- 1Liaoning Key Laboratory of Chinese Medicine Combining Disease and Syndrome of Diabetes, Liaoning University of Traditional Chinese Medicine, Shenyang, China
- 2College of Integrative Chinese and Western Medicine, Hebei University of Chinese Medicine, Shijiazhuang, China
- 3College of Traditional Chinese Medicine, Liaoning University of Traditional Chinese Medicine, Shenyang, China
- 4College of First College, Liaoning University of Traditional Chinese Medicine, Shenyang, China
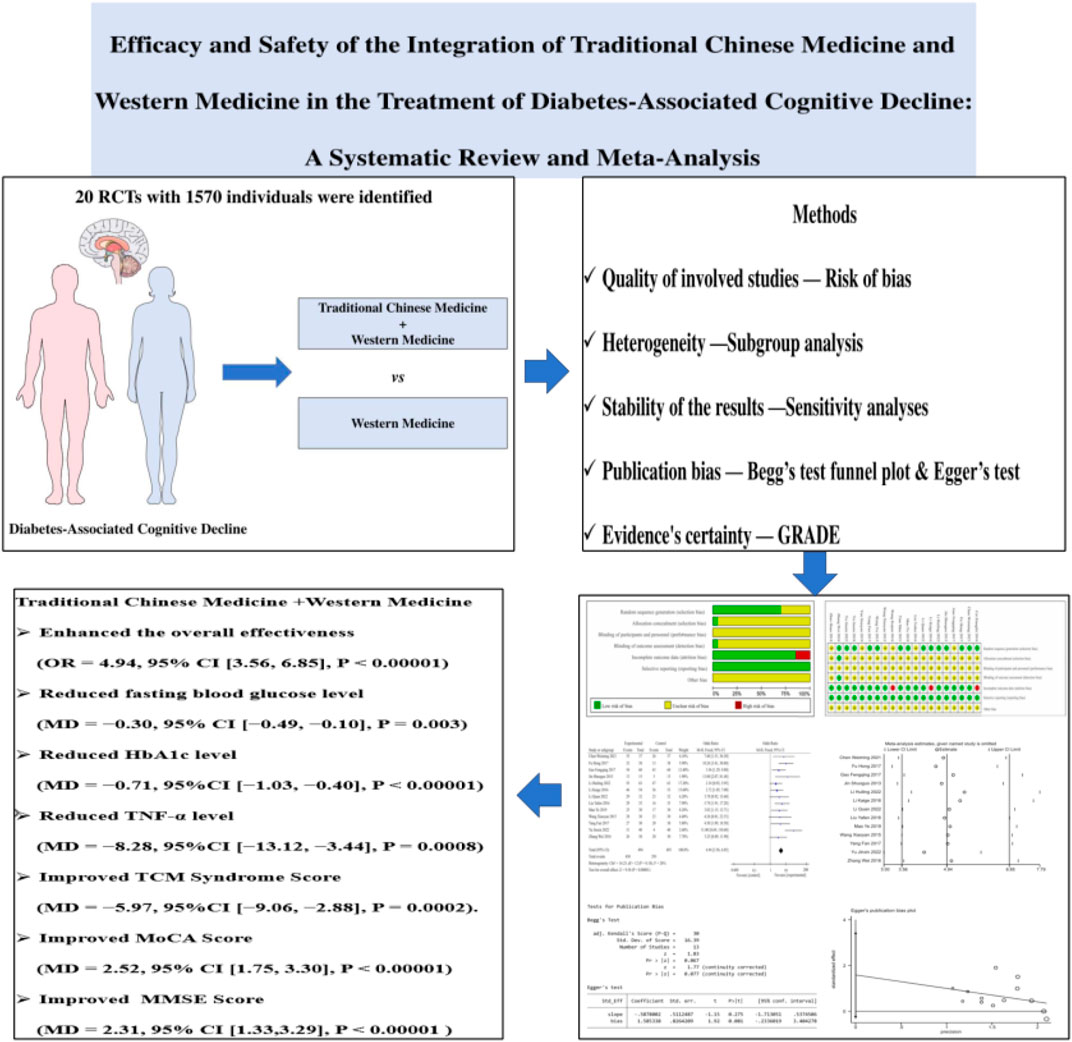
Objective: In order to offer possible therapeutic treatment evidence for diabetes-associated cognitive decline (DACD), we thoroughly evaluated the effectiveness and safety of combining Traditional Chinese Medicine (TCM) and Western Medicine (WM) in the current study.
Methods: The present study employed a comprehensive search strategy across multiple databases, namely, PubMed, EMBASE, Web of Science, the Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang Data, Chinese Scientific Journals Database (VIP), and Chinese Biomedical Literature Database (CBM), to identify relevant articles published until July 2023. Subsequently, a systematic review and meta-analysis of randomized controlled trials (RCTs) were conducted to assess the efficacy and safety of integrating TCM with WM for the treatment of DACD. The literature included in this study was assessed using the GRADE criteria and the Cochrane Handbook for Systematic Reviews of Interventions. Statistical analysis was conducted using RevMan 5.4 software.
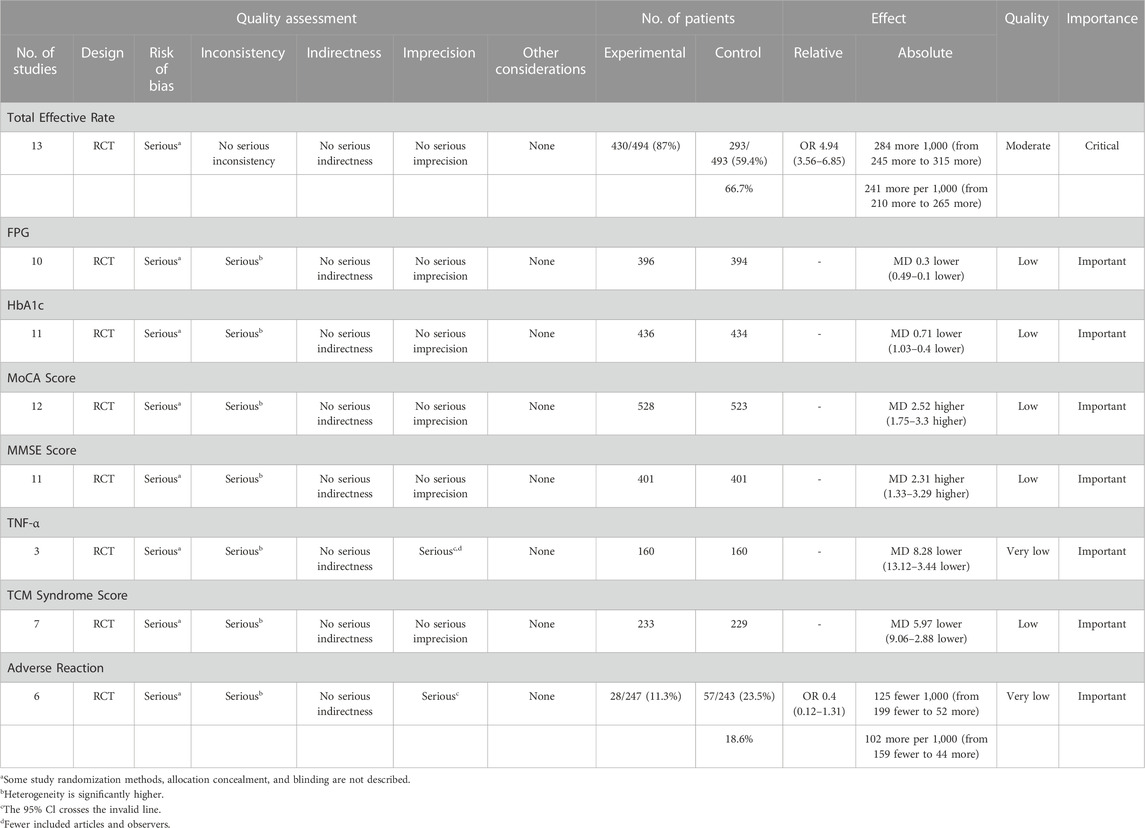
Results: A total of 20 RCTs involving 1,570 patients were ultimately included in this meta-analysis. The pooled results demonstrated that the integration of TCM and WM therapy significantly enhanced the overall effectiveness rate compared to WM therapy alone [OR = 4.94, 95% CI (3.56, 6.85), p < 0.00001]. Additionally, the combination therapy resulted in reductions in fasting blood glucose [MD = −0.30, 95% CI (−0.49, −0.10), p = 0.003], HbA1c [MD = −0.71, 95%CI (−1.03, −0.40), p < 0.00001], TNF-α levels [MD = −8.28, 95%CI (−13.12, −3.44), p = 0.0008], and TCM Syndrome Score [MD = −5.97, 95%CI (−9.06, −2.88), p = 0.0002]. Meanwhile, the combination therapy had a positive effect on MoCA Score [MD = 2.52, 95% CI (1.75, 3.30), p < 0.00001], and MMSE Score [MD = 2.31, 95% CI (1.33, 3.29), p < 0.00001]. In addition, the safety of the combination therapy was comparable to that of the WM alone [OR = 0.40, 95% CI (0.12, 1.31), p = 0.13].
Conclusion: The integration of TCM and WM therapy outperformed WM alone in DACD treatment. Simultaneously, the combination therapy could improve the therapeutic effect on blood glucose, cognitive function, and inflammation to a certain extent with few adverse effects. However, given the constraints imposed by the quality limitations of the incorporated studies, as well as the potential presence of reporting bias, it is imperative that our findings be substantiated through rigorous, large-scale, randomized controlled trials of superior quality in the future.
1 Introduction
Diabetes mellitus (DM) is a metabolic disorder that is becoming more prevalent, marked by chronic hyperglycemia and a deficiency in insulin production or sensitivity (Banday et al., 2020). Diabetes mellitus is spreading globally, with an estimated 366 million people in the world by 2030, and thus it has become an urgent and worldwide public health issue threatening human health (Aschner et al., 2021). Neurodegenerative disease is increasingly recognized as an additional complication of diabetes mellitus, in addition to the well-established microvascular and macrovascular complications (Mauricio et al., 2020). Extensive research has demonstrated a correlation between type 2 diabetes mellitus (T2DM) and the development of neurodegenerative diseases such as Alzheimer’s disease, vascular dementia, and cognitive impairment (Khaledi et al., 2019; Sutherland et al., 2017; Stoeckel et al., 2016). Notably, T2DM is closely linked to a heightened risk of cognitive impairment, with approximately 60%–70% of T2DM patients experiencing cognitive dysfunction (Gupta et al., 2022; Chatterjee et al., 2016).
