- 1Faculty of Public Health, Thai Nguyen University of Medicine and Pharmacy, Thai Nguyen, Vietnam
- 2General Hospital No. 4, Sa Pa, Lao Cai, Vietnam
- 3Vinh Loc District Health Center, Vinh Loc, Thanh Hoa, Vietnam
- 4Department of Pediatrics, Thai Nguyen University of Medicine and Pharmacy, Thai Nguyen, Vietnam
Background: Tooth decay remains one of the most prevalent chronic conditions affecting children globally, especially in underserved populations. Despite growing international attention, limited data exist on the oral health status of children in remote regions of Vietnam.
Objective: To assess factors associated with dental caries among primary schoolchildren in the mountainous province of northern Vietnam.
Methods: A cross-sectional study was conducted from April 2024 to April 2025 among 545 children enrolled in four primary schools in Sa Pa, Lao Cai Province. Clinical dental examinations were performed using the International Caries Detection and Assessment System (ICDAS). Data on oral health behaviors and sociodemographic characteristics were collected via structured interviews. Descriptive statistics summarized the prevalence of caries and oral hygiene practices. Associations were analyzed using stepwise logistic and linear regression models.
Results: The overall prevalence of dental caries was 91.4%, with 57.4% of children affected in permanent teeth and 82.2% in primary teeth. The mean DMFT and dmft scores were 1.31 and 5.38, respectively. Older age increased the risk of permanent caries but reduced primary caries and dmft scores. Significant disparities were observed by ethnicity, with Tay children showing higher odds of primary caries and Hmong children lower dmft scores compared to Dao peers. Children of non-farmer parents, particularly workers, had lower dmft scores than those of farmers. Frequent candy/snack and soda consumption were linked to higher primary caries, while poor brushing habits and symptomatic-only dental visits were associated with worse caries indices.
Conclusions: Children in remote mountainous areas of Vietnam bear an alarmingly high burden of untreated tooth decay, particularly in primary teeth. Sociodemographic factors and inadequate oral health practices significantly contribute to this burden. Tailored, school-based preventive interventions, improved parental education, and enhanced access to dental care are urgently needed to address disparities and improve children's oral health outcomes in these regions.
Introduction
Tooth decay, or dental caries, remains one of the most prevalent chronic diseases among children worldwide, posing a significant challenge to public health (1). Studies from different regions have consistently shown high and unequal prevalence rates of tooth decay in children. For instance, over 40% of preschool children in rural and remote areas of Western Australia have at least one decayed tooth, with Indigenous children experiencing a significantly higher rate of 69%, compared to 25% among non-Indigenous children (2). Similarly, research in China indicated that 8.7% of 7- to 8-year-olds had caries in their new adult teeth, with plaque detected in over 98% of cases (3). In the United States, 23% of children aged 2–11 years have untreated decay in primary teeth, particularly among low-income and minority groups (4). In Africa, the prevalence among 12-year-olds averages 36%, with large discrepancies between urban and rural settings (5), while in crisis-affected Syria, rates have soared to 79.1% among children aged 8–12 years (6).
Beyond prevalence, the burden of tooth decay manifests in significant health and social consequences. In Western Australia, tooth decay is a leading cause of hospitalization among preschool children, disproportionately affecting Indigenous communities (2). In the United States, untreated caries is associated with pain, infections, and functional impairments, highlighting the importance of preventive programs such as school-based sealants (7). Children with neurodevelopmental disabilities in New Zealand have higher rates of hospital admissions due to dental caries, suggesting the need for targeted interventions (8). Furthermore, research in Tanzania has shown that dental caries negatively impacts preschool children's quality of life, leading to pain, embarrassment, and stigma (9).
A multitude of factors contributes to the development and progression of tooth decay in children. Socioeconomic status is a central determinant, with children from low-income families facing greater challenges in accessing dental care and preventive services (4, 10). Racial and ethnic disparities further exacerbate the issue, especially in the United States, where Hispanic and Black children have higher rates of untreated decay due to systemic and structural barriers (11). Parental factors such as maternal education and infant feeding practices also play a role, as observed in Iran where lower maternal education and prolonged breastfeeding were associated with higher caries scores (12). In addition to socioeconomic and demographic influences, behavioral factors such as dietary habits and oral hygiene practices significantly impact children's oral health. A study in Peru found a strong association between frequent sweet consumption and early childhood caries (13). Regular tooth brushing and the use of fluoride toothpaste are essential preventive behaviors, yet many children fail to adhere to these recommendations, often due to a lack of parental guidance or education (14). Moreover, disparities in access to preventive services remain a major challenge. While interventions such as fluoride varnishes and routine dental visits are proven to reduce caries risk, children from underserved populations continue to face barriers in obtaining these services (4).
Despite the growing body of international evidence, there remains a scarcity of research focused on the oral health of children in remote and underserved regions such as mountainous areas in Vietnam. Limited access to healthcare infrastructure, socioeconomic challenges, and cultural factors may further compound the risk of tooth decay in these populations. Evidence from other regions of Vietnam highlights the scale of the problem: a study conducted in Southern and Central Vietnam found a high prevalence of early childhood caries (ECC) at 74.4% among children aged 1–6 years, with a significant portion of these cases being untreated (15). In Ho Chi Minh City, the prevalence of dental caries among 12-year-olds was influenced by community water fluoridation, with areas having lower fluoride levels showing higher caries rates (16). To address the existing research gap, the present study aims to assess the prevalence and associated factors of tooth decay among schoolchildren living in mountainous regions of northern Vietnam. This research will provide critical insights needed to inform public health policies and targeted interventions for improving oral health equity among vulnerable children.
