- 1College of Traditional Chinese Medicine, Changchun University of Traditional Chinese Medicine, Changchun, China
- 2Department of Hepatology, Affiliated Hospital of Changchun University of Traditional Chinese Medicine, Changchun, China
- 3Department of Emergency, The First Clinical Hospital of Jilin Academy of Traditional Chinese Medicine, Changchun, China
- 4Department of Cardiovascular Medicine, Affiliated Hospital of Changchun University of Traditional Chinese Medicine, Changchun, China
Objective: This study aimed to evaluate the intervention effect of curcumin in myocardial infarction rodent models.
Methods: A systematic retrieval of relevant studies on curcumin intervention in rats or mice myocardial infarction models was conducted, and the data were extracted. The outcome indicators included biochemical blood indicators, such as creatine kinase (CK), creatine kinase isoenzyme (CK-MB), malondialdehyde (MDA), lactate dehydrogenase (LDH) and superoxide dismutase (SOD), as well as cardiac tissue structure indicators, such as left ventricular weight to body weight ratio (LVW/BW), apoptosis index, left ventricular end-diastolic dimension (LVEDD), left ventricular end-systolic diameter (LVESD), and myocardial infarction area, and hemodynamic indexes, such as systolic blood pressure (SBP), diastolic blood pressure (DBP), left ventricular end-diastolic pressure (LVEDP), left ventricular ejection fraction (LVEF), left ventricular fractional shortening (LVFS), maximum rate of left ventricular pressure rise (+dp/dtmax), and maximum rate of left ventricular pressure decline (–dp/dtmax). These results were then analyzed by meta-analysis. Studies were evaluated for methodological quality using the syrcle’s bias risk tool.
Results: A total of 24 studies were included in the meta-analysis. The quality assessment of included studies revealed that the evidence was low quality and none of studies was judged as having a low risk of bias across all domains. The results revealed that curcumin could reduce CK-MB, CK, LDH, and MDA levels. They also revealed that it could lower SBP, DBP, LVEDP, LVW/BW, apoptosis index, LVEDD, LVESD, and myocardial infarction area and increase LVEF, LVFS, +dp/dtmax, and–dp/dtmax. However, it had no significant impact on the heart rate and the levels of SOD in the models.
Conclusion: Curcumin alleviates myocardial injury and oxidative stress in myocardial infarction rodent models in terms of blood biochemistry indicators, improves the diastolic and systolic capacity of the ventricle in terms of hemodynamic indexes, and reduces the necrosis and apoptosis of cardiomyocytes in terms of tissue structure. The methodological quality of the studies was low and additional research is warranted.
Introduction
Myocardial infarction refers to the necrosis of any size of myocardial cells caused by myocardial ischemia (Sumitra et al., 2007). Myocardial infarction seriously endangers human health and has a very high incidence and mortality worldwide (Boarescu et al., 2019a). In the report on cardiovascular health and diseases in China 2021: an updated summary, the mortality rate of myocardial infarction in China in 2019 was 60.2/100000 in urban areas and 78.24/100000 in rural areas, about half of the mortality rate of all kinds of tumors. The number of discharges from acute myocardial infarction in China in 2019 was 1,057,600. The epidemiological study on myocardial infarction in Korea points out that the prevalency in adults over 30 years was estimated to range from 0.34% to 0.70% in 2020 (Kim et al., 2022). The mortality was 19.3 per 100000 populations In Denmark, from 1 January 2005, through 4 August 2021, there were 116481 inch acute myocardial informations in approximately 4.5 million Danes aged ≥18 years (Christensen et al., 2022). With the extensive implementation of thrombolysis, cardiac interventional surgery, and the development of drug treatment, the dying myocardium can be effectively saved, and the prognosis of patients with myocardial infarction has greatly improved in recent years. However, many patients do not receive revascularization in time for various reasons, resulting in irreversible death of the myocardium, ventricular remodeling, deterioration of cardiac function, and finally, heart failure, which seriously affects a patient’s quality of life (Boarescu et al., 2019b).
Curcumin is a phenolic compound extracted from the roots of plants in the Zingiberaceae family (Duan et al., 2012; Lestari and Indrayanto, 2014). In recent years, it has been shown to have a wide range of pharmacological effects. In terms of cardiovascular disease, it has also been proven to protect against myocardial ischemia-reperfusion injury (Li et al., 2020), and there are many studies on its role in animal models. To further clarify the mechanism of curcumin on myocardial infarction, this study carried out a meta-analysis to evaluate the intervention effects of curcumin on rat and mouse myocardial infarction models to provide a reference and evidence for the clinical applications of curcumin.
Materials and methods
Literature review
Related studies were retrieved from PubMed, Embase, Cochrane Library, Web of Science, CNKI, VIP, and Wanfang. The time range was from the establishment of the databases to 9 June 2022. The keywords used for retrieval included three parts: 1) curcumin, 2) myocardial infarction, 3) rats or mice, and the three parts were connected by “and.”
The inclusion criteria for the studies were as follows:
1) Research subject: a rat or mouse myocardial infarction model; the preparation method of the model had to be recognized.
2) Intervention measures: The drugs used had to be curcumin or curcumin preparations. The experimental group could not additionally use other drugs that may affect the heart; the control group did not use any drugs, or only used a placebo.
3) Outcome indicators: The indicators for evaluating drug effects had to be in digital form to ensure that the key indicators could be extracted or calculated directly or indirectly, including their mean and standard deviation.
The exclusion criteria were as follows:
1) The data for evaluation indicators was incomplete.
2) Information regarding meta-analysis, systematic evaluation, and correspondence was incomplete.
3) The experimental group or the control group involved the use of other drugs.
4) The study involved animals other than a rat or mouse.
Two authors extracted data independently. Any differences were resolved through discussion until a consensus was reached, or a third author was consulted to add a decisive input. The following pieces of information were extracted from qualifying studies: author, year of publication, drugs used, modeling method, number of models, mode of administration, dosage, detection indexes, detection index unit, and detection results (Cheng and Liu, 2005; Wang, 2008; Hong et al., 2009; Gao et al., 2011; Sunagawa et al., 2011; Kim et al., 2012; Kong, 2012; Sunagawa et al., 2012; Chen, 2014; Sunagawa et al., 2014; Chen et al., 2015; Gao et al., 2015; He et al., 2015; Liu et al., 2015; Xu and Yang, 2015; Geng, 2016; Gu et al., 2016; Liu, 2018; Boarescu et al., 2019a; Mehdi et al., 2019; Cui et al., 2020; Guo et al., 2021; HJ W et al., 2021; Shaoxi et al., 2021). Finally, the outcome indicators were summarized. When there were less than three articles on the outcome indicators, the outcome indicators were excluded from the study.