Diabetes-associated cognitive decline (DACD) is a prevalent neurological complication of T2DM that primarily presents as cognitive deficits, involving attention and executive functions (Chen et al., 2018). Furthermore, it has gradually become a worldwide health concern due to the advancement of living standards, the acceleration of aging, and the changes in lifestyle (Srikanth et al., 2020). Unfortunately, we remain a shallow understanding on the exact pathogenesis of DACD until now, and thus the range of treatment options is constrained when there is a lack of efficacious and targeted therapeutic medications (Chinese Society of Endocrinology, 2022). The current approach to treating DACD primarily emphasizes the comprehensive management of multiple risk factors, such as blood glucose control, enhancement of cerebral blood supply, and preservation of cognitive function. However, the intricacy of multidrug regimens may engender the likelihood of nonadherence among patients, whereas the prolonged utilization of hypoglycemic agents may escalate the occurrence of adverse effects, including gastrointestinal discomfort, weight gain, and hepatic dysfunction (Chinese Society of Endocrinology, 2021). In light of the unsatisfactory outcomes associated with current treatments, clinicians are taking a closer look at Traditional Chinese Medicine (TCM) as an adjuvant or alternative treatment.
Traditional Chinese medicine therapy is extensive and profound, which has been inherited and applied for more than 2,000 years, is the treasure of Chinese culture. The theory of TCM promotes the principle of “harmony between man and nature” and strives for comprehensive treatment. The people-centered, holistic, and multitarget strategies employed by TCM offer distinct benefits in managing intricate conditions, including DM (Marín-Peñalver et al., 2016). There is no definite disease name of DACD in TCM literature, but according to its clinical characteristics and performance, it is classified as “Xiao Ke” combined with “Chi Dai” or “Jian Wang.” In recent years, a substantial body of preclinical (in vivo/in vitro) experiments and clinical observation studies has provided evidence supporting the therapeutic efficacy of the integration of traditional Chinese medicine and western medicine in the treatment of DACD. Meanwhile, the potential therapeutic mechanism is still being improved and supplemented, including oxidative stress (Hao et al., 2019), gut microbiota (Zheng et al., 2022), autophagy (Tian et al., 2022), neuroinflammation (Shi et al., 2021), etc. However, most of the published clinical studies are small single-center clinical trials, lacking high-quality systematic evaluation and review of clinical treatment. Efficacy and safety of this treatment must therefore be demonstrated through evidence-based studies. Given the aforementioned constraints, we conducted an extensive review of both domestic and foreign literature to impartially assess the clinical effectiveness and safety of combining TCM and Western Medicine (WM) for patients with DACD, aiming to shed light on clinical treatment approaches.
2 Materials and methods
The review procedure was carried out in accordance with PRISMA guidelines, and it has been submitted to the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY) under registration number INPLASY202320072.
2.1 Literature search strategy
To identify relevant studies on biological therapeutic interventions for DACD, an extensive search was conducted across several databases, including China National Knowledge Infrastructure (CNKI), Wanfang Database, Chinese Scientific Journals Database (VIP), Chinese Biomedical Literature Database (CBM), PubMed, EMBASE, Web of Science, and Cochrane Library. The retrieval period encompassed the entire duration of databases up until July 2023. No restrictions were placed on language, systemic conditions of participants, or publication year within the scope of this study. The search strategy employed a comprehensive approach, utilizing both MeSH terms and keywords, with a specific emphasis on the topics of “diabetic cognitive impairment” and “traditional Chinese medicine and western medicine.” Additionally, the search encompassed intervention measures and diseases associated with these topics, such as proprietary Chinese medicine, Chinese medicine herbs, herbal medicine, diabetic cognitive dysfunction, and diabetic encephalopathy etc. Furthermore, a manual search was conducted in the journal literature available at the Liaoning University of Traditional Chinese Medicine library to complement the initial search and identify any potential omissions. The specific search strategy of each database was shown in Supplementary Material S1.
2.2 Inclusion criteria
The inclusion criteria were established using the PICOS framework, encompassing participant, intervention, comparison, outcomes, and study design.
2.2.1 Types of participants
The study did not impose any limitations based on age, gender, or race. The participants included individuals who had received a diagnosis of DACD based on a well-defined definition or internationally recognized diagnostic criteria.
2.2.2 Types of interventions
The intervention implemented in this study entailed the integration of TCM and WM. In the treatment group, TCM treatment was exclusively employed as the positive intervention, contrasting with the control group. No limitations were imposed on the dosage or duration of medication.
2.2.3 Types of comparison
The use of WM treatment, including hypoglycemic agents, insulin, nimodipine, donepezil, and others, has been shown to effectively lower blood glucose levels and enhance cognitive function. The control groups in the studies employed the same specifications and dosage of WM as the treatment groups.
2.2.4 Types of outcomes
The primary outcome measure was the total effective rate, while secondary outcomes included fasting plasma glucose (FPG), glycated hemoglobin (HbA1c), MoCA score, MMSE score, TNF-α, TCM syndrome score, and adverse reactions. All included literature reported at least two results from the aforementioned outcomes.
2.2.5 Types of study design
All randomized controlled trials (RCTs) that reported the utilization of TCM in combination with WM for the treatment of DACD were included in this study. No restrictions were placed on publication status or language.
2.3 Exclusion criteria
The exclusion criteria were set as followed. 1) Non-RCTs or animal studies. 2) Control group included methods of TCM, such as acupuncture, Chinese patent medicine, herbal extracts and so on. 3) Repeated publication or repeated clinical data. 4) Original and unpublished data that could not be obtained and extracted after contacting the authors. 5) Outcome effect was not clear: The data were incomplete, the outcome effect was not clear, the statistical method was incorrect, and the data could not provide the mean and standard deviation.
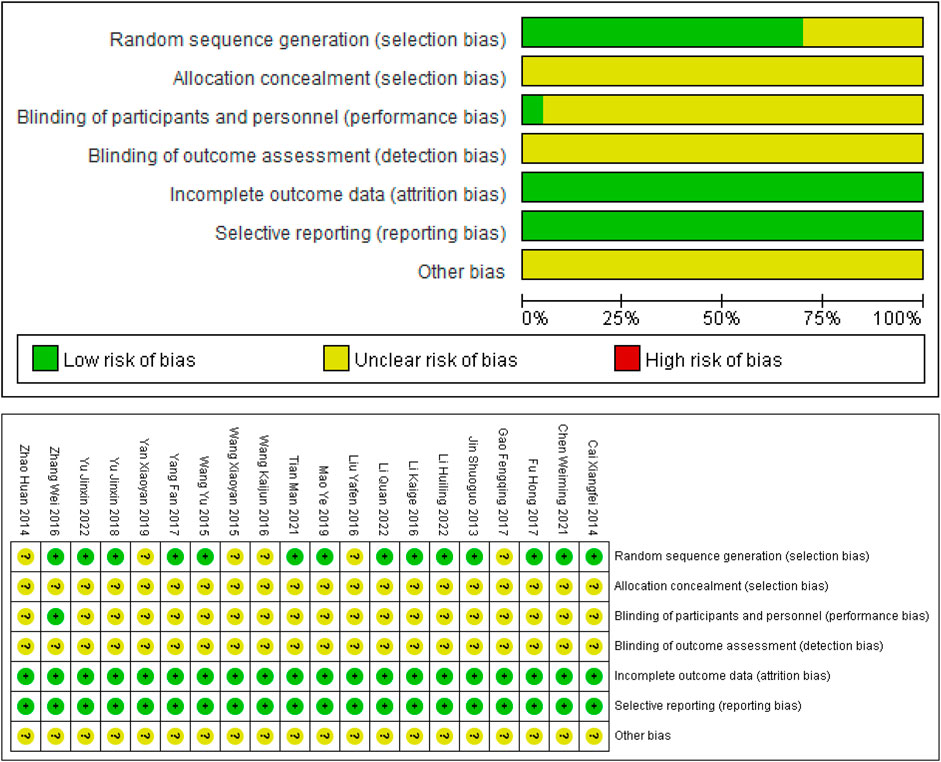
2.4 Baseline characteristics and assessment of included studies
The data extraction process for the studies was conducted by two independent reviewers (Jiren An and Guiyan Sun). To facilitate this process, a study-specific spreadsheet was created in Excel, encompassing variables such as authors, publication date, country, study design, sample size, average age, gender, intervention measures, follow-up duration, and outcome measures. Subsequently, all data were cross-verified and imported into Rev Man software (V.5.4). The Cochrane Handbook for Systematic Reviews was utilized to evaluate the risk of bias in all studies included in this analysis. These studies were categorized as having a low, high, or unclear risk of bias based on seven specific criteria: 1) random sequence generation; 2) allocation concealment; 3) blinding of participants and personnel; 4) blinding of outcome assessors; 5) incomplete outcome data; 6) selective reporting; and 7) other potential risks of bias. In cases where there was disagreement, a third reviewer investigator (Yufeng Yang) was consulted to reach a resolution.
2.5 Data analysis and synthesis
Statistical analyses were performed using the Review Manager program (version 5.4.1, The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark) and Stata software (version 16, The Stata Corporation, College Station, Texas, United States). To measure the effect size, Risk ratio (RR) with 95% confidence intervals (CIs) was used as an evaluation index for dichotomous data, including total effective rate and adverse reaction. Mean difference (MD) or standardized mean difference (SMD) with 95% CI was used as an evaluation index for continuous data, including FPG, HbA1c, MoCA score, MMSE score, TNF-α, AND TCM syndrome score.
Heterogeneity among the outcomes of the included studies was analyzed using the Cochrane Q test, while the magnitude of heterogeneity was determined quantitatively in combination with I2 (Higgins and Thompson, 2002). If there was no heterogeneity (p > 0.05, I2 ≤ 50%), the fixed-effect model was selected; if there was heterogeneity (p ≤ 0.05, I2 > 50%), the random-effect model was used. p < 0.05 was considered statistically significant.