Materials and method
Study design and participants
This study employed a descriptive cross-sectional design and was conducted from April 2024 to April 2025 among schoolchildren enrolled in four primary schools in Sa Pa Town, Lao Cai Province, Vietnam. The target population included all students attending these schools during the survey periodIn Sa Pa Town, there are a total of eight primary schools; four schools were randomly selected to participate in the study. Within each selected school, all classes from grades 1–5 were invited to take part. Eligibility criteria were clearly defined. All children who were present at school during the data collection period and whose parents or legal guardians provided written informed consent were invited to join the study. Exclusion criteria included: (i) children with congenital oral malformations, (ii) those suffering from infectious diseases or fever at the time of the dental examination, (iii) children whose parents or legal guardians declined to give written informed consent, and (iv) children who personally refused to participate. The sample size was calculated based on a formula for cross-sectional studies, using a margin of error (d) of 0.07 and an estimated prevalence (p) of 78.5% derived from a previous study in Malaysia and Myanmar (17). With a 95% confidence level, the required sample size was 532. To account for an anticipated 5% non-response rate, the final adjusted sample size was 559. In practice, 545 students fulfilled the inclusion criteria and consent requirements and were examined, yielding a participation rate of 97.5%.
Data collection and measurement
Data collection was carried out using two main instruments: a clinical dental examination form and a structured interview questionnaire. The clinical examination was conducted by licensed dentists specialized in Odonto-Stomatology, following a standardized protocol to ensure consistency and reliability. Each child was examined in a designated area within the school premises, under natural or artificial lighting as needed. Oral examinations were performed using sterilized dental instruments, including a mouth mirror and a blunt-tipped explorer, and adhered strictly to the diagnostic criteria of the International Caries Detection and Assessment System (ICDAS) (18). To optimize visibility and enable reliable detection of caries in a non-clinical setting, teeth were dried using sterile cotton rolls and gauze before examination. Only cavitated lesions (corresponding to ICDAS codes 3–6) were recorded in this study, while early enamel lesions (ICDAS 1–2) were not included. All teeth were examined in sequence, and each tooth surface was assessed for signs of cavitated decay. Prior to data collection, examiner calibration was conducted to ensure methodological rigor. The dentists underwent joint training sessions using ICDAS reference photographs and clinical cases, following established guidelines (19). Inter- and intra-examiner reliability were assessed on a subsample of 30 children not included in the main study (19). The kappa coefficients for caries detection ranged from 0.82–0.89, indicating high agreement. In addition to the caries assessment, the Decayed, Missing, and Filled Teeth index was calculated separately for permanent teeth (DMFT) and primary teeth (dmft) to quantify the overall burden of dental caries in the study population.
Sociodemographic and behavioral data were obtained through structured face-to-face interviews using a pre-designed questionnaire. The questionnaire was adapted from previously validated instruments on oral health practices and was translated into Vietnamese (9, 14, 20–22). It was then reviewed by local experts to ensure cultural appropriateness and face validity. A pilot test was conducted with 30 children and their parents/guardians in the study area to confirm clarity, language comprehension, and reliability before implementation in the main survey. The questionnaire collected information on age, gender, school grade, parental occupation, and number of children in the family. The questionnaire also explored understanding of correct oral hygiene methods, such as the appropriate type of toothbrush (child vs. adult), the number of tooth surfaces to brush, the recommended brushing duration and frequency, and suitable brushing times during the day (after meals, before sleep, upon waking). Additional questions evaluated practical behavior, such as how often the child brushed their teeth, when brushing occurred, how often toothbrushes were replaced, and their frequency of consuming sweets or soft drinks. Other behaviors included the use of toothpicks or dental floss, the habit of biting hard objects, and frequency of dental check-ups, ranging from regular preventive visits to visits only when experiencing pain or inflammation. Brushing technique was also directly assessed by observation using a standard toothbrush provided during the interview.
Statistical analysis
All data were coded and entered using Epidata 3.1, then analyzed with STATA version 17.0. Descriptive statistics (frequencies, percentages, means, and standard deviations) were used to summarize sociodemographic characteristics, oral health status, and knowledge/practices. Associations between independent variables and dental caries outcomes were assessed using stepwise logistic regression (for binary outcomes such as presence of caries) and linear regression (for continuous outcomes like DMFT score). A p-value < 0.2 was used as the threshold for selecting variables in the stepwise regression models (23, 24), and p < 0.05 was considered statistically significant in the final model.
Ethical approval
The study protocol was reviewed and approved by the Ethical Review Board of Thai Nguyen University of Medicine and Pharmacy under Decision No. 1197/ĐHYD-HĐĐĐ. Participation was voluntary, with written informed consent obtained from parents or legal guardians. The confidentiality and anonymity of participants were strictly maintained throughout the study. Children found to have oral health issues during the examination were referred for further consultation and management.