To assess the quality of the included studies, we used the SYstematic Review Center for Laboratory Animal Experimentation bias risk tool (syrcle’s bias risk tool) for animal studies (Musillo et al., 2021; Wang et al., 2021). Syrle’s bias risk tool is based on the Cochrane bias risk tool and adjusted for bias aspects that play a specific role in animal intervention studies. Two authors extracted data independently. Any differences were resolved through discussion until a consensus was reached, or a third author was consulted to add a decisive input.
Statistical methods
Meta-analysis was conducted using RevMan 5.1 software. Quantitative data were expressed as mean ± standard deviation (±SD). Cochran’s Q test and the I2 test were used to evaluate the existence and severity of heterogeneity were. When both p < 0.1 and I2 > 50%, it was considered that there was heterogeneity, and the random-effects model was used for meta-analysis; otherwise, the fixed-effects model was used.
Results
Results of the literature review
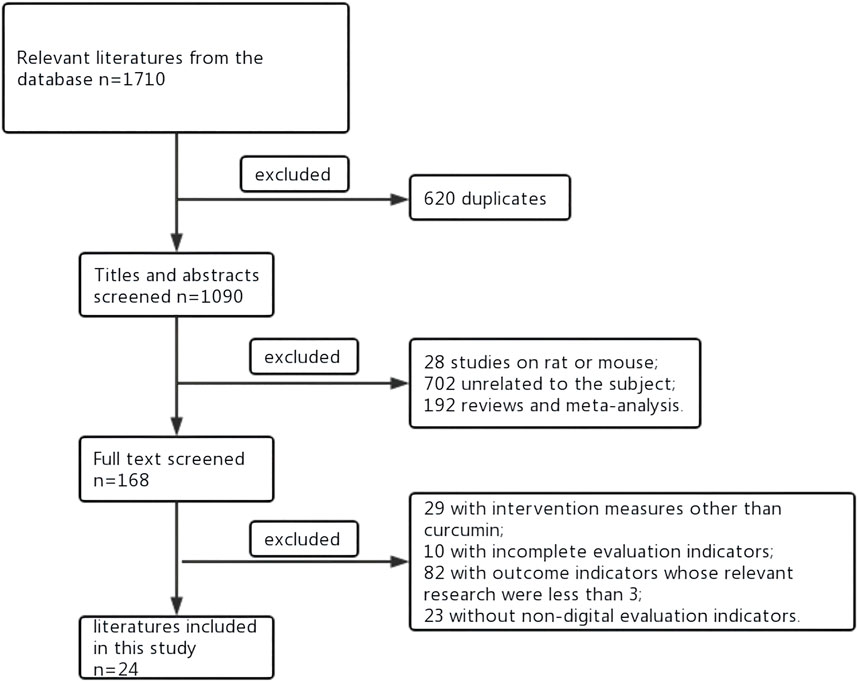
The literature review flow chart is shown in Figure 1. As shown in Figure 1, a total of 1,710 studies were retrieved from the databases. Of these, 620 were repeated studies that were then excluded, and 1,090 studies remained. Among those that remained, 702 studies were unrelated to the subject, 192 were reviews and meta-analyses, 28 were non-rat or non-mouse studies. There were 29 studies that involved intervention measures other than curcumin, 23 that involved non-digital evaluation indicators, and 10 that had incomplete evaluation indicators. There were 82 studies that involved outcome indicators whose relevant research were less than 3. Therefore, 24 studies were included in the final meta-analysis. The study ID, subjects, mode of administration, and other characteristics are shown in Table 1. In the included literature, if there were three groups in the article, they were sham operation group, model group and curcumin. If there were five groups in the article, it was the sham operation group, the model group and three different doses of Curcumin.
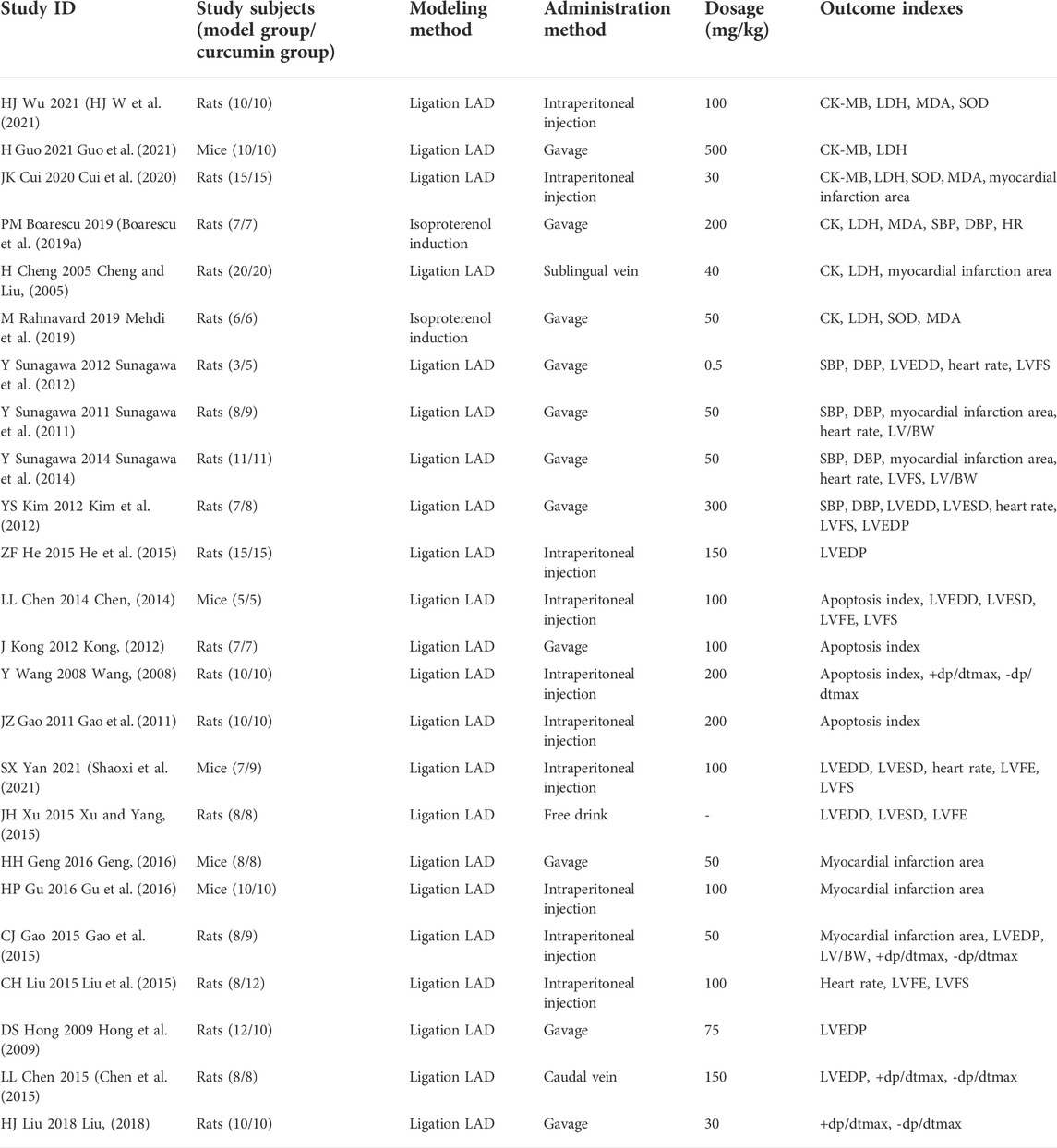
TABLE 1. Research ID, research subject, administration method and other research characteristics of included literatures.