2.6 Subgroup analyses, sensitivity analyses and publication bias
Subgroup analysis was performed on the clinical characteristics to investigate the causes of clinical heterogeneity. By excluding one study at a time, sensitivity analysis was used to examine whether low-quality studies affected the robustness and stability of the overall meta-analysis. Begg’s test funnel plot and Egger’s test were used to evaluate publication bias.
2.7 Evaluation of the certainty of the evidence
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) tool was used to evaluate the quality of cumulative evidence in this review (Goldet and Howick, 2013). By assessing the factors such as the risk of bias, inconsistency, and indirectness, the certainty level of evidence was judged using four categories of “very low,” “low,” “moderate,” and “high.”
3 Results
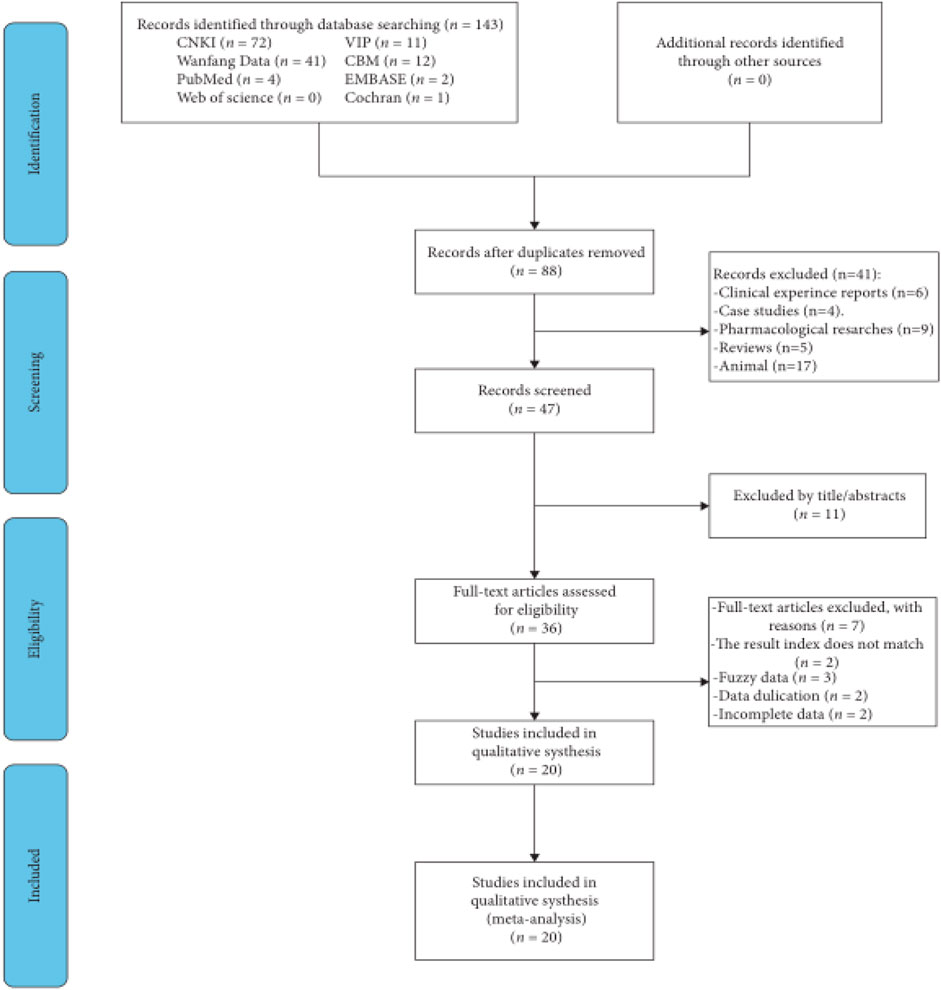
3.1 Literature retrieval process and results
A preliminary literature search turned up a total of 143 publications, and 20 articles (Cai, 2016; Chen et al., 2021; Fu et al., 2017; Gao et al., 2017; Jin et al., 2015; Li, 2022; Li, 2016; Li et al., 2022; Liu et al., 2016; Mao et al., 2019; Tian et al., 2021; Wang et al., 2016; Wang, 2015; Wang et al., 2015; Yan and Guan, 2019; Yang, 2017; Yu, 2018; Yu et al., 2022; Zhang, 2016; Zhao et al., 2014) that qualified were subsequently found. Figure 1 displayed the search procedures.
3.2 Study characteristics and assessment of risk of bias
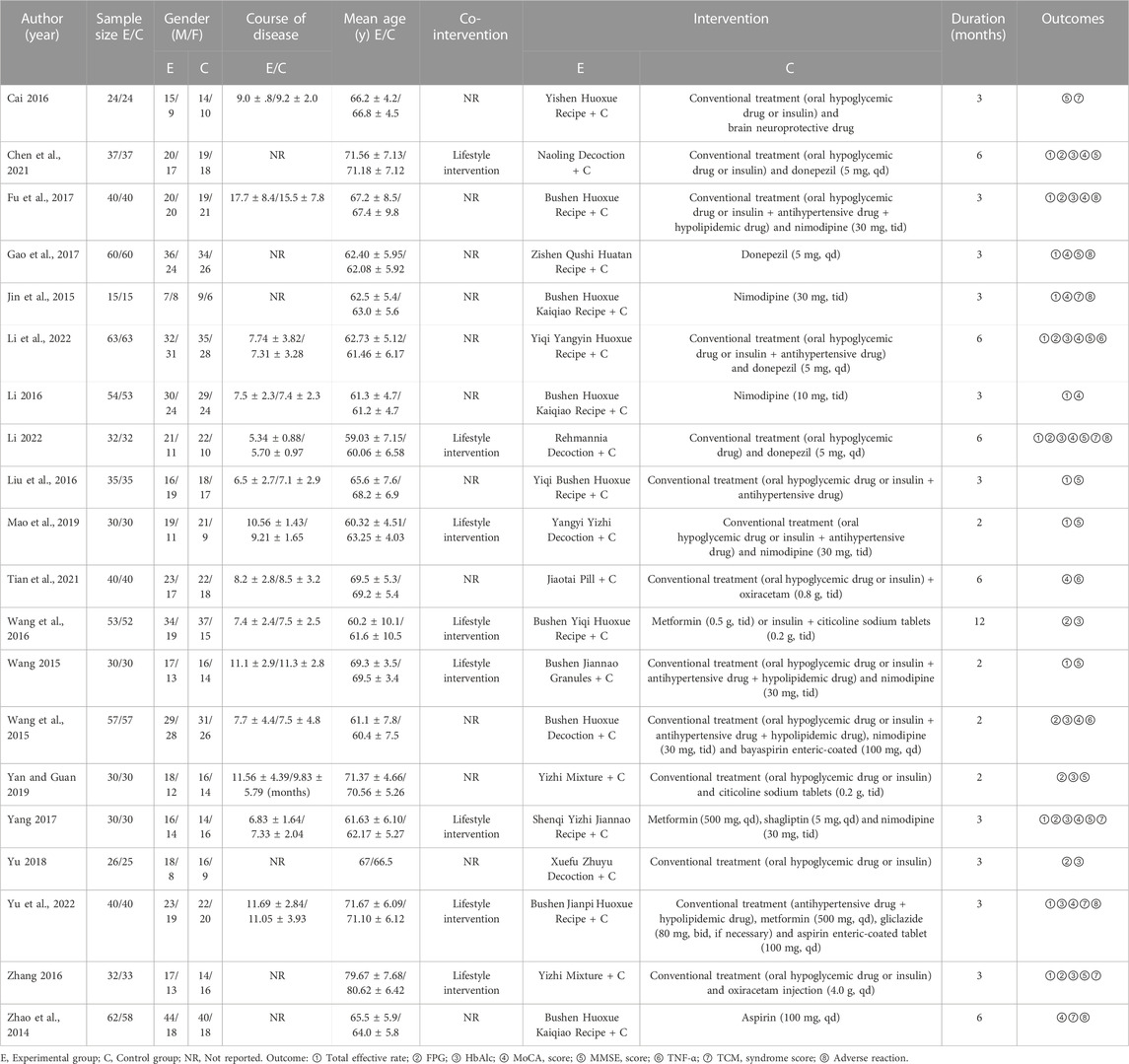
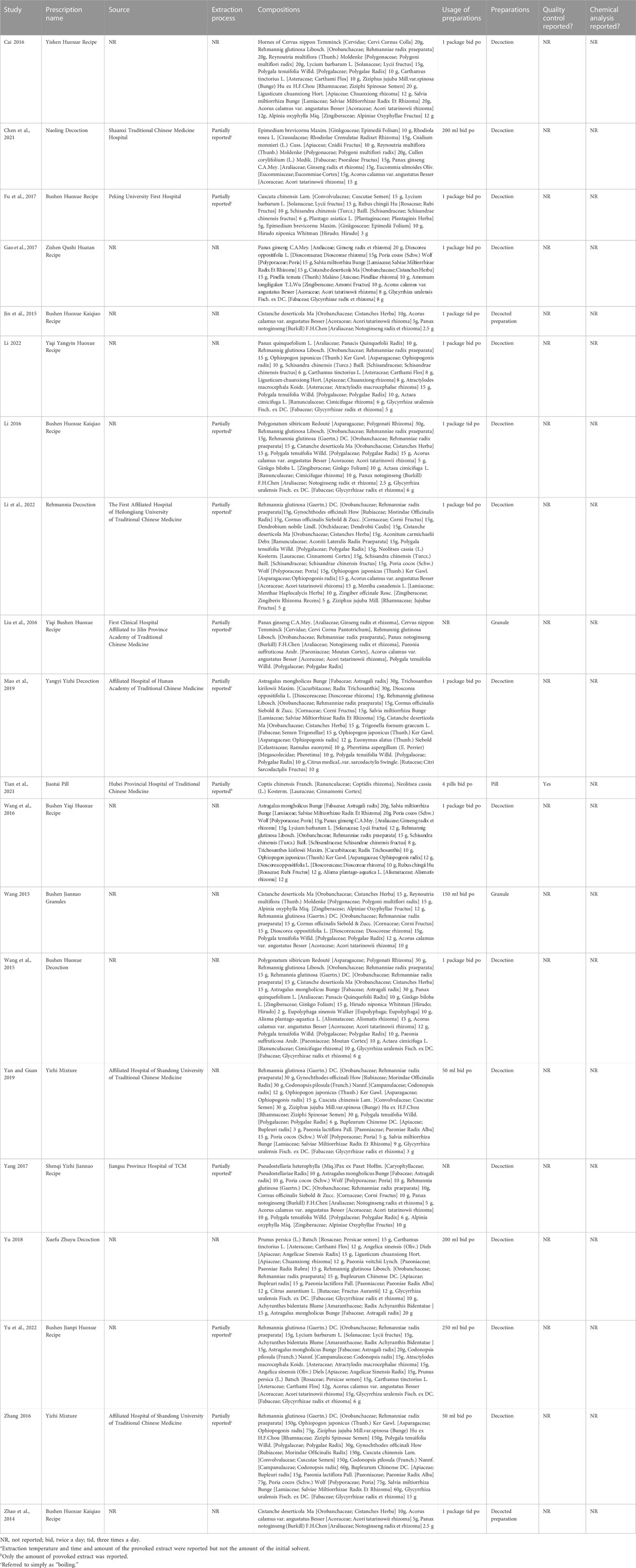
All studies were published before July 2023 and conducted in China. Totally, this meta-analysis involved 1,570 participants, of which 788 participants were designated to the experimental group while 782 patients were assigned to the control group. The sample size varied from 30 to 126, with a mean patient age ranging from 59 to 80 years old. and the average course of disease ranged from less than 12 months to more than 17 years. Regarding of the treatment measures, the control group adopted the therapy of western medicine alone, whereas the experimental group received combined treatment with TCM and WM. Specially, western medicine included hypoglycemic drug, antihypertensive drug, hypolipidemic drug, donepezil, nimodipine, oxiracetam citicoline sodium tablets, aspirin enteric-coated tablet, and insulin etc. Meanwhile, a total of 17 types of Chinese herbal medicine were used in the 20 RCTs, all of which were multi-herbal medicines, including Bushen Huoxue decoction, Bushen Huoxue Kaiqiao recipe, Bushen Huoxue recipe, Bushen Jiannao granules, Bushen Jianpi Huoxue recipe, Bushen Yiqi Huoxue recipe, Jiaotai pill, Naoling decoction, Rehmannia decoction, Shenqi Yizhi Jiannao recipe, Xuefu Zhuyu decoction, Yangyi Yizhi decoction, Yiqi Bushen Huoxue recipe, Yiqi Yangyin Huoxue recipe, Yishen Huoxue recipe, Yizhi Mixture, Zishen Qushi Huatan recipe. Among the 20 included studies, the duration of treatment ranged from 2 months to 12 months. In terms of the outcomes, 13 studies mentioned the total effective rate, 10 studies reported the FPG level, 11 studies reported the HbA1c level, 12 studies reported the MoCA score, 11 studies reported the MMSE score, 3 studies reported the TNF-α level, 7 studies reported the TCM syndrome score, and 12 studies reported the adverse reaction. The experimental group and the control group had equivalent pre-treatment data (such as age, sex ratio, outcome indicators, etc.). The basic characteristics of the included studies were summarized in Table 1, and components of Chinese herbal medicine used in the included studies were presented in Table 2.