Results
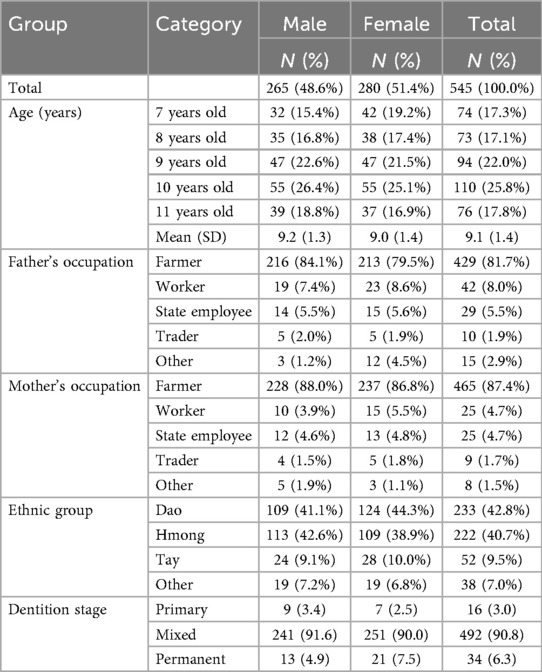
The study included 545 primary schoolchildren, comprising 265 boys (48.6%) and 280 girls (51.4%), with a mean age of 9.1 ± 1.4 years. The largest age group was 10 years old (25.8%), followed by 9 years (22.0%), 11 years (17.8%), 7 years (17.3%), and 8 years (17.1%). Most fathers were farmers (81.7%), while smaller proportions were workers (8.0%), state employees (5.5%), traders (1.9%), or had other occupations (2.9%). Similarly, the majority of mothers were farmers (87.4%), with fewer working as workers (4.7%), state employees (4.7%), traders (1.7%), or in other roles (1.5%). Regarding ethnicity, 42.8% were Dao, 40.7% Hmong, 9.5% Tay, and 7.0% belonged to other groups. In terms of dentition stage, most children were in the mixed dentition phase (90.8%), with 6.3% in permanent dentition and 3.0% still in primary dentition (Table 1).
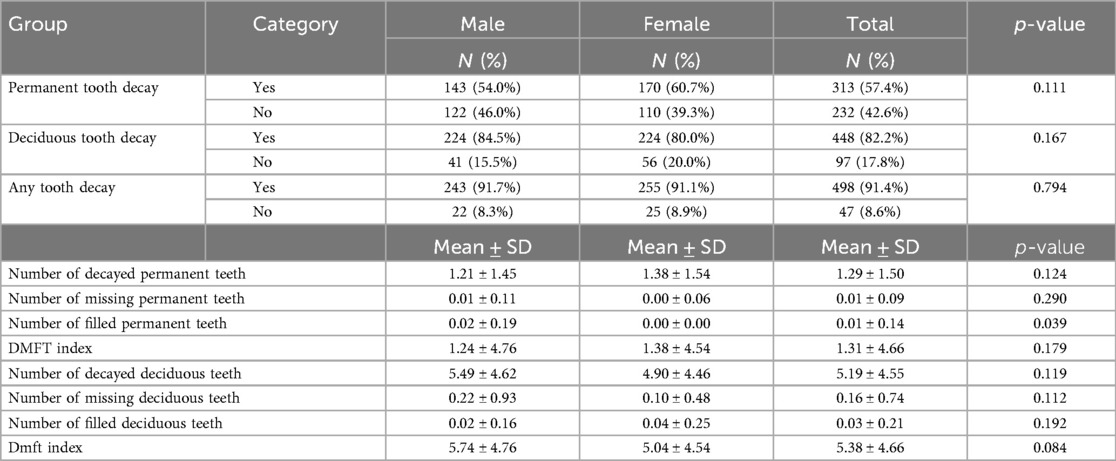
Table 2 summarizes the dental health status of schoolchildren by gender. The prevalence of permanent tooth decay was 54.0% in males and 60.7% in females, while deciduous tooth decay was observed in 84.5% of males and 80.0% of females. The proportion of children with any tooth decay was similar between genders (91.7% in males and 91.1% in females). The mean number of decayed permanent teeth was slightly higher in females (1.38 ± 1.54) than in males (1.21 ± 1.45), and the DMFT score was 1.38 ± 4.54 in females and 1.24 ± 4.76 in males. For deciduous teeth, males had a higher mean number of decayed (5.49 ± 4.62) and missing (0.22 ± 0.93) teeth compared to females (4.90 ± 4.46 and 0.10 ± 0.48, respectively), while females had a slightly higher mean number of filled deciduous teeth. The dmft index was higher in males (5.74 ± 4.76) than in females (5.04 ± 4.54). Most comparisons did not show statistically significant differences between genders, except for the number of filled permanent teeth (p = 0.039).
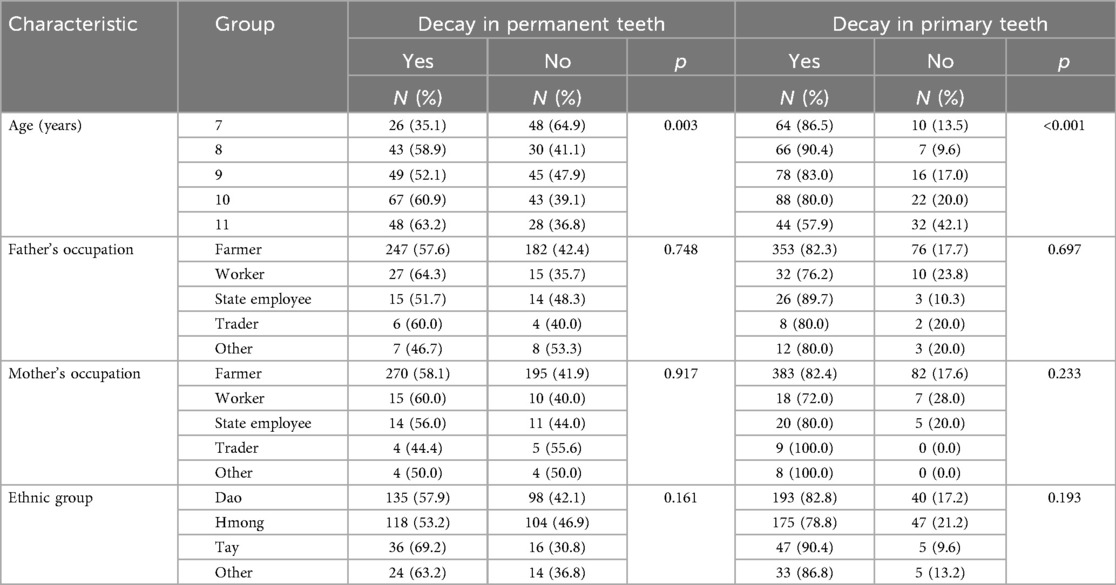
Among participant characteristics, only age showed a statistically significant association with dental caries in both permanent and primary teeth. In permanent dentition, the proportion of children with caries increased steadily from 35.1% at age 7%–63.2% at age 11 (p = 0.003). For primary dentition, the prevalence of decay was very high across all ages but decreased with increasing age, from 90.4% at 8 years and 86.5% at 7 years to 57.9% at 11 years (p < 0.001). No other variables demonstrated significant associations (Table 3).