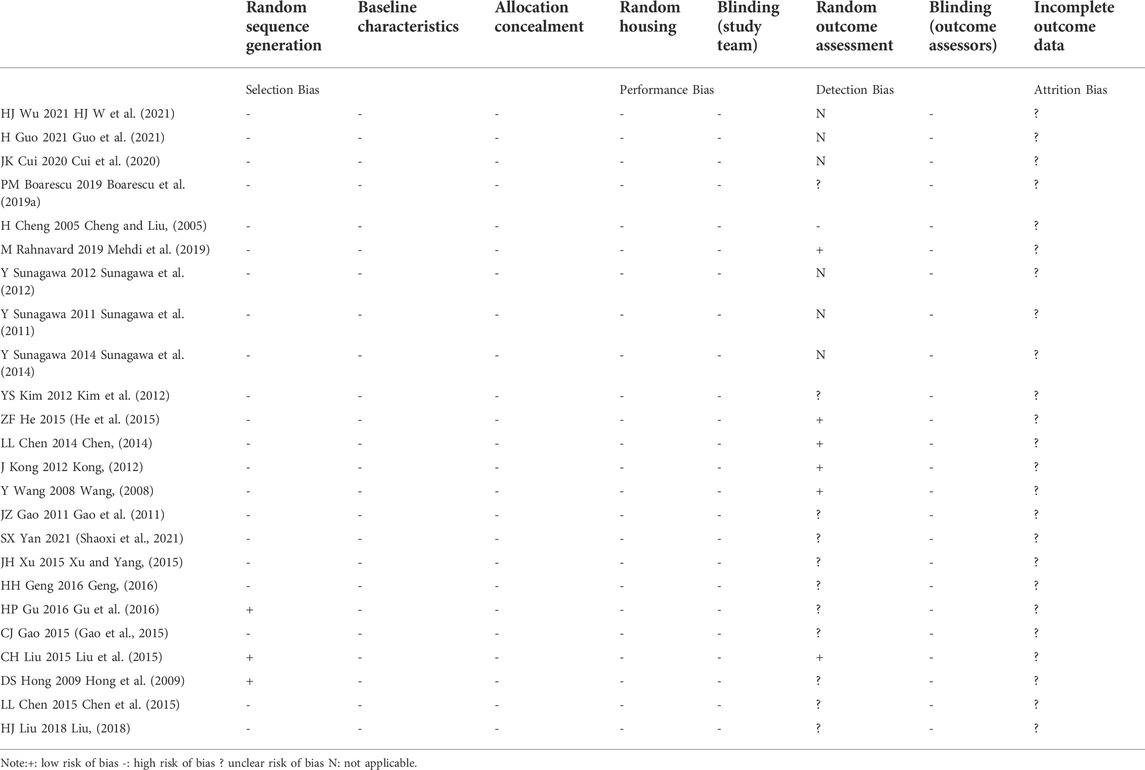
We assessed the quality of the included literature through syrcle’s bias risk tool, as shown in Table 2. Only 12.5% (n = 3) described the random sequence generation method like completely random design, Simple random sampling method and random block method (Hong et al., 2009; Liu et al., 2015; Gu et al., 2016); 25% (n = 6) reported random outcome assessments (Wang, 2008; Kong, 2012; Chen, 2014; He et al., 2015; Liu et al., 2015; Mehdi et al., 2019). Additionally, three studies that mentioned blinding only blinded echocardiographic studies, not other included parameters like MI area, HR, SBP, and DBP (Sunagawa et al., 2011; Sunagawa et al., 2012; Sunagawa et al., 2014). None of the studies reported details of baseline characteristics of animals, details of methods for allocation concealment, random housing, and blinding (high risk of bias = 100%), all studies had no incomplete results and selective results. None of the studies had a published pre-specified protocol.
The effects of curcumin on rats or mice centered on three aspects: blood biochemistry, cardiac tissue structure, and hemodynamics. In terms of blood biochemistry, the indicators measured were creatine kinase (CK), creatine kinase isoenzyme (CK-MB), malondialdehyde (MDA), and biochemical blood indicators, such as lactate dehydrogenase (LDH) and superoxide dismutase (SOD). The hemodynamic indexes measured included systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), left ventricular end-diastolic pressure (LVEDP), left ventricular ejection fraction (LVEF), left ventricular fractional shortening (LVFS), maximum rate of left ventricular pressure rise (+dp/dtmax), and maximum rate of left ventricular pressure decline (–dp/dtmax). The cardiac tissue structure examined included the left ventricular weight to body weight ratio (LVW/BW), apoptosis index (number of apoptotic nuclei/[number of apoptotic nuclei + number of normal nuclei] × 100%), left ventricular end-diastolic dimension (LVEDD), left ventricular end-systolic diameter (LVESD), and myocardial infarction area.