Assessment of risk biases were outlined as Figure 2. In general, the overall methodological qualities of the included studies were poor to moderate. In terms of random sequence generation, 14 studies provided a sufficient randomization process to generate random sequences with a low risk of bias, whereas the remaining 6 studies supplied unspecific details of randomization, and thus were assessed as unclear risk. None of the included studies explicitly mentioned the use of allocation concealment, which led to unclear risk of bias in the relative domain. Only 1 study described the implementation of single blinding of subjects, which was rated as low risk. None of other included studies explicitly mentioned the use of blind method, resulting in an unclear associated risk of bias. All studies included in the analysis published complete data regarding the outcomes, leading us to rate the risk of bias as low. Meanwhile, all included RCTs didn’t report the bias of selective reporting, thus assessing as low risk. As for other biases, none of the studies provided adequate information for risk judgment, resulting in an unclear risk of bias.
3.3 Meta-analysis results
3.3.1 Meta-analysis of total effective rate
Preliminary data from 13 studies revealed the disclosure of the total effective rate, as illustrated in Figure 3. Following the heterogeneity test (p = 0.18, I2 = 26%), the fixed-effects model was employed for analysis. The findings demonstrated a statistically significant increase in the total effective rate within the experimental group compared to the control group [OR = 4.94, 95% CI (3.56, 6.85), p < 0.00001]. Consequently, the combination of TCM and WM exhibited superior efficacy in treating DACD when compared to WM alone.
An additional subgroup analysis revealed that the combination of TCM and WM resulted in a significantly higher total effective rate compared to WM alone for treatment durations of 2 months [p = 0.77, I2 = 0%; OR = 3.01, 95% CI = (1.57, 5.77), p = 0.0009], 3 months [p = 0.16, I2 = 36%; OR = 7.47, 95% CI = (4.50, 12.41), p < 0.00001], and 6 months [p = 0.41, I2 = 0%; OR = 4.17, 95% CI (2.31, 7.51), p < 0.00001].
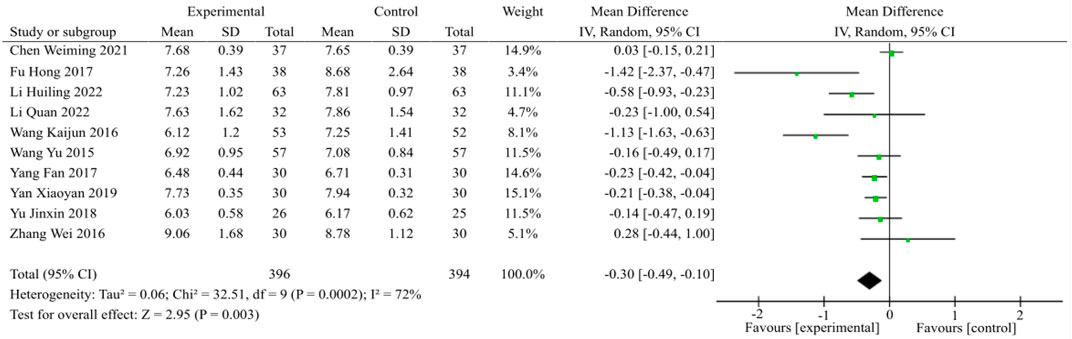
3.3.2 Meta-analysis of FPG
A total of 10 studies were incorporated into the analysis of FPG, as illustrated in Figure 4. The random effects model was chosen after considering the outcomes of the heterogeneity test (p = 0.0002, I2 = 72%). In comparison to the control group, the combination of TCM and WM demonstrated a significant reduction in FPG levels among patients with DACD [MD = −0.30, 95% CI (−0.49, −0.10), p = 0.003].
A subgroup analysis indicated not readily apparent heterogeneity (p = 0.19, I2 = 40%) during the ≤2 month treatment course. On the basis of the fixed effects model, TCM plus WM treatment of DACD was determined to induce a statistically significant effect compared with WM alone [MD = −0.34, 95%CI (−0.57, −0.11), p = 0.004]. Regarding the 3-month treatment course (p = 0.0006, I2 = 79%) and 6-month treatment course (p = 0.06, I2 = 73%), heterogeneity was significant, and the statistical analysis using the random effects model indicated that TCM plus WM was superior to the control group in terms of reducing FPG level during the 3-month treatment course [MD = −0.31, 95%CI (−0.46, −0.15), p < 0.0001]. However, there was no statistical significance between the two groups during 6-month treatment course [MD = −0.10, 95% CI (−0.22, 0.03), p = 0.13].
3.3.3 Meta-analysis of HbA1c
Eleven studies involving a total of 870 patients were included in the analysis, as illustrated in Figure 5. The statistical analysis was conducted using the random effects model, following the heterogeneity test (p < 0.00001, I2 = 93%). The findings of the meta-analysis revealed that the combination of TCM and WM exhibited a greater capacity to decrease HbA1c levels compared to the use of WM alone [MD = −0.71, 95%CI (−1.03, −0.40), p < 0.00001].
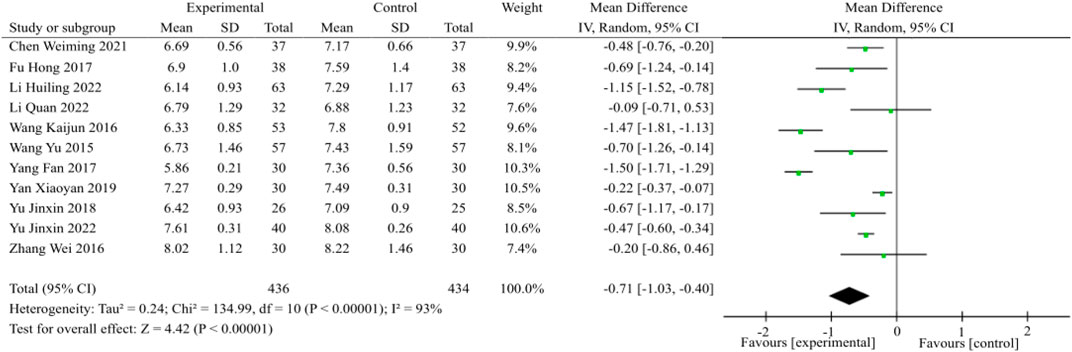
FIGURE 5. HbA1c meta-analysis forest plot. The subgroup analysis revealed that the benefits of TCM plus WM on lowering HbA1c surpassed that of the control group, irrespective of whether the duration was less than or equal to 2 months [p = 0.01, I2 = 77%; MD = −0.68, 95%CI (−1.27, −0.09), p = 0.02], 3 months [p < 0.00001, I2 = 94%; MD = −0.86, 95%CI (−1.38, −0.35), p = 0.001] or 6 months [p = 0.11, I2 = 61%; MD = −0.32, 95%CI (−0.57, −0.07), p = 0.01].