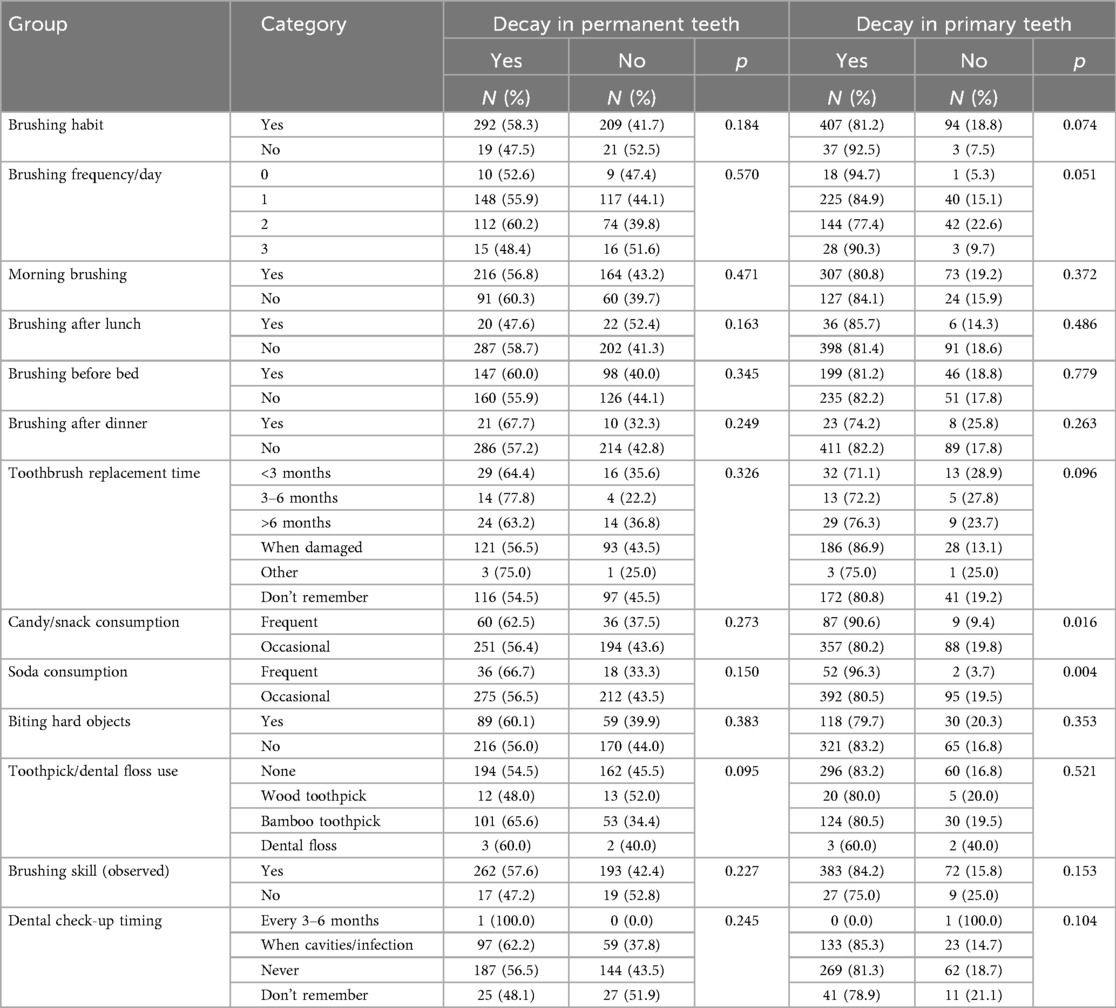
Table 4 presents the association between various oral health behaviors and the presence of dental caries among participants. Significant associations were observed for candy/snack consumption and soda consumption with dental caries in primary teeth. Children who frequently consumed candy or snacks had a higher prevalence of caries in primary teeth (90.6%) compared to those who consumed them occasionally (80.2%) (p = 0.016). Similarly, frequent soda consumption was associated with markedly higher caries prevalence in primary teeth (96.3%) compared to occasional consumption (80.5%) (p = 0.004). No other behaviors demonstrated statistically significant associations.