The effect of curcumin on blood biochemistry in rats or mice with myocardial infarction
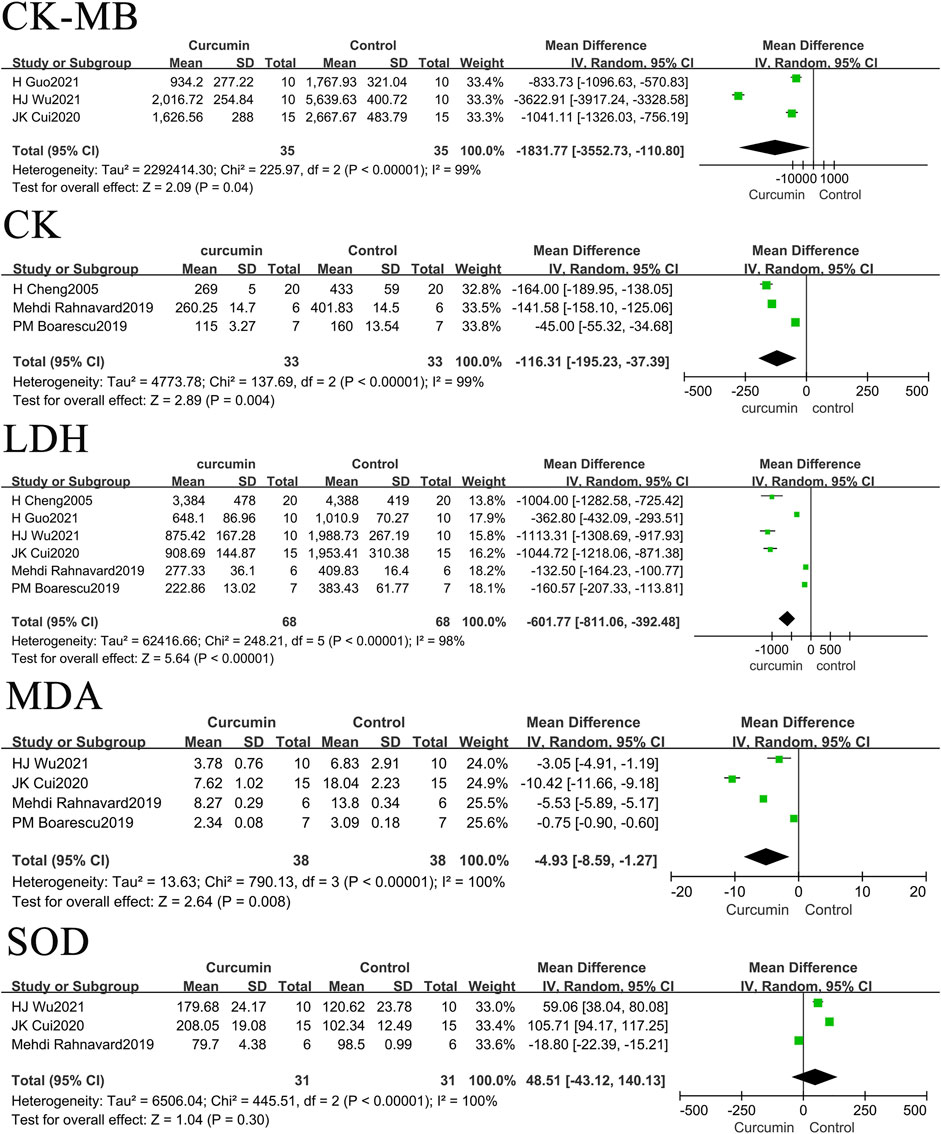
The present study sorted and merged related studies on the effects of curcumin on CK, CK-MB, MDA, and LDH levels in rats or mouse models of myocardial infarction. The results showed that curcumin could reduce CK, CK-MB, MDA, and LDH levels in myocardial infarction models but had no significant impact on SOD levels in myocardial infarction models.
The results also found that the use of curcumin can reduce the levels of CK-MB by 1,831.77 U/L (p = 0.04), CK by 116.31 U/L (p = 0.004), LDH by 601.77 U/L (p < 0.00001), and MDA by 4.93 nmol/L (p = 0.008) in rats or mice with myocardial infarction. The forest map is presented in Figure 2.
The effect of curcumin on hemodynamic indexes in rats or mice with myocardial infarction
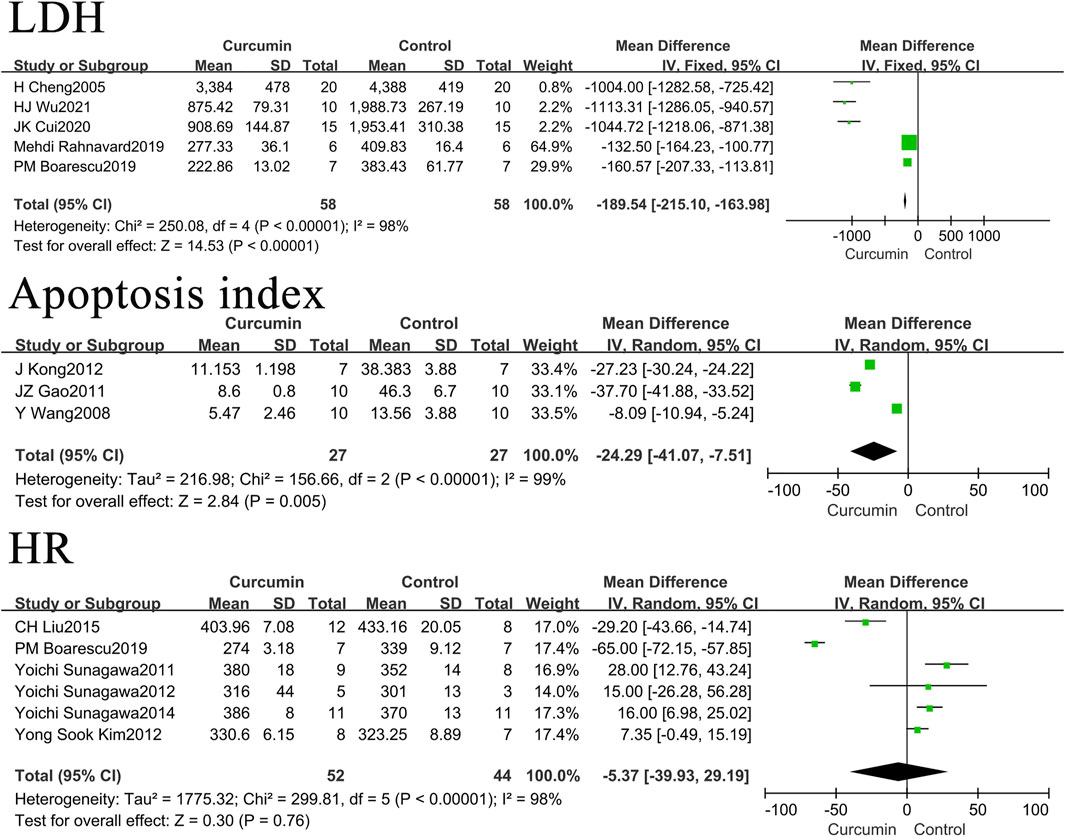
In rat or mouse myocardial infarction models, curcumin was found to reduce SBP by 10.05 mmHg (p < 0.00001) and DBP by 5.4 mmHg (p = 0.008). It was also found to increase LVEF by 13.56% (p < 0.00001), LVFS by 7.66% (p = 0.0006), LVEDP by 6.99 mmHg (p < 0.00001), +dp/dtmax by 1551.38 mmHg/s (p = 0.0008), and–dp/dtmax by 1184.05 mmHg/s (p = 0.0007). It had no significant impact on the heart rate in rats or mice models of myocardial infarction. The forest map is presented in Figure 3.