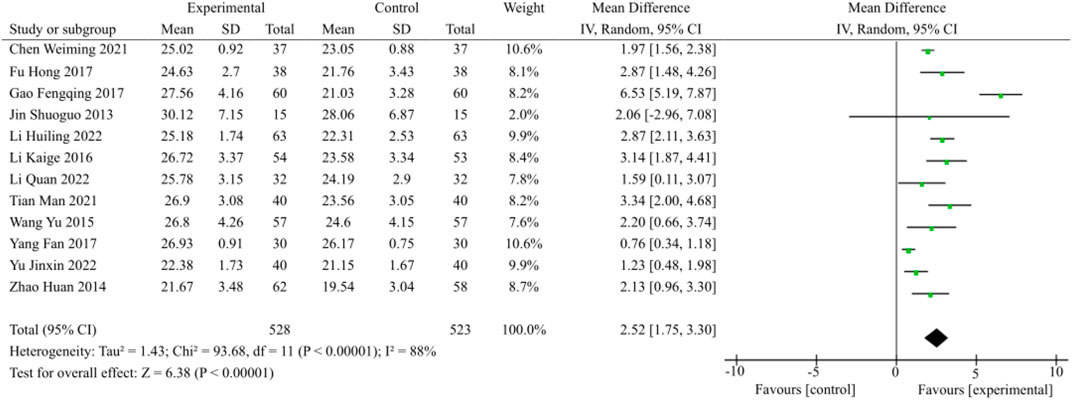
3.3.4 Meta-analysis of MoCA score
12 studies focused on MoCA scores, as illustrated in Figure 6. The heterogeneity was apparent (p < 0.00001, I2 = 88%); Therefore, the random effects model was selected. In patients with DACD, TCM plus WM significantly improved MoCA scores compared with WM alone [MD = 2.52, 95% CI (1.75, 3.30), p < 0.00001].
The MoCA scale consisted of the following 7 items, including visuospatial and executive, naming, attention, language, abstraction, memory and delayed recall, as well as orientation. In the present study, a total of 5 studies reported on the specific items of MoCA scale in detail. The pooled data of meta-analysis demonstrated the superior effect of TCM plus WM for items other than naming and orientation. The entire summary was provided in Table 3.
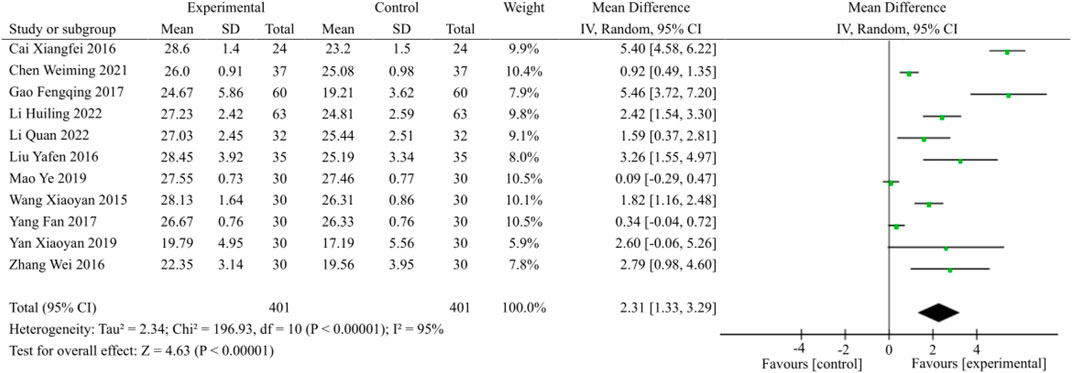
3.3.5 Meta-analysis of MMSE score
A total of 11 eligible studies, as illustrated in Figure 7, encompassing 802 patients evenly distributed across two study groups, were included for the purpose of analyzing the MMSE score. The random effects model was chosen for analysis due to the observed heterogeneity (p < 0.00001, I2 = 95%). The combination of TCM and WM demonstrated a significant improvement in MMSE scores among patients with DACD compared to the control group [MD = 2.31, 95% CI (1.33, 3.29), p < 0.00001].
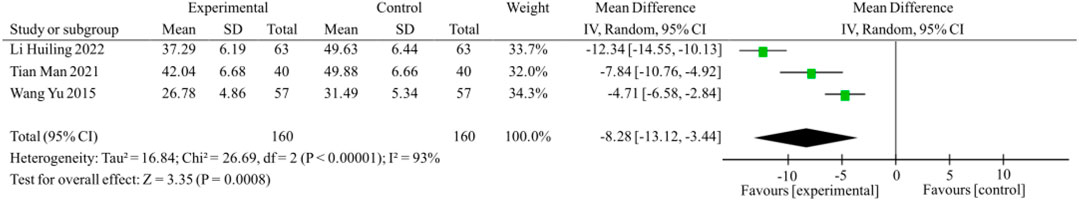
3.3.6 Meta-analysis of TNF-α
Furthermore, three studies specifically focused on the reduction of TNF-α, as illustrated in Figure 8. The random effects model was employed for analysis based on the results of the heterogeneity test (p < 0.00001, I2 = 93%). The meta-analysis results indicated a statistically significant difference between the two groups [MD = −8.28, 95%CI (−13.12, −3.44), p = 0.0008]. The findings of this study suggest that the combination of TCM and WM in the treatment of DACD is more effective in reducing TNF-α levels compared to WM alone (Figure 5).
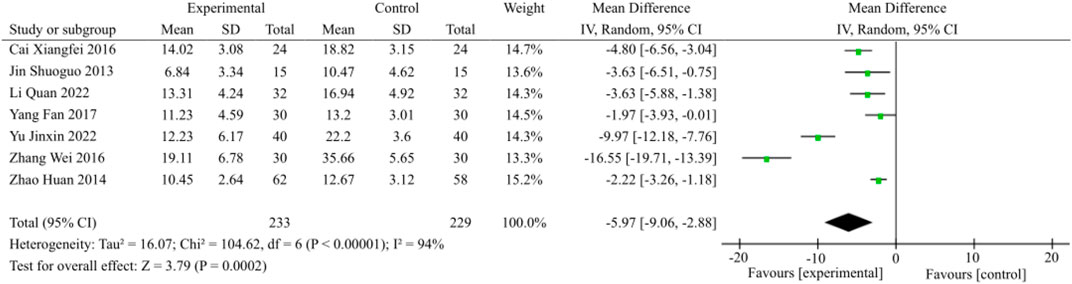
3.3.7 Meta-analysis of TCM syndrome score
Out of the included studies, a total of 7 articles reported improvements in TCM syndrome, as illustrated in Figure 9. Heterogeneity testing was conducted, followed by a meta-analysis using the random-effects model (p < 0.00001, I2 = 94%). The results showed a statistically significant difference with a MD of −5.97 and a 95% CI of (−9.06, −2.88). These findings indicate that the combination of TCM and WM is more effective in treating DACD by improving TCM syndrome (p = 0.0002).
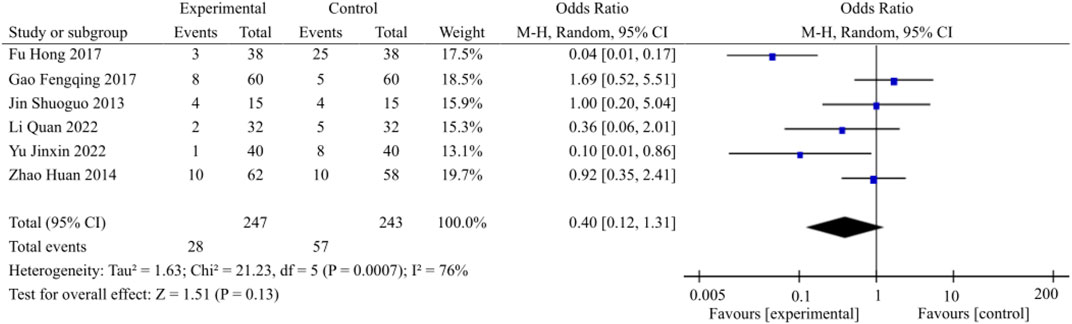
3.3.8 Meta-analysis of adverse reactions
Twelve studies within the encompassed literature made reference to the occurrence of adverse reactions, with only six of these studies reporting patients who experienced such reactions. Conversely, the remaining six studies documented no instances of adverse reactions among their respective patient populations. A total of 28 patients in the experimental group had adverse reactions during treatment, including 7 cases of dizziness, 2 cases of headache, 2 cases of gastrointestinal discomfort, 2 cases of facial flushing, 5 cases of nausea and vomiting, 4 cases of diarrhea, 1 case of albuminuria, 1 case of xerostomia, 1 case of fever, 2 cases of restlessness, and 1 case of insomnia; A total of 57 patients in the control group experienced adverse reactions, including 11 cases of dizziness, 7 cases of headache, 10 cases of gastrointestinal discomfort, 6 cases of decreased blood pressure, 1 case of facial flushing, 3 cases of nausea and vomiting, 1 case of diarrhea, 1 case of anemia, 2 cases of albuminuria, 1 case of impaired liver function, 2 cases of impaired renal function, 2 cases of xerostomia, 2 cases of fever, 2 cases of restlessness, 2 cases of insomnia, 2 cases of tinnitus, and 2 cases of constipation. The overall heterogeneity was manifested (p = 0.007, I2 = 76%), and thus the random effects model was selected. The data of meta-analysis showed that the differences were not statistically significant (OR = 0.40, 95% CI [0.12, 1.31], p = 0.13) (Figure 10). This observation suggests that the safety of medication administration was comparable between the experimental and control groups, namely, on the basis of WM, the additional use of TCM didn’t appear to result in an increase in adverse reactions.
