010) 18(5):529–36. doi: 10.1111/j.1365-2524.2010.00931.x
31. Kang J, Wu J, Aggarwal VR, Shiers D, Doran T, Palmier-Claus J. Investigating the relationship between oral health and severe mental illness: analysis of NHANES 1999–2016. Dentistry Journal. (2024) 12(7):191. doi: 10.3390/dj12070191
32. Powell T, Taylor H. The relationship between self-reported poor mental health and complete tooth loss among the US adult population in 2019. Front Oral Health. (2024) 5:1363982. doi: 10.3389/froh.2024.1363982
33. Sharma A, Blakemore A, Byrne M, Nazary M, Siroya K, Husain N, et al. Oral health primary preventive interventions for individuals with serious mental illness in low- and middle-income nations: scoping review. Glob Public Health. (2024) 19(1):2408597. doi: 10.1080/17441692.2024.2408597
34. Goh EZ, Beech N, Johnson NR. Dental anxiety in adult patients treated by dental students: a systematic review. J Dent Educ. (2020) 84(7):805–11. doi: 10.1002/jdd.12173
35. Wolf TG, Schläppi S, Benz CI, Campus G. Efficacy of hypnosis on dental anxiety and phobia: a systematic review and meta-analysis. Brain Sci. (2022) 12(5):521. doi: 10.3390/brainsci12050521
36. Suga T, Gamo Y, Iida S, Toyofuku A. Potential needs of outreach dental care for patients with mental conditions. Psychogeriatrics. (2025) 25(1):e13239. doi: 10.1111/psyg.13239
37. Zechner MR, Singhal V, Murphy AA, York J, Karyczak S, Muhammad A. Dental pre-doctoral student perceptions about serious mental illness: concerns and role clarification. J Dent Educ. (2023) 87(5):639–45. doi: 10.1002/jdd.13156
38. Turner E, Berry K, Aggarwal VR, Quinlivan L, Villanueva T, Palmier-Claus J. Oral health self-care behaviours in serious mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand. (2022) 145(1):29–41. doi: 10.1111/acps.13308
39. Goud V, Kannaiyan K, Rao BV, Abidullah M, Dharani V, Nayak M. Oral health status and treatment needs of psychiatric outpatients aged 18–64 years in district civil hospital, Raichur, Karnataka: a cross-sectional study. J Pharm Bioallied Sci. (2021) 13(Suppl 1):S598–601. doi: 10.4103/jpbs.JPBS_776_20
40. Sogi GM, Khan SA, Bathla M, Sudan J. Oral health status, self-perceived dental needs, and barriers to utilization of dental services among people with psychiatric disorders reporting to a tertiary care center in haryana. Dent Res J (Isfahan). (2020) 17(5):360–5.33343844
41. Brigg N, Patterson S, Pradhan A. Enabling people with severe mental illness to overcome barriers to access dental treatment: a qualitative study applying COM-B framework analysis. J Mental Health. (2020) 31:765–73. doi: 10.1080/09638237.2020.1803230
42. Ferry F, Rosato M, Leavey G. Mind the gap: an administrative data analysis of dental treatment outcomes and severe mental illness. J Ment Health. (2024) 33(4):474–80. doi: 10.1080/09638237.2022.2069722
43. Dai X, Dai M, Liang Y, Li X, Zhao W. Global burden and trends of oral disorders among adolescent and young adult (10–24 years old) from 1990 to 2021. BMC Oral Health. (2025) 25(1):486. doi: 10.1186/s12903-025-05864-z
44. Hossain A, Niroula B, Duwal S, Ahmed S, Kibria MG. Maternal profiles and social determinants of severe acute malnutrition among children under-five years of age: a case-control study in Nepal. Heliyon. (2020) 6(5):e03849. doi: 10.1016/j.heliyon.2020.e03849
45. Hossain A, Ahmed B, Rahman T, Sammonds P, Zaman S, Benzadid S, et al. Household food insecurity, income loss, and symptoms of psychological distress among adults following the cyclone amphan in coastal Bangladesh. PLoS One. (2021) 16(11):e0259098. doi: 10.1371/journal.pone.0259098
46. Hossain A, Suhel SA, Chowdhury SR, Islam S, Akther N, Dhor NR, et al. Hypertension and undiagnosed hypertension among Bangladeshi adults: identifying prevalence and associated factors using a nationwide survey. Front Public Health. (2022) 10:1066449. doi: 10.3389/fpubh.2022.1066449
Keywords: mental health, oral health, dental health, barriers to oral health care, qualitative study
Citation: Afroz T, Beyene J, Zaheer K, Alameddine M, Nabi MH, Hawlader MDH and Hossain A (2025) Oral health care challenges in individuals with severe mental illness: a qualitative meta-synthesis. Front. Oral Health 6:1655450. doi: 10.3389/froh.2025.1655450
Received: 27 June 2025; Accepted: 26 August 2025;
Published: 12 September 2025.
Edited by:
Gustavo Molina, Universidad Católica de Córdoba, ArgentinaReviewed by:
Tatiane Marega, São Leopoldo Mandic School, BrazilAlfredo Salinas, Universidad de Monterrey, Mexico
Copyright: © 2025 Afroz, Beyene, Zaheer, Alameddine, Nabi, Hawlader and Hossain. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmed Hossain, YWhtZWQuaG9zc2FpbkBzYWlzdGJkLm9yZw==
 Tanzina Afroz1
Tanzina Afroz1 Joseph Beyene
Joseph Beyene Mohamad Alameddine
Mohamad Alameddine Ahmed Hossain
Ahmed Hossain