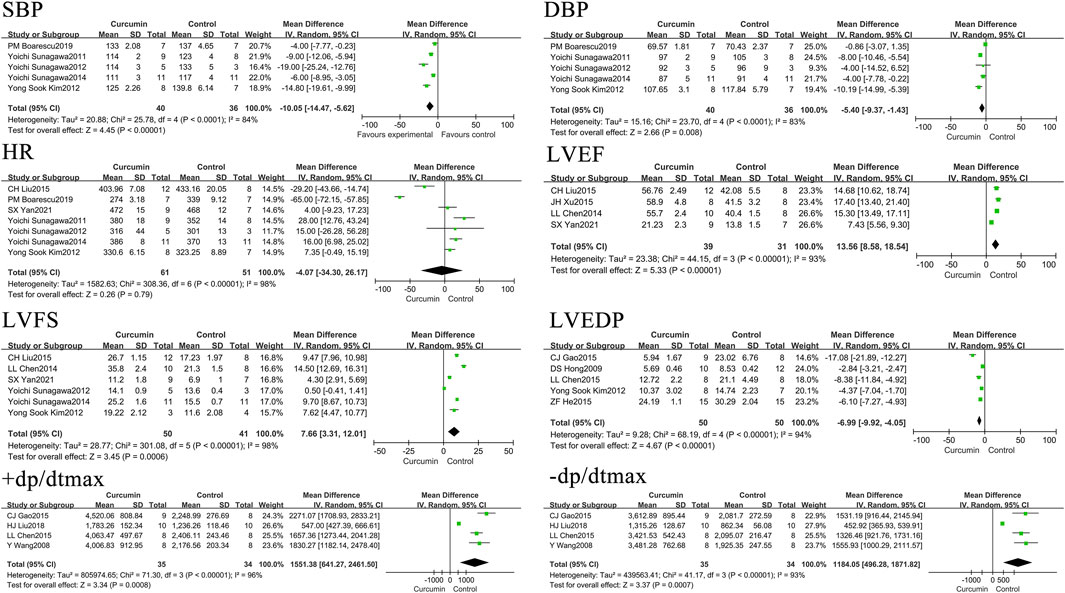
FIGURE 3. Forest plot of hemodynamic related indicators: SBP, DBP, HR, LVEF, LVFS, LVEDP, +dp/dtmax, - dp/dtmax.
The effect of curcumin on cardiac tissue and structure in rats or mice with myocardial infarction
Curcumin was found to reduce the LVW/BW by 0.2 (p = 0.003), the apoptosis index by 18.35% (p = 0.03), LVEDD by 0.65 mm (p = 0.0002), LVESD by 1.04 mm (p < 0.00001), and myocardial infarction area by 11.05% (p = 0.02). The forest map is presented in Figure 4.
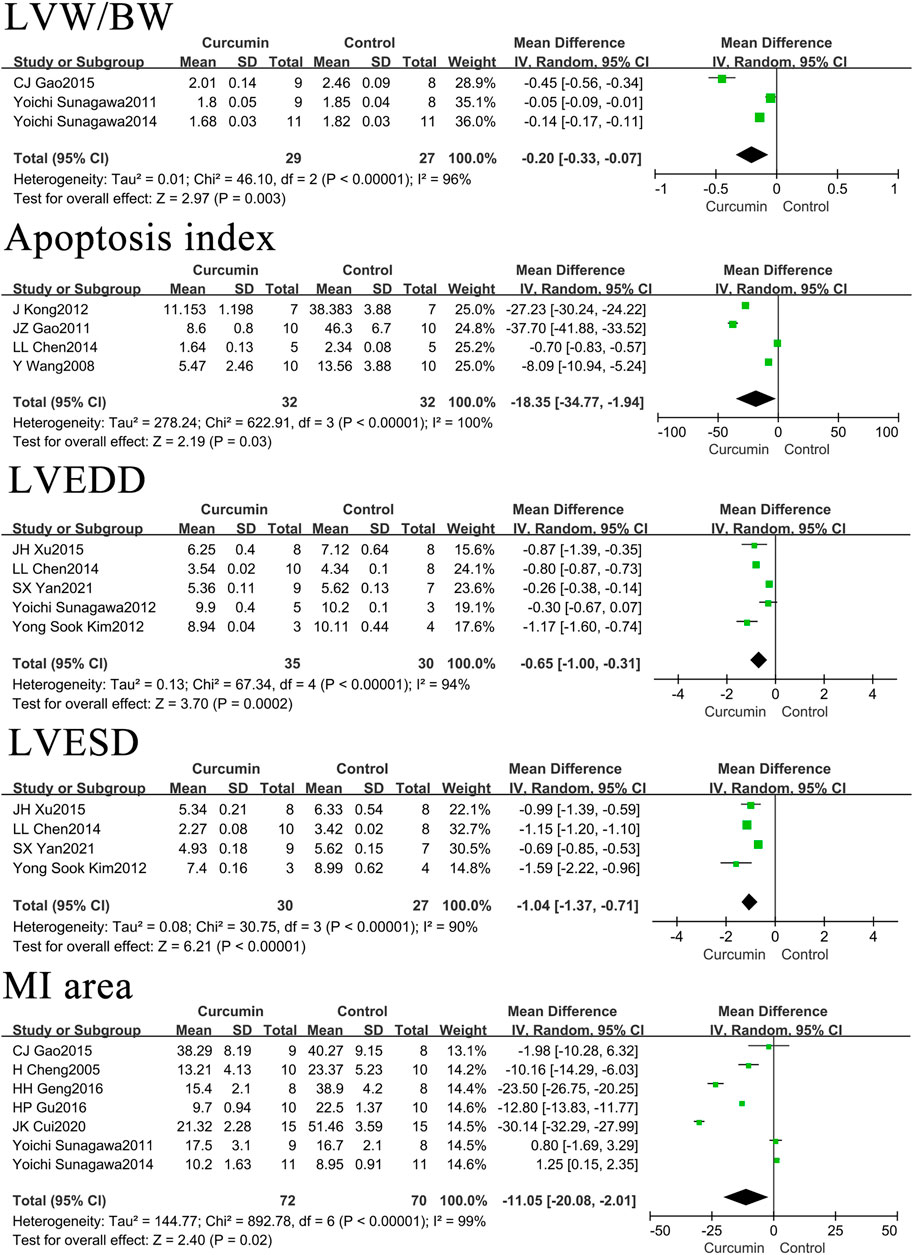
FIGURE 4. Forest plot of cardiac tissue structure related indicators: LVW/BW, Apoptosis index, LVEDD, LVESD, MI area.
Sub study of rats and mice
In order to study the effects of different animal species on the effects of curcumin on myocardial infarction, we classified the included literatures according to rats and mice.
Among the included research literatures on LDH, one is about the mouse myocardial infarction model, and the heart rate and apoptosis index are the same. We removed this study to observe the impact on the research results, as shown in Figure 5. The results found that the use of curcumin can reduce the levels of LDH by -189.54U/L (p < 0.00001), the apoptosis index by 24.29% (p = 0.005) in rats or mice with myocardial infarction. It had no significant impact on the heart rate in rats’ models of myocardial infarction. These results are not very different from those before the removal of mice.