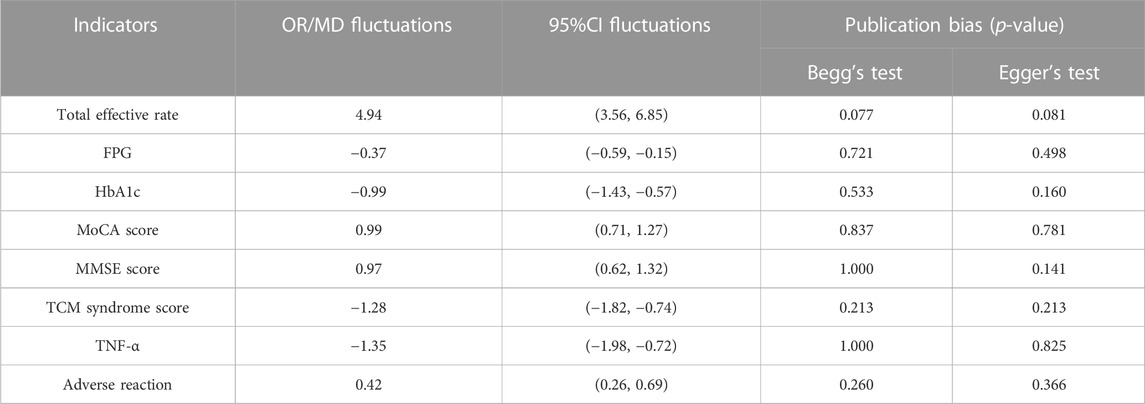
3.4 Sensitivity analysis and publication bias
In order to conduct a sensitivity analysis on the total effective rate, FPG, HbA1c, MoCA score, MMSE score, TCM syndrome score, TNF-α, and adverse reactions, a meticulous item-by-item elimination approach was employed to scrutinize the data extracted from the included literature. No notable alterations were observed in the stability of each study and the combined outcomes of each effect size, thereby affirming the credibility of the data analysis findings. Additionally, Egger’s test was conducted for each outcome to evaluate the likelihood of publication bias, with a significance level of p < 0.05 indicating the presence of such bias. The examination disclosed the absence of publication bias across all indicators. A comprehensive review of the literature indicated that all studies were conducted in China and reported favorable results. These details are comprehensively presented in Table 4. Therefore, it was postulated that the presence of publication bias could potentially be associated with geographical location, racial demographics, and the non-publication of negative findings.
3.5 Evidence quality rating of outcome indicators
The GRADE pro software was employed to assess the quality of evidence. The primary outcome measure, total effective rate, demonstrated a moderate level of reliability, whereas the majority of outcome indicators were deemed to be of low-quality evidence. In addition, two outcome indicators, including TNF-α and AD, were graded as very low-quality evidence (Table 5).
4 Discussion
4.1 Summary of evidence
In recent times, there has been a significant surge in the worldwide prevalence of diabetes mellitus. Data from the World Health Organization has emphasized that the estimated prevalence of diabetes is currently approaching 463 million adults with projection rising to 700 million by 2,045 years (Sun et al., 2022). Concurrently, the cognitive decline linked to diabetes has emerged as a growing area of concern. Substantial evidence has substantiated that DM serves as a significant etiological factor for cognitive impairments, which may subsequently advance to dementia (Datusalia and Sharma, 2016). The epidemiological data have long shown that T2DM populations are at significantly higher risk for developing cognitive deficits and dementia compared with healthy individuals (Seto et al., 2015; Bello-Chavolla et al., 2019). Moreover, a meta-analysis of such studies comprising 25 studies found that the T2DM had an approximately 50% and 60% greater risk of developing DACD and dementia, respectively (Cukierman et al., 2005). However, there is currently no vaccine or specific medicine for DACD. Hence, it is of great significance to identify novel and better anti-DACD drugs and explore new therapeutic schemes.
The application of syndrome differentiation in treatment represents a distinctive feature of the theoretical framework of TCM, and it holds that “Xiao Ke,” the signs of which are recognized as common symptoms of diabetes mellitus in modern medicine, is caused by the interaction of multiple factors, including advanced age, poor diet, emotional and mental disorders, viscera deficiency, and the depletion of a long-term illness. Its pathogenesis is determined as dryness-heat due to deficiency of yin, further resulting in disorder of viscera function and insufficiency of Qi and blood, Yin and Yang, gradually developing the combination of blood stasis and phlegm turbidity that may obstruct the meridians of brain, and eventually leading to the onset or aggravate of “Xiao Ke” complicated with “Chi Dai,” the symptoms of which are considered as analogous to DACD in modern medicine (Yang et al., 2021).
With an apparent dissatisfaction with the effect of conventional treatments, a growing number of DACD sufferers are turning to alternatives medicine, particularly TCM or integrated TCM and WM. It is of note that the integrated TCM and WM therapy has been shown to be more effective than single conventional treatment in improving the effectiveness of DACD and alleviating the side effects (Cai, 2016; Chen et al., 2021; Fu et al., 2017; Gao et al., 2017; Jin et al., 2015; Li, 2022; Li, 2016; Li et al., 2022; Liu et al., 2016; Mao et al., 2019; Tian et al., 2021; Wang et al., 2016; Wang, 2015; Wang et al., 2015; Yan and Guan, 2019; Yang, 2017; Yu, 2018; Yu et al., 2022; Zhang, 2016; Zhao et al., 2014). To date, integrated TCM and WM therapy for DACD has been reported increasingly, conversely, high-quality meta-analysis remains scarce. Here, we aimed to assess the efficacy and safety of integrated TCM and WM therapy for DACD and provide high quality evidence for its clinical therapeutic effects in this context.
The present meta-analysis incorporated 20 RCTs that met the inclusion criteria and included 1,570 subjects in total. In terms of total effective rate, the meta-analysis indicates that integrated TCM and WM therapy for DACD was superior to that of WM alone, possibly by improving glucose toxicity, membrane signal disorder, homeostasis imbalance, inflammation, oxidative stress injury and vascular diseases (Fiatarone Singh et al., 2014; Tian et al., 2016). Meanwhile, the combination therapy could significantly alleviate the TCM syndrome scores. Moreover, prolonged elevation of blood glucose levels has been demonstrated to exert detrimental effects on cognitive abilities and cerebral morphology (Thal et al., 2012). In our investigation, we evaluated both HbA1c and FPG as a composite measure to aid in the assessment of glycemic control. We confirmed that compared with WM alone, integrated TCM and WM therapy exhibited advantages in improving fasting plasma glucose and HbA1c levels. In addition, MMSE and MoCA most probably reflected lesion-associated cognitive impairments (Dong et al., 2010). Thus, we selected MMSE and MoCA for assessing cognitive function in the present meta-analysis. Our results demonstrated that the integrated TCM and WM significantly enhanced the MMSE and MoCA scores in DACD patients, indicating that the combination therapy is beneficial for the improvement of cognitive function. It has been reported that inflammation is associated with the onset of T2DM and progression of its complications, especially DACD. TNF-a is a cytokine with pro-inflammatory properties that was related to both T2DM and cognitive decline (Chu, 2013; Khosravi et al., 2013; Martínez-Mármol et al., 2019). Meta-analysis results showed that the combination therapy could lead to a mean greater reduction in TNF-α level, with statistically significant. Regarding safety, it suggested that the safety of integrated TCM and WM therapy was comparable to that of the WM alone.
4.2 Advantages and limitations
To our knowledge, this is the first meta-analysis to quantitatively estimate the beneficial effect of the integration of TCM and WM therapy for DACD, providing better evidence-based evaluation for the domestic and international researchers to understand this issue. Following the Cochrane Collaboration’s guidelines, the objective is to derive more comprehensive conclusions. The inclusion of additional outcome measures, like FPG, HbA1c, MoCA score, MMSE score, TNF-α, and TCM syndrome score, enables a multidimensional and multilevel assessment of the effectiveness of integrating traditional Chinese medicine (TCM) and Western medicine (WM) for treating DACD.
Despite our critical evaluation of the currently available evidence, some potential limitations should not be ignored. First and foremost, the methodological quality of our included studies was generally poor. The majority of the included trials were rated as “moderate” or “high” bias risk due to insufficient information on randomization process, allocation concealment, and methods of blinding outcome assessors. In particular, double-blinding was not conducted in all of the included studies. When both herbal decoction and WM are used as interventions, it is difficult to perform blinding due to their differences in external characteristics. Moreover, the review found that protocol registration information, quality control and chemical profile were not reported in any of the included studies, which has led to controversial conclusions. Second, despite the fact that sensitivity analysis verified the reliability of our findings, there was substantial heterogeneity in several of them. The clinical diagnosis and treatment of TCM rely on a comprehensive assessment of various factors, including the patient’s symptoms, tongue image, and pulse image, known as syndrome differentiation. Subsequently, treatments are tailored based on the identified TCM syndrome type, indicating that patients with distinct syndromes receive different medications, potentially resulting in heterogeneity. Additionally, the variability in composition and dosage of Chinese herbal medicine, along with diverse outcome indicators, may contribute to further heterogeneity in the study results. Furthermore, the presence of diverse western medicine interventions utilized in the control group constitutes an inherent factor contributing to the observed heterogeneity. Third, it is noteworthy that the studies encompassed within this research were exclusively conducted in China and published solely in the Chinese language. Consequently, the validation of our findings becomes imperative in order to ascertain the applicability of TCM in broader samples, diverse countries, and various ethnic groups. Fourth, Chinese clinical trials have become a relatively standardized, safe procedure in the last decade, and thus strict temporal constraints of the present study was made to uphold the study’s quality standards. However, this selection process led to the exclusion of a considerable number of studies that did not meet the intervention or diagnostic criteria. Thereafter, the insufficient number of included studies hindered the resolution of heterogeneities. Furthermore, a majority of the included studies had small sample sizes, which appeared to be one risk in exaggerating intervention benefits. Last but no the least, there is a dearth of studies that have presented follow-up data on the combination of TCM and WM in the treatment of DACD. Given the chronic and progressive nature of DACD, characterized by potential fluctuations over an extended period, it is imperative to conduct ongoing follow-up assessments to determine the true efficacy and long-term consequences of this therapeutic approach. Regrettably, the majority of studies have been limited by short treatment durations, with none of them encompassing long-term follow-up observations.
4.3 Implications for clinical practice and future research
Over the past dozen years, the integration of TCM and WM therapy is being increasingly investigated for their use in the treatment of DACD. However, the choice of Chinese herbal medicine is empirical and there is a lack of consensus among clinicians. The evidence available from our study demonstrated the effectiveness and safety of CHM therapy for DACD, which is able to offer a comprehensive and transparent framework for promoting clinical practice guidelines. Importantly, extensive and in-depth data mining in applying TCM to the treatment of DACD is conducive to inherit the clinical experience of ancient TCM, boost the understanding of the theory and practice of TCM in DACD treatment and enrich the treatment options for treating DACD. The findings from our study provide evidence supporting the efficacy and safety of the above-mentioned therapy for DACD, thereby offering a comprehensive and transparent framework for the promotion of clinical practice guidelines. Notably, the extensive and thorough study in the application of TCM for DACD treatment facilitates the preservation of ancient TCM clinical experience, enhances the comprehension of TCM theory and practice in DACD treatment, and expands the range of treatment options available for DACD management.