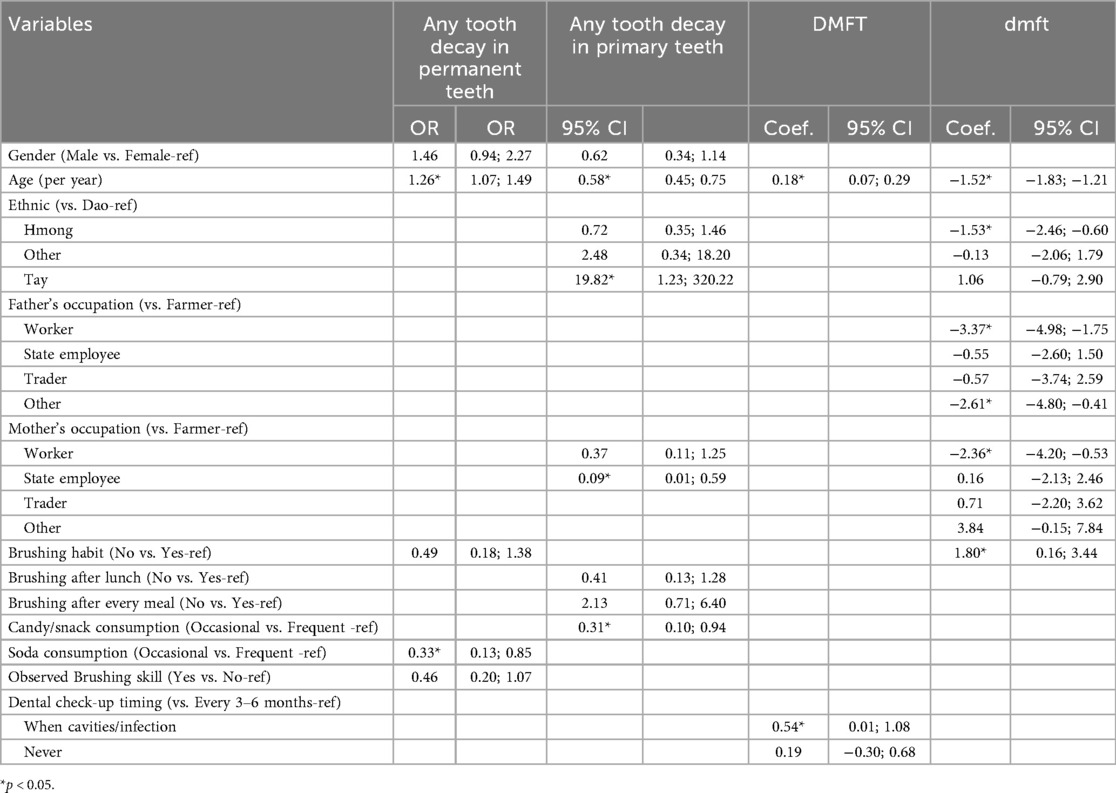
Table 5 presents factors associated with tooth decay (any decay in permant and primary teeth), DMFT, and dmft indices. In the analysis of factors associated with permanent tooth decay, age was significantly related: each additional year increased the odds of decay by 26% (OR = 1.26, 95% CI: 1.07–1.49). Soda consumption was also significant, with occasional consumers showing a lower odds of permanent tooth decay compared with frequent consumers (OR = 0.33, 95% CI: 0.13–0.85).
For primary teeth, older age was associated with a reduced likelihood of decay (OR = 0.58, 95% CI: 0.45–0.75). Among ethnic groups, children of Tay ethnicity had significantly higher odds of primary tooth decay compared to Dao (OR = 19.82, 95% CI: 1.23–320.22). Candy and snack consumption was also significant, as occasional consumers had lower odds of decay compared with frequent consumers (OR = 0.31, 95% CI: 0.10–0.94). Children having mother who were state employees had a lower odds of having primary tooth decay.
Regarding the DMFT index, older age was associated with an increase in score (Coef. = 0.18, 95% CI: 0.07–0.29). The timing of dental check-ups also showed a significant effect: children who sought care only when cavities or infections occurred had higher DMFT scores compared with those who checked every 3–6 months (Coef. = 0.54, 95% CI: 0.01–1.08).
For the dmft index, older age was significantly associated with lower scores (Coef. = –1.52, 95% CI: −1.83 to −1.21). Children of Hmong ethnicity had lower dmft scores than Dao (Coef. = –1.53, 95% CI: −2.46 to −0.60). Father's occupation was significant, with children of workers (Coef. = –3.37, 95% CI: −4.98 to −1.75) and those with fathers in “other” jobs (Coef. = –2.61, 95% CI: −4.80 to −0.41) showing lower dmft scores. Mother's occupation was also associated, with children of workers having lower scores (Coef. = –2.36, 95% CI: −4.20 to −0.53). In addition, brushing habits mattered, as children who did not brush regularly had higher dmft scores (Coef. = 1.80, 95% CI: 0.16–3.44).
Discussion
This study highlights a significantly high prevalence of dental caries among primary schoolchildren in a remote mountainous region of Northern Vietnam, with over 90% affected. While there were no major gender differences in decay prevalence, the study identified key sociodemographic and behavioral factors associated with DMFT and dmft scores, suggesting multiple pathways for oral health intervention.
The exceptionally high prevalence of tooth decay (91.4%) and elevated dmft index (mean = 5.38) observed in this study reflect a critical public health issue in the mountainous region under investigation. These findings indicate that most children suffer from untreated caries in their primary teeth, which likely impairs their nutrition, development, and quality of life. The DMFT score for permanent teeth (mean = 1.31), though lower, still signifies early onset of decay that remains unaddressed. In the context of remote mountainous areas, such oral health burdens may be exacerbated by geographical isolation, limited availability of dental professionals, lack of fluoridated water, and insufficient oral health promotion activities.