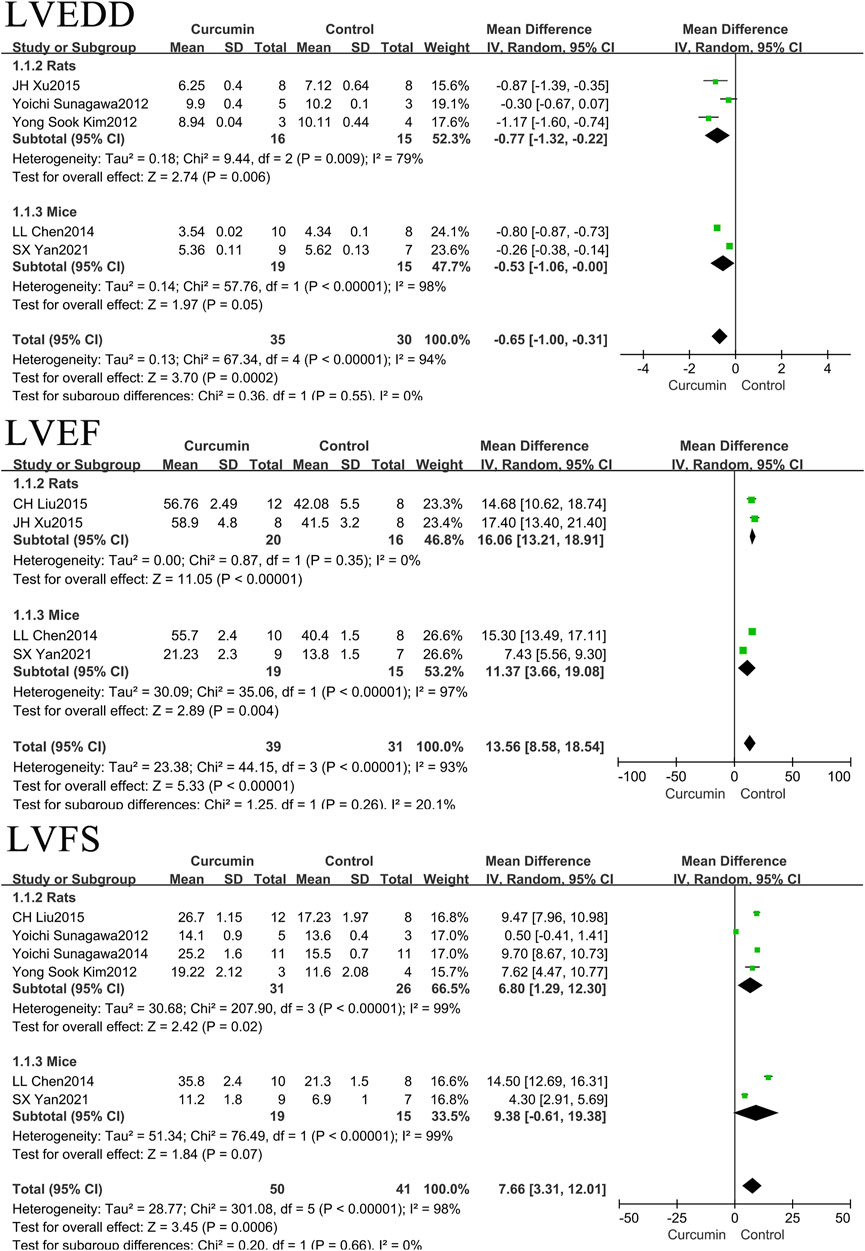
In our relevant research literature, rats and mice were included in the literature of LVEDD, LVEF and LVFS. We classified the rats and mice, as shown in Figure 6. The results found that the use of curcumin can reduce LVEDD by 0.77 mm (p = 0.006) in rats with myocardial infarction, LVEDD by 0.53 mm (p = 0.05) in mice with myocardial infarction. Curcumin was found to increase LVEF by 16.06% (p < 0.00001) in rats with myocardial infarction, LVEF by 11.37% (p = 0.004) in mice with myocardial infarction. Curcumin was found to increase LVFS by 6.80% (p = 0.02) in rats with myocardial infarction, LVFS by 7.66% (p = 0.0006) in mice with myocardial infarction.
Discussion
In this meta-analysis, we found that curcumin could reduce CK-MB, CK, LDH, and MDA levels. Also, it could lower SBP, DBP, LVEDP, LVW/BW, apoptosis index, LVEDD, LVESD, and myocardial infarction area and increase LVEF, LVFS, +dp/dtmax, and–dp/dtmax. However, it had no significant impact on the heart rate and the levels of SOD in the models.
The levels of CK, CK-MB, and LDH are commonly used markers of myocardial injury, as their changes can reflect the degree of myocardial injury. In myocardial infarction models, curcumin reduces CK, CK-MB, and LDH levels and alleviates myocardial injury. Inflammatory reaction and oxidative stress are the initiating and promoting factors of myocardial infarction, existing throughout the process of myocardial infarction. A by-product of lipid peroxidation in oxidative stress is MDA, changes in which can reflect the degree of oxidative stress. Curcumin reduces the MDA concentration in myocardial infarction models, indirectly confirming the antioxidant effect of curcumin.
Curcumin has also been found to reduce SBP, DBP, and LVEDP. Blood pressure has an important impact on the prognosis of acute myocardial infarction. However, in human epidemiological studies, there has been debate about the reasonable control range of blood pressure. An international cohort study observing data from 22,672 patients with coronary atherosclerotic heart disease demonstrated that when SBP was controlled between 120 and 140 mmHg (1 mmHg = 0.1333 kPa), the incidence of cardiovascular events was the lowest. However, an SBP <120 mmHg was associated with an increased risk of cardiovascular death and all-cause death, and a mean follow-up of 5 years revealed that an SBP ≥140 mmHg or <120 mmHg and a DBP ≥80 mmHg or <70 mmHg were associated with an increased risk of cardiovascular events and showed a J-curve relationship (Selvaraj et al., 2016).
Curcumin reduces indicator numbers of cardiac structure, including LVW/BW, LVEDD, and LVESD, reduces left ventricular dilatation, alleviates myocardial hypertrophy and remodeling, increases cardiac systolic function indicators, including LVFS, LVEF, +dp/dtmax, and–dp/dtmax, and improves the diastolic and systolic capacity of the ventricle.
Myocardial apoptosis is the main form of myocardial cell loss in the early stages of myocardial ischemia (Wang et al., 2018). During myocardial ischemia, the apoptosis mechanism is first initiated. With time and dependent on the aggravation of the degree of ischemia, the cells in the ischemic center then progress to necrosis. Cardiomyocytes around the ischemia are then in apoptosis, a state of reversible damage. This is why, in acute myocardial infarction, apoptotic cells appear in the center and periphery of the infarction, and more apoptotic cells are found in the peripheral area of the infarction (Jo et al., 2020; Zhou et al., 2020; Sheng et al., 2021). Curcumin reduces the myocardial infarction area and apoptosis index in rat or mouse myocardial infarction models and alleviates myocardial necrosis and apoptosis.