In light of our findings and aforementioned limitations, several recommendations can be made for future research and clinical practice. Firstly, it is recommended that multi-center studies with larger sample sizes be undertaken in order to augment the representativeness and reliability of the findings. Secondly, the efficacy of Traditional Chinese Medicine (TCM) hinges upon the precise differentiation and treatment of the syndrome, thus it is advisable to establish an evaluation system for assessing therapeutic effects that aligns with the distinctive attributes of TCM, and to explore pragmatic and discerning indicators for TCM. Thirdly, investigations pertaining to TCM ought to enhance their protocols and prioritize quality control, with particular emphasis on the meticulous implementation of randomization, blinding, and allocation concealment. We advise designing and reporting RCTs of DACD strictly according to the CONSORT 2010 statement (Schulz et al., 2010) and the CONSORT Extension for Chinese Herbal Medicine Formulas 2017 (Cheng et al., 2017). Fourthly, incorporating an appropriate follow-up period that aligns with the characteristics of the disease, in order to conduct longer-term research and clinical trials to confirm the long-term safety of TCM on DACD, explore the optimal dosage, duration of treatment, and potential adverse events, thereby providing valuable clinical insights. Fifthly, considering the research prospects associated with Chinese herbal medicines in the treatment of diabetes and its diverse complications, clinical and animal experimental studies focusing on the active ingredients of Chinese herbal medicines may elucidate the specific effects and intrinsic mechanisms of treating DACD, which could increase the evidence base for the clinical application of TCM in DACD as well as promote the inclusion of TCM in relevant international guidelines.
5 Conclusion
This systematic review has found some promising evidence for the integration of TCM and WM therapy in the treatment of DACD. Compared to WM alone, the integration of TCM and WM therapy appears to show a more favorable therapeutic effect. Meanwhile, it holds great potential in alleviating blood glucose, improving cognitive function, and reducing inflammation.
However, it is crucial to consider the limitations to the evidence base, notably the low methodological quality and small sample sizes of the included studies. These factors highlight the need for further research into the use of TCM for DACD. Specifically, we urgently need high-quality, multi-center studies with larger samples to strengthen the evidence supporting the clinical use of TCM for DACD. This kind of robust research is essential to guide clinical decision-making and to optimize patient care in the future.
Author contributions
JS: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. GS: Investigation, Methodology, Software, Supervision, Validation, Writing–original draft, Writing–review and editing. JA: Data curation, Investigation, Methodology, Software, Validation, Writing–original draft, Writing–review and editing. YA: Data curation, Formal Analysis, Investigation, Methodology, Writing–review and editing. JL: Data curation, Formal Analysis, Investigation, Methodology, Writing–review and editing. ZS: Investigation, Methodology, Resources, Software, Visualization, Writing–review and editing. LZ: Investigation, Methodology, Resources, Software, Visualization, Writing–review and editing. SZ: Investigation, Methodology, Writing–review and editing. YY: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing–review and editing. YS: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing–review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the National Leading Talents Support Program of Chinese Medicine–Qihuang Scholar [No. (2018)12], Youth Top Talent Grant of “Revitalizing Liaoning Elite Project” of Liaoning Province (No. XLYC1807145).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1280736/full#supplementary-material
References
Aschner, P., Karuranga, S., James, S., Simmons, D., Basit, A., Shaw, J. E., et al. (2021). The International Diabetes Federation's guide for diabetes epidemiological studies. Diabetes Res. Clin. Pract. 172, 108630. doi:10.1016/j.diabres.2020.108630
Banday, M. Z., Sameer, A. S., and Nissar, S. (2020). Pathophysiology of diabetes: an overview. Avicenna J. Med. 10 (4), 174–188. doi:10.4103/ajm.ajm_53_20
Bello-Chavolla, O. Y., Antonio-Villa, N. E., Vargas-Vázquez, A., Ávila-Funes, J. A., and Aguilar-Salinas, C. A. (2019). Pathophysiological mechanisms linking type 2 diabetes and dementia: review of evidence from clinical, translational and epidemiological research. Curr. Diabetes Rev. 15 (6), 456–470. doi:10.2174/1573399815666190129155654
Cai, X. (2016). Effect of tonifying kidney and promoting blood circulation on cognitive function of diabetes. Inn. Mong. J. Tradit. Chin. Med. 35 (11), 14–15. doi:10.16040/j.cnki.cn15-1101.2016.11.015
Chatterjee, S., Peters, S. A., Woodward, M., Mejia Arango, S., Batty, G. D., Beckett, N., et al. (2016). Type 2 diabetes as a risk factor for dementia in women compared with men: a pooled analysis of 2.3 million people comprising more than 100,000 cases of dementia. Diabetes Care 39 (2), 300–307. doi:10.2337/dc15-1588
Chen, R., Shi, J., Yin, Q., Li, X., Sheng, Y., Han, J., et al. (2018). Morphological and pathological characteristics of brain in diabetic encephalopathy. J. Alzheimers Dis. 65 (1), 15–28. doi:10.3233/JAD-180314
Chen, W., Li, J., Huo, L., Xi, Y. J., and Li, L. (2021). Clinical observation of Naoling Decoction in treating diabetic cognitive impairment. J. Guangzhou Univ. Tradit. Chin. Med. 38 (3), 449–454. doi:10.13359/j.cnki.gzxbtcm.2021.03.003
Cheng, C. W., Wu, T. X., Shang, H. C., Li, Y. P., Altman, D. G., Moher, D., et al. (2017). CONSORT extension for Chinese herbal medicine Formulas 2017: recommendations, explanation, and elaboration (traditional Chinese version). Ann. Intern Med. 167 (2), W7–W20. doi:10.7326/IsTranslatedFrom_M172977_1
Chinese Society of Endocrinology (2021). Expert consensus on diabetic cognitive dysfunction. Chin. J. Diabetes Mellit. 13 (7), 678–694. doi:10.3760/cma.j.cn115791-20210527-00291
Chinese Society of Endocrinology (2022). Chinese expert consensus on the prevention and treatment of cognitive dysfunction in type 2 diabetes mellitus. Chin. J. Endocrinol. Metab. 38, 453–464. doi:10.3760/cma.j.cn311282-20220518-00320
Chu, W. M. (2013). Tumor necrosis factor. Cancer Lett. 328 (2), 222–225. doi:10.1016/j.canlet.2012.10.014
Cukierman, T., Gerstein, H. C., and Williamson, J. D. (2005). Cognitive decline and dementia in diabetes--systematic overview of prospective observational studies. Diabetologia 48 (12), 2460–2469. doi:10.1007/s00125-005-0023-4
Datusalia, A. K., and Sharma, S. S. (2016). NF-κB inhibition resolves cognitive deficits in experimental type 2 diabetes mellitus through CREB and glutamate/GABA neurotransmitters pathway. Curr. Neurovasc Res. 13 (1), 22–32. doi:10.2174/1567202612666151030104810
Dong, Y., Sharma, V. K., Chan, B. P., Venketasubramanian, N., Teoh, H. L., Seet, R. C., et al. (2010). The Montreal Cognitive Assessment (MoCA) is superior to the Mini-Mental State Examination (MMSE) for the detection of vascular cognitive impairment after acute stroke. J. Neurol. Sci. 299 (1-2), 15–18. doi:10.1016/j.jns.2010.08.051
Fiatarone Singh, M. A., Gates, N., Saigal, N., Wilson, G. C., Meiklejohn, J., Brodaty, H., et al. (2014). The Study of Mental and Resistance Training (SMART) study—resistance training and/or cognitive training in mild cognitive impairment: a randomized, double-blind, double-sham controlled trial. J. Am. Med. Dir. Assoc. 15 (12), 873–880. doi:10.1016/j.jamda.2014.09.010
Fu, H., Li, W., Wang, H., Yang, J., Chu, S., Hong, J., et al. (2017). Clinical study of Bushen Huoxue Recipe in treating mild cognitive impairment of type 2 diabetes. Chin. J. Int. Med. 37 (6), 661–665. doi:10.7661/j.cjim.20170426.077
Gao, F., Ji, Y., Cao, H., and Wang, H. (2017). Therapeutic effect of nourishing kidney, eliminating dampness and resolving phlegm on vascular mild cognitive impairment secondary to senile diabetes mellitus and its Influence on oxidative stress index and acetylcholinesterase level. Mod J Int Tradit Chin West Med 26 (30), 3324–3327. doi:10.3969/j.issn.1008-8849.2017.30.006
Goldet, G., and Howick, J. (2013). Understanding GRADE: an introduction. J. Evid. Based. Med. 6 (1), 50–54. doi:10.1111/jebm.12018
Gupta, M., Pandey, S., Rumman, M., Singh, B., and Mahdi, A. A. (2022). Molecular mechanisms underlying hyperglycemia associated cognitive decline. IBRO Neurosci. Rep. 14, 57–63. doi:10.1016/j.ibneur.2022.12.006
Hao, X., Yuan, J., and Dong, H. (2019). Salidroside prevents diabetes-induced cognitive impairment via regulating the Rho pathway. Mol. Med. Rep. 19 (1), 678–684. doi:10.3892/mmr.2018.9621
Higgins, J. P., and Thompson, S. G. (2002). Quantifying heterogeneity in a metaanalysis. Stat. Med. 21 (11), 1539–1558. doi:10.1002/sim
Jin, S., Liang, J., Yang, X., Zhao, H., Shi, M., Chen, W., et al. (2015). Clinical study on Bushen Huoxue Kaiqiao Decoction in treating 30 cases of vascular mild cognitive impairment caused by diabetes. World Sci Tech -Mod Tradit Chin. 15 (5), 1051–1055. doi:10.11842/wst.2013.05.051
Khaledi, M., Haghighatdoost, F., Feizi, A., and Aminorroaya, A. (2019). The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. 56 (6), 631–650. doi:10.1007/s00592-019-01295-9
Khosravi, R., Ka, K., Huang, T., Khalili, S., Nguyen, B. H., Nicolau, B., et al. (2013). Tumor necrosis factor- α and interleukin-6: potential interorgan inflammatory mediators contributing to destructive periodontal disease in obesity or metabolic syndrome. Mediat. Inflamm. 2013, 728987. doi:10.1155/2013/728987
Li, H. (2022). Clinical study on yiqiyangyinhuoxue recipe in treatment of diabetic cognitive impairment based on collateral disease theory. Hubei J. Tradit. Chin. Med. 44 (5), 3–5.