Comparable challenges have been reported elsewhere in Vietnam. A study conducted in Southern and Central Vietnam found a high prevalence of early childhood caries (ECC) at 74.4% among children aged 1–6 years, with a significant portion of these cases being untreated (15). Similarly, in Ho Chi Minh City, the prevalence of dental caries among 12-year-olds was influenced by community water fluoridation, with areas having lower fluoride levels showing higher caries rates (16). These findings emphasize how both geographic and environmental factors, including water fluoride concentration, strongly shape oral health outcomes in Vietnamese children.
The combination of environmental barriers and socioeconomic disadvantages likely contributes to the persistent and severe nature of dental caries seen in this population. This situation is comparable to findings in other disadvantaged and remote settings worldwide. For instance, Bergeron et al. (2020) reported caries rates of 94%–98% among children in remote Andean communities (21). Trimble et al. (2024) noted an 83% rate in rural El Salvador (25), and Min et al. (2024) observed an 87% rate in Myanmar (17). Aimond et al. (2023) reported a high dental caries prevalence of 78.5% among children, with prevalence increasing with age (17). Peters et al. (2022) found that children in rural areas had a higher mean dmft + DMFT score (1.22) compared to urban children (0.96), with an overall caries prevalence of approximately 39% (26). These comparisons underscore that the problem observed in the mountainous area of northern Vietnam is not isolated but aligns with a broader global pattern affecting remote and underserved children. Effective interventions in this setting must be culturally appropriate, geographically accessible, and embedded in school and community structures to ensure sustainable improvements in oral health.
Sociodemographic factors showed significant associations with oral health outcomes in this study. Age was positively associated with DMFT but inversely related to dmft, indicating that as children grew older, caries experience in permanent teeth increased while the burden in primary teeth declined. This pattern aligns with prior research indicating that caries prevalence tends to decline with age due to improved hygiene practices and the natural exfoliation of primary teeth (20, 27). Ethnic differences were also evident, with Hmong children showing significantly lower dmft scores compared to the Dao group, while Tay children had markedly higher odds of primary tooth decay. Such disparities may stem from cultural dietary habits, oral hygiene norms, or uneven access to dental services among ethnic communities—similar to findings from North America, where Indigenous and minority children bear a higher burden of caries compared to their majority counterparts (11, 28). These results underscore the need to consider cultural and contextual differences in designing oral health interventions in ethnically diverse populations.
Parental occupation also influenced oral health outcomes. Children of fathers working as laborers or in “other” occupations had significantly lower dmft scores than those of farmer fathers, suggesting that income diversification or migration-related work may indirectly benefit oral health. This finding contrasts somewhat with global literature, where lower occupational status is often associated with higher caries risk (20, 29). However, in the local context, it is possible that non-farming parents—often engaged in labor migration or trade—may have higher income or better exposure to urban health literacy, enabling greater investment in their children's oral health. Similarly, maternal occupation was strongly associated with caries outcomes, with children of mothers who were workers having lower dmft scores compared to those of farmer mothers (29). These findings highlight the complex interaction between socioeconomic roles, cultural practices, and access to care, emphasizing the importance of tailoring oral health strategies to local demographic profiles.
Behavioral practices were another key determinant. Children who brushed irregularly, particularly those without a brushing habit, had significantly higher dmft scores, underscoring the protective role of consistent oral hygiene. In addition, frequent candy or snack consumption and frequent soda consumption were both strongly associated with higher odds of primary tooth decay, confirming the cariogenic impact of dietary sugar in this population. Furthermore, children with poor observed brushing skills had elevated dmft levels, highlighting that brushing frequency alone is insufficient without proper technique. This aligns with existing literature showing that many children, especially in disadvantaged settings, perform suboptimal brushing and miss critical areas like canine segments (30). These results emphasize the importance of both oral hygiene behaviors and effective brushing skills in preventing early childhood caries.
Patterns of dental care-seeking further shaped oral health outcomes. Children who visited the dentist only when cavities or infections occurred had significantly higher DMFT scores compared to those with regular preventive visits every 3–6 months. This finding reflects the predominance of curative over preventive care in rural settings, where services are scarce and access is hindered by cost and distance. Previous studies confirm that regular dental visits are associated with better oral health (31, 32), particularly when supported by proactive parental involvement and favorable attitudes toward dental care (22). These findings underline the need for school-based preventive programs and community education initiatives tailored to the geographic and socioeconomic realities of mountainous populations.
The findings of this study have several practical implications for oral health policy and practice in mountainous and underserved regions. The extremely high prevalence of tooth decay and elevated dmft and DMFT indices underscore the urgent need for targeted preventive programs. School-based interventions—such as supervised toothbrushing, regular fluoride varnish application, and parental education—should be prioritized in these settings. Culturally sensitive oral health promotion strategies that engage local communities and consider ethnic differences may also improve outcomes. Furthermore, training and deploying community-based oral health workers could help overcome access barriers in remote areas. Addressing socioeconomic determinants such as parental education and occupation is essential for achieving long-term improvements in children's oral health.
This study has several limitations. First, its cross-sectional design does not allow for causal inferences between behavioral or sociodemographic factors and oral health outcomes. The associations observed may be influenced by reverse causation or unmeasured confounders. Second, reliance on self-reported data (e.g., brushing frequency, toothbrush replacement) may introduce recall and reporting bias. Third, although efforts were made to include diverse ethnic groups, the sample may not be fully representative of all children living in remote mountainous regions. Finally, access to advanced clinical diagnostic tools was limited, and although trained examiners were used, some variation in caries detection may still occur.