In some of the included studies, the dosage of curcumin was divided into several levels. The results of almost all such articles showed that the dosage of curcumin showed a dose effect with different dosage, and the effect of curcumin increased with the increase of dosage. In our study, the research results of the maximum dosage included in the study were selected. Because the dose distribution of the included studies was quite different, it was not possible to classify the doses for the time being.
Conclusion
Curcumin alleviates myocardial injury and oxidative stress in myocardial infarction rodent models in terms of blood biochemistry indicators, improves the diastolic and systolic capacity of the ventricle in terms of hemodynamics, and reduces the necrosis and apoptosis of cardiomyocytes in terms of tissue structure. These results show the valuable effects of curcumin on myocardial infarction in the clinic. However, the methodological quality of the studies was low. Additional research is warranted focusing on rigour of assessment, intensity of interventions delivered and methodological limitations.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author contributions
Conception and design of the research: B-YP, YL, Y-HW, and L-HJ. Acquisition of data: B-YP, H-BD, Y-HW, and X-WJ. Analysis and interpretation of the data: B-YP, Y-HW, X-WJ and YL. Statistical analysis: B-YP and Y-HW. Obtaining financing: L-HJ. Writing of the manuscript: B-YP. Critical revision of the manuscript for intellectual content: YL and L-HJ. All authors read and approved the final draft.
Funding
National Natural Science Foundation of China (No. 81673846).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Boarescu, P-M., Boarescu, I., Bocșan, I. C., Pop, R. M., Gheban, D., Bulboacă, A. E., et al. (2019). Curcumin nanoparticles protect against isoproterenol induced myocardial infarction by alleviating myocardial tissue oxidative stress, electrocardiogram, and biological changes. Molecules 24, E2802. doi:10.3390/molecules24152802
Boarescu, P-M., Chirilă, I., Bulboacă, A. E., Bocșan, I. C., Pop, R. M., Gheban, D., et al. (2019). Effects of curcumin nanoparticles in isoproterenol-induced myocardial infarction. Oxidative Med. Cell. Longev. 2019, 7847142. doi:10.1155/2019/7847142
Chen, L. L. (2014). Protective effect and mechanism of curcumin on ventricular remodeling after myocardial infarction in mice. Southern Medical University.
Chen, L. L., Wang, Z. M., Chen, B., Wang, L. S., and Yang, Z. J. (2015). Inhibitory effect of curcumin on inflammatory response after myocardial infarction in rats and its mechanism. J. Nanjing Med. Univ. Sci. Ed. 35, 1552–1556.
Cheng, H., and Liu, W. W. (2005). Protective effect of curcumin on myocardial ischemia-reperfusion injury in rats. Chin. Pharmacol. Bull. 55, 95–99. doi:10.1080/13880209.2016.1214741
Christensen, D. M., Strange, J. E., Phelps, M., Schjerning, A. M., Sehested, T. S. G., Gerds, T., et al. (2022). Age- and sex-specific trends in the incidence of myocardial infarction in Denmark, 2005 to 2021. Atherosclerosis 346, 63–67. doi:10.1016/j.atherosclerosis.2022.03.003
Cui, J. K., Geng, N. Z., Meng, F. J., Shi, L. C., Tian, G., and Yang, G. Q. (2020). The protective effect of nomethoxycurcumin on myocardial ischemia-reperfusion injury in rats by regulating autophagy through PI3K-Akt-MTOR signaling pathway. Zhong Yi Yao Xue Bao 48, 19–24.
Duan, W., Yang, Y., Yan, J., Yu, S., Liu, J., Zhou, J., et al. (2012). The effects of curcumin post-treatment against myocardial ischemia and reperfusion by activation of the JAK2/STAT3 signaling pathway. Basic Res. Cardiol. 107, 263. doi:10.1007/s00395-012-0263-7
Gao, C. J., Gao, D. Z., and Wang, Y. (2015). Protective effect of curcumin on acute myocardial infarction model rats. Zhong Guo Yao Fang. 26, 1782–1785.
Gao, J. Z., Wang, Y. L., Li, D. L., and Zhang, J. Y. (2011). Curcumin preconditioning alleviates myocardial apoptosis in acute myocardial ischemia rats. Basic Med. Sci. Clin. 31, 1247–1250. doi:10.3892/mmr.2019.10371
Geng, H. H. (2016). Study on the functional regulation mechanism and effect of microrNA-7A in myocardial cell injury induced by acute myocardial infarction. Shandong University.
Gu, H. P., Wu, M. Y., and Guo, X. H. (2016). Protective effect of curcumin on myocardial ischemia-reperfusion injury in mice and its correlation with Toll-like receptor 4/nuclear factor -κB signaling pathway. Chin. J. Biol. Chin. J. Biol. 29, 932–935.
Guo, H., Xu, C. N., Zhang, Y., Sun, Y. G., Qioa, R., Jin, P., et al. (2021). Curcumin activates mammalian sirolimus target protein signaling to inhibit autophagy and alleviate myocardial infarction injury in mice. Chin. J. Clin. Pharmacol. 37, 3097–3101. doi:10.1002/ijc.21932
He, Z. F., Liu, C. H., Liu, C. H., Lu, J. K., Li, Y. H., Fan, L., et al. (2015). Effects of curcumin on hemodynamics and expression of matrix metalloproteinase-2 after myocardial infarction. Chin. Med. 50, 32–35.
Hj W, K. Z., Zhang, J. M., Ma, L. W., and Zhuang, Y. (2021). Mechanism of curcumin against myocardial ischaemia-reperfusion injury based on the P13K/Akt/mTOR signalling pathway. Eur. Rev. Med. Pharmacol. Sci. 25, 5490–5499. doi:10.26355/eurrev_202109_26658
Hong, D., Zeng, X., Xu, W., Ma, J., Tong, Y., and Chen, Y. (2009). Altered profiles of gene expression in curcumin-treated rats with experimentally induced myocardial infarction. Pharmacol. Res. 61, 142–148. doi:10.1016/j.phrs.2009.08.009
Jo, W., Min, B. S., Yang, H. Y., Park, N. H., Kang, K. K., Lee, S., et al. (2020). Sappanone A prevents left ventricular dysfunction in a rat myocardial ischemia reperfusion injury model. Int. J. Mol. Sci. 21, E6935. doi:10.3390/ijms21186935
Kim, R. B., Kim, J. R., and Hwang, J. Y. (2022). Epidemiology of myocardial infarction in Korea: Hospitalization incidence, prevalence, and mortality.. Epidemiol. Health 44, e2022057. doi:10.4178/epih.e2022057
Kim, Y. S., Kwon, J. S., Cho, Y. K., Jeong, M. H., Cho, J. G., Park, J. C., et al. (2012). Curcumin reduces the cardiac ischemia–reperfusion injury: Involvement of the toll-like receptor 2 in cardiomyocytes. J. Nutr. Biochem. 23, 1514–1523. doi:10.1016/j.jnutbio.2011.10.004
Kong, J. (2012). Effects of curcumin on the expression of NF-κB, PPAR-γ and Bcl-2 in rat myocardium after myocardial infarction. Xinxiang Medical University.