Li, K. (2016). Analysis of effect of Self-made Bushen Huoxue Kaiqiao Recipe on improving vascular mild cognitive impairment caused by diabete. J. Clin. Investig. 22 (6), 2.
Li, Q., Jia, T., and Guan, H. (2022). Clinical observation of Dihuang Yinzi in adjuvant treatment of type 2 diabetes with kidney deficiency and myelopenia complicated with mild cognitive impairment. Lishizhen Med. Mat. Med. Res. 38 (2), 410–412. doi:10.3969/j.issn.1008-0805.2022.02.41
Liu, Y., Li, X., Sun, L., and Zhao, L. (2016). Clinical study of Yiqi Bushen Huoxue Recipe in treating 35 cases of mild cognitive impairment of senile diabetes. Chin. Mod. Med. 23 (6), 100–102.
Mao, Y., Bu, X., Liu, C., Chen, Q., and Ma, J. (2019). Therapeutic effect of Yangyi Yizhi decoction combined with nimodipine on mild cognitive impairment in patients with type 2 diabetes. Hunan J. Tradit. Chin. Med. 35 (11), 4–6. doi:10.16808/j.cnki.issn1003-7705.2019.11.002
Marín-Peñalver, J. J., Martín-Timón, I., Sevillano-Collantes, C., and Del Cañizo-Gómez, F. J. (2016). Update on the treatment of type 2 diabetes mellitus. World J. Diabetes 7 (17), 354–395. doi:10.4239/wjd.v7.i17.354
Martínez-Mármol, R., Mohannak, N., Qian, L., Wang, T., Gormal, R. S., Ruitenberg, M. J., et al. (2019). p110δ PI3-kinase inhibition perturbs APP and TNFα trafficking, reduces plaque burden, dampens neuroinflammation, and prevents cognitive decline in an Alzheimer's disease mouse model. J. Neurosci. 39 (40), 7976–7991. doi:10.1523/JNEUROSCI.0674-19.2019
Mauricio, D., Alonso, N., and Gratacòs, M. (2020). Chronic diabetes complications: the need to move beyond classical concepts. Trends Endocrinol. Metab. 31 (4), 287–295. doi:10.1016/j.tem.2020.01.007
Schulz, K. F., Altman, D. G., and Moher, D.CONSORT Group (2010). Statement: updated guidelines for reporting parallel group randomized trials. Ann. Intern. Med. 152 (11), 726–732. doi:10.7326/0003-4819-152-11201006010-00232
Seto, S. W., Yang, G. Y., Kiat, H., Bensoussan, A., Kwan, Y. W., and Chang, D. (2015). Diabetes mellitus, cognitive impairment, and traditional Chinese medicine. Int. J. Endocrinol. 2015, 810439. doi:10.1155/2015/810439
Shi, J. J., Liu, H. F., Hu, T., Gao, X., Zhang, Y. B., Li, W. R., et al. (2021). Danggui-Shaoyao-San improves cognitive impairment through inhibiting O-GlcNAc-modification of estrogen α receptor in female db/db mice. J. Ethnopharmacol. 281, 114562. doi:10.1016/j.jep.2021.114562
Srikanth, V., Sinclair, A. J., Hill-Briggs, F., Moran, C., and Biessels, G. J. (2020). Type 2 diabetes and cognitive dysfunction-towards effective management of both comorbidities. Lancet Diabetes Endocrinol. 8 (6), 535–545. doi:10.1016/S2213-8587(20)30118-2
Stoeckel, L. E., Arvanitakis, Z., Gandy, S., Small, D., Kahn, C. R., Pascual-Leone, A., et al. (2016). Complex mechanisms linking neurocognitive dysfunction to insulin resistance and other metabolic dysfunction. F1000Res 5, 353. doi:10.12688/f1000research.8300.2
Sun, H., Saeedi, P., Karuranga, S., Pinkepank, M., Ogurtsova, K., Duncan, B. B., et al. (2022). IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119. doi:10.1016/j.diabres.2021.109119
Sutherland, G. T., Lim, J., Srikanth, V., and Bruce, D. G. (2017). Epidemiological approaches to understanding the link between type 2 diabetes and dementia. J. Alzheimers Dis. 59 (2), 393–403. doi:10.3233/JAD-161194
Thal, D. R., Grinberg, L. T., and Attems, J. (2012). Vascular dementia: different forms of vessel disorders contribute to the development of dementia in the elderly brain. Exp. Gerontol. 47 (11), 816–824. doi:10.1016/j.exger.2012.05.023
Tian, M., Li, Y., and Chen, Y. (2021). Discussion on the mechanism of Jiaotai Pill combined with oxiracetam in the treatment of diabetic cognitive dysfunction based on intestines-inflammation- brain axis. Mod J Int Tradit Chin West Med 30 (23), 2540–2544. doi:10.3969/j.issn.1008-8849.2021.23.007
Tian, R., Liu, X., Jing, L., Yang, L., Xie, N., Hou, Y., et al. (2022). Huang-Lian-Jie-Du decoction attenuates cognitive dysfunction of rats with type 2 diabetes by regulating autophagy and NLRP3 inflammasome activation. J. Ethnopharmacol. 292, 115196. doi:10.1016/j.jep.2022.115196
Tian, X., Liu, Y., Ren, G., Yin, L., Liang, X., Geng, T., et al. (2016). Resveratrol limits diabetes-associated cognitive decline in rats by preventing oxidative stress and inflammation and modulating hippocampal structural synaptic plasticity. Brain Res. 1650, 1–9. doi:10.1016/j.brainres.2016.08.032
Wang, K., Zhao, L., and Zhang, H. (2016). Effect of Bushen Yiq Huoxue decoction on recent memory ability and brain evoked potential in patients with type 2 diabetes and cerebral dysfunction. Mod J Int Tradit Chin West Med 25 (29), 3215–3217+3266. doi:10.3969/j.issn.1008-8849.2016.29.008
Wang, X. (2015). The effect of traditional Chinese medicine on mild cognitive impairment in diabetes. Cardiovasc. Dis J Int Tradit Chin West Med 3 (28), 78–79. doi:10.16282/j.cnki.cn11-9336/r.2015.28.046
Wang, Y., Jin, W., Liu, L., and Li, Z. (2015). Clinical analysis of bushen Huoxue decoction in treating cognition impairment of diabetes. Chin. J. Exp. Tradit. Med. Form. 21 (9), 196–199. doi:10.13422/j.cnki.syfjx.2015090196
Yan, X., and Guan, H. (2019). Effect of Yizhi heji on elderly patients with type 2 diabetes mellitus complicated with cognitive dysfunction. Guid J. Tradit. Chin. Med. Pharm. 25 (14), 97–100. doi:10.13862/j.cnki.cn43-1446/r.2019.14.030
Yang, F. (2017). Clinical observation of Shenqi Yizhi Jiannao Recipe on mild cognitive impairment in type 2 diabetes. Master degree [Master thesis]. Nanjing: Nanjing University of Chinese Medicine.
Yang, J., Zhang, Z., Li, J., Tian, X., and Li, L. (2021). Study on influencing factors and distribution characteristics of TCM syndromes in patients with type 2 diabetes mellitus with cognitive dysfunction. Chin J Int Med Cardio-/Cerebrovascuiar Dis. 19 (17), 2917–2920. doi:10.12102/j.issn.1672-1349.2021.17.008
Yu, J. (2018). Clinical effective observation on treating cognitive dysfunction in patients with elderly type 2 diabetes with the Xuefu Zhuyu decoction. Clin. J. Chin. Med. 10 (34), 86–88. doi:10.3969/j.issn.1674-7860.2018.34.033
Yu, J., Xia, W., Chen, Q., Xia, W., and Liu, C. (2022). Bushen Jianpi Huoxue Formula in effect on type 2 diabetic elderly patients with mild cognitive impairment of deficiency of spleen and kidney and blood stasis. Hebei J. Chin. Med. 44 (8), 1282–1286. doi:10.3969/j.issn.1002-2619.2022.08.011
Zhang, W. (2016). Clinical study of Yizhi Mixture in the treatment of senile type 2 diabetes complicated with cognitive impairment. Master degree [Master thesis]. Jinan: Shandong University of Traditional Chinses Medicine.
Zhao, H., Guo, Q., Yang, D., and Shi, M. (2014). Prescription for tonifying kidney, activating blood, and resuscitation in treatment of vascular mild cognitive impairment caused by diabetes: a clinical study of eight cases. Hunan J. Tradit. Chin. Med. 30 (23), 6–8. doi:10.16808/j.cnki.issn1003-7705.2014.12.003
Keywords: diabetes-associated cognitive decline, traditional Chinese medicine, meta-analysis, systematic review, grade evaluation
Citation: Su J, Sun G, An J, Ao Y, Li J, Shen Z, Zhang L, Zhang S, Yang Y and Shi Y (2023) Efficacy and safety of the integration of traditional Chinese medicine and western medicine in the treatment of diabetes-associated cognitive decline: a systematic review and meta-analysis. Front. Pharmacol. 14:1280736. doi: 10.3389/fphar.2023.1280736
Received: 23 August 2023; Accepted: 07 November 2023;
Published: 22 November 2023.
Edited by:
Guanhu Yang, Ohio University, United StatesReviewed by:
Songpeng Guo, Independent Researcher, Luzern, SwitzerlandJieying Zhang, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, China
Copyright © 2023 Su, Sun, An, Ao, Li, Shen, Zhang, Zhang, Yang and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yufeng Yang, bG50Y215eWZAMTI2LmNvbQ==; Yan Shi, bG50Y21zaGl5YW5AMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Jianan Su
Jianan Su Guiyan Sun1†
Guiyan Sun1† Jiren An
Jiren An Jing Li
Jing Li Yan Shi
Yan Shi