Despite these limitations, this study has several notable strengths. It is among the first investigations to provide age- and dentition-specific analyses of dental caries in a remote mountainous area of northern Vietnam, addressing an evidence gap in both national and international literature. The study also used a large sample drawn from multiple schools, enhancing its reliability and representativeness within the target region. Moreover, the standardized diagnostic criteria (ICDAS) and examiner calibration ensured methodological rigor, while the integration of both clinical and behavioral data allowed for a comprehensive assessment of caries determinants.
Conclusion
This study demonstrates that children in remote mountainous areas face an exceptionally high burden of untreated dental caries, influenced by sociodemographic conditions and oral health behaviors. These findings emphasize the urgent need for culturally tailored and geographically accessible oral health interventions to reduce inequalities and improve well-being among vulnerable populations. Future research should employ longitudinal designs to clarify causal pathways, incorporate more representative sampling across different mountainous provinces, and evaluate the effectiveness of school- and community-based preventive strategies such as fluoride supplementation, oral health education, and improved access to dental care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The study protocol was reviewed and approved by the Ethical Review Board of Thai Nguyen University of Medicine and Pharmacy under Decision No. 1,197/ĐHYD-HĐĐĐ. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
LH: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. PT: Data curation, Investigation, Methodology, Visualization, Writing – original draft. HV: Conceptualization, Data curation, Methodology, Visualization, Writing – original draft. TD: Conceptualization, Formal analysis, Investigation, Visualization, Writing – original draft. LD: Conceptualization, Data curation, Investigation, Methodology, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. He S, Yon MJY, Liu F, Lo ECM, Yiu CKY, Chu CH, et al. Prevalence of caries patterns in the 21st century preschool children: a systematic review and meta-analysis. J Evid Based Dent Pract. (2024) 24(3):101992. doi: 10.1016/j.jebdp.2024.101992
2. Fahd D, Estie K, Kate D, Marc T. Oral health of pre-school children in rural and remote Western Australia. Rural Remote Health. (2011) 11(4):1869–1869. doi: 10.22605/RRH1869
3. Jin-Dong W, Xi C, Jo EF, Minquan D, Zhi C. Dental caries and first permanent molar pit and fissure morphology in 7- to 8-year-old children in Wuhan, China. Int J Oral Sci. (2012) 4(3):157–60. doi: 10.1038/IJOS.2012.34
4. Susan OG, Laurie KB, Liang W, Chien-Hsun L, Melissa SA, Barbara FG. Use of dental care and effective preventive services in preventing tooth decay among U.S. children and adolescents–medical expenditure panel survey, United States, 2003–2009 and national health and nutrition examination survey, United States, 2005–2010. MMWR Suppl. (2014) 63(2):54–60.25208259
5. Faheema K-D, Ahmed B. Prevalence of dental caries in the permanent dentition amongst 12-year-olds in Africa: a systematic review and meta-analysis. BMC Oral Health. (2022) 22(1):453. doi: 10.1186/s12903-022-02489-4
6. Muhammed Al-Huda B, Mayssoon D. Caries prevalence and dental health of 8–12 year-old children in Damascus city in Syria during the Syrian crisis; A cross-sectional epidemiological oral health survey. BMC Oral Health. (2019) 19(1):16–16. doi: 10.1186/S12903-019-0713-9
7. Susan OG. Vital signs: dental sealant use and untreated tooth decay among U.S. school-aged children. Morb Mortal Wkly Rep. (2016) 65(41):1141–5. doi: 10.15585/MMWR.MM6541E1
8. Philip JS, Nicholas B, Joanne D, Laurie M, Martin L. Hospital dental admissions and caries experience among children with neurodevelopmental disabilities: a population-based record linkage cohort study. Community Dent Oral Epidemiol. (2024) 53(2):160–9. doi: 10.1111/cdoe.13018
9. Ray M, Tumaini SN, Lorna CC. Prevalence of dental caries in deciduous teeth and oral health related quality of life among preschool children aged 4–6 years in Kisarawe, Tanzania. BMC Oral Health. (2020) 20(1):1–10. doi: 10.1186/S12903-020-1032-X
10. Eduardo B, Elsa KD-A, Jason EM, Wagner M. Family income and tooth decay in US children: does the association change with age? Caries Res. (2012) 46(3):221–7. doi: 10.1159/000337389
11. Sung-Eun C, Joel MW, Elizabeth M, Sharon-Lise TN. Analysis of race and ethnicity, socioeconomic factors, and tooth decay among US children. JAMA Network Open. (2023) 6(6):e2318425–e2318425. doi: 10.1001/jamanetworkopen.2023.18425
12. Alireza M, Soraya Z, Hojjat M, Ali Mohammad M, Mohebat V, Abedinzade A. Dental caries experience and its relationship to demographic factors in 2–6 year old children in Fars—Iran in 2018. Int J Dent Hyg. (2022) 20(4):643–9. doi: 10.1111/idh.12595