Lestari, M. L., and Indrayanto, G. (2014). Curcumin. Profiles Drug Subst. Excip. Relat. Methodol. 39, 113–204. doi:10.1016/B978-0-12-800173-8.00003-9
Li, H., Sureda, A., Devkota, H. P., Pittalà, V., Barreca, D., Silva, A. S., et al. (2020). Curcumin, the golden spice in treating cardiovascular diseases. Biotechnol. Adv. 38, 107343. doi:10.1016/j.biotechadv.2019.01.010
Liu, C. H., He, Z. F., Liu, C. H., Li, A. X., Liu, C., Lu, J. K., et al. (2015).Effects of curcumin on cardiac function and myocardial fibrosis in rats with acute myocardial infarction. Xin Xue Guan Kang Fu Yi Xue Za ZHi 24, 407–410.
Liu, H. J. (2018). [Protective effect and mechanism of curcumin on myocardial ischemia-reperfusion injury in rats. Nanjing Medical University.
Mehdi, R., Mehdi, H., Mahdi, A., Morteza, H., Hassan, A., Zirak, J. M., et al. (2019). Curcumin ameliorated myocardial infarction by inhibition of cardiotoxicity in the rat model. J. Cell. Biochem. 120, 11965–11972. doi:10.1002/jcb.28480
Musillo, C., Borgi, M., Saul, N., Möller, S., Luyten, W., Berry, A., et al. (2021). Natural products improve healthspan in aged mice and rats: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 121, 89–105. doi:10.1016/j.neubiorev.2020.12.001
Selvaraj, S., Steg, P. G., Elbez, Y., Sorbets, E., Feldman, L. J., Eagle, K. A., et al. (2016). Pulse pressure and risk for cardiovascular events in patients with atherothrombosis: From the REACH registry. J. Am. Coll. Cardiol. 67, 392–403. doi:10.1016/j.jacc.2015.10.084
Shaoxi, Y., Mo, Z., Xiaoyun, Z., Yuanyuan, X., Juan, D., Mengwen, Y., et al. (2021). Anti-Inflammatory effect of curcumin on the mouse model of myocardial infarction through regulating macrophage polarization. Mediat. Inflamm. 21, 9976912. doi:10.1155/2021/9976912
Sheng, S., Yang, Q. N., Zhu, H. N., and Xian, Y. Y. (2021). Network pharmacology-based exploration of the mechanism of Guanxinning tablet for the treatment of stable coronary artery disease. World J. Tradit. Chin. Med. 7, 456–466. doi:10.4103/wjtcm.wjtcm_25_21
Sumitra, M., Manikandan, P., and Puvanakrishnan, R. (2007). Cardioprotective effects of curcumin. Adv. Exp. Med. Biol. 595, 359–377. doi:10.1007/978-0-387-46401-5_16
Sunagawa, Y., Morimoto, T., Wada, H., Takaya, T., Katanasaka, Y., Kawamura, T., et al. (2011). A natural p300-specific histone acetyltransferase inhibitor, curcumin, in addition to angiotensin-converting enzyme inhibitor, exerts beneficial effects on left ventricular systolic function after myocardial infarction in rats. Circ. J. 75, 2151–2159. doi:10.1253/circj.cj-10-1072
Sunagawa, Y., Sono, S., Katanasaka, Y., Funamoto, M., Hirano, S., Miyazaki, Y., et al. (2014). Optimal dose-setting study of curcumin for improvement of left ventricular systolic function after myocardial infarction in rats. J. Pharmacol. Sci. 126, 329–336. doi:10.1254/jphs.14151FP
Sunagawa, Y., Wada, H., Suzuki, H., Sasaki, H., Imaizumi, A., Fukuda, H., et al. (2012). A novel drug delivery system of oral curcumin markedly improves efficacy of treatment for heart failure after myocardial infarction in rats. Biol. Pharm. Bull. 35, 139–144. doi:10.1248/bpb.35.139
Wang, R., Yao, Q., Chen, W., Gao, F., Li, P., Wu, J., et al. (2021). Stem cell therapy for crohn's disease: Systematic review and meta-analysis of preclinical and clinical studies. Stem Cell Res. Ther. 12 (1), 463. doi:10.1186/s13287-021-02533-0
Wang, R., Zhang, J. Y., Zhang, M., Zhai, M. G., Di, S. Y., Han, Q. H., et al. (2018). Curcumin attenuates IR-induced myocardial injury by activating SIRT3. Eur. Rev. Med. Pharmacol. Sci. 22, 1150–1160. doi:10.26355/eurrev_201802_14404
Wang, Y. (2008). Effects of curcumin on apoptosis and cardiac function after myocardial infarction in rats. Chongqing Medical University.
Xu, J. H., and Yang, B. (2015). Effect of flavin on expression of AT_1 receptor in heart failure rats. Shi Yong Yu Fang. Yi Xue 22, 1069–1072.
Zhou, W. J., Li, J. L., Zhou, Q. M., Cai, F. F., Chen, X. L., LuYY, , et al. (2020). Ginsenoside Rb1 pretreatment attenuates myocardial ischemia by reducing calcium/calmodulin-dependent protein kinase II-medicated calcium release. World J. Tradit. Chin. Med. 6, 284–294. doi:10.4103/wjtcm.wjtcm_24_20
Keywords: curcumin, myocardial infarction, model, systematic evaluation, meta-analysis
Citation: Pang B-Y, Wang Y-H, Ji X-W, Leng Y, Deng H-B and Jiang L-H (2022) Systematic review and meta-analysis of the intervention effect of curcumin on rodent models of myocardial infarction. Front. Pharmacol. 13:999386. doi: 10.3389/fphar.2022.999386
Received: 21 July 2022; Accepted: 23 September 2022;
Published: 18 October 2022.
Edited by:
Jose R. Lopez, Mount Sinai Medical Center, United StatesReviewed by:
Shaobo Zhou, University of Bedfordshire, United KingdomPeter Ricci Pellegrino, University of Nebraska Medical Center, United States
Tomasz Tytus Gabrys, University of West Bohemia, Czechia
Copyright © 2022 Pang, Wang, Ji, Leng, Deng and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li-Hong Jiang, amFpbmdsaWhvbmdqbGg5OTY1QDEyNi5jb20=
†These authors have contributed equally to this work
 Bing-Yao Pang
Bing-Yao Pang Ya-Hong Wang
Ya-Hong Wang Xing-Wang Ji
Xing-Wang Ji Yan Leng
Yan Leng Hou-Bo Deng
Hou-Bo Deng Li-Hong Jiang
Li-Hong Jiang