13. Blanco-Victorio DJ, López-Luján NA, Bernaola-Silva W, Vicuña-Huaqui LA, Cacñahuaray-Palomino R, Diaz-Campos JS, et al. Sociodemographic and clinical factors associated with early childhood caries in Peruvian pre-schoolers. BMC Oral Health. (2025) 25(1):125. doi: 10.1186/s12903-025-05506-4
14. Gina T-E, Michele LJ, Mei L, Liang W, Lorena E, Eugenio DB-A. Use of toothpaste and toothbrushing patterns among children and adolescents—United States, 2013–2016. Morb Mortal Wkly Rep. (2019) 68(4):87–90. doi: 10.15585/MMWR.MM6804A3
15. Khanh LN, Ivey SL, Sokal-Gutierrez K, Barkan H, Ngo KM, Hoang HT, et al. Early childhood caries, mouth pain, and nutritional threats in Vietnam. Am J Public Health. (2015) 105(12):2510–7. doi: 10.2105/ajph.2015.302798
16. Hoang HT, Huynh NC, Tran TT, Nguyen MD, Beltrán-Aguilar ED. Sociodemographic, biological, and timing characteristics of dental caries and fluorosis using mixed-type cluster analysis on 12-year-olds in Ho Chi Minh city, 1989–2019. Heliyon. (2024) 10(2):e25035. doi: 10.1016/j.heliyon.2024.e25035
17. Min SN, Duangthip D, Gao SS, Detsomboonrat P. Self-reported oral health-related quality of life and caries experiences of 5-year-old children in Mandalay, Myanmar. BMC Oral Health. (2024) 24(1):31. doi: 10.1186/s12903-023-03803-4
18. Ekstrand KR, Gimenez T, Ferreira FR, Mendes FM, Braga MM. The international caries detection and assessment system—ICDAS: a systematic review. Caries Res. (2018) 52(5):406–19. doi: 10.1159/000486429
19. Hefti AF, Preshaw PM. Examiner alignment and assessment in clinical periodontal research. Periodontol 2000. (2012) 59(1):41–60. doi: 10.1111/j.1600-0757.2011.00436.x
20. Majid G, Soheila B, Armin S, Naghmeh E, Hamid S, Nadereh Moosavi F, et al. Dental caries experience and socio-economic status among Iranian children: a multilevel analysis. BMC Public Health. (2019) 19(1):1–8. doi: 10.1186/S12889-019-7693-1
21. Bergeron DA, Talbot LR, Gaboury I. Oral health status of schoolchildren living in remote rural andean communities: a cross-sectional study. J Int Soc Prev Community Dent. (2020) 10(2):156–62. doi: 10.4103/jispcd.JISPCD_438_19
22. Martin M, Pugach O, Avenetti D, Lee H, Salazar S, Rosales G, et al. Oral health behaviors in very young children in low-income urban areas in Chicago, Illinois, 2018–2019. Prev Chronic Dis. (2020) 17:E152. doi: 10.5888/PCD17.200213
23. Bendel RB, Afifi AA. Comparison of stopping rules in forward “stepwise” regression. J Am Stat Assoc. (1977) 72(357):46–53. doi: 10.2307/2286904
24. Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. (1989) 129(1):125–37. doi: 10.1093/oxfordjournals.aje.a115101
25. Trimble M, Susarla SM, Campos C, Turton B, Sokal-Gutierrez K. Pocket money and the risk of dental caries and oral pain in children. J Med Surg Public Health. (2024) 3:100106. doi: 10.1016/j.glmedi.2024.100106
26. Peters A, Brandt K, Wienke A, Schaller HG. Regional disparities in caries experience and associating factors of Ghanaian children aged 3 to 13 years in urban Accra and rural Kpando. Int J Environ Res Public Health. (2022) 19(9):5771. doi: 10.3390/ijerph19095771
27. Ann-Catrin André K, Max P, Magnus H, Anna-Lena Ö. Multiple socioeconomic factors and dental caries in Swedish children and adolescents. Caries Res. (2018) 52:42–50. doi: 10.1159/000481411
28. Shi C, Faris P, McNeil DA, Patterson S, Potestio ML, Thawer S, et al. Ethnic disparities in children’s oral health: findings from a population-based survey of grade 1 and 2 schoolchildren in Alberta, Canada. BMC Oral Health. (2018) 18(1):1–11. doi: 10.1186/S12903-017-0444-8
29. Bashirian S, Seyedzadeh-Sabounchi S, Shirahmadi S, Soltanian AR, Karimi-Shahanjarini A, Vahdatinia F. Socio-demographic determinants as predictors of oral hygiene status and gingivitis in schoolchildren aged 7–12 years old: a cross-sectional study. PLoS One. (2018) 13(12):e0208886. doi: 10.1371/JOURNAL.PONE.0208886
30. Vered M, Liran L, Michael Y, Malka A. Factors associated with toothbrushing performance among children: an observational cohort study. Int J Paediatr Dent. (2024) 35(2):405–13. doi: 10.1111/ipd.13251
31. Burak B. Pathways between parental and individual determinants of dental caries and dental visit behaviours among children: validation of a new conceptual model. Community Dent Oral Epidemiol. (2020) 48(4):280–7. doi: 10.1111/CDOE.12530
Keywords: dental caries, children, Vietnam, DMFT, oral health behavior, mountainous region, school-based intervention
Citation: Hoa LTT, Tue PX, Vinh HT, Duong TTT and Dung LTK (2025) Determinants of dental caries among primary schoolchildren in a mountainous region of Northern Vietnam. Front. Oral Health 6:1675274. doi: 10.3389/froh.2025.1675274
Received: 31 July 2025; Accepted: 16 September 2025;
Published: 3 October 2025.
Edited by:
Chloe Meng Jiang, The University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Kitty Jieyi Chen, Sun Yat-sen University, ChinaRuxandra Sfeatcu, Carol Davila University of Medicine and Pharmacy, Romania
Copyright: © 2025 Hoa, Tue, Vinh, Duong and Dung. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Le Thi Thanh Hoa, bGluaHRyYW5nMjQ5QGdtYWlsLmNvbQ==
†ORCID:
Le Thi Thanh Hoa
orcid.org/0009-0004-9022-0978
 Le Thi Thanh Hoa
Le Thi Thanh Hoa Pham Xuan Tue2
Pham Xuan Tue2